5 free worksheets for people struggling with OCD, developed by experts
By Elle Warren
• Clinically reviewed by April Kilduff, MA, LCPC
Dec 1, 2023 • 6 min read minute read
Reviewed by April Kilduff, MA, LCPC
There are a multitude of barriers to accessing mental healthcare. Whether it’s financial, insurance-related, time, or motivation, you may find yourself unable to immediately access treatment for OCD.
If you are experiencing those barriers, or if you just want a supplement to your treatment with some extra “homework,” we have resources for you. Putting your thoughts and experiences down on paper can be valuable for any mental health struggle—especially for highly behavioral conditions like OCD—so we’ve compiled 5 OCD worksheets developed with the help of leading experts in OCD treatment.
These worksheets focus on support systems, mental compulsions, taboo thoughts, relationship OCD: cognitive distortions & compulsions, and identifying your core fear(s).
Each worksheet also has a linked video that will explain and guide you through it. We recommend watching those before you begin, and following along in the worksheet.

Worksheet #1: Support Systems
This worksheet focuses on the importance of having support systems in OCD recovery, as well as the different forms support can take. Dr. Nicholas Farrell , Regional Clinical Director at NOCD, says support systems can be “very important to the recovery journey.”
When you’re facing the challenging but rewarding work of OCD recovery, it’s beneficial to have people in your life to encourage you and hold you accountable. This is true for most challenges in life, and mental health is no exception.
Moreover, it’s important for the people closest to you to understand your condition and treatment. If they don’t have an understanding of how your OCD shows up, and how you can get better, they may be more likely to engage in enabling behaviors that help keep you stuck.
This worksheet will ask you to reflect on the ways you receive emotional, tangible, informational, and social support. If you are lacking support in any of those areas, you can brainstorm ways to seek or ask for support.
There is also a section for you to reflect on the ways your loved ones have provided reassurance to you when you compulsively ask for it. It prompts you to instead reflect on how your loved ones could provide validation without the reassurance.
Follow along with the video guide for our Support Systems worksheet here.
Worksheet #2: Mental Compulsions
This worksheet offers education around mental compulsions, which are any internal actions done to relieve the distress of your intrusive thoughts & triggers.
Dr. Farrell says it’s important for people to know about mental compulsions because, naturally, “they tend to be hidden.” Outside of describing your experience to a mental health professional, you’re really the only one who can identify or notice them.
You will learn about three primary categories of mental compulsions:
- Mental review/rumination
- Thought neutralizing, blocking, or distracting
- Self-reassurance
You will reflect on what mental compulsions you engage in, which thoughts, feelings, and uncertainties you’re trying to avoid by doing them, and how you can prioritize long-term recovery over short-term relief (which is all that compulsions can provide).
Follow along with the video guide for our Mental Compulsions worksheet here.
We can help you tackle your intrusive thoughts, no matter what they are
Worksheet #3: Taboo Thoughts
This worksheet talks about a very common thread among OCD themes and intrusive thoughts: they can be taboo, inappropriate, or deeply uncomfortable in nature.
Some of the more taboo themes include harm OCD , pedophilia OCD , and sexual orientation OCD . While these can feel deeply shameful, Dr. Farrell stresses the “universal nature” of intrusive thoughts.
You might feel like you’re the only one who has ever had these thoughts, but in fact, there are decades of research that point to the contrary. Dr. Farrell likes to show clients this research about the prevalence of all sorts of intrusive thought themes, among those with and without OCD.
You will learn that intrusive thoughts are ego-dystonic, meaning they don’t align with the sufferer’s values, beliefs, or morals. You will then be asked to reflect on how you judge yourself and your intrusive thoughts—how do you label them in your head?
You will be guided in speaking to yourself as you would a friend. Would you tell your friend with these uncontrollable thoughts that they are shameful, disgusting, or bad? It’s highly unlikely that you would. This worksheet will help you practice not speaking to yourself that way, either.
Follow along with the video guide on Taboo Intrusive Thoughts here.
Worksheet #4: Relationship OCD: Cognitive distortions & compulsions
This worksheet focuses first on cognitive distortions that people often engage in when they’re struggling with relationship OCD, though the information can equally be applied to other themes, too.
Cognitive distortions are tricks that OCD plays on us. Dr. Farrell describes them as “thinking errors.” They include:
- All-or-nothing thinking ( My relationship has to be perfect otherwise we should break up )
- Catastrophizing ( If I can’t be 100% certain about our relationship right now, I’m going to ruin my life in the future )
- Selective abstraction ( My partner always gets stains on their clothes—can I live with that forever? )
- Mind reading ( Other people probably think we’re bad for each other )
- Hyper-responsibility ( If we don’t work out, I could be holding them back from meeting the right person, and it’ll all be my fault )
You’ll reflect on how cognitive distortions show up for you, then learn about common compulsions that people with relationship OCD engage in, such as constant “checking” of your feelings and attraction , “confessing” your intrusive thoughts because you feel so guilty, or seeking reassurance about your relationship (“we’re not going to break up, right?”).
You will then think how you can challenge both your cognitive distortions and compulsions to accept uncertainty and discomfort.
Follow along with the video guide on Cognitive Distortions in Relationship OCD here.
Worksheet #5: Core fears
The goal of this worksheet is to understand any “core fears” that are involved in your obsessions. As such, you will begin by learning more about obsessions—those repetitive, intrusive thoughts that often show up as “what ifs” and threaten our perception of safety.
After you get specific about your obsessions, you will learn more about the many faces of compulsions. Compulsions can show up in a million ways, and be mental (internal) or physical (external), but you will review a list of examples.
Finally, you will walk through the “downward arrow” exercise. You will start with your surface-level obsession ( what if I run over someone with my car? ) and then answer the question of, “If that came true, then…” until you get to the fundamental fear that causes you such distress. Perhaps the root is that you could be an evil person. Maybe it’s that you don’t have control over your impact on others.
Regardless, identifying your core fear allows you to get more specific about how you can face your fears—and at the end of the worksheet, you’ll brainstorm ways to do just that.
Follow along with the video guide on Core Fears here.
Get your life back from OCD
Use the OCD recovery tools at your disposal
Self-reflection and awareness is crucial to OCD recovery, but it can also be draining. Be patient and compassionate with yourself. You don’t have to do these all at once. If it feels overwhelming, you can do just one per day or even one per week, and really sit with each concept. Hopefully, you learn something new about OCD and about your unique experience of it.
If you want to give yourself the best chance at conquering OCD, please know that specialized, evidence-based therapy is available to you. The effectiveness of exposure and response prevention (ERP) therapy has been proven by decades of rigorous research, and it’s more accessible today than ever before.
Here at NOCD, every therapist receives intensive training in ERP, and we accept most major insurance plans to help you get started. If you’re ready to regain control of your life for OCD, I strongly encourage you to learn more about NOCD’s specialized approach to OCD treatment.
We specialize in treating OCD
Reach out to us. We're here to help.
Join our Newsletter
Get helpful tips and the latest information
CBT for OCD: How It Works, Examples & Effectiveness
Author: Sidney Deupree, MA, LPC, NCC
Sidney Deupree MA, LPC, NCC
Sidney a licensed professional counselor specializing in CBT for children, adolescents, and young adults.
Naveed Saleh MD, MS
Dr. Saleh is an experienced physician and a leading voice in medical journalism. His contributions to evidence-based mental health sites have helped raise awareness and reduce stigma associated with mental health disorders.
Cognitive behavioral therapy (CBT) for OCD helps people change problematic behaviors, thoughts, and emotions. CBT generally consists of weekly, one-hour therapy sessions lasting approximately six months, depending on the severity of someone’s OCD symptoms. Participants should practice what they learn outside of the therapy session to get the most benefit. Most people who receive CBT for OCD start noticing improvements within weeks.
Why NOCD for OCD? 9 in 10 People Show Improvement
NOCD Therapy is clinically proven to reduce OCD symptoms in over 90% of members. Our licensed ERP-trained therapists help you get better, we have 24/7 support to make sure you stay better, and we’re covered by many insurance plans.
How Does CBT for OCD Work?
People with obsessive-compulsive disorder (OCD) engage in specific compulsions to experience temporary relief from the obsessive thoughts that cause them severe distress. CBT for OCD works to break the automatic bond between obsessive thought and ritualistic compulsive behavior. CBT also trains the person to avoid ritualizing when they’re feeling anxious. 2
Cognitive behavioral therapy (CBT) focuses on the interconnected nature of thoughts, feelings, and behaviors. CBT suggests that problems in one area (your thoughts, feelings, or behaviors) can be fixed by making changes in other areas. By changing thought patterns and behavioral habits, CBT can improve negative feelings.
Are There Any Risks?
There are no specific risks of CBT for OCD, with the exception that it may not be effective for everyone. 10 CBT, when compared with no treatment, does effectively decrease the severity of OCD symptoms. In addition, CBT also improved the overall level of functioning and reduced the risk associated with OCD. 10
How Long Will CBT Take?
The standard treatment model of CBT for OCD is about 12 weeks with one hour-long session per week. However, CBT’s effectiveness can take time depending on other mental health issues the individual is dealing with or other traumatic histories. The key to success in therapy is trust between the therapist and the client and willingness to follow through on homework and directives. 11
10 CBT Techniques for OCD
The CBT techniques used to treat OCD include a variety of therapeutic modalities and subtypes of CBT, along with relaxation exercises like deep breathing and progressive muscle relaxation. We’ve included a CBT worksheet to help you learn cognitive restructuring for OCD.
Here are 10 CBT techniques commonly used to treat OCD:
1.Cognitive Restructuring
Cognitive restructuring involves challenging irrational thoughts or thinking patterns and replacing them with rational thoughts. The aim is to use facts to challenge thoughts based on emotional responses. Try using the worksheet below to reframe your thoughts.
Free Cognitive Restructuring for OCD Worksheet
Cognitive restructuring can help challenge and change the intrusive thoughts that lead to compulsive behaviors.
2. Exposure & Response Prevention Therapy (ERP)
Perhaps the most helpful CBT tool for treating OCD is exposure and response prevention therapy (ERP) . The ERP for OCD process involves exposing the patient to stress-inducing obsessive thoughts without allowing them to engage in the compulsive behavior. Doing so prevents them from experiencing the temporary relief associated with the compulsion and forces them to face their anxiety until the anxiety fades and they become desensitized to it. ERP is the most common treatment for OCD.
Components of ERP include: 2
- In vivo exposure: “Real-life exposure” in which someone is repeatedly placed in the presence of a feared stimulus over a prolonged period
- Imaginal exposure: The mental visualization of a feared stimulus and the consequences of being exposed to the stimulus
- Ritual or response prevention: Refraining from the ritualistic behavior after having been exposed to the feared stimulus
3. Inference-Based CBT
Inference-based CBT (I-CBT) is a treatment specially designed for OCD.12 Through I-CBT, the person with OCD learns the connection between obsessive doubts and the creation of faulty reasonings. I-CBT assumes that people with OCD confuse reality with imagination when they are distressed. Through therapy, they learn to practice alternative narratives that are grounded in common sense rather than obsessional doubts.
It is important to point out that I-CBT does not challenge the content of obsessional doubts. Instead, it challenges the doubting process. I-CBT assumes that it is the faulty reasoning or doubting process that keeps OCD symptoms around. Without the doubting process, the idea is that OCD symptoms will subside.
4. Deep Breathing Exercises
Breathwork exercises are exceptionally helpful for managing anxiety related to OCD. Although there are many different types of deep breathing exercises, they all work by slowing down the breath and heart rate, creating a calming effect.
5. Progressive Muscle Relaxation
Progressive muscle relaxation is a process that allows the person to tighten and release tension throughout their body physically. When we are stressed or anxious, our bodies can enter into the fight-or-flight response , often leading to tension. Training the body to disengage from this response is an essential component of stress management.
6. ABC Analysis
The ABC method of CBT is similar to cognitive restructuring and can help people challenge irrational thoughts and develop more rational thinking styles. ABC Analysis helps people break down a problem into smaller parts called antecedents (A), behaviors (B), and consequences (C). Through analyzing these parts, people can examine how their beliefs (B) affect their reactions (C) to the trigger (A). Through repetition, people can understand how to challenge and examine their irrational beliefs to produce better consequences.
7. Journaling
Traditional methods of journaling for CBT use a thought diary, which helps people mindfully track and process emotional experiences. Thought diaries typically break down emotional experiences into triggers, thoughts, emotions, physical sensations, and behaviors. Journaling encourages the person to slow down the space between intrusive thoughts and compulsive behaviors. Through journaling, people with OCD can approach each thought with objectivity and openness. You can use a traditional notebook and pen or try a CBT app like Clarity for thought journaling.
8. Mindfulness
Mindfulness encourages people to nonjudgmentally live in the present moment. Mindfulness is helpful for treating OCD because it helps people understand the difference between the content of the intrusive thought and the meaning attached to the thought. Once someone is able to separate the meaning attached to the thought from the intrusive thought itself, they can gain insight into stopping the compulsive cycle of OCD.
9. Activity Scheduling
The basic premise of activity scheduling is that pleasurable activities contribute to an elevated mood. People with OCD are prone to feelings of anxiety and depression, which may lead to isolation. Activity scheduling encourages the person with OCD to re-engage with hobbies, supportive people, and forms of movement. Regularly participating in these activities may also help discourage agoraphobia , another condition associated with OCD.
10. Worst & Best Case Scenario
Exploring scenarios gently exposes the person to their feared outcome, while also making room for other possible outcomes. Exploring the worst scenario is important for OCD because it exposes the person to the distress of their intrusive thoughts, which over time decreases anxiety around intrusive thoughts. When exploring the best case scenario, the person learns that their intrusive thoughts will always pull them toward negative and unlikely scenarios.
What is the best therapy for OCD?
Exposure And Response Prevention Therapy (ERP) – Do live video sessions with a therapist specialized in ERP, the gold standard treatment for OCD. Treatment from NOCD is covered by many insurance plans. Start With A Free 15 Minute Call
Examples of Cognitive Behavioral Therapy for OCD
Obsessions with or without compulsions characterize obsessive-compulsive disorder. The obsessions and compulsions related to OCD are irrational and highly distressing, and significantly impact a person’s quality of life. 3
Here are a few examples of the way OCD manifests differently and the treatment plan for OCD using CBT in each situation:
CBT for Fear of Germs & Illness Anxiety
Angie, a 46-year-old stay-at-home mom, constantly worries about falling ill and being unable to care for her children. Her fear is likely contamination OCD , and it drives her to take extreme precautions to avoid exposing herself to germs. She spends hours every day disinfecting her home while her children are at school. Any time she comes into contact with surfaces she believes are unclean, she feels compelled to immediately shower or wash her hands. Because of her excessive hand-washing, she has extremely dry, red, chapped, and cracked skin on her hands and arms.
The therapist will explore early experiences related to illness, cleanliness, and availability and health of caregivers when Angie was ill. They will determine when these obsessive thoughts began and what was happening at that time, discussing Angie’s perceived benefits of these obsessive thoughts and what she gets out of them.
Then, the therapist will use exposure to a used utensil or item and identify Angie’s intrusive thoughts. They will work to challenge these thoughts, using concrete reasons to understand how her behavior is detrimental (i.e., losing hours in a day, dry and damaged hands). Angie will work to understand these real consequences versus the perceived benefits of her compulsions, using these new thought patterns to guide behaviors moving forward.
CBT for Constant Checking
Tony recently moved into his first apartment on his own, is starting college, and lives with checking OCD behaviors. Before he leaves his apartment, he checks the stove to make sure it is turned off. He then walks to the bathroom and checks that the water is not running in the sink. He turns the water on and off making sure the handle is turned all the way to the off position. He does this eight times. He then returns to check the stove again, ensuring that it is turned off. He goes out his front door and locks it. He immediately worries that the stove is on and returns two more times to check it. He locks his front door and twists the handle eight times ensuring that it is locked and won’t open.
The therapist will role play Tony’s routine of leaving his apartment and challenge him to not recheck something, helping to identify intrusive thoughts. The therapist will explore with Tony why he questions himself and dissect these thoughts to reprogram them so he can challenge them as they arise. Tony and his therapist will work through what is found when uncovering the underlying issues related to these obsessive thoughts and coping methods to move forward without obsession.
CBT for Harm OCD
Sam is a freshman in high school. She fears that if she touches a person first that they will somehow come to serious harm. Because of this fear, she avoids social interactions and physical touch. If she accidentally touches someone she believes that the only way to prevent them from being hurt is to hurt herself. She carries a razor blade with her at all times and makes small cuts to her arms and legs whenever she is unsuccessful in avoiding contact.
The therapist will explore where these fears come from, when they started, and what occurred in her childhood that could be a contributing factor to her harm OCD . They will also discuss when this started and a history of her physical encounters beforehand to get an understanding of any history of trauma.
The therapist will discuss the likelihood of an accidental bump causing harm to another and Sam’s current perceived benefits of self-harm. The therapist will role play with Sam in sessions to identify intrusive thoughts and potentially uncover any underlying depression, anxiety, post-traumatic stress disorder (PTSD), or another mental health issue that may be a contributing factor, as well as an assessment of her home situation. Sam will work to challenge these behaviors and keep a log of when these thoughts begin, where she is, and what her response is, and she will continue to keep a thoughts journal that she brings to therapy to work through.
The therapist may also work with Sam to come up with a hierarchy of anxieties and gradually work their way through them through exposure. Doing graduated exposure can help Sam learn that she can tolerate not knowing what will happen as well as the discomfort associated with the thoughts, without performing compulsions such as cutting herself.
Is Cognitive Behavioral Therapy for OCD Effective?
Cognitive behavioral therapy has been proven to help thousands of people learn to manage obsessive compulsive disorder. In fact, ERP (a subset of CBT) is one of the only proven methods for effectively treating OCD. 4 Research shows that as many as 75% of patients who seek ERP as treatment for OCD find it to be effective in treating the disorder. 5
Here are some statistics regarding the effectiveness of CBT for OCD:
- In a randomized control trial comparing CBT and EMDR , it was found that both were statistically significant in improving OCD symptoms post-study and at a follow up six-month mark. 6
- In a study aimed at adults aged 18 years or older with OCD living in England, it was found that a 12-week course of group CBT led to improvements in OCD and co-occurring depression . 7
- In another study aimed at the use of CBT after deep brain stimulation (DBS) for those with severe OCD, CBT was found to be effective in conjunction with DBS for severe OCD symptom management and treatment. 8
- In another study of CBT for OCD, it was found that even virtual CBT interventions over a 10 week period yielded improvements of both depression symptoms and quality of life, as well as decrease of overall OCD symptoms. 9
Treatment for OCD
NOCD: Online OCD Treatment Covered by Insurance – Regain your life from OCD. Do live video sessions with a licensed therapist specialized in treating OCD. Treatment from NOCD is covered by most major insurance plans. Learn how you can use your insurance benefits. Visit NOCD
Talkiatry: Is OCD Medication Right for You? Speak with a Doctor – Talkiatry can match you with a psychiatrist who takes your insurance and is accepting new patients. They’re in-network with major insurers and offer medication management with supportive therapy. Free Assessment
How to Get the Most Out of CBT for OCD
CBT is a great option for OCD treatment, but not everyone will experience the same benefits.
Here are several tips to maximize the impacts of CBT for OCD:
- Acknowledge the impacts of OCD: Some people struggle to acknowledge the negative aspects of OCD. Be sure to review the harmful and damaging effects of OCD on your life and others.
- Explore a range of treatment levels: Standard outpatient treatment may not offer enough assistance, so intensive outpatient, partial hospitalization, or inpatient setting could be a better fit.
- Explore a range of treatment modalities: Similarly, individual therapy may be helpful, but perhaps family or group sessions offer greater benefit.
- Do your homework: Often, CBT for OCD uses homework to extend treatment between appointments. Being engaged in sessions and completing this homework will help accomplish treatment goals even faster.
- Trust your team: CBT for OCD may seem uncomfortable or too challenging, so having trust in your treatment team is essential. Without trust, it could be too scary to attempt the interventions.
How to Find a CBT Therapist
Many therapists are certified to practice cognitive behavioral therapy, so it shouldn’t be too difficult to find one in your area. An easy way to find a therapist is by using an local therapist directory , as it allows you to narrow your search by location, type of therapy, and whether or not they offer CBT online.
Finding Online CBT for OCD
CBT is one of the most widely-available treatments in-person and online. Trying online CBT can provide a person with great benefits from the comfort of their home. If you don’t have mental health insurance coverage, or simply want to try online CBT, online-therapy.com is an affordable option.
NOCD: Online OCD Treatment Covered By Insurance
Regain your life from OCD. Do live video sessions with a licensed therapist specialized in treating OCD. Treatment from NOCD is covered by most major insurance plans. Learn how you can use your insurance benefits.
At-Home CBT Exercises for OCD
While it is important to have the guidance of a qualified CBT therapist when starting treatment for OCD, you can also practice CBT for OCD at home on your own to help manage symptoms.
Here are some CBT exercises you can do at home to help with OCD symptoms:
Deep Breathing Exercise
There are an abundance of simple deep breathing exercises that can be performed at home.
Here’s a deep breathing exercise you can try when you’re feeling anxious:
- Breathe in through your nose for 5 seconds
- Hold your breath in your lungs for 5 seconds
- Breathe out through your mouth for 5 seconds
Grounding Exercise
While a grounding exercise can be done to stay focused on the present by seeking out sensory inputs in your current environment, this imagery-guided grounding exercise can also be used as a way to calm anxiety:
To begin, think of a place you find comforting: Somewhere in your house, a favorite spot in the park, a beach, or a memory from your childhood. Now spend 5-10 minutes visualizing this place that you have conjured in your mind.
Use your five senses to help you:
- What do you see? Look around and take in your surroundings in this space. What can you see in the distance? What do you see close to you? Try to notice small details that you might normally miss.
- What do you hear? Listen closely to the noises around you. Are the noises you hear soft or loud? Do they sound close by or far away?
- What do you taste? Are you eating or drinking something? If so, what does it taste like? Is it sweet or savory?
- What can you feel? Is it warm or cool? Is there a breeze? Is the sun shining on you warming your skin? Or are you bundled up in a soft blanket?
- What can you smell? What does the air smell like here? Is the scent strong or faint? Do you smell any flowers, or a scent wafting from your beverage?
Use this exercise to relax your mind when you are feeling anxious or stressed. Spend as long as you need visualizing your comfortable space. Allow yourself to feel calm and safe.
Exposure Therapy
While intensive exposure therapy for OCD should be done with a trained professional, you can practice exposure at home under the right conditions. To do so, simply deny acting on your compulsive behavior that provides you temporary relief from the anxiety felt in relation to obsessive thoughts.
The longer you are able to deny the compulsion, the more likely it is that the anxiety will begin to ebb. Continue doing so until the anxiety is gone. Repeat this practice each time you feel the need to engage in compulsive behavior. You can combine this practice with a deep-breathing or grounding exercise to lessen the anxiety you might feel when denying the compulsion.
Many therapy apps incorporate CBT techniques to help people cope with OCD symptoms. Sanvello , Happify or Wysa can help you practice CBT techniques between therapy sessions.
In My Experience
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy .
Randall C. Wyatt, PhD and Erika L. Seid, MA. Cognitive Behavioral Therapy with Donald Meichenbaum, PHD. Retrieved from: https://www.psychotherapy.net/video/meichenbaum-cognitive-behavioral-therapy
Understanding CBT for OCD. Center for the Treatment and Study of Anxiety, University of Pennsylvania. Retrieved from: https://www.med.upenn.edu/ctsa/forms_ocd_cbt.html
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
Cognitive Behavior Therapy, 2019. BeyondOCD.org. Retrieved from: https://beyondocd.org/information-for-individuals/cognitive-behavior-therapy
What is Cognitive Behavioural Therapy (CBT)? OCDUK.org. Retrieved from: https://www.ocduk.org/overcoming-ocd/cognitive-behavioural-therapy/
Marsden, Z., Lovell, K., Blore, D., Ali, S., & Delgadillo, J. (2018). A randomized controlled trial comparing EMDR and CBT for obsessive–compulsive disorder. Clinical psychology & psychotherapy, 25(1), e10-e18.
Papageorgiou, C., Carlile, K., Thorgaard, S., Waring, H., Haslam, J., Horne, L., & Wells, A. (2018). Group cognitive-behavior therapy or group metacognitive therapy for obsessive-compulsive disorder? benchmarking and comparative effectiveness in a routine clinical service. Frontiers in psychology, 9, 2551.
Görmezoğlu, M., Bouwens van der Vlis, T., Schruers, K., Ackermans, L., Polosan, M., & Leentjens, A. F. (2020). Effectiveness, timing and procedural aspects of cognitive behavioral therapy after deep brain stimulation for therapy-resistant obsessive compulsive disorder: A systematic review. Journal of clinical medicine, 9(8), 2383.
Patel, S. R., Wheaton, M. G., Andersson, E., Rück, C., Schmidt, A. B., La Lima, C. N., … & Simpson, H. B. (2018). Acceptability, feasibility, and effectiveness of internet-based cognitive-behavioral therapy for obsessive-compulsive disorder in New York. Behavior therapy, 49(4), 631-641.
Uhre, C. F., Uhre, V. F., Lønfeldt, N. N., Pretzmann, L., Vangkilde, S., Plessen, K. J., … & Pagsberg, A. K. (2020). Systematic review and meta-analysis: cognitive-behavioral therapy for obsessive-compulsive disorder in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 59(1), 64-77.
Osborne, D., Meyer, D., Moulding, R., Kyrios, M., Bailey, E., & Nedeljkovic, M. (2019). Cost-effectiveness of internet-based cognitive-behavioural therapy for obsessive-compulsive disorder. Internet interventions, 18, 100277.
We regularly update the articles on ChoosingTherapy.com to ensure we continue to reflect scientific consensus on the topics we cover, to incorporate new research into our articles, and to better answer our audience’s questions. When our content undergoes a significant revision, we summarize the changes that were made and the date on which they occurred. We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here .
Your Voice Matters
Can't find what you're looking for.
Request an article! Tell ChoosingTherapy.com’s editorial team what questions you have about mental health, emotional wellness, relationships, and parenting. The therapists who write for us love answering your questions!
Leave your feedback for our editors.
Share your feedback on this article with our editors. If there’s something we missed or something we could improve on, we’d love to hear it.
Our writers and editors love compliments, too. :)
Frequently Asked Questions
How much does cbt cost.
CBT for OCD is typically covered by insurance. While most insurances cover CBT, there is still usually a copay for mental health services, which can range between $10 and $100 or more depending on the insurance provider.
Out-of-network providers or those who do not accept insurance may charge anywhere from $80 to $200 per CBT session, which is similar to the cost of therapy in general. If the cost is a concern, ask about sliding scale options.
Additional Resources
To help our readers take the next step in their mental health journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy is compensated for marketing by the companies included below.
OCD Therapy
NOCD: Effective, Affordable, & Convenient OCD Therapy Do live, face-to-face video sessions with a therapist who specializes in treating OCD and get 24/7 support between sessions. NOCD is covered by many insurance plans and is available nationwide. Visit NOCD
Treatment from an Online Psychiatrist
Talkiatry OCD is treatable. Talkiatry specializes in OCD and provides personalized care with medication and additional support. Get started with a short assessment.
OCD Community - Free to Join!
Join others who are overcoming OCD. Participate anonymously. Find support, connect, and overcome challenges with us. The community is managed by NOCD. Join The Community
OCD Newsletter
A free newsletter from Choosing Therapy for those impacted by OCD. Get helpful tips and the latest information. Sign-Up
What to know when finding a therapist for OCD
With so much information out there regarding providers and treatment options for obsessive compulsive disorder, it can be hard to know exactly where to start—especially when you have to consider everything from the type of provider to the different treatment methods, as well as how you’ll fit it into your busy schedule.
Can OCD make it hard to make decisions?
From choosing what to wear in the morning to picking what to eat for dinner, decision-making is a part of everyone’s daily routine. But for millions of people with Obsessive-Compulsive Disorder (OCD), making any choice can feel like a daunting, sometimes impossible task.
CBT for OCD Infographics
A free newsletter for those impacted by OCD. Get helpful tips and the latest information.
FOR IMMEDIATE HELP CALL:
Medical Emergency: 911
Suicide Hotline: 988
© 2024 Choosing Therapy, Inc. All rights reserved.
Obsessive Compulsive Disorder (OCD) including Body Dysmorphic Disorder (BDD)
.st0{fill:none;stroke:#000;stroke-width:2;stroke-linecap:round;stroke-linejoin:round;stroke-miterlimit:10} filter.

Resource type
Therapy tool.

Cognitive Distortions – Unhelpful Thinking Styles (Extended)
Information handouts

Cognitive Distortions – Unhelpful Thinking Styles (Common)

Therapy Blueprint (Universal)

Embracing Uncertainty

Insufficient Self-Control

Intolerance Of Uncertainty

Obsessive Compulsive Disorder (OCD) Formulation
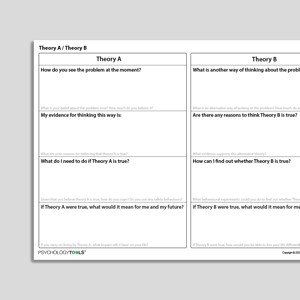
Theory A / Theory B

Unhelpful Thinking Styles (Archived)

Punitiveness

Social Isolation

Behavioral Experiment (Portrait Format)

Subjugation

Exposure And Response Prevention
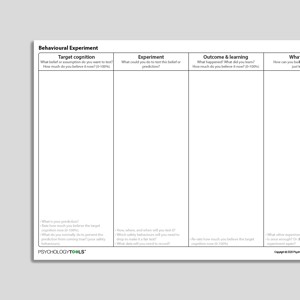
Behavioral Experiment

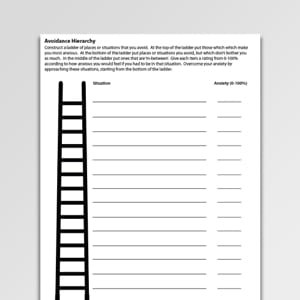
Fear Ladder

Intrusive Thoughts Images And Impulses

Failure To Achieve

Habituation

Understanding Obsessive Compulsive Disorder (OCD)

Emotional Inhibition

What Keeps Obsessive Compulsive Disorder (OCD) Going?

Catastrophizing

Exposure Session Record

OCD Hierarchy

Thought-Action Fusion

Defectiveness

Treating Your OCD With Exposure And Response (Ritual) Prevention (Second Edition): Workbook
Treatments That Work™

Thought Suppression And Intrusive Thoughts

"Should" Statements

Emotional Reasoning

Dependence / Incompetence


Cognitive Behavioral Model Of Intolerance Of Uncertainty And Generalized Anxiety Disorder Symptoms (Hebert, Dugas, 2019)

Approval-/Admiration-Seeking

Exposure Practice Form

Self-Monitoring Record (Universal)

Checking Certainty And Doubt

Cognitive Behavioral Treatment of Childhood OCD: It's Only a False Alarm: Workbook

Your Stone Age Brain

Uncertainty Beliefs – Experiment Record

Therapy Blueprint For OCD

Recognizing Obsessive Compulsive Disorder (OCD)

Exposure And Response (Ritual) Prevention For Obsessive Compulsive Disorder (Second Edition): Therapist Guide

What Is Exposure Therapy?

Intrusion Record

Maximizing The Effectiveness Of Exposure Therapy

Cognitive Behavioral Treatment Of Childhood OCD: It's Only A False Alarm: Therapist Guide

Intrusive Memory Record

Disqualifying The Positive

Facing Your Fears And Phobias

Understanding Body Dysmorphic Disorder

What Keeps Body Dysmorphic Disorder (BDD) Going?

Urges – Self-Monitoring Record
Avoidance Hierarchy (Archived)
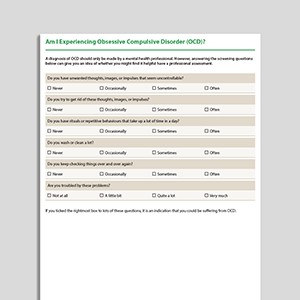
Am I Experiencing Obsessive Compulsive Disorder (OCD)?

Jumping To Conclusions

Personalizing
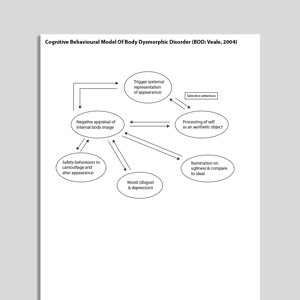
Cognitive Behavioral Model Of Body Dysmorphic Disorder (BDD: Veale, 2004)

What Is Body Dysmorphic Disorder (BDD)?
Links to external resources.
Psychology Tools makes every effort to check external links and review their content. However, we are not responsible for the quality or content of external links and cannot guarantee that these links will work all of the time.
- Scale Download Primary Link Archived Link
- Obsessive Compulsive Cognition Working Group. (2001). Development and initial validation of the Obsessive Beliefs Questionnaire and the Interpretation of Intrusions Inventory. Behaviour Research and Therapy, 39, 987–1006.
- Obsessive Compulsive Inventory (OCI) scoring grid Download Primary Link
- Relationship Obsessive Compulsive Inventory (ROCI) Download Primary Link Archived Link
- Partner Related Obsessive Compulsive Symptom Inventory Download Primary Link Archived Link
- OCD Trauma Timeline Interview (OTTI) | Wadsworth, Van Kirk,August, MacLaren Kelly, Jackson, Nelson & Luehrs | 2023 Download Primary Link Archived Link
- Vancouver Obsessional Compulsive Inventory (VOCI) Download Primary Link Archived Link
Guides and workbooks
- What you need to know about OCD | International OCD Foundation (IOCDF) Download Primary Link
- Managing obsessive compulsive disorder | Simon Enright Download Primary Link Archived Link
- Obsessive compulsive disorder: patient treatment manual | Clinical Research Unit for Anxiety and Depression (CRUfAD) Download Primary Link Archived Link
- OCD: An OCD-UK Information Guides For People Affected By Obsessive Compulsive Disorder | OCD-UK Download Archived Link
- Self-Help: Managing Your OCD At Home | Anxiety Canada Download Primary Link Archived Link
Information Handouts
- "Just Right" OCD Symptoms | IOCDF | 2009 Download Primary Link
- What are postpartum and perinatal OCD? | IOCDF Download Primary Link
Information (Professional)
- Scrupulosity and OCD: information packet for faith leaders | IOCDF, ADAA Download Primary Link Archived Link
Presentations
- Cognitive behavioral therapy for OCD | Sabine Wilhelm Download Primary Link Archived Link
- New directions in implementing exposure and response prevention: an inhibitory learning perspective | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- Cognitive Therapy for Contamination-Related OCD: ERP and Beyond | Adam Radomsky | 2011 Download Archived Link
- Interoceptive exposure: an underused weapon in the arsenal against obsessions and compulsions | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- Family affair: involving a partner or spouse in exposure and response prevention for OCD | Jonathan Abramowitz | 2018 Download Primary Link Archived Link
- A couple-based approach to CBT for BDD | Lillian Reuman, Jonathan Abramowitz | 2016 Download Primary Link Archived Link
- Body dysmorphic disorder | David Veale | 2017 Download Primary Link Archived Link
Treatment Guide
- NICE Guidelines For OCD and BDD | NICE | 2005 Download Primary Link
- Treatment of patients with OCD | American Psychiatric Association (APA) | 2007 Download Primary Link
- Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders (2014) | Katzman et al | 2014 Download Primary Link Archived Link
- A psychological perspective on hoarding – DCP good practice guidelines | Holmes, S., Whomsley, S., Kellet S. | 2015 Download Archived Link
- Treatment Manual For OCD | Clinical Research Unit for Anxiety Disorders (CRUFAD) | 2010 Download Primary Link Archived Link
Recommended Reading
- Veale, D. (2004). Advances in a cognitive behavioural model of body dysmorphic disorder. Body Image ,1, 113-125 Download Primary Link Archived Link
- Gillihan, S., Williams, M. T., Malcoun, E., Yadin, E., Foa, E. B. (2012) Common pitfalls in exposure and response prevention (EX/RP) for OCD. Journal of Obsessive-Compulsive and Related Disorders, 1, 251-257 Download Primary Link
- Rachman, S. (1997). A cognitive theory of obsessions. Behaviour Research and Therapy, 35(9), 793-802 Download Archived Link
- Mataix-Cols, D., et al (2010). Hoarding disorder: A new diagnosis for DSM-V? Depression and Anxiety, 27, 556-572. Download Archived Link
- Salkovskis, P. (1999). Psychological treatment of obsessive–compulsive disorder. Behaviour Research and Therapy, 37, S37-S52 Download Primary Link Archived Link
- Salkovskis, P. M. (2007). Psychological treatment of obsessive–compulsive disorder.Psychiatry,6(6), 229-233 Download Primary Link Archived Link
- Veale, D. (2007). Cognitive behavioural therapy for obsessive compulsive disorder. Advances in Psychiatric Treatment. 13, 438-446 Download Primary Link Archived Link
- Veale, D., Freeston, M., Krebs, G., Heyman, I., & Salkovskis, P. (2009). Risk assessment and management in obsessive–compulsive disorder. Advances in psychiatric treatment, 15(5), 332-343. Download Primary Link Archived Link
- Danesh, M., Beroukhim, K., Nguyen, C., Levin, E., & Koo, J. (2015). Body dysmorphic disorder screening tools for the dermatologist: A systematic review.Pract Dermatol,2, 44-49. Download Primary Link Archived Link
- Krebs, G., de la Cruz, L. F., & Mataix-Cols, D. (2017). Recent advances in understanding and managing body dysmorphic disorder. Evidence-Based Mental Health, 20(3), 71-75. Download Primary Link Archived Link
- Doron, G., & Derby, D. (2015). Assessment and treatment of relationship-related OCD symptoms (ROCD): a modular approach. Handbook of Obsessive-Compulsive Disorder across the Lifespan. Hoboken, NJ: Wiley (Forthcoming). Download Primary Link Archived Link
- Veale, D. (2001). Cognitive-behavioural therapy for body dysmorphic disorder. Advances in Psychiatric Treatment, 7, 125-132 Download Primary Link Archived Link
- Assessment and treatment of relationship-related OCD symptoms | Guy Doron, Danny Derby | 2017 Download Primary Link Archived Link
- Clark, D. A., & Rhyno, S. (2005). Unwanted intrusive thoughts in nonclinical individuals. Intrusive thoughts in clinical disorders: Theory, research, and treatment, 1-29 Download Primary Link Archived Link
What Is Obsessive Compulsive Disorder?
Signs and symptoms of ocd.
People with OCD experience obsessional thoughts, images, urges, and doubts. They often feel compelled to act or think in certain ways.
Obsessions are intrusive thoughts—thoughts that are unwanted and unacceptable, and which pop into our minds unbidden. Obsessions can be thoughts in the form of words, but also of images (pictures in our minds), urges or impulses, or feelings of doubt. Obsessive thoughts are experienced as unacceptable, disgusting, or senseless, and people with OCD find it hard not to pay attention to them. Examples of obsessions include:
- thoughts such as ‘My hands have been contaminated with germs’ or ‘Perhaps I am a pedophile’
- images of my family being murdered
- doubts such as ‘Have I left the stove on?’
- urges such as wanting to shout profanities
Compulsions follow from the way in which the individual interprets the intrusive thoughts. Compulsions are the reactions or mental actions that a person does in order to neutralize or ‘make safe’ following an obsession. People with OCD typically carry out compulsions in order to prevent a harm from happening for which they might be responsible, and/or to reduce any strong emotion which they feel. Exactly what someone with OCD may feel compelled to do will depend upon the meaning their intrusions have for them. Examples of compulsions might include:
- carefully washing food after having an intrusive thought about germs;
- calling family members to check they are OK after having an intrusive image about their deaths;
- going back to the house to check after doubting whether the stove was turned off;
- avoiding a public place after having an urge to shout profanities.
Prevalence of OCD
The lifetime prevalence rate of OCD in the United States is estimated to be 2.3% in adults (Kessler et al., 2005), and 1% to 2.3% in children and adolescents (Zohar, 1999).
Psychological Models and Theory of OCD
The cognitive behavioral theory of OCD proposes that when someone experiences an intrusive thought it is the appraisal—what they make of having the thought—that is most important (Salkovskis, Forrester, & Richards, 1998). Intrusive thoughts, even very unpleasant ones, are common and entirely normal . What seems to happen in OCD is that the fact of having intrusive thoughts is interpreted as being especially significant and, as a result, is especially anxiety-provoking. People with OCD are more likely to feel especially responsible for any potential harms and may feel especially strong emotion should they have intrusive thoughts about harm occurring. Compulsions are understood to be an active attempt to reduce harm. According to the cognitive model of OCD targets for intervention include:
- understanding and addressing the meaning of the intrusions;
- targeting compulsions and safety-seeking behaviors;
- modifying attentional biases.
Evidence-Based Psychological Approaches for Working with OCD
Cognitive behavioral therapy (CBT) is an evidence-based psychological treatment for OCD. Historically, CBT for OCD has involved the behavioral approach of exposure with response prevention (ERP). More cognitive approaches within CBT attempt to understand the patient’s appraisal of their intrusions and to find ways of exploring the validity and consequences of these appraisals.
Resources for Working with OCD
Psychology Tools resources available for working therapeutically with OCD may include:
- psychological models of obsessive-compulsive disorder (OCD)
- information handouts for obsessive-compulsive disorder (OCD)
- exercises for obsessive-compulsive disorder (OCD)
- CBT worksheets for obsessive-compulsive disorder (OCD)
- self-help programs for obsessive-compulsive disorder (OCD)
- Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry , 62 (6), 593–602.
- Salkovskis, P. M., Forrester, E., & Richards, C. (1998). Cognitive–behavioral approach to understanding obsessional thinking. The British Journal of Psychiatry , 173 (S35), 53–63.
- Zohar, A. H. (1999). The epidemiology of obsessive-compulsive disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America , 8 (3), 445–460.
- For clinicians
- For students
- Resources at your fingertips
- Designed for effectiveness
- Resources by problem
- Translation Project
- Help center
- Try us for free
- Terms & conditions
- Privacy Policy
- Cookies Policy
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Sweepstakes
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Psychological Therapy for OCD
Alain SHRODER / ONOKY / Getty Images
Psychological therapy is recognized by both researchers and healthcare providers as an effective treatment for reducing the frequency and intensity of OCD symptoms . Effective psychological therapy for OCD stresses changes in behavior and/or thoughts, sometimes referred to as cognitions.
Overall, cognitive and behavioral therapies appear to be even more effective than medications in both adults and children with OCD. When appropriate, behavioral and cognitive therapy for OCD can be combined with medications for the best result.
Behavioral Therapy
Although there are a variety of behavioral therapies for treating OCD , most of these focus on exposing you to those things that you fear most. This exposure provides you with an opportunity to gain new information in hopes of disconfirming your worst fears.
Exposure and Response Prevention
One of the most popular and effective forms of behavioral therapy for OCD is exposure and response prevention (ERP). ERP involves exposing you to the anxiety that is provoked by your obsessions and then preventing the use of rituals to reduce your anxiety. This cycle of exposure and response prevention is repeated until you are no longer troubled by your obsessions and/or compulsions.
How Long Does It Take?
ERP usually involves 15 to 20 exposure sessions that last about 90 minutes. These sessions usually take place at a therapist’s office, although you are usually asked to practice ERP at home.
While some therapists prefer to begin with exposure to the most feared stimuli (called flooding), others prefer to take a more gradual approach. For example, it is not uncommon to have people begin ERP by simply thinking about being exposed to the things they fear most.
Although behavior therapy is highly effective for about two-thirds of people who complete treatment, there are drawbacks:
- Behavior therapy involves facing your worst fears. Many patients drop out before treatment is complete.
- Behavior therapy is hard work and requires completing homework in between sessions.
- Behavior therapy may not be that effective for people who experience primarily obsessions without compulsions .
- Behavior therapy can be expensive, although insurance plans may cover all or part of the cost.
Cognitive Therapy
Cognitive therapy for OCD is based on the idea that distorted thoughts or cognitions cause and maintain harmful obsessions and compulsions. For example, although the majority of people report experiencing intrusive, and often bizarre, thoughts on a daily basis, if you have OCD you may over-inflate the importance or danger associated with such thoughts. You may even believe that by having such thoughts, you increase the likelihood of the feared thought, event, or action taking place or being true.
Magical Thinking
If you have OCD, you might dramatically overestimate the degree to which you are responsible for a catastrophic event taking place and feel you have to take actions to prevent it. For instance, you might experience an uncontrollable urge to count or order a particular object to prevent a plane crash. Of course, counting or ordering a particular object couldn’t possibly have any impact on whether a plane crashes or not. This illogical thought pattern is often called magical thinking .
Cognitive therapy involves examining harmful thought patterns and coming up with plausible alternatives that are more realistic and less threatening. It is not uncommon to be unaware of some of the distortions present in your thinking, and the therapist may help to point these out.
Also, cognitive therapy often integrates elements of behavior therapy. For example, your therapist may have you test out some of the plausible alternatives you have come up with through exposure therapy .
How Long Does It Take?
Like ERP, cognitive therapy is usually done over the course of 15 to 20 sessions, although the cognitive therapy sessions are often shorter in duration, lasting 50 to 60 minutes. As with ERP, you are often asked to do homework, which usually comprises of keeping a daily journal of your thoughts as well as keeping track of whether your worst fears actually came true.
Considerations
Deciding to engage in behavioral or cognitive therapy for OCD is a decision that should be made in consultation with your family doctor, psychiatrist, or psychologist as part of your overall treatment plan. In controlled research studies, behavioral and cognitive therapy seem to be equally effective. However, in practice, they are often combined for maximum effect. This is referred to as cognitive-behavior therapy .
No matter what type of therapy you choose to pursue, it's most helpful when you actively engage in an open discussion with your doctor or mental health professional—one in which you are honest about your symptoms, feelings, thoughts, and anything else that comes to your mind. This will help to form a full picture of what you require to move forward and progress.
OCD Discussion Guide
Get our printable guide to help you ask the right questions at your next doctor's appointment.
Learn the best ways to manage stress and negativity in your life.
Thank you, {{form.email}}, for signing up.
There was an error. Please try again.
Before engaging in psychotherapy, it may be helpful to ask yourself the following questions:
- Am I willing to try facing the very things I fear most?
- Will I be able to finance this on my own or will my insurance cover the costs?
- Am I willing to put in the time required to participate in weekly sessions for up to 20 weeks?
- On top of going to a weekly session, am I willing to complete homework assignments in between sessions?
Get Help Now
We've tried, tested, and written unbiased reviews of the best online therapy programs including Talkspace, BetterHelp, and ReGain. Find out which option is the best for you.
A Word From Verywell
Research shows that the people who have good results with psychotherapy are those who are highly motivated to change and willing to try and put in the commitment required. If you have questions about your readiness to participate in psychotherapy, talk to your doctor or psychologist.
If you do decide to include psychotherapy as part of your overall treatment plan, make sure you are comfortable with your therapist. If you feel something is preventing you from having a good working relationship, don’t be afraid to bring it up in therapy. A good therapist will be happy that you have brought this to their attention and will try to work through these issues with you.
Since online therapy (or telephone therapy) is becoming more common, researchers have analyzed whether this can be as effective as in-person therapy. So far, studies suggest that the answer is yes. But keep in mind that distant therapy is more difficult as both the client and therapist lack the ability to interpret body language and other factors. However, it is still a good option for those who live quite a distance from a good therapist.
Law C, Boisseau CL. Exposure and Response Prevention in the Treatment of Obsessive-Compulsive Disorder: Current Perspectives . Psychol Res Behav Manag . 2019;12:1167-1174. doi:10.2147/PRBM.S211117
Nezu CM, Martell CR, Nezu AM. Specialty Competencies in Cognitive and Behavioral Psychology . Oxford University Press . 2013.
Foa EB. Cognitive behavioral therapy of obsessive-compulsive disorder . Dialogues Clin Neurosci . 2010;12(2):199-207.
Abramowitz JS, McKay D, Storch EA. The Wiley Handbook of Obsessive Compulsive Disorders . Wiley . 2017.
Laforest M, Bouchard S, Bossé J, Mesly O. Effectiveness of In Virtuo Exposure and Response Prevention Treatment Using Cognitive-Behavioral Therapy for Obsessive-Compulsive Disorder: A Study Based on a Single-Case Study Protocol . Front Psychiatry . 2016;7:99. doi:10.3389/fpsyt.2016.00099
Ryan RM, Lynch MF, et al. Motivation and Autonomy in Counseling, Psychotherapy, and Behavior Change: A Look at Theory and Practice . The Counseling Psychologist . 2011;39(2):193–260. doi:10.1177/0011000009359313
Wootton BM. Remote cognitive-behavior therapy for obsessive-compulsive symptoms: A meta-analysis . Clin Psychol Rev . 2016;43:103-13. doi:10.1016/j.cpr.2015.10.001
Ost, L., Havnen, A., Hansen, B., and G. Kvale. Cognitive Behavioral Treatments of Obsessive-compulsive Disorder. A Systematic Review and Meta-analysis of Studies Published 1993-2014 Clinical Psychology Review . 2015. 40:156-69.
- Ost, L., Riise, E., Wergeland, G., Hansen, B., and G. Kvale. Cognitive Behavioral and Pharmacological Treatments of OCD in Children: A Systematic Review and Meta-Analysis . Journal of Anxiety Disorders . 2016. 43:58-69.
- Wootton, B. Remote Cognitive-Behavior Therapy for Obsessive-Compulsive Symptoms: A Meta-Analysis . Clinical Psychology Review . 2016. 43:103-13.
By Owen Kelly, PhD Owen Kelly, PhD, is a clinical psychologist, professor, and author in Ontario, ON, who specializes in anxiety and mood disorders.

Assessments & Worksheets
The following are a list of various assessments and worksheets that you may find helpful in your practice., assessments.
- Obsessional Beliefs Questionnaire (OBQ-44) and the Obsessional Beliefs Questionnaire Score Key
- Identifying Treatment-Interfering Behaviors (TIBS)
- ASI-IV and the ASI-IV Score Key
- Obsessive Concerns Checklist
- Compulsive Activities Checklist
- Child Saving Inventory - Parent Version
- BTTI Worry Management Worksheet
- BTTI Utility Analysis
- PISA Worksheet
- ERP Motivator IA - What Have I Lost To OCD?
- Response Prevention Plan
- Information-seekers vs reassurance-seekers
In This Section
More resources.
- Fact Sheets & Brochures
- Books About OCD
- From the Experts
- Educational Resources
Search iocdf.org
Your gift has the power to change the life of someone living with ocd..
Homework Completion in Treating Obsessive–Compulsive Disorder with Exposure and Ritual Prevention: A Review of the Empirical Literature
- Published: 16 June 2020
- Volume 45 , pages 236–249, ( 2021 )
Cite this article

- Michael G. Wheaton ORCID: orcid.org/0000-0002-7465-7879 1 &
- Stephanie R. Chen 2
2466 Accesses
23 Citations
Explore all metrics
Homework is an integral part of treating obsessive–compulsive disorder (OCD) with exposure and response prevention (ERP). Between-session homework assignments are prescribed in ERP protocols, including self-monitoring, self-guided exposure practices, and ritual prevention. This review seeks to explore the empirical literature on the importance of homework completion in ERP.
We completed a systematic review of existing studies and organized results to provide a narrative review with an emphasis on informing research and practice.
Heterogeneous methods have been utilized to operationalize and quantify homework completion in ERP. Several studies yielded evidence showing that that patient completion of between-session homework robustly predicts to treatment outcomes across ERP delivery methods (individual outpatient, intensive residential treatment) in both adults and pediatric samples. Some factors were linked to poor patient homework completion, including OCD features (e.g., avoidance, insight), patient expectancies, and the strength of the therapeutic alliance. Relatively few studies have investigated strategies to improve homework completion.
Conclusions
Homework completion is an important component of treating OCD with ERP. More research is needed to improve assessment tools and test strategies to enhance homework completion. We conclude with key practice points and directions for future research.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Patient adherence as a predictor of acute and long-term outcomes in concentrated exposure treatment for difficult-to-treat obsessive-compulsive disorder
When exposures go right: effective exposure-based treatment for obsessive–compulsive disorder, review of psychotherapeutic approaches for ocd and related disorders.
Abramowitz, J. S., Deacon, B. J., Olatunji, B. O., Wheaton, M. G., Berman, N. C., Losardo, D.,.. & Björgvinsson, T. (2010). Assessment of obsessive-compulsive symptom dimensions: Development and evaluation of the dimensional obsessive-compulsive scale. Psychological Assessment , 22 (1), 180
Abramowitz, J. S., Franklin, M. E., Zoellner, L. A., & Dibernardo, C. L. (2002). Treatment compliance and outcome in obsessive-compulsive disorder. Behavior Modification, 26 (4), 447–463.
PubMed Google Scholar
Aloe, A. M., & Thompson, C. G. (2013). The synthesis of partial effect sizes. Journal of the Society for Social Work and Research, 4 (4), 390–405.
Google Scholar
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders . Arlington: American Psychiatric Publishing.
Anand, N., Sudhir, P. M., Math, S. B., Thennarasu, K., & Reddy, Y. J. (2011). Cognitive behavior therapy in medication non-responders with obsessive–compulsive disorder: A prospective 1-year follow-up study. Journal of Anxiety Disorders, 25 (7), 939–945.
Andersson, E., Enander, J., Andrén, P., Hedman, E., Ljótsson, B., Hursti, T.,... & Rück, C. (2012). Internet-based cognitive behaviour therapy for obsessive–compulsive disorder: A randomized controlled trial. Psychological Medicine , 42 (10), 2193–2203
Arch, J. J., & Abramowitz, J. S. (2015). Exposure therapy for obsessive–compulsive disorder: An optimizing inhibitory learning approach. Journal of Obsessive-Compulsive and Related Disorders, 6 , 174–182.
Benito, K. G., Machan, J., Freeman, J. B., Garcia, A. M., Walther, M., Frank, H.,... & Sapyta, J. (2018). Measuring fear change within exposures: Functionally-defined habituation predicts outcome in three randomized controlled trials for pediatric OCD. Journal of Consulting and Clinical Psychology , 86 (7), 615–630
Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., & Vervliet, B. (2014). Maximizing exposure therapy: An inhibitory learning approach. Behaviour Research and Therapy, 58 , 10–23.
PubMed PubMed Central Google Scholar
Craske, M. G., & Tsao, J. C. (1999). Self-monitoring with panic and anxiety disorders. Psychological Assessment, 11 (4), 466.
De Araujo, L. A., Ito, L. M., & Marks, I. M. (1996). Early compliance and other factors predicting outcome of exposure for obsessive–compulsive disorder. The British Journal of Psychiatry, 169 (6), 747–752.
Dowling, N., Thomas, N., Blair-West, S., Bousman, C., Yap, K., Smith, D. J., et al. (2016). Intensive residential treatment for obsessive-compulsive disorder: Outcomes and predictors of patient adherence to cognitive-behavioural therapy. Journal of Obsessive-Compulsive and Related Disorders, 9 , 82–89.
Eisen, J. L., Pinto, A., Mancebo, M. C., Dyck, I. R., Orlando, M. E., & Rasmussen, S. A. (2010). A 2-year prospective follow-up study of the course of obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 71 (8), 1033–1039.
Fals-Stewart, W., & Lucente, S. (1993). An MCMI cluster typology of obsessive—Compulsives: A measure of personality characteristics and its relationship to treatment participation, compliance and outcome in behavior therapy. Journal of Psychiatric Research, 27 (2), 139–154.
CAS PubMed Google Scholar
Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99 (1), 20.
Foa, E. B., Yadin, E., & Lichner, T. K. (2012). Exposure and response (ritual) prevention for obsessive compulsive disorder: Therapist guide . Oxford: Oxford University Press.
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Delgado, P., Heninger, G. R., et al. (1989b). The Yale-Brown obsessive compulsive scale: II. Validity. Archives of General Psychiatry, 46 (11), 1012.
Goodman, W. K., Price, L. H., Rasmussen, S. A., Mazure, C., Fleischmann, R. L., Hill, C. L.,... & Charney, D. S. (1989a). The Yale-Brown obsessive compulsive scale: I. Development, use, and reliability. Archives of General Psychiatry , 46 (11), 1006
Guy, W. (1976). Clinical global impression scale. The ECDEU Assessment Manual for Psychopharmacology-Revised, 338 , 218–222.
Hatcher, R. L., & Gillaspy, J. A. (2006). Development and validation of a revised short version of the Working Alliance Inventory. Psychotherapy Research, 16 (1), 12–25.
Hong, N., Sanchez, A. L., & Comer, J. S. (2019). Multimedia field test: Can users strike out OCD With the NOCD app? Cognitive and Behavioral Practice . https://doi.org/10.1016/j.cbpra.2019.02.005 .
Article Google Scholar
Huppert, J. D., Roth Ledley, D., & Foa, E. B. (2006). The use of homework in behavior therapy for anxiety disorders. Journal of Psychotherapy Integration, 16 (2), 128–139.
Jacoby, R. J., & Abramowitz, J. S. (2016). Inhibitory learning approaches to exposure therapy: A critical review and translation to obsessive-compulsive disorder. Clinical Psychology Review, 49 , 28–40.
Kazantzis, N., Brownfield, N. R., Mosely, L., Usatoff, A. S., & Flighty, A. J. (2017). Homework in cognitive behavioral therapy: A systematic review of adherence assessment in anxiety and depression (2011–2016). Psychiatric Clinics, 40 (4), 625–639.
Kazantzis, N., Whittington, C., Zelencich, L., Kyrios, M., Norton, P. J., & Hofmann, S. G. (2016). Quantity and quality of homework compliance: A meta-analysis of relations with outcome in cognitive behavior therapy. Behavior Therapy, 47 (5), 755–772.
Kenwright, M., Marks, I., Graham, C., Franses, A., & Mataix-Cols, D. (2005). Brief scheduled phone support from a clinician to enhance computer-aided self-help for obsessive-compulsive disorder: Randomized controlled trial. Journal of Clinical Psychology, 61 (12), 1499–1508.
Koran, L., & Simpson, H. (2013). Guideline Watch (March 2013): Practice guideline for the treatment of patients with obsessive-compulsive disorder. In APA practice guidelines . American Psychiatric Publishing, Inc.
Kozak, M. J., & Foa, E. B. (1997). Mastery of obsessive-compulsive disorder: A cognitive-behavioral approach . San Antonio: The Psychological Corporation.
Lax, T., Başoǧlu, M., & Marks, I. M. (1992). Expectancy and compliance as predictors of outcome in obsessive-compulsive disorder. Behavioural and Cognitive Psychotherapy, 20 (3), 257–266.
Leahy, R. L. (2002). A model of emotional schemas. Cognitive and Behavioral Practice, 9 (3), 177–190.
Leahy, R. L. (2007). Emotional schemas and self-help: Homework compliance and obsessive-compulsive disorder. Cognitive and Behavioral Practice, 14 (3), 297–302.
Leeuwerik, T., Cavanagh, K., & Strauss, C. (2019). Patient adherence to cognitive behavioural therapy for obsessive-compulsive disorder: A systematic review and meta-analysis. Journal of Anxiety Disorders . https://doi.org/10.1016/j.janxdis.2019.102135 .
Article PubMed Google Scholar
Lewin, A. B., Peris, T. S., Bergman, R. L., McCracken, J. T., & Piacentini, J. (2011). The role of treatment expectancy in youth receiving exposure-based CBT for obsessive compulsive disorder. Behaviour Research and Therapy, 49 (9), 536–543.
Maher, M. J., Wang, Y., Zuckoff, A., Wall, M. M., Franklin, M., Foa, E. B., et al. (2012). Predictors of patient adherence to cognitive-behavioral therapy for obsessive-compulsive disorder. Psychotherapy and Psychosomatics, 81 (2), 124–125.
Maltby, N., & Tolin, D. F. (2005). A brief motivational intervention for treatment-refusing OCD patients. Cognitive Behaviour Therapy, 34 (3), 176–184.
Mataix-Cols, D., de la Cruz, L. F., Nordsletten, A. E., Lenhard, F., Isomura, K., & Simpson, H. B. (2016). Towards an international expert consensus for defining treatment response, remission, recovery and relapse in obsessive-compulsive disorder. World Psychiatry, 15 (1), 80–81.
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). New York: Guilford Press.
Millon, T. (1983). Manual for the millon multiaxial inventory . Minneapolis, MM
NICE. (2013). Obsessive-compulsive disorder: Evidence update September 2013 . NICE clinical guideline 31. Retrieved January 20, 2020 from https://www.nice.org.uk/guidance/cg31/evidence/evidence-update-194847085
Ojalehto, H. J., Abramowitz, J. S., Hellberg, S. N., Buchholz, J. L., & Twohig, M. P. (2020). Adherence to exposure and response prevention as a predictor of improvement in obsessive-compulsive symptom dimensions. Journal of Anxiety Disorders, 72 , 102210.
Olatunji, B. O., Rosenfield, D., Monzani, B., Krebs, G., Heyman, I., Turner, C.,... & Mataix‐Cols, D. (2015). Effects of homework compliance on cognitive‐behavioral therapy with d‐cycloserine augmentation for children with obsessive compulsive disorder. Depression and Anxiety , 32 (12), 935–943
Öst, L. G., Havnen, A., Hansen, B., & Kvale, G. (2015). Cognitive behavioral treatments of obsessive–compulsive disorder. A systematic review and meta-analysis of studies published 1993–2014. Clinical Psychology Review, 40 , 156–169.
O'Sullivan, G., Noshirvani, H., Marks, I., Monteiro, W., & Lelliott, P. (1991). Six-year follow-up after exposure and clomipramine therapy for obsessive compulsive disorder. The Journal of Clinical Psychiatry, 52 (4), 150–155.
Park, J. M., Small, B. J., Geller, D. A., Murphy, T. K., Lewin, A. B., & Storch, E. A. (2014). Does d-cycloserine augmentation of CBT improve therapeutic homework compliance for pediatric obsessive–compulsive disorder? Journal of Child and Family Studies, 23 (5), 863–871.
Pollard, C. A. (2006). Treatment readiness, ambivalence, and resistance. In M. M. Antony, C. Purdon, & L. J. Summerfeldt (Eds.), Psychological treatment of obsessive compulsive disorder: Fundamentals and beyond (pp. 61–78). Washington, D.C.: APA Books.
Primakoff, L., Epstein, N., & Covi, L. (1986). Homework compliance: An uncontrolled variable in cognitive therapy outcome research. Behavior Therapy, 17 (4), 433–446.
Reger, G. M., Hoffman, J., Riggs, D., Rothbaum, B. O., Ruzek, J., Holloway, K. M., et al. (2013). The “PE coach” smartphone application: An innovative approach to improving implementation, fidelity, and homework adherence during prolonged exposure. Psychological Services, 10 (3), 342–349.
Rizvi, S. L., Hughes, C. D., & Thomas, M. C. (2016). The DBT Coach mobile application as an adjunct to treatment for suicidal and self-injuring individuals with borderline personality disorder: A preliminary evaluation and challenges to client utilization. Psychological Services, 13 (4), 380–388.
Ruscio, A. M., Stein, D. J., Chiu, W. T., & Kessler, R. C. (2010). The epidemiology of obsessive-compulsive disorder in the National comorbidity survey replication. Molecular Psychiatry, 15 (1), 53–63.
Scahill, L., Riddle, M. A., McSwiggin-Hardin, M., Ort, S. I., King, R. A., Goodman, W. K.,... & Leckman, J. F. (1997). Children's Yale-Brown obsessive compulsive scale: reliability and validity. Journal of the American Academy of Child & Adolescent Psychiatry , 36 (6), 844–852
Selles, R. R., Belschner, L., Negreiros, J., Lin, S., Schuberth, D., McKenney, K.,... & Stewart, S. E. (2018). Group family-based cognitive behavioral therapy for pediatric obsessive compulsive disorder: Global outcomes and predictors of improvement. Psychiatry Research , 260 , 116–122
Simpson, H. B., Maher, M., Page, J. R., Gibbons, C. J., Franklin, M. E., & Foa, E. B. (2010a). Development of a patient adherence scale for exposure and response prevention therapy. Behavior Therapy, 41 (1), 30–37.
Simpson, H. B., Maher, M. J., Wang, Y., Bao, Y., Foa, E. B., & Franklin, M. (2011). Patient adherence predicts outcome from cognitive behavioral therapy in obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology, 79 (2), 247–252.
Simpson, H. B., Marcus, S. M., Zuckoff, A., Franklin, M., & Foa, E. B. (2012). Patient adherence to cognitive-behavioral therapy predicts long-term outcome in obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 73 (9), 1265.
Simpson, H. B., Zuckoff, A. M., Maher, M. J., Page, J. R., Franklin, M. E., Foa, E. B.,... & Wang, Y. (2010b). Challenges using motivational interviewing as an adjunct to exposure therapy for obsessive-compulsive disorder. Behaviour Research and Therapy , 48 , 941–948
Simpson, H. B., Zuckoff, A., Page, J. R., Franklin, M. E., & Foa, E. B. (2008). Adding motivational interviewing to exposure and ritual prevention for obsessive–compulsive disorder: An open pilot trial. Cognitive Behaviour Therapy, 37 , 38–49.
Skapinakis, P., Caldwell, D. M., Hollingworth, W., Bryden, P., Fineberg, N. A., Salkovskis, P.,... & Lewis, G. (2016). Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry , 3 (8), 730–739
Steketee, G. (1999). Overcoming obsessive compulsive disorder—Therapist protocol . Oakland: New Harbinger.
Tolin, D. F., Hannan, S., Maltby, N., Diefenbach, G. J., Worhunsky, P., & Brady, R. E. (2007). A randomized controlled trial of self-directed versus therapist-directed cognitive-behavioral therapy for obsessive-compulsive disorder patients with prior medication trials. Behavior Therapy, 38 (2), 179–191.
Tolin, D. F., Maltby, N., Diefenbach, G. J., Hannan, S. E., & Worhunsky, P. (2004). Cognitive-behavioral therapy for medication nonresponders with obsessive-compulsive disorder: A wait-list-controlled open trial. The Journal of Clinical Psychiatry, 65 , 922–931.
van Dyke, M. M., & Pollard, C. A. (2005). Treatment of refractory obsessive-compulsive disorder: The St-Louis Model. Cognitive and Behavioral Practice, 12 , 30–39.
Wanous, J. P., & Reichers, A. E. (1996). Estimating the reliability of a single-item measure. Psychological Reports, 78 (2), 631–634.
Wheaton, M. G., Galfalvy, H., Steinman, S. A., Wall, M. M., Foa, E. B., & Simpson, H. B. (2016a). Patient adherence and treatment outcome with exposure and response prevention for OCD: Which components of adherence matter and who becomes well? Behaviour Research and Therapy, 85 , 6–12.
Wheaton, M. G., Gershkovich, M., Gallagher, T., Foa, E. B., & Simpson, H. B. (2018). Behavioral avoidance predicts treatment outcome with exposure and response prevention for obsessive–compulsive disorder. Depression and Anxiety, 35 (3), 256–263.
CAS PubMed PubMed Central Google Scholar
Wheaton, M. G., Huppert, J. D., Foa, E. B., & Simpson, H. B. (2016b). How important is the therapeutic alliance in treating obsessive-compulsive disorder with exposure and response prevention? An empirical report. Clinical Neuropsychiatry, 13 (6), 88–93.
Wheaton, M. G., Schwartz, M. R., Pascucci, O., & Simpson, H. B. (2015). Cognitive-behavior therapy outcomes for obsessive-compulsive disorder: Exposure and response prevention. Psychiatric Annals, 45 (6), 303–307.
Whiteside, S. P., Ale, C. M., Vickers Douglas, K., Tiede, M. S., & Dammann, J. E. (2014). Case examples of enhancing pediatric OCD treatment with a smartphone application. Clinical Case Studies, 13 (1), 80–94.
Whittal, M. L., Thordarson, D. S., & McLean, P. D. (2005). Treatment of obsessive–compulsive disorder: Cognitive behavior therapy vs. exposure and response prevention. Behaviour Research and Therapy, 43 (12), 1559–1576.
Woods, C. M., Chambless, D. L., & Steketee, G. (2002). Homework compliance and behavior therapy outcome for panic with agoraphobia and obsessive compulsive disorder. Cognitive Behaviour Therapy, 31 (2), 88–95.
Download references
Author information
Authors and affiliations.
Department of Psychology, Barnard College, New York, NY, USA
Michael G. Wheaton
Teacher’s College, Columbia University, New York, NY, USA
Stephanie R. Chen
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michael G. Wheaton .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Informed Consent
No human subjects were involved in this review article.
Animal Rights Statements
No animal studies were carried out for this study.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Wheaton, M.G., Chen, S. Homework Completion in Treating Obsessive–Compulsive Disorder with Exposure and Ritual Prevention: A Review of the Empirical Literature. Cogn Ther Res 45 , 236–249 (2021). https://doi.org/10.1007/s10608-020-10125-0
Download citation
Published : 16 June 2020
Issue Date : April 2021
DOI : https://doi.org/10.1007/s10608-020-10125-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Homework compliance
- Patient adherence
- Exposure and ritual prevention
- Behavior therapy
- Find a journal
- Publish with us
- Track your research

Heather Lawson
Psychologist , psyd, my practice at a glance.
233 3rd Street North
Saint Petersburg, FL 33701
- Individual Sessions $250
- Pay by Cash, Check, Mastercard, Visa
Qualifications
- Verified by Psychology Today Licensed by State of Florida / PY9604 Heather Lawson
- Attended Nova Southeastern University , Graduated 2002
Specialties and Expertise
Top specialties.
- Borderline Personality (BPD)
- Emotional Disturbance
- Substance Use
- Alcohol Use
- Anger Management
- Behavioral Issues
- Bipolar Disorder
- Chronic Impulsivity
- Coping Skills
- Dual Diagnosis
- Eating Disorders
- Family Conflict
- Mood Disorders
- Obsessive-Compulsive (OCD)
- Peer Relationships
- Personality Disorders
- Relationship Issues
- School Issues
- Self Esteem
- Self-Harming
- Sleep or Insomnia
- Suicidal Ideation
Client Focus
Participants, communities, treatment approach, types of therapy.
- Cognitive Behavioral (CBT)
- Dialectical Behavior (DBT)
- Interpersonal
DBT Skills Group
My DBT group is a structured, psycho-educational group. Skills in all of the four DBT modules are taught. The group is an hour and a half and includes a mindfulness practice, review of homework, and didactic teaching.
Session Cost
Group meets, primary location, nearby areas.
- New York, NY
- Saint Petersburg, FL
Neighborhoods
- Greenwich Village
- Lower Manhattan
Make an Appointment: [email protected] | (727) 565-2424
360 Central Avenue, Suite 1230, Suite 430, Saint Petersburg, FL 33701 [email protected] | (727) 565-2424 | Fax: (727) 440-8148
“Sometimes in the waves of change, we find our true direction.”
At saible neuropsychology, our goal is to help people live more meaningful and satisfying lives by providing individualized, effective, psychological care. our providers offer individual therapy, psychological evaluation, and neuropsychological assessment. if you are looking for extra support and guidance through a challenging situation or you are just ready to move in a new direction in your life, we look forward to working with you to achieve your goals., if you're ready to..., • start enjoying life again, • achieve your goals, • and live authentically, …then let’s chat, here are some places to get started.

Our Providers

Our Services

What our clients and colleagues have to say
“i’ve worked with dr. saible in the past. she is very professional and her evaluations provide strong insight into underlying psychological and psychiatric issues.”, dr. alexandra hollander has been my therapist for around 5 months now and it has been a wonderful experience overall. she listens, relates, and identifies what i’m going through and the best ways for me to handle everything and deal with daily stress. i just finished my last semester of law school and she has been such an asses in getting me to that finish line.”, michaela c., “as a psychiatrist, i have worked with dr. saible for years. now in her own practice, i still refer my patients to her for neuropsych testing to help with diagnoses for adhd, depression, bipolar, anxiety, ocd, dementia, even personality disorders and autism spectrum. she accommodates my patients quickly and is very efficient with getting me the report so that treatment can move forward. the testing is thorough and she explains the process along the way. she is on most insurance plans and takes care of the authorization so the family knows exactly what is covered and what their copay will be before they come in. i trust her with my patients, and would not hesitate to send my own family to her. she’s top notch”, “if i need a referral for my neuropsychological needs, there is no one in the community that i trust more than dr. saible. i can rest assured that she will provide the same high quality level of unbiased care that i provide mine.”, “i had an appointment for my daughter with dr. kenny borgas. he was very professional and made sure he explained the process to aubrey and i and that she was comfortable with him. he really took the time to listen to my concerns before taking her back. when getting the report back he called to go over it with me and explained everything in great detail. he covered all my questions before i could even ask them. he was very thorough. he made me feel like my concerns mattered. i would definitely recommend him to anyone looking for a psychologist. also, the staff was very kind and welcoming.”, “dr. saible completed a neuro-psychological assessment for one of my clients. her assessment t and evaluation was detailed and recommendations were very useful.”, “i have worked with dr. saible over the past few years and we have shared many patients during evaluation. i can rely on her to give me a quality evaluation that helps me. she is very thorough and gives timely reports that i can trust.”, “dr. kenny borgas and his team was exceptional. while being evaluated, my daughter not only felt comfortable, she had fun. the evaluation came in a timely manner and was easy to understand. dr. borgas personally called to go over the report and answered any questions i had. highly recommended”, “dr. kenny borgas was very professional and made my son feel very comfortable with speaking with him for his evaluation. i feel the appointments went well. it is also a very clean and peaceful environment. i would highly recommend this office they seem to truly care about their patients.”, -patient review, “my daughter saw dr. kenny borgas as she was required to have an annual evaluation to track her progress for our homeschool program. dr. borgas and staff were very professional and pleasant to work with. the comprehensive testing helped us to gain prospective on how my daughter learns and where we need to improve to help her overcome challenges., additionally, we were given recommendations on tangible things to implement to help her excel in her capabilities. overall, i would certainly recommend saible neuropsychology to parents for their child’s needs.”, telehealth services, saible neuro offers telehealth therapy services to residents anywhere in the state of florida, our professional counselors are now able to support you right from your own home through a private and protected online telehealth platform., for more information or questions on telehealth services, please submit an inquiry and we would be happy to provide you with more information..

COMMENTS
OCD-driven thoughts trick them into believing will alleviate their anxiety—behavior that, paradoxically, only serves to strengthen it. This workbook will help you explore and assess the role OCD plays in your world so that you can take back your thoughts and live the life you desire. You will gather your personal strengths,
This OCD worksheet packet includes a blank exposure hierarchy template, and an exposure therapy homework form. The homework form provides a professional way for you to record your client's weekly exposure homework, and it gives your clients a nice place to keep track of their progress.
If you are experiencing those barriers, or if you just want a supplement to your treatment with some extra "homework," we have resources for you. Putting your thoughts and experiences down on paper can be valuable for any mental health struggle—especially for highly behavioral conditions like OCD—so we've compiled 5 OCD worksheets developed with the help of leading experts in OCD ...
Cognitive behavioral therapy (CBT) for OCD helps people change problematic behaviors, thoughts, and emotions. CBT generally consists of weekly, one-hour therapy sessions lasting approximately six months, depending on the severity of someone's OCD symptoms. Participants should practice what they learn outside of the therapy session to get the most benefit. Most people who receive CBT
Exposure & Ritual Prevention for OCD. EX/RP is a type of cognitive behavioral psychotherapy that is designed to break two types of associations that occur in OCD: The association between sensations of distress and the objects, situations, or thoughts that produce this distress ("obsession = anxiety up") The association between carrying out ...
Learn about the symptoms, causes, and evidence-based treatments of OCD. Find helpful resources, worksheets, and videos to cope with obsessive-compulsive disorder.
Obsessive-compulsive disorder (OCD) is characterized by intrusive thoughts, images, urges, or impulses that are interpreted as threating (obsessions). These lead to active and counterproductive attempts to reduce the thoughts and/or discharge the perceived responsibility associated with them (compulsions). Cognitive and behavioral approaches ...
Exposure Hierarchy Create a list of anxiety-producing situations, beginning with the most distressing, and ending with the least distressing. Rank how distressing each item is on a scale of 1 to 10.
13. Don't wait for the "perfect moment" to start your therapy homework assignments. Procrastination is a feature of many people's OCD, so start your therapy homework assignments the day you get them. The perfect moment is whenever you begin doing them.
Effective psychological therapy for OCD stresses changes in behavior and/or thoughts. Learn more about the specific methods used and what to expect.
Step 3: Building your OCD Management Toolbox. The best way to begin managing your OCD is to begin building a toolbox of strategies that will help you to deal with your obsessions in the long run. Breaking this vicious cycle involves: (1) Learning to gradually eliminate your unhelpful coping strategies (such as compulsions); and (2) Learning to ...
The following are a list of various assessments and worksheets that you may find helpful in your practice. Assessments DASS OC Chart Obsessional Beliefs Questionnaire (OBQ-44) and the Obsessional Beliefs Questionnaire Score... Read more »
Living with OCD comes with a range of daily challenges. Try using these methods to help you manage your symptoms day to day.
Background Homework is an integral part of treating obsessive-compulsive disorder (OCD) with exposure and response prevention (ERP). Between-session homework assignments are prescribed in ERP protocols, including self-monitoring, self-guided exposure practices, and ritual prevention. This review seeks to explore the empirical literature on the importance of homework completion in ERP. Method ...
Pure obsessional OCD is an unofficial type of OCD that may impact your social and occupational life. Here are the causes, signs, and tips to manage it.
Treatments for OCD. Cognitive-behavioral therapy is a treatment for OCD that uses two scientifically based techniques to change a person's behavior and thoughts: exposure and response prevention (ERP) and cognitive therapy. CBT is conducted by a cognitive-behavioral therapist who has special training in treating OCD.
I provide cognitive behavioral therapy (CBT) to adolescents and adults with obsessive compulsive disorder ( OCD ), anxiety related disorders, trauma, relationship difficulties, and depression.
I help individuals confront a variety of mental health bullies such as OCD, phobias, general anxiety, self-esteem issues and more. I believe that therapy is the greatest gift anyone can give to ...
worksheet. Exposure therapy is an evidence-based protocol for helping clients face their fears in a gradual, methodical way. Early in treatment, clients will create an exposure hierarchy, which is a list of scenarios they view as anxiety-provoking. Using the Subjective Units of Distress Scale (SUDS), they will rate these scenarios from 0 (no ...
Heather Lawson, Psychologist, Saint Petersburg, FL, 33701, I'm a licensed clinical psychologist who specializes in Cognitive Behavioral Therapies, including Dialectical Behavior Therapy. I have ...
Free therapy worksheets. Topics include CBT, anger management, self-esteem, relaxation, stress management, addictions, and more.
Now in her own practice, I still refer my patients to her for NeuroPsych testing to help with diagnoses for ADHD, Depression, Bipolar, Anxiety, OCD, Dementia, even personality disorders and Autism spectrum. She accommodates my patients quickly and is very efficient with getting me the report so that treatment can move forward.
Free worksheets, treatment guides, and videos for mental health professionals. Topics include CBT, anger management, self-esteem, relaxation, and more.