An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Ethnobiol Ethnomed


Quantitative ethnopharmacological documentation and molecular confirmation of medicinal plants used by the Manobo tribe of Agusan del Sur, Philippines
Mark lloyd g. dapar.
1 The Graduate School and Research Center for the Natural and Applied Sciences, University of Santo Tomas, España Boulevard, 1015 Manila, Philippines
3 Department of Plant Systematics, University of Bayreuth, Universitätsstr. 30, 95440 Bayreuth, Germany
Grecebio Jonathan D. Alejandro
2 College of Science, University of Santo Tomas, España Boulevard, 1015 Manila, Philippines
Ulrich Meve
Sigrid liede-schumann, associated data.
The authors declare that sequencing data of 24 species identified supporting the findings of this study are available within the article and its supplementary information files.
The Philippines is renowned as one of the species-rich countries and culturally megadiverse in ethnicity around the globe. However, ethnopharmacological studies in the Philippines are still limited especially in the most numerous ethnic tribal populations in the southern part of the archipelago. This present study aims to document the traditional practices, medicinal plant use, and knowledge; to determine the relative importance, consensus, and the extent of all medicinal plants used; and to integrate molecular confirmation of uncertain species used by the Agusan Manobo in Mindanao, Philippines.
Quantitative ethnopharmacological data were obtained using semi-structured interviews, group discussions, field observations, and guided field walks with a total of 335 key informants comprising of tribal chieftains, traditional healers, community elders, and Manobo members of the community with their medicinal plant knowledge. The use-report (UR), use categories (UC), use value (UV), cultural importance value (CIV), and use diversity (UD) were quantified and correlated. Other indices using fidelity level (FL), informant consensus factors (ICF), and Jaccard’s similarity index (JI) were also calculated. The key informants’ medicinal plant use knowledge and practices were statistically analyzed using descriptive and inferential statistics.
This study enumerated the ethnopharmacological use of 122 medicinal plant species, distributed among 108 genera and belonging to 51 families classified in 16 use categories. Integrative molecular approach confirmed 24 species with confusing species identity using multiple universal markers (ITS, mat K, psb A- trn H, and trn L-F). There was strong agreement among the key informants regarding ethnopharmacological uses of plants, with ICF values ranging from 0.97 to 0.99, with the highest number of species (88) being used for the treatment of abnormal signs and symptoms (ASS). Seven species were reported with maximum fidelity level (100%) in seven use categories. The correlations of the five variables (UR, UC, UV, CIV, and UD) were significant ( r s ≥ 0.69, p < 0.001), some being stronger than others. The degree of similarity of the three studied localities had JI ranged from 0.38 to 0.42, indicating species likeness among the tribal communities. Statistically, the medicinal plant knowledge among respondents was significantly different ( p < 0.001) when grouped according to education, gender, social position, occupation, civil status, and age but not ( p = 0.379) when grouped according to location. This study recorded the first quantitative ethnopharmacological documentation coupled with molecular confirmation of medicinal plants in Mindanao, Philippines, of which one medicinal plant species has never been studied pharmacologically to date.
Documenting such traditional knowledge of medicinal plants and practices is highly essential for future management and conservation strategies of these plant genetic resources. This ethnopharmacological study will serve as a future reference not only for more systematic ethnopharmacological documentation but also for further pharmacological studies and drug discovery to improve public healthcare worldwide.
Introduction
The application of traditional medicine has gained renewed attention for the use of traditional, complementary, and alternative medicine (TCAM) in the developing and industrialized countries [ 1 , 2 ]. Conventional drugs these days may serve as effective medicines and therapeutics, but some rural communities still prefer natural remedies to treat selected health-related problems and conditions. Medicinal plants have long been used since the prehistoric period [ 3 ], but the exact time when the use of plant-based drugs has begun is still uncertain [ 4 ]. The WHO has accounted about 60% of the world’s population relying on traditional medicine and 80% of the population in developing countries depend almost entirely on traditional medical practices, in particular, herbal remedies, for their primary health care [ 5 ]. Estimates for the numbers of plant species used medicinally worldwide include 35,000–70,000 [ 6 ] with 7000 in South Asia [ 7 ] comprising ca. 6500 in Southeast Asia [ 8 , 9 ]. In the Philippines, more than 1500 medicinal plants used by traditional healers have been documented [ 10 ], and 120 plants have been scientifically validated for safety and efficacy [ 11 ]. Of all documented Philippine medicinal plants, the top list of medicinal plants used for TCAM has been enumerated by [ 12 ]. Most of these Philippine medicinal plants have been evaluated to scientifically validate folkloric claims like the recent studies of [ 13 – 20 ].
Because of the increasing demand for drug discovery and development of medicinal plants, the application of a quantitative approach in ethnobotany [ 21 ] and ethnopharmacology [ 22 ] has been rising continuously in the last few decades including multivariate analysis [ 23 ]. However, few studies of quantitative ethnobotanical research were conducted despite the rich plant biodiversity and cultural diversity in the Philippines. In particular, the Ivatan community in Batan Island of Luzon [ 24 ] and the Ati Negrito community in Guimaras Island of Visayas [ 21 ] have been documented, while Mindanao has remained less studied. Despite the richness of indigenous knowledge in the Philippines, few ethnobotanical studies have been conducted and published [ 25 ].
The Philippines is culturally megadiverse in diversity and ethnicity among indigenous peoples (IPs) embracing more than a hundred divergent ethnolinguistic groups [ 26 , 27 ] with known specific identity, language, socio-political systems, and practices [ 28 ]. Of these IPs, 61% are mainly inhabiting Mindanao, followed by Luzon with 33%, and some groups in Visayas (6%) [ 29 ]. One of these local people and minorities is the indigenous group of Manobo , inhabiting several areas only in Mindanao. They are acknowledged to be the largest Philippine ethnic group occupying a wide area of distribution than other indigenous communities like the Bagobo, Higaonon, and Atta [ 30 ]. The Manobo (“river people”) was the term named after the “Mansuba” which means river people [ 19 ], coined from the “man” (people) and the “suba” (river) [ 31 ]. Among the provinces dwelled by the Manobo , the province of Agusan del Sur is mostly inhabited by this ethnic group known as the Agusan Manobo . The origin of Agusan Manobo is still uncertain and immemorial; however, they are known to have Butuano, Malay, Indonesian, and Chinese origin occupying mountain ranges and hinterlands in the province of Agusan del Sur [ 32 ].
Manobo indigenous peoples are clustered accordingly, occupying areas with varying dialects and some aspects of culture due to geographical separation. Their historic lifestyle and everyday livelihood are rural agriculture and primarily depend on their rice harvest, root crops, and vegetables for consumption [ 33 ]. Some Agusan Manobo are widely dispersed in highland communities above mountain drainage systems, indicating a suitable area for their indigenous medicinal plants in the province [ 34 ]. Every city or municipality is governed with a tribal chieftain known as the “Datu” (male) or “Bae” (female) with his or her respective tribal healer “Babaylan” and the tribal leaders “Datu” of each barangay (village) leading their community. Their tribe has passed several challenges over the years but has still maintained to conserve and protect their ancestral domain to continually sustain their cultural traditions, practices, and values up to this present generation. This culture implies that there is rich medicinal plant knowledge in the traditional practices of Agusan Manobo , but their indigenous knowledge has not been systematically documented. Furthermore, there are no comprehensive ethnobotanical studies of medicinal plants used among the Manobo tribe in the Philippines to date.
Documenting the ethnomedicinal plant use and knowledge, and molecular confirmation of species using integrative molecular approach will help in understanding the true identity of medicinal plants in the treatment of health-related problems of the people of Agusan del Sur. This will also help the entire Agusan Manobo community to implement conservation priorities of their indigenous plant species. Furthermore, the provincial government of Agusan del Sur may enforce the proper utilization of their plant resources from IPs. Ideas and knowledge about ethnomedicinal use and practices of medicinal plants give credence to the traditional methods and preparation of herbal medicine by ethnic groups.
Despite the limited funds and qualified personnel in the region, it is very relevant to recognize the role of ethnopharmacology and species identification in the conservation of these plant genetic resources with medicinal properties. With the introduction of the application of molecular barcodes for species identification by [ 35 ], the problem of unauthenticated medicinal species can now be resolved [ 19 , 36 – 43 ].
Significantly, researchers have recently developed the application of ethnopharmacological study into a quantitative approach with measuring values and indices to quantify the relationship between plant species and humans [ 44 – 48 ].
This study, therefore, aims to (1) conduct quantitative ethnopharmacological documentation of traditional therapy, (2) evaluate the medicinal plant use and knowledge, and (3) utilize integrative molecular approach for species confirmation of medicinal plants used by the Manobo tribe in Agusan del Sur, Philippines.
Materials and methods
Fieldwork was conducted in the province of Agusan del Sur, Philippines (8° 30′ N 125° 50′ E), bordered from the north by Agusan del Norte, to the south by Davao del Norte, and from the west by Misamis Oriental and Bukidnon, to the east by Surigao del Sur. Agusan del Sur is bounded with mountain ranges from the eastern and western sides forming an elongated basin or valley in the center longitudinal section of the land. The province is subdivided into 13 municipalities (from the largest to smallest land area): La Paz, Esperanza, Loreto, San Luis, Talacogon, Sibagat, Prosperidad, Bunawan, Trento, Veruela, Rosario, San Francisco, and Sta. Josefa; and the only component city, the City of Bayugan (Fig. (Fig.1). 1 ). Forestland comprises almost two thirds (74%) of the province of Agusan del Sur, while alienable and disposable (A&D) areas constitute around one-third (26%) of the total land area [ 49 ]. Every city or municipality has a respective community hospital and health center with limited doctors and rural health workers. Typically, local people only visit the hospitals or health centers for surgical and obstetric emergencies. Most residents rely on their medicinal plants for disease treatment and medication due to cost and poor access to healthcare services. This study purposively covered areas of selected city and municipalities (Bayugan, Esperanza, and Sibagat) for accessibility, availability, and security reasons to barangays (villages) with Certification of Ancestral Domain Title (CADT) as endorsed by the National Commission on Indigenous Peoples—CARAGA Administrative Region (NCIP-CARAGA).

Study sites (barangays) from the only city (Bayugan), and the two selected municipalities (Esperanza and Sibagat) in the province of Agusan del Sur
Sampling and interview
Fieldwork was undertaken from March 2018 to May 2019. It consisted of obtaining free prior informed consents, observing rituals, acquiring resolutions, certifications, and permits, conducting semi-structured interviews, focus group discussions, plant and field observations, and medicinal plant collections in selected barangays (villages) of Bayugan, Sibagat, and Esperanza (Fig. (Fig.1). 1 ). This study was initiated in coordination with the local government unit (LGU), NCIP-LGU, and Provincial Environment and Natural Resources Office (PENRO) of Agusan del Sur. Consultation meetings and discussions were carried out together with the concerned parties (tribal leaders, tribal healers, and NCIP officers) to discuss research intent as purely academic and to acquire mutual agreement and respect to conduct this study. As approved, the research intent was certified through resolution and certification duly signed by the tribal council of elders following the by-laws of NCIP for the welfare and protection of indigenous peoples, and finally certified by NCIP-CARAGA.
Ethnopharmacological data were collected through semi-structured interviews with Manobo key informants through purposive and snowball sampling who were certified Agusan Manobo . A sampling of these key informants was coordinated with the provincial and local government administration together with the assistance of the tribal leaders and NCIP focal persons in every city or municipality to each of the barangays in selecting those who have knowledge of their medicinal plants and practices. The respective barangay tribal leaders assisted interviews among respondents with no appointments made prior to the visits. The semi-structured questionnaire used was modified and adapted from the Traditional Knowledge Digital Library (TKDL) template, as suggested by the Department of Health—Philippine Institute of Traditional and Alternative Health Care (DOH-PITAHC) (see Additional file 1 ). The Ethics Review Committee of the Graduate School, University of Santo Tomas (USTGS-ERC), approved the study and the questionnaire used with a valid translation to Manobo dialect ( Minanubu ) with the help of a community member and NCIP officer. It has series of questions about the common health problems encountered by the respondents; the actions undertaken to address such problems; the medicinal plants they used (local or vernacular name); the plant’s part(s) used, forms, modes, quantity or dosage, and frequency of administration; the source or transfer of knowledge; and the experienced adverse or side effects. Interviews were accompanied by nurses and allied workers as coordinated by the rural health center to verify reported diseases accurately by the informants.
Meetings and focus group discussions were also performed to review the accuracy of acquired data among the respondents with the help of guided questions among the tribal council of elders comprising the NCIP-recognized indigenous peoples mandatory representatives (IPMRs), the tribal chieftains, the tribal healers, and the respective tribal leaders of every barangay tribal communities together with the NCIP officer.
Plant collection and identification
The collection of plant specimens was conducted through guided field walks with the aid of the traditional healers, expert plant gatherers, and members within the tribal community. The plant habit, habitat, morphological characteristics, vernacular names, and some indigenous terms of their uses were documented. Leaf samples were placed in zip-locked bags containing silica gel for molecular analysis [ 50 ] in preparation for further molecular confirmation. Voucher specimens were deposited in the University of Santo Tomas Herbarium (USTH). Putative plant identification using vernacular names was compared to the reference of local names, Dictionary of Philippines Plant Names by [ 51 ]. Plant identification was assisted by Mr. Danilo Tandang, a botanist and researcher at the National Museum of the Philippines. Specimens unidentifiable by morphology were selected for molecular confirmation. All scientific names were verified and checked for spelling and synonyms and family classification using The Plant List [ 52 ], World Flora Online [ 53 ], The International Plant Names Index [ 54 ], and Tropicos [ 55 ]. The occurrence, distribution, and species identification were further verified using the updated Co’s Digital Flora of the Philippines [ 56 ].
DNA extraction, amplification, and sequencing
Collected plant specimens with insufficient material for identification due to lack of reproductive parts and unfamiliarity were subjected to molecular confirmation. The total genomic DNA was extracted from the silica gel-dried leaf tissues of samples following the protocols of DNeasy Plant Minikit (Qiagen, Germany). The ITS (nrDNA), mat K, trn H- psb A, and trn L-F (cpDNA) markers were used for this study. Primer information and PCR conditions used for amplification using Biometra T-personal cycler (Germany) can be found in Table Table1 1 for future parameter reference. PCR amplicons were checked on a 1% TBE agarose to inspect for the presence and integrity of DNA. Amplified products were sent to Eurofins Genomics (Germany) for DNA sequencing reactions. Sequences were then assembled and edited using Codon Code Aligner v4.1.1. All sequences were then evaluated and compared using BLAST n search query available in the GenBank ( www.ncbi.nlm.nih.gov ). The BLAST n method estimates the reliability of species identification as a sequence similarity search program to determine the sequence of interest [ 62 ] regardless of the age, plant part, or environmental factors of the sample [ 63 ].
Gene regions, primers and amplification protocols used for polymerase chain reaction
| Gene region | Primer name | Reference | Primer sequence (5′ ➔ 3′) | PCR Protocol |
|---|---|---|---|---|
| ITS (ITS1, 5.8S gene, and ITS2) | F | [ ] | 5′- -3′ | 94 °C 5 min; 28 cycles of 94 °C 1 min, 48 °C 1 min, 72 °C 1 min; 72 °C 7 min; 10 °C paused |
| S R | 5′- -3′ | |||
| [ ] | 5′- -3′ | 94 °C 5 min; 30 cycles of 94 °C 1 min, 55 °C 1 min, 72 °C 1 min, 45 s; 72 °C 10 min; 10 °C paused | ||
| 5′- -3′ | ||||
| K | F F | [ ] | 5′- -3′ | 98 °C 45 s; 35 cycles of 98 °C 10 s, 52 °C 30 s, 72 °C 40 s; 72 °C 10 min; 10 °C paused |
| R R | 5′- -3′ | |||
| A- H | A F | [ ] | 5′- -3′ | 95 °C 4 min; 35 cycles of 94 °C 30 s, 55 °C 1 min, 72 °C 1 min; 72 °C 10 min; 10 °C paused |
| H R | 5′- -3′ | |||
| L-F | [ ] | 5′- -3′ | 94 °C 3 min; 30 cycles of 93 °C 1 min; 55 °C 1 min, 72 °C 2 min; 10 °C paused | |
| 5′- -3′ |
Quantitative ethnopharmacological analysis
The use-report (UR) is counted as the number of times a medicinal plant is being used in a particular purpose in each of the categories [ 21 , 24 ]. Only one use-report was counted for every time a plant was cited as being used in a specific disease or purpose and even multiple disease or purpose under the same category [ 64 ]. Multiple use-reports were counted when at least two interviewees cited the same plant for the same disease or purpose. The use value (UV) developed by [ 45 ] is used to indicate species that are considered highly important by the given population using the following formula: UV = (ΣUi)/ N , where Ui is the number of UR or citations per species and N is the total number of informants [ 47 , 48 ]. High UV implies high plant use-reports relative to its importance to the community and vice versa. However, it does not determine whether the use of the plant is for single or multiple purposes [ 21 , 24 ]. The relative importance of the plants was also determined by calculating the cultural importance value (CIV) by using the formula: CIV = Σ[(ΣUR)/ N ], where UR is the number of use-reports in use category and N is the number of informants reporting the plant [ 48 ]. The use diversity (UD) of each medicinal plant used was determined using the Shannon index of uses as calculated with the R package vegan [ 65 ].
The ICF introduced by [ 66 ] was used to analyze the degree of informants’ agreement based on their medicinal plant knowledge in each of the categories [ 21 , 24 ]. This is computed using the formula: ICF = (Nur − Nt)/(Nur − 1), where Nur is the number of UR in each category, and Nt is the number of species used for a particular category by all informants. Fidelity level (FL) developed by [ 67 ] is calculated using the formula: FL (%) = (Ip/Iu) × 100, where Ip is the number of informants who independently suggested a given species for a particular disease, and Iu is the total number of informants who mentioned the plant for any use or purpose regardless of category. The maximum value (1.00) means a high degree of informant agreement showing the effectiveness of medicinal plants in each ailment category [ 68 ]. However, a minimum value (0.00) implies no information exchange among the informants [ 69 ]. Jaccard’s similarity index (JI) by [ 70 ] was calculated to evaluate the similarity of medicinal plant species among the three studied areas. The formula of JI is represented as follows: J = C /( A + B ), where A is the number of species found in habitat a, B is the number of species found in habitat b, and C is the number of common species found in habitats a and b. The number species present in either of the habitats is given by A + B (Jaccard).
Statistical tools
The plant URs were computed and analyzed using IBM SPSS Statistics software v.23 [ 71 ]. Descriptive and non-parametric inferential statistics Mann-Whitney U and Kruskal-Wallis tests were employed to test for significant differences at 0.01 level of significance. These two statistical analyses measure and compare the medicinal plant use and knowledge of informants when grouped according to location, education, gender, social position, occupation, civil status, and age. The basic values and indices (UR, UC, UV, CIV, UD) were correlated using the Spearman correlation coefficient to compare variables that are not distributed normally.
Integrative molecular confirmation
Selected plant samples unidentifiable by morphology were subjected to an integrative molecular identification approach as previously recommended by [ 42 ] for accurate species identification of plant samples. Selected plant samples were compared with the available morphological characteristics, interview data on vernacular names and traditional knowledge, determining scientific names based on reference of local names using the Dictionary of Philippines Plant Names by [ 51 ], and utilizing multiple molecular markers, ITS (nrDNA), mat K, trn H- psb A, and trn L-F (cpDNA) for sequencing and BLAST matching. Two sequence similarity-based methods using BLAST [ 72 ] were applied for molecular confirmation. BLAST similarity-based identification was adapted from the study of [ 42 ] with a slight modification. This identification involved using the simple method taking the top hits and optimized approach. All successfully sequenced samples were sequentially queried using megablast [ 72 ] online at NCBI nucleotide BLAST against the nucleotide database. For the simple method, all top hits within a 5-point deviation down of the max score were considered. If the max score (− 5 points) showed only a single species, then a species level identification was assigned. On the other hand, if the max score (− 5 points) showed several species but similar genus, then a genus level identification was assigned. However, if the max score (− 5 points) showed multiple species in several genera of the same family, then a family level identification was assigned. In addition, within a 5-point deviation down of the max score, the highest max score and the highest percent identity were also determined. From the top 5 hits down of the max score, an optimized method using the formula, [max score (query cover/identity)], was calculated.
The integrative molecular confirmation combined the simple and optimized BLAST-based sequence matching results with reference of local names, and comparative morphology. As a result, all species identity and generic and familial affinity were further confirmed from the recorded occurrence and distribution of putative species in the study area based on the updated Co's Digital Flora of the Philippines [ 56 ].
Demography of Informants
A total of 335 Agusan Manobo key informants (more than 10% of the total Manobo population of selected barangays) including traditional healers, leaders, council, and members were interviewed comprised with 106 female and 229 male individuals in an age range from 18–87 years old (median age of 42 years). We considered key informants those who are certified Agusan Manobo and knowledgeable with their medicinal plant uses and practices, may it be tribal officials, elders, and members of the community. Demographics by location, educational level, gender, social position, occupation, civil status, and age of participants are summarized in Table Table2 2 .
Sociodemographic profile of the Manobo key informants in Sibagat, Esperanza, and Bayugan City, Agusan del Sur
| Category | Subcategory | No. of informants | % of informants |
|---|---|---|---|
| Location | Bayugan City | 150 | 44.8 |
| Sibagat | 90 | 26.9 | |
| Esperanza | 95 | 28.4 | |
| Education level | Primary | 57 | 17.0 |
| Secondary | 167 | 49.9 | |
| Higher education | 111 | 33.1 | |
| Gender | Male | 229 | 31.6 |
| Female | 106 | 68.4 | |
| Social Position | Tribal chieftain (Datu) | 45 | 13.4 |
| Tribal healer | 3 | 0.90 | |
| Tribal IPMR | 6 | 1.80 | |
| Tribal leader | 31 | 9.30 | |
| NCIP focal person | 4 | 1.20 | |
| council of elders | 7 | 2.10 | |
| members | 239 | 71.3 | |
| Occupation | Farming | 205 | 61.2 |
| Animal husbandry | 47 | 14.0 | |
| Employed | 49 | 14.6 | |
| Unemployed | 16 | 4.80 | |
| Others | 18 | 5.40 | |
| Civil Status | Single | 187 | 55.8 |
| Married | 133 | 39.7 | |
| Others | 15 | 4.50 | |
| Age | 18–34 years old | 142 | 42.4 |
| 35–49 years old | 103 | 30.7 | |
| 50–65 years old | 53 | 15.8 | |
| More than 65 years | 37 | 11.0 |
Medicinal plant knowledge of Agusan Manobo
The majority of the respondents (90.45%) cited their acquisition of medicinal plant knowledge from their parents. They also mentioned other sources of knowledge like fellow tribe band (67.76%), relatives (64.48%), community (61.49%), and through self-discovery (47.76%). However, the descriptive and inferential statistics revealed varying factors affecting the medicinal plant knowledge among the sampled key informants.
When grouped according to location, there was no significant difference on their medicinal plant knowledge as revealed in Kruskal-Wallis test ( p = 0.379) where the city of Bayugan had the highest number of UR (Md = 112, n = 150), followed by the two municipalities, Esperanza (Md = 111, n = 95) and Sibagat (Md = 108, n = 90). These results showed an exchange of information on these adjacent localities among the Manobo community might it be the council of elders and members who are medicinal plant gatherers, peddlers, and traders.
However, when grouped according to education, respondents who had secondary level as their highest educational attainment (Md = 116, n = 167) showed the topmost medicinal plant knowledge when compared to primary (Md = 105, n = 57) and tertiary (Md = 92, n = 111) as revealed by the highly significant difference presented in Kruskal-Wallis test ( p < 0.001). These results implied that respondents who finished tertiary were more educated with modern medicine and highly acquainted with commercial drugs available over-the-counter for immediate treatment and therapy of their health problems. On the other hand, members with lower educational levels had more medicinal plant knowledge, and most traditional healers, gatherers, and peddlers finished at most on the secondary level.
When grouped according to gender, non-parametric tests revealed that men (Md = 116, n = 229) had more medicinal plant knowledge than women (Md = 104, n = 106), as demonstrated by the significant difference in both Mann-Whitney U test ( p < 0.001) and Kruskal-Wallis test ( p < 0.001). It can be observed that men had more medicinal plant knowledge in Agusan Manobo culture, an observation supported by the fact that in two of the three selected localities, the tribal healers were males, and most of the tribal officials were also males. These results revealed contrary to the previous statistical findings of [ 21 ] in the Ati culture of Visayas where women were more knowledgeable than men because they were more involved in medicinal plant gathering and peddling, and women also played a big role in caring for their sick children.
Also, knowledge of the participants when grouped according to social position varied significantly, as revealed by the Kruskal-Wallis test ( p < 0.001). These results showed that the tribal healers remained the most knowledgeable (Md = 189, n = 3), followed by the Manobo tribal officials (Md = 172, n = 93) with more medicinal plant knowledge when compared to other members of the community (Md = 104, n = 239). The medicinal plant knowledge also varied among the Manobo tribal officials, namely tribal leaders (Md = 178, n = 31), tribal IPMRs (Md = 177, n = 6), tribal chieftains (Md = 172, n = 45), Manobo tribal council of elders (Md = 164, n = 7), and Manobo NCIP focal persons (Md = 160, n = 4).
When grouped according to the occupation, non-parametric Kruskal-Wallis test also significantly revealed ( p < 0.001) that informants with occupation in farming (Md = 118, n = 205) and animal husbandry (Md = 116, n = 47) had more medicinal plant knowledge compared to employed (Md = 98, n = 49) and unemployed (Md = 96, n = 16) informants. These results suggested that Manobo people working in line with agriculture were more exposed to medicinal plant knowledge. They were farming crops or raising animals in hinterlands and mountainous areas where most medicinal plants were located. Also, when grouped according to civil status, married informants (Md = 136, n = 147) showed higher medicinal plant knowledge than single ones (Md = 92, n = 188) as revealed by the very high significant difference in both Mann-Whitney U test ( p < 0.001) and Kruskal-Wallis test ( p < 0.001). These results implied that married respondents were more exposed during community gatherings, which involved discussions about medicinal plants with regard to their uses and applications. Exchange of information could be observed when couples were present during the scheduled tribal meetings.
Finally, when grouped according to age, descriptive and inferential statistics revealed that respondents from the age group of more than 65 years old had the highest medicinal plant knowledge (Md = 173, n = 37), followed by 50–65 years old (Md = 155, n = 53), 35–49 years old (Md = 102, n = 103), and 18–24 years old (Md = 96, n = 142), as revealed by the highly significant difference manifested in Kruskal-Wallis test ( p < 0.001). These results corresponded to our expectation because older informants most likely had more knowledge of medicinal plant uses and practices based on their long-term experience. These results may also imply that younger generations were becoming more acquainted and educated with modern therapeutic treatment making them more reluctant in their traditional medicinal plant practices like gathering and peddling. This transforming awareness, social, and cultural experiences could influence their medicinal plant interest, traditional knowledge, and attitudes among the Agusan Manobo . Younger generations are becoming more privileged to be educated as part of the government scholarship programs for indigenous communities resulting in migration to urban communities.
Medicinal plants used
A total of 122 reported medicinal plant species belonging to 108 genera and 51 families were classified in 16 use categories, as shown in Tables Tables3 3 and and4. 4 . All informants interviewed agreed about the healing power of medicinal plants, but only 58.5% of the informants use medicinal plants to treat their health conditions. While some respondents (30.75%) directly relied on seeking for tribal healers in their community, still all these Babaylans utilized their known medicinal plants for immediate treatment and therapy. The Agusan Manobo community believed that the combined healing gift and prayers of their Babaylans could increase the healing potential of their medicinal plants. However, the minority (10.75%) of the key informants depended on seeing a medical practitioner and allied health workers in the treatment of their health conditions at a nearby hospital or health center.
Use-reports (URs), use values (UVs), and informant consensus factors (ICFs) in every use category (UC).
| UC No. | UC names and abbreviations | Reported diseases or uses under each UC | No. of use-report | % of all use-reports | No. of species | % of all species | UV | ICF |
|---|---|---|---|---|---|---|---|---|
| 1 | Diseases caused by bacterial, viral, and parasitic infections (BVP) | Ascariasis, chicken pox, herpes simplex, scabies, jaundice (hepatitis), mumps (parotitis), athlete's foot, warts, amoebiasis, white spot (tinea flava), impetigo, measles, colds (influenza), dengue fever, malaria, typhoid fever, ringworm | 3588 | 8.70 | 61 | 9.49 | 3.04 | 0.98 |
| 2 | Tissue growth problems (TGP) | Cancer, cyst, tumor (myoma) | 991 | 2.40 | 18 | 2.80 | 0.95 | 0.98 |
| 3 | Endocrine, nutritional, and metabolic (ENM) | Diabetes, tonic, beriberi, hormonal imbalance, goiter | 1367 | 3.31 | 36 | 5.60 | 1.03 | 0.97 |
| 4 | Diseases of the nervous system (DNS) | Migraine, Parkinson's disease, nervous breakdown (depression, anxiety, mental stress, nervousness) | 239 | 0.58 | 7 | 1.09 | 0.19 | 0.97 |
| 5 | Diseases of the eye (EYE) | Sore eyes, cataract, eye problem (blurred vision, conjunctivitis, eye infection) | 308 | 0.75 | 8 | 1.24 | 0.25 | 0.98 |
| 6 | Diseases of the ear (EAR) | Ear congestion, ear infection, discharging ear (otorrhea) | 410 | 0.99 | 8 | 1.24 | 0.36 | 0.98 |
| 7 | Diseases of the circulatory system (DCS) | Anemia, hypertension, varicose veins, heart problem (enlargement), internal bleeding, hemorrhage | 1333 | 3.23 | 31 | 4.82 | 0.92 | 0.98 |
| 8 | Diseases of the respiratory system (DRS) | Asthma, pneumonia, emphysema, pulmonary tuberculosis, nasal congestion, lung nodule, cough, cough with phlegm, respiratory disease complex (rhinitis, tracheitis, bronchitis), sore throat (tonsillitis) | 3896 | 9.44 | 67 | 10.42 | 2.66 | 0.98 |
| 9 | Diseases of the digestive system (DDS) | Constipation, diarrhea, stomach trouble (dysentery, stomachache, bloating), vomiting (nausea), peptic ulcer, toothache, gum swelling, indigestion (dyspepsia), mouth sore (canker sore), stomach acidity (gastritis), swollen/bleeding gums (gingivitis), pancreatitis, liver problem (fatty liver), hemorrhoids, appetite enhancer | 6322 | 15.33 | 82 | 12.75 | 4.64 | 0.99 |
| 10 | Diseases of the skin (DOS) | Boils (furuncle/carbuncle), skin eruptions, skin rashes and itchiness (eczema, dermatitis), psoriasis, pimple and acne, hair loss, dandruff | 2563 | 6.21 | 40 | 6.22 | 2.10 | 0.99 |
| 11 | Musculoskeletal system and connective tissue problems (MCP) | Joint pain (arthritis, gout), rheumatism, sprain, tendon mass nodule, swollen muscles/swellings, muscle pain | 2597 | 6.30 | 42 | 6.53 | 2.23 | 0.98 |
| 12 | Genito-urinary problems (GUP) | Urination difficulty, kidney stones, kidney problem (high uric acid and creatinine), urinary bladder swelling, dysmenorrhea, delayed or irregular menstruation, urinary tract infection | 2358 | 5.72 | 39 | 6.07 | 1.72 | 0.98 |
| 13 | Uses in pregnancy to delivery, maternal and infant care (PMI) | Pregnancy (impotence and sterility), abortifacient, labor and delivery enhancer, childbirth tool, miscarriage, maternal care, postpartum care and recovery, new-born baby care, milk production enhancer | 1914 | 4.64 | 40 | 6.22 | 1.25 | 0.98 |
| 14 | Abnormal signs and symptoms (ASS) | Abdominal pain, backache, body ache, headache, fever, weakness and fatigue (asthenia), baby teething, child sleeplessness, malaise and fatigue, “pasmo” (cramp and spasm), “bughat” (relapse), skin numbness (paresthesia), dizziness and fainting, body chills, gas pain and flatulence, hangover | 8133 | 19.72 | 88 | 13.69 | 5.84 | 0.99 |
| 15 | Other problems of external causes (OEC) | Allergy, burns, cuts and wounds, fracture and dislocation, bruises and contusions, animal bites (snake, dog), insect bites (mosquito, wasp, scorpion), poisoning, contacts with plant or animal parts | 5023 | 12.18 | 70 | 10.89 | 3.98 | 0.99 |
| 16 | Other uses (OTU) | Circumcision antiseptic and anesthetic | 205 | 0.50 | 6 | 0.93 | 0.27 | 0.98 |
Medicinal plants used by the Agusan Manobo in Agusan del Sur, Philippines
| Plant no. | Scientific name | Family | Local name | Voucher no. | UR | UC | UV | CIV | UD | Disease or purpose | Parts used | Preparation and administration | Quantity or dosage | Administration frequency | Experienced adverse or side effects | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Nees | Acanthaceae | White flower | USTH 015616 | 480 | 9 | 1.43 | 3.07 | 2.09 | Jaundice, colds, malaria; cancer; diabetes; hypertension, heart enlargement, atherosclerosis; cough, respiratory disease complex, sore throat; diarrhea, ulcer, dyspepsia, liver problem; abortifacient; fever, gas pain and flatulence | Lf, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | Can cause abortion in pregnant women |
| Boils, skin rashes and itchiness, dermatitis | Wh | E | Apply decoction as wash | 3–5 glasses | Once a day or as needed | None | ||||||||||
| 2 | (L.) Kurz | Acanthaceae | Marvelosa or Serpentina | USTH 015622 | 583 | 6 | 1.74 | 2.90 | 1.74 | Colds; diabetes, beriberi; nervous breakdown; hypertension; diarrhea, stomachache; weakness and fatigue, cramp and spasm | Lf | I | Drink decoction | 1–3 glasses | Once a day for 3–5 days | None |
| 3 | L. | Amaranthaceae | Kudyapa | USTH 015589 | 211 | 9 | 0.63 | 2.75 | 2.06 | Diabetes; anemia; cough, bronchitis; dysentery, constipation; urinary tract infection; fever | Lf | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | None |
| Labor and delivery enhancer | Sd | I | Drink water-infused powdered seeds | 1–3 glasses | Twice a day or as needed | None | ||||||||||
| Boils, psoriasis, skin rashes, eczema, pimple, acne; snake and scorpion bite | Lf | E | Apply leaves as poultice | 3–5 leaves | Thrice a day or as needed | None | ||||||||||
| 4 | L. | Anacardiaceae | Mangga | USTH 015591 | 222 | 5 | 0.66 | 2.85 | 1.47 | Constipation | Fr | I | Eat fresh fruit directly | 1–3 fruits | Thrice a day or as needed | None |
| Cough, cough with phlegm, sore throat | Lf | I | Drink hot water-infused leaves or decoction | 3–5 glasses | Twice a day or as needed | None | ||||||||||
| Diarrhea, stomach trouble; headache | Bk | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None | ||||||||||
| Scabies; cuts and wounds | Bk, Lf | E | Rub crushed leaves or scraped bark | 3–5 leaves, 1 palm-sized bark | Twice a day or as needed | None | ||||||||||
| 5 | (L.f.) Kurz | Anacardiaceae | Abihid | USTH 015599 | 372 | 4 | 1.11 | 2.33 | 1.39 | Colds; diabetes; cough; fever | Bk, Lf | I | Drink decoction of leaves and scraped bark | 3–5 glasses | Once or twice a day for 3 days or as needed | None |
| Colds; fever | Bk, Lf | E | Bath water-infused leaves and scraped bark | 1 pail | Once a day or as needed | None | ||||||||||
| 6 | L. | Annonaceae | Guyabano | USTH 015593 | 209 | 8 | 0.62 | 2.17 | 2.02 | Cancer; diabetes; hypertension; dysentery | Fr | I | Eat fresh fruit directly | 3–5 glasses | Once or twice a week or as needed | In excess can cause blood viscosity |
| Ascariasis; cough; stomach trouble, stomach acidity; urination difficulty, urinary tract infection | Lf | I | Drink decoction | 3–5 glasses | Once a day or as needed | None | ||||||||||
| Skin eruptions, eczema | Lf, Sp | E | Apply leaf sap or crushed leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 7 | (Lam.) Hook.f. & Thomson | Annonaceae | Anangilan or Ilang-ilang | USTH 015577 | 358 | 7 | 1.07 | 2.47 | 1.85 | Colds; cough; stomach trouble, ulcer; fever, body chills | Bk, Lf | I | Drink decoction | 5–7 glasses | Once or twice a day or as needed | None |
| Scabies, athlete's foot; pimple; rheumatism, swollen muscles or swellings, muscle pain; insect bites | Fl | E | Apply oil from steamed flowers | Completely on affected part | 3–5 times a day or as needed | None | ||||||||||
| 8 | (Merr.) Steen. | Annonaceae | Talimughat taas | USTH 015558 | 198 | 3 | 0.59 | 2.08 | 0.90 | Muscle pain; labor and delivery enhancer, postpartum care and recovery; backache, body ache, weakness and fatigue, cramp and spasm, relapse | Bk, Lf, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day up to 3 days or as needed | None |
| 9 | Elmer | Annonaceae | Bigo | USTH 015662 | 195 | 5 | 0.58 | 0.70 | 1.56 | Amoebiasis; hypertension; fever, weakness and fatigue | St | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Hair loss; insect bites | St, Sp | E | Apply stem sap | 1/2–1 cup | As needed | None | ||||||||||
| 10 | Wall. ex G.Don | Apocynaceae | Dita | USTH 015546 | 386 | 9 | 1.15 | 2.71 | 2.04 | Tonic; ear congestion; cough; stomach trouble, toothache; urinary tract infection; abdominal pain, weakness and fatigue, hangover | Bk, Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Cuts and wounds, bruises and contusions, sprain | Lf | E | Apply crushed and heated leaves as poultice | 3–5 leaves | Once or twice a day or as needed | None | ||||||||||
| Scabies, impetigo, ringworm; boils | Bk | E | Apply water-infused powdered bark | 1 glass | Once or twice a day or as needed | None | ||||||||||
| Stomachache, snake bite | Bk | E | Drink local alcohol-tinctured bark | 1/2 to 1 glass | As needed | None | ||||||||||
| 11 | (King & Gamble) D.J.Middleton | Apocynaceae | Lunas tag-uli | USTH 015639 | 1134 | 12 | 3.39 | 3.68 | 2.22 | Cancer; diabetes; ear infections; diarrhea, stomach trouble, ulcer, toothache; arthritis, rheumatism; pregnancy; body ache, weakness and fatigue, cramp and spasm, relapse; poisoning | Sp, St | I | Drink stem sap | 1–3 glasses | Once a day or as needed | None |
| Colon and prostate cancer, cyst, tumor; diabetes; hypertension; pulmonary tuberculosis; diarrhea, stomach trouble, ulcer, toothache, swollen gums; arthritis, rheumatism; impotence and sterility, postpartum care and recovery; body ache, weakness and fatigue, cramp and spasm, relapse, gas pain, and flatulence; sprain; poisoning | St | I | Drink local alcohol-tinctured or decocted stem | 1/2 to 1 glass | Once or twice a day or as needed | None | ||||||||||
| Scabies, warts, impetigo, typhoid fever; boils, skin eruptions, skin rashes, and itchiness; arthritis, rheumatism, swellings, muscle pain; backache, body ache, weakness and fatigue, cramp and spasm, relapse gas pain and flatulence; allergy, burns, cuts and wounds, sprain, animal and insect bites, contacts with plants and animal parts | St | E | Apply coconut or Efficascent oil-infused stem | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| 12 | Decne. | Apocynaceae | Pikot-pikot | USTH 015618 | 57 | 2 | 0.17 | 0.86 | 0.69 | Boils; cuts and wounds | Lf | E | Apply coconut oil-infused burned and powdered leaves | Completely on affected part | As needed | None |
| 13 | Schott ex Van Houtte | Araceae | Lunas gabi | USTH 015614 | 44 | 1 | 0.13 | 0.60 | 0.00 | Allergy, cuts and wounds, snake and insect bite, poisoning | Lf, Sp, St | E | Apply stem or leaf sap | Completely on affected part | Once a day or as needed | None |
| 14 | Engl. ex Engl. & K.Krause | Araceae | Payaw | USTH 015597 | 466 | 7 | 1.39 | 2.00 | 1.83 | Colds; body ache, headache, fever | Lf, St | I/E | Sniff sliced and pounded leaf and stem or tie leaf and stem around the neck | 1–3 leaves | Once a day or as needed | None |
| Tonsillitis; pregnancy, impotence and sterility, labor and delivery enhancer | Rz | I | Drink extracted juice from crushed rhizome | 1–3 cups | Once to thrice a day or as needed | None | ||||||||||
| Rheumatism; cuts and wounds | Rz | E | Apply extracted juice from crushed rhizome | Completely on affected part | As needed | None | ||||||||||
| Hemorrhoids | Lf | E | Insert heated young leaf | 1 leaf | Once or twice a day or as needed | None | ||||||||||
| 15 | L. | Araliaceae | Goto Kola | USTH 015563 | 263 | 4 | 0.78 | 1.78 | 1.39 | Diabetes; hypertension; fever | Lf | I | Eat fresh leaves directly or drink decocted leaves | 3–5 leaves; 1 cup | Once a day or as needed | In excess can cause anemia, dizziness and weakening |
| Cuts and wounds | Lf, Sp | E | Apply leaf sap or crushed leaves as poultice | 1–3 leaves | As needed | None | ||||||||||
| 16 | L. | Arecaceae | Huling-huling | USTH 015610 | 42 | 1 | 0.13 | 0.70 | 0.69 | Breast cancer | Rt | I | Drink decoction | 3–5 glasses | Once or twice a day or as needed | None |
| 17 | Becc. | Arecaceae | Kapi | USTH 015608 | 168 | 4 | 0.50 | 1.65 | 1.28 | Hypertension; asthma; diarrhea, dyspepsia, gastritis, indigestion; arthritis, rheumatism | Rz | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| 18 | (Planch. ex Rolfe) ined. | Aristolochiaceae | Salimbagat | USTH 015643 | 278 | 3 | 0.83 | 1.75 | 1.10 | Amoebiasis; cancer; toothache | Lf, Rt | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| 19 | (Schult.f.) Byng & Christenh. | Asparagaceae | Espada-espada | USTH 015647 | 78 | 2 | 0.23 | 0.67 | 0.69 | Boils; snake bite | Lf | E | Apply leaf sap or pounded leaves as poultice | 5–7 drops | As needed | None |
| 20 | (Turcz.) R.K.Jansen | Asteraceae | Lunas pilipo | USTH 015548 | 396 | 4 | 1.18 | 2.40 | 1.33 | Toothache; anesthetic | Fl | I | Apply fresh flower directly | 1–3 flowers | As needed | None |
| Skin rashes and itchiness, psoriasis; cuts and wounds; anesthetic | Fl, Lf | E | Apply crushed flower or leaves as poultice | 1–3 flowers, 5–7 leaves | As needed | None | ||||||||||
| 21 | L. | Asteraceae | Albahaca | USTH 015602 | 77 | 3 | 0.23 | 1.89 | 1.10 | Abortifacient; weakness and fatigue | Lf | I | Drink decoction | 1–3 cups | Once a day or as needed | Can cause abortion in pregnant women |
| Cuts and wounds | E | Apply pounded leaves as poultice | 1–3 leaves | Once or twice a day or as needed | None | |||||||||||
| 22 | L. | Asteraceae | Helbas | USTH 015619 | 365 | 4 | 1.09 | 1.60 | 1.24 | Asthma, cough, cough with phlegm; diarrhea, dyspepsia; delayed menstruation; relapse | Lf | I | Drink decoction | 1–3 glasses | Thrice a day or as needed | In excess can cause anemia, dizziness and weakening |
| Abdominal pain, body ache, fever, cramp, and spasm | Lf | E | Apply crushed leaves as poultice | 3–5 leaves | Once a day or as needed | None | ||||||||||
| 23 | L. | Asteraceae | Tuway-tuway | USTH 015582 | 218 | 5 | 0.65 | 1.67 | 1.26 | Colds; diarrhea; muscle pain; backache, body ache, fever, weakness and fatigue, cramp and spasm, relapse, gas pain, and flatulence | Rt | I | Drink decoction | 3–5 glasses | Once or twice a day up to 3 days or as needed | None |
| Cuts and wounds, animal and insect bites | Lf | E | Apply crushed leaves as poultice | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| 24 | (L.) DC. | Asteraceae | Gabon | USTH 015573 | 412 | 6 | 1.23 | 2.60 | 1.58 | Hypertension; cough, cough with phlegm; urination difficulty; postpartum care and recovery; body ache, headache, fever, weakness and fatigue, gas pain and flatulence | Lf, Rt | I | Drink decoction | 3–5 glasses | Once or twice a day for 3 days or as needed | None |
| Headache | Lf | E | Apply steamed or pounded leaves in the forehead | 1–3 leaves | Once a day or as needed | None | ||||||||||
| Boils, skin rashes | Lf | E | Apply leaves as poultice | 1–3 leaves | Once or twice a day or as needed | None | ||||||||||
| 25 | (L.) R.M.King & H.Rob. | Asteraceae | Hagonoy | USTH 015632 | 448 | 5 | 1.34 | 2.50 | 1.56 | Tumor; hemorrhage; fever | Lf | I | Drink decoction | 3–5 glasses | Once a day for 3 days or as needed | None |
| Boils; burns, cuts, and wounds | Lf | E | Apply leaf sap or crushed leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 26 | (L.) H.Rob. | Asteraceae | Kanding-kanding | USTH 015587 | 476 | 5 | 1.42 | 2.78 | 1.42 | Colds, malaria; pulmonary tuberculosis; dog bite | Lf, Rt | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | None |
| Chicken pox, herpes simplex, measles; boils, skin eruptions, skin rashes and itchiness; weakness and fatigue, cramp and spasm | Fl, Lf, Rt | E | Bath water-infused leaves and roots or burn leaves and roots as incense | 1 pail as bath or 1 bowl as incense | Once or twice a day or as needed | None | ||||||||||
| 27 | (Link ex Spreng.) DC. | Asteraceae | Gapas-gapas bae | USTH 015666 | 208 | 3 | 0.62 | 2.25 | 1.01 | Stomachache, dyspepsia; body ache, headache, gas pain, and flatulence | Lf | I | Drink decoction | 3–5 glasses | Once or twice a day or as needed | None |
| Cuts and wounds | Lf, Sp | E | Apply sap or leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 28 | (Lour.) Merr. | Asteraceae | Ashitaba | USTH 015645 | 215 | 4 | 0.64 | 2.50 | 1.33 | Emphysema, cough; diarrhea, stomach trouble; kidney stones; abdominal pain | Lf | I | Drink brewed tea-prepared leaves or decoction | 3–5 cups | Once or twice a day or as needed | None |
| 29 | (Burm.f.) B.L.Rob. | Asteraceae | Moti-moti | USTH 015543 | 397 | 6 | 1.19 | 2.75 | 1.67 | Cough; ulcer | Lf | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| Sore eyes | Lf, Sp | I | Drop leaf sap | Completely on affected part | As needed | None | ||||||||||
| Skin rashes and itchiness; cuts and wounds, snake and scorpion bites; circumcision antiseptic | Lf | E | Apply leaf sap or crushed leaves as poultice | 5–7 leaves | As needed | None | ||||||||||
| 30 | (Juss.) Rohr | Asteraceae | Kukog banog | USTH 015564 | 500 | 5 | 1.49 | 2.50 | 1.44 | Urination difficulty, kidney problem, urinary bladder swelling, delayed menstruation, urinary tract infection; fever, weakness and fatigue, cramp and spasm | Lf, Rt | I | Drink brewed tea-prepared leaves or decoction | 3–5 glasses | Once a day or as needed | None |
| Sore eyes; eczema, skin rashes, and itchiness; cuts and wounds, sprain, snake bite | Lf, Sp | E | Apply drops of leaf sap | Completely on affected part | Thrice a day or as needed | None | ||||||||||
| 31 | (Retz.) Sw. | Athyriaceae | Pako-pako | USTH 015545 | 212 | 5 | 0.63 | 1.92 | 1.56 | Colds; cough; diarrhea, dysentery; labor and delivery enhancer, postpartum care and recovery; body ache, headache, fever | Sh | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| 32 | Warb. | Begoniaceae | Budag-budag | USTH 015654 | 85 | 2 | 0.25 | 1.33 | 0.64 | Pimple, dandruff; burns | Fl, Lf | E | Apply crushed flower and leaves as poultice | 1–3 flowers, 1–3 leaves | Once to thrice a day or as needed | None |
| 33 | (L.) Gaertn. | Bombacaceae | Doldol | USTH 015535 | 140 | 5 | 0.42 | 2.14 | 1.55 | Diabetes; pulmonary tuberculosis; diarrhea, dysentery; rheumatism, swollen muscles; snake bite | Bk, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 34 | Lam. | Boraginaceae | Alangitngit or Tsaang-Gubat | USTH 015638 | 336 | 4 | 1.00 | 2.60 | 1.39 | Diabetes; nervous breakdown; stomach acidity; food and drug allergy | Lf | I | Drink tea-prepared leaves | 1/2 to 1 cup | Once a day for 3 days or as needed | None |
| 35 | (L.) Merr. | Bromeliaceae | Pinya | USTH 015667 | 226 | 7 | 0.67 | 1.71 | 1.85 | Ascariasis, amoebiasis; cancer; diabetes; hypertension; constipation, stomach acidity | Fr | I | Eat fresh fruit directly | 1–3 slices | Once to thrice a day or as needed | None |
| Headache, fever, weakness, and fatigue | Lf, Sh | E | Apply crushed shoot or leaves as poultice | Completely on affected part | As needed | None | ||||||||||
| Cancer; swellings | Lf | I/E | Drink decoction or apply decocted leaves | 3–5 leaves | Once a day or as needed | None | ||||||||||
| 36 | (L.) L.f. | Byttneriaceae | Samboligawn | USTH 015637 | 329 | 8 | 0.98 | 2.69 | 1.98 | Diabetes, tonic; bronchitis; stomachache; dysmenorrhea, irregular menstruation; sterility | Bk, Lf, Rt | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| Scabies; boils, skin eruptions, dermatitis; cuts and wounds | Bk, Lf | E | Apply decoction as wash | 1–3 glasses | Once or twice a day or as needed | None | ||||||||||
| 37 | L. | Byttneriaceae | Bitan-ag | USTH 015631 | 146 | 6 | 0.44 | 2.50 | 1.70 | Tumor; asthma, pneumonia, cough; dyspepsia, liver problem; headache; baby teething | Lf | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | None |
| Scabies; psoriasis | Lf | E | Apply crushed leaves as poultice | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| 38 | (Houtt.) Stapf | Byttneriaceae | Banitlong | USTH 015649 | 265 | 4 | 0.79 | 1.76 | 1.24 | Rheumatism; backache, body ache, headache | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Canker sore; burns | Lf | E | Apply leaves as poultice | 3–5 leaves | Once a day or as needed | None | ||||||||||
| 39 | (L.) G.Don | Campanulaceae | Elepanteng puti | USTH 015583 | 213 | 5 | 0.64 | 1.83 | 1.56 | Toothache | Lf | I | Apply chewed or pounded leaves | 1–3 leaves | Once or twice a day or as needed | None |
| Nervous breakdown; asthma, bronchitis; fever | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None | ||||||||||
| Cuts and wounds | Lf | E | Apply decoction | 1 glass | As needed | None | ||||||||||
| 40 | L. | Caricaceae | Kapayas laki | USTH 015668 | 659 | 6 | 1.97 | 2.92 | 1.64 | Constipation, dyspepsia; milk production enhancer | Fr | I | Eat fresh fruit directly | 1–3 slices | Once a day or as needed | None |
| Tonic; asthma; stomach problem | Lf, Rt | I | Drink decoction | 3–5 glasses | Once a day or as needed | None | ||||||||||
| Dengue fever | Lf, Sp | I | Drink leaf sap | 5–7 leaves | Thrice a day or as needed | None | ||||||||||
| Body ache, fever, cramp, and spasm | Lf | I | Apply crushed and heated leaves as poultice | 1–3 leaves | Twice a day or as needed | None | ||||||||||
| 41 | (Jack) Blume | Clusiaceae/Guttiferae | Bansilay | USTH 015541 | 96 | 4 | 0.29 | 2.33 | 1.33 | Colds; cough; dysentery | Bk, Lf, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Toothache | Lf | I | Apply chewed or pounded leaves | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| Impetigo; cuts and wounds | Lf | E | Apply pounded leaves as poultice | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| 42 | (J.Koenig) Govaerts | Costaceae | Tambabasi or Tawasi | USTH 015578 | 744 | 8 | 2.22 | 2.58 | 2.03 | Diabetes, goiter; migraine; ear congestion; cough, lung nodule; urination difficulty, kidney problem; headache, fever | Lf, Rz | I | Drink decoction | 3–5 glasses | Once to thrice a day up to 3 days or as needed | None |
| Diarrhea, stomachache, dysentery | St | I | Drink stem sap | 1/2 cup | As needed | None | ||||||||||
| Sore eyes | Lf | I | Apply leaf sap | Completely on affected part | As needed | None | ||||||||||
| 43 | (Lam.) Pers. | Crassulaceae | Hanlilika | USTH 015584 | 486 | 12 | 1.45 | 2.88 | 2.21 | Diabetes; anemia, hypertension; asthma; cough; constipation, diarrhea, stomach trouble, hemorrhoids; kidney stone; labor and delivery enhancer; fever | Lf | I | Drink decoction | 3–5 leaves | Once a day or as needed | None |
| Herpes simplex; hemorrhoids; boils, eczema; swellings; burns, cuts and wounds, bruises and contusions, insect bites | Lf | I | Apply decocted leaves as wash | 1–3 leaves | Once a day or as needed | None | ||||||||||
| Abdominal pain, body ache, headache, fever | Lf | E | Apply heated leaves as hot compress | 1–3 leaves | Once a day or as needed | None | ||||||||||
| 44 | (L.) H.Pfeiff. | Cyperaceae | Busikad | USTH 015571 | 254 | 6 | 0.76 | 1.38 | 1.61 | Chicken pox, measles; cancer; cough; stomach acidity; fever, relapse, gas pain and flatulence; sprain | Wh | I | Drink decoction | 1–3 glasses | Once to thrice a day or as needed | None |
| Baby teething | Fl | I | Drink water-infused flower | 1/2–1 glass | Once to thrice a day | None | ||||||||||
| 45 | Oliv. | Dioscoreaceae | Banag | USTH 015537 | 540 | 6 | 1.61 | 2.36 | 1.70 | Myoma; migraine; arthritis, rheumatism; urination difficulty, urinary bladder swelling; postpartum care and recovery; headache, cramp and spasm, relapse | Rt | I | Drink decoction | 3–5 glasses | Once or twice a day for 3 days or as needed | None |
| 46 | L. | Euphorbiaceae | Tawa-tawa | USTH 015665 | 305 | 7 | 0.91 | 2.80 | 1.85 | Colds, dengue fever; asthma; diarrhea, vomiting; fever | Wh | I | Drink decoction of whole plant except flowers | 5–7 glasses | Thrice a day or as needed | In excess can cause thrombocytopenia |
| Ringworm; sore eyes; boils, skin rashes, and itchiness; cuts and wounds | Lf | I/E | Apply leaf sap or decocted leaves | 5–7 leaves | Thrice a day or as needed | None | ||||||||||
| 47 | L. | Euphorbiaceae | Tuba-tuba puti | USTH 015595 | 495 | 7 | 1.48 | 2.66 | 1.79 | Colds; pulmonary tuberculosis; diarrhea; arthritis, rheumatism; backache, body ache, fever, weakness and fatigue, cramp and spasm, relapse, gas pain, and flatulence | Lf, Rt | I | Drink decoction | 1–3 leaves | Once a day or as needed | None |
| Scabies, ringworm; ear infection, discharging ear; toothache; swollen muscles and swellings; cuts and wounds, fracture and dislocation, animal and insect bites | Bk, Rt | I/E | Apply decoction or pounded scraped bark as poultice | 1–3 palm-sized barks, 1/2–1 arm-sized roots | As needed | None | ||||||||||
| 48 | L. | Euphorbiaceae | Tuba-tuba tapol | USTH 015586 | 810 | 9 | 2.41 | 2.83 | 1.94 | Colds, malaria, typhoid fever; pulmonary tuberculosis; diarrhea; arthritis, rheumatism; dysmenorrhea, irregular menstruation; backache, body ache, fever, weakness and fatigue, cramp and spasm, relapse, gas pain, and flatulence | Lf, Rt | I | Drink decoction | 1–3 leaves, 1/2–1 arm-sized roots | Once a day or as needed | None |
| Ringworm; boils, carbuncles, dermatitis; swollen muscles and swellings, muscle pain; backache, body ache, fever; cuts and wounds | Lf | E | Bath or wash decocted leaves | 1–3 leaves | Once a day or as needed | None | ||||||||||
| Scabies, ringworm; ear infection, discharging ear; toothache, mouth sore; cuts and wounds, fracture and dislocation, animal and insect bites | Bk, Rt | I/E | Apply decoction or pounded scraped bark as poultice | 1–3 palm-sized barks, 1/2–1 arm-sized roots | As needed | None | ||||||||||
| 49 | (Reinw. ex Blume) Rchb. & Zoll. | Euphorbiaceae | Awom | USTH 015621 | 485 | 5 | 1.45 | 2.33 | 1.56 | Beriberi; emphysema, cough; diarrhea, stomach trouble | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Fibroma; body ache, weakness, and fatigue | Bk, Fl, Lf | E | Apply fresh or heated flower, leaves, and bark; sometimes mixed with little salt | 1–3 flowers, 1–3 leaves, 1–3 palm-sized barks | Once or twice a day or as needed | None | ||||||||||
| 50.1 | Pax & Hoffm. | Euphorbiaceae | Banti puti | USTH 015633 | 202 | 3 | 0.60 | 1.77 | 1.04 | Impetigo; diarrhea, stomach trouble; cuts and wounds | Lf | E | Apply pounded leaves as poultice | 3–5 leaves | Once to thrice a day or as needed | None |
| 50.2 | Pax & Hoffm. | Euphorbiaceae | Banti tapol | USTH 015554 | 203 | 3 | 0.61 | 1.60 | 1.04 | Impetigo; diarrhea, stomach trouble; cuts and wounds | Lf | E | Apply pounded leaves as poultice | 3–5 leaves | Once to thrice a day or as needed | None |
| 51 | sp. | Fabaceae | Talimughat pikas | USTH 015575 | 284 | 4 | 0.85 | 1.50 | 1.22 | Rheumatism, muscle pain; delayed menstruation; labor and delivery enhancer, postpartum care and recovery; backache, body ache, weakness and fatigue, cramp and spasm, relapse | Lf, St | I | Drink decoction | 3–5 glasses | Once to thrice a day up to 3 days or as needed | None |
| 52 | L. | Fabaceae | Sagay-sagay | USTH 015572 | 84 | 5 | 0.25 | 1.60 | 1.24 | Myoma; hormonal imbalance; cough; constipation; fever, weakness and fatigue, relapse | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day up to 3 days or as needed | None |
| 53 | (Jacq.) Kunth ex Steud | Fabaceae | Madre de Cacao | USTH 015620 | 153 | 6 | 0.46 | 1.83 | 1.68 | Scabies; boils, skin eruption, skin rashes, and itchiness; cuts and wounds | Lf, Sp | E | Apply leaf sap or pounded leaves as poultice | Completely on affected part | Once or twice a day or as needed | None |
| Eczema, dermatitis; arthritis and rheumatism; burns, cuts and wounds, bruises and contusions | Bk, Rt, Sp | E | Apply sap or decocted bark or root | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| Abortifacient, postpartum care, and recovery | Lf | E | Burn leaves as incense or apply heated leaves as hot compress | 3–5 leaves | Once a day or as needed | None | ||||||||||
| Body ache, headache, fever; fracture and dislocation, sprain | Bk | E | Apply scraped bark as poultice | 1–3 palm-sized barks | Once a day or as needed | None | ||||||||||
| 54 | L. | Fabaceae | Hibi-hibi or makahiya | USTH 015570 | 355 | 8 | 1.06 | 2.29 | 1.97 | Diabetes; hypertension; asthma, dysentery; urination difficulty; fever | Rt | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| Baby teething | Rt | I | Drink water-infused peeled roots | 1/2 to 1 cup | Once a day or as needed | None | ||||||||||
| Mumps; boils; child sleeplessness, malaise, and fatigue | Sh | E | Apply hot water-infused shoots | 1/2 to 1 glass | As needed | None | ||||||||||
| 55 | Baker | Fabaceae | Bahay | USTH 015625 | 522 | 5 | 1.56 | 2.36 | 1.56 | Atherosclerosis (high cholesterol) | Fr | I | Eat fresh fruit directly | 1–3 fruits | Once or twice a day or as needed | None |
| Typhoid fever; nervous breakdown; high cholesterol; kidney problem; fever | Bk | I | Drink decoction or local alcohol-tinctured bark | 1/2 to 1 cup | Once or twice a day or as needed | None | ||||||||||
| Nervousness; skin numbness | Bk, Rt | E | Apply Efficascent oil-infused bark and root | Fill a 250 ml glass bottle with bark and roots | As needed | None | ||||||||||
| 56.1 | (Roxb.) Benth. | Fabaceae | Alibangbang puti | USTH 015646 | 66 | 1 | 0.20 | 1.11 | 0.00 | Internal bleeding, hemorrhage | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 56.2 | (Roxb.) Benth. | Fabaceae | Alibangbang tapol | USTH 015634 | 53 | 1 | 0.16 | 1.00 | 0.00 | Internal bleeding, hemorrhage | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 57 | R.Br. | Lamiaceae | Awoy | USTH 015661 | 378 | 4 | 1.13 | 1.50 | 1.28 | Ulcer, pancreatitis, fatty liver; weakness and fatigue, cramp and spasm | Lf | I | Drink hot water-infused leaves | 1/2 to 1 cup | Once or twice a day or as needed | None |
| Asthma | Lf | E | Burn leaves as incense | 1–3 leaves | Once or twice a day or as needed | None | ||||||||||
| Swollen muscles, muscle pain; backache, body ache | Lf | E | Apply leaves as poultice | 1–3 leaves | Once or twice a day or as needed | None | ||||||||||
| 58 | Lour. | Lamiaceae | Kalabo | USTH 015617 | 380 | 4 | 1.13 | 1.78 | 1.31 | Asthma, cough, cough with phlegm; dyspepsia; abdominal pain, gas pain, and flatulence | Lf | I | Eat leaves directly or drink decoction | 1/2 to 1 cup | Once to thrice a day or as needed | In excess can cause anemia, weakness, and allergy |
| Burns, bruised and contusions, insect bites | Lf | E | Apply water-infused leaves | 1–3 glasses | As needed | None | ||||||||||
| 59.1 | (L.) Benth. | Lamiaceae | Mayana kanapkap | USTH 015567 | 260 | 5 | 0.78 | 1.67 | 1.47 | Anemia; asthma, pneumonia, cough; dyspepsia; gas pain and flatulence | Lf | I | Drink decoction | 1–3 glasses | Once a day for 3–5 days or as needed | None |
| Cuts and wounds, bruises and contusions, sprain | Lf, Sp | E | Apply leaf sap or crushed leaves as poultice | 5–7 leaves | Twice a day or as needed | None | ||||||||||
| 59.2 | (L.) Benth. | Lamiaceae | Mayana pula | USTH 015644 | 414 | 6 | 1.24 | 2.25 | 1.59 | Anemia; asthma, pneumonia, emphysema, pulmonary tuberculosis, cough; ulcer, dyspepsia; gas pain and flatulence | Lf | I | Drink decoction | 1–3 glasses | Once a day for 3–5 days or as needed | None |
| Conjunctivitis | Lf | I | Apply decoction as drop | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| Cuts and wounds, bruises and contusions, sprain | Lf | E | Apply crushed leaves as poultice | 5–7 leaves | Twice a day or as needed | None | ||||||||||
| 60 | Roxb. ex Sm. | Lamiaceae | Gmelina | USTH 015635 | 335 | 5 | 1.00 | 1.83 | 1.49 | Toothache, gum swelling | Lf | I | Apply chewed or pounded leaves | 3–5 leaves | As needed | None |
| Discharging ear | Fr | I | Drop extract of heated fruit | 1–3 fruits | As needed | Poisonous when eaten | ||||||||||
| Stomach bloating; maternal care; headache, gas pain and flatulence; cuts and wounds | Lf | E | Apply leaves directly or as poultice | 1–3 leaves | As needed | None | ||||||||||
| 61 | Jacq. | Lamiaceae | Sawan-sawan | USTH 015574 | 498 | 7 | 1.49 | 2.56 | 1.85 | Colds, malaria; cough; diarrhea, stomachache; new-born baby care; fever, gas pain and flatulence | Lf | I | Drink decoction or leaf sap | 3–5 glasses decoction or 1/2 cup leaf sap (adult); 1/2 cup decoction or 1 teaspoonful leaf sap (baby) | Once or twice a day or as needed | None |
| Delayed menstruation | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None | ||||||||||
| Toothache; cuts and wounds | Lf | E | Apply crushed leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 62 | L. | Lamiaceae | Herba buena | USTH 015669 | 174 | 6 | 0.52 | 2.71 | 1.59 | Measles; cough; diarrhea, dysentery; dysmenorrhea; headache, fever, cramp and spasm, gas pain and flatulence | Sh | I | Drink decoction | 3–5 glasses | Once or twice a day or as needed | None |
| Asthma; dizziness and fainting | Lf | I | Sniff crushed leaves or leaves infused with hot water | 3–5 leaves | As needed | None | ||||||||||
| Toothache; headache, fever; insect bites | Lf | E | Apply chewed or crushed leaves | 3–5 leaves | As needed | None | ||||||||||
| 63 | L. | Lamiaceae | Sencia | USTH 015670 | 432 | 9 | 1.29 | 2.81 | 2.04 | Sinusitis, cough; stomachache, vomiting; delayed menstruation; backache, body ache, headache, fever, gas pain and flatulence | Lf | I | Drink hot water-infused leaves or decoction | 3–5 glasses | Once or twice a day or as needed | None |
| Ringworm; ear infection and congestion; toothache | Lf | I/E | Apply leaf sap | Completely on affected part | As needed | None | ||||||||||
| Muscle pain, abdominal pain; cuts and wounds, dislocation, snake bite | Lf | E | Apply crushed leaves as poultice | Completely on affected part | Once a day or as needed | None | ||||||||||
| Skin rashes and itchiness, acne; rheumatism; cuts and wounds; animal and insect bites | Lf | E | Apply decoction as wash | 5–7 leaves | Twice a day or as needed | None | ||||||||||
| 64 | L. | Lamiaceae | Sangig | USTH 015630 | 385 | 9 | 1.15 | 2.33 | 2.09 | Cough, cough with phlegm; constipation, diarrhea, vomiting, hemorrhoids; delayed menstruation; postpartum care and recovery; headache, fever, gas pain and flatulence | Lf, Sh | I | Drink decoction or add in soup | 3–5 glasses | Twice a day or as needed | None |
| Ear congestion, infection, and discharge | Lf, Sp | I | Drop leaf sap | 3–5 leaves | As needed | None | ||||||||||
| Boils, skin rashes, and itchiness; arthritis, rheumatism; cuts and wounds, bruises and contusions | Lf | E | Apply decoction as wash | 3–5 leaves | Twice a day or as needed | None | ||||||||||
| Toothache; cuts and wounds, snake bites | Lf, Sh | I/E | Apply crushed shoot or leaves as poultice | 3–5 leaves, 1 shoot | As needed | None | ||||||||||
| 65 | (Blume) Miq. | Lamiaceae | Wachichao | USTH 015550 | 513 | 6 | 1.53 | 2.96 | 1.58 | Diabetes; hypertension; diarrhea, stomachache; joint pain, gout, rheumatism; urination difficulty, kidney stones, kidney problem, urinary bladder swelling, prostate problem; labor and delivery enhancer | Fl, Lf | I | Drink brewed tea-prepared leaves or decoction of leaves and flower | 3–5 cups | Once or twice a day or as needed | None |
| 66 | Blanco | Lamiaceae | Abgaw | USTH 015559 | 668 | 7 | 1.99 | 2.94 | 1.79 | Colds; nasal congestion, sinusitis, cough, cough with phlegm; diarrhea, ulcer; rheumatism; postpartum care and recovery; weakness and fatigue, gas pain and flatulence | Lf | I | Drink water-infused leaves | 3–5 glasses | Once or twice a day for 3 days or as needed | None |
| Cuts and wounds | E | Apply crushed leaves as poultice | 1–3 leaves | Once or twice a day or as needed | None | |||||||||||
| 67 | (Merr.) Bakh. | Lamiaceae | Kulipapa | USTH 015603 | 128 | 4 | 0.38 | 1.18 | 1.24 | Beriberi; muscle pain; labor and delivery; backache, body ache, cramp and spasm | Rt, St | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | None |
| 68 | L. | Lamiaceae | Lagundi | USTH 015562 | 475 | 5 | 1.42 | 2.69 | 1.55 | Cough, cough with phlegm; ulcer; rheumatism; postpartum care and recovery; headache, gas pain and flatulence | Lf | I | Drink decoction | 1/4 glass (young leaf) or 1/2 glass (mature leaf) | Thrice a day or as needed | None |
| 69 | S.Vidal | Lauraceae | Kaningag | USTH 015585 | 908 | 8 | 2.71 | 3.22 | 1.93 | Amoebiasis; cancer; hypertension; cough; diarrhea, stomach trouble, ulcer, stomach acidity; kidney problem, urinary tract infection; weakness and fatigue, cramp and spasm | Bk, Br, Rt | I | Drink decoction or local alcohol-tinctured bark, stem and root | 3–5 glasses | Once or twice a day or as needed | None |
| Cuts and wounds | Bk, Br, Rt | E | Apply coconut oil-infused bark, stem and root | Completely on affected part | As needed | None | ||||||||||
| 70 | (Jack) Hook.f. | Lauraceae | Loktob | USTH 015580 | 307 | 7 | 0.92 | 2.83 | 1.79 | Mumps; cyst, tumor, myoma; goiter; asthma, pneumonia, emphysema, cough; ulcer; arthritis; kidney problem, dysmenorrhea | Bk, Rt | I | Drink hot water-infused bark or decoction | 1–3 glasses | Once a day in thrice a week for 2 months or as needed | In excess can cause anemia, dizziness and weakening |
| 71 | Merr. | Lauraceae | Efficascent | USTH 015576 | 82 | 2 | 0.24 | 1.11 | 0.69 | Cough; weakness and fatigue | Sp, St | I | Drink sap from rubbed stem | 1/2 cup | Once a day or as needed | None |
| 72 | (L.) Pers. | Lythraceae | Banaba | USTH 015596 | 384 | 4 | 1.15 | 2.57 | 1.26 | Ulcer; urination difficulty, kidney stones, high uric acid, and creatinine; maternal care; backache, body ache, fever | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 73 | L. | Malvaceae | Gapas | USTH 015553 | 283 | 3 | 0.84 | 2.14 | 0.95 | Hemorrhage; postpartum care and recovery; body ache, fever, body chills | Rt | I | Drink decoction | 1 glass | Once a day for 3 days | In excess, can cause abnormalities in lactating mothers |
| 74 | L. | Malvaceae | Eskuba laki | USTH 015601 | 768 | 8 | 2.29 | 2.55 | 1.87 | Cough; stomach trouble; kidney stone, kidney problem, prostate problem, irregular menstruation | Lf, Rt | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| Chicken pox, herpes simplex, scabies; boils; swellings; backache, body ache, headache; cuts and wounds | Lf, Rt | E | Apply leaves as poultice or leaf and bark decoction as wash | 3–5 leaves | As needed | None | ||||||||||
| Fever | Bk | I | Drink decoction | 1–3 palm-sized barks | Once or twice a day or as needed | None | ||||||||||
| 75 | L. | Malvaceae | Dupang bae | USTH 015664 | 482 | 7 | 1.44 | 2.06 | 1.80 | Stomach trouble; arthritis, rheumatism; labor and delivery, postpartum care and recovery; fever; cuts and wounds, fracture and dislocation, bruises and contusion, sprain, animal bites | Wh | I/E | Drink or apply decoction or burn as incense | 1 bowl | Once a day or as needed | None |
| Diabetes; sore throat; toothache; abdominal pain | Sh | I | Drink decoction | 3–5 glasses | Once or twice a day or as needed | None | ||||||||||
| 76 | Sw. | Marattiaceae | Amampang | USTH 015658 | 126 | 3 | 0.38 | 1.50 | 0.87 | Muscle pain; postpartum care and recovery; backache, body ache, weakness, and fatigue, cramp and spasm | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 77 | Miq. | Melastomataceae | Tampion | USTH 015581 | 282 | 3 | 0.84 | 1.25 | 1.04 | Swollen muscles and swellings, muscle pain; gas pain and flatulence; sprain | Lf | E | Apply heated leaves as hot compress | 1–3 leaves | Once a day or as needed | None |
| 78 | L. | Melastomataceae | Hantutuknaw puti | USTH 015588 | 274 | 3 | 0.82 | 1.89 | 0.96 | Diarrhea, dysentery, stomachache, hemorrhoids; headache, fever | Sh | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| Toothache; cuts and wounds | Lf | I/E | Drop or drink stem sap | 1–3 leaves | As needed | None | ||||||||||
| 79 | Correa | Meliaceae | Lansones | USTH 015565 | 103 | 4 | 0.31 | 1.52 | 1.28 | Malaria; diarrhea, dysentery, dyspepsia; fever, gas pain and flatulence | Bk, Lf | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| Insect bites | Bk | E | Apply powdered bark | Completely on affected part | As needed | None | ||||||||||
| 80 | (Burm.f.) Merr. | Meliaceae | Santol | USTH 015624 | 464 | 7 | 1.39 | 1.78 | 1.85 | Tonic; hypertension; diarrhea, dysentery; postpartum care and recovery; abdominal pain, fever | Bk, Fr, Lf | I | Drink decoction of mesocarp, leaves and scraped bark | 3–5 glasses | Once a day or as needed | None |
| Toothache | Lf | I | Apply crushed leaves as poultice | 1–3 leaves | As needed | None | ||||||||||
| Boils, skin rashes and itchiness, dermatitis | Lf | E | Apply decoction as wash | 3–5 leaves | Once or twice a day or as needed | None | ||||||||||
| Ringworm | Bk | E | Apply pounded scraped bark as poultice | 1–3 palm-sized barks | Once or twice a day or as needed | None | ||||||||||
| 81 | (L.) Jacq. | Meliaceae | Mahogany | USTH 015671 | 334 | 9 | 1.00 | 2.29 | 2.14 | Dysmenorrhea, delayed menstruation; abortifacient; abdominal pain | Sd | I | Take powdered seed or drink decoction | 1–3 glasses | Once a day or as needed | Can cause abortion in pregnant women |
| Amoebiasis, malaria; cancer; tonic; hypertension; cough; diarrhea; miscarriage; fever | Bk | I | Drink decoction | 1–3 glasses | Once a day or as needed | None | ||||||||||
| 82 | (L.) Merr. | Menispermaceae | Lagtang or Abutra | USTH 015600 | 922 | 10 | 2.75 | 3.23 | 2.14 | Jaundice; tumor, myoma; diabetes, tonic; respiratory disease complex; diarrhea, dysentery, dyspepsia, ulcer, appetite enhancer; dysmenorrhea, delayed menstruation; abortifacient; fever | Rt, St | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | Can cause abortion in pregnant women |
| Scabies; boils, skin rashes and itchiness; cuts and wounds | Rt, St | E | Apply coconut oil-infused stem | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| 83 | (L.) Hook. f. & Thomson | Menispermaceae | Panyawan | USTH 015566 | 782 | 9 | 2.33 | 2.68 | 1.95 | Malaria; tonic; diarrhea, stomach trouble, vomiting, ulcer, toothache; arthritis, rheumatism; dysmenorrhea; abortifacient; abdominal pain, backache, body ache, fever | St | I | Drink local alcohol-tinctured or decocted stem | 1–3 glasses | Once or twice a day or as needed | Can cause abortion in pregnant women |
| Scabies; sore eyes; cuts and wounds | Sp, St | E | Drop stem sap | Completely on affected part | As needed | None | ||||||||||
| Arthritis, rheumatism; abortifacient; abdominal pain, body ache; gas pain and flatulence | St | E | Apply coconut oil-infused stem or stem mixed with gasoline | Completely on affected part | As needed | Can cause abortion in pregnant women | ||||||||||
| 84 | Miq | Moraceae | Kabiya | USTH 015672 | 53 | 1 | 0.16 | 0.96 | 0.00 | Headache, fever | Rt | I | Drink decoction | 1 arm-sized root | Twice a day or as needed | None |
| 85 | Elmer | Moraceae | Tobog tapol | USTH 015551 | 492 | 8 | 1.47 | 3.00 | 1.89 | Colds; diabetes; hypertension; asthma, cough, respiratory disease complex; diarrhea, stomachache; urinary tract infection; postpartum recovery, maternal care, milk production enhancer; weakness and fatigue, relapse | Bk, Rt | I | Drink decoction | 1–3 glasses | Thrice a day or as needed | None |
| Diabetes; hypertension | Fr | I | Eat fresh fruit directly | 1–3 fruits | Once a day or as needed | None | ||||||||||
| Body ache, headache, fever | Lf | E | Apply leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 86 | (Miq.) Miq. | Moraceae | Balete | USTH 015552 | 608 | 4 | 1.81 | 2.66 | 1.37 | Prostate cancer, cyst, tumor; arthritis, rheumatism; kidney problem, prostate problem | Bk, Lf, Rt | I | Drink decoction | 5–7 glasses | Once a day in thrice a week for 2 months | In excess can cause anemia, dizziness, and weakening |
| Cuts and wounds | Bk, Lf, Rt | E | Apply decoction as wash | 1–3 glasses | As needed | None | ||||||||||
| Fracture and dislocation, sprain | Bk, Rt | E | Apply fresh and heated bark and root as poultice | 1–3 palm-sized barks or 1 arm-sized root | Once a day or as needed | Bark can cause skin allergy or burn | ||||||||||
| 87 | Reinw. ex Blume | Moraceae | Tobog puti | USTH 015561 | 480 | 8 | 1.43 | 1.62 | 1.89 | Colds; diabetes; hypertension; asthma, cough, respiratory disease complex; diarrhea, stomachache; urinary tract infection; maternal care, postpartum recovery, milk production enhancer; weakness and fatigue, relapse | Bk, Rt | I | Drink decoction | 1–3 glasses | Thrice a day or as needed | None |
| Diabetes; hypertension | Fr | I | Eat fresh fruit directly | 1–3 fruits | Once a day or as needed | None | ||||||||||
| Body ache, headache, fever | Lf | E | Apply leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| 88 | Blanco | Moraceae | Lobi-lobi | USTH 015636 | 331 | 7 | 0.99 | 2.38 | 1.80 | Diabetes; hypertension, atherosclerosis, hemorrhage; diarrhea, stomach trouble, dyspepsia; kidney stones; muscle pain; postpartum care and recovery; cramp and spasm | Lf, Rt | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| 89 | Burm.f. | Moraceae | Lagnob | USTH 015623 | 576 | 7 | 1.72 | 2.13 | 1.77 | Stomach trouble; asthma, sinusitis; muscle pain; backache, body ache, headache, fever, weakness, and fatigue | Lf, Rt | I | Drink decoction | 3–5 glasses | Once a day for 3 days only | In excess can cause intestinal weakening |
| Warts; cataract, eye problem | Lf, Sp | E | Apply drops of leaf sap | 3–5 leaves | Twice a day or as needed | None | ||||||||||
| Herpes simplex; boils | Rt, Sp, St | E | Apply stem and root sap | Completely on affected part | Thrice a day or as needed | None | ||||||||||
| 90 | sp. | Moraceae | Tuwa-tuwa | USTH 015642 | 71 | 1 | 0.21 | 0.98 | 0.00 | Pregnancy, impotence and sterility, postpartum care and recovery | Lf | I | Drink decoction | 3–5 glasses | Once a day for 3–5 days or as needed | None |
| 91 | L. | Moraceae | Tahibo | USTH 015549 | 277 | 4 | 0.83 | 2.69 | 1.21 | Colds; asthma, pneumonia, lung nodule, cough; muscle pain; cramp and spasm, relapse | Lf | I | Drink decoction | 3–5 glasses | Twice to thrice a day for 3–5 days | In excess can cause acid reflux and hypocupremia |
| 92 | L. | Muntingiaceae | Mansanitas | USTH 015629 | 169 | 4 | 0.50 | 1.58 | 1.21 | Colds; diarrhea, stomachache, vomiting, ulcer; prostate problem; abdominal pain, headache | Lf | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| 93 | Elmer | Myristicaceae | Duguang kahoy | USTH 015611 | 194 | 2 | 0.58 | 1.96 | 0.69 | Measles; respiratory disease complex | Bk | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| 94 | L. | Myrtaceae | Bayabas | USTH 015663 | 275 | 5 | 0.82 | 2.15 | 1.43 | Diarrhea, ulcer | Bk, Lf, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Constipation | Fr | I | Eat fresh fruit directly | 1–3 fruits | Once to thrice a day or as needed | None | ||||||||||
| Scabies; toothache; skin eruptions; cuts and wounds | Lf | E | Apply chewed or pounded leaves | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| Dandruff; cuts and wounds; circumcision antiseptic | Lf | E | Apply decocted leaves as wash | 3–5 leaves | Once to thrice a day or as needed | None | ||||||||||
| 95 | Roxb. | Pandanaceae | Pandantsina | USTH 015555 | 197 | 2 | 0.59 | 1.98 | 0.60 | Heart enlargement, high cholesterol; urination difficulty, kidney stone, kidney problem, urinary bladder swelling, prostate problem | Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 96 | Schumach. & Thonn. | Phyllanthaceae | Talikod or Likod-likod | USTH 015590 | 459 | 9 | 1.37 | 2.35 | 2.01 | Jaundice, colds; tonic; coughs; stomach problem; kidney stone, kidney problem, urinary bladder swelling; new-born baby care; fever | Wh | I/E | Drink decoction or apply decocted leaves as wash | 3–5 glasses decoction or 1/2 cup leaf sap (adult); 1/2 cup decoction or 1 teaspoonful leaf sap (baby) | Once or twice a day or as needed | None |
| Scabies, jaundice, ringworm; skin rashness and itchiness, dermatitis, eczema; cuts and wounds | Fr, Rt | E | Apply decoction as wash | 3–5 glasses | Thrice a day or as needed | None | ||||||||||
| 97 | L. | Piperaceae | Lunas buyo | USTH 015568 | 193 | 2 | 0.58 | 1.14 | 0.56 | Skin rashes and itchiness; cuts and wounds, animal and insect bites | Lf, St | E | Apply decoction | Completely on affected part | Once or twice a day or as needed | In excess can cause intestinal weakening |
| 98 | L. | Piperaceae | Lunas bagon tapol | USTH 015544 | 1018 | 9 | 3.04 | 3.45 | 2.06 | Typhoid fever; cancer, cyst, tumor; pulmonary tuberculosis; diarrhea, stomach trouble, ulcer; gas pain and flatulence; poisoning | St | I | Drink local alcohol-tinctured stem | 1/2 to 1 glass | Once a day in thrice a week or as needed | In excess can cause intestinal weakening |
| Tonsillitis; toothache, gum swelling, canker sore | St | I | Gargle local alcohol-tinctured stem | 1/2 to 1 glass | Once or twice a day or as needed | None | ||||||||||
| Scabies, warts, impetigo; boils, skin eruptions, skin rashes and itchiness, pimple, acne; arthritis, rheumatism, swellings, muscle pain; backache, body ache, gas pain and flatulence; allergy, burns, cuts and wounds, sprain, snake, dog and insect bites, contacts with plants and animal parts; anesthetic | St | E | Apply coconut or Efficascent oil-infused stem | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| 99 | L. | Piperaceae | Lunas bagon puti | USTH 015560 | 824 | 9 | 2.46 | 2.41 | 1.20 | Cancer, cyst, tumor; tonsillitis; diarrhea, stomach trouble, ulcer, toothache, mouth sore, gum swelling; gas pain and flatulence; poisoning | St | I | Drink or gargle local alcohol-tinctured stem or drink decocted stem | 1/2 to 1 glass of local alcohol tincture or 3–5 glasses of decoction | Once a day in thrice a week or as needed | In excess can cause intestinal weakening |
| Scabies, warts, impetigo; breast cancer; boils, skin eruptions, skin rashes and itchiness, pimple, acne; arthritis, rheumatism, swellings, muscle pain; backache, body ache, gas pain, and flatulence; skin allergy, burns, cuts and wounds, animal and insect bites, contacts with plants and animals parts; anesthetic | St | E | Apply coconut oil-infused or decocted stem | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| 100 | sp. | Piperaceae | Buyo Pilipog | USTH 015592 | 296 | 3 | 0.88 | 1.33 | 1.04 | Asthma, cough; rheumatism; fracture and dislocation | Lf | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| 101 | (L.) Gaertn. | Poaceae | Bilabila | USTH 015569 | 481 | 11 | 1.44 | 3.04 | 2.34 | Measles; diabetes; internal bleeding; cough; diarrhea; arthritis; kidney problem; postpartum care and recovery; fever, cramp, and spasm; fracture and dislocation | Wh | I | Drink decoction | 3–5 glasses | Thrice a day or as needed | None |
| Ringworm; hair loss; cuts and wounds | Wh | E | Apply decoction | 1 glass | Once to thrice a day or as needed | None | ||||||||||
| 102 | (L.) P.Beauv. | Poaceae | Kogon | USTH 015605 | 107 | 4 | 0.32 | 1.90 | 1.35 | Urination difficulty | Sh | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Chicken pox, measles; diarrhea, toothache; fever, baby teething | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None | ||||||||||
| 103 | P.J.Bergius | Poeaceae | Miligoy | USTH 015627 | 124 | 3 | 0.37 | 2.30 | 1.04 | Diarrhea, dysentery | Rt | I | Drink decoction | 1 handful of roots | Twice a day or as needed | None |
| Hair loss; cuts and wounds | Rt | E | Apply decoction as wash | 1 handful of roots | Once a day or as needed | None | ||||||||||
| 104 | sp. | Rosaceae | Rose | USTH 015628 | 83 | 3 | 0.25 | 1.33 | 1.04 | Colds; nasal congestion, sinusitis | Fl | I | Drink or sniff hot water-infused flowers | 1 glass | Thrice a day or as needed | None |
| Cuts and wounds | Fl | E | Apply hot water-infused flowers as wash | 1 glass | As needed | None | ||||||||||
| 105 | A.Rich. | Rubiaceae | Buyon | USTH 015556 | 123 | 5 | 0.37 | 1.36 | 1.56 | Jaundice, colds; dysentery, stomachache; fever; snake bite | Bk, Lf | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| Asthma, cough | Fl | I | Eat fresh flower directly | 1–3 flowers | Once or twice a day or as needed | None | ||||||||||
| 106 | Wall. | Rubiaceae | Kawilan | USTH 015557 | 94 | 1 | 0.28 | 0.93 | 0.00 | Stomach trouble | Sp, St | I | Drink stem sap | 1/2 cup | Once or twice a day or as needed | None |
| Diarrhea | St | I | Drink local alcohol-tinctured bark | 1/2 to 1 glass | As needed | None | ||||||||||
| 107 | (DC.) T.G.Hartley | Rutaceae | Bagaynga | USTH 015540 | 43 | 1 | 0.13 | 0.92 | 0.00 | Cough | Bk | I | Drink decoction of scraped bark | 1–3 palm-sized barks | Once or twice a day or as needed | None |
| 108 | (Lam.) Merr. | Rutaceae | Dahile | USTH 015660 | 86 | 2 | 0.26 | 1.31 | 0.64 | Pulmonary tuberculosis, cough | Lf, Sp | I | Drink decoction or leaf sap | 3–5 glasses or 3–5 leaves of sap | Once to thrice a day or as needed | None |
| Snake bite | Lf, Sp | E | Apply leaf sap | Completely on affected part | As needed | None | ||||||||||
| 109 | (G.Forst.) Wight & Arn. | Rutaceae | Lunas kahoy | USTH 015538 | 955 | 9 | 2.85 | 3.28 | 2.03 | Cancer, cyst; diarrhea, stomach trouble, ulcer; poisoning | Lf, St | I | Drink local alcohol-tinctured or decocted stem | 1/2 to 1 glass | Once or twice a day or as needed | In excess can cause intestinal weakening |
| Tonsillitis; toothache, gum swelling, canker sore | Rt, St | E | Gargle local alcohol-tinctured stem | 1/2 to 1 glass | Once or twice a day or as needed | None | ||||||||||
| Scabies, warts, impetigo; boils, skin eruptions, skin rashes and itchiness, pimple, acne; joint pain, rheumatism, swellings, muscle pain; backache, body ache, gas pain, and flatulence; allergy, burns, cuts, and wounds; snake, dog, and insect bites; contacts with plants and animal parts; anesthetic | Rt, St | E | Apply coconut or Efficascent oil-infused stem | Completely on affected part | Once or twice a day or as needed | None | ||||||||||
| 110 | L. | Solanaceae | Sili na bisaya | USTH 015626 | 151 | 6 | 0.45 | 2.48 | 1.61 | Diabetes; hypertension | Fr | I | Eat fresh fruit directly or add as spice in cooking | 7 fruits | Once or twice a day or as needed | None |
| White spot, athlete's foot; appetite enhancer; boils, skin rashes and itchiness, psoriasis, dandruff; insect bites | Lf | E | Rub crushed leaves or leaf sap | 3–5 leaves | Once or twice a day or as needed | None | ||||||||||
| 111 | Vahl | Sparmanniaceae | Talimughat lingin | USTH 015547 | 474 | 5 | 1.41 | 1.75 | 1.42 | Diabetes; hypertension, heart enlargement; rheumatism; labor and delivery enhancer, postpartum care and recovery; backache, body ache, fever, weakness, and fatigue, relapse | Bk, Lf, Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day up to 3 days or as needed | None |
| Muscle pain; labor and delivery enhancer, postpartum care and recovery; backache, body ache, fever, cramp, and spasm; relapse | Bk, Rt | E | Apply coconut or Efficascent oil-infused bark and root | Completely on affected part | Once a day or as needed | None | ||||||||||
| 112 | (Wedd.) Chew | Urticaceae | Alingatong | USTH 015598 | 128 | 2 | 0.38 | 2.33 | 0.56 | Diabetes; joint pain, swollen muscles, and swellings, muscle pain | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 113 | Wedd. | Urticaceae | Anagasi | USTH 015542 | 28 | 1 | 0.08 | 0.96 | 0.00 | Stomach trouble and vomiting | Lf | I | Drink decoction | 3–5 glasses | Once or twice a day or as needed | None |
| 114 | (Blume) Miq. | Urticaceae | Kubi or Salin-ubod | USTH 015676 | 151 | 3 | 0.45 | 1.89 | 1.04 | Cough; diarrhea, stomach trouble; fever | Lf | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| 115 | (Link) C.B.Rob. | Urticaceae | Handamay | USTH 015673 | 540 | 6 | 1.61 | 2.25 | 1.58 | Depression, anxiety, nervousness; stomach acidity; backache, body ache, headache, fever, weakness, and fatigue | Lf | I | Eat fresh leaves or drink water solution of leaves | 3–5 glasses | Thrice a day for a month or as needed | None |
| Herpes simplex, scabies; boils, dermatitis | Lf | E | Rub crushed leaves | 3–5 leaves | Thrice a day or as needed | None | ||||||||||
| Skin rashes and infection; cuts and wounds | Bk | E | Apply pulp made from scraped bark as poultice | 1–3 palm-sized barks | Twice a day or as needed | None | ||||||||||
| 116 | (Trecul.) Merr. | Urticaceae | Hanupi | USTH 015655 | 243 | 6 | 0.73 | 2.06 | 1.67 | Sore eyes; ulcer; postpartum care and recovery; fever | Sp, St | I | Drink stem sap or decoction stem | 1 arm-sized stem | Once or twice a day or as needed | None |
| Skin rashes and itchiness; cuts and wounds; animal and insect bites | Rt, Sp | E | Apply decoction as wash | 1 arm-sized root | Once or twice a day or as needed | None | ||||||||||
| 117 | (L.) Vahl | Verbenaceae | Elepanteng lingganag | USTH 015594 | 396 | 5 | 1.18 | 2.04 | 1.56 | Ascariasis; abortifacient; fever | Rt | I | Drink decoction | 1 arm-sized root | Once to thrice a day or as needed | Can cause abortion in pregnant women |
| Boils; bruises, sprain | Lf | E | Apply crushed leaves as poultice | 3–5 glasses | As needed | None | ||||||||||
| 118 | (L.) DC. | Xanthorrhoeaceae | Ikug-ikug | USTH 015656 | 164 | 3 | 0.35 | 1.39 | 0.95 | Maternal care; postpartum care and recovery, milk production enhancer | Lf | I | Drink decoction | 3–5 glasses | Once a day or as needed | None |
| Cuts and wounds | Lf | E | Apply leaves as poultice | 3–5 leaves | As needed | None | ||||||||||
| Herpes simplex | Lf, Rt | E | Apply coconut oil-infused ashes of leaf and roots | Completely on affected part | Thrice a day or as needed | None | ||||||||||
| 119 | L. | Zingerberaceae | Duwaw yellow | USTH 015674 | 248 | 6 | 0.74 | 1.68 | 1.70 | Diabetes; cough; arthritis, rheumatism; delayed menstruation; fever, gas pain and flatulence | Rz | I | Drink grinded and brewed rhizome | 1–3 cups | Once or twice a day or as needed | None |
| Burns, cuts and wounds, insect bites | Rz | E | Apply extracted juice from crushed rhizome | Completely on affected part | As needed | None | ||||||||||
| 120 | (Christm.) Rosc. | Zingerberaceae | Duwaw violet | USTH 015645 | 83 | 2 | 0.24 | 1.88 | 0.69 | Cough; fever | Rz | I | Drink grinded and brewed rhizome | 1–3 cups | Once or twice a day or as needed | None |
| 121 | C.Presl | Zingiberaceae | Yanguas | USTH 015641 | 86 | 3 | 0.26 | 1.26 | 1.04 | Cough; stomachache; urination difficulty, urinary tract infection | Rt | I | Drink decoction | 3–5 glasses | Once to thrice a day or as needed | None |
| 122 | L. | Zingiberaceae | Kisol | USTH 015579 | 200 | 7 | 0.60 | 1.44 | 1.89 | Colds; tonic; cough, sore throat; dyspepsia, toothache; postpartum care and recovery; headache, fever | Rz | I | Drink decoction | 3–5 glasses | Twice a day or as needed | None |
| Toothache; headache, fever | Rz | I/E | Apply grinded rhizome as poultice | 1–3 rhizomes | Thrice a day or as needed | None | ||||||||||
| Tonic; postpartum care and recovery; headache, fever | Sh | E | Place washed clean shoot around the neck | 1–3 shoots | Once a day or as needed | None | ||||||||||
| Cough; rheumatism, swollen muscle | Lf | E | Rub heated and crashed leaves | 1–3 leaves | Thrice a day or as needed | None | ||||||||||
UR use-report, UC use category, UV use value, CIV cultural importance value, UD use diversity
a Bk , barks; Br , branch; Fl , flowers; Fr , fruits; Lf , leaves; Rt , roots; Rz , rhizomes; Sd , seeds; Sh , shoots; St , stems; Wh , whole plant
b I , internal; E , external
Integrative molecular approach
Due to inconclusive morphological identification, unfamiliarity, and confusing species identity because of local name similarity, a total of 24 medicinal plant species were confirmed by DNA sequencing and by comparing the sequences with those present in the GenBank. This method supported ethnopharmacological data to be deposited in a repository, which is essential and helpful for future researchers and investigators for use by data mining approaches [ 73 ]. The molecular data can also be useful to the growing barcoding studies of medicinal plants. Putative identification based on literature, comparative morphology, and molecular sequences using the BLAST search query were tabulated (Table (Table5). 5 ). The integrative approach combined with a priori data from putative identifications based on the interview data on local or vernacular names, local plant name dictionary, and assessment of available morphological characteristics along with a posteriori data from multiple universal markers, occurrence, and distribution of putative species in the Philippines. This paper applied a more detailed taxonomic identification since all reported medicinal plant taxa were identified (nearly all to species level), as shown in Table Table4. 4 . While all generic and familial affinities of medicinal plants were confirmed, four medicinal plants were not identified up to species level due to lack of morphological characteristics, concerning especially the reproductive parts of Piper and Ficus species, several cultivars and hybrids of Rosa species, and several species and varieties of Bauhinia species. Nevertheless, all generic and familial affinities of the medicinal plants documented here were verified combining similarity matching and a priori and a posteriori data as recommended by [ 42 ] to reduce ambiguity and to make it possible assigning a single species identification of their unidentifiable specimens. All determined plant samples with confusing identity having local name similarity and local species pairing, including plant samples with inconclusive morphological identification due to lack of reproductive parts upon collection, were accurately verified using an integrative molecular approach (Table 5 ).
Integrative molecular identification coalescing a priori and a posteriori data
| Taxon no. | Local name | Putative identification based on the [ ] | Species determination using present morphology | Molecular confirmation by BLAST-based sequence matching using multiple molecular markers | Integrative molecular identification approach | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ITS (nrDNA) | K (cpDNA) | A- H (cpDNA) | L-F (cpDNA) | |||||||||||||||||
| Simple BLAST | Optimized BLAST [max score× (query cover/percent identity)] | Simple BLAST | Optimized BLAST [max score × (query cover/percent identity)] | Simple BLAST | Optimized BLAST [max score × (query cover/percent identity)] | Simple BLAST | Optimized BLAST [max score × (query cover/percent identity)] | |||||||||||||
| Top 5 max score | Highest max score | Highest percent identity | Top 5 max core | Highest max score | Highest percent identity | Top 5 max score | Highest max score | Highest percent identity | Top 5 max score | Highest max score | Highest mercent identity | |||||||||
| 1 | Abgaw | sp. | spp. | spp. | spp. | spp. | Blanco | |||||||||||||
| 2 | Alibangbang (puti) | sp. | spp. | NONE | Fabaceae | Fabaceae | (Roxb.) Benth. | |||||||||||||
| 3 | Alibangbang (tapol) | sp. | spp. | NONE | Fabaceae | Fabaceae | (Roxb.) Benth. | |||||||||||||
| 4 | Awoy | None | cf. | spp. | spp. | sp. | Lamiaceae, Martyniaceae | R.Br. | ||||||||||||
| 5 | Balete | sp. | sp. | spp. | spp. | spp. | spp. | (Miq.) Miq. | ||||||||||||
| 6 | Banag | sp. | sp. | NONE | Dioscoreaceae | Dioscoreaceae, Arecaceae | Dioscoreaceae and Blandfordiaceae | Oliv | ||||||||||||
| 7 | Banitlong | sp. | Malvaceae | sp. | Convolvulaceae and Malvaceae | Convolvulaceae and Malvaceae | Convolvulaceae and Malvaceae |
(Houtt.) Stapf | ||||||||||||
| 8 | Banti (puti) | sp. | Euphorbiaceae | Euphorbiaceae | Ebenaceae, Euphorbiaceae | Euphorbiaceae | Pax & Hoffm. | |||||||||||||
| 9 | Banti (tapol) | sp. | Euphorbiaceae | Euphorbiaceae | Ebenaceae, Lauraceae | sp. | Euphorbiaceae | Pax & Hoffm. | ||||||||||||
| 10 | Gapas-gapas (bae) | sp. | Compositae | Compositae | Compositae | Compositae | (Link ex Spreng.) DC. | |||||||||||||
| 11 | Kaningag | cf. mercadoi | spp. | Lauraceae | Lauraceae | spp. | S.Vidal | |||||||||||||
| 12 | Kawilan | cf. | Rubiaceae | Rubiaceae | Rubiaceae | Wall. | ||||||||||||||
| 13 | Lunas-bagon (puti) | None | sp. | spp. | spp. | spp. | L. | |||||||||||||
| 14 | Mayana Kanapkap | sp. | Lamiaceae | NONE | Lamiaceae | spp. | syn. | (L.) Benth. | ||||||||||||
| 15 | Mayana Pula | sp. | spp. | NONE | Lamiaceae | spp. | syn. of | syn. of | syn. of | (L.) Benth. | ||||||||||
| 16 | Salimbagat | cf. | NONE | spp. | spp. | Aristolochiaceae | (Planch. ex Rolfe) ined. | |||||||||||||
| 17 | Talimughat 1 (lingin) | cf. | spp. | spp. | Malvaceae | Malvaceae | , syn. of | syn. of | , syn. of | Vahl | ||||||||||
| 18 | Talimughat 2 (taas) | cf. | NONE | Annonaceae | spp. | Annonaceae | sp. | All are equal | sp. | Annonaceae | and sp. | (Merr.) Steen. | ||||||||
| 19 | Talimughat 3 (pikas) | sp. | spp. | NONE | Fabaceae | spp. | sp. | |||||||||||||
| 20 | Tobog (puti) | cf. | spp. | spp. | spp. | and | spp. | Reinw. ex Blume | ||||||||||||
| 21 | Tobog (tapol) | cf. . | spp. | spp. | spp. | spp. | Elmer | |||||||||||||
| 22 | Tuba-tuba (puti) | cf. | NONE | spp. | L. | |||||||||||||||
| 23 | Tuba-tuba (tapol) | cf. | spp. | spp. | spp. | spp. | L. | |||||||||||||
| 24 | Tuwa-tuwa | None | cf. | spp. | NONE | spp. | Moraceae | sp. | ||||||||||||
NONE unsuccessfully amplified and/or sequenced
Plant local name similarity
Most notable medicinal plants of Agusan Manobo have confusing species identity bearing similar local names, gender identity, and local species pairing. It is popular to use medicinal plants known as “Lunas” (meaning “cure”) with several plants associated under its name. For instance, the top three medicinal plants in terms of use value and cultural importance value have local name similarity, namely Lunas tag-uli ( Anodendron borneense (King & Gamble) D.J.Middleton), Lunas bagon tapol ( Piper decumanum L.), and Lunas kahoy ( Micromelum minutum (G.Forst.) Wight & Arn.), respectively. These three medicinal plants with the initial word named “Lunas” had almost similar use-reports in nine use categories with high use diversity (UD > 2.0). Other “Lunas”-named specimens such as Lunas bagon puti ( Piper nigrum L.), Lunas pilipo ( Acmella grandiflora (Turcz.) R.K.Jansen), Lunas buyo ( Piper aduncum L.), and Lunas gabi ( Alocasia zebrina Schott ex Van Houtte) also shared similarities from the top three mentioned samples in terms of ethnomedicinal properties as a treatment for cuts and wounds. Also, another three medicinal plants were locally classified with the initial word named “Talimughat” (meaning “recover”), namely “Talimughat lingin” ( Grewia laevigata Vahl), “Talimughat taas” ( Friesodielsia lanceolata (Merr.) Steen.), and “Talimughat pikas” ( Bauhinia sp.). These three medicinal plants were noted with high fidelity for postpartum care and recovery. Plant samples with high fidelity for anemia also had similar local names which were found to be same species, namely “Mayana kanapkap” ( Coleus scutellarioides (L.) Benth . ) and “Mayana pula” ( Coleus scutellarioides (L.) Benth . ).
Some medicinal plants also have attached “genders” (male or female) in their local names, which specify the more effective plant “gender” for a specific medicinal use or purpose. Examples are “Kapayas laki” ( Carica papaya L., male), “Dupang bae” ( Urena lobata L., female), and “Gapas-gapas bae” ( Erechtites valerianifolius (Link ex Spreng.) DC . , female) as effective treatments for dengue virus, postpartum care and recovery, and gas pain and flatulence, respectively. Besides, most species with high use values had local species pairing which were classified by the tribe according to distinct white and red coloration, namely “puti” and “tapol,” respectively, with the latter as more effective than the former in treatment for various health conditions. The following recognized local species pairs as white and red plant samples, respectively, are “Alibangbang puti” ( Phanera semibifida (Roxb.) Benth.) and “Alibangbang tapol” ( Phanera semibifida (Roxb.) Benth.); “Banti puti” ( Omalanthus macradenius Pax & Hoffm.) and “Banti tapol” ( Omalanthus macradenius Pax & Hoffm.); “Lunas-bagon puti” ( Piper nigrum ) and “Lunas-bagon tapol” ( Piper decumanum ); “Tobog puti” ( Ficus fistulosa Reinw. ex Blume) and “Tobog tapol” ( Ficus cassidyana Elmer); and “Tuba-tuba puti” ( Jatropha curcas L.) and “Tuba-tuba tapol” ( Jatropha gossypifolia L.). Local species pairing of “Alibangbang puti” and “Alibangbang tapol” was found to be similar species ( Phanera semibifida (Roxb.) Benth.). Another species pair, “Banti puti” and “Banti tapol” was also found to be similar species ( Omalanthus macradenius Pax & Hoffm.). However, molecular confirmation of all species pairs by the locals did not necessarily point to the same species but were mostly referring to another species. An example study resolving species identity of Piper species used by the Agusan Manobo being a sterile species and unidentifiable by present morphology having confusing local names with the initial word “Lunas” has been molecularly confirmed lately using integrative molecular approach [ 19 ]. Thus, it is always important in any ethnomedicinal, ethnobotanical, and ethnopharmacological studies to obtain the correct identification of medicinal plants by integrating molecular data like this for accuracy, consistency, and dependable species identity for future pharmacological evaluation and natural product investigations.
Species molecular confirmation
Most of all extracted samples for molecular analysis were successfully amplified and sequenced (90%) using multiple universal markers (Table (Table5). 5 ). Some medicinal plants could not be successfully amplified using the given primer due to low levels of DNA present in the samples [ 74 ] or plant secondary metabolites present as inhibitory factors [ 75 ]. Molecular data obtained were also subject to the availability of sequences of plant samples in the GenBank. The 24 species identified were tabulated in Table Table6, 6 , showing six endemic species (27.3%) [ 56 ] and conservation status of all assessed species (37.5%) [ 76 , 77 ] presented five least concern species (83.3%) and a vulnerable species, Cinnamomum mercadoi S.Vidal (16.7%). All edited sequences of each of the four DNA markers in fasta file format were attached as supplementary materials (see Additional files 2 – 5 ) for future reference.
The 24 molecularly confirmed species with confusing species identity
| Taxon no. | Local name | Family | Species | Endemicity [ ] | Conservation status |
|---|---|---|---|---|---|
| 1 | Abgaw | Lamiaceae | Blanco | LC [ ] | |
| 2 | Alibangbang (puti) | Fabaceae | (Roxb.) Benth. | ||
| 3 | Alibangbang (tapol) | Fabaceae | (Roxb.) Benth. | ||
| 4 | Awoy | Lamiaceae | R.Br. | LC [ ] | |
| 5 | Balete | Moraceae | (Miq.) Miq. | LC [ ] | |
| 6 | Banag | Dioscoreaceae | Oliv. | ||
| 7 | Banitlong | Byttneriaceae | (Houtt.) Stapf | ||
| 8 | Banti (puti) | Euphorbiaceae | Pax & Hoffm. | EN | |
| 9 | Banti (tapol) | Euphorbiaceae | Pax & Hoffm. | EN | |
| 10 | Gapas-gapas (bae) | Asteraceae | (Link ex Spreng.) DC. | ||
| 11 | Kaningag | Lauraceae | S.Vidal | EN | VU [ ] |
| 12 | Kawilan | Rubiaceae | Wall. | ||
| 13 | Lunas-bagon (puti) | Piperaceae | L. | ||
| 14 | Mayana Kanapkap | Lamiaceae | (L.) Benth. | ||
| 15 | Mayana Pula | Lamiaceae | (L.) Benth. | ||
| 16 | Salimbagat | Aristolochiaceae | (Planch. ex Rolfe) ined. | EN | |
| 17 | Talimughat 1 (lingin) | Sparmanniaceae | Vahl | LC [ ] | |
| 18 | Talimughat 2 (taas) | Annonaceae | (Merr.) Steen. | EN | |
| 19 | Talimughat 3 (pikas) | Fabaceae | sp. | ||
| 20 | Tobog (puti) | Moraceae | Reinw. ex Blume | LC [ ] | |
| 21 | Tobog (tapol) | Moraceae | Elmer | EN | |
| 22 | Tuba-tuba (puti) | Euphorbiaceae | L. | ||
| 23 | Tuba-tuba (tapol) | Euphorbiaceae | L. | ||
| 24 | Tuwa-tuwa | Asteraceae | sp. |
Endemicity: E N endemic
Conservation status: LC least concern, VU vulnerable
The most certain identity confirmed by this molecular analysis is the familial and generic affinity wherein the specific epithet of each of the 24 medicinal plants presented had to be verified for its occurrence and distribution in the country. All species identified using simple and optimized BLAST-based sequence matching results were further reviewed on their present morphology using taxonomic keys and comparing images and specimens before consulting an expert. Some species names presented in BLAST search query have synonyms showing similar genus among species within 5 points deviation down of the max score. In contrast, others have several genera but under the same family. Two species with molecular data, namely Bauhinia sp. and Ficus sp., were only confirmed up to the genus level due to limited morphological material and because of a high number of varieties, species, and subspecies. A sterile Piper species was confirmed as P. nigrum based on its diagnostic characterization, which could be a new variety obtained only in the wild among the respondents and not the widely cultivated spice known as the world’s most consumed peppercorn.
Of all DNA markers used in this study, two markers, psb A- trn H and trn L-F (cpDNA) successfully amplified and sequenced all 24 uncertain species (100%). A total of 21 species (88%) were amplified and sequenced using the marker ITS (nrDNA), while the coding marker, mat K (cpDNA), recorded at least 17 amplified and sequenced species (71%). In this case, molecular data could increase its identification rate by using multiple universal markers. Several coding and non-coding regions were tested in plants, but a single locus has limited resolving capabilities for closely related species [ 79 , 80 ]. While local names are essential in ethnopharmacological studies, complexities of these local names could lead to confusion and ambiguity, hence, a need for further molecular analysis [ 19 ]. A number of ethnobotanical studies consider vernacular names coupled with morphological and molecular confirmation as part of the identification diagnostics [ 19 , 42 , 81 – 83 ].
Collection sites
The majority (57%) of the medicinal plants were collected in the wild, while some were collected within the community village (7.2%) and the houses (4.8%). Some local people were cultivating some of these medicinal plants near homes for their convenience, but collecting medicinal plants in the wild during seasonal times or in case of immediate treatment was highly encouraged for efficacy as the locals believed that the plants should grow in their natural setting rather than cultivation. Scientific studies tend to support the idea of medicinal plant collection in the wild because plant secondary metabolites will be mostly expressed in the natural setting under environmental stress and conditions, whereby they could not be comparably expressed under monoculture conditions [ 84 ]. Higher levels of secondary metabolites were also reported in wild populations where plants grow slowly, unlike in much faster-growing monocultures [ 85 ].
Plant parts used
All plant parts were used from different plant species against a variety of diseases. The most frequently used plant parts were the leaves (41.6%), followed by roots (16.1%), barks (12.0%), stems (8.5%), sap or latex (6.7%), and flowers (4.1%) (Fig. (Fig.2). 2 ). Sometimes, more than one plant part of the same species is used in combination, like leaves, barks, stems, and roots for preparation and administration, which the locals believed to have a synergistic effect and a more effective medication.

Plant parts used by the Agusan Manobo for medicinal application. Bk, barks; Br, branches; Fl, flowers; Fr, fruits; Lf, leaves; Rt, roots; Rz, rhizomes; Sd, seeds; Sh, shoots; Sp, sap or latex; St, stems; Wh, whole plant
Preparation and administration
The primary preparation method was decoction (34.0%), followed by pounding, crushing, rubbing, grinding, and powdering (13.7%); poultice (12.3%); extracting (9.0%); directly applying or eating (8.5%); infusion (7.1%); applying as wash, bath, hot compress (5.5%); heating or warming (3.6%); tincture (2.7%); brewing (1.6%); burning (1.4%); and steaming (0.5%) as depicted in Fig. Fig.3. 3 . The more common route of administration was internal (60%) rather than external (40%). This result is contrary to the previous reports in the other Philippine major island ethnic tribes like the Ati Negrito community of Visayas [ 21 ] and the Ivatan community in Luzon [ 24 ] where the external application was more common. While external administration could be safer, according to the Agusan Manobo , the internal application was more common since most of their health conditions were associated internally, making decoction as their most common preparation. In cases of external diseases and illnesses, more prolonged coconut oil infusions of medicinal plant stems and barks were often applied.

Mode of preparation of medicinal plants used by the Agusan Manobo . Bn, burning; Br, brewing; Dc, decoction; Di, directly applying or eating; Ex, extracting; Ht, heating or warming; In, infusion; Pd, pounding, crushing, rubbing, grinding, powdering; Po, poultice; Sm, steaming; Ti, tincture; Ws, as wash, bath, hot compress
Use categories (UC)
Reported medicinal uses of plants in this study were grouped into 16 category names based on the citations of informants and the likeness to the use category (Table (Table3). 3 ). Reported uses and diseases in medical terms were verified by the assigned local physicians and allied workers, nearby hospitals and health centers to confirm disease occurrence and epidemiology in the area. A total of 120 reported uses or diseases treated by 122 plant species were documented in the study sites.
Use-report (UR) and use value (UV)
Both UR and UV represent the relative importance of medicinal plants for certain categorized uses or diseases. High values were considered the most important species among the Agusan Manobo . Five medicinal plants with the highest URs (more than 900) as well as UVs (more than 2.5) were Anodendron borneense (UR = 1134; UV = 3.39) in 12 categories, Piper decumanum (UR = 1018; UV = 3.04) in 9 categories, Micromelum minutum (UR = 955; UV = 2.85) in 9 categories, Arcangelisia flava (L.) Merr. (UR = 922; UV = 2.75) in 10 categories, and Cinnamomum mercadoi (UR = 908; UV = 2.71) in 8 categories, as shown in Table Table4. 4 . These high UR and UV plants were the most frequently used plant species based on high fidelity level for pregnancy (FL = 88%), skin rashes and itchiness (FL = 95%), hemorrhage (FL = 97%), tumor (FL = 87%), and stomach trouble (FL = 100%), respectively, (Table (Table11 11 ).
The relative healing potential of the top 20 most cited medicinal plants used against particular disease
| No. | Scientific name | Particular use or disease | Ip | Iu | FL% |
|---|---|---|---|---|---|
| 1 | L. | Dengue fever | 158 | 158 | 100 |
| 2 | Blanco | Cough with phlegm | 238 | 238 | 100 |
| 3 | S.Vidal | Stomach trouble | 223 | 223 | 100 |
| 4 | (L.) Hook. f. & Thomson | Joint pain | 157 | 157 | 100 |
| 5 | (Miq.) Miq. | Fracture and dislocation | 41 | 41 | 100 |
| 6 | L. | Anesthetic | 68 | 68 | 100 |
| 7 | Link) C.B.Rob. | Herpes simplex | 59 | 59 | 100 |
| 8 | (L.) Kurz | Nervous breakdown | 44 | 45 | 98 |
| 9 | Oliv. | Urinary bladder swelling | 133 | 136 | 98 |
| 10 | (G.Forst.) Wight & Arn. | Hemorrhage | 70 | 72 | 97 |
| 11 | L. | Skin rashes and itchiness | 203 | 214 | 95 |
| 12 | L. | Discharging ear | 59 | 63 | 94 |
| 13 | (Blume) Miq. | Diabetes | 68 | 72 | 94 |
| 14 | Baker | Atherosclerosis | 63 | 69 | 91 |
| 15 | L. | Cramp and spasm | 71 | 79 | 90 |
| 16 | (Juss.) Rohr | Urinary tract infection | 85 | 95 | 89 |
| 17 | (King & Gamble) D.J.Middleton | Pregnancy | 38 | 43 | 88 |
| 18 | (L.) Merr. | Tumor | 73 | 84 | 87 |
| 19 | (J.Koenig) Govaerts | Goiter | 44 | 52 | 85 |
| 20 | Burm.f. | Eye problem | 32 | 39 | 82 |
FL% percentage of fidelity level, Ip the number of informants who independently cited the use of a species for a particular use or disease, Iu the total number of informants who mentioned the plant for any use or purpose regardless of category
The respondents consistently reported these in all study sites, but only harvested in the wild. Some other plants can be cultivated with high UVs, as shown in the top 20 species ranked by UV (Table (Table7). 7 ). While high UV species can often be harvested for medicinal use and purpose, these important species call for conservation priority [ 86 ]. The four medicinal plants included among the top 10 recommended medicinal plants by the Department of Health (DOH) of the Philippines, were cultivated by the Agusan Manobo respondents within their community. These scientifically validated medicinal plants were also reported with high URs, namely “Bayabas” Psidium guajava L. (275) “Lagundi” Vitex negundo L. (475), “Gabon” Blumea balsamifera (L.) DC. (412), and “Tsaang gubat” Ehretia microphylla Lam. (336).
The top 20 species ranked by use value (UV). Species which are on the top 20 lists ranked by cultural importance value (CIV) and use diversity (UD) are indicated by bold typeface in that column
| Scientific name | UV | CIV | UD |
|---|---|---|---|
| (King & Gamble) D.J.Middleton | 3.39 | ||
| L. | 3.04 | ||
| (G.Forst.) Wight & Arn. | 2.85 | ||
| (L.) Merr. | 2.75 | ||
| S.Vidal | 2.71 | ||
| L. | 2.46 | 2.41 | 1.20 |
| L. | 2.41 | ||
| (L.) Hook. f. & Thomson | 2.33 | 2.68 | |
| L. | 2.29 | 2.55 | 1.87 |
| (J.Koenig) Govaerts | 2.22 | 2.58 | |
| Blanco | 1.99 | 1.79 | |
| L. | 1.97 | 1.64 | |
| (Miq.) Miq. | 1.81 | 2.66 | 1.37 |
| (L.) Kurz | 1.74 | 1.74 | |
| Burm.f. | 1.72 | 2.13 | 1.77 |
| Oliv. | 1.61 | 2.36 | 1.70 |
| (Link) C.B.Rob. | 1.61 | 2.25 | 1.58 |
| Baker | 1.56 | 2.36 | 1.56 |
| (Blume) Miq. | 1.53 | 1.58 | |
| (Juss.) Rohr | 1.49 | 2.50 | 1.44 |
Cultural importance value (CIV)
CIV often identifies species with diverse use-reports in different use categories, which is relatively dependent on the sum of the proportion of informants who cited the medicinal plant use. The usefulness of species based on the number of informants for each species is not only accounted for this additive index but also its versatility [ 47 ]. The top 20 species ranked by CIV included some species with high UV and UD (Table (Table8 8 ).
The top 20 species ranked by cultural importance value (CIV). Species which are on the top 20 lists ranked by use value (UV) and use diversity (UD) are indicated by bold typeface in that column.
| Scientific name | CIV | UV | UD |
|---|---|---|---|
| (King & Gamble) D.J.Middleton | 3.68 | ||
| L. | 3.45 | ||
| (G.Forst.) Wight & Arn. | 3.28 | ||
| (L.) Merr. | 3.23 | ||
| S.Vidal | 3.22 | ||
| Nees | 3.07 | 1.43 | |
| (L.) Gaertn. | 3.04 | 1.44 | |
| Elmer | 3.00 | 1.47 | 1.89 |
| (Blume) Miq. | 2.96 | 1.58 | |
| Blanco | 2.94 | 1.79 | |
| L. | 2.92 | 1.64 | |
| (L.) Kurz | 2.90 | 1.74 | |
| (Lam.) Pers. | 2.88 | 1.45 | |
| L. | 2.85 | 0.66 | 1.47 |
| (Jack) Hook.f. | 2.83 | 0.92 | 1.79 |
| L. | 2.83 | ||
| L. | 2.81 | 1.29 | |
| L. | 2.80 | 0.91 | 1.85 |
| (L.) H.Rob. | 2.78 | 1.42 | 1.42 |
| (Burm.f.) B.L.Rob. | 2.75 | 1.19 | 1.67 |
Use diversity (UD)
UD determines medicinal plants dependent on the variety of uses in different use categories. This index considers the widespread contribution of each use category according to the number of reported diseases treated. The top 20 species with high UD did not include all high values of UV and CIV (Table (Table9 9 ).
The top 20 species ranked by use diversity (UD). Species which are on the top 20 lists ranked by use value (UV) and cultural importance value (CIV) are indicated by bold typeface in that column
| Scientific name | UD | UV | CIV |
|---|---|---|---|
| (L.) Gaertn. | 2.34 | 1.44 | |
| (King & Gamble) D.J.Middleton | 2.22 | ||
| (Lam.) Pers. | 2.21 | 1.45 | |
| (L.) Jacq. | 2.14 | 1.00 | 2.29 |
| (L.) Merr. | 2.14 | ||
| Nees | 2.09 | 1.43 | |
| L. | 2.09 | 1.15 | 2.33 |
| L. | 2.06 | ||
| L. | 2.06 | 0.63 | 2.75 |
| L. | 2.04 | 1.29 | |
| Wall. ex G.Don | 2.04 | 1.15 | 2.71 |
| (G.Forst.) Wight & Arn. | 2.03 | ||
| (J.Koenig) Govaerts | 2.03 | 2.58 | |
| L. | 2.02 | 0.62 | 2.17 |
| Schumach. & Thonn. | 2.01 | 1.37 | 2.35 |
| (L.) L.f. | 1.98 | 0.98 | 2.69 |
| L. | 1.97 | 1.06 | 2.29 |
| (L.) Hook. f. & Thomson | 1.95 | 2.68 | |
| L. | 1.94 | ||
| S.Vidal | 1.93 |
Correlation of the basic values and indices
Table Table10 10 presents the Spearman correlations among all the five variables used to quantify ethnopharmacological data. All correlations were moderate to strongly positive and significant at p < 0.01 ( n = 125). That is, as one variable increases, the other also increases. Of all the variables, UV is entirely dependent on UR (1.00), while UD is highly dependent on UC (0.97). However, the subjectivity of selection criteria among the use categories was avoided as the researcher consulted with physicians and other medical experts in the locality. The correlation index between UV and CIV was quite high (0.73), meaning that the relative importance of medicinal plants used among the Agusan Manobo was relatively dependent on the number of use mentions among the key informants as counted in UR. An interesting point that appeared to corroborate these data is that the number of UR was positively correlated (0.71–1.00), among other basic values and indices. These variables were correlated with the number of uses for a particular ailment and the number of categories considered. Thus, it can be argued that the relative importance of medicinal plants documented in this study was relatively dependent at least, on the number of use-reports among the key informants and the number of use categories following an objective manner. Despite the advantages and uses of these values and indices in determining the relative importance and usefulness of medicinal plants, it is practical to note that no single index can give information about the complete picture of plant importance.
Spearman rank order correlations among all five variables: basic values and indices
| UC | UV | CIV | UD | |
|---|---|---|---|---|
| UR | 0.74 | 1.00 | 0.73 | 0.71 |
| UC | 0.74 | 0.71 | 0.97 | |
| UV | 0.73 | 0.71 | ||
| CIV | 0.69 |
All the correlations are significant at p < 0.01 ( n = 125)
Informant consensus factor (ICF)
ICF measures the agreement among informants on the use of plant species for a particular purpose or disease category. While the agreement among the key informants varies in different categories, the ICF values are all greater than or equal to 0.97 (Table (Table3). 3 ). These results showed that the exchange of information could be evident among the Agusan Manobo community on their medicinal plant uses and practices. Among the 16 use categories, four categories, namely diseases of the digestive system (DDS), diseases of the skin (DOS), abnormal signs and symptoms (ASS), and other problems of external causes (OEC) had the highest ICF value of 0.99.
Fidelity level (FL)
FL implies the most preferred medicinal plant for a particular disease or purpose. FL value ranges from 1 to 100% depending on the URs cited by the informants for a given species for a particular ailment. Seven species were found with the maximum FL of 100%, including the identified species with the highest number of use mentions, Carica papaya , Premna odorata , Cinnamomum mercadoi , Tinospora crispa , Ficus concinna , Piper decumanum , and Pipturus arborescens which are used for dengue fever, cough with phlegm, stomach trouble, joint pain, fracture and dislocation, anesthetic, and herpes simplex, respectively (Table (Table11 11 ).
Jaccard’s similarity index (JI)
This is the first ethnopharmacological or ethnobotanical study of indigenous peoples in the province of Agusan del Sur. The variation of the medicinal plants used among the three studied localities was shown in JI (Fig. (Fig.4). 4 ). The most overlap of the obtained data and the Jaccard index (similarity) was between the city of Bayugan and the municipality of Sibagat (JI = 0.42), and the least one was between both municipalities of Esperanza and Sibagat (0.38). However, the degree of similarity among the three adjacent localities was proximate with JI ranged from 0.38 to 0.42. While JI conveyed a similarity index ca. 39.7%, the actual overlap is 52.5% (64 species cited among the localities). This similarity could be observed on their comparable ecological types being upland and well-drained areas and due to the active exchange of information on the uses of medicinal plants among the communities during monthly social meetings and preparations in the province of Agusan del Sur.

Overlap in the medicinal plants collected in the three studied localities (city of Bayugan and the municipalities of Sibagat and Esperanza)
Dosage, frequency, and experienced adverse or side effects of using medicinal plants
For a detailed ethnopharmacological study, it is essential to consider the therapeutic use, medication action, and possible side effects. This study involved documenting the quantity or dosage, administration frequency, and experienced adverse or side effects, as shown in Table Table4. 4 . A particular number of plant parts were followed in their mode of preparation. Having leaves as the most frequently used medicinal plant part, 3–5 leaves (or at least an odd number) of decocted, heated, and pounded leaves should be applied. Most of the medicinal plants (82%) were reported by the key informants with no experience of adverse or side effects, while 18% of medicinal plants were experienced with adverse or side effects. There were seven medicinal plants reported to cause abortion in pregnant women once taken or applied. Other listed medicinal plants, when taken in excess, can cause other adverse or side effects. Four of these medicinal plants can cause anemia, dizziness, and weakening, while other plants can cause acid reflux and hypocupremia, burn, and allergy and are even poisonous when eaten or applied. Other reported cases concern excessive intake, which can cause blood viscosity, intestinal weakening, thrombocytopenia, and abnormalities in lactating mothers. These reported adverse or side effects were verified by the attending local medical practitioners and allied medical workers during their hospital visits and in times of emergency. It can be argued that not all medicinal plants used by the tribe are safe for use with no side effects. Thus, it is essential to obtain the reported adverse effects or possible side effects of cited medicinal plants by the informants in all ethnopharmacological studies like this.
This ethnopharmacological documentation recorded a total of 122 medicinal plant species belonging to 108 genera and 51 families across 16 use or disease categories. The majority of medicinal plants are trees (36%) and herbs (33%), which are mostly found in the wild, while some are cultivated. These are followed by 17% shrubs, 11% climbers, 2% grasses, and 1% ferns. The highest percentage of medicinal trees documented in this study is parallel with the earlier ethnobotanical studies [ 21 , 87 ]. The highest frequency of using leaves and aerial plant organs was also reported in several ethnobotanical studies in the Philippines [ 21 , 24 , 25 , 87 – 90 ] and other countries [ 91 – 93 ]. The highest frequency of decoction for preparation and administration is similar to previous ethnobotanical investigations [ 21 , 87 – 90 ].
Lamiaceae was the most represented family with 12 species, followed by Asteraceae with 11, Moraceae with eight species, and Fabaceae with six species. This result is contrary to previous ethnobotanical studies in which Asteraceae were the most represented family [ 24 , 88 – 90 ]. The Lamiaceae (mint family) possess a wide variety of ornamental, medicinal, and aromatic plants producing essential oils that are used in traditional and modern medicine, food, cosmetics, and pharmaceutical industry [ 94 ]. This family is known for effective pain modulation with potential analgesic or antinociceptive effects, which includes several aromatic medicinal spices like mint, oregano, basil, and rosemary [ 95 ]. Asteraceae (the aster, daisy, composite, or sunflower family) are the largest family of flowering plants which were reported to have pharmacological activities such as antitumor, antibacterial, antifungal, and anti-inflammatory [ 96 ] containing phytochemical compounds such as polyphenols, flavonoids, and diterpenoids [ 97 , 98 ]. The Moraceae (fig family) was reported to have wide variety of chemical constituents with potential biological activities as previously investigated by [ 99 ] in Ficus racemosa L., and [ 100 ] in Ficus carica L., and [ 101 ] in Ficus benjamina L. Fabaceae (pea family) which is the third largest family also contain various bioactive constituents with potential pharmacological and toxicological effects [ 102 ]. A member of this family which has long been cultivated and introduced in the Philippines, Gliricidia sepium (Jacq.) Kunth ex Steud., was investigated to have antimicrobial and antioxidant activities, as well as several phytochemicals present [ 13 ].
The Department of Health (DOH) of the Philippines has continually endorsed 10 medicinal plant species in its traditional health maintenance program: (1) Cassia alata L., (2) Momordica charantia L., (3) Allium sativum L., (4) Psidium guajava L., (5) Vitex negundo L., (6) Quisqualis indica L., (7) Blumea balsamifera (L.) DC., (8) Ehretia microphylla Lam., (9) Peperomia pellucida (L.) Kunth, and (10) Clinopodium douglasii (Benth.) Kuntze . Of all these 10 recommended and clinically tested medicinal plants, four species were included in this survey.
Apparently, the societal gaps which differentiate educational level, gender, position, occupation, and age among the Manobo indigenous community may result in the disappearance of their medicinal plant knowledge and traditional practices. While there was no significant difference in their medicinal plant knowledge in different locations, it is still highly important to document their medicinal plant knowledge to perpetuate their cultural tradition and medicinal practices, as well as protect and conserve these important plant genetic resources.
Many ethnobotanical studies include vernacular names as part of the putative identification. While vernacular names are useful in ethnopharmacology, pharmacognosy, and pharmacovigilance [ 83 , 103 ], reliance on these vernacular names for species identification and classification can cause ambiguity and incorrect identification resulting to research invalidation [ 104 ]. DNA-based identification is a useful tool for accurate species identification. Correct identification of a medicinal plant should be examined using molecular data [ 105 ] for consistency of species and pharmacological investigations of natural products [ 106 ]. Although plant-based drug discovery from ethnobotanical data provides future drug leads, authentication of the plant material is a great challenge and opportunity [ 107 ].
Comparison with previous ethnobotanical studies
Several ethnobotanical and ethnomedicinal studies were conducted in the Philippines, but few involve quantitative analyses in their studies. The majority of ethnobotanical studies conducted in the Philippines purposively selected key informants who are just knowledgeable of their medicinal plants like residents, traditional healers, herbalists, gardeners, traders, and elders, but a limited count of researches focused on specific IPs or tribal communities in the country.
Among the three major islands in the Philippines (Luzon, Visayas, and Mindanao), the island of Mindanao is still underdocumented despite its largest population of indigenous cultural communities/indigenous peoples (ICCs/IPs) in the country. In Luzon, four indigenous groups were documented, namely the Kalanguya tribe in Tinoc, Ifugao [ 108 ]; the Ivatan in Batan Island Batanes [ 24 ]; the Ayta in Dinalupihan, Bataan [ 109 ]; and the Ilongot-Eǵongot in Maria Aurora, Aurora [ 110 ], communities. The plant utilization among local communities was also documented by [ 25 ] in Kabayan, Benguet Province, namely Ibaloi , Kankanaey and Kalanguya in addition to the earlier recorded tribes such as the Negritos [ 111 ], the Tasadays [ 112 , 113 ], the Ifugao [ 114 , 115 ] and the Bontoc [ 116 ]. Other studies of cultural communities involve indigenous knowledge and practices for sustainable management like the Ifugao forests in Cordillera, Philippines [ 117 ].
In Visayas, only the Ati Negrito of Guimaras island [ 21 ], while in Mindanao, three tribes were studied, namely the Higaonon tribe of Iligan City [ 88 ], Subanen tribe of Dumingag, Zamboanga del Sur [ 89 ]; Muslim Maranaos of Iligan City [ 90 ]; Subanen tribe of Lapuyan, Zamboanga del Sur [ 87 ]; and Tagabawa tribe of Davao del Sur [ 118 ]. Of all reported ethnobotanical studies in Mindanao, this is the first study utilizing detailed quantitative analysis of relative importance, effectivity consensus, correlation of indices, and the extent of the potential use of each medicinal plant species among the ICCs/IPs. Moreover, this study also integrated molecular confirmation for the first time applying multiple universal markers and coalescing a priori and a posteriori data for accurate species identification to resolve complex plant local or vernacular names and sterile or non-reproductive plant specimens.
In comparison with existing ethnobotanical studies in the Philippines, a novel plant medicinal use was recorded, namely Anodendron borneense with no existing records of ethnobotanical and pharmacological investigations in the world to date. The ethnopharmacological profile of this medicinal plant is a novel finding in this study, which is consistently on the top list among the values or indices used (UR, UV, and CIV), which is only known among the Agusan Manobo in the province of Agusan del Sur, Philippines. Incorporating data of experienced adverse or side effects in this study introduces a more detailed ethnopharmacological documentation in the Philippines, which could be a reference material for future ethnomedicinal, biological, and pharmacological studies.
Limitations of the present study
Ethnobotanical research broadly encompasses like ethnopharmacology, which involves field-based investigations. However, most of the remote areas and barangays in various municipalities and cities of the Philippines were not always safe from rebels and communists against the Philippine government. Majority of the Manobo tribes documented here live in far-flung hinterlands, remote upland areas alongside rivers, valleys, and creeks having security threats from the rebel movement known as the New People's Army (NPA). Study sites included here obtained security clearance from the provincial and local government administrations to ensure safety and accessibility in the area, and the availability of key informants on the actual documentation and field walks. Language barriers were barely encountered since most respondents could speak the national Filipino language and/or the regional Cebuano or Visayan language aside from their Minanubu dialect. Phenology and year-round seasonal variations are essential factors to consider for accurate observation of the plant and collection of specimens with complete reproductive parts. Some respondents are sometimes unwilling to share their medicinal plant knowledge with others due to their previous experience being taken advantage of by business-related parties of drug and pharmaceutical companies. It was also observed that most respondents are becoming educated with the help of government education programs for IPs, which made them more resistant to allowing themselves to be the subject of study by visitors and outsiders.
In spite of that, it is very important to gain trust, confidence, and respect among the Agusan Manobo community by embracing their rich cultural tradition through ritual observation and tribal immersion within their community. Although they maintain secrecy about their medicinal plant use and knowledge, it is also beneficial to practice keeping their knowledge from possible overexploitation of their medicinal plant resources. This study is the first in the country documenting the rich ethnopharmacological practices of indigenous tribes coupled with integrative molecular confirmation of medicinal plants used. It is highly important to recognize the role of indigenous cultural communities/indigenous peoples (ICCs/IPs) in the Philippines for shared information of ethnopharmacological practices for future preservation of knowledge and conservation priorities of their plant genetic resources. This will benefit their children and future generations before their knowledge becomes lost and forgotten.
Research highlights
- The current study revealed the rich ethnopharmacological practices, medicinal plant uses, and knowledge of the Manobo tribe in Agusan del Sur, Philippines.
- Exchange of information among the Agusan Manobo communities was observed in different localities; however, the younger generation has a potential decline of interest due to their acquaintance of over-the-counter drugs and modern medicines.
- This study reinforced the application of integrative molecular confirmation for medicinal plant species lacking reproductive parts upon collection and/or unidentifiable by present morphology (sterile or non-reproductive) plant material.
- Novel medicinal use and some new ethnopharmacological information of medicinal plants were reported in this study.
- The consolidated data of this quantitative ethnopharmacology study contributes to the repository of medicinal plant knowledge and the rich source of information for scientists, physicians, and experts such as botanists, taxonomists, phytochemists, pharmacists, environmentalists, conservation biologists, medical doctors, and allied professionals.
This study concluded the culturally rich ethnomedicinal knowledge and ethnopharmacological practices of the Manobo tribe in Agusan del Sur, Philippines. The results of the study revealed a high diversity of medicinal plants used by the Agusan Manobo with 122 species utilized in 16 use categories. Like any other ethnolinguistic indigenous group in the country, traditional knowledge may be lost or forgotten due to possible migration, acculturation, and declining interest of the younger generation in response to the increasing availability of commercial over-the-counter medicine. Their medicinal plants are known by a limited number of individuals, mostly by their healers, elders, and tribal officials. This quantitative ethnopharmacological documentation is the first to show the high consensus and relative importance of medicinal plants used by the Agusan Manobo and provides molecular confirmation of their medicinal plant species with uncertain identity. The combined quantitative ethnopharmacological documentation and species confirmation using an integrative molecular approach of medicinal plants used in traditional medicine is a breakthrough for obtaining more detailed and comprehensive findings that will be a valuable contribution to the repository of knowledge. The findings of this study will serve as reference material for future systematic, biochemical, and pharmacological studies. While the findings of this study are promising, regarding new potential therapeutic agents for healthcare improvement, it is of utmost concern to reconsider important medicinal plant species for conservation priorities as part of the government programs and initiatives to perpetuate the national and world heritage of traditional knowledge on medicinal plants used by many diverse cultural communities.
Supplementary information
Acknowledgements.
We are very grateful to the entire Agusan Manobo community of Bayugan City, Esperanza, and Sibagat, Agusan del Sur, for their active participation and support in the conduct of the study. The first author would like to thank his scholarship grant from the Department of Science and Technology—Accelerated Science and Technology Human Resource Development Program—National Science Consortium (DOST-ASTHRDP-NSC) and the Alexander von Humboldt Foundation as a Junior Researcher. The second author thanks the Department of Health—Philippine Institute of Traditional and Alternative Health Care (DOH-PITAHC) for the funding and the Alexander von Humboldt Foundation for a renewed research stay at the University of Bayreuth (Germany) in 2019.
Authors’ contributions
MLD proposed the research study, carried out the fieldwork, molecular work, and wrote the manuscript as the major contributor of the study. DT assisted with species identification and authentication at the Philippine National Herbarium. GJA evaluated the data of fieldwork and molecular work for inclusion in the manuscript. UM and SCS reviewed, analyzed, and gave critical comments. All authors have read and approved the final manuscript.
The authors would like to express their heartfelt thanks and gratitude for the financial support of the Department of Health—Philippine Institute of Traditional and Alternative Health Care (DOH-PITAHC).
Availability of data and materials
Competing interest.
The authors declare that they have no competing interests.
Ethics approval and consent to participate
All necessary approval, free prior informed consent, permit, and certification were secured from the local government units (LGUs), provincial government administration, PENRO-LGU and NCIP-LGU of Agusan del Sur, and regional agencies of CARAGA administrative region (Region XIII) obtaining DENR-CARAGA wildlife gratuitous permit (no. R13-2019-12) and NCIP-CARAGA certification (no. R13-2019-01). This study secured ethics approval from USTGS-ERC (protocol no. GS-2019-PN007). The purpose of the study was discussed to the tribal communities headed by the respective tribal chieftains, and they agreed to provide information following ritual observation as part of cultural immersion.
Consent for publication
Not applicable
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information accompanies this paper at 10.1186/s13002-020-00363-7.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Quantitative ethnopharmacological documentation and molecular confirmation of medicinal plants used by the Manobo tribe of Agusan del Sur, Philippines
Affiliations.
- 1 The Graduate School and Research Center for the Natural and Applied Sciences, University of Santo Tomas, España Boulevard, 1015, Manila, Philippines. [email protected].
- 2 Department of Plant Systematics, University of Bayreuth, Universitätsstr. 30, 95440, Bayreuth, Germany. [email protected].
- 3 The Graduate School and Research Center for the Natural and Applied Sciences, University of Santo Tomas, España Boulevard, 1015, Manila, Philippines.
- 4 College of Science, University of Santo Tomas, España Boulevard, 1015, Manila, Philippines.
- 5 Department of Plant Systematics, University of Bayreuth, Universitätsstr. 30, 95440, Bayreuth, Germany.
- PMID: 32138749
- PMCID: PMC7227330
- DOI: 10.1186/s13002-020-00363-7
Background: The Philippines is renowned as one of the species-rich countries and culturally megadiverse in ethnicity around the globe. However, ethnopharmacological studies in the Philippines are still limited especially in the most numerous ethnic tribal populations in the southern part of the archipelago. This present study aims to document the traditional practices, medicinal plant use, and knowledge; to determine the relative importance, consensus, and the extent of all medicinal plants used; and to integrate molecular confirmation of uncertain species used by the Agusan Manobo in Mindanao, Philippines.
Methods: Quantitative ethnopharmacological data were obtained using semi-structured interviews, group discussions, field observations, and guided field walks with a total of 335 key informants comprising of tribal chieftains, traditional healers, community elders, and Manobo members of the community with their medicinal plant knowledge. The use-report (UR), use categories (UC), use value (UV), cultural importance value (CIV), and use diversity (UD) were quantified and correlated. Other indices using fidelity level (FL), informant consensus factors (ICF), and Jaccard's similarity index (JI) were also calculated. The key informants' medicinal plant use knowledge and practices were statistically analyzed using descriptive and inferential statistics.
Results: This study enumerated the ethnopharmacological use of 122 medicinal plant species, distributed among 108 genera and belonging to 51 families classified in 16 use categories. Integrative molecular approach confirmed 24 species with confusing species identity using multiple universal markers (ITS, matK, psbA-trnH, and trnL-F). There was strong agreement among the key informants regarding ethnopharmacological uses of plants, with ICF values ranging from 0.97 to 0.99, with the highest number of species (88) being used for the treatment of abnormal signs and symptoms (ASS). Seven species were reported with maximum fidelity level (100%) in seven use categories. The correlations of the five variables (UR, UC, UV, CIV, and UD) were significant (r s ≥ 0.69, p < 0.001), some being stronger than others. The degree of similarity of the three studied localities had JI ranged from 0.38 to 0.42, indicating species likeness among the tribal communities. Statistically, the medicinal plant knowledge among respondents was significantly different (p < 0.001) when grouped according to education, gender, social position, occupation, civil status, and age but not (p = 0.379) when grouped according to location. This study recorded the first quantitative ethnopharmacological documentation coupled with molecular confirmation of medicinal plants in Mindanao, Philippines, of which one medicinal plant species has never been studied pharmacologically to date.
Conclusion: Documenting such traditional knowledge of medicinal plants and practices is highly essential for future management and conservation strategies of these plant genetic resources. This ethnopharmacological study will serve as a future reference not only for more systematic ethnopharmacological documentation but also for further pharmacological studies and drug discovery to improve public healthcare worldwide.
Keywords: Agusan Manobo; Cultural importance value; Ethnopharmacology; Mindanao; Molecular confirmation; Use diversity.
PubMed Disclaimer
Conflict of interest statement
The authors declare that they have no competing interests.
Study sites (barangays) from the…
Study sites (barangays) from the only city (Bayugan), and the two selected municipalities…
Plant parts used by the…
Plant parts used by the Agusan Manobo for medicinal application. Bk, barks; Br,…
Mode of preparation of medicinal…
Mode of preparation of medicinal plants used by the Agusan Manobo . Bn,…
Overlap in the medicinal plants…
Overlap in the medicinal plants collected in the three studied localities (city of…
Similar articles
- Quantitative ethnobotanical study of the medicinal plants used by the Ati Negrito indigenous group in Guimaras island, Philippines. Ong HG, Kim YD. Ong HG, et al. J Ethnopharmacol. 2014 Nov 18;157:228-42. doi: 10.1016/j.jep.2014.09.015. Epub 2014 Sep 18. J Ethnopharmacol. 2014. PMID: 25240586
- Indigenous knowledge of medicinal plants used by the Reang tribe of Tripura state of India. Shil S, Dutta Choudhury M, Das S. Shil S, et al. J Ethnopharmacol. 2014 Feb 27;152(1):135-41. doi: 10.1016/j.jep.2013.12.037. Epub 2014 Jan 7. J Ethnopharmacol. 2014. PMID: 24412549
- Contributions to the phytotherapies of digestive disorders: Traditional knowledge and cultural drivers of Manoor Valley, Northern Pakistan. Rahman IU, Ijaz F, Afzal A, Iqbal Z, Ali N, Khan SM. Rahman IU, et al. J Ethnopharmacol. 2016 Nov 4;192:30-52. doi: 10.1016/j.jep.2016.06.049. Epub 2016 Jun 25. J Ethnopharmacol. 2016. PMID: 27353866
- Ethnopharmacological study of medicinal plants in Sarvabad, Kurdistan province, Iran. Hosseini SH, Sadeghi Z, Hosseini SV, Bussmann RW. Hosseini SH, et al. J Ethnopharmacol. 2022 Apr 24;288:114985. doi: 10.1016/j.jep.2022.114985. Epub 2022 Jan 13. J Ethnopharmacol. 2022. PMID: 35032582
- An ethnobotanical study of medicinal plants and traditional therapies on Batan Island, the Philippines. Abe R, Ohtani K. Abe R, et al. J Ethnopharmacol. 2013 Jan 30;145(2):554-65. doi: 10.1016/j.jep.2012.11.029. Epub 2012 Nov 23. J Ethnopharmacol. 2013. PMID: 23183086
- Assessing anticancer, antidiabetic, and antioxidant capacities in green-synthesized zinc oxide nanoparticles and solvent-based plant extracts. Azeem M, Siddique MH, Imran M, Zubair M, Mumtaz R, Younas M, Abdel-Maksoud MA, El-Tayeb MA, Rizwan M, Yong JWH. Azeem M, et al. Heliyon. 2024 Jul 4;10(14):e34073. doi: 10.1016/j.heliyon.2024.e34073. eCollection 2024 Jul 30. Heliyon. 2024. PMID: 39092244 Free PMC article.
- The properties and mechanism of action of plant immunomodulators in regulation of immune response - A narrative review focusing on Curcuma longa L. , Panax ginseng C. A. Meyer and Moringa oleifera Lam. Balasubramaniam M, Sapuan S, Hashim IF, Ismail NI, Yaakop AS, Kamaruzaman NA, Ahmad Mokhtar AM. Balasubramaniam M, et al. Heliyon. 2024 Mar 21;10(7):e28261. doi: 10.1016/j.heliyon.2024.e28261. eCollection 2024 Apr 15. Heliyon. 2024. PMID: 38586374 Free PMC article. Review.
- Ethnobotanical study of medicinal plants used by the people of Mosop, Nandi County in Kenya. Maiyo ZC, Njeru SN, Toroitich FJ, Indieka SA, Obonyo MA. Maiyo ZC, et al. Front Pharmacol. 2024 Jan 19;14:1328903. doi: 10.3389/fphar.2023.1328903. eCollection 2023. Front Pharmacol. 2024. PMID: 38313073 Free PMC article.
- Ethnobotanical and ethnopharmacological survey of medicinal tree species used in the treatment of diseases by forest-fringe communities of Southwestern Ghana. Asigbaase M, Adusu D, Musah AA, Anaba L, Nsor CA, Abugre S, Derkyi M. Asigbaase M, et al. Heliyon. 2023 Dec 14;10(1):e23645. doi: 10.1016/j.heliyon.2023.e23645. eCollection 2024 Jan 15. Heliyon. 2023. PMID: 38226220 Free PMC article.
- Ethnomedicinal plants used for the prevention and treatment of anemia in the Philippines: a systematic review. Magtalas MC, Balbin PT, Cruz EC, Clemente RF, Buan AKG, Garcia JP, Lee KY, Tantengco OAG. Magtalas MC, et al. Trop Med Health. 2023 May 12;51(1):27. doi: 10.1186/s41182-023-00515-x. Trop Med Health. 2023. PMID: 37170350 Free PMC article. Review.
- UNESCO. Report of the IBC on traditional medicine systems and their ethical implications. 2013. https://unesdoc.unesco.org/ark:/48223/pf0000217457 . Accessed 15 Aug 2019.
- WHO. World Health Organization traditional medicine strategy: 2014-2023. WHO Library Cataloguing-in-Publication Data. 2013. https://apps.who.int/iris/bitstream/handle/10665/92455/9789241506090_eng... . Accessed 16 Aug 2019.
- WHO. Regulatory situation of herbal medicines. A worldwide review. Geneva: World Health Organization. 1998. p. 1–5.
- Jamshidi-Kia F, Lorigooini Z, Amini-Khoei H. Medicinal plants: past history and future perspective. J HerbMed Pharmacol. 2018;7:1–7. doi: 10.15171/jhp.2018.01. - DOI
- Farnsworth NR. Ethnopharmacology and drug development. Ciba found Symp. 1994;185:42–59. doi: 10.1002/9780470514634.ch4. - DOI - PubMed
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- BioMed Central
- Europe PubMed Central
- PubMed Central
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Research article
- Open access
- Published: 06 January 2021
Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study
- Aaron J. Harries ORCID: orcid.org/0000-0001-7107-0995 1 ,
- Carmen Lee 1 ,
- Lee Jones 2 ,
- Robert M. Rodriguez 1 ,
- John A. Davis 2 ,
- Megan Boysen-Osborn 3 ,
- Kathleen J. Kashima 4 ,
- N. Kevin Krane 5 ,
- Guenevere Rae 6 ,
- Nicholas Kman 7 ,
- Jodi M. Langsfeld 8 &
- Marianne Juarez 1
BMC Medical Education volume 21 , Article number: 14 ( 2021 ) Cite this article
145k Accesses
158 Citations
37 Altmetric
Metrics details
The COVID-19 pandemic disrupted the United States (US) medical education system with the necessary, yet unprecedented Association of American Medical Colleges (AAMC) national recommendation to pause all student clinical rotations with in-person patient care. This study is a quantitative analysis investigating the educational and psychological effects of the pandemic on US medical students and their reactions to the AAMC recommendation in order to inform medical education policy.
The authors sent a cross-sectional survey via email to medical students in their clinical training years at six medical schools during the initial peak phase of the COVID-19 pandemic. Survey questions aimed to evaluate students’ perceptions of COVID-19’s impact on medical education; ethical obligations during a pandemic; infection risk; anxiety and burnout; willingness and needed preparations to return to clinical rotations.
Seven hundred forty-one (29.5%) students responded. Nearly all students (93.7%) were not involved in clinical rotations with in-person patient contact at the time the study was conducted. Reactions to being removed were mixed, with 75.8% feeling this was appropriate, 34.7% guilty, 33.5% disappointed, and 27.0% relieved.
Most students (74.7%) agreed the pandemic had significantly disrupted their medical education, and believed they should continue with normal clinical rotations during this pandemic (61.3%). When asked if they would accept the risk of infection with COVID-19 if they returned to the clinical setting, 83.4% agreed.
Students reported the pandemic had moderate effects on their stress and anxiety levels with 84.1% of respondents feeling at least somewhat anxious. Adequate personal protective equipment (PPE) (53.5%) was the most important factor to feel safe returning to clinical rotations, followed by adequate testing for infection (19.3%) and antibody testing (16.2%).
Conclusions
The COVID-19 pandemic disrupted the education of US medical students in their clinical training years. The majority of students wanted to return to clinical rotations and were willing to accept the risk of COVID-19 infection. Students were most concerned with having enough PPE if allowed to return to clinical activities.
Peer Review reports
The COVID-19 pandemic has tested the limits of healthcare systems and challenged conventional practices in medical education. The rapid evolution of the pandemic dictated that critical decisions regarding the training of medical students in the United States (US) be made expeditiously, without significant input or guidance from the students themselves. On March 17, 2020, for the first time in modern US history, the Association of American Medical Colleges (AAMC), the largest national governing body of US medical schools, released guidance recommending that medical students immediately pause all clinical rotations to allow time to obtain additional information about the risks of COVID-19 and prepare for safe participation in the future. This decisive action would also conserve scarce resources such as personal protective equipment (PPE) and testing kits; minimize exposure of healthcare workers (HCWs) and the general population; and protect students’ education and wellbeing [ 1 ].
A similar precedent was set outside of the US during the SARS-CoV1 epidemic in 2003, where an initial cluster of infection in medical students in Hong Kong resulted in students being removed from hospital systems where SARS surfaced, including Hong Kong, Singapore and Toronto [ 2 , 3 ]. Later, studies demonstrated that the exclusion of Canadian students from those clinical environments resulted in frustration at lost learning opportunities and students’ inability to help [ 3 ]. International evidence also suggests that medical students perceive an ethical obligation to participate in pandemic response, and are willing to participate in scenarios similar to the current COVID-19 crisis, even when they believe the risk of infection to themselves to be high [ 4 , 5 , 6 ].
The sudden removal of some US medical students from educational settings has occurred previously in the wake of local disasters, with significant academic and personal impacts. In 2005, it was estimated that one-third of medical students experienced some degree of depression or post-traumatic stress disorder (PTSD) after Hurricane Katrina resulted in the closure of Tulane University School of Medicine [ 7 ].
Prior to the current COVID-19 pandemic, we found no studies investigating the effects of pandemics on the US medical education system or its students. The limited pool of evidence on medical student perceptions comes from two earlier global coronavirus surges, SARS and MERS, and studies of student anxiety related to pandemics are also limited to non-US populations [ 3 , 8 , 9 ]. Given the unprecedented nature of the current COVID-19 pandemic, there is concern that students may be missing out on meaningful educational experiences and months of clinical training with unknown effects on their current well-being or professional trajectory [ 10 ].
Our study, conducted during the initial peak phase of the COVID-19 pandemic, reports students’ perceptions of COVID-19’s impact on: medical student education; ethical obligations during a pandemic; perceptions of infection risk; anxiety and burnout; willingness to return to clinical rotations; and needed preparations to return safely. This data may help inform policies regarding the roles of medical students in clinical training during the current pandemic and prepare for the possibility of future pandemics.
We conducted a cross-sectional survey during the initial peak phase of the COVID-19 pandemic in the United States, from 4/20/20 to 5/25/20, via email sent to all clinically rotating medical students at six US medical schools: University of California San Francisco School of Medicine (San Francisco, CA), University of California Irvine School of Medicine (Irvine, CA), Tulane University School of Medicine (New Orleans, LA), University of Illinois College of Medicine (Chicago, Peoria, Rockford, and Urbana, IL), Ohio State University College of Medicine (Columbus, OH), and Zucker School of Medicine at Hofstra/Northwell (Hempstead, NY). Traditional undergraduate medical education in the US comprises 4 years of medical school with 2 years of primarily pre-clinical classroom learning followed by 2 years of clinical training involving direct patient care. Study participants were defined as medical students involved in their clinical training years at whom the AAMC guidance statement was directed. Depending on the curricular schedule of each medical school, this included intended graduation class years of 2020 (graduating 4th year student), 2021 (rising 4th year student), and 2022 (rising 3rd year student), exclusive of planned time off. Participating schools were specifically chosen to represent a broad spectrum of students from different regions of the country (West, South, Midwest, East) with variable COVID-19 prevalence. We excluded medical students not yet involved in clinical rotations. This study was deemed exempt by the respective Institutional Review Boards.
We developed a survey instrument modeled after a survey used in a previously published peer reviewed study evaluating the effects of the COVID-19 pandemic on Emergency Physicians, which incorporated items from validated stress scales [ 11 ]. The survey was modified for use in medical students to assess perceptions of the following domains: perceived impact on medical student education; ethical beliefs surrounding obligations to participate clinically during the pandemic; perceptions of personal infection risk; anxiety and burnout related to the pandemic; willingness to return to clinical rotations; and preparation needed for students to feel safe in the clinical environment. Once created, the survey underwent an iterative process of input and review from our team of authors with experience in survey methodology and psychometric measures to allow for optimization of content and validity. We tested a pilot of our preliminary instrument on five medical students to ensure question clarity, and confirm completion of the survey in approximately 10 min. The final survey consisted of 29 Likert, yes/no, multiple choice, and free response questions. Both medical school deans and student class representatives distributed the survey via email, with three follow-up emails to increase response rates. Data was collected anonymously.
For example, to assess the impact on students’ anxiety, participants were asked, “How much has the COVID-19 pandemic affected your stress or anxiety levels?” using a unipolar 7-point scale (1 = not at all, 4 = somewhat, 7 = extremely). To assess willingness to return to clinical rotations, participants were asked to rate on a bipolar scale (1 = strongly disagree, 2 = disagree, 3 = somewhat disagree, 4 = neither disagree nor agree, 5 = somewhat agree, 6 = agree, and 7 = strongly agree) their agreement with the statement: “to the extent possible, medical students should continue with normal clinical rotations during this pandemic.” (Survey Instrument, Supplemental Table 1 ).
Survey data was managed using Qualtrics hosted by the University of California, San Francisco. For data analysis we used STATA v15.1 (Stata Corp, College Station, TX). We summarized respondent characteristics and key responses as raw counts, frequency percent, medians and interquartile ranges (IQR). For responses to bipolar questions, we combined positive responses (somewhat agree, agree, or strongly agree) into an agreement percentage. To compare differences in medians we used a signed rank test with p value < 0.05 to show statistical difference. In a secondary analysis we stratified data to compare questions within key domains amongst the following sub-groups: female versus male, graduation year, local community COVID-19 prevalence (high, medium, low), and students on clinical rotations with in-person patient care. This secondary analysis used a chi square test with p value < 0.05 to show statistical difference between sub-group agreement percentages.
Of 2511 students contacted, we received 741 responses (29.5% response rate). Of these, 63.9% of respondents were female and 35.1% were male, with 1.0% reporting a different gender identity; 27.7% of responses came from the class of 2020, 53.5% from the class of 2021, and 18.7% from the class of 2022. (Demographics, Table 1 ).
Most student respondents (74.9%) had a clinical rotation that was cut short or canceled due to COVID-19 and 93.7% reported not being involved in clinical rotations with in-person patient contact at the time of the study. Regarding students’ perceptions of cancelled rotations (allowing for multiple reactions), 75.8% felt this was appropriate, 34.7% felt guilty for not being able to help patients and colleagues, 33.5% felt disappointed, and 27.0% felt relieved.
Most students (74.7%) agreed that their medical education had been significantly disrupted by the pandemic. Students also felt they were able to find meaningful learning experiences during the pandemic (72.1%). Free response examples included: taking a novel COVID-19 pandemic elective course, telehealth patient care, clinical rotations transitioned to virtual online courses, research or education electives, clinical and non-clinical COVID-19-related volunteering, and self-guided independent study electives. Students felt their medical schools were doing everything they could to help students adjust (72.7%). Overall, respondents felt the pandemic had interfered with their ability to develop skills needed to prepare for residency (61.4%), though fewer (45.7%) felt it had interfered with their ability to apply to residency. (Educational Impact, Fig. 1 ).
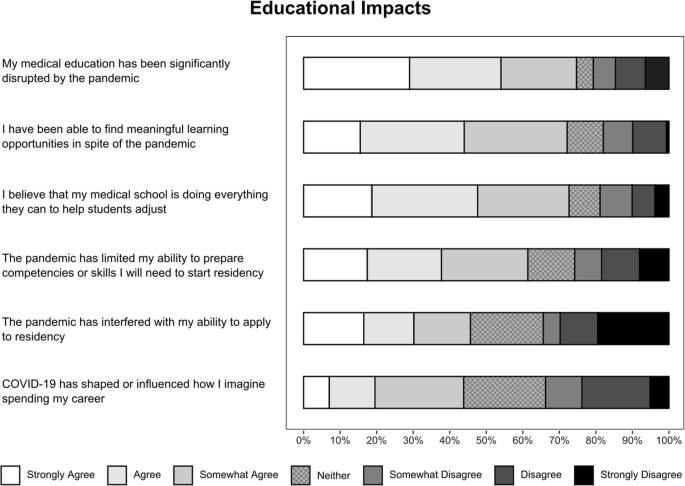
Perceived educational impacts of the COVID-19 pandemic on medical students
A majority of medical students agreed they should be allowed to continue with normal clinical rotations during this pandemic (61.3%). Most students agreed (83.4%) that they accepted the risk of being infected with COVID-19, if they returned. When asked if students should be allowed to volunteer in clinical settings even if there is not a healthcare worker (HCW) shortage, 63.5% agreed; however, in the case of a HCW shortage only 19.5% believed students should be required to volunteer clinically. (Willingness to Participate Clinically, Fig. 2 ).
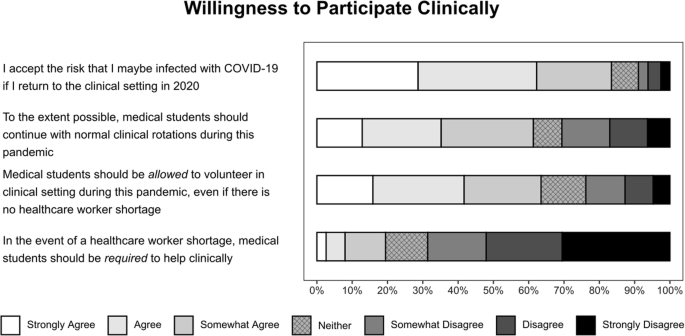
Willingness to participate clinically during the COVID-19 pandemic
When asked if they perceived a moral, ethical, or professional obligation for medical students to help, 37.8% agreed that medical students have such an obligation during the current pandemic. This is in contrast to their perceptions of physicians: 87.1% of students agreed with a physician obligation to help during the COVID-19 pandemic. For both groups, students were asked if this obligation persisted without adequate PPE: only 10.9% of students believed medical students had this obligation, while 34.0% agreed physicians had this obligation. (Ethical Obligation, Fig. 3 ).
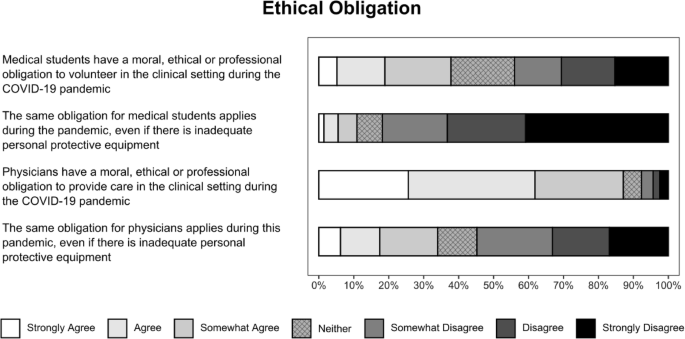
Ethical obligation to volunteer during the COVID-19 pandemic
Given the assumption that there will not be a COVID-19 vaccine until 2021, students felt the single most important factor in a safe return to clinical rotations was having access to adequate PPE (53.3%), followed by adequate testing for infection (19.3%) and antibody testing for possible immunity (16.2%). Few students (5%) stated that nothing would make them feel comfortable until a vaccine is available. On a 1–7 scale (1 = not at all, 4 = somewhat, 7 = extremely), students felt somewhat prepared to use PPE during this pandemic in the clinical setting, median = 4 (IQR 4,6), and somewhat confident identifying symptoms most concerning for COVID-19, median = 4 (IQR 4,5). Students preferred to learn about PPE via video demonstration (76.7%), online modules (47.7%), and in-person or Zoom style conferences (44.7%).
Students believed they were likely to contract COVID-19 in general (75.6%), independent of a return to the clinical environment. Most respondents believed that missing some school or work would be a likely outcome (90.5%), and only a minority of students believed that hospitalization (22.1%) or death (4.3%) was slightly, moderately, or extremely likely.
On a 1–7 scale (1 = not at all, 4 = somewhat, and 7 = extremely), the median (IQR) reported effect of the COVID-19 pandemic on students’ stress or anxiety level was 5 (4, 6) with 84.1% of respondents feeling at least somewhat anxious due to the pandemic. Students’ perceived emotional exhaustion and burnout before the pandemic was a median = 2 (IQR 2,4) and since the pandemic started a median = 4 (IQR 2,5) with a median difference Δ = 2, p value < 0.001.
Secondary analysis of key questions revealed statistical differences between sub-groups. Women were significantly more likely than men to agree that the pandemic had affected their anxiety. Several significant differences existed for the class of 2020 when compared to the classes of 2021 and 2022: they were less likely to report disruptions to their education, to prefer to return to rotations, and to report an effect on anxiety. There were no significant differences with students who were still involved with in-person patient care compared with those who were not. In comparing areas with high COVID-19 prevalence at the time of the survey (New York and Louisiana) with medium (Illinois and Ohio) and low prevalence (California), students were less likely to report that the pandemic had disrupted their education. Students in low prevalence areas were most likely to agree that medical students should return to rotations. There were no differences between prevalence groups in accepting the risk of infection to return, or subjective anxiety effects. (Stratification, Table 2 ).
The COVID-19 pandemic has fundamentally transformed education at all levels - from preschool to postgraduate. Although changes to K-12 and college education have been well documented [ 12 , 13 ], there have been very few studies to date investigating the effects of COVID-19 on undergraduate medical education [ 14 ]. To maintain the delicate balance between student safety and wellbeing, and the time-sensitive need to train future physicians, student input must guide decisions regarding their roles in the clinical arena. Student concerns related to the pandemic, paired with their desire to return to rotations despite the risks, suggest that medical students may take on emotional burdens as members of the patient care team even when not present in the clinical environment. This study offers insight into how best to support medical students as they return to clinical rotations, how to prepare them for successful careers ahead, and how to plan for their potential roles in future pandemics.
Previous international studies of medical student attitudes towards hypothetical influenza-like pandemics demonstrated a willingness (80%) [ 4 ] and a perceived ethical obligation to volunteer (77 and 70%), despite 40% of Canadian students in one study perceiving a high likelihood of becoming infected [ 5 , 6 ]. Amidst the current COVID-19 pandemic, our participants reported less agreement with a medical student ethical obligation to volunteer in the clinical setting at 37.8%, but believed in a higher likelihood of becoming infected at 75.6%. Their willingness to be allowed to volunteer freely (63.5%) may suggest that the stresses of an ongoing pandemic alter students’ perceptions of the ethical requirement more than their willingness to help. Students overwhelmingly agreed that physicians had an ethical obligation to provide care during the COVID-19 pandemic (87.1%), possibly reflecting how they view the ethical transition from student to physician, or differences between paid professionals and paying for an education.
At the time our study was conducted, there were widespread concerns for possible HCW shortages. It was unclear whether medical students would be called to volunteer when residents became ill, or even graduate early to start residency training immediately (as occurred at half of schools surveyed). This timing allowed us to capture a truly unique perspective amongst medical students, a majority of whom reported increased anxiety and burnout due to the pandemic. At the same time, students felt that their medical schools were doing everything possible to support them, perhaps driven by virtual town halls and daily communication updates.
Trends in secondary analysis show important differences in the impacts of the pandemic. Women were more likely to report increased anxiety as compared to men, which may reflect broader gender differences in medical student anxiety [ 15 ] but requires more study to rule out different pandemic stresses by gender. Graduating medical students (class of 2020) overall described less impact on medical education and anxiety, a decreased desire to return to rotations, but equal acceptance of the risk of infection in clinical settings, possibly reflecting a focus on their upcoming intern year rather than the remaining months of undergraduate medical education. Since this class’s responses decreased overall agreement on these questions, educational impacts and anxiety effects may have been even greater had they been assessed further from graduation. Interestingly, students from areas with high local COVID-19 prevalence (New York and Louisiana) reported a less significant effect of the pandemic on their education, a paradoxical result that may indicate that medical student tolerance for the disruptions was greater in high-prevalence areas, as these students were removed at the same, if not higher, rates as their peers. Our results suggest that in future waves of the current pandemic or other disasters, students may be more patient with educational impacts when they have more immediate awareness of strains on the healthcare system.
A limitation of our study was the survey response rate, which was anticipated given the challenges students were facing. Some may not have been living near campus; others may have stopped reading emails due to early graduation or limited access to email; and some would likely be dealing with additional personal challenges related to the pandemic. We attempted to increase response rates by having the study sent directly from medical school deans and leadership, as well as respective class representatives, and by sending reminders for completion. The survey was not incentivized, and a higher response rate in the class of 2021 across all schools may indicate that students who felt their education was most affected were most likely to respond. We addressed this potential source of bias in the secondary analysis, which showed no differences between 2021 and 2022 respondents. Another limitation was the inherent issue with survey data collection of missing responses for some questions that occurred in a small number of surveys. This resulted in slight variability in the total responses received for certain questions, which were not statistically significant. To be transparent about this limitation, we presented our data by stating each total response and denominator in the Tables.
This initial study lays the groundwork for future investigations and next steps. With 72.1% of students agreeing that they were able to find meaningful learning in spite of the pandemic, future research should investigate novel learning modalities that were successful during this time. Educators should consider additional training on PPE use, given only moderate levels of student comfort in this area, which may be best received via video. It is also important to study the long-term effects of missing several months of essential clinical training and identifying competencies that may not have been achieved, since students perceived a significant disruption to their ability to prepare skills for residency. Next steps could be to study curriculum interventions, such as capstone boot camps and targeted didactic skills training, to help students feel more comfortable as they transition into residency. Educators must also acknowledge that some students may not feel comfortable returning to the clinical environment until a vaccine becomes available (5%) and ensure they are equally supported. Lastly, it is vital to further investigate the mental health effects of the pandemic on medical students, identifying subgroups with additional stressors, needs related to anxiety or possible PTSD, and ways to minimize these negative effects.
In this cross-sectional survey, conducted during the initial peak phase of the COVID-19 pandemic, we capture a snapshot of the effects of the pandemic on US medical students and gain insight into their reactions to the unprecedented AAMC national recommendation for removal from clinical rotations. Student respondents from across the US similarly recognized a significant disruption to their medical education, shared a desire to continue with in-person rotations, and were willing to accept the risk of infection with COVID-19. Our novel results provide a solid foundation to help shape medical student roles in the clinical environment during this pandemic and future outbreaks.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Association of American Medical Colleges. Interim Guidance on Medical Students’ Participation in Direct Patient Contact Activities: Principles and Guidelines. https://www.aamc.org/news-insights/press-releases/important-guidance-medical-students-clinical-rotations-during-coronavirus-covid-19-outbreak . Published March 17, 2020. Accessed April 1, 2020.
Clark J. Fear of SARS thwarts medical education in Toronto. BMJ. 2003;326(7393):784. https://doi.org/10.1136/bmj.326.7393.784/c .
Article Google Scholar
Loh LC, Ali AM, Ang TH, Chelliah A. Impact of a spreading epidemic on medical students. Malays J Med Sci. 2006;13(2):30–6.
Google Scholar
Mortelmans LJ, Bouman SJ, Gaakeer MI, Dieltiens G, Anseeuw K, Sabbe MB. Dutch senior medical students and disaster medicine: a national survey. Int J Emerg Med. 2015;8(1):77. https://doi.org/10.1186/s12245-015-0077-0 .
Huapaya JA, Maquera-Afaray J, García PJ, Cárcamo C, Cieza JA. Conocimientos, prácticas y actitudes hacia el voluntariado ante una influenza pandémica: estudio transversal con estudiantes de medicina en Perú [Knowledge, practices and attitudes toward volunteer work in an influenza pandemic: cross-sectional study with Peruvian medical students]. Medwave. 2015;15(4):e6136Published 2015 May 8. https://doi.org/10.5867/medwave.2015.04.6136 .
Herman B, Rosychuk RJ, Bailey T, Lake R, Yonge O, Marrie TJ. Medical students and pandemic influenza. Emerg Infect Dis. 2007;13(11):1781–3. https://doi.org/10.3201/eid1311.070279 .
Kahn MJ, Markert RJ, Johnson JE, Owens D, Krane NK. Psychiatric issues and answers following hurricane Katrina. Acad Psychiatry. 2007;31(3):200–4. https://doi.org/10.1176/appi.ap.31.3.200 .
Al-Rabiaah A, Temsah MH, Al-Eyadhy AA, et al. Middle East respiratory syndrome-Corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health. 2020;13(5):687–91. https://doi.org/10.1016/j.jiph.2020.01.005 .
Wong JG, Cheung EP, Cheung V, et al. Psychological responses to the SARS outbreak in healthcare students in Hong Kong. Med Teach. 2004;26(7):657–9. https://doi.org/10.1080/01421590400006572 .
Stokes DC. Senior medical students in the COVID-19 response: an opportunity to be proactive. Acad Emerg Med. 2020;27(4):343–5. https://doi.org/10.1111/acem.13972 .
Rodriguez RM, Medak AJ, Baumann BM, et al. Academic emergency medicine physicians’ anxiety levels, stressors, and potential mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27(8):700–7. https://doi.org/10.1111/acem.14065 .
Sahu P. Closure of universities due to coronavirus disease 2019 (COVID-19): impact on education and mental health of students and academic staff. Cureus. 2020;12(4):e7541Published 2020 Apr 4. https://doi.org/10.7759/cureus.7541 .
Reimers FM, Schleicher A. A framework to guide an education response to the COVID-19 pandemic of 2020: OECD. https://www.hm.ee/sites/default/files/framework_guide_v1_002_harward.pdf .
Choi B, Jegatheeswaran L, Minocha A, Alhilani M, Nakhoul M, Mutengesa E. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Med Educ. 2020;20:206–16. https://doi.org/10.1186/s12909-020-02117-1 .
Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81(4):354–73. https://doi.org/10.1097/00001888-200604000-00009 .
Download references
Acknowledgments
The authors wish to thank Newton Addo, UCSF Statistician.
Author information
Authors and affiliations.
Department of Emergency Medicine, University of California San Francisco School of Medicine, San Francisco General Hospital, 1001 Potrero Avenue, Building 5, Room #6A4, San Francisco, California, 94110, USA
Aaron J. Harries, Carmen Lee, Robert M. Rodriguez & Marianne Juarez
University of California San Francisco School of Medicine, San Francisco, California, USA
Lee Jones & John A. Davis
Clinical Emergency Medicine, University of California Irvine School of Medicine, Irvine, CA, USA
Megan Boysen-Osborn
University of Illinois College of Medicine, Chicago, IL, USA
Kathleen J. Kashima
Deming Department of Medicine, Tulane University School of Medicine, New Orleans, Louisiana, USA
N. Kevin Krane
Basic Science Education, Tulane University School of Medicine, New Orleans, Louisiana, USA
Guenevere Rae
Emergency Medicine, Ohio State College of Medicine, Columbus, OH, USA
Nicholas Kman
Department of Science Education, Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, New York, USA
Jodi M. Langsfeld
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the study and met the specific conditions listed in the BMC Medical Education editorial policy for authorship. All authors have read and approved the manuscript. AH as principal investigator contributed to study design, survey instrument creation, IRB submission for his respective medical school, acquisition of data and recruitment of other participating medical schools, data analysis, writing and editing the manuscript. CL contributed to background literature review, study design, survey instrument creation, acquisition of data, data analysis, writing and editing the manuscript. LJ contributed to study design, survey instrument creation, acquisition of data from his respective medical school and recruitment of other participating medical schools, data analysis, and editing the manuscript. RR contributed to study design, survey instrument creation, data analysis, writing and editing the manuscript. JD contributed to study design, survey instrument creation, recruitment of other participating medical schools, data analysis, and editing the manuscript. MBO contributed as individual site principal investigator obtaining IRB exemption acceptance and acquisition of data from her respective medical school along with editing the manuscript. KK contributed as individual site principal investigator obtaining IRB exemption acceptance and acquisition of data from her respective medical school along with editing the manuscript. NKK contributed as individual site co-principal investigator obtaining IRB exemption acceptance and acquisition of data from his respective medical school along with editing the manuscript. GR contributed as individual site co-principal investigator obtaining IRB exemption acceptance and acquisition of data from her respective medical school along with editing the manuscript. NK contributed as individual site principal investigator obtaining IRB exemption acceptance and acquisition of data from his respective medical school along with editing the manuscript. JL contributed as individual site principal investigator obtaining IRB exemption acceptance and acquisition of data from her respective medical school along with editing the manuscript. MJ contributed to study design, survey instrument creation, data analysis, writing and editing the manuscript.
Corresponding authors
Correspondence to Aaron J. Harries or Marianne Juarez .
Ethics declarations
Ethics approval and consent to participate.
This study was reviewed and deemed exempt by each participating medical school’s Institutional Review Board (IRB): University of California San Francisco School of Medicine, IRB# 20–30712, Reference# 280106, Tulane University School of Medicine, Reference # 2020–331, University of Illinois College of Medicine), IRB Protocol # 2012–0783, Ohio State University College of Medicine, Study ID# 2020E0463, Zucker School of Medicine at Hofstra/Northwell, Reference # 20200527-SOM-LAN-1, University of California Irvine School of Medicine, submitted self-exemption IRB form. In accordance with the IRB exemption approval, each survey participant received an email consent describing the study and their optional participation.
Consent for publication
This manuscript does not contain any individualized person’s data, therefore consent for publication was not necessary according to the IRB exemption approval.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: table s1..
Survey Instrument
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Harries, A.J., Lee, C., Jones, L. et al. Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study. BMC Med Educ 21 , 14 (2021). https://doi.org/10.1186/s12909-020-02462-1
Download citation
Received : 29 July 2020
Accepted : 16 December 2020
Published : 06 January 2021
DOI : https://doi.org/10.1186/s12909-020-02462-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Undergraduate medical education
- COVID-19 pandemic
- Medical student anxiety
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Folk Medicine in the Philippines: A Phenomenological Study of Health-Seeking Individuals

2021, International Journal of Medical Students
Background: Folk medicine refers to traditional healing practices anchored on cultural beliefs of body physiology and health preservation. Reflective of indigenous heritage, it fosters a better understanding of health and disease, healthcare systems, and biocultural adaptation. In the Philippines, Quiapo is a well-known site for folk medicine services, cultural diversity, religious practices, and economic activities. Methods: This study utilized a phenomenological approach to comprehend the lived experiences of health-seeking individuals and the meaning behind their acquisition of folk medicine products. Using convenience sampling, seven participants acquiring folk medicine products in Quiapo on the day of data collection were approached and interviewed on separate instances. The collected data subsequently underwent thematic analysis. Results: Analysis revealed three emergent themes: health-seeking behavior, sources of knowledge, and folk medicine utilization. Health-seeking behavi...
Related Papers
Cognizance Journal of Multidisciplinary Studies
Cognizance Journal Multidisciplinary Studies , MICHAEL BIBON
For many years, folk medicine has been the resort of many less privileged families who do not have access to modern health care facilities. A parasantigwar is a term coined to a folk healer in Cagraray island, Philippines, a native version of a doctor trained in traditional manner providing indigenous medicinal help in the locale. This study aimed to ground the lived experiences of these parasantigwar on their acquisition of folk healing skills. Phenomenology approach was conducted by immersion and interview to 8 identified parasantigwar through referral sampling technique. Result revealed that (1) apprenticeship to a folk healer in the family and (2) life setbacks of families were grounds which opted the parasantigwar to resort into traditional healing through cultural transmission and motivation by needs deficiency. This resulted to the parasantigwar's acquisition of practices through (1) passed knowledge and (2) aggregated learned skill. It was concluded that family plays an important role in the assimilation of the folk healing skill where this immediate environment is responsible for the transmission of the observed culture and development of motivation to suffice needs. Further studies need to be conducted to understand healing practices especially to the surrounding islands showing similarity in origins of folk healing practice.
WEENALEI FAJARDO
The study aims to know the socio-demographic profile of traditional health practitioners of Bolinao, Pangasinan which will serve as baseline data for future correlation studies on cultural transmission and erosion involving ethnobotanical knowledge. Survey method was used in the study with 19 respondents which were purposively sampled. Socio-demographic characters such as sex, age, civil status, education, primary occupation, religion, number of children, and number of years practicing traditional healing were recorded. Results showed that they are mostly male, have the age of 60 and above, married, elementary graduates, Catholic, have more than three children, have 16-20 years of experience in traditional healing and have the primary occupation of fishing. It was revealed also in the study that the presence of deployed barangay health workers discouraged the consultation of folks to traditional health practitioners although herbalists were documented as such. Keywords—Socio-demogra...
Rai Anne Espole , christian muhat
This study aims to present the correlation between the two fields of medicine and distinguish whether it is better to move forward and leave folk medicine behind and only practice modern medicine or incorporate traditional medicine in today’s modern medicine.
Jovina Lazo
Human Organization
Marc Micozzi
Asia in transition
RACQUEL BARCELO
This thesis examines the social patterning in the use of traditional Javanese plant medicines, collectively called jamu, within the primarily ethnic Javanese city of Yogyakarta, in central Java, Indonesia. Using both qualitative and quantitative ethnographic research methods, forty-eight common and uncommon types of jamu are discussed, and five predictions are evaluated: 1. Jamu sold daily by door to door vendors (jamu gendong) will most often be preventatives, rather than curatives; 2. Jamu sold by sedentary vendors will more often be used for specific illnesses (curatives) than those sold by door to door vendors (jamu gendong),· 3. Seasonal differences (rainy versus dry seasons) will be observed in jamu use patterns; 4. Individuals of low economic standing will use both preventative and curative jamu remedies regularly for both minor health concerns and serious illnesses; and, 5. Individuals of high economic standing will generally use curative jamu only for disorders that are not...
Bannag: A Journal of Local Knowledge
The study of folk medicine in our country can be a ground of research and documentation. Presently, there is good number of folk medicine in almost all parts of the Philippines. In response to this, the present study attempted to gather information and data in the municipality of Baggao about the use of alternative medicines and practices in promoting health care. Descriptive design was used in the study. Results revealed that the people of Baggao, Cagayan accept the use of various herbal plnats as alternative medicines in treating different illnesses. Also, alternative medical practices are widely used in Baggao, Cagayan. And finally, alternative medicines and practices have helped to a large extent in promoting health care in Baggao, Cagayan.
BMC complementary and alternative medicine
György Purebl
Within the intercultural milieu of medical pluralism, a nexus of worldviews espousing distinct explanatory models of illness, our research aims at exploring factors leading to complementary and alternative medicine (CAM) use with special attention to their cultural context. The results are based on medical anthropological fieldwork (participant observation and in-depth interviews) spanning a period from January 2015 to May 2017 at four clinics of Traditional Chinese Medicine in Budapest, Hungary. Participant observation involved 105 patients (males N = 42); in-depth interviews were conducted with patients (N = 9) and practitioners (N = 9). The interviews were coded with Interpretative Phenomenological Analysis; all information was aggregated employing Atlas.ti software. In order to avoid the dichotomization of "push and pull factors," results obtained from the fieldwork and interviews were structured along milestones of the patient journey. These points of reference includ...
Dayang Hajyrayati Awg Kassim
This article presents findings of a survey and an in-depth interview conducted in Pulau Bruit as part of the research project entitled “Traditional health practices and its implication towards health-seeking behavior among the Melanau in Pulau Bruit: Documentation of local heritage”. The aim of the study is to explore health-seeking behavior related to the use of medicinal plant among the Melanau of Pulau Bruit. The survey data and interview reveals factors such as suitability, accessibility, and effectiveness of treatment plays significant roles in determining the health-seeking behavior of the Melanau community of Pulau Bruit. Although the major trend has shown the use of modern and traditional healing practices was combined, a vast majority of the households used medicinal plants totreat minor ailments. The study also reveals that there was a limited transfer of medicinal plants knowledge between generations within the Melanau community of Pulau Bruit. Furthermor, the decline of ...
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
'Healing is not just dealing with your body' A Reflexive Grounded Theory Study Exploring Women's Concepts and Approaches Underlying the Use of Traditional and Complementary Medicine in Indonesia
Nicole Weydmann
EPRA International Journal of Multidisciplinary Research
Romenick Molina
International Journal of Sciences: Basic and Applied Research
Acta Medica Philippina
Nina Carandang
John Paul Duarte
Patrick Van Damme , Evert Thomas , Ermias Lulekal , Cheryl Lans
Reynaldo Inocian
Indian Journal of Public Health
Acta horticulturae
Joanna Michel
tina kartika
Psychology and Education: A Multidisciplinary Journal
Psychology and Education , June Rex Bombales
Ramle Abdullah , Nur Hafizah Ramle
IOP Conference Series Earth and Environmental Science
Nurbaya Nurbaya
May Christina Bugash
Journal of Biodiversity and Environmental Sciences
Darin Jan Tindowen
Shahadat Hossan
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
ORIGINAL RESEARCH article
Impact of the covid-19 pandemic on physical and mental health in lower and upper middle-income asian countries: a comparison between the philippines and china.

- 1 College of Medicine, University of the Philippines Manila, Manila, Philippines
- 2 Faculty of Education, Institute of Cognitive Neuroscience, Huaibei Normal University, Huaibei, China
- 3 Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, Singapore
- 4 Southeast Asia One Health University Network, Chiang Mai, Thailand
- 5 Department of Psychological Medicine, National University Health System, Singapore, Singapore
- 6 Institute of Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore, Singapore
Objective: The differences between the physical and mental health of people living in a lower-middle-income country (LMIC) and upper-middle-income country (UMIC) during the COVID-19 pandemic was unknown. This study aimed to compare the levels of psychological impact and mental health between people from the Philippines (LMIC) and China (UMIC) and correlate mental health parameters with variables relating to physical symptoms and knowledge about COVID-19.
Methods: The survey collected information on demographic data, physical symptoms, contact history, and knowledge about COVID-19. The psychological impact was assessed using the Impact of Event Scale-Revised (IES-R), and mental health status was assessed by the Depression, Anxiety, and Stress Scale (DASS-21).
Findings: The study population included 849 participants from 71 cities in the Philippines and 861 participants from 159 cities in China. Filipino (LMIC) respondents reported significantly higher levels of depression, anxiety, and stress than Chinese (UMIC) during the COVID-19 ( p < 0.01) while only Chinese respondents' IES-R scores were above the cut-off for PTSD symptoms. Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection ( p < 0.05), recent use of but with lower confidence on medical services ( p < 0.01), recent direct and indirect contact with COVID ( p < 0.01), concerns about family members contracting COVID-19 ( p < 0.001), dissatisfaction with health information ( p < 0.001). In contrast, Chinese respondents requested more health information about COVID-19. For the Philippines, student status, low confidence in doctors, dissatisfaction with health information, long daily duration spent on health information, worries about family members contracting COVID-19, ostracization, and unnecessary worries about COVID-19 were associated with adverse mental health. Physical symptoms and poor self-rated health were associated with adverse mental health in both countries ( p < 0.05).
Conclusion: The findings of this study suggest the need for widely available COVID-19 testing in MIC to alleviate the adverse mental health in people who present with symptoms. A health education and literacy campaign is required in the Philippines to enhance the satisfaction of health information.
Introduction
The World Health Organization (WHO) declared coronavirus disease 2019 (COVID-19) to be a Public Health Emergency of International Concern on January 30 ( 1 ) and a pandemic on March 11, 2020 ( 2 ). COVID-19 predominantly presents with respiratory symptoms (cough, sneezing, and sore throat), along with fever, fatigue and myalgia. It is thought to spread through droplets, contaminated surfaces, and asymptomatic individuals ( 3 ). By the end of April, over 3 million people have been infected globally ( 4 ).
The first country to identify the novel virus as the cause of the pandemic was China. The authorities responded with unprecedented restrictions on movement. The response included stopping public transport before Chinese New Year, an annual event that sees workers' mass emigration to their hometowns, and a lockdown of whole cities and regions ( 1 ). Two new hospitals specifically designed for COVID-19 patients were rapidly built in Wuhan. Such measures help slow the transmission of COVID-19 in China. As of May 2, there are 83,959 confirmed cases and 4,637 deaths from the virus in China ( 4 ). The Philippines was also affected early by the current crisis. The first case was suspected on January 22, and the country reported the first death from COVID-19 outside of mainland China ( 5 ). Similar to China, the Philippines implemented lockdowns in Manila. Other measures included the closure of schools and allowing arrests for non-compliance with measures ( 6 ). At the beginning of May, the Philippines recorded 8,772 cases and 579 deaths ( 4 ).
China was one of the more severely affected countries in Asia in the early stage of pandemic ( 7 ) while the Philippines is still experiencing an upward trend in the COVID-19 cases ( 6 ). The gross national income (GNI) per capita of the Philippines and China are USD 3,830 and 9,460, respectively, were classified with lower (LMIC) and upper-middle-income countries (UMIC) by the Worldbank ( 8 ). During the COVID-19 pandemic, five high-income countries (HIC), including the United States, Italy, the United Kingdom, Spain, and France, account for 70% of global deaths ( 9 ). The HIC faced the following challenges: (1) the lack of personal protection equipment (PPE) for healthcare workers; (2) the delay in response strategy; (3) an overstretched healthcare system with the shortage of hospital beds, and (4) a large number of death cases from nursing homes ( 10 ). The COVID-19 crisis threatens to hit lower and middle-income countries due to lockdown excessively and economic recession ( 11 ). A systematic review on mental health in LMIC in Asia and Africa found that LMIC: (1) do not have enough mental health professionals; (2) the negative economic impact led to an exacerbation of mental issues; (3) there was a scarcity of COVID-19 related mental health research in Asian LMIC ( 12 ). This systematic review could not compare participants from different middle-income countries because each study used different questionnaires. During the previous Severe Acute Respiratory Syndrome (SARS) epidemic, the promotion of protective personal health practices to reduce transmission of the SARS virus was found to reduce the anxiety levels in the community ( 13 ).
Before COVID-19, previous studies found that stress might be a modifiable risk factor for depression in LMICs ( 14 ) and UMICs ( 15 – 17 ). Another study involving thirty countries found that unmodifiable risk factors for depression included female gender, and depression became more common in 2004 to 2014 compared to previous periods ( 18 ). Further, there were cultural differences in terms of patient-doctor relationship and attitudes toward healthcare systems before the COVID-19 pandemic. In China, <20% of the general public and medical professionals view the doctor and patient relationship as harmonious ( 19 ). In contrast, Filipino seemed to have more trust and be compliant to doctors' recommendations ( 20 ). Patient satisfaction was more important than hospital quality improvement to maintain patient loyalty to the Chinese healthcare system ( 21 ). For Filipinos, improvement in the quality of healthcare service was found to improve patients' satisfaction ( 22 ).
Based on the above studies, we have the following research questions: (1) whether COVID-19 pandemic could be an important stressor and risk factor for depression for the people living in LMIC and UMIC ( 23 ), (2) Are physical symptoms that resemble COVID-19 infection and other concerns be risk factors for adverse mental health? (3) Are knowledge of COVID-19 and health information protective factors for mental health? (4) Would there be any cultural differences in attitudes toward doctors and healthcare systems during the pandemic between China and the Philippines? We hypothesized that UMIC (China) would have better physical and mental health than LMIC (the Philippines). The aims of this study were (a) to compare the physical and mental health between citizens from an LMIC (the Philippines) and UMIC (China); (b) to correlate psychological impact, depression, anxiety, and stress scores with variables relating to physical symptoms, knowledge, and concerns about COVID-19 in people living in the Philippines (LMIC) and China (UMIC).
Study Design and Study Population
We conducted a cross-cultural and quantitative study to compare Filipinos' physical and mental health with Chinese during the COVID-19 pandemic. The study was conducted from February 28 to March 1 in China and March 28 to April 7, 2020 in the Philippines, when the number of COVID-19 daily reported cases increased in both countries. The Chinese participants were recruited from 159 cities and 27 provinces. The Filipino participants, on the other hand, were recruited from 71 cities and 40 provinces representing the Luzon, Visayas, and Mindanao archipelago. A respondent-driven recruitment strategy was utilized in both countries. The recruitment started with a set of initial respondents who were associated with the Huaibei Normal University of China and the University of the Philippines Manila; who referred other participants by email and social network; these in turn refer other participants across different cities in China and the Philippines.
As both Chinese and Filipino governments recommended that the public minimize face-to-face interaction and isolate themselves during the study period, new respondents were electronically invited by existing study respondents. The respondents completed the questionnaires through an online survey platform (“SurveyStar,” Changsha Ranxing Science and Technology in China and Survey Monkey Online Survey in the Philippines). The Institutional Review Board of the University of Philippines Manila Research Ethics Board (UPMREB 2020-198-01) and Huaibei Normal University (China) approved the research proposal (HBU-IRB-2020-002). All respondents provided informed or implied consent. The collected data were anonymous and treated as confidential.
This study used the National University of Singapore COVID-19 questionnaire, and its psychometric properties had been established in the initial phase of the COVID-19 epidemic ( 24 ). The National University of Singapore COVID-19 questionnaire consisted of questions that covered several areas: (1) demographic data; (2) physical symptoms related to COVID-19 in the past 14 days; (3) contact history with COVID-19 in the past 14 days; and (4) knowledge and concerns about COVID-19.
Demographic data about age, gender, education, household size, marital status, parental status, and residential city in the past 14 days were collected. Physical symptoms related to COVID-19 included breathing difficulty, chills, coryza, cough, dizziness, fever, headache, myalgia, sore throat, nausea, vomiting, and diarrhea. Respondents also rated their physical health status and stated their history of chronic medical illness. In the past 14 days, health service utilization variables included consultation with a doctor in the clinic, being quarantined by the health authority, recent testing for COVID-19 and medical insurance coverage. Knowledge and concerns related to COVID-19 included knowledge about the routes of transmission, level of confidence in diagnosis, source, and level of satisfaction of health information about COVID-19, the likelihood of contracting and surviving COVID-19 and the number of hours spent on viewing information about COVID-19 per day.
The psychological impact of COVID-19 was measured using the Impact of Event Scale-Revised (IES-R). The IES-R is a self-administered questionnaire that has been well-validated in the European and Asian population for determining the extent of psychological impact after exposure to a traumatic event (i.e., the COVID-19 pandemic) within one week of exposure ( 25 , 26 ). This 22-item questionnaire, composed of three subscales, aims to measure the mean avoidance, intrusion, and hyperarousal ( 27 ). The total IES-R score is divided into 0–23 (normal), 24–32 (mild psychological impact), 33–36 (moderate psychological impact) and >37 (severe psychological impact) ( 28 ). The total IES-R score > 24 suggests the presence of post-traumatic stress disorder (PTSD) symptoms ( 29 ).
The respondents' mental health status was measured using the Depression, Anxiety, and Stress Scale (DASS-21) and the calculation of scores was based on a previous Asian study ( 30 ). DASS has been demonstrated to be a reliable and valid measure in assessing mental health in Filipinos ( 31 – 33 ) and Chinese ( 34 , 35 ). IES-R and DASS-21 were previously used in research related to the COVID-19 epidemic ( 26 , 36 – 38 ).
Statistical Analysis
Descriptive statistics were calculated for demographic characteristics, physical symptom, and health service utilization variables, contact history variables, knowledge and concern variables, precautionary measure variables, and additional health information variables. To analyze the differences in the levels of psychological impact, levels of depression, anxiety and stress, the independent sample t -test was used to compare the mean score between the Filipino (LMIC) and Chinese (UMIC) respondents. The chi-squared test was used to analyze the differences in categorical variables between the two samples. We used linear regressions to calculate the univariate associations between independent and dependent variables, including the IES-S score and DASS stress, anxiety, and depression subscale scores for the Filipino and Chinese respondents separately with adjustment for age, marital status, and education levels. All tests were two-tailed, with a significance level of p < 0.05. Statistical analysis was performed on SPSS Statistic 21.0.
Demographic Characteristics and Their Association With Psychological Impact and Adverse Mental Health Status
We received 849 responses from the Philippines and 861 responses from China for 1,710 individual respondents from both countries. The majority of Filipino respondents were women (71.0%), age between 22 and 30 years (26.6%), having a household size of 3–5 people (53.4%), high educational attainment (91.4% with a bachelor or higher degree), and married (68.9%). Similarly, the majority of Chinese respondents were women (75%), having a household size of 3–5 people (80.4%) and high educational attainment (91.4% with a bachelor or higher degree). There was a significantly higher proportion of Chinese respondents who had children younger than 16 years ( p < 0.001) and student status ( p < 0.001; See Table 1 ).
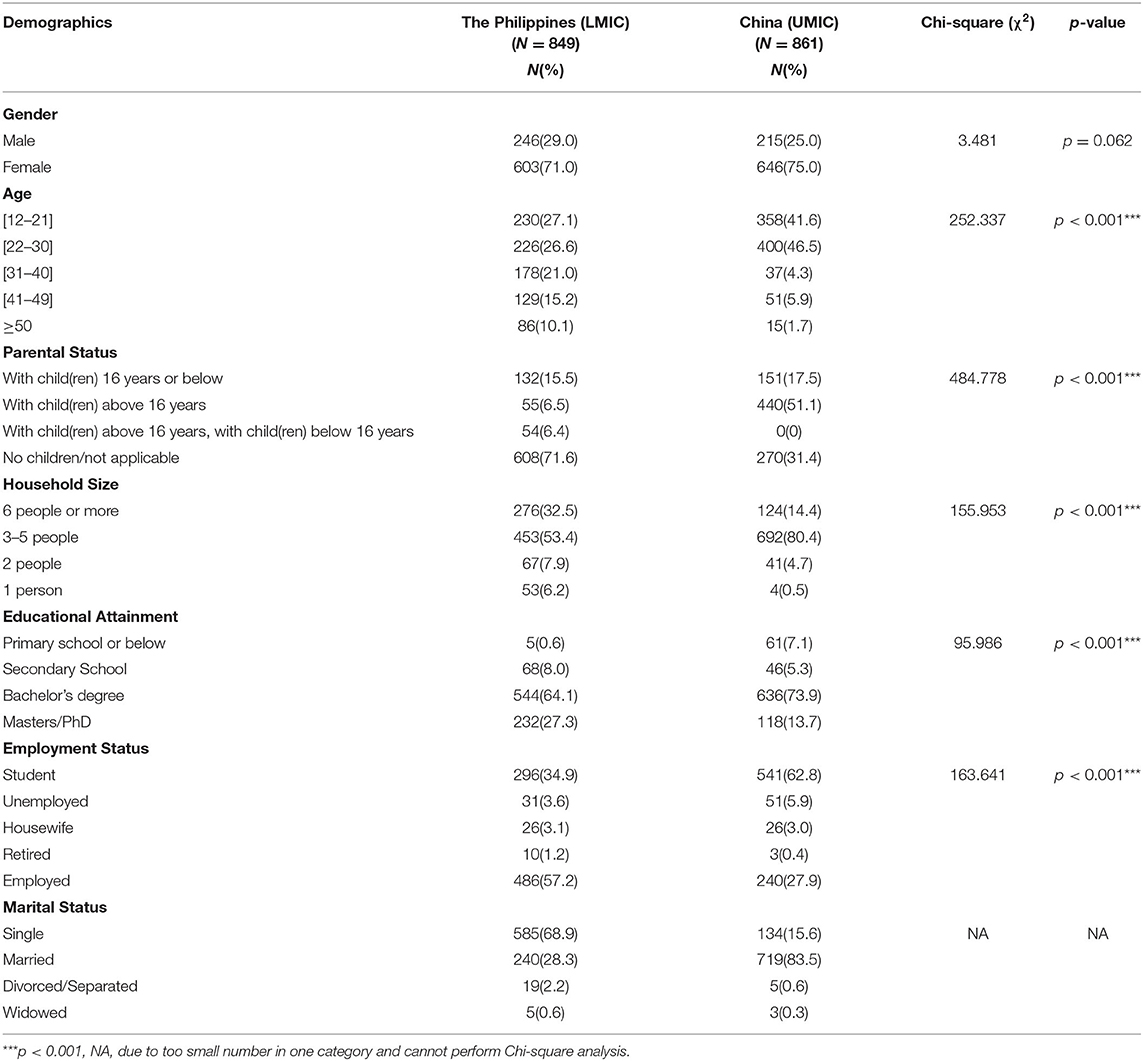
Table 1 . Comparison of demographic characteristics between Filipino (LMIC) and Chinese (UMIC) respondents ( N = 1,710).
For Filipino respondents, the male gender and having a child were protective factors significantly associated with the lower score of IES-R ( p < 0.05) and depression ( p < 0.001), respectively. Single status was significantly associated with depression ( p < 0.05), and student status was associated with higher IES-R, stress and depression scores ( p < 0.01) (see Table 2 ). For Chinese respondents, the male gender was significantly associated with a lower score of IES-R but higher DASS depression scores ( p < 0.01). Notwithstanding, there were other differences between Filipino and China respondents. Chinese respondents who stayed in a household with 3–5 people ( p < 0.05) and more than 6 people ( p < 0.05) were significantly associated with a higher score of IES-R as compared to respondents who stayed alone.
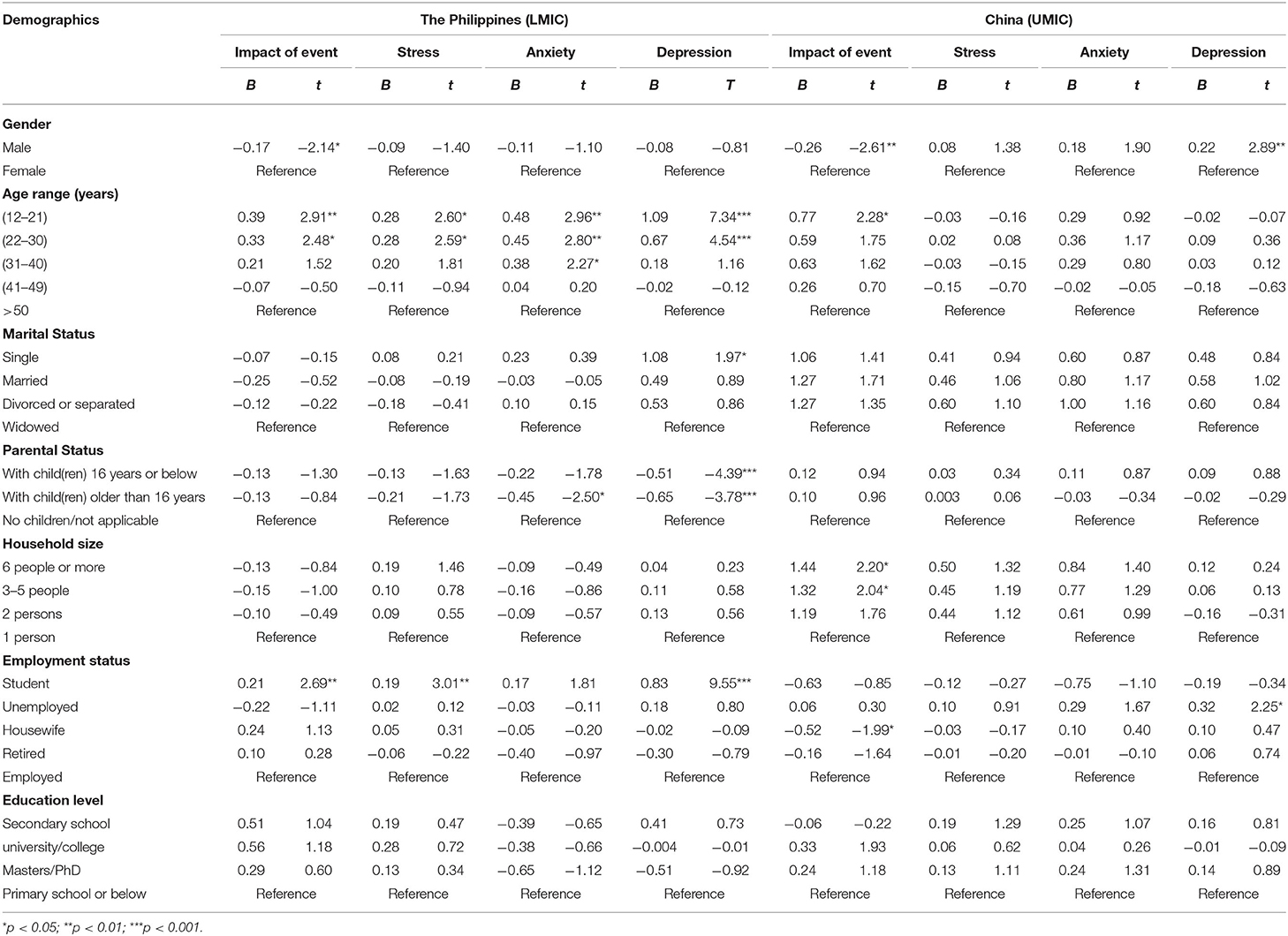
Table 2 . Comparison of the association between demographic variables and the psychological impact as well as adverse mental health status between Filipino (LMIC) and Chinese (UMIC) respondents ( n = 1,710).
Comparison Between the Filipino (LMIC) and Chinese (UMIC) Respondents and Their Mental Health Status
Figure 1 compares the mean scores of DASS-stress, anxiety, and depression subscales and IES-R scores between the Filipino and Chinese respondents. For the DASS-stress subscale, Filipino respondents reported significantly higher stress ( p < 0.001), anxiety ( p < 0.01), and depression ( p < 0.01) than Chinese (UMIC). For IES-R, Filipino (LMIC) had significantly lower scores than Chinese ( p < 0.001). The mean IES-R scores of Chinese were higher than 24 points, indicating the presence of PTSD symptoms in Chinese respondents only.
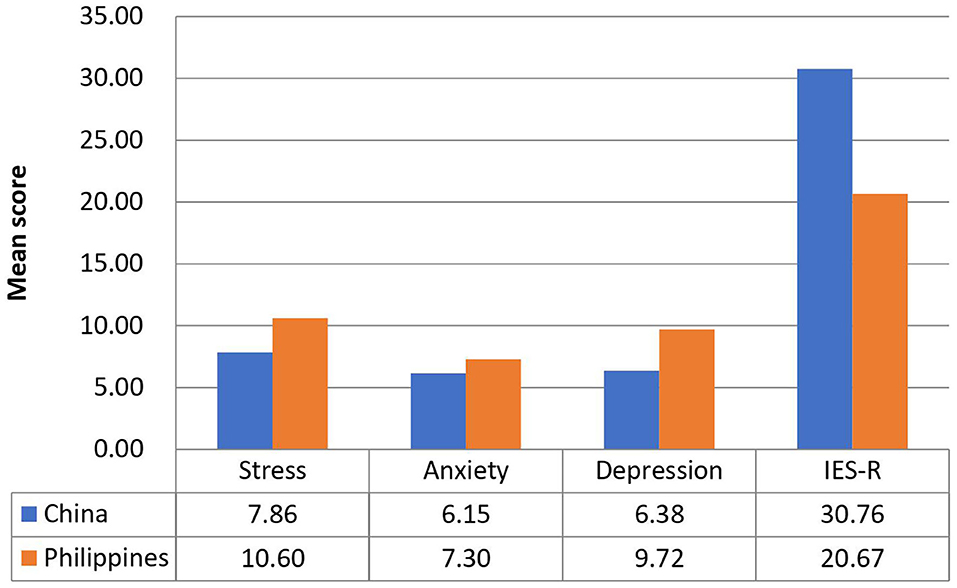
Figure 1 . Comparison of the mean scores of DASS-stress, anxiety and depression subscales, and IES-R scores between Filipino and Chinese respondents.
Physical Symptoms, Health Status, and Its Association With Psychological Impact and Adverse Mental Health Status
There were significant differences between Filipino (LMIC) and Chinese (UMIC) respondents regarding physical symptoms resembling COVID-19 and health status. There was a significantly higher proportion of Filipino respondents who reported headache ( p < 0.001), myalgia ( p < 0.001), cough ( p < 0.001), breathing difficulty ( p < 0.001), dizziness ( p < 0.05), coryza ( p < 0.001), sore throat ( p < 0.001), nausea and vomiting ( p < 0.001), recent consultation with a doctor ( p < 0.01), recent hospitalization ( p < 0.001), chronic illness ( p < 0.001), direct ( p < 0.001), and indirect ( p < 0.001) contact with a confirmed diagnosis of COVID-19 as compared to Chinese (see Supplementary Table 1 ). Significantly more Chinese respondents were under quarantine ( p < 0.001).
Linear regression showed that headache, myalgia, cough, dizziness, coryza as well as poor self-rated physical health were significantly associated with higher IES-R scores, DASS-21 stress, anxiety, and depression subscale scores in both countries after adjustment for confounding factors ( p < 0.05; see Table 3 ). Furthermore, breathing difficulty, sore throat, and gastrointestinal symptoms were significantly associated with higher DASS-21 stress, anxiety and depression subscale scores in both countries ( p < 0.05). Chills were significantly associated with higher DASS-21 stress and depression scores ( p < 0.01) in both countries. Recent quarantine was associated with higher DASS-21 subscale scores in Chinese respondents only ( p < 0.05).
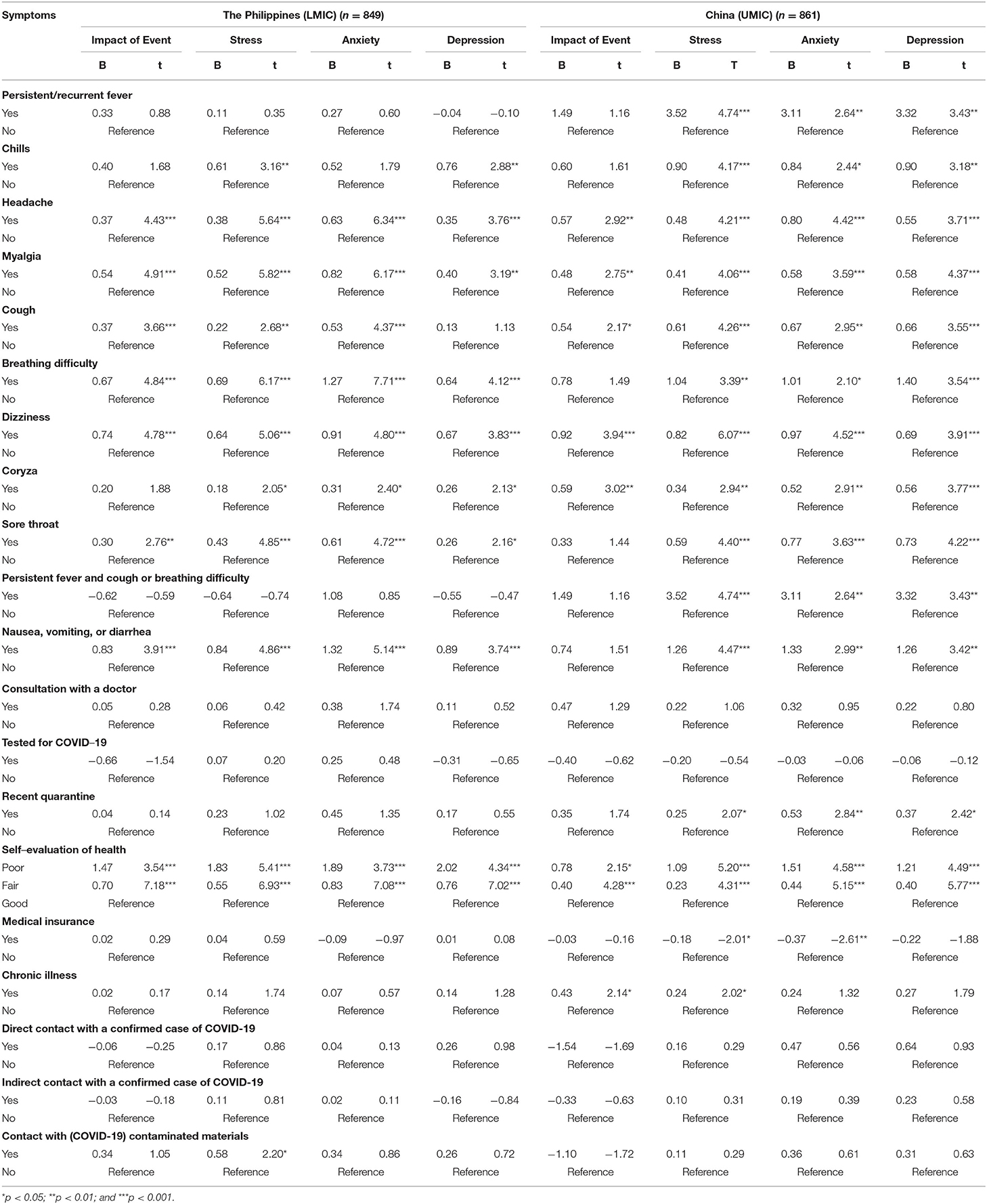
Table 3 . Association between physical health status and contact history and the perceived impact of COVID-19 outbreak as well as adverse mental health status during the epidemic after adjustment for age, gender, and marital status ( n = 1,710).
Perception, Knowledge, and Concerns About COVID-19 and Its Association With Psychological Impact and Adverse Mental Health Status
Filipino (LMIC) and Chinese (UMIC) respondents held significantly different perceptions in terms of knowledge and concerns related to COVID-19 (see Supplementary Table 2 ). For the routes of transmission, there were significantly more Filipino respondents who agreed that droplets transmitted the COVID-19 ( p < 0.001) and contact via contaminated objects ( p < 0.001), but significantly more Chinese agreed with the airborne transmission ( p < 0.001). For the detection and risk of contracting COVID-19, there were significantly more Filipino who were not confident about their doctor's ability to diagnose COVID-19 ( p < 0.001). There were significantly more Filipino respondents who were worried about their family members contracting COVID-19 ( p < 0.001). For health information, there were significantly more Filipino who were unsatisfied with the amount of health information ( p < 0.001) and spent more than three hours per day on the news related to COVID-19 ( p < 0.001). There were significantly more Chinese respondents who felt ostracized by other countries ( p < 0.001).
Linear regression analysis after adjustment of confounding factors showed that the Filipino and Chinese respondents showed different findings (see Table 4 ). Chinese respondents who reported a very low perceived likelihood of contracting COVID-19 were significantly associated with lower DASS depression scores ( p < 0.05). There were similarities between the two countries. Filipino and Chinese respondents who perceived a very high likelihood of survival were significantly associated with lower DASS-21 depression scores ( p < 0.05). Regarding the level of confidence in the doctor's ability to diagnose COVID-19, both Filipino and Chinese respondents who were very confident in their doctors were significantly associated with lower DASS-21 depression scores ( p < 0.01). Filipino and Chinese respondents who were satisfied with health information were significantly associated with lower DASS-21 anxiety and depression scores ( p < 0.01). Chinese and Filipino respondents who were worried about their family members contracting COVID-19 were associated with higher IES-R and DASS-21 subscale scores ( p < 0.05). In contrast, only Filipino respondents who spent <1 h per day monitoring COVID-19 information was significantly associated with lower IES-R and DASS-21 stress and anxiety scores ( p < 0.05). Filipino respondents who felt ostracized were associated with higher IES-R and stress scores ( p < 0.05).
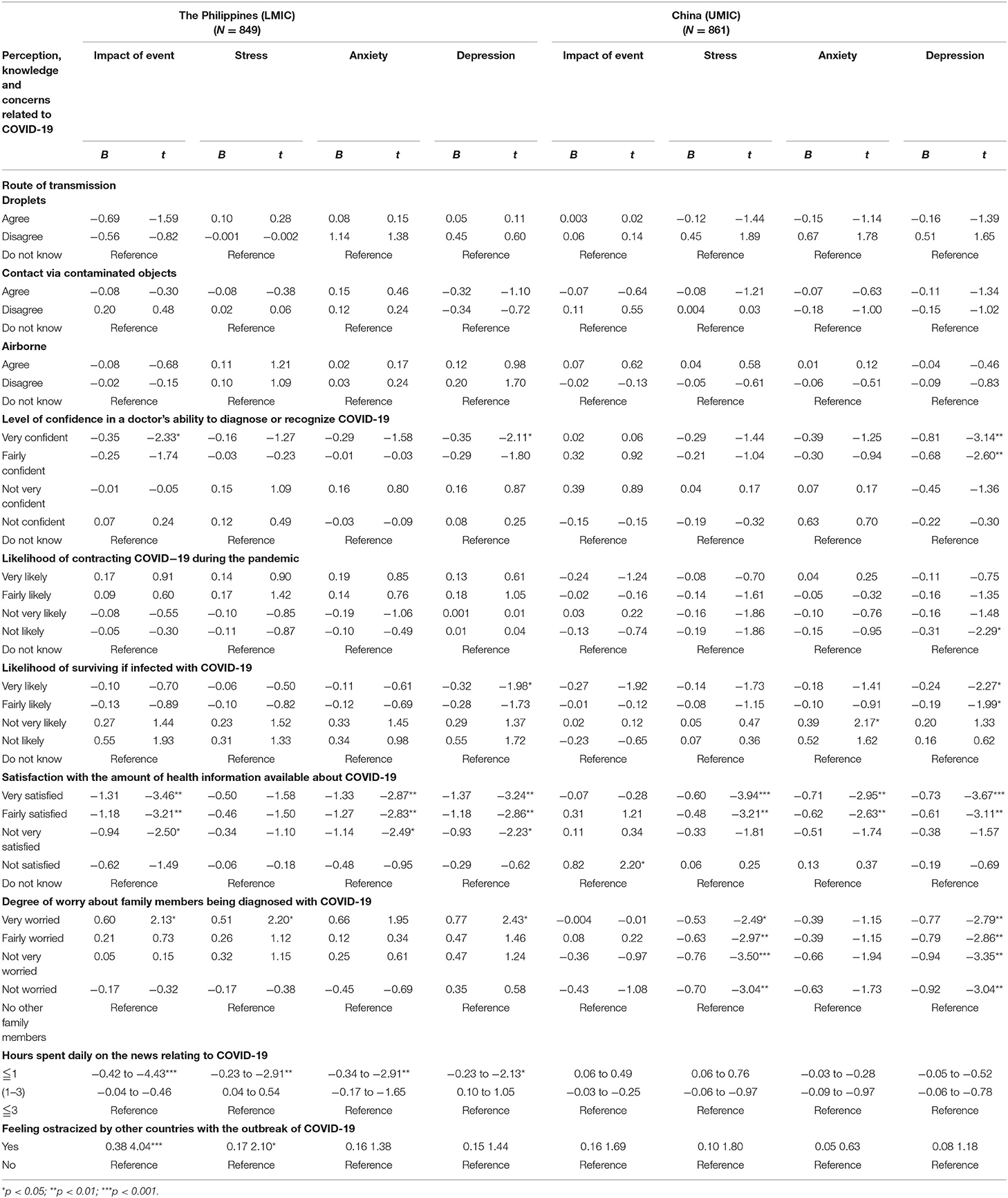
Table 4 . Comparison of association of knowledge and concerns related to COVID-19 with mental health status after adjustment for age, gender, and marital status ( N = 1,710).
Health Information About COVID-19 and Its Association With Psychological Impact and Adverse Mental Health Status
Filipino (LMIC) and Chinese (UMIC) respondents held significantly different views on the information required about COVID-19. There were significantly more Chinese respondents who needed information on the symptoms related to COVID-19, prevention methods, management and treatment methods, regular information updates, more personalized information, the effectiveness of drugs and vaccines, number of infected by geographical locations, travel advice and transmission methods as compared to Filipino ( p < 0.01; See Supplementary Table 3 ). In contrast, there were significantly more Filipino respondents who needed information on other countries' strategies and responses than Chinese ( p < 0.001).
Information on management methods and transmission methods were significantly associated with higher IES-R scores in Chinese respondents ( p < 0.05; see Table 5 ). Travel advice, local transmission data, and other countries' responses were significantly associated with lower DASS-21 stress and depression scores in Chinese respondents only ( p < 0.05). There was only one significant association observed in Filipino respondents; information on transmission methods was significantly associated with lower DASS-21 depression scores ( p < 0.05).
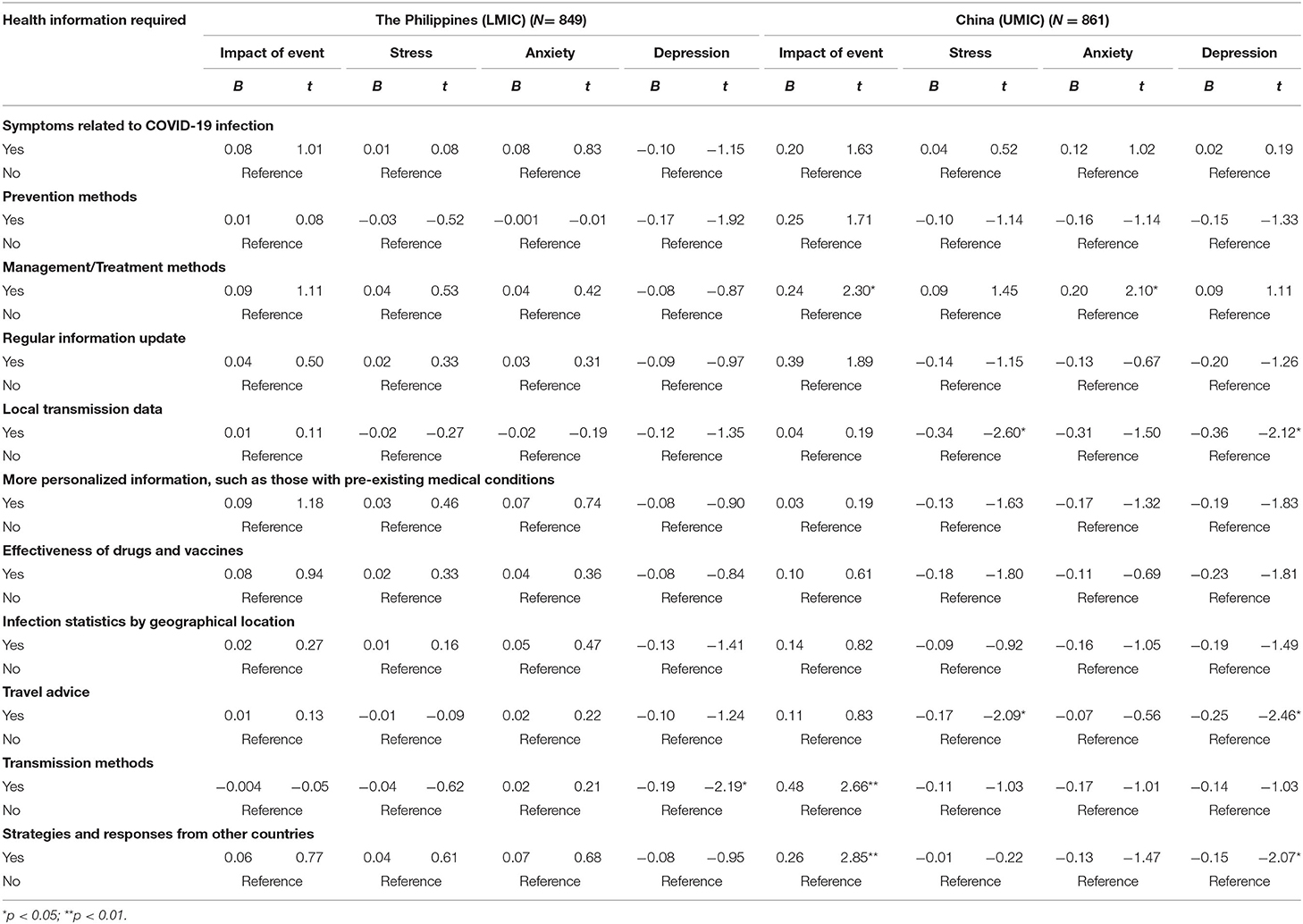
Table 5 . Comparison of the association between information needs about COVID-19 and the psychological impact as well as adverse mental health status between Filipino (LMIC) and Chinese (UMIC) participants after adjustment for age, gender, and marital status ( N = 1,710).
To our best knowledge, this is the first study that compared the physical and mental health as well as knowledge, attitude and belief about COVID-19 between citizens from an LMIC (The Philippines) and UMIC (China). Filipino respondents reported significantly higher levels of depression, anxiety and stress than Chinese during the COVID-19, but only the mean IES-R scores of Chinese respondents were above the cut-off scores for PTSD symptoms. Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection, recent use of medical services with lower confidence, recent direct, and indirect contact with COVID, concerns about family members contracting COVID-19 and dissatisfaction with health information. In contrast, Chinese respondents requested more health information about COVID-19 and were more likely to stay at home for more than 20–24 h per day. For the Filipino, student status, low confidence in doctors, unsatisfaction of health information, long hours spent on health information, worries about family members contracting COVID-19, ostracization, unnecessary worries about COVID-19 were associated with adverse mental health.
The most important implication of the present study is to understand the challenges faced by a sample of people from an LMIC (The Philippines) compared to a sample of people from a UMIC (China) in Asia. As physical symptoms resembling COVID-19 infection (e.g., headache, myalgia, dizziness, and coryza) were associated with adverse mental health in both countries, this association could be due to lack of confidence in healthcare system and lack of testing for coronavirus. Previous research demonstrated that adverse mental health such as depression could affect the immune system and lead to physical symptoms such as malaise and other somatic symptoms ( 39 , 40 ). Based on our findings, the strategic approach to safeguard physical and mental health for middle-income countries would be cost-effective and widely available testing for people present with COVID-19 symptoms, providing a high quality of health information about COVID-19 by health authorities.
Students were afraid that confinement and learning online would hinder their progress in their studies ( 41 ). This may explain why students from the Philippines reported higher levels of IES-R and depression scores. Schools and colleges should evaluate the blended implementation of online and face-to-face learning to optimize educational outcomes when local spread is under control. As a significantly higher proportion of Filipino respondents lack confidence in their doctors, health authorities should ensure adequate training and develop hospital facilities to isolate COVID-19 cases and prevent COVID-19 spread among healthcare workers and patients ( 42 ). Besides, our study found that Filipino respondents were dissatisfied with health information. In contrast, Chinese respondents demanded more health information related to COVID-19. The difference could be due to stronger public health campaign launched by the Chinese government including national health education campaigns, a health QR (Quick Response) code system and community engagement that effectively curtailed the spread of COVID-19 ( 43 ). The high expectation for health information could be explained by high education attainment of participants as about 91.4 and 87.6% of participants from China and the Philippines have a university education.
Furthermore, the governments must employ communication experts to craft information, education, and messaging materials that are target-appropriate to each level of understanding in the community. That the Chinese Government rapidly deployed medical personnel and treated COVID-19 patients at rapidly-built hospitals ( 44 ) is in itself a confidence-building measure. Nevertheless, recent quarantine was associated with higher DASS-21 subscale scores in Chinese respondents only. It could be due to stricter control and monitoring of movements imposed by the Chinese government during the lockdown ( 45 ). Chinese respondents who stayed with more than three family members were associated with higher IES-R scores. The high IES-R scores could be due to worries of the spread of COVID-19 to family members and overcrowded home environment during the lockdown. The Philippines also converted sports arena into quarantine/isolation areas for COVID-19 patients with mild symptoms. These prompt actions helped restore public confidence in the healthcare system ( 46 ). A recent study reported that cultural factors, demand pressure for information, the ease of information dissemination via social networks, marketing incentives, and the poor legal regulation of online contents are the main reasons for misinformation dissemination during the COVID-19 pandemic ( 47 ). Bastani and Bahrami ( 47 ) recommended the engagement of health professionals and authorities on social media during the pandemic and the improvement of public health literacy to counteract misinformation.
Chinese respondents were more likely to feel ostracized and Filipino respondents associated ostracization with adverse mental health. Recently, the editor-in-chief of The Lancet , Richard Horton, expressed concern of discrimination of a country or particular ethnic group, saying that while it is important to understand the origin and inter-species transmission of the coronavirus, it was both unhelpful and unscientific to point to a country as the origin of the Covid-19 pandemic, as such accusation could be highly stigmatizing and discriminatory ( 48 ). The global co-operation involves an exchange of expertise, adopting effective prevention strategies, sharing resources, and technologies among UMIC and LIMC to form a united front on tackling the COVID-19 pandemic remains a work in progress.
Strengths and Limitations
The main strength of this study lay in the fact that we performed in-depth analysis and studied the relationship between physical and mental outcomes and other variables related to COVID-19 in the Philippines and China. However, there are several limitations to be considered when interpreting the results. Although the Philippines is a LMIC and China is a UMIC, the findings cannot be generalized to other LIMCs and UMICs. Another limitation was the potential risk of sampling bias. This bias could be due to the online administration of questionnaires, and the majority of respondents from both countries were respondents with good educational attainment and internet access. We could not reach out to potential respondents without internet access (e.g., those who stayed in the countryside or remote areas). Further, our findings may not be generalizable to other middle-income countries.
During the COVID-19 pandemic, Filipinos (LMIC) respondents reported significantly higher levels of depression, anxiety and stress than Chinese (UMIC). Filipino respondents were more likely to report physical symptoms resembling COVID-19 infection, recent use of medical services with lower confidence, recent direct and indirect contact with COVID, concerns about family members contracting COVID-19 and dissatisfaction with health information than Chinese. For the current COVID-19 and future pandemic, Middle income countries need to adopt the strategic approach to safeguard physical and mental health by establishing cost-effective and widely available testing for people who present with COVID-19 symptoms; provision of high quality and accurate health information about COVID-19 by health authorities. Our findings urge middle income countries to prevent ostracization of a particular ethnic group, learn from each other, and unite to address the challenge of the COVID-19 pandemic and safeguard physical and mental health.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
Ethical review and approval was required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. The Institutional Review Board of the University of Philippines Manila Research Ethics Board (UPMREB 2020- 198-01) and Huaibei Normal University (China) approved the research proposal (HBU-IRB-2020-002).
Author Contributions
Concept and design: CW, MT, CT, RP, VK, and RH. Acquisition, analysis, and interpretation of data: CW, MT, CT, RP, LX, CHa, XW, YT, and VK. Drafting of the manuscript: CW, MT, CT, RH, and JA. Critical revision of the manuscript: MT, CT, CHo, and JA. Statistical analysis: CW, PR, RP, LX, XW, and YT. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.568929/full#supplementary-material
1. Sohrabi C, Alsafi Z, O'Neill N, Khan M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. (2020) 76:71–6. doi: 10.1016/j.ijsu.2020.02.034
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Mahase E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ. (2020) 368:m1036. doi: 10.1136/bmj.m1036
3. Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J. Pediatr. (2020) 87:281–6. doi: 10.1007/s12098-020-03263-6
CrossRef Full Text | Google Scholar
4. Oxford. Oxford U of. Coronavirus Disease (COVID-19) - Statistics and Research . (2020). Available online at: https://ourworldindata.org/coronavirus%0D (accessed May 17, 2020).
Google Scholar
5. Edrada EM, Lopez EB, Villarama JB, Salva Villarama EP, Dagoc BF, Smith C, et al. First COVID-19 infections in the Philippines: a case report. Trop Med Health. (2020) 48:21. doi: 10.1186/s41182-020-00218-7
6. CNN. TIMELINE: How the Philippines is Handling COVID-19. (2020). Available online at: https://cnnphilippines.com/news/2020/4/21/interactive-timeline-PH-handling-COVID-19.html (accessed May 17, 2020).
7. Worldmeters. COVID-19 Coronavirus Pandemic. (2020). Available online at: https://www.worldometers.info/coronavirus/ (accessed December 4 2020).
8. WorldBank. World Bank National Accounts Data, and OECD National Accounts Data Files . (2020). Available online at: https://data.worldbank.org/indicator/NY.GNP.PCAP.CD (accessed April 16 2020).
9. Schellekens P, Sourrouille D. The Unreal Dichotomy in COVID-19 Mortality between High-Income and Developing Countries. (2020). Available online at: https://www.brookings.edu/blog/future-development/2020/05/05/the-unreal-dichotomy-in-covid-19-mortality-between-high-income-and-developing-countries/ (accessed May 10 2020).
10. Medicalexpress. ‘Slow Response’: How Britain Became Worst-Hit in Europe by Virus. (2020). Available online at: https://medicalxpress.com/news/2020-05-response-britain-worst-hit-europe-virus.html (accessed May 8 2020).
11. Mamun MA, Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? - The forthcoming economic challenges for a developing country. Brain Behav Immun. (2020) 87:163–6. doi: 10.1016/j.bbi.2020.05.028
12. Kar SK, Oyetunji TP, Prakash AJ, Ogunmola OA, Tripathy S, Lawal MM, et al. Mental health research in the lower-middle-income countries of Africa and Asia during the COVID-19 pandemic: a scoping review. Neurol Psychiatry Brain Res. (2020) 38:54–64. doi: 10.1016/j.npbr.2020.10.003
13. Leung GM, Lam TH, Ho LM, Ho SY, Chan BH, Wong IO, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. (2003) 57:857–63. doi: 10.1136/jech.57.11.857
14. Cristóbal-Narváez P, Haro JM, Koyanagi A. Perceived stress and depression in 45 low- and middle-income countries. J Affect Disord. (2020) 274:799–805. doi: 10.1016/j.jad.2020.04.020
15. Vallejo MA, Vallejo-Slocker L, Fernández-Abascal EG, Mañanes G. Determining factors for stress perception assessed with the perceived stress scale (PSS-4) in Spanish and other European samples. Front Psychol. (2018) 9:37. doi: 10.3389/fpsyg.2018.00037
16. Shin C, Kim Y, Park S, Yoon S, Ko YH, Kim YK, et al. Prevalence and associated factors of depression in general population of Korea: results from the Korea National Health and Nutrition Examination Survey, 2014. J Korean Med Sci. (2017) 32:1861–9. doi: 10.3346/jkms.2017.32.11.1861
17. Olsen LR, Mortensen EL, Bech P. Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand. (2004) 109:96–103. doi: 10.1046/j.0001-690X.2003.00231.x
18. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and (2014). Sci Rep. (2018) 8:2861. doi: 10.1038/s41598-018-21243-x
19. Sang T, Zhou H, Li M, Li W, Shi H, Chen H, et al. Investigation of the differences between the medical personnel's and general population's view on the doctor-patient relationship in China by a cross-sectional survey. Global Health. (2020) 16:99. doi: 10.21203/rs.3.rs-41725/v2
20. Ferrer RR, Ramirez M, Beckman LJ, Danao LL, Ashing-Giwa KT. The impact of cultural characteristics on colorectal cancer screening adherence among Filipinos in the United States: a pilot study. Psychooncology. (2011) 20:862–70. doi: 10.1002/pon.1793
21. Lei P, Jolibert A. A three-model comparison of the relationship between quality, satisfaction and loyalty: an empirical study of the Chinese healthcare system. BMC Health Serv Res. (2012) 12:436. doi: 10.1186/1472-6963-12-436
22. Peabody JW, Florentino J, Shimkhada R, Solon O, Quimbo S. Quality variation and its impact on costs and satisfaction: evidence from the QIDS study. Med Care. (2010) 48:25–30. doi: 10.1097/MLR.0b013e3181bd47b2
23. Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
24. Wang C, Pan R, Wan X, Tan Y, Xu L, McIntyre RS, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. (2020) 87:40–8. doi: 10.1016/j.bbi.2020.04.028
25. Zhang MW, Ho CS, Fang P, Lu Y, Ho RC. Usage of social media and smartphone application in assessment of physical and psychological well-being of individuals in times of a major air pollution crisis. JMIR Mhealth Uhealth. (2014) 2:e16. doi: 10.2196/mhealth.2827
26. Chew NWS, Lee GKH, Tan BYQ, Jing M, Goh Y, Ngiam NJH, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
27. Zhang MWB, Ho CSH, Fang P, Lu Y, Ho RCM. Methodology of developing a smartphone application for crisis research and its clinical application. Technol Health Care. (2014) 22:547–59. doi: 10.3233/THC-140819
28. Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. (2003) 41:1489–96. doi: 10.1016/j.brat.2003.07.010
29. Lee SM, Kang WS, Cho A-R, Kim T, Park JK. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–7. doi: 10.1016/j.comppsych.2018.10.003
30. Le TA, Le MQT, Dang AD, Dang AK, Nguyen CT, Pham HQ, et al. Multi-level predictors of psychological problems among methadone maintenance treatment patients in difference types of settings in Vietnam. Subst Abuse Treat Prev Policy. (2019) 14:39. doi: 10.1186/s13011-019-0223-4
31. Cheung JTK, Tsoi VWY, Wong KHK, Chung RY. Abuse and depression among Filipino foreign domestic helpers. A cross-sectional survey in Hong Kong. Public Health. (2019) 166:121–7. doi: 10.1016/j.puhe.2018.09.020
32. Tee ML, Tee CA, Anlacan JP, Aligam KJG, Reyes PWC, Kuruchittham V, et al. Psychological impact of COVID-19 pandemic in the Philippines. J Affect Disord. (2020) 277:379–91. doi: 10.1016/j.jad.2020.08.043
33. Tee CA, Salido EO, Reyes PWC, Ho RC, Tee ML. Psychological State and Associated Factors During the 2019 Coronavirus Disease (COVID-19) pandemic among filipinos with rheumatoid arthritis or systemic lupus erythematosus. Open Access Rheumatol. (2020) 12:215–22. doi: 10.2147/OARRR.S269889
34. Ho CSH, Tan ELY, Ho RCM, Chiu MYL. Relationship of anxiety and depression with respiratory symptoms: comparison between depressed and non-depressed smokers in Singapore. Int J Environ Res Public Health. (2019) 16:163. doi: 10.3390/ijerph16010163
35. Quek TC, Ho CS, Choo CC, Nguyen LH, Tran BX, Ho RC. Misophonia in Singaporean psychiatric patients: a cross-sectional study. Int J Environ Res Public Health. (2018) 15:1410. doi: 10.3390/ijerph15071410
36. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. (2020) 87:100–6. doi: 10.1016/j.bbi.2020.04.069
37. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:E1729. doi: 10.3390/ijerph17051729
38. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med . (2020) 173:317–20. doi: 10.7326/M20-1083
39. Liu Y, Ho RC, Mak A. Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord. (2012) 139:230–9. doi: 10.1016/j.jad.2011.08.003
40. Viljoen M, Panzer A. Proinflammatory cytokines: a common denominator in depression and somatic symptoms? Can J Psychiatry. (2005) 50:128. doi: 10.1177/070674370505000216
41. Li HY, Cao H, Leung DYP, Mak YW. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int J Environ Res Public Health. (2020) 17:3933. doi: 10.3390/ijerph17113933
42. Krishnakumar B, Rana S. COVID 19 in INDIA: strategies to combat from combination threat of life and livelihood. J Microbiol Immunol Infect. (2020) 53:389–91. doi: 10.1016/j.jmii.2020.03.024
43. Huang Y, Wu Q, Wang P, Xu Y, Wang L, Zhao Y, et al. Measures undertaken in China to avoid COVID-19 infection: internet-based, cross-sectional survey study. J Med Internet Res. (2020) 22:e18718. doi: 10.2196/18718
44. Salo J. China Orders 1,400 Military Doctors, Nurses to Treat Coronavirus. (2020). Available online at: https://nypost.com/2020/02/02/china-orders-14000-military-doctors-nurses-to-treat-coronavirus/ (accessed March 22, 2020).
45. Burki T. China's successful control of COVID-19. Lancet Infect Dis. (2020) 20:1240–1. doi: 10.1016/S1473-3099(20)30800-8
46. Esguerra DJ. Philippine Arena to Start Accepting COVID-19 Patients Next Week . (2020). Available online at: https://newsinfo.inquirer.net/1255623/philippine-arena-to-start-accepting-covid-19-patients-next-week (accessed November 18, 2020).
47. Bastani P, Bahrami MA. COVID-19 related misinformation on social media: a qualitative study from Iran. J Med Internet Res. (2020). doi: 10.2196/preprints.18932. [Epub ahead of print].
48. Catherine W. It's Unfair to Blame China for Coronavirus Pandemic, Lancet Editor Tells State Media. (2020). Available online at: https://www.scmp.com/news/china/science/article/3082606/its-unfair-blame-china-coronavirus-pandemic-lancet-editor-tells (accessed May 8, 2020).
Keywords: anxiety, China, COVID-19, depression, middle-income, knowledge, precaution, Philippines
Citation: Tee M, Wang C, Tee C, Pan R, Reyes PW, Wan X, Anlacan J, Tan Y, Xu L, Harijanto C, Kuruchittham V, Ho C and Ho R (2021) Impact of the COVID-19 Pandemic on Physical and Mental Health in Lower and Upper Middle-Income Asian Countries: A Comparison Between the Philippines and China. Front. Psychiatry 11:568929. doi: 10.3389/fpsyt.2020.568929
Received: 02 June 2020; Accepted: 22 December 2020; Published: 09 February 2021.
Reviewed by:
Copyright © 2021 Tee, Wang, Tee, Pan, Reyes, Wan, Anlacan, Tan, Xu, Harijanto, Kuruchittham, Ho and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cuiyan Wang, wcy@chnu.edu.cn
† These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- DOI: 10.5195/ijms.2021.849
- Corpus ID: 237250502
Folk Medicine in the Philippines: A Phenomenological Study of Health-Seeking Individuals
- Nadine Angela Rondilla , I. C. Rocha , +6 authors Carina Viktoria Javier
- Published 2021
- Medicine, Sociology
Figures and Tables from this paper

24 Citations
Beliefs, perceptions, and tendencies of patients with diabetes towards folk-healing alternatives: a qualitative analysis, empowering communities : reviving traditional medicine for sustainable health and poverty reduction, the infusion of folk catholicism to tambal binisaya as an indigenous healing system in iligan city, from beliefs to practices: the lived experiences of filipino nurses utilizing traditional filipino health remedies at home, a phenomenology, indigenous communities in colombia: a cultural and holistic view of cancer management, lived experiences of palestinian patients with covid-19: a multi-center descriptive phenomenological study of recovery journey, ethnomedicinal documentation of polyherbal formulations and other folk medicines in aurora, zamboanga del sur, philippines, willingness to participate in entheogen use research in naturalistic settings, access to health services among low-income women in the philippines: a review, sanggar, pelimbonen, kaphaygo sa ragat: traversing the pre-islamic beliefs and traditions of the meranaws in the philippines, 38 references, albularyo folk healing: cultural beliefs on healthcare management in partido district, camarines sur, philippines, unveiling cebuano traditional healing practices, medical anthropology: a review, folk medicine in the filipino american experience, medical pluralism, traditional healing practices, and the partido albularyo: challenge in inclusion, the field of medical anthropology in social science & medicine., lay reflections of health experiences and sinhalese medicine in sri lanka, traditional medicine: past, present and future research and development prospects and integration in the national health system of cameroon., prevalence, and health- and sociodemographic associations for visits to traditional and complementary medical providers in the seventh survey of the tromsø study, traditional and folk medicine as a target for drug discovery, related papers.
Showing 1 through 3 of 0 Related Papers
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
August 13, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Quantitative ultrasound parameters offer new tool for diagnosing lung disease
by Matt Shipman, North Carolina State University
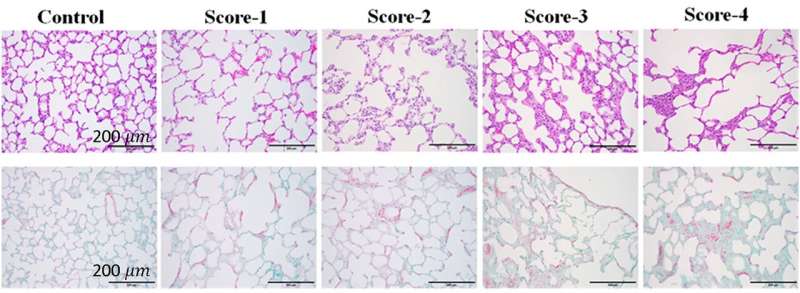
Researchers have established a suite of parameters that can be determined using ultrasound to quantitatively measure different physical characteristics of the lung. The researchers also demonstrated that the parameters can be used to accurately diagnose and assess the severity of lung diseases in an animal model.
The paper, " Lung quantitative ultrasound to stage and monitor interstitial lung diseases ," is published open access in the journal Scientific Reports .
"Diseases can affect lungs in many different ways," says Marie Muller, co-senior author of a paper on the work and an associate professor of mechanical and aerospace engineering at North Carolina State University. "They can change the microstructure of the lung, the elasticity of the lung tissue, the type and amount of fluid in the lungs, and so on. Each of these changes can be measured using ultrasound. Our goal with this work was to establish clear parameters for these lung characteristics and determine which combination of parameters is associated with different lung diseases."
"To be clear, we're talking about numeric measurements for each parameter," says Muller, who is also on faculty in the Joint Biomedical Engineering Department at NC State and the University of North Carolina at Chapel Hill.
"So, if there are three parameters associated with a disease, we'd have three numbers—one for each parameter. We can then use a mathematical formula that combines those three numbers to create a biomarker score. That score not only tells us whether a specific health problem is present, but how severe the problem is."
The researchers began by generating parameters for measuring a wide variety of lung characteristics, such as the density of alveoli or the amount of fluid in the lungs. The researchers also adapted existing ultrasound parameters used in other organs for use on lung tissue. Altogether, this resulted in a total of 60 parameters.
The researchers then measured all 60 parameters in the lungs of rats that were healthy or had various stages of fibrosis or edema. Fibrosis is scarring of the lung tissue. Edema refers to fluid build-up in the lung.
"We then used statistical methods to identify which combinations of parameters were both associated with a given health condition and sensitive enough to measure the severity of a health problem," Muller says.
Through this process, the researchers found that only five of the parameters were necessary for assessing fibrosis and edema: three for fibrosis and two for edema.
"One of the challenges with many diagnostic tools is that there is often a trade-off between sensitivity and specificity," Muller says. "A highly sensitive test may virtually guarantee that you detect a problem, but it also usually means that there can be a lot of false positives. On the other hand, a highly specific test will almost never give you a false positive, but it may also miss quite a few health problems it is supposed to detect, or not be able to assess the severity of a specific disease."
"We're excited about this new diagnostic tool because it is both highly sensitive and highly specific," Muller says. "And we're able to have that combination of specificity and sensitivity because we are measuring multiple parameters."
One way they were able to assess the sensitivity of the new tool is by making use of fibrosis treatments. As rats who had fibrosis received treatment, the new diagnostic tool was able to measure improvements in the rats' lung tissue.
The researchers have developed data processing software that can be used in conjunction with existing ultrasound hardware to determine the numbers for each parameter measurement, as well as establishing the biomarker scores for edema and fibrosis.
"We've established that this works well in a rat model," Muller says. "Next steps involve computational simulations, in vitro testing, and animal model testing to establish that this technique can work in cases where the ultrasound has to penetrate a much thicker chest wall. If that goes well, we'll pursue clinical trials.
"Also, because we have established 60 parameters—which is a lot—we're optimistic that this technique can be used in the future to identify diagnostic biomarkers for a range of other lung conditions."
Explore further
Feedback to editors

Researchers develop new chemical method to enhance drug discovery
2 hours ago

Rare diseases point to connections between metabolism and immunity
3 hours ago

Researchers discover novel nanoparticles in blood with potential to transform cancer diagnosis

Research shows how to reduce inappropriate IV use by more than a third
12 hours ago

Now that mpox is a global health emergency, will it trigger another pandemic?
16 hours ago

Knocking out one key gene leads to autistic traits, mouse study shows

Study: Rare cancer patients nearly three times more likely to develop anxiety and depression than common cancer patients
17 hours ago

Intervention for cleaning shared health care equipment could significantly reduce health care–associated infections

Lip reading activates brain regions similar to real speech, researchers show

Parents' excessive smartphone use could harm children's mental health
Related stories.

Ultrasound technique offers more precise, quantified assessments of lung health
Oct 15, 2020

Study says FAPI PET/CT bests FDG in predicting progressive lung disease
Jun 10, 2024

New study probes macrophages' role in developing pulmonary fibrosis
Apr 12, 2024

Hypersensitivity pneumonitis: Is your feather bedding making you sick?
Aug 21, 2023

Study identifies therapeutic target for high blood pressure in the lungs
Oct 1, 2019

Healthy omega-3 fats may slow deadly pulmonary fibrosis, research suggests
Jan 2, 2024
Recommended for you

Can a mouthwash-based test help predict head and neck cancer recurrence?
Aug 15, 2024

Hydrogel device enables painless transdermal delivery of nucleic acids for cancer immunotherapy

New way to extend 'shelf life' of blood stem cells can improve gene therapy

3D body scanner with AI predicts metabolic syndrome risk

New brain-computer interface allows man with ALS to 'speak' again
Aug 14, 2024

Scientists discover method to activate dormant stem cells in the brain
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
- Environment
- Science & Technology
- Business & Industry
- Health & Public Welfare
- Topics (CFR Indexing Terms)
- Public Inspection
- Presidential Documents
- Document Search
- Advanced Document Search
- Public Inspection Search
- Reader Aids Home
- Office of the Federal Register Announcements
- Using FederalRegister.Gov
- Understanding the Federal Register
- Recent Site Updates
- Federal Register & CFR Statistics
- Videos & Tutorials
- Developer Resources
- Government Policy and OFR Procedures
- Congressional Review
- My Clipboard
- My Comments
- My Subscriptions
- Sign In / Sign Up
- Site Feedback
- Search the Federal Register
This site displays a prototype of a “Web 2.0” version of the daily Federal Register. It is not an official legal edition of the Federal Register, and does not replace the official print version or the official electronic version on GPO’s govinfo.gov.
The documents posted on this site are XML renditions of published Federal Register documents. Each document posted on the site includes a link to the corresponding official PDF file on govinfo.gov. This prototype edition of the daily Federal Register on FederalRegister.gov will remain an unofficial informational resource until the Administrative Committee of the Federal Register (ACFR) issues a regulation granting it official legal status. For complete information about, and access to, our official publications and services, go to About the Federal Register on NARA's archives.gov.
The OFR/GPO partnership is committed to presenting accurate and reliable regulatory information on FederalRegister.gov with the objective of establishing the XML-based Federal Register as an ACFR-sanctioned publication in the future. While every effort has been made to ensure that the material on FederalRegister.gov is accurately displayed, consistent with the official SGML-based PDF version on govinfo.gov, those relying on it for legal research should verify their results against an official edition of the Federal Register. Until the ACFR grants it official status, the XML rendition of the daily Federal Register on FederalRegister.gov does not provide legal notice to the public or judicial notice to the courts.
Design Updates: As part of our ongoing effort to make FederalRegister.gov more accessible and easier to use we've enlarged the space available to the document content and moved all document related data into the utility bar on the left of the document. Read more in our feature announcement .
Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods; Draft Guidance for Industry (Edition 2); Availability
A Notice by the Food and Drug Administration on 08/16/2024
This document has a comment period that ends in 89 days. (11/14/2024) Submit a formal comment
Thank you for taking the time to create a comment. Your input is important.
Once you have filled in the required fields below you can preview and/or submit your comment to the Health and Human Services Department for review. All comments are considered public and will be posted online once the Health and Human Services Department has reviewed them.
You can view alternative ways to comment or you may also comment via Regulations.gov at /documents/2024/08/16/2024-18261/voluntary-sodium-reduction-goals-target-mean-and-upper-bound-concentrations-for-sodium-in .
- What is your comment about?
Note: You can attach your comment as a file and/or attach supporting documents to your comment. Attachment Requirements .
this will NOT be posted on regulations.gov
- Opt to receive email confirmation of submission and tracking number?
- Tell us about yourself! I am... *
- First Name *
- Last Name *
- State Alabama Alaska American Samoa Arizona Arkansas California Colorado Connecticut Delaware District of Columbia Florida Georgia Guam Hawaii Idaho Illinois Indiana Iowa Kansas Kentucky Louisiana Maine Maryland Massachusetts Michigan Minnesota Mississippi Missouri Montana Nebraska Nevada New Hampshire New Jersey New Mexico New York North Carolina North Dakota Ohio Oklahoma Oregon Pennsylvania Puerto Rico Rhode Island South Carolina South Dakota Tennessee Texas Utah Vermont Virgin Islands Virginia Washington West Virginia Wisconsin Wyoming
- Country Afghanistan Åland Islands Albania Algeria American Samoa Andorra Angola Anguilla Antarctica Antigua and Barbuda Argentina Armenia Aruba Australia Austria Azerbaijan Bahamas Bahrain Bangladesh Barbados Belarus Belgium Belize Benin Bermuda Bhutan Bolivia, Plurinational State of Bonaire, Sint Eustatius and Saba Bosnia and Herzegovina Botswana Bouvet Island Brazil British Indian Ocean Territory Brunei Darussalam Bulgaria Burkina Faso Burundi Cambodia Cameroon Canada Cape Verde Cayman Islands Central African Republic Chad Chile China Christmas Island Cocos (Keeling) Islands Colombia Comoros Congo Congo, the Democratic Republic of the Cook Islands Costa Rica Côte d'Ivoire Croatia Cuba Curaçao Cyprus Czech Republic Denmark Djibouti Dominica Dominican Republic Ecuador Egypt El Salvador Equatorial Guinea Eritrea Estonia Ethiopia Falkland Islands (Malvinas) Faroe Islands Fiji Finland France French Guiana French Polynesia French Southern Territories Gabon Gambia Georgia Germany Ghana Gibraltar Greece Greenland Grenada Guadeloupe Guam Guatemala Guernsey Guinea Guinea-Bissau Guyana Haiti Heard Island and McDonald Islands Holy See (Vatican City State) Honduras Hong Kong Hungary Iceland India Indonesia Iran, Islamic Republic of Iraq Ireland Isle of Man Israel Italy Jamaica Japan Jersey Jordan Kazakhstan Kenya Kiribati Korea, Democratic People's Republic of Korea, Republic of Kuwait Kyrgyzstan Lao People's Democratic Republic Latvia Lebanon Lesotho Liberia Libya Liechtenstein Lithuania Luxembourg Macao Macedonia, the Former Yugoslav Republic of Madagascar Malawi Malaysia Maldives Mali Malta Marshall Islands Martinique Mauritania Mauritius Mayotte Mexico Micronesia, Federated States of Moldova, Republic of Monaco Mongolia Montenegro Montserrat Morocco Mozambique Myanmar Namibia Nauru Nepal Netherlands New Caledonia New Zealand Nicaragua Niger Nigeria Niue Norfolk Island Northern Mariana Islands Norway Oman Pakistan Palau Palestine, State of Panama Papua New Guinea Paraguay Peru Philippines Pitcairn Poland Portugal Puerto Rico Qatar Réunion Romania Russian Federation Rwanda Saint Barthélemy Saint Helena, Ascension and Tristan da Cunha Saint Kitts and Nevis Saint Lucia Saint Martin (French part) Saint Pierre and Miquelon Saint Vincent and the Grenadines Samoa San Marino Sao Tome and Principe Saudi Arabia Senegal Serbia Seychelles Sierra Leone Singapore Sint Maarten (Dutch part) Slovakia Slovenia Solomon Islands Somalia South Africa South Georgia and the South Sandwich Islands South Sudan Spain Sri Lanka Sudan Suriname Svalbard and Jan Mayen Swaziland Sweden Switzerland Syrian Arab Republic Taiwan, Province of China Tajikistan Tanzania, United Republic of Thailand Timor-Leste Togo Tokelau Tonga Trinidad and Tobago Tunisia Turkey Turkmenistan Turks and Caicos Islands Tuvalu Uganda Ukraine United Arab Emirates United Kingdom United States United States Minor Outlying Islands Uruguay Uzbekistan Vanuatu Venezuela, Bolivarian Republic of Viet Nam Virgin Islands, British Virgin Islands, U.S. Wallis and Futuna Western Sahara Yemen Zambia Zimbabwe
- Organization Type * Company Organization Federal State Local Tribal Regional Foreign U.S. House of Representatives U.S. Senate
- Organization Name *
- You are filing a document into an official docket. Any personal information included in your comment text and/or uploaded attachment(s) may be publicly viewable on the web.
- I read and understand the statement above.
- Preview Comment
This document has been published in the Federal Register . Use the PDF linked in the document sidebar for the official electronic format.
- Document Details Published Content - Document Details Agencies Department of Health and Human Services Food and Drug Administration Agency/Docket Number Docket No. FDA-2014-D-0055 Document Citation 89 FR 66727 Document Number 2024-18261 Document Type Notice Pages 66727-66729 (3 pages) Publication Date 08/16/2024 Published Content - Document Details
- View printed version (PDF)
- Document Dates Published Content - Document Dates Comments Close 11/14/2024 Dates Text Submit either electronic or written comments on the draft guidance by November 14, 2024 to ensure that we consider your comment on the draft guidance before we begin work on the final version of the guidance. Published Content - Document Dates
This table of contents is a navigational tool, processed from the headings within the legal text of Federal Register documents. This repetition of headings to form internal navigation links has no substantive legal effect.
Electronic Submissions
Written/paper submissions, for further information contact:, supplementary information:, i. background, ii. paperwork reduction act of 1995, iii. electronic access, iv. references.
Comments are being accepted - Submit a public comment on this document .
FederalRegister.gov retrieves relevant information about this document from Regulations.gov to provide users with additional context. This information is not part of the official Federal Register document.
Voluntary Sodium Reduction Goals: Target Mean and Recommended Maximum Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods
- Sharing Enhanced Content - Sharing Shorter Document URL https://www.federalregister.gov/d/2024-18261 Email Email this document to a friend Enhanced Content - Sharing
- Print this document
Document page views are updated periodically throughout the day and are cumulative counts for this document. Counts are subject to sampling, reprocessing and revision (up or down) throughout the day.
This document is also available in the following formats:
More information and documentation can be found in our developer tools pages .
This PDF is the current document as it appeared on Public Inspection on 08/15/2024 at 8:45 am.
It was viewed 3 times while on Public Inspection.
If you are using public inspection listings for legal research, you should verify the contents of the documents against a final, official edition of the Federal Register. Only official editions of the Federal Register provide legal notice of publication to the public and judicial notice to the courts under 44 U.S.C. 1503 & 1507 . Learn more here .
Document headings vary by document type but may contain the following:
- the agency or agencies that issued and signed a document
- the number of the CFR title and the number of each part the document amends, proposes to amend, or is directly related to
- the agency docket number / agency internal file number
- the RIN which identifies each regulatory action listed in the Unified Agenda of Federal Regulatory and Deregulatory Actions
See the Document Drafting Handbook for more details.
Department of Health and Human Services
Food and drug administration.
- [Docket No. FDA-2014-D-0055]
Food and Drug Administration, HHS.
Notice of availability.
The Food and Drug Administration (FDA or we) is announcing the availability of a draft guidance for industry entitled “Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods (Edition 2).” The draft guidance, when finalized, will describe our views on the next voluntary goals (Phase II (3-year)) for sodium reduction in a variety of identified categories of foods that are commercially processed, packaged, or prepared. These goals are intended to address the excessive intake of sodium in the current population to help reduce the burden of diet-related chronic disease, promote improvements in public health, and advance health equity by supporting a healthier food supply.
Submit either electronic or written comments on the draft guidance by November 14, 2024 to ensure that we consider your comment on the draft ( print page 66728) guidance before we begin work on the final version of the guidance.
You may submit comments on any guidance at any time as follows:
Submit electronic comments in the following way:
- Federal eRulemaking Portal: https://www.regulations.gov . Follow the instructions for submitting comments. Comments submitted electronically, including attachments, to https://www.regulations.gov will be posted to the docket unchanged. Because your comment will be made public, you are solely responsible for ensuring that your comment does not include any confidential information that you or a third party may not wish to be posted, such as medical information, your or anyone else's Social Security number, or confidential business information, such as a manufacturing process. Please note that if you include your name, contact information, or other information that identifies you in the body of your comments, that information will be posted on https://www.regulations.gov .
- If you want to submit a comment with confidential information that you do not wish to be made available to the public, submit the comment as a written/paper submission and in the manner detailed (see “Written/Paper Submissions” and “Instructions”).
Submit written/paper submissions as follows:
- Mail/Hand delivery/Courier (for written/paper submissions): Dockets Management Staff (HFA-305), Food and Drug Administration, 5630 Fishers Lane, Rm. 1061, Rockville, MD 20852.
- For written/paper comments submitted to the Dockets Management Staff, FDA will post your comment, as well as any attachments, except for information submitted, marked and identified, as confidential, if submitted as detailed in “Instructions.”
Instructions: All submissions received must include the Docket No. FDA-2014-D-0055 for “Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods (Edition 2).” Received comments will be placed in the docket and, except for those submitted as “Confidential Submissions,” publicly viewable at https://www.regulations.gov or at the Dockets Management Staff between 9 a.m. and 4 p.m., Monday through Friday, 240-402-7500.
- Confidential Submissions—To submit a comment with confidential information that you do not wish to be made publicly available, submit your comments only as a written/paper submission. You should submit two copies total. One copy will include the information you claim to be confidential with a heading or cover note that states “THIS DOCUMENT CONTAINS CONFIDENTIAL INFORMATION.” We will review this copy, including the claimed confidential information, in our consideration of comments. The second copy, which will have the claimed confidential information redacted/blacked out, will be available for public viewing and posted on https://www.regulations.gov . Submit both copies to the Dockets Management Staff. If you do not wish your name and contact information to be made publicly available, you can provide this information on the cover sheet and not in the body of your comments and you must identify this information as “confidential.” Any information marked as “confidential” will not be disclosed except in accordance with 21 CFR 10.20 and other applicable disclosure law. For more information about FDA's posting of comments to public dockets, see 80 FR 56469 , September 18, 2015, or access the information at: https://www.govinfo.gov/content/pkg/FR-2015-09-18/pdf/2015-23389.pdf .
Docket: For access to the docket to read background documents or the electronic and written/paper comments received, go to https://www.regulations.gov and insert the docket number, found in brackets in the heading of this document, into the “Search” box and follow the prompts and/or go to the Dockets Management Staff, 5630 Fishers Lane, Rm. 1061, Rockville, MD 20852, 240-402-7500.
You may submit comments on any guidance at any time (see 21 CFR 10.115(g)(5) ).
Submit written requests for single copies of the draft guidance to the Office of Food Additive Safety, Center for Food Safety and Applied Nutrition, Food and Drug Administration, 5001 Campus Dr., College Park, MD 20740. Send two self-addressed adhesive labels to assist that office in processing your request. See the SUPPLEMENTARY INFORMATION section for electronic access to the draft guidance.
Kasey Heintz, Center for Food Safety and Applied Nutrition, Office of Food Additive Safety, Food and Drug Administration, 5001 Campus Dr., College Park, MD 20740, 240-402-1376; or Holli Kubicki, Center for Food Safety and Applied Nutrition, Office of Regulations and Policy, Food and Drug Administration, 5001 Campus Dr., College Park, MD 20740, 240-402-2378.
We are announcing the availability of a draft guidance for industry entitled “Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods (Edition 2).” We are issuing the draft guidance consistent with our good guidance practices regulation ( 21 CFR 10.115 ). The draft guidance, when finalized, will represent the current thinking of FDA on this topic. It does not establish any rights for any person and is not binding on FDA or the public. You can use an alternate approach if it satisfies the requirements of the applicable statutes and regulations.
Sodium is widely present in the American diet (most commonly, but not exclusively, as a result of eating or drinking foods to which sodium chloride, commonly referred to as “salt,” has been added). More than 70 percent of total sodium intake is from sodium added during food manufacturing and commercial food preparation (Ref. 1). The average sodium intake for those 1 year and older in the United States is approximately 3,400 milligrams/day (mg/day) (Ref 2). The “Dietary Guidelines for Americans, 2020-2025” (Ref. 2) advises individuals 14 years and older to limit their consumption to 2,300 mg/day; this aligns with recommendations from the National Academies of Sciences, Engineering, and Medicine, which set the chronic disease risk reduction intake for sodium at 2,300 mg/day for those 14 years and older (Ref. 3). The guidance aims to help Americans reduce average sodium intake to 2,750 mg/day (Phase II) by encouraging food manufacturers, restaurants, and food service operations to gradually reduce sodium in a wide variety of food categories over time. Although we recognize that a reduction even to 2,750 mg/day still would be higher than the recommended sodium limit of 2,300 mg/day, the Phase II goals are intended to balance the need for broad and gradual reductions in sodium and what is publicly known about technical and market constraints on sodium reduction and reformulation.
In the Federal Register of October 14, 2021, we announced the availability of the final guidance for industry, “Voluntary Sodium Reduction Goals: Target Mean and Upper Bound Concentrations for Sodium in Commercially Processed, Packaged, and Prepared Foods” ( 86 FR 57156 ). The ( print page 66729) draft guidance builds on the voluntary Phase I (2.5-year) sodium reduction goals issued in October 2021. When finalized, the draft guidance will describe our views on the next voluntary goals (Phase II (3-year)) for sodium reduction in a variety of identified categories of foods that are commercially processed, packaged, or prepared. The 3-year goals are intended to balance the need for broad and gradual reductions in sodium and what is publicly known about technical and market constraints on sodium reduction and reformulation. The distribution of sodium concentrations in currently available products in each category was a significant factor in developing these quantitative sodium concentration goals. We developed the goals with a particular emphasis on maintaining concentrations needed for food safety, given the function of salt as a food preservative. The Phase II goals are within the range of concentrations found in currently marketed foods and are feasible using existing technical strategies.
We note that we do not intend to finalize the draft long-term (10-year) sodium reduction goals that were included in the 2016 draft of the first edition of the guidance that we announced in the Federal Register of June 2, 2016 ( 81 FR 35363 ). We plan to announce any future sodium reduction goals via draft guidance.
While the guidance contains no collection of information, it does refer to previously approved FDA collections of information. The previously approved collections of information are subject to review by the Office of Management and Budget (OMB) under the Paperwork Reduction Act of 1995 (PRA) ( 44 U.S.C. 3501-3521 ). The collections of information in 21 CFR part 101 have been approved under OMB control number 0910-0381. The collections of information in 21 CFR 101.11 have been approved under OMB control number 0910-0782.
Persons with access to the internet may obtain the draft guidance at https://www.fda.gov/FoodGuidances , https://www.fda.gov/regulatory-information/search-fda-guidance-documents , or https://www.regulations.gov . Use the FDA website listed in the previous sentence to find the most current version of the guidance.
The following references are on display at the Dockets Management Staff (see ADDRESSES ) and are available for viewing by interested persons between 9 a.m. and 4 p.m., Monday through Friday; they are also available electronically at https://www.regulations.gov . Although FDA verified the website addresses in this document, please note that websites are subject to change over time.
1. Harnack L.J., M.E. Cogswell, J.M. Shikany, et al. “Sources of Sodium in U.S. Adults From 3 Geographic Regions.” Circulation, 135 (May 9, 2017): pp. 1775-1783. Available at: https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.116.024446 (accessed December 26, 2023).
2. U.S. Department of Agriculture and U.S. Department of Health and Human Services. “Dietary Guidelines for Americans, 2020-2025.” 9th Edition. December 2020. Available at: https://www.dietaryguidelines.gov/ (accessed December 26, 2023).
3. National Academies of Sciences, Engineering, and Medicine. “Dietary Reference Intakes for Sodium and Potassium” (March 2019). Washington, DC: The National Academies Press. Available at: http://www.nationalacademies.org/hmd/Reports/2019/dietary-reference-intakes-sodium-potassium.aspx (accessed December 26, 2023).
Dated: August 9, 2024.
Lauren K. Roth,
Associate Commissioner for Policy.
[ FR Doc. 2024-18261 Filed 8-15-24; 8:45 am]
BILLING CODE 4164-01-P
- Executive Orders
Reader Aids
Information.
- About This Site
- Legal Status
- Accessibility
- No Fear Act
- Continuity Information

IMAGES
COMMENTS
The Philippines is renowned as one of the species-rich countries and culturally megadiverse in ethnicity around the globe. However, ethnopharmacological studies in the Philippines are still limited especially in the most numerous ethnic tribal populations in the southern part of the archipelago. This present study aims to document the traditional practices, medicinal plant use, and knowledge ...
Methods. Quantitative ethnopharmacological data were obtained using semi-structured interviews, group discussions, field observations, and guided field walks with a total of 335 key informants comprising of tribal chieftains, traditional healers, community elders, and Manobo members of the community with their medicinal plant knowledge. The use-report (UR), use categories (UC), use value (UV ...
Introduction. Traditional medicine has been acknowledged to have an important role in the healthcare delivery system and one of the most common forms of practice is the use of medicinal plants (World Health Organization, WHO 2015).Medicinal plants are widely employed in primary healthcare services worldwide because they are cost-effective, safe, and efficient in promoting and maintaining good ...
even magic and sorcery. 1-3. Folk medicine is a field that falls under medical anthropology. It refers. to tradit ional health knowledge and healing practices anchored on. indigenous beliefs ...
The study compares the toxicity of 53 selected medicinal plants commonly used in the Philippines to treat various diseases. It uses as a benchmark Vitex negundo L., which was approved by the Philippine Food and Drug Administration as an herbal drug for cough and asthma after passing clinical trials for safety and efficacy. The methods were chosen for their simplicity and accessibility even for ...
Ethnopharmacological relevance: This study is (1) a documentation of medicinal plant use in traditional therapies, and (2) an evaluation of the medicinal plant knowledge and practices of the Ati Negrito indigenous people in Guimaras Island, Philippines. Materials and methods: A semi-structured interview was conducted to 65 informants in order to determine the medicinal plants and their uses in ...
1. Introduction1.1. Quantitative ethnobotany in the Philippines. Over the last century ethnobotany has evolved into a scientific discipline that looks at the people-plants relationship in a multidisciplinary manner using not only botany and anthropology, but also ecology, economics, public policy, pharmacology, public health, and other disciplines as needed (Balick and Cox, 1996).
Quantitative ethnopharmacological documentation and molecular confirmation of medicinal plants used by the Manobo tribe of Agusan del Sur, Philippines ... 1 The Graduate School and Research Center for the Natural and Applied Sciences, University of Santo Tomas ... The Philippines is renowned as one of the species-rich countries and culturally ...
Various studies have demonstrated overall poorer outcomes among patients with DM infected with COVID-199-16, these include increased mortality, respiratory failure, severity of COVID-19 ...
The COVID-19 pandemic disrupted the United States (US) medical education system with the necessary, yet unprecedented Association of American Medical Colleges (AAMC) national recommendation to pause all student clinical rotations with in-person patient care. This study is a quantitative analysis investigating the educational and psychological effects of the pandemic on US medical students and ...
This research utilized a multi-method quantitative study design registered under the Philippine Health Research Registry (PHRR210310-003279). Phase 1 used a psychometric study design to establish the internal consistency of PoPTQ by determining Cronbach's α value. Previous authors also used this
COVID-19 dynamics in the Philippines are driven by age, contact structure, mobility, and MHS adherence. Continued compliance with low-cost MHS should help the Philippines control the epidemic until vaccines are widely distributed, but disease resurgence may be occurring due to a combination of low population immunity and detection rates and new variants of concern.
PDF | On Sep 17, 2014, Homervergel G Ong and others published Quantitative ethnobotanical study of the medicinal plants used by the Ati Negrito indigenous group in Guimaras island, Philippines ...
The senior author (AML) has a background in health systems research, health policy, and epidemiology, and has published COVID-19 papers in the Philippine context. The lead and contributing authors (AVGN, LMMA, MCCB, DEHD, CBLL, GATS) have a background in medicine, with males and females well represented in the research team.
Background Community health workers (CHWs) are an important cadre of the primary health care (PHC) workforce in many low- and middle-income countries (LMICs). The Philippines was an early adopter of the CHW model for the delivery of PHC, launching the Barangay (village) Health Worker (BHW) programme in the early 1980s, yet little is known about the factors that motivate and sustain BHWs ...
Using both qualitative and quantitative ethnographic research methods, forty-eight common and uncommon types of jamu are discussed, and five predictions are evaluated: 1. Jamu sold daily by door to door vendors (jamu gendong) will most often be preventatives, rather than curatives; 2. ... Original Article Folk Medicine in the Philippines: A ...
a quantitative approach in ethnobotany [21] and ethnopharmacology [22] has been rising continuously in the last few decades including multivariate analysis [23]. However, few studies of quantitative ethnobotanical re-search were conducted despite the rich plant biodiversity and cultural diversity in the Philippines. In particular,
1 College of Medicine, University of the Philippines Manila, Manila, Philippines; 2 Faculty of Education, ... We conducted a cross-cultural and quantitative study to compare Filipinos' physical and mental health with Chinese during the COVID-19 pandemic. ... The Institutional Review Board of the University of Philippines Manila Research Ethics ...
In the Philippines, Quiapo is a well-known site for folk medicine services, cultural diversity, religious practices, and economic activities. Methods: This study utilized a phenomenological approach to comprehend the lived experiences of health-seeking individuals and the meaning behind their acquisition of folk medicine products.
This quantitative cross-secti onal study was conducted in the Philippines b etween February 2022 and March 2022 and was approved by the Centro Escol ar University Institutional Ethics Review Board ...
The growth of herbal medicine in the Philippines started to blossom in 1997 when former President Fidel V. Ramos signed into law the Traditional and Alternative Medicine Act, which paved for the creation of the Philippine Institute of Traditional and Alternative Health Care (PITAHC) [2].Along with the help of other governmental institutions especially the Department of Science and Technology ...
A cross-sectional survey of graduates from two Philippines medical schools: ADZU-SOM in the Mindanao region and a medical school with a more conventional curriculum, found ADZU-SOM graduates were more likely to have joined the medical profession due to a desire to help others (p = 0.002), came from lower socioeconomic strata (p = 0.001) and had ...
More information: Azadeh Dashti et al, Lung quantitative ultrasound to stage and monitor interstitial lung diseases, Scientific Reports (2024). DOI: 10.1038/s41598-024-66390-6 Journal information ...
The Medical Physics publishes papers helping health professionals perform their responsibilities more effectively and efficiently.
In the Philippines, laws promoting use of and access to generics drugs were enacted in 1988 and 2008, but uptake is poor. We investigated patient-related factors that may influence use of generics ...
Many US women report experiencing sexual violence, and many seek abortion for rape-related pregnancies. 1 Following the US Supreme Court's 2022 Dobbs v Jackson Women's Health Organization (Dobbs) decision overturning Roe v Wade, 14 states have outlawed abortion at any gestational duration. 2 Although 5 of these states allow exceptions for rape-related pregnancies, stringent gestational ...
The "Dietary Guidelines for Americans, 2020-2025" (Ref. 2) advises individuals 14 years and older to limit their consumption to 2,300 mg/day; this aligns with recommendations from the National Academies of Sciences, Engineering, and Medicine, which set the chronic disease risk reduction intake for sodium at 2,300 mg/day for those 14 years ...