Case Study: A Residential Septic System Affected by Home Hemodialysis
- By Sara Heger, Ph.D.
- February 17, 2020

Filed Under
Sign me up, sign up digital, subscribe to print.
The University of Minnesota Onsite Sewage Treatment Program assessed a residential septic system in Minnesota owned by a patient undergoing home hemodialysis treatment for kidney failure to evaluate the wastewater being generated by the household and determine whether the...
Popular Stories

Case Study: A Residential Septic System Affected by Home Hemodialysis
- By Sara Heger, Ph.D.
- February 27, 2020
Filed Under
Sign me up, sign up digital, subscribe to print.
The University of Minnesota Onsite Sewage Treatment Program assessed a residential septic system in Minnesota owned by a patient undergoing home hemodialysis treatment for kidney failure to evaluate the wastewater being generated by the household and determine whether the...
Popular Stories

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Outcome of home haemodialysis patients: a case-cohort study
Affiliation.
- 1 Division of Nephrology/Hypertension, University of Bern, Freiburgstrasse, 3010 Bern - Inselspital, Switzerland. E-mail: [email protected].
- PMID: 15665030
- DOI: 10.1093/ndt/gfh674
Background: Randomized, controlled comparisons between home haemodialysis (HHD) and centre haemodialysis (CHD) have not been performed to date. Reported survival benefits of HHD as compared with CHD from uncontrolled studies have been attributed largely to patient selection.
Methods: In order to minimize a selection bias, we have compared the outcome of our HHD and CHD patients with a nested case-cohort study. For each patient trained for HHD at our dialysis centre between 1970 and 1995 (n=103), a corresponding match was searched from the CHD patients by retrospective chart analysis. The pairs were matched for sex, age (+/-5 years), time of dialysis therapy onset (+/-2 years) and renal disease category. For 58 of the 103 HHD patients, a corresponding matched CHD patient was identified. Both treatment groups had the same mean age (50+/-13 years) at dialysis onset and were comparable with respect to the Khan comorbidity index, prevalence and duration of hypertension, smoking habits, history of myocardial infarction, stroke and peripheral vascular disease. In both groups, approximately 50% of the patients were transplanted during the observation period.
Results: HHD patients were hospitalized less often and tended to have fewer operations as compared with CHD patients. Survival was significantly longer in HHD as compared with CHD. Five, 10 and 20 year survival rates were 93 (n=55 patients at risk), 72 (41) and 34% (11) with HHD and 64 (38), 48 (26) and 23% (4) with CHD, respectively. This survival difference persisted after adjusting for predictors of mortality, i.e. age at onset of dialysis, year of start of dialysis therapy and Khan comorbidity index.
Conclusions: HHD offers a cheap and valuable alternative to CHD, with no apparent disadvantages.
PubMed Disclaimer
- HDD cannot be advocated for all patients. Cohen E, Charba D. Cohen E, et al. Nephrol Dial Transplant. 2005 Jun;20(6):1272; author reply 1272. doi: 10.1093/ndt/gfh844. Epub 2005 Apr 19. Nephrol Dial Transplant. 2005. PMID: 15840662 No abstract available.
- The true history of home haemodialysis. Shaldon S. Shaldon S. Nephrol Dial Transplant. 2005 Aug;20(8):1766; author reply 1767. doi: 10.1093/ndt/gfh853. Epub 2005 Apr 26. Nephrol Dial Transplant. 2005. PMID: 15855203 No abstract available.
Similar articles
- Systematic differences among patients initiated on home haemodialysis and peritoneal dialysis: the fallacy of potential competition. Rioux JP, Bargman JM, Chan CT. Rioux JP, et al. Nephrol Dial Transplant. 2010 Jul;25(7):2364-7. doi: 10.1093/ndt/gfq192. Epub 2010 Mar 31. Nephrol Dial Transplant. 2010. PMID: 20360014
- Outcomes of a provincial home haemodialysis programme--a two-year experience: establishing benchmarks for programme evaluation. Komenda P, Copland M, Er L, Djurdjev O, Levin A. Komenda P, et al. Nephrol Dial Transplant. 2008 Aug;23(8):2647-52. doi: 10.1093/ndt/gfn065. Epub 2008 Mar 10. Nephrol Dial Transplant. 2008. PMID: 18332070
- Cost analysis and health-related quality of life of home and self-care satellite haemodialysis. Malmström RK, Roine RP, Heikkilä A, Räsänen P, Sintonen H, Muroma-Karttunen R, Honkanen E. Malmström RK, et al. Nephrol Dial Transplant. 2008 Jun;23(6):1990-6. doi: 10.1093/ndt/gfm910. Epub 2008 Jan 26. Nephrol Dial Transplant. 2008. PMID: 18223263
- Future of home haemodialysis in Australia and New Zealand. Lynn KL, Buttimore AL. Lynn KL, et al. Nephrology (Carlton). 2005 Jun;10(3):231-3. doi: 10.1111/j.1440-1797.2005.00399.x. Nephrology (Carlton). 2005. PMID: 15958034 Review.
- Role of peritoneal dialysis in the era of the resurgence of home hemodialysis. Burkart J. Burkart J. Hemodial Int. 2008 Jul;12 Suppl 1:S51-4. doi: 10.1111/j.1542-4758.2008.00297.x. Hemodial Int. 2008. PMID: 18638242 Review.
- Home versus in-centre haemodialysis for people with kidney failure. Cheetham MS, Ethier I, Krishnasamy R, Cho Y, Palmer SC, Johnson DW, Craig JC, Stroumza P, Frantzen L, Hegbrant J, Strippoli GF. Cheetham MS, et al. Cochrane Database Syst Rev. 2024 Apr 8;4(4):CD009535. doi: 10.1002/14651858.CD009535.pub3. Cochrane Database Syst Rev. 2024. PMID: 38588450 Review.
- Main Barriers to the Introduction of a Home Haemodialysis Programme in Poland: A Review of the Challenges for Implementation and Criteria for a Successful Programme. Kendzia D, Lima F, Zawierucha J, Busink E, Apel C, Malyszko JS, Zebrowski P, Malyszko J. Kendzia D, et al. J Clin Med. 2022 Jul 18;11(14):4166. doi: 10.3390/jcm11144166. J Clin Med. 2022. PMID: 35887931 Free PMC article. Review.
- Fewer hospitalizations and prolonged technique survival with home hemodialysis- a matched cohort study from the Swedish Renal Registry. Rydell H, Ivarsson K, Almquist M, Clyne N, Segelmark M. Rydell H, et al. BMC Nephrol. 2019 Dec 30;20(1):480. doi: 10.1186/s12882-019-1644-z. BMC Nephrol. 2019. PMID: 31888674 Free PMC article.
- Autodialysis in Morocco: how much longer can we wait? Noto-Kadou-Kaza B, Mahamat HA, Mtioui N, Izem A, Abouamrane LM, El-Khayat S, Zamd M, Medkouri G, Benghanem MG, Ramdani B. Noto-Kadou-Kaza B, et al. Pan Afr Med J. 2019 Jul 3;33:162. doi: 10.11604/pamj.2019.33.162.13282. eCollection 2019. Pan Afr Med J. 2019. PMID: 31565124 Free PMC article.
- Improved long-term survival with home hemodialysis compared with institutional hemodialysis and peritoneal dialysis: a matched cohort study. Rydell H, Ivarsson K, Almquist M, Segelmark M, Clyne N. Rydell H, et al. BMC Nephrol. 2019 Feb 13;20(1):52. doi: 10.1186/s12882-019-1245-x. BMC Nephrol. 2019. PMID: 30760251 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.
- Silverchair Information Systems
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

Disclosure Statement
Choosing home hemodialysis: a critical review of patient outcomes.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Brent W. Miller , Rainer Himmele , Dixie-Ann Sawin , Jeeseon Kim , Robert J. Kossmann; Choosing Home Hemodialysis: A Critical Review of Patient Outcomes. Blood Purif 20 April 2018; 45 (1-3): 224–229. https://doi.org/10.1159/000485159
Download citation file:
- Ris (Zotero)
- Reference Manager
Background/Aim: Home hemodialysis (HHD) has been associated with improved clinical outcomes vs. in-center HD (ICHD). The prevalence of HHD in the United States is still very low at 1.8%. This critical review compares HHD and ICHD outcomes for survival, hospitalization, cardiovascular (CV), nutrition, and quality of life (QoL). Methods: Of 545 publications identified, 44 were not selected after applying exclusion criteria. A systematic review of the identified publications was conducted to compare HHD to ICHD outcomes for survival, hospitalization, CV outcomes, nutrition, and QoL. Results: Regarding mortality, 10 of 13 trials reported 13–52% reduction; three trials found no differences. According to 6 studies, blood pressure and left ventricular size measurements were generally lower in HHD patients compared to similar measurements in ICHD patients. Regarding nutritional status, conflicting results were reported (8 studies); some found improved muscle mass, total protein, and body mass index in HHD vs. ICHD patients, while others found no significant differences. There were no significant differences in the rate of hospitalization between HHD and ICHD in the 6 articles reviewed. Seven studies on QoL demonstrated positive trends in HHD vs. ICHD populations. Conclusions: Despite limitations in the current data, 66% of the publications reviewed (29/44) demonstrated improved clinical outcomes in patients who chose HHD. These include improved survival, CV, nutritional, and QoL parameters. Even though HHD may not be preferred in all patients, a review of the literature suggests that HHD should be provided as a modality choice for substantially more than the current 1.8% of HHD patients in the United States.
Favorable clinical outcomes have been associated with use of home hemodialysis (HHD) as a modality, including quality of life (QoL) parameters, survival and mortality, cardiovascular (CV) endpoints, phosphate control, nutritional status, and anemia management. However, differences in outcomes with HHD compared to conventional in-center HD (ICHD) are not well characterized. To more completely understand the effect of HHD on clinical outcomes in dialysis patients, we performed a critical review of the available literature to evaluate the effects of HHD on patient outcomes in comparison to ICHD.
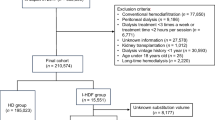
Medical and scientific literature were systematically reviewed for various outcomes comparing the use of HHD to ICHD. We conducted in-depth electronic searches in PubMed, Embase, and the Cochrane Central Register of Controlled Trials using the following search terms: HHD, end-stage renal disease, health-related QoL, QoL, mortality, survival, nutrition, hospitalization, morbidity, blood pressure (BP), CV, nocturnal, extended, in-center conventional hemodialysis, and self-care. Identified titles and abstracts of clinical, prospective and interventional studies (nonrandomized and randomized) were screened by 2 independent reviewers to determine study eligibility. Full-text versions of potentially eligible studies were then screened for key criteria. References were cataloged using the Mendeley database application ( www.Mendeley.com ). Inclusion and exclusion criteria are listed in Table 1 .
Details of selection criteria for included studies

For studies included in this analysis, a detailed description of the results and authors analysis was documented in a database and reviewed systematically for the above-mentioned outcomes. Figure 1 shows a schematic of the search results. Of the initial 545 identified publications on HHD and ICHD, 281 publications were excluded because they did not address any of our five main outcome parameters of interest for this review. From these, we excluded duplications, those that did not directly compare HHD to in-center, and/or contained at least one of the exclusion criteria listed in Table 1 , leaving 44 publications to be included in our analysis. In order to systematically assess these 44, we applied the validated Downs and Black approach with 26 items based on 5 subscales of reporting, external validity, bias, confounding and power [ 1 ]. Scores were generally reported as 0 or 1, with 2 exceptions (0–2 or 0–5 scales for a reporting and power question respectively). Studies for each outcome were ranked by group, with a maximum score possible of 31; higher scores indicated better data quality.

Schematic representation of studies identified.
Survival and Mortality in HHD vs. ICHD
Of 146 publications on survival and mortality, 13 met the selection criteria. Studies on mortality and survival had the highest quality score of all outcome data assessed in this review (Table 2 ; score: 17 out of 31), and included one randomized controlled trial [ 2 ] and 9 retrospective or prospective observational studies [ 3-11 ], an analysis of an observational study [ 12 ], a post-trial observational study of the long-term effects of a randomized controlled trial [ 13 ], and a recently published matched-cohort study [ 14 ]. Studies predominantly reported positive (9) effects of HHD on mortality or survival compared to ICHD; 2 studies showed negative or no effects.
Assessment of the quality of studies included for analysis of outcomes with HHD vs. ICHD

Large observational studies independently report that HHD imparts survival benefits (44–52% decreased risk) to patients compared to ICHD [ 4, 10 ]. Matched cohort studies also reported lower mortality risk (13–64%) in HHD vs. ICHD [ 3, 5, 15 ]. Lower 5-, 10-, and 20-year survival rates were also reported for HHD vs. CHD [ 6, 11, 14 ]. Over 14 years, Rydell et al. [ 14 ] found significantly longer survival in HHD vs. ICHD patients (mean survival: 17.3 vs. 13.0 years, respectively). Nocturnal HHD (NHHD) was also associated with reduced risk of death or comorbid events (e.g., acute myocardial infarction or stroke [hazard ratio (HR) 0.56; 95% CI 0.35–0.89; p = 0.01]) [ 5 ]. Kjellstrand et al. [ 6 ] further showed that the time to reach 50% mortality was longer in patients on SDHHD or self-care HD (5.1 ± 0.8 years) vs. matched ICHD (2.8 years). The standardized mortality rate for NHHD patients was also reportedly one third that for ICHD counterpart from USRDS data; cumulative survival was 79 and 64% at 5 and 10 years [ 9, 16 ].
In contrast, the Frequent Hemodialysis Network (FHN) trial found higher mortality in NHHD vs. ICHD (HR 3.88; 95% CI 1.27–11.79) [ 2, 13 ]. Neither Nitsch nor MacRae found any mortality benefits with HHD vs. ICHD in retrospective analyses [ 8, 12 ]. However, McRae’s sub-group analysis showed significantly higher mortality with HHD vs. ICHD (HR 1.10; 95% CI 1.04–1.17; p = 0.002) [ 12 ].
CV Outcomes
Fifty-one articles were identified for review. Six studies (overall quality rating: 14.7) met the inclusion criteria; all showed positive effects of HHD vs. ICHD. Studies report reduced BP and left ventricular mass (LVM) with HHD vs. ICHD [ 2, 17-21 ]. Culleton et al. [ 18 ] showed significantly greater LVM reduction vs. ICHD and lower systolic and diastolic BPs. In the FHN nocturnal trial, secondary outcome parameters of pre- and diastolic BP were significantly lower with NHHD in months 2–12 ( p < 0.001). Also, significantly fewer NHHD patients required saline administration, despite similar rates of intradialytic hypotensive episodes. A Cochrane Database review suggested a beneficial effect of HHD on BP [ 22 ], and a meta-analysis of observational and prospectively randomized studies found improvements in BP of 14 mm Hg and mean LVM of 31 g/m 2 [ 23 ].
Health-Related QoL
In the context of health-related quality of life (HRQoL), we identified 111 publications, of which 7 were included in this review. Although the overall quality score obtained for these studies was the lowest (Table 2 ; score: 12.1), most of the studies showed positive trends. Compared to ICHD, HHD-treated patients reported higher overall and specific component scores on standardized HRQoL tests [ 18, 24-29 ]. The only randomized controlled trial included in the analysis found improved QoL scores with NHHD vs. ICHD [ 18 ]: NHHD significantly improved scores for effects of kidney disease ( p = 0.01) and for burden of kidney disease ( p = 0.02). Using the short form (SF)-36 tool, the London Daily/Nocturnal Hemodialysis study found that quotidian dialysis yielded significantly fewer dialysis and disease-related symptoms than ICHD and was associated with better fluid management, less severe cramping, fewer headaches (SDHHD only), less hypotension, fewer episodes of dizziness, decreased fluid restrictions, better BP control, decreased interdialytic weight gain, fewer episodes of shortness of breath, and reduction in “feeling cold.” These patients also reported significantly less fatigue and decreased recovery time compared to controls. Data also showed that patients who converted from ICHD preferred to continue with quotidian dialysis when given a choice [ 25 ]. Using similar tools in Japanese patients, Watanabe et al. [ 28 ] also reported higher QoL scores and fewer dietary restrictions in HHD vs. ICHD patients.
Three studies specifically evaluated the impact of NHHD vs. ICHD on the overall HRQoL [ 18, 26, 27 ]. McFarlane et al. [ 26 ] ( n = 24) reported that NHHD was associated with significantly higher overall QoL vs. ICHD ( p = 0.03). In their prespecified outcomes, Culleton et al. [ 18 ] reported that NHHD significantly improved 2 of the 4 selected KDQOL-SF parameters: effects of kidney disease and burden of kidney disease. Mohr et al. [ 27 ] reviewed literature from 1969 to 2000 (4 studies) on nocturnal HD vs. ICHD and reported consistently improved aspects of QoL (mental health, physical ability, depression, energy-fatigue indices, symptoms, etc.) using different standardized tests (SF-36, beck depression inventory, KDQOL, Sickness Impact Profile) [ 27 ]. Regarding systematic reviews, Mowatt et al. [ 30 ] concluded that patients performing HHD modalities reported better QoL outcomes compared to ICHD. The Cochrane Review was inconclusive.
Despite the lack of high-quality studies comparing outcomes in HHD vs. ICHD, we identified several studies that when examined individually and collectively for their strengths, suggest that HHD can positively impact various clinical outcomes, and may even be better for many patients in selected circumstances compared to ICHD.
Large observational and matched cohort studies generally support a survival benefit over time in patients choosing HHD vs. ICHD [ 3, 4, 10, 14, 15 ]. Although the FHN results are negative, it should be noted that the nocturnal study was not powered to detect the mortality effects (primary outcome); ICHD patients had lower than average mortality vs. USRDS data [ 2, 13 ]; and patients were allowed to modify their dialysis prescription after study completion. Therefore, the observed increase in mortality might not be due to modality differences. In MacRae et al. [ 12 ], HHD patients who were more likely to reside at home had significantly lower mortality compared to other modalities, while the mortality risk of those who were more likely to reside at long-term care facilities was higher, suggesting patient characteristics as a confounder [ 12 ]. Although Nitsch et al. [ 8 ] reported no statistically significant differences in adjusted analyses, unadjusted analyses found a possible survival advantage with HHD vs. other modalities ( p < 0.001). Overall, the data points to a positive effect of HHD on survival for many patients who choose this modality.
Regarding CV outcomes, BP was assessed in 3 different randomized trials; each found at least a positive trend in controlling hypertension with HHD [ 2, 18, 19 ]. Notably, the conclusion from the Cochrane Database Review was that HHD could reduce 24-h ambulatory BP [ 22 ]. Culleton et al. [ 18 ] also met their primary endpoint, demonstrating significant reduction in LVM with HHD. Although a secondary outcome, they noted improved SBP after adjustment and reduction in anti-hypertensive medications. The FHN nocturnal trial also showed a positive effect on BP [ 2, 17 ] despite not being powered to detect this. The available evidence overwhelmingly suggest that compared to ICHD, HHD use can lead to improvement in BP in some patients.
Although the QoL data included for review here are derived from small, mostly observational studies, they consistently showed that most patients who chose HHD reported higher QoL scores vs. ICHD including improved mental health, physical ability, depression, energy-fatigue indices, and/or dialysis symptoms, which may persist over time.
Although not discussed in this paper, there was no statistically significant effect of HHD on overall hospitalizations, although, some authors suggest that the length of stay in the hospital may be reduced with HHD. Higher risk of infection-related hospitalization reported in the literature may be offset by reduced CV-related hospitalizations, leading to no net effect on the all-cause hospitalization risk. However, this notion has not been validated. Another aspect not addressed in this review but worth mentioning is the potential effect of HHD on nutrition. Studies suggest that compared to ICHD, HHD can improve nutritional status in some patients, shown by increased protein intake, muscle mass, body weight, serum albumin level, or other biochemical parameters.
There are several limitations to this study. Most of the studies identified and included were retrospective and observational in nature; thus, there is inherent residual confounding. In some studies, HHD patients were younger and healthier with fewer comorbidities, had education on different dialysis modalities, had different primary causes of CKD, and were more likely to have been referred to a nephrologist earlier. Others did not consider comorbidities to be confounders, did not use unstandardized protocols, did not perform subgroup analyses or include appropriate control groups, or report subjective data. In most studies, dose and frequency of HHD therapy were greater than that in in-center therapy and not adjusted for using appropriate statistical models. Thus, whether the positive effect is due to increased dialysis rather than a home vs. center effect cannot be ruled out. Even though some studies performed extensive propensity score matching, residual confounding may persist, as additional factors that could play a role in outcome assessments might not be considered, for example, degree of patient motivation; dialysis and medication adherence, vascular access type, and dependence on a caregiver to perform dialysis. In addition, many studies were not large enough to assess clinical outcome parameters or designed to address cause and effect. The few randomized controlled trials were also limited by many factors including low power, small size, short follow-up duration, and possible risk of false-positive findings, making generalization beyond the study population difficult.
In the absence of substantial equivalence through large, randomized, prospective trials, there is an increasing number of publications addressing the importance and impact of HHD on outcomes. Strengths of our approach include the application of uniform restrictive criteria to select studies that obtained clinical outcome data using validated methodology. We did not censor by technology, manufacturer, or country, and data was obtained from demographically and geographically diverse populations. The difference in populations, sample sizes, and study designs identified greatly reduces the possibility of performing quantitative meta-analysis on this data. Thus, a fair and balanced systematic qualitative review seems an appropriate approach to highlight the current state of literature and provide an overall picture of where the published evidence stands today.
In the United States, only 1.8% of dialysis patients are on HHD and comparing this small population to the much larger in-center population is difficult. Characteristics between HHD and in-center populations can differ, and nephrologists’ prescribing preferences also vary widely. Together, these factors make generalization of current evidence difficult and impede large, well-designed studies that report on clinical outcomes from being conducted. Despite these and other inherent limitations of the existing data, data on clinical outcomes in patients undergoing HHD are encouraging and there appears to be ample support for HHD as a viable, dialysis option that can allow many patients to experience improvements in several clinical outcomes including survival, CV, nutritional and QoL parameters. If indicated, HHD may be suitable for those patients, who at the very least, are empowered and want greater flexibility and control of their time, or those who may not be able to drive or have reliable transportation to a dialysis center or simply prefer to dialyze in the comfort of their homes. Although HHD may not be the preferred modality for all dialysis patients, the currently available data certainly suggest that HHD should be offered as a modality choice for substantially more than the small, minority of prevalent HHD patients in the United States.
B.W.M. is an employee of Fresenius Kidney Care; R.H., D.-A.S., and R.J.K. are employees of the Fresenius Renal Therapies Group.
Email alerts
Citing articles via, suggested reading.
- Online ISSN 1421-9735
- Print ISSN 0253-5068
INFORMATION
- Contact & Support
- Information & Downloads
- Rights & Permissions
- Terms & Conditions
- Catalogue & Pricing
- Policies & Information
- People & Organization
- Stay Up-to-Date
- Regional Offices
- Community Voice
SERVICES FOR
- Researchers
- Healthcare Professionals
- Patients & Supporters
- Health Sciences Industry
- Medical Societies
- Agents & Booksellers
Karger International
- S. Karger AG
- P.O Box, CH-4009 Basel (Switzerland)
- Allschwilerstrasse 10, CH-4055 Basel
- Tel: +41 61 306 11 11
- Fax: +41 61 306 12 34
- Contact: Front Office
- Experience Blog
- Privacy Policy
- Terms of Use
This Feature Is Available To Subscribers Only
Sign In or Create an Account

- News & Research >
- KidneyViews Blog >
Thriving Against the Odds: My Journey with Home Hemodialysis

My life has been shaped by a journey through end-stage renal disease (ESRD) since 2000. It all began after my third pregnancy when I was diagnosed with Membranoproliferative Glomerulonephritis Type II . The diagnosis was a turning point, marking the start of a challenging yet profoundly transformative path.
In 2005, I began my home dialysis journey. I chose PD as my modality and thrived on it for 9yrs . In 2014, I was blessed by two angels on earth through the paired exchange program at John Hopkins, I received a kidney from a live donor with the help of my loving, selfless husband donating his kidney. However, in 2021, my transplanted kidney began failing.
Unfortunately, my health was declining, and dialysis was inevitable. I was in denial at first but quickly realized how unwell I was feeling day by day. Eventually, I received education on HHD and even though I was terrified of the needles and having to cannulate myself, I found the courage to press on and empower myself to change my mindset .
One thing I've learned through this journey is that dialysis doesn't define my life; it's simply a part of it . With home hemodialysis, I have the flexibility to dialyze on my own schedule, allowing me to work, volunteer, travel, and socialize with friends—all while managing my health effectively.
Work has always been a cornerstone of my identity , and despite the challenges, I've continued to pursue my career with determination and passion. Whether I'm in the office or working remotely, my job gives me a sense of purpose and accomplishment that fuels my spirit.

Volunteering has also been a significant part of my life. Giving back to my community and helping others has been incredibly fulfilling . It's a reminder that despite my health challenges, I have the power to make a positive impact in the lives of those around me.
Travel has always been a passion of mine , and I've refused to let dialysis hold me back. Luckily with HHD, I can bring my machine with me to all my travel destinations. From exploring new cities to relaxing on beautiful beaches, every trip is a reminder that life is meant to be lived fully, regardless of the obstacles we face.
Socializing with friends and loved ones has been essential for my well-being. Whether it's gathering for dinner, celebrating milestones, or simply enjoying each other's company, their support and encouragement have been a constant source of strength throughout my journey .

Choosing home hemodialysis has significantly improved my quality of life. It has empowered me to live life on my terms . It's given me the flexibility and control I need to pursue my passions and responsibilities without compromise. Managing my health from the comfort of my own home has made a world of difference, allowing me to focus on what truly matters: living a fulfilling and meaningful life.
My journey with kidney disease has been challenging, but it has also been a journey of growth, resilience, and gratitude. It's taught me to appreciate every moment, to embrace life's uncertainties, and to never lose sight of the strength within myself . I hope my story serves as inspiration to others facing similar challenges—that with determination, support, and the right mindset, anything is possible.
As I continue this journey, I am grateful for every opportunity, experience, and person who has been a part of my story. I am proof that life with kidney disease can be rich and fulfilling, and I am determined to continue thriving, no matter what lies ahead.
Steven Cohn
Jul 17, 2024 3:45 PM
Reply to a Comment
Jul 13, 2024 4:10 PM
Leave a New Comment
Advertisement

Expanded home hemodialysis: case reports
- Nephrology - Original Paper
- Published: 15 April 2020
- Volume 52 , pages 977–980, ( 2020 )
Cite this article

- Alejandro Pérez-Alba ORCID: orcid.org/0000-0002-6732-4670 1 , 2 ,
- Javier Reque-Santiváñez 1 ,
- Milagros Vázquez-Gómez 1 &
- Ramón Pons-Prades 1
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
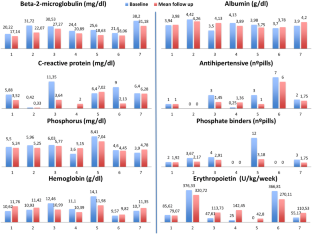
Among the different hemodialysis (HD) strategies, the short daily hemodialysis performed at home (SDHHD) provides clinical benefits to the patient. Expanded hemodialysis (HDx) employs cutoff medium membranes that exhibit greater clearance capacity of uremic toxins of medium–high molecular weight. This case series study reported the results of seven patients who were transferred to expanded hemodialysis at home (HHDx), from December 2017 to March 2019, over a 12-month follow-up period. The AK-98 monitor and Theranova 400 membrane (Baxter International Inc., Deerfield, IL, USA) were used. The main outcome measures were blood analytical values and drug consumption. The blood levels of β2-microglobulin were significantly reduced ( p = 0.0082), while maintaining albumin levels with less use of phosphorus binders. Regarding the safety profile, technique-related adverse events were not reported. According to the results of the current study, HHDx was a safe technique, which additionally had the ability to provide benefits to patients due to its greater purification capacity. Further studies, especially multicenter ones, with a greater number of patients are needed to confirm these results.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

- Hemodialysis
Intermittent infusion hemodiafiltration is associated with improved survival compared to hemodialysis

Effects of high albumin leakage on survival between online hemodiafiltration and super high-flux hemodialysis: the HISTORY study
Daugirdas JT, Chertow GM, Larive B, Pierratos A, Greene T, Ayus JC et al (2012) Effects of frequent hemodialysis on measures of CKD mineral and bone disorder. J Am Soc Nephrol 23:727–738
Article CAS Google Scholar
Brunati CCM, Gervasi F, Casati C, Querques ML, Montoli A, Colussi G (2018) Phosphate and calcium control in short frequent hemodialysis with the NxStage system one cycler: mass balance studies and comparison with standard thrice-weekly bicarbonate dialysis. Blood Purif 45:334–342
Article Google Scholar
Finkelstein FO, Schiller B, Daoui R, Gehr TW, Kraus MA, Lea J et al (2012) At-home short daily hemodialysis improves the long-term health-related quality of life. Kidney Int 82:561–569
Suri RS, Li L, Nesrallah GE (2015) The risk of hospitalization and modality failure with home dialysis. Kidney Int 88:360–368
Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW, Gassman JJ et al (2010) In-center hemodialysis six times per week versus three times per week. N Engl J Med 363:2287–2300
Pérez Alba A, Reque Santiváñez J, Vázquez Gómez M, Pons Prades R (2018) Spanish home hemodialysis experience. Rev Colomb Nefrol 5:127–136
Eloot S, Van Biesen W, Dhondt A, Van de Wynkele H, Glorieux G, Verdonck P et al (2008) Impact of hemodialysis duration on the removal of uremic retention solutes. Kidney Int 73:765–770
Maduell F, Sánchez-Canel JJ, Blasco JA, Navarro V, Rius A, Torregrosa E et al (2006) Middle molecules removal. Beyond beta2-microglobulin. Nefrologia 26:469–475
CAS PubMed Google Scholar
Kirsch AH, Lyko R, Nilsson LG, Beck W, Amdahl M, Lechner P et al (2017) Performance of hemodialyis with novel medium cut-off dialyzers. Nephrol Dial Transplant 32:165–172
Huang SS, Kaysen GA, Levin NW, Kliger AS, Beck GJ, Rocco MV et al (2019) The effect of increased frequency of hemodialysis on serum cystatin C and β2-microglobulin concentrations: a secondary analysis of the frequent hemodialysis network (FHN) trial. Hemodial Int 23:297–305
Nlandu Y, Padden M, Seidowsky A, Hamaz S, Vilaine E, Cheddani L et al (2019) Middle-molecule uremic toxins: a renewed interest. Nephrol Ther 15:82–90
Jelkmann W (2011) Regulation of erythropoietin production. J Physiol 589:1251–1258
Macías N, Vega A, Abad S, Santos A, Cedeño S, Linares T et al (2017) Is High-Volume online hemodiafiltration associated with malnutrition? Ther Apher Dial 21:361–369
Maduell F, Rodas L, Broseta JJ, Gómez M, Montagud-Marrahi E, Guillén E et al (2019) Evaluation of the influence of the surface membrane and blood flow in medium «cut-off» (MCO) dialyzers. Nefrologia 39:623–628
Download references
Acknowledgements
Medical writing and editorial assistant services have been provided by Ciencia y Deporte S.L. Support for this assistance was funded by Baxter.
Medical writing services has been provided by Baxter. Baxter did not participate in either data analysis or redaction of the manuscript.
Author information
Authors and affiliations.
Department of Nephrology, Hospital Universitari General de Castellón, Avinguda de Benicàssim, 128, 12004, Castellón de la Plana, Spain
Alejandro Pérez-Alba, Javier Reque-Santiváñez, Milagros Vázquez-Gómez & Ramón Pons-Prades
Universidad Politécnica de Madrid, Madrid, Spain
Alejandro Pérez-Alba
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Alejandro Pérez-Alba .
Ethics declarations
Conflict of interest.
Dr Alejandro Pérez-Alba has received consulting fees from Baxter during the conduct of the study. The rest of the authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Pérez-Alba, A., Reque-Santiváñez, J., Vázquez-Gómez, M. et al. Expanded home hemodialysis: case reports. Int Urol Nephrol 52 , 977–980 (2020). https://doi.org/10.1007/s11255-020-02455-5
Download citation
Received : 14 January 2020
Accepted : 27 March 2020
Published : 15 April 2020
Issue Date : May 2020
DOI : https://doi.org/10.1007/s11255-020-02455-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Expanded hemodialysis
- Short daily hemodialysis
- Home hemodialysis
- Find a journal
- Publish with us
- Track your research
HOME HEMODIALYSES IN PRACTICE - CASE STUDY
- December 2022
- Ošetřovatelské perspektivy 5(2):61-70
- This person is not on ResearchGate, or hasn't claimed this research yet.
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Jean-Christophe Szelag
- Cécile Courivaud
- Jean-Paul Cristol
- Andrew Shehata
- Hammad Choudhry
- Darell Hawley
- Roma Padalkar
- Catherine Morin
- Isabelle Gionest
- Louis-Philippe Laurin

- Brigit C. van Jaarsveld

- Alison M MacLeod

- INT J QUAL HEALTH C
- Omar Tombocon
- Peter Tregaskis
- Catherine Reid

- Donald L. Patrick

- Justin Ashley

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Case Rep Nephrol Dial
- v.11(3); Sep-Dec 2021

Hemodialysis Initiation in Oldest-Old Patients: A Case Series
Ryoichi maenosono.
a Department of Urology, Faculty of Medicine, Osaka Medical and Pharmaceutical University, Osaka, Japan
Tomohisa Matsunaga
Yuki yoshikawa, kazuki nishimura, haruhiko onaka.
b Department of Cardiology, Takatsuki Red Cross Hospital, Osaka, Japan
Kazumasa Komura
Hirofumi uehara, haruhito azuma, associated data.
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
With an increase in the number of older adults worldwide, the oldest-old population, defined as individuals over the age of 90, is also growing. Japan is now facing the problem of a “super-aged society” in which over 21% of the population is aged over 65. The oldest-old constituted 1.8% (2.31 million) of the Japanese population in 2019. Such individuals have special health-care needs. In cases of acute or chronic (or both) renal failure in the oldest-old, it becomes difficult to decide whether dialysis should be initiated. The issue is controversial, and there is some debate on whether dialysis should be avoided in elderly people because of their frailty or if it should be initiated to enable them to spend their remaining years with their families by improving their quality of life. Herein, we describe our experience in 4 cases of hemodialysis initiated in patients over the age of 90. In our experience, dialysis enabled them to spend the rest of their lives with their families, which could not have been possible without it. Although further studies are needed, we concluded that oldest-old individuals in good general health could be eligible for and benefit from hemodialysis.
Introduction
An “elderly” or older person is defined as an individual over the age of 65 years. The elderly population is increasing worldwide. According to the World Health Organization, the proportion of the world's population over 60 years will nearly double from 12 to 22% between 2015 and 2050 [ 1 ]. Japan is now facing the problem of a “super-aged society” wherein over 21% of the population comprises individuals aged >65 years. Moreover, according to the Japanese Ministry of Internal Affairs and Communications, 28.4% (35.88 million) of the Japanese population is aged over 60 years. In 2019, individuals over 90 years constituted 1.8% (2.31 million) of the Japanese population.
Generally, elderly individuals are frail, which is defined as multisystem impairment with increased vulnerability to stressors [ 2 ] due to age-related changes and are unsuitable candidates for high-risk operations, more so if they are aged over 90 years. However, whether individuals aged over 90 years should be treated with hemodialysis remains controversial. Herein, we narrate our experience with 4 cases of hemodialysis in patients aged over 90 years and then discuss whether hemodialysis initiation was suitable in these cases.
Case Presentation
We treated 4 chronic kidney disease (CKD) nonagenarians at our department between 2016 and 2020. Written informed consent was obtained from all patients. The patients' backgrounds and survival outcomes are summarized in Table Table1 1 and Figure Figure1, 1 , respectively. Concerning the preservation period of renal failure, we referred to Ottawa Personal Decision Guides (OPDG) to confirm their willingness. We evaluated each patient's general condition with the Charlson comorbidity index (CCI), subjective global assessment (SGA), and Geriatric nutritional risk index (GNRI).

Overall survival curve of our 4 oldest-old patients on hemodialysis.
Backgrounds of the 4 patients in whom hemodialysis was initiated after the age of 90 years
| Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|
| Age, hemodialysis initiation | 91 | 92 | 90 | 94 |
| Age, vascular access | 91 | 92 | 89 | 94 |
| Physical Examination, at initiation | ||||
| Sex | Female | Male | Male | Male |
| Height, m | 1.46 | 1.62 | 1.57 | 1.60 |
| Body weight, kg | 42.4 | 76.0 | 58.1 | 61.3 |
| BMI | 19.9 | 29.1 | 23.6 | 23.9 |
| Primary disease | DMN | AKI | DMN | NS |
| Laboratory Examination, at initiation | ||||
| Hemoglobin, g/dL | 9.9 | 9.5 | 9.6 | 10.2 |
| Serum albumin, g/dL | 2.3 | 3.7 | 3.4 | 4.1 |
| Brain natriuretic peptide, pg/mL | 453.8 | 907.2 | 189.6 | 262.9 |
| Emergency initiation? | Yes | Yes | No | No |
| CCI | 6 | 5 | 4 | 3 |
| SGA | C | C | A | B |
| GNRI, at initiation | 72.0 | 110.3 | 95.3 | 106.5 |
| GNRI, after 1 m | 75.7 | 83.0 | 94.3 | 95.6 |
AKI, acute kidney injury; Alb, albumin; BMI, body mass index; BW, body weight; CCI, Charlson comorbidity index; DMN, diabetic nephropathy; GNRI, geriatric nutritional risk index; IBW, ideal body weight; SGA, subjective global assessment.
*GNRI was calculated using the formula: GNRI = (1.489 × Alb) + 41.7 × (BW/IBW) [ 3 ].
A 91-year-old woman with a 40-year history of diabetes mellitus gradually developed azotemia (blood urea nitrogen [BUN] 102 mg/dL) and uremia requiring emergency hemodialysis. Although she was mostly in a wheelchair due to geriatric frailty, uremia also deprived her of her activity and appetite (CCI, 6; SGA, C; GNRI, 72.0). Prior to hemodialysis initiation, her attending physician presented the best supportive care without any dialysis as terminal care. Informed consent was obtained from this patient and her family after explaining the risks and benefits of hemodialysis. Her fatigability and appetite improved after hemodialysis; a GNRI of 87.5 at 1 year indicated improvement in her nutritional condition. After 1 year, she often experienced vascular access failure that caused inadequate dialysis; thus, her condition gradually deteriorated. She lived for 2 years.
A 92-year-old man with an abdominal aortic aneurysm suddenly developed a re-rupture of aneurysm after endovascular aortic repair. Although he had dementia and needed supportive care from his family (CCI, 5; SGA, C; GNRI, 110.3), there was no history of renal dysfunction (BUN 13 mg/dL, eGFR 56 mL/min/1.73 m 2 ). An emergency stent was placed in the renal artery, which soon caused acute kidney injury (BUN 46 mg/dL with anuria). The patient, however, could not express his real willingness under such conditions; he could not refer to OPDG to decide his treatment. After several discussions between his family and medical staff about risks and benefits, hemodialysis was initiated under shared decision-making. These emergent operations saved his life temporarily, but sudden changes caused physical debilitation and reduced his physical activity level. Although vascular access was unproblematic, he eventually underwent percutaneous endoscopic gastrostomy after hemodialysis initiation; GNRI was 74.5 at 6 months. To ensure optimal supportive care, he was moved to a hospice 6 months after the emergency hemodialysis initiation.
A 94-year-old man with hypertension and decreased renal function due to nephrosclerosis was referred to our hospital for follow-up. His condition and options had been thoroughly discussed with the patient and his family during the preservation period. A vascular access was placed in the left wrist prior to hemodialysis. Subsequently, he was transferred to our emergency department due to azotemia (BUN 108.8 mg/dL) and severe uremia, which prompted hemodialysis after obtaining informed consent (CCI, 4; SGA, A; GNRI, 95.3). Even though he initially agreed to undergo dialysis, he became reluctant later on; fatigue and restriction while on dialysis caused psychological distress. Hemodialysis treatment prolonged his life for one and a half years without any cardiovascular problems, while hemodialysis was discontinued in deference to his wishes. Thereafter, he was admitted to a hospice to spend his remaining days under good supportive care.
A 90-year-old man with diabetes mellitus and drug-induced nephropathy exhibited a willingness to undergo hemodialysis through the creation of vascular access during the previous year, owing to a supportive family. He had a medical history of angina and laryngeal cancer for which he had received treatment. He had also undergone endovascular aortic repair for a common iliac artery aneurysm. This case was thoroughly discussed among the patient, his family, his attending physician, and other medical staff during the preservation period of renal failure. Hemodialysis was initiated when the BUN level reached 96.1 mg/dL, and he started exhibiting signs of uremia (CCI, 3; SGA, A; GNRI, 106.5). The patient is still alive and has been undergoing hemodialysis for two and a half years (present age, 93 years). He has good adherence to our medication, and eventually can undergo a well-managed dialysis regimen; he spends quality time with his family, who provide the best supportive care and are satisfied with his treatment. Hemodialysis initiation was suitable for this patient.
In this report, we described 4 patients aged over 90 years with different backgrounds who underwent hemodialysis. As the aging population increases, the number of oldest-old patients with end-stage renal disease (ESRD) will also increase. According to the Japanese Society for Dialysis Therapy, there were only 2 patients (0.005% of all patients) aged over 90 years on hemodialysis in 1982, increasing to 2.3% in 2018 [ 4 ]. Aside from Japan, several other countries are now facing the problem of an “aged society” [ 5 ]. Thus, it can be predicted that more oldest-old people with ESRD will undergo hemodialysis treatment.
Developments in medicine have made it possible to provide improved care to the oldest-old, thereby increasing their life expectancy, which was not possible earlier. They have also slowed the progression of chronic disease toward disability. Some reports have expressed criticism [ 6 ] regarding the initiation of hemodialysis in the hyper-aged society, citing the increased burden on healthcare, issues pertaining to cost-effectiveness [ 7 ], or ethics [ 8 ] as reasons. Factors such as malnutrition [ 3 ], low activities of daily living (ADL) [ 9 ], emergent initiation [ 10 ], or comorbidities [ 11 ] could contribute to vulnerable outcomes; such factors increase with age. In this regard, patients 3 and 4, who exhibited good ADL and nutritional status (SGA and GNRI) and no emergent initiation, revealed better outcomes. Patient 4, especially, is currently in good health and undergoing regular dialysis with the support of his family, suggesting that age should not be a barrier to hemodialysis initiation [ 12 ]. In contrast, patient 1 might have been too frail to undergo hemodialysis due to poor functional and nutritional status and the presence of comorbidities (high CCI). Such patients are unsuitable for hemodialysis in our experience. The most challenging case was that of patient 2. Such cases could generate controversy regarding the decision to initiate hemodialysis [ 8 ]. In contrast, patient 1 had poor ADL scores; though the BUN levels improved, the patient gradually became weak. All physicians should ensure that the rights of elderly people with ESRD regarding the potential benefits and risks of hemodialysis are respected through a shared decision-making process at the early treatment stage and the end of life [ 13 ], and their functional and nutritional status and comorbidities are considered prior to arriving at a decision [ 14 ]. There were no troubles in 3 cases while discussing with the patients' families and medical staff for initiation dialysis. Almost all cases were referred to OPDG to confirm their willingness. However, it was difficult to decide to start hemodialysis for the case 2 patient. Although initiation of hemodialysis is medically considered by nephrologists when one or more CKD symptoms are present, an aggressive trial of nondialytic management of advanced symptoms might be warranted depending on the patient's preferences and circumstances. Thus, patients and their families must be informed of conservative management options, such as supportive care and hospice care [ 15 ].
This study has some major limitations, such as a small study sample, unclear criteria for hemodialysis initiation, and the lack of objective data regarding sarcopenia or frailty. Further, more clinical data are required to determine the validity of hemodialysis initiation in oldest-old people and decide whether hemodialysis or supportive care is better for elderly patients with ESRD. This issue is difficult and remains controversial [ 15 ], though it may be beneficial to initiate hemodialysis in patients with good general health.
Appropriate treatment, along with strong family support, can greatly improve a patient's health and quality of life. Studies on hemodialysis initiation and supportive care have revealed heterogeneous results due to a paucity of survival data for supportive care patients [ 15 ]. Further studies are warranted to ensure whether elderly CKD patients should undergo hemodialysis and determine factors considered for initiation.
Statement of Ethics
This case report did not require an approval from the Osaka Medical and Pharmaceutical University Ethics Committee as the study did not include any invasive investigation or clinical trial. The case study conformed to the guidelines of the Declaration of Helsinki. Written informed consent was obtained from the patients for publication of this case series.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions
R.M. performed analyzed data and wrote the manuscript. T.M., Y.Y., S.T., and H.O. collected and analyzed data. H.U. and K.K. helped with the preparation of the manuscript. H.A. supervised the project, wrote, and edited the manuscript.
Data Availability Statement
Acknowledgments.
We would like to express our deepest gratitude to Dr. Maki Kagitani, Dr. Hajime Hirano, and Dr. Hayahito Nomi, Osaka Medical and Pharmaceutical University Hospital Blood Purification Center, for their discussions and insight. We also appreciate Yukiko Kusunoki and the staff working at the Blood Purification Center for their highly skilled management of the patients. Finally, we thank Editage ( www.editage.com ) for English language editing.

IMAGES
COMMENTS
The University of Minnesota Onsite Sewage Treatment Program assessed a residential septic system in Minnesota owned by a patient undergoing home hemodialysis treatment for kidney failure to evaluate the wastewater being generated by the household and determine whether the...
The University of Minnesota Onsite Sewage Treatment Program assessed a residential septic system in Minnesota owned by a patient undergoing home hemodialysis treatment for kidney failure to evaluate the wastewater being generated by the household and determine whether the... Please login or register to view Pumper articles. It's free, fast and ...
This case series study reported the results of seven patients who were transferred to expanded hemodialysis at home (HHDx), from December 2017 to March 2019, over a 12-month follow-up period. The AK-98 monitor and Theranova 400 membrane (Baxter International Inc., Deerfield, IL, USA) were used. The main outcome measures were blood analytical ...
In 2019, Fresenius Medical Care merged with another organization, NxStage, that brought additional expertise in delivering hemodialysis in patients' homes as well as access to new home-monitoring technology. This case study describes Fresenius Kidney Care's strategic and operational approaches to increasing the utilization of home dialysis.
Methods: In order to minimize a selection bias, we have compared the outcome of our HHD and CHD patients with a nested case-cohort study. For each patient trained for HHD at our dialysis centre between 1970 and 1995 (n=103), a corresponding match was searched from the CHD patients by retrospective chart analysis.
Home hemodialysis (HD) was developed in the 1960s in the USA and the UK, and by the early 1970s, 59% of patients on dialysis in the UK and 32% of patients in the USA received dialysis at home, mostly overnight hemodiaysis. 1 At this time, hospital dialysis was accessible to only a limited number of patients with end-stage kidney disease (ESKD).
Home hemodialysis (HHD) offers several clinical, quality of life and cost-saving benefits for patients with end-stage kidney disease. While uptake of this modality has increased in recent years, its prevalence remains low and high rates of discontinuation remain a challenge. This comprehensive narrative review aims to better understand what is ...
Staying in touch with your dialysis center. lysis center about oncea month for a check-up, lab tests, and to see your kidney doctor, nurse, dieti. ian, and social worker. You may also need to receive some of your medicines, such as intraveno. s iron, at your center. Between visits to the center, your healthcar.
In Australia, 12% of the hemodialysis population dialyze at home. Until recently, the majority of these patients dialyzed for similar hours to those in satellite dialysis. However, in the past 5 years there has been a new departure such that in many centers the concept of home hemodialysis is now synonymous with extended hours dialysis.
Studies & Observations of More Frequent Therapy. Residents performing home hemodialysis in a Skilled Nursing Facility more frequently - >3 days a week. - have shown better survival and hospitalization rate1.In addition, more frequent hemodialysis in the general population is associated with: Less Risk of Cardiac-Related Hospitalizations2.
Recognizing the clinical and economic advantages of home dialysis (both peritoneal dialysis and home hemodialysis), the federal government issued an executive order in 2019 (the Advancing American Kidney Health Initiative) to increase home dialysis and kidney transplantation use to 80% of new patients with kidney failure by 2025.
Published November 4, 2010. N Engl J Med 2010;363: 1833 - 1845. DOI: 10.1056/NEJMra0902710. VOL. 363 NO. 19. Fifty years ago, Belding Scribner and his colleagues at the University of Washington ...
Google Scholar. This study has identified a number of themes around community house hemodialysis that are similar to patients' experiences of home hemodialysis, including freedom and flexibility, avoiding facility hemodialysis, and gaining independence, control of health, and self-efficacy. 15. Walker R.C.
The patient initiated home CAPD after an abdominal catheter was placed and a sterile dialysis room was constructed in his home. As of the writing of this case report, the patient has performed CAPD four times per day for 3 years. ... case study from Guatemala. Kidney Int Rep 2017; 2:762-5. 10.1016/j.ekir.2017.02.020 [PMC free article] [Google ...
Abstract. Background/Aim: Home hemodialysis (HHD) has been associated with improved clinical outcomes vs. in-center HD (ICHD). The prevalence of HHD in the United States is still very low at 1.8%. This critical review compares HHD and ICHD outcomes for survival, hospitalization, cardiovascular (CV), nutrition, and quality of life (QoL). Methods: Of 545 publications identified, 44 were not ...
People on home hemodialysis are followed by a nephrologist who writes the dialysis prescription and they rely on the support of a dialysis unit for back-up treatments and case management. Studies show that HHD improves patients' sense of well-being; the more they know about and control their own treatment the better they are likely to do on ...
This study has identified a number of themes around community house hemodialysis that are similar to patients' experiences of home hemodialysis, including freedom and flexibility, avoiding facility hemodialysis, and gaining independence, control of health, and self-efficacy. 15, 20, 30 Additionally, we found that community house hemodialysis ...
In 2005, I began my home dialysis journey. I chose PD as my modality and thrived on it for 9yrs. In 2014, I was blessed by two angels on earth through the paired exchange program at John Hopkins, I received a kidney from a live donor with the help of my loving, selfless husband donating his kidney. However, in 2021, my transplanted kidney began ...
This case series study reported the results of seven patients who were transferred to expanded hemodialysis at home (HHDx), from December 2017 to March 2019, over a 12-month follow-up period. The AK-98 monitor and Theranova 400 membrane (Baxter International Inc., Deerfield, IL, USA) were used. The main outcome measures were blood analytical ...
The presented case report describes the rst experience at our workplace. with training and initiation of home hemodialysis in the timeline of a speci c patient. with chronic kidney disease. This ...
Study participants had a substantial prevalence of coexisting conditions similar to that in the overall population of patients in the United States undergoing hemodialysis. The study included a ...
In a retrospective cohort study of 202 patients on home HD, only six patients had suspected air embolism that occurred during 183,603 dialysis sessions for an overall incidence less than one episode per 30,000 dialysis sessions. ... Schematic diagram illustrating an approach to evaluation of a suspected case of hemolysis during hemodialysis (HD ...
As the aging population increases, the number of oldest-old patients with end-stage renal disease (ESRD) will also increase. According to the Japanese Society for Dialysis Therapy, there were only 2 patients (0.005% of all patients) aged over 90 years on hemodialysis in 1982, increasing to 2.3% in 2018 [ 4 ].