

Case Presentation: A 23-Year-Old With Bipolar Disorder
Gus Alva, MD, DFAPA, presents the case of a 23-year-old female diagnosed with bipolar 1 disorder.

EP: 1 . Case Presentation: A 23-Year-Old With Bipolar Disorder
Ep: 2 . clinical impressions from the patient case, ep: 3 . clinical insights regarding the management of bipolar disorder.
Gus Alva, MD, DFAPA: Psychiatric Times presents this roundtable on the management of bipolar disorder, a phenomenal dialogue allowing clinicals a perspective regarding current trends and where we may be headed in the future.
This is an interesting case, as we take a look at this 23-year-old female who first comes in to see her psychiatrist with moderate depressive symptoms. At the time of the interview, her chief complaint included feeling like she’s lacking energy, she’s feeling depressed. She’s also reporting difficulty in paying attention, organizing her day, and accomplishing her tasks at work. Notably these symptoms started abruptly. Three weeks early, prior to that, she had been functioning better than usual, requiring very little sleep and getting more accomplished. Of significance, she reported two brief episodes of depression over the past 2 years. Each lasting about 2 months. And although the patient reported these depressive episodes as coming out of the blue, she learned after consulting with her therapist that they were related to significant psychosocial stress, stemming from the loss of her job and the deaths of 2 uncles, both of which were related to the COVID-19 pandemic. The patient reported that she still finds enjoyment talking to friends and socializing and she has hope of finding a new job and she’s constantly looking.
It’s noteworthy to bear in mind that in her first depressive episode she was treated with methylphenidate 25mg titrated up to 50 m and she stated feeling improved on this does with psychotherapy. Her second depressive episode, her does was bumped up to 100 mg which we saw improvement in depression, but she noted she felt a little activated and had trouble sleeping. With her third depressive episode, the therapist and PCP referred the patient over to a psychiatrist. Of great note should be her past psychological history: she was diagnosed with ADHD in middle school, during which time she responded well to methylphenidate. She continued to do well until her college years at which time she began experiencing difficulty falling asleep as well as irritability. At that time, she discontinued methylphenidate and was psychiatric drug free. She found that practicing mindfulness and yoga on a daily basis helped her residual ADHD symptoms. Of note, she had no history of suicidal thoughts or behavior, self-injurious behaviors, psychiatric hospitalization, or problems with substance abuse. Of note, regarding medical comorbidities, she was diagnosed a year earlier with type 2 diabetes, which was managed with metformin 1000 mg twice daily and her hemoglobin A1C was not poorly controlled. She was also diagnosed with high blood pressure 2 years earlier, that is managed by lisinopril 20 mg once daily. We noted that her BMI is 31, which is indicative of obesity. All other lab values were within normal limit. Significantly, her TSH was in the normal range and her urine toxicology screening was negative. Upon further querying of her family history, her maternal grandmother was diagnosed with a nervous breakdown and spent 2 months in a psychiatric hospital in her 30s. Her mother required little sleep, had a history of impulsive spending, and had a history of starting projects that she didn’t finish. The patient’s paternal uncles had a history of depression as well as alcohol abuse. Upon doing assessments, her PHQ9 is indicative of 18 points and her mood questionnaire she scored an 8.
Transcript Edited for Clarity

Evaluating the Efficacy of Lumateperone for MDD and Bipolar Depression With Mixed Features

Blue Light Blockers: A Behavior Therapy for Mania

Efficacy of Modafinil for Treatment of Neurocognitive Impairment in Bipolar Disorder

Blue Light, Depression, and Bipolar Disorder

Securing the Future of Lithium Research

An Update on Early Intervention in Psychotic Disorders
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference
CASE STUDY Sarah (bipolar disorder)
Case study details.
Sarah is a 42-year-old married woman who has a long history of both depressive and hypomanic episodes. Across the years she has been variable diagnoses as having major depression, borderline personality disorder, and most recently, bipolar disorder. Review of symptoms indicates that she indeed have multiple episodes of depression beginning in her late teens, but that clear hypomanic episodes later emerged. Her elevated interpersonal conflict, hyper-sexuality and alcohol use during her hypomanic episodes led to the provisional borderline diagnosis, but in the context of her full history, bipolar disorder appears the best diagnosis. Sarah notes that she is not currently in a relationship and that she feels alienated from her family. She has been taking mood stabilizers for the last year, but continues to have low level symptoms of depression. In the past, she has gone off her medication multiple times, but at present she says she is “tired of being in trouble all the time” and wants to try individual psychotherapy.
- Alcohol Use
- Elevated Mood
- Impulsivity
- Mania/Hypomania
- Mood Cycles
- Risky Behaviors
Diagnoses and Related Treatments
1. bipolar disorder.
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
- Open access
- Published: 06 November 2018
The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research
- Eva F. Maassen ORCID: orcid.org/0000-0003-0211-0994 1 , 2 ,
- Barbara J. Regeer 1 ,
- Eline J. Regeer 2 ,
- Joske F. G. Bunders 1 &
- Ralph W. Kupka 2 , 3
International Journal of Bipolar Disorders volume 6 , Article number: 23 ( 2018 ) Cite this article
39k Accesses
19 Citations
21 Altmetric
Metrics details
In mental health care, clinical practice is often based on the best available research evidence. However, research findings are difficult to apply to clinical practice, resulting in an implementation gap. To bridge the gap between research and clinical practice, patients’ perspectives should be used in health care and research. This study aimed to understand the challenges people with bipolar disorder (BD) experience and examine what these challenges imply for health care and research needs.
Two qualitative studies were used, one to formulate research needs and another to formulate healthcare needs. In both studies focus group discussions were conducted with patients to explore their challenges in living with BD and associated needs, focusing on the themes diagnosis, treatment and recovery.
Patients’ needs are clustered in ‘disorder-specific’ and ‘generic’ needs. Specific needs concern preventing late or incorrect diagnosis, support in search for individualized treatment and supporting clinical, functional, social and personal recovery. Generic needs concern health professionals, communication and the healthcare system.
Patients with BD address disorder-specific and generic healthcare and research needs. This indicates that disorder-specific treatment guidelines address only in part the needs of patients in everyday clinical practice.
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007 ). According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014 ). The estimated lifetime prevalence of BD is 1.3% in the Dutch adult population (de Graaf et al. 2012 ), and BD is associated with high direct (health expenditure) and indirect (e.g. unemployment) costs (Fajutrao et al. 2009 ; Michalak et al. 2012 ), making it an important public health issue. In addition to the economic impact on society, BD has a tremendous impact on patients and their caregivers (Granek et al. 2016 ; Rusner et al. 2009 ). Even between mood episodes, BD is often associated with functional impairment (Van Der Voort et al. 2015 ; Strejilevich et al. 2013 ), such as occupational or psychosocial impairment (Huxley and Baldessarini 2007 ; MacQueen et al. 2001 ; Yasuyama et al. 2017 ). Apart from symptomatic recovery, treatment can help to overcome these impairments and so improve the person’s quality of life (IsHak et al. 2012 ).
Evidence Based Medicine (EBM), introduced in the early 1990s, is a prominent paradigm in modern (mental) health care. It strives to deliver health care based on the best available research evidence, integrated with individual clinical expertise (Sackett et al. 1996 ). EBM was introduced as a new paradigm to ‘de - emphasize intuition’ and ‘ unsystematic clinical experience’ (Guyatt et al. 1992 ) (p. 2420). Despite its popularity in principle (Barratt 2008 ), EBM has also been criticized. One such criticism is the ignorance of patients’ preferences and healthcare needs (Bensing 2000 ). A second criticism relates to the difficulty of adopting evidence-based treatment options in clinical practice (Bensing 2000 ), due to the fact that research outcomes measured in ‘the gold standard’ randomized-controlled trials (RCTs) seldom correspond to the outcomes clinical practice seeks and are not responsive to patients’ needs (Newnham and Page 2010 ). Moreover, EBM provides an overview on population level instead of individual level (Darlenski et al. 2010 ). Thus, adopting research evidence in clinical practice entails difficulties, resulting in an implementation gap.
To bridge the gap between research and clinical practice, it is argued that patients’ perspectives should be used in both health care and research. Patients have experiential knowledge about their illness, living with it in their personal context and their care needs (Tait 2005 ). This is valuable for both clinical practice and research as their knowledge complements that of health professionals and researchers (Tait 2005 ; Broerse et al. 2010 ; Caron-Flinterman et al. 2005 ). This source of knowledge can be used in the process of translating evidence into clinical practice (Schrevel 2015 ). Moreover, patient participation can enhance the clinical relevance of and support for research and the outcomes in practice (Abma and Broerse 2010 ). Hence, it is argued that these perspectives should be explicated and integrated into clinical guidelines, clinical practice, and research (Misak 2010 ; Rycroft-Malone et al. 2004 ).
Given the advantages of including patients’ perspectives, patients are increasingly involved in healthcare services (Bagchus et al. 2014 ; Larsson et al. 2007 ), healthcare quality (e.g. guideline development) (Pittens et al. 2013 ) and health-related research (e.g. agenda setting, research design) (Broerse et al. 2010 ; Boote et al. 2010 ; Elberse et al. 2012 ; Teunissen et al. 2011 ). However, patients’ perspectives on health care and on research are often studied separately. We argue that to be able to provide care focused on the patients and their needs, care and research must closely interact.
We hypothesize that the challenges BD patients experience and the associated care and research needs are interwoven, and that combining them would provide a more comprehensive understanding. We hypothesize that this more comprehensive understanding would help to close the gap between clinical practice and research. For this reason, this study aims to understand the challenges people with BD experience and examine what these challenges imply for healthcare and research needs.
To understand the challenges and needs of people with BD, we undertook two qualitative studies. The first aimed to formulate a research agenda for BD from a patient’s perspective, by gaining insights into their challenges and research needs. A second study yielded an understanding of the care needs from a patient’s perspective. In this article, the results of these two studies are combined in order to investigate the relationship between research needs and care needs. Challenges are defined as ‘difficulties patients face, due to having BD’. Care needs are defined as that what patients ‘desire to receive from healthcare services to improve overall health’ (Asadi-Lari et al. 2004 ) (p. 2). Research needs are defined as that what patients ‘desire to receive from research to improve overall health’.
Study on research needs
In this study, mixed-methods were used to formulate research needs from a patient’s perspective. First six focus group discussions (FGDs) with 35 patients were conducted to formulate challenges in living with BD and hopes for the future, and to formulate research needs arising from these difficulties and aspirations. These research needs were validated in a larger sample (n = 219) by means of a questionnaire. We have reported this study in detail elsewhere (Maassen et al. 2018 ).
Study on care needs
This study was part of a nationwide Dutch project to generate a practical guideline for BD: a translation of the existing clinical guideline to clinical practice, resulting in a standard of care that patients with BD could expect. The practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ) was written by a taskforce comprising health professionals, patients. In addition to the involvement of three BD patients in the taskforce, a systematic qualitative study was conducted to gain insight into the needs of a broader group of patients.
Participants and data collection
To formulate the care needs of people with BD, seven FGDs were conducted, with a total of 56 participants, including patients (n = 49) and caregivers (n = 9); some participants were both patient and caregiver. The inclusion criteria for patients were having been diagnosed with BD, aged 18 years or older and euthymic at time of the FGDs. Inclusion criteria for caregivers were caring for someone with BD and aged 18 years or older. To recruit participants, a maximum variation sampling strategy was used to collect a broad range of care needs (Kuper et al. 2008 ). First, all outpatient clinics specialized in BD affiliated with the Dutch Foundation for Bipolar Disorder (Dutch: Kenniscentrum Bipolaire Stoornissen) were contacted by means of an announcement at regular meetings and by email if they were interested to participate. From these outpatient clinics, patients were recruited by means of flyers and posters. Second, patients were recruited at a quarterly meeting of the Dutch patient and caregiver association for bipolar disorder. The FGDs were conducted between March and May 2016.
The FGDs were designed to address challenges experienced in BD health care and areas of improvement for health care for people with BD. The FGDs were structured by means of a guide and each session was facilitated by two moderators. The leading moderator was either BJR or EFM, having both extensive experience with FGD’s from previous studies. The first FGD explored a broad range of needs. The subsequent six FGDs aimed to gain a deeper understanding of these care needs, and were structured according to the outline of the practical guideline (Netwerk Kwaliteitsontwikkeling GGZ 2017 ). Three chapters were of particular interest: diagnosis, treatment and recovery. These themes were discussed in the FGDs, two in each session, all themes three times in total. Moreover, questions on specific aspects of care formulated by the members of the workgroup were posed. The sessions took 90–120 min. The FGDs were audiotaped and transcribed verbatim. A summary of the FGDs was sent to the participants for a member check.
Data analysis
To analyze the data on challenges and needs, a framework for thematic analysis to identify, analyze and report patterns (themes) in qualitative data sets by Braun and Clarke ( 2006 ) was used. First, we familiarized ourselves with the data by carefully reading the transcripts. Second, open coding was used to derive initial codes from the data. These codes were provided to quotes that reflected a certain challenge or care need. Third, we searched for patterns within the codes reflecting challenges and within those reflecting needs. For both challenges and needs, similar or overlapping codes were clustered into themes. Subsequently, all needs were categorized as ‘specific’ or ‘generic’. The former are specific to BD and the latter are relevant for a broad range of psychiatric illnesses. Finally, a causal analysis provided a clear understanding of how challenges related to each other and how they related to the described needs.
To analyze the data on needs regarding recovery, four domains were distinguished, namely clinical, functional, social and personal recovery (Lloyd et al. 2008 ; van der Stel 2015 ). Clinical recovery refers to symptomatic remission; functional recovery concerns recovery of functioning that is impaired due to the disorder, particularly in the domain of executive functions; social recovery concerns the improvement of the patient’s position in society; personal recovery concerns the ability of the patient to give meaning to what had happened and to get a grip on their own life. The analyses were discussed between BR and EM. The qualitative software program MAX QDA 11.1.2 was used (MaxQDA).
Ethical considerations
According to the Medical Ethical Committee of VU University Medical Center, the Medical Research Involving Human Subjects Act does not apply to the current study. All participants gave written or verbal informed consent regarding the aim of the study and for audiotaping and its use for analysis and scientific publications. Participation was voluntary and participants could withdraw from the study at any time. Anonymity was ensured.
This section is in three parts. The first presents the participants’ characteristics. The second presents the challenges BD patients face, derived from both studies, and the disorder-specific care and research needs associated with these challenges. The third part describes the generic care needs that patients formulated.
Characteristics of the participants
In the study on care needs, 56 patients and caregivers participated. The mean age of the participants was 52 years (24–75), of whom 67.8% were women. The groups varied from four to sixteen participants, and all groups included men and women. Of all participants 87.5% was diagnosed with BD, of whom 48.9% was diagnosed with BD I. 3.5% was both caregivers and diagnosed with BD. Of 4 patients the age was missing, and from 6 patients the bipolar subtype.
Despite the fact that participants acknowledge the inevitable diagnostic difficulties of a complex disorder like BD, in both studies they describe a range of challenges in different phases of the diagnostic process (Fig. 1 ). Patients explained that the general practitioner (GP) and society in general did not recognize early-warning signs and mood swings were not well interpreted, resulting in late or incorrect diagnosis. Patients formulated a need for more research on what early-warning signs could be and on how to improve GPs’ knowledge about BD. Formulated care needs were associated with GPs using this knowledge to recognize early-warning signs in individual patients. One participant explained that certain symptoms must be noticed and placed in the right context:
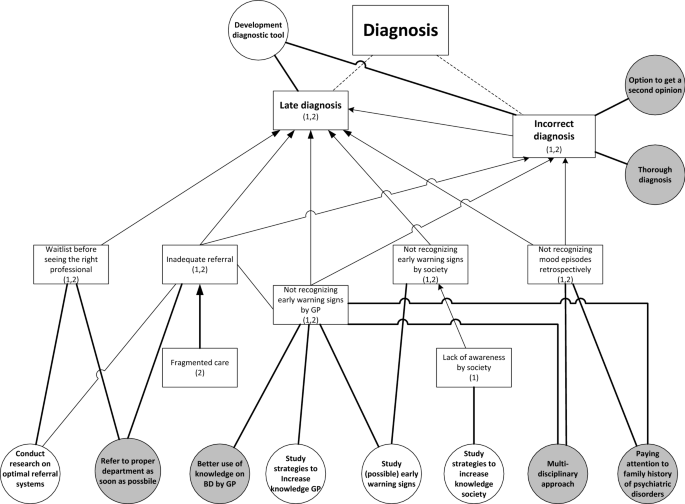
Challenges with diagnosis (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I call it, ‘testing overflow of ideas’. [….] When it happens for the first time you yourself do not recognize it. Someone else close to you or the health professional, who is often not involved yet, must signal it. (FG6)
Moreover, these challenges are associated with the need to pay attention to family history and to use a multidisciplinary approach to diagnosis to benefit from multiple perspectives. The untimely recognition of early symptoms also results in another challenge: inadequate referral to the right specialized health professional. After referral, people often face a waiting list, again causing delay in the diagnostic process. These challenges result in the need for research on optimal referral systems and the care need for timely referral. One participant described her process after the GP decided to refer her:
But, yes, at that moment the communication wasn’t good at all. Because the general practitioner said: ‘she urgently has to be seen by someone’. Subsequently, three weeks went by, until I finally arrived at depression [department]. And at that department they said: ‘well, you are in the wrong place, you need to go to bipolar [department ]’. (FG1)
The challenge of being misdiagnosed is associated with the need to be able to ask for a second opinion and to have a timely and thorough diagnosis. On the one hand, it is important for patients that health professionals quickly understand what is going on, on the other hand that health professionals take the time to thoroughly investigate the symptoms by making several appointments.
From both studies, two main challenges related to the treatment of BD were derived (Fig. 2 ). The first is finding appropriate and satisfactory treatment. Participants explained that it is difficult to find the right medication and dosage that is effective and has acceptable side-effects. One participant illustrates:
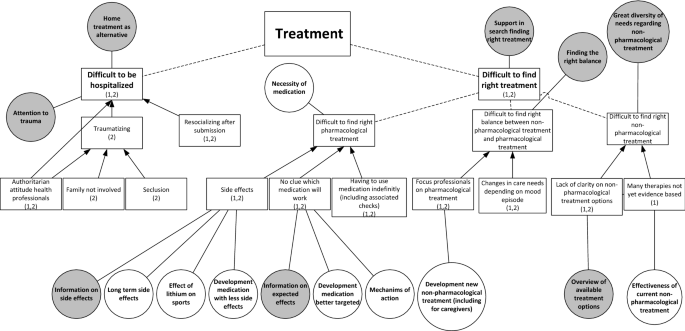
Challenges with treatment (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
I think, at one point, we have to choose, either overweight or depressed. (FG1)
Some participants said that they struggle with having to use medication indefinitely, including the associated medical checks. The difficult search for the right pharmacological treatment results in the need for research on long-term side-effects, on the mechanism of action of medicine and on the development of better targeted medication with fewer adverse side-effects. In care, patients would appreciate all the known information on the side-effects and intended effects. One participant explained the importance of being properly informed about medication:
I don’t read anything [about medication], because then I wouldn’t dare taking it. But I do think, when you explain it well, the advantages, the disadvantages, the treatment, the idea behind it, that would help a lot in compliance. (FG1)
A second aspect is the challenge of finding non-pharmacological therapies that fit patients’ needs. They said they and the health professionals often do not know which non-pharmacological therapies are available and effective:
But we found the carefarm ourselves Footnote 1 [….]. You have to search for yourself completely. Yes, I actually hoped that that would be presented to you, like: ‘this would be something for you’. (FG3)
Participants mentioned a variety of non-pharmacological therapies they found useful, namely cognitive behavior therapy (CBT), EMDR, running therapy, social-rhythm training, light therapy, mindfulness, psychotherapy, psychoeducation, and training in living with mood swings. They formulated the care need to receive an overview of all available treatment options in order to find a treatment best suited to their needs. They would appreciate research on the effectiveness of non-pharmacological treatments.
A third aspect within this challenge is finding the right balance between non-pharmacological and pharmacological treatment. Participants differed in their opinion about the need for medication. Whereas some participants stated that they need medication to function, others pointed out that they found non-pharmacological treatments effective, resulting in less or no medication use. They explained that the preferred balance can also change over time, depending on their mood. However, they experience a dominant focus on pharmacological treatment by the health professionals. To address this challenge, patients need support in searching for an appropriate balance.
Next to the challenge of finding appropriate and satisfactory treatment, a second treatment-related challenge is hospitalization. Participants often had a traumatic experience, due to seclusion, the authoritarian attitudes of clinical staff, and not involving their family. Patients therefore found it important to try preventing being hospitalized, for example by means of home treatment, which some participants experienced positively. Despite the challenges relating to hospitalization, participants did acknowledge that in some cases it cannot be avoided, in which case they urged for close family involvement, open communication and being treated by their own psychiatrist. Still, in the study on research needs, hospitalization did not emerge as an important research theme.
In both studies, participants described challenges in all four domains of recovery: clinical, functional, social and personal (Fig. 3 ). In relation to clinical recovery, participants struggled with the symptoms of mood episodes, the psychosis and the fear of a future episode. In contrast, some participants mentioned that they sometimes miss the hypomanic state they had experienced previously due to effective medical treatment. In the domain of functional recovery, participants contended with having to function below their educational level due to residual symptoms, such as cognitive problems, due to the importance of preventing stress in order to reduce the risk of a new episode, and because of low energy levels. This leads to the care need that health professionals should pay attention to the level of functioning of their patients.
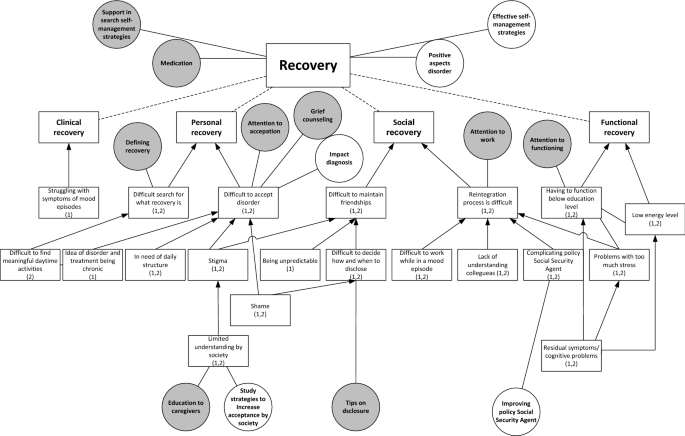
Challenges with recovery (squares) including relating research needs (white circles) and care needs (grey circles). (1): mentioned in study on research needs; (2): mentioned in study on care needs. Dotted lines: division of challenges into sub challenges. Arrows: causal relation between challenges
In the domain of social recovery, participants described challenges with maintaining friendships, due to stigma, being unpredictable and with deciding when to disclose the disorder. The latter resulted in the care need for tips on disclosure. Moreover, patients experienced challenges with reintegration to work, due to colleagues’ lack of understanding, problems with functioning during an episode, the complicating policy of the (Dutch) Employee Insurance Agency Footnote 2 in relation to the fluctuating course of BD and the negative impact of stress. These challenges are associated with the care need that health professionals should pay attention to work and the need for research on how to improve the Social Security Agency’s policy.
For their personal recovery, participants struggled with acceptance of the disorder, due to shame, stigma, having to live by structured rules and disciplines, and the chronic nature of BD. This results in care needs for grief counselling and attention to acceptance and the need for research on the impact of being diagnosed with BD. Limited understanding within society also causes problems with acceptance, corresponding with the care need for education for caregivers and for research on how to increase social acceptance. Another challenge in personal recovery was discovering what recovery means and what constitute meaningful daily activities. Patients appreciated the support of health professionals in this area. One participant described the difficult search for the meaning of recovery:
I have been looking to recover towards the situation [before diagnosis] for a long time; that I could do what I always did and what I liked. But then I was confronted with the fact that I shouldn’t expect that to happen, or only with a lot of effort. (…) Then you start thinking, now what? A compromise. I don’t want to call that recovery, but it is a recovered, partly accepted, situation. But it is not recovery as I expected it to be. (FG5)
In general, participants considered frequent contact with a nurse or psychiatrist supportive, to help them monitor their mood and help them find (efficient) self-management strategies. Most participants appreciated the involvement of caregivers in the treatment and contact with peers.
Generic care needs
We have described BD-specific needs, but patients mentioned also mentioned several generic care needs. The latter are clustered into three categories. The first concerns the health professionals . Participants stressed the importance of a good health professional, who carefully listens, takes time, and makes them feel understood, resulting in a sense of connection. Furthermore, a good health professional treats beyond the guideline, and focuses on the needs of the individual patient. When there is no sense of connection, it should be possible to change to another health professional. The second category concerns communication between the patient and the health professional . Health professionals should communicate in an open, honest and clear way both in the early diagnostic phase and during treatment. Open communication facilitates individualized care, in which the patient is involved in decision making. In addition, participants wanted to be treated as a person, not as a patient, and according to a strength-based approach. The third category concerns needs at the level of the healthcare system . Participants struggled with the availability of the health professionals and preferred access to good care 24/7 and being able to contact their health professional quickly when necessary. Currently, according to the participants, the care system is not geared to the mood swings of BD, because patients often faced waiting lists before they could see a health professional.
Is adequate treatment also having a number from a mental health institution you can always call when you are in need, that you can go there? And not that you can go in three weeks, but on a really short notice. So at least a phone call. (FG3)
Participants were often frustrated by the limited collaboration between health professionals, within their own team, between departments of the organization, and between different organizations, including complementary health professionals. They would appreciate being able to merge their conventional and complementary treatment, with greater collaboration among the different health professionals. Furthermore, they would like continuity of health professionals as this improves both the diagnostic phase and treatment, and because that health professional gets to know the patient.
We hypothesized that research and care needs of patients are closely intertwined and that understanding these, by explicating patients’ perspectives, could contribute to closing the gap between research and care. Therefore, this study aimed to understand the challenges patients with BD face and examine what these imply for both healthcare and research. In the study on needs for research and in the study on care needs, patients formulated challenges relating to receiving the correct diagnosis, finding the right treatment, including the proper balance between non-pharmacological and pharmacological treatment, and to their individual search for clinical, functional, social and personal recovery. The formulated needs in both studies clearly reflected these challenges, leading to closely corresponding needs. Another important finding of our study is that patients not only formulate disorder-specific needs, but also many generic needs.
The needs found in our study are in line with the current literature on the needs of patients with BD, namely for more non-pharmacological treatment (Malmström et al. 2016 ; Nestsiarovich et al. 2017 ), timely recognition of early-warning signs and self-management strategies to prevent a new episode (Goossens et al. 2014 ), better information on treatment and treatment alternatives (Malmström et al. 2016 ; Neogi et al. 2016 ) and coping with grief (Goossens et al. 2014 ). Moreover, the need for frequent contact with health professionals, being listened to, receiving enough time, shared decision-making on pharmacological treatment, involving caregivers (Malmström et al. 2016 ; Fisher et al. 2017 ; Skelly et al. 2013 ), and the urge for better access to health care and continuity of health professionals (Nestsiarovich et al. 2017 ; Skelly et al. 2013 ) are confirmed by the literature. Our study added to this set of literature by providing insights in patients’ needs in the diagnostic process and illustrating the interrelation between research needs and care needs from a patient’s perspective.
The generic healthcare needs patients addressed in this study are clustered into three categories: the health professional , communication between the patient and the health professional and the health system. These categories all fit in a model of patient-centered care (PCC) by Maassen et al. ( 2016 ) In their review, patients’ perspectives on good care are compared with academic perspectives of PCC and a model of PCC is created comprising four dimensions: patient, health professional, patient – professional interaction and healthcare organization. All the generic needs formulated in this study fit into these four dimensions. The need to be treated as a person with strengths fits the dimension ‘patient’, and the need for a good health professional who carefully listens, takes time and makes them feel understood, resulting in a good connection with the professional, fits the dimension ‘health professional’ of this model. Furthermore, patients in this study stressed the importance of open communication in order to provide individualized care, which fits the dimension of ‘patient–professional interaction’. The urge for better access to health care, geared to patients’ mood swings and the need for better collaboration between health professionals and continuity of health professionals fits the dimension of ‘health care organization’ of the model. This study confirms the findings from the review and contributes to the literature stressing the importance of a patient-centered care approach (Mills et al. 2014 ; Scholl et al. 2014 ).
In the prevailing healthcare paradigm, EBM, the best available evidence should guide treatment of patients (Sackett et al. 1996 ; Darlenski et al. 2010 ). This evidence is translated into clinical and practical guidelines, which thus facilitate EBM and could be used as a decision-making tool in clinical practice (Skelly et al. 2013 ). For many psychiatric disorders, treatment is based on such disorder - specific clinical and practical guidelines. However, this disease-focused healthcare system has contributed to its fragmented nature Stange ( 2009 ) argues that this fragmented care system has expanded without the corresponding ability to integrate and personalize accordingly. We argue that acknowledging that disorder - specific clinical and practical guidelines address only parts of the care needs is of major importance, since otherwise important aspects of the patients’ needs will be ignored. Because there is an increasing acknowledgement that health care should be responsive to the needs of patients and should change from being disease-focused towards being patient-focused (Mead and Bower 2000 ; Sidani and Fox 2014 ), currently in the Netherlands generic practical guidelines are written on specific care themes (e.g. co-morbidity, side-effects, daily activity and participation). These generic practical guidelines address some of the generic needs formulated by the patients in our study. We argue that in addition to disorder-specific guidelines, these generic practical guidelines should increasingly be integrated into clinical practice, while health professionals should continuously be sensitive to other emerging needs. We believe that an integration of a disorder-centered and a patient-centered focus is essential to address all needs a patient.
Strengths, limitations and future research
This study has several strengths. First, it contributes to the literature on the challenges and needs of patients with BD. Second, the study is conducted from a patient’s perspective. Moreover, addressing this aim by conducting two separate studies enabled us to triangulate the data.
This study also has several limitations. First, this study reflects the challenges, care needs and research needs of Dutch patient with BD and caregivers. Despite the fact that a maximum variation sampling strategy was used to derive a broad range of challenges and needs throughout the Netherlands, the Dutch setting of the study may limit the transferability to other countries. To understand the overlap and differences between countries, similar research should be conducted in other contexts. Second, given the design of the study, we could not differentiate between patients and caregivers since they participated together in the FGDs. More patients than caregivers participated in the study. For a more in-depth understanding of the challenges and needs faced by caregivers, in future research separate FGDs should be conducted. Third, due to the fixed outline of the practical guideline used to conduct the FGDs, only the healthcare needs for diagnosis, treatment and recovery of BD are studied. Despite the fact that these themes might cover a broad range of health care, it could have resulted in overlooking certain needs in related areas of well-being. Therefore, future research should focus on needs outside of these themes in order to provide a complete set of healthcare needs.
Patients and their caregivers face many challenges in living with BD. Our study contributes to the literature on care and research needs from a patient perspective. Needs specific for BD are preventing late or incorrect diagnosis, support in search for individualized treatment, and supporting clinical, functional, social and personal recovery. Generic healthcare needs concern health professionals, communication and the healthcare system. This explication of both disorder-specific and generic needs indicates that clinical practice guidelines should address and integrate both in order to be responsive to the needs of patients and their caregivers.
Care farm: farms that combine agriculture and services for people with disabilities (Iancu 2013 ). These farms are used as interventions in mental care throughout Europe and the USA to facilitate recovery (Iancu et al. 2014 ).
A government agency involved in the implementation of employee insurance and providing labor market and data services.
Abma T, Broerse J. Patient participation as dialogue: setting research agendas. Health Expect. 2010;13(2):160–73.
Article Google Scholar
APA. Beknopt overzicht van de criteria (DSM-5). Nederlands vertaling van de Desk Reference to the Diagnostic Criteria from DSM-5. Amsterdam: Boom; 2014.
Google Scholar
Asadi-Lari M, Tamburini M, Gray D. Patients’ needs, satisfaction, and health related quality of life: towards a comprehensive model. Health Qual Life Outcomes. 2004;2:1–15.
Bagchus C, Dedding C, Bunders JFG. “I”m happy that I can still walk’—participation of the elderly in home care as a specific group with specific needs and wishes. Health Expect. 2014;18(6):1–9.
Barratt A. Evidence based medicine and shared decision making: the challenge of getting both evidence and preferences into health care. Patient Educ Couns. 2008;73(3):407–12.
Bensing J. Bridging the gap. The separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000;39:17–25.
Article CAS Google Scholar
Boote J, Baird W, Beecroft C. Public involvement at the design stage of primary health research: a narrative review of case examples. Health Policy. 2010;95(1):10–23.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Broerse J, Zweekhorst M, van Rensen A, de Haan M. Involving burn survivors in agenda setting on burn research: an added value? Burns. 2010;36(2):217–31.
Caron-Flinterman JF, Broerse JEW, Bunders JFG. The experiential knowledge of patients: a new resource for biomedical research? Soc Sci Med. 2005;60(11):2575–84.
Darlenski RB, Neykov NV, Vlahov VD, Tsankov NK. Evidence-based medicine: facts and controversies. Clin Dermatol. 2010;28(5):553–7.
de Graaf R, ten Have M, van Gool C, van Dorsselaer S. Prevalence of mental disorders and trends from 1996 to 2009. Results from the Netherlands Mental Health Survey and Incidence Study-2. Soc Psychiatry Psychiatr Epidemiol. 2012;47(2):203–13.
Elberse J, Pittens C, de Cock Buning T, Broerse J. Patient involvement in a scientific advisory process: setting the research agenda for medical products. Health Policy. 2012;107(2–3):231–42.
Fajutrao L, Locklear J, Priaulx J, Heyes A. A systematic review of the evidence of the burden of bipolar disorder in Europe. Clin Pract Epidemiol Ment Health. 2009;5(1):3.
Fisher A, Manicavasagar V, Sharpe L, Laidsaar-Powell R, Juraskova I. A qualitative exploration of patient and family views and experiences of treatment decision-making in bipolar II disorder. J Ment Health. 2017;27(1):66–79.
Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorder and recurrent depression. 2nd ed. New York: Oxford University Press; 2007.
Goossens P, Knoopert-van der Klein E, Kroon H, Achterberg T. Self reported care needs of outpatients with a bipolar disorder in the Netherlands: a quantitative study. J Psychiatr Ment Health Nurs. 2014;14:549–57.
Granek L, Danan D, Bersudsky Y, Osher Y. Living with bipolar disorder: the impact on patients, spouses, and their marital relationship. Bipolar Disord. 2016;18(2):192–9.
Guyatt G, Cairns J, Churchill D, Cook D, Haynes B, Hirsh J, Irvine J, Levine M, Levine M, Nishikawa J, Sackett D, Brill-Edwards P, Gerstein H, Gibson J, Jaeschke R, Kerigan A, Neville A, Panju A, Detsky A, Enkin M, Frid P, Gerrity M, Laupacis A, Lawrence V, Menard J, Moyer V, Mulrow C, Links P, Oxman A, Sinclair J, Tugwell P. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992;268(17):2420–5.
Huxley N, Baldessarini R. Disability and its treatment in bipolar disorder patients. Bipolar Disord. 2007;9(1–2):183–96.
Iancu SC. New dynamics in mental health recovery and rehabilitation. Amsterdam: Vu University; 2013.
Iancu SC, Zweekhorst MBM, Veltman DJ, Van Balkom AJLM, Bunders JFG. Mental health recovery on care farms and day centres: a qualitative comparative study of users’ perspectives. Disabil Rehabil. 2014;36(7):573–83.
IsHak WW, Brown K, Aye SS, Kahloon M, Mobaraki S, Hanna R. Health-related quality of life in bipolar disorder. Bipolar Disord. 2012;14(1):6–18.
Kuper A, Lingard L, Levinson W. Critically appraising qualitative research. BMJ. 2008;337(7671):687–9.
Larsson IE, Sahlsten MJM, Sjöström B, Lindencrona CSC, Plos KAE. Patient participation in nursing care from a patient perspective: a grounded theory study. Scand J Caring Sci. 2007;21(3):313–20.
Lloyd C, Waghorn G, Williams PL. Conceptualising recovery in mental health. Br J Occup Ther. 2008;71:321–8.
Maassen EF, Schrevel SJC, Dedding CWM, Broerse JEW, Regeer BJ. Comparing patients’ perspectives of “good care” in Dutch outpatient psychiatric services with academic perspectives of patient-centred care. J Ment Health. 2016;26(1):1–11.
Maassen EF, Regeer BJ, Bunders JGF, Regeer EJ, Kupka RW. A research agenda for bipolar disorder developed from a patient’s perspective. J Affect Disord. 2018;239:11–17. https://doi.org/10.1016/j.jad.2018.05.061 .
Article PubMed Google Scholar
MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001;103(3):163–70.
Malmström E, Hörberg N, Kouros I, Haglund K, Ramklint M. Young patients’ views about provided psychiatric care. Nord J Psychiatry. 2016;70(7):521–7.
MaxQDA [Internet]. Available from: https://www.maxqda.com/ . Accessed 2 Aug 2018.
Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51(7):1087–110.
Michalak EE, Hole R, Livingston JD, Murray G, Parikh SV, Lapsley S, et al. Improving care and wellness in bipolar disorder: origins, evolution and future directions of a collaborative knowledge exchange network. Int J Ment Health Syst. 2012;6:16.
Mills I, Frost J, Cooper C, Moles DR, Kay E. Patient-centred care in general dental practice—a systematic review of the literature. BMC Oral Health. 2014;14(1):64.
Misak CJ. Narrative evidence and evidence-based medicine. J Eval Clin Pract. 2010;16(2):392–7.
Neogi R, Chakrabarti S, Grover S. Health-care needs of remitted patients with bipolar disorder: a comparison with schizophrenia. World J Psychiatry. 2016;6(4):431–41.
Nestsiarovich A, Hurwitz NG, Nelson SJ, Crisanti AS, Kerner B, Kuntz MJ, et al. Systemic challenges in bipolar disorder management: a patient-centered approach. Bipolar Disord. 2017;19(8):676–88.
Netwerk Kwaliteitsontwikkeling GGZ. Zorgstandaard Bipolaire stoornissen. 2017;1–54.
Newnham EA, Page AC. Bridging the gap between best evidence and best practice in mental health. Clin Psychol Rev. 2010;30(1):127–42.
Pittens C, Noordegraaf A, van Veen S, Broerse J. The involvement of gynaecological patients in the development of a clinical guideline for resumption of (work) activities in the Netherlands. Health Expect. 2013;18:1397–412.
Rusner M, Carlsson G, Brunt D, Nyström M. Extra dimensions in all aspects of life—the meaning of life with bipolar disorder. Int J Qual Stud Health Well-being. 2009;4(3):159–69.
Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs. 2004;47(1):81–90.
Sackett D, Rosenberg W, Gray J, Haynes R, Richardson W. Evidence based medicine: what it is and what it isn’t. Br Med J. 1996;312(7023):71–2.
Scholl I, Zill JM, Härter M, Dirmaier J. An integrative model of patient-centeredness—a systematic review and concept analysis. PLoS ONE. 2014;9(9):e107828.
Schrevel SJC. Surrounded by controversy: perspectives of adults with ADHD and health professionals on mental healthcare. Amsterdam: VU University; 2015.
Sidani S, Fox M. Patient-centered care: clarification of its specific elements to facilitate interprofessional care. J Interprof Care. 2014;28(2):134–41.
Skelly N, Schnittger RI, Butterly L, Frorath C, Morgan C, McLoughlin DM, et al. Quality of care in psychosis and bipolar disorder from the service user perspective. Qual Health Res. 2013;23(12):1672–85.
Stange KC. The problem of fragmentation and the need for integrative solutions. Ann Fam Med. 2009;7(2):100–3.
Strejilevich SA, Martino DJ, Murru A, Teitelbaum J, Fassi G, Marengo E, et al. Mood instability and functional recovery in bipolar disorders. Acta Psychiatr Scand. 2013;128(3):194–202.
Tait L. Encouraging user involvement in mental health services. Adv Psychiatr Treat. 2005;11(3):168–75.
Teunissen T, Visse M, De Boer P, Abma TA. Patient issues in health research and quality of care: an inventory and data synthesis. Health Expect. 2011;16:308–22.
van der Stel. Het begrip herstel in de psychische gezondheidzorg, Leiden; 2015. p. 1–3.
Van Der Voort TYG, Van Meijel B, Hoogendoorn AW, Goossens PJJ, Beekman ATF, Kupka RW. Collaborative care for patients with bipolar disorder: effects on functioning and quality of life. J Affect Disord. 2015;179:14–22.
Yasuyama T, Ohi K, Shimada T, Uehara T, Kawasaki Y. Differences in social functioning among patients with major psychiatric disorders: interpersonal communication is impaired in patients with schizophrenia and correlates with an increase in schizotypal traits. Psychiatry Res. 2017;249:30–4.
Download references
Authors’ contributions
EFM designed the study, contributed to the data collection, managed the analysis and wrote the first draft of the manuscript. BJR designed the study and contributed to the data collection, data analysis, and writing of the manuscript. JFGB contributed to the study design and critical revision of the manuscript. EJR contributed to the study conception and critical revision of the manuscript. RWK contributed to the study design, acquisition of data, and critical revision of the manuscript. All authors contributed to the final manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
The authors received no financial support for the research.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Athena Institute, Faculty of Earth and Life Sciences, VU University Amsterdam, Boelelaan 1085, 1081HV, Amsterdam, Netherlands
Eva F. Maassen, Barbara J. Regeer & Joske F. G. Bunders
Altrecht Institute for Mental Health Care, Nieuwe Houtenseweg 12, 3524 SH, Utrecht, Netherlands
Eva F. Maassen, Eline J. Regeer & Ralph W. Kupka
Amsterdam Public Health Research Institute, Amsterdam UMC, Vrije Universiteit Amsterdam, Psychiatry, De Boelelaan 1117, Amsterdam, Netherlands
Ralph W. Kupka
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Eva F. Maassen .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Maassen, E.F., Regeer, B.J., Regeer, E.J. et al. The challenges of living with bipolar disorder: a qualitative study of the implications for health care and research. Int J Bipolar Disord 6 , 23 (2018). https://doi.org/10.1186/s40345-018-0131-y
Download citation
Received : 06 June 2018
Accepted : 22 August 2018
Published : 06 November 2018
DOI : https://doi.org/10.1186/s40345-018-0131-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- General Healthcare
- Personal Recovery
- Focus Group Discussions
- Professional-patient Interaction
- Search Menu
Sign in through your institution
- Browse content in Arts and Humanities
- Browse content in Archaeology
- Anglo-Saxon and Medieval Archaeology
- Archaeological Methodology and Techniques
- Archaeology by Region
- Archaeology of Religion
- Archaeology of Trade and Exchange
- Biblical Archaeology
- Contemporary and Public Archaeology
- Environmental Archaeology
- Historical Archaeology
- History and Theory of Archaeology
- Industrial Archaeology
- Landscape Archaeology
- Mortuary Archaeology
- Prehistoric Archaeology
- Underwater Archaeology
- Zooarchaeology
- Browse content in Architecture
- Architectural Structure and Design
- History of Architecture
- Residential and Domestic Buildings
- Theory of Architecture
- Browse content in Art
- Art Subjects and Themes
- History of Art
- Industrial and Commercial Art
- Theory of Art
- Biographical Studies
- Byzantine Studies
- Browse content in Classical Studies
- Classical History
- Classical Philosophy
- Classical Mythology
- Classical Numismatics
- Classical Literature
- Classical Reception
- Classical Art and Architecture
- Classical Oratory and Rhetoric
- Greek and Roman Epigraphy
- Greek and Roman Law
- Greek and Roman Papyrology
- Greek and Roman Archaeology
- Late Antiquity
- Religion in the Ancient World
- Social History
- Digital Humanities
- Browse content in History
- Colonialism and Imperialism
- Diplomatic History
- Environmental History
- Genealogy, Heraldry, Names, and Honours
- Genocide and Ethnic Cleansing
- Historical Geography
- History by Period
- History of Emotions
- History of Agriculture
- History of Education
- History of Gender and Sexuality
- Industrial History
- Intellectual History
- International History
- Labour History
- Legal and Constitutional History
- Local and Family History
- Maritime History
- Military History
- National Liberation and Post-Colonialism
- Oral History
- Political History
- Public History
- Regional and National History
- Revolutions and Rebellions
- Slavery and Abolition of Slavery
- Social and Cultural History
- Theory, Methods, and Historiography
- Urban History
- World History
- Browse content in Language Teaching and Learning
- Language Learning (Specific Skills)
- Language Teaching Theory and Methods
- Browse content in Linguistics
- Applied Linguistics
- Cognitive Linguistics
- Computational Linguistics
- Forensic Linguistics
- Grammar, Syntax and Morphology
- Historical and Diachronic Linguistics
- History of English
- Language Acquisition
- Language Evolution
- Language Reference
- Language Variation
- Language Families
- Lexicography
- Linguistic Anthropology
- Linguistic Theories
- Linguistic Typology
- Phonetics and Phonology
- Psycholinguistics
- Sociolinguistics
- Translation and Interpretation
- Writing Systems
- Browse content in Literature
- Bibliography
- Children's Literature Studies
- Literary Studies (Asian)
- Literary Studies (European)
- Literary Studies (Eco-criticism)
- Literary Studies (Romanticism)
- Literary Studies (American)
- Literary Studies (Modernism)
- Literary Studies - World
- Literary Studies (1500 to 1800)
- Literary Studies (19th Century)
- Literary Studies (20th Century onwards)
- Literary Studies (African American Literature)
- Literary Studies (British and Irish)
- Literary Studies (Early and Medieval)
- Literary Studies (Fiction, Novelists, and Prose Writers)
- Literary Studies (Gender Studies)
- Literary Studies (Graphic Novels)
- Literary Studies (History of the Book)
- Literary Studies (Plays and Playwrights)
- Literary Studies (Poetry and Poets)
- Literary Studies (Postcolonial Literature)
- Literary Studies (Queer Studies)
- Literary Studies (Science Fiction)
- Literary Studies (Travel Literature)
- Literary Studies (War Literature)
- Literary Studies (Women's Writing)
- Literary Theory and Cultural Studies
- Mythology and Folklore
- Shakespeare Studies and Criticism
- Browse content in Media Studies
- Browse content in Music
- Applied Music
- Dance and Music
- Ethics in Music
- Ethnomusicology
- Gender and Sexuality in Music
- Medicine and Music
- Music Cultures
- Music and Religion
- Music and Media
- Music and Culture
- Music Education and Pedagogy
- Music Theory and Analysis
- Musical Scores, Lyrics, and Libretti
- Musical Structures, Styles, and Techniques
- Musicology and Music History
- Performance Practice and Studies
- Race and Ethnicity in Music
- Sound Studies
- Browse content in Performing Arts
- Browse content in Philosophy
- Aesthetics and Philosophy of Art
- Epistemology
- Feminist Philosophy
- History of Western Philosophy
- Metaphysics
- Moral Philosophy
- Non-Western Philosophy
- Philosophy of Science
- Philosophy of Language
- Philosophy of Mind
- Philosophy of Perception
- Philosophy of Action
- Philosophy of Law
- Philosophy of Religion
- Philosophy of Mathematics and Logic
- Practical Ethics
- Social and Political Philosophy
- Browse content in Religion
- Biblical Studies
- Christianity
- East Asian Religions
- History of Religion
- Judaism and Jewish Studies
- Qumran Studies
- Religion and Education
- Religion and Health
- Religion and Politics
- Religion and Science
- Religion and Law
- Religion and Art, Literature, and Music
- Religious Studies
- Browse content in Society and Culture
- Cookery, Food, and Drink
- Cultural Studies
- Customs and Traditions
- Ethical Issues and Debates
- Hobbies, Games, Arts and Crafts
- Natural world, Country Life, and Pets
- Popular Beliefs and Controversial Knowledge
- Sports and Outdoor Recreation
- Technology and Society
- Travel and Holiday
- Visual Culture
- Browse content in Law
- Arbitration
- Browse content in Company and Commercial Law
- Commercial Law
- Company Law
- Browse content in Comparative Law
- Systems of Law
- Competition Law
- Browse content in Constitutional and Administrative Law
- Government Powers
- Judicial Review
- Local Government Law
- Military and Defence Law
- Parliamentary and Legislative Practice
- Construction Law
- Contract Law
- Browse content in Criminal Law
- Criminal Procedure
- Criminal Evidence Law
- Sentencing and Punishment
- Employment and Labour Law
- Environment and Energy Law
- Browse content in Financial Law
- Banking Law
- Insolvency Law
- History of Law
- Human Rights and Immigration
- Intellectual Property Law
- Browse content in International Law
- Private International Law and Conflict of Laws
- Public International Law
- IT and Communications Law
- Jurisprudence and Philosophy of Law
- Law and Politics
- Law and Society
- Browse content in Legal System and Practice
- Courts and Procedure
- Legal Skills and Practice
- Primary Sources of Law
- Regulation of Legal Profession
- Medical and Healthcare Law
- Browse content in Policing
- Criminal Investigation and Detection
- Police and Security Services
- Police Procedure and Law
- Police Regional Planning
- Browse content in Property Law
- Personal Property Law
- Study and Revision
- Terrorism and National Security Law
- Browse content in Trusts Law
- Wills and Probate or Succession
- Browse content in Medicine and Health
- Browse content in Allied Health Professions
- Arts Therapies
- Clinical Science
- Dietetics and Nutrition
- Occupational Therapy
- Operating Department Practice
- Physiotherapy
- Radiography
- Speech and Language Therapy
- Browse content in Anaesthetics
- General Anaesthesia
- Neuroanaesthesia
- Browse content in Clinical Medicine
- Acute Medicine
- Cardiovascular Medicine
- Clinical Genetics
- Clinical Pharmacology and Therapeutics
- Dermatology
- Endocrinology and Diabetes
- Gastroenterology
- Genito-urinary Medicine
- Geriatric Medicine
- Infectious Diseases
- Medical Toxicology
- Medical Oncology
- Pain Medicine
- Palliative Medicine
- Rehabilitation Medicine
- Respiratory Medicine and Pulmonology
- Rheumatology
- Sleep Medicine
- Sports and Exercise Medicine
- Clinical Neuroscience
- Community Medical Services
- Critical Care
- Emergency Medicine
- Forensic Medicine
- Haematology
- History of Medicine
- Browse content in Medical Dentistry
- Oral and Maxillofacial Surgery
- Paediatric Dentistry
- Restorative Dentistry and Orthodontics
- Surgical Dentistry
- Browse content in Medical Skills
- Clinical Skills
- Communication Skills
- Nursing Skills
- Surgical Skills
- Medical Ethics
- Medical Statistics and Methodology
- Browse content in Neurology
- Clinical Neurophysiology
- Neuropathology
- Nursing Studies
- Browse content in Obstetrics and Gynaecology
- Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology (ENT)
- Browse content in Paediatrics
- Neonatology
- Browse content in Pathology
- Chemical Pathology
- Clinical Cytogenetics and Molecular Genetics
- Histopathology
- Medical Microbiology and Virology
- Patient Education and Information
- Browse content in Pharmacology
- Psychopharmacology
- Browse content in Popular Health
- Caring for Others
- Complementary and Alternative Medicine
- Self-help and Personal Development
- Browse content in Preclinical Medicine
- Cell Biology
- Molecular Biology and Genetics
- Reproduction, Growth and Development
- Primary Care
- Professional Development in Medicine
- Browse content in Psychiatry
- Addiction Medicine
- Child and Adolescent Psychiatry
- Forensic Psychiatry
- Learning Disabilities
- Old Age Psychiatry
- Psychotherapy
- Browse content in Public Health and Epidemiology
- Epidemiology
- Public Health
- Browse content in Radiology
- Clinical Radiology
- Interventional Radiology
- Nuclear Medicine
- Radiation Oncology
- Reproductive Medicine
- Browse content in Surgery
- Cardiothoracic Surgery
- Gastro-intestinal and Colorectal Surgery
- General Surgery
- Neurosurgery
- Paediatric Surgery
- Peri-operative Care
- Plastic and Reconstructive Surgery
- Surgical Oncology
- Transplant Surgery
- Trauma and Orthopaedic Surgery
- Vascular Surgery
- Browse content in Science and Mathematics
- Browse content in Biological Sciences
- Aquatic Biology
- Biochemistry
- Bioinformatics and Computational Biology
- Developmental Biology
- Ecology and Conservation
- Evolutionary Biology
- Genetics and Genomics
- Microbiology
- Molecular and Cell Biology
- Natural History
- Plant Sciences and Forestry
- Research Methods in Life Sciences
- Structural Biology
- Systems Biology
- Zoology and Animal Sciences
- Browse content in Chemistry
- Analytical Chemistry
- Computational Chemistry
- Crystallography
- Environmental Chemistry
- Industrial Chemistry
- Inorganic Chemistry
- Materials Chemistry
- Medicinal Chemistry
- Mineralogy and Gems
- Organic Chemistry
- Physical Chemistry
- Polymer Chemistry
- Study and Communication Skills in Chemistry
- Theoretical Chemistry
- Browse content in Computer Science
- Artificial Intelligence
- Computer Architecture and Logic Design
- Game Studies
- Human-Computer Interaction
- Mathematical Theory of Computation
- Programming Languages
- Software Engineering
- Systems Analysis and Design
- Virtual Reality
- Browse content in Computing
- Business Applications
- Computer Security
- Computer Games
- Computer Networking and Communications
- Digital Lifestyle
- Graphical and Digital Media Applications
- Operating Systems
- Browse content in Earth Sciences and Geography
- Atmospheric Sciences
- Environmental Geography
- Geology and the Lithosphere
- Maps and Map-making
- Meteorology and Climatology
- Oceanography and Hydrology
- Palaeontology
- Physical Geography and Topography
- Regional Geography
- Soil Science
- Urban Geography
- Browse content in Engineering and Technology
- Agriculture and Farming
- Biological Engineering
- Civil Engineering, Surveying, and Building
- Electronics and Communications Engineering
- Energy Technology
- Engineering (General)
- Environmental Science, Engineering, and Technology
- History of Engineering and Technology
- Mechanical Engineering and Materials
- Technology of Industrial Chemistry
- Transport Technology and Trades
- Browse content in Environmental Science
- Applied Ecology (Environmental Science)
- Conservation of the Environment (Environmental Science)
- Environmental Sustainability
- Environmentalist Thought and Ideology (Environmental Science)
- Management of Land and Natural Resources (Environmental Science)
- Natural Disasters (Environmental Science)
- Nuclear Issues (Environmental Science)
- Pollution and Threats to the Environment (Environmental Science)
- Social Impact of Environmental Issues (Environmental Science)
- History of Science and Technology
- Browse content in Materials Science
- Ceramics and Glasses
- Composite Materials
- Metals, Alloying, and Corrosion
- Nanotechnology
- Browse content in Mathematics
- Applied Mathematics
- Biomathematics and Statistics
- History of Mathematics
- Mathematical Education
- Mathematical Finance
- Mathematical Analysis
- Numerical and Computational Mathematics
- Probability and Statistics
- Pure Mathematics
- Browse content in Neuroscience
- Cognition and Behavioural Neuroscience
- Development of the Nervous System
- Disorders of the Nervous System
- History of Neuroscience
- Invertebrate Neurobiology
- Molecular and Cellular Systems
- Neuroendocrinology and Autonomic Nervous System
- Neuroscientific Techniques
- Sensory and Motor Systems
- Browse content in Physics
- Astronomy and Astrophysics
- Atomic, Molecular, and Optical Physics
- Biological and Medical Physics
- Classical Mechanics
- Computational Physics
- Condensed Matter Physics
- Electromagnetism, Optics, and Acoustics
- History of Physics
- Mathematical and Statistical Physics
- Measurement Science
- Nuclear Physics
- Particles and Fields
- Plasma Physics
- Quantum Physics
- Relativity and Gravitation
- Semiconductor and Mesoscopic Physics
- Browse content in Psychology
- Affective Sciences
- Clinical Psychology
- Cognitive Psychology
- Cognitive Neuroscience
- Criminal and Forensic Psychology
- Developmental Psychology
- Educational Psychology
- Evolutionary Psychology
- Health Psychology
- History and Systems in Psychology
- Music Psychology
- Neuropsychology
- Organizational Psychology
- Psychological Assessment and Testing
- Psychology of Human-Technology Interaction
- Psychology Professional Development and Training
- Research Methods in Psychology
- Social Psychology
- Browse content in Social Sciences
- Browse content in Anthropology
- Anthropology of Religion
- Human Evolution
- Medical Anthropology
- Physical Anthropology
- Regional Anthropology
- Social and Cultural Anthropology
- Theory and Practice of Anthropology
- Browse content in Business and Management
- Business Strategy
- Business Ethics
- Business History
- Business and Government
- Business and Technology
- Business and the Environment
- Comparative Management
- Corporate Governance
- Corporate Social Responsibility
- Entrepreneurship
- Health Management
- Human Resource Management
- Industrial and Employment Relations
- Industry Studies
- Information and Communication Technologies
- International Business
- Knowledge Management
- Management and Management Techniques
- Operations Management
- Organizational Theory and Behaviour
- Pensions and Pension Management
- Public and Nonprofit Management
- Social Issues in Business and Management
- Strategic Management
- Supply Chain Management
- Browse content in Criminology and Criminal Justice
- Criminal Justice
- Criminology
- Forms of Crime
- International and Comparative Criminology
- Youth Violence and Juvenile Justice
- Development Studies
- Browse content in Economics
- Agricultural, Environmental, and Natural Resource Economics
- Asian Economics
- Behavioural Finance
- Behavioural Economics and Neuroeconomics
- Econometrics and Mathematical Economics
- Economic Systems
- Economic History
- Economic Methodology
- Economic Development and Growth
- Financial Markets
- Financial Institutions and Services
- General Economics and Teaching
- Health, Education, and Welfare
- History of Economic Thought
- International Economics
- Labour and Demographic Economics
- Law and Economics
- Macroeconomics and Monetary Economics
- Microeconomics
- Public Economics
- Urban, Rural, and Regional Economics
- Welfare Economics
- Browse content in Education
- Adult Education and Continuous Learning
- Care and Counselling of Students
- Early Childhood and Elementary Education
- Educational Equipment and Technology
- Educational Strategies and Policy
- Higher and Further Education
- Organization and Management of Education
- Philosophy and Theory of Education
- Schools Studies
- Secondary Education
- Teaching of a Specific Subject
- Teaching of Specific Groups and Special Educational Needs
- Teaching Skills and Techniques
- Browse content in Environment
- Applied Ecology (Social Science)
- Climate Change
- Conservation of the Environment (Social Science)
- Environmentalist Thought and Ideology (Social Science)
- Management of Land and Natural Resources (Social Science)
- Natural Disasters (Environment)
- Social Impact of Environmental Issues (Social Science)
- Sustainability
- Browse content in Human Geography
- Cultural Geography
- Economic Geography
- Political Geography
- Browse content in Interdisciplinary Studies
- Communication Studies
- Museums, Libraries, and Information Sciences
- Browse content in Politics
- African Politics
- Asian Politics
- Chinese Politics
- Comparative Politics
- Conflict Politics
- Elections and Electoral Studies
- Environmental Politics
- Ethnic Politics
- European Union
- Foreign Policy
- Gender and Politics
- Human Rights and Politics
- Indian Politics
- International Relations
- International Organization (Politics)
- International Political Economy
- Irish Politics
- Latin American Politics
- Middle Eastern Politics
- Political Methodology
- Political Communication
- Political Philosophy
- Political Sociology
- Political Behaviour
- Political Economy
- Political Institutions
- Political Theory
- Politics and Law
- Politics of Development
- Public Administration
- Public Policy
- Qualitative Political Methodology
- Quantitative Political Methodology
- Regional Political Studies
- Russian Politics
- Security Studies
- State and Local Government
- UK Politics
- US Politics
- Browse content in Regional and Area Studies
- African Studies
- Asian Studies
- East Asian Studies
- Japanese Studies
- Latin American Studies
- Middle Eastern Studies
- Native American Studies
- Scottish Studies
- Browse content in Research and Information
- Research Methods
- Browse content in Social Work
- Addictions and Substance Misuse
- Adoption and Fostering
- Care of the Elderly
- Child and Adolescent Social Work
- Couple and Family Social Work
- Direct Practice and Clinical Social Work
- Emergency Services
- Human Behaviour and the Social Environment
- International and Global Issues in Social Work
- Mental and Behavioural Health
- Social Justice and Human Rights
- Social Policy and Advocacy
- Social Work and Crime and Justice
- Social Work Macro Practice
- Social Work Practice Settings
- Social Work Research and Evidence-based Practice
- Welfare and Benefit Systems
- Browse content in Sociology
- Childhood Studies
- Community Development
- Comparative and Historical Sociology
- Economic Sociology
- Gender and Sexuality
- Gerontology and Ageing
- Health, Illness, and Medicine
- Marriage and the Family
- Migration Studies
- Occupations, Professions, and Work
- Organizations
- Population and Demography
- Race and Ethnicity
- Social Theory
- Social Movements and Social Change
- Social Research and Statistics
- Social Stratification, Inequality, and Mobility
- Sociology of Religion
- Sociology of Education
- Sport and Leisure
- Urban and Rural Studies
- Browse content in Warfare and Defence
- Defence Strategy, Planning, and Research
- Land Forces and Warfare
- Military Administration
- Military Life and Institutions
- Naval Forces and Warfare
- Other Warfare and Defence Issues
- Peace Studies and Conflict Resolution
- Weapons and Equipment

- < Previous chapter
- Next chapter >

5 Psychiatric Treatment of Bipolar Disorder: The Case of Janice
- Published: February 2013
- Cite Icon Cite
- Permissions Icon Permissions
Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment, potential treatment obstacles, ethical considerations, common mistakes to avoid in treatment, and relapse prevention.
Personal account
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Our books are available by subscription or purchase to libraries and institutions.
| Month: | Total Views: |
|---|---|
| October 2022 | 4 |
| November 2022 | 1 |
| December 2022 | 5 |
| January 2023 | 6 |
| February 2023 | 4 |
| March 2023 | 6 |
| April 2023 | 1 |
| May 2023 | 1 |
| June 2023 | 3 |
| July 2023 | 2 |
| August 2023 | 2 |
| September 2023 | 4 |
| October 2023 | 4 |
| November 2023 | 3 |
| December 2023 | 4 |
| January 2024 | 14 |
| February 2024 | 6 |
| March 2024 | 3 |
| April 2024 | 3 |
| May 2024 | 6 |
| June 2024 | 5 |
| July 2024 | 2 |
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Clinical case report on bipolar affective disorder, mania

IP Journal of Paediatrics and Nursing Science
Bipolar disorder is an episodic, potentially life-long, disabling disorder that can be difficult to diagnose. Need to improve recognition, reduce sub-optimal care and improve long-term outcomes. There is variation in management of care across healthcare settings.Characteristics of a Manic Episode: A distinct period of abnormally and persistently elevated, expansive or irritable mood.During the period of mood disturbance, at least three of the following symptoms have persisted (four if the mood is only irritable) and have been persistent to a significant degree.1. Inflated self-esteem or grandiosity. 2. Decreased need for sleep. 3. More talkative than usual or pressure to keep talking. 4. Flight of ideas or subjective experience that thoughts are racing. 5. Distractability, i.e. attention too easily drawn to unimportant or irrelevant external stimuli. 6. Increase in goal-directed activity or psychomotor agitation. 7. Excessive involvement in pleasurable activities which have a high p...
Related Papers
Discovery medicine
Yuly Bersudsky
Extract: Bipolar disorder is one of the most distinct syndromes in psychiatry and has been described in numerous cultures over the course of history, in a manner that suggests considerable similarity of the syndrome in time and place. The unique phase of the illness is mania. However, depression can be the most prominent phase and the ratio of depressions to manias over the life course of the illness is highly variable. Depression in a bipolar disorder is a syndrome that can be understood by any human being, as all of us have experienced sadness and there are at least some commonalities between normal sadness and the state of depression. Mania is often difficult to explain to someone who has not seen a manic patient. In many ways, mania is the opposite of depression and is characterized by the following: an elevated mood or euphoria, an overactivity with a lack of the need for sleep, and an increased optimism that usually becomes so severe that the patient's judgment is impaired...
Colleen B Norton
Revista Brasileira de Psiquiatria
Renata Tamada , Sheila Caetano
Journal of Affective Disorders
Marcia Roberts Mikels
Manic episodes that are not caused by drugs or other substances and depressive symptoms including despair, withdrawal, and uncontrollable crying, are characteristic of Bipolar Disorder I as put forth by the DSM-5, the newest edition of the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). During the manic portion of this disorder, a client might exhibit an almost obsessive compulsion for promiscuous sex or over-spending and may become violent. When a client or patient displays this out-of-control behavior with little regard for consequences, it makes the manic part of Bipolar Disorder easy to diagnose as it is flagrant to family members and those that are daily with him or her. These behaviors will likely not be displayed in a clinical setting, and the information will not be volunteered by the patient. Therefore, other means of investigation will be needed such as interviews with people around the client, especially family members and standardized tests to help rule out other disorders such as personality disorders (Rahimi, Pmorrahimi, Ahmadpanah, Shamsaei, and Torabian, 2014). The disorder has both the markers of major depressive disorder and also these instances of negatively energetic outbursts/incidents which is why it is unique from a depressive disorder which does not have this flip-side. The cases outlined below are from case files and experiences but names and pertinent identifying facts must remain anonymous for the safety and confidentiality of the families involved. They are real cases with real people who have suffered either with Bipolar disorder themselves or as caretakers/domestic occupants with a BD subject.
Practice in Clinical Psychology
Marjan PoshtMashhadi
Archives of Rehabilitation
Objective: According to DSM-5, bipolar disorder is a condition in which the patient experiences one or several manic episodes and sometimes major depressive episodes too. The signs and symptoms of the disorders in DSM are generally influenced by cultural and ethnic factors. Therefore, the present study was aimed at identifying the clinical manifestations of mania in bipolar I disorder in Iranian population. Methods: The present work is a cross-sectional study. The participants included 64 patients in the manic phase of bipolar I disorder who were selected from the Razi psychiatric hospital and the Taleghani Hospital, using a convenience sampling method. The study data were gathered using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Young Mania Rating Scale (YMRS). Results: According to the findings, the most common signs and symptoms of mania in hospitalized patients with bipolar I disorder included reduced need for sleep (89.1), poor insight (87.5), elevated mood (85.9), talkativeness (79.7), and psychotic features (68.8). The major symptoms of the patients according to DSM-5 criteria included reduced need for sleep (89.1), talkativeness (79.7), and psychomotor agitation (40.6). According to t-test analysis, patients with and without a history of mental disorders did not have significantly different mania scores. The one-way analysis of variance (ANOVA) analysis indicated no significant difference in mania scores based on the age of onset of the disorder, marital status (single, married, divorced, or widow), education level, and number of hospitalizations. The chi-squared test revealed that patients with a lower education level showed more aggressive behaviors. Conclusion: According to our results, since the response of a patient to a particular treatment is largely influenced by the symptoms of the disorder, clinicians should pay critical attention to the most common signs and symptoms of any mania.
Christoffel Grobler , Jules Angst
In the classification of mood disorders, major depressive disorder is separate from bipolar disorders whereas mania is not. Studies on pure mania are therefore rare. Our paper reviews the evidence for distinguishing pure mania (M) and mania with mild depression (Md) from bipolar disorder. Two large epidemiological studies found a prevalence of 1.7–1.8 % of M/Md in adolescents and adults. Several clinical follow-up studies demonstrated good stabil- ity of the diagnosis after a previous history of three manic episodes. Compared to bipolar disorder, manic disorder is characterised by a weaker family history for depression, an earlier onset, fewer recurrences and better remission, and is less comorbid with anxiety disorders. In addition, mania is strongly associated with a hyperthymic temperament, mani- fests more psychotic symptoms and is more often treated with antipsychotics. Twin and family studies find mania to be more heritable than depression and show no signifi- cant transmission from depression to mania or from mania to depression. Cardiovascular mortality is elevated among patients with mood disorders generally and is highest among those with mania. In non-Western countries, mania and the manic episodes in bipolar disorder are reported to occur more frequently than in Western countries.
European Neuropsychopharmacology
Jules Angst
Materia Socio Medica
Izet Masic, MD, PhD, FWAAS, FEASA, FIAHSI, FEFMI, FACMI
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Dr. Taskin Sarikaya, MD
Progress in Neurology and Psychiatry
JAMES PANDARAKALAM
BIPOLARITY - PSYCHOTHERAPEUTIC AND PSYCHOPHARMACOLOGICAL INTERVENTION (Atena Editora)
Atena Editora
Bipolar Disorders
IOSR Journals
Starlin Mythri
Journal of affective disorders
Cristina Santana
Francesca Serra
Ziyad Rahman
Frontiers in Pharmacology
Michel Bourin
Shelley Hart
Revista brasileira de psiquiatria (Sao Paulo, Brazil : 1999)
Current neuropharmacology
Ross Baldessarini
Psychological Medicine
Paul Bebbington
Neuropsychiatric disease and treatment
Allan Young
Francesca Pellegrini
Archives of Neuropsychiatry
Evrim Erten
Psychiatry (Edgmont (Pa. : Township))
Russell F Lim
International Journal of Health Science
Glaciane Reis
Psychiatry Research
Tae-Youn Jun
International journal of bipolar disorders
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Case Rep Psychiatry
- v.2017; 2017

A Case Report of Mania and Psychosis Five Months after Traumatic Brain Injury Successfully Treated Using Olanzapine
Giordano f. cittolin-santos.
1 Faculty of Medicine, Federal University of Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil
Jesse C. Fredeen
2 Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, Atlanta, GA, USA
Robert O. Cotes
There are few published pharmacologic trials for the treatment of acute mania following traumatic brain injury (TBI). To our knowledge, we present the first case report of an individual being treated and stabilized with olanzapine monotherapy for this condition.
Case Presentation
We describe the case of a 53-year-old African American male admitted to an inpatient psychiatric hospital with one month of behavioral changes including irritability, decreased need for sleep, hyperverbal speech, hypergraphia, and paranoia five months after TBI. Using Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria, he was diagnosed with bipolar disorder due to traumatic brain injury, with manic features. He was serially evaluated with clinical rating scales to measure symptom severity. The Young Mania Rating Scale (YMRS) score upon admission was 31, and the Clinician-Rated Dimensions of Psychosis Symptom Severity (CRDPSS) score was initially 9. After eight days of milieu treatment and gradual titration of olanzapine to 15 mg nightly, his symptoms completely abated, with YMRS and CRDPSS scores at zero on the day of discharge.
Olanzapine was effective and well tolerated for the treatment of mania following TBI.
1. Introduction
Mania develops in 1.9–9% of individuals after experiencing traumatic brain injury (TBI) [ 1 , 2 ]. Yet, there is a dearth of literature on pharmacologic treatment options for mania following TBI. The guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury, published in 2006, concluded there was insufficient evidence to support the development of standards or guidelines in the treatment of TBI related mania [ 3 ]. Four studies were included in the review, including three case series (each with two patients) and one case report. Treatments successful in treating mania included clonidine [ 4 ], thioridazine/amitriptyline [ 5 ], electroconvulsive therapy [ 5 ], lithium [ 6 ], and valproate [ 6 ]. In addition to the studies presented in the 2006 guidelines, successful trials have been published with carbamazepine/lithium [ 7 ], lithium/thioridazine [ 8 ], lithium monotherapy [ 9 – 11 ], valproate/olanzapine [ 12 – 14 ], valproate monotherapy [ 15 ], carbamazepine/chlorpromazine [ 16 , 17 ], haloperidol [ 16 ], haloperidol/chlorpromazine [ 18 ], haloperidol/clonazepam [ 19 ], and quetiapine [ 20 ]. Here, we present the first case report of successful treatment with olanzapine monotherapy for mania after a traumatic brain injury.
2. Case Presentation
A 53-year-old African American male was brought by Emergency Medical Services (EMS) to the Emergency Room (ER) of an urban, public teaching hospital, due to threatening behavior, irritability, and an inability to care for himself. During the initial psychiatric consultation in the ER, the patient was hyperverbal with pressured speech and a tangential thought process. His mood was elevated, and his affect was labile with sudden and inappropriate bouts of tearfulness. He endorsed decreased need for sleep over the past few days and paranoid and persecutory delusions regarding strange noises around his apartment and his brother stealing money from his father. Per the EMS report, the patient was also emailing and texting neighbors paranoid and threatening messages, which resulted in multiple crisis hotline calls and the patient being brought to the hospital.
His past medical history was significant for a depressive episode treated successfully 25 years ago with sertraline and TBI five months prior to presentation. After the injury, he was followed by an outpatient neurologist for postconcussive syndrome. A brain MRI was ordered three months after TBI, which showed signs of mild white matter small vessel ischemic changes, but no other significant findings. The initial ER workup included a urinalysis, urine drug screen, complete metabolic panel, and thyroid function, all of which were unremarkable. A noncontrast CT scan of the brain was obtained and was unremarkable. He was admitted for inpatient psychiatric hospitalization. Using Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria [ 21 ], he was diagnosed with bipolar disorder due to traumatic brain injury, with manic features.
The patient was started on olanzapine 2.5 mg by mouth at bedtime upon admission. Manic features remained prominent, as he continued to demonstrate decreased need for sleep (three to five hours per night), pressured speech, irritability, emotional dysregulation, and labile affect. He often arose early in the morning and spent multiple hours writing questions for his treatment team. He refused valproate and lithium despite the team's suggestions. Olanzapine was gradually titrated and reached 15 mg on hospital day (HD) 6. Aside from one instance of refusal on HD 5, he was adherent with olanzapine throughout the hospitalization. Olanzapine was well tolerated. He was evaluated with serial clinical rating scales which included the Young Mania Rating Scale (YMRS) and the Clinician-Rated Dimensions of Psychosis Symptom Severity (CRDPSS). On HD 1, the YMRS score was 31 and CRDSS was 9. On HD 6, the YMRS score decreased to 30 and CRDPSS decreased to 7. On HD 7, he displayed significant clinical improvement. He slept throughout the night and on interview no longer had pressured speech. His thought process was logical, linear, and goal-directed, and the psychotic symptoms had also fully abated. On HD 8, the YMRS and CRDPSS scores were 0. He was subsequently discharged from hospital with appropriate outpatient follow-up.
3. Discussion
Mania due to TBI is a challenging diagnosis to make with confidence, and this can make the limited research challenging to interpret. TBI may be an independent risk factor for the development of bipolar disorder [ 1 , 22 – 24 ] and the DSM-5 does not report a definitive time course for which the diagnosis of TBI must take place and symptoms must emerge in order for the disorder to be characterized as mania due to TBI [ 21 ]. As in our case, the majority of individuals who ultimately develop bipolar disorder report a depressive episode first [ 25 ], but the later age of onset of manic symptoms and temporal relationship to TBI lends credence to the TBI's primary role in the development of manic symptoms. In the case presented here, the patient exhibited a combination of manic and psychotic symptoms, but manic symptoms were predominant. The duration of the manic episode (likely around 2 months) was within range of other manic episodes reported after TBI. In study of six patients following head injury who experienced mania, the duration of the episode was 2 months, and the mean estimated duration of elevated mood was 5.7 months [ 2 ].
Olanzapine is a second-generation antipsychotic medication effective for the treatment of acute bipolar mania [ 26 ] and recommended for acute mania by various guidelines across the world [ 27 – 29 ]. However, few pharmacologic (and no randomized) trials exist for the treatment of mania following TBI. Olanzapine has been used for acute mania following TBI in several reported cases. Grenne et al. [ 30 ] described a case of a 13-year-old boy treated with olanzapine 10 mg daily and zonisamide who had improvement of auditory hallucinations but continued mania and delusions. A 60-year-old man was treated with an unspecified dose of olanzapine and 2500 mg of valproate five months after a head injury [ 12 ]. A 42-year-old man was treated with olanzapine 15 mg daily and valproate 1000 mg daily for mania emerging three years after a head trauma [ 13 ]. A 69-year-old man eighteen months after TBI was treated with 7.5 mg of olanzapine and 250 mg of valproate three times daily [ 14 ]. In each of these cases, olanzapine was combined with another medication, and of note, valproate alone has been effective in treating mania secondary to TBI [ 15 ], making it challenging to know if the patient improved related to olanzapine or valproate. Furthermore, olanzapine monotherapy has been shown to be effective in treating psychotic symptoms following traumatic brain injury in two case reports [ 31 , 32 ]. In the case presented here, the patient was not agreeable to other pharmacologic treatments despite being offered lithium and valproate augmentation. In a 2014 review article, Jorge and Arciniegas recommended valproate or quetiapine as first-line therapies for bipolar disorder due to TBI [ 33 ]. We conclude that olanzapine could also be considered for this population, as it was effective and well tolerated in this case.
Conflicts of Interest
Dr. Robert O. Cotes has accepted research funding, consultation fees, and/or honoraria from Alkermes, Janssen, and Otsuka Pharmaceuticals. Drs. Giordano F. Cittolin-Santos and Jesse C. Fredeen have nothing to disclose.
- Open access
- Published: 18 July 2024
The economic burden of bipolar disorder: a case study in Southern Iran
- Zohreh Shaker 1 , 2 ,
- Zahra Goudarzi 2 ,
- Ramin Ravangard 2 ,
- Zinab Shaker 3 ,
- Arvin Hedayati 4 &
- Khosro Keshavarz 2 , 5
Cost Effectiveness and Resource Allocation volume 22 , Article number: 55 ( 2024 ) Cite this article
54 Accesses
Metrics details
Bipolar Disorder (BD) imposes considerable economic and social burdens on the community. Therefore, the present study aimed to determine the economic burden of bipolar disorder in patients referred to single-specialty psychiatric hospitals at the secondary and tertiary care level in 2022.
This partial economic evaluation was conducted as a cross-sectional study in the south of Iran in 2022, and 916 patients were selected through the census method. The prevalence-based and bottom-up approaches were used to collect cost information and calculate the costs, respectively. The data on Direct Medical Costs (DMC), Direct Non-Medical Costs (DNMC), and Indirect costs (IC) were obtained using the information from the patients’ medical records and bills as well as the self-reports by the patients or their companions. The human capital approach was also used to calculate IC.
: The results showed that in 2022, the annual cost of bipolar disorder was $4,227 per patient. The largest share of the costs was that of DMC (77.66%), with hoteling and ordinary beds accounting for the highest expenses (55.40%). The shares of DNMC and IC were 6.37% and 15.97%, respectively, and the economic burden of the disease in the country was estimated at $2,799,787,266 as well.
In general, the costs of bipolar disorder treatment could impose a heavy economic burden on the community, the health system, the insurance system, and the patients themselves. Considering the high costs of hoteling and ordinary beds, it is suggested that hospitalization of BD patients be reduced by managing treatment solutions along with prevention methods to reduce the economic burden of this disease. Furthermore, in order to reduce the costs, proper and fair distribution of psychiatrists and psychiatric beds as well as expansion of home care services and use of the Internet and virtual technologies to follow up the treatment of these patients are recommended.
Introduction
Bipolar Disorder (BD) is a type of brain disorder that causes extreme mood swings as well as changes in the body’s energy level and individual behaviors. People with bipolar disorder experience intense emotional states [ 1 , 2 ]. In other words, bipolar disorder is a lifelong periodic mental illness; this chronic health condition is associated with periods of mania, hypomania, and major depressive disorder [ 3 ].
In some BD patients, the symptoms are so severe that they experience significant problems in doing their daily activities, including daily routines as well as work tasks or school assignments, and their behaviors in the community are severely affected by the disease [ 4 ]. Furthermore, according to a study conducted in 2020, people with BD suffer from financial, social, or occupational problems due to the disease, and impose a considerable socioeconomic burden on their communities and families [ 5 ].
In addition to the fact that this disease may lead to functional and cognitive disorders and reduce the quality of life, it also imposes a great economic burden on the community [ 6 , 7 ]. The global prevalence of bipolar disease was 0.53% on average in 2019, with more than 39 million people suffering from the disease in the world [ 8 ]. The symptoms of this disease mostly start between the ages of 20 and 25 [ 9 ]. BD seems to be more common among women [ 10 ]. The lifetime prevalence of this disease and the prevalence for the age group of 18–65 years in 2019 in Iran were 0.92% and 1.1%, respectively, which were higher than the global average rates [ 8 ].
According to a study conducted in 2022, the annual economic burden of BD treatment in England was calculated at 6.43 billion pounds [ 11 ]. Similarly, another study conducted in the United States in 2015 showed that Direct Medical Costs (DMC) and Direct Non-Medical Costs (DNMC) were 23% and 5%, respectively (accounting for 28% of the costs altogether), and the rest was related to Indirect Costs (IC). The total cost of BD in 2015 was estimated at $202.1 billion as well [ 12 ].
In 2013, Bipolar Disorder was one of the 20 main causes of disability worldwide, leading to significant costs for communities [ 13 ]. According to what was mentioned above, health costs have increased significantly in recent decades around the world. Iran’s health system has also faced significant challenges due to the increased health costs. Considering the limited resources for providing health care services, the provision of effective services is one of the general concerns of health care systems around the world [ 14 ]. Cost-of-illness studies measure the economic burden of diseases [ 15 ].This type of study is used as a model to evaluate different therapeutic interventions and is also used in setting priorities for research in the field of health [ 16 ]. Cost-of-illness studies are common in health systems and are widely used by some organizations, including the World Health Organization and national health institutions [ 17 ].
As found out by reviewing the literature, related domestic studies were very few and to date, no study had been conducted on the economic burden of BD in Iran. According to the findings of the studies, the high prevalence of this disorder and the significant burden it imposed on individuals, the health system, and the community, multiplied the necessity of conducting the present study. Therefore, this research was conducted in order to determine the economic burden of bipolar disorder in Iran in 2022.
Materials and methods
This is a partial economic evaluation study of the cost-of-illness type conducted as cross-sectional research in 2022 in Fars province. The province is located in the south of Iran with a population of over 5 million people (More than %5 population of Iran resides in Fars province). It has 55 public hospitals affiliated with Shiraz, Fasa, Jahrom, Larestan, and Gerash Universities of Medical Sciences. Two hospitals, i.e. Professor Moharari Hospital and Ibn-e Sina Hospitals, are single-specialty and work in the field of psychiatric disorders. We considered secondary and tertiary care levels.
The referral system for mental health services in Iran is one of the strategies for the prevention and treatment of mental disorders. Patients with mental problems are visited by a family physician or a health liaison, and if needed, they are referred to a specialist doctor or psychiatric service center [ 18 ]. The study population included all bipolar disorder patients who were referred and admitted to these two hospitals in 2022. Psychiatrists have diagnosed patients with bipolar disorder with the help of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the International Classification of Diseases 11th Revision (ICD-11), which are two major diagnostic manuals. According to the statistics of these centers, a total of 916 patients were studied through the census method.
The study protocol was approved by the Ethics Committee in November 2022 (code: IR.SUMS.NUMIMG.REC.1401.063). Psychiatrists have diagnosed patients with bipolar disorder with the help of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) which is a major diagnostic manual. All participants were informed, both verbally and in writing, of their right to withdraw from the study at any time. The informed consent was obtained from all subjects and their legal guardian(s) to participate in the study.
In addition, the costs were collected using a researcher-made cost collection form as well as the opinions of psychiatrists and health economists and the patients’ self-reports. The data collection form included four sections as follows: the patients’ demographic characteristics (age, sex, marital status, education level, employment status, type of basic insurance coverage, number of hospitalizations, residence, and average monthly income), and the information on Direct Medical Costs (DMC), Direct Non-Medical Costs (DNMC), and Indirect Costs (IC). This study was conducted from a community perspective; thus, all costs, including DMC, DNMC, and IC, were taken into consideration. To increase the accuracy of the cost data, the researchers tried to consider the opinions of the patients, their companions, and the psychiatric specialists. Furthermore, to avoid recall errors in IC and DNMC, the Outpatient information of patients for the 3 months was separated (The 3-month period of assessment of the patient in euthymic mood and after hospitalization was related, and the patient was in a stable condition.) and then multiplied by 4 to estimate the total annual cost. We have asked the patients and their companions about the number and cost of psychiatrist visits after discharge from the hospital and the number and cost of medications taken by the patient after discharge from the hospital.
Face-to-face or telephone interviews were conducted with the patients or their companions with the help of 4 members (the interviewers were two masters in health economics and two associate professors in health economics). Before the interview, the purpose of the research, the data collection form, and the interview method were explained to the interviewers. Interviews were taken from the patients, but some patients were not able to answer, so we asked the patients’ companions. The required data were collected from December 15, 2022, to February 28, 2023.
Inclusion and exclusion criteria
As suggested by the experts and based on previous studies, the patients’ age was considered 18 to 65 years [ 19 , 20 ]. In addition, those who had only been referred as outpatients were not included in the study due to the lack of medical records, and admitted patients were taken for this study. The exclusion criteria were as follows: Bipolar patients with co-occurring psychiatric illnesses, mental disability along with bipolar disorder, having been affected by BD through head trauma, lack of consent to participate in the study, and unwillingness to continue participation in the study according to the consent form.
Measurement of direct medical cost
Each patient’s DMC was collected retrospectively using a researcher-made collection form by referring to the reference hospitals. The costs included visits, drugs, tests, radiology, concussion, hoteling services, etc., which were separately determined and extracted for inpatient services from the medical and financial records of the patients as well as the hospital information system in 2022 to increase the accuracy of the data. For outpatient services, they were collected through interviews with psychiatric specialists and the patients.
Calculation of direct medical cost
The average annual DMC per patient = (average number of visits × visit tariff) + (average number of each medical service × tariff for each medical service) + (average number of each diagnostic service × tariff of each diagnostic service) + (average number of hospitalizations × tariff for each day of hospitalization) + (cost of each drug dose × number of prescriptions during a treatment period) [ 21 ].
All inpatient services were based on public tariffs. However, for follow-up visits and diagnostic services, patients use both private and public services, which according to the Ministry of Health reports, this ratio is 65% from the private sector and 35% from the public sector. It is worth noting that the percentage of medical care used was taken into account when calculating each case under the supervision of specialists. In addition to drugs (including tablets and injections), ECT therapy is also included in DMC. Services received due to drug side effects and the susceptibility of bipolar disorder patients to diseases such as cardiovascular diseases, thyroid issues, diabetes, and ovarian cysts have also been considered [ 22 ].
Calculation of direct non-medical cost
The DNMC was obtained using a cost collection form and through patient interviews. It included travel expenses to medical centers to receive medical services, as well as accommodation and food expenses for the patients and their companions.
The average annual DNMC per BD patient was calculated as follows:
“Average cost per patient = number of visits to receive medical services per year × cost of each visit”.
Measurement and calculation of indirect cost
The IC included absenteeism and reduced productivity of the patients and their companions, which was calculated through interviews with the patients and their companions based on their average daily income loss due to absence from work for hospitalization or treatment follow-up and the average daily income lost of each patient companion due to absence from work to accompany or care for the patient. The calculation process was based on the human capital approach [ 23 ]. In the present study, the patients’ wages were used to calculate the income lost. The minimum daily wage determined by the Ministry of Labor for housewives and students aged 15 to 65 ($33 considered as the average daily wage in 2022 for eight hours equivalent to one working day) was used as well [ 24 ].
Therefore, in this study, the IC was calculated using a checklist as well as asking the patients and their companions, and based on their monthly income. The human capital approach was also applied [ 23 , 25 ].
Economic burden imposed on all patients with bipolar disorder
In the present study, prevalence-based and bottom-up approaches were used to calculate the economic burden and costs. The former measured patient costs over a period of usually one year and the latter measured the resources used by any individual. Thus, the bottom-up approach was able to distinguish treatment differences between the patients [ 26 ]. The economic burden of the disease was calculated using the following formula: [ 21 ]
Economic burden ∶ Total cost (Direct Medical Cost + Direct Non-medical Cost + Indirect Cost) × estimated number of patients aged 18–65 years in Iran.
It should be noted that in this research, all the costs were converted using the Rial rate and the reference currency index as each dollar was equivalent to 42,000 Rials in 2022 [ 27 ].
Estimation of prevalence
According to the statistics of the World Bank in 2021, 68% of the Iranian population was 18 to 65 years of age [ 28 ]. Besides, the United Nations had declared the population of Iran to be 88,550,570 people in 2022 [ 29 ], and considering the prevalence of this disease in Iran (1.1%) [ 8 ], it was expected that there would be 662,358 BC patients in this age range. The Excel 2016 software was used for data analysis.
Sensitivity analysis
To ensure the robustness of the results, the one-way sensitivity analysis was used in this study. For this purpose, the prevalence rate of bipolar disorder in Iran was considered variable according to the low and high prevalence limits reported by Global Health Data (GHD) (0.0088-0.0132) [ 8 ], and the disease population and the economic burden caused by it were calculated in the determined range. Furthermore, the cost components per patient were assumed constant.
Demographic characteristics
A total of 916 patients participated in the study, whose demographic characteristics are presented in Table 1 . The results showed that 67.03% of the patients were male. Besides, 40.93% of the patients were 18–34 years old, 47.81% were married, and 91.01% had a high school education level or lower. Of all the patients, 63.64% were unemployed, 93.77% were natives of Fars province, and 98.21% had insurance coverage. The average length of hospitalization was 25.05 days.
Direct and indirect costs
Table 2 shows the average direct and indirect costs of the patients with bipolar disorder. The average DMC for each patient was $3,281, and the cost of hoteling and bed was $1,819, accounting for the largest share of DMC (55.40%). The average DNMC for each patient was $271, the highest share of which was the cost of patient companions’ travel (47.92%). Finally, the average IC for each patient was $675, the largest share of which was related to patient absenteeism (84.31%).
Economic burden of costs for BD in Iran
The economic burden of BC costs in Iran was estimated according to the number of patients in the country based on the average prevalence of the disease among people aged 18 to 65. The costs extracted from the results of this study and the estimated economic burden for all bipolar disorder patients in Iran are presented in Table 3 . It was found that the total annual cost of BC patients in Iran was $2,799,787,266 in 2022. The annual cost of this disease per patient was $4,227 as well. The results also showed that DMC accounted for the largest share of the economic burden of bipolar disorder in the country with 77.66%. Figure 1 shows the average total costs of DMC, DNMC, and IC in Iran in 2022.
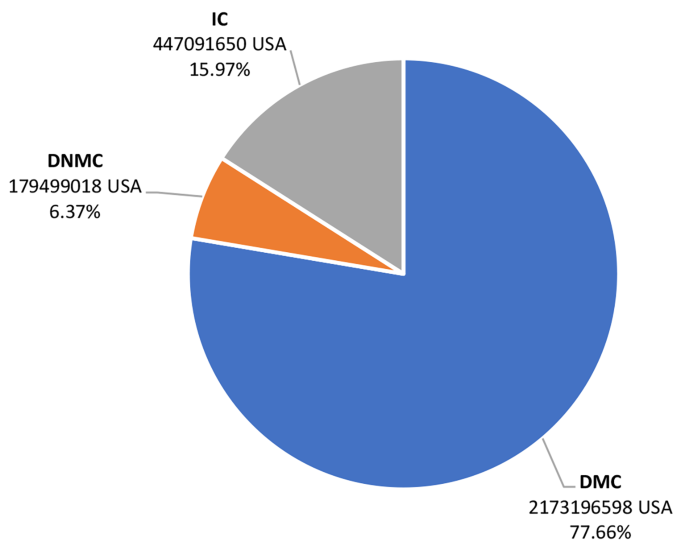
Estimation of annual economic burden of patients with bipolar disorder in Iran in 2022 from a social perspective (USD)
The results of the one-way sensitivity analysis are presented in Table 4 . Considering the changes in the prevalence rate, the total economic burden of bipolar disorder in Iran would vary from $1,530,460,384 to $2,295,689,132.
The increased costs of health systems around the world, especially in low- and middle-income countries like Iran, have become a major concern for health managers and policymakers. The main reason is the increase in the number of non-communicable and chronic diseases, such as bipolar disorder, whose treatment costs have increased rapidly in recent years [ 14 , 30 , 31 ]. This study aimed to calculate the costs of bipolar disorder for the patients referred to the reference medical centers in southern Iran and to determine the economic burden of this disease in the country in 2022.
The demographic characteristics in this study showed that most of the patients were male, in the age range of 18–34 years, married, with an education level below the high school diploma, unemployed, covered by a health insurance organization, living in the cities of Fars province, and without any income. The results of the study by Kheradmand et al. (2022) in Iran on BD patients also showed that most of the patients (52.5%) were male [ 32 ]. In their study, Amini et al.(2010) in Iran [ 33 ] showed that the mean age of the patients was 32.2 years, which is consistent with the results of the present study.
The results of this study showed that bipolar disorder imposed a significant economic burden on the health system and the community. The economic burden of this disease in the country was estimated to be $2,799,787,266, with about 5% of the total budget of the health system in 2022 allocated to it. Considering DMC, DNMC, and IC, it was found that DMC was the highest (77.66%), of which hoteling and bed (55.40%) had the largest share. The reason for the high cost of hoteling could be the high cost of beds and the services provided by the service providers to the studied patients as well as the high average number of their hospitalization days. In most previous studies, the costs of hospitalization and hoteling services had the largest share of DMC [ 6 , 19 , 34 , 35 ]. The studies by Matthias Akamen et al. (2013) on the economic burden of BC in Sweden [ 35 ], Katia Cilini et al. (2012) on the economic burden of BC (a systematic review) [ 19 ], Alan H. Young et al. (2011) on the economic burden of BC in England [ 34 ], and Laura J. Fisher et al. (2007) on the direct medical costs of BC in Australia [ 36 ]were consistent with the present study in terms of the largest share of DMC. However, in a systematic review by Leona Besonova et al. (2020) on the economic burden of BC, it was concluded that the largest share of DMC was related to frequent psychiatric interventions [ 37 ], the reason for which might be the difference in the prices of psychiatric services in America and the difference in their treatment guidelines. Hence, the present study’s observations differ from previous similar studies conducted in developed nations such as the US.
According to the findings of this study, DNMC accounted for 6.37% of the costs, of which the largest share was that of patient companions’ travel expenses (47.92%). The severalty of companions and the large number of their visits to medical centers for following up the patients’ treatment during hospitalization and discharge could be the reason for the high-cost patient companions’ travels in this research. The results of this study are consistent with the findings of Khosro Keshavarz et al. (2022) on the economic burden of major depressive disorder in Iran [ 25 ]. However, our results are not in line with the results of the study by Martin Cloutier et al. (2018) on the economic burden of bipolar disorder in the United States, in which BC drug abuse accounted for the largest share of DNMC [ 12 ]. Due to the lack of reliable and community-based information about the costs of crime and drug abuse related to mental disorders and bipolar disease, these costs were not included in the present research.
As far as IC was concerned (15.97%), the highest cost per patient was related to the patients’ work productivity lost due to their absence from work (84.31%). The results of this study were consistent with the studies by Khosro Keshavarz et al. (2022) on the economic burden of major depressive disorder in Iran [ 25 ], Matthias Akamen et al. [ 35 ], and Martin Cloutier et al. However, the results of the study by Judith Simon et al. (2021) on the costs of bipolar disorder in England [ 11 ] showed that productivity lost due to informal care accounted for the largest share of indirect costs, which is inconsistent with the results of the present study. The main reason for this discrepancy could be the high average number of hospitalization days (25.05 days) in the current study; thus; productivity lost due to the patients’ absenteeism was more than productivity lost due to their companions’ absence from work. Khosro Keshavarz et al. (2020) in Iran [ 25 ], estimated the average total costs per major depression patient to be $2026, which is almost half of the same amount in our study. The reason for this difference is that the average number of hospitalization days in the aforementioned study is less than in our study, and this in turn affects direct medical costs, non-medical direct costs, and indirect costs.
One limitation of the current research was the forgetting of some costs by the patients and as a result, the approximate inclusion of some costs. In addition, some patients refused to participate in the research. The patients who were referred as outpatients were not included in the study due to the lack of medical records. There were also some deficiencies in the medical information of some patients, including lack of data on comorbidities such as substance abuse. In addition, intangible costs were not calculated due to the impossibility of accurately measuring them. Finally, the lack of domestic research on the economic burden of BD was one of the limitations of this study.
In general, the results showed that due to the high prevalence of BD in Iran and the chronicity of the disease as well as the need for lifelong treatment, the costs of treating BD could impose a heavy economic burden on the society, the health care system, the insurance system, and the patients themselves. According to the obtained results, and in order to reduce the economic burden of this disease, it is suggested that necessary plans and measures be taken. Considering the high costs of hoteling and ordinary beds, it is suggested that periodic follow-ups of these patients, along with psychological training and counseling by psychologists, be applied to reduce the hospitalization of these patients and consequently, reduce the economic burden of the disease. In addition, to reduce the costs, proper and fair distribution of psychiatrists and psychiatric beds and expansion of home care services are recommended. Following up the treatment of BD patients, especially in future visits, and possibly using the technologies related to the Internet and remote communication channels, i.e. telemedicine, can help reduce the costs of BD patients and their families due to going to the medical centers.
Data availability
No datasets were generated or analysed during the current study.
Goodwin G, Haddad P, Ferrier I, et al. Evidence-based guidelines for treating bipolar disorder: revised third edition recommendations from the British Association for Psychopharmacology. Psychopharmacology. 2016;30(6):495–553.
Article CAS Google Scholar
Cheniaux E, Nardi AE. Evaluating the efficacy and safety of antidepressants in patients with bipolar disorder. Exp Opin Drug Saf. 2019;18(10):893–913.
Anderson IM, Haddad PM, Scott J. Bipolar disorder. BMJ: Br Med J 2012 Published 27 December;345.
Gautam S, Jain A, Gautam M, et al. Clinical practice guidelines for bipolar affective disorder (BPAD) in children and adolescents. Indian J Psychiatry. 2019;61(Suppl 2):294.
Article PubMed PubMed Central Google Scholar
Rostami Z, Abedi MR, Nilforooshan P. Lived experienced of patients with bipolar disorder in the workplace: a phenomenological. Razi J Med Sci. 2020;27:29–45.
Google Scholar
Vahia NV. Diagnostic and statistical manual of mental disorders 5: a quick glance. Indian J Psychiatry. 2013;55(3):220.
Schmitt A, Malchow B, Hasan A, et al. The impact of environmental factors in severe psychiatric disorders. Front NeuroSci. 2014;8:19.
F J, H F, GH B, al e. Institute for Health Metrics and Evaluation. Global Health Data Exchange. 2019.
Carvalho AF, Firth J, Vieta E. Bipolar disorder. N Engl J Med. 2020;383(1):58–66.
Article CAS PubMed Google Scholar
Grande I, Berk M, Birmaher B et al. Bipolar disorder. Journal The Lancet. 2016 9–15 April 387(10027):1561-72.
Simon J, Pari AAA, Wolstenholme J et al. The costs of bipolar disorder in the United Kingdom. Brain and Behavior. 2021;11(10):e2351.
Cloutier M, Greene M, Guerin A, et al. The economic burden of bipolar I disorder in the United States in 2015. J Affect Disord. 2018;226:45–51.
Article PubMed Google Scholar
Ferrari AJ, Stockings E, Khoo JP, Erskine HE, Degenhardt L, Vos T, et al. The prevalence and burden of bipolar disorder: findings from the global burden of Disease Study 2013. Bipolar Disord. 2016;18(5):440–50.
Max W, Sung H-Y, Stark B. The economic burden of breast cancer in California. Breast Cancer Res Treat. 2009;116(1):201–7.
Costa N, Derumeaux H, Rapp T, Garnault V, Ferlicoq L, Gillette S, et al. Methodological considerations in cost of illness studies on Alzheimer disease. Health Econ Rev. 2012;2(1):1–12.
Article Google Scholar
Brown ML, Yabroff KR. 12, Economic impact of cancer in the United States. Cancer epidemiology and prevention. 2006;202.
Tarricone R. Cost-of-illness analysis: what room in health economics? Health Policy. 2006;77(1):51–63.
Nasrollahpour Shirvani D, Ashrafian Amiri H, Motlagh M, Kabir M, Maleki MR, Shabestani Monfared A, et al. Evaluation of the function of referral system in family physician program in northern provinces of Iran: 2008. J Babol Univ Med Sci. 2010;11(6):46–52.
Kleine-Budde K, Touil E, Moock J, Bramesfeld A, Kawohl W, Rössler W. Cost of illness for bipolar disorder: a systematic review of the economic burden. Bipolar Disord. 2014;16(4):337–53.
Pan Y-J, Kuo K-H, Yeh L-L. Healthcare cost, service use and mortality in major psychiatric disorders in Taiwan. J Affect Disord. 2019;246:112–20.
Keshavarz K, Kebriaeezadeh A, Alavian SM, Sari AA, Dorkoosh FA, Keshvari M et al. Economic burden of hepatitis B virus-related diseases: evidence from Iran. Hepat Monthly. 2015;15(4).
Iran MCotIRo. Ministry of Health tariff in 2021. Medical Council of the Islamic Republic of Iran. 2021.
Witter S, Ensor T, Thompson R, Jowett M. Health Economics for developing countries. A Practical Guide: MacMillan Education; 2000.
Ministry of Cooperatives L, and Social Welfare. The amount of salaries and wages of workers covered by the labor law in 2022. 2022 – 1401.
Keshavarz K, Hedayati A, Rezaei M, Goudarzi Z, Moghimi E, Rezaee M, et al. Economic burden of major depressive disorder: a case study in Southern Iran. BMC Psychiatry. 2022;22(1):1–10.
Morris S, Devlin N, Parkin D, Spencer A. Economic analysis in healthcare: Wiley; 2012.
Iran CBoTIRo. dollar price in the Central Bank of The Islamic Republic of Iran. 1400.
World Bank. worldbank. 2021;United Nations(Population ages 18–65(% of total population)).
worldometers.info. Nations U. worldometers. Services Statistics counters wwwmacrotrendsnet. 2022(Iran Population).
Noorbala AA, Maleki A, Yazdi SAB, Faghihzadeh E, Hoseinzadeh Z, Hajibabaei M, et al. Survey on mental health status in Iranian population aged 15 and above one year after the outbreak of COVID-19 disease: a population-based study. Arch Iran Med. 2022;25(4):201–8.
PubMed Google Scholar
Raaj S, Navanathan S, Tharmaselan M, Lally J. Mental disorders in Malaysia: an increase in lifetime prevalence. BJPsych Int. 2021;18(4):97–9.
Ahmadzadeh Asl M, Shojaee A, Shariati B, et al. A comparative study on the Burden of Disease of Schizophrenia, bipolar disorder type I, and Autism Spectrum Disorder on the Family caregivers in Iran. Archives Rehabilitation. 2021;22(3):341–20.
Amini H, Sharifi V, Nejatisafa A, et al. One year follow-up of patients with bipolar disorder admitted to Roozbeh Hospital. Iran J Psychiatry Clin Psychol. 2009;15(2):168–74.
Young AH, Rigney U, Shaw S, Emmas C, Thompson JM. Annual cost of managing bipolar disorder to the UK healthcare system. J Affect Disord. 2011;133(3):450–6.
Ekman M, Granström O, Omérov S, Jacob J, Landén M. The societal cost of bipolar disorder in Sweden. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1601–10.
Fisher LJ, Goldney RD, Grande ED, et al. Bipolar disorders in Australia. Soc Psychiatry Psychiatr Epidemiol. 2007;42(2):105–9.
Bessonova L, Ogden K, Doane MJ, O’Sullivan AK, Tohen M. The economic burden of bipolar disorder in the United States: a systematic literature review. ClinicoEconomics Outcomes Res. 2020:481–97.
Download references
Acknowledgements
The present article was adopted from the thesis Number P-26595 that was supported by Shiraz University of Medical Sciences. The authors appreciate all the patients and their companions who patiently contributed to this study despite the suffering caused by the disease.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Student Research Committee, School of Health Management and Information Sciences, Shiraz University of Medical Sciences, Shiraz, Iran
Zohreh Shaker
Health Human Resources Research Center, School of Health Management and Information Sciences, Shiraz University of Medical Sciences, Shiraz, Iran
Zohreh Shaker, Zahra Goudarzi, Ramin Ravangard & Khosro Keshavarz
Faculty of Management and Medical Information Sciences, Kerman University of Medical Sciences, Kerman, Iran
Zinab Shaker
Department of Psychiatry, School of Medicine, Research Center for Psychiatry and Behavior Science, Hafez Hospital, Ebnesina Hospital, Shiraz University of Medical Sciences, Shiraz, Iran
Arvin Hedayati
Emergency Medicine Research Center, Shiraz University of Medical Sciences, Shiraz, Iran
Khosro Keshavarz
You can also search for this author in PubMed Google Scholar
Contributions
K.K., A.H., Z.G., Z.O.S. and Z.E.S. participated in data collection. R.R., Z.O.S. and K.K. contributed to analyze the data and interpret its result. R.R. organized and led this study and wrote draft of the manuscript Z.O.S., Z.G., K.K., R.R., A.H., Z.H. contributed to discussion and writing manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Khosro Keshavarz .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with International Declaration of Helsinki. The study protocol was approved by the Ethics Committee of Shiraz University of Medical Sciences, code IR.SUMS.NUMIMG.REC.1401.063. All participants were informed, both verbally and in writing, of their right to withdraw from the study at any time. The informed consent was obtained from all subjects and their legal guardian(s) to participate in the study.

Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zohreh Shaker and Zahra Goudarzi are co-first authors.
Khosro Keshavarz and Arvin Hedayati are co-corresponding authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shaker, Z., Goudarzi, Z., Ravangard, R. et al. The economic burden of bipolar disorder: a case study in Southern Iran. Cost Eff Resour Alloc 22 , 55 (2024). https://doi.org/10.1186/s12962-024-00560-1
Download citation
Received : 20 November 2023
Accepted : 12 June 2024
Published : 18 July 2024
DOI : https://doi.org/10.1186/s12962-024-00560-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Economic Burden
- Bipolar disorder
- Direct Medical cost
- Direct non-medical cost
- Indirect cost
Cost Effectiveness and Resource Allocation
ISSN: 1478-7547
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 July 2024
A bipolar disorder-associated missense variant alters adenylyl cyclase 2 activity and promotes mania-like behavior
- Paromita Sen ORCID: orcid.org/0000-0001-9862-6914 1 ,
- Oskar Ortiz 2 ,
- Elena Brivio ORCID: orcid.org/0000-0002-6213-0973 3 , 4 , 5 ,
- Danusa Menegaz 6 ,
- Laura Sotillos Elliott 1 ,
- Ying Du 1 ,
- Clemens Ries 1 ,
- Alon Chen ORCID: orcid.org/0000-0003-3625-8233 3 , 4 , 5 ,
- Wolfgang Wurst ORCID: orcid.org/0000-0003-4422-7410 2 , 7 , 8 , 9 ,
- Juan Pablo Lopez 3 , 10 ,
- Matthias Eder 6 &
- Jan M. Deussing ORCID: orcid.org/0000-0002-9329-5252 1
Molecular Psychiatry ( 2024 ) Cite this article
605 Accesses
4 Altmetric
Metrics details
- Bipolar disorder
- Neuroscience
The single nucleotide polymorphism rs13166360, causing a substitution of valine (Val) 147 to leucine (Leu) in the adenylyl cyclase 2 (ADCY2), has previously been associated with bipolar disorder (BD). Here we show that the disease-associated ADCY2 missense mutation diminishes the enzyme´s capacity to generate the second messenger 3’,5’-cylic adenosine monophosphate (cAMP) by altering its subcellular localization. We established mice specifically carrying the Val to Leu substitution using CRISPR/Cas9-based gene editing. Mice homozygous for the Leu variant display symptoms of a mania-like state accompanied by cognitive impairments. Mutant animals show additional characteristic signs of rodent mania models, i.e., they are hypersensitive to amphetamine, the observed mania-like behaviors are responsive to lithium treatment and the Val to Leu substitution results in a shifted excitatory/inhibitory synaptic balance towards more excitation. Exposure to chronic social defeat stress switches homozygous Leu variant carriers from a mania- to a depressive-like state, a transition which is reminiscent of the alternations characterizing the symptomatology in BD patients. Single-cell RNA-seq (scRNA-seq) revealed widespread Adcy2 mRNA expression in numerous hippocampal cell types. Differentially expressed genes particularly identified from glutamatergic CA1 neurons point towards ADCY2 variant-dependent alterations in multiple biological processes including cAMP-related signaling pathways. These results validate ADCY2 as a BD risk gene, provide insights into underlying disease mechanisms, and potentially open novel avenues for therapeutic intervention strategies.
Similar content being viewed by others

CADPS functional mutations in patients with bipolar disorder increase the sensitivity to stress

Valproate reverses mania-like behaviors in mice via preferential targeting of HDAC2

Exploring lithium’s transcriptional mechanisms of action in bipolar disorder: a multi-step study
Introduction.
Bipolar disorder (BD) collectively terms a group of chronic psychiatric disorders characterized by recurrent manic and depressive episodes. With a lifetime prevalence of 1%, BD is a leading contributor to the global burden of disease [ 1 ]. This group of mental disorders is accompanied by severely impaired psychosocial functioning and premature mortality [ 2 ]. The disease´s pathophysiology and etiology remain largely elusive. However, based on twin and family studies, a heritability of 60–85% has been estimated, which is comparably high among psychiatric disorders, suggesting a significant genetic component that interacts with other factors, such as adverse environmental exposure, to shape the disease risk [ 3 , 4 , 5 ]. Genome-wide association studies (GWAS) have identified numerous loci associated with BD over the past years [ 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 ]. Among these loci, the adenylyl cyclase 2 gene ( ADCY2 ) has been identified as a potential risk gene for BD [ 14 ], a finding which has been replicated by the latest, and to date largest, BD GWAS meta-analyses [ 15 , 16 ].
ADCYs are enzymes converting adenosine triphosphate (ATP) into the central intracellular signaling mediator 3’,5’-cyclic adenosine monophosphate (cAMP) and pyrophosphate. Their activity is controlled by heteromeric G proteins. Thereby, these enzymes are capable of integrating signals from various G protein-coupled receptors (GPCRs) which are conveyed onto downstream signaling pathways via the second messenger cAMP [ 17 ]. The family of mammalian membrane-bound ADCYs comprises 9 isoforms, which are classified according to their signaling properties. ADCY2, together with ADCY4 and ADCY7, belongs to the group II ADCYs, which are activated by Gαs and Gβγ but insensitive to Ca 2+ /calmodulin (CaM). Similar to all other ADCYs, ADCY2 is expressed in the central nervous system but displays a distinct and broader expression pattern compared to other group II ADCYs [ 18 ].
In the past decades, psychiatric research has particularly focused on neurotransmitter- and neuromodulator-related GPCRs as potential risk factors and drug targets for therapeutic intervention [ 19 , 20 ]. In contrast, ADCYs, which are essential for the generation of the second messenger cAMP, have largely been ignored [ 21 ]. This is somewhat surprising as accumulating evidence from human [ 14 , 22 , 23 , 24 ] and mouse [ 25 , 26 , 27 , 28 , 29 , 30 ] studies suggests an involvement of different ADCYs in psychiatric disorders including autism, schizophrenia, depression and BD.
In contrast to the vast majority of disease-associated SNPs, which are intergenic or intronic, one of the BD-associated SNPs - rs13166360 - is located in the 3 rd exon of the ADCY2 gene (Fig. 1a ). Hence, it encodes a missense mutation resulting in a Val to Leu substitution at position 147 (Val147Leu) within the 4 th transmembrane helix of the first transmembrane domain (Fig. 1b ). Among ADCYs, this missense mutation is unique and its functional consequences are unclear. In ADCY2 homologs of different species, Val 147 is fully conserved. Among other family members, however, it is only found in its closest relative ADCY7 (Fig. 1c ). Based on ADCYs´ role as integrators of extracellular signals, it has been proposed that altered ADCY activity might have a more pronounced effect on BD susceptibility compared to functional variation on the level of individual neurotransmitter or neuromodulator receptors which provide a higher degree of redundancy facilitating compensatory processes [ 14 ].
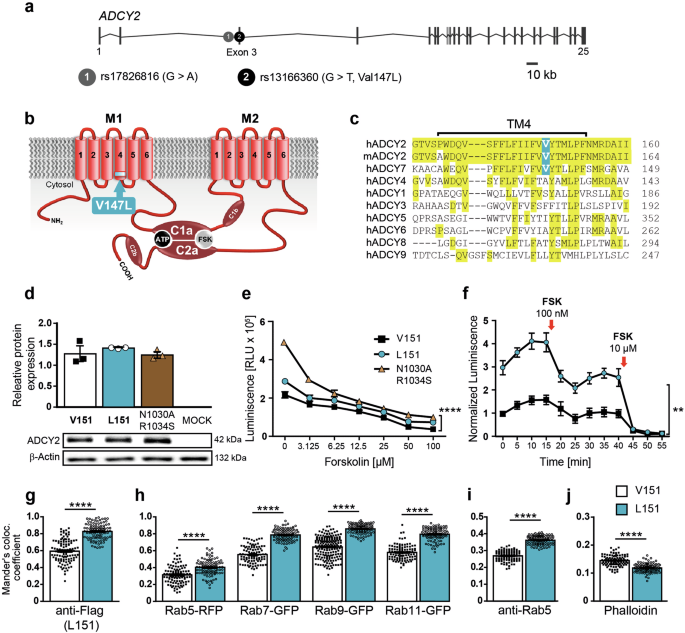
a Organization of human ADCY2 gene and localization of BD-associated SNPs rs17826816 and rs13166360. b rs13166360 causes a Val147 Leu substitution in the 4 th transmembrane helix (TM4) of the first transmembrane domain (M1). c Alignment of TM4 and adjacent regions of human and murine ADCY2 with human membrane bound ADCY paralogues. d Quantification and representative Western blot showing expression levels of ADCY2-V151, ADCY2-L151 and ADCY2-N1030A/R1034S in transiently transfected HEK293 cells (n = 3). e Forskolin (FSK) concentration-dependent stimulation of cAMP production by ADCY2 variants compared to the catalytically inactive variant ADCY2-N1030A/R1034S (n = 3; two-way ANOVA, ADCY2 variants: F (1,14) = 127.6, **** p < 0.0001, concentration: F (6,14) = 207.9, p < 0.0001, variants × concentration: F (6,14) = 20.18, p < 0.0001). f Time course of cAMP production of ADCY2 variants at baseline and following repeated FSK stimulation (n = 3; two-way ANOVA repeated measures, ADCY2 variants: F (2,3) = 98.37, ** p = 0.0018, time: F (2,7) = 301 , p < 0.0001, variants × time: F (12,18) = 22.17, p < 0.0001). Quantification of co-localization of HA-tagged ADCY2-V151 and HA-tagged ADCY2-L151 with: ( g ) FLAG-tagged ADCY2-L151, ( h ) RFP-tagged Rab5, GFP-tag g ed Rab7, Rab9, RAB11, ( i ) endogenous Rab5 and ( j ) phalloidin using Mander’s co-localization co-efficient. In all comparisons, unpaired t test, **** p < 0.0001. Each dot represents an individual cell. All data are presented as mean ± s.e.m..
Here we investigated the direct consequences of rs13166360 on ADCY2 function in vitro and in vivo. To validate ADCY2 as a potential BD risk gene, we used heterologous expression to study protein function and generated a transgenic mouse model carrying the Val to Leu substitution. The latter approach allowed us to interrogate effects of the missense mutation with regards to BD-related endophenotypes and to probe its potential interaction with chronic stress as an environmental risk factor. Finally, we unraveled how the presence of the disease-associated SNP altered the transcriptional landscape in the ventral hippocampus, a brain structure involved in the regulation of emotionality and BD-related behavioral phenotypes.
Materials and methods
Cell culture experiments.
Expression vectors pcDNA3.1-Adcy2-V151-HA and pcDNA3.1-Adcy2-V151-FLAG were cloned from mouse brain mRNA. pcDNA3.1-ADCY2-L151-HA, pcDNA3.1-ADCY2-L151-FLAG and the loss-of-function variant pcDNA3.1-ADCY2-N1030A/R1034S-HA were generated using the QuikChange II Mutagenesis Kit (Agilent). HEK293 and COS-7 cells were transfected with plasmid DNA using Lipofectamine 3000 according to the manufacturer´s protocol (ThermoFisher Scientific). Protein expression was assessed by Western blot and immunofluorescence. For details, refer to online Supplementary Information . Cell lines, originally purchased from the American Type Culture Collection, are regularly tested for mycoplasma contamination using PCR test.
cAMP assays
cAMP levels of transfected cells were measured using the NanoBit® Protein:Protein Interaction System (Promega) and the cAMP-Glo TM Assay (Promega) according to the manufacturer´s instructions. Fluorescence and luminescence signals were recorded using TriStar² LB 942 microplate reader. For details, refer to online Supplementary Information .
Image acquisition and analysis
Images were taken using a Zeiss confocal microscope (LSM800) and digitalized using Zeiss Zen Microscope software and Fiji’s Image J. Image analyses were carried out using Fiji’s Image J and Image J plugin JACoP. Mander’s correlation coefficient was calculated and taken as a measure of the amount of co-localization.
All animal experiments were conducted with the approval of and in accordance with the Guide of the Care and Use of Laboratory Animals of the Government of Upper Bavaria, Germany (Az.: 55.2-1-54-2532-142-2015). Mice were group-housed under standard lab conditions (22 ± 1 °C, 55 ± 5% humidity) and maintained under a 12 h light-dark cycle with food and water ad libitum. All experiments were conducted with adult male mice (age: 2–5 months).
Generation of Adcy2 V151L mice
Mice were generated using CRISPR/Cas9 technology as previously described [ 31 ]. Briefly, we designed two specific sgRNAs located 5´ (sgAdcy2-b) and 3´ (sgAdcy2-a) of Val151 in exon 3 of the Adcy2 gene (Fig. 2a,b ) . These sgRNAs were co-injected with a single-stranded oligonucleotide (ssODN) as a targeting vector into fertilized C57BL/6 J oocytes. The ssODN contained 2 silent mutations, one that added a restriction enzyme site ( Alu I) for genotyping purposes and another one that obliterated the PAM sequence (NGG) so that the donor DNA was not cleaved by Cas9 (Fig. 2b ). A heterozygous founder carrying the Leu151 mutation was used to establish the Adcy2 V151L line. Genotyping was done by PCR using primers Adcy2-I2-fwd 5´-CCA-CCG-CCA-ATG-CTT-CCT-GC-3´ and Adcy2-E3-rev 5´-AAC-AGG-TGC-TCC-TTG-GCC-CC-3´. For genotype determination, the 323 bp PCR product was either subjected to restriction endonuclease digest with Alu I or sequenced. Mice were backcrossed to C57BL/6 N for 5 generations and kept on a mixed C57BL/6 J × C57BL/6 N background. Potential off-target sites were identified using CRISPRscan and Cas-OFFinder allowing up to 2 mismatches [ 32 , 33 ]. Potential off-target sites on chromosome 13 were amplified and sequenced using primers: Off-a2-1C: 5´-TAA-TGG-AGC-AGG-CCA-CTG-TC-3, Off-a2-1NC: 5´-TGT-CCC-CTC-AGA-ACT-TGA-TGC, Off-b6-1C: 5´-GCT-TGC-TGA-GAA-TGG-CTG-ATG, Off-b6-1NC: 5´-AGC-TGT-GCT-TGA-CTG-ACC-TC-3´, Off-b7-1C: 5´-TAC-CAC-AGG-ATG-GGG-GAA-GT-3´, Off-b7-1NC: 5´-TGA-GTC-CTC-AGA-GCC-CTA-CC-3´.
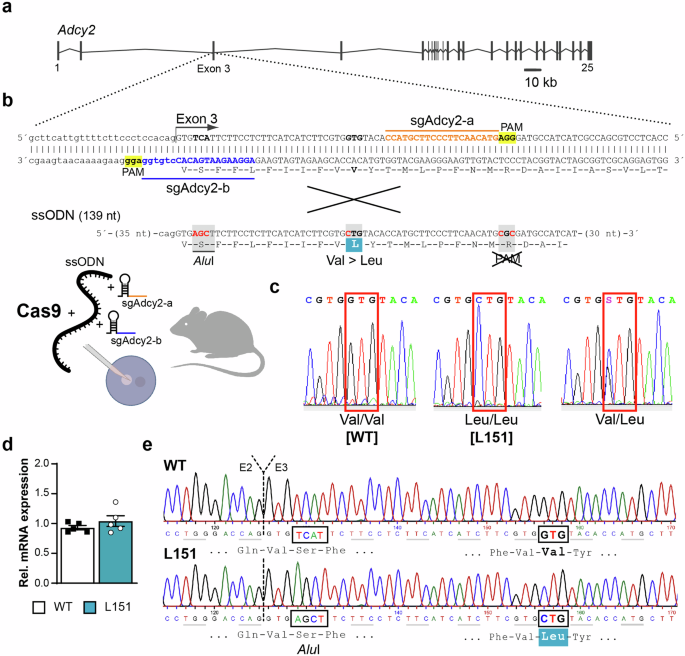
a Organization of the murine Adcy2 gene. b CRISPR/Cas9-based strategy targeting exon 3 using sgRNAs sgAdcy2-a and sgAdcy2-b in combination with a ssODN to replace Val by Leu at position 151. c Representative electropherograms depicting possible genotypes of offspring from heterozygous breedings. d Quantification of Adcy2 mRNA expression in the cortex of WT and L151 mice (n = 5 each) by RT-qPCR. e Representative electropherograms of Adcy2 cDNA from WT and L151 mice covering the transition from exon 2 (E2) to exon 3 (E3). Highlighted are the Alu I restriction site and the Val151Leu substitution present in L151 mice.
Chronic social defeat stress (CSDS) paradigm
The chronic social defeat was performed as previously described [ 34 ]. For details, refer to online Supplementary Information .
Behavioral testing
All behavioral tests were performed between 08:00 am and 12:00 pm in a room adjacent to the animal housing room. Independent batches of animals were used for basal behavioral characterization, cognitive assessment, amphetamine treatment, lithium chloride treatment, and chronic social defeat. The behavioral testing was conducted in the following order: open field test, dark-light box, forced swim test. Recording, tracking and scoring of animal behaviors was carried out using the automated video tracking system ANY-maze (ANY-maze 6.18; Stoelting Co, Wood Dale, IL, USA). All tests were performed by an experienced, blinded researcher and according to established protocols. For details, refer to online Supplementary Information .
Amphetamine-induced hyperlocomotion
Mice were habituated in an OF arena by letting them freely explore the arena for 30 min. The next day, the mice were again introduced to the arena and allowed to freely explore it for 10 min. They were then injected intraperitoneally with amphetamine (4 mg/kg of body weight) or saline solution and placed back in the OF arena, which they were allowed to freely explore for the next 50 min.
Lithium chloride administration
Lithium chloride (LiCl) was administered via the drinking water (600 mg/l) for 10 days. This dosage was chosen as previously described in the literature [ 35 ]. Behavioral testing started between day 10 and day 12, throughout which LiCl was continuously administered.
Electrophysiology
The influence of the ADCY2 V151L substitution on hippocampal long-term potentiation was conducted as previously described [ 34 ]. Patch-clamp experiments were used for recording miniature excitatory postsynaptic currents (mEPSCs) and miniature inhibitory postsynaptic currents (mIPSCs) in the ventral hippocampus. For details, refer to online Supplementary Information .
Determination of dopamine content by enzyme-linked immunosorbent assay
Brain regions of interest (PFC, striatum, nucleus accumbens, hippocampus) were isolated from freshly dissected brains. Brain tissue was homogenized in sterile PBS and dopamine content was determined using a dopamine ELISA kit (Aviva) according to the manufacturer´s protocol.
Single cell RNA sequencing (ScRNA-seq)
Single-cell procedures were performed as previously described [ 36 , 37 ]. For details, refer to online Supplementary Information .
Gene Ontology Analysis
The gene ontology functional enrichment analysis was performed with g:Profiler ( https://biit.cs.ut.ee/gprofiler/gost , version e106_eg53_p16_65fcd97) applying the Kyoto Encyclopedia of Gene and Genome (KEGG) biological pathways as a data source [ 38 ].
Statistical analysis
Statistical analyses were performed using the commercially available software GraphPad Prism v5.0 (GraphPad Software, La Jolla, CA, USA). The sample size was chosen such that with a type 1 error of 0.05 and a type 2 error of 0.2, the effect size should be at least 1.2-fold of the pooled standard deviation. All results are presented as mean ± s.e.m.. All data was tested for normality with Shapiro-Wilk test. Behavioral phenotypic differences between two genotypes were evaluated with Student’s t test (two-tailed). Time-dependent measures were assessed with multi-factorial analysis of variance (ANOVA) with repeated measures. For experiments looking at the effect of pharmacological agents and for CSDS experiments, the effects of genotype and condition on all other behavioral and neuroendocrine parameters were assessed by two factorial ANOVA (two-way ANOVA). Whenever significant main or interaction effects were found by the ANOVAs, Bonferroni post hoc tests were carried out to locate simple effects. Statistical significance was defined as p < 0.05. All data were tested for outliers using Grubbs’ test. Animals were allocated to the experimental groups in a semi-randomized manner and data analysis was performed blinded to the group allocation.
Val151Leu substitution in transmembrane domain 1 alters ADCY2 activity and subcellular localization
To test whether the SNP rs13166360 has a direct impact on protein function, we characterized ADCY2 variants with regards to expression, activity and subcellular localization. With the perspective of testing the Val to Leu missense mutation also in vivo, we focused on murine ADCY2, which shares 95% homology with the human protein but harbors an additional 4 amino acids at its N-terminus, shifting Val 147 of the human protein to position 151 in the mouse ADCY2. We generated N-terminally HA- or FLAG-tagged wild-type (ADCY2-V151) and mutant (ADCY2-L151) variants of murine ADCY2, reflecting the human Val147Leu substitution. In addition, we generated an inactive ADCY2 variant (ADCY2-N1030A/R1034S) as a negative control. To study ADCY2 function by heterologous expression, we chose HEK293 cells as they endogenously express low levels of ADCY2 mRNA (Supplementary Fig. 1 ). All three ADCY2 variants showed comparable levels of protein expression in transiently transfected HEK293 cells (Fig. 1d ). However, comparison of ADCY2 activity by measuring cAMP production induced by the ADCY agonist forskolin (FSK) revealed reduced basal activity of ADCY2-L151 compared to the wild-type ADCY2-V151 variant as indicated by a significantly higher luminescence measured in the cAMP-Glo TM assay, which is inversely proportional to cAMP levels. Nevertheless, the ADCY2-L151 activity was significantly higher than the background activity of endogenous ADCYs, as revealed by comparison to the inactive ADCY2-N1030A/R1034S variant (Fig. 1e ). Similarly, assessment of cAMP production kinetics confirmed a reduced baseline activity of the ADCY2-L151 variant (Fig. 1f ). Apart from the difference in baseline activity, the kinetics of cAMP production in response to different FSK concentrations or repeated stimulation thereby was comparable between both variants (Fig. 1e, f ).
Since the difference in activity could not be attributed to different levels of protein expression or turnover, we hypothesized alterations in ADCY2 localization or trafficking. To this end, we directly compared the subcellular localization of ADCY2 variants and interrogated their localization in relation to different markers of the endosomal/lysosomal compartment. COS-7 cells were transiently transfected either with an HA-tagged variant of ADCY2-V151 or ADCY2-L151, each combined with a FLAG-tagged variant of ADCY2-L151 (Fig. 1g , Supplementary Fig. 2 ). Determination of Mander´s co-localization coefficient revealed a decreased degree of co-localization between ADCY2-V151 and ADCY2-L151 compared to the co-localization observed between the HA- and FLAG-tagged ADCY2-L151 variants. Moreover, ADCY2-L151 showed a significantly higher degree of co-localization with fluorescently tagged Rab5, Rab7, Rab9 and Rab11 compared to ADCY2-V151 (Fig. 1h , Supplementary Fig. 2 ). Similarly, antibody staining of transiently transfected cells for endogenous Rab5 revealed an increased co-localization with the ADCY2-L151 variant (Fig. 1i , Supplementary Fig. 2 ). In contrast, phalloidin staining of transiently transfected COS-7 cells revealed reduced co-localization of ADCY2-L151 with the plasma membrane compared to ADCY2-V151 (Fig. 1j , Supplementary Fig. 2 ). Taken together, these findings suggest a redistribution of the ADCY2-L151 variant from the plasma membrane to intracellular compartments.
Homozygous mutant L151 mice show signs of a mania-like state
Next, we aimed at investigating the in vivo consequences of rs13166360 on mouse behavior. Therefore, we applied CRISPR/Cas9 technology to generate mice carrying the Val151Leu substitution. We used Cas-OFFinder and CRISPRscan [ 32 , 33 ] to predict potential off-target sites (Supplementary Table 1 ). Selective amplification and sequencing of predicted off-target sites co-localized with Adcy2 on chromosome 13, which might escape segregation during meiosis, did not reveal any undesired off-target effects. Breeding of heterozygous mice obtained wild-type Adcy2 V151/V151 (WT) and homozygous mutant Adcy L151/L151 (L151) mice at mendelian ratio (Fig. 2a–c ). Besides confirming the introduced Val151Leu mutation on the genomic DNA level, we substantiated equal expression levels of Ady2-WT and Adcy2-L151 mRNA in WT and L151 mice (Fig. 2d, e ). Homozygous mutant L151 mice did not show any gross abnormalities.
Adcy2 V151L mice were tested in a battery of behavioral paradigms to assess locomotion, exploratory and anxiety-related behavior, stress-coping strategies and cognitive performance. First, we assessed general activity and habituation to a novel environment over a period of 96 hours. In particular in the first two dark phases, L151 mice showed significantly higher activity compared to WT littermates (Fig. 3a ). In the open field test (OFT), the distance traveled was not different between WT and L151 littermates. However, L151 mice entered the inner zone more often and spent more time in the center compared to WT mice (Fig. 3b ). L151 mice also spent more time in the lit zone of the dark-light box (DaLi) (Fig. 3c ). To further investigate object directed exploratory behavior, Adcy2 V151L mice were subjected to a novel object exploration (NOE) test. L151 mice showed increased time exploring the novel object and a trend towards more entries to the object zone (Fig. 3d ). In the forced swim test (FST), L151 mice showed more active stress-coping behavior compared to WT littermates as indicated by decreased floating and increased swimming (Fig. 3e ). To assess cognitive performance, Adcy2 V151L mice were subjected to the Morris water maze (MWM), showing that L151 mice were slower learners compared to their WT littermates (Fig. 3f ) and displayed deficits in long-term memory as indicated by the reduced time spent in the target quadrant at day 7 (Fig. 3f ). In view of the reduced performance in the MWM, we additionally evaluated hippocampal long-term potentiation (LTP) at CA3-CA1 synapses. Sixty minutes after high-frequency stimulation, L151 mice showed a significant decrease in LTP compared to their WT littermates (Fig. 3g ). In summary, L151 mice revealed typical signs reminiscent of a mania-like state observable in rodent mania models as reflected by delayed ambulatory habituation to a novel environment, enhanced exploratory drive and cognitive deficits.

a Locomotor activity during adaptation to a novel home cage (WT n = 8, L151 n = 9; two-way ANOVA repeated measures, 1 st dark phase: genotype: F (1,15) = 4.748, * p = 0.0457, time: F (2, 32) = 5.468, p = 0.006, genotype × time: F (9,120) = 0.8536, p = 0.5687; 2nd dark phase: genotype: F (1,14) = 5.215, * p = 0.0385, time: F (5,75) = 12.54, p < 0.0001, genotype × time: F (11,154) = 0.9820, p = 0.4652). b Distance traveled, number of entries into (unpaired t test, * p = 0.0199 ) and time spent in the inner zone (unpaired t test, * p = 0.035) of the open field test. c Time spent in and number of entries into the lit zone of the dark-light box (unpaired t test, * p = 0.0344 ) . d Exploration of the object (unpaired t test, * p = 0.0227) and object zone entries (unpaired t test, T p = 0.087) in the novel object exploration test ( b–d : WT n = 16, L151 n = 13). e Time spent floating and swimming in the forced swim test (WT n = 16, L151 = 12; unpaired t test, floating and swimming time: p < 0.0001 for both). f Latency to find the platform in the Morris water maze test (WT n = 10, L151 n = 9; two-way ANOVA repeated measures, genotype: *** p = 0.0003, F (1,17) = 20.33, Bonferroni multiple comparisons test: day 2: * p = 0.0478, day 3: * p = 0.0187) and time spent in the target quadrant during memory retrieval (unpaired t test, * p = 0.0325). g LTP at CA3-CA1 synapses in dorsal hippocampal slices from WT and L151 mice (n = 17 slices from 5 WT mice and 18 slices from 5 L151 mice; unpaired t test, * p = 0.0298). Representative recording traces depict fEPSPs before and 60 min after LTP induction. All data are presented as mean ± s.e.m..
L151 mice are more reactive to amphetamine, responsive to lithium treatment and show a shifted excitatory/inhibitory balance
Another characteristic mania-like behavior in animal models of BD is a hypersensitivity towards amphetamine [ 39 ]. As expected, amphetamine treatment (4 mg/kg) induced a strong increase in locomotor activity in Adcy2 V151L mice compared to saline treated animals. However, L151 mice showed an augmented response to amphetamine as indicated by enhanced locomotion compared to WT mice (Fig. 4a ). Considering the difference in amphetamine sensitivity, we assessed dopamine (DA) levels in the prefrontal cortex (PFC), striatum (STR), nucleus accumbens (NAc) and hippocampus (HIP) of Adcy2 V151L mice 90 min after amphetamine application. Amphetamine treatment generally resulted in increased DA levels compared to saline treatment. Again, L151 mice displayed a stronger response to amphetamine as indicated by significantly increased dopamine levels in the PFC, striatum and hippocampus compared to WT mice (Fig. 4b ).

a Locomotor activity following amphetamine treatment (WT n = 11, L151 n = 9; one-way ANOVA repeated measures, genotype: F (3,7) = 8.1386, ** p = 0.0014). b Assessment of dopamine content in the prefrontal cortex (PFC), striatum (STR), nucleus accumbens (NAc) and hippocampus (HIP) following amphetamine treatment (WT n = 3; L151 n = 3; two-way ANOVA; PFC: genotype: F (1,21) = 6.167, p = 0.0091, treatment: F (1,21) = 21.63, p < 0.001, genotype × treatment: p = 23.514; STR: genotype: F (1,21) = 8.914, p = 0.0141, treatment: F (1,21) = 13.615, p = 0.010, genotype × treatment: F (1,21) = 21.631, p = 0.017; NAc: genotype: F (1,22) = 9.762, p = 0.610, treatment: F (1,22) = 12.218, p = 0.012, genotype × treatment: F (1,22) = 21.426, p = 0.047; HIP: genotype: F (1,21) = 10.21, p = 0.0493, treatment: F (1,21) = 6.514, p = 0.0121, genotype × treatment: F (1,21) = 11.426, p = 0.0521). c , d Behavioral assessment of WT and L151 mice following 2 weeks of LiCl treatment (WT control n = 8, L151 control n = 10, WT LiCl n = 9, L151 LiCl n = 10). c Time spent in the inner zone of the open field test (two-way ANOVA, genotype: F (1,31) = 8.641, p = 0.0062, treatment: F (1,31) = 6.763, p = 0 .0141, genotype × treatment: F (1,31) = 13.29, p = 0.001). d Time spent floating (two-way ANOVA, genotype: F (1,33) = 4.530, p = 0.0409, treatment: F (1,33) = 0.1745, p = 0.6788, genotype × treatment: F (1,33) = 324.1, p < 0.0001) and swimming (two-way ANOVA, genotype: F (1,33) = 169.4, p = 0.0409, treatment: F (1,33) = 0.1745, p = 0.6788, genotype × treatment: F (1,33) = 169.4, p < 0.000) in the forced swim test. e Representative traces, ( f ) amplitude and ( g ) frequency (unpaired t test, p = 0.0108) of patch-clamp recordings in the ventral hippocampus of miniature excitatory postsynaptic currents (mEPSCs; WT: n = 5 mice, 19 cells; L151: n = 4 mice, 22 cells). h Representative traces, ( i ) amplitude and ( j ) frequency (unpaired t test, p = 0.0005) of patch-clamp recordings in the ventral hippocampus of miniature inhibitory postsynaptic currents (mIPSCs; WT: n = 4 mice, 37 cells; L151: n = 4 mice, 32 cells). Bonferroni post hoc tests in ( b – d ): T p = 0.0531, * significantly different from WT of the same condition, p < 0.05; # significantly different from the basal condition of the same genotype, p < 0.05. All data are presented as mean ± s.e.m..
Lithium is a commonly prescribed mood stabilizer for the treatment of mania, which is also able to reverse many of the behavioral abnormalities observed in genetic mouse models of mania [ 35 ]. Therefore, we assessed whether the mania-like state presented by homozygous mutant Adcy2 V151L mice could be reversed by lithium treatment. At first place, we confirmed previously observed signs of mania-like behavior in the untreated control group of L151 mice, i.e., increased inner zone time in the OFT (Fig. 4c ) and decreased immobility as well as increased swimming in the FST (Fig. 4d ). In the LiCl treated group, a normalization of behaviors of L151 mice was observed, which reached the level shown by untreated WT mice in the OFT (Fig. 4c ) and in the FST (Fig. 4d ).
A shift in the excitatory and inhibitory (E/I) synaptic balance has been suggested as a potential pathomechanism in BD, particularly playing a role in the manic phase [ 40 ]. Therefore, we recorded AMPA receptor-mediated miniature excitatory postsynaptic currents (mEPSCs) in CA1 pyramidal neurons of the ventral hippocampus (Fig. 4e ). While the amplitude of mEPSCs was comparable between genotypes, the frequency was significantly increased in L151 compared to WT mice (Fig. 4f, g ). We additionally recorded GABA A receptor-mediated miniature inhibitory postsynaptic currents (mIPSCs) in WT and L151 mice (Fig. 4h ). These measurements again revealed a comparable amplitude of recorded mIPSCs, but a significantly decreased frequency in L151 compared to WT mice (Fig. 4i, j ).
The altered frequency of mEPSCs and mIPSCs suggest alterations in synaptic release probabilities. Therefore, we investigated the expression of the synaptic vesicle protein synapsin 1 (SYN1) as a presynaptic marker. Quantification of SYN1 levels by immunofluorescence in different subfields of the ventral hippocampus did not reveal any difference between WT and L151 mice with regards to SYN1 expression levels (Supplementary Fig. 3 ).
Together, with the enhanced reactivity to amphetamine and responsiveness to LiCl, the shift of the E/I balance towards increased excitation supports the notion that L151 mice present a mania-like state.
Chronic social defeat stress induces a switch from a mania- to a depressive-like state in L151 mice
Like most psychiatric disorders, BD involves genetic and environmental factors underlying its etiology. Particularly, the exposure to stressful life events is one factor that has been linked to the development of BD [ 41 , 42 , 43 ]. Therefore, we tested the behavioral consequences of chronic social defeat stress (CSDS) in Adcy2 V151L mice. Following 3 weeks of CSDS, Adcy2 V151L mice showed increased adrenal gland (Fig. 5a ) and decreased thymus (Fig. 5b ) weight independent of genotype, indicating the general efficiency of the CSDS. Similarly, exposure to CSDS entailed clear signs of social-avoidance behavior (Fig. 5c ). In the OFT, stressed mice showed overall reduced locomotor activity independent of genotype (Fig. 5d ). In the control group, L151 mice showed again signs of mania-like behavior as indicated by increased time spent in the center and an increased number of entries to the center of the OFT. However, while the performance of the stressed WT mice was indistinguishable from WT control mice, L151 mice displayed a significant reduction in the time spent in the inner zone (Fig. 5e ) and in the number of entries to the inner zone of the OFT (Fig. 5f ). Similarly, L151 mice responded to CSDS with reduction of the time spent in the lit zone of the DaLi box (Fig. 5g ). Finally, we subjected Adcy2 V151L mice to the FST. Once more, we confirmed the previously observed enhanced active stress-coping behavior of L151 mice in the FST indicated by decreased floating and increased swimming time compared to WT littermates. Interestingly, L151 mice responded to CSDS by enhanced passive stress-coping behavior in comparison to unstressed L151 mice and WT littermates as reflected by increased floating (Fig. 5h ) and decreased swimming (Fig. 5i ) time. Taken together, the findings from the CSDS paradigm suggest a stress-induced switch from a mania- to a depressive-like state.

a–c Validation of efficiency of chronic social defeat stress (CSDS) paradigm. Adrenal weight ( a ) (two-way ANOVA, stress: F (1,45) = 99.06, p < 0.001), thymus weight ( b ) (two-way ANOVA, stress: F (1,45) = 76.27, p < 0.001) and social avoidance ratio ( c ) (two-way ANOVA, stress: F (1,47) = 43.88, p < 0.0001) of Adcy V151L mice subjected to the CSDS. Distance traveled ( d ) (two-way ANOVA, stress: F (1,49) = 24.33, p < 0.001), time spent in the inner zone ( e ) (two-way ANOVA, genotype: F (1,48) = 32.97, p < 0.001, stress: F (1,48) = 23.88, p < 0.001, genotype × stress: F (1,48) = 19.02, p < 0.001) and entries to the inner zone ( f ) (two-way ANOVA, genotype: F (1,50) = 11.56, p = 0.0013, stress: F (1,50) = 19.72, p < 0.001, genotype × stress: F (1,50) = 10.25, p = 0.0024) of the open field. g Time spent in the lit zone of the dark-light box (two-way ANOVA, genotype: F (1,47) = 0.6375, p = 0.4286, stress: F (1,47) = 1.142, p = 0.2906, genotype × stress: F (1,47) = 10.73, p < 0.002). Time spent floating ( h ) (two-way ANOVA, genotype: F (1,48) = 2.437, p = 0.1250, stress: F (1,48) = 39.05, p < 0.001, genotype × stress: F (1,48) = 34.55, p < 0.001) and swimming ( i ) in the forced swim test (two-way ANOVA, genotype: F (1,48) = 2.972, p = 0.0912, stress: F (1,48) = 33.15, p < 0.001, genotype × stress: F (1,48) = 40.31, p < 0.0001). Groups: WT basal n = 16-17, L151 basal n = 10–14, WT stressed n = 10–15, L151 stressed n = 9–11. Bonferroni post hoc tests in ( a-i ): p < 0.05. * significantly different from WT of the same condition, p < 0.05; # significantly different from the basal condition of the same genotype. All data are presented as mean ± s.e.m..
ScRNA-seq uncovers Val151Leu-dependent transcriptional and cellular alterations in the ventral hippocampus
To resolve the cellular expression of Adcy2 mRNA and to assess whether the Val151Leu missense mutation has any impact on downstream gene expression, we performed scRNA-seq on the ventral hippocampus (vHPC) of WT and L151 mice as previously described [ 36 , 37 ]. We focused on the vHPC as a brain structure central for the regulation of emotionality which is potentially involved in BD-related behavioral phenotypes. Using the droplet-based 10x Genomics system, we collected 8477 individual cells that passed our quality control and identified 33 clusters belonging to 17 main cell types (Fig. 6a , Supplementary Fig. 4 , Supplementary Fig. 5 ). Furthermore, we found that Adcy2 mRNA is broadly expressed as it was detectable in various neuronal, glial and epithelial cells of the vHPC (Fig. 6b ). To evaluate the impact of the ADCY2 missense mutation onto the transcriptional state of vHPC cell types, we performed differential gene expression analysis between WT and L151 conditions. In accordance with previous bulk protein expression experiments, Adcy2 mRNA itself was not differentially expressed between cells derived from WT and L151 mice in any of the identified clusters (considering clusters with > 25 cells/cluster, Fig. 6c ). In total, 71 differentially expressed genes (DEGs) were identified between WT and L151 mice and assigned to several clusters, i.e., CA1, CA3 and DG glutamatergic neurons, oligodendrocytes, OPC-COP, microglia, astrocytes, and endothelial cells (Fig. 6d , Supplementary Table 2 ).

a Dimensionality reduction Uniform Manifold Approximation and Projection (UMAP) plot showing 33 clusters belonging to 17 main cell types. b Expression of ADCY2 in various cell types of the ventral hippocampus. c Violin plots comparing ADCY2 expression in different cell types of the ventral hippocampus of WT and L151 mice. d Number of differentially expressed genes between L151 and WT cells in various cell types. e Gene ontology functional enrichment analysis using Kyoto Encyclopedia of Gene and Genome (KEGG) biological pathways. f List of significantly enriched KEGG terms.
To analyze the biological relevance of discovered genes, we chose the cell types with at least 10 DEGs (Fig. 6d ) for a gene enrichment analysis using the Kyoto Encyclopedia of Genes and Genomes (KEGG) database (Fig. 6e ). The largest number of enriched KEGG terms was identified from glutamatergic CA1 neuron-specific DEGs, while only 4 KEGG terms were found using astrocyte-specific DEGs, of which 3 were also identified using oligodendrocyte-specific DEGs (Fig. 6e ). In sum, the gene enrichment analysis revealed a wide range of processes and pathways which are potentially contributing to the behavioral alterations observed in L151 mice (Fig. 6f ).
Besides the analysis of gene expression, we used the scRNA-seq data as a proxy to evaluate the cellular composition of the ventral hippocampus. Therefore, we performed a binominal test for each of the identified clusters [ 44 ] in order to identify which of the observed numbers deviated from a binominal distribution indicating an enrichment of WT or mutant L151 cells. This analysis revealed significantly lower numbers of endothelial cells and DG glutamatergic neurons and OPC-COPs in the ventral hippocampus of L151 compared to WT mice. In contrast, the numbers of CA1 and CA3 glutamatergic neurons as well as OPCs were significantly higher in L151 mice (Supplementary Fig. 6a ). Similar results were obtained by using a Fisher t test for each cluster to test enrichment/depletion of L151 cells versus WT cells (Supplementary Fig. 6b ).
In recent years, ever larger GWAS have identified numerous BD-associated SNPs and respective gene loci. However, their role and contribution to disease etiology and pathophysiology remains largely unclear. Here we demonstrate that rs13166360 directly interferes with ADCY2 activity, diminishing its capacity to generate cAMP. Our results suggest that the impaired activity is not a consequence of reduced enzyme levels but is rather related to altered subcellular localization induced by the Val to Leu substitution in the 4 th transmembrane helix of transmembrane domain M1. Another example of a naturally occurring missense mutation among human ADCY family members is rs3730071, which leads to an alanine to serine substitution at position 674 of ADCY6. This mutation, which is located in the 7 th transmembrane helix of the M2 domain, also attenuates enzyme activity [ 45 ]. Interestingly, the highest frequency of polymorphisms and disease-associated mutations in human transmembrane proteins is found in transmembrane regions with non-polar to non-polar substitutions. Among these, Val to Leu substitutions are the most common ones [ 46 ]. Despite the conservative nature of this substitution, functional consequences, e.g., due to altered protein folding and protein-protein interactions, have been repeatedly reported for various proteins [ 47 , 48 , 49 , 50 , 51 ]. Thus, it is tempting to speculate that the disease-associated ADCY2 SNP might affect the proper interaction of the two transmembrane domains, which has been shown to be critical for correct targeting and functional assembly of ADCYs [ 52 ]. The fact that we demonstrate the reduced enzyme activity as a result of an altered subcellular localization of ADCY2-L151 only in a heterologous system involving overexpression of ADCY2 variants is admittedly a limitation of the study. However, current technical obstacles prevent a specific assessment in tissues or cells derived from Adcy2 V151L mice. On the one hand, there are no suitable ADCY2 antibodies available which would be a prerequisite to address endogenous ADCY2 localization in vivo, e.g., in neurons of ADCY2 mice. Simultaneous discrimination of both variants would even require to equip both variants with suitable tags for detection by immunocytochemistry and Western blot or for precipitation of interaction partners. On the other hand, the assessment of endogenous ADCY2-dependent cAMP levels or respective alterations caused by the V151L mutation is technically not practicable as the measurements will be masked by a high background caused by the other members of the ADCY family which cannot be completely blocked. The functional redundancy, overlapping and low expression, lack of isoform specific agonist and antagonist as well as the absence of reliable antibodies are intricacies inherent to the research on ADCY family members in vivo [ 17 , 53 , 54 , 55 , 56 ].
Besides genetic associations of ADCYs [ 14 , 22 , 24 , 26 ], general alterations in cAMP-dependent signaling pathways have been linked to psychiatric disorders [ 21 , 57 , 58 ]. In the case of BD, some studies have even suggested hyperactivation of cAMP-dependent pathways, which to some extent can be mitigated by lithium or carbamazepine treatment [ 59 , 60 ]. Focused investigation of cAMP signaling-related genes revealed an association of PDE10A, DISC1 and GNAS with BD. Moreover, SNP × SNP interaction studies showed that variants in several of the analyzed cAMP signaling components including ADCY8 interact to increase the risk for BD [ 61 ]. Moreover, genetic mouse models targeting individual ADCYs have provided supportive evidence for their potential role in psychiatric disorders [ 25 , 27 , 28 , 29 , 30 ]. However, none of those studies has addressed the causal involvement of disease-associated ADCY SNPs so far. To specifically study the in vivo consequences of rs13166360 on BD-associated endophenotypes, we established the Adcy2 V151L mouse line. Homozygous mutant L151 mice displayed signs of a mania-like state compared to WT littermates. These included hyperactivity, reduced anxiety-related behavior, increased exploratory drive and increased active stress-coping behavior. Hyperactivity of L151 mice was observed when mice were introduced into a novel home cage. However, this effect was only detectable during the first two nights but vanished with habituation to the novel setting. This is in accordance with observations in BD patients who also show increased locomotion in a novel environment as a result of delayed habituation [ 62 ]. In the light phase, no differences in activity were observed, which might also explain why L151 mice did not show hyperactivity in the OFT and DaLi. Nevertheless, L151 mice presented with significantly reduced anxiety-related behavior in these tests. Enhanced exploration of aversive areas in classical anxiety tests has been observed in many rodent models of mania reflecting enhanced risk-taking behavior and/or impulsivity, which is characteristic for BD individuals in a manic phase [ 35 , 63 , 64 ]. Similarly, the increased time spent on exploring a novel object in the NOE task mirrors signs of increased object exploration reported from patients with bipolar mania which discriminate BD from other psychiatric disorders like schizophrenia [ 62 ]. As many other psychiatric disorders, BD is also associated with significant cognitive impairments [ 65 , 66 ] and mouse models of BD often show cognitive deficits [ 34 ]. L151 mice also displayed deficits in accomplishing spatial learning and memory tasks, which were additionally reflected by reduced hippocampal LTP indicating alterations in synaptic plasticity induced by the disease-associated ADCY2 variant. The involvement of Ca 2+ -dependent ADCYs in LTP has specifically been demonstrated earlier [ 67 , 68 ]. However, increasing cAMP levels could also have a Ca 2+ independent origin connected to direct activation of ADCY2 through the alpha subunit of various Gs protein-coupled receptors [ 69 ] [ 68 ].
The most common model of BD involves psychostimulant-induced hyperlocomotion. Amphetamine induces mania-like symptoms in healthy controls and aggravates symptoms in patients [ 70 , 71 ]. Amphetamine-induced hyperactivity is considered as the ‘gold-standard’ rodent model of mania and is often reported in the context of genetic models of BD. Here we observed that amphetamine-induced hyperlocomotion is more pronounced in L151 mice compared to WT littermates. Concomitantly, we found higher DA levels in response to amphetamine in L151 mice in regions innervated by midbrain dopaminergic neurons. Currently, it remains unclear whether the detected differences are directly related to alterations in DA release kinetics or its turnover. Along these lines, hyperdopaminergic DA transporter knockdown mice also showed impaired habituation and increased exploratory behavior in novel environments [ 72 ]. DA mainly acts onto D1 and D2 receptor subtypes, which are positively and negatively coupled to ADCYs [ 73 ]. These results suggest a direct impact of altered ADCY2 activity on the dopaminergic system contributing to the observed behavioral phenotype. Lithium classically serves as a first-line medication for the treatment of BD patients during a manic episode. Accordingly, mouse models of BD particularly show reversibility of manic-like symptoms in response to lithium treatment [ 35 , 39 ]. Chronic treatment of L151 mice was able to ameliorate behavioral alterations in the OFT and FST to the level of untreated WT mice, supporting previous reports connecting the effect of lithium at least partially to its direct or indirect impact on various ADCYs [ 74 , 75 ].
We observed a specific shift in the frequency of mEPSCs and mIPSCs recorded in the ventral hippocampus indicating increased excitation in L151 mice and suggesting changes in the synaptic release probability. Accordingly, we did not observe genotype-dependent alterations in the presynaptic marker SYN1, suggesting no gross alterations in synaptic connectivity. Disturbances of E/I synaptic balance have been associated with various neurodevelopmental and neuropsychiatric disorders [ 76 ]. Although the role of such disturbances in BD is less explored, there are some genetic mouse models of mania which also show clear signs of E/I synaptic dysfunction [ 40 ]. SHANK3 overexpressing mice showed a reduction in mIPSC frequency and an increased amplitude of spontaneous EPSCs (sEPSCs) which was accompanied by a reduction of inhibitory and an increase in excitatory synaptic markers [ 77 ] [ 76 ]. To what extent the observed alterations in E/I synaptic balance in L151 mice are related to altered activity of GABAergic interneurons or even to an altered cellular composition of the ventral hippocampus is currently unclear but worth investigating in more detail in the future.
Our results indicate that Adcy2 V151L mice recapitulate many aspects of human mania. However, BD is a complex disease with patients alternating between manic and depressive episodes with euthymic or normal mood states between episodes. Relapse from one state to the other can be triggered by physical or sociopsychological stressors, although spontaneous alternations have also been reported. The development of mouse models spontaneously cycling between manic and depressive behavioral states has been challenging [ 78 ]. Chronic stress or even the treatment with glucocorticoids can trigger both manic and depressive episodes in BD patients [ 79 , 80 ]. To test whether depression-like symptoms can be induced by an environmental trigger, Adcy2 V151L mice were exposed to CSDS. L151 and WT mice showed similar physiological signs indicative of a chronically stressed state. Their behavioral response, however, differed significantly. While anxiety-related and stress-coping behavior were largely unaffected in WT mice, L151 mice profoundly responded to the CSDS paradigm. The latter switched from a manic to a depressive-like state as indicated by increased anxiety-related behavior in the OFT and DaLi. Moreover, L151 mice transitioned from an active to a passive stress-coping strategy in the FST. Taken together, these results suggest that L151 mice are able to cycle between manic and depressive episodes following chronic stress exposure, closely resembling the switch between the manic and depressive state in BD patients.
Finally, scRNA-Seq revealed that Adcy2 is not only widely expressed in the murine brain but is also present in a variety of different cell types, albeit the Val151Leu missense mutation did not have an impact on the expression of Adcy2 mRNA itself in any of the identified cell clusters thereby confirming the bulk expression analysis in the cortex based on RT-qPCR (Fig. 2d ). However, ADCYs are the central generators of the second messenger cAMP, which regulates numerous downstream pathways including transcription factors, such as CREB [ 81 ]. Thus, it is not surprising that the observed alteration in ADCY2 activity due to the Val151Leu substitution resulted in differential gene expression, particularly in CA1 glutamatergic neurons but also in oligodendrocytes and, to a lesser extent, in astrocytes. The gene ontology enrichment analysis of DEGs using the KEGG database yielded the highest number of affected processes and pathways in glutamatergic CA1 neurons. Among these, the term cAMP signaling pathway (KEGG: 040204) stands out as it is directly connected to ADCY2´s innate capacity to generate cAMP. Along these lines, Rap1 signaling (KEGG:04015) and Ras signaling (KEGG: 04014) are also linked to cAMP signaling via exchange proteins directly activated by cAMP (EPACs). EPACs, as intracellular sensors, respond to cAMP and act as specific guanine nucleotide exchange factors (GEFs) for small G proteins of the Ras family, such as Rap1 [ 82 ]. Similarly, cGMP-PKG signaling (KEGG04022) has been shown to play a role together with cAMP signaling in the context of LTP (KEGG: 04720) and long-term memory formation. Memory formation requires not only early-phase cGMP/PKG signaling but also late-phase cAMP/PKA-signaling [ 83 ]. Alterations in these pathways may indeed be causally linked to the reduced LTP and altered cognitive performance shown by L151 mice. cAMP and cGMP, in turn, can also modulate the activity of the 1,4,5-trisphosphate (InsP3) receptor, which is activated by InsP3 to trigger the release of Ca 2+ from intracellular stores in the endoplasmatic reticulum, thereby linking the calcium signaling pathway (KEGG: 04020) to the phosphatidylinositol signaling system (KEGG:04070). Interestingly, the gene ontology enrichment analysis also identified terms like dopaminergic synapse (KEGG: 04728) and amphetamine addiction (KEGG: 04728), which is in line with our findings with respect to the increased amphetamine sensitivity and altered DA content in some of the analyzed brain structures of L151 mice, pointing towards disturbances related to the DA hypothesis of BD [ 84 ]. Nevertheless, the scRNA-Seq approach serves here as an initial screen which requires independent confirmation of DEGs and related pathways. In sum, the scRNA-seq analysis provides valuable entry points for a mechanistic understanding of alterations induced by the BD-associated ADCY2 variant which merit closer inspection in future studies.
In conclusion, the herein reported results provide evidence that the BD-associated Val147Leu missense mutation affects ADCY2 activity promoting mania-like symptoms in homozygous mice which, in combination with chronic stress exposure, are converted into a depressive-like state. These ADCY2-specific findings contribute to a growing number of human and mouse studies collectively pointing towards a prominent role of cAMP-related signaling pathways in psychiatric disorders including BD.
Data availability
All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials . Additional data related to this paper may be requested from the authors. Raw sequencing data and annotated gene-barcode matrices are accessible on GEO using the accession number GSE214733 .
Ferrari AJ, Stockings E, Khoo JP, Erskine HE, Degenhardt L, Vos T, et al. The prevalence and burden of bipolar disorder: findings from the Global Burden of Disease Study 2013. Bipolar Disord. 2016;18:440–450.
Article PubMed Google Scholar
Vieta E, Berk M, Schulze TG, Carvalho AF, Suppes T, Calabrese JR, et al. Bipolar disorders. Nat Rev Dis Primers. 2018;4:18008.
Uher R. Gene-environment interactions in severe mental illness. Front Psychiatry. 2014;5:48.
Article PubMed PubMed Central Google Scholar
Gordovez FJA, McMahon FJ. The genetics of bipolar disorder. Mol Psychiatry. 2020;25:544–559.
Fabbri C. The Role of Genetics in Bipolar Disorder. Curr Top Behav Neurosci. 2021;48:41–60.
Article PubMed CAS Google Scholar
Ferreira MA, O’Donovan MC, Meng YA, Jones IR, Ruderfer DM, Jones L, et al. Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet. 2008;40:1056–1058.
Article PubMed PubMed Central CAS Google Scholar
Psychiatric GCBDWG Large-scale genome-wide association analysis of bipolar disorder identifies a new susceptibility locus near ODZ4. Nat Genet 2011;43: 977–983.
Ikeda M, Takahashi A, Kamatani Y, Okahisa Y, Kunugi H, Mori N, et al. A genome-wide association study identifies two novel susceptibility loci and trans population polygenicity associated with bipolar disorder. Mol Psychiatry. 2018;23:639–647.
Cichon S, Muhleisen TW, Degenhardt FA, Mattheisen M, Miro X, Strohmaier J, et al. Genome-wide association study identifies genetic variation in neurocan as a susceptibility factor for bipolar disorder. Am J Hum Genet. 2011;88:372–381.
Baum AE, Akula N, Cabanero M, Cardona I, Corona W, Klemens B, et al. A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Mol Psychiatry. 2008;13:197–207.
Green EK, Hamshere M, Forty L, Gordon-Smith K, Fraser C, Russell E, et al. Replication of bipolar disorder susceptibility alleles and identification of two novel genome-wide significant associations in a new bipolar disorder case-control sample. Mol Psychiatry. 2013;18:1302–1307.
Chen DT, Jiang X, Akula N, Shugart YY, Wendland JR, Steele CJ, et al. Genome-wide association study meta-analysis of European and Asian-ancestry samples identifies three novel loci associated with bipolar disorder. Mol Psychiatry. 2013;18:195–205.
Hou L, Bergen SE, Akula N, Song J, Hultman CM, Landen M, et al. Genome-wide association study of 40,000 individuals identifies two novel loci associated with bipolar disorder. Hum Mol Genet. 2016;25:3383–3394.
Muhleisen TW, Leber M, Schulze TG, Strohmaier J, Degenhardt F, Treutlein J, et al. Genome-wide association study reveals two new risk loci for bipolar disorder. Nat Commun. 2014;5:3339.
Stahl EA, Breen G, Forstner AJ, McQuillin A, Ripke S, Trubetskoy V, et al. Genome-wide association study identifies 30 loci associated with bipolar disorder. Nat Genet. 2019;51:793–803.
Mullins N, Forstner AJ, O’Connell KS, Coombes B, Coleman JRI, Qiao Z, et al. Genome-wide association study of more than 40,000 bipolar disorder cases provides new insights into the underlying biology. Nat Genet. 2021;53:817–829.
Ostrom KF, LaVigne JE, Brust TF, Seifert R, Dessauer CW, Watts VJ, et al. Physiological roles of mammalian transmembrane adenylyl cyclase isoforms. Physiol Rev. 2022;102:815–857.
Sanabra C, Mengod G. Neuroanatomical distribution and neurochemical characterization of cells expressing adenylyl cyclase isoforms in mouse and rat brain. J Chem Neuroanat. 2011;41:43–54.
Mantas I, Saarinen M, Xu ZD, Svenningsson P. Update on GPCR-based targets for the development of novel antidepressants. Mol Psychiatry. 2022;27:534–558.
Griebel G, Holsboer F. Neuropeptide receptor ligands as drugs for psychiatric diseases: the end of the beginning? Nat Rev Drug Discov. 2012;11:462–478.
Tabakoff B, Hoffman PL. Transducing emotionality: the role of adenylyl cyclases. Biol Psychiatry. 2012;71:572–573.
Wray NR, Pergadia ML, Blackwood DH, Penninx BW, Gordon SD, Nyholt DR, et al. Genome-wide association study of major depressive disorder: new results, meta-analysis, and lessons learned. Mol Psychiatry. 2012;17:36–48.
Funk AJ, McCullumsmith RE, Haroutunian V, Meador-Woodruff JH. Abnormal activity of the MAPK- and cAMP-associated signaling pathways in frontal cortical areas in postmortem brain in schizophrenia. Neuropsychopharmacology. 2012;37:896–905.
O’Roak BJ, Vives L, Girirajan S, Karakoc E, Krumm N, Coe BP, et al. Sporadic autism exomes reveal a highly interconnected protein network of de novo mutations. Nature. 2012;485:246–250.
Hines LM, Hoffman PL, Bhave S, Saba L, Kaiser A, Snell L, et al. A sex-specific role of type VII adenylyl cyclase in depression. J Neurosci. 2006;26:12609–12619.
Joeyen-Waldorf J, Nikolova YS, Edgar N, Walsh C, Kota R, Lewis DA, et al. Adenylate cyclase 7 is implicated in the biology of depression and modulation of affective neural circuitry. Biol Psychiatry. 2012;71:627–632.
Chen X, Luo J, Leng Y, Yang Y, Zweifel LS, Palmiter RD, et al. Ablation of Type III Adenylyl Cyclase in Mice Causes Reduced Neuronal Activity, Altered Sleep Pattern, and Depression-like Phenotypes. Biol Psychiatry. 2016;80:836–848.
Kim H, Lee Y, Park JY, Kim JE, Kim TK, Choi J, et al. Loss of Adenylyl Cyclase Type-5 in the Dorsal Striatum Produces Autistic-Like Behaviors. Mol Neurobiol. 2017;54:7994–8008.
Sethna F, Feng W, Ding Q, Robison AJ, Feng Y, Wang H. Enhanced expression of ADCY1 underlies aberrant neuronal signalling and behaviour in a syndromic autism model. Nat Commun. 2017;8:14359.
Razzoli M, Andreoli M, Maraia G, Di Francesco C, Arban R. Functional role of Calcium-stimulated adenylyl cyclase 8 in adaptations to psychological stressors in the mouse: implications for mood disorders. Neuroscience. 2010;170:429–440.
Wefers B, Bashir S, Rossius J, Wurst W, Kuhn R. Gene editing in mouse zygotes using the CRISPR/Cas9 system. Methods. 2017;121-122:55–67.
Moreno-Mateos MA, Vejnar CE, Beaudoin JD, Fernandez JP, Mis EK, Khokha MK, et al. CRISPRscan: designing highly efficient sgRNAs for CRISPR-Cas9 targeting in vivo. Nat Methods. 2015;12:982–988.
Bae S, Park J, Kim JS. Cas-OFFinder: a fast and versatile algorithm that searches for potential off-target sites of Cas9 RNA-guided endonucleases. Bioinformatics. 2014;30:1473–1475.
Dedic N, Pohlmann ML, Richter JS, Mehta D, Czamara D, Metzger MW, et al. Cross-disorder risk gene CACNA1C differentially modulates susceptibility to psychiatric disorders during development and adulthood. Mol Psychiatry. 2018;23:533–543.
Roybal K, Theobold D, Graham A, DiNieri JA, Russo SJ, Krishnan V, et al. Mania-like behavior induced by disruption of CLOCK. Proc Natl Acad Sci USA. 2007;104:6406–6411.
Lopez JP, Lucken MD, Brivio E, Karamihalev S, Kos A, De Donno C, et al. Ketamine exerts its sustained antidepressant effects via cell-type-specific regulation of Kcnq2. Neuron. 2022;110:2283–2298 e2289.
Lopez JP, Brivio E, Santambrogio A, De Donno C, Kos A, Peters M, et al. Single-cell molecular profiling of all three components of the HPA axis reveals adrenal ABCB1 as a regulator of stress adaptation. Sci Adv. 2021;7:eabe4497.
Raudvere U, Kolberg L, Kuzmin I, Arak T, Adler P, Peterson H, et al. g:Profiler: a web server for functional enrichment analysis and conversions of gene lists (2019 update). Nucleic Acids Res. 2019;47:W191–W198.
Logan RW, McClung CA. Animal models of bipolar mania: The past, present and future. Neuroscience. 2016;321:163–188.
Lee Y, Zhang Y, Kim S, Han K. Excitatory and inhibitory synaptic dysfunction in mania: an emerging hypothesis from animal model studies. Exp Mol Med. 2018;50:1–11.
Kim EY, Miklowitz DJ, Biuckians A, Mullen K. Life stress and the course of early-onset bipolar disorder. J Affect Disord. 2007;99:37–44.
Dienes KA, Hammen C, Henry RM, Cohen AN, Daley SE. The stress sensitization hypothesis: understanding the course of bipolar disorder. J Affect Disord. 2006;95:43–49.
Pugliese V, Bruni A, Carbone EA, Calabro G, Cerminara G, Sampogna G, et al. Maternal stress, prenatal medical illnesses and obstetric complications: Risk factors for schizophrenia spectrum disorder, bipolar disorder and major depressive disorder. Psychiatry Res. 2019;271:23–30.
Romanov RA, Zeisel A, Bakker J, Girach F, Hellysaz A, Tomer R, et al. Molecular interrogation of hypothalamic organization reveals distinct dopamine neuronal subtypes. Nat Neurosci. 2017;20:176–188.
Gros R, Ding Q, Cao H, Main T, Hegele RA, Feldman RD. Identification of a dysfunctional missense single nucleotide variant of human adenylyl cyclase VI. Clin Pharmacol Ther. 2005;77:271–278.
Molnar J, Szakacs G, Tusnady GE. Characterization of Disease-Associated Mutations in Human Transmembrane Proteins. PLoS One. 2016;11:e0151760.
Kazemi-Esfarjani P, Beitel LK, Trifiro M, Kaufman M, Rennie P, Sheppard P, et al. Substitution of valine-865 by methionine or leucine in the human androgen receptor causes complete or partial androgen insensitivity, respectively with distinct androgen receptor phenotypes. Mol Endocrinol. 1993;7:37–46.
PubMed CAS Google Scholar
Persson E, Bak H, Olsen OH. Substitution of valine for leucine 305 in factor VIIa increases the intrinsic enzymatic activity. J Biol Chem. 2001;276:29195–29199.
Marballi KK, McCullumsmith RE, Yates S, Escamilla MA, Leach RJ, Raventos H, et al. Global signaling effects of a schizophrenia-associated missense mutation in neuregulin 1: an exploratory study using whole genome and novel kinome approaches. J Neural Transm (Vienna). 2014;121:479–490.
Tibbs ZE, Guidry AL, Falany JL, Kadlubar SA, Falany CN. A high frequency missense SULT1B1 allelic variant (L145V) selectively expressed in African descendants exhibits altered kinetic properties. Xenobiotica. 2018;48:79–88.
Zheng H, Shao C, Zheng Y, He JW, Fu WZ, Wang C, et al. Two novel mutations of CLCN7 gene in Chinese families with autosomal dominant osteopetrosis (type II). J Bone Miner Metab. 2016;34:440–446.
Gu C, Sorkin A, Cooper DM. Persistent interactions between the two transmembrane clusters dictate the targeting and functional assembly of adenylyl cyclase. Curr Biol. 2001;11:185–190.
Sadana R, Dessauer CW. Physiological roles for G protein-regulated adenylyl cyclase isoforms: insights from knockout and overexpression studies. Neurosignals. 2009;17:5–22.
Seifert R, Lushington GH, Mou TC, Gille A, Sprang SR. Inhibitors of membranous adenylyl cyclases. Trends Pharmacol Sci. 2012;33:64–78.
Dessauer CW, Watts VJ, Ostrom RS, Conti M, Dove S, Seifert R. International Union of Basic and Clinical Pharmacology. CI. Structures and Small Molecule Modulators of Mammalian Adenylyl Cyclases. Pharmacol Rev. 2017;69:93–139.
Ostrom RS, Bogard AS, Gros R, Feldman RD. Choreographing the adenylyl cyclase signalosome: sorting out the partners and the steps. Naunyn Schmiedebergs Arch Pharmacol. 2012;385:5–12.
Gould TD, Manji HK. Signaling networks in the pathophysiology and treatment of mood disorders. J Psychosom Res. 2002;53:687–697.
Dwivedi Y, Pandey GN. Adenylyl cyclase-cyclicAMP signaling in mood disorders: role of the crucial phosphorylating enzyme protein kinase A. Neuropsychiatr Dis Treat. 2008;4:161–176.
Masana MI, Bitran JA, Hsiao JK, Mefford IN, Potter WZ. Lithium effects on noradrenergic-linked adenylate cyclase activity in intact rat brain: an in vivo microdialysis study. Brain Res. 1991;538:333–336.
Palmer GC. Interactions of antiepileptic drugs on adenylate cyclase and phosphodiesterases in rat and mouse cerebrum. Exp Neurol. 1979;63:322–335.
McDonald ML, MacMullen C, Liu DJ, Leal SM, Davis RL. Genetic association of cyclic AMP signaling genes with bipolar disorder. Transl Psychiatry. 2012;2:e169.
Perry W, Minassian A, Henry B, Kincaid M, Young JW, Geyer MA. Quantifying over-activity in bipolar and schizophrenia patients in a human open field paradigm. Psychiatry Res. 2010;178:84–91.
Shaltiel G, Maeng S, Malkesman O, Pearson B, Schloesser RJ, Tragon T, et al. Evidence for the involvement of the kainate receptor subunit GluR6 (GRIK2) in mediating behavioral displays related to behavioral symptoms of mania. Mol Psychiatry. 2008;13:858–872.
Kirshenbaum GS, Clapcote SJ, Duffy S, Burgess CR, Petersen J, Jarowek KJ, et al. Mania-like behavior induced by genetic dysfunction of the neuron-specific Na+,K+-ATPase alpha3 sodium pump. Proc Natl Acad Sci USA. 2011;108:18144–18149.
Burdick KE, Braga RJ, Goldberg JF, Malhotra AK. Cognitive dysfunction in bipolar disorder: future place of pharmacotherapy. CNS Drugs. 2007;21:971–981.
Goodwin GM, Martinez-Aran A, Glahn DC, Vieta E. Cognitive impairment in bipolar disorder: neurodevelopment or neurodegeneration? An ECNP expert meeting report. Eur Neuropsychopharmacol. 2008;18:787–793.
Wong ST, Athos J, Figueroa XA, Pineda VV, Schaefer ML, Chavkin CC, et al. Calcium-stimulated adenylyl cyclase activity is critical for hippocampus-dependent long-term memory and late phase LTP. Neuron. 1999;23:787–798.
Wozny C, Maier N, Fidzinski P, Breustedt J, Behr J, Schmitz D. Differential cAMP signaling at hippocampal output synapses. J Neurosci. 2008;28:14358–14362.
Shahoha M, Cohen R, Ben-Simon Y, Ashery U. cAMP-Dependent Synaptic Plasticity at the Hippocampal Mossy Fiber Terminal. Front Synaptic Neurosci. 2022;14:861215.
Nurnberger JI Jr., Gershon ES, Simmons S, Ebert M, Kessler LR, Dibble ED, et al. Behavioral, biochemical and neuroendocrine responses to amphetamine in normal twins and ‘well-state’ bipolar patients. Psychoneuroendocrinology. 1982;7:163–176.
Jacobs D, Silverstone T. Dextroamphetamine-induced arousal in human subjects as a model for mania. Psychol Med. 1986;16:323–329.
Zhuang X, Oosting RS, Jones SR, Gainetdinov RR, Miller GW, Caron MG, et al. Hyperactivity and impaired response habituation in hyperdopaminergic mice. Proc Natl Acad Sci USA. 2001;98:1982–1987.
Andrianarivelo A, Saint-Jour E, Walle R, Trifilieff P, Vanhoutte P. Modulation and functions of dopamine receptor heteromers in drugs of abuse-induced adaptations. Neuropharmacology. 2019;152:42–50.
Risby ED, Hsiao JK, Manji HK, Bitran J, Moses F, Zhou DF, et al. The mechanisms of action of lithium. II. Effects on adenylate cyclase activity and beta-adrenergic receptor binding in normal subjects. Arch Gen Psychiatry. 1991;48:513–524.
Montezinho LP, Mork A, Duarte CB, Penschuck S, Geraldes CF, Castro MM. Effects of mood stabilizers on the inhibition of adenylate cyclase via dopamine D(2)-like receptors. Bipolar Disord. 2007;9:290–297.
Selten M, van Bokhoven H, Nadif Kasri N. Inhibitory control of the excitatory/inhibitory balance in psychiatric disorders. F1000Res. 2018;7:23.
Han K, Holder JL Jr, Schaaf CP, Lu H, Chen H. SHANK3 overexpression causes manic-like behaviour with unique pharmacogenetic properties. Nature. 2013;503:72–77.
Sidor MM, Spencer SM, Dzirasa K, Parekh PK, Tye KM, Warden MR, et al. Daytime spikes in dopaminergic activity drive rapid mood-cycling in mice. Mol Psychiatry. 2015;20:1406–1419.
Koenders MA, Giltay EJ, Spijker AT, Hoencamp E, Spinhoven P, Elzinga BM. Stressful life events in bipolar I and II disorder: cause or consequence of mood symptoms? J Affect Disord. 2014;161:55–64.
Salvadore G, Quiroz JA, Machado-Vieira R, Henter ID, Manji HK, Zarate CA Jr. The neurobiology of the switch process in bipolar disorder: a review. J Clin Psychiatry. 2010;71:1488–1501.
Wang H, Xu J, Lazarovici P, Quirion R, Zheng W. cAMP Response Element-Binding Protein (CREB): A Possible Signaling Molecule Link in the Pathophysiology of Schizophrenia. Front Mol Neurosci. 2018;11:255.
Breckler M, Berthouze M, Laurent AC, Crozatier B, Morel E, Lezoualc’h F. Rap-linked cAMP signaling Epac proteins: compartmentation, functioning and disease implications. Cell Signal. 2011;23:1257–1266.
Bollen E, Puzzo D, Rutten K, Privitera L, De Vry J, Vanmierlo T, et al. Improved long-term memory via enhancing cGMP-PKG signaling requires cAMP-PKA signaling. Neuropsychopharmacology. 2014;39:2497–2505.
Ashok AH, Marques TR, Jauhar S, Nour MM, Goodwin GM, Young AH, et al. The dopamine hypothesis of bipolar affective disorder: the state of the art and implications for treatment. Mol Psychiatry. 2017;22:666–679.
Download references
Acknowledgements
We would like to thank Albin Varga, head of the animal facility, and his staff for their dedicated support with animal care; Andrea Parl, Stefanie Unkmeir and Sabrina Bauer of the scientific core unit Genetically Engineered Mouse Models for technical support; Elmira Anderzhanova for advising the dopamine measurements; Giuseppina Maccarrone for sharing her proteomics expertise, Elfi Fesl for proofreading and editing of the manuscript. We thank Marcella Rietschel and Andreas Forstner for scientific discussion and advice. The project was supported by the Max Planck Society (JMD) and the German Ministry of Science and Education (IntegraMent: Integrated Understanding of Causes and Mechanisms in Mental Disorders FKZ 01ZX1314H, WW; FKZ 01KU1901, JMD).
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Molecular Neurogenetics, Max Planck Institute of Psychiatry, 80804, Munich, Germany
Paromita Sen, Laura Sotillos Elliott, Ying Du, Clemens Ries & Jan M. Deussing
Institute of Developmental Genetics, Helmholtz Zentrum München, 85764, Neuherberg, Germany
Oskar Ortiz & Wolfgang Wurst
Department Stress Neurobiology and Neurogenetics, Max Planck Institute of Psychiatry, 80804, Munich, Germany
Elena Brivio, Alon Chen & Juan Pablo Lopez
Department of Brain Sciences, Weizmann Institute of Science, Rehovot, 76100, Israel
Elena Brivio & Alon Chen
Department of Molecular Neuroscience, Weizmann Institute of Science, Rehovot, 76100, Israel
Scientific Core Unit Electrophysiology, Max Planck Institute of Psychiatry, 80804, Munich, Germany
Danusa Menegaz & Matthias Eder
Chair of Developmental Genetics, Munich School of Life Sciences Weihenstephan, Technical University of Munich, 85354, Freising, Germany
Wolfgang Wurst
Munich Cluster of Systems Neurology (SyNergy), Munich, Germany
German Center for Neurodegenerative Diseases (DZNE) site Munich, 81377, Munich, Germany
Department of Neuroscience, Karolinska Institutet, Stockholm, 17177, Sweden
Juan Pablo Lopez
You can also search for this author in PubMed Google Scholar
Contributions
PS performed cell culture and behavioral experiments, analyzed and interpreted data and wrote the first draft of the manuscript. OO and WW designed the gene editing strategy and generated transgenic mice. DM and ME performed electrophysiological recordings. LSE performed cell culture experiments. YD quantified gene expression. CR performed immunostainings and quantified synaptic markers. EB, JPL and AC supervised and executed the single cell experiment including the data analysis. JMD supervised all experiments and analyses, edited the manuscript and provided scientific advice, guidance, and support. All authors reviewed the manuscript.
Corresponding author
Correspondence to Jan M. Deussing .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval
All animal experiments were conducted with the approval of and in accordance with the Guide of the Care and Use of Laboratory Animals of the Government of Upper Bavaria, Germany.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Sen, P., Ortiz, O., Brivio, E. et al. A bipolar disorder-associated missense variant alters adenylyl cyclase 2 activity and promotes mania-like behavior. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02663-w
Download citation
Received : 13 December 2022
Revised : 21 June 2024
Accepted : 04 July 2024
Published : 13 July 2024
DOI : https://doi.org/10.1038/s41380-024-02663-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Mental Illness
- Mood Disorders
- Clinical Psychology
Bipolar Affective Disorder -Mania with Psychotic Symptoms: A Case Study
- 3(5):164-167
- This person is not on ResearchGate, or hasn't claimed this research yet.

- Eternal University

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- Yogananda R.

- Wan-Ju Tseng
- Lin-Mei Chen
- Chin-Hong Chan

- AM J GERIAT PSYCHIAT
- MW Van Gerpen
- J E Johnson

- Lana A Vornik

- J Lópezcastromán
- E Baca García
- Botillo Martín
- Quintero Gutiérrez Del Álamo
- Navarro Jiménez
- R Negueruelalópez
- R C Kessler
- D R Rubinow
- J M Abelson
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Introduction
- Conclusions
- Article Information
Plots depict standardized group means and standard errors. A, BD PRS: OR, 1.50; P < .001; schizophrenia PRS: OR, 1.30; P = .02. B, BD vs MDD: OR = 1.47; P = .02; BD vs no mood disorder: OR, 1.52; P = .002. ADHD indicates attention-deficit/hyperactivity disorder; BD, bipolar disorder; MDD, major depressive disorder; OR, odds ratio; PRS, polygenic risk score.
Plots depict standardized means and standard errors. A, Significant contrast: BD PRS P = .02. B, Significant contrasts: OBP with mood disorder vs ONBP with no mood disorder ( P < .001), OBP with mood disorder vs OBP with no mood disorder ( P = .003). ADHD indicates attention-deficit/hyperactivity disorder; BD, bipolar disorder; MDD, major depressive disorder; OBP, offspring of parents with bipolar disorder; ONBP, offspring of parents without bipolar disorder; PRS, polygenic risk score.
BD indicates bipolar disorder; HR, hazard ratio; OR, odds ratio.
eFigure 1. Criteria for Bipolar Disorder Not Otherwise Specified (BD-NOS) from the Course and Outcome of Bipolar Youth (COBY) Study
eFigure 2. Flow diagram of genome-wide genotyping quality control and imputation with variant and individual inclusion and exclusion information
eFigure 3. Mediation Path Analysis Predicting Offspring Depressive Disorders Risk
eMethods 1. DNA extraction, genotyping, and polygenic scores
eMethods 2. Additional Statistical Information
eReferences
- Error in Tables JAMA Psychiatry Correction June 1, 2022
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Birmaher B , Hafeman D , Merranko J, et al. Role of Polygenic Risk Score in the Familial Transmission of Bipolar Disorder in Youth. JAMA Psychiatry. 2022;79(2):160–168. doi:10.1001/jamapsychiatry.2021.3700
Manage citations:
© 2024
- Permissions
Role of Polygenic Risk Score in the Familial Transmission of Bipolar Disorder in Youth
- 1 Western Psychiatric Hospital, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania
- 2 Department of Psychiatry, Dalhousie University, Halifax, Nova Scotia, Canada
- 3 Dalhousie Medicine New Brunswick, Dalhousie University, St John, New Brunswick, Canada
- 4 Center for Addiction and Mental Health, University of Toronto Faculty of Medicine, Toronto, Ontario, Canada
- 5 Nationwide Children’s Hospital and Ohio State College of Medicine, Columbus,
- 6 University of Pittsburgh, Pittsburgh, Pennsylvania
- 7 Department of Psychiatry, Dalhousie University, Nova Scotia, Canada
- Correction Error in Tables JAMA Psychiatry
Question Is bipolar disorder (BD) polygenic risk score (PRS) specifically associated with the familial transmission of BD in youth?
Findings In this case-control study of 336 parents and 409 offspring, particularly those with mood disorders showed significantly and specifically higher BD PRS than those without BD. Parental and offspring BD PRS were associated with increased risk for offspring to develop BD, beyond the associations of parental BD diagnosis.
Meaning Specifically higher BD PRS in BD offspring may add to the clinical validation of BD in youth and increases the risk for BD; however, given the BD PRS’s small association, it cannot be used alone to determine risk to develop BD.
Importance Establishing genetic contributions to the transmission of bipolar disorder (BD) from parents to offspring may inform the risk of developing this disorder and further serve to validate BD in youth.
Objective To evaluate the specific association of BD polygenic risk scores (PRSs) on the familial transmission and validity of pediatric BD.
Design, Setting, and Participants This community-based case-control longitudinal study (Pittsburgh Biological Offspring Study) included parents with BD I/II and their offspring and parents without BD (healthy or non-BD psychopathology) and their offspring. Participants were recruited between March 2001 and May 2007, and analysis took place from December 2020 to September 2021.
Exposures PRSs for BD, major depressive disorder, schizophrenia, and attention-deficit/hyperactivity disorder.
Main Outcomes and Measures Participants were prospectively evaluated using standardized interviews blind to parental diagnosis. DNA was extracted from saliva and genotyped. PRSs were constructed based on independent large-scale genome-wide association studies.
Results A total of 156 parents with BD I/II and 180 parents without BD (mean [SD] age, 39.6 [7.9] years; 241 female [72%]) as well as 251 offspring of parents with BD and 158 offspring of parents without BD (mean [SD] age, 10.4 [4.7] years; 213 female [52%]) of European ancestry were analyzed. Participants were assessed a mean of 6.7 times during a mean (SD) of 13 (3.4) years of follow-up (84% retention). More offspring of parents with BD developed BD (58 [23.1%] vs 8 [5.1%]; P < .001) and depression (126 [50.2%] vs 52 [32.9%]; P < .001) compared with offspring of parents without BD. BD PRS was higher in both parents and offspring with BD than parents and offspring without BD (parents: odds ratio, 1.50; 95% CI, 1.19-1.89; P < .001; explained 4.8% of the phenotypic variance vs offspring: hazard ratio, 1.34; 95% CI, 1.03-1.7; P = .02; explained 5.0% of the phenotypic variance). BD PRS did not differ across BD subtypes. In a model combining parental and offspring BD PRS, the parental BD PRS association with offspring BD was fully mediated by offspring BD PRS (hazard ratio, 1.40; 95% CI, 1.05-1.86; P = .02). Parental BD had a stronger direct association than parental or offspring BD PRS with offspring BD risk (hazard ratio, 5.21; 95% CI, 1.86-14.62; P = .002), explaining 30% of the variance. Parental and offspring BD PRS explained 6% of the BD onset variance beyond parental diagnosis. There were no significant between-group differences in PRSs for major depressive disorder, schizophrenia, and attention-deficit/hyperactivity disorder in parents or offspring and they were not significantly associated with BD onset.
Conclusions and Relevance The findings of this study add to the extant clinical validation of BD in youth. Parental BD and offspring BD PRS independently associated with the risk of BD in offspring. Although this is promising, the association of BD PRS was relatively small and cannot be used alone to determine BD risk until further developments occur.
Bipolar disorder (BD) is a familial illness that affects 2% to 3% of youth and is associated with functional impairment and increased risk for suicide and substance use, emphasizing the need for early identification and treatment. 1 - 3
To identify who is at risk of BD, several family high-risk studies in youth have been carried out. 4 - 9 One of the largest and longest studies, the Pittsburgh Bipolar Offspring Study (BIOS), 10 - 12 found that offspring of parents with BD were at elevated, specific risk to develop BD compared with controls (22% vs 4%, respectively). 10 , 11 Parental early-onset BD and symptoms of depression/anxiety, mood lability, and subclinical mania were associated with higher risk of BD. However, these factors alone are insufficient to predict BD, highlighting the need to identify additional predictive factors (eg, biological).
BD is highly heritable, suggesting that genetic information may contribute to risk detection. 10 - 15 Large genome-wide association studies (GWAS) have identified many common genetic variants (single-nucleotide variations [SNVs]) associated with risk for BD. Each SNV accounts for a small proportion of variance in BD risk. 13 , 16 - 20 However, the polygenic risk score (PRS), reflecting the combined effects of many SNVs across the genome, is robustly associated with an individual’s risk to develop the condition of interest. 17 - 20
Studies in adults with BD show that the BD PRS is increased in adults with BD compared with controls, 21 - 28 their unaffected relatives, 23 , 24 , 29 - 31 and adults with depression who developed BD, had family history of BD, early onset, high depressive recurrence rates, or high BD familial burden. 31 , 32 BD PRS has been associated with attention-deficit/hyperactivity disorder (ADHD) and with higher scores in self-reported hypomanic symptoms during adulthood. 25
To our knowledge, only 1 study has examined BD PRS in offspring of parents with BD. This study reported significantly higher BD PRS in offspring of parents with BD (aged 12-30 years) compared with controls. 24 However, this study was cross-sectional, did not report whether the offspring had BD, used a limited panel of SNVs in a mixed-ethnicity sample, and did not include PRSs for other psychiatric disorders. Consequently, the predictive validity and specificity of BD PRS in offspring of parents with BD remain unknown.
In this study, we evaluated whether parents with BD and their offspring had specifically increased BD PRS compared with PRSs for depression, schizophrenia, and ADHD. ADHD PRS was included owing to overlapping symptoms with BD and, although controversial, the reported cotransmission of BD and ADHD. 33 Also, for the first time in the literature to our knowledge, we examined pathways by which parental diagnosis of BD and parental BD PRS influenced the risk for offspring to develop BD.
The methods of Pittsburgh BIOS have been described in prior publications. 10 , 11 Briefly, biological parents with DSM-IV 34 BD I/II who had offspring aged 6 to 18 years were recruited, primarily through advertisements. Schizophrenia and IQ less than 70 were excluded. Community control parents, healthy or with non-BD disorders and without a spouse or first-degree relatives with BD, were recruited at random, group-matched by age, sex, and neighborhood. Participants were recruited from March 2001 to May 2007.
Parents with BD and a subgroup of biological coparents (31%) were assessed for lifetime (intake and follow-up) psychopathology using the Structured Clinical Interview for DSM-IV . 35 Family psychiatric history and psychiatric history of coparents who were not available for direct interview were obtained from the parent proband using the Family History Research Diagnostic Criteria. 36
Offspring were recruited through their parents. Except for IQ less than 70, autism, or conditions that interfered with the evaluation, all offspring were included. Offspring’s lifetime (intake and follow-up) disorders were ascertained by interviewing offspring and parents using the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version. 37 Offspring older than 19 years were assessed using the Structured Clinical Interview for DSM-IV . Specific BD–not otherwise specified (BD-NOS) criteria were used 38 (eFigure 1 in the Supplement ). Socioeconomic status was determined using the Hollingshead scale. 39
Follow-ups were performed every 2 years by trained interviewers who were blind to parents’ diagnoses. A child psychiatrist, also blind to parental diagnosis, confirmed the diagnoses. The κ for diagnostic reliability for each disorder was 0.64 or higher. 10 - 12 The University of Pittsburgh’s institutional review board approved the study, and written consent and/or assent was obtained from offspring and their parents.
For this study, only parents (probands) and biological coparents of European ancestry were included because the discovery GWAS samples included only individuals of this ancestry. 16 - 32 , 40 - 43 After quality control of genetic data (eFigure 2 in the Supplement ), parents with BD I and II, parents without BD, and their offspring were included.
The methods regarding DNA extraction, genotyping, and PRSs are shown in eMethods 1 in the Supplement . Genotypes were pruned using clumping to obtain an independent set of SNVs in linkage equilibrium with r 2 < 0.1 within any 500-kb window. The PRSs were constructed using PRSice-2 44 and the results of meta-analyses of GWAS of BD, schizophrenia, major depressive disorder (MDD), and ADHD using the P value threshold that maximally captured variance in the discovery GWAS sample (BD = .20, MDD = .05, schizophrenia = .05, ADHD = .50). 16 , 40 - 42 , 45 When constructing the PRS, the contribution of each allele was weighted by the effect size of its association with each phenotype in the reference sample GWAS.
Between-group demographic/clinical differences were analyzed using t and χ 2 tests and mixed linear/generalized linear models (random intercept for familial clustering). Associations with multiple categorical outcomes were tested with multinomial logistic regression. Survival analyses modeling the onset of depressive disorders treated BD onset as a competing risk outcome because a BD diagnosis precludes depressive diagnoses; all other survival analyses implemented Cox proportional hazards regression (frailty models accounting for familial clustering; proportional hazards assumption verified via Schoenfeld residuals test) and/or Kaplan-Meier estimation. Associations were estimated as odds ratios (OR) in logistic regressions and hazard ratios (HR) in Cox regressions. Effect sizes were standardized to report the association per 1-SD increase in the PRS. Intercorrelation between PRSs was low (all Pearson r ≤0.25), which enabled the use of multiple regression to estimate and test multiple PRS effects in the same model to try and separate the marginal effects of each. Because genetic analyses can be skewed by population stratification, we used PLINK2 to perform principal component analysis, 46 and all genetic analyses controlled for population structure indexed with 10 principal components of linkage disequilibrium–pruned genetic variants as well as sex. Mediation models implemented robust standard errors to account for familial clustering, tested indirect effects using bootstrap standard errors, and estimated total association as the sum of the direct association and indirect association for each submodel. Percent of variation statistics were estimated using Nagelkerke pseudo R 2 in logistic regressions 47 and the coefficient of explained randomness in Cox regressions. 48 Further details are included in eMethods 2 in the Supplement . Analysis took place from December 2020 to September 2021.
A total of 156 parents with BD (including 2 coparents with BD) (BD I: 115; BD II: 41) and 180 parents (including 90 coparents) without BD were included ( Table 1 ). Offspring included 251 offspring of parents with BD and 158 offspring of parents without BD with a mean (SD) age at intake of 10 (4.7) years ( Table 2 ). Offspring were assessed a mean of 6.7 times over 13 years (mean [SD] age at last follow-up, 23 [5.6] years; retention at last follow-up: offspring of parents with BD, 83%; offspring of parents without BD, 86%).
At intake, compared with parents without BD, parents with BD had lower socioeconomic status, were less likely to be married ( Table 1 ), and had lower overall functioning during follow-up and more lifetime (intake plus follow-up) anxiety disorders, major depressive episodes, psychosis, ADHD, disruptive behavior disorders, and substance use disorder.
Higher BD PRS was significantly associated with BD diagnosis (OR, 1.50; 95% CI, 1.19-1.89; P < .001), explaining 4.8% of the phenotypic variance (BD vs no BD) ( Figure 1 A). Controlling for demographic/clinical differences and family history of BD did not change the results. Increased BD PRS was independently associated with BD I (OR, 1.44; 95% CI, 1.13-1.85; P = .004) and BD II (OR, 1.68; 95% CI, 1.19-2.36; P = .003) vs no BD. There were no significant differences in BD PRS between BD I and II; thus, they were combined for all comparisons. There were no significant associations between BD PRS and age at BD onset as a continuous or a dichotomous measure (older/younger than 18 years).
The schizophrenia PRS was also significantly higher in parents with vs without BD (OR = 1.30; 95% CI, 1.05-1.62; P = .02) ( Figure 1 A) but became nonsignificant after adjusting for confounders (mainly socioeconomic status). Further, after running the models only with BD PRS and then only with schizophrenia PRS, we ran a model with both BD PRS and schizophrenia PRS in the same model, comparing the forward and reverse models. Results indicated that when modeling BD risk with BD PRS and schizophrenia PRS as predictors in the same multiple logistic regression model, the schizophrenia PRS association was nonsignificant (OR, 1.20; 95% CI, 0.96-1.51; P = .10), whereas the BD PRS remained significant (OR, 1.44; 95% CI, 1.14-1.83; P = .003). After adjusting for confounders, the results were similar. There was an insufficient number of parents with psychosis to evaluate whether the high scores in the schizophrenia PRS were associated with these parents. There were no significant between-group differences in the PRSs for MDD or for ADHD.
To evaluate whether higher BD PRS was specific for BD and not for mood disorders in general, parents with BD were compared with 62 parents with unipolar MDD and 118 parents without BD or MDD ( Figure 1 B). BD PRS was significantly higher in parents with BD than those with unipolar MDD (OR, 1.47; 95% CI, 1.07-2.01; P = .02) or without MDD (OR, = 1.52; 95% CI, 1.17-1.97; P = .002). There were no BD PRS differences between parents with or without MDD.
Offspring of parents with BD had significantly lower socioeconomic status and overall functioning, their mothers were younger at offspring birth, and they had more lifetime depression, anxiety, ADHD, disruptive behavior disorders, and substance use disorder than offspring of parents without BD ( Table 2 ). More offspring of parents with BD developed BD (BD I: 18; BD II: 12; BD-NOS: 28) than offspring of parents without BD (BD I: 1; BD II: 3; BD-NOS: 4).
After adjusting for within-family correlations, there were no significant between-group differences in PRSs for MDD, schizophrenia, and ADHD. In contrast, offspring of parents with BD showed significantly higher BD PRS ( F = 5.67, P = .02) ( Figure 2 A). There were no statistical differences in BD PRS between BD I/II and BD-NOS and between offspring of parents with BD with depression vs BD.
There were too few offspring of parents without BD with BD (n = 8) to analyze statistically. Thus, subsequent offspring analyses grouped offspring by mood vs no mood disorder ( Figure 2 B). Offspring of parents with BD with mood disorders had significantly higher mean BD PRSs than offspring of parents without BD with no mood disorders (Cohen d = .51, P < .001) and offspring of parents with BD with no mood disorders (Cohen d = .51, P = .003) and marginally higher mean BD PRS than offspring of parents without BD with a mood disorder (Cohen d = .51, P = .06). Offspring of parents with BD with no mood disorders and offspring of parents without BD and without mood disorders did not significantly differ. Thus, BD PRS differences between offspring of parents with BD and without BD were driven by offspring of parents with BD or depression.
Higher BD PRS was significantly associated with higher BD risk (standardized HR, 1.34; 95% CI, 1.03-1.75; P = .02). BD PRS explained 5.0% of phenotypic variance (BD vs no BD). Within the offspring who developed BD, there were no significant BD PRS associations with BD age of onset (standardized HR, 0.91; 95% CI, 0.74-1.13; P = .40) or significant differences in BD PRS between offspring with BD onset by age 18 years (54 [82%]) vs later (12 [18%]) ( F = 0.21, P = .70). Controlling for between-group demographic/clinical differences and family history of BD in the offspring models above did not change the findings.
As expected, parental BD PRS was significantly associated with parental BD (standardized OR, 1.39; 95% CI, 1.11-1.73; P = .004) and offspring BD PRS with offspring BD (HR, 1.40; 95% CI, 1.05-1.86; P = .02) ( Figure 3 ). Parental BD diagnosis was a strong direct predictor of offspring BD risk (HR, 5.21; 95% CI, 1.86-14.6; P = .002), with no significant indirect association via offspring BD PRS (bootstrap indirect effect P = .17). The parental BD PRS association with offspring BD risk was fully mediated (no significant direct association) by a significant indirect association via offspring BD PRS ( P = .03, accounting for 51% of the total association of parental BD PRS with offspring BD risk, consistent with mendelian predictions). Specifically, each 1-SD increase in parental BD PRS was associated with an increase in offspring BD PRS by an estimated 0.35 SDs (standardized β, 0.35; 95% CI, 0.26-0.44; P < .001), and each 1-SD increase in offspring BD PRS increased hazard of BD onset by an estimated 40% (HR, 1.40; 95% CI, 1.05-1.86; P = .02). In the combined path model, parent/offspring model, parental BD accounted for 30% of the BD risk variation, whereas parental and offspring BD PRS combined model accounted for 6% of offspring variance risk.
Fitting the same path model for risk of depression as the outcome variable, both the direct association of offspring BD PRS (HR, 1.26; 95% CI, 0.98-1.63; P = .06) and indirect association of parental BD PRS via the mediator (offspring BD PRS; bootstrap indirect effect P = .07) were nonsignificant (eFigure 3 in the Supplement ).
In this study, we found that parents with BD had higher BD PRS than parents without BD and a subset of parents with unipolar MDD. Also, offspring of parents with BD, particularly those with mood disorders, showed higher BD PRS than offspring of parents without BD. BD PRS explained a similar proportion of variance of outcome (lifetime BD diagnosis) in parents and offspring (4.8% and 5.0%, respectively). For parents and offspring, there were no significant between-group differences in PRSs for MDD, schizophrenia, or ADHD.
As expected, in a model combining parental and offspring BD PRS, parental BD PRS association with offspring BD risk was fully mediated by the offspring BD PRS. While parental BD had a stronger association than BD PRS, it was still significant beyond the association with parental BD diagnosis. Offspring BD PRS was not significantly associated with depressive disorders.
Replicating studies among adults with BD, 19 - 28 higher BD PRS was significantly associated with BD in parents. We found no significant differences between BD I and II, while the few studies published have reported inconsistent findings. 21 , 23 , 26 Also, comparable with other publications, 21 , 22 , 26 , 28 , 29 , 31 , 32 , 49 parents with BD showed higher schizophrenia PRS than parents without BD, a finding that may be explained by pleiotropy 50 or other factors because this comparison was no longer significant after adjusting for confounders, mainly socioeconomic status. Similar to another adult study, the schizophrenia PRS was no longer significant after including the BD PRS in the model. 32 Because there was a subgroup of parents with unipolar MDD, we further compared this group with parents with BD and found that parents with BD had significantly higher BD PRS than parents with MDD. The above findings together with the lack of differences in MDD PRS and ADHD provide support for a degree of specificity of BD PRS.
Like a prior cross-sectional high-risk study, 24 BD PRS was higher in offspring of parents with BD than offspring of parents without BD. There were no between-group differences in the groups for PRSs for MDD, schizophrenia, and ADHD, again providing further evidence for the specificity of the association between BD PRS and offspring of parents with BD.
Offspring of parents with BD who developed depressive disorders showed comparable BD PRS as offspring with BD suggesting that, at least in youth, BD PRS is associated with mood disorders in general and not only BD. These results are not surprising given that approximately half of the offspring were younger than 21 years at the last follow-up; thus, they had not yet passed through the period of highest risk to develop BD. 1 - 3 These offspring are particularly at risk to develop BD because most of their parents had early-onset BD. 1 , 3 , 11 , 49 Moreover, in adults with unipolar MDD, particularly those with family history of BD, BD PRS was specifically associated with conversion to BD. 49
Because BD is a highly heritable illness, 1 - 3 , 13 , 14 it is expected that genetic factors contribute to the increased risk of BD that is seen among offspring of parents with BD. In fact, we found that the association of parental BD PRS with offspring BD risk was mediated by the offspring BD PRS beyond the associations of parental diagnosis of BD. To our knowledge, only one other study compared the associations of BD PRS and parental history of BD with risk to develop BD in adults with MDD. 49 Mirroring our results, the associations of parental BD were much stronger than the BD PRS; here, we add to the literature the finding that BD PRS and parental BD made independent contributions to offspring risk. Both the current study and most priors PRS studies indicate small associations of PRS. 17 - 20 These findings are explained, at least partly, by the limited number of SNVs included in PRS, 17 - 20 can perhaps be addressed by increasing the sample size of the discovery samples used for GWAS, and as a result the number of SNVs to be included in the PRS. In addition, other factors may account for the small associations of the PRS; for example, existing PRS analyses do not consider the complex interactions among SNVs, the associations of other categories of genetic variants (eg, copy number variants), and environmental factors. 17 - 20
Importantly, for the first time in the pediatric BD literature to our knowledge, this study contributes to the validation of the diagnosis of BD in youth by adding a biological criterion to existing clinical criteria (eg, longitudinal course and family history) necessary to validate the existence of any disorder. 1 , 3 , 51 In fact, offspring showed the same magnitude of genetic risk alleles as their parents with BD, multiple other large-scale studies of adults with BD 20 - 28 , 32 and the original BD GWAS meta-analysis (4.6%). 16 Also, BD PRS in parents were associated with the onset of BD in offspring, controlling for BD PRS in the offspring fully accounted for the increased risk associated with parental genotypes (suggested that it was same risk alleles passed on from parent to offspring), and offspring BD PRS predicted offspring BD even after accounting for parental BD diagnosis in the model, suggesting that the pediatric BD may have similar underlying genetic risk structure to adult BD.
Finally, there were no differences in the BD PRS between offspring with BD I/II and BD-NOS, giving biological evidence in support of the diagnosis of BD-NOS, a BD subtype that increases the risk to develop BD I/II and is as strongly associated with family history of BD, suicidality, and substance use disorder as are BD I/II. 1 , 3 , 38 , 52 , 53
The following limitations need to be considered. Although BIOS is the largest existing high-risk BD study in youth, the sample size of offspring with BD was relatively small. Thus, results that depended on failure to detect differences between subgroups need to be taken cautiously. Also, the discovery GWAS samples predominantly included individuals of European ancestry, 17 - 20 precluding generalization of the results to other groups.
In conclusion, using PRSs for BD, MDD, schizophrenia, and ADHD in a sample of parents with vs without BD and their offspring, this study demonstrated that BD PRS is specifically elevated among parents with BD and among offspring of parents with BD with mood disorders. The BD PRS was associated with increased risk of offspring BD, above and beyond the association of parental BD diagnosis. These results and the finding that BD PRS was associated with similar risk variance to develop BD between adults and offspring with vs without BD and the existing BD PRS literature provide biological evidence for pediatric BD. Although promising, given the small associations, BD PRS is not yet suitable for clinical use to determine individual risk of BD. However, as suggested by the literature, when the methods to derive the PRS improve and the discovery samples become larger, BD PRS has the potential to be useful to predict BD in at-risk populations, inform differential diagnosis (eg, with ADHD or unipolar MDD) and response to treatment, and use in research studies of at-risk youth and youth with BD. 17 - 20 The genetic data used in this study will be reanalyzed once additional associations between SNVs and BD are identified and when methods to include other types of genetic variants and environmental factors into the PRS become available. 17 - 20
Corresponding Author: Boris Birmaher, MD, Western Psychiatric Hospital, 3811 O’Hara St, Bellefield Towers, Room 612, Pittsburgh, PA 15213 ( [email protected] ).
Accepted for Publication: October 24, 2021.
Published Online: December 22, 2021. doi:10.1001/jamapsychiatry.2021.3700
Correction: This article was corrected on April 6, 2022, to fix errors in Tables 1 and 2.
Author Contributions: Dr Birmaher and Mr Merranko had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Birmaher, Axelson, Iyengar, Diler, Nimgaonkar, Uher.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Birmaher, Merranko, Hickey, Diler, Nimgaonkar.
Critical revision of the manuscript for important intellectual content: Birmaher, Hafeman, Zwicker, B. Goldstein, T. Goldstein, Axelson, Monk, Sakolsky, Iyengar, Diler, Nimgaonkar, Uher.
Statistical analysis: Birmaher, Merranko, Zwicker, Hickey, Iyengar, Diler, Uher.
Obtained funding: Birmaher, Axelson.
Administrative, technical, or material support: Birmaher, T. Goldstein, Monk, Hickey, Sakolsky, Diler, Nimgaonkar.
Supervision: Birmaher, T. Goldstein, Axelson, Diler, Uher.
Conflict of Interest Disclosures: Dr Birmaher reports grants from the National Institute of Mental Health (NIMH) during the conduct of the study; support for genetic analyses from the Koplowitz Foundation during the conduct of the study; and royalties from Random House, UpToDate, and Lippincot Williams & Wilkins outside of the submitted work. Dr Hafeman reported grants from Brain & Behavior Research Foundation and NIMH and personal fees from Milken Institute Center for Strategic Philanthropy outside the submitted work. Dr B. Goldstein reports grant funding from Brain Canada, Canadian Institutes of Health Research, Heart and Stroke Foundation of Canada, NIMH, and the Department of Psychiatry at the University of Toronto and acknowledges salary support from the RBC Investments Chair, held at the Centre for Addiction and Mental Health and the University of Toronto Department of Psychiatry. Dr T. Goldstein reported grants from NIMH, American Foundation for Suicide Prevention, Brain & Behavior Research Foundation, and University of Pittsburgh Clinical and Translational Science Institute and royalties from Guilford Press outside the submitted work. Dr Axelson reports grants from NIMH, during the conduct of the study; and royalties from Wolters Kluwer/UpToDate outside the submitted work. Drs Sakolsky and Diler reported grants from NIMH during the conduct of the study. No other disclosures were reported.
Funding/Support: This article was supported by the National Institute of Mental Health (grant RO1 MH060952). The study was also partially funded by the Koplowitz Foundation and the Fine Foundation.
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional Contributions: We thank the studies’ participants and their families, the research assistants, Bernie Devlin, PhD (Western Psychiatric Hospital, University of Pittsburgh School of Medicine), for statistical consultation and editing and Rita Scholle, BA (Western Psychiatric Hospital, University of Pittsburgh School of Medicine), for preparation of the manuscript. Thanks also goes to the Fine Foundation, the Koplowitz Foundation, and the National Institute of Mental Health. We would also like to acknowledge Stacia Friedman-Hill, PhD (National Institute of Mental Health), for her continued encouragement and support. No individuals received compensation.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Author Biographies
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
The role of selected speech signal characteristics in discriminating unipolar and bipolar disorders.

1. Introduction
- Pharmacotherapy—the mood is controlled (i.e., stabilized), and symptoms are alleviated with the help of an adapted and difficult-to-define combination of at least one of the following: antidepressants, antipsychotics, mood stabilizers, and other drugs, e.g., anxiolytics, hypnotics.
- Psychotherapy—patients are trained to manage symptoms and find practical ways to prevent episodes through behavioral and lifestyle choices such as routine sleep, social activity, and appropriate stress management.
- Psychoeducation—patients and their relatives and close friends are taught about the intricacies of unipolar and bipolar disorders, the causes of episode recurrences, and how to deal with the disease.
2. Related Research
2.1. speech-based depression recognition, 2.1.1. datasets, 2.1.2. depression recognition methods.
- Prosodies such as pitch, fundamental frequency (F0), energy, speaking rate, and pauses [ 26 , 27 , 28 ];
- Spectral features like MFCC [ 29 , 30 , 31 ] and LPC [ 32 , 33 ];
- Vocal tract descriptors—formants [ 34 , 35 ];
- Voice quality features, e.g., jitter and shimmer [ 36 ].
2.2. Speech-Based Mania Recognition
2.2.1. datasets, 2.2.2. mania recognition methods.
- Prosodies such as pitch, intensity (energy), rate of speech, and pause duration [ 49 ];
- Spectra-like MFCC [ 47 ] and LPC coefficients [ 50 ].
3. Methodology
3.1. experimental specification.
- Patient voice data related to the daily recordings of the voice samples.
- Sleep data (i.e., Mi Fit band or sleep survey).
- Data on physical activity (e.g., number of steps).
- Other behavioral data (e.g., number of phone calls made).
- The observational part of the clinical trial involved the observation of 100 patients (60 women, 40 men);
- A total of 546 changes in patients’ condition were observed during this period;
- The average age of the patients in the study was 41 years; most of them were single (48), married (37), divorced (13), or widowed (2);
- On average, each patient had 124 recordings of voice samples.
3.2. Speech Signal
3.2.1. fundamental frequency (f0), pitch, 3.2.2. short-time energy, 3.2.3. zero crossing rate (zcr), 3.2.4. pauses, 3.2.5. jitter and shimmer, 3.2.6. lpc and formants, 3.2.7. mfcc, 4.1. feature selection, 4.2. classification, 5. discussion and conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005 , 62 , 617–627. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Anker, S.D.; Morley, J.E.; von Haehling, S. Welcome to the ICD-10 code for sarcopenia. J. Cachexia Sarcopenia Muscle 2016 , 7 , 512–514. [ Google Scholar ] [ PubMed ]
- OECD; European Union. Health at a Glance: Europe 2018: State of Health in the EU Cycle ; OECD: Paris, France, 2018. [ Google Scholar ]
- OECD; European Union. Health at a Glance: Europe 2020 ; OECD: Paris, France, 2020; p. 237. [ Google Scholar ] [ CrossRef ]
- Kessing, L.V.; Andersen, P.K. Predictive effects of previous episodes on the risk of recurrence in depressive and bipolar disorders. Curr. Psychos. Ther. Rep. 2005 , 3 , 123–130. [ Google Scholar ]
- Park, D.Y.; Do, D.; Chang, L.; Shah, S.; Yuen, L.D.; Hooshmand, F.; Wang, P.W.; Miller, S.; Ketter, T.A. Episode accumulation associated with hastened recurrence and delayed recovery in bipolar disorder. J. Affect. Disord. 2018 , 227 , 657–664. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Vieta, E.; Berk, M.; Schulze, T.; Carvalho, A.; Suppes, T.; Calabrese, J.; Gao, K.; Miskowiak, K.; Grande, I. Bipolar disorders. Nat. Rev. Dis. Prim. 2018 , 4 , 18008. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Halfin, A. Depression: The benefits of early and appropriate treatment. Am. J. Manag. Care 2007 , 13 , S92. [ Google Scholar ] [ PubMed ]
- Popova, E.; Benabarre, A.; Cruz, N.; Asenjo, M.A.; Vieta, E. Long-term mental health resource utilisation and cost of care following group psychoeducation or unstructured group support for bipolar disorders: A cost-benefit analysis. J. Clin. Psychiatry 2009 , 70 , 378–386. [ Google Scholar ]
- Sachs, G.S. Bipolar mood disorder: Practical strategies for acute and maintenance phase treatment. J. Clin. Psychopharmacol. 1996 , 16 , 32S–47S. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nicholas, J.; Larsen, M.E.; Proudfoot, J.; Christensen, H. Mobile apps for bipolar disorder: A systematic review of features and content quality. J. Med. Internet Res. 2015 , 17 , e4581. [ Google Scholar ] [ CrossRef ]
- Ekman, P. Facial Action Coding System (FACS). A Human Face ; Oxford University Press: Oxford, UK, 2002. [ Google Scholar ]
- Pease, A.; McIntosh, J.; Cullen, P. Body Language; Camel ; Malor Books: Los Altos, CA, USA, 1981. [ Google Scholar ]
- Izdebski, K. Emotions in the Human Voice, Volume 3: Culture and Perception ; Plural Publishing: San Diego, CA, USA, 2008; Volume 3. [ Google Scholar ]
- Kim, J.; André, E. Emotion recognition based on physiological changes in music listening. IEEE Trans. Pattern Anal. Mach. Intell. 2008 , 30 , 2067–2083. [ Google Scholar ] [ CrossRef ]
- de Melo, W.C.; Granger, E.; Hadid, A. Combining global and local convolutional 3d networks for detecting depression from facial expressions. In Proceedings of the 2019 14th IEEE International Conference on Automatic Face & Gesture Recognition (FG 2019), Lille, France, 14–18 May 2019; pp. 1–8. [ Google Scholar ]
- Li, W.; Wang, Q.; Liu, X.; Yu, Y. Simple action for depression detection: Using kinect-recorded human kinematic skeletal data. BMC Psychiatry 2021 , 21 , 205. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yasin, S.; Hussain, S.A.; Aslan, S.; Raza, I.; Muzammel, M.; Othmani, A. EEG based Major Depressive disorder and Bipolar disorder detection using Neural Networks: A review. Comput. Methods Programs Biomed. 2021 , 202 , 106007. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zangani, C.; Casetta, C.; Saunders, A.S.; Donati, F.; Maggioni, E.; D’Agostino, A. Sleep abnormalities across different clinical stages of Bipolar Disorder: A review of EEG studies. Neurosci. Biobehav. Rev. 2020 , 118 , 247–257. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Abaei, N.; Al Osman, H. A Hybrid Model for Bipolar Disorder Classification from Visual Information. In Proceedings of the International Conference on Acoustics, Speech, and Signal Processing, Barcelona, Spain, 4–8 May 2020; Volume 2020, pp. 4107–4111. [ Google Scholar ]
- Wang, Y.; Lyu, H.L.; Tian, X.H.; Lang, B.; Wang, X.Y.; St Clair, D.; Wu, R.; Zhao, J. The similar eye movement dysfunction between major depressive disorder, bipolar depression and bipolar mania. World J. Biol. Psychiatry 2022 , 23 , 689–702. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Valstar, M.; Schuller, B.; Smith, K.; Almaev, T.; Eyben, F.; Krajewski, J.; Cowie, R.; Pantic, M. Avec 2014: 3d dimensional affect and depression recognition challenge. In Proceedings of the 4th International Workshop on Audio/Visual Emotion Challenge, Orlando, FL, USA, 7 November 2014; pp. 3–10. [ Google Scholar ]
- Gratch, J.; Artstein, R.; Lucas, G.; Stratou, G.; Scherer, S.; Nazarian, A.; Wood, R.; Boberg, J.; DeVault, D.; Marsella, S.; et al. The Distress Analysis Interview Corpus of Human and Computer Interviews ; Technical Report; University of Southern California: Los Angeles, CA, USA, 2014. [ Google Scholar ]
- Ringeval, F.; Schuller, B.; Valstar, M.; Cummins, N.; Cowie, R.; Tavabi, L.; Schmitt, M.; Alisamir, S.; Amiriparian, S.; Messner, E.M.; et al. AVEC 2019 workshop and challenge: State-of-mind, detecting depression with AI, and cross-cultural affect recognition. In Proceedings of the 9th International on Audio/Visual Emotion Challenge and Workshop, Nice, France, 21 October 2019; pp. 3–12. [ Google Scholar ]
- Liu, Z.; Wang, D.; Zhang, L.; Hu, B. A novel decision tree for depression recognition in speech. arXiv 2020 , arXiv:2002.12759. [ Google Scholar ]
- Cohn, J.F.; Kruez, T.S.; Matthews, I.; Yang, Y.; Nguyen, M.H.; Padilla, M.T.; Zhou, F.; De la Torre, F. Detecting depression from facial actions and vocal prosody. In Proceedings of the 2009 3rd International Conference on Affective Computing and Intelligent Interaction and Workshops, Amsterdam, The Netherlands, 10–12 September 2009; pp. 1–7. [ Google Scholar ]
- Yang, Y.; Fairbairn, C.; Cohn, J.F. Detecting depression severity from vocal prosody. IEEE Trans. Affect. Comput. 2012 , 4 , 142–150. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mundt, J.C.; Vogel, A.P.; Feltner, D.E.; Lenderking, W.R. Vocal acoustic biomarkers of depression severity and treatment response. Biol. Psychiatry 2012 , 72 , 580–587. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rejaibi, E.; Komaty, A.; Meriaudeau, F.; Agrebi, S.; Othmani, A. MFCC-based recurrent neural network for automatic clinical depression recognition and assessment from speech. Biomed. Signal Process. Control. 2022 , 71 , 103107. [ Google Scholar ] [ CrossRef ]
- Cummins, N.; Epps, J.; Breakspear, M.; Goecke, R. An investigation of depressed speech detection: Features and normalization. In Proceedings of the 12th Annual Conference of the International Speech Communication Association, Florence, Italy, 27–31 August 2011. [ Google Scholar ]
- Taguchi, T.; Tachikawa, H.; Nemoto, K.; Suzuki, M.; Nagano, T.; Tachibana, R.; Nishimura, M.; Arai, T. Major depressive disorder discrimination using vocal acoustic features. J. Affect. Disord. 2018 , 225 , 214–220. [ Google Scholar ] [ CrossRef ]
- Lopez-Otero, P.; Docio-Fernandez, L.; Garcia-Mateo, C. Assessing speaker independence on a speech-based depression level estimation system. Pattern Recognit. Lett. 2015 , 68 , 343–350. [ Google Scholar ] [ CrossRef ]
- Ringeval, F.; Schuller, B.; Valstar, M.; Gratch, J.; Cowie, R.; Scherer, S.; Mozgai, S.; Cummins, N.; Schmitt, M.; Pantic, M. Avec 2017: Real-life depression, and affect recognition workshop and challenge. In Proceedings of the 7th Annual Workshop on Audio/visual Emotion Challenge, Mountain View, CA, USA, 23 October 2017; pp. 3–9. [ Google Scholar ]
- Cummins, N.; Vlasenko, B.; Sagha, H.; Schuller, B. Enhancing speech-based depression detection through gender dependent vowel-level formant features. In Proceedings of the Conference on Artificial Intelligence in Medicine in Europe, Vienna, Austria, 21–24 June 2017; Springer: Berlin/Heidelberg, Germany, 2017; pp. 209–214. [ Google Scholar ]
- Moore, E.; Clements, M.; Peifer, J.; Weisser, L. Comparing objective feature statistics of speech for classifying clinical depression. In Proceedings of the The 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; Volume 1, pp. 17–20. [ Google Scholar ]
- Alghowinem, S.; Goecke, R.; Wagner, M.; Epps, J.; Breakspear, M.; Parker, G. Detecting depression: A comparison between spontaneous and read speech. In Proceedings of the 2013 IEEE International Conference on Acoustics, Speech and Signal Processing, Vancouver, BC, Canada, 26–31 May 2013; pp. 7547–7551. [ Google Scholar ]
- Jiang, H.; Hu, B.; Liu, Z.; Wang, G.; Zhang, L.; Li, X.; Kang, H. Detecting depression using an ensemble logistic regression model based on multiple speech features. Comput. Math. Methods Med. 2018 , 2018 , 6508319. [ Google Scholar ] [ CrossRef ]
- Sturim, D.; Torres-Carrasquillo, P.A.; Quatieri, T.F.; Malyska, N.; McCree, A. Automatic detection of depression in speech using gaussian mixture modeling with factor analysis. In Proceedings of the Twelfth Annual Conference of the International Speech Communication Association, Florence, Italy, 27–31 August 2011. [ Google Scholar ]
- Wu, P.; Wang, R.; Lin, H.; Zhang, F.; Tu, J.; Sun, M. Automatic depression recognition by intelligent speech signal processing: A systematic survey. CAAI Trans. Intell. Technol. 2022 , 8 , 701–711. [ Google Scholar ] [ CrossRef ]
- Muzammel, M.; Salam, H.; Hoffmann, Y.; Chetouani, M.; Othmani, A. AudVowelConsNet: A phoneme-level based deep CNN architecture for clinical depression diagnosis. Mach. Learn. Appl. 2020 , 2 , 100005. [ Google Scholar ] [ CrossRef ]
- Zhao, Y.; Xie, Y.; Liang, R.; Zhang, L.; Zhao, L.; Liu, C. Detecting Depression from Speech through an Attentive LSTM Network. IEICE Trans. Inf. Syst. 2021 , 104 , 2019–2023. [ Google Scholar ] [ CrossRef ]
- Harati, S.; Crowell, A.; Mayberg, H.; Nemati, S. Depression severity classification from speech emotion. In Proceedings of the 2018 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Honolulu, HI, USA, 18–21 July 2018; pp. 5763–5766. [ Google Scholar ]
- Çiftçi, E.; Kaya, H.; Güleç, H.; Salah, A.A. The turkish audio-visual bipolar disorder corpus. In Proceedings of the 2018 First Asian Conference on Affective Computing and Intelligent Interaction (ACII Asia), Beijing, China, 20–22 May 2018; pp. 1–6. [ Google Scholar ]
- Ringeval, F.; Schuller, B.; Valstar, M.; Cowie, R.; Kaya, H.; Schmitt, M.; Amiriparian, S.; Cummins, N.; Lalanne, D.; Michaud, A.; et al. AVEC 2018 workshop and challenge: Bipolar disorder and cross-cultural affect recognition. In Proceedings of the 2018 on Audio/Visual Emotion Challenge and Workshop, Seoul, Republic of Korea, 22 October 2018; pp. 3–13. [ Google Scholar ]
- Zhang, J.; Pan, Z.; Gui, C.; Xue, T.; Lin, Y.; Zhu, J.; Cui, D. Analysis on speech signal features of manic patients. J. Psychiatr. Res. 2018 , 98 , 59–63. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- McInnis, M.; Ryan, K.; Assari, S.; Evans, S.; Gideon, J.; Khorram, S.; Provost, E. Predicting individual outcomes for rapid intervention (priori). In Bipolar Disorders ; Wiley: Hoboken, NJ, USA, 2017; Volume 19, p. 29. [ Google Scholar ]
- Pan, Z.; Gui, C.; Zhang, J.; Zhu, J.; Cui, D. Detecting manic state of bipolar disorder based on support vector machine and gaussian mixture model using spontaneous speech. Psychiatry Investig. 2018 , 15 , 695. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Faurholt-Jepsen, M.; Rohani, D.A.; Busk, J.; Vinberg, M.; Bardram, J.E.; Kessing, L.V. Voice analyses using smartphone-based data in patients with bipolar disorder, unaffected relatives and healthy control individuals, and during different affective states. Int. J. Bipolar Disord. 2021 , 9 , 38. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Farrús, M.; Codina-Filbà, J.; Escudero, J. Acoustic and prosodic information for home monitoring of bipolar disorder. Health Inform. J. 2021 , 27 , 1460458220972755. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bedi, G.; Carrillo, F.; Cecchi, G.A.; Slezak, D.F.; Sigman, M.; Mota, N.B.; Ribeiro, S.; Javitt, D.C.; Copelli, M.; Corcoran, C.M. Automated analysis of free speech predicts psychosis onset in high-risk youths. NPJ Schizophr. 2015 , 1 , 1–7. [ Google Scholar ] [ CrossRef ]
- Faurholt-Jepsen, M.; Busk, J.; Frost, M.; Vinberg, M.; Christensen, E.M.; Winther, O.; Bardram, J.E.; Kessing, L.V. Voice analysis as an objective state marker in bipolar disorder. Transl. Psychiatry 2016 , 6 , e856. [ Google Scholar ] [ CrossRef ]
- Muaremi, A.; Gravenhorst, F.; Grünerbl, A.; Arnrich, B.; Tröster, G. Assessing bipolar episodes using speech cues derived from phone calls. In Proceedings of the Pervasive Computing Paradigms for Mental Health: 4th International Symposium, MindCare 2014, Tokyo, Japan, 8–9 May 2014; Springer: Berlin/Heidelberg, Germany, 2014; pp. 103–114. [ Google Scholar ]
- Picard, R.W. Affective Computing ; MIT Press: Cambridge, MA, USA, 2000. [ Google Scholar ]
- Williams, C.E.; Stevens, K.N. Emotions and speech: Some acoustical correlates. J. Acoust. Soc. Am. 1972 , 52 , 1238–1250. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nakatsu, R.; Nicholson, J.; Tosa, N. Emotion recognition and its application to computer agents with spontaneous interactive capabilities. In Proceedings of the 7th ACM International Conference on Multimedia (Part 1), Orlando, FL, USA, 30 October–5 November 1999; pp. 343–351. [ Google Scholar ]
- Li, S.; Jain, A. Fundamental Frequency, Pitch, F0. In Encyclopedia of Biometrics ; Springer: Boston, MA, USA, 2009. [ Google Scholar ]
- Jalil, M.; Butt, F.A.; Malik, A. Short-time energy, magnitude, zero crossing rate and autocorrelation measurement for discriminating voiced and unvoiced segments of speech signals. In Proceedings of the 2013 The International Conference On Technological Advances in Electrical, Electronics and Computer Engineering (TAEECE), Konya, Turkey, 9–11 May 2013; pp. 208–212. [ Google Scholar ]
- Ying, S.; Zhang, X. A study of zero-crossings with peak-amplitudes in speech emotion classification. In Proceedings of the 2010 First International Conference on Pervasive Computing, Signal Processing and Applications, Harbin, China, 17–19 September 2010; pp. 328–331. [ Google Scholar ]
- Teixeira, J.P.; Gonçalves, A. Algorithm for jitter and shimmer measurement in pathologic voices. Procedia Comput. Sci. 2016 , 100 , 271–279. [ Google Scholar ] [ CrossRef ]
- Gupta, H.; Gupta, D. LPC and LPCC method of feature extraction in Speech Recognition System. In Proceedings of the 2016 6th International Conference-Cloud System and Big Data Engineering (Confluence), Noida, India, 14–15 January 2016; pp. 498–502. [ Google Scholar ]
- Han, W.; Chan, C.F.; Choy, C.S.; Pun, K.P. An efficient MFCC extraction method in speech recognition. In Proceedings of the 2006 IEEE International Symposium on Circuits and Systems (ISCAS), Kos, Greece, 21–24 May 2006; p. 4. [ Google Scholar ]
- Bogdanov, D.; Wack, N.; Gómez Gutiérrez, E.; Gulati, S.; Boyer, H.; Mayor, O.; Roma Trepat, G.; Salamon, J.; Zapata González, J.R.; Serra, X.; et al. Essentia: An audio analysis library for music information retrieval. Proceedings 14th Conference of the International Society for Music Information Retrieval (ISMIR), Curitiba, Brazil, 4–8 November 2013; Britto, A., Gouyon, F., Dixon, S., Eds.; International Society for Music Information Retrieval (ISMIR): Montreal, QC, Canada, 2013; pp. 493–498. [ Google Scholar ]
- Reeves, S.J.; Zhe, Z. Sequential algorithms for observation selection. IEEE Trans. Signal Process. 1999 , 47 , 123–132. [ Google Scholar ] [ CrossRef ]
- Chen, X.W.; Jeong, J.C. Enhanced recursive feature elimination. In Proceedings of the Sixth International Conference on Machine Learning and Applications (ICMLA 2007), Cincinnati, OH, USA, 13–15 December 2007; pp. 429–435. [ Google Scholar ]
- Vergara, J.R.; Estévez, P.A. A review of feature selection methods based on mutual information. Neural Comput. Appl. 2014 , 24 , 175–186. [ Google Scholar ] [ CrossRef ]
- Mohammad, A.H. Comparing two feature selections methods (information gain and gain ratio) on three different classification algorithms using arabic dataset. J. Theor. Appl. Inf. Technol. 2018 , 96 , 1561–1569. [ Google Scholar ]
- Fonti, V.; Belitser, E. Feature Selection Using Lasso ; Vrije Universiteit Amsterdam: Amsterdam, The Netherlands, 2017; Volume 30, pp. 1–25. [ Google Scholar ]
- Parmar, A.; Katariya, R.; Patel, V. A review on random forest: An ensemble classifier. In Proceedings of the International Conference on Intelligent Data Communication Technologies and Internet of Things (ICICI), Coimbatore, India, 7–8 August 2018; Springer: Berlin/Heidelberg, Germany, 2019; pp. 758–763. [ Google Scholar ]
- Yan, Z.; Xu, C. Combining KNN algorithm and other classifiers. In Proceedings of the 9th IEEE International Conference on Cognitive Informatics (ICCI’10), Beijing, China, 7–9 July 2010; pp. 800–805. [ Google Scholar ]
- Liao, X.; Xue, Y.; Carin, L. Logistic regression with an auxiliary data source. In Proceedings of the 22nd International Conference on Machine Learning, Bonn, Germany, 7–11 August 2005; pp. 505–512. [ Google Scholar ]
- Morariu, D.; Crețulescu, R.; Breazu, M. The weka multilayer perceptron classifier. Int. J. Adv. Stat. It&C Econ. Life Sci. 2017 , 7 . Available online: https://magazines.ulbsibiu.ro/ijasitels/index.php/IJASITELS/article/view/17 (accessed on 13 April 2024).
Click here to enlarge figure
| Dataset | # of Subjects | # of Clips | Recording Method |
|---|---|---|---|
| AVEC2014 [ ] | 84 patients | 300 | reading aloud/questions responding |
| DAIC-WOZ [ ] | 189 patients | 189 | Wizard-of-Oz and automated agent |
| E-DAIC [ ] | 351 patients | 275 | Wizard-of-Oz and automated agent |
| MODMA [ ] | 23 depressed 29 control | 1508 | interviewing, reading, and picture description |
| CGI# | MI | SFS | SBS | LASSO | RFE | IGR |
|---|---|---|---|---|---|---|
| 7 | 71.7/67.7 | 72.6/68.5 | 72.6/68.5 | 72.7/68.3 | 72.2/68.4 | |
| 4 | 76.3/74.2 | 76.9/74.8 | 75.9/73.9 | 75.9/73.9 | ||
| 2 | 92.8/92.8 | 92.4 /92.4 | 92.6/92.6 | 93.0/93.0 | 91.5/91.5 |
| CGI# | MI | SFS | SBS | LASSO | RFE | IGR |
|---|---|---|---|---|---|---|
| 7 | 64.7/64.2 | 66.6/65.9 | 57.3/58.4 | 65.2/64.5 | 67.1/65.5 | |
| 4 | 68.2/67.6 | 66.2/65.8 | 69.2/68.7 | 63.8/63.3 | 70.1/68.7 | |
| 2 | 86.8/86.8 | 87.4/87.4 | 88.0/88.0 | 88.6/88.6 | 87.3/87.3 |
| CGI# | MI | SFS | SBS | LASSO | RFE | IGR |
|---|---|---|---|---|---|---|
| 7 | 57.8/57.6 | 57.7/57.3 | 57.5/57.3 | 57.3/58.4 | 57.6/57.4 | |
| 4 | 64.8/64.7 | 64.2/64.2 | 64.6/64.5 | 64.4/64.3 | 65.4/64.6 | |
| 2 | 81.8/81.8 | 82.6/82.6 | 81.4 /81.4 | 81.6/81.6 | 82.8/82.8 |
| CGI# | MI | SFS | SBS | LASSO | RFE | IGR |
|---|---|---|---|---|---|---|
| 7 | 62.9/62.7 | 69.2/59.9 | 62.3/62.4 | 63.6/63.3 | 63.8/63.4 | |
| 4 | 66.8/66.2 | 68.5/67.8 | 67.1 /66.5 | 68.5/67.8 | 69.0/68.2 | |
| 2 | 76.4/76.4 | 72.6/72.5 | 73.9/73.9 | 73.8 /73.5 | 74.7/74.4 |
| CGI# | MI | SFS | SBS | LASSO | RFE | IGR |
|---|---|---|---|---|---|---|
| 7 | 70.5/66.6 | 68.7/65.1 | 70.0/66.4 | 70.0/65.8 | 69.6/65.8 | |
| 4 | 75.5/73.4 | 75.0/73.8 | 73.6/73.6 | 74.9/72.8 | 75.0/72.8 | |
| 2 | 93.8/93.8 | 94.0 /94.0 | 94.8/94.8 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Kamińska, D.; Kamińska, O.; Sochacka, M.; Sokół-Szawłowska, M. The Role of Selected Speech Signal Characteristics in Discriminating Unipolar and Bipolar Disorders. Sensors 2024 , 24 , 4721. https://doi.org/10.3390/s24144721
Kamińska D, Kamińska O, Sochacka M, Sokół-Szawłowska M. The Role of Selected Speech Signal Characteristics in Discriminating Unipolar and Bipolar Disorders. Sensors . 2024; 24(14):4721. https://doi.org/10.3390/s24144721
Kamińska, Dorota, Olga Kamińska, Małgorzata Sochacka, and Marlena Sokół-Szawłowska. 2024. "The Role of Selected Speech Signal Characteristics in Discriminating Unipolar and Bipolar Disorders" Sensors 24, no. 14: 4721. https://doi.org/10.3390/s24144721
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Fact sheets /
Bipolar disorder
- Bipolar disorder is a mental health condition that affects a person’s mood, energy, activity and thought and is characterized by manic (or hypomanic) and depressive episodes.
- An estimated 40 million people live with bipolar disorder worldwide.
- Bipolar disorder is associated with significant disability and difficulties in many areas of life.
- Many people with bipolar disorder are misdiagnosed or untreated and experience discrimination and stigma.
- There are a range of effective care options, which combine medicines and psychosocial interventions to help people with bipolar disorder stay well.
In 2019, approximately 1 in 150 adults (40 million people, or 0.53% of the global population) were living with bipolar disorder (1) . The condition is primarily observed among working-age people, but also in youth. While the prevalence of bipolar disorder among men and women is approximately equal, available data indicate that women are more often diagnosed.
Worldwide, the treatment coverage for people with bipolar disorder is low. Both men and women are often misdiagnosed. Many lack access to services and recommended interventions, especially in low- and middle-income countries (LMICs).
Stigma and discrimination against people with bipolar disorder are widespread, both in communities and health services. This can undermine access to health care. It also fuels social exclusion and can limit opportunities for education, employment and housing.
Bipolar disorder is one of the leading causes of disability globally as it can affect many areas of life. People with bipolar disorder may experience strained relationships, problems at school or work, and difficulties in carrying out daily activities. Having bipolar disorder also increases the risk of suicide and of developing anxiety and substance use disorders.
People with bipolar disorder are more likely to smoke, use alcohol, have a physical health condition (e.g. cardiovascular or respiratory disease), and experience difficulties in accessing health care. On average, people with bipolar disorder die more than 10 years earlier than the general population (2) .
Symptoms and patterns
Bipolar disorder is a mental health condition characterized by mood swings from one extreme to another.
During a manic episode, a person experiences an extremely high mood with lots of energy (feeling very happy, excited, overactive). They may have a sense of euphoria, sudden shifts in mood or an excess of emotion (uncontrollable laughing or feeling much more irritable, agitated or restless than usual).
In manic episodes, the changes in mood and activities are accompanied by other characteristic symptoms, which may include:
- highly inflated sense of self-worth or self-esteem;
- talking quickly and rapidly shifting from one idea to the next;
- having trouble concentrating and being easily distracted;
- decreased need for sleep;
- reckless or risk-taking behaviour, for example overspending, risky sexual activity, drinking, or harming oneself or others; and
- fixed and mistaken grandiose or persecutory beliefs in something untrue (e.g. “I am a very famous person”, “My neighbour is spying on me”).
On the contrary, during a depressive episode, a person experiences a depressed mood (feeling sad, irritable, empty). They may feel a loss of interest or pleasure in activities that they had previously enjoyed.
Other symptoms are also present, which may include:
- poor concentration
- feelings of excessive guilt or low self-worth
- hopelessness about the future
- thoughts about dying or suicide
- disrupted sleep
- changes in appetite or weight
- feeling very tired or low in energy.
A depressive episode is different from mood fluctuations commonly experienced by most people, in that the symptoms last most of the day, nearly every day, for at least two weeks.
Both manic and depressive episodes can cause significant difficulties in all aspects of life, including at home, work and school. They may require specialized care to prevent the person from doing harm to themselves or others.
Some people with bipolar disorder may experience what are called hypomanic episodes. Hypomanic episodes involve similar symptoms to manic episodes, but the symptoms are less intense and do not typically disrupt the person’s ability to function to the same extent.
There are two main types of bipolar disorder, depending on patterns of manic or hypomanic and depressive episodes.
- People with bipolar type I disorder experience one or more manic episodes interspaced with episodes of depression which usually become more common over time (compared with manic episodes).
- People with bipolar type II disorder have had one or more hypomanic episodes and at least one depressive episode, but no history of manic episodes.
Risks and protective factors
The exact cause of bipolar disorder is unknown. Several factors – including biological (e.g. genetic), psychological, social and structural factors – may contribute to its onset, trajectory and outcomes.
Adverse circumstances or life-altering events can trigger or exacerbate the symptoms of bipolar disorder. These may include bereavement, violence or the breakdown of a relationship. The use of alcohol or drugs can also influence the onset and trajectory of bipolar disorder.
Although employment can be a source of stress for people living with bipolar disorder, it can also be protective. Under good working conditions, and when supported at their workplace with reasonable adjustments, employment can promote recovery by improving functioning, reducing symptoms and leading to a higher quality of life and improved self-esteem.
Treatment and care
Even though symptoms often recur, recovery is possible. With appropriate care, people with bipolar disorder can cope with their symptoms and live meaningful and productive lives.
There are a range of effective treatment options, typically a mix of medicines and psychological and psychosocial interventions. Medicines are considered essential for treatment, but themselves are usually insufficient to achieve full recovery. People with bipolar disorder should be treated with respect and dignity and should be meaningfully involved in care choices, including through shared decision-making regarding treatment and care, balancing effectiveness, side-effects and individual preferences.
People with bipolar disorder need treatment and care across acute episodes of mania and depression and when indicated, longer-term treatment to prevent relapse.
Mood stabilizers (such as lithium, valproate) and antipsychotics are proven to help manage acute mania. Lithium prescription requires clinical and laboratory monitoring. Girls and women who are pregnant, breastfeeding or have childbearing potential should not use valproate. Lithium and carbamazepine also need to be avoided during pregnancy and breastfeeding whenever possible.
Antidepressants should not be taken during a manic episode and they may be combined with mood stabilizers or antipsychotics during episodes of depression.
Some medicines for bipolar disorder can make people feel sleepy, have involuntary muscle spasms or tremors, or experience metabolic changes (e.g. involving weight gain). These side effects can affect adherence to treatment and should be monitored and managed.
Adults with bipolar disorder who are in complete remission (no symptoms) usually need to continue with mood stabilizers or antipsychotic medicines for at least six months. Those experiencing multiple episodes of mania and depression will usually require longer-term treatment to minimize relapses.
Psychological and psychosocial interventions
People with bipolar disorder can benefit from lifestyle changes involving regular sleep, physical activity, a healthy diet, reduction of stressors, and mood monitoring.
Psychological interventions (e.g. cognitive behavioural therapy, interpersonal therapy, psychoeducation) can effectively reduce depressive symptoms and the possibility of them coming back.
Family psychoeducation can also help families understand and support their loved one better. Support from family and friends is very important. Support groups – where people can receive encouragement, learn coping skills, and share experiences – can be helpful to people with bipolar disorder and their families.
Recovery-oriented psychosocial interventions include supported employment, supported housing, peer support, and social and life skills training. They serve to promote hope and to support the autonomy, personal empowerment and social inclusion of people with bipolar disorder.
Medicines and psychological or psychosocial interventions should be tailored to the needs of the person and combined for best outcomes.
WHO response
The Comprehensive Mental Health Action Plan 2013-2030 highlights the steps needed to provide appropriate services for people with mental health conditions, including bipolar disorder. The WHO Special Initiative for Mental Health aims to further progress towards the plan’s objectives by ensuring 100 million more people can access quality and affordable care for mental health conditions.
WHO's Mental Health Gap Action Programme (mhGAP) , which is being implemented in more than 100 countries, provides evidence-based technical guidance, tools and training packages to build capacities and expand treatment coverage for a set of priority conditions, including bipolar disorder, in non-specialized settings in LMICs.
WHO’s guidelines on Management of physical health conditions in adults with severe mental disorders provide evidence-based recommendations to practitioners on how to recognize and manage comorbid physical and mental health conditions, including bipolar disorder.
WHO’s QualityRights initiative aims to improve the quality of care and human rights standards in mental health and social care facilities and to empower organizations to advocate for the health of people with mental health conditions, including bipolar disorder.
The Guidance on community mental health services and person-centred and rights-based approaches describes what person-centred and human rights-based approaches look like in mental health, and give examples of good practice services.
- GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50. doi: 10.1016/S2215-0366(21)00395-3 .
- Kwun Nam Chan J, Ho Yi Yong C, Sau Man Wong C, Yu Hai Chen E, Chung Chang W. Life expectancy and years of potential life lost in bipolar disorder: systematic review and meta-analysis. Br J Psychiatry. 2022;221(3):567–76. doi: 10.1192/bjp.2022.19 .
- mhGAP guideline for mental, neurological and substance use disorders
- mhGAP Intervention Guide - Version 2.
- World Mental Health Report: transforming mental health for al
- More on mental health

IMAGES
VIDEO
COMMENTS
se Report on Bipolar Afective Disorder: Mania with Psychotic SymptomsInvestIgAtIonsBlood investigation findings showed: serum creatinine—0.75 mg/dL, serum urea—15 mg/dL, seru. sodium—142 mEq/dL, serum potassium—5.1 mEq/dL, and serum chloride—101 mEq/dL. She underwent special investigation such as psychometric assessment—young mania ...
Introduction. In the United States, the aggregate twelve-month prevalence rate of DSM-V bipolar I and. II disorders, along with bipolar disorder not otherwise specified, is 1.8%, and the ...
1.5.1. Definition of bipolar disorders. Bipolar disorder is an episodic, potentially life-long, disabling disorder that can be difficult to diagnose. Need to. improve recognition, reduce sub ...
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Theoretical and research basis for treatment. Bipolar disorder is a major psychiatric illness, with a lifetime prevalence of one to three per cent. It is estimated that an adult developing bipolar affective disorder (BPAD) in his/her mid 20s effectively loses nine years of life, 12 years of normal health, and 14 years of work activity.[1]
Abstract. Bipolar disorders (BDs) are recurrent and sometimes chronic disorders of mood that afect around 2% of the world's population and encompass a spectrum between severe elevated and excitable mood states (mania) to the dysphoria, low energy, and despondency of depressive episodes. The illness commonly starts in young adults and is a ...
Gus Alva, MD, DFAPA: Psychiatric Times presents this roundtable on the management of bipolar disorder, a phenomenal dialogue allowing clinicals a perspective regarding current trends and where we may be headed in the future. This is an interesting case, as we take a look at this 23-year-old female who first comes in to see her psychiatrist with moderate depressive symptoms.
Case Study Details. Sarah is a 42-year-old married woman who has a long history of both depressive and hypomanic episodes. Across the years she has been variable diagnoses as having major depression, borderline personality disorder, and most recently, bipolar disorder. Review of symptoms indicates that she indeed have multiple episodes of ...
60 n engl j med 383;1 nejm.org July 2, 2020 The new england journal of medicine tion deficit-hyperactivity disorder (in 10 to 20%). When these additional problems are present, they increase the ...
Disclosure Forms (nejmra1906193_disclosures.pdf) Download; 169.16 KB; ... The economic burden of bipolar disorder: a case study in Southern Iran, Cost Effectiveness and Resource Allocation, 22, 1, ...
PDF | Introduction: Bipolar disorder is a mental illness in which patients often display a significantly disturbed mood and behaviour. ... The work has been supplemented with a case study of a ...
Bipolar disorder (BD) is a major mood disorder characterized by recurrent episodes of depression and (hypo)mania (Goodwin and Jamison 2007).According to the Diagnostic and Statistical Manual 5 (DSM-5), the two main subtypes are BD-I (manic episodes, often combined with depression) and BD-II (hypomanic episodes, combined with depression) (APA 2014).
DS47-2 Case Study 47 Bipolar Disorder Age of onset for both BPI and BPII varies greatly from childhood to age 50 years with a mean age of approximately 21 years. Most cases are diagnosed when individuals are age 15-30 years. Significance Bipolar disorder is often a serious, chronic, and recurring struggle for both patients and their families.
Case Studies in Clinical Psychological Science: Bridging the Gap from Science to Practice William O'Donohue (ed.), Scott ... Chapter 5 covers the psychiatric treatment of bipolar disorder, including a case history, key principles, assessment strategy, differential diagnosis, case formulation, treatment planning, nonspecific factors in treatment ...
A case report: bipolar disorder. ri5, Al-Batool Fahad Ali Al-Mousa5ABSTRACTBackground: Bipolar disorder (BD) is considered as one of the most common chronic diseases among popula-tions that are always conjugated by depression; however, in chronic. cases, it might increase the risk of death. Case presentation: A 65-year-old Saudi male presented ...
Key words: bipolar disorder - migraines - epilepsy - case report * * * * * INTRODUCTION Bipolar disorder; epilepsy and migraines are three common and broad-spectrum disorders, for which their pathophysiological mechanisms still remain uncertain. Epidemiological studies have shown that these condi-tions often exist as co-morbidities (Ortiz ...
This case study looked at Bipolar I and Bipolar II disorder. Specifically, the researcher focused on understanding the different mood episodes of the participants through the determining factor involved in bipolar disorder like family background, educational background, social economic status, and other behavioral observations along with each management of bipolar disorder. data was gathered ...
Description of disease 1.5.1. Definition of bipolar disorders Bipolar disorder is an episodic, potentially life-long, disabling disorder that can be difficult to diagnose. Need to improve recognition, reduce sub-optimal care and improve long-term outcomes. There is variation in management of care across healthcare settings. 1 1.2.
According to the diagnostic criteria of DSM -5, symptoms. of a depressive episode include depressed mood, sign ificant. changes in sleep patterns and appetite, psychomoto r agitation or ...
case study on Mania - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. This document provides background information and details regarding a case study of a 27-year-old female patient diagnosed with mania. It includes sections on the patient's bio-data, presenting complaints, history of present illness, past history, personal history, family ...
As in our case, the majority of individuals who ultimately develop bipolar disorder report a depressive episode first , but the later age of onset of manic symptoms and temporal relationship to TBI lends credence to the TBI's primary role in the development of manic symptoms. In the case presented here, the patient exhibited a combination of ...
Deepika, K. (2019). conducted a study on a case report on bipolar affective disorder: Mania with psychotic symptoms. The study adopted the method of a case study which aims to find the key characteristics and implications of mania with psychotic symptoms. Akdemir, D., & Gokler, B. (2017) conducted a study on
Bipolar Disorder (BD) imposes considerable economic and social burdens on the community. Therefore, the present study aimed to determine the economic burden of bipolar disorder in patients referred to single-specialty psychiatric hospitals at the secondary and tertiary care level in 2022. This partial economic evaluation was conducted as a cross-sectional study in the south of Iran in 2022 ...
Lifestyle factors are being increasingly studied in bipolar disorder (BD) due to their possible effects on both course of disease and physical health. The aim of this study was to jointly describe and explore the interrelations between diet patterns, exercise, pharmacological treatment with course of disease and metabolic profile in BD. Methods
Bipolar disorder (BD) collectively terms a group of chronic psychiatric disorders characterized by recurrent manic and depressive episodes. With a lifetime prevalence of 1%, BD is a leading ...
Abstract. Bipolar disorder (formerly called manic-depressive illness or manic depression) is a mental disorder that causes unusual shifts in mood, energy, activity levels, concentration, and the ...
Question Is bipolar disorder (BD) polygenic risk score (PRS) specifically associated with the familial transmission of BD in youth? Findings In this case-control study of 336 parents and 409 offspring, particularly those with mood disorders showed significantly and specifically higher BD PRS than those without BD. Parental and offspring BD PRS ...
Objective:The objective of this study is to explore and enhance the diagnostic process of unipolar and bipolar disorders. The primary focus is on leveraging automated processes to improve the accuracy and accessibility of diagnosis. The study aims to introduce an audio corpus collected from patients diagnosed with these disorders, annotated using the Clinical Global Impressions Scale (CGI) by ...
Bipolar disorder is one of the leading causes of disability globally as it can affect many areas of life. People with bipolar disorder may experience strained relationships, problems at school or work, and difficulties in carrying out daily activities. ... 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet ...