- Subscribe to journal Subscribe
- Get new issue alerts Get alerts

Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Anabolic-Androgenic Steroid Use in Sports, Health, and Society
BHASIN, SHALENDER; HATFIELD, DISA L.; HOFFMAN, JAY R.; KRAEMER, WILLIAM J.; LABOTZ, MICHELE; PHILLIPS, STUART M.; RATAMESS, NICHOLAS A.
1 Department of Medicine, Brigham and Women’s Hospital, Boston, MA
2 Department of Kinesiology, University of Rhode Island, Kingston, RI
3 Department of Physical Therapy, Ariel University, Ariel, Israel
4 Department of Human Sciences, The Ohio State University, Columbus, OH
5 InterMed, P.A., South Portland, ME
6 Department of Pediatrics, Tufts University School of Medicine, Boston, MA
7 Department of Kinesiology, McMaster University, Hamilton, ON
8 Department of Health and Exercise Science, The College of New Jersey, Ewing, NJ
Address for correspondence: Stuart M. Phillips, Ph.D., F.A.C.S.M., Department of Kinesiology, McMaster University Ivor Wynne Centre 1280 Main St, West Hamilton, Ontario, Canada L8S 4K1; E-mail: [email protected] .
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site ( www.acsm-msse.org ).
This consensus statement is an update of the 1987 American College of Sports Medicine (ACSM) position stand on the use of anabolic-androgenic steroids (AAS). Substantial data have been collected since the previous position stand, and AAS use patterns have changed significantly. The ACSM acknowledges that lawful and ethical therapeutic use of AAS is now an accepted mainstream treatment for several clinical disorders; however, there is increased recognition that AAS are commonly used illicitly to enhance performance and appearance in several segments of the population, including competitive athletes. The illicit use of AAS by competitive athletes is contrary to the rules and ethics of many sport governing bodies. Thus, the ACSM deplores the illicit use of AAS for athletic and recreational purposes. This consensus statement provides a brief history of AAS use, an update on the science of how we now understand AAS to be working metabolically/biochemically, potential side effects, the prevalence of use among athletes, and the use of AAS in clinical scenarios.
This consensus statement is an update of the previous position stand from the American College of Sports Medicine (ACSM), published in 1987 ( 1 ). Since then, a substantial amount of scientific data on anabolic-androgenic steroids (AAS) has emerged and the circumstances of AAS use has evolved in the athletic, recreational, and clinical communities. The objective of this consensus statement is to provide readers with a brief summary of the current evidence and extend the recommendations provided in the 1987 document ( 1 ). Key topics discussed are the brief history of AAS, epidemiology, methods, and patterns of AAS use, androgen physiology and ergogenic effects, side effects of AAS, and clinical uses of AAS (see Box 1). The writing group used the rating system of the National Heart Lung and Blood Institute ( Table 1 ) and a consensus approach to synthesize the available evidence from clinical trials and case reports, narrative and systematic reviews, and meta-analyses ( 3 ). The recommendations represent the consensus of the writing panel, the ACSM, and incorporate guidance from other professional organizations with expertise in the area.
| Evidence Category | Sources of Evidence | Definition |
|---|---|---|
| A | RCT (rich body of data) | Evidence is from endpoints of well-designed RCT (or trials that depart only minimally from randomization) that provide a consistent pattern of findings in the population for which the recommendation is made. Category A therefore requires substantial numbers of studies involving substantial numbers of participants. |
| B | RCT (limited body of data) | Evidence is from endpoints of intervention studies that include only a limited number of RCT, or subgroup analysis of RCT, or meta-analysis of RCT. In general, Category B pertains when few randomized trials exist, they are small in size, and the trial results are somewhat inconsistent, or the trials were undertaken in a population that differs from the target population of the recommendation. |
| C | Non-RCT and observational studies | Evidence is from outcomes of uncontrolled or nonrandomized trials or from observational studies. |
| D | Panel consensus judgment | Expert judgment is based on the panel’s synthesis of evidence from experimental research described in the literature and/or derived from the consensus of panel members based on clinical experience or knowledge that does not meet the above-listed criteria. This category is used only in cases where the provision of some guidance was deemed valuable but an adequately compelling clinical literature addressing the subject of the recommendation was deemed insufficient to justify placement in one of the other categories (A through C) |
BOX 1. ACSM Consensus Statements and Recommendations Summary.
Consensus Statements and Recommendations
- 1. The administration of AAS in a dose-dependent manner significantly increases muscle strength, lean body mass, endurance, and power. The effects are primarily seen when AAS use is accompanied by a progressive training program. Evidence Category A .
- 2. Historically, AAS use was primarily seen in competitive athletes and aspiring bodybuilders and powerlifters. Recreational AAS use appears to have surpassed athletic AAS use indicated by survey prevalence estimates demonstrating that recreational trainees are the leading consumers of AAS. The ACSM deplores the illicit use of AAS for recreational purposes. Evidence Category C .
- 3. AAS are classified as schedule III drugs, banned by several sport governing bodies, and are illegal to use for athletic purposes. The ACSM deplores the illicit use of AAS for recreational use and performance enhancement in athletes. Evidence Category D .
- 4. Coaches, trainers, and medical staffs should monitor and be cognizant of visible signs of AAS use and abuse. These include (but are not limited to): a substantial increase in muscle mass, strength, and power in a relatively short period of time (or the reverse which could denote AAS withdrawal); acne that is resistant to medical treatment; development of unexplainable rash, gynecomastia, increased body hair, and prominent increases in surface vascularity; changes in temperament, mood, and aggressive behavior (severe depression or suicidality could indicate AAS withdrawal); facial masculinization and fluid retention; and muscle mass that appears disproportionate to body structure or pubertal status in young athletes. In addition, the presence of AAS-related materials (books, articles, websites, dealer information, needles, vials) on the individual could reflect intent and may warrant further dialogue from the coaching, trainer, and medical staffs. Medical staff should be aware of regulations and documentation requirements regarding use of AAS for athletes with medical indications for their use. Evidence Category C .
- 5. Use and abuse of AAS is associated with several notable adverse effects in men and women including (but not limited to) suppression of the hypothalamic-pituitary-gonadal axis, psychological changes, immunosuppression, and unhealthy cardiovascular, hematological, reproductive, hepatic, renal, integumentary, musculoskeletal, and metabolic effects. Several adverse effects may be reversible upon discontinuation but some could pose health risks beyond the duration of AAS use. Evidence Category B .
- 6. Use of AAS in prepubertal and peripubertal children may lead to early virilization, premature growth plate closure, and reduced stature. Evidence Category C .
- 7. Coaches, trainers, and medical staffs should be cognizant of the reasons for AAS use and abuse and deter use when possible. Prevention programs based on education may assist; and providing the individual with scientific nutrition and training advice is a recommended strategy to mitigate the temptation of AAS use. Evidence Category D .
- 8. Androgen replacement therapy is approved for the medical treatment of several clinical diseases and abnormalities. The ACSM acknowledges the lawful and ethical use of AAS for clinical purposes and supports the physicians’ ability to provide androgen therapy to patients when deemed medically necessary. The reader is referred to guidelines established by the Endocrine Society ( 4 ). Evidence Category C .
INTRODUCTION
Anabolic-androgenic steroids are drugs chemically and pharmacologically related to testosterone (T) that promote muscle growth and are not estrogens, progestins, or corticosteroids. An androgen is any natural or synthetic steroid hormone capable of promoting the development of male primary and secondary sexual characteristics via binding to androgen receptors at the tissue level. The term anabolic describes a hormone or other substance capable of enhancing the growth of somatic tissue, such as skeletal muscle and bone. In a sport-related setting, this is typically used to describe the enhancement of skeletal muscle. Table 2 presents nomenclature associated with AAS. In the United States, AAS are classified as Schedule III controlled substances ( 5 ). Although AAS have legitimate medicinal use, nontherapeutic use among athletes and recreationally active young men and women is performed to improve strength, power, increase muscle mass, and improve appearance. Athletic and recreational (i.e., noncompetitive) use of AAS has been widespread over the last 50 yr, creating considerable interest by the scientific and medical communities, as well as sport governing bodies, in examining the potential medical, legal, and ethical issues surrounding the use of these substances. All major national and international sports organizations have banned the illicit use of AAS by athletes.
| Testosterone | Hormone with strong anabolic and androgenic effects. produced by the testes in males. lesser quantities are produced by ovaries in women and by the adrenal glands in both sexes. the hypothalamus and pituitary regulate testosterone production in humans. |
| Testosterone derivative | Chemically altered testosterone resulting in changes in solubility, pharmacokinetics, and/or clinical effects. |
| Testosterone esters | Testosterone derivative with an ester group bound to testosterone to enhance oil solubility. This slows testosterone absorption and increases duration of effect, and allows for depot injections of testosterone |
| SARM | Drugs designed to optimize anabolic tissue growth, while minimizing androgenic side effects. No current clinical applications, but research suggests potential therapeutic benefit in cancer, prostatic hyperplasia, and hypogonadism |
| Designer anabolic-androgenic steroids | Synthetic steroids fabricated with intent to evade drug testing, or current laws prohibiting nonprescribed use |
| Testosterone enhancers/boosters | Variety of substances purported to increase testosterone levels or effects, usually by increasing endogenous testosterone production or decreasing metabolism |
| HCG | An analog to LH. Stimulates Leydig cells in the testes. Increases testosterone levels and sperm production |
| Clomiphene citrate (Clomid) | Estrogen receptor modulator. Increases LH production. Has been shown relieve hypogonadal symptoms and maintain testosterone levels in men with symptomatic hypogonadism for up to 3 yr |
| Kisspeptins | Peptide that appears to be important for onset of puberty and regulation of sperm production. Current evidence not definitive in regards to effects on androgen production in humans. |
HISTORICAL PERSPECTIVES
Anabolic-androgenic steroids use has been examined extensively in various chapters, books, meta-analyses, and reviews ( 5–12 ). The effects of testicular extracts and castration on animals and humans have been a source of fascination for thousands of years ( 13,14 ). Suggestions that the consumption of testis tissue could improve impotence were noted ~140 BC ( 13 ). The mid 1700s to late 1800s marked a time where interest in testicular endocrinology increased ( 14 ). Table 3 depicts a brief historical timeline of some key events in AAS use in athletes. Testosterone was synthesized and biochemically described in the late 1920s and 1930s, and a host of different synthetic variations have been developed since ( 5,15,16 ). Testosterone or AAS use by athletes began in the 1940s and 1950s, and increased considerably thereafter, culminating in high usage during the 1968 Olympic Games ( 5,6 ). It has been speculated that the first appearance of AAS use among female athletes dates back to the late 1950s/early 1960s in Soviet track and field athletes ( 17 ).
| Year | Event |
|---|---|
| 1889 | Brown-Sequard suggest increases in muscle strength and endurance can occur following the injection of testicular extracts over a span of 2 wk |
| 1896 | Zoth and Pregel first suggested androgen use in athletes and investigated effects of testicular extracts on muscular strength and athletic performance |
| 1927 | Fred Koch and Lemuel McGee (University of Chicago) isolated an impure but potent form of T by pulverizing several tons of bull testicles |
| 1928 | The IAAF were first to ban doping agents |
| 1935 | Testosterone was isolated and the first two papers on testosterone synthesis were published—oral and injectable preparations were available to the medical community shortly thereafter—Kochakian reported T stimulates anabolism and suggested therapies could be useful for several disorders |
| Early 1940s | Case studies suggested that human subjects were given testosterone in Germany and undocumented reports suggested AAS was administered to German soldiers during World War II |
| 1942 | Samuels, Henschel, and Keys published “Influence of methyl testosterone on muscular work and creatine metabolism in normal young men” in the Journal of Clinical Endocrinology and Metabolism—an early study investigating AAS in men |
| 1945 | De Kruif published “The Male Hormone” and suggested interest in athletes using testosterone to see the beneficial effects |
| Late 1940s | West Coast bodybuilders began experimenting with T preparations |
| 1952 | Legendary strength athlete and coach Bob Hoffman of York Barbell speculates that Soviet athletes were using hormones during the Olympic Games |
| 1954 | Dr. John Ziegler was told by Soviet coaches that Soviet Weightlifters were using testosterone—he returned to United States and experimented on himself along with some weightlifters |
| 1958 | Ciba Pharmaceutical Company manufactured Dianabol—soon thereafter Dr. Ziegler began administering the drug to some of the York Barbell Weightlifting team |
| 1963 | Reports of NFL players first using AAS |
| 1964 | Androgen use increased greatly primarily in strength and power sports |
| 1965 | Oral Turinabol was synthesized by a German state-owned pharmaceutical company A few scientists gained interest in studying AAS and performance in men as 2 studies were published between 1965 and 1969 |
| 1967 | The IOC established a medical commission and developed a list of prohibited substances and methods |
| 1968 | Large increases in AAS use was seen including stacking and doses exceeding 2–5 times therapeutic doses—estimated that at least 1/3 of US track & field team and most of the German team used drugs in the 1968 Olympics |
| 1969 | The editor of Track & Field News (John Hendershott) called AAS the “Breakfast of Champions” |
| 1973–1974 | First testing procedures for androgens proposed radioimmunoassay and gas chromatography and mass spectrometry (RIA, GC-MS) and used in 1974 at the Commonwealth Games in Auckland New Zealand where 9 of 55 samples testing positive for androgens |
| 1976 | Drug testing instituted at the Olympic Games in Montreal—only 8 of 275 tests were deemed positive despite the majority of athletes admitting to using AAS in training—athletes began shifting to T from AAS as a result of drug testing |
| 1976 | The ACSM National Conference included a symposium and roundtable meeting on AAS in sports—two polarized groups evolved: those who thought AAS were “fool’s gold” or “myth” versus those who understood the ergogenic potential of the drugs—the prevailing medical opinion was that AAS were ineffective until the 1980s (possibly to dissuade use in part) which lead to mistrust between athletes and the medical community leading athletes to the black market for drugs and information |
| 1977 | The ACSM publishes the “Position statement on the use and abuse of anabolic-androgenic steroids in sports”—concluded that “… there is no conclusive evidence that extremely large doses of anabolic-androgenic steroids either aid or hinder performance …” |
| 1980 | Dr. Manfred Donike developed a method for testing testosterone—the 6:1 T:E ratio |
| 1981 | 1st edition of the (by Dan Duchaine [nicknamed “The Steroid Guru”]) was published |
| 1982–1983 | Methods to circumvent T:E ratio (i.e., use of hCG, clomiphene, epitestosterone, and timing of T administration) were used to enable doping without detection |
| 1984 | ACSM National Conference included symposium on “Drug Use in Sports” with >12 scientific presentations with several focusing on AAS in athletes |
| 1987 | The ACSM publishes an updated position stand “The use of anabolic-androgenic steroids in sports”—revised position to AAS in the presence of an adequate diet and training can contribute to increases in lean body weight and muscular strength |
| 1988 | Testing for masking agents and diuretics begins—US government passes the Anti-Drug Abuse Act which made distribution or possession of AAS for nonmedical reasons a federal offense |
| 1990 | US government passes Anabolic Steroid Control Act—inserted 27 AAS and related drugs as Class III drugs where simple possession could result in incarceration |
| 1994 | US Congress passes Dietary Supplement Health and Education Act to protect consumers from certain substances |
| 2001 | The WADA was formed |
| 2002 | The advent of designer AAS began |
| 2004 | The Anabolic Steroid Control Act is revised to include 26 new compounds including prohormones |
| 2005 | T:E ratio lowered to 4:1 by WADA for a positive doping test |
The sophistication of AAS use by athletes in the late 1960s was characterized by a host of different “stacking routines” (i.e., the consumption of two or more drugs in an attempt to improve the response) using various oral and injectable AAS preparations ( 5 ). Initially, many physicians did not believe AAS improved performance, and the International Olympic Committee (IOC) did not include AAS on the banned substance list. The ACSM adopted this position in their first AAS position stand in 1977 but later corrected in the 1987 publication ( 1 ). Although the 1970s marked a time where AAS use was known mostly among competitive athletes, the 1980s marked a time where AAS use spread well beyond athletics to gyms, health clubs, and public awareness of AAS use increased. The Anti-Drug Abuse Act (1988), Anabolic Steroid Control Act (1990, 2004), and Dietary Supplement Health and Education Act (1994) were enacted, in part, to stem the growing use of AAS. Only a few studies (~17) on AAS use and strength/hypertrophy increases were conducted before the 1980s, and these cumulatively showed minimal effects in untrained men, but significant responses in trained men, despite doses less than that used by many athletes ( 6,7,10 ). The sophisticated protocols and array of drugs used recreationally and by athletes remained a “black box” from a research perspective.
Of current concern is the ease by which AAS users may obtain AAS via the Internet and the proliferation of men’s health clinics. In addition to the use of AAS by competitive athletes, a growing segment of AAS users are nonathletes. Management of men with damaged hypothalamic-pituitary-gonadal regulatory pathways became a new area of medicine resulting in indiscriminate AAS use ( 18 ). Interest in AAS persists as research identifies new information regarding the performance and health aspects of the drugs and through stories of purported use in the sports world. The World Anti-Doping Agency (WADA) has developed new antidoping measures, including blood sampling, guidelines for international information gathering and sharing and revamping their “Athlete Biological Passport” guidelines. While AAS use in sports continues, increases in AAS use in the general population appear to have outpaced athletic use in the last decade ( 19 ).
EPIDEMIOLOGY OF AAS USE
Peer-reviewed studies examining the frequency of illicit AAS use have declined in the past decade despite concern over the growing AAS epidemic in the United States. These studies often rely on self-reports and are fraught with sampling bias, small sample sizes, possible confusion regarding supplement and AAS use, and suboptimal ascertainment ( 5 ). Many AAS users are secretive, with one survey finding that 56% of respondents would not disclose their physicians’ use ( 20 ). Athletes may be unwilling to discuss their use with researchers even when anonymity and confidentially are guaranteed for fear it may jeopardize their career; thus, leading to differences in what athletes reported on surveys versus their actual activities ( 21 ).
In 2014, the National Institute on Drug Abuse estimated that 1.3 million Americans were AAS users, while the Endocrine Society estimated between 2.9 and 4.0 million Americans have used AAS at some point in their lives ( 18,22,23 ). Other reports showed that the number of users might be as high as 4 million men in the United States, with ~100,000 new AAS users annually ( 6,23,24 ). The age of onset of use begins later than most drugs, with only 6% of users starting before 18 ( 23 ).
Although the general public and medical communities attribute AAS use primarily to competitive athletes ( 6 ), research does not support this misperception. Muscle dysmorphia (“megarexia”) is a dominant risk factor for illicit AAS use and indicates that AAS use is often used in pursuit of a more muscular appearance rather than for enhanced athletic performance ( 25 ). Recreationally active individuals age 15 to 24 yr are more likely to use AAS than athletes participating in organized sport ( 26 ). However, reports on the prevalence of illicit AAS use in athlete and nonathlete populations are widely variable. Anabolic-androgenic steroids have been reported in 9% to 67% of elite athletes, while reports of AAS use among gym attendees ranged from 3.5% to 80% ( 27 ). In all areas, men report higher prevalence than women, although the prevalence in women is increasing ( 28 ). Studies in girls have shown prevalence rates between 0.4% and 1.0% in adolescents, ~1.2% in collegiate athletes, and ~10.3% in elite athletes ( 27 ). Others have reported AAS use in young athletes ranging between 0.6% and 6.6% in teenage boys, 0.0% to 3.3% in teenage girls, and between 0.8% and 9.1% for collegiate male athletes ( 29–32 ). Peer-reviewed studies report the highest prevalence of use in weightlifters, powerlifters and bodybuilders, with rates ranging from 33.3% to 79.5% ( 31,33 ).
Several studies have examined sport and activity participation among self-reported AAS users. A survey study of >500 male AAS users (mean age of 29) showed ~70% were recreational exercisers versus 12% competitive bodybuilders, 8% competitive weightlifters, and 9% competitive athletes in other sports ( 34 ). Participation in high school sports was not associated with an increased risk of AAS use ( 34 ). A survey of 12 female AAS users indicated that 33% of the women were recreational users, while 67% participated in competitive bodybuilding and weightlifting. These women used a polypharmacy approach, but their weekly dose was lower than male AAS users ( 35 ). Female users were less likely to stack, more likely to pyramid and less likely to inject AAS than male users ( 35 ).
Rates of AAS use in athletes are sometimes inferred from rates of positive doping tests. However, this data has some inherent limitations, including ongoing updates to banned substances lists, variable drug testing methodologies, and variable lists of targeted substances tested by organizations that do not follow WADA protocols. It has been estimated that drug testing alone may underestimate drug use in elite athletes by 8-fold ( 21 ). The Anti-Doping Administration and Management System maintained by WADA now allows any sports body to share drug testing information. While AAS use in particular divisions, such as men’s vs women’s and underage athletes is still difficult to obtain, the testing databases now include much larger numbers of athletes than in the past. Anabolic agents constitute 87% of atypical findings reported by WADA and 46% of all adverse analytical findings (International Amateur Athletics Federation) ( 36,37 ). Stanazolol and nandrolone have the highest number of AAF at 20% and 14%, respectively, while an “unidentified anabolic agent” (e.g., “designer” AAS) was the third most common at 11% ( 36 ).
The true nature of AAS use and abuse in athletes and recreationally trained individuals is difficult to discern and is often underestimated. In addition to surveys and doping results, other sources of information on AAS use include investigated journalism and government hearings. Unfortunately, all of these methods have significant methodological issues that reduce their estimation accuracy ( 17 ). Journalists have interviewed current and former athletes, coaches, team physicians, and trainers whose estimate of AAS use in sports is much higher than survey reports. There has been an inconsistency between the number of individuals demonstrating signs of AAS use and the statistical prevalence generated via surveys. Drug testing is often limited by circumventing positive tests and has done little to quantify “real-life” use or dissuade AAS use at high levels of competition. Obtaining accurate measures of AAS use in athletes is difficult given the challenges of reducing bias; testing issues, and sincerity needed during interviews and survey completion, for example, fear of accountability, fear of loss of potential income or suspension, or fear of being perceived as a cheater or athlete who needed drugs to be successful.
Attempts have been made to identify the type of individual prone to using AAS ( 38–40 ). Hildebrandt et al. ( 39 ) reported 4 clusters of users from highest to lowest risk, each with different levels of motivation for AAS use: 1) polypharmacy (i.e., use of multiple drugs) approach with high risk (~11%); 2) fat burning (~17%); 3) muscle building (~21%); and 4) low-risk use designed to reduce fat and build muscle (~52%). Others have reported a four-level typology: 1) expert type (exemplifies controlled risk-taking, is knowledgeable about AAS and fascinated with effects on the human body, is scientific and may be focused on muscularity); 2) athlete type (interested in performance enhancement and is competitive); 3) well-being type (interested in looking and feeling good with low risk-taking); and 4) YOLO “You Only Live Once” type (is haphazard using risky behavior, quick improvements, impressing others and peer recognition is important) ( 38,40 ). Despite the typology, athletes’ motivation to use AAS is multi-faceted and influenced by many factors ( Table 4 ).
| ↑ muscle mass, strength, power, endurance, speed, fitness levels, energy, blood volume, BMD | Encouragement from friends, family, coaches to do so |
| ↑ sex drive | ↑ recovery between workouts and competitions, pain tolerance |
| ↑ athletic success, chances of winning, individual performance, strive to maximize potential | Fear their opponents are using and they must use AAS in order to maintain competitive balance |
| ↑ social recognition, peer acceptance, self-confidence, aggression, mental intensity and alertness | Lack of fear in getting caught or being held accountable by sport governing bodies |
| ↑ financial gain, chance at scholarship, notoriety | ↓ body fat and injury risk, ↑ weight loss |
| Improve appearance, self-esteem, mood, personal protection | ↓ aging effects, likelihood of muscle dysmorphia |
Several extensive, national studies indicate an overall downward trend in lifetime AAS use among adolescents since peaking in the early 2000s ( 42 ). Monitoring the Future (MTF) is administered annually to a sample of 8th, 10th, and 12th grade students ( 43 ). The MTF reported peak prevalence rates for lifetime AAS use in 2000 to 2002 of 3% to 4% compared with 2018 data in Table 5 (i.e., ~1%–3%). The Youth Risk Behavior Survey (YRBS) is administered annually to a sample of high school students and reports an overall prevalence of 2.9% in 2017 (See Table 6 ), after peaking in 2001 at 5% ( 44 ). Although the YRBS is widely cited, concern has been raised that the term “steroid” is vague and potentially conflated with corticosteroids or steroid-like dietary supplements ( 45 ). Surveys that delineate the type of steroid show usage rates that are markedly lower than those seen in the YRBS data ( 45 ). Although AAS use rates in adolescents are low, ~1 in 8 AAS users initiates their use before age 18 ( 23 ). Several correlates of increased AAS use risk in this group include fitness-related activity ( 46,47 ); weight-related concerns (perceptions of very underweight or overweight status) ( 48,49 ); sexual preference and gender identity ( 25,44 ); and race and ethnicity ( 43,44 ). Some view current AAS use as an epidemic given the emergence of AAS availability through internet/mail order and “backroom” laboratories ( 18,50 ).
| 8th Grade | 10th Grade | 12th Grade | |
|---|---|---|---|
| Overall | 1.1% | 1.2% | 1.6% |
| Male | 1.0% | 1.3% | 2.2% |
| Female | 1.1% | 0.9% | 0.9% |
| White | 1.0% | 1.1% | 1.4% |
| African American | 1.2% | 1.3% | 2.9% |
| Hispanic | 1.1% | 1.0% | 1.3% |
| Overall | Females | Males | |
|---|---|---|---|
| Ever used steroids | 2.9% | 2.4% | 3.3% |
| By race/ethnicity | |||
| Black | 2.2% | 1.8% | 2.7% |
| White | 3.6% | 2.6% | 4.6% |
| Hispanic | 3.5% | 3.1% | 3.8% |
| By sexual contact | |||
| Opposite sex only | 3.9% | 2.6% | 4.9% |
| Same sex or both sexes | 8.0% | 7.2% | 10.1% |
| No sexual contact | 0.7% | 1.0% | 0.5% |
METHODS/PATTERNS OF AAS USE
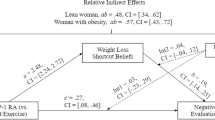
Patterns of AAS use in athletes and resistance-trained populations vary greatly and depend upon: AAS type, self-administration routes, dosages, cycling patterns and durations, and ancillary drugs. A “polypharmacy approach” is commonly used where supraphysiologic doses of injectable and oral AAS are stacked and pyramided progressively in cycles, while ancillary drugs are consumed to minimize side effects, promote other areas of health and fitness, and/or enhance T levels during off-cycles, or periods in between cycles ( Table 7 ). Figure 1 depicts survey results from two studies on usage patterns for >2400 predominately male AAS users ( 34,41 ). These studies indicated that 99.2% of users reported using injectable AAS or a combination of oral and injectable AAS, and >40% used ancillary drugs, such as antiestrogens ( 41 ). Ip et al. ( 34 ) reported that 79% of AAS users “stacked” drugs, 18% used the “pyramid” approach (i.e., where drug intake is progressively increased, plateaus, and then is decreased or tapered until the end of the cycle), and only 9% thought physicians and pharmacists were knowledgeable about AAS. Interestingly, AAS users spent an average of 268 ± 472 h researching AAS prior to use ( 34 ).
| AAS | |
|---|---|
| Anabol 4–19 (norclostebol acetate) | Myagen (bolasterone) |
| Anadrol (oxymetholone) | Parabolan (trenbolone hexahydrobenzylcarbonate) |
| Anavar (oxandrolone) | |
| Cheque drops (mibolerone) | Primobolan (methenolone) |
| Dianabol (methandrostenolone) | Primobolan depot (methenolone enanthate) |
| Deca durabolin (nandrolone decanoate) | Proviron (mesterolone) |
| Durabolin (nandrolone phenylproprionate) | Testosterone (androderm, AndroGel, Striant, testoderm) |
| Dynabol (nandrolone cypionate) | |
| Dynabolan (nandrolone undecanoate) | Testosterone blend (Sustanon, Omnadren, Equitest, Sten, Testoviron) |
| Equipoise (boldenone undecanoate) | |
| Finajet (trenbolone acetate) | Testosterone cypionate (Depo-Testosterone) |
| Genabol (norbolethone) | TE (Delatestryl) |
| Halotestin (fluoxymesterone) | Testosterone proprionate (Oreton) |
| Madol (desoxymethyltestosterone) | Testosterone suspension (Andronaq) |
| Masteron (drostanolone) | Tetrahydrogestrinone |
| Metandren (methyltestosterone) | Trenabol (trenbolone enanthate) |
| Metribolone (methyltrienolone) | Turinabol (chlorodehydromethyltestosterone) |
| Miotolan (furazabol) | Winstrol (stanozolol) |
| Banned Prohormone/OTC Steroids | |
| 1-Testosterone | Epi-DHT |
| 4-Hydroxytestosterone | 19-Norandrostenediol |
| Boldione | 19-Norandrostenedione |
| Androstenediol, 1-,4-Androstenediol | Halodrol |
| Androstenedione, 1-, 5-Androstenedione | Superdrol |
| 1-Androsterone | Methylhydroxynandrolone |
| Androstanolone | Prostanozol |
| Epiandrosterone, 1-Epiandrosterone | |
| Andarine (S4) | RAD-140 (testolone) |
| Ligandrol (LGD-4033) | YK-11 |
| Ostarine (enobosarm) | |
| Antiestrogens | |
| Arimidex (anastrozole) | Faslodex (fulvestrant) |
| Aromasin (exemestane) | Femara (letrozole) |
| Clomid (clomiphene citrate) | Fertodur (cyclofenil) |
| Cytadren (aminoglutethimide) | Lentaron (formestane) |
| Evista (raloxifene) | Nolvadex (tamoxifen citrate) |
| Fareston (toremifene citrate) | Teslac (testolactone) |
| Ancillary Drugs | |
| Accutane (isotretinoin) | Lasix (furosemide) |
| Cardarine | Cytomel (liothyronine sodium) |
| Abuterol | Synthroid (levothyroxine sodium) |
| Clenbuterol | Human growth hormone (somatotropin, protropin, nutropin, humatrope, genotropin, norditropin) |
| Ephedrine | |
| HCG | |
| Catapres | GHRH secratogues (CJC-1295, Mod GRF 1–29, Egrifta [tesamorelin acetate], Geref [sermorelin acetate]) |
| Aldactone (spironolactone) | |
| Dyrenium (triamterene) | |
| Hydrodiuril (hydrochlorthiazide) | Growth hormone releasing peptides (Lenomorelin [Ghrelin]. GHRP-1 to GHRP-6, hexarelin [examorelin], ipamorelin, ibutamoren mesylate [MK-677]) |
| Epitestosterone | |
| Probenecid (masking agent) | |
| Synthol (site enhancer) | |
| GH fragments (HGH fragment 176–191, AOD-9604) | |
| IGF-1 and variants (Increlex [mecasermin]) | |
| Mechano growth factor | |
| Insulin | |

ANDROGEN PHYSIOLOGY
Testosterone is the principal androgen and has both androgenic (masculinizing) and anabolic (tissue building) effects. Testosterone is synthesized from cholesterol via the Δ-4 or Δ-5 pathways through the sequential action of several enzymes ( Fig. 2 ). In men, >95% of T is synthesized in the Leydig cells of the testes (with smaller adrenal contributions) under control of the hypothalamic-anterior pituitary-gonadal axis where gonadotropin-releasing hormone stimulates the release of luteinizing hormone (LH). Healthy men produce ~4 to 9 mg of T per day (10–35 nmol·L −1 ) whereas women have approximately 0.5 to 2.3 nmol·L −1 of circulating T in the blood ( 5 ). Gonadotropin-releasing hormone function is under the control of hypothalamic neuropeptides, such as kisspeptins, neurokinin-B, dynorphin-A, and phoenixins ( 51 ). In women, androgens are produced primarily by the ovaries and adrenal glands ( 52 ). Skeletal muscle produces small amounts of androgens ( 53 ). Testosterone circulates in the blood bound to sex hormone-binding globulin (44%–60%), albumin, orosomucoid, and cortisol-binding globulin. Testosterone and other 19-carbon androgens can be converted to 5α-dihydrotestosterone (DHT) by the action of steroid 5α-reductase or converted to estradiol or estrone by the aromatase enzyme. The liver inactivates T, and the resultant metabolites are excreted in the urine.

Androgens perform many ergogenic, anabolic, and anticatabolic functions in skeletal muscle and neuronal tissue, leading to increased muscle strength, power, endurance, and hypertrophy in a dose-dependent manner ( 54 ). A meta-analysis concluded that short-term AAS use increases muscle strength substantially more than placebo and that strength gains and muscle hypertrophy are greater in trained individuals than in nontrained individuals ( 55 ). Gains in body mass and lean body mass (LBM) of ~5% to 20% from AAS use have been reported ( 56 ). Figure 3 depicts some physiological ramifications of androgens that could affect physical performance. However, the findings of controlled clinical trials of T and other AAS may differ from the practical experience of athletes due to the inclusion of mostly untrained subjects in controlled clinical trials; the use of lower doses of T or AAS in clinical trials than those used by many athletes; the use of multiple AAS in stacks with other drugs over long periods; and differences in nutritional patterns, training programs, and study design ( 5,27 ).

Exogenous androgens are often administered orally or parenterally but are also available in cream, nasal spray, buccal, subcutaneous pellets, patches, and gel. Orally administered T is absorbed well but is degraded rapidly. The esterification of the 17-beta-hydroxyl group (e.g., T enanthate, cypionate, decanoate, undecanoate, propionate) makes the androgen more hydrophobic, causing a slow release from the muscle into circulation, increasing the duration of action. When administered intramuscularly, the androgen ester is slowly absorbed into the circulation, where it is then rapidly de-esterified by esterase enzymes to T. Intrinsic potency, bioavailability, and rate of clearance from the circulation are determinants of the biological activity. Other oral and injectable AAS are T, DHT, or 19-nortestosterone derivatives (e.g., methyltestosterone, methandrostenolone, fluoxymesterone, nandrolone decanoate, oxandrolone, trenbolone, stanozolol, and other designer-AAS).
An important and relevant question is how long the effects of a dose of AAS would last in an athlete? That is, how long would potential strength gains or gains in muscle mass persist? The answer to the question is undoubtedly complex and dependent on the AAS being used and their potency (see Fig. 1 ), the history of AAS in the athlete ( 57 ), the athlete’s training age, sex ( 58,59 ), and potentially the developmental stage of the athlete relative to puberty and adulthood (i.e., 18 yr of age). The literature in this area is, unsurprisingly, sparse, but some studies suggest that the effects of AAS persist for weeks after taking the steroids, but at ~12 wk after taking AAS that the effects, at least insofar as strength and muscle mass are concerned, are largely absent ( 55,60 ). For example, Giorgi et al. ( 61 ) showed that testosterone enanthate (TE) (3.5 mg·kg −1 ) administration for 12 wk during training resulted in greater increases in strength, muscle girth, and muscle thickness than a group given a placebo. However, after 12 wk without TE administration, but while still training, there was a reversion of strength and muscle in the TE group to levels no different from the placebo group. In contrast, others have observed preservation of AAS-induced gains in strength and LBM that persist after AAS usage has ceased, at least in the short-term ( 62 ).
Persistent and long-term (at least 5 yr) AAS use in a mixed sample of strength (strongman and powerlifters) and aesthetic sport (bodybuilding) athletes has been reported, in comparison to non-AAS, to result in persistent (i.e., in comparison to a matched group) elevations in LBM, muscle fiber area, capillary density, myonuclei density, and strength that were dose-dependent ( 57 ). The observation that long-term AAS use results in increased myonuclei density ( 57 ) suggesting that a much longer ‘muscle memory’ is perhaps possible in AAS users, particularly those who use AAS early in life. Evidence for such a mechanism comes from preclinical models ( 10 ), where young mice were exposed to AAS and subsequently increased their myonuclear content, resulting in a substantial hypertrophic advantage later in life. The authors of this work ( 63 ) even went so far as to suggest, “… the benefits of even episodic drug [AAS] abuse might be long lasting, if not permanent, in athletes. Our data suggest that the World Anti-Doping Code calling for only 2 yr of ineligibility after… [a doping violation for AAS] use… should be reconsidered.” Support for whether an AAS-induced increase in myonuclear number in humans is lacking; however, if present, then AAS-induced increases in myonuclei are theoretically advantageous to an athlete even if strength and lean mass advantages have been lost.
Residual effects of endogenous testosterone exposure in testosterone-suppressed transgender females are areas of active study and debate. These effects vary greatly depending upon the developmental stage of treatment initiation and will be much less when treatment is initiated before pubertal onset. There is a dichotomy when looking at measures of prepubertal athletic performance. Studies evaluating age-group athletic records report no significant differences in top age-group performances between boys and girls younger than 10 to 12 yr old ( 64–66 ). However, some studies evaluating more specific measures of strength and aerobic capacity reveal an 8% to 10% advantage in prepubertal biologic males relative to females, even after normalizing for body size ( 67,68 ). These performance differences may be residual effects from higher testosterone levels during early infancy (e.g., “mini-puberty”) and/or nonandrogenic genetic factors. Currently, there are no data on the durability of these performance differences in transgender females who start gender-affirming treatment before puberty.
Postpubertal testosterone suppression has variable impacts on performance-related parameters. Within 3 months of starting hormone suppression, hematocrit decreases by 4% to within normal values for cisgender females ( 69 ). A recent systematic review also evaluated evidence to date regarding treatment-related reductions in muscle size, strength, and LBM ( 70 ), summarized in Table 8 . Although the changes documented in Table 8 , along with an increase in fat mass, may contribute to significant reductions in athletic performance, the current lack of data in active or athletic populations makes the magnitude of these changes difficult to assess.
| Cisgender Males (Reference) | Cisgender Females (Relative to Cisgender Males) | Transgender Females (Pretreatment, Relative to Cisgender Males) | Reductions in Transgender Females with T Supression (12 mo Posttreatment) | |
|---|---|---|---|---|
| LBM | 100 | 70% | 94%–92% | −1% to 5.5%* |
| Muscle CSA | 100 | 94%–88% | −1.5% to 12% | |
| Strength | 100 | 64% (handgrip) | 90%–86% (handgrip) | 1.5% to –7% (handgrip) |
ANDROGEN SIGNALING
Androgen signaling at the tissue level occurs primarily genomically through the classical androgen receptor (AR) with multiple levels of integration with other anabolic/catabolic pathways ( 71 ). Testosterone, DHT, and other AAS bind to cytoplasmic AR ( 72 ). Androgen receptor activity is altered at various sites; phosphorylation may augment androgen/AR transcriptional action (in the presence or absence of androgens) ( 73 ). Androgen receptor signaling is activated primarily by ligand binding, but under some circumstances through ligand-independent mechanisms (e.g., insulin like-growth factor-1 [IGF-1] induced mitogen-activated protein kinase-ERK1/2, p38 and c-Jun N-terminal kinase phosphorylation) ( 74 ) that may sensitize it to anabolic signals in the presence of low androgens ( 75 ). The AR is up-regulated following resistance training and short-term androgen administration ( 54 ).
Upon androgen binding to the ligand-binding domain (LBD) of the AR, the liganded AR undergoes phosphorylation, dimerization, and conformational changes, recruits coregulators, and translocates into the nucleus, where it regulates the transcription of androgen response elements (ARE) of the androgen-responsive genes ( 76 ). Androgen binding activates and stabilizes the AR, which is selectively induced by T, DHT, and AAS ( 77 ). Greater stability is seen with DHT than T ( 78 ). Binding affinity for the AR varies between androgens. Nandrolone and metenolone have a higher binding affinity than T, while stanozolol, methandienone, and fluoxymesterone have a lower binding affinity than T; and oxymetholone has a minimal binding affinity ( 79 ). Androgen binding to the AR completes the pocket that serves as a recruiting surface for co-activators ( 80 ). Some co-activators include BAF57 and 60a, SRC1 and 3, and ARA50 and 74. The activity of these co-regulators and the role of T in ribosome biogenesis may be important in mediating the anabolic effects of AAS on skeletal muscle.
Androgen/AR binding activates signaling through the Wnt-β-catenin pathway. The presence of T (in a dose-dependent manner) increases AR-β-catenin interaction and transcriptional capacity ( 81 ). Androgens promote myogenesis via multiple pathways. Satellite cells and myoblasts express AR and androgen binding, increasing satellite cell activation, proliferation, mobilization, differentiation, and incorporation into skeletal muscle ( 82 ). Androgens increase myogenesis via increased Notch signaling of satellite cells ( 83 ) and increased expression of IGF-1 ( 84 ). Androgen binding to AR on pluripotent mesenchymal cells increases their commitment to myogenesis and inhibits adipogenic differentiation via β-catenin signaling ( 85,86 ). Testosterone upregulates follistatin expression (which blocks signaling through the TGFβ-SMAD 2/3) and increases myogenic differentiation ( 82,84,86–88 ). Androgens may be anticatabolic by decreasing glucocorticoid receptor (GR) expression, interfering with cortisol binding, or the AR-T complex may compete with the cortisol-GR complex for cis -element binding sites on DNA ( 88–91 ).
Nongenomic AR signaling is rapid, with short latency periods acting independently of nuclear receptors ( 92 ). Nongenomic effects are thought to be mediated by direct binding to a target molecule, through intracellular AR activation (i.e., Src kinase), through a transmembrane AR receptor, or via changes in membrane fluidity ( 92 ). Nongenomic signaling involving G-protein 2nd messenger system and may either increase intracellular calcium concentrations via PI3K, phospholipase C, and IP 3 signaling ( 93 ), stimulate the activation of mitogen-activated protein kinase signaling ( 94 ), and mammalian target of rapamycin pathway signaling ( 95 ). Cross-talk between IGF-1 signaling and nongenomic AR signaling appears critical to mediating some anabolic effects ( 96 ). Nongenomic signaling occurs rapidly within seconds to minutes, much faster than classic genomic signaling, which takes hours and requires the constant presence of androgens to maintain intracellular signaling.
SIDE EFFECTS ASSOCIATED WITH ANDROGEN USE AND ABUSE
Investigations examining the safety of androgen use in various populations have been largely inadequate as there is tremendous variability in androgen dosages and patterns of use, including stacking of multiple AAS and concurrent use of accessory drugs ( 5 ). Figure 4 depicts the variety of adverse physiological and psychological effects associated with AAS use. These include relatively rare effects and those that are commonly expected, particularly with long-term AAS abuse ( 30 ).

A survey of 500 AAS users (99% male) who had extensive experience (8 wk to 25 yr with 95% having >1–3 yr of AAS use) with high doses showed that 23% to 64% of respondents reported minor side effects (e.g., testicular atrophy, acne, fluid retention, insomnia, sexual dysfunction, gynecomastia) ( 97 ). Other common effects of AAS use include deleterious changes in cardiovascular (CV) risk factors: decreased plasma high-density lipoprotein (HDL) cholesterol ( 98 ), changes in clotting factors ( 99 ), and mood or psychiatric disturbances ( 79 ). Suppression of the hypothalamic-pituitary-testicular axis and spermatogenesis may result in infertility, while elevations in liver enzymes may reflect liver dysfunction ( 100–102 ). In one study, competitive athletes who used AAS during their competitive careers were more likely to die prematurely than athletes who did not ( 103 ). The use of nonsterile needles and needle sharing practices for intramuscular injections increase the risk for infection, muscle abscess, sepsis, and communicable diseases, such as human immunodeficiency virus (HIV) and hepatitis B and C ( 5 ).
Although CV effects are commonly reported with AAS use, based on an extensive review, the FDA concluded that “... the studies have significant limitations that weaken their evidentiary value for confirming a causal relationship between testosterone and adverse cardiovascular outcomes ” ( 104 ). Part of the difficulty in studying the effects of AAS on CV health is that the impacts of androgens on CV function vary with dose, method of administration, and aromatization potential ( 5 ). Parenteral administration of physiologic T replacement doses are associated with CV function and vary with dose, method of administration, and aromatization potential ( 5 ) with small decreases in plasma HDL, with little or no effect on total cholesterol, low-density lipoprotein (LDL) or triglycerides ( 105–107 ). However, supraphysiologic T doses are associated with significant reductions in HDL ( 108,109 ). Orally administered 17-alpha-alkylated, nonaromatizing AAS produce greater reductions in HDL and increases in LDL than when AAS are administered parenterally ( 110 ). Angell et al. ( 111 ) reported that self-administering AAS (median daily dose = 228 mg) for >2 yr was associated with smaller longitudinal LV strain, right ventricular (RV) ejection fraction, and altered diastolic function compared with nonusers. Others showed impaired RV free wall strain and strain rate associations with AAS abuse in competitive bodybuilders ( 112 ). D’Andrea et al. ( 113 ) showed associations between AAS use (~31 wk; weekly dose = 525 mg) and left atrial impairment (a marker of diastolic burden) in elite bodybuilders compared with nonusers. An increase in left ventricular (LV) mass occurs during resistance training ( 114–116 ); however, potential additional effects from AAS use in humans are unclear. In rats, only high T doses (up to 20 mg per kg body mass) induced cardiac hypertrophy with an impaired contractile process ( 117 ).
Deceased men who had used AAS showed greater cardiac mass than nonusers ( 118 ). Multivariate analysis indicated that increases in heart size were explained by increased body mass and by AAS use. Risk for adverse cardiac events associated with LV mass is supported by case reports detailing sudden death among power athletes who self-administered AAS ( 100,119–122 ). Case reports are largely anecdotal, and a causal relationship between AAS use and risk of sudden death has not been established. Strength/power athletes self-administering AAS have short QT intervals but increased QT dispersion compared with endurance athletes with similar LV mass who have long QT intervals but do not have increased QT dispersion ( 123 ). The interval from the peak to the end of the ECG T wave (Tp-e), Tp-e/QT ratio, and Tp-e/QTc ratio increases in AAS users, suggesting a link between AAS and ventricular arrhythmias, which may increase the risk for sudden death ( 124 ).
Increases in liver enzymes, cholestatic jaundice, hepatic neoplasms, and peliosis hepatis are associated with the use of oral, 17-alpha alkylated AAS ( 102,125,126 ), but not with parenterally administered T or its esters ( 127 ). The association between liver toxicity and AAS use is based on increases in AST and ALT. These enzymes are not liver-specific and are often elevated from muscle damage after resistance exercise ( 101,128 ); thus, possibly overstating the risk of hepatic dysfunction ( 128,129 ).
Endogenous LH and follicle stimulating hormone secretion are suppressed during AAS use, with subsequent effects on testicular T secretion and sperm count ( 130,131 ). Depending on the dose and duration of AAS use, endogenous T, LH, and follicle stimulating hormone may take weeks to months to return to homeostatic levels ( 132 ), and the long-term effects are not well understood. High-dose androgen administration in men is associated with breast tenderness and enlargement, for example, gynecomastia ( 5,133 ), thought to result from peripheral conversion of androgens to estrogens in men administering aromatizable AAS ( 134 ). The prevalence of gynecomastia is unknown, but prevalence rates as high as 54% were reported in AAS users ( 5 ). The use of nonsterile needles and needle-sharing practices for intramuscular injections increases the risk for infection, muscle abscess, sepsis, and communicable diseases, such as HIV and hepatitis B and C ( 5 ).
There is no evidence that T causes prostate cancer, but testosterone replacement therapy (TRT) is associated with a small increase in prostate specific antigen levels in older men with low T, which increases the risk of urological referral for prostate biopsy ( 5 ). Because many older men harbor subclinical prostate cancer, a prostate biopsy may lead to subclinical low-grade prostate cancer detection. Notably, however, TRT increases the risk of prostate biopsy.
The psychological effects of AAS use have garnered much publicity, especially on issues of aggression and suicide. However, the evidence is inconclusive due to the lack of sensitivity of the research instruments used to measure aggressive behavior, large variability in RT programs, preexisting personality or psychiatric disorders, and prevalence of multiple high-risk behaviors and use of other substances, such as alcohol, psychoactive drugs, and dietary supplements ( 5 ). Interestingly, physiologic T replacement in hypogonadal men may improve mood and attenuate negative aspects of mood ( 4 ). Morrison et al. ( 135 ) reported that the aggression and anxiety-provoking influences of androgens in animals are likely a developmental phenomenon and that adult exposure may be anxiolytic over the long term. However, underlying psychological dysfunction may cause a greater susceptibility to AAS use, and high doses of AAS may provoke a “rage” reaction in some individuals with preexisting psychopathology ( 136,137 ). Self-administration of AAS may increase the risk for mood disorders, such as mania, hypomania and depression ( 136,138 ). Resting T concentrations are related to posttraumatic stress (PTSD), in which higher T is associated with a lower risk for PTSD ( 139 ). Further, long-term use of AAS in former weightlifters was associated with poor cognitive function and negative changes in brain morphology ( 140,141 ). Approximately 30% of illicit AAS users will develop AAS dependence, and there is some overlap between AAS dependence and the mechanisms and risk for opioid dependence ( 142,143 ). Sudden discontinuation of exogenous AAS use in those who are dependent or have suppressed endogenous production may result in severe depression and suicidality ( 142,143 ). A multidisciplinary and medically supervised treatment program is indicated for individuals with AAS dependence.
Women self-administering AAS may undergo masculinization and experience hirsutism, deepening of the voice, enlargement of the clitoris, widening of the upper torso, decreased breast size, menstrual irregularities, and male pattern baldness ( 144 ). Some of these adverse effects may not be reversible ( 5 ).
Many of the side effects in adults may be seen in adolescents, but information on use in children is scant. Exogenous AAS exposure in preadolescence triggers pubertal onset and may result in early epiphyseal maturation and closure, leading to loss of ultimate height potential ( 40 ). Although mild acne is common during adolescence ( 40 ), AAS use may result in severe nodular acne, particularly on the back and shoulders, which is often resistant to treatment.
CLINICAL USES OF ANDROGEN THERAPY
Although athletes and recreational trainees have reported obtaining AAS from physicians for illicit purposes ( 26,33,50 ), several clinically approved uses of T exist. Of concern are potential illicit use stemming from a clinical prescription of T given the increased number of antiaging and wellness clinics. The sale of therapeutic T preparations in the United States quadrupled between 2001 and 2011 ( 145 ), and an estimated >2.3 million men received physician-prescribed T therapy as of 2013 ( 146 ). In military treatment facilities, the number of androgen prescriptions increased > twofold (23% per year) from 2007 to 2011, mainly in 35- to-44-yr-old men ( 147 ). Currently, therapeutic T is mostly used to treat primary (i.e., testicular failure) and secondary (i.e., reduced LH) hypogonadism ( 148 ). Androgen therapy has numerous clinical uses outlined in Table 9 ( 145,146 ). A substantial fraction of young men receiving T prescriptions are former AAS users trying to restore endogenous T production ( 149–151 ). The Endocrine Society Clinical Practice Guideline ( 148 ) details decision making regarding androgen therapy and the reader is referred to their specific guidelines on the diagnosis, treatment, and monitoring of hypogonadism in men ( 134 ).
| Male hypogonadism |
| Primary |
| Examples: Testicular trauma/torsion/irradiation, cryptorchidism, orchiectomy, Klinefelter syndrome, chromosome abnormalities, LH and follicle stimulating hormone receptor gene mutations, androgen synthesis disorders, myotonic dystrophy, hypothyroidism |
| Secondary |
| Examples: Irradiation/tumor of hypothalamus or pituitary, drugs/medications (opioids, marijuana, glucocorticoids, AAS), alcoholism, sleep deprivation, surgery, trauma, eating disorder/relative energy deficiency, Kallman syndrome, Prader-Willi syndrome |
| Mixed primary and secondary |
| Examples: diabetes, obesity, HIV infection, chronic obstructive pulmonary disease, chronic kidney disease, liver disease, aging, cancer |
| Hypoactive sexual desire disorder in postmenopausal females |
| Constitutional delay of growth and puberty |
| Gender-affirming treatment for transgender males |
| Contraindications: |
| Cancer: prostate, breast, skin |
| High prostate specific antigen |
| Erythrocytosis/polycythemia |
| Sleep apnea |
| Venous thromboembolism |
| CV disease |
| Fertility problems |
Testosterone replacement therapy has been shown to improve sexual activity ( 152–155 ), vertebral and femoral bone mineral density (BMD) and microarchitecture ( 156,157 ), hemoglobin content ( 158,159 ), LBM, maximal voluntary strength and physical function ( 160–164 ), and reduces body fat and BMI ( 162,165,166 ). There have also been reports of TRT reducing neuroinflammation and depressive symptoms ( 167–169 ), reducing blood pressure and improving lipid profiles ( 166 ), and neuronal regeneration ( 154,156,170–177 ), and may not change or improve cognitive function in older men ( 174,178,179 ). There is a low frequency of adverse events associated with TRT ( 2,148,153,180–190 ). However, all TRT should be accompanied by a structured monitoring plan ( 148 ). The Endocrine Society recommends evaluating symptoms, adverse events, lower urinary tract symptoms, and measurements of T levels, hematocrit, and prostate specific antigen at baseline, 3 to 6 months after starting treatment, and annually thereafter ( 148 ).
Testosterone and free T levels decline with advancing age after peaking in the second and third decades of life ( 191–194 ), leading to increased risk of sexual dysfunction; decreased muscle mass and strength, BMD, mobility; increased falls and fractures, late-life low grade persistent depressive disorder (dysthymia), and CV mortality ( 148,195 ). Low T is associated with an increased risk of diabetes, metabolic syndrome, and increased carotid artery intima-media thickness ( 196,197 ). Whether older men with age-related T decline should receive TRT remains a matter of debate. The Endocrine Society Guideline for TRT of hypogonadal men recommends against routinely prescribing T to all men, 65 yr or older, with low T levels ( 148 ). Decisions regarding TRT should be individualized after discussing potential risks and benefits in men with both symptoms suggestive of consistent T deficiency and burden of symptoms (e.g., low libido, unexplained anemia, osteoporosis) and presence of other co-morbid conditions that increase the risk of T treatment ( 148 ). The shared decision making should weigh the patient’s and clinician’s values. In male children, physiologic doses of T are used for brief periods to initiate pubertal development in those with constitutional delay of growth and puberty. Testosterone is needed permanently for children with congenital or acquired hypogonadism.
Recent interest has focused on the role of T in athletic performance in transgender and sexual developmentally distinct athletes. Individuals transitioning to females may require a therapeutic-use exemption for spironolactone, which is often used to block the androgen receptor and lower overall testosterone levels. Currently, trans female athletes subject to WADA testing must document subthreshold T levels for at least 12 months before being allowed to compete as a female. The IOC sets this threshold at <10 nM, and World Athletics (formerly the International Amateur Athletics Federation) at <5 nM. Interested readers can obtain a much deeper discussion of this topic in several reviews ( 198–200 ).
CONCLUSIONS
Anabolic-androgenic steroids include a wide spectrum of compounds that exert their effects through various mechanisms. Anabolic-androgenic steroid use is advantageous in athletic performance predominantly through enhancements in strength, power, increases in muscle mass, reduced recovery time, and other factors. Major competitive sporting bodies ban the use of AAS; however, the predominant area of AAS usage has now expanded into clinical scenarios, persons undergoing sexual reassignment, and by those interested in AAS for purely aesthetic enhancement. Thus, it is not only athletes who are using AAS to gain performance advantages but also other individuals for various reasons. Use for AAS to enhance athletic performance is banned, and coaches, trainers, and medical staff should monitor for signs of use. The use/abuse of AAS has several notable side effects with various consequences that are, in some cases, reversible. Coaches, parents, trainers, and medical staff need to understand why athletes might use AAS and provide educational programming in a preventive capacity. The position of the ACSM is that the illicit use of AAS for athletic and recreational purposes is, in many cases, illegal, unethical and also poses a substantial health risk. Nonetheless, TRT is used in treating various conditions, and clinicians may elect to use this therapy when medically necessary. The ACSM acknowledges the lawful and ethical use of AAS for clinical purposes and supports the physicians’ ability to provide androgen therapy to patients when deemed medically necessary.
This article is published as an official pronouncement of the American College of Sports Medicine and is an update of the 1987 ACSM position stand on the use of anabolic-androgenic steroids. Click here https://links.lww.com/MSS/C362 to download a slide deck that summarizes this ACSM pronouncement on anabolic-androgenic steroid use. This pronouncement was reviewed for the American College of Sports Medicine by members-at-large and the Pronouncements Committee.
Care has been taken to confirm the accuracy of the information present and to describe generally accepted practices. However, the authors, editors, and publisher are not responsible for errors or omissions or for any consequences from the application of the information in this publication and make no warranty, expressed or implied, with respect to the currency, completeness, or accuracy of the contents of the publication. The application of this information in a particular situation remains the professional responsibility of the practitioner; the clinical treatments described and recommended may not be considered absolute and universal recommendations.
- Cited Here |
- Google Scholar
TESTOSTERONE; HYPERTROPHY; SKELETAL MUSCLE; ANDROGEN; STRENGTH; PERFORMANCE
Supplemental Digital Content
- MSS_2022_10_31_PHILLIPS_20-01062_SDC1.pptx; [PowerPoint] (4.24 MB)
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Nutrition and athletic performance, quantity and quality of exercise for developing and maintaining..., the female athlete triad, exercise and physical activity for older adults, position stand on the use of anabolic-androgenic steroids in sports.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 01 June 2022
Anabolic–androgenic steroid use is associated with psychopathy, risk-taking, anger, and physical problems
- Bryan S. Nelson 1 ,
- Tom Hildebrandt 2 &
- Pascal Wallisch 1
Scientific Reports volume 12 , Article number: 9133 ( 2022 ) Cite this article
13k Accesses
14 Citations
88 Altmetric
Metrics details
- Human behaviour
Previous research has uncovered medical and psychological effects of anabolic–androgenic steroid (AAS) use, but the specific relationship between AAS use and risk-taking behaviors as well as between AAS use and psychopathic tendencies remains understudied. To explore these potential relationships, we anonymously recruited 492 biologically male, self-identified bodybuilders (median age 22; range 18–47 years) from online bodybuilding fora to complete an online survey on Appearance and Performance Enhancing Drug (APED) use, psychological traits, lifestyle choices, and health behaviors. We computed odds ratios and 95% confidence intervals using logistic regression, adjusting for age, race, education, exercise frequency, caloric intake, and lean BMI. Bodybuilders with a prior history of AAS use exhibited heightened odds of psychopathic traits, sexual and substance use risk-taking behaviors, anger problems, and physical problems compared to those with no prior history of AAS use. This study is among the first to directly assess psychopathy within AAS users. Our results on risk-taking, anger problems, and physical problems are consistent with prior AAS research as well as with existing frameworks of AAS use as a risk behavior. Future research should focus on ascertaining causality, specifically whether psychopathy is a risk associated with or a result of AAS use.
Similar content being viewed by others

The intersection of physical activity type and gender in patterns of disordered eating
Adverse effects and potential benefits among selective androgen receptor modulators users: a cross-sectional survey.
The effect of GLP-1 receptor agonist use on negative evaluations of women with higher and lower body weight
Introduction.
An estimated 6% of males globally 1 (including 2.9–4 million Americans 2 ) have used anabolic–androgenic steroids (AAS) such as methyltestosterone, danazol, and oxandrolone, which are a series of synthetic variants of the male sex hormone testosterone that increase lean muscle protein synthesis without increasing fat mass 3 , 4 . Although there are medical uses such as for AIDS-related wasting syndrome 5 , AAS are commonly used by individuals for the purposes of bodybuilding and appearance modification 2 , 3 , 6 . In these cases, doses are commonly 10 to 100 times higher than clinical doses and are typically “cycled” intermittently (i.e., used for a few months, stopped to minimize the stress that AAS impart on the body, then resumed shortly thereafter) 3 , 7 . AAS have a 30% dependence rate among long-term users, higher than many other prescription or illicit drugs such as cocaine and have been linked to medical issues such as liver and kidney damage, cardiovascular problems, testicular atrophy, infertility, hair loss, and gynecomastia 2 , 3 , 7 , 8 , 9 , 10 . AAS use is strongly associated with other substance abuse 8 , 9 , 11 , 12 , and users often exhibit negative, although idiosyncratic, psychological issues 8 , 13 , 14 , 15 , 16 , 17 . Some users report delusions of grandeur and invincibility, while others experience depression and various mood disturbances 8 , 18 , 19 , 20 . As dosage increases, AAS users may become impulsive, moody, aggressive, or even violent 9 , 18 , 19 , 21 , 22 , 23 , 24 , 25 , 26 , 27 . Recent neurobiological studies have focused on effects of AAS on central nervous system functions such as cognition, anxiety, depression, and aggression 10 , 28 , 29 . In recent imaging studies, AAS use was associated with cortex thinning as well as decreased gray matter and increased right amygdala volume 30 , 31 , 32 . AAS use seems to accelerate brain aging through oxidative stress and apoptosis 33 , 34 , 35 , is associated with lower cognitive function 36 , 37 , and may disrupt normal neuronal function in the forebrain, which can increase anxiety and aggressiveness and diminish inhibitory control 10 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 . Increased depression has been frequently observed during AAS withdrawal 32 , 46 .
One area that remains understudied among AAS users is psychopathy, a personality disorder characterized by shallow emotional affect, lack of empathy, and antisocial behavior 47 , 48 , 49 . Psychopathy research has frequently associated psychopathy with violence, repeated imprisonment, disrespect for authority, and substance misuse/abuse 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 . There is growing evidence that AAS use may be associated with psychopathy, including a direct association between AAS and psychopathy in an Iranian sample 56 as well as numerous reports of associations between AAS use and violent crime or “roid rage” 19 , 21 , 22 , 23 , 25 , 27 , 57 . Prior studies examining AAS use and elements of the “Dark Triad” and “Big Five” personality traits suggest that the relationship between AAS use and both violence and risk-behaviors may be due to self-regulatory deficits and low conscientiousness, and that AAS use is predicted by narcissism, low agreeableness, neuroticism, impulsivity, and inability to delay gratification 56 , 58 . Hauger et al. 28 recently identified significantly lower emotion recognition in AAS dependent users compared to AAS non-using weightlifters, suggesting that this lower emotion recognition may contribute to the higher frequencies of antisocial traits that AAS users have previously reported 59 , 60 . Antisocial personality disorder, which is characterized by the disregard for laws and norms, irritability, and the failure to regard the safety of self and others 61 has been suggested as the mechanism that underlies the link between AAS use and aggression 3 , 9 , 60 , 62 , 63 . Conceptually, there are overlaps between antisocial personality disorder and psychopathy 64 . We therefore argue that psychopathic traits among AAS users are worth exploring.
Thus, the present study assessed whether AAS users were more likely than nonusers to exhibit psychopathic traits, risk-taking behaviors such as sharing needles, anger problems such as getting into altercations, emotional problems such as panic attacks and depression, cognitive problems such as difficulty remembering, and physical problems such as hair loss. We hypothesized that AAS users would display heightened odds of psychopathic traits, substance use risk-taking behaviors, sexual risk-taking behaviors, anger problems, emotional stability problems, cognitive problems, depressive symptoms, anxiety symptoms, impulsivity symptoms, and physical problems, although we recognize that many of these traits are highly idiosyncratic in nature. Finally, we hypothesized there is a dose-dependent relationship between these traits and the variety of substances used as well as the number of cycles.
Participants and procedure
This study was approved by the NYU Committee on Activities Involving Human Subjects and we conducted in accordance with the Declaration of Helsinki principles. We anonymously recruited a large online sample of 492 (Mean age = 22.9, SD age = 4.3) adult biologically male bodybuilders and asked them questions about their Appearance and Performance Enhancing Drug (APED) use (if any), exercise and dietary habits, psychological states, risk-taking behaviors, and any physical problems they might have experienced. The anonymous internet survey was posted to online fitness fora in fall 2015. All participants provided informed consent prior to their participation. Participants had the option to enter an online raffle for one of twenty $50 Amazon gift cards, which were distributed via email.
The following subsections are presented in the same order as the online survey.
Diet and exercise
Participants reported how often they had exercised in the past month (every day, most days, some days, very rarely/never) and rated their caloric intake in the past month on a 5-point ordinal scale (1 = extreme restriction of calories, 5 = extreme over-consumption of calories). We measured caloric intake in terms of restriction, maintenance, or surplus rather than total calories per day because participants likely vary in caloric requirements (i.e., 3000 cal/day may be a surplus for some but a deficit for others).
Appearance and performance enhancing drugs
Each participant indicated whether he had ever used oral, injectable, or topical AAS (“yes, currently,” “yes, formerly,” “no, but considered taking,” “no, never considered taking” for each). Additionally, participants reported how many AAS cycles they had completed and responded whether they had ever used the following APEDs (each with “yes”/”no” options): Testosterone, Dianabol (Methandrostenolone), Deca Durabolin (Nandrolone Decanoate), Winstrol (Stanozolol), Anadrol (Oxymetholone), Human Growth Hormone (Somatropin), Synthol, Anti-Estrogens, Fat Burners (Insulin, Clenbuterol, Cytomel, Cynomel), Trenbolone, or Anavar.
Self-reported events
Participants rated each of the following items as “yes, currently,” “yes, formerly,” or “no, never”.
General events Participants self-reported whether they experienced the following events: depression, increased number of mood swings, getting into altercations, panic attacks, irritability, lack of frustration tolerance, aggression, difficulty focusing, racing thoughts, difficulty making decisions, difficulty remembering, suicidal thoughts, acne, trouble sleeping, water retention, hair loss, changes in appetite, and heart problems.
Risk-taking behavior Participants indicated whether they had engaged in or experienced the following: unprotected sex, sex with multiple partners, sexually transmitted disease or infection (STD), sharing needles, reusing needles, using stimulants without prescription (such as crack, powdered cocaine, methamphetamine, amphetamine, or ecstasy [MDMA]), using opiates without prescription (such as heroin, morphine, codeine, or Oxycontin), using hallucinogens without prescription (such as LSD, mescaline, and psilocybin), using depressants without prescription (such as Valium, Xanax, Librium, and barbiturates), drinking alcohol, smoking tobacco, and smoking marijuana.
Impulsivity
We used the Barratt Impulsiveness Scale to quantify impulsivity (BIS-11) 65 . Participants responded to 30 statements such as “I often have extraneous thoughts” using a 4-point ordinal rating scale (1 = rarely/never, 4 = almost always/always). The BIS-11 displayed strong reliability in this sample (Cronbach’s α = 0.84).
Psychopathic traits
We employed the Levenson Self-Report Psychopathy Scale (LSRP) to assess psychopathy 66 . The scale has 26 items graded on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree) and was strongly reliable in this sample (Cronbach’s α = 0.88).
We assessed anxiety with the Generalized Anxiety Disorder 7-item Scale (GAD-7) 67 . Participants responded to each of the seven items such as “being so restless it is hard to sit still” on a 4-point ordinal rating scale (0 = not at all, 3 = nearly every day). The GAD-7 displayed excellent internal consistency (Cronbach’s α = 0.89). Possible scores range from 0 to 21.
We included the 10-item Center for Epidemiologic Studies Short Depression Scale (CES-D 10) 68 to measure depression. Participants rated statements such as “I felt lonely” on a 4-point ordinal rating scale (0 = rarely or none of the time, 3 = all the time). The CES-D 10 was highly reliable (Cronbach’s α = 0.82), with possible scores ranging from 0 to 30.
Aggravation
Participants responded to the 7-item aggravation subscale of the State Hostility Scale 69 , 70 . In the subscale, participants rate possible descriptions of their current mood (e.g., “stormy” or “vexed”) on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree). The aggravation subscale of the State Hostility Scale had strong reliability (Cronbach’s α = 0.90).
Demographic questions
Lastly, participants reported their age (years), height (inches), weight (pounds), body fat percentage, racial background, and level of education.
Statistical analysis
The survey was convenience sampled, with no pre-specified sample size or power calculation. For our primary analysis, we grouped participants who responded “yes, currently” or “yes, formerly” to having used AAS (oral, injectable, or topical) as AAS users (n = 154, 31.3%). We considered those who responded “no, but considered taking” or “no, never considered taking” to be AAS nonusers (n = 338, 68.7%). We also conducted a secondary analysis using all four categories (current AAS users (n = 121, 24.6%); former AAS users (n = 33, 6.7%); AAS nonuser, considered using (n = 200, 40.7%); AAS nonuser, never considered using (n = 138, 28.0%)).
Both AAS cycle experience and APED variety were self-reported. APED variety was the number of different APED types used (the number each participant responded “yes” to taking of Testosterone, Dianabol (Methandrostenolone), Deca Durabolin (Nandrolone Decanoate), Winstrol (Stanozolol), Anadrol (Oxymetholone), Human Growth Hormone (Somatropin), Synthol, Anti-Estrogens, Fat Burners (Insulin, Clenbuterol, Cytomel, Cynomel), Trenbolone, and Anavar). AAS cycle experience was the number of AAS cycles participants reported. If the participant was an AAS nonuser, then both APED variety and AAS cycle experience were scored as 0.
We grouped traits of interest into the following categories: psychopathic traits, substance use risk-taking behavior, sexual risk-taking behavior, anger problems, emotional stability problems, cognitive problems, depressive symptoms, anxiety symptoms, impulsivity symptoms, and physical problems. Following Brinkley et al. 71 , we considered participants in the top third of the LSRP distribution to have psychopathic traits. We considered any participant that reported sharing needles, reusing needles, hallucinogen use, stimulant use, depressant use, or opiate use as engaging in substance use risk-taking. Similarly, any participant that reported an STD, engaging in unprotected sex, or having multiple sexual partners was categorized as having sexual risk-taking behavior. Any participant scoring in the top half of the aggravation subscale of the State Hostility Scale, reporting physical altercations, or reporting increased aggression was categorized as having anger problems. Participants who reported mood swings, lower frustration tolerance, or irritability were considered to have emotional stability problems while participants with difficulty remembering, difficulty focusing, or trouble making decisions were considered to have cognitive problems. We considered participants with depressive symptoms as those that reported suicidal thoughts, reported increased depression, or had a CES-D 10 score greater than 10 (the established cut point 68 ). Those with anxiety symptoms either had a GAD-7 score greater than the established cut point 67 of 8 or reported panic attacks. A participant who reported racing thoughts or who scored in the top half of the Barratt Impulsiveness Scale was considered to have impulsivity symptoms. Finally, we considered participants to have physical problems if they reported heart problems, appetite changes, water retention, acne, or hair loss.
We used logistic regression to assess possible associations between these traits of interest and AAS use, number of AAS cycles, and variety of APEDs used. We computed odds ratios (OR) with 95% confidence intervals (CI). All analyses adjusted for age, race, education, exercise frequency, caloric intake, and lean BMI. Age, race, and education were included as basic demographic variables, while exercise frequency, caloric intake, and lean BMI were included to account for differences in bodybuilding goals, success, and dedication. We chose to calculate lean BMI to assess how muscular participants were. We used the standard (kg/m 2 ) BMI formula but used each participant’s lean bodyweight instead of his total bodyweight. Lean body weight was calculated by using each participant’s self-reported body fat percentage to determine how much he weighed excluding his body fat (weight in kg * (100%-bodyfat%)). Given that both psychopathy and AAS use are associated with illicit drug use 21 , we conducted a post hoc subgroup analysis among participants without history of polysubstance use (3 or more different drug classes) to ensure any association between AAS use and psychopathic traits was not confounded by polysubstance use. All analyses were conducted in R (version 3.5.1).
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of New York University.
Consent to participate
Participants provided informed consent prior to their participation in this anonymous internet survey.
Participant characteristics are listed in Table 1 . Most participants were younger than 25 years old (56.5% of AAS users; 79.0% of AAS nonusers), white (85.7% of AAS users; 77.5% of AAS nonusers), and had education beyond high school (75.3% of AAS users; 59.1% of AAS nonusers). The majority in each group exercised most days of the week (79.2% of AAS users; 74.8% of AAS nonusers) and were attempting to gain weight (51.3% of AAS users; 51.2% of AAS nonusers). For AAS users and nonusers, the median (Q1-Q3) lean BMI was 23.6 (22.3–25.4) and 21.6 (20.3–23.3) kg/m 2 . AAS users began use at a median (Q1-Q3) of 21 (20–24) years, had completed 2 (1–3) AAS cycles, and used 4 (2–5) different APED types; 78.6% (121/154) were current AAS users. Among AAS nonusers, 59.2% (200/338) had considered using AAS.
Tables 2 and 3 summarize traits of interest and specific substance use risk-taking behaviors by AAS use status; 25.8% (39/154) of AAS users and 10.2% (34/338) of AAS nonusers had a history of polysubstance use. AAS users had over twice the odds of exhibiting psychopathic traits (OR = 2.50, 95% CI 1.52–4.15), over three times the odds of engaging in substance use risk-taking behaviors (OR = 3.10, 95% CI 1.97–4.93), nearly twice the odds of engaging in sexual risk-taking behaviors (OR = 1.79, 95% CI 1.01–3.26), nearly twice the odds of experiencing anger problems (OR = 1.71, 95% CI 1.02–2.95), and over twice the odds of exhibiting physical problems (OR = 2.23, 95% CI 1.16–4.51) compared to AAS nonusers (Table 4 ). In a post hoc subgroup analysis, AAS users without history of polysubstance use had higher odds of psychopathic traits compared to nonusers without history of polysubstance use (OR = 2.73, 95% CI 1.54–4.90).
In secondary analyses with four levels of AAS use, AAS nonusers who considered using had higher odds of psychopathic traits (OR = 2.19, 95% CI 1.27–3.87), substance use risk-taking (OR = 3.51, 95% CI 2.06–6.14), sexual risk-taking (OR = 3.38, 95% CI 2.00–5.78), anger problems (OR = 3.16, 95% CI 1.86–5.42), emotional stability problems (OR = 1.87, 95% CI 1.16–3.01), depressive symptoms (OR = 2.12, 95% CI 1.32–3.44), and impulsivity symptoms (OR = 2.17, 95% CI 1.31–3.61) compared to AAS nonusers who never considered using; former AAS users had lower odds of both anxiety symptoms (OR = 0.30, 95% CI 0.08–0.84) and impulsivity symptoms (OR = 0.33, 95% CI 0.14–0.74) compared to AAS nonusers who considered using; and current AAS users had higher odds of both impulsivity symptoms (OR = 2.92, 95% CI 1.27–6.84) and physical problems (OR = 5.86, 95% CI 1.83–19.74) compared to former AAS users.
Lastly, we assessed possible relationships between (i) the number of different APED types used and (ii) the number of AAS cycles with the same traits of interest as before. Each additional type of APED used was associated with a 19% increase in the odds of psychopathic traits (OR = 1.19, 95% CI 1.07–1.33), a 24% increase in the odds of substance use risk-taking (OR = 1.24, 95% CI 1.12–1.38), an 18% increase in the odds of sexual risk-taking (OR = 1.18, 95% CI 1.02–1.38), a 15% increase in the odds of emotional stability problems (OR = 1.15, 95% CI 1.04–1.27), and a 33% increase in the odds of physical problems (OR = 1.33, 95% CI 1.12–1.66). For every one-unit increase in the number of AAS cycles, there was a 26% increase in the odds of substance use risk-taking (OR = 1.26, 95% CI 1.10–1.46) and an 85% increase in the odds of physical problems (OR = 1.85, 95% CI 1.29–3.01).
In our online survey of adult biologically male bodybuilders, we found AAS use was associated with higher odds of psychopathic traits, both for AAS users compared to nonusers as well as for increased APED variety. Importantly, this association was also present among participants with no history of polysubstance use. It is not certain whether AAS use predicts psychopathic traits or if the existence of psychopathic traits may actually be a risk factor for AAS use. We note that AAS nonusers who considered AAS use had over twice the odds of psychopathic traits compared to AAS nonusers who never considered AAS use. A recent study of 285 competitive athletes reported that Machiavellianism and psychopathy explained 29% of the variance in positive attitude toward AAS 72 . This is supported generally by the well-established association between psychopathic traits and risk-taking behaviors such as substance abuse 48 . In that case, a large proportion of bodybuilders willing to make the jump to using AAS may already have pre-existing psychopathic traits. Psychopathy is related to both antisocial personality disorder and conduct disorder, each of which is associated with AAS use 9 , 60 . Conduct disorder in particular is a major risk factor for AAS use 9 that cannot be entirely explained by use of other drugs 59 . The relationship may be dynamic; bodybuilders with psychopathic tendencies may be more willing to begin AAS in the first place. Subsequently, these traits might be amplified either chemically by AAS use or psychologically by the environment; prior work has shown the difference between psychopaths and non-psychopaths in emotional-regulatory activity in the aPFC is modified by endogenous testosterone level 73 . With this in mind, longitudinal research is needed to further explore the causal nature of this relationship.
Our study is one of many to link AAS use substance use risk-taking behaviors 74 , 75 and sexual risk-taking behaviors 59 , 76 . It is difficult to ascertain the specific relationship between AAS use and risk-taking. Unlike physical, psychological, cognitive, and anger problems, which have all had experimental and translational research done to strengthen causal interpretations of such links 16 , 77 , there has not been experimental work to test whether risk-taking behaviors are caused by AAS use. In fact, it is important to consider that AAS use is itself a risk behavior, and another form of substance use, so AAS users may already engage in many other risk-taking behaviors prior to their first use. This may be especially true in light of our findings that AAS nonusers who considered AAS use had over three-times the odds of both substance use and sexual risk-taking behaviors compared to AAS nonusers who never considered AAS use, as well as our results regarding APED variety and AAS cycle experience. AAS users willing to try more types of APEDs or willing to undergo more AAS cycles may be more likely to also engage in risk-taking behaviors. Perhaps the relationship between AAS and risk-taking behaviors is bidirectional and interactive, where athletes that engage in these risk behaviors such as illicit drug use experiment with AAS, which may lower their inhibitions to take further risks.
Our finding that AAS users have higher odds of experiencing anger problems is in line with prior research 16 , 19 , 20 . Notably, anger has been previously reported as both a potential risk factor 78 as well as a potential outcome 27 . We did not observe associations between AAS use and emotional stability problems, cognitive problems, depressive symptoms, anxiety symptoms, or impulsivity symptoms. Prior research has identified various psychological and cognitive traits among AAS users such as depression, impulsivity, and mania 18 , 19 , 20 , but they are generally idiosyncratic in nature 8 , 79 , 80 , 81 . We do note that AAS nonusers who considered AAS use had higher odds of emotional stability problems, depressive symptoms, and impulsivity symptoms compared to AAS nonusers who never considered AAS use, former AAS users had lower odds of anxiety symptoms and impulsivity symptoms compared to AAS nonusers who considered AAS use, and current AAS users had higher odds of impulsivity symptoms compared to former AAS users. These findings comparing AAS nonusers who considered vs. never considered AAS use are consistent with prior research about factors relating to the decision to use AAS, including research on the “Big Five” personality traits 58 . Additionally, we observed increased odds of emotional stability problems with increased APED variety. Lastly, our hypothesis about physical problems was supported for AAS users compared to nonusers as well as the dose dependent response in relation to increased APED variety and increased AAS cycle experience. These findings are consistent with prior studies 3 , 8 , 10 , 32 .
There are several limitations. Although we successfully elicited responses from real-world users of AAS, there remain questions about how representative our sample is. AAS users in our sample were relatively new users (median of 2 prior cycles). Our findings may have been different with a group of more experienced users. It is also possible that our online survey was more likely to attract individuals with psychopathic traits or that AAS users with psychopathic traits are more willing to take an online survey than other users. We note that > 50% of AAS users and nonusers were considered to have substance use risk-taking, sexual risk-taking, anger problems, emotional stability problems, cognitive problems, depressive symptoms, impulsivity symptoms, and physical problems. Lastly, this cross-sectional study is entirely correlational and any attempts to speculate about causality should be made with extreme caution. Further prospective or experimental studies are needed. In light of the findings on Machiavellianism and psychopathy in relation to willingness to use AAS 72 , it would be interesting to also examine the link to narcissism and self-esteem/insecurity 82 . We wonder whether self-esteem or narcissistic traits could play an additional role in the motivation to begin AAS use, given the known downsides.
This study is among the first to directly assess psychopathy within AAS users. Our results on risk-taking, anger problems, and physical problems are consistent with prior AAS research as well as with existing frameworks of AAS use as a risk behavior. Increased psychopathic traits in AAS users may serve as the underlying mechanism to predict increased anger problems (see 60 regarding antisocial personality disorder as a mechanism between AAS and aggression). Although the present study highlights the relationship between AAS use and psychopathic traits, future research should emphasize possible causal explanations and try to elucidate the directionality of this relationship. Additionally, the mechanisms between AAS use and risk and violent behaviors should be further explored.
Data availability
All data generated or analyzed during this study are included in this published article’s supplementary information files. R code used in data analysis can be made available upon reasonable request to the corresponding author.
Sagoe, D., Molde, H., Andreassen, C. S., Torsheim, T. & Pallesen, S. The global epidemiology of anabolic-androgenic steroid use: A meta-analysis and meta-regression analysis. Ann. Epidemiol. 24 , 383–398 (2014).
Article PubMed Google Scholar
Pope, H. G. Jr. et al. The lifetime prevalence of anabolic-androgenic steroid use and dependence in Americans: Current best estimates. Am. J. Addict. 23 , 371–377 (2014).
Kanayama, G., Brower, K. J., Wood, R. I., Hudson, J. I. & Pope, H. G. Jr. Anabolic-androgenic steroid dependence: An emerging disorder. Addiction 104 , 1966–1978 (2009).
Article PubMed PubMed Central Google Scholar
Kanayama, G., Hudson, J. I. & Pope, H. G. Features of men with anabolic-androgenic steroid dependence: A comparison with nondependent AAS users and with AAS nonusers. Drug Alcohol Depend. 102 , 130–137 (2009).
Article CAS PubMed PubMed Central Google Scholar
Woerdeman, J. & de Ronde, W. Therapeutic effects of anabolic androgenic steroids on chronic diseases associated with muscle wasting. Expert Opin. Investig. Drugs 20 , 87–97 (2011).
Article CAS PubMed Google Scholar
Buckley, W. E. et al. Estimated prevalence of anabolic steroid use among male high school seniors. J. Am. Med. Assoc. 260 , 3441–3445 (1988).
Article CAS Google Scholar
National Institute on Drug Abuse. Anabolic Steroids DrugFacts. National Institute on Drug Abuse https://www.drugabuse.gov/publications/drugfacts/anabolic-steroids (2018).
Pope, H. G. et al. Adverse health consequences of performance-enhancing drugs: An endocrine society scientific statement. Endocr. Rev. 35 , 341–375 (2014).
Kanayama, G., Pope, H. G. & Hudson, J. I. Associations of anabolic-androgenic steroid use with other behavioral disorders: an analysis using directed acyclic graphs. Psychol. Med. 48 , 2601–2608 (2018).
Albano, G. D. et al. Adverse effects of anabolic-androgenic steroids: A literature review. Healthc. Basel 9 , 97 (2021).
Article Google Scholar
DuRant, R. H., Rickert, V. I., Ashworth, C. S., Newman, C. & Slavens, G. Use of multiple drugs among adolescents who use anabolic steroids. N. Engl. J. Med. 328 , 922–926 (1993).
Melia, P., Pipe, A. & Greenberg, L. The use of anabolic-androgenic steroids by Canadian students. Clin. J. Sport Med. 6 , 9–14 (1996).
Hartgens, F. & Kuipers, H. Effects of androgenic-anabolic steroids in athletes. Sports Med. 34 , 513–554 (2004).
Lood, Y., Eklund, A., Garle, M. & Ahlner, J. Anabolic androgenic steroids in police cases in Sweden 1999–2009. Forensic Sci. Int. 219 , 199–204 (2012).
Pope Jr, H. G. & Kanayama, G. Anabolic-androgenic steroids. In Drug Abuse and Addiction in Medical Illness: Causes, Consequences and Treatment (Springer, 2012). https://doi.org/10.1007/978-1-4614-3375-0 .
Su, T.-P. et al. Neuropsychiatric effects of anabolic steroids in male normal volunteers. J. Am. Med. Assoc. 269 , 2760–2764 (1993).
Scarth, M. et al. Severity of anabolic steroid dependence, executive function, and personality traits in substance use disorder patients in Norway. Drug Alcohol Depend. 231 , 109275–109275 (2022).
Corrigan, B. Anabolic steroids and the mind. Med. J. Aust. 165 , 222–226 (1996).
Pope, H. G. Jr. & Katz, D. L. Homicide and near-homicide by abanolic steroid users. J. Clin. Psychiatry 51 , 28–31 (1990).
PubMed Google Scholar
Pope, H. G. & Katz, D. L. Psychiatric and medical effects of anabolic-androgenic steroid use: A controlled study of 160 athletes. Arch. Gen. Psychiatry 51 , 375–382 (1994).
Lundholm, L., Frisell, T., Lichtenstein, P. & Langstrom, N. Anabolic androgenic steroids and violent offending: Confounding by polysubstance abuse among 10365 general population men. Addiction 110 , 100–108 (2015).
Skarberg, K., Nyberg, F. & Engstrom, I. Is there an association between the use of anabolic-androgenic steroids and criminality?. Eur. Addict. Res. 16 , 213–219 (2010).
Klötz, F., Garle, M., Granath, F. & Thiblin, I. Criminality among individuals testing positive for the presence of anabolic androgenic steroids. Arch. Gen. Psychiatry 63 , 1274–1279 (2006).
Perry, P. et al. Measures of aggression and mood changes in male weightlifters with and without androgenic anabolic steroid use. J. Forensic Sci. 48 , 646–651 (2003).
Thiblin, I. & Parlklo, T. Anabolic androgenic steroids and violence. Acta Psychiatr. Scand. 106 , 125–128 (2002).
Williamson, D. J. & Young, A. H. Psychiatric effects of androgenic and anabolic-androgenic steroid abuse in men: A brief review of the literature. J. Psychopharmacol. 6 , 20–26 (1992).
Thiblin, I., Kristiansson, M. & Rajs, J. Anabolic androgenic steroids and behavioural patterns among violent offenders. J. Forensic Psychiatry 8 , 299–310 (1997).
Hauger, L. E. et al. Anabolic androgenic steroid dependence is associated with impaired emotion recognition. Psychopharmacology 236 , 2667–2676 (2019).
Almeida, O. P., Yeap, B. B., Hankey, G. J., Jamrozik, K. & Flicker, L. Low free testosterone concentration as a potentially treatable cause of depressive symptoms in older men. Arch. Gen. Psychiatry 65 , 283–289 (2008).
Bjørnebekk, A. et al. Structural brain imaging of long-term anabolic-androgenic steroid users and nonusing weightlifters. Biol. Psychiatry 1969 (82), 294–302 (2016).
Google Scholar
Kaufman, M. J. et al. Brain and cognition abnormalities in long-term anabolic-androgenic steroid users. Drug Alcohol Depend. 152 , 47–56 (2015).
Grönbladh, A., Nylander, E. & Hallberg, M. The neurobiology and addiction potential of anabolic androgenic steroids and the effects of growth hormone. Brain Res. Bull. 126 , 127–137 (2016).
Article PubMed CAS Google Scholar
Bjørnebekk, A. et al. Long-term anabolic-androgenic steroid use is associated with deviant brain aging. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 6 , 579–589 (2021).
Kaufman, M. J., Kanayama, G., Hudson, J. I. & Pope, H. G. Supraphysiologic-dose anabolic–androgenic steroid use: A risk factor for dementia?. Neurosci. Biobehav. Rev. 100 , 180–207 (2019).
Piacentino, D. et al. Anabolic-androgenic Steroid use and Psychopathology in Athletes. A systematic review. Curr. Neuropharmacol. 13 , 101–121 (2015).
Kanayama, G., Kean, J., Hudson, J. I. & Pope, H. G. Cognitive deficits in long-term anabolic-androgenic steroid users. Drug Alcohol Depend. 130 , 208–214 (2013).
Bjørnebekk, A. et al. Cognitive performance and structural brain correlates in long-term anabolic-androgenic steroid exposed and nonexposed weightlifters. Neuropsychology 33 , 547–559 (2019).
Caraci, F. et al. Neurotoxic properties of the anabolic androgenic steroids nandrolone and methandrostenolone in primary neuronal cultures. J. Neurosci. Res. 89 , 592–600 (2011).
Penatti, C. A. A., Porter, D. M. & Henderson, L. P. Chronic exposure to anabolic androgenic steroids alters neuronal function in the mammalian forebrain via androgen receptor- and estrogen receptor-mediated mechanisms. J. Neurosci. 29 , 12484–12496 (2009).
Robinson, S., Penatti, C. A. A. & Clark, A. S. The role of the androgen receptor in anabolic androgenic steroid-induced aggressive behavior in C57BL/6J and Tfm mice. Horm. Behav. 61 , 67–75 (2012).
Bueno, A., Carvalho, F. B., Gutierres, J. A. M., Lhamas, C. & Andrade, C. M. A comparative study of the effect of the dose and exposure duration of anabolic androgenic steroids on behavior, cholinergic regulation, and oxidative stress in rats. PLoS ONE 12 , e0177623–e0177623 (2017).
Article PubMed PubMed Central CAS Google Scholar
Henderson, L. P., Penatti, C. A. A., Jones, B. L., Yang, P. & Clark, A. S. Anabolic androgenic steroids and forebrain GABAergic transmission. Neuroact. Steroids Old Play. New Game 138 , 793–799 (2006).
CAS Google Scholar
Melloni, R. H. & Ricci, L. A. Adolescent exposure to anabolic/androgenic steroids and the neurobiology of offensive aggression: A hypothalamic neural model based on findings in pubertal Syrian hamsters. Sex Drugs Sex Differ. Horm Eff. Drug Abuse. 58 , 177–191 (2010).
Quaglio, G. et al. Anabolic steroids: Dependence and complications of chronic use. Intern. Emerg. Med. 4 , 289–296 (2009).
Bertozzi, G. et al. The role of anabolic androgenic steroids in disruption of the physiological function in discrete areas of the central nervous system. Mol. Neurobiol. 55 , 5548–5556 (2018).
Brady, K., Levin, F. R., Galanter, M., Kleber, H. D. & American Psychiatric Association Publishing, issuing body. In The American Psychiatric Association Publishing Textbook of Substance Use Disorder Treatment . (American Psychiatric Association Publishing, 2021).
Hare, R. D. Manual for the Revised Psychopathy Checklist (Multi-Health Systems, 1991).
Patrick, C. J. Handbook of Psychopathy (The Guilford Press, 2005).
Blair, J. The Psychopath: Emotion and the Brain (Blackwell, 2005).
Coid, J. et al. Psychopathy among prisoners in England and Wales. Int. J. Law Psychiatry 32 , 134–141 (2009).
Hildebrand, M. & de Ruiter, C. Psychopathic traits and change on indicators of dynamic risk factors during inpatient forensic psychiatric treatment. Int. J. Law Psychiatry 35 , 276–288 (2012).
Kantor, M. The Psychopathy of Everyday Life: How Antisocial Personality Disorder Affects All of Us (Praeger, 2006).
Neumann, C. S. & Hare, R. D. Psychopathic traits in a large community sample: Links to violence, alcohol use, and intelligence. J. Consult. Clin. Psychol. 76 , 893–899 (2008).
Smith, S. S. & Newman, J. P. Alcohol and drug abuse-dependence disorders in psychopathic and nonpsychopathic criminal offenders. J. Abnorm. Psychol. 99 , 430–439 (1990).
Woodworth, M. & Porter, S. In cold blood: Characteristics of criminal homicides as a function of psychopathy. J. Abnorm. Psychol. 111 , 436–445 (2002).
Chegeni, R., Sagoe, D., Bergen, S. P. & Maleki, A. The dark triad and big five personality traits in anabolic steroid users (2019).
Pope, H. G., Kanayama, G., Hudson, J. I. & Kaufman, M. J. Review article: Anabolic-androgenic steroids, violence, and crime: Two cases and literature review. Am. J. Addict. 30 , 423–432 (2021).
Garcia-Argibay, M. The relationship between the big five personality traits, impulsivity, and anabolic steroid use. Subst. Use Misuse 54 , 236–246 (2019).
Hallgren, M. et al. Anti-social behaviors associated with anabolic-androgenic steroid use among male adolescents. Eur. Addict. Res. 21 , 321–326 (2015).
Yates, W. R., Perry, P. J. & Andersen, K. H. Illicit anabolic steroid use: A controlled personality study. Acta Psychiatr. Scand. 81 , 548–550 (1990).
Diagnostic and statistical manual of mental disorders : DSM-5 . (American Psychiatric Association, 2013).
Hauger, L. E., Havnes, I. A., Jørstad, M. L. & Bjørnebekk, A. Anabolic androgenic steroids, antisocial personality traits, aggression and violence. Drug Alcohol Depend. 221 , 108604–108604 (2021).
Borjesson, A. et al. Male anabolic androgenic steroid users with personality disorders report more aggressive feelings, suicidal thoughts, and criminality. Med. Kaunas Lith. 56 , 265 (2020).
Warren, J. I. & South, S. C. Comparing the constructs of antisocial personality disorder and psychopathy in a sample of incarcerated women. Behav. Sci. Law 24 , 1–20 (2006).
Patton, J. H., Stanford, M. S. & Barratt, E. S. Factor structure of the Barratt Impulsiveness Scale. J. Clin. Psychol. 51 , 768–774 (1995).
Levenson, M. R., Kiehl, K. A. & Fitzpatrick, C. M. Assessing psychopathic attributes in a noninstitutionalized population. J. Pers. Soc. Psychol. 68 , 151–158 (1995).
Spitzer, R. L., Kroenke, K., Williams, J. B. W. & Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 166 , 1092–1097 (2006).
Radloff, L. S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1 , 385–401 (1977).
Anderson, C. A., Deuser, W. E. & DeNeve, K. M. Hot temperatures, hostile affect, hostile cognition, and arousal: Tests of a general model of affective aggression. Pers. Soc. Psychol. Bull. 21 , 434–448 (1995).
Anderson, C. A. & Carnagey, N. L. Causal effects of violent sports video games on aggression: Is it competitiveness or violent content?. J. Exp. Soc. Psychol. 45 , 731–739 (2009).
Brinkley, C. A., Schmitt, W. A., Smith, S. S. & Newman, J. P. Construct validation of a self-report psychopathy scale: Does Levenson’s self-report psychopathy scale measure the same constructs as Hare’s psychopathy checklist-revised?. Personal. Individ. Differ. 31 , 1021–1038 (2001).
Nicholls, A. R., Madigan, D. J., Backhouse, S. H. & Levy, A. R. Personality traits and performance enhancing drugs: The Dark Triad and doping attitudes among competitive athletes. Personal. Individ. Differ. 112 , 113–116 (2017).
Volman, I. A. C. et al. Testosterone modulates altered prefrontal control of emotional actions in psychopathic offenders. eNeuro 3 , ENEURO.0107–15.2016 (2016).
Dodge, T. & Hoagland, M. F. The use of anabolic androgenic steroids and polypharmacy: A review of the literature. Drug Alcohol Depend. 114 , 100–109 (2010).
Sagoe, D. et al. Polypharmacy among anabolic-androgenic steroid users: A descriptive metasynthesis. Subst. Abuse Treat. Prev. Policy 10 , 12–12 (2015).
Ganson, K. T., Jackson, D. B., Testa, A., Murnane, P. M. & Nagata, J. M. Performance-enhancing substance use and sexual risk behaviors among U.S. Men: Results from a prospective cohort study. J. Sex Res. 1–7. ahead-of-print.
Benson, E. More male than male. Monit. Psychol. 33 , 49 (2002).
Sagoe, D., Mentzoni, R. A., Hanss, D. & Pallesen, S. Aggression is associated with increased anabolic-androgenic steroid use contemplation among adolescents. Subst. Use Misuse 51 , 1462–1469 (2016).
Kanayama, G., Hudson, J. I. & Pope, H. G. Illicit anabolic–androgenic steroid use. Horm. Behav. 58 , 111–121 (2010).
Chegeni, R., Notelaers, G., Pallesen, S. & Sagoe, D. Aggression and psychological distress in male and female anabolic-androgenic steroid users: A multigroup latent class analysis. Front. Psychiatry 12 , 629428–629428 (2021).
Hildebrandt, T., Langenbucher, J. W., Carr, S. J. & Sanjuan, P. Modeling population heterogeneity in appearance- and performance-enhancing drug (APED) use: Applications of mixture modeling in 400 regular APED users. J. Abnorm. Psychol. 1965 (116), 717–733 (2007).
Kowalchyk, M., Palmieri, H., Conte, E. & Wallisch, P. Narcissism through the lens of performative self-elevation. Personal. Individ. Differ. 177 , 110780 (2021).
Download references
Acknowledgements
We thank Ward Pettibone and Andre Nakkab for administrative assistance. This work was supported by the New York University Dean’s Undergraduate Research Fund.
This work was supported by the New York University Dean’s Undergraduate Research Fund.
Author information
Authors and affiliations.
Department of Psychology, New York University, New York, NY, USA
Bryan S. Nelson & Pascal Wallisch
Department of Psychiatry, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Tom Hildebrandt
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation was performed by BSN, TH, and PW. Data recording and analysis was performed by BSN. The first draft of the manuscript was written by BSN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Bryan S. Nelson .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information 1., supplementary information 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Nelson, B.S., Hildebrandt, T. & Wallisch, P. Anabolic–androgenic steroid use is associated with psychopathy, risk-taking, anger, and physical problems. Sci Rep 12 , 9133 (2022). https://doi.org/10.1038/s41598-022-13048-w
Download citation
Received : 05 October 2021
Accepted : 25 April 2022
Published : 01 June 2022
DOI : https://doi.org/10.1038/s41598-022-13048-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 13 March 2024
Exploring the prevalence of anabolic steroid use among men and women resistance training practitioners after the COVID-19 pandemic
- Rastegar Hoseini ORCID: orcid.org/0000-0001-8685-2471 1 &
- Zahra Hoseini ORCID: orcid.org/0000-0002-7933-2221 1
BMC Public Health volume 24 , Article number: 798 ( 2024 ) Cite this article
3395 Accesses
6 Altmetric
Metrics details
The COVID-19 pandemic has had a significant impact on individual health and fitness routines globally. Resistance training, in particular, has become increasingly popular among men and women looking to maintain or improve their physical fitness during the pandemic. However, using Anabolic Steroids (AS) for performance enhancement in resistance training has known adverse effects. Thus, this study aimed to explore the prevalence of AS use among men and women resistance training practitioners after the COVID-19 pandemic.
A cross-sectional survey was conducted among 3,603 resistance training practitioners (1,855 men and 1,748 women) in various geographical locations impacted by COVID-19. The participants were asked to complete self-administered questionnaires, which included questions regarding demographic information, training habits, and current or prior usage of AS. The data were analyzed using SPSS statistical software and the chi-square method, with a significance level of ( P < 0.05).
A total of 3603 men and women resistance training practitioners completed the survey. In the study, 53.05% of men and 41.99% of women used anabolic and androgenic steroids. Of those men who used steroids, 29.47% used Testosterone, while 31.20% of women used Winstrol. Additionally, 50.30% of men used steroids via injection, while 49.05% of women used them orally. According to the study, 49.99% of the participants had 6 to 12 months of experience with resistance training, and 64.25% of them underwent three training sessions per week. The analysis using the χ2 test did not reveal any significant difference between men and women in terms of duration of bodybuilding, frequency per week, and engagement in other activities.
This study shows that a significant proportion of men and women resistance training practitioners used AS, particularly among young adults with limited training experience. Thus, there is a need for targeted education and awareness campaigns to address the hazards of AS use and promote healthy training habits during the COVID-19 pandemic.
Peer Review reports
Introduction
The coronavirus pandemic has caused significant disruption to the daily activities of individuals across the world [ 1 ]. One of the areas of life that has been significantly affected is physical exercise [ 2 ]. With the closure of gyms and other sports facilities and restrictions on outdoor exercise, resistance training practitioners have been forced to adapt to new methods of training to maintain their fitness levels [ 3 ]. This disruption to training habits may have had an impact on Anabolic Steroid (AS) usage among men and women resistance training practitioners [ 4 ]. AS are synthetic substances designed to mimic the effects of natural testosterone in the body [ 5 ]. These substances have numerous applications, including medical treatment for hormonal imbalances and muscle-wasting diseases. However, their abuse in the fitness industry, particularly among bodybuilders and other resistance training practitioners, has become widespread, primarily due to their performance-enhancing effects.
Several previous studies have explored the prevalence of AS consumption in various populations, including athletes, bodybuilders, and fitness enthusiasts [ 6 , 7 ]. These studies have demonstrated that the use of these substances is not limited to men and is consumed among women as well. According to a meta-analysis studying a wide range of samples, such as students, university students, resistance training practitioners, and the general public, the global prevalence of AS consumption was estimated at approximately 3.3% [ 8 ]. About Iran, a prevalence of 0.3% AS consumption among the adult population [ 6 , 9 ]. This percentage increased to 36.66% in 2020, which was primarily investigated among men aged between 18 and 34 years [ 10 ]. Furthermore, the prevalence of AS consumption varies widely across different countries, with rates of up to 25% reported in some cases [ 11 , 12 ]. Recent studies have raised concerns that the Coronavirus Disease 2019 (COVID-19) COVID-19 pandemic might have led to an increased prevalence of AS consumption in the resistance training community [ 4 , 13 ]. The pandemic response measures have forced many people to adjust to new, home-based training methods, with limited availability of gym and fitness facilities. This shift in training patterns may have led to increased use or abuse of AS among resistance training practitioners. However, the novelty of this study lies in its focus on resistance training practitioners, the examination of anabolic steroid use after the COVID-19 pandemic, and the inclusion of both men and women in the study population. To date, no research has explored the prevalence of AS consumption among resistance trainers after the COVID-19 pandemic in the Iranian population. Despite the growing popularity of resistance training during the pandemic, there is limited research specifically examining the prevalence of AS use among individuals engaging in resistance training. This research gap is crucial as it allows us to understand the extent of AS use and its associated risks within this specific population. By addressing this research gap, valuable insights can be provided into the prevalence of AS use and its potential implications for the health and well-being of resistance training practitioners. This study aims to address the research gap by exploring the prevalence of AS use among men and women resistance training practitioners after the COVID-19 pandemic. The novelty of this study lies in its focus on a specific population and its potential to provide valuable insights into AS use within the resistance training community. By linking the research gap to the goal of the article, the existing literature aims to be contributed to and awareness of the hazards of AS use while fostering healthy training habits during the COVID-19 pandemic aims to be promoted. Thus, this study aimed to investigate the prevalence of AS consumption among men and women resistance training practitioners after the COVID-19 pandemic.
Study design and population
The survey was conducted in Kermanshah, Iran, a city with an approximate population of 1 million. The survey obtained information on the number and location of gyms in Kermanshah from the Regional Council of Physical Education in the city between May and July 2023. A total of 356 fitness centers that offered resistance training were identified, out of which 286 centers were included in the study. With a confidence interval of 95% and assuming a p = q = 50% probability, a total of 100 resistance training centers were calculated, with an error margin of 7.9%, and used to estimate the population of resistance training practitioners in the city. The gyms were selected randomly and systematically from the five administrative regions of the city, based on the proportion of the number of gyms in each region. The gym management was contacted and explained about the study before obtaining their consent. Individuals aged 18 years and above, training for resistance exercise during morning, afternoon, or night hours were identified in each center. On average, 568 resistance training practitioners were identified per gym. A total number of 4,198 individuals were selected proportionately from each gym based on the number of resistance training practitioners, with a sampling error of 1.25% and a confidence interval of 95%. After screening out incomplete responses, 3603 individuals (1,855 men and 1,748 women) were included in the final analyses. At the commencement of the questionnaires, the participants were provided with information regarding the objectives of the study, and the confidential handling of data, and participants completed the consent form. Also, all educated participants and the legal guardians of illiterate participants were asked to complete the written informed consent at the beginning of the study. The study was conducted in adherence to the seventh and current modification (World Medical Association, 2013) of the Declaration of Helsinki. All experimental protocols were approved by the Committee of Research in Public Sports Board, Kermanshah, Iran.
Data collection
A self-administered questionnaire, consisting of 32 questions, was devised through a scholarly literature review of relevant articles [ 14 , 15 ]. The Questionnaire included the following variables: gender, age, profession, marital status, schooling, socioeconomic status, practice time of resistance training, duration, and purpose of training, nutritional monitoring, use of supplements, and use of AS. The questionnaire underwent a validation process, which determined its clarity, content, and construct indices. The questionnaire’s construction and content were evaluated and validated by professional health practitioners, while the clarity aspect was reviewed by individuals sharing the same traits, including class, age, and lifestyle of the intended research population. A pilot study was conducted to assess the questionnaire’s feasibility for use among the target populace.
To standardize the approach and application of the questionnaire, a pre-training session was conducted with the researchers. Following the pre-training, a pilot study with 40 individuals was carried out at the Kani Gym, which was not included in the survey data. Data collection was conducted throughout the working day by researchers positioned at the entrance of the gym and dressed in uniform to be easily identified. To approach participants, they were explained the research purpose, either at the beginning or end of their workout. Participants who agreed to participate in the study signed an informed consent form. The researchers provided clarification for any queries or ambiguities related to the questionnaire before allowing the participants to complete the form independently, without interference.
Statistical analysis
Statistical analysis in this study was performed using SPSS statistical software (version 21; SPSS Inc., Chicago, IL, USA) with a significance level of P < 0.05. The normality of distribution was assessed with the Kolmogorov-Smirnov test. Both descriptive statistics, including mean, standard deviation, and percentage, and deductive statistics the Chi-square method, were utilized for analysis.
A total of 3,603 (1,855 men and 1,748 women) resistance training practitioners from various regions participated in the survey. A total of (number) participants took part in this study, of which 46% were aged between 18 and 29 years old (46.15% men and 45.08% women), 34.08% were aged between 30 and 44 years old (34.17% men and 33.98% women), 14.13% were aged between 45 and 59 years old (14.33% men and 13.90% women), and 6.16% were aged over 60 years old (5.34% men and 7.04% women). Also, 27.59% were single (30.02% men and 25.06% women), and 72.41% were married (69.98% men and 74.94% women). Furthermore, 0.72% of the participants were illiterate (0.81% men and 0.63% women), while 19.18% had a bachelor’s degree (18.01% men and 20.42% women). The majority of the participants, 80.10%, were university-educated (18.18% men and 78.95% women). Regarding employment status, 44.93% of the participants were employed (68.46% men and 19.97% women), 30.01% were enrolled as students (27.01% men and 33.18% women), and 25.06% were unemployed (4.53% men and 46.85% women). Only a small proportion of the sample, 3.99%, reported being smokers (4.96% men and 2.98% women), while 13.60% of the participants were hospitalized due to COVID-19 (15.94% men and 12.08% women) (Table 1 ).
The χ2 test was conducted to examine potential gender differences for all of these variables. The results demonstrated that employment status was the only variable with a statistically significant gender difference, with a higher proportion of men being employed compared to women ( p < 0.05). No significant differences were found in the distribution of other variables based on gender (Table 1 ).
In this study, 49.99% of the participants had 6 to 12 months of experience with resistance training, and 64.25% of them underwent three training sessions per week. The results of analysis using the χ2 test revealed no significant difference in the duration of bodybuilding, frequency per week, and engagement in other activities between men and women. However, a significant difference in the purpose of performing resistance exercises was found, with 51.37% of men attending the gym for hypertrophy and 55.94% of women attending for weight loss. These findings suggest that men and women exhibit similar patterns of engagement in resistance training, but their motivations for doing so may differ (Table 2 ).
Table 3 presents the results showing that 53.05% of men and 41.99% of women used anabolic and androgenic steroids, with consumption methods differing between genders; 50.30% of men used it via injection, while 49.05% of women used it orally. The results of the χ2 test demonstrated a significant difference in the amount and consumption method of anabolic and androgenic steroid use between men and women. Furthermore, it was found that Testosterone was used by 29.47% of men, while Winstrol was used by 31.20% of women. These findings provide insight into gender-based differences in the use of anabolic and androgenic steroids and suggest that gender-specific strategies may be necessary to address this practice.
Resistance training is a popular form of exercise that has gained significant attention in recent years due to its numerous health benefits. The current study aims to investigate the exploring the prevalence of AS use among men and women resistance training practitioners after the COVID-19 pandemic. The results of the present study revealed a sample of 3,603 individuals, with approximately equal representation of men and women (51.42% versus 48.58%, respectively). The age distribution of participants showed that resistance training is popular among young adults, with 46% of participants aged between 18 and 29 years old. The originality of our study lies in its comprehensive analysis of the characteristics and gender differences of resistance training practitioners from various regions. This age range was nearly uniformly split between men and women; this finding is significant as it indicates that resistance training is equally popular among both genders, particularly among young adults, with 46% of participants aged between 18 and 29 years old. The findings of the present study indicate that the majority of participants were university-educated, which is consistent with previous research demonstrating that a higher level of education is associated with higher participation in exercise and sports [ 16 , 17 ]. Additionally, the results showed that the majority of participants were married, which suggests that resistance training may be a popular form of exercise for those with responsibilities such as marriage and children. In terms of employment status, these results suggest that there is a gender difference, with a higher proportion of men being employed compared to women. This finding is consistent with previous research demonstrating that men are more likely to be employed than women [ 18 ], and may reflect societal norms and gender roles. Finally, this study revealed a low prevalence of smoking among resistance training practitioners, which is encouraging given the detrimental health effects of smoking. However, a relatively high rate of hospitalization due to COVID-19 was found among the sample, which could be attributed to increased exposure to the virus in fitness facilities. This emphasizes the importance of implementing and promoting preventive measures to mitigate the risk of COVID-19 transmission in fitness facilities Overall, this study contributes to a better understanding of the characteristics and gender differences of resistance training practitioners from various regions. These findings suggest that resistance training is popular among both genders, particularly among young adults, and can be practiced by individuals with diverse educational and marital backgrounds. This is significant as it broadens our understanding of the demographic profile of resistance training practitioners. However, future research should investigate the motivations and expectations of resistance training practitioners, as well as the factors that influence how this form of exercise is adopted and maintained over time.
Also, the results of this study showed that a high percentage of participants had between 6 and 12 months of resistance training experience, and the majority underwent three weekly training sessions. Furthermore, these results showed no significant differences in the length of bodybuilding, frequency per week, and engagement in other activities between genders. These findings suggest that men and women exhibit similar exercise habits in resistance training. However, a significant difference in motivations between genders was found. The gym was attended by over half of the men (51.37%) for hypertrophy, while over half of the women (55.94%) attended for weight loss. Thus, these findings indicate that the motivations behind resistance training may differ between genders. It is worth noting that despite these differences in motivations, both men and women seem to have an equal level of engagement in resistance training. These findings have important implications for resistance training interventions. For example, hypertrophy may be less of a motivator for women in resistance training, while emphasizing weight loss may be more effective in increasing women’s participation in resistance training programs. However, more research is needed to determine the most effective ways to motivate men and women differently in resistance training interventions.
However, this study highlights the importance of considering gender differences in motivations for resistance training. While men and women exhibit similar exercise habits, their motivations may differ significantly. These findings may have important implications for resistance training interventions aimed at increasing participation and adherence in both men and women. Further research is needed to identify effective methods of motivating men and women in resistance training interventions. These results suggest that there are significant differences between men and women in terms of both the prevalence and consumption method of steroid use. Specifically, 53.05% of men and 41.99% of women reported using anabolic and androgenic steroids. This finding is significant as it highlights the need for gender-specific interventions to address steroid use. The size of the sample, participants, and gyms used in the literature varied considerably. For instance, a study conducted in Germany approximately 15 years ago involved 113 gyms and 621 individuals and reported a prevalence of AS use of 13.5% [ 14 ]. In Stockholm, Sweden, the prevalence was 3.8% with 64 gyms and 1746 individuals [ 19 ]. On the other hand, in Al-Ain, United Arab Emirates, the prevalence was 22.1% with 18 gyms and 154 individuals [ 20 ]. However, some studies had smaller sample sizes; for example, a study in El Paso, United States, evaluated three gyms and 516 individuals, revealing a prevalence of 11.0% [ 21 ]. Several factors, such as the sample distribution, the regional characteristics, and the individual characteristics of the samples, could have contributed to the variability in the prevalence of AS use among these studies. For instance, a study in the Netherlands that involved 92 gyms and 718 individuals reported a prevalence of AS use of 1% [ 22 ]. These findings are consistent with previous studies that have found that men are more likely to use anabolic and androgenic steroids than women [ 23 , 24 , 25 ]. The reason for lower consumption of AS among women is often due to their desire not to become excessively muscular or develop male characteristics [ 26 ]. On the other hand, men use AS not only to attain their desired body but also to gain status, admiration, and popularity in their social circle [ 27 ]. Furthermore, using AS helps them to be recognized and accepted by their peers [ 28 ]. These results also revealed important gender-based differences in the methods of steroid consumption, with 50.30% of men using intravenous injection and 49.05% of women using oral consumption. These differences may be due to various factors such as differences in physiology, availability, and perceived effectiveness. Of particular importance is the use of Testosterone by men and Winstrol by women, which were found to be the most commonly used steroids among the respective genders. While the reasons for these gender-based differences are unclear, they may reflect differences in physique ideals or perceived benefits or side effects.
Strength and limitations
These findings have important implications for the development of interventions to address anabolic and androgenic steroid use. The fact that gender-based differences were found in both the prevalence and consumption method of steroid use highlights the need for gender-specific interventions that take into account the unique factors driving steroid use among men and women. For instance, interventions targeting men may need to focus on reducing intravenous injection use, while interventions targeting women may need to focus on reducing oral consumption. While this study provides valuable insights into gender-specific differences in anabolic and androgenic steroid use, it is important to note that the sample used in this study was limited to a specific population and may not be representative of the broader population. Additionally, self-reported data are subject to social desirability bias and may not reflect the true prevalence of anabolic and androgenic steroid use. Future studies should aim to replicate these findings with larger, more representative samples, and employ more objective measures of steroid use such as biological markers.
In conclusion, our study significantly contributes to the understanding of resistance training practices among both genders, particularly among young adults. It underscores that resistance training is not limited to a specific demographic but is embraced by individuals with diverse educational and marital backgrounds. A key finding of our research is the distinct motivations for resistance training between men and women, with hypertrophy being a primary driver for men and weight loss for women. This divergence in motivations necessitates the development of gender-specific resistance training interventions to enhance participation and adherence. Furthermore, our study unveils critical gender differences in the prevalence and methods of anabolic steroid (AS) use. Men reported higher usage rates and a preference for intravenous injection, while women predominantly opted for oral consumption. These findings are pivotal, highlighting the need for gender-specific considerations when designing interventions and educational programs to address AS use among resistance training practitioners. Our research, therefore, provides valuable insights that can guide the development of more effective, gender-tailored strategies in the field of resistance training.
Future studies
In future studies, several suggestions can be considered to enhance the straightness of research on anabolic steroid use among resistance training practitioners. First, adopting a longitudinal approach would provide valuable insights into the changes in steroid use over time post-pandemic, identifying shifts in prevalence, patterns, and influencing factors. Also, supplementing quantitative data with in-depth interviews would offer a deeper understanding of motivations, perceptions, and experiences related to steroid use. Moreover, comparing steroid use across different training settings, such as home-based workouts, commercial gyms, or community centers, would allow for a comparison of prevalence rates and factors associated with steroid use within these environments. Additionally, exploring psychological factors such as body image dissatisfaction, social pressure, or self-esteem would provide a more comprehensive understanding of the motivations behind steroid use. Lastly, investigating the effectiveness of educational initiatives aimed at raising awareness and assessing their impact on attitudes, knowledge, and behaviors related to steroid use would assist in designing evidence-based preventive strategies. Implementing these suggestions would contribute to a more comprehensive and robust understanding of anabolic steroid use among resistance training practitioners.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
Anabolic Steroid
Coronavirus Disease 2019
Rahim HA, Hoseini R, Hoseini Z, Abbas EN, Kareem DA. Health-related factors of the Iraqi adult population during the 2020 COVID-19 pandemic: physical activity, eating behavior, quality of life, general health, and mood states cross-talk. BMC Public Health. 2023;23(1):1046.
Article PubMed PubMed Central Google Scholar
Cairney J, Dudley D, Kwan M, Bulten R, Kriellaars D. Physical literacy, physical activity, and health: toward an evidence-informed conceptual model. Sports Med. 2019;49:371–83.
Article PubMed Google Scholar
Dor-Haim H, Katzburg S, Revach P, Levine H, Barak S. The impact of COVID-19 lockdown on physical activity and weight gain among active adult population in Israel: a cross-sectional study. BMC Public Health. 2021;21(1):1–10.
Article Google Scholar
Zoob Carter BN, Boardley ID, Van de Ven K. The impact of the COVID-19 pandemic on male strength athletes who use non-prescribed anabolic-androgenic steroids. Front Psychiatry. 2021;12:636706.
Barany QL, Sofi A, Al-Barwary MK. Neurosteroid, natural and anabolic steroids: physiological, immunological and histopathological study on Diabetic albino rats. Egypt J Veterinary Sci. 2023;54(5):863–81.
Google Scholar
Arazi H, Hosseini R. The prevalence of anabolic-androgenic steroids abuse, knowledge and attitue of their side effects, and attitude toward them among the bodybuilding athletes in Rasht. J Guilan Univ Med Sci. 2011;20(80):34–41.
Pereira E, Moysés SJ, Ignácio SA, Mendes DK, Silva DSD, Carneiro E, et al. Prevalence and profile of users and non-users of anabolic steroids among resistance training practitioners. BMC Public Health. 2019;19:1–8.
Article CAS Google Scholar
Sagoe D, Molde H, Andreassen CS, Torsheim T, Pallesen S. The global epidemiology of anabolic-androgenic steroid use: a meta-analysis and meta-regression analysis. Ann Epidemiol. 2014;24(5):383–98.
Fayyazi Bordbar MR, Abdollahian E, Samadi R, Dolatabadi H. Frequency of use, awareness, and attitudes toward side effects of anabolic–androgenic steroids consumption among male medical students in Iran. Subst Use Misuse. 2014;49(13):1751–8.
Hoseini M, Yousefi B, Khazaei AA. The prevalence of anabolic-androgenic steroids abuse, knowledge and attitude of their side effects, and attitude toward them among the female bodybuilding athletes in Kermanshah. J Adv Biomedical Sci. 2020;10(3):2439–47.
de Zeeuw TI, Brunt TM, van Amsterdam J, van de Ven K, van den Brink W. Anabolic androgenic steroid use patterns and steroid use disorders in a sample of male gym visitors. Eur Addict Res. 2023;29(2):99–108.
Hammoud S, van den Bemt BJ, Jaber A, Kurdi M. Chronic anabolic androgenic steroid administration reduces global longitudinal strain among off-cycle bodybuilders. Int J Cardiol. 2023;381:153–60.
Crisp P, Sims J. COVID-19 and anabolic-androgenic steroids (AAS) as immunosuppresors: is it time to revisit Government Policy and Governance arrangements on AAS? Archives Sports Med. 2020;4(2):245–6.
Striegel H, Simon P, Frisch S, Roecker K, Dietz K, Dickhuth H-H, et al. Anabolic ergogenic substance users in fitness-sports: a distinct group supported by the health care system. Drug Alcohol Depend. 2006;81(1):11–9.
da Silva PR, Machado Júnior LC, Figueiredo VC, Cioffi AP, Prestes MC, Czepielewski MA. Prevalence of the use of anabolic agents among strength training apprentices in Porto Alegre, RS. Arquivos Brasileiros De Endocrinologia Metabologia. 2007;51:104–10.
Hebert JJ, Møller NC, Andersen LB, Wedderkopp N. Organized sport participation is associated with higher levels of overall health-related physical activity in children (CHAMPS study-DK). PLoS ONE. 2015;10(8):e0134621.
Fox CK, Barr-Anderson D, Neumark‐Sztainer D, Wall M. Physical activity and sports team participation: associations with academic outcomes in middle school and high school students. J Sch Health. 2010;80(1):31–7.
Helfand BK, Webb M, Gartaganis SL, Fuller L, Kwon C-S, Inouye SK. The exclusion of older persons from vaccine and treatment trials for coronavirus disease 2019—missing the target. JAMA Intern Med. 2020;180(11):1546–9.
Article CAS PubMed PubMed Central Google Scholar
Leifman H, Rehnman C, Sjöblom E, Holgersson S. Anabolic androgenic steroids—use and correlates among gym users—an assessment study using questionnaires and observations at gyms in the Stockholm region. Int J Environ Res Public Health. 2011;8(7):2656–74.
Al-Falasi O, Al-Dahmani K, Al-Eisaei K, Al-Ameri S, Al-Maskari F, Nagelkerke N, et al. Knowledge, attitude and practice of anabolic steroids use among gym users in Al-Ain district, United Arab Emirates. Open Sports Med J. 2008;2:75–81.
STREET C. Steroids from Mexico: educating the strength and conditioning community. J Strength Conditioning Res. 2000;14(3):289–94.
Stubbe JH, Chorus AM, Frank LE, de Hon O, van der Heijden PG. Prevalence of use of performance enhancing drugs by fitness centre members. Drug Test Anal. 2014;6(5):434–8.
Article CAS PubMed Google Scholar
Lundholm L, Käll K, Wallin S, Thiblin I. Use of anabolic androgenic steroids in substance abusers arrested for crime. Drug Alcohol Depend. 2010;111(3):222–6.
Ip EJ, Barnett MJ, Tenerowicz MJ, Kim JA, Wei H, Perry PJ. Women and anabolic steroids: an analysis of a dozen users. Clin J Sport Med. 2010;20(6):475–81.
Santos AF, Mendonça PMH, Santos LA, Silva NF, Tavares JKL. Anabolic steroids: concepts according to muscular activity practisers in Aracaju (SE). Psicologia em Estudo. 2006;11:371–80.
Kanayama G, Hudson JI, Pope HG Jr. Illicit anabolic–androgenic steroid use. Horm Behav. 2010;58(1):111–21.
Iriart JAB, Chaves JC, Orleans RG. Body cult and use of anabolic steroids by bodybuilders. Cadernos De saúde Publica. 2009;25:773–82.
Hilkens L, Cruyff M, Woertman L, Benjamins J, Evers C. Social media, body image and resistance training: creating the perfect ‘me’with dietary supplements, anabolic steroids and SARM’s. Sports medicine-open. 2021;7(1):1–13.
Download references
Acknowledgements
We would like to thank the subjects for their willing participation in this study.
The authors declared that the research did not receive any financial grants.
Author information
Authors and affiliations.
Department of Exercise Physiology, Faculty of Sport Sciences, Razi University, Kermanshah, P.O. Box. 6714414971, Iran
Rastegar Hoseini & Zahra Hoseini
You can also search for this author in PubMed Google Scholar
Contributions
RH: contributed to the study conception, design, investigation, data analysis, and writing of the manuscript. ZH: contributed to the data acquisition, interpretation, data analysis, and revision of the manuscript. All authors have approved the final version of the manuscript and agreed to be accountable for all aspects of the study.
Corresponding author
Correspondence to Rastegar Hoseini .
Ethics declarations
Ethics approval and consent to participate.
Participants were provided with detailed information regarding the research purpose, procedures, risks, and benefits. They provided informed consent to participate in the study and were informed that they could withdraw from the study at any time without any penalty. The confidentiality and anonymity of participants were maintained throughout the study, and the data collected were used for research purposes only. All research procedures were conducted in compliance with ethical principles as outlined in the Declaration of Helsinki, the applicable regulations, and the guidelines provided by the IRB/IEC. The authors confirm that all methods were performed following relevant guidelines and regulations. All experimental protocols were approved by the ethics committee of Research in Public Sports Board, Kermanshah, Iran. Also, all educated participants and the legal guardian of illiterate participants were asked to complete the written informed consent at the beginning of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hoseini, R., Hoseini, Z. Exploring the prevalence of anabolic steroid use among men and women resistance training practitioners after the COVID-19 pandemic. BMC Public Health 24 , 798 (2024). https://doi.org/10.1186/s12889-024-18292-5
Download citation
Received : 28 July 2023
Accepted : 05 March 2024
Published : 13 March 2024
DOI : https://doi.org/10.1186/s12889-024-18292-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Resistance training
- Young adults
- Awareness campaigns
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
- Open access
- Published: 30 December 2019
Treatments for people who use anabolic androgenic steroids: a scoping review
- Geoff Bates ORCID: orcid.org/0000-0001-6932-2372 1 ,
- Marie-Claire Van Hout 1 ,
- Joseph Tay Wee Teck 2 &
- Jim McVeigh 3
Harm Reduction Journal volume 16 , Article number: 75 ( 2019 ) Cite this article
16k Accesses
34 Citations
15 Altmetric
Metrics details
A growing body of evidence suggests that anabolic androgenic steroids (AAS) are used globally by a diverse population with varying motivations. Evidence has increased greatly in recent years to support understanding of this form of substance use and the associated health harms, but there remains little evidence regarding interventions to support cessation and treat the consequences of use. In this scoping review, we identify and describe what is known about interventions that aim to support and achieve cessation of AAS, and treat and prevent associated health problems.
A comprehensive search strategy was developed in four bibliographic databases, supported by an iterative citation searching process to identify eligible studies. Studies of any psychological or medical treatment interventions delivered in response to non-prescribed use of AAS or an associated harm in any setting were eligible.
In total, 109 eligible studies were identified, which included case reports representing a diverse range of disciplines and sources. Studies predominantly focussed on treatments for harms associated with AAS use, with scant evidence on interventions to support cessation of AAS use or responding to dependence. The types of conditions requiring treatment included psychiatric, neuroendocrine, hepatic, kidney, cardiovascular, musculoskeletal and infectious. There was limited evidence of engagement with users or delivery of psychosocial interventions as part of treatment for any condition, and of harm reduction interventions initiated alongside, or following, treatment. Findings were limited throughout by the case report study designs and limited information was provided.
This scoping review indicates that while a range of case reports describe treatments provided to AAS users, there is scarce evidence on treating dependence, managing withdrawal, or initiating behaviour change in users in any settings. Evidence is urgently required to support the development of effective services for users and of evidence-based guidance and interventions to respond to users in a range of healthcare settings. More consistent reporting in articles of whether engagement or assessment relating to AAS was initiated, and publication within broader health- or drug-related journals, will support development of the evidence base.
Introduction
Human enhancement drug use differs from other forms of drug use by virtue of the motivation or purpose of their use. Typically, they are not consumed either for a treatment of an illness or injury nor for instant gratification through their psychoactive properties. Instead, their function is an attempt to change an individual’s appearance or improve a skill, ability or activity [ 1 , 2 ]. Characterised by man’s endeavour to gain an advantage over his competitor, their usage is by no means a new phenomenon, featured in social, ritual and sporting contexts throughout recorded history. Attempts to classify enhancement drugs have resulted in the six broad categories of drugs to increase lean muscle mass, to suppress appetite or reduce weight, to change the appearance of the hair or skin, to increase sexual desire or enhance performance, to improve cognitive function and to enhance mood or social interaction. Over the past 30 years, there has been growing media, policy and academic interest in this form of drug use, in particular the classification of drugs used to enhance musculature size and strength. Most notable within this category are the anabolic androgenic steroids (AAS) and their associated drugs [ 3 , 4 , 5 , 6 ]. Also included in this classification are a range of other hormones [ 7 , 8 , 9 , 10 , 11 ] including human growth hormone [ 12 , 13 ] and insulin [ 7 , 14 ].
While AAS doping remains a concern for sport, both at elite and recreational levels [ 15 , 16 , 17 ], the wider societal impact is now apparent [ 4 , 18 , 19 ]. Although prevalence estimates of clandestine behaviours such as AAS are notoriously difficult, a growing body of evidence has indicated that while well established in North America, northern Europe and Australia, there are concerns across the globe [ 6 , 19 ].
In recent years, research has provided a more nuanced understanding of AAS use in relation to the diverse characteristics and motivations of users [ 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 ], together with knowledge of the variety and patterns of drug use from both academic studies [ 28 , 29 , 30 , 31 , 32 , 33 , 34 ] and other sources [ 35 ]. Extensive research and comprehensive reviews have provided details of the identified adverse health conditions experienced by users of these durgs [ 36 ], while new research has identified new and concerning health risks [ 37 , 38 ] and the potential for transmission of blood-borne viruses [ 20 , 29 , 39 , 40 , 41 , 42 , 43 ].
A body of research has discussed the risk of developing AAS dependence and it is estimated that up to 30% of AAS users may develop dependence, characterised by the simultaneous use of multiple AAS in large doses over long periods of time [ 36 , 44 ]. While AAS are not explicitly recognised in the Diagnostic and statistical manual of mental disorders (DSM 5) as one of nine classes of drugs [ 45 ], they may be considered under the tenth ‘other (or unknown) substance’ class. The DSM 5 determines the severity of a substance use disorder from mild to severe according to the presence of up to 11 criteria. It is argued that while there are differences between AAS and psychoactive drugs dependence, such as that AAS are typically used over a period of weeks and months to increase muscularity rather than to achieve a ‘high’ in the short-term, these criteria are still highly applicable to AAS dependence [ 46 ]. Criteria such as tolerance, withdrawal, use of the substance in larger amounts, unsuccessful attempts to reduce or stop using the substance, and time spent on activity related to the substance use have all been identified as features of AAS dependence [ 44 , 46 ]. A number of hypotheses to explain AAS dependence have been put forward [ 47 , 48 ] and recommendations for treating what has been described as steroid ‘abuse’ or dependence have long been proposed [ 49 , 50 , 51 ].
Recent recommendations to treat steroid dependence include a staged discontinuation, managing withdrawal symptoms, maintaining abstinence and attenuating complications of chronic use [ 51 , 52 , 53 ]. Long-term use of AAS at high doses may lead to the development of a range of withdrawal symptoms following cessation, including depression, insomnia, suicidal ideation and fatigue, which may persist for many months [ 47 , 51 , 54 ]. Withdrawal is characterised by psychiatric and neuroendocrine symptoms, with the user ultimately re-initiating AAS to alleviate or avoid their onset. Supporting discontinuation may require a multidisciplinary approach with input from health professionals such as a GP, addiction specialist, psychiatrist and endocrinologist [ 53 ]. Swedish guidelines for diagnosing and treating AAS ‘abuse’ [ 55 ] include advice around psychosocial treatments, such as cognitive behavioural therapy, counselling group therapy and motivational interviewing. These therapies address the user’s preoccupation with enhancing their muscularity, their experiences of past bullying or violence, and resulting self-esteem and confidence issues. Brower (2009) believes that these entrenched psychological issues should be addressed once acute withdrawal is resolved as part of successful treatment [ 51 ]. Muscle dysmorphia and associated drive for muscularity [ 56 , 57 , 58 ] may be risk factors for both initiating and continuing AAS use, and potentially dependence [ 52 ]. It may be necessary to identify and address such disorders through counselling or psychotherapies as part of AAS treatment to reduce likelihood of re-initiation [ 53 ].
There has been a fourfold increase in the number of English language academic papers published between 1995 and 2015 [ 59 ]. However, there remains scant evidence in relation to effective policy and practice within the topic. While we have a greater understanding of the environmental influences and risk factors for use [ 17 , 60 , 61 , 62 ], there are few robust findings to support the effective prevention of AAS use. Little progress has been made in answering the fundamental questions of how do we make AAS less attractive and how do we make these drugs less accessible to those at risk of initiating use [ 63 , 64 , 65 , 66 ].
Tensions between some AAS users and the medical community are well documented [ 26 , 67 , 68 , 69 ] and long established [ 70 ], predating anti-doping or legislative control in most countries. Although psychological harm and the potential demand for interventions to address dependence are also well recognised [ 71 , 72 , 73 , 74 , 75 ] and diagnostic tools available [ 52 , 76 ], available services are few and far between. Harm reduction programmes, in the form of needle and syringe programmes (NSP), have clearly been successful in engaging AAS users in Australia [ 42 , 43 , 77 , 78 ] and, in particular, the United Kingdom [ 5 , 30 , 79 , 80 ]. However, even where uptake of service is high, substantial numbers of AAS users do not access these services [ 26 , 68 , 80 , 81 ]. Policy guidance regarding the delivery of harm reduction services for AAS users, centred around NSP provision, is in place in the United Kingdom [ 82 , 83 ], with its importance recognised in National Drug Strategy and Treatment guidelines [ 84 , 85 ]. While these guidelines are based on well-established principles of treatment engagement and harm reduction, there is an urgent need to identify where we have evidence to support specific interventions and where the evidence gaps remain.
The overall aim of this review was to identify and describe what is known about psychosocial and medical interventions that aim to support and achieve cessation of AAS, and treat and prevent associated health consequences. Specifically, the review aimed to identify:
What studies have examined the implementation and impact of interventions to support ASS cessation, and manage the health consequences related to cessation?
What studies have examined the implementation and impact of interventions to treat the harms or side effects associated with AAS use?
What are the implications of these findings, and what are the gaps in the evidence base that research in this area needs to address?
Methodology
The review was undertaken following Arksey and O’Malley’s guidance for scoping reviews, which informed the development of review methods and write-up of methods and findings [ 86 ].
Inclusion and exclusion criteria
Studies were eligible that included males or females with current or discontinued use of AAS alone, or AAS use alongside other substances. Use for any reason (for example, strength or sporting enhancement, aesthetic reasons) was acceptable with the exception of where AAS were prescribed or taken as part of a treatment regimen or in a controlled medical setting. Studies of any psychosocial or medical treatment interventions were eligible, including those that aimed to support individuals to discontinue AAS use or to treat the health consequences of current or past use. This included, but was not restricted to, treating AAS withdrawal, physical or psychological dependence, injuries, acute conditions, chronic conditions, side effects and blood-borne viruses. Studies that did not provide a description of the treatment given or those that did not describe any outcome following treatment at any follow-up time were excluded. Interventions that took place in any setting were eligible, including, but not restricted to, primary and secondary care, community settings such as drugs misuse services, NSPs and AAS clinics, sport and fitness environments, and prisons.
All types of study designs were considered due to the anticipated lack of high-quality controlled trials. Articles published in English were eligible with no date restrictions.
Search strategy
Initially, a comprehensive search was carried out in four bibliographic databases (Medline, PsycINFO, Sports Discus and the Social Sciences Citation Index) in January 2018. A search strategy was developed initially in Medline and adapted for the other databases. The full Medline search is provided in Additional file 2 .
The reference lists of all identified papers were screened to identify potentially eligible studies. Forward citation searches for included articles were executed in PubMed and the identified studies were assessed against the review inclusion criteria. This iterative process continued for all articles identified through these steps. Due to the nature of the evidence base, with studies likely to cover a broad range of topics and to be published in a wide variety of sources, these additional searches were expected to be important to identify relevant literature. Initially, titles and abstracts for all articles identified were reviewed against the inclusion criteria by one reviewer. A sample of 10% was independently reviewed by a second reviewer. The full texts for all articles included at this stage were retrieved and subjected to further screening against inclusion criteria.
Data extraction and synthesis
The relevant characteristics of identified studies were extracted into structured tables. This included population characteristics and details of their AAS use, the symptoms requiring treatment or reasons for seeking help, diagnosis, details of the treatment given and the outcomes of this treatment. Studies were grouped by the types of harms identified in Pope and colleagues’ review of the harms associated with AAS use [ 36 ]. A formal assessment of study quality was not undertaken, as this step is not recommended for scoping reviews [ 86 ]. However, comments on the overall nature, strengths and limitations of the evidence base are provided alongside discussion of review findings.

Identification of studies
Database searching identified 3,684 articles. Following screening of article title and abstracts against review inclusion criteria, full-text articles were accessed for 76 articles and these were again reviewed against the inclusion criteria. An additional 64 studies were identified through checking the reference lists and citations of the included articles. These were screened in the same manner. Following full-text screening, 46 articles were excluded, predominantly because no treatments were reported. The reasons for exclusion at this stage are reported in Fig. 1 .
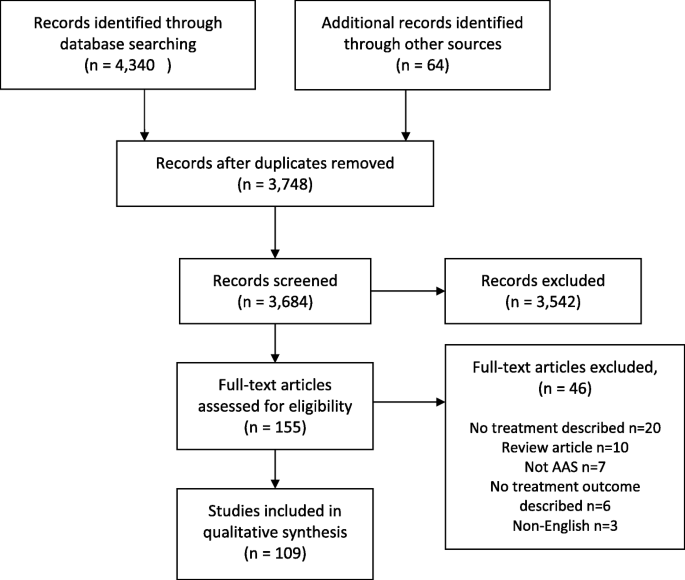
Flow of studies through the review
Summary of findings
In total, 109 studies met the review inclusion criteria. Summaries of the included studies are provided in Table 1 , grouped by the type of condition that required treatment. The studies were carried out in 28 countries, most prominently the USA ( n = 33) and the UK ( n = 21). One study followed a retrospective chart review design with the others case report ( n = 94) or case series ( n = 14) designs. With the lack of any controlled studies, it was difficult to draw conclusions relating to the effectiveness of any treatments provided. Additionally, there were substantial variations across studies in the depth of reporting about participants, settings, condition requiring treatment, the treatments provided and outcomes. The identified studies were published in sources representing a diverse range of disciplines.
Across the included studies, all participants were male. They included a wide range of ages, with the majority in their 20s and 30s, and represented a broad range of experience using AAS from recent initiators to long-term use. Participants’ motivations and history were not reported in a consistent manner to understand factors driving AAS use, but they were frequently described as participating in bodybuilding or weight-lifting activities. The types of conditions requiring treatment included psychiatric ( n = 12), neuroendocrine ( n = 11), hepatic ( n = 25), kidney ( n = 6), cardiovascular ( n = 26), musculoskeletal ( n = 13) and infectious ( n = 7). A further eight studies were categorised as ‘other’ disorders. In a small number of studies, participants were diagnosed with multiple conditions, but they have been grouped by the primary diagnosis.
Further details on participants’ AAS use, conditions requiring treatment, the treatments provided and outcomes are provided in Additional file 1 .
Treatment to support AAS cessation
Four studies reported abstinence-focussed interventions following a diagnosis of AAS dependence. In two cases, patients participated briefly in a drug treatment programme [ 88 , 97 ] before withdrawing. In one, the patient received medication and psychosocial interventions to manage AAS and opioid withdrawal [ 93 ] and withdrawal symptoms abated over time. Detail on the nature of these treatments was not provided. In the remaining study, the patient received medication for a short period before deciding to resume their AAS use due to withdrawal symptoms [ 98 ]. There was no evidence identified here, however, regarding psychosocial interventions that have sought to address any associated psychological disorders amongst users seeking treatment for their AAS use or any other condition. Additionally, no evidence was identified on approaches to reduce risk of relapse by developing social support systems, improving self-confidence or managing stress, all identified as potentially important factors to be addressed during AAS treatment [ 51 , 52 , 55 ].
Two studies were identified in this review where individuals who discontinued AAS use needed treatment for subsequent psychiatric symptoms including depression and suicidal ideation [ 87 , 89 ]. A further 11 studies reported treatments for neuroendocrine disorders, primarily with men who had discontinued their AAS use prior to the onset of symptoms. Administering AAS suppresses the hypothalamic–pituitary testicular axis, particularly when used in large amounts and for long periods, and inhibits production of testosterone [ 195 ]. Men who discontinue long-term AAS use are at risk of hypogonadism and while this may frequently be temporary and resolve spontaneously, it may in some cases persist for long periods after cessation, requiring medical treatment [ 51 , 196 , 197 , 198 ]. Symptoms of hypogonadism may be behind the withdrawal experiences of people with a dependence on AAS [ 51 ]. These difficult experiences have been identified as an influencing factor in users’ decisions to continue or re-instate AAS use [ 52 ]. The limited evidence here shows that positive outcomes are consistently reported in the treatment of men suffering with neuroendocrine disorders following AAS cessation.
Treatment for harms associated with AAS use
The bulk of the evidence identified related to current or former users receiving treatment for an acute or chronic condition or injury associated with their AAS use. This included psychiatric disorders ( n = 12), hepatic and kidney disorders ( n = 31), cardiovascular disorders ( n = 26), musculoskeletal disorders ( n = 13) and a range of other disorders ( n = 8). The management of such conditions in the AAS-using group is similar to that of the general population [ 53 ] and details are described in the tables in the additional material provided. There was, however, limited evidence of engagement with users regarding their AAS use as part of their more general treatment. There were examples where participants were stated to have discontinued AAS following treatment and remained abstinent at follow-up [ 133 , 157 , 159 ], but patients’ AAS status at this time was not routinely reported.
Treatment as an opportunity for engagement
In a small proportion of studies ( n = 10), it was reported that some form of intervention to bring about, or maintain change in AAS use was included as part of the treatment provided. This was most commonly instruction or advice to discontinue AAS use, with a more substantial element such as counselling only reported in three studies [ 139 , 145 , 180 ]. Where reported, such efforts were based on suppling risk information associated with AAS but not support with discontinuation, such as managing withdrawal symptoms. No form of harm reduction interventions were initiated alongside or following any treatments provided. Only one study [ 145 ] reported signposting or referral to another service for further support.
In comparison to people who use other psychoactive drugs, AAS users are less likely to suffer acute adverse effects from their substance use, or to have their occupational performance or relationships impaired and are, therefore, less reliant upon health professionals [ 44 ]. Research has consistently indicated this group to be reluctant to seek medical help or engage with health professionals [ 67 , 199 , 200 , 201 ]. Where health professionals identify AAS use in a patient and are providing treatment for an associated harm, this may, therefore, provide a rare opportunity to motivate changes in behaviour. There were examples in this review of studies that included recent initiators. For example, in 12/25 studies included here reporting hepatic disorders, patients had initiated AAS use fewer than 6 months prior to treatment. Contact with a health professional at this stage could provide a valuable opportunity to engage with the individual about their motivations and substance use before habitual use develops or becomes entrenched, or identify and treat any underlying factors. In a further 5/25 studies, long-term AAS use of over 5 years was reported, and up to 15 years. For such individuals, this contact could provide opportunity to test for disorders associated with long-term use, promote behaviour change and discuss long-term plans for discontinuation of use.
Encouraging discontinuation and delivering harm reduction with patients treated for a disorder associated with AAS
Where a patient is receiving treatment, there will be a range of factors that affect the appropriateness of delivering any form of AAS intervention or investigating any other potential harms. For example, in many of the studies identified, the individuals treated had discontinued their AAS use a substantial time prior to seeking treatment. Additionally, many were diagnosed with acute conditions, for which immediate, and in some cases substantial, treatment was required. In such cases, it is not surprising that the acute harm will be the focus of the treatment. However, where AAS use is suspected or confirmed, a number of diagnostic tests may be appropriate to identify potential physiological or psychiatric harms [ 53 ]. Recommendations for general practitioners who identify AAS use in a patient include strongly encouraging cessation and management of withdrawal symptoms in those that do discontinue, as well as information on injecting practices, promoting alternatives to AAS and informing about long-term health harms for those who continue to use [ 202 ]. Continued encouragement and monitoring of psychiatric and physiological complications is recommended for those who are not prepared to consider discontinuation [ 53 ].
An instruction not to use AAS may be effective in some cases, but for individuals who are highly motivated to use AAS in response to a desire to change their appearance or performance, it may have little impact. Experiencing harm or increasing knowledge of potential risks may not only reduce motivation to use amongst users who may accept risks as a potential consequence of use, but also one that they can manage through their practices [ 60 ]. Where it is identified that users intend to continue administering AAS following treatment, it is important that they receive appropriate harm reduction advice, such as on safe injecting, blood-borne viruses (BBVs) and AAS cycles. For example, in seven studies, treatments for infectious complications associating with injecting AAS were reported. There was no indication of relevant harm reduction work included alongside treatment, such as advice or demonstration relating to injecting or injecting techniques in any of these studies, with the exception of Rich and colleagues who reported provision of counselling on the risks of BBVs [ 180 ].
Research over the past 30 years has provided a far richer understanding of the populations of AAS users, their characteristics, behaviours and motivations. While the specific risks attached to each AAS and the probability or magnitude of harm associated with highly individualised and complex drug regimens cannot be known, we now have a far greater understanding of the potential harms caused by these drugs. However, the evidence base for interventions has not kept pace. The examples of treatment identified in this review were set within primary and secondary care facilities. No studies were identified that explored the effectiveness of any approaches to encourage cessation or treat dependence within other settings where health professionals are likely to encounter users, such as steroid clinics, drugs services or NSPs. Consequently, there is a lack of any evidence on the effectiveness of such services for bringing about behaviour change in users. Within any setting there is scarce evidence on treating AAS dependence, including initiating and maintain cessation and managing withdrawal symptoms outside of case reports of former users seeking support for neuroendocrine disorders.
The findings of this scoping review are characterised by missed opportunities. While the failure to report good practice or supplementary activity is not proof that it does not occur, without confirmation we cannot make assumptions. The extensive literature outlining the symptomatic treatment of AAS-related harms within numerous medical and surgical specialisms fails to provide evidence of intervention or referral to address the major causative factor, the patients’ AAS use. This scoping review has reported only a sample of the myriad of case reports involving the treatment of AAS-related harms. These case reports not only demonstrate the lack of evidence of intervention effectiveness to support the cessation of AAS use or reduce the associated harms, they also fail to show that actual activity occurred. As a minimum, future case reports should report if any assessment for AAS dependence were conducted. Details of advice or interventions provided to AAS users or any referral or signposting are also essential information. Referrals to primary care, endocrinologists, addiction specialists or harm reduction providers are essential building blocks in identifying care pathways and potential effective interventions. Case reports are published predominantly in clinical journals, often relating to medical or surgical specialisms. The publication of reports in broader health or public health journals or journals related to drug use, addiction or harm reduction would facilitate the inclusion of clinical experiences within a wider approach to addressing the harms associated with AAS use.
Despite the comprehensive research and literature relating to AAS dependence, there remains little evidence regarding effective interventions to support cessation of use or management of withdrawal. It is hoped that the development diagnostic tools [ 46 ], guidelines for clinical management [ 85 ] and harm reduction [ 82 ] or the commissioning of health services [ 83 ] will be accompanied by robust research and evaluation. Evaluations to date have been small scale and lack generalizability.
In addition to the need to ensure accurate and consistent reporting of activity and an upscaling of research and evaluation, there is a need to ensure that interventions are culturally appropriate to the target groups. Much of the work to date has focused on the bodybuilding communities of North America, Northern Europe and Australia. It is clear that AAS use is a global issue, with research emerging from low–middle income countries around the world in addition to industrialised high-income states. Of added significance is the diversity of individual AAS users. Interventions will need to be tailored to meet the varied characteristics and motivations of users, going beyond those looking to achieve a stylised “bodybuilding appearance” or excel at sport or even the young males attempting to bulk up. Evidence from the United Kingdom indicates that there are as many AAS users over 40 years of age as there are those under the age of 25 years [ 31 ]. It is well established that AAS use is not restricted to men and while rates amongst women are much lower [ 203 ], the complexities of treatment and care are undoubtedly much higher [ 23 , 204 , 205 ]. Prevalence of AAS use is higher amongst groups with specific characteristics such as professions where size or strength is an asset [ 206 , 207 , 208 , 209 ], amongst gay and bisexual men [ 20 , 22 , 29 , 210 , 211 ] and those using or who have previously used other drugs [ 212 ] [ 30 , 33 , 67 , 212 , 213 , 214 ]. These “sub groups” may or may not require specific interventions and may merely illustrate the complexities of human nature. The majority of AAS users will not initiate or continue AAS by virtue of membership of one of these groups but will have a range of susceptibilities and motivations for use.
Beyond these challenges, to develop effective services for users of AAS is the ongoing lack of confidence that some communities of AAS users feel towards health care professionals and primary care in particular [ 30 , 67 , 199 ] and a feeling that reliable and relevant health information can be gained elsewhere [ 215 ]. Built on the long-standing dismissive approach towards the effectiveness of anabolic steroids by elements of the health profession [ 216 , 217 ] and an ongoing ‘just say no’ stance amongst some practitioners, it is evident that establishing trust through listening to the AAS-using communities will be an essential element of intervention and service development [ 26 ].
Conclusions
This scoping review of the literature has identified treatments given to AAS users for a wide range of physiological and psychological harms. Despite the large number of articles identified, the evidence base consists of case reports of predominantly treatment of physiological harms and there is scarce evidence on treating dependence, managing withdrawal, or initiating behaviour change in users in any settings. Evidence is urgently required to support the development of effective services for users and of evidence-based guidance and interventions to respond to users in a range of healthcare settings. More consistent reporting in articles of whether engagement or assessment relating to AAS was initiated, and publication within broader health- or drug-related journals, will support development of the evidence base.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- Anabolic androgenic steroids
Blood-borne virus
Diagnostic and statistical manual of mental disorders
Needle and syringe programme
Evans-Brown M, McVeigh J, Perkins C, Bellis M. Human enhancement drugs: the emerging challenges to public health. Liverpool: North West Public Health Observatory; 2012.
Google Scholar
McVeigh J, Evans-Brown M, Bellis MA. Human enhancement drugs and the pursuit of perfection. Adicciones. 2012;24(3):185–90.
Article PubMed Google Scholar
Kanayama G, Pope HG. History and epidemiology of anabolic androgens in athletes and non-athletes. Mol Cell Endocrinol. 2018;464(C):4–13.
Article CAS PubMed Google Scholar
Kanayama G, Kaufman MJ, Pope HG. Public health impact of androgens. Curr Opin Endocrinol. 2018;25(3):218–23.
Article CAS Google Scholar
McVeigh J, Begley E. Anabolic steroids in the UK: an increasing issue for public health. Drugs. 2017;24(3):278–85.
Sagoe D, Pallesen S. Androgen abuse epidemiology. Curr Opin Endocrinol Diabetes Obes. 2018;25(3):185–94.
Anderson LJ, Tamayose JM, Garcia JM. Use of growth hormone, IGF-I, and insulin for anabolic purpose: Pharmacological basis, methods of detection, and adverse effects. Mol Cell Endocrinol. 2017.
Van Hout MC, Hearne E. Netnography of female use of the synthetic growth hormone CJC-1295: pulses and potions. Subst Use Misuse. 2016;51(1):73–84.
Brennan R, Van Hout MC, Wells J. Heuristics of human enhancement risk: a little chemical help? Int J Health Prom Educ. 2013;51(4):212–27.
Article Google Scholar
Thevis M, Thomas A, Kohler M, Beuck S, Schanzer W. Emerging drugs: mechanism of action, mass spectrometry and doping control analysis. J Mass Spectrom. 2009;44(4):442–60.
Thevis M, Beuck S, Thomas A, Kortner B, Kohler M, Rodchenkov G, et al. Doping control analysis of emerging drugs in human plasma - identification of GW501516, S-107, JTV-519, and S-40503. Rapid Commun Mass Spectrom. 2009;23(8):1139–46.
Holt RI, Sonksen PH. Growth hormone, IGF-I and insulin and their abuse in sport. Br J Pharmacol. 2008;154(3):542–56.
Article CAS PubMed PubMed Central Google Scholar
Evans-Brown M, McVeigh J. Injecting human growth hormone as a performance-enhancing drug-perspectives from the United Kingdom. J Substance Use. 2009;14(5):267–88.
Underwood M. "Slin is the safest and most anabolic hormone": exploring bodybuilders' use of insulin as a performance and image enhancing drug. Drug Alcohol Rev. 2018;37:S70–S.
Ulrich R, Pope HG, Cleret L, Petroczi A, Nepusz T, Schaffer J, et al. Doping in two elite athletics competitions assessed by randomized-response surveys. Sports Med. 2018;48(1):211–9.
Mottram DR, Chester N. Drugs in Sport. 7 ed: Routledge; 2018.
Backhouse SH, Griffiths C, McKenna J. Tackling doping in sport: a call to take action on the dopogenic environment. Br J Sports Med. 2017.
Auchus RJ, Brower KJ. The public health consequences of performance-enhancing substances: who bears responsibility? JAMA. 2017;318(20):1983–4.
Sagoe D, Molde H, Andreassen CS, Torsheim T, Pallesen S. The global epidemiology of anabolic-androgenic steroid use: a meta-analysis and meta-regression analysis. Ann Epidemiol. 2014;24(5):383–98.
Ip EJ, Doroudgar S, Shah-Manek B, Barnett MJ, Tenerowicz MJ, Ortanez M, et al. The CASTRO study: unsafe sexual behaviors and illicit drug use among gay and bisexual men who use anabolic steroids. Am J Addict. 2019;28:101.
PubMed Google Scholar
Blashill AJ, Calzo JP, Griffiths S, Murray SB. Anabolic steroid misuse among US adolescent boys: disparities by sexual orientation and race/ethnicity. Am J Public Health 2017(0):e1-e3.
Griffiths S, Murray SB, Dunn M, Blashill AJ. Anabolic steroid use among gay and bisexual men living in Australia and New Zealand: Associations with demographics, body dissatisfaction, eating disorder psychopathology, and quality of life. Drug Alcohol Dependence. 2017;181:170–6.
Börjesson A, Gårevik N, Dahl M-L, Rane A, Ekström L. Recruitment to doping and help-seeking behavior of eight female AAS users. Subst Abuse Treat Prev Policy. 11(2016, 1):11.
Zahnow R, McVeigh J, Bates G, Hope V, Kean J, Campbell J, et al. Identifying a typology of men who use anabolic androgenic steroids (AAS). Int J Drug Policy. 2018;55:105–12.
Christiansen AV, Vinther AS, Liokaftos D. Outline of a typology of men’s use of anabolic androgenic steroids in fitness and strength training environments. Drugs. 2016;24(3):295–305.
Underwood M. The unintended consequences of the current approach to blood borne virus prevention amongst people who inject image and performance enhancing drugs: a commentary based on enhanced bodybuilder perspectives. Int J Drug Policy. 2019;67:19–23.
Ip EJ, Trinh K, Tenerowicz MJ, Pal J, Lindfelt TA, Perry PJ. Characteristics and behaviors of older male anabolic steroid users. J Pharm Pract. 2015;28(5):450–6.
Teck JTW, McCann M. Tracking internet interest in anabolic-androgenic steroids using Google Trends. Int J Drug Policy. 2018;51:52–5.
Ip EJ, Yadao MA, Shah BM, Doroudgar S, Perry PJ, Tenerowicz MJ, et al. Polypharmacy, infectious diseases, sexual behavior, and psychophysical health among anabolic steroid-using homosexual and heterosexual gym patrons in San Francisco's Castro District. Subst Use Misuse. 2017;52(7):959–68.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Prevalence of, and risk factors for, HIV, hepatitis B and C infections among men who inject image and performance enhancing drugs: a cross-sectional study. BMJ Open. 2013;3(9):e003207–e.
Article PubMed PubMed Central Google Scholar
Begley E, McVeigh J, Hope V, Bates G, Glass R, Campbell J, et al. Image and Performance Enhancing Drugs: 2016 National Survey Results. Liverpool: Liverpool John Moores University; 2017.
Dodge T, Hoagland MF. The use of anabolic androgenic steroids and polypharmacy: A review of the literature. Drug Alcohol Depend. 2011.
Sagoe D, McVeigh J, Bjornebekk A, Essilfie MS, Andreassen CS, Pallesen S. Polypharmacy among anabolic-androgenic steroid users: a descriptive metasynthesis. Subst Abuse Treat Pr. 2015;10(ARTN 12).
Jennings CJ, Patten E, Kennedy MC, Kelly C. Examining the profile and perspectives of individuals attending harm reduction services who are users of performance and image enhancing drugs. Merchants Quay Ireland: Dublin; 2014.
Llewellyn W. Anabolics. 11 ed. Jupiter, FL: Molecular Nutrition; 2017.
Pope HG, Wood RI, Rogol A, Nyberg F, Bowers L, Bhasin S. Adverse health consequences of performance-enhancing drugs: an Endocrine Society scientific statement. Endocr Rev. 2014;35(3):341–75.
Westlye LT, Kaufmann T, Alnaes D, Hullstein IR, Bjornebekk A. Brain connectivity aberrations in anabolic-androgenic steroid users. Neuroimage Clin. 2017;13:62–9.
Bjornebekk A, Walhovd KB, Jorstad ML, Due-Tonnessen P, Hullstein IR, Fjell AM. Structural brain imaging of long-term anabolic-androgenic steroid users and nonusing weightlifters. Biol Psychiatry. 2017;82(4):294–302.
Article PubMed CAS Google Scholar
Hope VD, McVeigh J, Smith J, Glass R, Njoroge J, Tanner C, et al. Low levels of hepatitis C diagnosis and testing uptake among people who inject image and performance enhancing drugs in England and Wales, 2012-15. Drug Alcohol Depend. 2017;179:83–6.
Hope VD, Harris R, McVeigh J, Cullen KJ, Smith J, Parry JV, et al. Risk of HIV and hepatitis B and C over time among men who inject image and performance enhancing drugs in England and Wales: Results from cross-sectional prevalence surveys, 1992-2013. Jaids-J Acq Imm Def. 2016;71(3):331–7.
Ip EJ, Yadao MA, Shah BM, Lau B. Infectious disease, injection practices, and risky sexual behavior among anabolic steroid users. Aids Care. 2016;28(3):294–9.
Rowe R, Berger I, Yaseen B, Copeland J. Risk and blood-borne virus testing among men who inject image and performance enhancing drugs, Sydney, Australia. Drug Alcohol Rev. 2017;36(5):658–66.
Iversen J, Hope VD, McVeigh J. Access to needle and syringe programs by people who inject image and performance enhancing drugs. Int J Drug Policy. 2016;31:199–200.
Kanayama G, Brower K, Wood R, Hudson J, Pope H. Anabolic-androgenic steroid dependence: an emerging disorder. Addiction. 2009;104(12):1966–78.
Association AP. Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub; 2013.
Book Google Scholar
Kanayama G, Brower KJ, Wood RI, Hudson JI, Pope HG. Issues for DSM-V: clarifying the diagnostic criteria for anabolic-androgenic steroid dependence. Am J Psychiatr. 2009;166(6):642–4.
Kashkin KB, Kleber HD. Hooked on hormones?: An anabolic steroid addiction hypothesis. JAMA. 1989;262(22):3166–70.
Brower KJ. Rehabilitation for anabolic-androgenic steroid dependence. Clin Sport Med. 1989;1:171–81.
Giannini AJ, Miller N, Kocjan DK. Treating steroid abuse: a psychiatric perspective. Clin Pediatr. 1991;30(9):538–42.
Corcoran JP, Longo ED. Psychological treatment of anabolic-androgenic steroid-dependent individuals. J Subst Abuse Treat. 1992;9(3):229–35.
Brower KJ. Anabolic steroid abuse and dependence in clinical practice. Phys Sportsmed. 2009;37(4):131–40.
Kanayama G, Brower KJ, Wood RI, Hudson JI, Pope HG Jr. Treatment of anabolic-androgenic steroid dependence: Emerging evidence and its implications. Drug Alcohol Depend. 2010;109(1-3):6–13.
Casavant M, Griffith J. Anabolic steroid use disorder New Jersey: BMJ Americas Office; 2017 [Available from: https://bestpractice.bmj.com/topics/en-gb/987 ]. Accessed Aug 2018.
Malone DA, Dimeff RJ, Lombardo JA, Sample RH. Psychiatric effects and psychoactive substance use in anabolic-androgenic steroid users. Clin J Sport Med. 1995;5(1):25–31.
Arver S, Borjesson A, Bottiger Y, Edin A, Garevic N, Lundmark J, et al. Swedish clinical guidelines on: The abuse of anabolic androgenic steroids and other hormonal drugs. Stockholm: Karolinska University Hospital; 2013.
Rohman L. The relationship between anabolic androgenic steroids and muscle dysmorhpia: a review. Eating Disord. 2009;17(3):187–99.
Kanayama G, Barry S, Hudson J, Pope H. Body image and attitudes toward male roles in anabolic-androgenic steroid users. Am J Psychiatr. 2006;163(4):697–703.
Pope H, Gruber AJ, Choi P, Olivardia R, Phillips KA. Muscle dysmorphia: an underrecognized form of body dysmorphic disorder. Psychosomatics. 1997;38(6):548–57.
McVeigh J. The public health implications of anabolic steroid use in the United Kingdom. A shot in the Dark: Steroids, IPEDs - the Hidden Harm Conference; 26th April 2018; Colchester2018.
Hanley Santos G, Coomber R. The risk environment of anabolic-androgenic steroid users in the UK: examining motivations, practices and accounts of use. Int J Drug Policy. 2017;40:35–43.
Bates G, Tod D, Leavey C, McVeigh J. An evidence-based socioecological framework to understand men’s use of anabolic androgenic steroids and inform interventions in this area. Drugs. 2018:1–9.
Pope HG, Kanayama G, Hudson JI. Risk factors for illicit anabolic-androgenic steroid use in male weightlifters: a cross-sectional cohort study. Biol Psychiatr. 2012;71(3):254–61.
de Ronde W. Preventing anabolic steroid abuse: a long way to go. J Intern Med. 2018.
Bates G, Begley E, Tod D, Jones L, Leavey C, McVeigh J. A systematic review investigating the behaviour change strategies in interventions to prevent misuse of anabolic steroids. J Health Psychol. 2017. https://doi.org/10.1177/1359105317737607 .
Backhouse S, Collins C, Defoort Y, McNamee M, Parkinson A, Sauer M. Study on doping prevention: a map of legal, regulatory and prevention practice provisions in EU 28. Luxembourg: Publications Office of the European Union; 2014. Report No.: 9279435426.
NICE. Drug misuse prevention: targeted interventions (NG64). London: NICE; 2017.
Zahnow R, McVeigh J, Ferris J, Winstock A. Adverse effects, health service engagement, and service satisfaction among anabolic androgenic steroid users. Contemp Drug Prob. 2017;44(1):69–83.
Kimergard A, McVeigh J. Variability and dilemmas in harm reduction for anabolic steroid users in the UK: a multi-area interview study. Harm Reduct J. 2014;11(ARTN 19).
Dunn M, Henshaw R, McKay F. Understanding health service use and needs of performance and image enhancing drug users in regional Queensland. Drug Alcohol Rev. 2014;33:24.
Wade CH. Anabolic steroids: doctors denounce them, but athletes aren't listening. Science. 1972;176:1401–3.
Brower KJ, Blow FC, Beresford TP, Fuelling C. Anabolic-androgenic steroid dependence. J Clin Psychiatry. 1989;50(1):31–3.
CAS PubMed Google Scholar
Copeland J, Peters R, Dillon P. A study of 100 anabolic-androgenic steroid users. Med J Aust. 1998;168(6):311–2.
Midgley SJ, Heather N, Davies JB. Dependence-producing potential of anabolic-androgenic steroids. Addict Res. 1999;7(6):539–50.
Pope HG Jr, Kanayama G, Athey A, Ryan E, Hudson JI, Baggish A. The lifetime prevalence of anabolic-androgenic steroid use and dependence in Americans: current best estimates. Am J Addict. 2014;23(4):371–7.
Ip EJ, Lu DH, Barnett MJ, Tenerowicz MJ, Vo JC, Perry PJ. Psychological and physical impact of anabolic-androgenic steroid dependence. Pharmacotherapy. 2012;32(10):910–9.
Pope HG Jr, Kean J, Nash A, Kanayama G, Samuel DB, Bickel WK, et al. A diagnostic interview module for anabolic-androgenic steroid dependence: preliminary evidence of reliability and validity. Exp Clin Psychopharmacol. 2010;18(3):203–2013.
Van de Ven K, Maher L, Wand H, Memedovic S, Jackson E, Iversen J. Health risk and health seeking behaviours among people who inject performance and image enhancing drugs who access needle syringe programs in Australia. Drug Alcohol Rev. 2018:doi: https://doi.org/10.1111/dar.12831 .
Jacka B, Peacock A, Degenhardt L, Bruno R, Clare P, Kemp R, et al. Trends in PIEDs use among male clients of needle-syringe programs in Queensland, Australia; 2007-2015. Int J Drug Policy. 2017;46:74–8.
Kimergard A, McVeigh J. Environments, risk and health harms: a qualitative investigation into the illicit use of anabolic steroids among people using harm reduction services in the UK. BMJ OPEN. 2014;4(6).
McVeigh J, Beynon C, Bellis MA. New challenges for agency based syringe exchange schemes: analysis of 11 years of data (1991–2001) in Merseyside and Cheshire, United Kingdom. Int J Drug Policy. 2003;14(5-6):399–405.
Glass R, Hope VD, Njoroge J, Edmundson C, Smith J, McVeigh J, et al. Secondary distribution of injecting equipment obtained from needle and syringe programmes by people injecting image and performance enhancing drugs: England and Wales, 2012-15. Drug Alcohol Depend. 2018;195:40–4.
NICE. Needle and syringe programmes NICE public health guidance. NICE: National Institute for Health and Care Excellence; 2014.
Public Health England. Providing effective services for people who use image and performance enhancing drugs. London: PHE Publications; 2015.
HM Government. 2017 Drug Strategy. London 2017.
Department of Health. Drug misuse and dependence: UK guidelines on clinical management. London: Department of Health; 2017.
Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Malone DA, Dimeff RJ. The use of fluoxetine in depression associated with anabolic steroid withdrawal: a case series. J Clin Psychiatry. 1992;53(4):130–2.
Hays LR, Littleton S, Stillner V. Anabolic steroid dependence. Am J Psychiatr. 1990;147(1):122.
Allnutt S, Chaimowitz G. Anabolic steroid withdrawal depression: a case report. The Canadian Journal of Psychiatry / La Revue canadienne de psychiatrie. 1994;39(5):317–8.
Papazisis G, Kouvelas D, Mastrogianni A, Karastergiou A. Anabolic androgenic steroid abuse and mood disorder: a case report. Int J Neuropsychopharmacol. 2007;10(2):291–3.
Gahr M, Kolle MA, Baumgarten E, Freudenmann RW. Mania related to mesterolone in a previously mentally healthy person. J Clinical Psychopharmacol. 2012;32(5):734–5.
Rashid W. Testosterone abuse and affective disorders. J Subst Abuse Treatment. 2000;18(2):179–84.
Ranjan R, Parmar A, Pattanayak RD, Dhawan A. Dependence on anabolic-androgenic steroids: a case report and brief review. Delhi Psychiatry J. 2014;17(2):481–4.
Duffy RM, Kelly BD. Steroids, psychosis and poly-substance abuse. Irish J Psychol Med. 2015;32(2):227–30.
Franey DG, Espiridion ED. Anabolic steroid-induced mania. Cureus. 2018;10(8):e3163–e.
PubMed PubMed Central Google Scholar
Stanley A, Ward M. Anabolic steroids--the drugs that give and take away manhood. A case with an unusual physical sign. Med Sci Law. 1994;34(1):82–3.
Brower KJ, Blow FC, Beresford TP, Fuelling C. Anabolic-androgenic steroid dependence. J Clin Psychiatry. 1989;50:31.
Tennant F, Black DL, Voy RO. Anabolic steroid dependence with opioid-type features. N Engl J Med. 1988;319(9):578.
van Breda E, Keizer HA, Kuipers H, Wolffenbuttel BHR. Androgenic anabolic steroid use and severe hypothalamic-pituitary dysfunction: a case study. Int J Sports Med. 2003;24(3):195–6.
Tan RS, Vasudevan D. Use of clomiphene citrate to reverse premature andropause secondary to steroid abuse. Fertility Sterility. 2003;79(1):203–5.
Menon DK. Successful treatment of anabolic steroid-induced azoospermia with human chorionic gonadotropin and human menopausal gonadotropin. Fertil Steril. 2003;79(Suppl 3):1659–61.
Gill GV. Anabolic steroid induced hypogonadism treated with human chorionic gonadotropin. Postgrad Med J. 1998;74(867):45–6.
Gazvani MR, Buckett W, Luckas MJ, Aird IA, Hipkin LJ, Lewis-Jones DI. Conservative management of azoospermia following steroid abuse. Hum Reprod. 1997;12(8):1706–8.
Bickelman C, Ferries L, Eaton RP. Impotence related to anabolic steroid use in a body builder. Response to clomiphene citrate. Western J Med. 1995;162(2):158–60.
CAS Google Scholar
Turek PJ, Williams RH, Gilbaugh JH III, Lipshultz LI. The reversibility of anabolic steroid-induced azoospermia. J Urol. 1995;153(5):1628–30.
Cohen JJ, Honig S. Anabolic steroid-associated infertility: a potentially treatable and reversible cause of male infertility. Fertility Sterility. 2005;84:S223.
Pirola I, Cappelli C, Delbarba A, Scalvini T, Agosti B, Assanelli D, et al. Anabolic steroids purchased on the Internet as a cause of prolonged hypogonadotropic hypogonadism. Fertility Sterility. 2010;94(6):2331.e1–3.
Street C, Scally MC. Pharmaceutical intervention of anabolic steroid induced hypogonadism - our success at restoration of the HPG axis. Med Sci Sports Exercise. 2000;32(5S).
Jarow JP, Lipshultz LI. Anabolic steroid-induced hypogonadotropic hypogonadism. Am J Sports Med. 1990;18(4):429–31.
Martin NM, Abu Dayyeh BK, Chung RT. Anabolic steroid abuse causing recurrent hepatic adenomas and hemorrhage. World J Gastroenterol. 2008;14(28):4573–5.
Sánchez-Osorio M, Duarte-Rojo A, Martínez-Benítez B, Torre A, Uribe M. Anabolic-androgenic steroids and liver injury. Liver Int. 2008;28(2):278–82.
Chahla E, Hammami MB, Befeler AS. Hepatotoxicity associated with anabolic androgenic steroids present in over-the-counter supplements: a case series. International Journal of Applied. 2014;4(3).
Awai HI, Yu EL, Ellis LS, Schwimmer JB. Liver toxicity of anabolic androgenic steroid use in an adolescent with nonalcoholic fatty liver disease. J Pediatr Gastroenterol Nutr. 2014;59(3):e32–e3.
Krishnan PV, Feng Z-Z, Gordon SC. Prolonged intrahepatic cholestasis and renal failure secondary to anabolic androgenic steroid-enriched dietary supplements. J Clin Gastroenterol. 2009;43(7):672–5.
Socas L, Zumbado M, Perez-Luzardo O, Ramos A, Perez C, Hernandez JR, et al. Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature. Br J Sports Med. 2005;39(5):e27.
Patil JJ, O'Donohoe B, Loyden CF, Shanahan D. Near-fatal spontaneous hepatic rupture associated with anabolic androgenic steroid use: a case report. Br J Sports Med. 2007;41(7):462–3.
Solbach P, Potthoff A, Raatschen HJ, Soudah B, Lehmann U, Schneider A, et al. Testosterone-receptor positive hepatocellular carcinoma in a 29-year old bodybuilder with a history of anabolic androgenic steroid abuse: a case report. BMC Gastroenterol. 2015;15:60.
Gorayski P, Thompson CH, Subhash HS, Thomas AC. Hepatocellular carcinoma associated with recreational anabolic steroid use. Br J Sports Med. 2008;42(1):74–5 discussion 5.
El Khoury C, Sabbouh T, Farhat H, Ferzli A. Severe cholestasis and bile cast nephropathy induced by anabolic steroids successfully treated with plasma exchange. Case Reports Med. 2017;2017.
Li C, Adhikari BK, Gao L, Zhang S, Liu Q, Wang Y, et al. Performance-enhancing drugs abuse caused cardiomyopathy and acute hepatic injury in a young bodybuilder. Am J Mens Health. 2018;12(5):1700–4.
Stepien PM, Reczko K, Wieczorek A, Zarebska-Michaluk D, Pabjan P, Krol T, et al. Severe intrahepatic cholestasis and liver failure after stanozolol usage - case report and review of the literature. Clin Exper Hepatol. 2015;1(1):30–3.
Elsharkawy AM, McPherson S, Masson S, Burt AD, Dawson RT, Hudson M. Cholestasis secondary to anabolic steroid use in young men. BMJ. 2012;344:e468.
Ampuero J, Garcia ES, Lorenzo MM, Calle R, Ferrero P, Gomez MR. Stanozolol-induced bland cholestasis. Gastroenterol Hepatol. 2014;37(2):71–2.
Singh V, Rudraraju M, Carey EJ, Byrne TJ, Vargas HE, Williams JE, et al. Severe hepatotoxicity caused by a methasteron-containing performance-enhancing supplement. J Clin Gastroenterol. 2008;43(3):287.
Boks M, Tiebosch AT, van der Waaij LA. A jaundiced bodybuilder Cholestatic hepatitis as side effect of injectable anabolic–androgenic steroids AU - Boks. Marije N J Sport Sci. 2017;35(22):2262–4.
Winwood PJ, Robertson DA, Wright R. Bleeding oesophageal varices associated with anabolic steroid use in an athlete. Postgrad Med J. 1990;66(780):864–5.
Ding NS, De Cruz P, Lim L, Thompson A, Desmond P. Androgenic-anabolic steroid drug-induced liver injury. Intern Med J. 2013;43(2):215–6.
Nasr J, Ahmad J. Severe cholestasis and renal failure associated with the use of the designer steroid Superdrol (methasteron): a case report and literature review. Dig Dis Sci. 2009;54(5):1144–6.
Marcacuzco Quinto AA, Manrique Municio A, Loinaz Segurola C, Jimenez Romero LC. Spontaneous hepatic rupture associated with the use of anabolic steroids. Cirugia Espanola. 2014;92(8):570–2.
Hymel BM, Victor DW, Alvarez L, Shores NJ, Balart LA. Mastabol induced acute cholestasis: a case report. World J Hepatol. 2013;5(3):133–6.
Flores A, Nustas R, Nguyen HL, Rahimi RS. Severe cholestasis and bile acid nephropathy from anabolic steroids successfully treated with plasmapheresis. ACG Case Rep J. 2016;3(2):133–5.
Diaz FC, Saez-Gonzalez E, Benlloch S, Alvarez-Sotomayor D, Conde I, Polo B, et al. Albumin dialysis with MARS for the treatment of anabolic steroid-induced cholestasis. Ann Hepatol. 2016;15(6):939–43.
Pais-Costa SR, Lima OA, Soares AF. Giant hepatic adenoma associated with anabolic-androgenic steroid abuse: case report. Arquivos brasileiros de cirurgia digestiva : ABCD = Brazilian archives of digestive surgery. 2012;25(3):180-2.
Hardt A, Stippel D, Odenthal M, Hölscher AH, Dienes H-P, Drebber U. Development of hepatocellular carcinoma associated with anabolic androgenic steroid abuse in a young bodybuilder: a case report. Case Reports in Pathology. 2012;2012:195607.
Kesler T, Sandhu RS, Krishnamoorthy S. Hepatology: hepatocellular carcinoma in a young man secondary to androgenic anabolic steroid abuse. J Gastroenterol Hepatol. 2014;29(11):1852.
Merino Garcia E, Borrego Utiel FJ, Martinez Arcos MA, Borrego Hinojosa J, Perez Del Barrio MP. Kidney damage due to the use of anabolic androgenic steroides and practice of bodybuilding. Nefrologia. 2018;38(1):101–3.
Tarashande Foumani A, Elyasi F. Oxymetholone-induced acute renal failure: a case report. Caspian J Intern Med. 2018;9(4):410–2.
Daher EF, Silva Junior GB, Queiroz AL, Ramos LM, Santos SQ, Barreto DM, et al. Acute kidney injury due to anabolic steroid and vitamin supplement abuse: report of two cases and a literature review. Int Urol Nephrol. 2009;41(3):717–23.
Colburn S, Childers WK, Chacon A, Swailes A, Ahmed FM, Sahi R. The cost of seeking an edge: recurrent renal infarction in setting of recreational use of anabolic steroids. Anna Med Surgery (2012). 2017;14:25–8.
Samaha AA, Nasser-Eddine W, Shatila E, Haddad JJ, Wazne J, Eid AH. Multi-organ damage induced by anabolic steroid supplements: a case report and literature review. J Med Case Rep. 2008;2:340.
Shimada Y, Yoritaka A, Tanaka Y, Miyamoto N, Ueno Y, Hattori N, et al. Cerebral infarction in a young man using high-dose anabolic steroids. J Stroke Cerebrovasc Dis. 2012;21(8):906.e9–11.
Sveinsson O, Herrman L. Cortical venous thrombosis following exogenous androgen use for bodybuilding. BMJ Case Rep. 2013;2013.
Garg P, Davis G, Wilson JI, Sivananthan M. Intravascular ultrasound and angiographic demonstration of left main stem thrombus-high-risk presentation in a young adult with anabolic steroid abuse. Am Heart Hosp J. 2010;8(2):E125–E7.
Shamloul RM, Aborayah AF, Hashad A, Abd-Allah F. Anabolic steroids abuse-induced cardiomyopathy and ischaemic stroke in a young male patient. BMJ Case Rep. 2014;2014.
Luc JGY, Buchholz H, Kim DH, MacArthur RGG. Left ventricular assist device for ventricular recovery of anabolic steroid-induced cardiomyopathy. J Surg Case Rep. 2018;2018(8):rjy221–rjy.
Santamarina RD, Besocke AG, Romano LM, Ioli PL, Gonorazky SE. Ischemic stroke related to anabolic abuse. Clin Neuropharmacol. 2008;31(2):80–5.
Edvardsson B. Hypertensive encephalopathy associated with anabolic–androgenic steroids used for bodybuilding. Acta Neurologica Belgica. 2015;115(3):457–8.
Sonmez E, Turkdogan KA, Yilmaz C, Kucukbuzcu S, Ozkan A, Sogutt O. Chronic anabolic androgenic steroid usage associated with acute coronary syndrome in bodybuilder. Turkish J Emerg Med. 2016;16(1):35–7.
Falkenberg M, Karlsson J, Ortenwall P. Peripheral arterial thrombosis in two young men using anabolic steroids. Eur J Vasc Endovasc. 1997;13(2):223–6.
Laroche GP. Steroid anabolic drugs and arterial complications in an athlete--a case history. Angiology. 1990;41(11):964–9.
Youssef MYZ, Alqallaf A, Abdella N. Anabolic androgenic steroid-induced cardiomyopathy, stroke and peripheral vascular disease. BMJ Case Reports. 2011;2011. https://doi.org/10.1136/bcr.12.2010.3650 .
Bispo M, Valente A, Maldonado R, Palma R, Glória H, Nóbrega J, et al. Anabolic steroid-induced cardiomyopathy underlying acute liver failure in a young bodybuilder. World J Gastroenterol. 2009;15(23):2920.
Goldstein DR, Dobbs T, Krull B, Plumb VJ. Clenbuterol and anabolic steroids: a previously unreported cause of myocardial infarction with normal coronary arteriograms. South Med J. 1998;91(8):780–4.
Güneþ Y, Erbaþ C, Okuyan E, Babalýk E, Gürmen T. Myocardial infarction with intracoronary thrombus induced by anabolic steroids. Anatol J Cardiol. 2004;4(4):357–8.
Christou GA, Christou KA, Nikas DN, Goudevenos JA. Acute myocardial infarction in a young bodybuilder taking anabolic androgenic steroids: a case report and critical review of the literature. Eur J Prev Cardiol. 2016;23(16):1785–96.
Stergiopoulos K, Brennan JJ, Mathews R, Setaro JF, Kort S. Anabolic steroids, acute myocardial infarction and polycythemia: a case report and review of the literature. Vasc Health Risk Manag. 2008;4(6):1475–80.
Santos RP, Pereira A, Guedes H, Lourenço C, Azevedo J, Pinto P. Anabolic drugs and myocardial infarction - a clinical case report. Arquivos brasileiros de cardiologia. 2015;105(3):316–9.
CAS PubMed PubMed Central Google Scholar
Ýlhan E, Demirci D, Güvenç TS, Çalýk AN. Acute myocardial infarction and renal infarction in a bodybuilder using anabolic steroids. Turk Kardiyol Dern Ars. 2010;38(4):275–8.
Huie MJ. An acute myocardial infarction occurring in an anabolic steroid user. Med Sci Sports Exerc. 1994;26(4):408–13.
Ferenchick GS, Adelman S. Myocardial infarction associated with anabolic steroid use in a previously healthy 37-year-old weight lifter. Am Heart J. 1992;124(2):507–8.
Lau DH, Stiles MK, John B, Shashidhar, Young GD, Sanders P. Atrial fibrillation and anabolic steroid abuse. Int J Cardiol. 2007;117(2):e86–7.
Mewis C, Spyridopoulos I, Kuhlkamp V, Seipel L. Manifestation of severe coronary heart disease after anabolic drug abuse. Clin Cardiol. 1996;19(2):153–5.
Ment J, Ludman PF. Coronary thrombus in a 23 year old anabolic steroid user. Heart. 2002;88(4):342.
Ahlgrim C, Guglin M. Anabolics and Cardiomyopathy in a bodybuilder: case report and literature review. J Card Fail. 2009;15(6):496–500.
Joseph J, Naqvi S, Sturm E. Reversible anabolic androgenic steroid-induced cardiomyopathy. Cardiovasc Disord Med. 2017;2(3):1–3.
Nieminen MS, Ramo MP, Viitasalo M, Heikkila P, Karjalainen J, Mantysaari M, et al. Serious cardiovascular side effects of large doses of anabolic steroids in weight lifters. Eur Heart J. 1996;17(10):1576–83.
Stannard JP, Bucknell AL. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med. 1993;21(3):482–5.
Farkash U, Shabshin N, Pritsch M. Rhabdomyolysis of the deltoid muscle in a bodybuilder using anabolic-androgenic steroids: a case report. J Athletic Train (National Athletic Trainers' Association). 2009;44(1):98–100.
Fenelon C, Dalton DM, Galbraith JG, Masterson EL. Synchronous quadriceps tendon rupture and unilateral ACL tear in a weightlifter, associated with anabolic steroid use. BMJ Case Rep. 2016;2016.
Bagherifard A, Jabalameli M, Rezazadeh J, Ghaffari S, Tabrizian P. Simultaneous bilateral quadriceps tendon rupture following a low - energy trauma in a male body builder with the history of anabolic - androgenic steroids consumption. Shafa Orthopedic J. 2018;5(2).
Liow RY, Tavares S. Bilateral rupture of the quadriceps tendon associated with anabolic steroids. British J Sports Med. 1995;29(2):77–9.
KramhØFt M, Solgaard S. Spontaneous rupture of the extensor pollicis longus tendon after anabolic steroids. J Hand Surg. 1986;11(1):87.
Tapaninen T, P V. Simultaneous bilateral rupture of the quadriceps tendon associated with anabolic steroids - a case report. Annals of Clinical Case Reports. 2016;1(1220).
David HG, Green JT, Grant AJ, Wilson CA. Simultaneous bilateral quadriceps rupture: a complication of anabolic steroid abuse. J Bone Joint Surgery British Volume. 1995;77(1):159–60.
Visuri T, Lindholm H. Bilateral distal biceps tendon avulsions with use of anabolic steroids. Med Sci Sports Exerc. 1994;26(8):941–4.
Freeman BJ, Rooker GD. Spontaneous rupture of the anterior cruciate ligament after anabolic steroids. Br J Sports Med. 1995;29(4):274–5.
Adamson R, Rambaran C, D'Cruz DP. Anabolic steroid-induced rhabdomyolysis. Hospital Med (London, England: 1998). 2005;66(6):362.
Erturan G, Davies N, Williams H, Deo S. Bilateral simultaneous traumatic upper arm compartment syndromes associated with anabolic steroids. J Emerg Med. 2013;44(1):89–91.
Leopardi P, Vico G, Rosa D, Cigala F, Maffulli N. Reconstruction of a chronic quadriceps tendon tear in a body builder. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1007–11.
Rich JD, Dickinson BP, Flanigan TP, Valone SE. Abscess related to anabolic-androgenic steroid injection. Med Sci Sports Exerc. 1999;31(2):207–9.
Friedman O, Arad E, Ben AO. Body builder's nightmare: black market steroid injection gone wrong: a case report. Plastic Reconstructive Surgery Global Open. 2016;4(9):e1040.
Shiber JR. Pyomyositis due to anabolic steroid injection. J Emerg Med. 2013;44(1):e69–70.
Evans NA. Local complications of self administered anabolic steroid injections. Br J Sports Med. 1997;31(4):349–50.
Tüzel E. Spontaneous corpus cavernosum abscess in a healthy man using long-term androgenic anabolic steroids. World J Mens Health. 2015;33(1):36–8.
Grant S, Dearing J, Ghosh S, Collier A, Bal AM. Necrotizing myositis of the deltoid following intramuscular injection of anabolic steroid. Int J Infect Dis. 2010;14(9):e823–4.
Marquis C, Maffulli N. Anabolic steroid related abscess - a risk worth taking? Injury Extra. 2006;37:451–4.
Ray S, Masood A, Pickles J, Moumoulidis I. Severe laryngitis following chronic anabolic steroid abuse. J Laryngol Otol. 2008;122(3):230–2.
Maini AAN, Maxwell-Scott H, Marks DJB. Severe alkalosis and hypokalemia with stanozolol misuse. Am J Emerg Med. 2014;32(2):196.e3–4.
Labib M, Haddon A. The Adverse effects of anabolic steroids on serum lipids. Ann Clin Biochem. 1996;33(3):263–4.
Cooper I, Reeve N, Doherty W. Delayed diagnosis of a cerebrovascular accident associated with anabolic steroid use. BMJ Case Rep. 2011;2011.
Unai S, Miessau J, Karbowski P, Baram M, Cavarocchi NC, Hirose H. Caution for anabolic androgenic steroid use: a case report of multiple organ dysfunction syndrome. Respiratory Care. 2013;58(12):e159–63.
Geraci MJ, Cole M, Davis P. New onset diabetes associated with bovine growth hormone and testosterone abuse in a young body builder. Hum Exp Toxicol. 2011;30(12):2007–12.
Alaraj AM, Chamoun RB, Dahdaleh NS, Haddad GF, Comair YG. Spontaneous subdural haematoma in anabolic steroids dependent weight lifters: reports of two cases and review of literature. Acta Neurochir (Wien). 2005;147(1):85–7 discussion 7-8.
Moor JW, Khan MI. Growth hormone abuse and bodybuilding as aetiological factors in the development of bilateral internal laryngocoeles. a case report. Eur Arch Otorhinolaryngol. 2005;262(7):570–2.
Tan RS, Scally MC. Anabolic steroid-induced hypogonadism – towards a unified hypothesis of anabolic steroid action. Med Hypotheses. 2009;72(6):723–8.
Kanayama G, Hudson JI, Pope HG. Long-term psychiatric and medical consequences of anabolic–androgenic steroid abuse: a looming public health concern? Drug Alcohol Depend. 2008;98(1):1–12.
Kanayama G, Hudson JI, DeLuca J, Isaacs S, Baggish A, Weiner R, et al. Prolonged hypogonadism in males following withdrawal from anabolic-androgenic steroids: an under-recognized problem. Addiction (Abingdon, England). 2015;110(5):823–31.
de Souza GL, Hallak J. Anabolic steroids and male infertility: a comprehensive review. BJU Int. 2011;108(11):1860–5.
Pope HG, Kanayama G, Ionescu-Pioggia M, Hudson JI. Anabolic steroid users' attitudes towards physicians. Addiction. 2004;99(9):1189–94.
Hope VD, McVeigh J, Marongiu A, Evans-Brown M, Smith J, Kimergard A, et al. Injection site infections and injuries in men who inject image- and performance-enhancing drugs: prevalence, risks factors, and healthcare seeking. Epidemiol Infection. 2015;143(1):132–40.
Bates G, McVeigh J. Image and performance enhancing drugs - 2015 survey results. Liverpool: Centre for Public Health; 2016.
Brooks JHM, Ahmad I, Easton G. 10-minute consultation anabolic steroid use. Bmj-Brit Med J. 2016;355.
Kanayama G, Boynes M, Hudson JI, Field AE, Pope HG. Anabolic steroid abuse among teenage girls: an illusory problem? Drug Alcohol Depend. 2007;88(2-3):156–62.
Korkia P, Lenehan P, McVeigh J. Non-medical use of androgens among women. J Perform Enhanc Drugs. 1996;1(2):71.
Ip EJ, Barnett MJ, Tenerowicz MJ, Kim JA, Wei H, Perry PJ. Women and anabolic steroids: an analysis of a dozen users. Clin J Sport Med. 2010;20(6):475–81.
Hoberman J. Dopers in uniform: Police officers' use of anabolic steroids in the United States. In: Møller V, Waddington I, Hoberman JM, Møller V, Waddington I, Hoberman JM, editors. Routledge handbook of drugs and sport. New York, NY, US: Routledge/Taylor & Francis Group; 2015. p. 439–52.
Chapter Google Scholar
Turvey BE, Crowder S. Anabolic steroid abuse in public safety personnel: a forensic manual. San Diego: Academic Press; 2015.
Humphrey KR, Decker KP, Goldberg L, G. PH, Green GA. Anabolic steroid use and abuse by police officers: policy & prevention. The Police Chief. 2008;LXXV.
Waterhouse J. Rise in soldiers testing positive for steroid use. Newsbeat [Internet]. 2014 25/3/2019.
Bolding G, Sherr L, Maguire M, Elford J. HIV risk behaviours among gay men who use anabolic steroids. Addiction (Abingdon, England). 1999;94(12):1829–35.
Bolding G, Sherr L, Elford J. Use of anabolic steroids and associated health risks among gay men attending London gyms. Addiction. 2002;97(2):195–203.
Cornford CS, Kean J, Nash A. Anabolic-androgenic steroids and heroin use: a qualitative study exploring the connection. Int J Drug Policy. 2014;25(5):928–30.
Kanayama G, Pope HG, Hudson JI. Associations of anabolic-androgenic steroid use with other behavioral disorders: an analysis using directed acyclic graphs. Psychol Med. 2018:1–8.
Salinas M, Floodgate W, Ralphs R. Polydrug use and polydrug markets amongst image and performance enhancing drug users: Implications for harm reduction interventions and drug policy. Int J Drug Policy. 2019;67:43–51.
Kimergard A. A qualitative study of anabolic steroid use amongst gym users in the United Kingdom: motives, beliefs and experiences. J Subst Use. 2015;20(4):288–94.
Taylor WN. Anabolic steroids and the athlete. 2 ed. Jefferson, NC: MacFarland and Company Inc. Publishers; 2001.
Pampel FC. Drugs and Sport. New York: Facts on File; 2007.
Download references
Acknowledgements
Not applicable.
No funding was received to support this review.
Author information
Authors and affiliations.
Public Health Institute, Liverpool John Moores University, Liverpool, England
Geoff Bates & Marie-Claire Van Hout
MRC/CSO SPHSU, University of Glasgow, Glasgow, Scotland
Joseph Tay Wee Teck
Department of Sociology, Manchester Metropolitan University, Manchester, England
Jim McVeigh
You can also search for this author in PubMed Google Scholar
Contributions
GB managed the review and lead protocol development, evidence search, article screening, data extraction and data synthesis. GB drafted the article methodology and result sections. MCVH provided methodological and topic expertise and helped to shape the review through supporting the development of the protocol and search strategy. MCVH screened a proportion of articles and commented on findings and written drafts. JT provided medical expertise supporting the development of the review and presentation of data, checked data extraction, and commented on written drafts. JMV provided topic expertise and helped to shape the review through supporting the development of the protocol, data extraction, data synthesis and presentation of findings. JMV drafted the article introduction and discussion sections. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Geoff Bates .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Data extraction tables. The data extraction tables contain the full data extracted from the 109 articles included in the review. This includes participant information, condition requiring treatment, the treatment provided and the outcomes of treatment.
Additional file 2.
Search strategy. The full search strategy used in Medline is provided.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bates, G., Van Hout, MC., Teck, J.T.W. et al. Treatments for people who use anabolic androgenic steroids: a scoping review. Harm Reduct J 16 , 75 (2019). https://doi.org/10.1186/s12954-019-0343-1
Download citation
Received : 02 May 2019
Accepted : 21 November 2019
Published : 30 December 2019
DOI : https://doi.org/10.1186/s12954-019-0343-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Drug treatment
- Health care
- Behaviour change
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
6 Serious Health Risks of Steroid Drug Use to Boost Athletic Ability
Taking anabolic steroids for muscle and performance enhancement is illegal. And doctors want you to know they can also pose significant risks to health.
Next up video playing in 10 seconds
In sports, the use of performance-enhancing drugs is illegal and has led to a fall from grace for some big athletes.
In 2007, the Olympic runner Marion Jones was stripped of five medals won during the 2000 Olympic games after she admitted to using anabolic steroids. The scandal around Major League Baseball’s Barry Bonds’s steroid use lasted years during the early 2000s, and resulted in his being convicted of perjury.
But some social media users may have forgotten these high-profile downfalls, as they boast of the fitness and muscle gains from taking the same illegal drugs.
The bodybuilder and TikToker David Rau (25,600 followers) has been open about his experience. In videos, he’s shared how-tos , comparison photos of physiques attained naturally versus with steroids , and the purported benefits of being on anabolic steroids, according to him (confidence, mental sharpness, and increased muscle mass).
Others, like the TikToker Caroline Mathias (34,000 followers) are calling out steroid drug use by popular social media personal-trainer influencers.
Doctors warn people not to be duped by the attention and praise social media influencers are gathering for these drugs. Anabolic steroids and other performance-enhancing drugs can come with some serious and irreversible health risks and consequences.

What Are Anabolic Steroids?
Anabolic-androgenic steroids (AAS) are man-made versions of testosterone, which is the primary sex hormone in men, according to MedlinePlus . Testosterone is responsible for the appearance of features we associate with masculinity — a deep voice, facial hair, and bulging muscles. The steroids can be taken orally, as injections, or applied topically to the skin.
These hormones are widely misused in high doses because people want large muscles and improved athletic performance, according to a review published in December 2022 in Frontiers in Endocrinology .
“Anabolic steroids greatly enhance muscle mass and increase metabolism and fat breakdown,” says Diederik Smit, an internist specializing in endocrinology and the use of anabolic steroids in Tilburg, Netherlands, and a coauthor of the review. “Besides larger muscles and increased strength, men using AAS usually are leaner. This makes the steroids very suitable for bodybuilding purposes because this is all about muscle size and definition.”
Some anabolic steroid drugs include:
- Testosterone
- Fluoxymesterone
- Mesterolone
- Methyltestosterone
- Nandrolone deconoate
- Nandrolone phenpropionate
- Oxandrolone
- Oxymetholone
Anabolic steroids have been used in this way since the 1950s, according to research . But since then they’ve been banned by several athletic organizations as performance-enhancing drugs (more on that below).
Anabolic steroids can serve a medical purpose. According to the Department of Justice’s Drug Enforcement Administration (DEA) , they’re called on as treatments for:
- Testosterone deficiency
- Delayed puberty
- Breast cancer
- Low red blood cell count
- AIDS-related tissue wasting
They can also be prescribed to help people gain weight after illness, injury, or infection, or to those who have trouble gaining weight for unknown reasons, according to the Mayo Clinic .
A few anabolic steroids are approved for medical use in humans and pets for the aforementioned conditions with a valid prescription, but by and large these are illegal and classified as Schedule 3 substances under the Controlled Substances Act, according to the DEA.
They’ve also been banned by the International Olympic Committee since the mid-1970s, and subsequently by most athletic organizations, per previous research.
It’s when these steroids are used for the wrong reasons (and at doses of 10 to 100 times higher than doses that would be used to treat medical conditions), such as for bodybuilding or enhancing athletic performance, that they become dangerous and illegal, according to MedlinePlus.
Anabolic steroids are different from general steroids, known as corticosteroids, which are anti-inflammatory drugs such as prednisone and cortisone, according to the Cleveland Clinic .
6 Risks of Anabolic Steroids When Used for the Wrong Reasons
Not only are they illegal when taken outside of the care of a medical professional to treat specific medical conditions, but they can be dangerous. Side effects can start after about two or three weeks of use, generally around the same time that the positive effects reveal themselves, Smit says.
Here are six potential side effects of anabolic steroids when they're taken at high doses and absent a clear medical indication.
1. Heart and Liver Trouble
“The increased risk of cardiovascular disease is one of the most serious consequences of steroid use,” says Sean Byers, MD , a medical adviser in Los Angeles for Health Report Live.
The DEA reports the steroids could heighten cholesterol levels, which may lead to stroke, heart attack, or coronary artery disease.
A study published November 2018 in the International Journal of Sports and Exercise Medicine found that anabolic steroids decrease HDL cholesterol (so-called “good cholesterol”) by more than 90 percent and increase LDL cholesterol (“bad cholesterol”) by about 50 percent. The researchers found levels returned to normal about four months after participants stopped taking them.
“Long-term use [of steroids] predisposes to heart attacks and strokes, much like smoking, hypertension, and bad cholesterol do,” Smit says. “The heart muscle also increases in size, and not particularly in a good manner. This so-called hypertrophy may decrease cardiac function and cause dangerous arrhythmias.”
Oral steroids can also lead to liver trouble, including the development of tumors, according to research published in May 2020 in LiverTox .
2. Stunted Growth in Young People
These steroids could impact adult height if they're taken in adolescence, according to the DEA. This happens because the bones end up maturing too quickly and then stop growing, according to Nemours KidsHealth .
3. Aggressive Behavior
Ever heard the term “roid rage”? This is the personality change one may experience as a result of taking anabolic steroids. Many people find themselves becoming hostile, experiencing major mood swings, and engaging in aggressive behavior, per the DEA. This can sometimes lead to depression and suicide once the steroids have been stopped.
4. Physical Changes
Many of the side effects are the same for men and women, Smit says. But not all. Men on anabolic steroids may experience baldness, breast growth, and shrinking testicles, according to MedlinePlus.
Women, on the other hand, may find themselves with a deeper voice, more hair on the face and body, male pattern baldness, changes to their menstrual cycle, and a lengthening of the clitoris, according to the DEA . And while many of the side effects for anabolic steroids go away once the drugs are stopped, some of these changes to women can become permanent, Smit says.
5. Male Infertility
Steroids can negatively impact a man’s fertility. Testosterone plays an important role in male reproductive organs and sexual function, according to research , but taking testosterone through steroids can inhibit two other reproductive hormones — FSH and LH.
Steroids can also lead to abnormalities in sperm motility and morphology. It’s possible this can be reversed — the previous study showed sperm can return to normal after four months or so.
Smit adds, though, that other studies haven’t been so promising, so it’s unknown if male fertility always rebounds. “This may have consequences if they still desire to have children later in life,” he says.
Acne tends to appear along the chest, face, neck, back, and arms in response to high doses of steroids, according to the DermNet . The chest is the most common area, and steroid acne tends to be more uniform than usual acne. While not the most serious of side effects, it’s worth noting because it can affect about half of steroid abusers, according to previous research . “Acne can be disfiguring but is manageable,” Smit says.
For men, many of these side effects can be reversed once the steroid is stopped, according to the Cleveland Clinic . But it can be hard to stop, with more than 50 percent of users becoming dependent, per previous research.
Anabolic Steroids - Abuse, Side Effects and Safety
Medically reviewed by Leigh Ann Anderson, PharmD . Last updated on July 16, 2024.
What are Anabolic Steroids?
Androgens and anabolic steroids include the endogenous male sex hormone testosterone and dihydrotestosterone, and other agents that behave like these sex hormones. Androgens stimulate the development of male sexual characteristics (such as deepening of the voice and beard growth) and development of male sex organs. Anabolic steroids stimulate growth in many other types of tissues, especially bone and muscle. Anabolic effects also include increased production of red blood cells.
Medically, androgens and anabolic steroids are used to treat:
- delayed puberty in adolescent boys
- hypogonadism and impotence in men
- breast cancer
- osteoporosis
- weight loss disease in HIV
- endometriosis
- other conditions with hormonal imbalance
Anabolic steroids can be given by injection, taken by mouth, or used externally. In the U.S. they are primarily classified as Schedule III Controlled Substances due to the possibility of serious adverse effects and a high potential for abuse.
Are Anabolic Steroids Prohibited in Sports?
Some athletes may abuse anabolic steroids to build muscle, prolong endurance and enhance performance. Anabolic agents are prohibited at all times, both in- and out-of-competition in collegiate and professional sports and appear on both the World Anti-Doping Agency (WADA) and U.S. Anti-Doping Agency (USADA) Prohibited Lists . Anabolic steroid use is also prohibited by the International Olympic Committee (IOC) as well as the National Collegiate Athletic Association (NCAA). 1,2
Anabolic steroids include all synthetic derivatives of testosterone, both oral and injectable. Examples of anabolic steroids include testosterone, methyltestosterone, danazol, and oxandrolone. Anabolic steroids are performance-enhancing drugs and act by increasing lean muscle protein synthesis and body weight, without increasing fat mass. 3
What is the Extent of Illicit Anabolic Steroid Use in the U.S?
Illegal use and street purchase of anabolic steroids is risky. Illicit steroids may be sold at gyms, sporting competitions, and via mail order. Buyers may be at risk of purchasing adulterated or contaminated products.
Often, illicit steroids are smuggled into the U.S. from countries that do not require a prescription for the purchase of steroids. Steroids may also be illegally sourced from U.S. pharmacies or synthesized in backroom laboratories.
Anabolic steroids were made illegal to purchase or sell without a prescription in the Anabolic Steroids Control Act of 1990. 9
Common street names that are used to refer to anabolic steroids may include:
Abuse of anabolic steroids can occur in any age group, but statistics on their abuse is difficult to determine because many surveys on drug abuse do not include steroids. According to the National Institute on Drug Abuse (NIDA), scientific evidence indicates that anabolic steroid abuse among athletes may range between 1 and 6 percent. 2 , 5
Not surprisingly, prevalence of steroid use is higher in males than females. Laboratory drug testing can usually detect the presence of anabolic steroids, and athletes in higher level sports are frequently monitored for abuse of a large number of drugs, including steroids.
In the 2023 Monitoring the Future Survey , high school seniors reported a 0.7% use of steroids in the last 12 months, a drop from 1.3% in 2022. 7,9 Reported anabolic steroid use was 0.6% in 8th graders and 0.5% in 10th graders in the past 12 months for the 2023 survey. In 2023 the lifetime prevalence of anabolic steroid use was 1% in all grades. 9
Steroid use for grades 8-12 reached a peak in 2001-2002 (ranging from 1.6% to 2.5% in the last 12 months) and have since declined substantially.
Steroidal dietary supplements can be converted into testosterone or other androgenic compounds in the body. Steroidal over-the-counter dietary supplements such as androstenedione and tetrahydrogestrinone (THG) were previously available without prescription through health food stores, however, these supplements are now classified as controlled substances. 3,8
Dehydroepiandrosterone (DHEA), another steroidal dietary supplement is still available legally; however, it does appear on the U.S. Anti-Doping Agency’s list of prohibited agents for both in- and out-of-competition. In almost all countries except the U.S., DHEA is treated as a controlled anabolic steroid. Clinical research reports indicate that these agents are ineffective or lack evidence of performance-enhancing effects, and can be linked with many serious side effects and drug interactions. 3,4 ,6
Related : Explore the World Anti-Doping Agency (WADA) list of prohibited agents in sports
What are the Most Common Side Effects That May Occur with Anabolic Steroid Use?
There is a wide array of serious side effects associated with abuse of anabolic steroids - an example list can be found here. 4
Steroid use can alter the normal hormonal production in the body. Most side effects can be reversed if the drugs are stopped, but some, such as a deepened voice in women may persist. Data on long-term side effects primarily come from case reports and not from well-controlled, long-term epidemiological studies, which might be more reliable. 4
Common side effects with anabolic steroids may include:
- severe acne , oily skin and hair
- l iver disease , such as liver tumors and cysts
- kidney disease
- heart disease, such as heart attack and stroke
- altered mood, irritability, increased aggression, depression or suicidal tendencies
- alterations in cholesterol and other blood lipids
- high blood pressure
- gynecomastia (abnormal development of mammary glands in men causing breast enlargement)
- shrinking of testicles
- azoospermia (absence of sperm in semen)
- menstrual irregularities in women
- infertility
- excess facial or body hair (hirsutism), deeper voice in women
- stunted growth and height in teens
- risk of viral or bacterial infections due to unsterile injections
Are Anabolic Steroids Addictive?
Users of anabolic steroids can become both physically and psychologically dependent upon the drugs, as evidenced by:
- a drug-seeking behavior
- continued use even with adverse effects
- physical withdrawal symptoms such as mood swings, fatigue, restlessness, loss of appetite, insomnia, reduced sex drive, and steroid cravings.
Severe withdrawal can lead to depression and possible suicide. Depressive symptoms can persist for up to one year after the user stops taking the steroid. 4
Supportive treatments and medication interventions may be needed for severe addiction. Medications that have been used for treating anabolic steroid withdrawal allow the natural hormonal system to restore. Other medications target specific withdrawal symptoms.
For example, antidepressants may be prescribed to treat depressive episodes and analgesics , such as acetaminophen or ibuprofen, may be used for headaches and muscle and joint pains. Some patients may also undergo behavioral therapies. 4
What is Being Done to Combat Anabolic Steroid Abuse?
Awareness and educational efforts are working to help prevent anabolic steroid abuse in schools and communities. The Adolescents Training and Learning to Avoid Steroids (ATLAS) and the Athletes Targeting Healthy Exercise and Nutrition Alternatives (ATHENA) programs are scientifically-proven programs that teach athletes they do not need steroids to build powerful muscles and improve athletic performance.
These programs provide:
- weight-training and nutrition alternatives
- increase healthy behaviors
- less likelihood to try steroids
- less likelihood to engage in other dangerous behaviors such as drinking and driving, use of marijuana and alcohol , and and improved body image.
- education on ways to refuse an offer of illicit drugs
Both Congress and the Substance Abuse and Mental Health Services Administration endorsed these model prevention programs. 4,7
Learn more : The Risks for Teenagers of Using Steroids
- Blood Doping: Lance Armstrong & Pro Cycling
- Can a Drug Test Lead to a False Positive?
- Drug Testing FAQs
- The Risks for Teenagers of Using Steroids
- Toxicology Drug Testing
- U-47700 (Pink)
Treatment options
- Medications for Substance Abuse
Symptoms and treatments
- Sedative, Hypnotic or Anxiolytic Drug Use Disorder
- United States Global Drug Reference Online. Drug Search. Accessed July 16, 2024 at https://www.globaldro.com/us/search
- The World Anti-Doping Agency (WADA) Website. 2020 List of Prohibited Substances and Methods. Accessed July 16, 2024. https://www.wada-ama.org/en/prohibited-list
- Jenkinson DM, Harbert AJ. Supplements and sports. Am Fam Physician. 2008 Nov 1;78(9):1039-46. PMID: 19007050. Accessed July 16, 2024.
- National Institute on Drug Abuse (NIDA). Anabolic steroids and other Appearance and Performance Enhancing Drugs (APEDs). Accessed July 16, 2024 at https://nida.nih.gov/research-topics/anabolic-steroids
- Dehydroepiandrosterone (DHEA). NPP. Drugs.com. Accessed July 16, 2024 at https://www.drugs.com/npp/dehydroepiandrosterone.html
- ATLAS and ATHENA Program Materials. Oregon Health and Science University. Accessed July 16, 2024 at https://www.ohsu.edu/ortho/high-school-athlete-program
- Monitoring the Future: National Survey Results on Drug Use 1975-2021. Jan. 2022. Institute for Social Research The University of Michigan.
- Controlled Substances. DEA. April 12, 2022. Accessed July 16, 2024 at https://www.deadiversion.usdoj.gov/schedules/orangebook/c_cs_alpha.pdf
- Miech, R. A., Johnston, L. D., Patrick, M. E., et al. (2024). Monitoring the Future national survey results on drug use, 1975–2023: Overview and detailed results for secondary school students. Monitoring the Future Monograph Series. Ann Arbor, MI: Institute for Social Research, University of Michigan. Accessed July 16, 2024 at https://monitoringthefuture.org/data/bx-by/drug-prevalence/#drug=%22Steroids%22
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
- Men's Health
- Sexual Health Problems
- Men’s Conditions
- Living Better
- View Full Guide
How Dangerous Are Anabolic Steroids?

What Are Anabolic Steroids?
Anabolic steroids are drugs made in a lab that mimic the naturally occurring male sex hormones called androgens. Testosterone is the primary type of androgen. Doctors prescribe anabolic steroids to promote the growth of skeletal muscle and the development of male sexual characteristics for conditions such as low testosterone (male hypogonadism), certain cancers , or acquired immunodeficiency syndrome (AIDS).
Around 3 to 4 million people in the U.S. use anabolic steroids without a prescription for nonmedical purposes. They're the most common appearance- and performance-enhancing drugs (APEDs). Some athletes and bodybuilders may use them as a way to enhance their physical appearance.
Anabolic steroid street names
Slang words for steroids are hard to find. Most people just say steroids.
The scientific name for this class of drugs is anabolic-androgenic steroids. Anabolic refers to muscle building . Androgenic refers to increased male characteristics. But even scientists shorten it to anabolic steroids.
Although the nicknames for anabolic steroids change over time, some of the current common names according to the United States Drug Enforcement Administration include:
- Weight gainers
Anabolic steroids vs. corticosteroids
Corticosteroids are general steroid medications that reduce inflammation and dampen the activity of your immune system. They're lab-made to work like cortisol, a hormone made by your adrenal glands.
Doctors prescribe corticosteroids much more often than anabolic steroids. You may need them to treat conditions such as asthma , eczema, muscle and joint conditions, lupus, or multiple sclerosis.
How Do Anabolic Steroids Work?
Anabolic steroids activate androgen receptors in your body. That means they create the same effect that androgens do in the body. This makes them an ideal treatment for people dealing with low testosterone levels.
They can also help lower estrogen levels, which can help treat estrogen receptor positive breast cancer by blocking the growth of cancer cells that use estrogen to grow. For people with cancer or AIDS who are losing muscle, anabolic steroids increase the number of androgen receptors in skeletal muscle and increase it in size and strength.
Anabolic Steroid Types
Anabolic steroid pills
Anabolic steroids you take by mouth are available in tablet or capsule form. Some you take sublingually, which means under the tongue.
Other forms of anabolic steroids
- Creams or topical gels
- Pellets you implant under the skin
List of anabolic steroids
The different types of anabolic steroids a doctor can prescribe include:
- Danazol (Danocrine)
- Fluoxymesterone (Androxy, Halotestin)
- Mesterolone (Proviron)
- Methyltestosterone (Android, Methitest, Testred, Virilon)
- Nandrolone Decanoate (Deca-Durabolin)
- Nandrolone Phenpropionate (Durabolin)
- Oxandrolone (Oxandrin)
- Oxymetholone (Anadrol)
- Testosterone buccal system (Striant)
- Testosterone capsules (Jatenzo)
- Testosterone injection (Andro-L.A., Aveed, Delatestryl, Depo-Testosterone, Virilon, Xyosted)
- Testosterone nasal gel (Natesto)
- Testosterone patches (Androderm, Testoderm)
- Testosterone skin solution (Axiron)
- Testosterone subcutaneous pellets (Testopel)
Anabolic Steroid Uses
Doctors use these drugs to help treat delayed puberty, and improve muscle mass and strength in people who have conditions that reduce muscle tissue. Some doctors prescribe it for testosterone supplementation therapy to improve mood and sexual performance in older men.
Anabolic steroids for muscle growth
The misuse of anabolic steroids is common among athletes because it increases lean muscle mass more quickly and dramatically when combined with weight lifting than weight lifting alone. Many people who take it deal with a body dysmorphic disorder called muscle dysmorphia, which is a preoccupation with muscle size and the fear that muscles are too small.
Cycling and stacking
Some people "cycle" their anabolic steroid use by taking the drugs for a while and then pausing for a while before they start them again. Another method called "stacking" involves taking more than one type of anabolic steroid at a time in hopes that this will make the drugs work better.
"Pyramiding" is another type of anabolic steroid usage people try to prevent harmful side effects. This involves a combination of both stacking and cycling. You start by taking a low dose of one or more anabolic steroids, and then increase your dosage over time. Once you get to a maximum dose, you stop taking them for a rest period before starting again.
When anabolic steroids are staggered, overlapped, or substituted with another type of steroid to avoid developing tolerance, this is called "plateauing." There's no scientific research that shows any of these methods improve the drugs or reduce the risk of negative effects.
Anabolic Steroid Effects
To use anabolic steroids safely, you need a prescription and supervision of a doctor.
Some of the typical side effects of the drug include:
- Ankle swelling
- Problems peeing
- Breast enlargement in people assigned male at birth
- Reduced breast size in people assigned female at birth
- Worse sleep apnea, if you have it
- Decrease in testicle size
- Vaginal dryness, burning, itching, or bleeding
- Changes to your period
The average nonprescription dose of anabolic steroids is 10–100 times stronger than one a doctor would prescribe. This makes side effects much more severe when you use them without a prescription. Some can be reversed, but some are permanent.
Anabolic Steroid Side Effects
If you take anabolic steroids outside of a doctor's care, you may have serious side effects that can have a negative impact on your health. You're at risk of:
- High blood pressure
- Blood clots
- Heart issues, including heart attack
- Liver damage
- Short stature (if you're an adolescent)
- Male-pattern baldness
- Major depressive disorder.
Are anabolic steroids addictive?
Nearly one-third of people who misuse anabolic steroids become dependent on them. That means over time it starts to take higher and more frequent doses to get the same effects.
People who become dependent on anabolic steroids can also have withdrawal symptoms if they stop taking them. Without the drug in their system, they may feel tired and restless, stop eating and sleeping, lose their sex drive, and crave the drug. In some cases, withdrawal causes depression and thoughts of suicide.
Anabolic Steroid Complications
Your moods and emotions are balanced by the limbic system of your brain. Steroids act on the limbic system and may cause irritability and mild depression. Eventually, steroids can cause mania, delusions, and violent aggression, or "roid rage."
When steroids get into the body, they go to different organs and muscles. Steroids affect individual cells and make them create proteins. These proteins cause issues such as:
- Tumor growth in the liver
- Peliosis hepatis (blood-filled cysts on the liver that can rupture and cause internal bleeding)
- Atherosclerosis , which causes fat deposits inside arteries to disrupt blood flow. When blood flow to the heart is blocked, a heart attack can occur. If blood flow to the brain is blocked, a stroke can result.
- Weakened immune system, which increases your risk of infection and illness
If you inject anabolic steroids and share a needle with others, you're at great risk of getting HIV, hepatitis B, and hepatitis C.
Can you overdose on anabolic steroids?
Anabolic steroids aren't a drug you can overdose on. The negative effects of the drug are ones that develop over time.
Treatment for Anabolic Steroid Misuse
Studies show that few people who misuse anabolic steroids seek treatment to stop using them. To treat steroid use, the most effective methods involve uncovering the underlying causes of the misuse.
Treatment options include:
- Therapy and possibly medication for muscle dysmorphia
- Endocrine therapies to help treat low testosterone levels after stopping anabolic steroids to help prevent and reduce symptoms of depression
- Antidepressants
- Drug and psychosocial treatments for people who are also dependent on opioids. These methods may work to reduce dependence on anabolic steroids
Are Anabolic Steroids Illegal?
Anabolic steroids are Schedule III substances under the Controlled Substances Act. That means it's illegal to use them without a prescription. Only a small number of anabolic steroids are approved for either human or veterinary use.
Legal anabolic steroids
The only way to use steroids legally is to have a prescription for them.
Preventing Anabolic Steroid Misuse
Research on high school athletes shows they're less likely to misuse anabolic steroids if their friends and family disapprove. Peer pressure has a strong effect.
But simply educating students about the dangers of anabolic steroid misuse doesn't have the same preventive results. Studies show it's more effective to talk about the whole picture of anabolic steroids: the risks and the benefits. Often, this helps them believe the negative aspects are true (and that they should avoid them).
Other research shows that focusing on the prevention of high-risk behavior in general can be a catchall to help ward off anabolic steroid use.
Doctors prescribe anabolic steroids to help with skeletal muscle and the development of male sexual characteristics. Around 3 to 4 million people in the U.S., however, use anabolic steroids without a prescription for nonmedical purposes, including as appearance- and performance-enhancing drugs (APEDs). If you take anabolic steroids outside of a doctor's care, you may have serious side effects that can have a negative impact on your health. Talk to your doctor about possible treatment plans if you're worried about misusing steroids.
Anabolic Steroids FAQs
- What are anabolic steroids mainly used for? Around 3 to 4 million people in the U.S. use anabolic steroids without a prescription for nonmedical purposes. They're the most common appearance- and performance-enhancing drugs (APEDs).
- Are anabolic steroids ever safe? Doctors prescribe anabolic steroids to help with skeletal muscle and the development of male sexual characteristics for conditions like low testosterone (male hypogonadism), certain cancers, or acquired immunodeficiency syndrome (AIDS).
- Are anabolic steroids illegal? It's illegal to use anabolic steroids without a prescription.

Top doctors in ,
Find more top doctors on, related links.
- Men's Health Resources News
- Men's Health Resources Reference
- Men's Health Resources Slideshows
- Men's Health Resources Quizzes
- Men's Health Resources Videos
- Subscribe to Newsletters
- Enlarged Prostate
- Erectile Dysfunction
- Flat Abs Exercises
- Manage Your Migraine
- Prostate Cancer
- Sexual Conditions
- Strength Training
- More Related Topics
Or search by: Administrative Department | Academic Division
- Books & Merchandise
- Clayton Center for the Arts
- Corporate Sales & Events
- Financial Aid System
- Highland Echo
- Lamar Memorial Library
- Metz Dining
- Mountain Challenge
- Self Service
- Tuition Payment Plan
Newsroom / MC students study use of anabolic agents in livestock production
Colby Huffman ’25 and Ellie Jaynes ’26 work to trace anabolic agents from the farm to the kitchen
Aug. 13, 2024
EDITOR’S NOTE: This is the sixth in an ongoing series spotlighting summer research projects and internships by Maryville College STEM students , made possible through a $645,000 Fund to Improve Post-Secondary Education (FIPSE) grant, administered through the U.S. Department of Education. The grant was earmarked for the expansion of MC’s Scots Science Scholars program and build on STEM initiatives provided by the College to “increase access to hands-on experiences and industry exposure, with a focus on addressing emerging technologies and scientific innovation in natural sciences, computational science and engineering.”
The use of anabolic agents in agriculture, specifically by farmers who raise beef cattle, has been a topic of much debate for years, to the point that some European countries banned them decades ago.
It was in BIO-412, MC Biology Professor Dr. Drew Crain ’s Animal Physiology class, that Colby Huffman ’25 first became aware of them, and he found the subject so fascinating that he asked to work with Crain over the summer to research the amount of those agents — steroid hormones, in most cases — can be found in beef.
“This is important, because most producers use beef enhancement that makes their cows develop more muscle quicker, which is great for the farmer because it’s economical, but maybe not so much for the people eating the meat,” Huffman said. “That question is still up in the air, though, so hopefully this project will shed some light on the situation. I’m asking the question, ‘How much of these enhancers are staying in the meat?’ This is the first step to determining if there are potential impacts on the consumer.”
“When discussing the endocrine system, I mentioned in passing about how we do not know much about the impact of hormone supplements for cattle,” Crain added. “For instance, do any of the hormones end up in the meat, and does cooking the meat impact this? Colby’s family owns a beef cattle farm, and Colby approached me inquiring if he could pursue this question with me. When we heard that Ellie Jaynes (’26) , who has a very quantitative and mathematical mind, could help us, this project was born.
“I act as a faculty mentor to Colby and Ellie. As I explained to them, I am treating this like a graduate school research project. I meet with them regularly giving advice and direction, and then they do the research.”
The first experiment with anabolic agents to support livestock growth took place in 1948, according to the National Institute of Health , and over the next several decades, they’ve been explored for use in both agriculture and pharmaceuticals. The misuse of growth stimulants in livestock, however, led to a ban in the Netherlands in 1961. Other European countries followed suit, and that decision spurred Huffman’s interests in determining whether the presence of such steroid hormones might have an effect on people. Like their peers in the labs and fields this summer, Huffman and Jaynes can afford to spend their summer doing research thanks to compensation via the FIPSE grant.
“The process for doing so is to get a sample of beef for the grocery store, extract the steroids from the meat, and then measure them using a very sophisticated instrument called High-Performance Liquid Chromatography-tandem Mass Spectrometry (HPLC-MS/MS or LC-MS/MS),” he said.
Jaynes, a rising junior Mathematics major, then analyzes the resulting data to determine the specificity and the amount of the anabolic agents discovered in those grocery store samples. Collecting that data is the first step, Huffman said, and determining the effects of those agents on people rather than livestock is a much more complex scientific feat.
“Another exciting portion is that this is a pretty big project, but it has so much potential to keep evolving and taking on more and more to study,” Huffman said. “An example would be analyzing waterways because the cows also urinate some of these substances out, and most water treatment plants, to my knowledge, do not filter these substances, which could be another way they are consumed by people.
“Needless to say, I am extremely interested in this project and often get lost in planning the crossroads and different avenues. However, I would like to keep working on this through my senior thesis and explore some more avenues that this project and protocol can offer at Maryville.”
Up next: Jonathan Yost ’26 mines marigolds for repellent !
After Colby Huffman '25 gathers samples of meat sold to the public, Ellie Jaynes '26 works to analyze it.
Colby Huffman '25 (left) and Ellie Jaynes '26 work together in the lab.
Colby Huffman '25 analyzes data on anabolic agents used to promote livestock growth.

| Maryville College is a nationally-ranked institution of higher learning and one of America’s oldest colleges. For more than 200 years we’ve educated students to be giving citizens and gifted leaders, to study everything, so that they are prepared for anything — to address any problem, engage with any audience and launch successful careers right away. Located in , between the and the city of , Maryville College offers nearly 1,200 students from around the world both the beauty of a rural setting and the advantages of an urban center, as well as , seven pre-professional programs and from their first day on campus to their last. Today, our 10,000 alumni are living life strong of mind and brave of heart and are prepared, in the words of our , to “do good on the largest possible scale.” |
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Sports Sci Med
- v.5(2); 2006 Jun
Medical Issues Associated with Anabolic Steroid Use: Are They Exaggerated?
For the past 50 years anabolic steroids have been at the forefront of the controversy surrounding performance enhancing drugs. For almost half of this time no attempt was made by sports governing bodies to control its use, and only recently have all of the major sports governing bodies in North America agreed to ban from competition and punish athletes who test positive for anabolic steroids. These punitive measures were developed with the primary concern for promotion of fair play and eliminating potential health risks associated with androgenic-anabolic steroids. Yet, controversy exists whether these testing programs deter anabolic steroid use. Although the scope of this paper does not focus on the effectiveness of testing, or the issue of fair play, it is of interest to understand why many athletes underestimate the health risks associated from these drugs. What creates further curiosity is the seemingly well-publicized health hazards that the medical community has depicted concerning anabolic steroidabuse. Is there something that the athletes know, or are they simply naïve regarding the dangers? The focus of this review is to provide a brief history of anabolic steroid use in North America, the prevalence of its use in both athletic and recreational populations and its efficacy. Primary discussion will focus on health issues associated with anabolic steroid use with an examination of the contrasting views held between the medical community and the athletes that are using these ergogenic drugs. Existing data suggest that in certain circumstances the medical risk associated with anabolic steroid use may have been somewhat exaggerated, possibly to dissuade use in athletes.
- For many years the scientific and medical communities depicted a lack of efficacy and serious adverse effects from anabolic steroid use.
- Clinical case studies continue to link anabolic steroid administration with myocardial infarct, suicide, and cancer, evidence to support a cause and effect relationship is lacking.
- It may be other contributing factors (i.e. genetic predisposition, diet, etc.) that play a substantial role and potentiate the harmful effects from anabolic steroids.
Introduction
Anabolic-androgenic steroids (herein referred to as only anabolic steroids) are the man-made derivatives of the male sex hormone testosterone. Physiologically, elevations in testosterone concentrations stimulate protein synthesis resulting in improvements in muscle size, body mass and strength (Bhasin et al., 1996 ; 2001 ). In addition, testosterone and its synthetic derivatives are responsible for the development and maturation of male secondary sexual characteristics (i.e. increase in body hair, masculine voice, development of male pattern baldness, libido, sperm production and aggressiveness).
Testosterone was isolated in the early 20 th century and its discovery led to studies demonstrating that this substance stimulated a strong positive nitrogen balance in castrated dogs and rats (Kochakian, 1950 ). Testosterone, because of its rapid degradation when given through either oral or parenteral administration, poses some limitations as an ergogenic aid. Although its potency is rapidly observed, the high frequency of administration needed becomes problematic. In addition, testosterone has a therapeutic index of 1 meaning there is similarity in the proportion between the anabolic and androgenic effects. As a result it becomes necessary to chemically modify testosterone to retard the degradation process and reduce some of the negative side effects. This allows for maintenance of effective blood concentrations for longer periods of time, may increase its interaction with the androgen receptor, and achieves the desired anabolic and androgenic changes.
Boje, 1939 was the first to suggest that exogenous testosterone administration may enhance athletic performance. By the late 1940’s and 1950’s testosterone compounds were experimented with by some west coast bodybuilders (Yesalis et al., 2000 ). The first dramatic reports of anabolic steroid use occurred following the 1954 world weightlifting championships (Yesalis et al., 2000 ). Use of these drugs spread quickly through the 1960’s and became popular among athletes in a variety of Olympic sports (Dubin, 1990 ). Wide spread use has also been reported in power lifters (Wagman et al., 1995 ), National Football League players (Yesalis et al., 2000 ), collegiate athletes (Yesalis, 1992 ), and recent claims of wide spread use in many sports including Major League Baseball players has made anabolic steroids the number one sports story of 2005 in some markets (Quinn, 2006 ). The ergogenic effects associated with anabolic steroids are presented in Table 1 .
Ergogenic effects associated with anabolic steroid use.
Athletes typically use anabolic steroids in a “stacking” regimen, in which they administer several different drugs simultaneously. The rationale for stacking is to increase the potency of each drug. That is, the potency of one anabolic agent may be enhanced when consumed simultaneously with another anabolic agent. They will use both oral and parenteral compounds. Most users will take anabolic steroids in a cyclic pattern, meaning the athletes will use the drugs for several weeks or months and alternate these cycles with periods of discontinued use. Often the athletes will administer the drugs in a pyramid (step-up) pattern in which dosages are steadily increased over several weeks. Towards the end of the cycle the athlete will ‘step-down’ to reduce the likelihood of negative side effects. At this point, some athletes will discontinue drug use or perhaps initiate another cycle of different drugs (i.e., drugs that may increase endogenous testosterone production to prevent the undesirable drop in testosterone concentrations that follows the removal of the pharmaceutical agents). A recent study has shown that the typical steroid regimen involved 3.1 agents, with a typical cycle ranging from 5 – 10 weeks (Perry et al., 2005 ). The dose that the athlete administers was reported to vary between 5 - 29 times greater than physiological replacement doses (Perry et al., 2005 ). These higher pharmacological dosages appear necessary to elicit the gains that these athletes desire. In a classic study on the dose-response curve of anabolic steroids, Forbes, 1985 demonstrated that the total dose of anabolic steroids have a logarithmic relationship to increases in lean body mass. These results exacerbate the athlete’s philosophy that if a low dose is effective, then more must be better.
Adverse effects associated with anabolic steroid use are listed in Table 2 . For years, the medical and scientific communities attempted to reduce anabolic steroid use by athletes by underscoring their efficacy and focusing on the unhealthy side effects (Biely, 1987 ; Darden, 1983 ; Fahey and Brown, 1973 ; Fowler et al., 1965 ; Golding et al., 1974 ). For the most part, this may have proved to be ineffective and caused athletes to lose trust in the physician’s knowledge of anabolic steroids thereby forcing them to seek advice from friends, internet sites or drug suppliers (Pope et al., 2004 ). However, recent literature has suggested that the medical issues associated with anabolic steroids may be somewhat overstated (Berning et al., 2004 ; Sturmi and Diorio, 1998 ; Street et al., 1996 ) considering that many of the side effects associated with anabolic steroid abuse are reversible upon cessation. It is important to note that there are differences in the side effects associated with anabolic steroid use (i.e.under medical supervision) versus abuse (i.e. consumption of many drugs at high doses).
Adverse effects associated with anabolic steroid use.
| | |
The clinical examination of anabolic steroid use is quite limited. Much of the problem in prospectively examining the effects of anabolic steroids on the athletic population is related to the unwillingness of institutional review boards to approve such studies in a non-clinical population. As a result, most of the investigations concerning medical issues associated with anabolic steroid administration have been performed on athletes self-administering the drugs. Anecdotally, it appears that a disproportionate magnitude of use and incidence of adverse effects are evident in bodybuilders (who are also known for consuming several other drugs that relieve some side effects but potentiate other risk factors as well, i.e. diuretics, thyroid hormones, insulin, anti-estrogens, etc.) compared to strength/power athletes. The mindset and motivation of these two types of athletes can be quite different. The strength/power athlete will typically use anabolic steroids to prepare themselves for a season of competition. They will generally cycle the drug to help them reach peak condition at a specific time of the training year. In contrast, bodybuilders use anabolic steroids to enhance muscle growth and definition. Their success is predicated on their aesthetic appearance. As a result many of these athletes may use anabolic steroids excessively for severalyears without cycling off or perhaps minimizing the length of “off cycles” depending on their competition schedule. Recent research has indicated that those athletes exhibit behavior that are consistent with substance dependence disorder (Perry et al., 2005 ). Although the medical issues associated with anabolic steroids may be quite different between these two types of athletes, the scientific literature generally does not differentiate between the two. The following sections will discuss adverse effects on specific physiological systems associated with anabolic-androgenic steroid use. It is important to note that many athletes consume multiple drugs in addition to anabolic steroids. Thus, the unhealthy side effects could be potentiated by the use of drugs such as human growth hormone or IGF-1.
Cardiovascular System
In both the medical and lay literature one of the principal adverse effects generally associated with anabolic steroid use is the increased risk for myocardial infarction. This is primarily based upon several case reports published over the past 20 years describing the occurrence of myocardial infarctions in young and middle-aged body builders or weight lifters attributed to anabolic steroid use and/or abuse (Bowman, 1989 ; Ferenchick and Adelman, 1992 ; Gunes et al., 2004 ; Kennedy and Lawrence, 1993 ; Luke et al., 1990 ; McNutt et al., 1988 ). However, direct evidence showing cause and effect between anabolic steroid administration and myocardial infarction is limited. Many of the case studies reported normal coronary arterial function in anabolic steroid users that experienced an infarct (Kennedy and Lawrence, 1993 ; Luke et al., 1990 ), while others have shown occluded arteries with thrombus formation (Ferenchick and Adelman, 1992 ; Gunes et al., 2004 ; McNutt et al., 1988 ). Still, some of these studies have reported abnormal lipoprotein concentrations with serum cholesterol levels nearly approaching 600 mg·dl -1 (McNutt et al., 1988 ). Interestingly, in most case studies the effects of diet or genetic predisposition for cardiovascular disease were not disseminated and could not be excluded as contributing factors.
Alterations in serum lipids, elevations in blood pressure and an increased risk of thrombosis are additional cardiovascular changes often associated with anabolic steroid use (Cohen et al., 1986 ; Costill et al., 1984 ; Dhar et al., 2005 ; Kuipers et al., 1991 ; LaRoche, 1990 ). The magnitude of these effects may differ depending upon the type, duration, and volume of anabolic steroids used. Interesting to note is that these effects appear to be reversible upon cessation of the drug (Dhar et al., 2005 , Parssinen and Seppala, 2002 ). In instances where the athlete remains on anabolic steroids for prolonged periods of time (e.g “abuse”), the risk for developing cardiovascular disease may increase. Sader and colleagues ( 2001 ) noted that despite low HDL levels in bodybuilders, anabolic steroid use did not appear to cause significant vascular dysfunction. Interestingly, athletes participating in power sports appear to have a higher incidence of cardiovascular dysfunction than other athletes, regardless of androgen use (Tikkanen et al., 1991 ; 1998 ). Thus, a strength/power athlete with underlying cardiovascular abnormalities that begins using anabolic steroids is at a much higher risk for cardiovascular disease. However, anabolic steroid-induced changes in lipid profiles may not, per se, lead to significant cardiovascular dysfunction.
The risk of sudden death from cardiovascular complications in the athlete consuming anabolic steroids can occur in the absence of atherosclerosis. Thrombus formation has been reported in several case studies of bodybuilders self-administering anabolic steroids (Ferenchick, 1991 ; Fineschi et al., 2001 ; McCarthy et al., 2000 ; Sahraian et al., 2004 ). Melchert and Welder, 1995 have suggested that the use of 17α-alkylated steroids (primarily from oral ingestion) likely present the highest risk for thrombus formation. They hypothesized that anabolic steroid consumption can elevate platelet aggregation, possibly through an increase in platelet production of thromboxane A 2 and/or decreasing platelet production of prostaglandin PgI 2, resulting in a hypercoagulable state.
Left ventricular function and anabolic steroid use/abuse has been examined. Climstein and colleagues ( 2003 ) demonstrated that highly strength-trained athletes, with no history of anabolic steroid use exhibited a higher incidence of wave form abnormalities relative to recreationally-trained or sedentary individuals. However, when these athletes self-administered anabolic steroids, a higher percentage of wave form abnormalities were exhibited. Further evidence suggestive of left ventricular dysfunction has been reported in rodent models. A study on rats has shown that 8 weeks of testosterone administration increased left ventricle stiffness and caused a reduction in stroke volume and cardiac performance (LeGros et al., 2000 ). It was hypothesized that the increased stiffness may have been related to formation of crosslinks between adjacent collagen molecules within the heart. Others have suggested that anabolic steroid use may suppress the increases normally shown in myocardial capillary density following prolonged endurance training (Tagarakis et al., 2000 ). However, there are a number of interpretational issues with this study. The changes reported were not statistically significant. In addition, the exercise stimulus employed (prolonged endurance training) is not the primary mode of exercise frequently used by anabolic steroid users. Resistance training, independent of anabolic steroid administration, has been shown to increase left ventricular wall and septal thickness due to the high magnitude of pressure overload (Fleck et al., 1993 ; Fleck, 2003 ; Hoffman, 2002 ). This is known as concentric hypertrophy and does not occur at the expense of left ventricular diameter. In general, cardiac hypertrophy (resulting from a pressure overload, i.e. hypertension) may not be accompanied by a proportional increase in capillary density (Tomanek, 1986 ). Therefore, the potential for a reduction in coronary vasculature density exists for the resistance- trained athlete. However, it does not appear to pose a significant cardiac risk for these athletes. Recent observations have shown a dose-dependent increase in left ventricular hypertrophy (LVH) in anabolic steroid users (Parssinen and Seppala, 2002 ). This may have the potential to exacerbate the reduction in coronary vasculature density. However, the authors have acknowledged that their results may have been potentiated by a concomitant use of human growth hormone by their subjects. Other studies have failed to show additive effects of anabolic steroid administration and LVH in resistance-trained athletes (Palatini et al., 1996 ; Dickerman et al., 1998 ).
Hepatic System
An elevated risk for liver tumors, damage, hepatocellular adenomas, and peliosis hepatitis are often associated with anabolic steroid use or abuse. This is likely due to the liver being the primary site of steroid clearance. In addition, hepatic cancers have been shown to generally occur with higher frequency in males compared to females (El-Serag, 2004 ). It is thought that high endogenous concentrations of testosterone and low estrogen concentrations increase the risk of hepatic carcinomas (Tanaka et al., 2000 ). However, this appears to be prevalent for men with pre-existing liver disease. In normal, healthy men the relationship between testosterone concentrations and liver cancer has not been firmly established. Additional reports of liver cancer and anabolic steroids have been reported in non- athletic populations being treated with testosterone for aplastic anemia (Nakao et al., 2000 ). In regards to liver cancer and disease in athletes consuming anabolic steroids, many concerns have been raised based primarily on several case studies that have documented liver disease in bodybuilders using anabolic steroids (Cabasso, 1994 ; Socas et al., 2005 ; Soe et al., 1992 ).
A few studies have recently questioned the risk to hepatic dysfunction from anabolic steroid use (Dickerman et al., 1999 ). A recent study examining the blood chemistry of bodybuilders self-administering anabolic steroids reported elevations in aspartate aminotransferase (AST), alanine aminotransferase (ALT) and creatine kinase (CK), but no change in the often-regarded more sensitive gamma- glutamyltranspeptidase (GGT) concentration (Dickerman et al., 1999 ). Thus, some experts have questioned these criteria tools because of the difficulty in dissociating the effects of muscle damage resulting from training from potential liver dysfunction. This has prompted some researchers to suggest that steroid-induced hepatotoxicity may be overstated. Another study involved a survey sent to physicians asking them to provide a diagnosis for a 28-year-old anabolic steroid using bodybuilder with abnormal serum chemistry profile (elevations in AST, ALT, CK, but with a normal GGT) (Pertusi et al., 2001 ). The majority of physicians (63%) indicated liver disease as the primary diagnosis as 56% of physicians failed to acknowledge the potential role of muscle damage or disease thereby increasing the likelihood of overemphasized anabolic steroid-induced hepatotoxicity diagnoses. Many case reports involving anabolic steroid administration and hepatic cancers examined individuals who were treated with oral steroids (17α-alkylated) for many years. No cysts or tumors have been reported in athletes using 17β-alkylated steroids. Thus, evidence appears to indicate that the risk for hepatic disease from anabolic steroid use may not be as high as the medical community had originally thought although a risk does exist especially with oral anabolic steroid use or abuse.
Bone and Connective Tissue
The issue of anabolic steroids and bone growth has been examined in both young and adult populations. In both populations, androgens have been successfully used as part of the treatment for growth delay (Albanese et al., 1994 ; Bagatell and Bremner, 1996 ; Doeker et al., 1998 ), and for osteoporosis in women (Geusens et al., 1986 ). Androgens are bi-phasic in that they stimulate endochondral bone formation and induce growth plate closure at the end of puberty. The actions of androgens on the growth plate are mediated to a large extent by aromatization to estrogens (Vanderschueren et al., 2004 ; Hoffman, 2002 ). Anabolic steroid use results in significant elevations in estrogens thought to impact premature closure of the growth plate. The acceleration of growth in adolescents treated with testosterone has raised concern for the premature closure of the epiphyseal plate (NIDA, 1996 ; Sturmi and Diorio, 1998 ). However, there does not appear to be any reports documenting the occurrence of premature stunted growth inadolescents taking anabolic steroids. Interesting, anabolic steroid administration in colts has been reported to delay epiphyseal plate closure (Koskinen and Katila, 1997 ). Although comparisons between humans and animals are difficult to make, suprapharmacological dosages that most athletes use may pose a greater risk than the doses studied to date. Thus, for the adolescent athlete using anabolic steroids the risk of premature epiphyseal plate closure may exist.
Anabolic steroids have been suggested to increase the risk of tendon tears in athletes (David et al., 1994 ; Stannard and Bucknell, 1993 ). Studies in mice have suggested that anabolic steroids may lead to degeneration of collagen (proportional to duration of steroid administration) and potentially lead to a decrease in tensile strength (Michna, 1986 ). In addition, a decrease in collagen synthesis has been reported from anabolic steroid administration in rats (Karpakka et al., 1992 ). The response in humans has been less clear. Mechanical failure has been suggested as a mechanism in anabolic steroid-using athletes. Skeletal muscle adaptations (i.e. hypertrophy and strength increases) take place rather rapidly in comparison to connective tissue. Therefore, tendon injuries in athletes are thought to occur from a rapid increase in training intensity and volume where connective tissue fails to withstand the overload. However, case reports of spontaneous tendon ruptures of weightlifters and athletes are limited.Although experimental data from animal models suggest that anabolic steroids may alter biomechanical properties of tendons, ultrastructural evidence supporting this claim is lacking. One study has shown that high doses of anabolic steroids decrease the degradation and increase the synthesis of type I collagen (Parssinen et al., 2000 ). Evans and colleagues ( 1998 ) performed an ultrastructural analysis on ruptured tendons from anabolic steroid users. They concluded that anabolic steroids did not induce any ultrastructural collagen changes that would increase the risk of tendon ruptures. Although the incidences of tendon rupture in anabolic steroid users should not be discounted, it is important to consider it in relation to the mechanical stress encountered from the rapid increases in muscular performance. Prospective research on anabolic steroid use and connective tissue injury is warranted.
Psychological and Behavioral
An issue that is often raised with anabolic steroid use is the psychological and behavioral effects. Increases in aggressiveness, arousal and irritability have been associated with anabolic steroid use. This has potentially beneficial and harmful implications. Elevations in arousal and self-esteem may be a positive side effect for the athlete. The increase in aggressiveness is a benefit that athletes participating in a contact sport may possess. However, increased aggressiveness may occur outside of the athletic arena thereby posing significant risks for anabolic steroid users and those they come in contact with. Anabolic steroids are associated with mood swings and increases in psychotic episodes. Studies have shown that nearly 60% of anabolic steroid users experience increases in irritability and aggressiveness (Pope and Katz, 1994 ; Silvester, 1995 ). A recent study by Pope and colleagues ( 2000 ) reported that significant elevations in aggressiveness and manic scores were observed following 12 weeks of testosterone cypionate injections in a controlled double-blind cross-over study. Interestingly, the results of this study were not uniform across the subjects. Most subjects showed little psychological effect and few developed prominent effects. A cause and effect relationship has yet to be identified in anabolic steroid users and it does appear that individuals who experience psychological or behavioral changes do recover when steroid use is discontinued (Fudula et al., 2003 ).
Additional Adverse Effects Associated with Anabolic Steroid Use
Other adverse events generally associated with anabolic steroid use include acne, male pattern baldness, gynecomastia, decreased sperm count, testicular atrophy, impotence, and transient infertility. Acne is one of the more common side effects associated with anabolic steroid administration. One study reported that 43% of users experienced acne as a consequence from androgen use (O’Sullivan et al., 2000 ). Few other investigations have been able to prospectively determine the occurrence of side effects associated with androgen administration. Increases in acne are thought to be related to a stimulation of sebaceous glands to produce more oil. The most common sites of acne development are on the face and back. Acne appears to disappear upon cessation of androgen administration.
Male pattern baldness does not appear to be a common adverse effect, but is often discussed as a potential side effect associated with androgen use. This is likely related to the role that androgens have in regulating hair growth (Lee et al., 2005 ). An abnormal expression of a specific cutaneous androgen receptor increases the likelihood of androgenic alopecia (Kaufman and Dawber, 1999 ; Lee et al., 2005 ). Thus, it is likely that androgenic alopecia observed as a result of exogenous androgen use is more prevalent in individuals that have a genetic predisposition to balding.
Gynecomastia is a common adverse effect associated with anabolic steroid use. Research has demonstrated a prevalence rate of 37% in anabolic steroid users (O’Sullivan et al., 2000 ). Gynecomastia isa benign enlargement of the male breast resulting from an altered estrogen-androgen balance, or increased breast sensitivity to a circulating estrogen level. Increases in estrogen production in men are seen primarily through the aromatization of circulating testosterone. Many anabolic steroid users will use anti-estrogens (selective estrogen receptor modulators) such as tamoxifen and clomiphene or anastrozole which is a nonsteroidal aromatase inhibitor to minimize side effects of estrogen and stimulate testosterone production. Once gynecomastia is diagnosed cosmetic surgery is often needed to correct the problem.
Changes in libido appear to be the most common adverse event (approximately 61% of users) reported in a small sample of anabolic steroid users (O’Sullivan et al., 2000 ). Although testosterone is often used in hypogonadal men to restore normal sexual function, increasing testosterone above the normal physiological range does not appear to increase sexual interest or frequency of sexual behavior in healthy men administered anabolic steroids in supraphysiological dosages (up to 500 mg·wk -1 ) for 14 weeks (Yates et al., 1999 ). Other studies confirm unchanged libido following 10 weeks of anabolic steroid administration in dosages ranging up to 200 mg·wk -1 (Schurmeyer, et al., 1984 ). However, reports do indicate that towards the end of an androgen cycle some men may experience loss of libido (O’Sullivan et al., 2000 ). It was thought that the decreased libido was related to the transient hypogonadism which typically occurs during exogenous androgen administration. Decreases in libido as a result of hypogonadism appear to be a function of high baseline levels of sexual functioning and desire (Schmidt et al., 2004 ). This may explain the conflicting reports seen in the literature. Regardless, changes in libido do appear to normalize once baseline endogenous testosterone concentrations return (Schmidt et al., 2004 ).
Another frequent adverse event relating to sexual function in males administering anabolic steroids is reversible azoospermia and oligospermia (Alen and Suominen, 1984 ; Schurmeyer et al., 1984 ). As exogenous androgen use increases, endogenous testosterone production is reduced. As a result, testicular size is reduced within three months of androgen administration (Alen and Suominen, 1984 ). In addition, sperm concentration and the number of spermatozoa in ejaculate may be reduced or eliminated by 7 weeks of administration (Schurmeyer et al., 1984 ). During this time risk for infertility is elevated. However, the changes seen in testicular volume, sperm count and concentration are reversible. Anabolic steroid-induced hypogonadism returns to baseline levels within 4 months following discontinuation of androgen use (Jarow and Lipshultz, 1990 ), and sperm counts and concentration return to normal during this time frame (Alen and Suominen, 1984 ; Schurmeyer et al., 1984 ).
Medical Issues Associated with Female Steroid Use
In female anabolic steroid users the medical issues are quite different than that shown in men. Deepening of the voice, enlargement of the clitoris, decreased breast size, altered menstruation, hirsutism and male pattern baldness are all clinical features common to hyperandrogenism in females (Derman, 1995 ). Androgen excess may occur as the result of polycystic ovary syndrome, congenital adrenal hyperplasia and possibly Cushing’s syndrome (Derman, 1995 ; Redmond, 1995 ). However, these clinical symptoms are seen in young, female athletes that are self-administering anabolic steroids. In contrast to men, many of these adverse events in the female anabolic steroid user may not be transient (Pavlatos et al., 2001 ).
Long Term Health Issues Associated with Anabolic Steroid Administration
The acute health issues associated with anabolic steroid use appear to be transient and more prevalent in individuals with genetic predisposition (e.g. hair loss, heart disease). It is the long-term effects that become a larger issue. However, limited data are available. In one study in mice, anabolic steroids were administered in relative dosages typically used by bodybuilders. However, the duration of the study was 1/5 the life span of the mouse which is relatively greater than that experienced by most athletes self-administering androgens. The results demonstrated a shortened life span of the mice with evidence of liver, kidney and heart pathology (Bronson and Matherne, 1997 ). In a study on Finnish power lifters, investigators examined 62 athletes who finished in the top 5 in various weight classes between the years 1977 and 1982 (Parssinen et al., 2000 ). These investigators reported that during a 12-year follow-up, the mortality rate for the power lifters was 12.1% compared to 3.1% in a control population. They concluded that their study depicted the detrimental long-term health effects from anabolic steroid use. Others have suggested that prolonged anabolic steroid use may increase the risk for premature death, but this may be more relevant in subjects with substance abuse or underlying psychiatric disease (Petersson et al., 2006 ).
The use of anabolic steroids in strength/power athletes has been reported for more than 50 years in North America. As discussed in the beginning of this review, during the 1970’s and 1980’s anecdotal reports on the rampant use of anabolic steroids in professional athletes were prevalent. However, little information is available concerning steroid-related diseases or associated deaths in these former strength/power athletes who are now well into middle age. Regardless, research should focus on these former athletes to ascertain possible long-term effects from androgen use.
Is There a Clinical Role of Androgenic Anabolic Steroids?
The efficacy of anabolic steroids in enhancing muscle strength and lean tissue accruement is no longer an issue for debate. While the issue of medical risks in individuals self-administering anabolic steroids is still being hotly debated, the medical community is no longer denying the potential clinical use of these androgens (Dobs, 1999 ). In recent years clinical treatment with anabolic steroids has increased lean tissue and improved daily functional performance in AIDS patients (Strawford et al., 1999 ) patients receiving dialysis (Johansen et al., 1999 ), patients with chronic obstructive pulmonary disease (Ferreira et al., 1998 ), and patients recovering from a myocardial infarction (Nahrendorf et al., 2003 ). In addition, research has demonstrated a positive effect on healing from muscle contusion injuries (Beiner et al., 1999 ). Although the medical community has generally taken a conservative approach to promoting anabolic steroids as part of a treatment plan in combating diseases involving muscle wasting, the body of knowledge that has developed indicates the potential positive effects of androgen therapy for certain diseased populations.
Conclusions
For many years the scientific and medical communities depicted a lack of efficacy and serious adverse effects from anabolic steroid use. However, competitive athletes continued to experiment with, use, and abuse anabolic steroids on a regular basis to enhance athletic performance despite the potential harmful side effects. The empirical evidence that the athletes viewed may have led to the development of distrust between the athletic and medical communities. Science has been lagging several years behind the experimental practices of athletes. In fact, most athletes consume anabolic steroids on a trial and error approach based on information gained from other athletes, coaches, websites, or gym “gurus.” Science has lacked in its approach to study anabolic steroids because only few studies have examined long-term cyclical patterns, high doses, and the effects of stacking different brands of steroids. These practices are common to the athletic community and not for the medicinal purposes of anabolic steroid therapy. In addition, some athletes (especially bodybuilders) have experimented with drugs unbeknown to the medical community, i.e. insulin, thyroid hormones, and site-specific enhancers such as Synthol and Esiclene to name a few.
When examining the potential medical issues associated with anabolic steroid use, evidence indicates that most known side effects are transient. More so, few studies have been able to directly link anabolic steroids to many of the serious adverse effects listed. Although clinical case studies continue to link anabolic steroid administration with myocardial infarct, suicide, and cancer, the evidence to support a cause and effect relationship is lacking and it may be other contributing factors (i.e. genetic predisposition, diet, etc.) play a substantial role and potentiate the harmful effects from anabolic steroids. Consistent physician monitoring is critical to the athlete who consumes anabolic steroids. However, many athletes may not undergo extensive medical exams prior to androgen administration and few physicians may be willing to provide such monitoring.
The purpose of this review was not to support or condone anabolic steroid use. Rather, the aim was to discuss pertinent medical issues and provide another perspective in light of the fact that many anabolic steroids users do not appear to prioritize the health/safety hazards or potential adverse medical events. In order to maintain credibility with the athlete, it is important to provide accurate information to the athlete in regards to these performance enhancing drugs, and provide education about alternative means and potential risks. Finally, anabolic steroids have been used legitimately for several clinical purposes such as muscle wasting or hypogonadal related diseases.
Biographies
Jay R. HOFFMAN
The College of New Jersey.
Research interests
Sport supplementation, resistance training, eExercise endocrinology.
E-mail: ude.jnct@jnamffoh
Nicholas A. RATAMESS
Sport supplementation, resistance training, exercise endocrinolgy.
E-mail: ude.jnct@ssematar
- Albanesey A., Kewley G.D., Long A., Pearl K.N., Robins D.G., Stanhope R. (1994) Oral treatment for constitutional delay of growth and puberty in boys: a randomised trial of an anabolic steroid or testosterone undecanoate . Archives of Disease in Childhood 71 , 315-317 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alen M., Suominen J. (1984) Effect of androgenic and anabolic steroids on spermatogenesis in power athletes . International Journal of Sports Medicine 5 , 189-192 [ Google Scholar ]
- Bagatell C.J., Bremner W.J. (1996) Androgens in men – uses and abuses . New England Journal of Medicine 334 , 707-714 [ PubMed ] [ Google Scholar ]
- Beiner J.M., Jokl P., Cholewicki J., Panjabi M.M. (1999) The effect of anabolic steroids and corticosteroids on healing of muscle contusion injury . American Journal of Sports Medicine . 27 , 2-9 [ PubMed ] [ Google Scholar ]
- Berning J.M., Adams K.J., Stamford B.A. (2004) Anabolic steroid usage in athletics: Facts, fiction, and public relations . Journal of Strength and Conditioning Research 18 , 908-917 [ PubMed ] [ Google Scholar ]
- Bhasin S., Storer T.W., Berman N., Callegari C., Clevenger B., Phillips J., Bunnell T.J., Tricker R., Shirazi A., Casaburi R. (1996) The effects of supraphysiologic doses of testosterone on muscle size and strength in men . New England Journal of Medicine 335 , 1-7 [ PubMed ] [ Google Scholar ]
- Bhasin S., Woodhouse L., Storer T.W. (2001) Proof of the effect of testosterone on skeletal muscle . Journal of Endocrinology 170 , 27-38 [ PubMed ] [ Google Scholar ]
- Biely J.R. (1987) Use of anabolic steroids by athletes. Do the risks outweigh the benefits? Postgraduate Medicine 82 , 71-74 [ PubMed ] [ Google Scholar ]
- Bowman S.J. (1989) Anabolic steroids and infarction . British Medical Journal 299 , 632 [ Google Scholar ]
- Boje O. (1939) Doping . Bulletin of the Health Organization of the League of Nations 8 , 439-469 [ Google Scholar ]
- Bronson F.H., Matherne C.M. (1997) Exposure to anabolic-androgenic steroids shortens life span of male mice . Medicine and Science in Sports and Exercise 29 , 615-619 [ PubMed ] [ Google Scholar ]
- Cabasso A. (1994) Peliosis hepatis in a young adult bodybuilder . Medicine and Science in Sports and Exercise 26 , 2-4 [ PubMed ] [ Google Scholar ]
- Climstein M., O’Shea P., Adams K.J., DiBeliso M. (2003) The effects of anabolic-androgenic steroids upon resting and peak exercise left ventricular heart wall motion kinetics in male strength and power athletes . Journal of Science and Medicine and Sport . 6 , 387-397 [ PubMed ] [ Google Scholar ]
- Cohen J.C., Faber W.M., Spinnler Benade A.J., Noakes T.D. (1986) Altered serum lipoprotein profiles in male and female power lifters ingesting anabolic steroids . Physician and Sportsmedicine 14 , 131-136 [ PubMed ] [ Google Scholar ]
- Costill D.L., Pearson D.R., Fink W.J. (1984) Anabolic steroid use among athletes: Changes in HDL-C levels . Physician and Sportsmedicine 12 , 113-117 [ Google Scholar ]
- Darden E. (1983) The facts about anabolic steroids . Athletic Journal March, 100-101 [ Google Scholar ]
- David H.G., Green J.T., Green A.J., Wilson C.A. (1994) Simultaneous bilateral quadriceps rupture: a complication of anabolic steroid use . Journal of Bone and Joint Surgery, British Volume 77 , 159-160 [ PubMed ] [ Google Scholar ]
- Derman R.J. (1995) Effects of sex steroids on women’s health: Implications for practitioners . American Journal of Medicine . 98 ( Suppl ), 137S-143S [ PubMed ] [ Google Scholar ]
- Dhar R., Stout C.W., Link M.S., Homoud M.K., Weinstock J., Estes N.A., III. (2005) Cardiovascular toxicities of performance-enhancing substances in sports . Mayo Clinic Proceedings 80 , 1308-1315 [ PubMed ] [ Google Scholar ]
- Dickerman R.D., Schaller F., McConathy W.J. (1998) Left ventricular wall thickening does occur in elite power athletes with or without anabolic steroid use . Cardiology 90 , 145-148 [ PubMed ] [ Google Scholar ]
- Dickerman R.D., Pertusi R.M., Zachariah N.Y., Dufour D.R., McConathy W.J. (1999) Anabolic steroid-induced hepatotoxicity: Is it overstated? Clinical Journal of Sport Medicine 9 , 34-39 [ PubMed ] [ Google Scholar ]
- Dobs A.S. (1999) Is there a role for androgenic anabolic steroids in medical practice . Journal of American Medical Association 281 , 1326-1327 [ PubMed ] [ Google Scholar ]
- Doeker B., Müller-Michaels J., Andler W. (1998) Induction of early puberty in a boy after treatment with oxandrolone? Hormone Research 50 , 46-48 [ PubMed ] [ Google Scholar ]
- Dubin C. (1990) Commission of inquiry into the use of drugs and banned practices intended to increase athletic performance . (Catalogue No. CP32-56/1990E, ISBN 0-660-13610-4) . Ottawa, ON: Canadian Government Publishing Center [ Google Scholar ]
- El-Serag H.B. (2004) Hepatocellular carcinoma: recent trends in the United States . Gastroenterology 127 , S27-S34 [ PubMed ] [ Google Scholar ]
- Evans N.A., Bowrey D.J., Newman G.R. (1998) Ultrastructural analysis of ruptured tendon from anabolic steroid users . Injury 29 , 769-773 [ PubMed ] [ Google Scholar ]
- Fahey T.D., Brown C.H. (1973) The effects of an anabolic steroid on the strength, body composition, and endurance of college males when accompanied by a weight training program . Medicine and Science in Sports 5 , 272-276 [ PubMed ] [ Google Scholar ]
- Ferenchick G.S. (1991) Anabolic/androgenic steroid abuse and thrombosis: Is there a connection? Medical Hypothesis 35 , 27-31 [ PubMed ] [ Google Scholar ]
- Ferenchick G.S., Adelman S. (1992) Myocardial infarction associated with anabolic steroid use in a previously healthy 37-year old weight lifter . American Heart Journal 124 , 507-508 [ PubMed ] [ Google Scholar ]
- Ferreira I.M., Verreschi I.T., Nery L.E., Goldstein R.S., Zamel N., Brooks D., Jardim J.R. (1998) The influence of 6 months of oral anabolic steroids on body mass and respiratory muscle sin undernourished COPD patients . Chest 114 , 19-28 [ PubMed ] [ Google Scholar ]
- Fineschi V., Baroldi G., Monciotti F., Paglicci Reattelli L., Turillazzi E. (2001) Anabolic steroid abuse and cardiac sudden death: A pathologic study . Archives of Pathology and Laboratory Medicine 125 , 253-255 [ PubMed ] [ Google Scholar ]
- Fleck S.J., Pattany P.M., Stone M.H., Kraemer W.J., Thrush J., Wong K. (1993) Magnetic resonance imaging determination of left ventricular mass: junior Olympic weightlifters . Medicine and Science in Sports and Exercise 25 , 522-527 [ PubMed ] [ Google Scholar ]
- Fleck S.J. (2003) Cardiovascular responses to strength training . In: Strength and Power in Sport . : Komi P.V.2nd edition Malden, MA: Blackwell Science; 387-406 [ Google Scholar ]
- Forbes G.B. (1985) The effect of anabolic steroids on lean body mass: The dose response curve . Metabolism 34 , 571-573 [ PubMed ] [ Google Scholar ]
- Fowler W.M., Jr., Gardner G.W., Egstrom G.H. (1965) Effect of an anabolic steroid on physical performance in young men . Journal of Applied Physiology 20 , 1038-1040 [ PubMed ] [ Google Scholar ]
- Fudula P.J., Weinrieb R.M., Calarco J.S., Kampman K.M., Boardman C. (2003) An evaluation of anabolic-androgenic steroid abusers over a period of 1 year: seven case studies . Annals of Clinical Psychiatry 15 , 121-130 [ PubMed ] [ Google Scholar ]
- Geusens P., Dequeker J., Verstraeten A., Nils J., Van Holsbeeck M. (1986) Bone mineral content, cortical thickness and fracture rate in osteoporotic women after withdrawal of treatment with nandrolone decanoate, 1-alpha hydroxyvitamin D3, or intermittent calcium infusions . Maturitas 8 , 281-289 [ PubMed ] [ Google Scholar ]
- Golding L.A., Freydinger J.E., Fishel S.S. (1974) The effect of an androgenic-anabolic steroid and a protein supplement on size, strength, weight and body composition in athletes . Physician and Sportsmedicine 2 , 39-45 [ Google Scholar ]
- Gunes Y., Erbas C, Okuyan E, Babalık E., Gurmen T. (2004) Myocardial infarction with intracoronary thrombus induced by anabolic steroids . Anadolu Kardiyoloji Dergisi 4 , 357-358 [ PubMed ] [ Google Scholar ]
- Hoffman J.R. (2002) Physiological aspects of sport training and performance . Champaign, IL: Human Kinetics; 15-26 [ Google Scholar ]
- Jarow J.P., Lipshultz L.I. (1990) Anabolic steroid-induced hypogonadotropic hypogonadism . American Journal of Sports Medicine 18 , 429-431 [ PubMed ] [ Google Scholar ]
- Johansen K.L., Mulligan K., Schambelan M. (1999) Anabolic effects of nandrolone decanoate in patients receiving dialysis . Journal of American Medical Association 281 , 1275-1281 [ PubMed ] [ Google Scholar ]
- Karpakka J.A., Pesola M.K., Takala T.E. (1992) The effects of anabolic steroids on collagen synthesis in rat skeletal muscle and tendon. A preliminary report . American Journal of Sports Medicine 20 , 262-266 [ PubMed ] [ Google Scholar ]
- Kaufman K.D., Dawber R.P. (1999) Finasteride, a type 2 5alpha-reductase inhibitor, in the treatment of men with androgenic alopecia . Expert Opinion of Investigational Drugs 8 , 403-415 [ PubMed ] [ Google Scholar ]
- Kennedy M.C., Lawrence C. (1993) Anabolic steroid abuse and cardiac death . Medical Journal of Australia 158 , 346-348 [ PubMed ] [ Google Scholar ]
- Kochakian C.D. (1950) Comparison of protein anabolic property of various androgens in the castrated rat . American Journal of Physiology 160 , 53-61 [ PubMed ] [ Google Scholar ]
- Koskinen E., Katila T. (1997) Effect of 19-norandrostenololylaurate on serum testosterone concentration, libido, and closure of distal radial growth plate in colts . Acta Veterinaria Scandinavica 38 , 59-67 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuipers H., Wijnen J.A., Hartgens F., Willems S.M. (1991) Influence of anabolic steroids on body composition, blood pressure, lipid profile, and liver function in amateur bodybuilders . International Journal of Sports Medicine 12 , 413-418 [ PubMed ] [ Google Scholar ]
- LaRoche G.P. (1990) Steroid anabolic drugs and arterial complications in an athlete – a case history . Angiology 41 , 964-969 [ PubMed ] [ Google Scholar ]
- Lee P., Zhu C.C., Sadick N.S., Diwan A.H., Zhang P.S., Liu J.S., Prieto V.G. (2005) Expression of androgen receptor coactivator ARA70/ELE1 in androgenic alopecia . Journal of Cutaneous Pathology 32 , 567-571 [ PubMed ] [ Google Scholar ]
- LeGros T., McConnell D., Murry T., Edavettal M., Racey-Burns L.A., Shepherd R.E., Burns A.H. (2000) The effects of 17 α-methyltestosterone on myocardial function in vitro . Medicine and Science in Sports and Exercise 32 , 897-903 [ PubMed ] [ Google Scholar ]
- Luke J.L., Farb A., Virmani R., Barry Sample R.H. (1990) Sudden cardiac death during exercise in a weight lifter using anabolic androgenic steroids: pathological and toxicological findings . Journal of Forensic Science 35 , 1441-1447 [ PubMed ] [ Google Scholar ]
- McCarthy K., Tang A.T., Dalrymple-Hay M.J., Haw M.P. (2000) Ventricular thrombosis and systemic embolism in bodybuilders: etiology and management . Annals of Thoracic Surgery 70 , 658-660 [ PubMed ] [ Google Scholar ]
- McNutt R.A., Ferenchick G.S., Kirlin P.C., Hamlin N.J. (1988) Acute myocardial infarction in a 22-year-old world class weight lifter using anabolic steroids . American Journal of Cardiology 62 , 164. [ PubMed ] [ Google Scholar ]
- Melchert R.B., Welder A.A. (1995) Cardiovascular effects of androgenic-anabolic steroids . Medicine and Science in Sports and Exercise 27 , 1252-1262 [ PubMed ] [ Google Scholar ]
- Michna H. (1986) Organisation of collagen fibrils in tendon: changes induced by an anabolic steroid. I. Functional and ultrastructural studies . Virchows Archive B (Cell Pathology Including Molecular Pathology) 52 , 75-86 [ PubMed ] [ Google Scholar ]
- Nahrendorf M., Frantz S., Hu K., von zur Muhlen C., Tomaszewski M., Scheuermann H, Kaiser R., Jazbutyte V., Beer S., Bauer W., Neubauer S., Ertl G., Allolio B., Callies F. (2003) Effect of testosterone on post-myocardial infarction remodeling and function . Cardiovascular Research 57 , 370-378 [ PubMed ] [ Google Scholar ]
- Nakao A., Sakagami K., Nakata Y., Komazawa K., Amimoto T., Nakashima K., Isozaki H., Takakura N., Tanaka N. (2000) Multiple hepatic adenomas caused by long-term administration of androgenic steroids for aplastic anemia in association with familial adenomatous polyposis . Journal of Gastroenterology 35 , 557-562 [ PubMed ] [ Google Scholar ]
- National Institute on Drug Abuse (1996) Anabolic steroids: A threat to mind and body . U.S. Department of Health and Human Services; NIH publication No. 96-3721 [ Google Scholar ]
- O’Sullivan A.J., Kennedy M.C., Casey J.H., Day R.O., Corrigan B., Wodak A.D. (2000) Anabolic-androgenic steroids: Medical assessment of present, past and potential users . Medical Journal of Australia 173 , 323-327 [ PubMed ] [ Google Scholar ]
- Palatini P., Giada F., Garavelli G., Sinisi F., Mario L., Michielleto M., Baldo-Enzi G. (1996) Cardiovascular effects of anabolic steroids in weight-trained subjects . Journal of Clinical Pharmacology 36 , 1132-1140 [ PubMed ] [ Google Scholar ]
- Parssinen M., Karila T., Kovanen V., Seppala T. (2000) The effect of supraphysiological doses of anabolic androgenic steroids on collagen metabolism . International Journal of Sports Medicine 21 , 406-411 [ PubMed ] [ Google Scholar ]
- Parssinen M., Seppala T. (2002) Steroid use and long-term health risks in former athletes . Sports Medicine 32 , 83-94 [ PubMed ] [ Google Scholar ]
- Parssinen M., Kujala U., Vartiainen E., Sarna S., Seppala T. (2000) Increased premature mortality of competitive powerlifters suspected to have used anabolic agents . International Journal of Sports Medicine 21 , 225-227 [ PubMed ] [ Google Scholar ]
- Pavlatos A.M., Fultz O., Monberg M.J., Vootkur A. (2001) Review of oxymtholone: A 17α-alkylated anabolic-androgenic steroid . Clinical Therapy 23 , 789-801 [ PubMed ] [ Google Scholar ]
- Perry P.J., Lund B.C., Deninger M.J., Kutscher E.C., Schneider J. (2005) Anabolic steroid use in weightlifters and bodybuilders. An internet survey of drug utilization . Clinical Journal of Sports Medicine 15 , 326-330 [ PubMed ] [ Google Scholar ]
- Pertusi R., Dickerman R.D., McConathy W.J. (2001) Evaluation of aminotransferases elevations in a bodybuilder using anabolic steroids: hepatitis or rhabdomyolysis . Journal of American Osteopathic Association 101 , 391-394 [ PubMed ] [ Google Scholar ]
- Petersson A., Garle M., Granath F., Thiblin I. (2006) Morbidity and mortality in patients testing positively for the presence of anabolic androgenic steroids in connection with receiving medical care. A controlled retrospective cohort study . Drug and Alcohol Dependence 81 , 215-220 [ PubMed ] [ Google Scholar ]
- Pope H.G., Katz D.L. (1994) Psychiatric and medical effects of anabolic-androgenic steroid use. A controlled study of 160 athletes . Archives of General Psychiatry 51 , 375-382 [ PubMed ] [ Google Scholar ]
- Pope H.G., Kouri E.M., Hudson J.I. (2000) Effects of supraphysiologic doses of testosterone on mood and aggression in normal men . Archives of General Psychiatry 57 , 133-140 [ PubMed ] [ Google Scholar ]
- Pope H.G., Kanayama G., Ionescu-Pioggia M., Hudson J.I. (2004) Anabolic steroid users’ attitudes towards physicians . Addiction 99 , 1189-1194 [ PubMed ] [ Google Scholar ]
- Quinn T.J. (2006) Year of the Juice. Steroid scandal top story of 2005 . New York Daily News . January 3 [ Google Scholar ]
- Redmond G.P. (1995) Androgenic disorders of women: Diagnostic and therapeutic decision making . American Journal of Medicine 98z ( Suppl ), 120S-129S [ PubMed ] [ Google Scholar ]
- Sader M.A., Griffiths K.A., McCredie R.J., Handelsman D.J., Celermajer D.S. (2001) Androgenic anabolic steroids and arterial structure and function in male bodybuilders . Journal of American College of Cardiology 37 , 224-230 [ PubMed ] [ Google Scholar ]
- Sahraian M.A., Mottamedi M., Azimi A.R., Moghimi B. (2004) Androgen-induced cerebral venous sinus thrombosis in a young body builder: case report . BMC Neurology 4 , 22. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schmidt P.J., Berlin K.L., Danacceau M.A., Neeren A., Haq N.A., Roca C.A., Rubinow D.R. (2004) The effects of pharmacologically induced hypogonadism on mood in healthy men . Archives of General Psychiatry 61 , 997-1004 [ PubMed ] [ Google Scholar ]
- Schurmeyer T., Knuth U.A., Belkien L., Nieschlag E. (1984) Reversible azoospermia induced by the anabolic steroid 10-nortestosterone . Lancet 25 , 417-420 [ PubMed ] [ Google Scholar ]
- Silvester L.J. (1995) Self-perceptions of the acute and long-range effects of anabolic-androgenic steroids . Journal of Strength and Conditioning Research 9 , 95-98 [ Google Scholar ]
- Socas L., Zumbardo M., Perez-Luzardo O., Ramos A., Perez C., Hernandez J.R., Boada L.D. (2005) Hepatocellular adenomas associated with anabolic androgenic steroid abuse in bodybuilders: a report of two cases and a review of the literature . British Journal of Sports Medicine 39 , e27. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soe K.L., Soe M., Gluud C. (1992) Liver pathology associated with the use of anabolic-androgenic steroids . Liver 12 , 73-79 [ PubMed ] [ Google Scholar ]
- Stannard J.P., Bucknell A.L. (1993) Rupture of the triceps tendon associated with steroid injections . American Journal of Sports Medicine 21 , 482-485 [ PubMed ] [ Google Scholar ]
- Strawford A., Barbieri T, Van Loan M., Parks E., Catlin D, Barton N., Neese R., Christiansen M., King J., Hellerstein M.K. (1999) Resistance exercise and supraphysiologic androgen therapy in eugonadal men with HIV-related weight loss . Journal of American Medical Association 281 , 1282-1290 [ PubMed ] [ Google Scholar ]
- Street C., Antonio J., Cudlipp D. (1996) Androgen use by athletes: a re-evaluation of the health risks . Canadian Journal of Applied Physiology 21 , 421-440 [ PubMed ] [ Google Scholar ]
- Sturmi J.E., Diorio D.J. (1998) Anabolic agents . Clinics in Sports Medicine 17 , 261-282 [ PubMed ] [ Google Scholar ]
- Sullivan M.L., Martinez C.M., Gennis P., Gallagher E.J. (1998) The cardiac toxicity of anabolic steroids . Progress in Cardiovascular Diseases . 41 , 1-15 [ PubMed ] [ Google Scholar ]
- Tagarakis C.V.M., Bloch W., Hartmann G., Hollmann W., Addicks K. (2000) Testosterone-propionate impairs the response of the cardiac capillary bed to exercise . Medicine and Science in Sports and Exercise 32 , 946-953 [ PubMed ] [ Google Scholar ]
- Tanaka K., Sakai H., Hashizume M., Hirohata T. (2000) Serum testosterone; estradiol ratio and the development of hepatocellular carcinoma among male cirrhotic patients . Cancer Research 60 , 5106-5110 [ PubMed ] [ Google Scholar ]
- Tikkanen H.O., Hamalainen E., Sarna S., Adlercreutz H., Harkonen M. (1998) Associations between skeletal muscle properties, physical fitness, physical activity and coronary heart disease risk factors in men . Atherosclerosis 137 , 377-389 [ PubMed ] [ Google Scholar ]
- Tikkanen H.O., Harkonen M., Naveri H. (1991) Relationship of skeletal muscle fiber type to serum high density lipoprotein cholesterol and apolipoprotein A-I levels . Atherosclerosis 90 , 48-57 [ PubMed ] [ Google Scholar ]
- Tomanek R.J. (1986) Capillary and pre-capillary coronary vascular growth during left ventricular hypertrophy . Canadian Journal of Cardiology 2 , 114-119 [ PubMed ] [ Google Scholar ]
- Vanderschueren D., Vandenput L., Boonen S., Lindberg M.K., Bouillon R., Ohlsson C. (2004) Androgens and bone . Endocrine Reviews . 25 : 389-425 [ PubMed ] [ Google Scholar ]
- Wagman D.F., Curry L.A., Cook D.L. (1995) An investigation into anabolic androgenic steroid use by elite U.S. powerlifters . Journal of Strength and Conditioning Research 9 , 149-153 [ Google Scholar ]
- Yates W.R., Perry P.J., MacIndoe J., Holman T., Ellingrod V. (1999) Psychosexual effects of three doses of testosterone cycling in normal men . Biology Psychiatry 45 , 254-260 [ PubMed ] [ Google Scholar ]
- Yesalis C.E. (1992) Epidemiology and patterns of anabolic-androgenic steroid use . Psychiatric Annals 22 , 7-18 [ Google Scholar ]
- Yesalis C.E., Courson S.P., Wright J. (2000) History of anabolic steroid use in sport and exercise . In: Anabolic steroids in sport and exercise . : Yesalis C.E.2nd editionChampaign, IL: Human Kinetics; 51-71 [ Google Scholar ]

IMAGES
COMMENTS
Research with human cells demonstrates that anabolic steroids also interact with certain types of GABA A receptors, which could mediate the increased anxiety reported by steroid users. 105,106 In addition, animal studies show that anabolic steroids increase serotonin levels in brain regions involved in mood 107 and dopamine levels in reward ...
Anabolic-androgenic steroids (AAS) are a class of hormones that are widely abused for their muscle-building and strength-increasing properties in high, nontherapeutic, dosages. This review provides an up-to-date and comprehensive overview on how these hormones work and what side effects they might elicit. ... Research in individuals with ...
Abstract. Anabolic-androgenic steroids (AASs) are a large group of molecules including endogenously produced androgens, such as testosterone, as well as synthetically manufactured derivatives. AAS use is widespread due to their ability to improve muscle growth for aesthetic purposes and athletes' performance, minimizing androgenic effects.
The Anabolic Steroid Control Act is revised to include 26 new compounds including prohormones: 2005: T:E ratio lowered to 4:1 by WADA for a positive doping test ... Interest in AAS persists as research identifies new information regarding the performance and health aspects of the drugs and through stories of purported use in the sports world ...
Anabolic steroids' chemical structures and activity have undergone modifications to amplify anabolic effects and minimize androgenic ones. 45 While some steroids have been withdrawn in several countries, they remain available in others for medical use, such as methandienone, methyltestosterone, oxandrolone, and stanozolol. In the United ...
The effects of an anabolic steroid on the strength, body composition, and endurance of college males when accompanied by a weight training program. Med Sci Sports 1973;5:272-276 Crossref
To fully appreciate just how effective steroids are at building muscle, one should turn to the research of Shalendar Bhasin, the world's foremost authority on the effects of exogenous testosterone (steroids) on male body composition. ... Empirical discourse on steroids has justifiably focused on the health consequences of anabolic steroids, a ...
Previous research has uncovered medical and psychological effects of anabolic-androgenic steroid (AAS) use, but the specific relationship between AAS use and risk-taking behaviors as well as ...
In future studies, several suggestions can be considered to enhance the straightness of research on anabolic steroid use among resistance training practitioners. First, adopting a longitudinal approach would provide valuable insights into the changes in steroid use over time post-pandemic, identifying shifts in prevalence, patterns, and ...
The use of anabolic androgenic steroids (AAS) and associated image and performance enhancing drugs (IPEDs) is now a global phenomenon. There is a need to develop evidence to support the development of interventions to prevent the commencement of use, to minimise the potential harms or to support those in their cessation of use. While the United Kingdom (UK) is no exception to this issue, its ...
A growing body of evidence suggests that anabolic androgenic steroids (AAS) are used globally by a diverse population with varying motivations. Evidence has increased greatly in recent years to support understanding of this form of substance use and the associated health harms, but there remains little evidence regarding interventions to support cessation and treat the consequences of use.
Anabolic steroids (AS) are also used by non-athletes in order to improve their physical abilities and ... nandrolone (Deca-Durabolin), and methandrostenolone (Dianabol). Multiple research articles have shown that these drugs have a wide range of side effects, resulting in reproductive and metabolic disorders, psychological disturbances ...
Anabolic steroids have been used in this way since the 1950s, according to research. But since then they've been banned by several athletic organizations as performance-enhancing drugs (more on ...
Anabolic steroid users also report that their muscles recover faster from intense strain and muscle injury. Research in animals has not conclusively supported this belief, with some showing that anabolic steroids can enhance recovery from certain types of muscle damage, but others finding no benefit in taking anabolic steroids to
Common side effects with anabolic steroids may include: severe acne, oily skin and hair. hair loss. l iver disease, such as liver tumors and cysts. kidney disease. heart disease, such as heart attack and stroke. altered mood, irritability, increased aggression, depression or suicidal tendencies. alterations in cholesterol and other blood lipids.
The term "anabolic steroids" refers to testosterone derivatives that are used either clinically or by athletes for their anabolic properties. However, scientists have questioned the anabolic effects of testosterone and its derivatives in normal men for decades. Most scientists concluded that anaboli ….
Anabolic Steroids CYNTHIA M. KUHN Department of Pharmacology and Cancer Biology, Duke University Medical Center, Durham, North Carolina 27710 ... unlikely that regimens used by athletes will prove anabolic but the research has not been conducted. No published studies report effective anabolic activity of suprapharmacologic doses of androstenedione.
Introduction. Anabolic-androgenic steroids (AAS) are synthetic androgens with several potential effects. In clinical settings, AAS can be used to treat conditions such as male hypogonadism, pathological loss of muscle mass and anaemia, 1 with findings suggesting their efficacy in the treatment of depression 2 and conditions associated with type 2 diabetes. 3 Beneficial effects of AAS include ...
Preventing Anabolic Steroid Misuse Research on high school athletes shows they're less likely to misuse anabolic steroids if their friends and family disapprove. Peer pressure has a strong effect.
Anabolic steroid testing remains crucial in competitive sports to maintain fairness. ... Further research demonstrated that the internal standards (testosterone-16,16,17-d 3 and 5a-androstane-3a,17b-diol -d 3) were undergoing oxidation followed by H/D exchange to form the analytes resulting in a false positive result. The authors emphasize ...
The term "anabolic" means the use of body energy to promote growth and regulate constructive metabolism. Anabolic-androgenic steroids (AAS) are steroidal androgens, which include natural androgens such as male sex hormone testosterone or could be synthetic to mimic the action of the endogenous male hormone. Androgen use has become a major public health concern due to the transition of the use ...
While anabolic steroids are primarily sought for their performance-enhancing effects, the use of counterfeit products can negate these benefits and pose significant health risks. ... Regular surveys and research on harm reduction practices can provide valuable insights into the effectiveness of existing strategies and highlight areas for ...
Colby Huffman '25 and Ellie Jaynes '26 work to trace anabolic agents from the farm to the kitchen. Aug. 13, 2024. EDITOR'S NOTE: This is the sixth in an ongoing series spotlighting summer research projects and internships by Maryville College STEM students, made possible through a $645,000 Fund to Improve Post-Secondary Education (FIPSE) grant, administered through the U.S. Department of ...
Prospective research on anabolic steroid use and connective tissue injury is warranted. Psychological and Behavioral. An issue that is often raised with anabolic steroid use is the psychological and behavioral effects. Increases in aggressiveness, arousal and irritability have been associated with anabolic steroid use. This has potentially ...