Appointments at Mayo Clinic
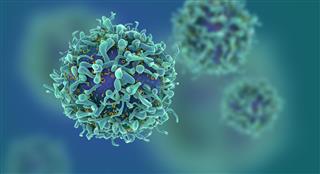
Stem cells: what they are and what they do.
Stem cells offer promise for new medical treatments. Learn about stem cell types, current and possible uses, and the state of research and practice.
You've heard about stem cells in the news, and perhaps you've wondered if they might help you or a loved one with a serious disease. Here are some answers to frequently asked questions about stem cells.

What are stem cells?
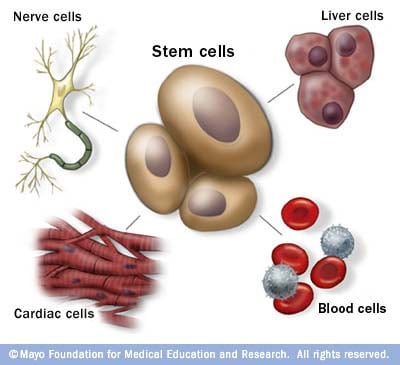
Stem cells: The body's master cells
Stem cells are the body's master cells. All other cells arise from stem cells, including blood cells, nerve cells and other cells.
Stem cells are a special type of cells that have two important properties. They are able to make more cells like themselves. That is, they self-renew. And they can become other cells that do different things in a process known as differentiation. Stem cells are found in almost all tissues of the body. And they are needed for the maintenance of tissue as well as for repair after injury.
Depending on where the stem cells are, they can develop into different tissues. For example, hematopoietic stem cells reside in the bone marrow and can produce all the cells that function in the blood. Stem cells also can become brain cells, heart muscle cells, bone cells or other cell types.
There are various types of stem cells. Embryonic stem cells are the most versatile since they can develop into all the cells of the developing fetus. The majority of stem cells in the body have fewer abilities to give rise to cells and may only help maintain and repair the tissues and organs in which they reside.
No other cell in the body has the natural ability to generate new cell types.
Why is there such an interest in stem cells?
Researchers are studying stem cells to see if they can help to:
- Increase understanding of how diseases occur. By watching stem cells mature into cells in bones, heart muscle, nerves, and other organs and tissue, researchers may better understand how diseases and conditions develop.
Generate healthy cells to replace cells affected by disease (regenerative medicine). Stem cells can be guided into becoming specific cells that can be used in people to regenerate and repair tissues that have been damaged or affected by disease.
People who might benefit from stem cell therapies include those with leukemia, Hodgkin disease, non-Hodgkin lymphoma and some solid tumor cancers. Stem cell therapies also might benefit people who have aplastic anemia, immunodeficiencies and inherited conditions of metabolism.
Stem cells are being studied to treat type 1 diabetes, Parkinson's disease, amyotrophic lateral sclerosis, heart failure, osteoarthritis and other conditions.
Stem cells may have the potential to be grown to become new tissue for use in transplant and regenerative medicine. Researchers continue to advance the knowledge on stem cells and their applications in transplant and regenerative medicine.
Test new drugs for safety and effectiveness. Before giving drugs in development to people, researchers can use some types of stem cells to test the drugs for safety and quality. This type of testing may help assess drugs in development for toxicity to the heart.
New areas of study include the effectiveness of using human stem cells that have been programmed into tissue-specific cells to test new drugs. For the testing of new drugs to be accurate, the cells must be programmed to acquire properties of the type of cells targeted by the drug. Techniques to program cells into specific cells are under study.
Where do stem cells come from?
There are several sources of stem cells:
Embryonic stem cells. These stem cells come from embryos that are 3 to 5 days old. At this stage, an embryo is called a blastocyst and has about 150 cells.
These are pluripotent (ploo-RIP-uh-tunt) stem cells, meaning they can divide into more stem cells or can become any type of cell in the body. This allows embryonic stem cells to be used to regenerate or repair diseased tissue and organs.
- Adult stem cells. These stem cells are found in small numbers in most adult tissues, such as bone marrow or fat. Compared with embryonic stem cells, adult stem cells have a more limited ability to give rise to various cells of the body.
Adult cells altered to have properties of embryonic stem cells. Scientists have transformed regular adult cells into stem cells using genetic reprogramming. By altering the genes in the adult cells, researchers can make the cells act similarly to embryonic stem cells. These cells are called induced pluripotent stem cells (iPSCs).
This new technique may allow use of reprogrammed cells instead of embryonic stem cells and prevent immune system rejection of the new stem cells. However, scientists don't yet know whether using altered adult cells will cause adverse effects in humans.
Researchers have been able to take regular connective tissue cells and reprogram them to become functional heart cells. In studies, animals with heart failure that were injected with new heart cells had better heart function and survival time.
Perinatal stem cells. Researchers have discovered stem cells in amniotic fluid as well as umbilical cord blood. These stem cells can change into specialized cells.
Amniotic fluid fills the sac that surrounds and protects a developing fetus in the uterus. Researchers have identified stem cells in samples of amniotic fluid drawn from pregnant women for testing or treatment — a procedure called amniocentesis.
Why is there controversy about using embryonic stem cells?
The National Institutes of Health created guidelines for human stem cell research in 2009. The guidelines define embryonic stem cells and how they may be used in research and include recommendations for the donation of embryonic stem cells. Also, the guidelines state that embryonic stem cells from embryos created by in vitro fertilization can be used only when the embryo is no longer needed.
Where do these embryos come from?
The embryos being used in embryonic stem cell research come from eggs that were fertilized at in vitro fertilization clinics but never implanted in women's uteruses. The stem cells are donated with informed consent from donors. The stem cells can live and grow in special solutions in test tubes or petri dishes in laboratories.
Why can't researchers use adult stem cells instead?
Progress in cell reprogramming and the formation of iPSCs has greatly enhanced research in this field. However, reprogramming is an inefficient process. When possible, iPSCs are used instead of embryonic stem cells since this avoids the ethical issues about use of embryonic stem cells that may be morally objectionable for some people.
Although research into adult stem cells is promising, adult stem cells may not be as versatile and durable as are embryonic stem cells. Adult stem cells may not be able to be manipulated to produce all cell types, which limits how adult stem cells can be used to treat diseases.
Adult stem cells are also more likely to contain irregularities due to environmental hazards, such as toxins, or from errors acquired by the cells during replication. However, researchers have found that adult stem cells are more adaptable than was first thought.
What are stem cell lines, and why do researchers want to use them?
A stem cell line is a group of cells that all descend from a single original stem cell and are grown in a lab. Cells in a stem cell line keep growing but don't become specialized cells. Ideally, they remain free of genetic defects and continue to create more stem cells. Clusters of cells can be taken from a stem cell line and frozen for storage or shared with other researchers.
What is stem cell therapy (regenerative medicine), and how does it work?
Stem cell therapy, also known as regenerative medicine, promotes the repair response of diseased, dysfunctional or injured tissue using stem cells or their derivatives. It is the next chapter in organ transplantation and uses cells instead of donor organs, which are limited in supply.
Researchers grow stem cells in a lab. These stem cells are manipulated to specialize into specific types of cells, such as heart muscle cells, blood cells or nerve cells.
The specialized cells can then be implanted into a person. For example, if the person has heart disease, the cells could be injected into the heart muscle. The healthy transplanted heart muscle cells could then contribute to repairing the injured heart muscle.
Researchers have already shown that adult bone marrow cells guided to become heart-like cells can repair heart tissue in people, and more research is ongoing.
Have stem cells already been used to treat diseases?
Yes. Doctors have performed stem cell transplants, also known as bone marrow transplants, for many decades. In hematopoietic stem cell transplants, stem cells replace cells damaged by chemotherapy or disease or serve as a way for the donor's immune system to fight some types of cancer and blood-related diseases. Leukemia, lymphoma, neuroblastoma and multiple myeloma often are treated this way. These transplants use adult stem cells or umbilical cord blood.
Researchers are testing adult stem cells to treat other conditions, including some degenerative diseases such as heart failure.
What are the potential problems with using embryonic stem cells in humans?
For embryonic stem cells to be useful, researchers must be certain that the stem cells will differentiate into the specific cell types desired.
Researchers have discovered ways to direct stem cells to become specific types of cells, such as directing embryonic stem cells to become heart cells. Research is ongoing in this area.
Embryonic stem cells also can grow irregularly or specialize in different cell types spontaneously. Researchers are studying how to control the growth and development of embryonic stem cells.
Embryonic stem cells also might trigger an immune response in which the recipient's body attacks the stem cells as foreign invaders, or the stem cells might simply fail to function as expected, with unknown consequences. Researchers continue to study how to avoid these possible complications.
What is therapeutic cloning, and what benefits might it offer?
Therapeutic cloning, also called somatic cell nuclear transfer, is a way to create versatile stem cells independent of fertilized eggs. In this technique, the nucleus is removed from an unfertilized egg. This nucleus contains the genetic material. The nucleus also is removed from the cell of a donor.
This donor nucleus is then injected into the egg, replacing the nucleus that was removed, in a process called nuclear transfer. The egg is allowed to divide and soon forms a blastocyst. This process creates a line of stem cells that is genetically identical to the donor's cells — in essence, a clone.
Some researchers believe that stem cells derived from therapeutic cloning may offer benefits over those from fertilized eggs because cloned cells are less likely to be rejected once transplanted back into the donor. And it may allow researchers to see exactly how a disease develops.
Has therapeutic cloning in people been successful?
No. Researchers haven't been able to successfully perform therapeutic cloning with humans despite success in a number of other species.
Researchers continue to study the potential of therapeutic cloning in people.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Stem cell basics. National Institutes of Health. https://stemcells.nih.gov/info/basics/stc-basics/#stc-I. Accessed March 21, 2024.
- Lovell-Badge R, et al. ISSCR guidelines for stem cell research and clinical translation: The 2021 update. Stem Cell Reports. 2021; doi:10.1016/j.stemcr.2021.05.012.
- AskMayoExpert. Hematopoietic stem cell transplant. Mayo Clinic; 2024.
- Stem cell transplants in cancer treatment. National Cancer Institute. https://www.cancer.gov/about-cancer/treatment/types/stem-cell-transplant/. Accessed March 21, 2024.
- Townsend CM Jr, et al. Regenerative medicine. In: Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 21st ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed March 21, 2024.
- Kumar D, et al. Stem cell based preclinical drug development and toxicity prediction. Current Pharmaceutical Design. 2021; doi:10.2174/1381612826666201019104712.
- NIH guidelines for human stem cell research. National Institutes of Health. https://stemcells.nih.gov/research-policy/guidelines-for-human-stem-cell-research. Accessed March 21, 2024.
- De la Torre P, et al. Current status and future prospects of perinatal stem cells. Genes. 2020; doi:10.3390/genes12010006.
- Yen Ling Wang A. Human induced pluripotent stem cell-derived exosomes as a new therapeutic strategy for various diseases. International Journal of Molecular Sciences. 2021; doi:10.3390/ijms22041769.
- Alessandrini M, et al. Stem cell therapy for neurological disorders. South African Medical Journal. 2019; doi:10.7196/SAMJ.2019.v109i8b.14009.
- Goldenberg D, et al. Regenerative engineering: Current applications and future perspectives. Frontiers in Surgery. 2021; doi:10.3389/fsurg.2021.731031.
- Brown MA, et al. Update on stem cell technologies in congenital heart disease. Journal of Cardiac Surgery. 2020; doi:10.1111/jocs.14312.
- Li M, et al. Brachyury engineers cardiac repair competent stem cells. Stem Cells Translational Medicine. 2021; doi:10.1002/sctm.20-0193.
- Augustine R, et al. Stem cell-based approaches in cardiac tissue engineering: Controlling the microenvironment for autologous cells. Biomedical Pharmacotherapy. 2021; doi:10.1016/j.biopha.2021.111425.
- Cloning fact sheet. National Human Genome Research Institute. https://www.genome.gov/about-genomics/fact-sheets/Cloning-Fact-Sheet. Accessed March 21, 2024.
- Dingli D (expert opinion). Mayo Clinic. Nov. 17, 2023.
Products and Services
- A Book: Living Medicine
- Give today to find cancer cures for tomorrow
- Acute lymphocytic leukemia
- Acute myelogenous leukemia
- Adjuvant therapy for cancer
- Amyloidosis
- Aplastic anemia
- Atypical cells: Are they cancer?
- Biopsy procedures
- Blood Cancers and Disorders
- Bone marrow transplant
- Cancer blood tests
- Myths about cancer causes
- Infographic: Cancer Clinical Trials Offer Many Benefits
- Cancer diagnosis: 11 tips for coping
- Cancer-related fatigue
- Cancer pain: Relief is possible
- Cancer risk: What the numbers mean
- Cancer surgery
- Cancer survival rate
- Cancer survivors: Care for your body after treatment
- Cancer survivors: Late effects of cancer treatment
- Cancer survivors: Managing your emotions after cancer treatment
- Cancer treatment myths
- Chemotherapy side effects: A cause of heart disease?
- Chronic lymphocytic leukemia
- Chronic myelogenous leukemia
- Curcumin: Can it slow cancer growth?
- What is type 1 diabetes? A Mayo Clinic expert explains
- Type 1 diabetes FAQs
- Cancer-related diarrhea
- DiGeorge syndrome (22q11.2 deletion syndrome)
- Eating during cancer treatment: Tips to make food tastier
- Epidermolysis bullosa
- Gaucher disease
- Heart cancer: Is there such a thing?
- High-dose vitamin C: Can it kill cancer cells?
- Hodgkin lymphoma (Hodgkin disease)
- Hodgkin's vs. non-Hodgkin's lymphoma: What's the difference?
- Low blood counts
- Measles Virus as a Cancer Fighter
- Monoclonal antibody drugs
- Mort Crim and Cancer
- Mouth sores caused by cancer treatment: How to cope
- Multiple myeloma
- Infographic: Multiple Myeloma
- Myelofibrosis
- Neuroblastoma
- No appetite? How to get nutrition during cancer treatment
- Non-Hodgkin's lymphoma
- Scleroderma
- Self-Image During Cancer
- Sickle cell anemia
- Sisters' Bone Marrow Transplant
- Small cell, large cell cancer: What this means
- Stem Cells 101
- Thalassemia
- Tumor vs. cyst: What's the difference?
- Type 1 diabetes
- Stem cell transplant
- How cancer spreads
- PICC line placement
- When cancer returns: How to cope with cancer recurrence
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Stem cells What they are and what they do
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.

19 Advantages and Disadvantages of Stem Cell Research
Stem cell research takes two primary forms: adult stem cells and embryonic stem cells. Each cell line that is harvested offers the opportunity to develop new treatments that may help to stop a plethora of diseases that affect humanity. Cord blood treatments that involve stem cells have helped to treat more than 6,000 people and 60+ diseases and that is just the beginning of what this medical research may offer.
One of the primary advantages of stem cell research is the availability of cell lines and that they can be obtained ethically. Adult stem cells can be harvested from healthy individuals by accessing their bone marrow and other tissue sources. Embryonic stem cells can be obtained from cord blood taken after the umbilical cord has been removed.
As for disadvantages, one of the primary points of content against this type of research is how some embryonic stem cells are obtained. These cells require the destruction of an embryo when harvested, which to some is a direct decision to end a human life. No amount of medical research, it would be argued, should come at the expense of life itself, no matter the number of people who could be potentially treated from processes developed from the research.
There are additional advantages and disadvantages of stem cell research that must be considered. Here are the key points to look at.
What Are the Advantages of Stem Cell Research?
1. Adult stem cells have low rejection rates. Therapies can be developed from adult stem cells that are taken from each patient. These cells can then be transformed into various therapies that run a low risk of rejection because the cells are taken from the individual needing treatment. Even when familiar umbilical cord blood cells are used to develop treatments, the rejection rates are quite low. This limits the need for immunosuppressant treatments to maintain a positive quality of life in the future.
2. Some stem cells can be transformed into pluripotent stem cells. Adult stem cells, through the use of iPS reprogramming factors, have the ability to be reprogrammed into pluripotent stem cells. Once this occurs, they can be activated into mesoderm, endoderm, or ectoderm cells. This process allows for the potential benefits that embryonic stem cell lines could provide for medical treatments without the need to destroy embryos to collect the cells that are needed.
3. The current treatment options for stem cells are numerous. The most common use of stem cell therapy currently used is to treat leukemia and lymphoma patients with bone marrow transplantation. A stem cell therapy called Prochymal has been conditionally approved in Canada to manage graft vs host disease in children who do not respond to steroid treatments. Holoclar is another potential treatment that can help people with severe limbal deficiencies because of burns to the eye. In the US, there are 5 hematopoietic cord blood treatments that have been approved by the FDA.
4. This research gives us insights into how human life works. Stem cell research allows us to understand how the cells in our bodies work. By understanding these processes better, it becomes possible to understand how an illness or disease develops. Even if a stem cell therapy isn’t developed from this research, the understanding obtained can help to create new treatments that can potentially cure what is damaging our cells. That allows us to extend average life expectancy rates, stop diseases, and even reduce the costs of medical treatments.
5. Because stem cells have regenerative properties, the potential is unlimited. Imagine being able to grow a replacement organ for one that is failing. Or having a veteran who lost a limb in an attack could have a replacement grown in a lab setting and then attached so they don’t need a prosthetic – they could have the real thing. The potential of stem cell research is unlimited, including offering the chance to improve mental health. Improving insulin production, repairing damaged heart muscle after a heart attack, repairing torn tendons or ligaments, and even attacking cancers or viruses. Embryonic stem cells offer a similar potential, along with the possibility of being able to treat certain genetic disorders or birth defects so more people could go on to live happy and healthy lives.
6. Embryonic treatments can be developed through stem cell research. Many issues that afflict the human condition occur during the initial stages of development for the embryo. Errors in the cell’s coding can lead to potential birth defects as the embryo transitions into being a fetus. By studying how stem cells begin to transform into the 200+ different cell types of the human body, medical science has the potential to learn how defects, genetic errors, and other problems develop and stop that process before it starts – even if the parents are carriers of current genetic disorders.
7. Stem cell research could reduce pregnancy loss. Miscarriage is defined as the spontaneous loss of a pregnancy before the 20th week. Up to 20% of known pregnancies end in a miscarriage, those the number is likely higher because most miscarriages occur so early on at the embryonic stage of development that women don’t realize they’ve become pregnant. Stem cell research offers the potential of reducing this issue so that more pregnancies can be successful with individualized treatments developed from this work.
8. Stem cells can self-replicate in enormous numbers. It only takes a few adult stem cells to create potentially trillions of cells that are specialized to a certain treatment. With ongoing research, even current cell lines, including embryonic lines, can continue to self-replicate and provide ongoing research opportunities.
What Are the Disadvantages of Stem Cell Research?
1. Embryonic stem cells can have high rejection rates. Embryonic stem cell therapies have been known to create several future health problems. Rejection rates are high for these therapies. Research has shown that these therapies encourage the development of tumors. Some embryonic stem cells do not respond to the activation sequences as intended.
2. Adult stem cells have a determined cell type. Without iPS reprogramming, adult stem cells have a determined cell type. This means they cannot be changed into different cell tissues. This limits the therapies that can be developed by stem cell research because the cells, in their raw form, can only involve the same type of tissue from which they were harvested in the first place.
3. Obtaining any form of stem cell is a difficult process. To collect embryonic stem cells, the embryo must be grown in a culture. Once harvested, it takes several months for the stem cells to grow enough to the point where they could be potentially used for the creation of a therapy. Adult stem cells, especially those which are obtained from a person’s bone marrow, can be extremely painful to obtain for the patient. Some individuals may not live anywhere near a facility that has the capabilities of obtaining those cells, which creates another set of logistics which must be solved.
4. Stem cell treatments are an unproven commodity. The treatments developed from stem cells are experimental at the current phase of research. There is the potential of having such a treatment work with current research, but there is a better chance that nothing could happen. The most effective therapy right now is hematopoietic stem cell transplantation (HSCtx). They are 90% effective and about 50,000 transplants occur per year.
5. Stem cell research is a costly process. The cost of a single stem cell treatment that has been approved for use in the United States is typically about $10,000. Some clinics have found ways to reduce this cost by up to 20%. Outside of the United States, the costs of a single treatment can be as high as $100,000. The cost of harvesting an embryo for stem cells is up to $2,000 per instance. Services rendered to take adult stem cells may not be included in the treatment cost and could be several thousand dollars. And, because stem cell treatments are experimental in most instances, health insurance plans and government-provided benefits do not generally provide access to them.
6. We do not know if there are long-term side effects to worry about. Tens of thousands of people are receiving stem cell transplants every year, with efficacy rates improving each year for the dozens of illnesses and diseases that respond positively to such treatments. What we do not know yet is if there are long-term consequences to such therapies, even if there are short-term benefits that are being seen. More than 3,500 different research studies are happening right now to determine the effectiveness of stem cell research and therapies, but the results are still pending.
7. There will always be some limitation to the research possibilities. The ethics of stem cell research will always place limitations on the medical potential of this research. Individuals must decide on their own how they will respond to the ethics of this research. Is it permitted to alter adult stem cells or umbilical embryonic stem cells? What are the consequences of destroying an embryo to get stem cells, even if that embryo was going to be discarded? Some people will feel the entire process is unethical and that has the potential to hold this research back.
8. Research has been held back by factual contradictions. Some of the research in this field has been discredited because it contains hundreds of factual contradictions. This includes some of the pioneering work in stem cell research by Bodo-Eckehard Strauer, who focused on how stem cells could help to treat cardiovascular conditions. Current research has had to correct these contradictions before proceeding with future potential benefits.
9. Research opportunities are somewhat limited, especially in the United States. In 2001, when the US Government took steps to limit the funding and availability of stem cell research to just 19 lines. The research itself wasn’t banned, but the severe restrictions placed on having funding for that research made it virtually impossible to conduct for more than a decade. Some states in the US have or have an interest in additional restrictions or complete bans on embryonic stem cell research in its current state.
10. Adults have very few stem cells. The treatment options that are available for adult stem cells without reprogramming are few because the number of cells that adults have are very few. Although they reside in many different areas of the body, they are isolated from tissue samples and their current source is unknown. Being able to separate them is a time-consuming and costly process and self-renewal within the body may be slow to occur.
11. Current embryonic stem cell harvesting requires the death of an embryo. Harvesting embryonic stem cells and germ cells may offer numerous research advantages compared to adult stem cells, but current methods of harvesting require the death of the embryo. Embryonic stem cells also have limited self-renewals, measured at 2 years. Germ cells can double a maximum of up to 80 times. This limits the research potential of any existing line.
The advantages and disadvantages of stem cell research go beyond the ethics of this field. Although the proven benefits of stem cell research are somewhat limited according to current science, the future potential of these treatments continues to inspire hope for many. As the processes to develop adult stem cells into programmable cells, the ethical questions may begin to fade. Until then, each key point must be considered before a final conclusion can be reached.
- Branches of Biology
- Importance of Biology
- Domain Archaea
- Domain Eukarya
- Biological Organization
- Biological Species Concept
- Biological Weathering
- Cellular Organization
- Cellular Respiration
- Types of Plants
- Plant Cells Vs. Animal Cells
- Prokaryotic Cells Vs. Eukaryotic Cells
- Amphibians Vs. Reptiles
- Anatomy Vs. Physiology
- Diffusion vs. Osmosis
- Mitosis Vs. Meiosis
- Chromosome Vs. Chromatid
- History of Biology
- Biology News

- Cell Biology
- Pros and Cons
Top 17 Stem Cell Research Pros and Cons

The human body is made up of trillions of cells that are the foundation for different tissue and organ systems. When an injury or damage is incurred, new cells are generated from unspecialized precursor cells.
These precursor cells are known as stem cells , and they are known to have potent regenerative capabilities. Stem cells are the basis for worldwide research in the field of therapeutics and are widely viewed as an effective treatment regime for some different diseases.
We will explore some of the stem cell research pros and cons within the scope of this article. Let’s begin.
Table of Contents
What is Stem Cell Therapy?
1. stem cells in therapeutics & regenerative medicine:, 2. stem cell research detects birth defects early:, 3. stem cell research opens up new avenues in cell biology:, 4. transplant rejection minimized using stem cells:, 5. stem cell research enables generation of body organs:, 6. embryonic stem cell research utilizes miscarried embryos:, 7. stem cell research helps for better drug testing:, 8. certain stem cells can be converted into pluripotent stem cells:, 9. stem cells can reduce the incidence of pregnancy loss:, 10. stem cells grow & replicate in bulk:, 1. long-term effects of stem cell therapy are unknown:, 2. harvest of embryonic stem cells is a long-debated issue:, 3. adult stem cells can specialize only into specific lineages:, 4. stem cell research may not provide solutions to all ailments:, 5. embryonic stem cell transplants mostly rejected:, 6. stem cell research is expensive & requires funding:, 7. stem cell therapy has side effects:.
Stem cell therapy involves isolating stem cells from their respective niche and using them to treat a disorder, area of injury or damaged tissue.
- The ability of stem cells to renew themselves and generate new cells can aid in the treatment of neurological diseases such as Parkinson’s and Alzheimer’s, diabetes, or in the regeneration of bone and cardiac tissues, as well as in bone and spinal cord injuries.
- There are different types of stem cells and based on the types, a plethora of therapeutic applications exist for stem cells.
- However, the use of stem cell therapy entails specific advantages, disadvantages and ethical concerns .
Pros/Advantages of Stem Cell Research:
The immense regenerative and specialization potential of stem cells makes them valuable for the treatment of neurodegenerative diseases, injuries or damages to tissues, and diseases such as diabetes.
- In a disease such as diabetes, the pancreatic cells are destroyed by the immune cells, thereby reducing the production of insulin for the body.
- Stem cells can be engineered to be transformed into pancreatic cells that can produce insulin. These cells can then be transplanted into the patient’s body that will help cure the effects of diabetes.
- Stem cell treatments are also used in spinal cord injuries and are actively being researched upon for artificial limb generation.
- Research into stem cell development can help researchers understand problems that arise during these stages that lead to birth defects, and other problems that occur during pregnancy.
- For instance, researchers may be able to study closely the development of the embryo and changes that can lead to the occurrence of physical and genetic defects in the fetus. Detecting these defects at an early stage is crucial for prospective treatment and care.
Stem cell research can help scientists understand and investigate cellular growth and development.
- The field of stem cells is in itself a separate field that encompasses its principles, modes of research and techniques. Over time, it has proven to be one of the most widely researched upon, and popular fields in science.
- It provides insight into cell biology , by helping scientists understand the genetic mechanisms of the cell that control cell specialization and cellular markers that define each stage of the cell cycle .
- It enables scientists to study closely, the mechanism of cellular regeneration and the changes associated with the transformation of one cell type to another. Using this information, scientists have successfully been able to replicate the transformation process in vitro.
- Stem cells are genetically and physiologically the cells of the patient’s own body, thus reducing the risk of rejection when these cells are transplanted for therapeutic purposes. This is true only for adult stem cells that are extracted from the patient’s tissue.
- Adult stem cells have the capability of transforming into a cell type of their lineage. For example, the Hematopoietic stem cell can transform into any blood cell type .
Stem cells can be used to grow organs or limbs in patients with loss of limb or loss of function of an organ.
- Since stem cells have the endless capacity to replicate and transform into specialized cells , isolating bone stem cells, can help regenerate and grow bone cells in vitro by providing them with the required factors and growth factor.
- This is true for other tissues as well such as pancreatic tissue, and retinal cells of the eye.
Embryonic stem cells have immense potential in therapy, as they can regenerate into any cell type of the body.
- Embryos are scientifically thought not to have a life. However, there are many debates related to this topic. Embryonic stem cells are isolated from the blastocyst stage of the embryo.
- Individuals who have experienced pregnancy loss at this stage, sometimes donate the embryos for research purposes.
The use of stem cells in therapeutics can minimize the need for animal testing. With stem cells, a colony of cells can be grown that mimic a disease and act as a model for drug testing and treatment (E.g., cancer cells).
Although adult stem cells only retain the capacity to specialize in a specific cell type, they are reprogrammable into pluripotent stem cells.
Some pregnancies end in miscarriage mostly because of a defect or a fault at the embryonic stage of development.
- A look into embryonic growth and how stem cells function can provide insight into how they can be used to prevent pregnancy loss in the early trimester.
- Scientists may be able to pinpoint the genetic defects and underlying causes that lead to pregnancy loss in the early trimester by studying isolated embryos that have miscarried and the properties of embryonic stem cells within.
Embryonic stem cells have large regenerative capacities and can be maintained as cell lines for research and treatment purposes.
- The regenerative capacity of the embryonic stem cells makes it very easy to propagate and culture different kinds of cell lines for research and testing purposes.
7 Cons/Disadvantages of Stem Cell Research:
With any new technology, the long-term effects may be unknown or hard to decipher. Similarly, the effects of stem-cell therapy on treatment of diseases or transplants may be untested in the long run and treatments in clinical trials should be well planned and studied before administering it on patients as a medical product.
Embryonic stem cells, albeit highly potential, are the center of much debate and discussion. This is because embryonic stem cells are harvested from the blastocyst stage of the embryos that are either miscarried or aborted.
- To some groups, embryos are the equivalent of human beings and using embryos for this purpose is unethical, as embryos are considered to have life from the time of conception and should not be used for research or testing purposes.
Adult stem cells have limited specialization properties.
- They can specialize only in cells of their respective lineage and as such cannot be cultured to produce any cells in the body.
- Moreover, harvesting volumes of adult stem cells are usually low. For example, adult stem cells isolated from pancreatic tissue retain the ability to specialize in the alpha and beta type of pancreatic cells that produce glucagon and insulin respectively.
Stem cell therapy may not apply to genetic disorders which are more complicated.
- Genetic conditions have their root at the gene level, as such, other types of treatments need to be developed to target genetic disorders.
- Stem cells may provide the answer to symptomatic treatment of such disorders but may not cure it at its root.
Embryonic stem cells are harvested from blastocysts or embryos. Therefore, they are not a patient’s body cells and may be rejected on transplantation. This differs from adult stem cells which do not pose a risk of rejection as they are a patient’s cells.
It is known that stem cell researchers rely heavily on external funding and the procedures are likely an expensive affair. Still, many scientists and researchers believe that the potential benefits outweigh the cost incurred.
Stem cell transplants in the treatment of cancer may have certain side effects such as nausea, vomiting, etc. Like all treatments, stem cell treatment also has its side effects.
Stem cell research today is of prime importance and extremely beneficial. With the rates at which diseases are progressing, it is vital today, to efficiently be able to employ stem cell therapy into total practice and reap the benefits it offers in the field of therapeutics.
Further research in this field, can help decipher how to control side effects, and what long-term effects these therapies may render.
By large, stem cells can revolutionize the field of medicine and therapeutics and provide a solution to some different ailments that are widespread today.
Cite This Page
- “Pros and Cons of Stem Cell Therapy” . Accessed April 12, 2018. Link .
- “What is Stem Cell Therapy? | ReeLabs” . Accessed April 12, 2018. Link .
- “Stem Cell Research – Advantages and Disadvantages – Advantages and disadvantages table in GCSE Biology” . Accessed April 12, 2018. Link .
- “14 Key Pros and Cons of Embryonic Stem Cell Research | Green Garage” . Accessed April 12, 2018. Link .
- “19 Advantages and Disadvantages of Stem Cell Research | Vittana.org” . Accessed April 12, 2018. Link .
RELATED ARTICLES MORE FROM AUTHOR

Top Cell Biology News of 2020 – A Round Up
Top 10 Cell Biology Discoveries in 2019

Explore The Top 8 Functions of Golgi Apparatus
Explore Mitochondria Functions & Their Importance

Top 15 Discoveries in Cell Biology for 2018

Top 20 Biomass Energy Pros and Cons
[…] bioexplorer.net […]
LEAVE A REPLY Cancel reply
Save my name, email, and website in this browser for the next time I comment.
By using this form you agree with the storage and handling of your data by this website. *
Recent Posts

The Top 25 Bicolor Flowers: Nature’s Two-Toned Wonders

Top 18 Amazon Rainforest Plants

Top 26 Best Hawaiian Flowers

25 Must-See Colorful Orchids

What Do Peacocks Eat?

World’s Top 15 Poisonous Caterpillars
Marine Biology 101: Ocean Life Explained

25 Reasons That Emphasizes The Importance of Biology

Top 27 Biology-themed Movies

Biology Boomtowns: 10 Best US Cities for Job Opportunities
Uncovering the Fathers of Biology: The Geniuses Who Unveiled Life’s Secrets
25 Mind-Blowing Biology Breakthroughs That Shaped Our World!

Types of Doctors
40 Different Types of Birds
334 Types of Monkeys
Biology history.

History of Anatomy
History of Biochemistry

History of Biotechnology
History of Botany

History of Cell Biology

History of Ecology
Complete History of Evolution

History of Genetics
History of Immunology

History of Microbiology
- Privacy Policy

- Foundations
- Write Paper
Search form
- Experiments
- Anthropology
- Self-Esteem
- Social Anxiety
- Foundations >
Stem Cell Research
Pros and cons in research.
The debate of the pros and cons of stem cell research clearly illustrate the difficult ethics evaluations researchers sometimes must do.
This article is a part of the guide:
- Ethics in Research
- Tuskegee Syphilis Study
- Privacy for Participants
- Scientific Misconduct
Browse Full Outline
- 1 Ethics in Research
- 2.1.1 Tuskegee Syphilis Study
- 3 Privacy for Participants
- 4 Animals in Research
- 5 Stem Cells
- 6.1 Scientific Misconduct
- 6.2.1 Subliminal Messages - An Example of Fraud
- 6.2.2 Scientific Falsification
- 6.3 Grant Funding
- 7.1 Academic Plagiarism
- 7.2 Sham Peer Review
- 8 Whistleblowers
All scientists must consider whether the positive effects from their research are likely to be significantly higher than the negative effects.
What are Stem Cells?
Stem Cells are crucial to develop organisms. They are nonspecialized cells which have the potential to create other types of specific cells, such as blood-, brain-, tissue- or muscle-cells.
Stem cells are in all of our body and lives, but are far more potent in a fetus (also spelled foetus, fœtus, faetus, or fætus) than in an adult body.
Some types of stem cells may be able to create all other cells in the body. Others have the potential to repair or replace damaged tissue or cells.
Embryonic Stem Cells are developed from a female egg after it is fertilized by sperm. The process takes 4-5 days.

What is Stem Cell Research?
Stem cell research is used for investigation of basic cells which develop organisms. The cells are grown in laboratories where tests are carried out to investigate fundamental properties of the cells.
The controversy surrounding stem cell research led to an intense debate about ethics. Up until the recent years, the research method mainly focused on Embryonic Stem Cells, which involves taking tissue from an aborted embryo to get proper material to study. This is typically done just days after conception or between the 5th and 9th week.
Since then, researchers have moved on to more ethical study methods, such as Induced Pluripotent Stem Cells (iPS). iPS are artificially derived from a non-pluripotent cell, such as adult somatic cells.
This is probably an important advancement in stem cell research, since it allows researchers to obtain pluripotent stem cells, which are important in research, without the controversial use of embryos.
There were two main issues concerning stem cell research with both pros and cons:
- How the knowledge will be used
- Concerns about the methods
The first issue is really not just about stem cell research, as it may be applied to most research about human health.
Since 2007, the second point, concerns about the methods involved, has been less debated, because of scientific developments such as iPS.
1) Stem Cell Research - Arguments Regarding the Usage of the Knowledge
As you will most probably notice, the following arguments are not exclusively in use when talking about stem cell research.
Stem cell research can potentially help treat a range of medical problems. It could lead humanity closer to better treatment and possibly cure a number of diseases:
- Parkinson’s Disease
- Alzheimer’s Disease
- Heart Diseases, Stroke and Diabetes (Type 1)
- Birth Defects
- Spinal Cord Injuries
- Replace or Repair Damaged Organs
- Reduced Risk of Transplantation (You could possibly get a copy of your own heart in a heart-transplantation in the future
- Stem cells may play a major role in cancer
Better treatment of these diseases could also give significant social benefits for individuals and economic gains for society
- "We should not mess with human life."
- "Humans should not be trying to play God"
- Some argue that stem cell research in the far future can lead to knowledge on how to clone humans. It is hard to say whether this is true, but we have seen devastating consequences of other research-programs, even with good intentions, such as nuclear research.
2) Stem Cell Research - Pros and Cons About the Methods Involved
The controversy regarding the method involved was much tenser when researchers used Embryonic Stem Cells as their main method for stem cell research.
DISCLAIMER: These points are based on the old debate about the methods of stem cells research, from before 2007. Since then, scientists have moved on to use more ethical methods for stem cell research, such as iPS. This section serves as an illustration of the difficult evaluations researchers may have to analyze.
Pros Before 2007
- "The benefits of stem cell research have such a great outcome that they outweigh the ethical issues." (Cost-benefit-analysis)
- "If someone is going to have an abortion, isn’t it better that we use it for something useful?"
- Adult stem cells would not be that interesting because they do not have the same properties as stem cells from a fetus.
- The research would give great insights about the basics of the body.
Cons Before 2007
- Critics against stem cell research argued that the ethical issues of scientific work on aborted fetuses did not justify the possible benefits.
- "A life is a life and that should never be compromised. A fertilized egg should be valued as a human life even if it is in its very first weeks. Destroying human life in the hopes of saving human life is not ethical."
- We should (and will) develop more ethical methods (such as using adult stem cells) which will enable us to research ethically. We should wait until those methods are available.
- The scientific value has been overstated or has flaws. E.g. we do not know for sure that we can use stem cells to clone transplantable organs.
The stem cell-research is an example of the, sometimes difficult, cost-benefit analysis in ethics which scientists need to do. Even though many issues regarding the ethics of stem cell research have now been solved, it serves as a valuable example of ethical cost-benefit analysis.
The previously heated debate seems to have lead to new solutions which makes both sides happier.
Stem Cell pros and cons had to be valued carefully, for a number of reasons.
When you are planning a research project, ethics must always be considered. If you cannot defend a study ethically, you should not and will not be allowed to conduct it. You cannot defend a study ethically unless the presumed cost is lower than expected benefits. The analysis needs to include human/animal discomfort/risks, environmental issues, material costs/benefits, economy etc.
Why was the debate regarding the stem cell research so intense?
First, it was a matter of life - something impossible to measure. And in this case, researchers had to do exactly that: measure life against life.
Both an abortion and someone dying, suffering from a possible curable disease, is a tragedy. Which have the highest value? Does a big breakthrough in the research justify the use of the method in the present?
Would the benefits of studying abortions outweigh the costs? The choice was subjective: Nobody knows all the risks or all the possible outcomes, so we had to value it with our perception of the outcome. Perception is influenced by our individual feelings, morals and knowledge about the issue.
Second, at the time we did not know whether the research was necessary and sufficient to give us the mentioned health benefits.
Third, other consequences of the research are uncertain. Could the research be misused in the future or not? We simply do not know. All knowledge acquired, within research or other arenas, may be used for evil causes in the future - it is impossible to know.
The Stem cell research-debate is an example on how people value various aspects differently. It is also an example of how critics and debate can lead to significant improvements for both sides.
- Psychology 101
- Flags and Countries
- Capitals and Countries
Explorable.com (Mar 20, 2008). Stem Cell Research. Retrieved Sep 03, 2024 from Explorable.com: https://explorable.com/stem-cell-pros-and-cons
You Are Allowed To Copy The Text
The text in this article is licensed under the Creative Commons-License Attribution 4.0 International (CC BY 4.0) .
This means you're free to copy, share and adapt any parts (or all) of the text in the article, as long as you give appropriate credit and provide a link/reference to this page.
That is it. You don't need our permission to copy the article; just include a link/reference back to this page. You can use it freely (with some kind of link), and we're also okay with people reprinting in publications like books, blogs, newsletters, course-material, papers, wikipedia and presentations (with clear attribution).
Related articles
Embryonic Stems Cells - Nobel Prize Medicine 2007
Want to stay up to date? Follow us!
Save this course for later.
Don't have time for it all now? No problem, save it as a course and come back to it later.
Footer bottom
- Privacy Policy
- Subscribe to our RSS Feed
- Like us on Facebook
- Follow us on Twitter
- Utility Menu
GA4 tracking code

Examining the ethics of embryonic stem cell research

Following the recent passage by both houses of Congress of the Stem Cell Research Enhancement Act of 2007, which would permit federal funding of research using donated surplus embryonic stem cells from fertility clinics, the president has once again threatened a veto.
Because neither the House nor the Senate had sufficient votes to override a presidential veto, it appears unlikely this new bill will be enacted into law, further stalling the pace of this research. “This bill crosses a moral line that I and others find troubling,” stated Bush, following the Senate’s vote.
SCL : What are th e main arguments for and against embryonic stem cell research? MS : Proponents argue that embryonic stem cell research holds great promise for understanding and curing diabetes, Parkinson’s disease, spinal cord injury, and other debilitating conditions. Opponents argue that the research is unethical, because deriving the stem cells destroys the blastocyst, an unimplanted human embryo at the sixth to eighth day of development. As Bush declared when he vetoed last year’s stem cell bill, the federal government should not support “the taking of innocent human life.”
It is surprising that, despite the extensive public debate—in Congress, during the 2004 and 2006 election campaigns, and on the Sunday morning talk shows—relatively little attention has been paid to the moral issue at the heart of the controversy: Are the opponents of stem cell research correct in their claim that the unimplanted human embryo is already a human being, morally equivalent to a person?

“It is important to be clear about the embryo from which stem cells are extracted. It is not implanted and growing in a woman’s uterus. It is not a fetus. It has no recognizable human features or form. It is, rather, a blastocyst, a cluster of 180 to 200 cells, growing in a petri dish, barely visible to the naked eye.”
SCL : What are the contradictions in Bush’s stance? MS : Before we address that, it is important to be clear about the embryo from which stem cells are extracted. It is not implanted and growing in a woman’s uterus. It is not a fetus. It has no recognizable human features or form.
It is, rather, a blastocyst, a cluster of 180 to 200 cells, growing in a petri dish, barely visible to the naked eye. Such blastocysts are either cloned in the lab or created in fertility clinics. The bill recently passed by Congress would fund stem cell research only on excess blastocysts left over from infertility treatments.
The blastocyst represents such an early stage of embryonic development that the cells it contains have not yet differentiated, or taken on the properties of particular organs or tissues—kidneys, muscles, spinal cord, and so on. This is why the stem cells that are extracted from the blastocyst hold the promise of developing, with proper coaxing in the lab, into any kind of cell the researcher wants to study or repair.
The moral and political controversy arises from the fact that extracting the stem cells destroys the blastocyst. It is important to grasp the full force of the claim that the embryo is morally equivalent to a person, a fully developed human being.
For those who hold this view, extracting stem cells from a blastocyst is as morally abhorrent as harvesting organs from a baby to save other people’s lives. This is the position of Senator Sam Brownback, Republican of Kansas, a leading advocate of the right-to-life position. In Brownback’s view, “a human embryo . . . is a human being just like you and me; and it deserves the same respect that our laws give to us all.
If Brownback is right, then embryonic stem cell research is immoral because it amounts to killing a person to treat other people’s diseases.
SCL : What is the basis for the belief that personhood begins at conception? MS : Some base this belief on the religious conviction that the soul enters the body at the moment of conception. Others defend it without recourse to religion, by the following line of reasoning: Human beings are not things. Their lives must not be sacrificed against their will, even for the sake of good ends, like saving other people’s lives. The reason human beings must not be treated as things is that they are inviolable. At what point do humans acquire this inviolability? The answer cannot depend on the age or developmental stage of a particular human life. Infants are inviolable, and few people would countenance harvesting organs for transplantation even from a fetus.
Every human being—each one of us—began life as an embryo. Unless we can point to a definitive moment in the passage from conception to birth that marks the emergence of the human person, we must regard embryos as possessing the same inviolability as fully developed human beings.
SCL : By this line of reasoning, human embryos are inviolable and should not be used for research, even if that research might save many lives. MS : Yes, but this argument can be challenged on a number of grounds. First, it is undeniable that a human embryo is “human life” in the biological sense that it is living rather than dead, and human rather than, say, bovine.
But this biological fact does not establish that the blastocyst is a human being, or a person. Any living human cell (a skin cell, for example) is “human life” in the sense of being human rather than bovine and living rather than dead. But no one would consider a skin cell a person, or deem it inviolable. Showing that a blastocyst is a human being, or a person, requires further argument.
Some try to base such an argument on the fact that human beings develop from embryo to fetus to child. Every person was once an embryo, the argument goes, and there is no clear, non-arbitrary line between conception and adulthood that can tell us when personhood begins. Given the lack of such a line, we should regard the blastocyst as a person, as morally equivalent to a fully developed human being.
SCL : What is the flaw in this argument? MS : Consider an analogy: although every oak tree was once an acorn, it does not follow that acorns are oak trees, or that I should treat the loss of an acorn eaten by a squirrel in my front yard as the same kind of loss as the death of an oak tree felled by a storm. Despite their developmental continuity, acorns and oak trees differ. So do human embryos and human beings, and in the same way. Just as acorns are potential oaks, human embryos are potential human beings.
The distinction between a potential person and an actual one makes a moral difference. Sentient creatures make claims on us that nonsentient ones do not; beings capable of experience and consciousness make higher claims still. Human life develops by degrees.
SCL : Yet there are people who disagree that life develops by degrees, and believe that a blastocyst is a person and, therefore, morally equivalent to a fully developed human being. MS : Certainly some people hold this belief. But a reason to be skeptical of the notion that blastocysts are persons is to notice that many who invoke it do not embrace its full implications.
President Bush is a case in point. In 2001, he announced a policy that restricted federal funding to already existing stem cell lines, so that no taxpayer funds would encourage or support the destruction of embryos. And in 2006, he vetoed a bill that would have funded new embryonic stem cell research, saying that he did not want to support “the taking of innocent human life.”
“The distinction between a potential person and an actual one makes a moral difference. Sentient creatures make claims on us that nonsentient ones do not; beings capable of experience and consciousness make higher claims still. Human life develops by degrees.”
But it is a striking feature of the president’s position that, while restricting the funding of embryonic stem cell research, he has made no effort to ban it. To adapt a slogan from the Clinton administration, the Bush policy might be summarized as “don’t fund, don’t ban.” But this policy is at odds with the notion that embryos are human beings.
SCL : If Bush’s policy were consistent with his stated beliefs, how, in your opinion, would it differ from his current “don’t fund, don’t ban” policy? MS : If harvesting stem cells from a blastocyst were truly on a par with harvesting organs from a baby, then the morally responsible policy would be to ban it, not merely deny it federal funding.
If some doctors made a practice of killing children to get organs for transplantation, no one would take the position that the infanticide should be ineligible for federal funding but allowed to continue in the private sector. In fact, if we were persuaded that embryonic stem cell research were tantamount to infanticide, we would not only ban it but treat it as a grisly form of murder and subject scientists who performed it to criminal punishment.
SCL : Couldn’t it be argued, in defense of the president’s policy, that Congress would be unlikely to enact an outright ban on embryonic stem cell research? MS : Perhaps. But this does not explain why, if the president really considers embryos to be human beings, he has not at least called for such a ban, nor even called upon scientists to stop doing stem cell research that involves the destruction of embryos. In fact, Bush has cited the fact that “there is no ban on embryonic stem cell research” in touting the virtues of his “balanced approach.”
The moral oddness of the Bush “don’t fund, don’t ban” position confused even his spokesman, Tony Snow. Last year, Snow told the White House press corps that the president vetoed the stem cell bill because he considered embryonic stem cell research to be “murder,” something the federal government should not support. When the comment drew a flurry of critical press attention, the White House retreated. No, the president did not believe that destroying an embryo was murder. The press secretary retracted his statement, and apologized for having “overstated the president’s position.”
How exactly the spokesman had overstated the president’s position is unclear. If embryonic stem cell research does constitute the deliberate taking of innocent human life, it is hard to see how it differs from murder. The chastened press secretary made no attempt to parse the distinction. His errant statement that the president considered embryo destruction to be “murder” simply followed the moral logic of the notion that embryos are human beings. It was a gaffe only because the Bush policy does not follow that logic.
SCL : You have stated that the president’s refusal to ban privately funded embryonic stem cell research is not the only way in which his policies betray the principle that embryos are persons. How so? MS : In the course of treating infertility, American fertility clinics routinely discard thousands of human embryos. The bill that recently passed in the Senate would fund stem cell research only on these excess embryos, which are already bound for destruction. (This is also the position taken by former governor Mitt Romney, who supports stem cell research on embryos left over from fertility clinics.) Although Bush would ban the use of such embryos in federally funded research, he has not called for legislation to ban the creation and destruction of embryos by fertility clinics.
SCL : If embryos are morally equivalent to fully developed human beings, doesn’t it then follow that allowing fertility clinics to discard thousands of embryos is condoning mass murder? MS : It does. If embryos are human beings, to allow fertility clinics to discard them is to countenance, in effect, the widespread creation and destruction of surplus children. Those who believe that a blastocyst is morally equivalent to a baby must believe that the 400,000 excess embryos languishing in freezers in U.S. fertility clinics are like newborns left to die by exposure on a mountainside. But those who view embryos in this way should not only be opposing embryonic stem cell research; they should also be leading a campaign to shut down what they must regard as rampant infanticide in fertility clinics.
Some principled right-to-life opponents of stem cell research meet this test of moral consistency. Bush’s “don’t fund, don’t ban” policy does not. Those who fail to take seriously the belief that embryos are persons miss this point. Rather than simply complain that the president’s stem cell policy allows religion to trump science, critics should ask why the president does not pursue the full implications of the principle he invokes.
If he does not want to ban embryonic stem cell research, or prosecute stem cell scientists for murder, or ban fertility clinics from creating and discarding excess embryos, this must mean that he does not really consider human embryos as morally equivalent to fully developed human beings after all.
But if he doesn’t believe that embryos are persons, then why ban federally funded embryonic stem cell research that holds promise for curing diseases and saving lives?
- Skip to primary navigation
- Skip to main content
- Skip to footer
Biology Wise
Pros and Cons of Stem Cell Research: Ethics or Possibilities
Stem cell research has brought about a major breakthrough in the field of medical research. It refers to the study of mammalian stem cells for determining their use in remedial measures for various health disorders. This write-up talks about the pros and cons of stem cell research.
Like it? Share it!

It might seem like stuff from science fiction, but stem cell research is a reality today. It is a major field of study, using which, scientists the world over are exploring and uncovering hoards of medical possibilities that seem to be nothing short of miraculous. But every coin has two sides, and so, here, along with the positives, we shall also be looking at the negatives of this exciting field of science. But before that, let’s begin by understanding what stem cells actually are.
What are Stem Cells?
Stem cells are found in multi-cellular organisms. These cells are crucial for the growth of an organism, as they have the capacity to renew themselves, enabling them to divide and perform specialized functions. In mammals, there are two types of stem cells – embryonic and adult. Stem cell research is carried out on these two types of cells.
Stem Cell Research
Stem cell research is a relatively new field in medical science, which entails employing primitive human cells (stem cells), and developing them into any of the numerous types of cells found in the human body, including blood and brain cells.
This research is being touted as being extremely useful for treating the most serious of diseases, and ultimately for curing them. Be it neuro degenerative diseases, heart diseases, or Parkinson’s disease; the benefits of stem cell research encompass all.
Apart from being talked about as the next big thing in the field of medical science, stem cell research has also been a bone of contention because of the possibility of genetic engineering and human cloning.
Pros and Cons
Talking about the brighter side, stem cell research has led scientists and medical experts closer to finding the cures for birth defects, spinal cord injuries, heart diseases, diabetes, and so on. Another major benefit is the possibility that a way to replace or repair damaged organs can be forged from it. Stem cell research has the potential of leading to methods which may reduce the risks of organ transplants as well.
Apart from this, by closely studying how stem cells develop and grow, scientists may be able to use them for therapeutic cloning and regenerative medicines. There is also an argument that embryos can be used to extract cells from. This will pave the way for engineering stem cells to replicate specialized cells, such as those found in the brain, liver, and skin.
On the darker side of things, stem cell research is deemed to be unethical. Many argue that its benefits, however substantial, should not be allowed to shroud the issue of ethics. Cloning is vehemently objected to by those who are against it. It has also been said to have been declared illegal in some countries.
Another point of argument is that, human life shouldn’t be compromised for any purpose, even if it is in the form of an embryo. Some believe that life does not begin until birth, but those who argue against it say that an embryo is where life originates, and hence, using it for research is akin to killing.
Thus, it is clearly difficult to demarcate stem cell research as being advantageous or disadvantageous. While it may have indeed ushered in a new age for medical science, it still raises difficult questions when viewed from a moral or ethical standpoint. So, whether its medical benefits outweigh its ethical drawbacks, for now we leave it up to you, the reader, to decide.
Get Updates Right to Your Inbox
Privacy overview.

Embryonic and Adult Stem Cell Research - Addressing the Facts and the Issues: Pros and Cons of Stem Cell Research
- Pros and Cons of Stem Cell Research
- Stem Cells - Some Basics for Review
- News About Stem Cell Research and Developments
Positions in Favor of Stem Cell Research - Embryonic and/or Adult
- Examining the Ethics of Embryonic Stem Cell Research Source - Harvard Stem Cell Institute
- The Case for Embryonic Stem Cell Research: An Interview with Jonathan Moreno Moreno is the David and Lyn Silfen University Professor, and Professor of Medical Ethics and of History and Sociology of Science at the University of Pennsylvania, as well as a senior fellow at the Center for American Progress in Washington, D.C. Previously, he was president of the American Society for Bioethics and Humanities and served as a senior staff member for two presidential advisory committees.
Overviews (Pros and Cons) of Ethical Issues
- Debating Pros and Cons Stem Cell Research From the Journal of the American Medical Association, August 9, 2000, Vol. 284, No. 6: 681-682. Retrieved from the MAC Library's print collection
- Ethical Issues in Stem Cell Research Article from the research journal Endocrine Reviews, authored by Bernard Lo and Lindsay Parham, May 2009, 30(3): 204-213. Accessed through PubMed Central
- Ethics of Stem Cell Research Stanford Encyclopedia of Philosophy
- Pros and Cons of Embryonic Stem Cell Research This article is from ThoughtCo, a group of websites offering advice primarily on personal finance. The information appears to be objective and is presented for educational purposes.
- Stem Cells Hastings Center Bioethics Briefings for journalists, policy makers, and educators.
- Stem Cell Research as Innovation: Expanding the Ethical and Policy Conversation This article is from the research journal, The Journal of Law, Medicine & Ethics, authored by Rebecca Dresser, Summer 2010, 38(2): 332-341. Accessed through PubMed Central.
The Pew Research Center - Religion and Public Life
- Religious Groups' Official Positions on Stem Cell Research
- Stem Cell Research: At the Crossroads of Religion and Politics
- Stem Cell Research Around the World
- Religion and Stem Cell Research
About Pew Research Center Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. We conduct public opinion polling, demographic research, content analysis and other data-driven social science research. We do not take policy positions.
Our Mission We generate a foundation of facts that enriches the public dialogue and supports sound decision-making. We are nonprofit, nonpartisan and nonadvocacy. We value independence, objectivity, accuracy, rigor, humility, transparency and innovation.

The Ethics of Stem Cells
California Institute for Regenerative Medicine
Positions not in favor of stem cell research - embryonic and/or adult.
- The Ethics of Stem Cell Research Rev. Tadeusz Pacholczyk, Ph.D. is Director of Education of The National Catholic Bioethics Center.
- Stem Cell Research From The Center for Bioethics & Human Dignity: Exploring the Nexus of Biomedicine, Biotechnology, & Our Common Humanity (Trinity International University).
- The Case Against Embryonic Cell Research: An Interview with Yuval Levin Yuval Levin is the author of Tyranny of Reason. Previously, Levin was the executive director of the President’s Council on Bioethics. Currently, he is the Hertog Fellow at the Ethics and Public Policy Center in Washington, D.C., where he also directs the center’s Bioethics and American Democracy program.
- Bishops Campaign Against Embryonic Stem Cells From The National Catholic Reporter
Concerns About the Uses of Stem Cell Therapies
- The Trouble with Stem Cell Therapy A new industry is booming. But critics worry that the treatments are ineffective and dangerous. Here's how to protect yourself. From Consumer Reports
- A Slow Road for Stem Cells From the journal Nature: International Journal of Science.
- Regulating the Stem Cell Industry: Needs and Responsibilities From the Bulletin of the World Health Organization.
- Current Biosafety Considerations in Stem Cell Therapy Article from the research publication Cell Journal, authored by M. Mousavinejad, P.W. Andrews, & E.K. Shoraki, July-September 2016, 18(2): 281-287. Accessed through PubMed Central.
Normal Stem Cells

This file is licensed under the Creative Commons Attributed-Share Alike 3.0 Unported license. Malymajo [CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0)]
- << Previous: Home
- Next: Stem Cells - Some Basics for Review >>
- Last Updated: Jul 10, 2024 4:12 PM
- URL: https://libguides.mtaloy.edu/stem-cell-research
5 Proven Advantages and Disadvantages of Stem Cell Research
How many cells are in the human body? More than 30 trillion.
Some examples include muscle cells, brain cells, blood cells, and bone cells. As it is, they're all specialized to carry out a specific function.
Stem cells, however, are a little different. They're capable of giving rise to specialized cell types. Put it simply, they can become any type of cell in the body.
Given that, it's not surprising to know that they've become the target of scientific research.
What are the advantages and disadvantages of stem cell research?
Want to know? If so, be sure to keep reading-because that's what we'll be talking about below!
What Are Stem Cells?
Stem cells are undifferentiated cells. Not only do they have the ability to turn into other cells but they can also proliferate indefinitely.
In contrast, normal cells can only replicate themselves a few times before breaking down.
Where can you find stem cells? In most body tissues such as the bone marrow, skeletal muscles, and brain.
The Advantages and Disadvantages of Stem Cell Research
Stem cell research holds tremendous promise for medical treatments, however, there are downsides. Here are some of its pros and cons.
Stem cell research offers countless medical possibilities. After all, the cells are undifferentiated; this means that they can be used to treat various conditions.
For example, researchers may be able to treat diabetes by turning stem cells into insulin-producing cells. Other conditions that may benefit from such therapies include spinal injuries, stroke, Parkinson's disease, and Alzheimer's disease.
Another benefit is that it can help progress cancer research. How? Embryonic stem cells are similar to cancer cells in that they can reproduce themselves indefinitely.
By studying them, researchers may be able to develop treatments that are more effective against cancer cells.
Disadvantages
The main disadvantage of stem cell research has to do with the way that they're acquired-that is, it involves the destruction of human embryos. This makes it immoral for those who believe that life begins at contraception.
Another drawback is that we currently do not have a complete understanding of how embryonic stem cells work. For example, there might be long-term health effects that we're not yet aware of.
Last but not least, transplanted stem cells can have high rejection rates. After all, they're derived from foreign embryos. In other words, therapy may not always be successful.
The Stem Cell Therapy Market
The stem cell therapy market is booming. Nowadays, more and more clinics are offering these types of treatments.
One way for them to find patients is through lead generation services. For example, they might use these strategies .
Understanding Stem Cell Research
Hopefully, that gives you a better idea of the advantages and disadvantages of stem cell research. As you can see, there are both pros and cons to these types of therapies.
Looking for more health-related posts? If so, be sure to check out the rest of our blog!
Most Popular

5 Reasons Why You Feel Tired All the Time

Unleashing Innovation: The Next Generation PROSPER ULTRA 520 Printer

From Code to Solutions: Deep Dive into Backend Technologies and Data Mastery

How to Choose the Right Counsellor

Find the Best Forex Trading Signal Channels on Telegram: Top 10 Picks for 2024
Latest stories.

Why Partnering with an E-commerce Fulfillment Center Can Boost Your Bottom Line?

Solar-Powered Windows: The Future of Renewable Energy

What Are Some of the Top Preventive Maintenance Strategies for Fleets?

Subscribe to The Science Times!
Sign up for our free newsletter for the Latest coverage!
Recommended Stories

Why Scientific Support for Alcohol's Health Benefits Is Fading
![stem cell research pros and cons Solar Particle Events Could Deplete Ozone, Raise UV Levels and Increase DNA Damage [Study]](https://1721181113.rsc.cdn77.org/data/thumbs/full/54817/258/146/50/40/solar-particle-events-could-deplete-ozone-raise-uv-levels-and-increase-dna-damage-study.jpg)
Solar Particle Events Could Deplete Ozone, Raise UV Levels and Increase DNA Damage [Study]

“Smoking Gun” Evidence of Rare Massive Cosmic Void Revealed by Fast-Moving Stars; Could It Be the Missing Link in Black Hole Formation?
Uranus' Weak Radiation Belts Possibly Linked to Tilted, Lopsided Magnetic Field Causing 'Traffic Jams'
Pros & Cons of Embryonic Stem Cell Research
- Liberal Voices and Events
- The U. S. Government
- U.S. Foreign Policy
- U.S. Conservative Politics
- Women's Issues
- Civil Liberties
- The Middle East
- Race Relations
- Immigration
- Crime & Punishment
- Canadian Government
- Understanding Types of Government
- M.B.A., California State University, Long Beach
- B.A., Journalism and Nonfiction Writing, University of California, Los Angeles
On March 9, 2009, President Barack Obama lifted, by Executive Order , the Bush administration's eight-year ban on federal funding of embryonic stem cell research .
Remarked the President, "Today... we will bring the change that so many scientists and researchers, doctors and innovators, patients and loved ones have hoped for, and fought for, these past eight years."
In Obama's Remarks on Lifting the Embryonic Stem Cell Research Ban, he also signed a Presidential Memorandum directing the development of a strategy for restoring scientific integrity to government decision-making.
Bush Vetoes
In 2005, H.R. 810, the Stem Cell Research Enhancement Act of 2005, was passed by the Republican-led House in May 2005 by a vote of 238 to 194. The Senate passed the bill in July 2006 by a bipartisan vote of 63 to 37.
President Bush opposed embryonic stem cell research on ideological grounds. He exercised his first presidential veto on July 19, 2006, when he refused to allow H.R. 810 to become law. Congress was unable to muster enough votes to override the veto.
In April 2007, the Democratic-led Senate passed the Stem Cell Research Enhancement Act of 2007 by a vote of 63 to 34. In June 2007, the House passed the legislation by a vote of 247 to 176.
President Bush vetoed the bill on June 20, 2007.
Public Support for Embryonic Stem Cell Research
For years, all polls report that the American public STRONGLY supports federal funding of embryonic stem cell research.
Reported the Washington Post in March 2009 : "In a January Washington Post-ABC News poll, 59 percent of Americans said they supported loosening the current restrictions, with support topping 60 percent among both Democrats and independents. Most Republicans, however, stood in opposition (55 percent opposed; 40 percent in support)."
Despite public perceptions, embryonic stem cell research was legal in the U.S. during the Bush administration: the President had banned the use of federal funds for research. He did not ban private and state research funding, much of which was being conducted by pharmaceutical mega-corporations.
In Fall 2004, California voters approved a $3 billion bond to fund embryonic stem cell research. In contrast, embryonic stem cell research is prohibited in Arkansas, Iowa, North and South Dakota and Michigan.
Developments in Stem Cell Research
In August 2005, Harvard University scientists announced a breakthrough discovery that fuses "blank" embryonic stem cells with adult skin cells, rather than with fertilized embryos, to create all-purpose stem cells viable to treat diseases and disabilities.
This discovery doesn't result in the death of fertilized human embryos and thus would effectively respond to pro-life objections to embryonic stem cell research and therapy.
Harvard researchers warned that it could take up to ten years to perfect this highly promising process.
As South Korea, Great Britain, Japan, Germany, India and other countries rapidly pioneer this new technological frontier, the US is being left farther and farther behind in medical technology. The US is also losing out on billions in new economic opportunities at a time when the country sorely needs new sources of revenues.
Therapeutic cloning is a method to produce stem cell lines that were genetic matches for adults and children.
Steps in therapeutic cloning are:
- An egg is obtained from a human donor.
- The nucleus (DNA) is removed from the egg.
- Skin cells are taken from the patient.
- The nucleus (DNA) is removed from a skin cell.
- A skin cell nucleus is implanted in the egg.
- The reconstructed egg, called a blastocyst, is stimulated with chemicals or electric current.
- In 3 to 5 days, the embryonic stem cells are removed.
- The blastocyst is destroyed.
- Stem cells can be used to generate an organ or tissue that is a genetic match to the skin cell donor.
The first 6 steps are same for reproductive cloning . However, instead of removing stem cells, the blastocyst is implanted in a woman and allowed to gestate to birth. Reproductive cloning is outlawed in most countries.
Before Bush stopped federal research in 2001, a minor amount of embryonic stem cell research was performed by US scientists using embryos created at fertility clinics and donated by couples who no longer needed them. The pending bipartisan Congressional bills all propose using excess fertility clinic embryos.
Stem cells are found in limited quantities in every human body and can be extracted from adult tissue with great effort but without harm. The consensus among researchers has been that adult stem cells are limited in usefulness because they can be used to produce only a few of the 220 types of cells found in the human body. However, evidence has recently emerged that adult cells may be more flexible than previously believed.
Embryonic stem cells are blank cells that have not yet been categorized or programmed by the body and can be prompted to generate any of the 220 human cell types. Embryonic stem cells are extremely flexible.
Embryonic stem cells are thought by most scientists and researchers to hold potential cures for spinal cord injuries, multiple sclerosis, diabetes, Parkinson's disease, cancer, Alzheimer's disease, heart disease, hundreds of rare immune system and genetic disorders and much more.
Scientists see almost infinite value in the use of embryonic stem cell research to understand human development and the growth and treatment of diseases.
Actual cures are many years away, though, since research has not progressed to the point where even one cure has yet been generated by embryonic stem cell research.
Over 100 million Americans suffer from diseases that eventually may be treated more effectively or even cured with embryonic stem cell therapy. Some researchers regard this as the greatest potential for the alleviation of human suffering since the advent of antibiotics.
Many pro-lifers believe that the proper moral and religious course of action is to save existing life through embryonic stem cell therapy.
Some staunch pro-lifers and most pro-life organizations regard the destruction of the blastocyst, which is a laboratory-fertilized human egg, to be the murder of human life. They believe that life begins at conception, and that destruction of this pre-born life is morally unacceptable.
They believe that it is immoral to destroy a few-days-old human embryo, even to save or reduce suffering in existing human life.
Many also believe that insufficient attention been given to explore the potential of adult stem cells, which have already been used to successfully cure many diseases. They also argue that too little attention has been paid to the potential of umbilical cord blood for stem cell research. They also point out that no cures have yet been produced by embryonic stem cell therapy.
At every step of the embryonic stem cell therapy process, decisions are made by scientists, researchers, medical professionals and women who donate eggs...decisions that are fraught with serious ethical and moral implications. Those against embryonic stem cell research argue that funding should be used to greatly expand adult stem research, to circumvent the many moral issues involving the use of human embryos.
Lifting the Ban
Now that President Obama has lifted the federal funding ban for embryonic stem cell research, financial support will soon flow to federal and state agencies to commence the necessary scientific research. The timeline for therapeutic solutions available to all Americans could be years away.
President Obama observed on March 9, 2009, when he lifted the ban:
"Medical miracles do not happen simply by accident. They result from painstaking and costly research, from years of lonely trial and error, much of which never bears fruit, and from a government willing to support that work...
"Ultimately, I cannot guarantee that we will find the treatments and cures we seek. No President can promise that.
"But I can promise that we will seek them -- actively, responsibly, and with the urgency required to make up for lost ground."
- Pros & Cons of the Death Penalty
- Top 10 Must-Reads for Liberals
- New Challenges to the Death Penalty
- The Top 3 Arguments for Gun Control
- What Are U.S. Farm Subsidies?
- 5 Reasons Why Obama Won the 2008 U.S. Presidential Election
- Biography of Elizabeth Warren, Senator and Scholar
- Biography of Elizabeth Vargas, ABC News Journalist
- Congress Members Who Voted Against the 2002 Iraq War
- What Is Gun Ownership Like State by State
- The Obama Administration's Animal Protection Record, 2010-2011
- The 7 Most Liberal Supreme Court Justices in American History
- Top 10 Classic Films With a Social Message
- Biography of Joe Biden, 46th President of the United States
- Alexandria Ocasio-Cortez Biography
- Biography of Ross Perot, Third-Party Presidential Candidate

- Stem Cell Basics
- Stem Cell FAQs
- Stem Cells at UNMC
What are Stem Cells?
Types of Stem Cells
Why are Stem Cells Important?
Can doctors use stem cells to treat patients?
Pros and Cons of Using Stem Cells
What are Stem Cells?
- Stem cells are unspecialized cells that have not yet “decided” what type of adult cell they will be.
- They can self-renew and make two new stem cell
- They can differentiate to make multiple types of cells
- They ultimately amplify by expanding the number of differentiated & mature cells
There are several different types of stem cells produced and maintained in our system throughout life. Depending on the circumstances and life cycle stages, these cells have different properties and functions. There are even stem cells that have been created in the laboratory that can help us learn more about how stem cells differentiate and function. A few key things to remember about stem cells before we venture into more detail:
- Stem Cells are NOT new to science
- The definition is relatively simple (see above)
- Adult Stem Cells (ASC)
- Embryonic Stem Cells (ESC)
- Induced Pluripotent Stem Cells (iPS)
- Stem Cells are important in tissue homeostasis (maintenance), repair and regeneration
- Some Stem Cells (adult) are clinically useful NOW
- Other Stem Cells (ESC, iPS) MAY be clinically useful someday – already useful in basic research
- All Stem Cell types are important in research
- There are both ethical and political issues with the use of some types of stem cells. UNMC continues to work closely with federal and state legislature as well as the International Society for Stem Cell Research (ISSCR) to promote responsible, transparent, and uniform practices that conform to both federal and state guidelines.
Stem cells are the foundation cells for every organ and tissue in our bodies. The highly specialized cells that make up these tissues originally came from an initial pool of stem cells formed shortly after fertilization. Throughout our lives, we continue to rely on stem cells to replace injured tissues and cells that are lost every day, such as those in our skin, hair, blood and the lining of our gut.
Source ISSCR
Stem Cell History
Until recently, scientists primarily worked with two kinds of stem cells from animals and humans: embryonic stem cells and non-embryonic "somatic" or "adult" stem cells. Scientists discovered ways to derive embryonic stem cells from early mouse embryos nearly 30 years ago, in 1981. The detailed study of the biology of mouse stem cells led to the discovery, in 1998, of a method to derive stem cells from human embryos and grow the cells in the laboratory. These cells are called human embryonic stem cells. The embryos used in these studies were created for reproductive purposes through in vitro fertilization procedures. When they were no longer needed for that purpose, they were donated for research with the informed consent of the donor. In 2006, researchers made another breakthrough by identifying conditions that would allow some specialized adult cells to be "reprogrammed" genetically to assume a stem cell-like state. This new type of stem cell is now known as induced pluripotent stem cells (iPSCs).
Types of Stem Cells
Adult Stem Cells (ASCs):
ASCs are undifferentiated cells found living within specific differentiated tissues in our bodies that can renew themselves or generate new cells that can replenish dead or damaged tissue. You may also see the term “somatic stem cell” used to refer to adult stem cells. The term “somatic” refers to non-reproductive cells in the body (eggs or sperm). ASCs are typically scarce in native tissues which have rendered them difficult to study and extract for research purposes.
Resident in most tissues of the human body, discrete populations of ASCs generate cells to replace those that are lost through normal repair, disease, or injury. ASCs are found throughout ones lifetime in tissues such as the umbilical cord, placenta, bone marrow, muscle, brain, fat tissue, skin, gut, etc. The first ASCs were extracted and used for blood production in 1948. This procedure was expanded in 1968 when the first adult bone marrow cells were used in clinical therapies for blood disease.
Studies proving the specificity of developing ASCs are controversial; some showing that ASCs can only generate the cell types of their resident tissue whereas others have shown that ASCs may be able to generate other tissue types than those they reside in. More studies are necessary to confirm the dispute.
Types of Adult Stem Cells
- Hematopoietic Stem Cells (Blood Stem Cells)
- Mesenchymal Stem Cells
- Neural Stem Cells
- Epithelial Stem Cells
- Skin Stem Cells
Embryonic Stem Cells (ESCs):
During days 3-5 following fertilization and prior to implantation, the embryo (at this stage, called a blastocyst), contains an inner cell mass that is capable of generating all the specialized tissues that make up the human body. ESCs are derived from the inner cell mass of an embryo that has been fertilized in vitro and donated for research purposes following informed consent. ESCs are not derived from eggs fertilized in a woman’s body.
These pluripotent stem cells have the potential to become almost any cell type and are only found during the first stages of development. Scientists hope to understand how these cells differentiate during development. As we begin to understand these developmental processes we may be able to apply them to stem cells grown in vitro and potentially regrow cells such as nerve, skin, intestine, liver, etc for transplantation.
Induced Pluripotent Stem Cells (iPSCs)
Induced pluripotent stem cells are stem cells that are created in the laboratory, a happy medium between adult stem cells and embryonic stem cells. iPSCs are created through the introduction of embryonic genes into a somatic cell (a skin cell for example) that cause it to revert back to a “stem cell like” state. These cells, like ESCs are considered pluripotent Discovered in 2007, this method of genetic reprogramming to create embryonic like cells, is novel and needs many more years of research before use in clinical therapies.
Why are Stem Cells Important?
Stem cells are important for living organisms for many reasons. In the 3- to 5-day-old embryo, called a blastocyst, the inner cells give rise to the entire body of the organism, including all of the many specialized cell types and organs such as the heart, lung, skin, sperm, eggs and other tissues. In some adult tissues, such as bone marrow, muscle, and brain, discrete populations of adult stem cells generate replacements for cells that are lost through normal wear and tear, injury, or disease.
Given their unique regenerative abilities, stem cells offer new potentials for treating diseases such as diabetes, and heart disease. However, much work remains to be done in the laboratory and the clinic to understand how to use these cells for cell-based therapies to treat disease, which is also referred to as regenerative or reparative medicine.
Laboratory studies of stem cells enable scientists to learn about the cells’ essential properties and what makes them different from specialized cell types. Scientists are already using stem cells in the laboratory to screen new drugs and to develop model systems to study normal growth and identify the causes of birth defects.
Research on stem cells continues to advance knowledge about how an organism develops from a single cell and how healthy cells replace damaged cells in adult organisms. Stem cell research is one of the most fascinating areas of contemporary biology, but, as with many expanding fields of scientific inquiry, research on stem cells raises scientific questions as rapidly as it generates new discoveries.
Can doctors use stem cells to treat patients?
Some stem cells, such as the adult bone marrow or peripheral blood stem cells, have been used in clinical therapies for over 40 years. Other therapies utilizing stem cells include skin replacement from adult stem cells harvested from hair follicles that have been grown in culture to produce skin grafts. Other clinical trials for neuronal damage/disease have also been conducted using neural stem cells. There were side effects accompanying these studies and further investigation is warranted. Although there is much research to be conducted in the future, these studies give us hope for the future of therapeutics with stem cell research.
Potential Therapies using Stem Cells
Adult Stem Cell Therapies
Bone marrow and peripheral blood stem cell transplants have been utilized for over 40 years as therapy for blood disorders such as leukemia and lymphoma, amongst many others. Scientists have also shown that stem cells reside in most tissues of the body and research continues to learn how to identify, extract, and proliferate these cells for further use in therapy. Scientists hope to yield therapies for diseases such as type I diabetes and repair of heart muscle following heart attack.
Scientists have also shown that there is potential in reprogramming ASCs to cause them to transdifferentiate (turn back into a different cell type than the resident tissue it was replenishing).
Embryonic Stem Cell (ESC) Therapies
There is potential with ESCs to treat certain diseases in the future. Scientists continue to learn how ESCs differentiate and once this method is better understood, the hope is to apply the knowledge to get ESCs to differentiate into the cell of choice that is needed for patient therapy. Diseases that are being targeted with ESC therapy include diabetes, spinal cord injury, muscular dystrophy, heart disease, and vision/hearing loss.
Induced Pluripotent Stem Cell Therapies
Therapies using iPSCs are exciting because somatic cells of the recipient can be reprogrammed to en “ESC like” state. Then mechanisms to differentiate these cells may be applied to generate the cells in need. This is appealing to clinicians because this avoids the issue of histocompatibility and lifelong immunosuppression, which is needed if transplants use donor stem cells.
iPS cells mimic most ESC properties in that they are pluripotent cells, but do not currently carry the ethical baggage of ESC research and use because iPS cells have not been able to be manipulated to grow the outer layer of an embryonic cell required for the development of the cell into a human being.
Pros and Cons of Using Various Stem Cells
- Abundant somatic cells of donor can be used
- Issues of histocompatibility with donor/recipient transplants can be avoided
- Very useful for drug development and developmental studies
| | | | |
| but is not well studied | | therapies to reprogram damaged or diseased cells/tissues | |
| | |||
| |
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How Does Stem Cell Therapy Work?
What are stem cells.
- How the Therapy Works
- What It Treats
Stem cell therapy is a type of regenerative medicine used to treat and study disease. It is used in cancer treatment and to reduce the risk of infection . Researchers are looking for other ways to use stem cells in medical therapies.
This article will cover stem cells, which conditions they treat, and their safety. It will also discuss stem cell therapy's side effects and risks.
Westend61 / Getty Images
Stem cells are unspecialized cells in the body. They can develop into any cell and in some cases can renew themselves an unlimited amount of times.
Stem cells are found in embryos and adult cells . There are two types of stem cells pluripotent and somatic.
Pluripotent stem cells are embryonic stem cells or induced pluripotent stem cells. These cells can become any of the cells in the body. Somatic stem cells, also known as adult stem cells can form tissue or an entire organ.
Stem cell therapy is the use of stem cells as a treatment for a condition.
Stem cells are given to people to replace cells that have been destroyed or have died. In the case of people with cancer , they may be used to help the body regain the ability to produce stem cells after treatment.
In people with multiple myeloma and certain types of leukemia, stem cell therapy is used to destroy cancer cells. This type of therapy is called graft-versus-cancer, the donor's white blood cells (WBCs) are used to destroy the cancerous tumor.
Stem Cell Treatment Cost
Stem cell treatments are very expensive. It is a new therapy and in some cases is still considered experimental. It's important to know how much insurance will cover before undergoing stem cell treatment. Some insurance companies have transplant case managers who can help navigate the process of getting insurance coverage and finding out what expenses may be like.
Learn more: Medicare and Stem Cell Therapy: What's Covered?
What Can Stem Cell Therapy Treat?
Stem cell therapy is a newer treatment that is still being researched. As a result, the Food and Drug Administration (FDA) has only approved it for certain cancers and conditions that affect the blood and immune system.
Conditions stem cell therapy is FDA-approved to treat are:
- Neuroblastoma
- Multiple myeloma
It is also used to reduce the risk of infection after stem cell transplantation in people with blood cancers.
Researchers are studying how stem cells can treat many other conditions than those listed above. There are stem cell clinical trials looking into using the therapy for neurodegenerative diseases like Parkinson's disease , Alzheimer's disease , multiple sclerosis (MS), and amyotrophic lateral sclerosis (ALS).
Companies that claim to use stem cells to treat other conditions are doing so illegally. Products that claim to treat arthritis, joint pain, or fight the signs of aging are not FDA-approved.
Types of Stem Cell Therapy
During stem cell therapy, stem cells are given through an intravenous (IV) line in the vein. The three places where blood-forming stem cells can come from are bone marrow, the umbilical cord, and blood. The transplants can be:
- Autologous : The stem cells are taken from the person who will be receiving the therapy.
- Allogeneic: The stem cells are donated by another person.
- Syngeneic: The stem cells come from an identical twin, if the person has one.
Is Stem Cell Therapy Safe?
While stem cell therapy has many great benefits there are risks to the therapy.
One of the greatest risks is graft-versus-host disease (GVHD). It occurs in one-half to one-third of allogeneic transplant recipients. This is when the body does not recognize the donor's WBCs and attacks them. This can cause problems throughout the body. Treatment involves medications to suppress the immune system to stop the body from attacking the donor cells.
Other potential risks to stem cell therapy include:
- Hepatic veno-occlusive disease
- Cancer relapse
- Post-transplant lymphoproliferative disorder (PTLD)
What Is the Future of Stem Cell Therapy?
The future of stem cell therapy is bright. Researchers are constantly looking to find out how stem cells can treat certain conditions and find new ways to use stem cells to treat and cure many diseases.
Stem cell therapy has been researched for over twenty years to find treatments for conditions like macular degeneration , glaucoma , stroke , and Alzheimer's disease .
Stem cell therapy is a newer medical treatment that uses stem cells to treat conditions like cancer. Some clinics sell stem cell therapy without FDA approval and this places the patient at a higher risk for side effects and poor outcomes. Talk to a trusted healthcare provider about where to find a reliable stem cell therapy provider.
American Cancer Society. How stem cell and bone marrow transplants are used to treat cancer .
National Institutes of Health. Stem cell basics .
Centers for Disease Control and Prevention. Stem cell and exosome products .
National Cancer Institute. Stem cell transplants in cancer treatment .
U.S. Food & Drug Administration. FDA approves cell therapy for patients with blood cancers to reduce risk of infection following stem cell transplantation .
Aly RM. Current state of stem cell-based therapies: an overview . Stem Cell Investig . 2020;7:8. doi:10.21037/sci-2020-001
American Cancer Society. Stem cell or bone marrow transplant side effects .
National Institutes of Health. Putting stem cell-based therapies in context .
By Patty Weasler, RN, BSN Weasler is a Wisconsin-based registered nurse with over a decade of experience in pediatric critical care.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Orthop Rev (Pavia)
- v.14(3); 2022

Stem cells: a comprehensive review of origins and emerging clinical roles in medical practice
Salomon poliwoda.
1 Department of Anesthesiology, Mount Sinai Medical Center
2 LSU Health Science Center Shreveport School of Medicine, Shreveport, LA
Amanda Schaaf
3 University of Arizona College of Medicine-Phoenix, Phoenix, AZ
Abigail Cantwell
Latha ganti.
4 Department of Emergency Medicine, University of Central Florida
Alan D. Kaye
5 Department of Anesthesiology, Louisiana State University Health Sciences Center Shreveport
Luke I. Mosel
Caroline b. carroll, omar viswanath.
6 Department of Anesthesiology, Louisiana State University Health Sciences Center Shreveport, Innovative Pain and Wellness, Creighton University School of Medicine
Stem cells are types of cells that have unique ability to self-renew and to differentiate into more than one cell lineage. They are considered building blocks of tissues and organs. Over recent decades, they have been studied and utilized for repair and regenerative medicine. One way to classify these cells is based on their differentiation capacity. Totipotent stem cells can give rise to any cell of an embryo but also to extra-embryonic tissue as well. Pluripotent stem cells are limited to any of the three embryonic germ layers; however, they cannot differentiate into extra-embryonic tissue. Multipotent stem cells can only differentiate into one germ line tissue. Oligopotent and unipotent stem cells are seen in adult organ tissues that have committed to a cell lineage. Another way to differentiate these cells is based on their origins. Stem cells can be extracted from different sources, including bone marrow, amniotic cells, adipose tissue, umbilical cord, and placental tissue. Stem cells began their role in modern regenerative medicine in the 1950’s with the first bone marrow transplantation occurring in 1956. Stem cell therapies are at present indicated for a range of clinical conditions beyond traditional origins to treat genetic blood diseases and have seen substantial success. In this regard, emerging use for stem cells is their potential to treat pain states and neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease. Stem cells offer hope in neurodegeneration to replace neurons damaged during certain disease states. This review compares stem cells arising from these different sources of origin and include clinical roles for stem cells in modern medical practice.
I. Introduction
Stem cells are a unique population of cells present in all stages of life that possess the ability to self-renew and differentiate into multiple cell lineages. These cells are key mediators in the development of neonates and in restorative processes after injury or disease as they are the source from which specific cell types within differentiated tissues and organs are derived. 1 Within the neonate stage of life stem cells serve to differentiate and proliferate into the multitude of cell types and lineages required for continuing development, while in adults their primary role is regenerative and restorative in nature. 2 Stem cells have unique properties that set them apart from terminally differentiated cells allowing for their specific physiological roles. The ability of stem cells to differentiate into multiple cell types is termed potency, and stem cells can be classified by their potential for differentiation as well as by their origin. Totipotent or omnipotent stem cells can form embryonic tissues and can differentiate into all cell lineages required for an adult. Pluripotent stem cells can differentiate into all three germ layers while multipotent stem cells may only differentiate into one kind of germ line tissue. Oligopotent and unipotent stem cells are the type seen in adult organ tissues that have committed to a cell lineage and can only diversify into cell types within that lineage. 1 Embryonic stem cells are derived from the inner cell mass of a blastocysts and are totipotent. The range of their use is typically restricted due to legal and ethical factors and for this reason mesenchymal stem cells are typically preferred. Mesenchymal stem cells can be isolated from a variety of both neonate and adult tissues but still maintain the ability to differentiate into multiple cell types allowing for their clinical and research utilization without the ethical issues associated with embryonic stem cells. 3
Another key feature of stem cells is their ability to self-renew and proliferate providing a continuous supply of progeny to replace aging or damaged cells. During the developmental phase this proliferation allows for the growth necessary to mature into an adult. After the developmental phase has concluded, this continued proliferation allows for healing and restoration on a cellular level after tissue or organ injury has taken place. 2 These physiological and developmental characteristics make stem cells an integral part in the field of regenerative medicine due to their ability to generate entire tissues and organs from just a handful of progenitor cells.
Stem cells began their role in modern regenerative medicine in the 1950’s with the first bone marrow transplantation occurring in 1956. This breakthrough shed light on the potential treatments possible in the future with further development and refinement of clinical techniques and paved the way for the stem cell therapies that are now available. 4,5 Stem cell therapies are now indicated for a range of clinical conditions beyond traditional origins to treat genetic blood diseases and have seen substantial success where other treatments have fallen short. One emerging use for stem cells is their potential to treat paint states and neurodegenerative diseases such as Parkinson’s and Alzheimer’s disease. Stem cells offer the hope in the setting of neurodegeneration to replace the neurons damaged during the pathogenesis of certain diseases, a goal not achievable utilizing current technologies and methods. 6
Organ bioengineering is yet another a rapidly developing and exciting new application for stem cells with both clinical and research implications. 7 Immunosuppression free organ transplants are now a possibility with the advancement organ manufacturing utilizing the patient’s own cells. 8 This along with the potential for eliminating organ donor waiting lists is an enticing prospect, but many technological developments are necessary before this technology can be implemented in clinical settings on a wide scale. Research has already benefitted greatly from this field because organ like tissues can be grown in lab settings to model disease progression. This offers the potential to develop new treatments while determining their efficacy on a cellular level without risk to patients. 9,10
Currently one of the most prolific clinical uses of stem cells in the field of regenerative medicine is to treat inherited blood diseases. Within these diseases a genetic defect or defects prevents the proper function of cells derived from the hematopoietic stem cell lineage. Treatment includes implantation of genetically normal cells from a healthy donor to serve as a lifelong self-renewing source of normally functioning blood cells. However these treatments are limited by the availability of suitable donors. 11
Stem cells can be derived from multiple sources including adult tissues or neonatal tissues such as the umbilical cord or placenta. Embryonic stem cells have been utilized in the past for research, but ethical concerns have led to them being replaced largely by stem cells derived from other origins. 12 Common tissues from which adult oligopotent and unipotent stem cells are isolated include bone marrow, adipose tissue, and trabecular bone. 13 Bone marrow has traditionally been the most common site from which to extract non neonatal derived stem cells but involves an invasive and painful procedure. Peripheral blood progenitor cells have been utilized to avoid harvesting cells from bone marrow. However, this technique has issues and risks of its own and was initially a less potent source of stem cells. It is also now known that stem cells differ in their proliferative and differentiation potential based on their origin. Cells sourced from umbilical Wharton’s jelly and adipose tissue were found to proliferate significantly more quickly than cells sourced from bone marrow and placental sources. 14,15
A rapidly advancing source of stem cells known as induced pluripotent stem cells (iPSC’s) are now being utilized clinically as well. These iPSC’s are derived from somatic cells that have been reprogrammed back to a pluripotent state utilizing reprogramming factors and require less invasive techniques to harvest in comparison to traditional sources. 16,17 Once returned to a pluripotent state, the cells then undergo a process called directed differentiation in which they are converted into desired cell types. Directed differentiation is achieved by mimicking microenvironments and extracellular signals in vitro in a manner that produces predictable cell types. 18 In the future, this technique could provide a novel form of personalized gene therapy in which oligopotent or unipotent cells are procured from tissue, reprogrammed back to a less differentiated state, and then reintroduced into a different location within the patient. Work is also being done to combine this technique with modern gene editing methods to provide an entirely new subset of therapies. 19 This method of transplantation would greatly reduce the chance for rejection and does not require a suitable donor, as the cells are sourced from the patient being treated. 20,21
II. Bone marrow as a source for stem cells
Stem cells are required by self-renewing tissues to replace damaged and aging cells because of normal biological processes. Both myeloid and lymphoid lineage cells derived from hematopoietic stem cells are relatively short-lived cell types and require a continuous source of newly differentiated replacement cells. 22 Hematopoietic stem cells (HSC’s) are those that reside within the bone marrow and provide a source for the multiple types of blood cells required for normal physiological and immunological functions. These cells inhabit a physiological niche which allows them to undergo the process of asymmetric division. When stem cells divide asymmetrically the progeny of the division includes one identical daughter cell but also results in the production of a differentiated daughter cell. Differentiation of these daughter cell into specialized cell types is guided by certain microenvironments, extrinsic cues, and growth factors that the cell comes in contact with. 23,24 This mechanism allows for bone marrow stem cell numbers to stay relatively constant despite sustained proliferation and differentiation of progeny taking place. 22,25,26
HSC’s are the most studied class of adult tissue derived stem cells and their clinical potential was recognized early in the history of regenerative medicine. At the beginning of the 1960’s, HSC’s were isolated from bone marrow and therapeutic models in mice induced with leukemia were developed in order to show the efficacy of bone marrow derived stem cell treatments. Success in these experiments led to further refinement of techniques and by the 1970’s and 80’s clinical stem cell transplants were a regular occurrence and began to make the impact on blood diseases that we continue to see today. 27,28
Bone marrow has historically been the predominant harvesting site for stem cell collection due to its accessibility, early identification as a source, and lengthy research history. Isolating stem cell from bone marrow involves an invasive and painful surgical procedure and does come with a risk hospitalization or other complications. Patients also report increased post procedural pain and pre-procedural anxiety when compared with other harvesting techniques. 29,30 Bone marrow however has proved to be a denser source of cells than other harvesting methods yielding 18 times more cells than peripheral blood progenitor cell harvesting techniques initially. As technology and methods improved however, it was found that treating patients with a cytokine treatment prior to peripheral blood progenitor cell harvesting mobilized many of the desired cells into the blood stream and drastically increased the efficacy of this technique, making it clinically viable. 31–33 In a double blinded randomized study 40 patients underwent bone marrow and peripheral blood progenitor cell collections and the yield of useable harvested cells were compared. It was found that blood progenitor cell collection yielded significantly more useable stem cells and patients were able to undergo the collection procedure more frequently when compared to the bone marrow harvesting method. 32 This, coupled with the invasiveness and risks associated with harvesting stem cells from bone marrow have increased peripheral blood progenitor cell collections popularity.
Overall, bone marrow as a reservoir of stem cells continues to be a clinical and research necessity related to its well understood and documented history as a source of viable stem cells and track record of efficacy. According to the European Group for Blood and Marrow Transplantation, only one fatal event was recorded stemming from the first 27,770 hematopoietic stem cell transplants sourced from bone marrow during the period of 1993-2005. 34 This undeniable track record of safety coupled with clinicians’ experience performing bone marrow transplant procedures guarantees the continued use of bone marrow as a source of HSC’s for the near future.
III. Amniotic cells as a source for stem cells
Historically, the two most common types of pluripotent stem cells include embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs). 35 However, despite the many research efforts to improve ESC and iPSC technologies, there are still enormous clinical challenges. 35 Two significant issues posed by ESC and iPSC technologies include low survival rate of transplanted cells and tumorigenicity. 35 Recently, researchers have isolated pluripotent stem cells from gestational tissues such as amniotic fluid and the placental membrane. 35 Human amnion-derived stem cells (hADSCs), including amniotic epithelial cells and amniotic mesenchymal cells, are a relatively new stem cell source that have been found to have several advantageous characteristics. 35,36
For background, human amniotic stem cells begin emerging during the second week of gestation when a small cavity forms within the blastocyst and primordial cells lining this cavity are differentiated into amnioblasts. 36 Human amniotic epithelial stem cells (hAESCs) are formed when epiblasts differentiate into amnioblasts, whereas human amniotic mesenchymal stem cells (hAMSCs) are formed when hypoblasts differentiate into amnioblasts. 35,36 This differentiation occurs prior to gastrulation, so amnioblasts do not belong to one of the 3 germ layers, making them theoretically pluripotent. 35–37
Previously, pluripotency and immunomodulation are qualities that have been thought to be mutually exclusive, as pluripotency has traditionally been regarded as a characteristic limited to embryonic stem cells whereas immunomodulation has been a recognized property of mesenchymal stem cells. 36 However, many recent studies have found that these two qualities coexist in hADSCs. 35,36
In recent years, hADSCs, including human amniotic epithelial stem cells (hAESCs) and human amniotic mesenchymal stem cells (hAMSCs) have been attractive cell sources for clinical trials and medical research, and have been shown to have advantages over other stem cells types. 35,37 These advantages include low immunogenicity and high histocompatibility, no tumorigenicity, immunomodulatory effects, and significant paracrine effects. 35 Also, several studies have evaluated the proangiogenic ability of hADSCs. 35 Interestingly, they found that hAMSCs were shown to augment blood perfusion and capillary architecture when transplanted into ischemic limbs of mice, suggesting that hAMSCs stimulate neovascularization. 35,38 Additionally, another advantage is that hADSCs are easier to obtain compared to other stem cell sources, such as bone marrow stem cells (BMSCs). 35
Regarding the low immunogenicity, hADSCs have been shown to have a low expression of major histocompatibility class I antigen ( HLA-ABC ), and no expression of major histocompatibility class II antigen ( HLA-DR ), β2 microglobulin, and HLA-ABC costimulatory molecules, including CD40, CD80 and CD8635. Notably, there have been reports of transplantation of hAMSCs into patients with lysosomal diseases who had no obvious rejection. 35 Moreover, a recent study demonstrated no hemolysis, allergic reactions, or tumor formations in mice who received intravenous hAESCs. 35,39
Additionally, studies have demonstrated that both hAESCs and hAMSCs have great potential to play an important role in regenerative medicine. They both have demonstrated that they can differentiate into several specialized cells, including adipocytes, bone cells, nerve cells, cardiomyocytes, skeletal muscle cells, hepatocytes, hematopoietic cells, endothelial cells, kidney cells, and retinal cells. 35
Multiple preclinical studies have revealed the potential for hADSCs to be used in the treatment of several diseases including premature ovarian failure, diabetes mellitus, inflammatory bowel disease, brain/spine diseases, and more. 35,40,41 For example, one preclinical study investigated the effect of hAMSC-therapy on ovarian function in natural aging ovaries within mice. 40 They found that after the hAMSCs were transplanted into the mice, the hAMSCs significantly improved follicle proliferation and therefore ovarian function. 40 Another study investigated the effect of hAESC-therapy on outcomes after stroke in mice. 41 They found that, administration of hAESCs after acute (within 1.5 hours) stroke in mice reduced brain infarct development, inflammation, and functional deficits. 41 Additionally, they found that after late administration (1-3 days poststroke) of hAESCs, functional recovery in the mice was still improved. 41 Overall, they concluded that administration of hAESCs following a stroke in mice showed a significant neuroprotective effect and facilitated repair and recovery of the brain. 41
Although a number of preclinical studies, like the ones previously described, have shown considerable promise regarding the use of ADSC-therapy, more studies are needed. Future studies can continue to work toward determining if hADSCs are capable of being used for cell replacement and better elucidate the mechanisms by which hADSCs work.
IV. Adipose tissue as a source for stem cells
Although the use of bone marrow stem cells (BMSCs) is now standard, dilemmas regarding harvesting techniques and the potential for low cell yields has driven researchers to search for other mesenchymal stem cell (MSCs) sources. 42 One source that has been investigated is human adipose tissue. 42
After enzymatic digestion of adipose tissue, a heterogenous group of adipocyte precursors are generated within a group of cells called the stromal vascular fraction (SVF). 42 Adipose-derived stem cells (ADSCs) are found in the SVF. 42,43 Studies have demonstrated that ADSCs possess properties typically associated with MSCs, and that they have been found to express several CD markers that MSCs characteristically express. 43 ADSCs are multipotent and have been shown to differentiate into other cells of mesodermal origin, including osteoblasts, chondroblasts, myocytes, tendocytes, and more, upon in vitro induction. 42–45 Additionally, ADSCs have demonstrated in vitro capacity for multi-lineage differentiation into specialized cells, like insulin-secreting cells. 43,46
A significant advantage of ADSCs over BMSCs is how easy they are to harvest. 43,45 White adipose tissue (WAT) contains an abundance of ADSCs. 43 The main stores of WAT in humans are subcutaneous stores in the buttocks, thighs, abdomen and visceral depots. 43 Due to this, ADSCs can be harvested relatively easily by liposuction procedures from these areas of the body. 43,45 Moreover, ADSCs make up as much as 1-2% of the SVF within WAT, sometimes even nearing 30% in some tissues. 43,45 This is a significant difference from the .0001-.0002% stem cells present in bone marrow. 43 Given this difference in stem cell concentration between the sources, there will be more ADSCs per sample of WAT compared to stem cells per bone marrow sample, further demonstrating an easier acquisition of stem cells when using adipose tissue.
Another advantage of ADSCs is their immune privilege status due to a lack of major histocompatibility complex II (MHC II) and costimulatory molecules. 42,43,45,47 Some studies have even demonstrated a higher immunosuppression capacity in ADSCs compared to BMSCs as ADSCs expressed lower levels of human antigen class I (HLA I) antigen. 47 They also have a unique secretome and can produce immunomodulatory, anti-apoptotic, hematopoietic, and angiogenic factors that can help with repair of tissues – characteristics that may support successful transplantations without the need for immunosuppression. 42–45 Moreover, ADSCs have the ability to be reprogrammed to induced pluripotent stem (iPS) cells. 43
The number of ADSC clinical trials has risen over the past decade, and some have shown significant promise. They have demonstrated abilities to differentiate into multiple cell lines in a reproducible manner and be safe for both autogenetic and allogeneic transplantations. 45 Several recent studies have demonstrated that ADSC-therapy may potentially be useful in the treatment of several conditions, including diabetes mellitus, Crohn’s disease, multiple sclerosis, fistulas, arthritis, ischemic pathologies, cardiac injury, spinal injury, bone injuries and more. 44–48
One clinical trial conducted in 2013 investigated the therapeutic effect of co-infusion of autologous adipose-derived differentiated insulin-secreting stem cells and hematopoietic stem cells (HSCs) on patients with insulin-dependent diabetes mellitus. 46 Ten patients were followed over an average of about thirty-two months, and they found that all the patients had improvement in C-peptide, HbA1c, blood sugar status, and exogenous insulin requirement. 46 Notably, there were no unpleasant side effects of the treatment and all ten patients had rehabilitated to a normal, unrestricted diet and lifestyle. 46
In another 4-patient clinical trial in which ADSCs were used to heal fistulas in patients with Crohn’s disease, full healing occurred in 6 out of the 8 fistulas with partial healing in the remaining two. 44 No complications were observed in the patients 12 months following the trial. 44 Although these results are promising, the mechanism by which the healing took place remains unclear. When considering the properties of ADSCs, there are a number of factors that could have played a role in the healing, such as the result of paracrine expression of angiogenic and/or anti-apoptotic factors, stem cell differentiation, and/or local immunosuppression. 44
Other exciting studies have demonstrated a use of ADSCs in the treatment of osteoarthritis (OA). One meta-analysis compared the use of ADSCs and BMSCs in the treatment of osteoarthritis. 47 This meta-analysis included 14 studies comprising 461 original patient records. 47 Overall, the comparison between treatment of OA didn’t show a significant difference in the disease severity score change rate between patients treated with ADSCs and those treated with BMSCs. 47 However, there was significantly more variability in the outcomes of those treated with BMSCs with the highest change rate being 79.65% in one study and the lowest being 22.57% in another study. 47 Given this, ADSCs may represent a more stable cell source for the treatment of OA. 47 Although this study is specific to OA treatment, it is worth acknowledging the possibility that ADSCs may also represent a more stable cell source for treatment of other diseases as well.
Though recent ADSC research, as described above, has been promising, unfortunately reproducible in vivo studies are still lacking in both quality and quantity. 42 Therefore, further studies are necessary prior to progression to routine patient administration. 42
V. Umbilical Cord as a source for stem cells
Umbilical Cord stem cells can be drawn from a variety of locations including umbilical cord blood, umbilical cord perivascular cells, umbilical vein endothelial cells, umbilical lining, chorion, and amnion. Umbilical cord blood can be drawn with minimal risk to the donor, and it has been used since 1988 as a source for hematopoietic stem cells. 49 When compared to stem cells obtained from bone marrow, umbilical cord derived stem cells are much more readily available. With a birth rate of more than a 100 million people per year globally, there is a lot of opportunity to use umbilical cord blood as a source for stem cells.
The process of extracting the blood is very simple and involves a venipuncture followed by drainage into a sterile anti-coagulant-filled blood bag. It is then cryopreserved and stored in liquid nitrogen. There are quite a few benefits to utilizing umbilical cord stem cells rather than stem cells drawn from adults. One of the biggest benefits is that the cells are more immature which means that there is a lower chance of rejection after implantation in a host and would lead to decreased rates of graft-versus-host disease. They also can differentiate into a very wide variety of tissues. For example, when compared with bone marrow stem cells or mobilized peripheral blood, umbilical cord blood stem cells have a greater repopulating ability. 50 Cord blood derived CD34+ cells have very potent hematopoietic abilities, and this is attributed to the immaturity of the stem cells relative to adult derived cells. Studies have been done that analyze long term survival of children with hematologic disorders who were transplanted with umbilical cord blood from a sibling donor. These studied revealed the same or better survival in the children that received the umbilical cord blood relative to those that got transplantation from bone marrow cells. Furthermore, rates of relapse were the same for both umbilical cord blood and bone marrow transplant. 51
One of the unique features of stem cells taken from umbilical cord blood is the potential to differentiate into a wide variety of cell types. There are three different kinds of stem cells that can be found in the umbilical cord blood which include hematopoietic, mesenchymal, and embryonic-like stem cells. Not only can these cell types all renew themselves, but they can differentiate into many different mature cell types through a complex number of signaling pathways. This means that these cells could give rise to not only hematopoietic cells but bone, neural and endothelial cells. There are studies taking place currently to see if umbilical cord blood derived stem cells can be utilized for cardiomyogenic purposes. Several studies have showed the ability to transform umbilical cord blood mesenchymal stem cells into cells of cardiomyogenic lineage utilizing activations of Wnt signaling pathways. 52 Studies are also being conducted on the potential of neurological applications. If successful, this could help diseases such as cerebral palsy, stroke, spinal cord injury and neurodegenerative diseases. Given these cell’s ability to differentiate into tissues from the mesoderm, endoderm and ectoderm, they could be utilized for neurological issues in place of embryonic stem cells that are currently extremely controversial. 53 There are currently studies involving in vitro work, pre-clinical animal studies, and patient clinical trials, all for the application of stem cells in neurological applications. There is big potential for the use of umbilical blood stem cells in the future of regenerative medicine.
VI. Placental Tissue as a Source for Stem Cells
Placental tissue contains both stem cells and epithelial cells that can differentiate into a wide variety of tissue types which include adipogenic, myogenic, hepatogenic, osteogenic, cardiac, endothelial, pancreatic, pulmonary, and neurological. Placental cells can differentiate in to all these different kinds of tissues due to lineages originating from different parts of the placenta such as the hematopoietic cells that come from the chorion, allantois, and yolk sac while the mesenchymal lineages come from the chorion and the amnion. 54 It can be helpful to think of human fetal placental cells as being divided into four different groups: amniotic epithelial cells, amniotic mesenchymal stromal cells, chorionic mesenchymal stromal cells and chorionic trophoblast cells. 54
Human amniotic epithelial cells (hAECs) can be obtained from the amnion membrane where they are then enzymatically digested to be separated from the chorion. When cultured under certain settings hAECs have been found to be able to produce neuronal cells that synthesize acetylcholine, norepinephrine as well as dopamine. 55,56 This ability would mean they have potential for regenerative purposes in diseases such as Parkinson’s Disease, multiple sclerosis, and spinal cord injury. There is also research being done to utilize hAECs for ophthalmological purposes, lung fibrosis, liver disease, metabolic diseases, and familial hypercholesterolemia. Once cultured, hAECs have been shown to produce both albumin and alpha-fetoprotein as well as showing ability to store glycogen. Furthermore, they have been found to metabolize ammonia and testosterone. In more recent studies conducted in mouse models, these cells have been found to have therapeutic efficacy after transplantation for cirrhosis. 57
Mesenchymal stem cells are in many different tissues such as the bone marrow, umbilical cord blood, adipose tissue, Wharton’s jelly, amniotic fluid, lungs, muscle and the placenta. Placental mesenchymal stromal cells specifically originate from the extraembryonic mesoderm. Human amniotic mesenchymal stromal cells (hAMSCs) and chorionic mesenchymal stromal cells (hCMSCs) have both been found to have very low levels of HLA-A,B,C. This means that they have immune privileged profiles for potential transplantation. 58,59 Placental derived mesenchymal stem cells have been shown to have expression of CD29, CD44, CD105 and CD166 which is the same as adipose derived mesenchymal stem cells. These markers have been shown to have osteogenic differentiating abilities. 57 An interesting element of placental mesenchymal stem cells is that their properties differ depending on the gestational age of the placenta. When cells are harvested at lower gestational ages, they show faster generation doubling times, better proliferative abilities, wider differentiation potential and more phenotypic stability than cells harvested from placental tissue that is considered to be at term. 60 Furthermore, they have great potential to be used clinically. Placental mesenchymal stromal cells have been studied for use in treating acute graft-versus-host disease that was refractory to steroid treatment. Studies have shown that the 1-year survival rates in patients treated with placenta derived stromal cells were 73% while retrospective control only showed 6% survival. 61 Placenta derived MSCs have also been found to aid in wound healing and could potentially be used to aid with certain inherited skin conditions such as epidermolysis bullosa. 62
Stem cells are diverse in their differentiation capacity as well as their source of origin. As we can see from this review, there are similarities and differences when these cells are extracted from different sources. Research has shown initial promise in neurodegenerative diseases such as Alzheimer’s and Parkinson’s Disease. It has also shown to be beneficial in the areas of musculoskeletal regenerative medicine and other pain states. Organ bioengineering for transplantation is another potential benefit that stem cells may offer. For these reasons, extensive research is still needed in this area of medicine to pave the way for new developing therapy modalities.
Conflict of Interest of each author
Dedications.
This review is dedicated to Dr. Justine C. Goldberg MD
Funding Statement
- 1. Kolios G, Moodley Y. Introduction to Stem Cells and Regenerative Medicine. Respiration . 2013;85(1):3-10. doi:10.1159/000345615 [ PubMed ] [ Google Scholar ]
- 2. Dekoninck S, Blanpain C. Stem cell dynamics, migration and plasticity during wound healing. Nat Cell Biol . 2019;21(1):18-24. doi:10.1038/s41556-018-0237-6 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. Ding DC, Shyu WC, Lin SZ. Mesenchymal stem cells. Cell Transplant . 2011;20(1):5-14. doi:10.3727/096368910x [ PubMed ] [ Google Scholar ]
- 4. Simpson E, Dazzi F. Bone Marrow Transplantation. Front Immunol . 2019;10(1246). doi:10.3389/fimmu.2019.01246 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Dameshek W. Bone Marrow Transplantation—A Present-Day Challenge. Blood . 1957;12(4):321-323. doi:10.1182/blood.v12.4.321.321 [ PubMed ] [ Google Scholar ]
- 6. Song CG, Zhang YZ, Wu HN, et al. Stem cells: a promising candidate to treat neurological disorders. Neural Regen Res . 2018;13(7):1294. doi:10.4103/1673-5374.235085 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Urits I, Capuco A, Sharma M, et al. Stem Cell Therapies for Treatment of Discogenic Low Back Pain: a Comprehensive Review. Curr Pain Headache Rep . 2019;23(9). doi:10.1007/s11916-019-0804-y [ PubMed ] [ Google Scholar ]
- 8. Edgar L, Pu T, Porter B, et al. Regenerative medicine, organ bioengineering and transplantation. British Journal of Surgery . 2020;107(7):793-800. doi:10.1002/bjs.11686 [ PubMed ] [ Google Scholar ]
- 9. Welman T, Michel S, Segaren N, Shanmugarajah K. Bioengineering for Organ Transplantation: Progress and Challenges. Bioengineered . 2015;6(5):257-261. doi:10.1080/21655979.2015.1081320 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Edgar L, Pu T, Porter B, et al. Regenerative medicine, organ bioengineering and transplantation. British Journal of Surgery . 2020;107(7):793-800. doi:10.1002/bjs.11686 [ PubMed ] [ Google Scholar ]
- 11. Morgan RA, Gray D, Lomova A, Kohn DB. Hematopoietic Stem Cell Gene Therapy: Progress and Lessons Learned. Cell Stem Cell . 2017;21(5):574-590. doi:10.1016/j.stem.2017.10.010 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Lo B, Parham L. Ethical Issues in Stem Cell Research. Endocrine Reviews . 2009;30(3):204-213. doi:10.1210/er.2008-0031 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Hass R, Kasper C, Böhm S, Jacobs R. Different populations and sources of human mesenchymal stem cells (MSC): A comparison of adult and neonatal tissue-derived MSC. Cell Communication and Signaling . 2011;9(1):1-14. doi:10.1186/1478-811X-9-12/FIGURES/3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Fong CY, Subramanian A, Biswas A, et al. Derivation efficiency, cell proliferation, freeze–thaw survival, stem-cell properties and differentiation of human Wharton’s jelly stem cells. Reproductive BioMedicine Online . 2010;21(3):391-401. doi:10.1016/j.rbmo.2010.04.010 [ PubMed ] [ Google Scholar ]
- 15. Li X, Bai J, Ji X, Li R, Xuan Y, Wang Y. Comprehensive characterization of four different populations of human mesenchymal stem cells as regards their immune properties, proliferation and differentiation. Int J Mol Med . 2014;34(3):695-704. doi:10.3892/ijmm.2014.1821 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Dakhore S, Nayer B, Hasegawa K. Human Pluripotent Stem Cell Culture: Current Status, Challenges, and Advancement. Stem Cells International . 2018;2018:1-17. doi:10.1155/2018/7396905 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Liu G, David BT, Trawczynski M, Fessler RG. Advances in Pluripotent Stem Cells: History, Mechanisms, Technologies, and Applications. Stem Cell Rev and Rep . 2019;16(1):3-32. doi:10.1007/s12015-019-09935-x [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Zakrzewski W, Dobrzyński M, Szymonowicz M, Rybak Z. Stem cells: Past, present, and future. Stem Cell Res Ther . 2019;10(1). doi:10.1186/s13287-019-1165-5 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Benati D, Miselli F, Cocchiarella F, et al. CRISPR/Cas9-Mediated In Situ Correction of LAMB3 Gene in Keratinocytes Derived from a Junctional Epidermolysis Bullosa Patient. Molecular Therapy . 2018;26(11):2592-2603. doi:10.1016/j.ymthe.2018.07.024 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Karagiannis P, Takahashi K, Saito M, et al. Induced pluripotent stem cells and their use in human models of disease and development. Physiological Reviews . 2019;99(1):79-114. doi:10.1152/PHYSREV.00039.2017/ASSET/IMAGES/LARGE/Z9J0041828840008.JPEG [ PubMed ] [ Google Scholar ]
- 21. Rowe RG, Daley GQ. Induced pluripotent stem cells in disease modelling and drug discovery. Nat Rev Genet . 2019;20(7):377-388. doi:10.1038/s41576-019-0100-z [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Seita J, Weissman IL. Hematopoietic stem cell: self-renewal versus differentiation. Wiley Interdisciplinary Reviews: Systems Biology and Medicine . 2010;2(6):640-653. doi:10.1002/wsbm.86 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Kaur-Bollinger P, Gotze KS, Oostendorp RAJ. Role of secreted factors in the regulation of hematopoietic stem cells by the bone marrow microenvironment. Front Biosci . 2012;17(3):876-891. doi:10.2741/3962 [ PubMed ] [ Google Scholar ]
- 24. Comazzetto S, Shen B, Morrison SJ. Niches that regulate stem cells and hematopoiesis in adult bone marrow. Dev Cell . 2021;56(13):1848-1860. doi:10.1016/j.devcel.2021.05.018 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Adams GB, Scadden DT. The hematopoietic stem cell in its place. Nat Immunol . 2006;7(4):333-337. doi:10.1038/ni1331 [ PubMed ] [ Google Scholar ]
- 26. Venkei ZG, Yamashita YM. Emerging mechanisms of asymmetric stem cell division. Journal of Cell Biology . 2018;217(11):3785-3795. doi:10.1083/jcb.201807037 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Weissman IL, Shizuru JA. The origins of the identification and isolation of hematopoietic stem cells, and their capability to induce donor-specific transplantation tolerance and treat autoimmune diseases. Blood . 2008;112(9):3543-3553. doi:10.1182/blood-2008-08-078220 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Rossi L, Challen GA, Sirin O, Lin KKY, Goodell MA. Hematopoietic Stem Cell Characterization and Isolation. Methods Mol Biol . 2011;750(47):47-59. doi:10.1007/978-1-61779-145-1_3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Siddiq S, Pamphilon D, Brunskill S, Doree C, Hyde C, Stanworth S. Bone marrow harvest versus peripheral stem cell collection for haemopoietic stem cell donation in healthy donors. Cochrane Database of Systematic Reviews . 2009;(1). doi:10.1002/14651858.CD006406.PUB2/INFORMATION/EN [ PubMed ]
- 30. Auquier P, Macquart-Moulin G, Moatti J, et al. Comparison of anxiety, pain and discomfort in two procedures of hematopoietic stem cell collection: leukacytapheresis and bone marrow harvest. Bone Marrow Transplantation . 1995;16(4):541-547. https://europepmc.org/article/med/8528170 [ PubMed ] [ Google Scholar ]
- 31. Cutler C, Antin JH. Peripheral Blood Stem Cells for Allogeneic Transplantation: A Review. Stem Cells . 2001;19(2):108-117. doi:10.1634/stemcells.19-2-108 [ PubMed ] [ Google Scholar ]
- 32. Singhal S, Powles R, Kulkarni S, et al. Comparison of marrow and blood cell yields from the same donors in a double-blind, randomized study of allogeneic marrow vs blood stem cell transplantation. Bone Marrow Transplant . 2000;25(5):501-505. doi:10.1038/sj.bmt.1702173 [ PubMed ] [ Google Scholar ]
- 33. Körbling M, Anderlini P. Peripheral blood stem cell versus bone marrow allotransplantation: does the source of hematopoietic stem cells matter? Blood . 2001;98(10):2900-2908. doi:10.1182/blood.v98.10.2900 [ PubMed ] [ Google Scholar ]
- 34. Bosi A, Bartolozzi B. Safety of Bone Marrow Stem Cell Donation: A Review. Transplantation Proceedings . 2010;42(6):2192-2194. doi:10.1016/j.transproceed.2010.05.029 [ PubMed ] [ Google Scholar ]
- 35. Liu QW, Huang QM, Wu HY, et al. Characteristics and Therapeutic Potential of Human Amnion-Derived Stem Cells. Int J Mol Sci . 2021;22(2):1-33. doi:10.3390/ijms22020970 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 36. Miki T. Stem cell characteristics and the therapeutic potential of amniotic epithelial cells. Am J Reprod Immunol . 2018;80(4):e13003. doi:10.1111/aji.13003 [ PubMed ] [ Google Scholar ]
- 37. Qiu C, Ge Z, Cui W, Yu L, Li J. Human Amniotic Epithelial Stem Cells: A Promising Seed Cell for Clinical Applications. IJMS . 2020;21(20):1-26. doi:10.3390/ijms21207730 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 38. Kim SW, Zhang HZ, Kim CE, An HS, Kim JM, Kim MH. Amniotic mesenchymal stem cells have robust angiogenic properties and are effective in treating hindlimb ischaemia. Cardiovasc Res . 2012;93(3):525-534. doi:10.1093/cvr/cvr328 [ PubMed ] [ Google Scholar ]
- 39. Yang P jie, Yuan W xin, Liu J, et al. Biological characterization of human amniotic epithelial cells in a serum-free system and their safety evaluation. Acta Pharmacol Sin . 2018;39(8):1305-1316. doi:10.1038/aps.2018.22 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Ding C, Zou Q, Wang F, et al. Human amniotic mesenchymal stem cells improve ovarian function in natural aging through secreting hepatocyte growth factor and epidermal growth factor. Stem Cell Research and Therapy . 2018;9(1):1-11. doi:10.1186/S13287-018-0781-9/FIGURES/7 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Evans MA, Lim R, Kim HA, et al. Acute or Delayed Systemic Administration of Human Amnion Epithelial Cells Improves Outcomes in Experimental Stroke. Stroke . 2018;49(3):700-709. doi:10.1161/strokeaha.117.019136 [ PubMed ] [ Google Scholar ]
- 42. Johal KS, Lees VC, Reid AJ. Adipose-derived stem cells: selecting for translational success. Regenerative Med . 2015;10(1):79-96. doi:10.2217/rme.14.72 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Ong WK, Sugii S. Adipose-derived stem cells: fatty potentials for therapy. Int J Biochem Cell Biol . 2013;45(6):1083-1086. doi:10.1016/j.biocel.2013.02.013 [ PubMed ] [ Google Scholar ]
- 44. Fraser JK, Wulur I, Alfonso Z, Hedrick MH. Fat tissue: an underappreciated source of stem cells for biotechnology. Trends Biotechnol . 2006;24(4):150-154. doi:10.1016/j.tibtech.2006.01.010 [ PubMed ] [ Google Scholar ]
- 45. Mazini L, Rochette L, Amine M, Malka G. Regenerative Capacity of Adipose Derived Stem Cells (ADSCs), Comparison with Mesenchymal Stem Cells (MSCs). IJMS . 2019;20(10):2523. doi:10.3390/ijms20102523 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 46. Dave SD, Vanikar AV, Trivedi HL, Thakkar UG, Gopal SC, Chandra T. Novel therapy for insulin-dependent diabetes mellitus: infusion of in vitro-generated insulin-secreting cells. Clin Exp Med . 2015;15(1):41-45. doi:10.1007/s10238-013-0266-1 [ PubMed ] [ Google Scholar ]
- 47. Zhou W, Lin J, Zhao K, et al. Single-Cell Profiles and Clinically Useful Properties of Human Mesenchymal Stem Cells of Adipose and Bone Marrow Origin. Am J Sports Med . 2019;47(7):1722-1733. doi:10.1177/0363546519848678 [ PubMed ] [ Google Scholar ]
- 48. Stepien A, Dabrowska NL, Maciagowska M, et al. Clinical Application of Autologous Adipose Stem Cells in Patients with Multiple Sclerosis: Preliminary Results. Mediators of Inflammation . 2016;2016:1-5. doi:10.1155/2016/5302120 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Gluckman E, Broxmeyer HE, Auerbach AD, et al. Hematopoietic reconstitution in a patient with Fanconi’s anemia by means of umbilical-cord blood from an HLA-identical sibling. N Engl J Med . 1989;321(17):1174-1178. doi:10.1056/nejm198910263211707 [ PubMed ] [ Google Scholar ]
- 50. Jaing TH. Umbilical cord blood: A trustworthy source of multipotent stem cells for regenerative medicine. Cell Transplant . 2014;23(4-5):493-496. doi:10.3727/096368914x678300 [ PubMed ] [ Google Scholar ]
- 51. Bojanic I, Golubic Cepulic B. Umbilical cord blood as a source of stem cells. PubMed. https://pubmed.ncbi.nlm.nih.gov/16933834/ [ PubMed ]
- 52. Roura S, Pujal JM, Gálvez-Montón C, Bayes-Genis A. Impact of umbilical cord blood-derived mesenchymal stem cells on cardiovascular research. BioMed Research International . 2015;2015:1-6. doi:10.1155/2015/975302 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. Harris DT. Cord blood stem cells: a review of potential neurological applications. Stem Cell Rev . 2008;4(4):269-274. doi:10.1007/s12015-008-9039-8 [ PubMed ] [ Google Scholar ]
- 54. Antoniadou E, David AL. Placental stem cells. Best Practice & Research Clinical Obstetrics & Gynaecology . 2016;31:13-29. doi:10.1016/j.bpobgyn.2015.08.014 [ PubMed ] [ Google Scholar ]
- 55. Kakishita K, Elwan MA, Nakao N, Itakura T, Sakuragawa N. Human amniotic epithelial cells produce dopamine and survive after implantation into the striatum of a rat model of Parkinson’s disease: A potential source of donor for transplantation therapy. Experimental Neurology . 2000;165(1):27-34. doi:10.1006/exnr.2000.7449 [ PubMed ] [ Google Scholar ]
- 56. Elwan M, Sakuragawa N. Evidence for synthesis and release of catecholamines by human amniotic epithelial cells. NeuroReport . Published online 1997. Accessed May 20, 2022. https://journals.lww.com/neuroreport/Abstract/1997/11100/Evidence_for_synthesis_and_release_of.4.aspx [ PubMed ]
- 57. Mohammadi Z, Afshari JT, Keramati MR, et al. Differentiation of adipocytes and osteocytes from human adipose and placental mesenchymal stem cells. Iranian Journal of Basic Medical Sciences . 2015;18(3):259. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. Lin JS, Zhou L, Sagayaraj A, et al. Hepatic differentiation of human amniotic epithelial cells and in vivo therapeutic effect on animal model of cirrhosis. J Gastroenterol Hepatol . 2015;30(11):1673-1682. doi:10.1111/jgh.12991 [ PubMed ] [ Google Scholar ]
- 59. Marongiu F, Gramignoli R, Dorko K, et al. Hepatic differentiation of amniotic epithelial cells. Hepatology . 2011;53(5):1719-1729. doi:10.1002/hep.24255 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 60. Sung HJ, Hong SC, Yoo JH, et al. Stemness evaluation of mesenchymal stem cells from placentas according to developmental stage: Comparison to those from adult bone marrow. J Korean Med Sci . 2010;25(10):1418-1426. doi:10.3346/jkms.2010.25.10.1418 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Ringden O, Solders M, Erkers T, et al. Placenta-Derived Decidual Stromal Cells for Graft-Versus-Host Disease, Hemorrhaging, and Toxicity after Allogeneic Hematopoietic Stem Cell Transplantation. Biology of Blood and Marrow Transplantation . 2015;21(2):S149. doi:10.1016/j.bbmt.2014.11.209 [ Google Scholar ]
- 62. Nevala-Plagemann C, Lee C, Tolar J. Placenta-based therapies for the treatment of epidermolysis bullosa. Cytotherapy . 2015;17(6):786-795. doi:10.1016/j.jcyt.2015.03.006 [ PMC free article ] [ PubMed ] [ Google Scholar ]
14 Advantages and Disadvantages of Embryonic Stem Cell Research
Embryonic stem cells are derived from embryos that develop from eggs that were created through the in vitro fertilization process. These eggs are then donated for research purposes with the informed consent of their donors. Researchers do not derive embryonic stem cells from eggs that are fertilized in a woman’s body.
Women do not have abortions to harvest their embryonic stem cells, nor do any providers sell fetal tissue for these cell lines to develop.
Human embryonic stem cells come from a transference of cells from a preimplantation-stage embryo in a laboratory culture dish. It is mixed with culture medium, allowing the cells to divide, and then spread over the surface of this dish. These cells can then develop into all three derivatives of the primary germ layers, making it possible for them to eventually turn into one of the over 200 different cell types that are found in the human body.
It is not possible to save the embryo when these cells are harvested from it, which ends the potential future viability of human life. That is where a majority of the embryonic stem cell research pros and cons focus on when discussing this subject. How you personally define human life will usually dictate which side of the debate you support.
List of the Pros of Embryonic Stem Cell Research
1. The embryonic stem cells are harvested 5-7 days after conception. Adult stem cells do not provide the same benefits as embryonic ones from a therapeutic standpoint. They fall short in their viability to treat genetic diseases. That’s because the same disease found in the adult body can be present in their stem cells. When the harvesting takes place, it occurs during the first week after conception. At this stage, the embryo has not yet developed to a stage where a personal identity can be assigned to it, nor can it live outside of a specialized environment. It is essentially a mass of cells.
2. Researchers use the embryonic stem cells from discarded embryos. The IVF process which creates embryos for transplantation in the first place are often discarded without a second though. Reporting by The Telegraph in 2012 found that over 1.7 million human embryos were discarded during or after the conception process. Between 1991-2012, there were 3.5 million human embryos created, but only roughly 235,000 successful implantation procedures. About 840, 000 were put into cold storage, while just 2,000 were stored for donation.
Approximately 6,000 embryos during this two-decade period were set aside for medical research. Compared to the 1.4 million that were implanted as a way to start a pregnancy, where 1 in 6 failed, the issue of morality is more complex than the black-and-white world that some people create.
3. Embryonic stem cells can be harvested ethically from almost any perspective. New technologies make it possible for doctors to harvest remaining embryonic stem cells from the umbilical cord after a child is born. Even if parents decide to store cord blood instead of make a donation, the product can still contain a line of embryonic stem cells that could be useful for research purposes. Since the umbilical cord doesn’t stay attached to the child, nor does the cord blood get reabsorbed into the mother or the baby, the only way to unethically take this resource is to do it without asking.
4. Pain is not felt during the embryonic stem cell procedure. When researchers destroy an embryo as they harvest the line of stem cells that develops, there is no pain experienced by this cell group. Researchers believe that a fetus doesn’t have the concept of pain developed until around the 20th week of gestation. Most of the embryos that are used for this process have been frozen anyway, kept in storage because there is no intention to use the cells to hopefully create a pregnancy one day anyway.
Fetal tissues wouldn’t supply the embryonic stem cells anyway because at that stage of development, they have already turned into what they are going to be. That makes it virtually impossible to study their qualities at the level where they would be medically beneficial.
5. No embryonic stem cells are taken without consent. IVF doctors don’t take fertilized eggs away from women or couples with an evil laugh, thinking about all the dastardly ways they can manipulate embryonic stem cells for personal gain. People don’t steal frozen embryos, encourage abortions, or harvest the tissues from a growing fetus to serve a medical or political agenda. Every embryonic stem cell line comes from the consent of its donor. No research on those cells will take place unless there is explicit consent offered by those involved.
6. We do not know the full potential of this new field of medical science. We are still in the early stages of research to determine the full potential value of embryonic stem cells as a treatment option for some individuals. As the University of Michigan notes, it may lead to more effective treatments for serious human ailments. The future discoveries in this field could alleviate the suffering for millions of people around the world. Spinal cord injuries, Parkinson’s disease, Alzheimer’s disease, and juvenile diabetes are just a few of the conditions which could be improved if medical studies are given time and funding to reach a conclusion.
7. Treatments using embryonic stem cells have already produced results. Early embryonic stem cell treatments through the use of cord blood therapies have already produce positive outcomes for roughly 10,000 people. These treatments offer new ways to find a cure for 70+ different diseases with this option. Kids that have an immunodeficiency disorder and receive this form of treatment see a treatment success rate of 90% today – and that figure continues to grow.
List of the Cons of Embryonic Stem Cell Research
1. It destroys the future potential of human life. Whether you feel that life begins at conception, at some stage in the womb, or after birth, everyone can agree on the idea that an embryo represent the future potential of life. We can get lost in the semantics of how life begins to support how we feel, but the bottom line here is that the termination of an embryo stops the future potential for that group of cells. Using it for research purposes, even with the consent of the mother or couple involved, means you’re trading future human potentiality for current potentiality. Is that really a justifiable action?
2. The number of successful treatment outcomes is relatively minor. There are significant barriers in place when looking at the potential of an embryonic stem cell treatment. There are unstable gene expressions which occur when this method is used, along with the formation of tumors, and some people even see a failure in the cell’s ability to activate to a specific purpose. Until these challenges are addressed in clinical settings, the full potential of this treatment can never be realized. Does it make sense to continue harvesting cells from embryos if the failure rate remains high?
3. People can still reject embryonic stem cell treatments. The human body naturally rejects the items that are not part of its regular genetic makeup through its immune system response. That is why the people who go through an organ transplant procedure receive anti-rejection medication that slows or stops this response. Even if the embryonic stems cells go through their regular activation method, there is still the potential of rejection present.
Even if an embryonic clone of an individual could be created to product exact cells which mimic the body’s genetic makeup, there would still be a risk of rejection because of the genetic duplication process.
4. It can be argued that embryos do meet the definition of “life” from a scientific view. There are currently three specific guidelines in the framework of the definition of life as we think of it when encountered on our planet or perhaps elsewhere in our solar system or galaxy one day.
• There must be a capacity for growth that produces functional activity. • It must offer some type of reproduction capability during one stage of its existence. • There must be a change which occurs over the lifetime of the cells in question that happens before death.
5. People fund research activities with their taxes. Federal law in the United States prohibits taxpayer funding to be used for abortion services unless specific exceptions apply. What many people do not realize is that over $500 million in research funding has been given to this medical field since 1996 because even though portions of this field were outlawed, all existing stem cell lines currently being worked on at the time were grandfathered into the legislative process.
The Supreme Court affirmed the federal stem cell research could continue in 2013 despite a long-running appeal that such an action is a violation of the Dickey-Wicker Act that prohibits the destruction of an embryo.
6. It is a time-consuming process to create viable embryonic stem cells. For the stem cells to become a viable research tool, they must undergo several months of development in strict laboratory conditions before they are valuable in any way. Then there is the cost involved with the process as well. The 2017 estimated federal funding for all categories of stem cell research was $1.58 billion. Embryonic stem cell research received $347 million, while umbilical cord blood or placenta-based stem cells received $34 million.
7. Many of the stem cell lines under research are two decades’ old. Most of the approved embryonic stem cell research lines that are worked on in the United States were created on or before August 2001. Those lines were found to be contaminated with animal proteins, which seems to have prevented any of them from being created as a model to treat human disease. Only 16 out of the 70 lines approved by the federal government remain because a majority of them were inadequately characterized. These cells also came from an Israeli clinic, which means they do not incorporate the levels of racial and ethnic diversity that genuine research requires.
The pros and cons of embryonic stem cells look at the potential of what this new field of medical research could provide compared to the harm it may cause. There are deeper issues here that go beyond “we can” or “we shouldn’t.” Since a majority of embryos are thrown away, shouldn’t there be outrage over that fact from the pro-life movement? And since 1 in 6 attempted implants fails, is there not more to consider here than the intentional actions of research? By taking a look at all sides of this issue, the debate tends to become a complex set of moral judgments made on the individual level instead of a generic right or wrong answer to determine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 06 August 2022
Stem cell-based therapy for human diseases
- Duc M. Hoang ORCID: orcid.org/0000-0001-5444-561X 1 ,
- Phuong T. Pham 2 ,
- Trung Q. Bach 1 ,
- Anh T. L. Ngo 2 ,
- Quyen T. Nguyen 1 ,
- Trang T. K. Phan 1 ,
- Giang H. Nguyen 1 ,
- Phuong T. T. Le 1 ,
- Van T. Hoang 1 ,
- Nicholas R. Forsyth 3 ,
- Michael Heke 4 &
- Liem Thanh Nguyen 1
Signal Transduction and Targeted Therapy volume 7 , Article number: 272 ( 2022 ) Cite this article
82k Accesses
327 Citations
66 Altmetric
Metrics details
- Mesenchymal stem cells
- Stem-cell research
Recent advancements in stem cell technology open a new door for patients suffering from diseases and disorders that have yet to be treated. Stem cell-based therapy, including human pluripotent stem cells (hPSCs) and multipotent mesenchymal stem cells (MSCs), has recently emerged as a key player in regenerative medicine. hPSCs are defined as self-renewable cell types conferring the ability to differentiate into various cellular phenotypes of the human body, including three germ layers. MSCs are multipotent progenitor cells possessing self-renewal ability (limited in vitro) and differentiation potential into mesenchymal lineages, according to the International Society for Cell and Gene Therapy (ISCT). This review provides an update on recent clinical applications using either hPSCs or MSCs derived from bone marrow (BM), adipose tissue (AT), or the umbilical cord (UC) for the treatment of human diseases, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and cardiovascular conditions. Moreover, we discuss our own clinical trial experiences on targeted therapies using MSCs in a clinical setting, and we propose and discuss the MSC tissue origin concept and how MSC origin may contribute to the role of MSCs in downstream applications, with the ultimate objective of facilitating translational research in regenerative medicine into clinical applications. The mechanisms discussed here support the proposed hypothesis that BM-MSCs are potentially good candidates for brain and spinal cord injury treatment, AT-MSCs are potentially good candidates for reproductive disorder treatment and skin regeneration, and UC-MSCs are potentially good candidates for pulmonary disease and acute respiratory distress syndrome treatment.
Similar content being viewed by others

Mesenchymal stem cell perspective: cell biology to clinical progress

Mesenchymal stem cell-derived extracellular vesicles for immunomodulation and regeneration: a next generation therapeutic tool?

Next-generation stem cells — ushering in a new era of cell-based therapies
Introduction.
The successful approval of cancer immunotherapies in the US and mesenchymal stem cell (MSC)-based therapies in Europe have turned the wheel of regenerative medicine to become prominent treatment modalities. 1 , 2 , 3 Cell-based therapy, especially stem cells, provides new hope for patients suffering from incurable diseases where treatment approaches focus on management of the disease not treat it. Stem cell-based therapy is an important branch of regenerative medicine with the ultimate goal of enhancing the body repair machinery via stimulation, modulation, and regulation of the endogenous stem cell population and/or replenishing the cell pool toward tissue homeostasis and regeneration. 4 Since the stem cell definition was introduced with their unique properties of self-renewal and differentiation, they have been subjected to numerous basic research and clinical studies and are defined as potential therapeutic agents. As the main agenda of regenerative medicine is related to tissue regeneration and cellular replacement and to achieve these targets, different types of stem cells have been used, including human pluripotent stem cells (hPSCs), multipotent stem cells and progenitor cells. 5 However, the emergence of private and unproven clinics that claim the effectiveness of stem cell therapy as “magic cells” has raised highly publicized concerns about the safety of stem cell therapy. The most notable case involved the injection of a cell population derived from fractionated lipoaspirate into the eyes of three patients diagnosed with macular degeneration, resulting in the loss of vision for these patients. 6 Thus, as regenerative medicine continues to progress and evolve and to clear the myth of the “magic” cells, this review provides a brief overview of stem cell-based therapy for the treatment of human diseases.
Stem cell therapy is a novel therapeutic approach that utilizes the unique properties of stem cells, including self-renewal and differentiation, to regenerate damaged cells and tissues in the human body or replace these cells with new, healthy and fully functional cells by delivering exogenous cells into a patient. 7 Stem cells for cell-based therapy can be of (1) autologous, also known as self-to-self therapy, an approach using the patient’s own cells, and (2) allogeneic sources, which use cells from a healthy donor for the treatment. 8 The term “stem cell” were first used by the eminent German biologist Ernst Haeckel to describe the properties of fertilized egg to give rise to all cells of the organism in 1868. 9 The history of stem cell therapy started in 1888, when the definition of stem cell was first coined by two German zoologists Theodor Heinrich Boveri and Valentin Haecker, 9 who set out to identify the distinct cell population in the embryo capable of differentiating to more specialized cells (Fig. 1a ). In 1902, studies carried out by the histologist Franz Ernst Christian Neumann, who was working on bone marrow research, and Alexander Alexandrowitsch Maximov demonstrated the presence of common progenitor cells that give rise to mature blood cells, a process also known as haematopoiesis. 10 From this study, Maximov proposed the concept of polyblasts, which later were named stem cells based on their proliferation and differentiation by Ernst Haeckel. 11 Maximov described a hematopoietic population presented in the bone marrow. In 1939, the first case report described the transplantation of human bone marrow for a patient diagnosed with aplastic anemia. Twenty years later, in 1958, the first stem cell transplantation was performed by the French oncologist George Mathe to treat six nuclear researchers who were accidentally exposed to radioactive substances using bone marrow transplantation. 12 Another study by George Mathe in 1963 shed light on the scientific community, as he successfully conducted bone marrow transplantation in a patient with leukemia. The first allogeneic hematopoietic stem cell transplantation (HSCT) was pioneered by Dr. E. Donnall Thomas in 1957. 13 In this initial study, all six patients died, and only two patients showed evidence of transient engraftment due to the unknown quantities and potential hazards of bone marrow transplantation at that time. In 1969, Dr. E. Donnall Thomas conducted the first bone marrow transplantation in the US, although the success of the allogeneic treatment remained exclusive. In 1972, the year marked the discovery of cyclosporine (the immune suppressive drug), 14 the first successes of allogeneic transplantation for aplastic anemia and acute myeloid leukemia were reported in a 16-year-old girl. 15 From the 1960s to the 1970s, series of works conducted by Friendenstein and coworkers on bone marrow aspirates demonstrated the relationship between osteogenic differentiation and a minor subpopulation of cells derived from bone marrow. 16 These cells were later proven to be distinguishable from the hematopoietic population and to be able to proliferate rapidly as adherent cells in tissue culture vessels. Another important breakthrough from Friendenstein’s team was the discovery that these cells could form the colony-forming unit when bone marrow was seeded as suspension culture following by differentiation into osteoblasts, adipocytes, and chondrocytes, suggesting that these cells confer the ability to proliferate and differentiate into different cell types. 17 In 1991, combined with the discovery of human embryonic stem cells (hESCs), which will be discussed in the next section, the term “mesenchymal stem cells”, previously known as stromal stem cells or “osteogenic” stem cells, was first coined in Caplan and widely used to date. 18 Starting with bone marrow transplantation 60 years ago, the journey of stem cell therapy has developed throughout the years to become a novel therapeutic agent of regenerative medicine to treat numerous incurable diseases, which will be reviewed and discussed in this review, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and cardiovascular conditions).
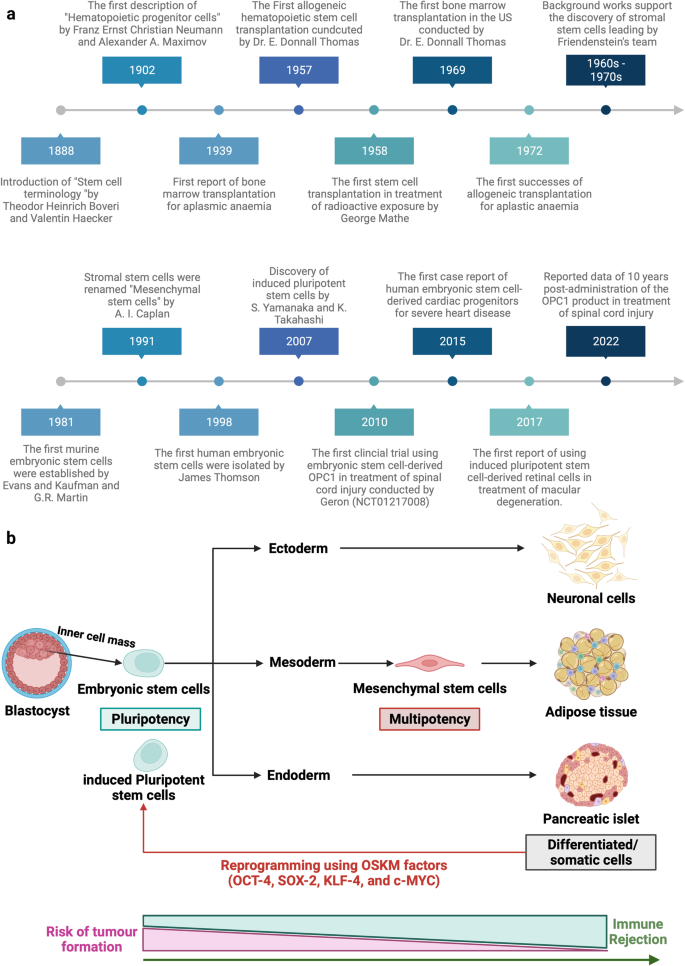
Stem cell-based therapy: the history and cell source. a The timeline of major discoveries and advances in basic research and clinical applications of stem cell-based therapy. The term “stem cells” was first described in 1888, setting the first milestone in regenerative medicine. The hematopoietic progenitor cells were first discovered in 1902. In 1939, the first bone marrow transplantation was conducted in the treatment of aplasmic anemia. Since then, the translation of basic research to preclinical studies to clinical trials has driven the development of stem cell-based therapy by many discoveries and milestones. The isolations of “mesenchymal stem cells” in 1991 following by the discovery of human pluripotent stem cells have recently contributed to the progress of stem cell-based therapy in the treatment of human diseases. b Schematic of the different cell sources that can be used in stem cell-based therapy. (1) Human pluripotent stem cells, including embryonic stem cells (derived from inner cell mass of blastocyst) and induced pluripotent stem cells confer the ability to proliferate indefinitely in vitro and differentiate into numerous cell types of the human body, including three germ layers. (2) Mesenchymal stem cells are multipotent stem cells derived from mesoderm possessing self-renewal ability (limited in vitro) and differentiation potential into mesenchymal lineages. The differentiated/somatic cells can be reprogrammed back to the pluripotent stage using OSKM factors to generate induced pluripotent stem cells. It is important to note that stem cells show a relatively higher risk of tumor formation and lower risk of immune rejection (in the case of mesenchymal stem cells) when compared to that of somatic cells. The figure was created with BioRender.com
In this review, we described the different types of stem cell-based therapies (Fig. 1b ), including hPSCs and MSCs, and provided an overview of their definition, history, and outstanding clinical applications. In addition, we further created the first literature portfolio for the “targeted therapy” of MSCs based on their origin, delineating their different tissue origins and downstream applications with an in-depth discussion of their mechanism of action. Finally, we provide our perspective on why the tissue origin of MSCs could contribute greatly to their downstream applications as a proposed hypothesis that needs to be proven or disproven in the future to further enhance the safety and effectiveness of stem cell-based therapy.
Stem cell-based therapy: an overview of current clinical applications
Cardiovascular diseases.
The clinical applications of stem cell-based therapies for heart diseases have been recently discussed comprehensively in the reviews 19 , 20 and therefore will be elaborated in this study as the focus discussions related to hPSCs and MSCs in the following sections. In general, the safety profiles of stem cell-based therapies are supported by a large body of preclinical and clinical studies, especially adult stem cell therapy (such as MSC-based products). However, clinical trials have not yet yielded data supporting the efficacy of the treatment, as numerous studies have shown paradoxical results and no statistically significant differences in infarct size, cardiac function, or clinical outcomes, even in phase III trials. 21 The results of a meta-analysis showed that stem cells derived from different sources did not exhibit any therapeutic effects on the improvement of myocardial contractility, cardiovascular remodeling, or clinical outcomes. 22 The disappointing results obtained from the clinical trials thus far could be explained by the fact that the administered cells may exert their therapeutic effects via an immune modulation rather than regenerative function. Thus, well-designed, randomized and placebo-controlled phase III trials with appropriate cell-preparation methods, patient selection, follow-up schedules and suitable clinical measurements need to be conducted to determine the efficacy of the treatments. In addition, concerns related to optimum cell source and dose, delivery route and timing of administration, cell distribution post administration and the mechanism of action also need to be addressed. In the following section of this review, we present clinical trials related to MSC-based therapy in cardiovascular disease with the aim of discussing the contradictory results of these trials and analyzing the potential challenges underlying the current approaches.
Digestive system diseases
Gastrointestinal diseases are among the most diagnosed conditions in the developed world, altering the life of one-third of individuals in Western countries. The gastrointestinal tract is protected from adverse substances in the gut environment by a single layer of epithelial cells that are known to have great regenerative ability in response to injuries and normal cell turnover. 23 These epithelial cells have a rapid turnover rate of every 2–7 days under normal conditions and even more rapidly following tissue damage and inflammation. This rapid proliferation ability is possible owing to the presence of a specific stem cell population that is strictly compartmentalized in the intestinal crypts. 24 The gastrointestinal tract is highly vulnerable to damage, tissue inflammation and diseases once the degradation of the mucosal lining layer occurs. The exposure of intestinal stem cells to the surrounding environment of the gut might result in the direct destruction of the stem cell layer or disruption of intestinal functions and lead to overt clinical symptoms. 25 In addition, the accumulation of stem cell defects as well as the presence of chronic inflammation and stress also contributes to the reduction of intestinal stem cell quality.
In terms of digestive disorders, Crohn’s disease (CD) and ulcerative colitis are the two major forms of inflammatory bowel disease (IBD) and represent a significant burden on the healthcare system. The former is a chronic, uncontrolled inflammatory condition of the intestinal mucosa characterized by segmental transmural mucosal inflammation and granulomatous changes. 26 The latter is a chronic inflammatory bowel disease affecting the colon and rectum, characterized by mucosal inflammation initiating in the rectum and extending proximal to the colon in a continuous fashion. 27 Cellular therapy in the treatment of CD can be divided into haematopoietic stem cell-based therapy and MSC-based therapy. The indication and recommendation of using HSCs for the treatment of IBD were proposed in 1995 by an international committee with four important criteria: (1) refractory to immunosuppressive treatment; (2) persistence of the disease conditions indicated via endoscopy, colonoscopy or magnetic resonance enterography; (3) patients who underwent an imminent surgical procedure with a high risk of short bowel syndromes or refractory colonic disease; and (4) patients who refused to treat persistent perianal lesions using coloproctectomy with a definitive stroma implant. 28 In the standard operation procedure, patents’ HSCs were recruited using cyclophosphamide, which is associated with granulocyte colony-stimulating factor (G-CSF), at two different administered concentrations (4 g/m 2 and 2 g/m 2 ). Recently, it was reported that high doses of cyclophosphamide do not improve the number of recruited HSCs but increase the risk of cardiac and bladder toxicity. An interest in using HSCTs in CD originated from case reports that autologous HSCTs can induce sustained disease remission in some 29 , 30 but not all patients 31 , 32 , 33 with CD. The first phase I trial was conducted in Chicago and recruited 12 patients with active moderate to severe CD refractory to conventional therapies. Eleven of 12 patients demonstrated sustained remission after a median follow-up of 18.5 months, and one patient developed recurrence of active CD. 31 The ASTIC trial (the Autologous Stem Cell Transplantation International Crohn Disease) was the first randomized clinical trial with the largest cohort of patients undergoing HSCT for refractory CD in 2015. 34 The early report of the trial showed no statistically significant improvement in clinical outcomes of mobilization and autologous HSCT compared with mobilization followed by conventional therapy. In addition, the procedure was associated with significant toxicity, leading to the suggestion that HSCT for patients with refractory CD should not be widespread. Interestingly, by using conventional assessments for clinical trials for CD, a group reassessed the outcomes of patients enrolled in the ASTIC trial showing clinical and endoscopic benefits, although a high number of adverse events were also detected. 35 A recent systematic review evaluated 18 human studies including 360 patients diagnosed with CD and showed that eleven studies confirmed the improvement of Crohn’s disease activity index between HSCT groups compared to the control group. 36 Towards the cell sources, HSCs are the better sources as they afforded more stable outcomes when compared to that of MSC-based therapy. 37 Moreover, autologous stem cells were better than their allogeneic counterparts. 36 The safety of stem cell-based therapy in the treatment of CD has attracted our attention, as the risk of infection in patients with CD was relatively higher than that in those undergoing administration to treat cancer or other diseases. During the stem cell mobilization process, patient immunity is significantly compromised, leading to a high risk of infection, and requires carefully nursed and suitable antibiotic treatment to reduce the development of adverse events. Taken together, stem cell-based therapy for digestive disease reduced inflammation and improved the patient’s quality of life as well as bowel functions, although the high risk of adverse events needs to be carefully monitored to further improve patient safety and treatment outcomes.
Liver diseases
The liver is the largest vital organ in the human body and performs essential biological functions, including detoxification of the organism, metabolism, supporting digestion, vitamin storage, and other functions. 38 The disruption of liver homeostasis and function might lead to the development of pathological conditions such as liver failure, cirrhosis, cancer, alcoholic liver disease, nonalcoholic fatty liver disease (NAFLD), and autoimmune liver disease (ALD). Orthotropic liver transplantation is the only effective treatment for severe liver diseases, but the number of available and suitable donor organs is very limited. Currently, stem cell-based therapies in the treatment of liver disease are associated with HSCs, MSCs, hPSCs, and liver progenitor cells.
Liver failure is a critical condition characterized by severe liver dysfunctions or decompensation caused by numerous factors with a relatively high mortality rate. Stem cell-based therapy is a novel alternative approach in the treatment of liver failure, as it is believed to participate in the enhancement of liver regeneration and recovery. The results of a meta-analysis including four randomized controlled trials and six nonrandomized controlled trials in the treatment of acute-on-chronic liver failure (ACLF) demonstrated that clinical outcomes of stem cell therapy were achieved in the short term, requiring multiple doses of stem cells to prolong the therapeutic effects. 39 , 40 Interestingly, although MSC-based therapies improved liver functions, including the model of end-stage liver disease score, albumin level, total bilirubin, and coagulation, beneficial effects on survival rate and aminotransferase level were not observed. 41 A randomized controlled trial illustrated the improvement of liver functions and reduction of severe infections in patients with hepatitis B virus-related ACLF receiving allogeneic bone marrow-derived MSCs (BM-MSCs) via peripheral infusion. 42 HSCs from peripheral blood after the G-CSF mobilization process were used in a phase I clinical trial and exhibited an improvement in serum bilirubin and albumin in patients with chronic liver failure without any specific adverse events related to the administration. 43 Taken together, an overview of stem cell-based therapy in the treatment of liver failure indicates the potential therapeutic effects on liver functions with a strong safety profile, although larger randomized controlled trials are still needed to assure the conclusions.
Liver cirrhosis is one of the major causes of morbidity and mortality worldwide and is characterized by diffuse nodular regeneration with dense fibrotic septa and subsequent parenchymal extinction leading to the collapse of liver vascular structure. 44 In fact, liver cirrhosis is considered the end-stage of liver disease that eventually leads to death unless liver transplantation is performed. Stem cell-based therapy, especially MSCs, currently emerges as a potential treatment with encouraging results for treating liver cirrhosis. In a clinical trial using umbilical cord-derived MSCs (UC-MSCs), 45 chronic hepatitis B patients with decompensated liver cirrhosis were divided into two groups: the MSC group ( n = 30) and the control group ( n = 15). 45 The results showed a significant reduction in ascites volume in the MSC group compared with the control. Liver function was also significantly improved in the MSC groups, as indicated by the increase in serum albumin concentration, reduction in total serum bilirubin levels, and decrease in the sodium model for end-stage liver disease score. 45 Similar results were also reported from a phase II trial using BM-MSCs in 25 patients with HCV-induced liver cirrhosis. 46 Consistent with these studies, three other clinical trials targeting liver cirrhosis caused by hepatitis B and alcoholic cirrhosis were conducted and confirmed that MSC administration enhanced and recovered liver functions. 47 , 48 , 49 With the large cohort study as the clinical trial conducted by Fang, the safety and potential therapeutic effects of MSC-based therapies could be further strengthened and confirmed the feasibility of the treatment in virus-related liver cirrhosis. 49 In terms of delivery route, a randomized controlled phase 2 trial suggested that systemic delivery of BM-MSCs does not show therapeutic effects on patients with liver cirrhosis. 50 MSCs are not the only cell source for liver cirrhosis. Recently, an open-label clinical trial conducted in 19 children with liver cirrhosis due to biliary atresia after the Kasai operation illustrated the safety and feasibility of the approach by showing the improvement of liver function after bone marrow mononuclear cell (BMNC) administration assessed by biochemical tests and pediatric end-stage liver disease (PELD) scores. 51 Another study using BMNCs in 32 decompensated liver cirrhosis patients illustrated the safety and effectiveness of BMNC administration in comparison with the control group. 52 Recently, a long-term analysis of patients receiving peripheral blood-derived stem cells indicated a significant improvement in the long-term survival rate when compared to the control group, and the risk of hepatocellular carcinoma formation did not increase. 53 CD133 + HSC infusion was performed in a multicentre, open, randomized controlled phase 2 trial in patients with liver cirrhosis; the results did not support the improvement of liver conditions, and cirrhosis persisted. 54 Notably, these results are in line with a previous randomized controlled study, which also reported that G-CSF and bone marrow-derived stem cells delivered via the hepatic artery did not introduce therapeutic potential as expected. 55 Thus, stem cell-based therapy for liver cirrhosis is still in its immature stage and requires larger trials with well-designed experiments to confirm the efficacy of the treatment.
Nonalcoholic fatty liver disease (NAFLD) is the most common medical condition caused by genetic and lifestyle factors and results in a severe liver condition and increased cardiovascular risk. 56 NAFLD is the hidden enemy, as most patients are asymptomatic for a long time, and their routine life is unaffected. Thus, the detection, identification, and management of NAFLD conditions are challenging tasks, as patients diagnosed with NAFLD often develop nonalcoholic steatohepatitis, cirrhosis, and hepatocellular carcinoma. 57 Although preclinical studies have shown that stem cell administration could enhance liver function in NAFLD models, a limited number of clinical trials were performed in human subjects. Recently, a multi-institutional clinical trial using freshly isolated autologous adipose tissue-derived regenerative cells was performed in Japan to treat seven NAFLD patients. 58 The results illustrated the improvement in the serum albumin level of six patients and prothrombin activity of five patients, and no treatment-related adverse events or severe adverse events were observed. This study illustrates the therapeutic potential of stem cell-based therapy in the treatment of NAFLD.
Autoimmune liver disease (ALD) is a severe liver condition affecting children and adults worldwide, with a female predominance. 59 The condition occurs in genetically predisposed patients when a stimulator, such as virus infection, leads to a T-cell-mediated autoimmune response directed against liver autoantigens. As a result, patients with ALD might develop liver cirrhosis, hepatocellular carcinoma, and, in severe cases, death. To date, HSCT and bone marrow transplantation are the two common stem cell-based therapies exhibiting therapeutic potential for ALD in clinical trials. An interesting report illustrated that haploidentical HSCTs could cure ALD in patients with sickle cells. 60 This report is particularly important, as it illustrates the potential therapeutic approach of using haploidentical HSCTs to treat patients with both sickle cells and ALD. Another case report described a 19-year-old man with a 4-year history of ALD who developed acute lymphoblastic leukemia and required allogeneic bone marrow transplantation from this wholesome brother. 61 The clinical data showed that immunosuppressive therapy for transplantation generated ALD remission in the patient. 62 However, the data also provided valid information related to the sustained remission and the normalization of ASGPR-specific suppressor-inducer T-cell activity following bone marrow transplantation, suggesting that these suppressor functions originated from donor T cells. 61 Thus, it was suggested that if standard immunosuppressive treatment fails, alternative cellular immunotherapy would be a viable option for patients with ALD. Primary biliary cholangitis (PBC), usually known as primary biliary cirrhosis, is a type of ALD characterized by a slow, progressive destruction of small bile ducts of the liver leading to the formation of cirrhosis and accumulation of bile and other toxins in the liver. A pilot, single-arm trial from China recruited seven patents with PBC who had a suboptimal response to ursodeoxycholic acid (UDCA) treatment. 63 These patients received UDCA treatment in combination with three rounds of allogeneic UC-MSCs at 4-week intervals with a dose of 0.5 × 10 6 cells/kg of patient body weight via the peripheral vein. No treatment-related adverse events or severe adverse events were observed throughout the course of the study. The clinical data indicated significant improvement in liver function, including reduction of serum ALP and gamma-glutamyltransferase (GGT) at 48 weeks post administration. The common symptoms of PBC, including fatigue, pruritus, and hypogastric ascites volume, were also reduced, supporting the feasibility of MSC-based therapy in the treatment of PBC, although major limitations of the study were nonrandomized, no control group and small sample size. Another study was conducted in China with ten PBC patients who underwent incompetent UDCA treatment for more than 1 year. These patients received a range of 3–5 allogeneic BM-MSCs/kg body weight by intravenous infusion. 64 Although these early studies have several limitations, such as small sample size, nonrandomization, and no control group, their preliminary data related to safety and efficacy herald the prospects and support the feasibility of stem cell-based therapy in the treatment of ALD.
In summary, the current number of trials for liver disease using stem cell-based therapy has provided fundamental data supporting the safety and potential therapeutic effects in various liver diseases. Unfortunately, due to the small number of trials, several obstacles need to be overcome to prove the effectiveness of the treatments, including (1) stem cell source and dose, (2) administration route, (3) time of intervention, and (4) clinical assessments during the follow-up period. Only by addressing these challenges we will be able to prove, facilitate and promote stem cell-based therapy as a mainstream treatment for liver diseases.
Arthritis is a general term describing cartilage conditions that cause pain and inflammation of the joints. Osteoarthritis (OA) is the most common form of arthritis caused by persistent degeneration and poor recovery of articular cartilage. 65 OA affects one or several diarthrodial joints, such as small joints at the hand and large joints at the knee and hips, leading to severe pain and subsequent reduction in the mobility of patients. There are two types of OA: (1) primary OA or idiopathic OA and secondary OA caused by causative factors such as trauma, surgery, and abnormal joint development at birth. 66 As conventional treatments for OA are not consistent in their effectiveness and might cause unbearable pain as well as long-term rehabilitation (in the case of joint replacement), there is a need for a more reliable, less painful, and curative therapy targeting the root of OA. 67 Thus, stem cell therapy has recently emerged as an alternative approach for OA and has drawn great attention in the regenerative field.
The administration of HSCs has been proven to reduce bone lesions, enhance bone regeneration and stimulate the vascularization process in degenerative cartilage. Attempts were made to evaluate the efficacy of peripheral blood stem cells in ten OA patients by three intraarticular injections. Post-administration analysis indicated a reduction in the WOMAC index with a significant reduction in all parameters. All patients completed 6-min walk tests with an increase of more than 54 meters. MRI analysis indicated an improvement in cartilage thickness, suggesting that cartilage degeneration was reduced post administration. To further enhance the therapeutic potential of HSCT, CD34 + stem cells were proposed to be used in combination with the rehabilitation algorithm, which included three stages: preoperative, hospitalization and outpatient periods. 68 Currently, a large wave of studies has been directed to MSC-based therapy for the treatment of OA due to their immunoregulatory functions and anti-inflammatory characteristics. MSCs have been used as the main cell source in several multiple and small-scale trials, proving their safety profile and potential effectiveness in alleviating pain, reducing cartilage degeneration, and enhancing the regeneration of cartilage structure and morphology in some cases. However, the best source of MSCs, whether from bone marrow, adipose tissue, or umbilical cord, for the management of OA is still a great question to be answered. A systematic review investigating over sixty-one of 3172 articles with approximately 2390 OA patients supported the positive effects of MSC-based therapy on OA patients, although the study also pointed out the fact that these therapeutic potentials were based on limited high-quality evidence and long-term follow-up. 69 Moreover, the study found no obvious evidence supporting the most effective source of MSCs for treating OA. Another systematic review covering 36 clinical trials, of which 14 studies were randomized trials, provides an interesting view in terms of the efficacy of autologous MSC-based therapy in the treatment of OA. 70 In terms of BM-MSCs, 14 clinical trials reported the clinical outcomes at the 1-year follow-up, in which 57% of trials reported clinical outcomes that were significantly better in comparison with the control group. However, strength analysis of the data set showed that outcomes from six trials were low, whereas the outcomes of the remaining eight trials were extremely low. Moreover, the positive evidence obtained from MRI analysis was low to very low strength of evidence after 1-year post administration. 70 Similar results were also found in the outcome analysis of autologous adipose tissue-derived MSCs (AT-MSCs). Thus, the review indicated low quality of evidence for the therapeutic potential of MSC therapy on clinical outcomes and MRI analysis. The low quality of clinical outcomes could be explained by the differences in interventions (including cell sources, cell doses, and administration routes), combination treatments (with hyaluronic acid, 71 peripheral blood plasma, 72 etc.), control treatments and clinical outcome measurements between randomized clinical trials. 73 In addition, the data of the systematic analysis could not prove the better source of MSCs for OA treatment. Taken together, although stem cell-based therapy has been shown to be safe and feasible in the management of OA, the authors support the notion that stem cell-based therapy could be considered an alternative treatment for OA when first-line treatments, such as education, exercise, and body weight management, have failed.
Cancer treatment
Stem cell therapy in the treatment of cancer is a sensitive term and needs to be used and discussed with caution. Clinicians and researchers should protect patients with cancer from expensive and potentially dangerous or ineffective stem cell-based therapy and patients without a cancer diagnosis from the risk of malignancy development. In general, unproven stem cell clinics employed three cell-based therapies for cancer management, including autologous HSCTs, stromal vascular fraction (SVF), and multipotent stem cells, such as MSCs. Allogeneic HSCTs confer the ability to generate donor lymphocytes that contribute to the suppression and regression of hematological malignancies and select solid tumors, a specific condition known as “graft-versus-tumor effects”. 74 However, stem cell clinics provide allogeneic cell-based therapy for the treatment of solid malignancies despite limited scientific evidence supporting the safety and efficacy of the treatment. High-quality evidence from the Cochrane library shows that marrow transplantation via autologous HSCTs in combination with high-dose chemotherapy does not improve the overall survival of women with metastatic breast cancer. In addition, a study including more than 41,000 breast cancer patients demonstrated no significant difference in survival benefits between patients who received HSCTs following high-dose chemotherapy and patients who underwent conventional treatment. 75 Thus, the use of autologous T-cell transplants as monotherapy and advertising stem cell-based therapies as if they are medically approved or preferred treatment of solid tumors is considered untrue statements and needs to be alerted to cancer patients. 76
Over the past decades, many preclinical studies have demonstrated the potential of MSC-based therapy in cancer treatment due to their unique properties. They confer the ability to migrate toward damaged sites via inherent tropism controlled by growth factors, chemokines, and cytokines. MSCs express specific C–X–C chemokine receptor type 4 (CXCR4) and other chemokine receptors (including CCR1, CCR2, CCR4, CCR7, etc.) that are essential to respond to the surrounding signals. 77 In addition, specific adherent proteins, including CD49d, CD44, CD54, CD102, and CD106, are also expressed on the MSC surface, allowing them to attach, rotate, migrate, and penetrate the blood vessel lumen to infiltrate the damaged tissue. 78 Similar to damaged tissues, tumors secrete a wide range of chemoattractant that also attract MSC migration via the CXCL12/CXCR4 axis. Previous studies also found that MSC migration toward the cancer site is tightly controlled by diffusible cytokines such as interleukin 8 (IL-8) and growth factors including transforming growth factor-beta 1 (TGF-β1), 79 platelet-derived growth factor (PDGF), 80 fibroblast growth factor 2 (FGF-2), 81 vascular endothelial growth factor (VEGF), 81 and extracellular matrix molecules such as matrix metalloproteinase-2 (MMP-2). 82 Once MSCs migrate successfully to cancerous tissue, accumulating evidence demonstrates the interaction between MSCs and cancer cells to exhibit their protumour and antitumour effects, which are the major concerns of MSC-based therapy. MSCs are well-known for their regenerative effects that regulate tissue repair and recovery. This unique ability is also attributed to the protumour functions of these cells. A previous study reported that breast cancer cells induce MSC secretion of chemokine (C–C motif) ligand 5 (CCL-5), which regulates the tumor invasion process. 83 , 84 Other studies also found that MSCs secrete a wide range of growth factors (VEGF, basic FGF, HGF, PDGF, etc.) that inhibits apoptosis of cancer cells. 85 Moreover, MSCs also respond to signals released from cancer cells, such as TGF-β, 86 to transform into cancer-associated fibroblasts, a specific cell type residing within the tumor microenvironment capable of promoting tumorigenesis. 87 Although MSCs have been proven to be involved in protumour activities, they also have potent tumor suppression abilities that have been used to develop cancer treatments. It has been suggested that MSCs exhibit their tumor inhibitory effects by inhibiting the Wnt and AKT signaling pathways, 88 reducing the angiogenesis process, 89 stimulating inflammatory cell infiltration, 90 and inducing tumor cell cycle arrest and apoptosis. 91 To date, the exact functions of MSCs in both protumour and antitumor activities are still a controversial issue across the stem cell field. Other approaches exploit gene editing and tissue engineering to convert MSCs into “a Trojan horse” that could exhibit antitumor functions. In addition, MSCs can also be modified to express specific anticancer miRNAs exhibiting tumor-suppressive behaviors. 92 However, genetically modified MSCs are still underdeveloped and require intensive investigation in the clinical setting.
To date, ~25 clinical trials have been registered on ClinicalTrials.gov aimed at using MSCs as a therapeutic treatment for cancer. 93 These trials are mostly phase 1 and 2 studies focusing on evaluating the safety and efficacy of the treatment. Studies exploiting MSC-based therapy have combined MSCs with an oncolytic virus approach. Oncolytic viruses are specific types of viruses that can be genetically engineered or naturally present, conferring the ability to selectively infect cancer cells and kill them without damaging the surrounding healthy cells. 94 A completed phase I/II study using BM-MSCs infected with the oncolytic adenovirus ICOVIR5 in the treatment of metastatic and refractory solid tumors in children and adult patients demonstrated the safety of the treatment and provided preliminary data supporting their therapeutic potential. 95 The same group also reported a complete disappearance of all signs of cancer in response to MSC-based therapy in one pediatric case three years post administration. 96 A reported study in 2019 claimed that adipose-derived MSCs infected with vaccinia virus have the potential to eradicate resistant tumor cells via the combination of potent virus amplification and senitization of the tumor cells to virus infection. 97 However, in a recently published review, a valid question was posed regarding the 2019 study that “do these reported data merit inclusion in the publication record when they were collected by such groups using a dubious therapeutic that was eventually confiscated by US Marshals?” 76
Taken together, cancer research and therapy have entered an innovative and fascinating era with advancements in traditional therapies such as chemotherapy, radiotherapy, and surgery on one hand and stem cell-based therapy on the other hand. Although stem cell-based therapy has been considered a novel and attractive therapeutic approach for cancer treatment, it has been hampered by contradictory results describing the protumour and antitumour effects in preclinical studies. Despite this contradictory reality, the use of stem cell-based therapy, especially MSCs, offers new hope to cancer patients by providing a new and more effective tool in personalized medicine. The authors support the use of MSC-based therapy as a Trojan horse to deliver specific anticancer functions toward cancer cells to suppress their proliferation, eradicate cancer cells, or limit the vascularization process of cancerous tissue to improve the clinical safety and efficacy of the treatment.
Human pluripotent stem cell-based therapy: a growing giant
The discovery of hPSCs, including human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs), has revolutionized stem cell research and cell-based therapy. 98 hESCs were first isolated from blastocyst-stage embryos in 1998, 99 followed by breakthrough reprogramming research that converted somatic cells into hiPSCs using just four genetic factors. 100 , 101 Methods have been developed to maintain these cells long-term in vitro and initiate their differentiation into a wide variety of cell types, opening a new era in regenerative medicine, particularly cell therapy to replace lost or damaged tissues.
History of hPSCs
hPSCs are defined as self-renewable cell types that confer the ability to differentiate into various cellular phenotypes of the human body, including three germ layers. 102 Historically, the first pluripotent cell lines to be generated were embryonic carcinoma (EC) cell lines established from human germ cell tumors 103 and murine undifferentiated compartments. 104 Although EC cells are a powerful tool in vitro, these cells are not suitable for clinical applications due to their cancer-derived origin and aneuploidy genotype. 105 The first murine ESCs were established in 1981 based on the culture techniques obtained from EC research. 106 Murine ESCs are derived from the inner cell mass (ICM) of the pre-implantation blastocyst, a unique biological structure that contains outer trophoblast layers that give rise to the placenta and ICM. 107 In vivo ESCs only exist for a short period during the embryo’s development, and they can be isolated and maintained indefinitely in vitro in an undifferentiated state. The discovery of murine ESCs has dramatically changed the field of biomedical research and regenerative medicine over the last 40 years. Since then, enormous investigations have been made to isolate and culture ESCs from other species, including hESCs, in 1998. 99 The success of Thomson et al. in 1998 triggered the great controversy in media and ethical research boards across the globe, with particularly strong objections being raised to the use of human embryos for research purposes. 108 Several studies using hESCs have been conducted demonstrating their therapeutic potential in the clinical setting. However, the use of hESCs is limited due to (1) the ethical barrier related to the destruction of human embryos and (2) the potential risk of immunological rejection, as hESCs are isolated from pre-implantation blastocysts, which are not autologous in origin. To overcome these two great obstacles, several research groups have been trying to develop technology to generate hESCs, including nuclear transfer technology, the well-known strategy that creates Dolly sheep, although the generation of human nuclear transfer ESCs remains technically challenging. 109 Taking a different approach, in 2006, Yamanaka and Takahashi generated artificial PSCs from adult and embryonic mouse somatic cells using four transcription factors ( Oct-3/4 , Sox2 , Klf4 , and c-Myc , called OSKM) reduced from 24 factors. 100 Thereafter, in 2007, Takahashi and colleagues successfully generated the first hiPSCs exhibiting molecular and biological features similar to those of hESCs using the same OSKM factors. 101 Since then, hiPSCs have been widely studied to expand our knowledge of the pathogenesis of numerous diseases and aid in developing new cell-based therapies as well as personalized medicine.
Clinical applications of hPSCs
Since its beginning 24 years ago, hPSC research has evolved momentously toward applications in regenerative medicine, disease modeling, drug screening and discovery, and stem cell-based therapy. In clinical trial settings, the uses of hESCs are restricted by ethical concerns and tight regulation, and the limited preclinical data support their therapeutic potential. However, it is important to acknowledge several successful outcomes of hESC-based therapies in treating human diseases. In 2012, Steven Schwartz and his team reported the first clinical evidence of using hESC-derived retinal pigment epithelium (RPE) in the treatment of Stargardt’s macular dystrophy, the most common pediatric macular degeneration, and an individual with dry age-related macular degeneration. 110 , 111 With a differentiation efficiency of RPE greater than 99%, 5 × 10 4 RPEs were injected into the subretinal space of one eye in each patient. As the hESC source of RPE differentiation was exposed to mouse embryonic stem cells, it was considered a xenotransplantation product and required a lower dose of immunosuppression treatment. This study showed that hESCs improved the vision of patients by differentiating into functional RPE without any severe adverse events. The trial was then expanded into two open-label, phase I/II studies with the published results in 2015 supporting the primary findings. 112 In these trials, patients were divided into three groups receiving three different doses of hESC-derived RPE, including 10 × 10 4 , 15 × 10 4 and 50 × 10 4 RPE cells per eye. After 22 months of follow-up, 19 patients showed improvement in eyesight, seven patients exhibited no improvement, and one patient experienced a further loss of eyesight. The technical challenge of hESC-derived RPE engraftment was an unbalanced proliferation of RPE post administration, which was observed in 72% of treated patients. A similar approach was also conducted in two South Korean patients diagnosed with age-induced macular degeneration and two patients with Stargardt macular dystrophy. 113 The results supported the safety of hESC-derived RPE cells and illustrated an improvement in visual acuity in three patients. Recently, clinical-graded hESC-derived RPE cells were also developed by Chinese researchers under xeno-free culture conditions to treat patients with wet age-related degeneration. 114 As hESC development is still associated with ethical concerns and immunological complications related to allogeneic administration, hiPSC-derived RPE cells have emerged as a potential cell source for macular degeneration. Although RPE differentiation protocols have been developed and optimized to improve the efficacy of hiPSC-derived RPE cells, they are still insufficient, time-consuming and labor intensive. 115 , 116 For clinical application, an efficient differentiation of “primed” to “naïve” state hiPSCs toward the RPE was developed using feeder-free culture conditions utilizing the transient inhibition of the FGF/MAPK signaling pathway. 117 Overexpression of specific transcription factors in hiPSCs throughout the differentiation process is also an interesting approach to generate a large number of RPE cells for clinical use. In a recent study, overexpression of three eye-field transcription factors, including OTX2, PAX6, and MITF , stimulated RPE differentiation in hiPSCs and generated functional RPE cells suitable for transplantation. 118 To date, although reported data from phase I/II clinical trials have been produced enough to support the safety of hESC-derived RPE cells, the treatment is still in its immature stage. Thus, future studies should focus on the development of the cellular manufacturing process of RPE and the subretinal administration route to further improve the outcomes of RPE fabrication and engraftment into the patient’s retina (recommended review 119 ).
Numerous studies have demonstrated that hESC-derived cardiomyocytes exhibit cardiac transcription factors and display a cardiomyocyte phenotype and immature electrical phenotype. In addition, using hPSC-derived cardiomyocytes could provide a large number of cells required for true remuscularization and transplantation. Thus, these cells can be a promising novel therapeutic approach for the treatment of human cardiovascular diseases. In a case report, hESC-derived cardiomyocytes showed potential therapeutic effects in patients with severe heart failure without any subsequent complications. 120 This study was a phase I trial (ESCORT [Transplantation of Human Embryonic Stem Cell-derived Progenitors in Severe Heart Failure] trial) to evaluate the safety of cardiomyocyte progenitor cells derived from hESCs seeded in fibrin gel scaffolds for 10 patients with severe heart failure (NCT02057900). The encouraging results from this study demonstrated the feasibility of producing hESC-derived cardiomyocyte progenitor cells toward clinical-grade standards and combining them with a tissue-engineered scaffold to treat severe heart disease (the first patient of this trial has already reached the 7-year follow-up in October 2021). 121 Currently, the two ongoing clinical trials using hPSC-derived cardiomyocytes have drawn great attention, as their results would pave the way to lift the bar for approving therapies for commercial use. The first trial was conducted by a team led by cardiac surgeon Yoshiki Sawa at Osaka University using hiPSC-derived cardiomyocytes embedded in a cell sheet for engraftment (jRCT2052190081). The trials started first with three patients followed by ten patients to assess the safety of the approach. Once safety is met, the treatment can be sold commercially under Japan’s fast-track system for regenerative medicine. 122 Another trial used a collagen-based construct called BioVAT-HF to contain hiPSC-derived cardiomyocytes. The trial was divided into two parts to evaluate the cell dose: (Part A) recruiting 18 patients and (Part B) recruiting 35 patients to test a broad range of engineered human myocardium (EHM) doses. The expected results from this study will provide the “proof-of-concept” for the use of EHM in the stimulation of heart remuscularization in humans. To date, no adverse events or severe adverse events have been reported from these trials, supporting the safety of the procedure. However, as the number of treated patients was relatively small, limitations in drawing conclusions regarding efficacy are not yet possible. 21 , 123
One of the first clinical trials using hPSC-based therapy was conducted by Geron Corporation in 2010 using hESC-derived oligodendrocyte progenitor cells (OPC1) to treat spinal cord injury (SCI). The results confirmed the safety one year post administration in five participants, and magnetic resonance imaging demonstrated improvement of spinal cord deterioration in four participants. 124 Asterias Biotherapeutic (AST) continued the Geron study by conducting the SCiStar Phase I/IIa study to evaluate the therapeutic effects of AST-OPC1 (NCT02302157). The trial’s results published in clinicaltrials.gov demonstrated significant improvement in running speed, forelimb stride length, forelimb longitudinal deviations, and rear stride frequency. Interestingly, the recently published data of a phase 1, multicentre, nonrandomized, single-group assignment, interventional trial illustrated no evidence of neurological decline, enlarging masses, further spinal cord damage, or syrinx formation in patients 10 years post administration of the OPC1 product. 125 This data set provides solid evidence supporting the safety of OPC1 with an event-free period of up to 10 years, which strengthens the safety profile of the SCiStar trial.
Analysis of the global trends in clinical trials using hPSC-based therapy showed that 77.1% of studies were observational (no cells were administered into patient), and only 22.9% of studies used hPSC-derived cells as interventional treatment. 126 The number of studies using hiPSCs was relatively higher than that using hESCs, which was 74.8% compared to 25.2%, respectively. The majority of observational studies were performed in developed countries, including the USA (41.6%) and France (16.8%), whereas interventional studies were conducted in Asian countries, including China (36.7%), Japan (13.3%), and South Korea (10%). The trends in therapeutic studies were also clear in terms of targeted diseases. The three most studied diseases were ophthalmological conditions, circulatory disorders, and nervous systems. 127 However, it is surprising that the clinical applications of hPSCs have achieved little progress since the first hESCs were discovered worldwide. The relatively low number of clinical trials focusing on using iPSCs as therapeutic agents to administer into patients could be ascribed to the unstable genome of hiPSCs, 128 immunological rejection, 129 and the potential for tumor formation. 130
Mesenchymal stem/stromal cell-based therapy: is it time to consider their origin toward targeted therapy?
Approximately 55 years ago, fibroblast-like, plastic-adherent cells, later named mesenchymal stem cells (MSCs) by Arnold L. Caplan, 18 were discovered for the first time in mouse bone marrow (BM) and were later demonstrated to be able to form colony-like structures, proliferate, and differentiate into bone/reticular tissue, cartilage, and fat. 131 Protocols were subsequently established to directly culture this subpopulation of stromal cells from BM in vitro and to stimulate their differentiation into adipocytes, chondroblasts, and osteoblasts. 132 Since then, MSCs have been found in and derived from different human tissue sources, including adipose tissue (AT), the umbilical cord (UC), UC blood, the placenta, dental pulp, amniotic fluid, etc. 133 To standardize and define MSCs, the International Society for Cell and Gene Therapy (ISCT) set minimal identification criteria for MSCs derived from multiple tissue sources. 134 Among them, MSCs derived from AT, BM, and UC are the most commonly studied MSCs in human clinical trials, 135 and they constitute the three major tissue sources of MSCs that will be discussed in this review.
The discovery of MSCs opened an era during which preclinical studies and clinical trials have been performed to assess the safety and efficacy of MSCs in the treatment of various diseases. The major conclusion of these studies and trials is that MSC-based therapy is safe, although the outcomes have usually been either neutral or at best marginally positive in terms of the clinically relevant endpoints regardless of MSC tissue origin, route of infusion, dose, administration duration, and preconditioning. 136 It is important to note that a solid background of knowledge has been generated from all these studies that has fueled the recent translational research in MSC-based therapy. As MSCs have been intensively studied over the last 55 years and have become the subject of multiple reviews, systematic reviews, and meta-analyses, the objective of this paper is not to duplicate these publications. Rather, we will discuss the questions that both clinicians and researchers are currently exploring with regard to MSC-based therapy, diligently seeking answers to the following:
“With a solid body of data supporting their safety profiles derived from both preclinical and clinical studies, does the tissue origin of MSCs also play a role in their downstream clinical applications in the treatment of different human diseases?”
“Do MSCs derived from AT, BM, and UC exhibit similar efficacy in the treatment of neurological diseases, metabolic/endocrine-related disorders, reproductive dysfunction, skin burns, lung fibrosis, pulmonary disease, and cardiovascular conditions?”
To answer these questions, we will first focus on the most recently published clinical data regarding these targeted conditions, including neurological disorders, pulmonary dysfunctions, metabolic/endocrine-related diseases, reproductive disorders, skin burns, and heart-related diseases, to analyze the potential efficacy of MSCs derived from AT, BM, and UC. Based on the level of clinical improvement observed in each trial, we analyzed the potential efficacy of MSCs derived from each source to visualize the correlation between patient improvement and MSC sources. We will then address recent trends in the exclusive use of MSC-based products, focusing on the efficacy of treatment with MSCs from each of the abovementioned sources, and we will analyze the relationship between the respective efficacies of MSCs from these sources in relation to the targeted disease conditions. Finally, we propose a hypothesis and mechanism to achieve the currently still unmet objective of evaluating the use of MSCs from AT, BM, and UC in regenerative medicine.
An overview of MSC tissue origins and therapeutic potential
In general, MSCs are reported to be isolated from numerous tissue types, but all of these types can be organized into two major sources: adult 137 and perinatal sources 138 (Fig. 2 ). Adult sources of MSCs are defined as tissues that can be harvested or obtained from an individual, such as dental pulp, 139 BM, peripheral blood, 140 AT, 141 lungs, 142 hair, 143 or the heart. 144 Adult MSCs usually reside in specialized structures called stem cell niches, which provide the microenvironment, growth factors, cell-to-cell contacts and external signals necessary for maintaining stemness and differentiation ability. 145 BM was the first adult source of MSCs discovered by Friedenstein 131 and has become one of the most documented and largely used MSC sources to date, followed by AT. BM-MSCs are isolated and cultured in vitro from BM aspirates using a Ficoll gradient-centrifugation method 146 or a red blood cell lysate buffer to collect BM mononuclear cell populations, whereas AT-MSCs are obtained from stromal vascular fractions of enzymatically digested AT obtained through liposuction, 141 lipoplasty, or lipectomy procedures. 147 These tissue collection procedures are invasive and painful for the patient and are accompanied by a risk of infection, although BM aspiration and adipose liposuction are considered safe procedures for BM and AT biopsies. The number of MSCs that can be isolated from these adult tissues varies significantly in a tissue-dependent manner. The percentage of MSCs in BM mononuclear cells ranges from 0.001 to 0.01% following gradient centrifugation. 132 The number of MSCs in AT is at least 500 times higher than that in BM, with approximately 5,000 MSCs per 1 g of AT. Perinatal sources of MSCs consist of UC-derived components, such as UC, Wharton’s jelly, and UC blood, and placental structures, such as the placental membrane, amnion, chorion membrane, and amniotic fluid. 138 The collection of perinatal MSCs, such as UC-MSCs, is noninvasive, as the placenta, UC, UC blood, and amnion are considered waste products that are usually discarded after birth (with no ethical barriers). 148 Although MSCs represent only 10 −7 % the cells found in UC, their higher proliferation rate and rapid population doubling time allow these cells to rapidly replicate and increase in number during in vitro culture. 149 Under standardized xeno-free and serum-free culture platforms, AT-MSCs show a faster proliferation rate and a higher number of colony-forming units than BM-MSCs. 149 UC-MSCs have the fastest population doubling time compared to AT-MSCs and BM-MSCs in both conventional culture conditions and xeno- and serum-free environments. 149 MSCs extracted from AT, BM and UC exhibit all minimal criteria listed by the ISCT, including morphology (plastic adherence and spindle shape), MSC surface markers (95% positive for CD73, CD90 and CD105; less than 2% negative for CD11, CD13, CD19, CD34, CD45, and HLR-DR) and differentiation ability into chondrocytes, osteocytes, and adipocytes. 150
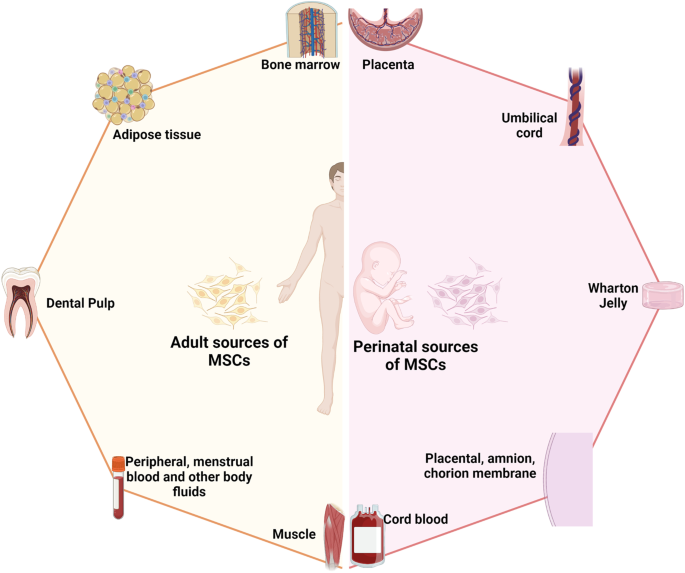
The two major sources of MSCs: adult and perinatal sources. The adult sources of MSCs are specific tissue in human body where MSCs could be isolated, including bone marrow, adipose tissue, dental pulp, peripheral blood, menstrual blood, muscle, etc. The perinatal sources of MSCs consist of umbilical cord-derived components, such as umbilical cord, Wharton’s jelly, umbilical cord blood, and placental structures, such as placental membrane, amnion, chorion membrane, amniotic fluid, etc. The figure was created with BioRender.com
In fact, although MSCs derived from either adult or perinatal sources exhibit similar morphology and the basic characteristics of MSCs, studies have demonstrated that these cells also differ from each other. Regarding immunophenotyping, AT-MSCs express high levels of CD49d and low levels of Stro-1. An analysis of the expression of CD49d and CD106 showed that the former is strongly expressed in AT-MSCs, in contrast to BM-MSCs, whereas CD106 is expressed in BM-MSCs but not in AT-MSCs. 151 Increased expression of CD133, which is associated with stem cell regeneration, differentiation, and metabolic functions, 152 was observed in BM-MSCs compared to MSCs from other sources. 153 A recent study showed that CD146 expression in UC-MSCs was higher than that in AT- and BM-MSCs, 153 supporting the observation that UC-MSCs have a stronger attachment and a higher proliferation rate than MSCs from other sources, as CD146 is a key cell adhesion protein in vascular and endothelial cell types. 154 In terms of differentiation ability, donor-matched BM-MSCs exhibit a higher ability to differentiate into chondrogenic and osteogenic cell types than AT-MSCs, whereas AT-MSCs show a stronger capacity toward the adipogenic lineage. 150 The findings from an in vitro differentiation study indicated that BM-MSCs are prone to osteogenic differentiation, whereas AT-MSCs possess stronger adipogenic differentiation ability, which can be explained by the fact that the epigenetic memory obtained from either BM or AT drives the favored MSC differentiation along an osteoblastic or adipocytic lineage. 155 Interestingly, although UC-MSCs have the ability to differentiate into adipocytes, osteocytes, or chondrocytes, their osteogenic differentiation ability has been proven to be stronger than that of BM-MSCs. 156 The most interesting characteristic of MSCs is their immunoregulatory functions, which are speculated to be related to either cell-to-cell contact or growth factor and cytokine secretion in response to environmental/microenvironmental stimuli. MSCs from different sources almost completely inhibit the proliferation of peripheral blood mononuclear cells (PBMCs) at PBMC:MSC ratios of 1:1 and 10:1. 149 At a higher ratio, BM-MSCs showed a significantly higher inhibitory effect than AT- or UC-MSCs. 153 Direct analysis of the immunosuppressive effects of BM- and UC-MSCs has revealed that these cells exert similar inhibitory effects in vitro with different mechanisms involved. 157 With these conflicting data, the mechanism of action related to the immune response of MSCs from different sources is still poorly understood, and long-term investigations both in preclinical studies and in clinical trial settings are needed to shed light on this complex immunomodulation function.
The great concern in MSC-based therapy is the fate of these cells post administration, especially through different delivery routes, including systemic administration via an intravenous (IV) route or tissue-specific administration, such as dorsal pancreatic administration. It is important to understand the distribution of these cells after injection to expand our understanding of the underlying mechanisms of action of treatments; in addition, this knowledge is required by authorized bodies (the Food and Drug Administration (FDA) in the United States or the regulation of advanced-therapy medicinal products in Europe, No. 1394/2007) prior to using these cells in clinical trials. The preclinical data using various labeling techniques provide important information demonstrating that MSCs do not have unwanted homing that could lead to the incorrect differentiation of the cells or inappropriate tumor formation. In a mouse model, human BM-MSCs and AT-MSCs delivered via an IV route are rapidly trapped in the lungs and then recirculate through the body after the first embolization process, with a small number of infused cells found mainly in the liver after the second embolization. 158 Using the technetium-99 m labeling method, intravenously infused human cells showed long-term persistence up to 13 months in the bone, BM compartment, spleen, muscle, and cartilage. 159 A similar result was reported in baboons, confirming the long-term homing of human MSCs in various tissues post administration. 160 Although the retainment of MSCs in the lungs might potentially reduce their systemic therapeutic effects, 161 it provides a strong advantage when these cells are used in the treatment of respiratory diseases. Local injection of MSCs also revealed their tissue-specific homing, as an injection of MSCs via the renal artery route resulted in the majority of the injected cells being found in the renal cortex. 162 Numerous studies have been conducted to track the migration of administered MSCs in human subjects. Henriksson and his team used MSCs labeled with iron sucrose in the treatment of intervertebral disc degeneration. 163 Their study showed that chondrocytes differentiated from infused MSCs could be detected at the injured intervertebral discs at 8 months but not at 28 months. A study conducted in a patient with hemophilia A using In-oxine-labeled MSCs showed that the majority of the cells were trapped in the lungs and liver 1 h post administration, followed by a reduction in the lungs and an increase in the number of cells in the liver after 6 days. 164 Interestingly, a small proportion of infused MSCs were found in the hemarthrosis site at the right ankle after 24 h, suggesting that MSCs are attracted and migrate to the injured site. The distribution of MSCs was also reported in the treatment of 21 patients diagnosed with type 2 diabetes using 18-FDG-tagged MSCs and visualized using positron emission tomography (PET). 165 The results illustrated that local delivery of MSCs via an intraarterial route is more effective than delivery via an IV route, as MSCs home to the pancreatic head (pancreaticoduodenal artery) or body (splenic artery). Therefore, although the available data related to the biodistribution of infused MSCs are still limited, the results obtained from both preclinical and clinical studies illustrate a comparable set of data supporting results on homing, migration to the injured site, and the major organs where infused MSCs are located. The following comprehensive and interesting reviews are highly recommended. 166 , 167 , 168
To date, 1426 registered clinical trials spanning different trial phases have used MSCs for therapeutic purposes, which is four times the number reported in 2013. 169 , 170 As supported by a large body of preclinical studies and advancements in conducting clinical trials, MSCs have been proven to be effective in the treatment of numerous diseases, including nervous system and brain disorders, pulmonary diseases, 171 cardiovascular conditions, 172 wound healing, etc. The outcomes of MSC-based therapy have been the subject of many intensive reviews and systematic analyses with the solid conclusion that these cells exhibit strong safety profiles and positive outcomes in most tested conditions. 173 , 174 , 175 In addition, the available data have revealed several potential mechanisms that could explain the beneficial effects of MSCs, including their homing efficiency, differentiation potential, production of trophic factors (including cytokines, chemokines, and growth factors), and immunomodulatory abilities. However, it is still not known which MSC types should be used for which diseases, as it seems to be that MSCs exhibit beneficial effects regardless of their sources. 169
Acquired brain and spinal cord injury treatment: BM-MSCs have emerged as key players
The theory that brain cells can never regenerate has been challenged by the discovery of newly formed neurons in the human adult hippocampus or the migration of stem cells in the brain in animal models. 176 These observations have triggered hope for regeneration in the context of neuronal diseases by using exogenous stem cell sources to replenish or boost the stem cell population in the brain. Moreover, the limited regenerative capacity of the brain and spinal cord is an obstacle for traditional treatments of neurodegenerative diseases, such as autism, cerebral palsy, stroke, and spinal cord injury (SCI). As current treatments cannot halt the progression of these diseases, studies throughout the world have sought to exploit cell-based therapies to treat neurodegenerative diseases on the basis of advances in the understanding and development of stem cell technology, including the use of MSCs. Successful stem cell therapy for treating brain disease requires therapeutic cells to reach the injured sites, where they can repair, replace, or at least prevent the deteriorative effects of neuronal damage. 177 Hence, the gold standard of cell-based therapy is to deliver the cells to the target site, stimulate the tissue repair machinery, and regulate immunological responses via either cell-to-cell contact or paracrine effects. 178 Among 315 registered clinical trials using stem cells for the treatment of brain diseases, MSCs and hematopoietic stem cells (HSCs; CD34+ cells isolated from either BM aspirate or UC blood) are the two main cell types investigated, whereas approximately 102 clinical trials used MSCs and 62 trials used HSCs for the treatment of brain disease (main search data from clinicaltrial.gov). MSCs are widely used in almost all clinical trials targeting different neuronal diseases, including multiple sclerosis, 179 stroke, 180 SCI, 181 cerebral palsy, 182 hypoxic-ischemic encephalopathy, 183 autism, 184 Parkinson’s disease, 185 Alzheimer’s disease 185 and ataxia. Among these trials in which MSCs were the major cells used, nearly two-thirds were for stroke, SCI, or multiple sclerosis. MSCs have been widely used in 29 registered clinical trials for stroke, with BM-MSCs being used in 16 of these trials. With 26 registered clinical trials, SCI is the second most common indication for using MSCs, with 16 of these trials using mainly expanded BM-MSCs. For multiple sclerosis, 15 trials employed BM-MSCs among a total of 23 trials conducted for the treatment of this disease. Hence, it is important to note that in neuronal diseases and disorders, BM-MSCs have emerged as the most commonly used therapeutic cells among other MSCs, such as AT-MSCs and UC-MSCs.
The outcomes of the use of BM-MSCs in the treatment of neuronal diseases have been widely reported in various clinical trial types. A review by Zheng et al. indicated that although the treatments appeared to be safe in patients diagnosed with stroke, there is a need for well-designed phase II multicentre studies to confirm the outcomes. 173 One of the earliest trials using autologous BM-MSCs was conducted by Bang et al. in five patients diagnosed with stroke in 2005. The results supported the safety and showed an improved Barthel index (BI) in MSC-treated patients. 186 In a 2-year follow-up clinical trial, 16 patients with stroke received BM-MSC infusions, and the results showed that the treatment was safe and improved clinical outcomes, such as motor impairment scale scores. 187 A study conducted in 12 patients with ischemic stroke showed that autologous BM-MSCs expanded in vitro using autologous serum improved the patient’s modified Rankin Scale (mRS), with a mean lesion volume reduced by 20% at 1 week post cell infusion. 188 In 2011, a modest increase in the Fugl Meyer and modified BI scores was observed after autologous administration of BM-MSCs in patients with chronic stroke. 189 More recently, a prospective, open-label, randomized controlled trial with blinded outcome evaluation was conducted, with 39 patients and 15 patients in the BM-MSC administration and control groups, respectively. The results of this study indicated that autologous BM-MSCs with autologous serum administration were safe, but the treatment led to no improvements at 3 months in modified Rankin Scale (mRS) scores, although leg motor improvement was observed. 180 Researchers explored whether the efficacy of BM-MSC administration was maintained over time in a 5-year follow-up clinical trial. Patients (85) were randomly assigned to either the MSC group or the control group, and follow-ups on safety and efficacy were performed for 5 years, with 52 patients being examined at the end of the study. The MSC group exhibited a significant improvement in terms of decreased mRS scores, whereas the number of patients with an mRS score increase of 0–3 was statistically significant. 187 Although autologous BM-MSCs did not improve the Basel index, mRS, or National Institutes of Health Stroke Scale (NIHSS) score 2 years post infusion, patients who received BM-MSC therapy showed improvement in their motor function score. 190 In addition, a prospective, open-label, randomized controlled trial by Lee et al. showed that autologous BM-MSCs primed with autologous “ischemic” serum significantly improved motor functions in the MSC-treated group. Neuroimaging analysis also illustrated a significant increase in interhemispheric connectivity and ipsilesional connectivity in the MSC group. 191 Recently, a single intravenous infection of allogeneic BM-MSCs has been proven to be safe and feasible in patients with chronic stroke with a significant improvement in BI score and NIHSS score. 192
In two systematic reviews using MSCs for the treatment of SCI, BM-MSCs ( n = 16) and UC-MSCs ( n = 5) were reported to be safe and well-tolerated. 193 , 194 The results indicated significant improvements in the stem cell administration groups compared with the control groups in terms of a composite of the American Spinal Injury Association (ASIA) impairment scale (AIS) grade, AIS grade A, and ASIA sensory scores and bladder function (Table 1 ). However, larger experimental groups with a randomized and multicentre design are needed for further confirmation of these findings. For multiple sclerosis, several early-phase (phase I/II) registered clinical studies have used BM-MSCs. A study compared the potential efficacy of BM-MSC and BM mononuclear cell (BMMNC) transplantation in 105 patients with spastic cerebral palsy. 195 The results showed that the GMFM (gross motor function measure) and the FMFM (fine motor function measure) scores of the BM-MSC transplant group were higher than those of the BMNNC transplant group at 3, 6, and 12 months of assessment. In terms of autism spectrum disorder, a review of 254 children after BMMNC transplantation found that over 90% of patients’ ISAA (Indian Scale for Assessment of Autism) and CARS (Childhood Autism Rating Scale) scores improved. Young patients and those in whom autism spectrum disorder was detected early generally showed better improvement. 196
One of the biggest limitations when using BM-MSCs is the bone marrow aspiration process, as it is an invasive procedure that can introduce a risk of complications, especially in pediatric and elderly patients. 197 Therefore, UC-MSCs have been suggested as an alternative to BM-MSCs and are being studied in clinical trials for the treatment of neurological diseases in approximately 1550 patients throughout the world; however, only three studies have been completed, with data published recently. 198 A recent study showed that UC-MSC administration improved both gross motor function and cognitive skills, assessed using the Activities of Daily Living (ADL), Comprehensive Function Assessment (CFA), and GMFM, in patients diagnosed with cerebral palsy. The improvements peaked 6 months post administration and lasted for 12 months after the first transplantation. 199 In a single-targeted phase I/II clinical trial using UC-MSCs for the treatment of autism, Riordan et al. reported decreases in Autism Treatment Evaluation Checklist (ATEC) and CARS scores for eight patients, but the paper has been retracted due to a violation of the journal’s guidelines. 200 In an open-label, phase I study, UC-MSCs were used as the main cells to treat 12 patients with autism spectrum disorder via IV infusions. It is important to note that five participants developed new class I anti-human leukocyte antigen in response to the specific lot of manufactured UC-MSCs, although these responses did not exhibit any immunological response or clinical manifestations. Only 50% of participants showed improvements in at least two autism-specific measurements. 201 Although not as widely used as BM-MSCs, these trials have demonstrated the efficacy of using UC-MSCs in the treatment of SCIs. In a pilot clinical study, Yang et al. showed that the use of UC-MSCs has the potential to improve disease status through an increase in total ASIA and SCI Functional Rating Scale of the International Association of Neurorestoratology (IANR-SCIFRS) scores, as well as an improvement in pinprick, light touch, motor and sphincter scores. 202 A study of 22 patients with SCIs showed a potential therapeutic effect in 13 patients post UC-MSC infusion. 203 AT-MSCs were also used to treat SCI, with a single case report indicating an improvement in neurological and motor functions in a domestic ferret patient. 204 However, a result obtained from another phase I trial using AT-MSCs showed mild improvements in neurological function in a small number of patients. 205 A phase II, randomized, double-blind, placebo-controlled, single-center, pilot clinical trial using AT-MSCs in the treatment of acute ischemic stroke published a data set that supports the safety of the therapy, although patients who received AT-MSCs showed a nonsignificant improvement after 24 months of follow-up. 206 In all of the above studies, the safety of using either AT-MSCs or UC-MSCs was evaluated, and no significant reactions were reported after infusion.
Therefore, based on the number of recovered patients post-transplantation and the number of recruited patients in large-scale trials using BM-MSCs, it seems that BM-MSCs are the prominent cells in regard to treating neurodegenerative disease with potentially good outcomes (Table 1 ). It is important to note that we do not negate the fact that AT- and UC-MSCs also show positive outcomes in the treatment of neuronal diseases, with numerous ongoing large-scale, multicentre, randomized, and placebo-control trials, 207 , 208 but we suggest alternative and thoughtful decisions regarding which sources of MSCs are best for the treatment of neuronal diseases and degenerative disorders.
Respiratory disease and lung fibrosis: clinical data support UC as a good source of MSCs
In the last decade, significant increases in respiratory disease incidence due to air pollution, smoking behavior, population aging, and recently, respiratory virus infections such as coronavirus disease 2019 (COVID-19) 209 have been observed, leading to substantial burdens on public health and healthcare systems worldwide. Respiratory inflammatory diseases, including bronchopulmonary dysplasia (BPD), chronic obstructive pulmonary disease (COPD), and acute respiratory distress syndrome (ARDS), have recently emerged as three prevalent pulmonary diseases in children and adults. These conditions are usually associated with inflammatory cell infiltration, a disruption of alveolar structural integrity, a reduction in alveolar fluid clearance ability, cytokine release and associated cytokine storms, airway remodeling, and the development of pulmonary fibrosis. Traditional treatments are focused on relieving symptoms and preventing disease progression using surfactants, artificial respiratory support, mechanical ventilation, and antibiotic/anti-inflammatory drugs, with limited effects on the damaged airway, alveolar fluid clearance, and other detrimental effects caused by the inflammatory response. MSCs are known for their immunomodulatory abilities, showing potential in injury reduction and aiding lung recovery after injury. According to ClinicalTrials.gov, from 2017 to date, there have been 159 studies testing the application of MSCs in the treatment of pulmonary diseases, including but not limited to BPD, COPD, and ARDS, suggesting a trend in the use of MSCs as an alternative approach for the treatment of respiratory diseases, especially MSCs from UC as an “off-the-shelf” and allogeneic source.
Extremely premature infants are born with arrested lung development at the canalicular-saccular phases prior to alveolarization and before pulmonary maturation occurs, which results in the development of BPD. 210 These infants require intensive care during the first three months of life using postnatal interventions, including positive pressure mechanical ventilation, external oxygen support, and surfactant infusions, and the newborns have recurrent infections that further compromise normal lung development. 211 To date, 13 clinical trials have been proposed to use UC-MSCs in the treatment of BPD, recruiting ~566 premature infants throughout the world, including Vietnam, Korea, the United States, Spain, Australia, and China. The majority of these trials use UC-derived stem cells for phases I and II, focusing on evaluating the safety and efficacy of stem cell-based therapy. 212 Human UC tissue and its derivative components are considered the most attractive cell sources for MSCs in the treatment of BPD due to the ease of obtaining them, being readily available, with no ethical concerns, low antigenicity, a high cell proliferation rate, and superior regenerative potential. Chang et al. used MSCs derived from UC blood in a phase I dose-escalation clinical trial to treat 9 preterm infants via intratracheal administration to prevent the development of BPD. 213 All 9 preterm infants survived, and only three developed BPD; these infants had significantly decreased BPD severity compared with the historically matched control group. A follow-up study of the same patients after 24 months indicated that only one infant had an E. cloacae infection after discharge at 4 months, with subsequent disseminated intravascular coagulation, which was later proven to be unrelated to the intervention. The remaining eight patients survived with normal pulmonary development and function, suggesting that the therapy was safe. MSCs from UC blood were also used for the treatment of 12 extremely low birthweight preterm patients using the same administration route, which further confirmed the safety of the therapy in the treatment of BPD, although ten of 12 infants still developed severe BPD at 36 weeks. 214 Our group also reported the safety and potential efficacy of using UC-MSCs in the treatment of four preterm infants, and the results supported the safety of UC-MSCs and demonstrated that patients could be weaned from oxygen supply and develop normal lung structure and function. 215 A phase II clinical trial of 66 infants born at 23–28 weeks with a birthweight of 500–1250 g who were recruited and randomized into an MSC-administration group and a control group was conducted. Although the results supported the safety of MSC administration in preterm infants, the efficacy of the treatment was not supported by statistical analysis, potentially due to the small sample size. Subgroup analysis showed that patients with severe BPD born at 23–24 weeks showed a significant improvement in BPD severity, but those born at 25–28 weeks did not. 216 Hence, it is important to conduct controlled phase II clinical trials with larger cohort sizes to further substantiate the efficacy of UC blood-derived MSCs in the treatment of infants with BPD.
With more than 65 million patients worldwide, COPD was the third-leading cause of death in 2020, according to World Health Organization records. COPD is classified as a chronic inflammatory and destructive pulmonary disease characterized by a progressive reduction in lung function. Averyanov et al. performed a randomized, placebo-controlled phase I/IIa study in 20 patients with mild to moderate idiopathic pulmonary fibrosis (IPF). Treatment group patients received two IV doses of allogeneic MSCs (2 × 10 8 cells) every 3 months, and the second group received a placebo. 217 Evaluation tests were performed at weeks 13, 26, 39, and 52. The 6-min walking test distance (6MWTD) results showed that patient fitness improved from week 13 onwards and was maintained until up to the 52nd week. Pulmonary function indicators improved markedly before and after treatment in the treated group but did not change significantly in the placebo group. The goal of MSC therapy in the treatment of COPD is to promote the regeneration of parenchymal cells and alveolar structure and the restoration of lung function. Based on the results of a phase I trial of a commercial BM-MSC product, Prochymal TM , which led to improvements in pulmonary function in treated patients, a multicentre, double-blind, placebo-controlled phase II trial was conducted in 62 patients diagnosed with COPD to determine the safety and potential efficacy of the product. Although the results supported the safety of BM-MSCs, their effectiveness in the treatment of COPD was not assured. No statistically significant differences in FEV 1 or FEV 1% , total lung capacity, or carbon monoxide diffusing capacity were detected after 2 years of follow-up between the two treatment groups. To date, there have been five clinical trials using BM-MSCs as the main stem cells for the treatment of COPD, but the overall clinical outcomes did not demonstrate the potential therapeutic effects of the treatment. 218 , 219 , 220 , 221 , 222 In clinical trial NCT001110252, the results showed that there was an overall reduction in the process of COPD pathological development 3 years after the administration of BM-MSCs, although the trial had a phase I design, with no control group, and evaluated only a small cohort (four patients). 219 To alleviate local inflammatory progression in COPD, Oliveira et al. studied the combination treatment of one-way endobronchial valve (EBV) and BM-MSC intubation. 223 Ten GOLD (Global Initiative for Obstructive Lung Disease) stage C or D patients were equally divided into 2 groups: one group received a dose of 10 8 cells before valve insertion, and the other group received a normal saline infusion. The follow-up time was 90 days. Inflammation was significantly improved as assessed by the CRP (C-reactive protein) index at 30 and 90 days after infusion. In addition, improvements in St. George’s Respiratory Questionnaire (SGRQ) scores indicated improved patient quality of life. Furthermore, an investigation into the homing ability of MSCs in vivo was performed on 9 GOLD patients, from stage A to stage D. Each patient received two 2 × 10 6 BM-MSC/kg IV infusions 1-week apart. 224 The marking of MSCs with indium-111 showed that MSCs were retained in the pulmonary vasculature longer in patients with mild COPD and that the levels of inflammatory mediators improved after 7 days of treatment. The results of the evaluation survey conducted after 1 year showed that the number of COPD exacerbations decreased to six times/year compared to 11 times/year before treatment. In addition, AT-MSCs present in the stromal vascular fraction were used to treat patients with COPD, and no adverse events were observed after 12 months of follow-up, but the clinical improvements post administration were not clear. 225 The results from a phase I clinical trial using AT-MSCs in eight patients with COPD also reported no significant change in pulmonary function test parameters. 226 A study evaluating the use of AT-MSCs as adjunctive therapy for COPD in 12 patients was performed. 227 AT was obtained using standard liposuction, MSCs were isolated, and 150–300 million cells were intravenously infused. The patients showed improvements in quality of life, with improved SGRQ scores after 3 and 6 months of treatment. Recently, UC-MSCs have emerged as potential allogeneic stem cell candidates for the treatment of COPD. 228 In a pilot clinical study, it was demonstrated that allogeneic administration of UC-MSCs in the treatment of COPD was safe and potentially effective. 229 In one study, 20 patients, including 9 at stage C and 11 at stage D per the GOLD classification, with histories of smoking were recruited and received cell-based therapy. The patients who received UC-MSC treatment showed significant reductions in Modified Medical Research Council scores, COPD assessment test scores, and the number of pulmonary exacerbations 6 months post administration. The results of the second trial using UC-MSCs showed that the mean FEV 1 /FVC ratios were increased along with improvements in SGRQ scores and 6MWTDs at three months post administration. 230 Although thorough assessments of the effectiveness of UC-MSCs are still in the early stages, the number of trials using UC-MSCs for the treatment of COPD is increasing steadily, with larger sample sizes and stronger designs (randomized or matched case–control studies), providing a data set strongly supporting the future applications of UC-MSCs. 231
The ongoing pandemic of the 21st century, the COVID-19 pandemic, emerged as a major pulmonary health problem worldwide, with a relatively high mortality rate. Numerous studies, reviews, and systematic analyses have been conducted to discuss and expand our knowledge of the virus and propose different mechanisms by which the virus could alter the immune system. 232 One of the most critical mechanisms is the generation of cytokine storms, which result from the initiation of hyperreactions of the adaptive immune response to viral infection. 233 These cytokine storms are formed by the establishment of waves of hypercytokinaemia generated from overreactive immune cells, which enhance their expression of TNF-α, IL-6, and IL-10, preventing T-lymphocyte recruitment and proliferation and culminating in T-lymphocyte apoptosis and T-cell exhaustion. In COVID-19, once a cytokine storm is formed, it spreads from an initial focal area through the body via circulation, which has been discussed in a comprehensive review by Jamilloux et al. 234 At the time of writing this review, there were 74 clinical trials using MSCs from UC (29 trials; including WJ-derived MSCs (WJ-MSCs) and placenta-derived MSCs (PL-MSCs)), AT (15 trials), and BM (11 trials) (comprehensive review 171 , 235 ). Hence, UC-MSCs have emerged as the most common MSCs for the treatment of COVID-19, with a total of 1047 patients participating in these trials. Among these trials, 15 completed trials using UC-MSCs (including WJ- and PL-MSCs) have been reported, with clinical data from approximately 600 recruited patients. 232 Eight of these 15 studies used allogenic UC-MSC transplantation to treat critically ill patients. 236 A list of case reports using UC-MSCs showed that the treatments were safe and well-tolerated in 14 patients with COVID-19, with the primary outcomes including increased percentages and numbers of T cells, 237 , 238 improved respiratory and renal functions, 239 reductions in inflammatory biomarker levels, 240 and positive outcomes in the PaO 2 /FiO 2 ratio. 240 In a pilot study conducted in ten patients with severe COVID-19, a single dose of UC-MSCs was safe and improved clinical outcomes, although the study did not investigate whether multiple doses of UC-MSCs could further improve the outcomes. 241 Two trials without a control group were conducted in 47 patients, and the results indicated that UC-MSCs were safe and feasible for the treatment of patients with COVID-19. 235 , 242 A single-center, open-label, individually randomized, standard treatment-controlled trial was performed in 41 patients (12 patients assigned to the UC-MSC group), and the results showed that significant improvements in C-reactive protein levels, IL-6 levels, oxygen indices, and lymphocyte numbers were found in the MSC groups. Chest computed tomography (CT) illustrated significant reductions in lung inflammatory responses as reflected by CT findings, the number of lobes involved, and pulmonary consolidation. 238 In a phase I trial conducted in 18 hospitalized patients with COVID-19, UC-MSCs were administered via an IV route in nine patients (five patients with moderate COVID-19 and 4 patients with severe COVID-19) at days 0, 3, and 6, with no treatment-related adverse events or severe adverse events. 243 Only one patient in the UC-MSC group required mechanical ventilation, compared to four patients in the control group. However, the clinical outcomes, such as COVID-19 symptoms, laboratory test results, CT findings of lung damage, and pulmonary function test parameters, were improved in both groups. Interestingly, a 1-year follow-up of the same sample revealed that the patients who received UC-MSC administration improved in terms of whole-lung lesion volume compared to the control group. 244 Moreover, chest CT at 12 months showed significant regeneration of lung tissue in the MSC-administered groups, whereas lung fibrosis was found in all patients in the control group. This finding is of interest because it indicates that a long time is needed to detect the regenerative functions of MSC-based therapy, as the biological process to enhance lung tissue regeneration occurs relatively slowly and requires multiple steps. The effects of UC-MSCs in the attenuation and prevention of the development of cytokine storms were illustrated in an interventional, prospective, three-parallel arm study with two control arms conducted in 30 patients in moderate and critical clinical conditions. 245 The results indicated a significant decrease in proinflammatory cytokines (IFNγ, IL-6, IL-17A, IL-2, and IL-12) and an increase in anti-inflammatory cytokines (IL-10, IL-13, and IL-1ra), suggesting that UC-MSCs might participate in the prevention of cytokine storm development. Lanzoni et al. performed a double-blind, randomized, controlled trial and found that UC-MSC infusions significantly decreased cytokine levels at day 6 and improved survival in patients with COVID-19 with ARDS. In this trial, 24 patients were randomized and assigned 1:1 to receive either MSCs or placebo. 246 MSC treatment was associated with a significant improvement in the survival rate without serious adverse events. To date, other trials conducted using UC-MSCs as the main MSCs provide a solid data set on their safety and efficacy in preventing the development of cytokine storms, reducing the inflammatory response, improving pulmonary function, reducing intensive care unit (ICU) stay duration, enhancing lung tissue regeneration, and reducing lung fibrosis progression. 240 , 247 , 248 , 249 In two large cohort studies (phase I with 210 patients and phase II with 100 patients), the volume of lung lesions and solid component injuries of patients’ lungs were reduced significantly after the administration of UC-MSCs, 250 and clinical symptoms and inflammatory levels were improved. 251 Of the 26 reported clinical trials for the treatment of COVID-19 with MSCs, 1 study used AT-MSCs as the main MSCs. 236 Thirteen COVID-19 adult patients under invasive mechanical ventilation who had received previous antiviral and/or anti-inflammatory treatments (including steroids, lopinavir/ritonavir, hydroxychloroquine, and/or tocilizumab, among others) were treated with allogeneic AT-MSCs. With a mean follow-up time of 16 days after infusion, 9/13 patients’ clinical symptoms improved, and 7/13 patients were intubated. A decrease in inflammatory cytokines and an increase in immunoregulatory cells were also observed in patients, especially in the group of patients with overall clinical improvement. Although there is a lack of clinical efficacy data supporting the use of AT-MSCs in the treatment of patients with COVID-19, AT-MSCs are still potential candidates for inhibiting COVID-19 due to their high secretory activity, strong immune-modulatory effects, and homing ability. 252 , 253 , 254
For ARDS, in a phase IIa trial, 60 patients with moderate to severe disease were randomized into 2 groups. A group of 40 patients received a single infusion of BM-MSCs at a dose of 1 × 10 6 cells/kg body weight, and another 20 patients received a placebo. 255 After 6 and 24 h of infusion, the decrease in plasma inflammatory cytokine levels in the MSC group was significantly greater than that in the placebo group. For severe pulmonary hypertension (PH) associated with BPD (BPD-PH), in a small trial, two preterm infants born at 26–27 weeks of age were intravenously administered heterologous BM-MSCs at a dose of 5 × 10 6 cells per kg of body weight; the treatment reduced oxygen requirements and supported respiration in the infants. 256 The administration of allogeneic AT-MSCs in the treatment of ARDS appeared to be safe and well-tolerated in 12 adult patients, but clinical outcomes were not observed. 257 The results of two patients who received BM-MSCs showed that both patients had improved respiratory function and hemodynamic function and a reduction in multiorgan failure. 258 Although the safety of BM-MSCs was confirmed in a multicentre, open-label, dose-escalation, phase I clinical trial (The Stem cells for ARDS treatment—START trial), 259 no significant improvements were found in a phase II trial, including in respiratory function and ARDS conditions. 260 The safety profile of UC-MSCs is also supported by the findings of a previous phase I clinical trial conducted in 9 patients, which showed that a single IV administration of UC-MSCs was safe and led to positive outcomes in terms of respiratory function and a reduction in the inflammatory response. 261 The findings of this study were also supported by those of the REALIST (Repair of Acute Respiratory Distress with Stromal Cell Administration) trial, which further confirmed the maximum tolerated dose of allogeneic UC-MSCs in patients with moderate to severe ARDS. 262
Although AT- and BM-MSCs have demonstrated therapeutic potential with similar mechanisms of action, UC-MSCs have emerged as potential candidates in the treatment of pulmonary diseases due to their ease of production as “off-the-shelf” products, rapid proliferation, noninvasive isolation methods, and supreme immunological regulation as well as anti-inflammatory effects. 263 However, it is important to note that there is a need to conduct phase III clinical trials with larger cohorts and trials with at least two sources of MSCs in the treatment of pulmonary conditions to further confirm this speculation. 264 Table 2 summarizes several clinical trials with published results discussed in this review.
Endocrine disorders, infertility/reproductive function recovery, and skin burns: should we consider AT-MSCs as the main MSCs based on their origin?
Endocrine disorders.
The human body maintains function and homeostatic regulation via a complex network of endocrine glands that synthesize and release a wide range of hormones. The endocrine system regulates body functions, including heartbeat, bone regeneration, sexual function, and metabolic activity. Endocrine system dysregulation plays a vital role in the development of diabetes, thyroid disease, growth disorder, sexual dysfunction, reproductive malfunction, and other metabolic disorders. The central dogma of regenerative medicine is the use of adult stem cells as a footprint for tissue regeneration and organ renewal. The functions of these stem cells are tightly regulated by microenvironmental stimuli from the nervous system (rapid response) and endocrine signals via hormones, growth factors, and cytokines. This harmonized and orchestrated system creates a symphony of signals that directly regulate tissue homeostasis and repair after injury. The disruption of these complex networks results in an imbalance of tissue homeostasis and regeneration that can lead to the development of endocrine disorders in humans, such as diabetes, sexual hormone deficiency, premature ovarian failure (POF), and Asherman syndrome.
In recent years, obesity and diabetes (type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM)) have been the two biggest challenges in endocrinology research, and the application of MSCs has emerged as a novel approach for therapeutic consideration. T1DM is characterized by the autoimmune destruction of pancreatic β-cells, whereas T2DM is defined as a combination of insulin resistance and pancreatic insulin-producing cell dysfunction. Regenerative medicine seeks to provide an exogenous cell source for replacing damaged or lost β-cells to achieve the goal of stabilizing patients’ blood glucose levels. To date, there are 28 clinical trials using MSCs in the treatment of T1DM ( http://www.clinicaltrials.gov , searched in October 2021), among which three trials were completed using autologous BM-MSCs (NCT01068951), allogeneic BM-MSCs (NCT00690066), and allogeneic AT-MSCs (NCT03920397). Interestingly, UC-MSCs were the most favored MSCs for the remaining trials. All published studies confirmed the safety of MSC therapy in the treatment of T1DM with no adverse events. The first study using autologous BM-MSCs showed that patients who were randomized into the MSC-administration group showed an increase in C-peptide levels in response to a mixed-meal tolerance test (MMTT) in comparison to the control group. 265 Unfortunately, there was no significant improvement in C-peptide levels, HbA1 C or insulin requirements. The use of autologous AT-MSCs in combination with vitamin D was safe and improved HbA1 C levels 6 months post administration. 266 WJ-MSCs were used as the main MSCs for the treatment of new-onset T1DM, which showed a significant improvement in both HbA1 C and C-peptide levels when compared to those of the control group at three and six months post administration. 267 , 268 The combination of allogeneic WJ-MSCs with autologous BM-derived mononuclear cells improved insulin secretion and reduced insulin requirements in patients with T1DM. 269 In terms of T2DM, 23 studies were registered on clinicaltrials.gov (searched in October 2021), with six completed studies (three studies used BM-MSCs and three studies used allogeneic UC-MSCs). Although the number of studies using MSCs for the treatment of T2DM is small, their findings support the safety of MSCs, with no severe adverse events observed during the course of these studies. 270 It was confirmed that MSC therapy potentially reduced fasting blood glucose and HbA1 C levels and increased C-peptide levels. However, these effects were short-term, and multiple doses were required to maintain the MSC effects. Interestingly, the autologous MSC approach in the treatment of patients with diabetes in general is hampered, as both BM-MSCs and AT-MSCs isolated from patients with diabetes showed reduced stemness and functional characteristics. 271 , 272 In addition, the durations of diabetes and obesity are strongly associated with autologous BM-MSC metabolic function, especially mitochondrial respiration, and the accumulation of mitochondrial DNA, which directly interfere with the functions of BM-MSCs and reduce the effectiveness of the therapy. 271 Therefore, the allogeneic approach using MSCs from healthy donors provides an alternative approach for stem cell therapy in the treatment of patients with diabetes.
Infertility and reproductive function recovery
Modern society is increasingly facing the problem of infertility, which is defined as the inability to become pregnant after more than 1 year of unprotected intercourse. 273 This problem has emerged as an important worldwide health issue and social burden. Assisted reproductive techniques and in vitro fertilization technology have recently become the most effective methods for the treatment of infertility in humans, but the use of these approaches is limited, as they cannot be applied in patients with no sperm or those who are unable to support implantation during pregnancy, they are associated with complications, they are time-consuming and expensive, and they are associated with ethical issues in certain territories. 274 Numerous conditions are related to infertility, including POF, nonobstructive azoospermia, endometrial dysfunction, and Asherman syndrome. Recent progress has been illustrated in preclinical studies for the potential applications of stem cell-based therapy for reproductive function recovery, especially recent studies in the field of MSCs, which provide new hope for patients with infertility and reproductive disorders. 275
POF is characterized by a loss of ovarian activity during middle age (before 40 years old) and affects 1–2% of women of reproductive age. 276 Patients diagnosed with POF exhibit oligo-/amenorrhea for at least 4 months, with increased levels of follicle-stimulating hormone (FSH) (>25 IU/L) on two occasions more than 1 month apart. 277 Diverse factors, such as genetic backgrounds, autoimmune disorders, environmental conditions, and iatrogenic and idiopathic situations, have been reported to be the cause of POF. 278 POF can be treated with limited effectiveness via psychosocial support, hormone replacement intervention, and fertility management. 279 MSCs from AT, BM, and UC have been used in the treatment of POF, with improvements in ovarian function in preclinical studies using chemotherapy-induced POF animal models. The early published POF study using BM-MSCs as the main cell source is a single case report in which a perimenopausal woman showed an improvement in follicular regeneration, and increased AMH levels resulted in a successful pregnancy followed by delivery of a healthy infant. 280 A report using autologous BM-MSCs in two women with POF illustrated an increase in baseline estrogen levels and the volume of the treated ovaries along with amelioration of menopausal symptoms. 281 The clinical procedures used in this early trial were invasive, as patients underwent two operations: (1) BM aspiration and (2) laparoscopy. A similar approach was used in two trials conducted in 10 women with POF (age range from 26–33 years old) and 30 patients (age from 18 to 40 years old). 282 A later study investigated two different routes of cell delivery, including laparoscopy and the ovarian artery, but the results have not been reported at this time. 282 Based on the positive outcomes of the mouse model, an autologous stem cell ovarian transplantation (ASCOT) trial was deployed using BM-derived stem cells with encouraging observations of improved ovarian function, as determined by elevated levels of AMH and AFC in 81.3% of participants, six pregnancies, and the successful delivery of three healthy babies. 283 A randomized trial (NCT03535480) was conducted in 20 patients with POF aged less than 39 years to further elaborate on the results of the ASCOT trial. 284 To date, there are no completed trials using AT-MSCs or UC-MSCs in the treatment of patients with POF, limiting the evaluation of these MSCs in the treatment of POF. The speculated reason is that POF is a rare disease, affecting 1% of women younger than 40 years, and with improvements in assisted productive technology, patients have several alternative options to enhance the recovery of reproductive function. 285
Wound healing and skin burns
Burns are the fourth most common injury worldwide, affecting ~11 million people, and are a major cause of death (180,000 patients annually). The severity of burns is defined based on the percentage of surface area burned, burn depth, burn location and patient age, and burns are usually classified into first-, second-, third-, and fourth-degree burns on the basis of their severity. 286 Postburn recovery depends on the severity of the burn and the effectiveness of treatment. Rapid healing may occur over weeks, while alternatively, healing can take months, with the ultimate result being scar formation and disability in patients with severe burns. Different from mechanical injury, burn injury is an invasive progression of damage to tissue at the burn site, including both mechanical damage to the skin surface and biological damage caused by natural apoptosis that prolongs excessive inflammation, oxidative stress, and impaired tissue perfusion. 287 To date, completely reversing the devastating damage of severe burns remains unachievable in medicine, and stem cell therapy provides an alternative option for patients with burn injury. The first case report of the use of BM-MSCs to treat a 45-year-old patient with burns on 40% of their body demonstrated the safety of the therapy and showed partial improvements in vascularization at the wound site and reduced coarse cicatrices. 288 , 289 Later, patients with second- and third-degree burns as well as deep burns were treated using either autologous BM-MSCs or allogeneic BM-MSCs by spraying the MSCs onto the burn sites or adding MSCs over a dermal matrix sheet to cover the wound. The results in these case reports revealed the potential efficacy of MSC-based therapy, which not only enhanced the speed of wound recovery but also reduced pain and improved blood supply without introducing infection. 288 , 290 , 291 In 2017, a study conducted in 60 patients with 10–25% of their total body surface areas burned treated with either autologous BM-MSCs or UC-MSCs showed that both MSC types improved the rate of healing and reduced the hospitalization period. 292 The drawback of BM-MSCs in the treatment of burns is the invasive harvesting method, which causes pain and possible complications in patients. Hence, treatment with allogeneic MSCs obtained from healthy donors is the method of choice, and AT- and UC-MSCs are two suitable candidates for this option. To date, a limited number of clinical trials have been conducted using MSC therapy. These trials have several limitations in trial design, such as a lack of a negative control group and blinding, small sample sizes, and the use of standardized measurement tools for burn injury and wound healing. Currently, AT-MSCs are being used in seven ongoing phase I and II trials in the treatment of burns. Hence, it is important to note that among the most widely studied MSCs, AT-MSCs have advantages over BM-MSCs when obtained from an allogeneic source, while their abilities in burn treatment remain to be determined. The main MSCs that should be used in the regeneration of burn tissue remain undefined (Table 3 ), and we observed the trend that AT-MSCs are more suitable candidates due to their biological nature, which contributes to the generation of keratinocytes and secretion profiles that strongly enhance the skin regeneration process. 293 , 294 , 295 , 296
MSC applications in cardiovascular disease: a promising but still controversial field
In the last two decades, great advancements have been achieved in the development of novel regenerative medicine and cardiovascular research, especially stem cell technology. 297 The discovery of human embryonic stem cells and human induced pluripotent stem cells (hiPSCs) opened a new door for basic research and therapeutic investigation of the use of these cells to treat different diseases. 298 However, the clinical path of hiPSCs and hiPSC-derived cardiomyocytes in the treatment of cardiovascular diseases is limited due to the potential for teratoma formation with hiPSCs and the immaturity of hiPSC-derived cardiomyocytes, which might pose a risk of cancer formation, 299 arrhythmia, and cardiac arrest to patients. 300 A recently emerged stem cell type is adult stem cells/progenitor cells, including MSCs, which can stimulate myocardial repair post administration due to their paracrine effects. Promising results of MSC-based therapy obtained from preclinical studies of cardiac diseases enhance the knowledge and strengthen the clinical research to investigate the safety and efficacy in a clinical trial setting. There are papers that discuss the importance of MSC therapy in the treatment of cardiovascular diseases, with the following references being highly recommended. 301 , 302 , 303 , 304 , 305 , 306 To date, 36 trials have evaluated the therapeutic potential of MSCs in different pathological conditions, with the most prevalent types being BM-MSCs (25 trials), followed by UC-MSCs (7 trials) and AT-MSCs (4 trials). 303 However, the reported results are contradictory and create controversy about the efficacy of the treatments.
One of the first trials using MSCs in the treatment of chronic heart failure was the Cardiopoietic Stem Cell Therapy in Heart Failure (C-CURE) trial, a multicentre, randomized clinical trial that recruited 47 patients. The trial findings supported the safety of BM-MSC therapy and provided a data set that demonstrated improvements in cardiovascular scores along with New York Heart Association functional class, quality of life, and general physical health. 307 Despite these encouraging results in the phase I trial, the treatment failed to achieve the primary outcomes in the phase II/III trial (CHART-1 trial), including no significant improvements in cardiac structure or function or patient quality of life. 308 A positive outcome was also found in a phase I/II, randomized pilot study called the POSEIDON trial, which was the first trial to demonstrate the superior effectiveness of the administration of allogeneic BM-MSCs compared to allogeneic MSCs from other sources. 309 , 310 Published results from the MSC-HF study, with 4 years of follow-up results, 311 , 312 and the TRIDENT study 313 illustrated the positive outcomes of BM-MSCs in the treatment of heart failure. However, a contradictory result from the recently published CONCERT-HF trial demonstrated that the administration of autologous BM-MSCs to patients diagnosed with chronic ischemic heart failure did not improve left ventricular function or reduce scar size at 12 months post administration, but the patient’s quality of life was improved. 314 This observation is similar to that of the TAC-HFT trial 315 but completely different from the reported results of the MSC-HF trial. A comprehensive investigation is still needed to determine the reasons behind these contradictory results. The largest clinical trial to date using BM-MSCs is the DREAM-HF study, which was a randomized, double-blind, placebo-controlled, phase III trial that was conducted at 55 sites across North America and recruited a total of 565 patients with ischemic and nonischaemic heart failure. 172 Although recent reports from the sponsor confirmed that the trial missed its primary endpoint (a reduction in recurrent heart failure-related hospitalization), other prespecified endpoints were met, such as a reduction in overall major adverse cardiac events (including death, myocardial infarction, and stroke). 306 Thus, a complete report from the DREAM-HF trial will provide pivotal data supporting the therapeutic potential of BM-MSCs in the treatment of heart failure and open a new path for the FDA to approve cell-based therapy for cardiovascular diseases.
The early trial using AT-derived cells was the PRECISE trial, which was a phase I, randomized, placebo-controlled, double-blind study that examined the safety and efficacy of adipose-derived regenerative cells (ADRCs) in the treatment of chronic ischemic cardiomyopathy. 316 ADRCs are a homogenous population of cells obtained from the vascular stromal fraction of AT, which contains a small proportion of AT-MSCs. 317 Although the study supported the safety of ADRC administration and illustrated a preserved functional capacity (peak VO 2 ) in the treated group and improvements in heart wall motion, neither poor left ventricle (LV) volume nor poor left ventricular ejection fraction (LVEF) was ameliorated. The follow-up trial of the PRECISE trial, called the ATHENA trial, was conducted in 31 patients, although the study was terminated prematurely because two cerebrovascular events occurred, which were not related to the cell product itself. 318 The results of the study illustrated increases in functional capacity, hospitalization rate, and MLHFQ scores, but the LV volume and LVEF were not significantly different between the two groups. Kastrup and colleagues conducted the first in vitro expanded AT-MSC trial in ten patients with ischemic heart disease and ischemic heart failure in 2017. The results confirmed that ready-to-use AT-MSCs were well-tolerated and potentially effective in the treatment of ischemic heart disease and heart failure. 319 Comparable results of AT-MSCs were also reported from the MyStromalCell Trial, which was a randomized placebo-controlled study. In this trial, 61 patients were randomized at a 2:1 ratio into two groups, with the results showing no significant difference in the primary endpoint, which was a change in the maximal bicycle exercise tolerance test (ETT) score from baseline to 6 months post administration. 320 A 3-year follow-up report from the MyStromalCell Trial confirmed that patients who received AT-MSC administration maintained their preserved exercise capacity and their cardiac symptoms improved, whereas the control group experienced a significant reduction in exercise performance and a worsened cardiovascular condition. 321
UC-MSCs are potential allogeneic cells for the treatment of cardiovascular disease, as they are “ready to use” and easy to isolate, they rapidly proliferate, and they secrete hepatocyte growth factors, 322 which are involved in cardioprotection and cardiovascular regeneration. 323 The pilot study using UC-MSCs in 30 patients with heart failure, called the RIMECARD trial, was the first reported trial for which the results supported the effectiveness of UC-MSCs, as seen in the improved ejection fraction, left ventricular function, functional status, and quality of life in patients administered UC-MSCs. 324 Encouraging results reported from a phase I/II HUC-HEART trial 325 showed improvements in LVEF and reductions in the size of the injured area of the myocardium. However, the opposite observations were also reported from a recently published phase I randomized trial using a combination of UC-MSCs and a collagen scaffold in patients with ischemic heart conditions, in which the size of fibrotic scar tissue was not significantly reduced. 326
Although MSCs from AT, BM, and UC have proven to be safe and feasible in the treatment of cardiovascular diseases, the correlation between the MSC types and their therapeutic potentials is still uncertain because different results have been reported from different clinical trials (Table 4 ). The mechanisms by which MSCs participate in recovery and enhance myocardial regeneration have been discussed comprehensively in a recently published review; 305 , 327 therefore, they will not be discussed in this review. In fact, the challenges of MSC-based therapy in cardiovascular diseases have been clearly described previously, 328 including (1) the lack of an in vitro evaluation of the transdifferentiation potential of MSCs to functional cardiac and endothelial cells, 329 (2) the uncontrollable differentiation of MSCs to undesirable cell types post administration, 330 and (3) the undistinguishable nature of MSCs derived from different sources with various levels of differentiation potential. 331 Therefore, the applications of MSC-based therapy in cardiovascular disease are still in their immature stage, with potential benefits to patients. Thus, there is a need to conduct large-scale, well-designed randomized clinical trials not only to confirm the therapeutic potential of MSCs from various sources but also to enhance our knowledge of cardiovascular regeneration post administration.
Proposed mechanism of BM-MSCs in the treatment of acquired brain and spinal injury
Bones are complex structures constituting a part of the vertebrate skeleton, and they play a vital role in the production of blood cells from HSCs. Similar to the functions of most vertebrate organs, bone function is tightly regulated by its constituents and by long-range signaling from AT and the adrenal glands, parathyroid glands, and nervous system. 332 The central nervous system (CNS) orchestrates the voluntary and involuntary input transmitted by a network of peripheral nerves, which act as the bridge between the nervous system and target organs. The CNS controls involuntary responses via the autonomic nervous system (ANS), consisting of the sympathetic nervous system and the parasympathetic nervous system, and voluntary responses via the somatic nervous system. The ANS penetrates deep into the BM cavity, reaching the regions of hematopoietic activity to deliver neurotransmitters that tightly regulate BM stem cell niches. 333 The BM microenvironment consists of various cell types that participate in the maintenance of HSC niches, which are composed of specialized cells, including BM-MSCs (Fig. 3a ). The release of a specific neurotransmitter, circadian norepinephrine, from the sympathetic nervous system at nerve terminals leads to a reduction in the circadian expression of C–X-C chemokine ligand 12 (CXCL12, which is also known as stromal cell-derived factor-1 (SDF-1)) by Nestin + /NG2 2+ BM-MSCs, resulting in the secretion of HSCs into the peripheral bloodstream. 334 , 335 In fact, BM-MSCs play a significant role in the regulation of HSC quiescence and are closely associated with arterioles and sympathetic nervous system nerve fibers. Nestin-expressing BM-MSCs have been shown to express high levels of SDF-1, stem cell factor (SCF), angiopoietin-1 (Ang-1), interleukin-7, vascular cell adhesion molecule 1 (VCAM-1), and osteopontin (OPN), which are directly involved in the regulation and maintenance of HSC quiescence. 336 The depletion of BM-MSCs in BM leads to the mobilization of HSCs into the peripheral bloodstream and spleen. The findings from a previous study demonstrated that reduced SDF-1 expression in norepinephrine-treated BM-MSCs resulted in the mobilization of CXCR4 + HSCs into circulation. 337 The ability of BM-MSCs to produce SDF-1 is tightly related to their neuronal protective functions. 338 SDF-1 is a member of a chemokine subfamily that orchestrates an enormous diversity of pathways and functions in the CNS, such as neuronal survival and proliferation. The chemokine has two receptors, CXCR4 and CXCR7, that are involved in the pathogenic development of neurodegenerative and neuroinflammatory diseases. 339 In the damaged brain, SDF-1 functions as a stem cell homing signal, and in acquired immune deficiency syndrome (AIDS), SDF-1 has been reported to be involved in the protection of damaged neurons by preventing apoptosis. In a traumatic brain injury model, SDF-1 was found to function as an inhibitor of the caspase-3 pathway by upregulating the Bcl-2/Bax ratio, which in turn protects neurons from apoptosis. 340 Moreover, the release of SDF-1 also facilitates cell recruitment, cell migration, and the homing of neuronal precursor cells in the adult CNS by activating the CXCR4 receptor. 341 , 342 Existing data support that SDF-1 acts as the guiding signal for the regeneration of axon growth in damaged neurons and enhances spinal nerve regeneration. 343 , 344 Hence, the ability of BM-MSCs to express SDF-1 in response to the neuronal environment provides a unique neuronal protective effect that could explain the potential therapeutic efficacy of BM-MSCs in the treatment of neurodegenerative diseases (Fig. 3b ).
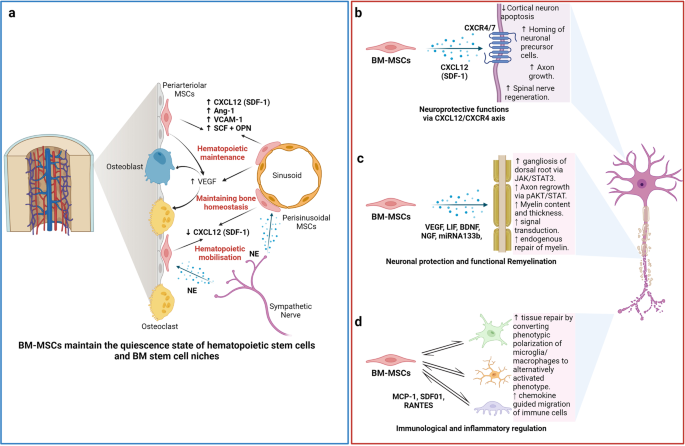
The nature of the “stem niche” of bone marrow-derived mesenchymal stem cells (BM-MSCs) supports their therapeutic potential in neuron-related diseases. a Bone marrow is a complex stem cell niche regulated directly by the central nervous system to maintain bone marrow homeostasis and haematopoietic stem cell (HSC) functions. MSCs in bone marrow respond to the environmental changes through the release of norepinephrine (NE) from the sympathetic nerves that regulate the synthesis of SDF-1 and the migration of HSCs through the sinusoids. The secretion of stem cell factors (SCFs), VCAM-1 and angiotensin-1 from MSCs also plays a significant role in the maintenance of HSCs. b BM-MSCs have the ability to produce and release SDF-1, which directly contributes to neuroprotective functions at the damaged site through interaction with its receptors CXCR4/7, located on the neuronal membrane. c Neuronal protection and the functional remyelination induced by BM-MSCs are also modulated by the release of a wide range of growth factors, including VEGF, BDNF, and NGF, by the BM-MSCs. d BM-MSCs also have the ability to regulate neuronal immune responses by direct interaction or paracrine communication with microglia. Figure was created with BioRender.com
The migration of exogenous MSCs after systemic administration to the brain is limited by the physical blood–brain barrier (BBB), which is a selective barrier formed by CNS endothelial cells to restrict the passage of molecules and cells. The mechanism of molecular movement across the BBB is well established, but how stem cells can bypass the BBB and home to the brain remains unclear. Recent studies have reported that MSCs are able to migrate through endothelial cell sheets by paracellular or transcellular transport followed by migration to the injured or inflammatory site of the brain. 345 , 346 During certain injuries or ischemic events, such as brain injury, stroke, or cerebral palsy, the integrity and efficiency of BBB protection is compromised, which allows MSC migration across the BBB via paracellular transport through the transient formation of interendothelial gaps. 347 CD24 expression has been detected in human BM-MSCs, which are regulated by TGF-β3, 348 allowing them to interact with activated endothelial cells via P-selectin and initiate the tethering and rolling steps of MSCs. 349 Additionally, BM-MSCs express high levels of CXCR4 or CXCR7, 350 , 351 which bind to integrin receptors, such as VLA-4, to activate the integrin-binding process and allow the cells to anchor to endothelial cells, followed by the migration of MSCs through the endothelial cell layer and basement membrane in a process called transmigration. 352 This process is facilitated by the secretion of matrix metalloproteinases (MMPs), which degrade the endothelial basement membrane, allowing BM-MSCs to enter the brain environment. 353 , 354 BM-MSCs can also regulate the integrity of the BBB via the secretion of tissue inhibitor of matrix metalloproteinase-3 (TIMP3), which has been shown to ameliorate the effects of a compromised BBB in traumatic brain injury. 355 The secretion of TIMP3 from MSCs directly blocked vascular endothelial growth factor a (VEGF-a)-induced breakdown of endothelial cell adherent junctions, demonstrating the potential mechanism of BM-MSCs in the regulation of BBB integrity.
The therapeutic applications of BM-MSCs in neurodegenerative conditions have been significantly increased by the demonstration of BM-MSC involvement in axonal and functional remyelination processes. Remyelination is a spontaneous regenerative process occurring in the human CNS to protect oligodendrocytes, neurons, and myelin sheaths from neuronal degenerative diseases. 356 Remyelination is considered a neuroprotective process that limits axonal degeneration by demyelination and neuronal damage. The first mechanism of action of BM-MSCs related to remyelination is the activation of the JAK/STAT3 pathway to regulate dorsal root ganglia development. 357 It was reported that BM-MSCs secrete vascular endothelial growth factor-A (VEGF-A), 358 brain-derived neurotrophic factor (BDNF), interleukin-6, and leukemia inhibitor factor (LIF), which directly function in neurogenesis and neurite growth. 357 VEGF-A is a key regulator of hemangiogenesis during development and bone homeostasis. Postnatally, osteoblast- and MSC-derived VEGF plays a critical role in maintaining and regulating bone homeostasis by stimulating MSC differentiation into osteoblasts and suppressing their adipogenic differentiation. 359 , 360 , 361 To balance osteoblast and adipogenic differentiation, VEGF forms a functional link with the nuclear envelope protein laminin A, which in turn directly regulates the osteoblast and adipocyte transcription factors Runx2 and PPARγ, respectively. 361 , 362 In the brain, VEGF is a potent growth factor mediating angiogenesis, neural migration, and neuroprotection. VEGF-A, secreted from BM-MSCs under in vitro xeno- and serum-free culture conditions, is the most studied member of the VEGF family and is suggested to play a protective role against cognitive impairment, such as in the context of Alzheimer’s disease pathology or stroke. 363 , 364 , 365 Recently, it was reported that the neurotrophic and neuroprotective function of VEGF is mediated through VEGFR2/Flk-1 receptors, which are expressed in the neuroproliferative zones and extend to astroglia and endothelial cells. 366 In animal models of intracerebral hemorrhage and cerebral ischemia, the transfusion of Flk-1-positive BM-MSCs promotes behavioral recovery and anti-inflammatory and angiogenic effects. 367 , 368 Moreover, supplementation with VEGF-A in neuronal disorders enhances intraneural angiogenesis, improves nerve regeneration, and promotes neurotrophic capacities, which in turn increase myelin thickness via the activation of the prosurvival transcription factor nuclear factor-kappa B (NF-kB). This activation, together with the downregulation of Mdm2 and increased expression of the pro-apoptotic transcription factor p53, is considered to be the neuroprotective process associated with an increased VEGF-A level. 369 , 370 , 371 An analysis of microRNA (miRNA) in extracellular vesicles (EVs) secreted from BM-MSCs revealed that BM-MSCs release substantial amounts of miRNA133b, which suppresses the expression of connective tissue growth factor (CTGF) and protects hippocampal neurons from apoptosis and inflammatory injury 372 , 373 , 374 (Fig. 3c ).
In terms of immunoregulatory functions, the administration of human BM-MSCs into immunocompetent mice subjected to SCI or brain ischemia showed that BM-MSCs exhibited a short-term neuronal protective function against neurological damage (Fig. 3d ). Further investigation demonstrated the ability of BM-MSCs to directly communicate with host microglia/macrophages and convert them from phenotypic polarization into alternative activated microglia/macrophages (AAMs), which are key players in axonal extension and the reconstruction of neuronal networks. 375 Other studies have also illustrated that the administration of AAMs directly to the injured spinal cord induced axonal regrowth and functional improvement. 376 The mechanism by which BM-MSCs activate the conversion of microglia/macrophages occurs through two representative macrophage-related chemokine axes, CCL2/CCR2 and CCL-5/CCR5, both of which exhibit acute or chronic elevation following brain injury or SCI. 377 The CCL2/CCR2 axis contributed to the enhancement of inflammatory function, and BM-MSC-mediated induction of CCL2 did not alter the total granulocyte number (Fig. 3d ). Although the chemokine-mediated mechanism of BM-MSCs in the activation of AAMs and enhanced axonal regeneration at the damage sites is evident, the direct mechanism by which the communication between BM-MSCs and the target cells results in these phenomena remains unclear, and further investigation is needed.
BM-MSCs also confer the ability to regulate the inflammatory regulation of the immune cells present in the brain by (1) promoting the polarization of macrophages toward the M2 type, (2) suppressing T-lymphocyte activities, (3) stimulating the proliferation and differentiation of regulatory T cells (Tregs), and (4) inhibiting the activation of natural killer (NK) cells. BM-MSCs secrete glial cell line-derived neurotrophic factor (GDNF), a specific growth factor that contributes directly to the transition of the microglial destructive M1 phenotype into the regenerative M2 phenotype during the neuroinflammatory process. 378 A similar result was also found in AT- 379 and UC-MSCs 380 under neuroinflammation-associated conditions, suggesting that AT-, BM-, and UC-MSCs share the same mechanism in promoting macrophage polarization. In terms of T-lymphocyte suppression, compared to MSCs from AT and BM, UC-MSCs show the strongest potential to inhibit the proliferation of T-lymphocytes by promoting cell cycle arrest (G0/G1 phase) and apoptosis. 381 In addition, UC-MSCs have been proven to be more effective in promoting the proliferation of Tregs 382 and inhibiting NK activation. 383 Although MSCs are well-known for their inflammatory regulatory ability, the mechanism is not exclusive to BM-MSCs, especially in neurological disorders. 384
Proposed mechanism of UC-MSCs in the treatment of pulmonary diseases and lung fibrosis
In contrast to AT-MSCs and BM-MSCs, UC-MSCs have lower expression of major histocompatibility complex I (MHC I) and no expression of MHC II, which prevents the complications of immune rejection. 385 Moreover, as UC is considered a waste product after birth, with the option of noninvasive collection, UC-MSCs are easier to obtain and culture than AD- and BM-MSCs. 386 These advantages of UC-MSCs have contributed to their use in the treatment of pulmonary diseases, especially during the rampant COVID-19 pandemic, as “off-the-shelf” products. Numerous pulmonary diseases have been the subject of applications of UC-MSCs, including BPD, COPD, ARDS, and COVID-19-induced ARDS. In BPD, premature infants are born before the alveolarization process, resulting in arrested lung development and alveolar maturation. Upon administration via an IV route, the majority of exogenous UC-MSCs reach the immature lung and directly interact with immune cells to exert their immunomodulatory properties via cell-to-cell interaction mechanisms (Fig. 4a ). UC-MSCs interact with T cells via the PD-L1 ligand, which binds to the PD-1 inhibitory molecule on T cells, resulting in the suppression of CD3+ T-cell proliferation and effector T-cell responses. 387 In addition, UC-MSCs also express CD54 (ICAM-1), which plays a crucial role in the immunomodulatory functions of T cells. 388 Direct contact between UC-MSCs and macrophages via CD54 expression on UC-MSCs promotes the immune regulation of UC-MSCs via the regulation of phagocytosis by monocytes. 389 Moreover, the contact of UC-MSCs with macrophages during proinflammatory responses increases the secretion of TSG-6 by UC-MSCs, which in turn promotes the inhibitory regulation of CD3+ T cells, macrophages, and monocytes by MSCs. 390 Recently, upregulation of SDF-1 was described in neonatal lung injury, especially in layers of the respiratory epithelium. 391 SDF-1 has been shown to participate in the migration and initiation of the homing process of MSCs via the CXCR4 receptors on their surface. 392 It was reported that UC-MSCs express low levels of CXCR4, allowing them to induce SDF-1-associated migration processes via the Akt, ERK, and p38 signal transduction pathways. 393 Hence, in BPD, the upregulation of SDF-1 together with the homing ability of UC-MSCs strongly supports the therapeutic effects of UC-MSCs in the treatment of BPD. Furthermore, UC-MSCs have the ability to communicate with immune cells via cell-to-cell contact to reduce proinflammatory responses and the production of proinflammatory cytokines (such as TGF-β, INF-γ, macrophage MIF, and TNF-α). The modulation of the human innate immune system by UC-MSCs is mediated by cell–cell interactions via CD54-LFA-1 that switch macrophage polarization processes, promoting the proliferation of M2 macrophages, which in turn reduce inflammatory responses in the immature lung. 394 Moreover, UC-MSCs also have the ability to produce VEGF and hepatocyte growth factors (HGFs), promoting angiogenesis and enhancing lung maturation. 395
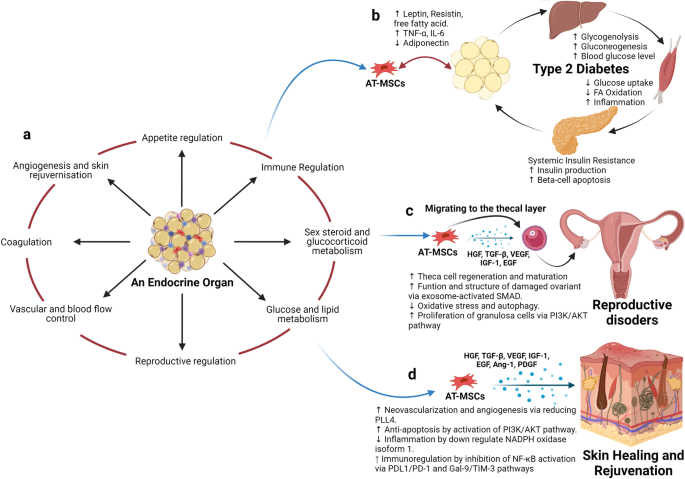
Adipose tissue-derived mesenchymal stem cells (AT-MSCs) and the nature of their tissue of origin support their use in therapeutic applications. a Adipose tissue is considered an endocrine organ, supporting and regulating various functions, including appetite regulation, immune regulation, sex hormone and glucocorticoid metabolism, energy production, the orchestration of reproduction, the control of vascularization, and blood flow, the regulation of coagulation, and angiogenesis and skin regeneration. b In terms of metabolic disorders, such as type 2 diabetes mellitus (T2DM), as adipose tissue is directly involved in the metabolism of glucose and lipids and the regulation of appetite, the detrimental effects of T2DM also alter the functions of AT-MSCs, which in turn, hampers their therapeutic effects. Hence, the use of autologous AT-MSCs is not recommended for the treatment of metabolic disorders, including T2DM, suggesting that allogeneic AT-MSCs from healthy donors could be a better alternative approach. c AT-MSCs are suitable for the treatment of reproductive disorders due to their unique ability to mobilize and home to the thecal layer of the injured ovary, enhance the regeneration and maturation of thecal cells, increase the structure and function of damaged ovaries via exosome-activated SMAD, decrease oxidative stress and autophagy, and increase the proliferation of granulosa cells via PI3K/AKT pathways. These functions are regulated specifically by growth hormones produced by AT-MSCs in response to the surrounding environment, including HGF, TGF-β, IGF-1, and EGF. d AT-MSCs are also good candidates for skin healing and regeneration as their growth factors strongly support neovascularization and angiogenesis by reducing PLL4, increase anti-apoptosis via the activation of PI3K/AKT pathways, regulate inflammation by downregulating NADPH oxidase isoform 1, and increase immunoregulation through the inhibition of NF-κB activation. The figure was created with BioRender.com
COPD is characterized by an increase in hyperinflammatory reactions in the lung, compromising lung function and increasing the development of lung fibrosis. The mechanism by which UC-MSCs contribute to the response to COPD is inflammatory regulation (Fig. 4b ). The administration of UC-MSCs prevented the infiltration of inflammatory cells in peribronchiolar, perivascular, and alveolar septa and switched macrophage polarization to M2. 396 A significant reduction in proinflammatory cytokines, including IL-1β, TNF-α, and IL-8, was also observed following UC-MSC administration. 224 MSCs, including UC-MSCs, have been reported to trigger the production of secretory leukocyte protease inhibitors in epithelial cells through the secretion of HGF and epidermal growth factor (EGF), which is believed to have beneficial effects on COPD. 397 , 398 In addition to their inflammatory regulation ability, UC-MSCs exhibit antimicrobial effects through the inhibition of bacterial growth and the alleviation of antibiotic resistance during Pseudomonas aeruginosa infection. 399 The combination of the regulation of the host immune response and the antimicrobial effects of UC-MSCs may be relevant for the prevention and treatment of COPD exacerbations, as inflammation and bacterial infections are important risk factors that significantly contribute to the morbidity and mortality of patients with COPD. In terms of regenerative functions, UC-MSCs were reported to be able to differentiate into type 2 alveolar epithelial cells in vitro and alleviate the development of pulmonary fibrosis via β-catenin-regulated cell apoptosis. 400 Furthermore, UC-MSCs enhanced alveolar epithelial cell migration and proliferation by increasing matrix metalloproteinase-2 levels and reduced their endogenous inhibitors, tissue inhibitors of matrix metalloproteinases, providing a potential mechanism underlying their anti-pulmonary-fibrosis effects. 401 , 402
In ARDS, especially that associated with COVID-19, the proinflammatory state is initiated by increases in plasma concentrations of proinflammatory cytokines, such as IL-1 beta, IL-7, IL-8, IL-9, IL-10, bFGF, granulocyte colony-stimulating factor (G-CSF), GM-CSF, IFN-γ, and TNF-α. The significant increases in the concentrations of these cytokines in patient plasma suggest the development of a cytokine storm, which is a leading cause of COVID-induced mortality. In addition to the immunomodulatory functions regulated via cell-to-cell interactions between UC-MSCs and immune cells, such as macrophages, monocytes, and T cells, UC-MSCs exert their functions via paracrine effects through the secretion of growth factors, cytokines, and exosomes (Fig. 4c ). The most relevant immunomodulatory function of UC-MSCs is considered to be their inhibition of effector T cells via the induction of T-cell apoptosis and cell cycle arrest by the production of indoleamine 2,3- dioxygenase (IDO), prostaglandin E2 (PGE-2), and TGF-β. Elevated levels of PGE-2 in patients with COVID-19 are reported to be a crucial factor in the initiation of inflammatory regulation by UC-MSCs post administration and prevent the development of cytokine storms by direct inhibition of T- and B lymphocytes. 403 UC-MSCs exert these inhibitory activities through a PGE-2-dependent mechanism. 404 It was reported that UC-MSCs confer the ability to secrete tolerogenic mediators, including TGF-β1, PGE-2, nitric oxide (NO), and TNF-α, which are directly involved in their immunoregulatory mechanism. The secretion of NO from UC-MSCs is reported to be associated with the desensitization of T cells via the IFN-inducible nitric oxide synthase (iNOS) pathways and to stimulate the migration of T cells in close proximity to MSCs that subsequently suppress T-cell sensitivities via NO. 405 Lung infection with viruses usually leads to impairments in alveolar fluid clearance and protein permeability. The administration of UC-MSCs enhances alveolar protection and restores fluid clearance in patients with COVID-19. UC-MSCs secrete growth factors associated with angiogenesis and the regeneration of pulmonary blood vessels and micronetworks, including angiotensin-1, VEGF, and HGF, which also reduce oxidative stress and prevent fibrosis formation in the lungs. These trophic factors have been identified as key players in the modulation of the microenvironment and promote pulmonary repair. Additionally, UC-MSCs are more effective than BM-MSCs in the restoration of impaired alveolar fluid clearance and the permeability of airways in vitro, supporting the use of UC-MSCs in the treatment of patients with pulmonary pneumonia. 406 In the context of pulmonary regeneration, UC-MSCs were shown to inhibit apoptosis and fibrosis in pulmonary tissue by activating the PI3K/AKT/mTOR pathways via the secretion of HGF, which also acts as an inhibitory stimulus that blocks alveolar epithelial-to-mesenchymal transition. 407 , 408 Moreover, UC-MSCs can reverse the process of fibrosis via enhanced expression of macrophage matrix-metallopeptidase-9 for collagen degradation and facilitate alveolar regeneration via Toll-like receptor-4 signaling pathways. 409 UC-MSCs were shown to communicate with CD4+ T cells through HGF induction not only to inhibit their differentiation into Th17 cells, reducing the secretion of IL-17 and IL-22 but also to switch their differentiation into regulatory T cells. 410 , 411 In addition, UC-MSCs conferred the ability to facilitate the number of M2 macrophages and reduce M1 cells via the control of the macrophage polarization process. 412
There are several potential mechanisms of UC-MSCs in the treatment of patients with pulmonary diseases and pneumonia, including the regulation of immune cell function, immunomodulation, the enhancement of alveolar fluid clearance and protein permeability, the modulation of endoplasmic reticulum stress, and the attenuation of pulmonary fibrosis. Hence, based on these discussions, UC-MSCs are recommended as suitable candidates for the treatment of pulmonary disease both in pediatric and adult patients.
Proposed mechanism of AT-MSCs in the treatment of endocrinological diseases, reproductive disorders, and skin burns
Human AT was first viewed as a passive reservoir for energy storage and later as a major site for sex hormone metabolism, the production of endocrine factors (such as adipsin and leptin), and a secretion source of bioactive peptides known as adipokines. 413 It is now clear that AT functions as a complex and highly active metabolic and endocrine organ, orchestrating numerous different biological features 414 (Fig. 5a ). In addition to adipocytes, AT contains hematopoietic-derived progenitor cells, connective tissue, nerve tissue, stromal cells, endothelial cells, MSCs, and pericytes. AT-MSCs and pericytes mobilize from their perivascular locations to aid in healing and tissue regeneration throughout the body. As AT is involved directly in energy storage and metabolism, AT-MSCs are also mediated and regulated by growth factors related to these pathways. In particular, interleukin-6 (IL-6), IL-33, and leptin regulate the maintenance of metabolic activities by increasing insulin sensitivity and preserving homeostasis related to AT. Nevertheless, in the development of obesity and diabetes, omental and subcutaneous AT maintains a low-grade state of inflammation, resulting in the impairment of glucose metabolism and potentially contributing to the development of insulin resistance. 415 In normal AT, direct regulation of Pre-B-cell leukemia homeobox (Pbx)-regulating protein-1 (PREP1) by leptin and thyroid growth factor-beta 1 (TGF-β1) in AT-MSCs and mature adipocytes is involved in the protective function and maintenance of AT homeostasis. However, under diabetic conditions, the balance between the expression of leptin and the secretion of TGF-β1 is compromised, resulting in the malfunction of AT-MSC metabolic activity and the proliferation, differentiation, and maturation of adipocytes. Therefore, the use of autologous AT-MSCs in the treatment of diabetic conditions is not a suitable option, as the functions of AT-MSCs are directly altered by diabetic conditions, which reduces their effectiveness in cell-based therapy (Fig. 5b ).
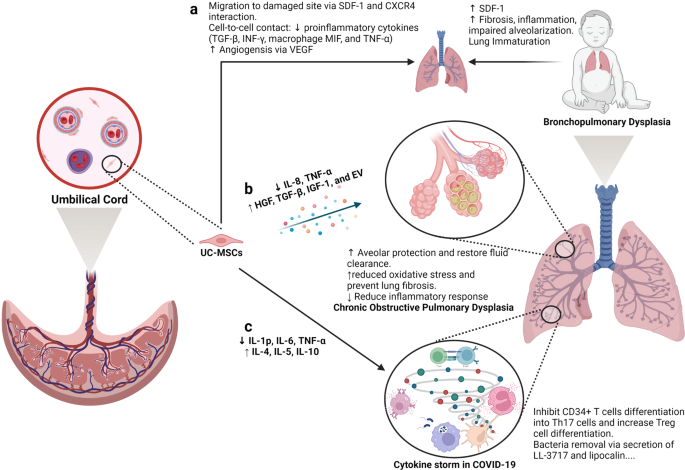
Umbilical cord-derived mesenchymal stem cells (UC-MSCs) are good candidates for the treatment of pulmonary diseases. a Lung immaturity and fibrosis are the major problems of patients with bronchopulmonary dysplasia and lead to increased levels of SDF-1, the development of fibrosis, the induction of the inflammatory response, and the impairment of alveolarization. UC-MSCs are attracted to the damaged lung via the chemoattractant SDF-1, which is constantly released from the immature lung via SDF-1 and CXCR4 communication. Moreover, UC-MSCs reduce the level of proinflammatory cytokines (TGF-β, INF-γ, macrophage MIF, and TNF-α) via a cell-to-cell contact mechanism. The ability of UC-MSCs to produce and secrete VEGF also involves in the regeneration of the immature lung through enhanced angiogenesis. b Upon an exacerbation of chronic obstructive pulmonary disease (COPD), UC-MSCs respond to the surrounding stimuli by reducing IL-8 and TNF-α levels, resulting in the inhibition of the inflammatory response but an increase in the secretion of growth factors participating in the protection of alveoli, fluid clearance and reduced oxidative stress and lung fibrosis, including HGF, TGF-β, IGF-1, and exosomes. c In a similar manner, UC-MSCs prevent the formation of cytokine storms in coronavirus disease 2019 (COVID-19) by inhibiting CD34+ T-cell differentiation into Th17 cells and enhancing the number of regulatory T cells. Moreover, UC-MSCs also have antibacterial activity by secreting LL-3717 and lipocalin. Figure was created with BioRender.com
Preclinical studies and clinical trials have revealed the therapeutic effects of MSCs, in general, and AT-MSCs, in particular, in the management of POF, with relatively high efficacy and enhanced regeneration of the ovaries. Understanding the molecular and cellular mechanisms underlying these effects is the first step in the development of suitable MSC-based therapies for POF. One of the mechanisms by which MSCs exert their therapeutic effects is their ability to migrate to sites of injury, a process known as “homing”. Studies have shown that MSCs from different sources have the ability to migrate to different compartments of the injured ovary. For example, BM-MSCs administered through IV routes migrated mostly to the ovarian hilum and medulla, 416 whereas a significant number of UC-MSCs were found in the medulla. 417 Interestingly, AT-MSCs were found to be engrafted in the theca layers of the ovary but not in the follicles, where they acted as supportive cells to promote follicular growth and the regeneration of thecal layers. 418 The structure and function of the thecal layer have a great impact on fertility, which has been reviewed elsewhere. 419 In brief, the thecal layer consists of two distinct parts, the theca interna, which contains endocrine cells, and the theca externa, which is an outer fibrous layer. The thecal layer contains not only endocrine-derived cells but also vascular- and immune-derived cells, whose functions are to maintain the structural integrity of the follicles, transport nutrients to the inner compartment of the ovary and produce key reproductive hormones such as androgens (testosterone and dihydrotestosterone) and growth factors (morphogenic proteins, e.g., BMPs and TGF-β). 420 As AT-MSCs originate from an endocrine organ, their ability to sense signals and migrate to the thecal layer is anticipated. Additionally, secretome analysis of AT-MSCs showed a wide range of growth factors, including HGF, TBG-β, VEGF, insulin-like growth factor-1 (IGF-1), and EGF, 421 that are directly involved in the restoration of the structure and function of damaged ovaries by stimulating cell proliferation and reducing the aging process of oocytes via the activation of the SIRT1/FOXO1 pathway, a key regulator of vascular endothelial homeostasis. 422 , 423 In POF pathology, autophagy and its correlated oxidative stress contribute to the development of POF throughout a patient’s life. Recently, AT-MSCs were shown to be able to improve the structure and function of mouse ovaries by reducing oxidative stress and inflammation, providing essential data supporting the mechanism of AT-MSCs in the treatment of POF. 424 Several studies have illustrated that AT-MSCs secrete biologically active EVs that regulate the proliferation of ovarian granulosa cells via the PI3K/AKT pathway, resulting in the enhancement of ovarian function. 425 Direct regulation of ovarian cell proliferation modulates the state of these cells, which in turn restores the ovarian reserve. 426 Other mechanisms supporting the effectiveness of MSCs have been carefully reviewed, confirming the therapeutic potential of MSCs derived from different sources 426 (Fig. 5c ).
In the last decade, the number of clinical trials using AT-MSCs in the treatment of chronic skin wounds and skin regeneration has exponentially increased, with data supporting the enhancement of the skin healing processes, the reduction of scar formation, and improvements in skin structure and quality. Several mechanisms are directly linked to the origin of AT-MSCs, including differentiation ability, neovascularization, anti-apoptosis, and immunological regulation. AT is a connective and supportive tissue positioned just beneath the skin layers. AT-MSCs have a strong ability to differentiate into adipocytes, endothelial cells, 427 epithelial cells 428 and muscle cells. 429 The adipogenic differentiation of AT-MSCs is one of the three mesoderm lineages that defines MSC features, and AT-MSCs are likely to be the best MSC type harboring this ability compared to BM- and UC-MSCs. Recent reports detailed that AT-MSCs accelerated diabetic wound tissue closure through the recruitment and differentiation of endothelial cell progenitor cells into endothelial cells mediated by the VEGF-PLCγ-ERK1/ERK2 pathway. 430 Upon injury, the skin must be healed as quickly as possible to prevent inflammation and excessive blood loss. The reparation process occurs through distinct overlapping phases and involves various cell types and processes, including endothelial cells, keratinocyte proliferation, stem cell differentiation, and the restoration of skin homeostasis. 431 Hence, the differentiation ability of AT-MSCs plays a critical role in their therapeutic effect on skin wound regeneration and healing processes. AT-MSCs accelerate wound healing via the production of exosomes that serve as paracrine factors. It was reported that AT-MSCs responded to skin wound injury stimuli by increasing their expression of the lncRNA H19 exosome, which upregulated SOX9 expression via miR-19b, resulting in the acceleration of human skin fibroblast proliferation, migration, and invasion. 432 In addition, the engraftment of AT-MSCs supported wound bed blood flow and epithelialization processes. 433 Anti-apoptosis plays a critical role in AT-MSC-based therapy, as without a microvascular supply network established within 4 days post injury, adipocytes undergo apoptosis and degenerate. Exogenous sources of AT-MSCs mediate anti-apoptosis via IGF-1 and exosome secretion by triggering the activation of PI3K signaling pathways. 434 Another mechanism supporting the therapeutic potential of AT-MSCs is their anti-inflammatory function, which results in the reduction of proinflammatory factors, such as tumor necrosis factor (TNF) and interferon-γ (IFN-γ), and increases the production of the anti-inflammatory factors IL-10 and IL-4. Exosomes from AT-MSCs in response to a wound environment were found to contain high levels of Nrf2, which downregulated wound NADPH oxidase isoform 1 (NOX1), NADPH oxidase isoform 4 (NOX4), IL-1β, IL-6, and TNF-α expression. The anti-inflammatory functions of AT-MSCs are also regulated by their immunomodulatory ability, partially through the inhibition of NF-κB activation in T cells via the PD-L1/PD-1 and Gal-9/TIM-3 pathways, providing a novel target for the acceleration of wound healing 435 (Fig. 5d ).
Therefore, as an endocrine organ in the human body, AT and its derivative stem cells, including AT-MSCs, have shown great potential in the treatment of reproductive disorders and skin diseases. Their potential is supported by mechanisms that are directly related to the nature of AT-MSCs in the maintenance of tissue homeostasis, angiogenesis, anti-apoptosis, and the regulation of inflammatory responses.
The current challenges for MSC-based therapies
Over the past decades, MSC-based research and therapy have made tremendous advancements due to their advantages, including immune evasion, diverse tissue sources for harvesting, ease of isolation, rapid expansion, and cryopreservation as “off-the-shelf” products. However, several important challenges have to be addressed to further enhance the safety profile and efficacy of MSC-based therapy. In our opinion, the most important challenge of MSC-based therapy is the fate of these cells post administration, especially the long-term survival of allogeneic cells in the treatment of certain diseases. Although reported data confirm that the majority of MSCs are trapped in the lung and rapidly removed from the circulation, caution has been raised related to the occurrence of embolism events post infusion, which was proven to be related to MSC-induced innate immune attack (called instant blood-mediated inflammatory reaction). 436 Another related challenge is the homing ability of infused cells, as successful homing at targeted tissue might result in long-term benefits to patients. Other concerns related to MSC-based therapy are the number of dead cells infused into the patients. An interesting study reported that dead MSCs alone still exerted the same immunomodulatory property as live MSCs by releasing phosphatidylserine. 437 This is an interesting observation, as there is always a certain number of dead cells present in the cell-based product, and concerns are always raised related to their effects on the patient’s health. Finally, the hypothesis presented in this review is also a great challenge of the field, which has been proposed for future studies to answer the question: “What is the impact of MSC sources on their downstream application?”. Tables 5 and 6 illustrate the comparative studies that were conducted in preclinical and clinical settings to address the MSC source challenge. Other challenges of MSC-based therapies have been discussed in several reviews and systematic studies, 135 , 185 , 438 , 439 which are highly recommended.
Limitations of the current hypothesis
The proposed hypothesis presented in this review was made based on (1) the calculated number of recovered patients from published clinical trials; (2) the empirical experience of the authors in the treatment of brain-related diseases, 440 pulmonary disorders, 215 and endocrinological conditions; 271 , 441 and (3) the proposed mechanisms by which each type of MSC exhibits its best potential for downstream applications. The authors understand that the approach that we used has a certain level of research bias, as a comprehensive meta-analysis is needed to first confirm the correlation between the origins of MSCs and their downstream clinical outcomes before a complete hypothesis can be made. However, to date, a limited number of clinical trials have been conducted to directly compare the efficacy of MSCs from different sources in treating the same disease, which in turn dampened our analysis to prove this hypothesis. In addition, MSC-based therapy is still in its early stages, as controversy and arguments are still present in the field, including (1) the name of MSCs (medicinal signaling cells vs. MSCs or mesenchymal stromal cells), 442 , 443 (2) the existence of “magic cells” (one cell type for the treatment of all diseases), 444 , 445 (3) the conflicting results from large-scale clinical trials, 135 and (4) the dangerous issues of unauthorized, unproven stem cell therapies and clinics. 446 , 447 Therefore, our hypothesis is proposed at this time to encourage active researchers and clinicians to either prove or disprove it so that future research can strengthen the uses of MSC-based therapies with solid mechanistic study results and clarify results for “one cell type for the treatment of all diseases”.
Another limitation is the knowledge coverage in the field of MSC-based regenerative medicine, as discussed in this study. First, the abovementioned diseases were narrowed to four major disease categories for which MSC-based therapy is widely applied, including neuronal, pulmonary, cardiovascular, and endocrinological conditions. In fact, other diseases also receive great benefits from MSC therapy, including liver cirrhosis, 448 bone regeneration, 360 plastic surgery, 449 autoimmune disease, 450 etc., which are not fully discussed in this review and included in our hypothesis. Recently, the secretome profile of MSCs and its potential application in clinical settings have emerged as a new player in the field, with a recently published comprehensive review including MSC-derived exosomes. 451 , 452 To date, the therapeutic potential of MSCs is believed to be strongly influenced by their secretomes, including growth factors, cytokines, chemokines, and exosomes. 453 However, this body of knowledge is also not fully included in our discussion, as this review focuses on the function and potency of MSCs as a whole with considerations derived from published clinical data. Therefore, the authors believe in and support the future applications of the secreted components derived from MSCs, including exosomes, in the treatment of human diseases. In fact, this potential approach could elevate the uses of MSCs to the next level, where the sources of MSCs could be neglected with advancements in the development of protocols that allow strict control of the secretome profiles of MSCs under specific conditions. 454 , 455 , 456 Finally, strategies that could potentially enhance the therapeutic outcomes of MSC-based therapy, such as the “priming” process, are not discussed in this review. The idea of “priming” MSCs is based on the nature of MSCs, which is similar to the immune cells, 457 that MSCs have proven to be able to “remember” the stimulus from the surrounding environment. 458 , 459 Thus, activating or priming MSCs using certain conditions, such as hypoxia, matrix mechanics, 3D environment, hormones, or inflammatory cytokines, could trigger the memory mechanism of the MSCs in vitro so that these cells are ready to function towards specific therapeutic activities without the need for in vivo activation. 3 , 460
From a cellular and molecular perspective and from our own experience in a clinical trial setting, AD-, BM- and UC-MSCs exhibit different functional activities and treatment effectiveness across a wide range of human diseases. In this paper, we have provided up-to-date data from the most recently published clinical trials conducted in neuronal diseases, endocrine and reproductive disorders, skin regeneration, pulmonary dysplasia, and cardiovascular diseases. The implications of the results and discussions presented in this review and in a very large body of comprehensive and excellent reviews as well as systematic analyses in the literature provide a different aspect and perspective on the use of MSCs from different sources in the treatment of human diseases. We strongly believe that the field of regenerative medicine and MSC-based therapy will benefit from active discussion, which in turn will significantly advance our knowledge of MSCs. Based on the proposed mechanisms presented in this review, we suggest several key mechanistic issues and questions that need to be addressed in the future:
The confirmation and demonstration of the mechanism of action prove that tissue origin plays a significant role in the downstream applications of the originated MSCs.
Is it required that MSCs derived from particular cell sources need to have certain functionalities that are unique to or superior in the original tissue sources?
As mechanisms may rely on the secretion of factors from MSCs, it is important to identify the specific stimuli from the wound environments to understand how MSCs from different sources can exhibit similar functions in the same disease and whether or not MSCs derived from a particular source have stronger effects than their counterparts derived from other tissue sources.
Should we create “universal” MSCs that could be functionally equal in the treatment of all diseases regardless of their origin by modeling their genetic materials?
Can new sources of MSCs from either perinatal or adult tissues better stimulate the innate mechanisms of specific cell types in our body, providing a better tool for MSC-based treatment?
A potential ‘priming’ protocol that allows priming, activating, and switching the potency of MSCs from one source to another with a more appropriate clinical phenotype to treat certain diseases. This idea is potentially relevant to our suggestion that each MSC type could be more beneficial in downstream applications, and the development of such a “priming” protocol would allow us to expand the bioavailability of specific MSC types.
From our clinical perspective, the underlying proposal in our review is to no longer use MSCs for applications while disregarding their sources but rather to match the MSC tissue source to the application, shifting from one cell type for the treatment of all diseases to cell source-specific disease treatments. Whether the application of MSCs from different sources still shows their effectiveness to a certain extent in the treatment of diseases or not, the transplantation of MSCs derived from different sources for each particular disease needs to be further investigated, and protocols need to be established via multicentre, randomized, placebo-controlled phase II and III clinical trials (Fig. 6 ).
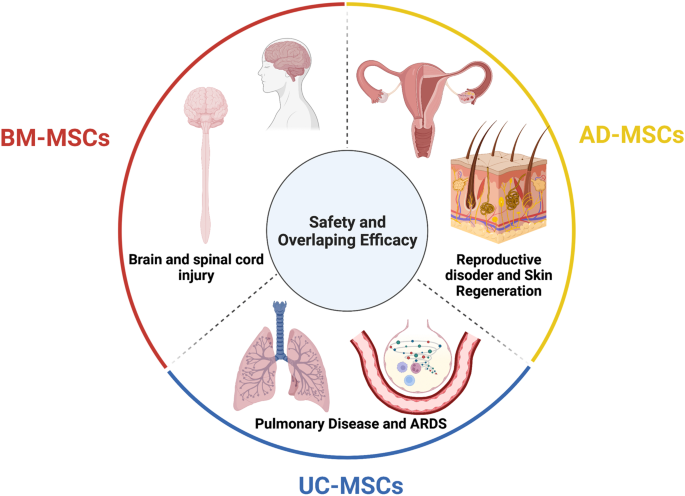
The tissue sources of mesenchymal stem cells (MSCs) contribute greatly to their therapeutic potential, as all MSC types share safety profiles and overlapping efficacy. Although a large body of data and their review and systematic analysis indicated the shared safety and potential efficacy of MSCs derived from different tissue sources, targeted therapies considering MSC origin as an important factor are imperative to enhance the downstream therapeutic effects of MSCs. We suggest that bone marrow-derived MSCs (BM-MSCs) are good candidates for the treatment of brain and spinal cord injury, adipose tissue-derived MSCs (AT-MSCs) are suitable for the treatment of reproductive disorders and skin regeneration, and umbilical cord-derived MSCs (UC-MSCs) could be alternatives for the treatment of pulmonary diseases and acute respiratory distress syndrome (ARDS). Figure was created with BioRender.com
Data availability
All data generated or analyzed in this study are included in this published article.
Mellman, I., Coukos, G. & Dranoff, G. Cancer immunotherapy comes of age. Nature 480 , 480–489 (2011).
Article PubMed PubMed Central CAS Google Scholar
Ancans, J. Cell therapy medicinal product regulatory framework in Europe and its application for MSC-based therapy development. Front. Immunol. 3 , 253 (2012).
Article PubMed PubMed Central Google Scholar
Yin, J. Q., Zhu, J. & Ankrum, J. A. Manufacturing of primed mesenchymal stromal cells for therapy. Nat. Biomed. Eng. 3 , 90–104 (2019).
Article PubMed CAS Google Scholar
O’Brien, T. & Barry, F. P. Stem cell therapy and regenerative medicine. Mayo Clin. Proc. 84 , 859–861 (2009).
Mousaei Ghasroldasht, M., Seok, J., Park, H. S., Liakath Ali, F. B. & Al-Hendy, A. Stem cell therapy: from idea to clinical practice. Int. J. Mol. Sci . 23 , 2850 (2022).
Kuriyan, A. E. et al. Vision loss after intravitreal injection of autologous “stem cells” for AMD. N. Engl. J. Med. 376 , 1047–1053 (2017).
Biehl, J. K. & Russell, B. Introduction to stem cell therapy. J. Cardiovasc. Nurs. 24 , 98–103 (2009). quiz 104-105.
Srijaya, T. C., Ramasamy, T. S. & Kasim, N. H. Advancing stem cell therapy from bench to bedside: lessons from drug therapies. J. Transl. Med. 12 , 243 (2014).
Ramalho-Santos, M. & Willenbring, H. On the origin of the term “stem cell”. Cell Stem Cell 1 , 35–38 (2007).
Konstantinov, I. E. In search of Alexander A. Maximow: the man behind the unitarian theory of hematopoiesis. Perspect. Biol. Med. 43 , 269–276 (2000).
Droscher, A. Images of cell trees, cell lines, and cell fates: the legacy of Ernst Haeckel and August Weismann in stem cell research. Hist. Philos. Life Sci. 36 , 157–186 (2014).
Article PubMed Google Scholar
Jansen, J. The first successful allogeneic bone-marrow transplant: Georges Mathe. Transfus. Med. Rev. 19 , 246–248 (2005).
Blume, K. G. & Weissman, I. L. E. Donnall Thomas (1920-2012). Proc. Natl Acad. Sci. USA 109 , 20777–20778 (2012).
Cheng, M. Hartmann Stahelin (1925-2011) and the contested history of cyclosporin A. Clin. Transpl. 27 , 326–329 (2013).
Article CAS Google Scholar
Thomas, E. D. et al. Aplastic anaemia treated by marrow transplantation. Lancet 1 , 284–289 (1972).
Friedenstein, A. J., Chailakhyan, R. K. & Gerasimov, U. V. Bone marrow osteogenic stem cells: in vitro cultivation and transplantation in diffusion chambers. Cell Tissue Kinet. 20 , 263–272 (1987).
PubMed CAS Google Scholar
Friedenstein, A. J., Chailakhjan, R. K. & Lalykina, K. S. The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet. 3 , 393–403 (1970).
Caplan, A. I. Mesenchymal stem cells. J. Orthop. Res. 9 , 641–650 (1991).
Bolli, R., Tang, X. L., Guo, Y. & Li, Q. After the storm: an objective appraisal of the efficacy of c-kit+ cardiac progenitor cells in preclinical models of heart disease. Can. J. Physiol. Pharm. 99 , 129–139 (2021).
Liu, C., Han, D., Liang, P., Li, Y. & Cao, F. The current dilemma and breakthrough of stem cell therapy in ischemic heart disease. Front. Cell Dev. Biol. 9 , 636136 (2021).
Zhang, J. et al. Basic and translational research in cardiac repair and regeneration: JACC state-of-the-art review. J. Am. Coll. Cardiol. 78 , 2092–2105 (2021).
Gyongyosi, M., Wojakowski, W., Navarese, E. P., Moye, L. A. & Investigators, A. Meta-analyses of human cell-based cardiac regeneration therapies: controversies in meta-analyses results on cardiac cell-based regenerative studies. Circ. Res. 118 , 1254–1263 (2016).
Okamoto, R., Matsumoto, T. & Watanabe, M. Regeneration of the intestinal epithelia: regulation of bone marrow-derived epithelial cell differentiation towards secretory lineage cells. Hum. Cell 19 , 71–75 (2006).
Gehart, H. & Clevers, H. Tales from the crypt: new insights into intestinal stem cells. Nat. Rev. Gastroenterol. Hepatol. 16 , 19–34 (2019).
Santos, A. J. M., Lo, Y. H., Mah, A. T. & Kuo, C. J. The intestinal stem cell niche: homeostasis and adaptations. Trends Cell Biol. 28 , 1062–1078 (2018).
Roda, G. et al. Crohn’s disease. Nat. Rev. Dis. Prim. 6 , 22 (2020).
Kobayashi, T. et al. Ulcerative colitis. Nat. Rev. Dis. Prim. 6 , 74 (2020).
Gratwohl, A. et al. Autologous hematopoietic stem cell transplantation for autoimmune diseases. Bone Marrow Transpl. 35 , 869–879 (2005).
Kashyap, A. & Forman, S. J. Autologous bone marrow transplantation for non-Hodgkin’s lymphoma resulting in long-term remission of coincidental Crohn’s disease. Br. J. Haematol. 103 , 651–652 (1998).
Hurley, J. M., Lee, S. G., Andrews, R. E. Jr., Klowden, M. J. & Bulla, L. A. Jr. Separation of the cytolytic and mosquitocidal proteins of Bacillus thuringiensis subsp. israelensis. Biochem Biophys. Res. Commun. 126 , 961–965 (1985).
Oyama, Y. et al. Autologous hematopoietic stem cell transplantation in patients with refractory Crohn’s disease. Gastroenterology 128 , 552–563 (2005).
Burt, R. K. et al. Autologous nonmyeloablative hematopoietic stem cell transplantation in patients with severe anti-TNF refractory Crohn disease: long-term follow-up. Blood 116 , 6123–6132 (2010).
Hasselblatt, P. et al. Remission of refractory Crohn’s disease by high-dose cyclophosphamide and autologous peripheral blood stem cell transplantation. Aliment Pharm. Ther. 36 , 725–735 (2012).
Hawkey, C. J. et al. Autologous hematopoetic stem cell transplantation for refractory Crohn disease: a randomized clinical trial. J. Am. Med. Assoc. 314 , 2524–2534 (2015).
Lindsay, J. O. et al. Autologous stem-cell transplantation in treatment-refractory Crohn’s disease: an analysis of pooled data from the ASTIC trial. Lancet Gastroenterol. Hepatol. 2 , 399–406 (2017).
Wang, R. et al. Stem cell therapy for Crohn’s disease: systematic review and meta-analysis of preclinical and clinical studies. Stem Cell Res Ther. 12 , 463 (2021).
Hawkey, C. J. Hematopoietic stem cell transplantation in Crohn’s disease: state-of-the-art treatment. Dig. Dis. 35 , 107–114 (2017).
Si-Tayeb, K., Lemaigre, F. P. & Duncan, S. A. Organogenesis and development of the liver. Dev. Cell 18 , 175–189 (2010).
Xue, R. et al. Clinical performance of stem cell therapy in patients with acute-on-chronic liver failure: a systematic review and meta-analysis. J. Transl. Med. 16 , 126 (2018).
Shi, M. et al. Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem Cells Transl. Med. 1 , 725–731 (2012).
Liu, Y., Dong, Y., Wu, X., Xu, X. & Niu, J. The assessment of mesenchymal stem cells therapy in acute on chronic liver failure and chronic liver disease: a systematic review and meta-analysis of randomized controlled clinical trials. Stem Cell Res. Ther. 13 , 204 (2022).
Lin, B. L. et al. Allogeneic bone marrow-derived mesenchymal stromal cells for hepatitis B virus-related acute-on-chronic liver failure: a randomized controlled trial. Hepatology 66 , 209–219 (2017).
Gordon, M. Y. et al. Characterization and clinical application of human CD34+ stem/progenitor cell populations mobilized into the blood by granulocyte colony-stimulating factor. Stem Cells 24 , 1822–1830 (2006).
Arroyo, V. et al. Acute-on-chronic liver failure in cirrhosis. Nat. Rev. Dis. Prim. 2 , 16041 (2016).
Zhang, Z. et al. Human umbilical cord mesenchymal stem cells improve liver function and ascites in decompensated liver cirrhosis patients. J. Gastroenterol. Hepatol. 27 (Suppl 2), 112–120 (2012).
El-Ansary, M. et al. Phase II trial: undifferentiated versus differentiated autologous mesenchymal stem cells transplantation in Egyptian patients with HCV induced liver cirrhosis. Stem Cell Rev. Rep. 8 , 972–981 (2012).
Xu, L. et al. Randomized trial of autologous bone marrow mesenchymal stem cells transplantation for hepatitis B virus cirrhosis: regulation of Treg/Th17 cells. J. Gastroenterol. Hepatol. 29 , 1620–1628 (2014).
Suk, K. T. et al. Transplantation with autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: Phase 2 trial. Hepatology 64 , 2185–2197 (2016).
Fang, X. et al. A study about immunomodulatory effect and efficacy and prognosis of human umbilical cord mesenchymal stem cells in patients with chronic hepatitis B-induced decompensated liver cirrhosis. J. Gastroenterol. Hepatol. 33 , 774–780 (2018).
Mohamadnejad, M. et al. Randomized placebo-controlled trial of mesenchymal stem cell transplantation in decompensated cirrhosis. Liver Int. 33 , 1490–1496 (2013).
Nguyen, T. L. et al. Autologous bone marrow mononuclear cell infusion for liver cirrhosis after the Kasai operation in children with biliary atresia. Stem Cell Res. Ther. 13 , 108 (2022).
Bai, Y. Q. et al. Outcomes of autologous bone marrow mononuclear cell transplantation in decompensated liver cirrhosis. World J. Gastroenterol. 20 , 8660–8666 (2014).
Guo, C. et al. Long-term outcomes of autologous peripheral blood stem cell transplantation in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 17 , 1175–1182 e1172 (2019).
Newsome, P. N. et al. Granulocyte colony-stimulating factor and autologous CD133-positive stem-cell therapy in liver cirrhosis (REALISTIC): an open-label, randomised, controlled phase 2 trial. Lancet Gastroenterol. Hepatol. 3 , 25–36 (2018).
Spahr, L. et al. Autologous bone marrow mononuclear cell transplantation in patients with decompensated alcoholic liver disease: a randomized controlled trial. PLoS ONE 8 , e53719 (2013).
Maurice, J. & Manousou, P. Non-alcoholic fatty liver disease. Clin. Med. 18 , 245–250 (2018).
Article Google Scholar
Huang, T. D., Behary, J. & Zekry, A. Non-alcoholic fatty liver disease: a review of epidemiology, risk factors, diagnosis and management. Intern. Med. J. 50 , 1038–1047 (2020).
Sakai, Y. et al. Clinical trial of autologous adipose tissue-derived regenerative (stem) cells therapy for exploration of its safety and efficacy. Regen. Ther. 18 , 97–101 (2021).
Mieli-Vergani, G. et al. Autoimmune hepatitis. Nat. Rev. Dis. Primers 4 , 18018 (2018).
Calore, E. et al. Haploidentical stem cell transplantation cures autoimmune hepatitis and cerebrovascular disease in a patient with sickle cell disease. Bone Marrow Transpl. 53 , 644–646 (2018).
Vento, S., Cainelli, F., Renzini, C., Ghironzi, G. & Concia, E. Resolution of autoimmune hepatitis after bone-marrow transplantation. Lancet 348 , 544–545 (1996).
Terziroli Beretta-Piccoli, B., Mieli-Vergani, G. & Vergani, D. Autoimmmune hepatitis. Cell Mol. Immunol. 19 , 158–176 (2022).
Wang, L. et al. Pilot study of umbilical cord-derived mesenchymal stem cell transfusion in patients with primary biliary cirrhosis. J. Gastroenterol. Hepatol. 28 (Suppl 1), 85–92 (2013).
Wang, L. et al. Allogeneic bone marrow mesenchymal stem cell transplantation in patients with UDCA-resistant primary biliary cirrhosis. Stem Cells Dev. 23 , 2482–2489 (2014).
Martel-Pelletier, J. et al. Osteoarthritis. Nat. Rev. Dis. Prim. 2 , 16072 (2016).
Olsson, S., Akbarian, E., Lind, A., Razavian, A. S. & Gordon, M. Automating classification of osteoarthritis according to Kellgren-Lawrence in the knee using deep learning in an unfiltered adult population. BMC Musculoskelet. Disord. 22 , 844 (2021).
Mahmoudian, A., Lohmander, L. S., Mobasheri, A., Englund, M. & Luyten, F. P. Early-stage symptomatic osteoarthritis of the knee—time for action. Nat. Rev. Rheumatol. 17 , 621–632 (2021).
Kubsik-Gidlewska, A. et al. CD34+ stem cell treatment for knee osteoarthritis: a treatment and rehabilitation algorithm. J. Rehabil. Med Clin. Commun. 3 , 1000012 (2018).
Jevotovsky, D. S., Alfonso, A. R., Einhorn, T. A. & Chiu, E. S. Osteoarthritis and stem cell therapy in humans: a systematic review. Osteoarthr. Cartil. 26 , 711–729 (2018).
Wiggers, T. G., Winters, M., Van den Boom, N. A., Haisma, H. J. & Moen, M. H. Autologous stem cell therapy in knee osteoarthritis: a systematic review of randomised controlled trials. Br. J. Sports Med 55 , 1161–1169 (2021).
Han, S. B., Seo, I. W. & Shin, Y. S. Intra-articular injections of hyaluronic acid or steroids associated with better outcomes than platelet-rich plasma, adipose mesenchymal stromal cells, or placebo in knee osteoarthritis: a network meta-analysis. Arthroscopy 37 , 292–306 (2021).
Bastos, R. et al. Intra-articular injections of expanded mesenchymal stem cells with and without addition of platelet-rich plasma are safe and effective for knee osteoarthritis. Knee Surg. Sports Traumatol. Arthrosc. 26 , 3342–3350 (2018).
Molnar, V. et al. Mesenchymal stem cell mechanisms of action and clinical effects in osteoarthritis: a narrative review. Genes 13 , 949 (2022).
Barisic, S. & Childs, R. W. Graft-versus-solid-tumor effect: from hematopoietic stem cell transplantation to adoptive cell therapies. Stem Cells 40 , 556–563 (2022).
Mello, M. M. & Brennan, T. A. The controversy over high-dose chemotherapy with autologous bone marrow transplant for breast cancer. Health Aff. (Millwood) 20 , 101–117 (2001).
Sissung, T. M. & Figg, W. D. Stem cell clinics: risk of proliferation. Lancet Oncol. 21 , 205–206 (2020).
Fu, X. et al. Mesenchymal stem cell migration and tissue repair. Cells 8 , 784 (2019).
Zachar, L., Bacenkova, D. & Rosocha, J. Activation, homing, and role of the mesenchymal stem cells in the inflammatory environment. J. Inflamm. Res. 9 , 231–240 (2016).
de Araujo Farias, V., Carrillo-Galvez, A. B., Martin, F. & Anderson, P. TGF-beta and mesenchymal stromal cells in regenerative medicine, autoimmunity and cancer. Cytokine Growth Factor Rev. 43 , 25–37 (2018).
Ding, W. et al. Platelet-derived growth factor (PDGF)-PDGF receptor interaction activates bone marrow-derived mesenchymal stromal cells derived from chronic lymphocytic leukemia: implications for an angiogenic switch. Blood 116 , 2984–2993 (2010).
Ritter, E. et al. Breast cancer cell-derived fibroblast growth factor 2 and vascular endothelial growth factor are chemoattractants for bone marrow stromal stem cells. Ann. Surg. 247 , 310–314 (2008).
Cronwright, G. et al. Cancer/testis antigen expression in human mesenchymal stem cells: down-regulation of SSX impairs cell migration and matrix metalloproteinase 2 expression. Cancer Res. 65 , 2207–2215 (2005).
Aldinucci, D., Borghese, C. & Casagrande, N. The CCL5/CCR5 axis in cancer progression. Cancers 12 , 1765 (2020).
Karnoub, A. E. et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature 449 , 557–563 (2007).
Kucerova, L., Matuskova, M., Hlubinova, K., Altanerova, V. & Altaner, C. Tumor cell behaviour modulation by mesenchymal stromal cells. Mol. Cancer 9 , 129 (2010).
Schmohl, K. A., Muller, A. M., Nelson, P. J. & Spitzweg, C. Thyroid hormone effects on mesenchymal stem cell biology in the tumour microenvironment. Exp. Clin. Endocrinol. Diabetes 128 , 462–468 (2020).
Mishra, P. J. et al. Carcinoma-associated fibroblast-like differentiation of human mesenchymal stem cells. Cancer Res. 68 , 4331–4339 (2008).
Liu, J., Han, G., Liu, H. & Qin, C. Suppression of cholangiocarcinoma cell growth by human umbilical cord mesenchymal stem cells: a possible role of Wnt and Akt signaling. PLoS ONE 8 , e62844 (2013).
Ho, I. A. et al. Human bone marrow-derived mesenchymal stem cells suppress human glioma growth through inhibition of angiogenesis. Stem Cells 31 , 146–155 (2013).
Sun, Z., Wang, S. & Zhao, R. C. The roles of mesenchymal stem cells in tumor inflammatory microenvironment. J. Hematol. Oncol. 7 , 14 (2014).
Rhee, K. J., Lee, J. I. & Eom, Y. W. Mesenchymal stem cell-mediated effects of tumor support or suppression. Int. J. Mol. Sci. 16 , 30015–30033 (2015).
Liang, W. et al. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol. Biol. Lett. 26 , 3 (2021).
Hmadcha, A., Martin-Montalvo, A., Gauthier, B. R., Soria, B. & Capilla-Gonzalez, V. Therapeutic potential of mesenchymal stem cells for cancer therapy. Front. Bioeng. Biotechnol. 8 , 43 (2020).
Cao, G. D. et al. The oncolytic virus in cancer diagnosis and treatment. Front. Oncol. 10 , 1786 (2020).
Melen, G. J. et al. Influence of carrier cells on the clinical outcome of children with neuroblastoma treated with high dose of oncolytic adenovirus delivered in mesenchymal stem cells. Cancer Lett. 371 , 161–170 (2016).
Garcia-Castro, J. et al. Treatment of metastatic neuroblastoma with systemic oncolytic virotherapy delivered by autologous mesenchymal stem cells: an exploratory study. Cancer Gene Ther. 17 , 476–483 (2010).
Draganov, D. D. et al. Delivery of oncolytic vaccinia virus by matched allogeneic stem cells overcomes critical innate and adaptive immune barriers. J. Transl. Med. 17 , 100 (2019).
Cyranoski, D. How human embryonic stem cells sparked a revolution. Nature 555 , 428–430 (2018).
Thomson, J. A. et al. Embryonic stem cell lines derived from human blastocysts. Science 282 , 1145–1147 (1998).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126 , 663–676 (2006).
Takahashi, K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131 , 861–872 (2007).
Gepstein, L. Derivation and potential applications of human embryonic stem cells. Circ. Res. 91 , 866–876 (2002).
Andrews, P. W. From teratocarcinomas to embryonic stem cells. Philos. Trans. R. Soc. Lond. B Biol. Sci. 357 , 405–417 (2002).
Finch, B. W. & Ephrussi, B. Retention of multiple developmental potentialities by cells of a mouse testicular teratocarcinoma during prolonged culture in vitro and their extinction upon hybridization with cells of permanent lines. Proc. Natl Acad. Sci. USA 57 , 615–621 (1967).
Ried, T. et al. The consequences of chromosomal aneuploidy on the transcriptome of cancer cells. Biochim Biophys. Acta 1819 , 784–793 (2012).
Evans, M. J. & Kaufman, M. H. Establishment in culture of pluripotential cells from mouse embryos. Nature 292 , 154–156 (1981).
Martin, G. R. Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc. Natl Acad. Sci. USA 78 , 7634–7638 (1981).
Lo, B. & Parham, L. Ethical issues in stem cell research. Endocr. Rev. 30 , 204–213 (2009).
Wilmut, I., Schnieke, A. E., McWhir, J., Kind, A. J. & Campbell, K. H. Viable offspring derived from fetal and adult mammalian cells. Nature 385 , 810–813 (1997).
Schwartz, S. D. et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet 379 , 713–720 (2012).
Atala, A. Human embryonic stem cells: early hints on safety and efficacy. Lancet 379 , 689–690 (2012).
Schwartz, S. D. et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet 385 , 509–516 (2015).
Song, W. K. et al. Treatment of macular degeneration using embryonic stem cell-derived retinal pigment epithelium: preliminary results in Asian patients. Stem Cell Rep. 4 , 860–872 (2015).
Liu, Y. et al. Human embryonic stem cell-derived retinal pigment epithelium transplants as a potential treatment for wet age-related macular degeneration. Cell Discov. 4 , 50 (2018).
Limnios, I. J., Chau, Y. Q., Skabo, S. J., Surrao, D. C. & O’Neill, H. C. Efficient differentiation of human embryonic stem cells to retinal pigment epithelium under defined conditions. Stem Cell Res. Ther. 12 , 248 (2021).
Foltz, L. P. & Clegg, D. O. Rapid, directed differentiation of retinal pigment epithelial cells from human embryonic or induced pluripotent stem cells. J. Vis. Exp. 128 , e56274 (2017).
Kuroda, T., Ando, S., Takeno, Y., Kishino, A. & Kimura, T. Robust induction of retinal pigment epithelium cells from human induced pluripotent stem cells by inhibiting FGF/MAPK signaling. Stem Cell Res 39 , 101514 (2019).
Dewell, T. E. et al. Transcription factor overexpression drives reliable differentiation of retinal pigment epithelium from human induced pluripotent stem cells. Stem Cell Res. 53 , 102368 (2021).
Dehghan, S., Mirshahi, R., Shoae-Hassani, A. & Naseripour, M. Human-induced pluripotent stem cells-derived retinal pigmented epithelium, a new horizon for cells-based therapies for age-related macular degeneration. Stem Cell Res. Ther. 13 , 217 (2022).
Menasche, P. et al. Human embryonic stem cell-derived cardiac progenitors for severe heart failure treatment: first clinical case report. Eur. Heart J. 36 , 2011–2017 (2015).
Menasche, P. et al. Transplantation of human embryonic stem cell-derived cardiovascular progenitors for severe ischemic left ventricular dysfunction. J. Am. Coll. Cardiol. 71 , 429–438 (2018).
Cyranoski, D. ‘Reprogrammed’ stem cells approved to mend human hearts for the first time. Nature 557 , 619–620 (2018).
Povsic, T. J. & Gersh, B. J. Stem cells in cardiovascular diseases: 30,000-foot view. Cells 10 , 600 (2021).
Romito, A. & Cobellis, G. Pluripotent stem cells: current understanding and future directions. Stem Cells Int. 2016 , 9451492 (2016).
McKenna, S. L. et al. Ten-year safety of pluripotent stem cell transplantation in acute thoracic spinal cord injury. J. Neurosurg. Spine 1 , 1–10 (2022).
Deinsberger, J., Reisinger, D. & Weber, B. Global trends in clinical trials involving pluripotent stem cells: a systematic multi-database analysis. NPJ Regen. Med. 5 , 15 (2020).
Kim, J. Y., Nam, Y., Rim, Y. A. & Ju, J. H. Review of the current trends in clinical trials involving induced pluripotent stem cells. Stem Cell Rev. Rep. 18 , 142–154 (2022).
Ji, P., Manupipatpong, S., Xie, N. & Li, Y. Induced pluripotent stem cells: generation strategy and epigenetic mystery behind reprogramming. Stem Cells Int. 2016 , 8415010 (2016).
Fu, X. The immunogenicity of cells derived from induced pluripotent stem cells. Cell Mol. Immunol. 11 , 14–16 (2014).
Lee, A. S., Tang, C., Rao, M. S., Weissman, I. L. & Wu, J. C. Tumorigenicity as a clinical hurdle for pluripotent stem cell therapies. Nat. Med. 19 , 998–1004 (2013).
Friedenstein, A. J., Piatetzky, S. II & Petrakova, K. V. Osteogenesis in transplants of bone marrow cells. J. Embryol. Exp. Morphol. 16 , 381–390 (1966).
Pittenger, M. F. et al. Multilineage potential of adult human mesenchymal stem cells. Science 284 , 143–147 (1999).
Nombela-Arrieta, C., Ritz, J. & Silberstein, L. E. The elusive nature and function of mesenchymal stem cells. Nat. Rev. Mol. Cell Biol. 12 , 126–131 (2011).
Dominici, M. et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy 8 , 315–317 (2006).
Zhou, T. et al. Challenges and advances in clinical applications of mesenchymal stromal cells. J. Hematol. Oncol. 14 , 24 (2021).
Ankrum, J. & Karp, J. M. Mesenchymal stem cell therapy: two steps forward, one step back. Trends Mol. Med. 16 , 203–209 (2010).
Tuan, R. S., Boland, G. & Tuli, R. Adult mesenchymal stem cells and cell-based tissue engineering. Arthritis Res. Ther. 5 , 32–45 (2003).
Witkowska-Zimny, M. & Wrobel, E. Perinatal sources of mesenchymal stem cells: Wharton’s jelly, amnion and chorion. Cell Mol. Biol. Lett. 16 , 493–514 (2011).
Alkhalil, M., Smajilagic, A. & Redzic, A. Human dental pulp mesenchymal stem cells isolation and osteoblast differentiation. Med. Glas. (Zenica) 12 , 27–32 (2015).
Google Scholar
Ouryazdanpanah, N., Dabiri, S., Derakhshani, A., Vahidi, R. & Farsinejad, A. Peripheral blood-derived mesenchymal stem cells: growth factor-free isolation, molecular characterization and differentiation. Iran. J. Pathol. 13 , 461–466 (2018).
PubMed PubMed Central Google Scholar
Francis, M. P., Sachs, P. C., Elmore, L. W. & Holt, S. E. Isolating adipose-derived mesenchymal stem cells from lipoaspirate blood and saline fraction. Organogenesis 6 , 11–14 (2010).
Gong, X. et al. Isolation and characterization of lung resident mesenchymal stem cells capable of differentiating into alveolar epithelial type II cells. Cell Biol. Int. 38 , 405–411 (2014).
Wang, B. et al. Human hair follicle-derived mesenchymal stem cells: Isolation, expansion, and differentiation. World J. Stem Cells 12 , 462–470 (2020).
Pilato, C. A. et al. Isolation and characterization of cardiac mesenchymal stromal cells from endomyocardial bioptic samples of arrhythmogenic cardiomyopathy patients. J. Vis. Exp . 132 , e57263 (2018).
Mannino, G. et al. Adult stem cell niches for tissue homeostasis. J. Cell Physiol. 237 , 239–257 (2022).
Pavlushina, S. V., Orlova, T. G. & Tabagari, D. Z. [Isolation of mononuclear cells from the bone marrow of patients with hemoblastoses using one-step ficoll-verographin density gradient separation]. Eksp. Onkol. 6 , 68–70 (1984).
Schneider, S., Unger, M., van Griensven, M. & Balmayor, E. R. Adipose-derived mesenchymal stem cells from liposuction and resected fat are feasible sources for regenerative medicine. Eur. J. Med Res. 22 , 17 (2017).
Torre, P. & Flores, A. I. Current status and future prospects of perinatal stem cells. Genes 12 , 6 (2020).
Hoang, V. T. et al. Standardized xeno- and serum-free culture platform enables large-scale expansion of high-quality mesenchymal stem/stromal cells from perinatal and adult tissue sources. Cytotherapy 23 , 88–99 (2020).
Mohamed-Ahmed, S. et al. Adipose-derived and bone marrow mesenchymal stem cells: a donor-matched comparison. Stem Cell Res. Ther. 9 , 168 (2018).
Zuk, P. A. et al. Human adipose tissue is a source of multipotent stem cells. Mol. Biol. Cell 13 , 4279–4295 (2002).
Li, Z. CD133: a stem cell biomarker and beyond. Exp. Hematol. Oncol. 2 , 17 (2013).
Petrenko, Y. et al. A comparative analysis of multipotent mesenchymal stromal cells derived from different sources, with a focus on neuroregenerative potential. Sci. Rep. 10 , 4290 (2020).
Wang, Z. & Yan, X. CD146, a multi-functional molecule beyond adhesion. Cancer Lett. 330 , 150–162 (2013).
Xu, L. et al. Tissue source determines the differentiation potentials of mesenchymal stem cells: a comparative study of human mesenchymal stem cells from bone marrow and adipose tissue. Stem Cell Res Ther. 8 , 275 (2017).
Han, I., Kwon, B. S., Park, H. K. & Kim, K. S. Differentiation potential of mesenchymal stem cells is related to their intrinsic mechanical properties. Int. Neurourol. J. 21 , S24–S31 (2017).
Song, Y. et al. Human mesenchymal stem cells derived from umbilical cord and bone marrow exert immunomodulatory effects in different mechanisms. World J. Stem Cells 12 , 1032–1049 (2020).
Lee, R. H. et al. Intravenous hMSCs improve myocardial infarction in mice because cells embolized in lung are activated to secrete the anti-inflammatory protein TSG-6. Cell Stem Cell 5 , 54–63 (2009).
Allers, C. et al. Dynamic of distribution of human bone marrow-derived mesenchymal stem cells after transplantation into adult unconditioned mice. Transplantation 78 , 503–508 (2004).
Devine, S. M., Cobbs, C., Jennings, M., Bartholomew, A. & Hoffman, R. Mesenchymal stem cells distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood 101 , 2999–3001 (2003).
Fischer, U. M. et al. Pulmonary passage is a major obstacle for intravenous stem cell delivery: the pulmonary first-pass effect. Stem Cells Dev. 18 , 683–692 (2009).
Sierra-Parraga, J. M. et al. Mesenchymal stromal cells are retained in the porcine renal cortex independently of their metabolic state after renal intra-arterial infusion. Stem Cells Dev. 28 , 1224–1235 (2019).
Henriksson, H. B. et al. The traceability of mesenchymal stromal cells after injection into degenerated discs in patients with low back pain. Stem Cells Dev. 28 , 1203–1211 (2019).
Sokal, E. M. et al. Biodistribution of liver-derived mesenchymal stem cells after peripheral injection in a hemophilia A patient. Transplantation 101 , 1845–1851 (2017).
Sood, V. et al. Biodistribution of 18F-FDG-labeled autologous bone marrow-derived stem cells in patients with type 2 diabetes mellitus: exploring targeted and intravenous routes of delivery. Clin. Nucl. Med. 40 , 697–700 (2015).
Sanchez-Diaz, M. et al. Biodistribution of mesenchymal stromal cells after administration in animal models and humans: a systematic review. J. Clin. Med. 10 , 2925 (2021).
Sensebe, L. & Fleury-Cappellesso, S. Biodistribution of mesenchymal stem/stromal cells in a preclinical setting. Stem Cells Int. 2013 , 678063 (2013).
Zhuang, W. Z. et al. Mesenchymal stem/stromal cell-based therapy: mechanism, systemic safety and biodistribution for precision clinical applications. J. Biomed. Sci. 28 , 28 (2021).
Wei, X. et al. Mesenchymal stem cells: a new trend for cell therapy. Acta Pharm. Sin. 34 , 747–754 (2013).
Kouchakian, M. R. et al. The clinical trials of mesenchymal stromal cells therapy. Stem Cells Int. 2021 , 1634782 (2021).
Chen, L. et al. Mesenchymal stem cell-based treatments for COVID-19: status and future perspectives for clinical applications. Cell Mol. Life Sci. 79 , 142 (2022).
Borow, K. M., Yaroshinsky, A., Greenberg, B. & Perin, E. C. Phase 3 DREAM-HF trial of mesenchymal precursor cells in chronic heart failure. Circ. Res. 125 , 265–281 (2019).
Zheng, H. et al. Mesenchymal stem cell therapy in stroke: a systematic review of literature in pre-clinical and clinical research. Cell Transpl. 27 , 1723–1730 (2018).
Rodriguez-Fuentes, D. E. et al. Mesenchymal stem cells current clinical applications: a systematic review. Arch. Med. Res. 52 , 93–101 (2021).
Shi, L. et al. Mesenchymal stem cell therapy for severe COVID-19. Signal Transduct. Target Ther. 6 , 339 (2021).
Carney, B. J. & Shah, K. Migration and fate of therapeutic stem cells in different brain disease models. Neuroscience 197 , 37–47 (2011).
Yao, P., Zhou, L., Zhu, L., Zhou, B. & Yu, Q. Mesenchymal stem cells: a potential therapeutic strategy for neurodegenerative diseases. Eur. Neurol. 83 , 235–241 (2020).
Bonaventura, G. et al. Stem cells: innovative therapeutic options for neurodegenerative diseases? Cells 10 , 1992 (2021).
Mansoor, S. R., Zabihi, E. & Ghasemi-Kasman, M. The potential use of mesenchymal stem cells for the treatment of multiple sclerosis. Life Sci. 235 , 116830 (2019).
Chung, J. W. et al. Efficacy and safety of intravenous mesenchymal stem cells for ischemic stroke. Neurology 96 , e1012–e1023 (2021).
Yamazaki, K., Kawabori, M., Seki, T. & Houkin, K. Clinical trials of stem cell treatment for spinal cord injury. Int. J. Mol. Sci . 21 , 3994 (2020).
Xie, B., Chen, M., Hu, R., Han, W. & Ding, S. Therapeutic evidence of human mesenchymal stem cell transplantation for cerebral palsy: a meta-analysis of randomized controlled trials. Stem Cells Int. 2020 , 5701920 (2020).
McDonald, C. A. et al. Intranasal delivery of mesenchymal stromal cells protects against neonatal hypoxic(-)ischemic brain injury. Int. J. Mol. Sci . 20 , 2449 (2019).
Liu, Q. et al. Rational use of mesenchymal stem cells in the treatment of autism spectrum disorders. World J. Stem Cells 11 , 55–72 (2019).
Fricova, D., Korchak, J. A. & Zubair, A. C. Challenges and translational considerations of mesenchymal stem/stromal cell therapy for Parkinson’s disease. npj Regen. Med. 5 , 20 (2020).
Bang, O. Y., Lee, J. S., Lee, P. H. & Lee, G. Autologous mesenchymal stem cell transplantation in stroke patients. Ann. Neurol. 57 , 874–882 (2005).
Lee, J. S. et al. A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 28 , 1099–1106 (2010).
Honmou, O. et al. Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 134 , 1790–1807 (2011).
Bhasin, A. et al. Autologous mesenchymal stem cells in chronic stroke. Cerebrovasc. Dis. Extra 1 , 93–104 (2011).
Jaillard, A. et al. Autologous mesenchymal stem cells improve motor recovery in subacute ischemic stroke: a randomized clinical trial. Transl. Stroke Res. 11 , 910–923 (2020).
Lee, J. et al. Efficacy of intravenous mesenchymal stem cells for motor recovery after ischemic stroke: a neuroimaging study. Stroke 53 , 20–28 (2022).
Levy, M. L. et al. Phase I/II study of safety and preliminary efficacy of intravenous allogeneic mesenchymal stem cells in chronic stroke. Stroke 50 , 2835–2841 (2019).
Xu, P. & Yang, X. The efficacy and safety of mesenchymal stem cell transplantation for spinal cord injury patients: a meta-analysis and systematic review. Cell Transpl. 28 , 36–46 (2019).
Liau, L. L. et al. Treatment of spinal cord injury with mesenchymal stem cells. Cell Biosci. 10 , 112 (2020).
Liu, X. et al. Comparative analysis of curative effect of bone marrow mesenchymal stem cell and bone marrow mononuclear cell transplantation for spastic cerebral palsy. J. Transl. Med. 15 , 1–9 (2017).
Sharma, A. K. et al. Cell transplantation as a novel therapeutic strategy for autism spectrum disorders: a clinical study. Am J. Stem Cells 9 , 89 (2020).
Ballen, K. & Kurtzberg, J. Exploring new therapies for children with autism: “Do no harm” does not mean do not try. Stem Cells Transl. Med. 10 , 823–825 (2021).
Reyhani, S., Abbaspanah, B. & Mousavi, S. H. Umbilical cord-derived mesenchymal stem cells in neurodegenerative disorders: from literature to clinical practice. Regen. Med. 15 , 1561–1578 (2020).
Gu, J. et al. Therapeutic evidence of umbilical cord-derived mesenchymal stem cell transplantation for cerebral palsy: a randomized, controlled trial. Stem Cell Res Ther. 11 , 43 (2020).
Retraction. Stem Cells Transl. Med. 10 , 1717 (2021).
Sun, J. M. et al. Infusion of human umbilical cord tissue mesenchymal stromal cells in children with autism spectrum disorder. Stem Cells Transl. Med. 9 , 1137–1146 (2020).
Yang, Y. et al. Repeated subarachnoid administrations of allogeneic human umbilical cord mesenchymal stem cells for spinal cord injury: a phase 1/2 pilot study. Cytotherapy 23 , 57–64 (2021).
Liu, J. et al. Clinical analysis of the treatment of spinal cord injury with umbilical cord mesenchymal stem cells. Cytotherapy 15 , 185–191 (2013).
Przekora, A. & Juszkiewicz, L. The effect of autologous adipose tissue-derived mesenchymal stem cells’ therapy in the treatment of chronic posttraumatic spinal cord injury in a domestic ferret patient. Cell Transpl. 29 , 963689720928982 (2020).
Hur, J. W. et al. Intrathecal transplantation of autologous adipose-derived mesenchymal stem cells for treating spinal cord injury: a human trial. J. Spinal Cord. Med. 39 , 655–664 (2016).
de Celis-Ruiz, E. et al. Final results of allogeneic adipose tissue-derived mesenchymal stem cells in acute ischemic stroke (AMASCIS): a phase II, randomized, double-blind, placebo-controlled, single-center, pilot clinical trial. Cell Transpl. 31 , 9636897221083863 (2022).
Yang, Y. et al. Human umbilical cord mesenchymal stem cells to treat spinal cord injury in the early chronic phase: study protocol for a prospective, multicenter, randomized, placebo-controlled, single-blinded clinical trial. Neural Regen. Res. 15 , 1532–1538 (2020).
de Celis-Ruiz, E. et al. Allogeneic adipose tissue-derived mesenchymal stem cells in ischaemic stroke (AMASCIS-02): a phase IIb, multicentre, double-blind, placebo-controlled clinical trial protocol. BMJ Open 11 , e051790 (2021).
Murray, C. J. L. COVID-19 will continue but the end of the pandemic is near. Lancet 399 , 417–419 (2022).
Thebaud, B. et al. Bronchopulmonary dysplasia. Nat. Rev. Dis. Prim. 5 , 78 (2019).
Mohamed, T., Abdul-Hafez, A., Gewolb, I. H. & Uhal, B. D. Oxygen injury in neonates: which is worse? hyperoxia, hypoxia, or alternating hyperoxia/hypoxia. J. Lung Pulm. Respir. Res. 7 , 4–13 (2020).
Omar, S. A. et al. Stem-cell therapy for bronchopulmonary dysplasia (BPD) in newborns. Cells 11 , 1275 (2022).
Chang, Y. S. et al. Mesenchymal stem cells for bronchopulmonary dysplasia: phase 1 dose-escalation clinical trial. J. Pediatr. 164 , 966–972 e966 (2014).
Powell, S. B. & Silvestri, J. M. Safety of intratracheal administration of human umbilical cord blood derived mesenchymal stromal cells in extremely low birth weight preterm infants. J. Pediatr. 210 , 209–213 e202 (2019).
Nguyen, L. T. et al. Allogeneic administration of human umbilical cord-derived mesenchymal stem/stromal cells for bronchopulmonary dysplasia: preliminary outcomes in four Vietnamese infants. J. Transl. Med. 18 , 398 (2020).
Ahn, S. Y. et al. Stem cells for bronchopulmonary dysplasia in preterm infants: a randomized controlled phase II trial. Stem Cells Transl. Med. 10 , 1129–1137 (2021).
Averyanov, A. et al. First-in-human high-cumulative-dose stem cell therapy in idiopathic pulmonary fibrosis with rapid lung function decline. Stem Cells Transl. Med. 9 , 6–16 (2020).
Ribeiro-Paes, J. T. et al. Unicentric study of cell therapy in chronic obstructive pulmonary disease/pulmonary emphysema. Int. J. Chron. Obstruct Pulmon Dis. 6 , 63–71 (2011).
Stessuk, T. et al. Phase I clinical trial of cell therapy in patients with advanced chronic obstructive pulmonary disease: follow-up of up to 3 years. Rev. Bras. Hematol. Hemoter. 35 , 352–357 (2013).
Weiss, D. J., Casaburi, R., Flannery, R., LeRoux-Williams, M. & Tashkin, D. P. A placebo-controlled, randomized trial of mesenchymal stem cells in COPD. Chest 143 , 1590–1598 (2013).
de Oliveira, H. G. et al. Combined bone marrow-derived mesenchymal stromal cell therapy and one-way endobronchial valve placement in patients with pulmonary emphysema: a phase I clinical trial. Stem Cells Transl. Med. 6 , 962–969 (2017).
Stolk, J. et al. A phase I study for intravenous autologous mesenchymal stromal cell administration to patients with severe emphysema. QJM 109 , 331–336 (2016).
Armitage, J. et al. Mesenchymal stromal cell infusion modulates systemic immunological responses in stable COPD patients: a phase I pilot study. Eur. Respir. J. 51 , 1702369 (2018).
Comella, K. et al. Autologous stromal vascular fraction in the intravenous treatment of end-stage chronic obstructive pulmonary disease: a phase I trial of safety and tolerability. J. Clin. Med. Res. 9 , 701–708 (2017).
Tzilas, V. et al . Prospective phase 1 open clinical trial to study the safety of adipose derived mesenchymal stem cells (ADMSCs) in COPD and combined pulmonary fibrosis and emphysema (CPFE). Eur. Respir. J. 46 , (2015).
Glassberg, M. K., Csete, I., Simonet, E. & Elliot, S. J. Stem cell therapy for COPD: hope and exploitation. Chest 160 , 1271–1281 (2021).
Le Thi Bich, P. et al. Allogeneic umbilical cord-derived mesenchymal stem cell transplantation for treating chronic obstructive pulmonary disease: a pilot clinical study. Stem Cell Res. Ther. 60 , 11 (2020).
Karaoz, E., Kalemci, S. & Ece, F. Improving effects of mesenchymal stem cells on symptoms of chronic obstructive pulmonary disease. Bratisl. Lek. Listy. 121 , 188–191 (2020).
Hoang, D. M., Nguyen, K. T., Nguyen, A. H., Nguyen, B. N. & Nguyen, L. T. Allogeneic human umbilical cord-derived mesenchymal stem/stromal cells for chronic obstructive pulmonary disease (COPD): study protocol for a matched case-control, phase I/II trial. BMJ Open 11 , e045788 (2021).
Xu, R., Feng, Z. & Wang, F. S. Mesenchymal stem cell treatment for COVID-19. EBioMedicine 77 , 103920 (2022).
Khoury, M. et al. Current status of cell-based therapies for respiratory virus infections: applicability to COVID-19. Eur. Respir. J. 55 , 2000858 (2020).
Jamilloux, Y. et al. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun. Rev. 19 , 102567 (2020).
Feng, Y. et al. Safety and feasibility of umbilical cord mesenchymal stem cells in patients with COVID-19 pneumonia: a pilot study. Cell Prolif. 53 , e12947 (2020).
Primorac, D. et al. Mesenchymal stromal cells: potential option for COVID-19 treatment. Pharmaceutic 13 , 1481 (2021).
Zhang, Y. et al. Intravenous infusion of human umbilical cord Wharton’s jelly-derived mesenchymal stem cells as a potential treatment for patients with COVID-19 pneumonia. Stem Cell Res. Ther. 11 , 207 (2020).
Shu, L. et al. Treatment of severe COVID-19 with human umbilical cord mesenchymal stem cells. Stem Cell Res. Ther. 11 , 361 (2020).
Tao, J. et al. Umbilical cord blood-derived mesenchymal stem cells in treating a critically ill COVID-19 patient. J. Infect. Dev. Ctries 14 , 1138–1145 (2020).
Saleh, M. et al. Cell therapy in patients with COVID-19 using Wharton’s jelly mesenchymal stem cells: a phase 1 clinical trial. Stem Cell Res. Ther. 12 , 410 (2021).
Leng, Z. et al. Transplantation of ACE2(-) mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 11 , 216–228 (2020).
Guo, Z. et al. Administration of umbilical cord mesenchymal stem cells in patients with severe COVID-19 pneumonia. Crit. Care 24 , 420 (2020).
Meng, F. et al. Human umbilical cord-derived mesenchymal stem cell therapy in patients with COVID-19: a phase 1 clinical trial. Signal Transduct. Target Ther. 5 , 172 (2020).
Shi, L. et al. Human mesenchymal stem cells treatment for severe COVID-19: 1-year follow-up results of a randomized, double-blind, placebo-controlled trial. EBioMedicine 75 , 103789 (2021).
Adas, G. et al. The systematic effect of mesenchymal stem cell therapy in critical COVID-19 patients: a prospective double controlled trial. Cell Transpl. 30 , 9636897211024942 (2021).
Shi, L. et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: a randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Targeted Ther. 6 , 58 (2021).
Lanzoni, G. et al. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: a double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl. Med. 10 , 660–673 (2021).
Hashemian, S. R. et al. Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: a case series. Stem Cell Res Ther. 12 , 91 (2021).
Zhu, R. et al. Mesenchymal stem cell treatment improves outcome of COVID-19 patients via multiple immunomodulatory mechanisms. Cell Res. 31 , 1244–1262 (2021).
Shi, L. et al. Effect of human umbilical cord-derived mesenchymal stem cells on lung damage in severe COVID-19 patients: a randomized, double-blind, placebo-controlled phase 2 trial. Signal Transduct. Target Ther. 6 , 58 (2021).
N, O. E., Pekkoc-Uyanik, K. C., Alpaydin, N., Gulay, G. R. & Simsek, M. Clinical experience on umbilical cord mesenchymal stem cell treatment in 210 severe and critical COVID-19 cases in Turkey. Stem Cell Rev. Rep. 17 , 1917–1925 (2021).
Gentile, P., Sterodimas, A., Pizzicannella, J., Calabrese, C. & Garcovich, S. Research progress on mesenchymal stem cells (MSCs), adipose-derived mesenchymal stem cells (AD-MSCs), drugs, and vaccines in inhibiting COVID-19 disease. Aging Dis. 11 , 1191–1201 (2020).
Copcu, H. E. Potential using of fat-derived stromal cells in the treatment of active disease, and also, in both pre- and post-periods in COVID-19. Aging Dis. 11 , 730–736 (2020).
Gentile, P. & Sterodimas, A. Adipose-derived stromal stem cells (ASCs) as a new regenerative immediate therapy combating coronavirus (COVID-19)-induced pneumonia. Expert Opin. Biol. Ther. 20 , 711–716 (2020).
Matthay, M. A. et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir. Med. 7 , 154–162 (2019).
Álvarez-Fuente, M. et al. Off-label mesenchymal stromal cell treatment in two infants with severe bronchopulmonary dysplasia: clinical course and biomarkers profile. Cytotherapy 20 , 1337–1344 (2018).
Zheng, G. et al. Treatment of acute respiratory distress syndrome with allogeneic adipose-derived mesenchymal stem cells: a randomized, placebo-controlled pilot study. Respir. Res. 15 , 39 (2014).
Simonson, O. E. et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl. Med. 4 , 1199–1213 (2015).
Wilson, J. G. et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir. Med. 3 , 24–32 (2015).
Yip, H. K. et al. Human umbilical cord-derived mesenchymal stem cells for acute respiratory distress syndrome. Crit. Care Med 48 , e391–e399 (2020).
Gorman, E. et al. Repair of acute respiratory distress syndrome by stromal cell administration (REALIST) trial: a phase 1 trial. EClinicalMedicine 41 , 101167 (2021).
Le Thi Bich, P. et al. Allogeneic umbilical cord-derived mesenchymal stem cell transplantation for treating chronic obstructive pulmonary disease: a pilot clinical study. Stem Cell Res. Ther. 11 , 60 (2020).
Wang, M. Y. et al. Current therapeutic strategies for respiratory diseases using mesenchymal stem cells. MedComm 2 , 351–380 (2021).
Carlsson, P. O., Schwarcz, E., Korsgren, O. & Le Blanc, K. Preserved beta-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes 64 , 587–592 (2015).
Dantas, J. R. et al. Adipose tissue-derived stromal/stem cells + cholecalciferol: a pilot study in recent-onset type 1 diabetes patients. Arch. Endocrinol. Metab. 65 , 342–351 (2021).
PubMed Google Scholar
Joseph, U. A. & Jhingran, S. G. Technetium-99m labeled RBC imaging in gastrointestinal bleeding from gastric leiomyoma. Clin. Nucl. Med. 13 , 23–25 (1988).
Hu, J. et al. Long term effects of the implantation of Wharton’s jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus. Endocr. J. 60 , 347–357 (2013).
Cai, J. et al. Umbilical cord mesenchymal stromal cell with autologous bone marrow cell transplantation in established type 1 diabetes: a pilot randomized controlled open-label clinical study to assess safety and impact on insulin secretion. Diabetes Care 39 , 149–157 (2016).
Huang, Q., Huang, Y. & Liu, J. Mesenchymal stem cells: an excellent candidate for the treatment of diabetes mellitus. Int. J. Endocrinol. 2021 , 9938658 (2021).
Nguyen, L. T. et al. Type 2 diabetes mellitus duration and obesity alter the efficacy of autologously transplanted bone marrow-derived mesenchymal stem/stromal cells. Stem Cells Transl. Med. 10 , 1266–1278 (2021).
Alicka, M., Major, P., Wysocki, M. & Marycz, K. Adipose-derived mesenchymal stem cells isolated from patients with type 2 diabetes show reduced “stemness” through an altered secretome profile, impaired anti-oxidative protection, and mitochondrial dynamics deterioration. J. Clin. Med. 8 , 765 (2019).
Agarwal, A. et al. Male infertility. Lancet 397 , 319–333 (2021).
Farquhar, C. & Marjoribanks, J. Assisted reproductive technology: an overview of Cochrane reviews. Cochrane Database Syst. Rev. 8 , CD010537 (2018).
Chang, Z. et al. Mesenchymal stem cells in preclinical infertility cytotherapy: a retrospective review. Stem Cells Int. 2021 , 8882368 (2021).
Fenton, A. J. Premature ovarian insufficiency: pathogenesis and management. J. Midlife Health 6 , 147–153 (2015).
Coulam, C. B. Premature gonadal failure. Fertil. Steril. 38 , 645–655 (1982).
Huhtaniemi, I. et al. Advances in the molecular pathophysiology, genetics, and treatment of primary ovarian insufficiency. Trends Endocrinol. Metab. 29 , 400–419 (2018).
Torrealday, S., Kodaman, P. & Pal, L. Premature ovarian Insufficiency—an update on recent advances in understanding and management. F1000Res 6 , 2069 (2017).
Gupta, S., Lodha, P., Karthick, M. S. & Tandulwadkar, S. R. Role of autologous bone marrow-derived stem cell therapy for follicular recruitment in premature ovarian insufficiency: review of literature and a case report of world’s first baby with ovarian autologous stem cell therapy in a perimenopausal woman of age 45 year. J. Hum. Reprod. Sci. 11 , 125–130 (2018).
Igboeli, P. et al. Intraovarian injection of autologous human mesenchymal stem cells increases estrogen production and reduces menopausal symptoms in women with premature ovarian failure: two case reports and a review of the literature. J. Med. Case Rep. 14 , 108 (2020).
Ulin, M. et al. Human mesenchymal stem cell therapy and other novel treatment approaches for premature ovarian insufficiency. Reprod. Sci. 28 , 1688–1696 (2021).
Herraiz, S. et al. Autologous stem cell ovarian transplantation to increase reproductive potential in patients who are poor responders. Fertil. Steril. 110 , 496–505 e491 (2018).
Ding, L. et al. Transplantation of UC-MSCs on collagen scaffold activates follicles in dormant ovaries of POF patients with long history of infertility. Sci. China Life Sci. 61 , 1554–1565 (2018).
Wang, M. Y., Wang, Y. X., Li-Ling, J. & Xie, H. Q. Adult stem cell therapy for premature ovarian failure: from bench to bedside. Tissue Eng. Part B Rev. 28 , 63–78 (2022).
Kaddoura, I., Abu-Sittah, G., Ibrahim, A., Karamanoukian, R. & Papazian, N. Burn injury: review of pathophysiology and therapeutic modalities in major burns. Ann. Burns Fire Disasters 30 , 95–102 (2017).
PubMed PubMed Central CAS Google Scholar
Jeschke, M. G. et al. Burn injury. Nat. Rev. Dis. Prim. 6 , 11 (2020).
Rasulov, M. F. et al. First experience of the use bone marrow mesenchymal stem cells for the treatment of a patient with deep skin burns. Bull. Exp. Biol. Med. 139 , 141–144 (2005).
Mansilla, E. et al. Cadaveric bone marrow mesenchymal stem cells: first experience treating a patient with large severe burns. Burns Trauma 3 , 17 (2015).
Xu, Y., Huang, S. & Fu, X. Autologous transplantation of bone marrow-derived mesenchymal stem cells: a promising therapeutic strategy for prevention of skin-graft contraction. Clin. Exp. Dermatol. 37 , 497–500 (2012).
Yoshikawa, T. et al. Wound therapy by marrow mesenchymal cell transplantation. Plast. Reconstr. Surg. 121 , 860–877 (2008).
Abo-Elkheir, W. et al. Role of cord blood and bone marrow mesenchymal stem cells in recent deep burn: a case-control prospective study. Am. J. Stem Cells 6 , 23–35 (2017).
Li, L. et al. Conditioned medium from human adipose-derived mesenchymal stem cell culture prevents UVB-induced skin aging in human keratinocytes and dermal fibroblasts. Int. J. Mol. Sci. 21 , 49 (2019).
Lotfi, M. et al. Adipose tissue-derived mesenchymal stem cells and keratinocytes co-culture on gelatin/chitosan/beta-glycerol phosphate nanoscaffold in skin regeneration. Cell Biol. Int. 43 , 1365–1378 (2019).
Yang, J. A., Chung, H. M., Won, C. H. & Sung, J. H. Potential application of adipose-derived stem cells and their secretory factors to skin: discussion from both clinical and industrial viewpoints. Expert Opin. Biol. Ther. 10 , 495–503 (2010).
Zhou, Y. et al. Combined topical and systemic administration with human adipose-derived mesenchymal stem cells (hADSC) and hADSC-derived exosomes markedly promoted cutaneous wound healing and regeneration. Stem Cell Res. Ther. 12 , 257 (2021).
Arjmand, B. et al. Regenerative medicine for the treatment of ischemic heart disease; status and future perspectives. Front. Cell Dev. Biol. 9 , 704903 (2021).
Denning, C. et al. Cardiomyocytes from human pluripotent stem cells: from laboratory curiosity to industrial biomedical platform. Biochim Biophys. Acta 1863 , 1728–1748 (2016).
Wu, R., Hu, X. & Wang, J. Concise review: optimized strategies for stem cell-based therapy in myocardial repair: clinical translatability and potential limitation. Stem Cells 36 , 482–500 (2018).
Chong, J. J. et al. Human embryonic-stem-cell-derived cardiomyocytes regenerate non-human primate hearts. Nature 510 , 273–277 (2014).
Bagno, L., Hatzistergos, K. E., Balkan, W. & Hare, J. M. Mesenchymal stem cell-based therapy for cardiovascular disease: progress and challenges. Mol. Ther. 26 , 1610–1623 (2018).
Demurtas, J. et al. Stem cells for treatment of cardiovascular diseases: an umbrella review of randomized controlled trials. Ageing Res. Rev. 67 , 101257 (2021).
Gubert, F. et al. Mesenchymal stem cells therapies on fibrotic heart diseases. Int. J. Mol. Sci. 22 , 7447 (2021).
da Silva, J. S. et al. Mesenchymal stem cell therapy in diabetic cardiomyopathy. Cells 11 , 240 (2022).
He, X. et al. Signaling cascades in the failing heart and emerging therapeutic strategies. Signal Transduct. Target Ther. 7 , 134 (2022).
Bolli, R., Solankhi, M., Tang, X. L. & Kahlon, A. Cell therapy in patients with heart failure: a comprehensive review and emerging concepts. Cardiovasc Res. 118 , 951–976 (2022).
Bartunek, J. et al. Cardiopoietic stem cell therapy in heart failure: the C-CURE (cardiopoietic stem Cell therapy in heart failURE) multicenter randomized trial with lineage-specified biologics. J. Am. Coll. Cardiol. 61 , 2329–2338 (2013).
Bartunek, J. et al. Cardiopoietic cell therapy for advanced ischaemic heart failure: results at 39 weeks of the prospective, randomized, double blind, sham-controlled CHART-1 clinical trial. Eur. Heart J. 38 , 648–660 (2017).
Hare, J. M. et al. Comparison of allogeneic vs autologous bone marrow-derived mesenchymal stem cells delivered by transendocardial injection in patients with ischemic cardiomyopathy: the POSEIDON randomized trial. J. Am. Med. Assoc. 308 , 2369–2379 (2012).
Hare, J. M. et al. Randomized comparison of allogeneic versus autologous mesenchymal stem cells for nonischemic dilated cardiomyopathy: POSEIDON-DCM trial. J. Am. Coll. Cardiol. 69 , 526–537 (2017).
Mathiasen, A. B. et al. Bone marrow-derived mesenchymal stromal cell treatment in patients with severe ischaemic heart failure: a randomized placebo-controlled trial (MSC-HF trial). Eur. Heart J. 36 , 1744–1753 (2015).
Mathiasen, A. B. et al. Bone marrow-derived mesenchymal stromal cell treatment in patients with ischaemic heart failure: final 4-year follow-up of the MSC-HF trial. Eur. J. Heart Fail 22 , 884–892 (2020).
Florea, V. et al. Dose comparison study of allogeneic mesenchymal stem cells in patients with ischemic cardiomyopathy (The TRIDENT Study). Circ. Res. 121 , 1279–1290 (2017).
Bolli, R. et al. A Phase II study of autologous mesenchymal stromal cells and c-kit positive cardiac cells, alone or in combination, in patients with ischaemic heart failure: the CCTRN CONCERT-HF trial. Eur. J. Heart Fail 23 , 661–674 (2021).
Heldman, A. W. et al. Transendocardial mesenchymal stem cells and mononuclear bone marrow cells for ischemic cardiomyopathy: the TAC-HFT randomized trial. J. Am. Med. Assoc. 311 , 62–73 (2014).
Perin, E. C. et al. Adipose-derived regenerative cells in patients with ischemic cardiomyopathy: the PRECISE trial. Am. Heart J. 168 , 88–95 e82 (2014).
Han, S., Sun, H. M., Hwang, K. C. & Kim, S. W. Adipose-derived stromal vascular fraction cells: update on clinical utility and efficacy. Crit. Rev. Eukaryot. Gene Expr. 25 , 145–152 (2015).
Henry, T. D. et al. The Athena trials: autologous adipose-derived regenerative cells for refractory chronic myocardial ischemia with left ventricular dysfunction. Catheter Cardiovasc Inter. 89 , 169–177 (2017).
Kastrup, J. et al. Cryopreserved off-the-shelf allogeneic adipose-derived stromal cells for therapy in patients with ischemic heart disease and heart failure—a safety study. Stem Cells Transl. Med. 6 , 1963–1971 (2017).
Qayyum, A. A. et al. Adipose-derived stromal cells for treatment of patients with chronic ischemic heart disease (MyStromalCell Trial): a randomized placebo-controlled study. Stem Cells Int. 2017 , 5237063 (2017).
Qayyum, A. A. et al. Autologous adipose-derived stromal cell treatment for patients with refractory angina (MyStromalCell Trial): 3-years follow-up results. J. Transl. Med. 17 , 360 (2019).
Ngo, A. T. L. et al. Clinically relevant preservation conditions for mesenchymal stem/stromal cells derived from perinatal and adult tissue sources. J. Cell Mol. Med. 25 , 10747–10760 (2021).
Madonna, R., Cevik, C., Nasser, M. & De Caterina, R. Hepatocyte growth factor: molecular biomarker and player in cardioprotection and cardiovascular regeneration. Thromb. Haemost. 107 , 656–661 (2012).
Bartolucci, J. et al. Safety and efficacy of the intravenous infusion of umbilical cord mesenchymal stem cells in patients with heart failure: a phase 1/2 randomized controlled trial (RIMECARD Trial [randomized clinical trial of intravenous infusion umbilical cord mesenchymal stem cells on cardiopathy]). Circ. Res. 121 , 1192–1204 (2017).
Ulus, A. T. et al. Intramyocardial transplantation of umbilical cord mesenchymal stromal cells in chronic ischemic cardiomyopathy: a controlled, randomized clinical trial (HUC-HEART trial). Int. J. Stem Cells 13 , 364–376 (2020).
He, X. et al. Effect of intramyocardial grafting collagen scaffold with mesenchymal stromal cells in patients with chronic ischemic heart disease: a randomized clinical trial. JAMA Netw. Open 3 , e2016236 (2020).
Zhang, Q. et al. Signaling pathways and targeted therapy for myocardial infarction. Signal Transduct. Target Ther. 7 , 78 (2022).
Poomani, M. S. et al. Mesenchymal stem cell (MSCs) therapy for ischemic heart disease: a promising frontier. Glob. Heart 17 , 19 (2022).
Xu, W. et al. Mesenchymal stem cells from adult human bone marrow differentiate into a cardiomyocyte phenotype in vitro. Exp. Biol. Med. 229 , 623–631 (2004).
Jeong, J. O. et al. Malignant tumor formation after transplantation of short-term cultured bone marrow mesenchymal stem cells in experimental myocardial infarction and diabetic neuropathy. Circ. Res. 108 , 1340–1347 (2011).
Denu, R. A. et al. Fibroblasts and mesenchymal stromal/stem cells are phenotypically indistinguishable. Acta Haematol. 136 , 85–97 (2016).
Birbrair, A. & Frenette, P. S. Niche heterogeneity in the bone marrow. Ann. N. Y Acad. Sci. 1370 , 82–96 (2016).
Pinho, S. & Frenette, P. S. Haematopoietic stem cell activity and interactions with the niche. Nat. Rev. Mol. Cell Biol. 20 , 303–320 (2019).
Ono, N. et al. Vasculature-associated cells expressing nestin in developing bones encompass early cells in the osteoblast and endothelial lineage. Dev. Cell 29 , 330–339 (2014).
Sugiyama, T., Kohara, H., Noda, M. & Nagasawa, T. Maintenance of the hematopoietic stem cell pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity 25 , 977–988 (2006).
Ehninger, A. & Trumpp, A. The bone marrow stem cell niche grows up: mesenchymal stem cells and macrophages move in. J. Exp. Med. 208 , 421–428 (2011).
Golan, K., Kollet, O., Markus, R. P. & Lapidot, T. Daily light and darkness onset and circadian rhythms metabolically synchronize hematopoietic stem cell differentiation and maintenance: the role of bone marrow norepinephrine, tumor necrosis factor, and melatonin cycles. Exp. Hematol. 78 , 1–10 (2019).
Cheng, X. et al. The role of SDF-1/CXCR4/CXCR7 in neuronal regeneration after cerebral ischemia. Front. Neurosci. 11 , 590 (2017).
Zou, Y. R., Kottmann, A. H., Kuroda, M., Taniuchi, I. & Littman, D. R. Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature 393 , 595–599 (1998).
Mao, W., Yi, X., Qin, J., Tian, M. & Jin, G. CXCL12 inhibits cortical neuron apoptosis by increasing the ratio of Bcl-2/Bax after traumatic brain injury. Int. J. Neurosci. 124 , 281–290 (2014).
Wang, Q. et al. Stromal cell-derived factor 1alpha decreases beta-amyloid deposition in Alzheimer’s disease mouse model. Brain Res. 1459 , 15–26 (2012).
Yellowley, C. CXCL12/CXCR4 signaling and other recruitment and homing pathways in fracture repair. Bonekey Rep. 2 , 300 (2013).
Li, J. et al. CXCL12 promotes spinal nerve regeneration and functional recovery after spinal cord injury. Neuroreport 32 , 450–457 (2021).
Gensel, J. C., Kigerl, K. A., Mandrekar-Colucci, S. S., Gaudet, A. D. & Popovich, P. G. Achieving CNS axon regeneration by manipulating convergent neuro-immune signaling. Cell Tissue Res. 349 , 201–213 (2012).
Matsushita, T. et al. Mesenchymal stem cells transmigrate across brain microvascular endothelial cell monolayers through transiently formed inter-endothelial gaps. Neurosci. Lett. 502 , 41–45 (2011).
Schmidt, A. et al. Mesenchymal stem cells transmigrate over the endothelial barrier. Eur. J. Cell Biol. 85 , 1179–1188 (2006).
Yarygin, K. N. et al. Cell therapy of stroke: do the intra-arterially transplanted mesenchymal stem cells cross the blood-brain barrier? Cells 10 , 2997 (2021).
Schack, L. M. et al. Expression of CD24 in human bone marrow-derived mesenchymal stromal cells is regulated by TGFbeta3 and induces a myofibroblast-like genotype. Stem Cells Int. 2016 , 1319578 (2016).
Ruster, B. et al. Mesenchymal stem cells display coordinated rolling and adhesion behavior on endothelial cells. Blood 108 , 3938–3944 (2006).
Pluchino, N. et al. CXCR4 or CXCR7 antagonists treat endometriosis by reducing bone marrow cell trafficking. J. Cell Mol. Med. 24 , 2464–2474 (2020).
Kowalski, K. et al. Stem cells migration during skeletal muscle regeneration—the role of Sdf-1/Cxcr4 and Sdf-1/Cxcr7 axis. Cell Adh. Migr. 11 , 384–398 (2017).
Liu, L. et al. From blood to the brain: can systemically transplanted mesenchymal stem cells cross the blood-brain barrier? Stem Cells Int. 2013 , 435093 (2013).
Lozito, T. P. & Tuan, R. S. Mesenchymal stem cells inhibit both endogenous and exogenous MMPs via secreted TIMPs. J. Cell Physiol. 226 , 385–396 (2011).
Lozito, T. P., Jackson, W. M., Nesti, L. J. & Tuan, R. S. Human mesenchymal stem cells generate a distinct pericellular zone of MMP activities via binding of MMPs and secretion of high levels of TIMPs. Matrix Biol. 34 , 132–143 (2014).
Menge, T. et al. Mesenchymal stem cells regulate blood-brain barrier integrity through TIMP3 release after traumatic brain injury. Sci. Transl. Med. 4 , 161ra150 (2012).
Franklin, R. J. M. & Ffrench-Constant, C. Regenerating CNS myelin—from mechanisms to experimental medicines. Nat. Rev. Neurosci. 18 , 753–769 (2017).
Brick, R. M., Sun, A. X. & Tuan, R. S. Neurotrophically induced mesenchymal progenitor cells derived from induced pluripotent stem cells enhance neuritogenesis via neurotrophin and cytokine production. Stem Cells Transl. Med. 7 , 45–58 (2018).
Zupanc, H. R. H., Alexander, P. G. & Tuan, R. S. Neurotrophic support by traumatized muscle-derived multipotent progenitor cells: role of endothelial cells and vascular endothelial growth factor-A. Stem Cell Res. Ther. 8 , 226 (2017).
Liu, Y. & Olsen, B. R. Distinct VEGF functions during bone development and homeostasis. Arch. Immunol. Ther. Exp. 62 , 363–368 (2014).
Kangari, P., Talaei-Khozani, T., Razeghian-Jahromi, I. & Razmkhah, M. Mesenchymal stem cells: amazing remedies for bone and cartilage defects. Stem Cell Res. Ther. 11 , 492 (2020).
Liu, Y. et al. Intracellular VEGF regulates the balance between osteoblast and adipocyte differentiation. J. Clin. Investig. 122 , 3101–3113 (2012).
Berendsen, A. D. & Olsen, B. R. How vascular endothelial growth factor-A (VEGF) regulates differentiation of mesenchymal stem cells. J. Histochem Cytochem. 62 , 103–108 (2014).
Garcia, K. O. et al. Therapeutic effects of the transplantation of VEGF overexpressing bone marrow mesenchymal stem cells in the hippocampus of murine model of Alzheimer’s disease. Front. Aging Neurosci. 6 , 30 (2014).
Hohman, T. J., Bell, S. P. & Jefferson, A. L., Alzheimer’s Disease Neuroimaging, I. The role of vascular endothelial growth factor in neurodegeneration and cognitive decline: exploring interactions with biomarkers of Alzheimer disease. JAMA Neurol. 72 , 520–529 (2015).
Zhang, W. et al. Neuroprotective effects of SOX5 against ischemic stroke by regulating VEGF/PI3K/AKT pathway. Gene 767 , 145148 (2021).
Jin, K. et al. Vascular endothelial growth factor (VEGF) stimulates neurogenesis in vitro and in vivo. Proc. Natl Acad. Sci. USA 99 , 11946–11950 (2002).
Bao, X. J. et al. Transplantation of Flk-1+ human bone marrow-derived mesenchymal stem cells promotes behavioral recovery and anti-inflammatory and angiogenesis effects in an intracerebral hemorrhage rat model. Int. J. Mol. Med. 31 , 1087–1096 (2013).
Bao, X. et al. Transplantation of Flk-1+ human bone marrow-derived mesenchymal stem cells promotes angiogenesis and neurogenesis after cerebral ischemia in rats. Eur. J. Neurosci. 34 , 87–98 (2011).
Pelletier, J. et al. VEGF-A promotes both pro-angiogenic and neurotrophic capacities for nerve recovery after compressive neuropathy in rats. Mol. Neurobiol. 51 , 240–251 (2015).
Hobson, M. I., Green, C. J. & Terenghi, G. VEGF enhances intraneural angiogenesis and improves nerve regeneration after axotomy. J. Anat. 197 (Pt 4), 591–605 (2000).
Hayakawa, K. et al. Vascular endothelial growth factor regulates the migration of oligodendrocyte precursor cells. J. Neurosci. 31 , 10666–10670 (2011).
Pei, G., Xu, L., Huang, W. & Yin, J. The protective role of microRNA-133b in restricting hippocampal neurons apoptosis and inflammatory injury in rats with depression by suppressing CTGF. Int. Immunopharmacol. 78 , 106076 (2020).
Xu, H. et al. Mesenchymal stem cell-derived exosomal microRNA-133b suppresses glioma progression via Wnt/beta-catenin signaling pathway by targeting EZH2. Stem Cell Res. Ther. 10 , 381 (2019).
Xin, H. et al. MiR-133b promotes neural plasticity and functional recovery after treatment of stroke with multipotent mesenchymal stromal cells in rats via transfer of exosome-enriched extracellular particles. Stem Cells 31 , 2737–2746 (2013).
Kigerl, K. A. et al. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J. Neurosci. 29 , 13435–13444 (2009).
Knoller, N. et al. Clinical experience using incubated autologous macrophages as a treatment for complete spinal cord injury: phase I study results. J. Neurosurg. Spine 3 , 173–181 (2005).
Yagura, K. et al. The enhancement of CCL2 and CCL5 by human bone marrow-derived mesenchymal stem/stromal cells might contribute to inflammatory suppression and axonal extension after spinal cord injury. PLoS ONE 15 , e0230080 (2020).
Zhong, Z. et al. Bone marrow mesenchymal stem cells upregulate PI3K/AKT pathway and down-regulate NF-kappaB pathway by secreting glial cell-derived neurotrophic factors to regulate microglial polarization and alleviate deafferentation pain in rats. Neurobiol. Dis. 143 , 104945 (2020).
Zhong, Z. et al. Adipose-derived stem cells modulate BV2 microglial M1/M2 polarization by producing GDNF. Stem Cells Dev. 29 , 714–727 (2020).
Dong, B. et al. Exosomes from human umbilical cord mesenchymal stem cells attenuate the inflammation of severe steroid-resistant asthma by reshaping macrophage polarization. Stem Cell Res. Ther. 12 , 204 (2021).
Li, X. et al. Umbilical cord tissue-derived mesenchymal stem cells induce T lymphocyte apoptosis and cell cycle arrest by expression of indoleamine 2, 3-dioxygenase. Stem Cells Int. 2016 , 7495135 (2016).
Wang, A. Y. L. et al. Human Wharton’s jelly mesenchymal stem cell-mediated sciatic nerve recovery is associated with the upregulation of regulatory T cells. Int. J. Mol. Sci. 21 , 6310 (2020).
Noone, C., Kihm, A., English, K., O’Dea, S. & Mahon, B. P. IFN-gamma stimulated human umbilical-tissue-derived cells potently suppress NK activation and resist NK-mediated cytotoxicity in vitro. Stem Cells Dev. 22 , 3003–3014 (2013).
Li, X. et al. Immunomodulatory effects of mesenchymal stem cells in peripheral nerve injury. Stem Cell Res. Ther. 13 , 18 (2022).
Shang, Y., Guan, H. & Zhou, F. Biological characteristics of umbilical cord mesenchymal stem cells and its therapeutic potential for hematological disorders. Front. Cell Dev. Biol. 9 , 570179 (2021).
Mennan, C. et al. Isolation and characterisation of mesenchymal stem cells from different regions of the human umbilical cord. Biomed. Res. Int. 2013 , 916136 (2013).
D’Addio, F. et al. The link between the PDL1 costimulatory pathway and Th17 in fetomaternal tolerance. J. Immunol. 187 , 4530–4541 (2011).
Amable, P. R., Teixeira, M. V., Carias, R. B., Granjeiro, J. M. & Borojevic, R. Protein synthesis and secretion in human mesenchymal cells derived from bone marrow, adipose tissue and Wharton’s jelly. Stem Cell Res. Ther. 5 , 53 (2014).
de Witte, S. F. H. et al. Immunomodulation by therapeutic mesenchymal stromal cells (MSC) is triggered through phagocytosis of MSC by monocytic cells. Stem Cells 36 , 602–615 (2018).
Li, Y. et al. Cell-cell contact with proinflammatory macrophages enhances the immunotherapeutic effect of mesenchymal stem cells in two abortion models. Cell Mol. Immunol. 16 , 908–920 (2019).
De Paepe, M. E., Wong, T., Chu, S. & Mao, Q. Stromal cell-derived factor-1 (SDF-1) expression in very preterm human lungs: potential relevance for stem cell therapy for bronchopulmonary dysplasia. Exp. Lung Res. 46 , 146–156 (2020).
Wynn, R. F. et al. A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood 104 , 2643–2645 (2004).
Ryu, C. H. et al. Migration of human umbilical cord blood mesenchymal stem cells mediated by stromal cell-derived factor-1/CXCR4 axis via Akt, ERK, and p38 signal transduction pathways. Biochem Biophys. Res. Commun. 398 , 105–110 (2010).
Yang, C. et al. The biological changes of umbilical cord mesenchymal stem cells in inflammatory environment induced by different cytokines. Mol. Cell Biochem. 446 , 171–184 (2018).
Seedorf, G. et al. Hepatocyte growth factor as a downstream mediator of vascular endothelial growth factor-dependent preservation of growth in the developing lung. Am. J. Physiol. Lung Cell Mol. Physiol. 310 , L1098–L1110 (2016).
Chen, X. Y. et al. Therapeutic potential of human umbilical cord-derived mesenchymal stem cells in recovering from murine pulmonary emphysema under cigarette smoke exposure. Front. Med. 8 , 713824 (2021).
Katsha, A. M. et al. Paracrine factors of multipotent stromal cells ameliorate lung injury in an elastase-induced emphysema model. Mol. Ther. 19 , 196–203 (2011).
Kyurkchiev, D. et al. Secretion of immunoregulatory cytokines by mesenchymal stem cells. World J. Stem Cells 6 , 552–570 (2014).
Ren, Z. et al. Human umbilical-cord mesenchymal stem cells inhibit bacterial growth and alleviate antibiotic resistance in neonatal imipenem-resistant Pseudomonas aeruginosa infection. Innate Immun. 26 , 215–221 (2020).
Liu, J. et al. Type 2 alveolar epithelial cells differentiated from human umbilical cord mesenchymal stem cells alleviate mouse pulmonary fibrosis through beta-catenin-regulated cell apoptosis. Stem Cells Dev. 30 , 660–670 (2021).
Moodley, Y. et al. Human umbilical cord mesenchymal stem cells reduce fibrosis of bleomycin-induced lung injury. Am. J. Pathol. 175 , 303–313 (2009).
Li, D. Y., Li, R. F., Sun, D. X., Pu, D. D. & Zhang, Y. H. Mesenchymal stem cell therapy in pulmonary fibrosis: a meta-analysis of preclinical studies. Stem Cell Res. Ther. 12 , 461 (2021).
Lam, G., Zhou, Y., Wang, J. X. & Tsui, Y. P. Targeting mesenchymal stem cell therapy for severe pneumonia patients. World J. Stem Cells 13 , 139–154 (2021).
Chen, K. et al. Human umbilical cord mesenchymal stem cells hUC-MSCs exert immunosuppressive activities through a PGE2-dependent mechanism. Clin. Immunol. 135 , 448–458 (2010).
Ren, G. et al. Mesenchymal stem cell-mediated immunosuppression occurs via concerted action of chemokines and nitric oxide. Cell Stem Cell 2 , 141–150 (2008).
Loy, H. et al. Therapeutic implications of human umbilical cord mesenchymal stromal cells in attenuating influenza A(H5N1) virus-associated acute lung injury. J. Infect. Dis. 219 , 186–196 (2019).
Gazdhar, A. et al. Targeted gene transfer of hepatocyte growth factor to alveolar type II epithelial cells reduces lung fibrosis in rats. Hum. Gene Ther. 24 , 105–116 (2013).
Wang, W. et al. Therapeutic mechanisms of mesenchymal stem cells in acute respiratory distress syndrome reveal potentials for Covid-19 treatment. J. Transl. Med. 19 , 198 (2021).
Chu, K. A. et al. Reversal of bleomycin-induced rat pulmonary fibrosis by a xenograft of human umbilical mesenchymal stem cells from Wharton’s jelly. Theranostics 9 , 6646–6664 (2019).
Chen, Q. H. et al. Mesenchymal stem cells regulate the Th17/Treg cell balance partly through hepatocyte growth factor in vitro. Stem Cell Res. Ther. 11 , 91 (2020).
Li, L. et al. Human umbilical cord-derived mesenchymal stem cells downregulate inflammatory responses by shifting the Treg/Th17 profile in experimental colitis. Pharmacology 92 , 257–264 (2013).
Zheng, L., Wang, S., Yang, H. & Lyu, X. [Research progress of mesenchymal stem cells attenuating acute respiratory distress syndrome by regulating the balance of M1/M2 macrophage polarization]. Zhonghua Wei Zhong Bing. Ji Jiu Yi Xue 33 , 509–512 (2021).
Fasshauer, M. & Bluher, M. Adipokines in health and disease. Trends Pharm. Sci. 36 , 461–470 (2015).
Kershaw, E. E. & Flier, J. S. Adipose tissue as an endocrine organ. J. Clin. Endocrinol. Metab. 89 , 2548–2556 (2004).
Kurylowicz, A. & Kozniewski, K. Anti-inflammatory strategies targeting metaflammation in type 2 diabetes. Molecules 25 , 2224 (2020).
Liu, J. et al. Homing and restorative effects of bone marrow-derived mesenchymal stem cells on cisplatin injured ovaries in rats. Mol. Cells 37 , 865–872 (2014).
Jalalie, L. et al. Distribution of the CM-Dil-labeled human umbilical cord vein mesenchymal stem cells migrated to the cyclophosphamide-injured ovaries in C57BL/6 mice. Iran. Biomed. J. 23 , 200–208 (2019).
Takehara, Y. et al. The restorative effects of adipose-derived mesenchymal stem cells on damaged ovarian function. Lab. Investig. 93 , 181–193 (2013).
Richards, J. S., Ren, Y. A., Candelaria, N., Adams, J. E. & Rajkovic, A. Ovarian Follicular Theca Cell Recruitment, Differentiation, and Impact on Fertility: 2017 Update. Endocr. Rev. 39 , 1–20 (2018).
Young, J. M. & McNeilly, A. S. Theca: the forgotten cell of the ovarian follicle. Reproduction 140 , 489–504 (2010).
Trzyna, A. & Banas-Zabczyk, A. Adipose-derived stem cells secretome and its potential application in “stem cell-free therapy”. Biomolecules 11 , 878 (2021).
Ding, C. et al. Human amniotic mesenchymal stem cells improve ovarian function in natural aging through secreting hepatocyte growth factor and epidermal growth factor. Stem Cell Res. Ther. 9 , 55 (2018).
Kedenko, L. et al. Genetic polymorphisms at SIRT1 and FOXO1 are associated with carotid atherosclerosis in the SAPHIR cohort. BMC Med. Genet. 15 , 112 (2014).
Shojafar, E., Soleimani Mehranjani, M. & Shariatzadeh, S. M. A. Adipose derived mesenchymal stem cells improve the structure and function of autografted mice ovaries through reducing oxidative stress and inflammation: a stereological and biochemical analysis. Tissue Cell 56 , 23–30 (2019).
Liu, M. et al. Small extracellular vesicles derived from embryonic stem cells restore ovarian function of premature ovarian failure through PI3K/AKT signaling pathway. Stem Cell Res. Ther. 11 , 3 (2020).
Li, Z., Zhang, M., Tian, Y., Li, Q. & Huang, X. Mesenchymal stem cells in premature ovarian insufficiency: mechanisms and prospects. Front. Cell Dev. Biol. 9 , 718192 (2021).
Forghani, A. et al. Differentiation of adipose tissue-derived CD34+/CD31- cells into endothelial cells in vitro. Regen. Eng. Transl. Med 6 , 101–110 (2020).
Baer, P. C. Adipose-derived stem cells and their potential to differentiate into the epithelial lineage. Stem Cells Dev. 20 , 1805–1816 (2011).
Wang, C. et al. Differentiation of adipose-derived stem cells into contractile smooth muscle cells induced by transforming growth factor-beta1 and bone morphogenetic protein-4. Tissue Eng. Part A 16 , 1201–1213 (2010).
Chen, L. et al. Adipose-derived stem cells promote diabetic wound healing via the recruitment and differentiation of endothelial progenitor cells into endothelial cells mediated by the VEGF-PLCgamma-ERK pathway. Arch. Biochem Biophys. 692 , 108531 (2020).
Dekoninck, S. & Blanpain, C. Stem cell dynamics, migration and plasticity during wound healing. Nat. Cell Biol. 21 , 18–24 (2019).
Qian, L., Pi, L., Fang, B. R. & Meng, X. X. Adipose mesenchymal stem cell-derived exosomes accelerate skin wound healing via the lncRNA H19/miR-19b/SOX9 axis. Lab. Investig. 101 , 1254–1266 (2021).
Fujiwara, O. et al. Adipose-derived stem cells improve grafted burn wound healing by promoting wound bed blood flow. Burns Trauma 8 , tkaa009 (2020).
Chen, T. et al. Efficient and sustained IGF-1 expression in the adipose tissue-derived stem cells mediated via a lentiviral vector. J. Mol. Histol. 46 , 1–11 (2015).
Zhou, K. et al. Immunosuppression of human adipose-derived stem cells on T cell subsets via the reduction of NF-kappaB activation mediated by PD-L1/PD-1 and Gal-9/TIM-3 pathways. Stem Cells Dev. 27 , 1191–1202 (2018).
Moll, G. et al. Intravascular mesenchymal stromal/stem cell therapy product diversification: time for new clinical guidelines. Trends Mol. Med. 25 , 149–163 (2019).
He, X. et al. Spontaneous apoptosis of cells in therapeutic stem cell preparation exert immunomodulatory effects through release of phosphatidylserine. Signal Transduct. Target Ther. 6 , 270 (2021).
Lukomska, B. et al. Challenges and controversies in human mesenchymal stem cell therapy. Stem Cells Int. 2019 , 9628536 (2019).
Li, C., Zhao, H. & Wang, B. Challenges for mesenchymal stem cell-based therapy for COVID-19. Drug Des. Devel Ther. 14 , 3995–4001 (2020).
Nguyen Thanh, L. et al. Outcomes of bone marrow mononuclear cell transplantation combined with interventional education for autism spectrum disorder. Stem Cells Transl. Med. 10 , 14–26 (2020).
Nguyen Thanh, L. et al. Can autologous adipose-derived mesenchymal stem cell transplantation improve sexual function in people with sexual functional deficiency? Stem Cell Rev. Rep. 17 , 2153–2163 (2021).
Caplan, A. I. Mesenchymal stem cells: time to change the name! Stem Cells Transl. Med. 6 , 1445–1451 (2017).
de Windt, T. S., Vonk, L. A. & Saris, D. B. F. Response to: Mesenchymal stem cells: time to change the name! Stem Cells Transl. Med. 6 , 1747–1748 (2017).
Boregowda, S. V., Booker, C. N. & Phinney, D. G. Mesenchymal stem cells: the moniker fits the science. Stem Cells 36 , 7–10 (2018).
Masterson, C. & O’Toole, D. The mesenchymal stromal cell magic bullet finds yet another target. Stem Cell Res. Ther. 5 , 82 (2014).
Murray, I. R. et al. Rogue stem cell clinics. Bone Jt. J. 102-B , 148–154 (2020).
Lyons, S., Salgaonkar, S. & Flaherty, G. T. International stem cell tourism: a critical literature review and evidence-based recommendations. Int. Health 14 , 132–141 (2022).
He, C. et al. Mesenchymal stem cell-based treatment in autoimmune liver diseases: underlying roles, advantages and challenges. Ther. Adv. Chronic Dis. 12 , 2040622321993442 (2021).
Bertheuil, N. et al. Adipose mesenchymal stromal cells: definition, immunomodulatory properties, mechanical isolation and interest for plastic surgery. Ann. Chir. Plast. Esthet. 64 , 1–10 (2019).
Chen, Y., Yu, Q., Hu, Y. & Shi, Y. Current research and use of mesenchymal stem cells in the therapy of autoimmune diseases. Curr. Stem Cell Res. Ther. 14 , 579–582 (2019).
Han, Y. et al. The secretion profile of mesenchymal stem cells and potential applications in treating human diseases. Signal Transduct. Target Ther. 7 , 92 (2022).
Rahmani, A. et al. Mesenchymal stem cell-derived extracellular vesicle-based therapies protect against coupled degeneration of the central nervous and vascular systems in stroke. Ageing Res. Rev. 62 , 101106 (2020).
Zhou, W. et al. Single-cell profiles and clinically useful properties of human mesenchymal stem cells of adipose and bone marrow origin. Am. J. Sports Med. 47 , 1722–1733 (2019).
Pachler, K. et al. A good manufacturing practice-grade standard protocol for exclusively human mesenchymal stromal cell-derived extracellular vesicles. Cytotherapy 19 , 458–472 (2017).
Borger, V., Staubach, S., Dittrich, R., Stambouli, O. & Giebel, B. Scaled isolation of mesenchymal stem/stromal cell-derived extracellular vesicles. Curr. Protoc. Stem Cell Biol. 55 , e128 (2020).
Nikfarjam, S., Rezaie, J., Zolbanin, N. M. & Jafari, R. Mesenchymal stem cell derived-exosomes: a modern approach in translational medicine. J. Transl. Med. 18 , 449 (2020).
Monticelli, S. & Natoli, G. Short-term memory of danger signals and environmental stimuli in immune cells. Nat. Immunol. 14 , 777–784 (2013).
Venkatesha, S. et al. Soluble endoglin contributes to the pathogenesis of preeclampsia. Nat. Med. 12 , 642–649 (2006).
Bernardo, M. E. & Fibbe, W. E. Mesenchymal stromal cells: sensors and switchers of inflammation. Cell Stem Cell 13 , 392–402 (2013).
Liu, G. Y. et al. Short-term memory of danger signals or environmental stimuli in mesenchymal stem cells: implications for therapeutic potential. Cell Mol. Immunol. 13 , 369–378 (2016).
Diez-Tejedor, E. et al. Reparative therapy for acute ischemic stroke with allogeneic mesenchymal stem cells from adipose tissue: a safety assessment: a phase II randomized, double-blind, placebo-controlled, single-center, pilot clinical trial. J. Stroke Cerebrovasc. Dis. 23 , 2694–2700 (2014).
Laskowitz, D. T. et al. Allogeneic umbilical cord blood infusion for adults with ischemic stroke: clinical outcomes from a phase I safety study. Stem Cells Transl. Med. 7 , 521–529 (2018).
Jeon, S. R. et al. Treatment of spinal cord injury with bone marrow-derived, cultured autologous mesenchymal stem cells. Tissue Eng. Regenerative Med. 7 , 316–322 (2010).
Park, J. H. et al. Long-term results of spinal cord injury therapy using mesenchymal stem cells derived from bone marrow in humans. Neurosurgery 70 , 1238–1247 (2012).
Saito, F. et al. Administration of cultured autologous bone marrow stromal cells into cerebrospinal fluid in spinal injury patients: a pilot study. Restor. Neurol. Neurosci. 30 , 127–136 (2012).
El-Kheir, W. A. et al. Autologous bone marrow-derived cell therapy combined with physical therapy induces functional improvement in chronic spinal cord injury patients. Cell Transpl. 23 , 729–745 (2014).
Karamouzian, S., Nematollahi-Mahani, S. N., Nakhaee, N. & Eskandary, H. Clinical safety and primary efficacy of bone marrow mesenchymal cell transplantation in subacute spinal cord injured patients. Clin. Neurol. Neurosurg. 114 , 935–939 (2012).
Pal, R. et al. Ex vivo-expanded autologous bone marrow-derived mesenchymal stromal cells in human spinal cord injury/paraplegia: a pilot clinical study. Cytotherapy 11 , 897–911 (2009).
Mendonca, M. V. et al. Safety and neurological assessments after autologous transplantation of bone marrow mesenchymal stem cells in subjects with chronic spinal cord injury. Stem Cell Res. Ther. 5 , 126 (2014).
Vaquero, J. et al. Intrathecal administration of autologous mesenchymal stromal cells for spinal cord injury: safety and efficacy of the 100/3 guideline. Cytotherapy 20 , 806–819 (2018).
Dai, G. et al. Transplantation of autologous bone marrow mesenchymal stem cells in the treatment of complete and chronic cervical spinal cord injury. Brain Res. 1533 , 73–79 (2013).
Jiang, P. C. et al. A clinical trial report of autologous bone marrow-derived mesenchymal stem cell transplantation in patients with spinal cord injury. Exp. Ther. Med. 6 , 140–146 (2013).
Jarocha, D., Milczarek, O., Wedrychowicz, A., Kwiatkowski, S. & Majka, M. Continuous improvement after multiple mesenchymal stem cell transplantations in a patient with complete spinal cord injury. Cell Transpl. 24 , 661–672 (2015).
Huang, L. et al. A randomized, placebo-controlled trial of human umbilical cord blood mesenchymal stem cell infusion for children with cerebral palsy. Cell Transpl. 27 , 325–334 (2018).
Karussis, D. et al. Safety and immunological effects of mesenchymal stem cell transplantation in patients with multiple sclerosis and amyotrophic lateral sclerosis. Arch. Neurol. 67 , 1187–1194 (2010).
Yamout, B. et al. Bone marrow mesenchymal stem cell transplantation in patients with multiple sclerosis: a pilot study. J. Neuroimmunol. 227 , 185–189 (2010).
Mohajeri, M., Farazmand, A., Mohyeddin Bonab, M., Nikbin, B. & Minagar, A. FOXP3 gene expression in multiple sclerosis patients pre- and post mesenchymal stem cell therapy. Iran. J. Allergy Asthma Immunol. 10 , 155–161 (2011).
Odinak, M. M. et al. [Transplantation of mesenchymal stem cells in multiple sclerosis]. Zh . Nevrol. Psikhiatr Im. S S Korsakova 111 , 72–76 (2011).
Bonab, M. M. et al. Autologous mesenchymal stem cell therapy in progressive multiple sclerosis: an open label study. Curr. Stem Cell Res Ther. 7 , 407–414 (2012).
Mohyeddin Bonab, M. et al. Evaluation of cytokines in multiple sclerosis patients treated with mesenchymal stem cells. Arch. Med Res. 44 , 266–272 (2013).
Llufriu, S. et al. Randomized placebo-controlled phase II trial of autologous mesenchymal stem cells in multiple sclerosis. PLoS ONE 9 , e113936 (2014).
Harris, V. K., Vyshkina, T. & Sadiq, S. A. Clinical safety of intrathecal administration of mesenchymal stromal cell-derived neural progenitors in multiple sclerosis. Cytotherapy 18 , 1476–1482 (2016).
Dahbour, S. et al. Mesenchymal stem cells and conditioned media in the treatment of multiple sclerosis patients: clinical, ophthalmological and radiological assessments of safety and efficacy. CNS Neurosci. Ther. 23 , 866–874 (2017).
Meng, M. et al. Umbilical cord mesenchymal stem cell transplantation in the treatment of multiple sclerosis. Am. J. Transl. Res. 10 , 212–223 (2018).
Fernandez, O. et al. Adipose-derived mesenchymal stem cells (AdMSC) for the treatment of secondary-progressive multiple sclerosis: a triple blinded, placebo controlled, randomized phase I/II safety and feasibility study. PLoS ONE 13 , e0195891 (2018).
Alvarez-Fuente, M. et al. Off-label mesenchymal stromal cell treatment in two infants with severe bronchopulmonary dysplasia: clinical course and biomarkers profile. Cytotherapy 20 , 1337–1344 (2018).
Edessy, M. et al. Autologous stem cells therapy, The first baby of idiopathic premature ovarian failure. Acta Med. Int. 3 , 19–23 (2016).
Gabr, H., Elkheir, W. & El-Gazzar, A. Autologous stem cell transplantation in patients with idiopathic premature ovarian failure. J. Tissue Sci. Eng. 7 , 27 (2016).
Bakhtiary, M. et al. Comparison of transplantation of bone marrow stromal cells (BMSC) and stem cell mobilization by granulocyte colony stimulating factor after traumatic brain injury in rat. Iran. Biomed. J. 14 , 142–149 (2010).
Zhou, Z. et al. Comparison of mesenchymal stromal cells from human bone marrow and adipose tissue for the treatment of spinal cord injury. Cytotherapy 15 , 434–448 (2013).
Yousefifard, M. et al. Human bone marrow-derived and umbilical cord-derived mesenchymal stem cells for alleviating neuropathic pain in a spinal cord injury model. Stem Cell Res. Ther. 7 , 36 (2016).
Takahashi, A. et al. Comparison of mesenchymal stromal cells isolated from murine adipose tissue and bone marrow in the treatment of spinal cord injury. Cell Transpl. 27 , 1126–1139 (2018).
Hao, T. et al. Comparison of bone marrow-vs. adipose tissue-derived mesenchymal stem cells for attenuating liver fibrosis. Exp. Ther. Med. 14 , 5956–5964 (2017).
Zare, H., Jamshidi, S., Dehghan, M. M., Saheli, M. & Piryaei, A. Bone marrow or adipose tissue mesenchymal stem cells: Comparison of the therapeutic potentials in mice model of acute liver failure. J. Cell Biochem 119 , 5834–5842 (2018).
Arminan, A. et al. Mesenchymal stem cells provide better results than hematopoietic precursors for the treatment of myocardial infarction. J. Am. Coll. Cardiol. 55 , 2244–2253 (2010).
Gaebel, R. et al. Cell origin of human mesenchymal stem cells determines a different healing performance in cardiac regeneration. PLoS ONE 6 , e15652 (2011).
Dayan, V. et al. Mesenchymal stromal cells mediate a switch to alternatively activated monocytes/macrophages after acute myocardial infarction. Basic Res. Cardiol. 106 , 1299–1310 (2011).
Lopez, Y. et al. Wharton’s jelly or bone marrow mesenchymal stromal cells improve cardiac function following myocardial infarction for more than 32 weeks in a rat model: a preliminary report. Curr. Stem Cell Res. Ther. 8 , 46–59 (2013).
Rasmussen, J. G. et al. Comparison of human adipose-derived stem cells and bone marrow-derived stem cells in a myocardial infarction model. Cell Transpl. 23 , 195–206 (2014).
Abd Emami, B. et al. Mechanical and chemical predifferentiation of mesenchymal stem cells into cardiomyocytes and their effectiveness on acute myocardial infarction. Artif. Organs 42 , E114–E126 (2018).
Omar, A. M., Meleis, A. E., Arfa, S. A., Zahran, N. M. & Mehanna, R. A. Comparative study of the therapeutic potential of mesenchymal stem cells derived from adipose tissue and bone marrow on acute myocardial infarction model. Oman Med. J. 34 , 534–543 (2019).
Download references
Acknowledgements
The authors would like to thank the Vingroup Scientific Research and Clinical Application Fund (grant number: PRO. 19.47) for supporting this work. All figures were created with Biorender.com. This work is supported by the Vingroup Scientific Research and Clinical Application Fund (Grant number: PRO.19.47).
Author information
Authors and affiliations.
Department of Research and Development, Vinmec Research Institute of Stem Cell and Gene Technology, Vinmec Healthcare System, Hanoi, Vietnam
Duc M. Hoang, Trung Q. Bach, Quyen T. Nguyen, Trang T. K. Phan, Giang H. Nguyen, Phuong T. T. Le, Van T. Hoang & Liem Thanh Nguyen
Department of Cellular Therapy, Vinmec High-Tech Center, Vinmec Healthcare System, Hanoi, Vietnam
Phuong T. Pham & Anh T. L. Ngo
Institute for Science & Technology in Medicine, Keele University, Keele, UK
Nicholas R. Forsyth
Department of Biology, Stanford University, Stanford, CA, USA
Michael Heke
You can also search for this author in PubMed Google Scholar
Contributions
D.M.H.: conception and design, manuscript writing, administrative support, data analysis and interpretation, and final approval of the manuscript. P.T.P.: manuscript writing (BM- and UC-MSC sections) and data analysis and interpretation. T.Q.B.: manuscript writing (BM- and UC-MSC sections) and data analysis and interpretation. A.T.L.N.: manuscript writing (UC-MSC section), figure presentation, and data analysis and interpretation. Q.T.N., T.T.K.P., G.H.N., P.T.T.L., and V.T.H.: manuscript writing and data analysis and interpretation. N.R.F. and M.H.: manuscript writing and editing and data analysis and interpretation. L.T.N.: manuscript writing, administrative support, and final approval of the manuscript. All authors have read and approved the article.
Corresponding author
Correspondence to Duc M. Hoang .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hoang, D.M., Pham, P.T., Bach, T.Q. et al. Stem cell-based therapy for human diseases. Sig Transduct Target Ther 7 , 272 (2022). https://doi.org/10.1038/s41392-022-01134-4
Download citation
Received : 15 March 2022
Revised : 19 July 2022
Accepted : 21 July 2022
Published : 06 August 2022
DOI : https://doi.org/10.1038/s41392-022-01134-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

IMAGES
VIDEO
COMMENTS
Abstract. The potential impact of stem cell technology on medical and dental practice is vast. Stem cell research will not only provide the foundation for future therapies, but also reveal unique insights into basic disease mechanisms. Therefore, an understanding of stem cell technology will be necessary for clinicians in the future.
Learn about the benefits and drawbacks of stem cell research, from treating diseases to ethical issues. Compare embryonic and non-embryonic stem cells, and explore the potential and challenges of this medical technology.
Stem cells: The body's master cells. Stem cells are a special type of cells that have two important properties. They are able to make more cells like themselves. That is, they self-renew. And they can become other cells that do different things in a process known as differentiation. Stem cells are found in almost all tissues of the body.
Abstract. The ethical implications of stem cell research are often described in terms of risks, side effects, safety, and therapeutic value, which are examples of so-called hard impacts. Hard impacts are typically measurable and quantifiable. To understand the broader spectrum of ethical implications of stem cell research on science and society ...
Pros and Cons. Pros and Cons of Using Various Stem Cells. Limitations on ASC ability to differentiate are still uncertain; currently thought to be multi or unipotent. Unsure whether they would be rejected if used in transplants. Methods for ensured reproducibility and maintenance, as differentiated tissues are not certain.
Learn about the pros and cons of stem cell research, including adult and embryonic stem cells, and how they can be used for medical treatments. Find out the ethical, scientific, and practical issues involved in this field of study.
The Role of Various Factors in Neural Differentiation of Human Umbilical Cord Mesenchymal Stem Cells with a Special Focus on the Physical Stimulants, Current Stem Cell Research & Therapy, 19, 2 ...
7. Stem cell research Helps For Better Drug Testing: The use of stem cells in therapeutics can minimize the need for animal testing. With stem cells, a colony of cells can be grown that mimic a disease and act as a model for drug testing and treatment (E.g., cancer cells).
The drug is based on expanded adipose-derived stem cells 26. In both cases the drugs are allogeneic, which provides strong advantage other autologous products due to possibility of detailed testing regarding both safety and potency before release. Nowadays other sources of MSCs are also used for clinical therapies.
2) Stem Cell Research - Pros and Cons About the Methods Involved. The controversy regarding the method involved was much tenser when researchers used Embryonic Stem Cells as their main method for stem cell research. DISCLAIMER: These points are based on the old debate about the methods of stem cells research, from before 2007.
MS: Proponents argue that embryonic stem cell research holds great promise for understanding and curing diabetes, Parkinson's disease, spinal cord injury, and other debilitating conditions. Opponents argue that the research is unethical, because deriving the stem cells destroys the blastocyst, an unimplanted human embryo at the sixth to ...
Stem cell research has brought about a major breakthrough in the field of medical research. It refers to the study of mammalian stem cells for determining their use in remedial measures for various health disorders. This write-up talks about the pros and cons of stem cell research.
Debating Pros and Cons Stem Cell Research From the Journal of the American Medical Association, August 9, 2000, Vol. 284, No. 6: 681-682. Retrieved from the MAC Library's print collection
According to the Mayo Clinic, stem cells can be used to: grow new cells in a laboratory to replace damaged organs or tissues. correct parts of organs that don't work properly. research causes of ...
Here are some of its pros and cons. Advantages. Stem cell research offers countless medical possibilities. After all, the cells are undifferentiated; this means that they can be used to treat ...
Therapeutic cloning is a method to produce stem cell lines that were genetic matches for adults and children. Steps in therapeutic cloning are: An egg is obtained from a human donor. The nucleus (DNA) is removed from the egg. Skin cells are taken from the patient. The nucleus (DNA) is removed from a skin cell.
Stem cell research is one of the most fascinating areas of contemporary biology, but, as with many expanding fields of scientific inquiry, research on stem cells raises scientific questions as rapidly as it generates new discoveries. ... Pros and Cons of Using Various Stem Cells.
Stem cell therapy is the use of stem cells as a treatment for a condition. Stem cells are given to people to replace cells that have been destroyed or have died. In the case of people with cancer, they may be used to help the body regain the ability to produce stem cells after treatment. In people with multiple myeloma and certain types of ...
Stem cells began their role in modern regenerative medicine in the 1950's with the first bone marrow transplantation occurring in 1956. Stem cell therapies are at present indicated for a range of clinical conditions beyond traditional origins to treat genetic blood diseases and have seen substantial success.
That is where a majority of the embryonic stem cell research pros and cons focus on when discussing this subject. How you personally define human life will usually dictate which side of the debate you support. List of the Pros of Embryonic Stem Cell Research. 1. The embryonic stem cells are harvested 5-7 days after conception.
Stem cells are noted for their ability to self-renew and differentiate into a variety of cell types. Some stem cells, described as totipotent cells, have tremendous capacity to self-renew and differentiate. Embryonic stem cells have pluripotent capacity, able to form tissues of all 3 germ layers but unable to form an entire live being. Research with embryonic stem cells has enabled ...
Stem cell therapy is a novel therapeutic approach that utilizes the unique properties of stem cells, including self-renewal and differentiation, to regenerate damaged cells and tissues in the ...