Home — Essay Samples — Education — Health Education — The Importance of Heart Diseases

The Importance of Heart Diseases
- Categories: Health Education
About this sample

Words: 500 |
Published: Mar 20, 2024
Words: 500 | Page: 1 | 3 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Education

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 609 words
3 pages / 1214 words
2 pages / 989 words
1 pages / 560 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Health Education
Community health refers to the health status and outcomes of a community as a whole, encompassing a variety of factors such as access to healthcare, environmental conditions, and individual behaviors. The importance of enhancing [...]
The pharmacy and drugstore industry is predominantly dominated by a duopoly consisting of Walgreens Boots Alliance and CVS Health Corporation, which make up just over 60% of the market share. Surprisingly, this industry is [...]
Dental hygiene is a vital component of healthcare that focuses on promoting oral health and preventing dental diseases. Dental hygienists play a crucial role in educating patients about proper oral hygiene practices, conducting [...]
Today I spent most of the day working at a caffeine Health Hub in the Life Science Complex. This topic was especially relevant due to it being the start of midterm week, a week where students drink a lot of coffee and energy [...]
Mental health education is a critical component of overall well-being, transcending individual experiences. Educational institutions and communities both play integral roles in disseminating this education, reaching individuals [...]
Health education is a comprehensive field that encompasses a range of strategies and approaches aimed at empowering individuals with knowledge and skills to make informed decisions about their health and well-being. Its scope [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
24/7 writing help on your phone
To install StudyMoose App tap and then “Add to Home Screen”

Heart Disease - Free Essay Examples and Topic Ideas
Heart disease refers to a range of conditions that affect the heart’s ability to function properly. These conditions may include issues with the heart’s blood vessels, valves, or rhythm. Heart disease is a leading cause of death worldwide, and common risk factors include a poor diet, lack of exercise, smoking, and high blood pressure or cholesterol. Symptoms of heart disease may include chest pain, shortness of breath, fatigue, and palpitations. Treatment options range from medications and lifestyle changes to surgery or other medical procedures, depending on the severity of the condition.
- 📘 Free essay examples for your ideas about Heart Disease
- 🏆 Best Essay Topics on Heart Disease
- ⚡ Simple & Heart Disease Easy Topics
- 🎓 Good Research Topics about Heart Disease
Essay examples
Essay topic.
Save to my list
Remove from my list
- Congestive Heart Failure
- Heart Failure
- Mrs. Mallard’s Heart Disease
- Heart Diseases in Cardiovascular Medicine
- Obesity and Heart Disease as a Consequences of Eating Fast Food
- Aarkstore Enterprise Disease and Therapy Review: Heart Failure
- Heart Transplant
- Congested Heart Failure Case Study
- Hypoplastic left heart syndrome HLHS is a rare congenital disease that is
- Heart Sounds Case
- A Change of Heart
- R.M.’s Symptoms – Heart
- The Heart and the Fist
- Structure And Function Of The Heart Physical Education
- Heart TransplantThe first ever heart transplant was done on a dog by
- Nervous System of Heart
- Introduction Learning for Life and Work Personal Development often referred to
- Heart Dissection Report
- Interviewing A Kind Heart
- Consequences of Phobia in Edgar Allan Poe’s The Tell-Tale Heart
- Book Review: Reclaim Your Heart
- A Change Of Heart About Animals: Rifkin’s Analysis
- “Art For Heart’s Sake” by R. Goldberg Analysis
- The Crucible and Heart of Drakness summary
- How does music affect your heart beat?
- Essay on Bury My Heart at Wounded Knee
- Whisper of the Heart vs. Linda Linda Linda
- Stakeholders Influencing the Purpose of Apple and British Heart Foundation
- Evil depiction in Heart of Darkness
- Examining The Heart Of Darkness English Literature Essay
- A Matter of the heart and Coach Knight
- Darkness in Heart of Darkness
FAQ about Heart Disease
👋 Hi! I’m your smart assistant Amy!
Don’t know where to start? Type your requirements and I’ll connect you to an academic expert within 3 minutes.
- Twin Cities
- Other Locations
Reflection and perspective are invited, collected, and presented here about the causes, care, control, prevention, epidemiology, and public policy of heart attacks.
| Title | Category |
|---|---|
| Coronary Disease-CVD-Trends | |
| References | |
| Institutions-Reports | |
| Personalities | |
| Memoirs | |
| Personalities | |
| Studies | |
| Studies | |
| Institutions-Reports | |
| Perspective | |
| Study Design-Methods | |
| Institutions-Reports | |
| Institutions-Reports | |
| Perspective | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Studies | |
| Study Design-Methods | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Other Risk Factors | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Institutions-Reports | |
| Institutions-Reports | |
| Study Design-Methods | |
| Study Design-Methods | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Study Design-Methods | |
| Institutions-Reports | |
| Perspective | |
| Perspective | |
| Institutions-Reports | |
| Study Design-Methods | |
| Other Risk Factors | |
| Perspective | |
| Stories | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Stories | |
| Studies | |
| Study Design-Methods | |
| Perspective | |
| Studies | |
| Coronary Disease-CVD-Trends | |
| Perspective | |
| Perspective | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Perspective | |
| Perspective | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Institutions-Reports | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Study Design-Methods | |
| Institutions-Reports | |
| Studies | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Perspective | |
| Perspective | |
| Institutions-Reports | |
| Other Risk Factors | |
| Studies | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Other Risk Factors | |
| Other Risk Factors | |
| Perspective | |
| Institutions-Reports | |
| Perspective | |
| Institutions-Reports | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Perspective | |
| Studies | |
| Perspective | |
| Perspective | |
| Perspective | |
| Perspective | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Perspective | |
| Institutions-Reports | |
| Perspective | |
| Perspective | |
| Study Design-Methods | |
| Perspective | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Institutions-Reports | |
| Study Design-Methods | |
| Other Risk Factors | |
| Studies | |
| Studies | |
| Studies | |
| Perspective | |
| Other Risk Factors | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Institutions-Reports | |
| Studies | |
| Study Design-Methods | |
| Study Design-Methods | |
| Study Design-Methods | |
| Perspective | |
| Study Design-Methods | |
| Study Design-Methods | |
| Institutions-Reports | |
| Study Design-Methods | |
| Perspective | |
| Perspective | |
| Institutions-Reports | |
| Study Design-Methods | |
| Institutions-Reports | |
| Studies | |
| Coronary Disease-CVD-Trends | |
| Other Risk Factors | |
| Other Risk Factors | |
| Other Risk Factors | |
| Other Risk Factors | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Coronary Disease-CVD-Trends | |
| Institutions-Reports | |
| Perspective | |
| Perspective | |
| Perspective | |
| Perspective | |
| Perspective | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Perspective | |
| Perspective | |
| Institutions-Reports | |
| Perspective | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Coronary Disease-CVD-Trends | |
| Studies | |
| Personalities | |
| Personalities | |
| Coronary Disease-CVD-Trends | |
| Perspective | |
| Perspective | |
| Studies | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Studies | |
| Institutions-Reports | |
| Perspective | |
| Coronary Disease-CVD-Trends | |
| Other Risk Factors | |
| Other Risk Factors | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Institutions-Reports | |
| Diet-Heart: Hypothesis to Theory to Practice to Policy | |
| Study Design-Methods | |
- Coronary Disease-CVD-Trends
- Diet-Heart: Hypothesis to Theory to Practice to Policy
- Institutions-Reports
- Other Risk Factors
- Personalities
- Perspective
- Study Design-Methods

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Heart-Healthy Living
- High Blood Pressure
- Sickle Cell Disease
- Sleep Apnea
- Information & Resources on COVID-19
- The Heart Truth®
- Learn More Breathe Better®
- Blood Diseases and Disorders Education Program
- Publications and Resources
- Blood Disorders and Blood Safety
- Sleep Science and Sleep Disorders
- Lung Diseases
- Health Disparities and Inequities
- Heart and Vascular Diseases
- Precision Medicine Activities
- Obesity, Nutrition, and Physical Activity
- Population and Epidemiology Studies
- Women’s Health
- Research Topics
- Clinical Trials
- All Science A-Z
- Grants and Training Home
- Policies and Guidelines
- Funding Opportunities and Contacts
- Training and Career Development
- Email Alerts
- NHLBI in the Press
- Research Features
- Ask a Scientist
- Past Events
- Upcoming Events
- Mission and Strategic Vision
- Divisions, Offices and Centers
- Advisory Committees
- Budget and Legislative Information
- Jobs and Working at the NHLBI
- Contact and FAQs
- NIH Sleep Research Plan
- < Back To Research Topics
Coronary Heart Disease Research
Language switcher.
For almost 75 years, the NHLBI has been at the forefront of improving the nation’s health and reducing the burden of heart and vascular diseases . Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to prevent and treat the onset of coronary heart disease and associated medical conditions.
NHLBI research that really made a difference
The NHLBI supports a wide range of long-term studies to understand the risk factors of coronary heart disease. These ongoing studies, among others, have led to many discoveries that have increased our understanding of the causes of cardiovascular disease among different populations, helping to shape evidence-based clinical practice guidelines.
- Risk factors that can be changed: The NHLBI Framingham Heart Study (FHS) revealed that cardiovascular disease is caused by modifiable risk factors such as smoking, high blood pressure , obesity , high cholesterol levels, and physical inactivity. It is why, in routine physicals, healthcare providers check for high blood pressure, high cholesterol, unhealthy eating patterns, smoking, physical inactivity, and unhealthy weight. The FHS found that cigarette smoking increases the risk of heart disease. Researchers also showed that cardiovascular disease can affect people differently depending on sex or race, underscoring the need to address health disparities.
- Risk factors for Hispanic/Latino adults: The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) found that heart disease risk factors are widespread among Hispanic/Latino adults in the United States , with 80% of men and 71% of women having at least one risk factor. Researchers also used HCHS/SOL genetic data to explore genes linked with central adiposity (the tendency to have excess body fat around the waist) in Hispanic/Latino adults. Before this study, genes linked with central adiposity, a risk factor for coronary heart disease, had been identified in people of European ancestry. These results showed that those genes also predict central adiposity for Hispanic/Latino communities. Some of the genes identified were more common among people with Mexican or Central/South American ancestry, while others were more common among people of Caribbean ancestry.
- Risk factors for African Americans: The Jackson Heart Study (JHS) began in 1997 and includes more than 5,300 African American men and women in Jackson, Mississippi. It has studied genetic and environmental factors that raise the risk of heart problems, especially high blood pressure, coronary heart disease, heart failure , stroke , and peripheral artery disease (PAD) . Researchers discovered a gene variant in African American individuals that doubles the risk of heart disease. They also found that even small spikes in blood pressure can lead to a higher risk of death. A community engagement component of the JHS is putting 20 years of the study’s findings into action by turning traditional gathering places, such as barbershops and churches, into health information hubs.
- Risk factors for American Indians: The NHLBI actively supports the Strong Heart Study , a long-term study that began in 1988 to examine cardiovascular disease and its risk factors among American Indian men and women. The Strong Heart Study is one of the largest epidemiological studies of American Indian people ever undertaken. It involves a partnership with 12 Tribal Nations and has followed more than 8,000 participants, many of whom live in low-income rural areas of Arizona, Oklahoma, and the Dakotas. Cardiovascular disease remains the leading cause of death for American Indian people. Yet the prevalence and severity of cardiovascular disease among American Indian people has been challenging to study because of the small sizes of the communities, as well as the relatively young age, cultural diversity, and wide geographic distribution of the population. In 2019, the NHLBI renewed its commitment to the Strong Heart Study with a new study phase that includes more funding for community-driven pilot projects and a continued emphasis on training and development. Read more about the goals and key findings of the Strong Heart Study.
Current research funded by the NHLBI
Within our Division of Cardiovascular Sciences , the Atherothrombosis and Coronary Artery Disease Branch of its Adult and Pediatric Cardiac Research Program and the Center for Translation Research and Implementation Science oversee much of our funded research on coronary heart disease.
Research funding
Find funding opportunities and program contacts for research on coronary heart disease.
Current research on preventing coronary heart disease
- Blood cholesterol and coronary heart disease: The NHLBI supports new research into lowering the risk of coronary heart disease by reducing levels of cholesterol in the blood. High levels of blood cholesterol, especially a type called low-density lipoprotein (LDL) cholesterol, raise the risk of coronary heart disease. However, even with medicine that lowers LDL cholesterol, there is still a risk of coronary heart disease due to other proteins, called triglyceride-rich ApoB-containing lipoproteins (ApoBCLs), that circulate in the blood. Researchers are working to find innovative ways to reduce the levels of ApoBCLs, which may help prevent coronary heart disease and other cardiovascular conditions.
- Pregnancy, preeclampsia, and coronary heart disease risk: NHLBI-supported researchers are investigating the link between developing preeclampsia during pregnancy and an increased risk for heart disease over the lifespan . This project uses “omics” data – such as genomics, proteomics, and other research areas – from three different cohorts of women to define and assess preeclampsia biomarkers associated with cardiovascular health outcomes. Researchers have determined that high blood pressure during pregnancy and low birth weight are predictors of atherosclerotic cardiovascular disease in women . Ultimately, these findings can inform new preventive strategies to lower the risk of coronary heart disease.
- Community-level efforts to lower heart disease risk among African American people: The NHLBI is funding initiatives to partner with churches in order to engage with African American communities and lower disparities in heart health . Studies have found that church-led interventions reduce risk factors for coronary heart disease and other cardiovascular conditions. NHLBI-supported researchers assessed data from more than 17,000 participants across multiple studies and determined that these community-based approaches are effective in lowering heart disease risk factors .
Find more NHLBI-funded studies on preventing coronary heart disease on the NIH RePORTER.

Learn about the impact of COVID-19 on your risk of coronary heart disease.
Current research on understanding the causes of coronary heart disease
- Pregnancy and long-term heart disease: NHLBI researchers are continuing the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-be (nuMoM2b) study to understand the relationship between pregnancy-related problems, such as gestational hypertension, and heart problems. The study also looks at how problems during pregnancy may increase risk factors for heart disease later in life. NuMoM2b launched in 2010, and long-term studies are ongoing, with the goal of collecting high-quality data and understanding how heart disease develops in women after pregnancy.
- How coronary artery disease affects heart attack risk: NHLBI-funded researchers are investigating why some people with coronary artery disease are more at risk for heart attacks than others. Researchers have found that people with coronary artery disease who have high-risk coronary plaques are more likely to have serious cardiac events, including heart attacks. However, we do not know why some people develop high-risk coronary plaques and others do not. Researchers hope that this study will help providers better identify which people are most at risk of heart attacks before they occur.
- Genetics of coronary heart disease: The NHLBI supports studies to identify genetic variants associated with coronary heart disease . Researchers are investigating how genes affect important molecular cascades involved in the development of coronary heart disease . This deeper understanding of the underlying causes for plaque buildup and damage to the blood vessels can inform prevention strategies and help healthcare providers develop personalized treatment for people with coronary heart disease caused by specific genetic mutations.
Find more NHLBI-funded studies on understanding the causes of coronary heart disease on the NIH RePORTER.

Recent findings suggest that cholesterol-lowering treatment can lower the risk of heart disease complications in people with HIV.
Current research on treatments for coronary heart disease
- Insight into new molecular targets for treatment: NHLBI-supported researchers are investigating the role of high-density lipoprotein (HDL) cholesterol in coronary heart disease and other medical conditions . Understanding how the molecular pathways of cholesterol affect the disease mechanism for atherosclerosis and plaque buildup in the blood vessels of the heart can lead to new therapeutic approaches for the treatment of coronary heart disease. Researchers have found evidence that treatments that boost HDL function can lower systemic inflammation and slow down plaque buildup . This mechanism could be targeted to develop a new treatment approach for coronary heart disease.
- Long-term studies of treatment effectiveness: The NHLBI is supporting the International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial EXTENDed Follow-up (EXTEND) , which compares the long-term outcomes of an initial invasive versus conservative strategy for more than 5,000 surviving participants of the original ISCHEMIA trial. Researchers have found no difference in mortality outcomes between invasive and conservative management strategies for patients with chronic coronary heart disease after more than 3 years. They will continue to follow up with participants for up to 10 years. Researchers are also assessing the impact of nonfatal events on long-term heart disease and mortality. A more accurate heart disease risk score will be constructed to help healthcare providers deliver more precise care for their patients.
- Evaluating a new therapy for protecting new mothers: The NHLBI is supporting the Randomized Evaluation of Bromocriptine In Myocardial Recovery Therapy for Peripartum Cardiomyopathy (REBIRTH) , for determining the role of bromocriptine as a treatment for peripartum cardiomyopathy (PPCM). Previous research suggests that prolactin, a hormone that stimulates the production of milk for breastfeeding, may contribute to the development of cardiomyopathy late in pregnancy or the first several months postpartum. Bromocriptine, once commonly used in the United States to stop milk production, has shown promising results in studies conducted in South Africa and Germany. Researchers will enroll approximately 200 women across North America who have been diagnosed with PPCM and assess their heart function after 6 months.
- Impact of mental health on response to treatment: NHLBI-supported researchers are investigating how mental health conditions can affect treatment effectiveness for people with coronary heart disease. Studies show that depression is linked to a higher risk for negative outcomes from coronary heart disease. Researchers found that having depression is associated with poor adherence to medical treatment for coronary heart disease . This means that people with depression are less likely to follow through with their heart disease treatment plans, possibly contributing to their chances of experiencing worse outcomes. Researchers are also studying new ways to treat depression in patients with coronary heart disease .
Find more NHLBI-funded studies on treating coronary heart disease on the NIH RePORTER.

Researchers have found no clear difference in patient survival or heart attack risk between managing heart disease through medication and lifestyle changes compared with invasive procedures.
Coronary heart disease research labs at the NHLBI
- Laboratory of Cardiac Physiology
- Laboratory of Cardiovascular Biology
- Minority Health and Health Disparities Population Laboratory
- Social Determinants of Obesity and Cardiovascular Risk Laboratory
- Laboratory for Cardiovascular Epidemiology and Genomics
- Laboratory for Hemostasis and Platelet Biology
Related coronary heart disease programs
- In 2002, the NHLBI launched The Heart Truth® , the first federally sponsored national health education program designed to raise awareness about heart disease as the leading cause of death in women. The NHLBI and The Heart Truth® supported the creation of the Red Dress® as the national symbol for awareness about women and heart disease, and also coordinate National Wear Red Day ® and American Heart Month each February.
- The Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC) facilitates access to and maximizes the scientific value of NHLBI biospecimen and data collections. A main goal is to promote the use of these scientific resources by the broader research community. BioLINCC serves to coordinate searches across data and biospecimen collections and provide an electronic means for requesting additional information and submitting requests for collections. Researchers wanting to submit biospecimen collections to the NHLBI Biorepository to share with qualified investigators may also use the website to initiate the application process.
- Our Trans-Omics for Precision Medicine (TOPMed) Program studies the ways genetic information, along with information about health status, lifestyle, and the environment, can be used to predict the best ways to prevent and treat heart, lung, blood, and sleep disorders. TOPMed specifically supports NHLBI’s Precision Medicine Activities.
- NHLBI population and epidemiology studies in different groups of people, including the Atherosclerosis Risk in Communities (ARIC) Study , the Multi-Ethnic Study of Atherosclerosis (MESA) , and the Cardiovascular Health Study (CHS) , have made major contributions to understanding the causes and prevention of heart and vascular diseases, including coronary heart disease.
- The Cardiothoracic Surgical Trials Network (CTSN) is an international clinical research enterprise that studies heart valve disease , arrhythmias , heart failure, coronary heart disease, and surgical complications. The trials span all phases of development, from early translation to completion, and have more than 14,000 participants. The trials include six completed randomized clinical trials, three large observational studies, and many other smaller studies.

Learn how heart disease may be different for women than for men.
Explore more NHLBI research on coronary heart disease
The sections above provide you with the highlights of NHLBI-supported research on coronary heart disease. You can explore the full list of NHLBI-funded studies on the NIH RePORTER .
To find more studies:
- Type your search words into the Quick Search box and press enter.
- Check Active Projects if you want current research.
- Select the Agencies arrow, then the NIH arrow, then check NHLBI .
If you want to sort the projects by budget size — from the biggest to the smallest — click on the FY Total Cost by IC column heading.
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
How Stress Can Increase Your Risk of Heart Disease
Can stress affect your heart.
- Exploring the Link
- Other Risk Factors
Signs That Stress May Be Affecting Your Heart
- Stress Management
When to Contact a Healthcare Provider
In the short term, stress can be beneficial; however, prolonged stress can lead to inflammation and coping mechanisms that can be harmful to your heart health. People with chronic stress, such as stress related to social isolation, work, finances, and/or racism, may face a higher risk of heart disease and risk factors like high blood pressure and cholesterol problems. This article explains the connection between stress and heart disease, as well as prevention methods to keep your heart as healthy as possible.
Goodboy Picture Company / Getty Images
Stress affects your body in many ways and can certainly impact heart health. Both acute and chronic stress lead to changes in the heart and blood vessels.
A Word From Verywell
Chronic stress can increase your risk of developing heart disease by affecting your blood pressure, increasing plaque buildup in your blood vessels, and leading to an increased overall state of inflammation. There are many techniques for dealing with stress. Make sure to speak with your healthcare provider regarding the best strategies to help manage your stress.
Acute Stress
In general, acute or sudden and short-lived stress isn't necessarily a problem for the heart. The human body has evolved the stress response, or fight-or-flight response, as a useful way to counteract danger. During a sudden stressful moment, the body releases adrenaline (epinephrine) which causes various effects on the cardiovascular system that can help escape or avoid danger. These include:
- Increased heart rate
- Stronger contraction of the heart muscle
- Change in blood vessels to direct blood flow to muscles
Chronic Stress
Chronic stress is stress that goes on for the long term. It affects the heart in several ways, leading to high cortisol levels and inflammation. This can lead to the following changes in the heart and blood vessels:
- High blood pressure
- Dyslipidemia , or abnormal cholesterol levels
- Atherosclerosis , or plaque buildup in blood vessels in the body and the heart
- Increased potential for blood clot formation
Is There a Link Between Stress and Heart Disease?
The stress-related changes in the heart and blood vessels in both acute and chronic stress can lead to heart disease.
Most of the time, the body can handle acute stress just fine and revert to its normal prestress state. However, in a condition known as stress cardiomyopathy (also known as Takotsubo cardiomyopathy and broken heart syndrome), the sudden stress results in the weakening of the heart muscle. This can cause heart failure, dangerous heart rhythm disturbances (arrhythmias), and even death. People with stress cardiomyopathy may experience the following symptoms:
- Sudden severe chest pain
- Shortness of breath
- Difficulty breathing
- Lightheadedness
- Loss of consciousness
Increased cortisol levels and dysregulation of the immune system that are directly related to stress can contribute to inflammation, atherosclerosis (plaque buildup in the arteries), and other risk factors of heart disease. In addition, unhealthy coping strategies for chronic stress (a sedentary lifestyle, certain eating patterns, and smoking cigarettes) can further increase this risk. Chronic stress and other mental health conditions are associated with the following heart and vascular conditions:
- Hypertension (high blood pressure)
- Atherosclerosis
- Heart attacks
- Heart failure
Other Risk Factors Related to Stress
In addition to the impact of stress on the heart, stress can also cause conditions that are also risk factors for heart disease. Stress and its impact on behavior can cause risk factors for heart disease, including:
- Insulin resistance and diabetes
- Immune system dysregulation
- Inflammation
It's important to recognize potential heart problems and risk factors and have an evaluation with your healthcare provider to diagnose and treat them. Possible signs that stress and other risk factors may be causing heart problems include the following:
- Chest discomfort
- Shortness of breath or feeling more winded than usual with your activities
- Palpitations, or the feeling of rapid or irregular heartbeats
- Sudden weight gain, which can be a sign of heart failure
If you feel that chronic stress is impacting your daily life, it's a sign that stress could be affecting other parts of the body, such as the heart. A healthcare provider can screen for other risk factors and help manage stress and related mental health conditions like anxiety and depression. Signs of chronic stress include:
- Fatigue and low energy levels
- Sleeping troubles
- Changes in bowel habits
- Weight gain or loss
- Mood changes, such as anxiety or depression
- Trouble concentrating
Stress Management Techniques for Heart Health
Managing stress can improve your quality of life and may help counteract the negative effects of stress on your body, including your heart. Some stress management techniques also have direct benefits for your heart.
Get Regular Exercise
Physical activity has numerous benefits for the body and mind. Exercise can release endorphins , the feel-good chemicals that can improve mood and manage stress. In addition, regular physical activity is one of the major lifestyle factors to improve and maintain heart health. The American Heart Association recommends getting 150 minutes of moderate-intensity activity per week.
Aim for getting some exercise daily by doing activities you enjoy, such as:
- A brisk walk or jog outside
- Exercise dance classes
- Playing sports like tennis, pickleball, soccer, or basketball
- Yoga and strengthening exercises
Try Relaxation Techniques
Relaxation techniques are meant to counteract the stress response and activate the part of the nervous system that promotes rest. They can be particularly effective during times of acute stress or anxiety. Though there is little direct evidence of their benefit for heart health, some studies show the benefits of relaxation techniques in lowering blood pressure.
Some examples of relaxation techniques include:
- Meditation with guided imagery
- Breathing exercises
- Progressive relaxation, or tensing and then relaxing your muscles
Get Enough Sleep
Poor sleep is associated with both chronic stress and risk of heart disease as well as other long-term health conditions. Getting enough high-quality sleep is important to manage stress and protect heart health. The American Heart Association recognizes sleep as one of the pillars of lifestyle management for a healthy heart and states that most adults should aim for seven to nine hours of high-quality rest each night.
Connect With Others
Another important way to counteract stress is to connect with others. Some people may cope with stress through isolation; however, social isolation and loneliness are linked to increased stress and worse cardiovascular health.
Social connection can be a good way to counteract stress, and it also lowers the risk of heart disease and stroke. A support network can provide support during hard times, help cope with stress, and promote overall well-being. Some ways to connect with others include:
- Participating in events at neighborhood, community, school, church, park, and recreational centers
- Joining a book club or activities at your library
- Participating in a gardening, nature, or walking club
- Volunteering
If you are having symptoms of chronic stress, you can schedule a visit with a healthcare provider who can provide tips and referrals for managing stress, such as counseling.
If you have any concerning heart attack symptoms, seek medical attention immediately by calling 9-1-1 to be transported to the nearest hospital. Heart attack symptoms include:
- Chest or upper abdominal pain or discomfort
- Discomfort might radiate to the neck, jaw, or upper arms
Our bodies evolved the stress response as a protective mechanism, and both acute and chronic stress can affect the heart in various ways. Usually, acute stress doesn't cause heart problems, but some people can develop stress-related cardiomyopathy. Chronic stress can lead to inflammation, high blood pressure, abnormal cholesterol, and atherosclerosis. Our coping mechanisms for stress, like sedentary behavior, dietary patterns, and smoking, can increase heart disease risk.
To counteract the effects of stress and keep a healthy heart, aim for regular physical activity, healthy sleep, and connection with others.
Osborne MT, Shin LM, Mehta NN, et al. Disentangling the links between psychosocial stress and cardiovascular disease . Circ Cardiovasc Imaging . 2020;13(8):e010931. doi:10.1161/CIRCIMAGING.120.010931
Centers for Disease Control and Prevention. About heart disease and mental health .
American Psychological Association. Stress effects on the body .
Singh T, Khan H, Gamble DT, et al. Takotsubo syndrome: pathophysiology, emerging concepts, and clinical implications . Circulation . 2022;145(13):1002-1019. doi:10.1161/CIRCULATIONAHA.121.055854
American Heart Association. Stress and heart health .
American Heart Association. Warning signs of a heart attack .
American Heart Association. Symptoms of heart failure .
MedlinePlus. Stress and your health .
Smith PJ, Merwin RM. The role of exercise in management of mental health disorders: an integrative review . Annu Rev Med. 2020;72:45-62. doi:10.1146/annurev-med-060619-022943
American Heart Association. Life's Essential 8 .
American Heart Association. Exercise within reach .
National Center for Complementary and Integrative Health. Relaxation techniques: what you need to know .
Cené CW, Beckie TM, Sims M, et al. Effects of objective and perceived social isolation on cardiovascular and brain health: a scientific statement from the American Heart Association . J Am Heart Assoc . 2022;11(16):e026493. doi:10.1161/JAHA.122.026493
American Psychological Association. The risks of social isolation .
Centers for Disease Control and Prevention. Social connection .
By Angela Ryan Lee, MD Dr. Lee is an Ohio-based board-certified physician specializing in cardiovascular diseases and internal medicine.
Heart Disease: Causal Effects of Cardiovascular Risk Factors Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction: Defining the Process of Cause and Effect
Monocausation versus multicausation of heart disease, preferred approach: multicausation, works cited.
The process of cause and effect can be described as a relationship between issues where one is the outcome of the other. The principle of causation incorporates two interdependent elements: action and reaction. When only one cause is involved, the process is called monocausation. One example of the process of cause and effect would be the impact of obesity on health. Obesity causes heart disease. Because it is identified as the most common reason that people develop this serious health problem, obesity is considered the major cause in this causation process. According to Bastien et al., obesity presents a danger to people since it leads to many negative outcomes including heart disease (369–370).
Excessive weight leads to an increase in fat cells in the body, and an increased amount of fatty and cholesterol deposits makes it more difficult for blood to reach the heart. This condition is called atherosclerosis (Bastien et al. 374). If the flow of blood becomes fully restricted, a person can have a heart attack. In such a case, the artery supplying blood to the heart muscle does not receive nutrients and oxygen, and this leads to damage to the heart’s muscle system.
Therefore, obesity can be considered a severe condition, and medical specialists all over the world are working on ways to eliminate its detrimental impact. Special interventions are being developed for obese people, along with supportive and educational programs.
While obesity is considered the most common cause of heart disease, it is not the only reason why people may develop this condition. Alternative causes include smoking, high blood pressure, unhealthy diet, or family history. The danger of smoking may be manifested in several ways. First, smoking impairs the lining of the arteries. This effect is similar to that produced by obesity: fatty material builds up, and arteries become too narrow for the heart to function normally (Breitling et al. 2841–2843).
Second, the carbon monoxide in cigarette smoke decreases the amount of oxygen in the blood. Third, nicotine stimulates the production of adrenaline, making the heart work harder. Finally, smokers’ blood is under threat of clotting, which increases the likelihood of stroke or heart attack.
High blood pressure (hypertension) is another serious cause of heart disease (Dickinson et al. 650–651). The damage from hypertension stems from the fact that coronary arteries gradually narrow because of cholesterol, fat, and other substances, the combination of which is referred to as plaque. Thus, it should be noted that atherosclerosis may develop not only as a result of obesity but also due to high blood pressure.
The role of diet is considered crucial in the prevention of heart disease. Therefore, an unhealthy diet is the next serious cause of this health condition (Jørgensen et al. g3617). The health of an individual who does not follow healthy eating habits is subject to significant deterioration. Eating fatty food does not present the only danger. The absence of such nutritional elements as fruit and vegetables, nuts, and fish is damaging for the organism. Apart from the impact of saturated fats, heart disease may be induced when a person consumes excessive amounts of salt or refined carbohydrates. Professionals strongly advise people with a high disposition to heart problems to reconsider their diet and make it more favorable for the organism.
In the same way, as in the development of many other diseases, family history plays a crucial role in the establishment of heart disease (Pandey et al. 285–286). People having relatives with such health problems are at a higher risk of developing heart disease. Since this condition does not depend on a person and cannot be changed, it is necessary to guard one’s health. People with a family history of heart disease should have regular check-ups, maintain a healthy weight, and refrain from smoking.
In my opinion, the multicausation approach is more suitable than monocausation when discussing the causes of heart disease. While obesity is considered a major factor, other causes lead to similar outcomes. Obesity is not the only factor that can lead to that artery blockage referred to as atherosclerosis. Smoking, high blood pressure, and an unhealthy diet can also be identified as culprits. Therefore, it is not possible to say that obesity is a single contributor to developing heart disease. Moreover, apart from bad habits, there remains one cause that cannot be controlled and puts people under threat regardless of their food preferences. A family history raises the chances to develop heart disease, and its role in an individual’s health should not be underestimated.
The principle of causation is an inevitability in the health-care system. Every disease has a cause that leads to specific outcomes. While some health conditions can be explained with the help of monocausation, others require a multicausation approach. In the case of heart disease, several factors whose impact is almost equal can contribute to the development of the disease. Therefore, although obesity may be regarded as the main cause of heart disease, monocausation cannot be applied in this case.
Bastien, Marjorie, et al. “Overview of Epidemiology and Contribution of Obesity to Cardiovascular Disease.” Progress in Cardiovascular Diseases , vol. 56, 2014, pp. 369-381.
Breitling, Lutz Philipp, et al. “Smoking, F2RL3 Methylation, and Prognosis in Stable Coronary Heart Disease.” European Heart Journal , vol. 33, no. 22, 2012, pp. 2841-2848.
Dickinson, Brent, et al. “Plasma MicroRNAs Serve as Biomarkers of Therapeutic Efficacy and Disease Progression in Hypertension-Induced Heart Failure.” European Journal of Heart Failure , vol. 15, no. 6, 2013, pp. 650-659.
Jørgensen, Torben, et al. “Effect of Screening and Lifestyle Counselling on Incidence of Ischaemic Heart Disease in General Population: Inter99 Randomised Trial.” BMJ , no. 348, 2014, pp. g3617.
Pandey, Arvind, et al. “Family History of Coronary Heart Disease and Markers of Subclinical Cardiovascular Disease: Where do We Stand?” Atherosclerosis , vol. 228, 2013, pp. 285-294.
- Heart Disease and Alzheimer's in Adult Women
- Prevalence of Cardiovascular Disease and Associated Risks
- The Buckling Instability in Arteries
- Atherosclerosis and Prostatitis: Inflammatory Markers
- Oxygenation and Supply of Blood to the Brain
- Cardiovascular Diseases as a Public Health Challenge
- Hypertension Care Plan for a Young Woman
- Magnetocardiography Advantages and Disadvantages
- Cardiovascular Diseases in the UAE
- Cardiovascular System: Pharmacokinetics and Pharmacodynamics
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2020, November 21). Heart Disease: Causal Effects of Cardiovascular Risk Factors. https://ivypanda.com/essays/heart-disease-and-contributing-factors/
"Heart Disease: Causal Effects of Cardiovascular Risk Factors." IvyPanda , 21 Nov. 2020, ivypanda.com/essays/heart-disease-and-contributing-factors/.
IvyPanda . (2020) 'Heart Disease: Causal Effects of Cardiovascular Risk Factors'. 21 November.
IvyPanda . 2020. "Heart Disease: Causal Effects of Cardiovascular Risk Factors." November 21, 2020. https://ivypanda.com/essays/heart-disease-and-contributing-factors/.
1. IvyPanda . "Heart Disease: Causal Effects of Cardiovascular Risk Factors." November 21, 2020. https://ivypanda.com/essays/heart-disease-and-contributing-factors/.
Bibliography
IvyPanda . "Heart Disease: Causal Effects of Cardiovascular Risk Factors." November 21, 2020. https://ivypanda.com/essays/heart-disease-and-contributing-factors/.
Investigation on Genetic Mutations Leading to Monogenic and Polygenic Heart Diseases Using Publicly Available Disease Databases
- Sanika Javeri Indiana University
An investigation was completed use publicly available NCBI and DISGNET databases to determine the genetic association to predominant heart diseases. Preliminary research was conducted to detect the two most common types of heart disease, hypertrophic cardiomyopathy (HCM) and coronary artery disease (CAD), and the respective monogenic and polygenic genes responsible for causing these diseases. The genetic etiology of the mutating genes was investigated with hopes that the phenotypic results could be established on publicly available databases. This would allow countless changes in medicine regarding heart disease such as accurate genetic counseling, treatment guidance, risk assessment, and preventative measures, such as living heart friendly lifestyle, can be taken to positively influence the disease course. This course of action would lead to early diagnosis in affected individuals and possibly preventing sudden cardiac death.
How to Cite
- Endnote/Zotero/Mendeley (RIS)
Copyright (c) 2024 Sanika Javeri

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License .
Copyright holder(s) granted JSR a perpetual, non-exclusive license to distriute & display this article.
Announcements
Call for papers: volume 13 issue 4.
If you are an undergraduate or graduate student at a college or university aspiring to publish, we are accepting submissions. Submit Your Article Now!
Deadline: 11:59 p.m. August 31, 2024
- heart disease
First artificial heart transplant in Houston offering hope for people with end-stage heart disease

HOUSTON, Texas (KTRK) -- A groundbreaking procedure performed in Houston is offering new hope for people with end-stage heart disease.
For the first time ever, doctors at the Texas Heart Institute at Baylor St. Luke's Medical Center implanted an artificial heart in a patient.
The 58-year-old had late-stage heart disease.
Behind the BiVACOR artificial heart
The BiVACOR Total Artificial Heart (TAH) is made out of titanium.
The device uses "magnetic levitation technology," also used in high-speed trains, to pump blood through the body.
The man received the device earlier this month and has since gotten a "real heart transplant."
The goal of the artificial device is to keep a patient alive long enough to get a real heart.
But there's hope. If trials are successful, the device could be a permanent solution.
"The other attempts at a permanent artificial heart have had several hundred moving parts. This has one. They've been limited," Dr. William Cohn said.
"We have to do that experiment. I can tell you in Huntington Beach, we have eight pumps that have been going without a failure in an aquarium," he continued. "Could this be a permanent device? Absolutely. Do we need to show it's safe and effective? Absolutely."
Four more patients will get the device as part of the ongoing study.

Why it could be a game-changer
At least 26 million people are affected worldwide by the epidemic.
Experts say 6.7 million Americans have heart failure.
Half of those newly diagnosed die within five years, and 90% die within 10 years.
The successful transplant also addresses critical challenges in cardiac care, such as long transplantation waitlists.
Related Topics
- HEALTH & FITNESS
- HEART DISEASE
- HEART TRANSPLANT
- TEXAS MEDICAL CENTER
Heart Disease

Jimmy Kimmel's 7-year-old son Billy undergoes third open-heart surgery

Medicare can now cover Wegovy for more senior citizens

Oral health linked to your heart function? Here's what experts say

2 heart transplant recipients honored during American Heart Month
Top stories.

Residents worry about safety after string of robberies in high-rises

Houston trades Loperfido, Billy Wagner's son Will in deadline deal

Houston under heightened security as dignitaries descend on city

West U 'Darth Vader' home with complex legal history is for sale

President Joe Biden outlines Supreme Court changes in Austin
Saharan dust arrives Tuesday but rain chances return this weekend
Texas Senate committee grills CenterPoint about Beryl response
ABC13 joins ABC News in new initiative for climate change education
The independent source for health policy research, polling, and news.
A New Use for Wegovy Opens the Door to Medicare Coverage for Millions of People with Obesity
Juliette Cubanski , Tricia Neuman , Nolan Sroczynski , and Anthony Damico Published: Apr 24, 2024
The FDA recently approved a new use for Wegovy (semaglutide), the blockbuster anti-obesity drug, to reduce the risk of heart attacks and stroke in people with cardiovascular disease who are overweight or obese. Wegovy belongs to a class of medications called GLP-1 (glucagon-like peptide-1) agonists that were initially approved to treat type 2 diabetes but are also highly effective anti-obesity drugs. The new FDA-approved indication for Wegovy paves the way for Medicare coverage of this drug and broader coverage by other insurers. Medicare is currently prohibited by law from covering Wegovy and other medications when used specifically for obesity. However, semaglutide is covered by Medicare as a treatment for diabetes, branded as Ozempic.
What does the FDA’s decision mean for Medicare coverage of Wegovy?
The FDA’s decision opens the door to Medicare coverage of Wegovy, which was first approved by the FDA as an anti-obesity medication. Soon after the FDA’s approval of the new use for Wegovy, the Centers for Medicare & Medicaid Services (CMS) issued a memo indicating that Medicare Part D plans can add Wegovy to their formularies now that it has a medically-accepted indication that is not specifically excluded from Medicare coverage . Because Wegovy is a self-administered injectable drug, coverage will be provided under Part D , Medicare’s outpatient drug benefit offered by private stand-alone drug plans and Medicare Advantage plans, not Part B, which covers physician-administered drugs.
How many Medicare beneficiaries could be eligible for coverage of Wegovy for its new use?
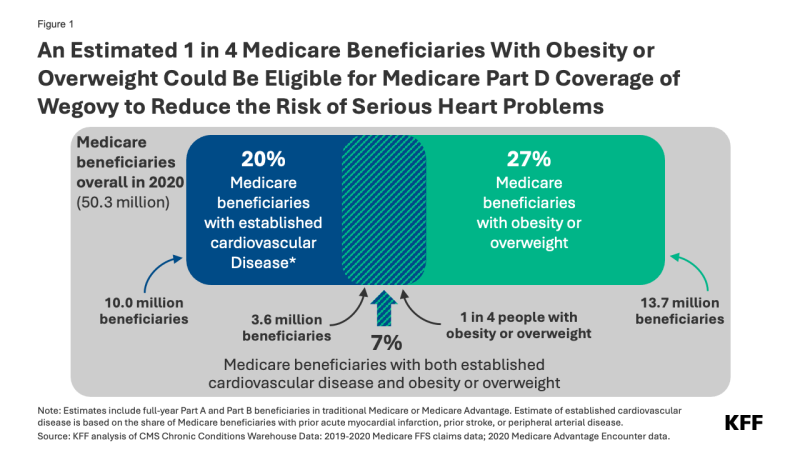
Of these 3.6 million beneficiaries, 1.9 million also had diabetes (other than Type 1) and may already have been eligible for Medicare coverage of GLP-1s as diabetes treatments prior to the FDA’s approval of the new use of Wegovy.
Not all people who are eligible based on the new indication are likely to take Wegovy, however. Some might be dissuaded by the potential side effects and adverse reactions . Out-of-pocket costs could also be a barrier. Based on the list price of $1,300 per month (not including rebates or other discounts negotiated by pharmacy benefit managers), Wegovy could be covered as a specialty tier drug, where Part D plans are allowed to charge coinsurance of 25% to 33%. Because coinsurance amounts are pegged to the list price, Medicare beneficiaries required to pay coinsurance could face monthly costs of $325 to $430 before they reach the new cap on annual out-of-pocket drug spending established by the Inflation Reduction Act – around $3,300 in 2024, based on brand drugs only, and $2,000 in 2025. But even paying $2,000 out of pocket would still be beyond the reach of many people with Medicare who live on modest incomes . Ultimately, how much beneficiaries pay out of pocket will depend on Part D plan coverage and formulary tier placement of Wegovy.
Further, some people may have difficulty accessing Wegovy if Part D plans apply prior authorization and step therapy tools to manage costs and ensure appropriate use. These factors could have a dampening effect on use by Medicare beneficiaries, even among the target population.
When will Medicare Part D plans begin covering Wegovy?
Some Part D plans have already announced that they will begin covering Wegovy this year, although it is not yet clear how widespread coverage will be in 2024. While Medicare drug plans can add new drugs to their formularies during the year to reflect new approvals and expanded indications, plans are not required to cover every new drug that comes to market. Part D plans are required to cover at least two drugs in each category or class and all or substantially all drugs in six protected classes . However, facing a relatively high price and potentially large patient population for Wegovy, many Part D plans might be reluctant to expand coverage now, since they can’t adjust their premiums mid-year to account for higher costs associated with use of this drug. So, broader coverage in 2025 could be more likely.
How might expanded coverage of Wegovy affect Medicare spending?
The impact on Medicare spending associated with expanded coverage of Wegovy will depend in part on how many Part D plans add coverage for it and the extent to which plans apply restrictions on use like prior authorization; how many people who qualify to take the drug use it; and negotiated prices paid by plans. For example, if plans receive a 50% rebate on the list price of $1,300 per month (or $15,600 per year), that could mean annual net costs per person around $7,800. If 10% of the target population (an estimated 360,000 people) uses Wegovy for a full year, that would amount to additional net Medicare Part D spending of $2.8 billion for one year for this one drug alone.
It’s possible that Medicare could select semaglutide for drug price negotiation as early as 2025, based on the earliest FDA approval of Ozempic in late 2017 . For small-molecule drugs like semaglutide, at least seven years must have passed from its FDA approval date to be eligible for selection, and for drugs with multiple FDA approvals, CMS will use the earliest approval date to make this determination. If semaglutide is selected for negotiation next year, a negotiated price would be available beginning in 2027. This could help to lower Medicare and out-of-pocket spending on semaglutide products, including Wegovy as well as Ozempic and Rybelsus, the oral formulation approved for type 2 diabetes. As of 2022, gross Medicare spending on Ozempic alone placed it sixth among the 10 top-selling drugs in Medicare Part D, with annual gross spending of $4.6 billion, based on KFF analysis . This estimate does not include rebates, which Medicare’s actuaries estimated to be 31.5% overall in 2022 but could be as high as 69% for Ozempic, according to one estimate.
What does this mean for Medicare coverage of anti-obesity drugs?
For now, use of GLP-1s specifically for obesity continues to be excluded from Medicare coverage by law. But the FDA’s decision signals a turning point for broader Medicare coverage of GLP-1s since Wegovy can now be used to reduce the risk of heart attack and stroke by people with cardiovascular disease and obesity or overweight, and not only as an anti-obesity drug. And more pathways to Medicare coverage could open up if these drugs gain FDA approval for other uses . For example, Eli Lilly has just reported clinical trial results showing the benefits of its GLP-1, Zepbound (tirzepatide), in reducing the occurrence of sleep apnea events among people with obesity or overweight. Lilly reportedly plans to seek FDA approval for this use and if approved, the drug would be the first pharmaceutical treatment on the market for sleep apnea.
If more Medicare beneficiaries with obesity or overweight gain access to GLP-1s based on other approved uses for these medications, that could reduce the cost of proposed legislation to lift the statutory prohibition on Medicare coverage of anti-obesity drugs. This is because the Congressional Budget Office (CBO), Congress’s official scorekeeper for proposed legislation, would incorporate the cost of coverage for these other uses into its baseline estimates for Medicare spending, which means that the incremental cost of changing the law to allow Medicare coverage for anti-obesity drugs would be lower than it would be without FDA’s approval of these drugs for other uses. Ultimately how widely Medicare Part D coverage of GLP-1s expands could have far-reaching effects on people with obesity and on Medicare spending.
| The estimate of Medicare beneficiaries who could be eligible for Medicare coverage of Wegovy for cardiovascular disease is based on individual-level claims and encounter data for beneficiaries in traditional Medicare and Medicare Advantage from the Chronic Conditions Data Warehouse (CCW). For beneficiaries in traditional Medicare, coding of individual-level fee-for-service (FFS) claims data matched the following chronic condition flags in the 2020 Medicare Beneficiary Summary File and segments: AMI_EVER, STROKE_TIA_EVER, and OBESITY. In addition to obesity, beneficiaries were coded with overweight if the following ICD-10 codes were identified in the claims with the same requirements as the CCW OBESITY flag: E66.3, Z68.25, Z68.26, Z68.27, Z68.28. Z68.29. To identify beneficiaries with peripheral arterial disease (PAD), we used ICD-9 diagnosis codes for PAD identified by either or in their analyses of peripheral arterial disease among Medicare beneficiaries; these studies are two of three references cited by CCW in the for peripheral vascular disease. We used the to convert the ICD-9 codes used in the Hirsch and Jaff studies to corresponding ICD-10 codes for our analysis based on the 2020 data (ICD-9 codes were replaced by ICD-10 codes in 2015). Beneficiaries who were coded with obesity or overweight and either a prior heart attack (AMI_EVER), prior stroke (STROKE_TIA_EVER), or peripheral arterial disease were coded as being eligible for the new use of Wegovy. Among this group, beneficiaries who were flagged as having diabetes (not including Type 1 Diabetes Mellitus) based on ICD-10 codes and using the same requirements as the CCW DIABETES flag, were identified as being eligible for GLP-1s approved for use as diabetes treatments. For Medicare Advantage enrollees, the ICD-10 codes for the CCW-developed algorithms for AMI, stroke, obesity, and diabetes (not including Type 1), plus ICD-10 codes specified above for overweight and peripheral arterial disease, were used to identify whether enrollees were eligible for the new use of Wegovy, based on 2020 encounter data and utilizing a within-year lookback period for all conditions (rather than ever, or in some cases a 2-year lookback that is used for traditional Medicare enrollees). Earlier years of data to enable a longer lookback period were not available for this analysis. Among the factors contributing to imprecision in the overall estimate: It is not possible to measure the degree of uncertainty associated with these different factors. |
- Medicare Part D
- Chronic Diseases
- Heart Disease
- Medicare Advantage
news release
- An Estimated 1 in 4 Medicare Beneficiaries With Obesity or Overweight Could Be Eligible for Medicare Coverage of Wegovy, an Anti-Obesity Drug, to Reduce Heart Risk
Also of Interest
- An Overview of the Medicare Part D Prescription Drug Benefit
- FAQs about the Inflation Reduction Act’s Medicare Drug Price Negotiation Program
- What Could New Anti-Obesity Drugs Mean for Medicare?
- Medicare Spending on Ozempic and Other GLP-1s Is Skyrocketing
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can J Cardiol
- v.26(Suppl C); Aug-Sep 2010
Language: English | French
The impact of social determinants on cardiovascular disease
Catherine kreatsoulas.
1 McMaster University;
Sonia S Anand
Cardiovascular disease is the leading cause of death among high-income countries and is projected to be the leading cause of death worldwide by 2030. Much of the current research efforts have been aimed toward the identification, modification and treatment of individual-level risk factors. Despite significant advancements, gross inequalities continue to persist over space and time. Although increasing at different rates worldwide, the magnitude of increase in the prevalence of various cardiovascular risk factors has shifted research efforts to study the causes of the risk factors (ie, the ‘causes of the causes’), which include the social determinants of health. The social determinants of health reflect the impact of the social environment on health among people sharing a particular community. Imbalances in the social determinants of health have been attributed to the inequities in health observed between and within countries. The present article reviews the role of the social determinants of health on a global level, describing the epidemiological transition and the persistent trend known as the ‘inverse social gradient’. The impact of social determinants in Canada will also be examined, including data from ethnic and Aboriginal communities. Possible solutions and future directions to reduce the impact of social factors on cardiovascular health are proposed.
La maladie cardiovasculaire est la principale cause de mortalité dans les pays à revenus élevés et on s’attend à ce qu’elle devienne la principale cause de mortalité dans le monde d’ici 2030. Une bonne part de la recherche actuelle s’est attardée à la reconnaissance, à la modification et au traitement des facteurs de risque à l’échelon individuel. Or, malgré des progrès significatifs, d’importantes disparités persistent dans l’espace et le temps. Même si elle croît à un rythme différent selon les régions du monde, la prévalence de divers facteurs de risque cardiovasculaires force maintenant les chercheurs à étudier désormais l’origine des facteurs de risque eux-mêmes (c.à-d., « la cause des causes »), ce qui inclut les déterminants sociaux de la santé. Les déterminants sociaux de la santé témoignent de l’impact de l’environnement social sur la santé des personnes d’une communauté donnée. Les disparités quant aux déterminants sociaux de la santé ont été attribuées aux inégalités en matière de santé observées à l’intérieur des pays et entre eux. Le présent article fait le point sur le rôle des déterminants sociaux de la santé d’un point de vue mondial en décrivant l’évolution de l’épidémiologie et la tendance persistante connue sous le nom de « gradient social inverse ». L’impact des déterminants sociaux au Canada fera l’objet d’une analyse qui portera entre autres sur les données provenant des communautés ethniques et autochtones. On propose des solutions et des orientations qui pourraient éventuellement réduire l’impact des déterminants sociaux sur la santé cardiovasculaire.
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality among high-income countries of the industrialized world, accounting for more than one-third of total deaths ( 1 , 2 ). CVD is the leading cause of noncommunicable morbidity and mortality among low- and middle-income countries, accounting for almost 25% of total deaths ( 3 ) and, by the year 2030, is projected to be the leading cause of death worldwide ( 1 , 2 ). One of the most important advances in cardiovascular research of the 20th century was the identification of risk factors associated with CVD, with subsequent treatments developed and rigorously tested to modify these risk factors with the goal of preventing CVD. The INTERHEART study ( 4 ) examined more than 27,000 cases and controls from 52 countries and found that more than 90% of the population-attributable risk for myocardial infarction can be explained by nine potentially modifiable risk factors: apolipoprotein B/apolipoprotein A ratio, smoking, diabetes, hypertension, abdominal obesity, psychosocial factors, fruit/vegetable consumption, physical activity and alcohol consumption; thus, it is reasonable to believe that modification of these individual risk factors will significantly improve cardiovascular health. However, despite advances in the primary and secondary prevention of CVD, there are still gross inequalities in cardiovascular health care across space and time ( 5 – 7 ). To date, epidemiological studies have focused on identifying, modifying and treating individual risk factors; however, many cardiovascular risk factors have been increasing at different rates worldwide. Efforts to narrow the persistent health gap has spurred recent interest in developing approaches to study the causes of risk factors (ie, the ‘causes of the causes’), which include the social determinants of health.
The term ‘social determinants of health’ is used to describe the health impact of the social environment on people living in a particular community ( 8 ). Specifically, they include the conditions in which people are born, grow, live, work and age, and are shaped by the distribution of money, power and resources at global, national and local levels ( 9 ). The social determinants of health (including the health care system) are mostly responsible for health inequities between and within countries ( 9 ). Historical research has significantly established the impact of economic development and social organization on health ( 10 ). Because the prevalence of some cardiovascular risk factors (eg, obesity, hypertension and diabetes) is rising worldwide ( 2 , 10 , 11 ), it is necessary to focus efforts on understanding the role of the ‘causes of the causes’ (ie, the social determinants of health) to help bridge the current gap in equality. For the purpose of the present article, the social determinants of health as they pertain to CVD will first be explored on a global level and, second, within Canada, including data from ethnic and Aboriginal communities. Possible solutions to reduce the impact of social factors on CVD are also proposed.
THE GLOBAL BURDEN OF DISEASE
The World Bank and the WHO commissioned the Global Burden of Disease study ( 1 , 2 ) to quantify mortality, morbidity and the health effects of selected diseases, injuries and risk factors for the world as a whole and within specific regions. Among worldwide noncommunicable causes of death, CVD accounts for more than one-half ( 1 ); this finding has been consistently projected to remain unchanged across multiple models for at least the next 20 years in countries of both the developed and developing world ( 1 , 2 , 11 ). This finding is at odds with the popular perception that noncommunicable disease, such as CVD, are ‘diseases of affluence’ whereby related risk factors are perceived to be more prevalent in high-income countries and not present among low-income countries ( 12 ). However, this apparent paradox of substantial noncommunicable death in adults of the developing world has insidiously been established without attracting global attention or local action ( 12 , 13 ). The magnitude of this problem has been greatly overlooked because more than 80% of CVD deaths worldwide currently occur in low- and middle-income countries ( 13 ). By the year 2020, CVD is expected to surpass infectious disease as the world’s leading cause of death and disability ( 3 ), increasing from 25% in 1990 to 40% in 2020, illustrating the scale of this epidemic ( 13 ). Several factors are likely driving the worldwide increase in CVD, including the projected increase of 60% in the global population between 1990 and 2020, the increasing average life expectancy (due to a multitude of factors including improvements in nutrition, public health and medical care, while decreasing the rates of communicable diseases) and the economic, social and cultural changes that have led to increases in CVD risk factors including tobacco use, obesity, hypertension and diabetes ( 3 ). To put this into perspective, smoking, for example, is projected to kill 50% more people in 2015 than HIV/AIDS, and will be responsible for 10% of all deaths globally ( 11 ).
The epidemiological transition
Global patterns of death and disability have been observed over time. As societies become increasingly urban and industrialized, infant mortality declines, and the major causes of death and disability shift from nutritional deficiencies and infectious disease to degenerative or noncommunicable diseases such as CVD, resulting in an increasing average life expectancy. This shift has come to be known as the ‘epidemiological transition’ ( 3 , 14 ). Originally, three main transition states were identified ( 15 ); however, recently, up to five transition states have been described and characterize the total rates of CVD change ( 3 , 10 , 16 ) as illustrated in Figure 1 . Briefly, the first stage, known as ‘the age of pestilence and famine’, is indicative of countries in the earliest stage of development, in which death from CVD accounts for less than 10%, predominantly as rheumatic heart disease and cardiomyopathies due to infection and malnutrition ( 3 , 10 ). Geographical regions currently experiencing this transition state include sub-Saharan Africa and rural areas of South America and Asia. During the second stage, known as ‘the age of receding pandemics’, infectious disease burdens are reduced, nutrition improves and, correspondingly, deaths attributed to CVD increase to up to 35%, manifesting mostly as rheumatic heart disease, hypertension, coronary artery disease and stroke ( 3 , 10 , 16 ). Geographical regions currently experiencing this transition state include China and other Asian countries. In the third stage – ‘the age of degenerative and man-made diseases’ – life expectancy continues to improve, diets include higher fat content, cigarette smoking becomes more prevalent and sedentary lifestyles become more common ( 10 ). Not surprisingly, deaths attributed to CVD continue to rise, accounting for 35% to 65% of total deaths, primarily manifesting as atherosclerosis, coronary artery disease and stroke, often at ages younger than 50 years ( 10 ). Regions currently experiencing this stage include urban India, Latin America and former socialist European eastern block countries. In the developed world, most countries are in the fourth stage of transition referred to as ‘the age of delayed degenerative diseases’, in which up to 50% of deaths are attributed to CVD and typically present as coronary artery disease, stroke or congestive heart failure at more advanced ages ( 3 , 10 , 16 ). More recently, a fifth stage has been identified – ‘the age of health regression and social upheaval’ – which is used to describe conditions of social upheaval or war, resulting in a breakdown of the health system in which there is a resurgence of diseases seen in transition states one and two (eg, rheumatic heart disease), while the CVD diseases common in the third and fourth stage (eg, atherosclerosis) continue to persist ( 10 ). In total, approximately 35% to 55% of deaths are attributed to CVD, with a lower average life expectancy similar to what is currently experienced in Russia ( 10 ).

The epidemiological transition states of cardiovascular disease (CVD). CHD Coronary heart disease. Reproduced with permission from reference 10
Epidemiological transition states occur on a macro level, affecting specific countries or regions; however, they may also occur on a micro level within a country, including affluent countries. A country or a region can enter an epidemiological transition state at any time, with the progression from one state to another closely associated with parallel economic, demographic and nutritional ‘transitions’. From an economic perspective, progression through the transition states is often accompanied by an increase in per capita income; a social transition to industrialization, shifting from predominately rural to urban life; and the establishment of a public health infrastructure including wider access to health care ( 3 ). At the same time, a demographic transition occurs in which fertility and age-adjusted mortality decline, leading to an increase in average life expectancy and an aging population ( 3 ). As life expectancy increases, a shift in nutrition also occurs and populations are exposed to more cardiovascular risk factors including ‘Westernized’ diets (higher animal products and fat), sedentary behaviours and low physical activity, which lead to an elevation in blood pressure, body weight, blood sugar levels and lipid concentrations ( 13 ). This pattern has been repeatedly observed in many developing countries. For example, body mass index and blood cholesterol levels have dramatically increased in the Chinese population, likely due to a sharp increase in fat consumption; it is expected that China will soon experience a rapid escalation of coronary artery disease, surpassing the current one-third of total lives that it claims each year ( 13 , 17 ). Even with China’s booming economic growth, health care costs are currently unsustainable – the impact of which has been detrimental to the poor. Health care is less accessible while the health care system is inundated, having to cope with the double burden of infectious and chronic disease in an excessively large population ( 13 , 17 ).
The epidemiological transition has been observed to occur within countries. Affluent regions are typically affected first and, as the epidemic matures, the socioeconomically disadvantaged groups become increasingly more vulnerable, widening the health inequality gap in a phenomenon widely known as ‘the inverse social gradient’ ( 13 ). The socioeconomically disadvantaged groups have a greater exposure to cardiovascular risk factors such as smoking, increasing incidence of atherosclerotic risk factors (eg, obesity, diabetes, dyslipidemia and hypertension), poor working and living conditions, stress, lower rates of formal education, and reduced access to health care and health education ( 3 , 5 , 13 , 17 ). As research continues to emerge, evidence is mounting, indicating that epidemiological transition is a poor and incomplete model to understand how the social determinants of health interact with cardiovascular health because education, occupation, social norms, culture, geography, policy, economic factors and environment are considered to be independent individual risk factors. A comprehensive understanding of the social determinants of health must consider their dynamic nature, which inevitably includes a temporal component of early life and childhood exposures impacting adult health. The life course perspective is a methodological approach that takes into account the cross-sectional relationship of social circumstances from the early stages of life that may later be accompanied by similar social advantage/disadvantage in other spheres of adult life ( 5 , 18 ) ( Figure 2 ). For example, a longitudinal study ( 19 ) from Scotland found that social disadvantage, defined by a father’s occupation and neighbourhood (postal code of residence), contributed to CVD even after controlling for CVD risk factors. An increasing number of longitudinal epidemiological studies have demonstrated the importance of early-life socioeconomic circumstances with respect to future development of cardiovascular risk factors and CVD in later life ( 20 ).

Socioeconomic influences on cardiovascular disease (CVD) from a lifecourse perspective. Reproduced with permission from reference 18
CARDIOVASCULAR RISK FACTORS AND SOCIAL DETERMINANTS IN CANADA
CVD is the leading cause of death in Canada, accounting for one-third of total deaths ( 21 , 22 ). Despite the decline in CVD-related deaths over time in Canada, there are wide regional variations in death rates and risk factors ( 22 ). For example, the overall Canadian age-standardized CVD mortality rate (ASMR) from 1995 to 1997 was 245.8 per 100,000 population ( 22 ). Within Canada, there are significant differences in the ASMR from CVD, with Newfoundland and Labrador having the highest CVD mortality rate at 320.6 per 100,000 population, and the Northwest Territories having the lowest at 196.9 per 100,000. An east to west gradient in CVD mortality has been described, in which provinces in eastern Canada have higher CVD-related ASMR, with mortality rates generally decreasing westward, where the province of British Columbia has the lowest ASMR from CVD. However, the Territories have the lowest CVD ASMR in the country ( 22 ). In addition to between province/territory variation, variability within provinces has been observed. In a study using cross-sectional data from the National Population Health Survey of 1994, in combination with the Canadian Community Health Survey of 2005, Lee et al ( 21 ) compared temporal trends in the prevalence of cardiovascular risk factors across Canada. Over a 10-year study period, the prevalence of diabetes and obesity significantly increased, the prevalence of hypertension nearly doubled while smoking rates significantly declined ( 21 ). The prevalence of risk factors, when analyzed according to age and sex, indicates that they are increasing in both sexes and in all age groups among Canadians, particularly among the younger population groups ( 21 ). Such trends have important short- and long-term implications because the early presence of risk factors predisposes people to earlier onset of CVD, incurring greater health resource consumption and a greater potential for life-years lost ( 21 , 23 , 24 ).
Evidence of the inverse social gradient in Canada
When analyzing CVD mortality and risk factor prevalence rates according to income group, it is alarming to realize that despite affluence in Canada, individuals of lower socioeconomic status are more vulnerable to CVD than those of higher socioeconomic status ( 3 , 25 ). Evidence of the inverse social gradient and inequity gap reveals that mortality is highest among those in the poorest income group and, as income increases, the mortality rate decreases ( 3 , 25 ). Not surprisingly, these trends are also consistent with CVD risk factor prevalence rates in which individuals in a lower income group, especially in urban areas, have a greater exposure to risk factors (such as smoking and atherosclerosis) that manifest as obesity, diabetes, dyslipidemia and hypertension ( 21 , 22 ). Alarmingly, the inverse social gradient and inequity gap not only persisted but grew when the prevalence of cardiovascular risk factors according to income category over time were considered. Specifically, heart disease, hypertension, diabetes, smoking and obesity increased as income decreased in 1994. This trend was exaggerated when individual risk factors were compared between decades and within income group, with the exception of smoking ( 21 ). What is remarkable about these trends in a country such as Canada, is that they are persisting despite the availability and universality of health care. The presence and persistence of an inverse social gradient related to CVD mortality and associated risk factors is especially concerning because the inequity gap is widening between the highest and lowest income groups, and this trend is worsening with time ( 21 ).
It is likely that multiple factors contribute to the persistence of the inverse social gradient. Consistent with trends observed in the epidemiological transition state, the concurrent decline in malnutrition and communicable disease while CVD risk factors increase typically occur in privileged groups first, soon followed by higher rates of CVD including ischemic heart disease and stroke. This trend is likely responsible for the popular perception that CVD is a ‘disease of affluence’ ( 1 , 13 ). However, as the middle class expands and the epidemiological transition spreads to a broader population, individuals with the lowest socioeconomic status tend to acquire the harmful risk factors last, mostly due to their financial situation and the heavy physical activity usually associated with their work ( 3 , 17 ). At the same time, the socioeconomically disadvantaged are also less likely to have access to advanced health services, treatments and information for risk factor modification and, as a result, CVD mortality rates are slower to decline in this group ( 3 , 17 ). For example, of the percentage of the population living in poverty in Canada, two-parent families comprise the highest income group whereas female lone-parent families comprise the lowest-income group – a trend that has remained consistent over time ( Figure 3 ). Socioeconomic status has been widely acknowledged as the most powerful social determinant of health; however, there are a multitude of factors that intersect with socioeconomic status, including systematic inequalities due to ethnicity and sex.

Canadian poverty rates over time, 1984 to 2004. Reproduced with permission from reference 28
The inverse social gradient and Aboriginals in Canada
Ethnicity is a construct that embodies both genetic and cultural differences including language, religion and diet, to name a few. The construct of ethnicity is intertwined with variations in lifestyle, geography, socioeconomic position and education. Differences in morbidity and mortality among various ethnic groups are well documented within Canada. The Study of Health Assessment and Risk in Ethnic groups (SHARE) ( 26 ) used a population-based approach and confirmed differences in risk factor prevalence rates among three ethnic groups in Canada ( 26 ). This is an important finding because the overall prevalence of CVD is declining in Canada; however, CVD was observed to be rising within some ethnic groups. There are a number of explanations proposed for these differences including the concept of social exclusion, differences in risk factor frequency, access to screening/prevention, differences in treatment and adherence to treatment ( 26 ). Specifically, Aboriginals in Canada have been identified as the population group with the shortest life expectancy ( 25 , 27 ), averaging five to 14 years less than their fellow Canadians ( 28 ) despite a decline in infectious disease deaths. Aboriginal infant mortality rates that are 1.5 to four times greater than the Canadian rate contributed to the shorter life expectancy ( 29 ).
Not surprisingly, CVD health among Aboriginals is also poor. It has been demonstrated that Aboriginals have a higher prevalence of CVD and a greater burden of atherosclerosis than Canadians of European ancestry ( 27 ). Correspondingly, they also have a higher prevalence of conventional risk factors including higher rates of smoking, diabetes, obesity, abdominal obesity, hypertension, cholesterol and family history, which likely account for observed ethnic group differences ( 27 ). However, Aboriginals have also been identified to have an excess of social disparities including environmental dispossession – a term used to refer to the processes through which Aboriginal Peoples’ access to the resources of their traditional environments are greatly reduced ( 30 ) – and high levels of poverty ( 27 ). Consistent with trends among other disadvantaged groups, there is evidence of an inverse social gradient; however, the social gradient is strikingly pronounced among Aboriginals when compared with their European-Canadian counterparts of similar income. In The Study of Health Assessment and Risk Evaluation in Aboriginal Peoples (SHARE-AP) ( 27 ), both Aboriginals and European-Canadians had the highest prevalence of CVD; however, even among individuals in the lowest income group (less than $20,000 household income), the absolute rate of CVD was significantly higher among Aboriginals than among European-Canadians of all income ranges ( 27 ), as illustrated in Figure 4 . Consistent with this trend (and equally as shocking!), the burden of CVD risk factors (more than three CVD risk factors) was greatest among people in the lowest income group in both Aboriginals and European-Canadians; however, the absolute rate of CVD risk factor burden was at least twice as high in Aboriginals compared with European-Canadians within each income level group ( 27 ) ( Figure 5 ). The social disadvantage index score was developed to incorporate social and economic exposures into a single continuous measure, and found that increased social disadvantage is associated with an increased burden of some – but not all – cardiovascular risk factors independently associated with CVD ( 31 ). Specifically, social disadvantage was found to increase with age, was higher among women than men and varied greatly according to ethnic group, in which the highest risk for CVD was among Aboriginal men ( Figure 6 ) ( 31 ).

Socioeconomic gradient and cardiovascular disease (CVD) among Aboriginal Peoples and European descendants in Canada. Reproduced with permission from reference 27

Cardiovascular disease (CVD) risk factor prevalence and income among Aboriginal Peoples and European descendants in Canada. Reproduced with permission from reference 27

Risk of cardiovascular disease and social disadvantage. Reproduced with permission from reference 31
THE TREATMENT GAP
In addition to the health inequities examined, both on a global and national level, the ‘10/90 gap’ has been recognized as a serious limitation to the improvement of health care, citing that less than 10% of global health research spending is devoted to diseases that account for 90% of the global disease burden ( 32 ). Globalization may negatively affect countries in a lower epidemiological transition state by accelerating the transition of Western products and behaviours to non-Western cultures ( 13 ). At the same time, globalization can also offer opportunities to facilitate the prevention of CVD through risk factor modification, applying evidence of effective interventions and promoting health behaviour through mass media ( 13 ). Despite this, current effective therapies for secondary prevention, such as treatment with acetylsalicylic acid, blood pressure-lowering drugs and statins, are highly undersused. For example, a study conducted in rural India ( 13 ), where CVD is the leading cause of death, reported that less than one-sixth of the patients who experienced a previous CVD event acknowledged taking antiplatelet therapy.
The reasons for the treatment gap are complex. Several proposed explanations include the following: incomplete guidelines for physicians, health care systems and policy; the cost of therapy relative to wages; cultural barriers such as the stigma of taking long-term medication; urban versus rural accessibility to health care; and international neglect, for which low- and middle-income countries account for one-third of the world’s population but only receive 2% of global health resources ( 17 ). Even within affluent countries such as Canada and the United States, a ‘5/95 gap’ is used to describe the ratio of resources devoted to prevention versus treatment ( 33 ).
To help address issues related to health inequities occurring at both a global and local level, the Centre for Urban Health – commissioned by the WHO – created a document titled ‘The Solid Facts’ to “promote awareness, informed debate and above all, action…a valuable tool for broadening the understanding of stimulating debate and action on the social determinants of health” ( 8 ). The Solid Facts document identifies 10 social determinants of health: social gradient, stress, early life, social exclusion, work, unemployment, social support, addiction, food and transport ( 8 ). This document is widely available, and every member state of the European Union (EU) has currently made efforts to integrate it into their health care agendas. Among the objectives for generating this document was to encourage other countries outside the EU to use it as a model/template for their health care agendas ( 8 ). However, current health models and dissemination of health information to the public from various government and health bodies have been strongly and individually oriented, and take the position that individuals can control the factors that determine their health, as exemplified in the ‘Traditional 10 tips for better health’ ( 29 ) depicted in Table 1 . However, these conceptualizations have been recently refined to incorporate the information established from research on the social determinants of health using a socially oriented perspective, which assumes that the most important determinants of health are beyond the control of most individuals. The traditional 10 tips can be contrasted with the ‘Social determinants 10 tips for better health’ presented in Table 2 ( 29 ).
The traditional 10 tips for better health
Reproduced with permission from reference 29
The social determinants 10 tips for better health
Because CVD is increasing globally, it is crucial that we understand the social and economic forces that promote the development of risk factors affecting who is screened and who is treated. The dissemination of knowledge and the application of effective strategies are essential. The social determinants of health are tools to help illuminate how social processes interact with CVD health on a global, national and individual level. Specifically, if disadvantaged groups can be identified, intervention strategies can then be tailored at an early age before the individual exhibits the conventional risk factors thereby improving population health and reducing the burden placed on health care resources. It is critical that people – including the scientific community – advocate, educate, organize, lobby and convince policy makers that minimizing social and economic inequities will diminish the social gradients of cardiovascular risk factors and CVD.
Improvements to implement change must be made on many levels. Currently, there is an international plea to improve national health monitoring and surveillance systems ( 34 , 35 ). Advances in statistical linkage techniques (eg, geocoding and area-based socioeconomic measures), in addition to multilevel hierarchical analysis frameworks, have contributed to assessing public health outcomes to identify disadvantaged groups ( 35 ). In particular, these techniques have aided researchers and policy makers to study risk factors such as smoking ( 36 ) and physical activity level ( 37 ) at the neighbourhood-of-residence level so that new approaches to develop community-level interventions can be targeted ( 36 ). For example, clean indoor air legislation prohibiting smoking in the workplace has aided in reducing overall cigarette consumption ( 38 , 39 ). Similarly, a study ( 40 ) using hierarchical regression analysis techniques suggested that greater social cohesion, which seeks to capture the presence of strong social bonds and the absence of latent social conflict, was found to be directly associated with more general physical activity in Chicago (United States) neighbourhoods, independent of previous participation in recreational programs and other neighbourhood- and individual-level covariates. To increase the promotion of physical activity in this urban population, the authors recommended that efforts should target neighbourhood-level social and psychosocial processes that influence social cohesion ( 37 ). These examples highlight that an understanding of the community and household determinants of the major cardiovascular risk factors, which may vary by geographical region and cultural background, is required to develop prevention strategies. Finally, such context-dependent strategies must be evaluated to ensure that they are efficacious.
CONFLICTS OF INTEREST: The authors have no financial disclosures or conflicts of interest to declare.
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- Wunderkinds Nomination
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
New cardiovascular risk model could greatly decrease use of statins and increase heart attacks, study warns
By Elizabeth Cooney July 29, 2024

I f millions of Americans no longer qualify for a statin or a blood pressure medication based on a new calculator updated to better predict their risk, that could lead to 107,000 more heart attacks and strokes over 10 years, a new study estimates.
The research paper, published Monday in JAMA , is the second in two months drawing attention to widely used medicines designed to prevent the leading cause of death in the United States.
advertisement
The research is creating a buzz in cardiology circles while two medical societies formulate new guidelines to inform practice, weighing the new risk models and existing thresholds that trigger prescriptions.
“This is concerning that we could reverse eligibility for many millions of Americans,” Raj Manrai, assistant professor of biomedical informatics in the Blavatnik Institute at Harvard Medical School and senior author of the new study, said in an interview. “We really need to reexamine the other side of the equation here, which is how those risk estimates are going to be used by patients and physicians to decide who and when individuals receive preventative care, particularly statins and antihypertensive blood pressure medications.”
Related: Millions fewer people may need statins, a new study suggests. But guidelines have yet to agree
Just who should be taking a statin is at the heart of both research papers analyzing risk equations released in November 2023, called Predicting Risk of cardiovascular disease EVENTs (PREVENT). That model , developed by the American Heart Association, aimed to improve on a version created in 2013, known as the Pooled Cohort Equations (PCE) and widely criticized for overestimating risk .
PREVENT drew on billing and electronic health record data from a more diverse real-world population than the older one, incorporating current statin use as well as metabolic and kidney diseases. Current guidelines used by primary care doctors are based on PCE, while the American Heart Association and American College of Cardiology review the newer PREVENT model and complete new guidelines.
Under guidelines based on the 2013 calculator, most people with a 10-year risk of 7.5% or more for developing cardiovascular disease are advised to take a statin, while at a 5% risk, they’re told only that they and their doctors should consider doing so. The threshold for hypertension treatment is blood pressure at or above 140/90 mmHg or blood pressure at or above 130/80 mmHg combined with a 10% risk for other reasons.
Rather than debate which risk calculator is better, some experts said resetting the thresholds they use is more urgent.
“It is a well-known fact that PCE overestimates risk by about two-fold,” Sadiya Khan, a cardiologist and associate professor of medicine and preventive medicine at Northwestern University Feinberg School of Medicine, told STAT in an email. She was not involved in either study but chaired the group that developed the PREVENT equations . “The PREVENT estimates more closely match contemporary event rates and therefore are approximately half of the PCE estimate. So the question isn’t more deaths or events if the threshold is the same, but what should the guidelines consider as the new threshold.”
Harvard’s Manrai concurred. “To me, the data really says that’s a very, very important and urgent conversation to be having, whether that 7.5% is that magic number at which we should initiate statins and which rests on some risk-benefit calculus which I think needs to be reexamined.”
Statins, available for about $40 a year in the U.S., work very well to lower LDL, the “bad” cholesterol that clogs blood vessels. If that atherosclerotic condition gets bad enough, it can starve the heart or the brain of oxygen-rich blood, causing a heart attack or a stroke. A variety of blood pressure medications, also at low cost, relax and open blood vessels that when blocked could lead to heart attack or stroke.
Sign up for Morning Rounds
Understand how science, health policy, and medicine shape the world every day
Statins’ drawbacks include potentially higher risk of type 2 diabetes. But the drugs have dramatically improved cardiovascular health, although about 40% of Americans who could benefit from statins under current guidelines don’t take them.
“Even if we leave aside the question of what is the best and most accurate model for our patients in 2024 (which I think is the first fundamental question), we still know we have a huge gap in patients being on the right treatment even when eligible,” Khan said.
Last month’s JAMA Internal Medicine study used the newer PREVENT risk equations to determine that overall, among the 3,785 adults who were 40 to 75 years old in a 2017-2020 the National Health and Nutrition Examination Survey survey there was a 4% estimated mean 10-year risk of developing cardiovascular disease, compared to the 8% mean 10-year risk previously predicted by the PCE. If applied in doctors’ offices around the country, the study estimated, the number of adults recommended for statins could drop by 17.3 million.
Monday’s JAMA study similarly applied the PREVENT risk calculator to 7,765 adults age 30 to 79 who answered the same national survey but from 2011-2020 (also ending as the pandemic began in March) before concluding 14.3 million fewer people would no longer meet eligibility for statins and 2.6 million fewer people would be candidates for blood pressure medications.
Then the authors went on to predict what that could mean for heart attacks and strokes if new risk tools reduced the number of people advised to take statins or blood pressure drugs. Their answer: 107,000 more heart attacks and strokes over 10 years if people are reclassified to lower risk and thus no longer benefit from preventive medications. More men than women would potentially be affected, but similar proportions of Black and white adults. People determined to be ineligible for treatment had fewer risk factors, including lower rates of obesity, hypertension, and chronic kidney disease.
“This estimate is based on the assumption that fewer people would be treated, which assumes the same threshold would be applied,” Khan said about the JAMA paper. “I think we have to expect that the threshold should and needs to change because we now have a more accurate model.”
Manrai said he was struck by the potential magnitude of changing the risk equation. “I think anytime you see a number like 107,000 heart attacks and strokes — we checked this a hundred times. We did, like, 15 sensitivity analyses to it,” he said. “I really do think it’s a pretty stunning projection for the potential impact of changing these equations across the U.S.”
Related: Reversing progress, stroke rates are rising, especially in working-age adults
Timothy Anderson, a primary care physician and an assistant professor of medicine at University of Pittsburgh Medical Center, was an author of the June analysis. He thinks there is going to be a conversation in the both primary care and cardiology communities about what is the right risk threshold.
“I’ve never seen some sort of study that tells us 5% is the perfect number versus 7% versus 2% versus 20%. Ultimately, statins are safe drugs and they do work very well,” he said in an interview. “For a lot of people, they’re willing to tolerate some amount of risk and they’re also willing to perhaps think about if I decline that statin, I will work on exercise and weight loss and get my blood pressure under control.”
Manrai and his co-authors noted there are downsides to both statins and blood pressure medications. There is an increased risk of type 2 diabetes in people treated with statins, possibly because the drugs interfere with insulin. So under the PREVENT model, which suggests less statin use, the researchers project there would be 57,800 fewer new cases of type 2 diabetes over 10 years. People on blood pressure medications can suffer sudden drops in blood pressure, lower blood supply, or sexual dysfunction, side effects that enter into decisions for patient and doctor about costs and benefits.
“There is no perfect risk estimation equation,” Jelani Grant, Chiadi Ndumele, and Seth Martin of Johns Hopkins wrote in a companion editorial. “These equations provide a starting point for risk discussions and shared decision-making in the primary prevention setting. Further risk assessment via risk-enhancing factors and arterial imaging can help tailor individual treatment plans.”
Manrai has heard that cardiologists are already plugging values from PREVENT into their risk estimates.
Not Steven Nissen, a cardiologist at the Cleveland Clinic. Nissen believes problems with risk calculators arise when they’re misconstrued as mandates.
“In my humble opinion, there is no substitute for a well-informed physician who knows what the current medical literature looks like, and he looks at the patient in front of him, and factors in everything that we know,” he said in an interview.
Asserting statins’ value across the lifespan, he has been leading an effort in collaboration with AstraZeneca to make the 5-milligram dose of its drug Crestor (rosuvastatin) available without a prescription .
“What they’re trying to say here is that if we make a mistake with a risk calculator, it can be very costly,” Nissen said about the new JAMA paper, in which he did not play a role. “I think they’re right that if we miss the mark, we are going to produce societal harm. We need to have a more thoughtful approach to deciding who to treat and not put all of our emphasis on somebody’s mathematical risk calculator.”
Khan said new thresholds for treatment would ideally be based on randomized clinical trials following people to see how well the risk model predicted later heart attacks or strokes. That would help establish at what level of risk the most benefit and least harm could be achieved from prescribing statins and blood pressure medications.
“Guidelines do not recommend a one-size-fits-all threshold,” she said. Instead, doctors and patients should discuss individual risk-enhancing factors, such as a family member who’d had a heart attack at a young age or developed the dangerous condition preeclampsia in pregnancy, as well as imaging of calcium levels in the coronary arteries.
“One of the most important parts of this discussion is to make sure that patients do not stop their statins without speaking with their doctors based on a new model until there are new guidelines available to indicate when therapy should be started or stopped,” Khan said.
STAT’s coverage of chronic health issues is supported by a grant from Bloomberg Philanthropies . Our financial supporters are not involved in any decisions about our journalism.
About the Author Reprints
Elizabeth cooney.
Cardiovascular Disease Reporter
Elizabeth Cooney is a cardiovascular disease reporter at STAT, covering heart, stroke, and metabolic conditions.
cardiovascular disease
Pharmaceuticals
public health
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

STAT Plus: Older GLP-1 drug may help protect brains of Alzheimer’s patients, early study suggests

How artificial intelligence can bolster Europe’s competitive edge in biopharma

STAT Plus: Health Care's Colossus: How UnitedHealth harnesses its physician empire to squeeze profits out of patients

STAT Plus: Sarepta demanded Duchenne patient advocacy group censor video critical of the company

STAT Plus: How Pfizer’s grand gene therapy ambitions crumbled
- Share full article
Advertisement
Supported by
Guest Essay
How on Earth Is There a Syphilis Epidemic in 2024?

By Ina Park
Dr. Park is a professor of family and community medicine at the University of California, San Francisco.
Nobody should be dying of syphilis in 2024. That’s the credo of Elizabeth Glaser, a public health nurse for the Indian Health Service, who drives thousands of miles throughout the Navajo Nation searching for community members with the infection. Once they’re found, Dr. Glaser administers shots of penicillin as treatment, at people’s homes, RVs, even in the back seat of her car.
Yet despite the good work of those like Dr. Glaser and the availability of cheap and effective treatment, the United States is experiencing rampant increases in syphilis. Left untreated, infection can lead to devastating neurological consequences such as blindness , deafness, madness and death. While other reportable sexually transmitted infections declined or remained flat during the pandemic, over 207,000 cases of syphilis were reported in 2022 , an 80 percent increase since 2018 and the highest number reported since 1950.
Most disturbing within this trend is the rise in congenital syphilis. Over 3,700 cases were reported in 2022, which is more than double the number of cases of mother-to-child transmission of H.I.V. at the height of the AIDS crisis. Nearly 300 infected babies were stillborn or died in the first year of life.
How did we get into this situation? More important, how do we get out of it? The answers differ for each population most affected by the epidemic: pregnant women, and gay and bisexual men. To tackle congenital syphilis, we must cast off societal squeamishness about S.T.I.s and invest in proven control strategies: public education, testing, treatment and contact tracing. For gay and bisexual men, we need to embrace novel prevention interventions if we are to outwit this wily disease.
Syphilis is often referred to as the Great Masquerader: a painless genital ulcer or rash on the hands and feet are textbook signs, but a bloodshot eye, a white patch on the tongue or hair loss can be signs too. It can look like anything yet often looks like nothing, able to lie dormant for decades with no apparent symptoms.
But the surge in congenital syphilis isn’t due to the infection’s many disguises; it’s because of failures of our health system and safety net. According to the C.D.C., nine of 10 congenital syphilis cases in 2022 were preventable ; lack of prenatal testing and timely treatment were the most common culprits, intersecting with social ills such as poverty, homelessness, substance use and incarceration. Because of systemic inequities, Indigenous, Pacific Islander and Black communities are hardest hit; one in 155 Native American births was affected by congenital syphilis in 2022.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

IMAGES
VIDEO
COMMENTS
The Importance of Heart Diseases. Heart disease is a prevalent and serious health issue that affects millions of people worldwide. It is one of the leading causes of death globally, and its impact on individuals, families, and societies is significant. In this essay, we will explore the importance of heart diseases, including their prevalence ...
Cardiovascular disease (CVD) is a collective term designating all types of affliction affecting the blood circulatory system, including the heart and vasculature, which, respectively, displaces and conveys the blood. This multifactorial disorder encompasses numerous congenital and acquired maladies. CVD represents the leading noncommunicable cause of death in Europe (∼50% of all deaths; ∼ ...
Antioxidants: The Role in Preventing Cancer and Heart Disease. Some of antioxidants are more widely known as vitamins E, C, and carotenoids, and have a reputation of preventing cardiovascular diseases and cancer. We will write a custom essay specifically for you by our professional experts. 183 writers online.
Cardiovascular Benefits of Intermittent Hypoxic Conditioning in Elderly Subjects. The present study may serve as a foundation for research in the field of cardiovascular benefits of the IHC due to inflammatory markers' ability to catalyze cardiac issues among elderly subjects. The Effect of Vitamin E on Cardiovascular Diseases.
Heart Disease - Free Essay Examples and Topic Ideas. Heart disease refers to a range of conditions that affect the heart's ability to function properly. These conditions may include issues with the heart's blood vessels, valves, or rhythm. Heart disease is a leading cause of death worldwide, and common risk factors include a poor diet, lack ...
Heart disease or Cardiovascular disease is an abnormal function of the heart or blood vessels. It can cause an increase in risk for heart attack, heart failure, sudden death, stroke and cardiac rhythm problems, thus resulting in decreased quality of life and decreased life expectancy. The causes of cardiovascular disease range from structural ...
Introduction and background. Atherosclerosis is the process of formation of plaque composed of cholesterol, fat, calcium, and other substances in the wall of large and medium-sized arteries causing diminished blood flow to an area of the body [1,2].Moreover, atherosclerotic vascular disease can be classified into two arenas: a cardiovascular disease affecting the heart and peripheral blood ...
Heart Disease begins with inflammation and irritation of the inner lining of the coronary arteries and over time, cholesterol in the bloodstream can collect in the inflamed areas and begin the formation of a plaque (Werdo, n.d.). This plaque grows and as it does, the diameter of the artery. Free Essays from Bartleby | of the case study ...
The clinical manifestations of coronary heart disease include symptoms and signs that might signalize the problem. Firstly, the signs that might indicate coronary heart disease in a patient include dizziness, cold sweat, pain in the neck, shortness of breath, difficulty sleeping, and weakness (National Heart, Lung, and Blood Institute, n. d.).
Coronary Heart Disease (CHD) it is also know as Coronary Artery Disease. It happens when the blood vessels delivering to the heart develop blockage or are narrowed by plaque, which reduces the flow of the blood, oxygen and nutrients supplied to the heart. If this happens the person starts to feel chest pain (also known as angina pectoris) and ...
The thesis of this essay is that the longstanding emphasis on cardiovascular disease (CVD) has at last yielded to a mounting force behind cardiovascular health (CVH), manifest in adoption by the American Heart Association (AHA) of its 2020 Impact Goal: "By 2020, to improve the CVH of all Americans by 20% while reducing deaths from CVDs and stroke by 20%." 1 It is proposed that this shift ...
Heart disease or Cardiovascular disease is an abnormal function of the heart or blood vessels. It can cause an increase in risk for heart attack, heart failure, sudden death, stroke and cardiac rhythm problems, thus resulting in decreased quality of life and decreased life expectancy. The causes of cardiovascular disease range from structural ...
Cardiovascular disease has many symptoms, causes and risk factors. Most heart related diseases start with pain in the chest and shortness of breath. Other symptoms include weakness, dizziness, nausea, sweating and many more. If you are experiencing heart disease you may also experience palpitations, also known as irregular heartbeats or "flip ...
The cardiovascular system consists of the heart and blood vessels.[1] There is a wide array of problems that may arise within the cardiovascular system, for example, endocarditis, rheumatic heart disease, abnormalities in the conduction system, among others, cardiovascular disease (CVD) or heart disease refer to the following 4 entities that are the focus of this article[2]:
Essays. Reflection and perspective are invited, collected, and presented here about the causes, care, control, prevention, epidemiology, and public policy of heart attacks. A. Keys response to G. Mann's 1977 NEJM Op-Ed: "Diet-Heart. End of an Era.".
Heart disease, including coronary heart disease, remains the leading cause of death in the United States. However, the rate of heart disease deaths has declined by 70% over the past 50 years, thanks in part to NHLBI-funded research. Many current studies funded by the NHLBI focus on discovering genetic associations and finding new ways to ...
Chronic Stress . Increased cortisol levels and dysregulation of the immune system that are directly related to stress can contribute to inflammation, atherosclerosis (plaque buildup in the arteries), and other risk factors of heart disease. In addition, unhealthy coping strategies for chronic stress (a sedentary lifestyle, certain eating patterns, and smoking cigarettes) can further increase ...
Get a custom essay on Heart Disease: Causal Effects of Cardiovascular Risk Factors---writers online . Learn More . Excessive weight leads to an increase in fat cells in the body, and an increased amount of fatty and cholesterol deposits makes it more difficult for blood to reach the heart. This condition is called atherosclerosis (Bastien et al ...
Argumentative Essay On Heart Transplant; Argumentative Essay On Heart Transplant. 1106 Words 5 Pages. ... When someone has congenital heart disease the blood in someone's body does not circulate correctly and could cause strokes, heart failure, and heart infections, and some children have it bad enough, they cannot go to school and live a ...
Search for more papers by this author. Melanie Greenland, Melanie Greenland. Oxford Vaccine Group, University of Oxford, Oxford, United Kingdom. ... (91.2%), with 62.1% living in remote areas. The number of ARF and rheumatic heart disease (RHD) diagnoses per year increased from 1987 to 2017 with notable peaks in 2013 and 2017. The average ...
Two blood tests you probably haven't heard of might predict your risk of heart disease better than standard tests do. The first measures a protein called apolipoprotein B, or apoB for short ...
Ischemic heart disease is a state of repeating mid-section agony or distress that happens when a part of the heart does not get enough blood. This condition happens regularly amid effort or energy, when the heart requires more noteworthy blood stream. Ischemic heart disease, likewise called coronary illness, is regular in the United States and ...
An investigation was completed use publicly available NCBI and DISGNET databases to determine the genetic association to predominant heart diseases. Preliminary research was conducted to detect the two most common types of heart disease, hypertrophic cardiomyopathy (HCM) and coronary artery disease (CAD), and the respective monogenic and polygenic genes responsible for causing these diseases.
For the first time ever, doctors at the Texas Heart Institute at Baylor St. Luke's Medical Center implanted an artificial heart in a patient. The 58-year-old had late-stage heart disease. Behind ...
The FDA recently approved a new use for Wegovy, the blockbuster anti-obesity drug, to reduce the risk of heart attacks and stroke in people with cardiovascular disease who are overweight or obese ...
THE GLOBAL BURDEN OF DISEASE. The World Bank and the WHO commissioned the Global Burden of Disease study (1,2) to quantify mortality, morbidity and the health effects of selected diseases, injuries and risk factors for the world as a whole and within specific regions.Among worldwide noncommunicable causes of death, CVD accounts for more than one-half (); this finding has been consistently ...
Just who should be taking a statin is at the heart of both research papers analyzing risk equations released in November 2023, called Predicting Risk of cardiovascular disease EVENTs (PREVENT).
Coronary artery disease: As the most common type of heart disease, coronary artery disease can lead to heart attack, heart failure and more. It's the leading cause of death in the United States.
Researchers criticized a top health association for a new cardiovascular disease risk calculator that could improperly render up to 16 million people ineligible for medication because of the ...
Gay and bisexual men bear the biggest burden of disease, composing just 2 percent of the U.S. population but over 40 percent of primary and secondary syphilis cases from 2018 to 2022. Syphilis has ...