COVID-19: Stress and Anxiety
[Additional essays and videocasts regarding psychological ramifications of the COVID-19 virus outbreak can be found at: https://communitiescollaborating.com/[
The COVID-19 virus knows all about the human psyche. The virus is aware that we experience stress and become anxious when we keep a distance from other people and are forced to isolate ourselves from direct, physical contact with the people we love and cherish. Under conditons of stress and as we become more anxious, our vulnerability also increases — leaving us even more anxious. A vicious cycle . . . and a cycle that we need to stop!!
This essay includes material prepared by members of the Global Psychology Task Force–a group of experienced professional psychologists from around the world who have come together to address the psychological ramifications of the COVID-19 virus. They have prepared a website (www.communities collaborating.com) that incorporates essays, video clips and links to other references that address these ramifications. This essay is derived from the content of this website.

Stress Ruts, Lions and Lumens
We start with a brief video presentation by Dr. William Bergquist, a member of the Global Psychology Task Force. He has titled his presentation: “Stress Ruts, Lions and Lumens in the Age of the Pandemic”:
Reducing the Stress and Anxiety
This essay concerns the way to reduce the stress and anxiety. In addressing this psychological dynamic we turn to both the anxiety aroused by those who have tested positive for the virus and those who have not been tested or have been tested and are negative but still worry about the physical and psychological health of other people in their life, as well as their own economic health and the economic and societal health of their community and country.
https://www.vox.com/identities/2020/3/21/21188362/manage-anxiety-pandemic
We turn now to someone who have been infected by COVID-19
Managing the Anxiety as Someone Who Has Been Infected
The anxiety associated with any major illness is quite understandable and is not in any way a sign of weakness. There are many ways in which to address this anxiety–such as looking to loved ones for support (even if they can’t be physically present), reducing other sources of stress in one’s life, identifying daily plans for dealing with the virus–and most importantly taking actions that enable you to feel less powerless and victimized.
It is perhaps best to turn from these general recommendations to the insights offered by someone who has been infected and struggled for a lengthy period of time with the infestation and related fever and isolation. This person is Dr. Suzanne Brennen-Nathan, one or our Global Psychology Task Force members. Suzanne is a highly experienced psychotherapist who has specialized in the treatment of trauma in her clinical practice. Who better to reflect on the illness and offer recommendations then someone “who has been there” and has expertise in the traumatizing impact of a major illness like COVID-19. Suzanne has been interviewed by Dr. William Bergquist, another member of the Task Force:
Managing the Anxiety as Someone Who Hasn’t Been Tested or Is Negative But Still Fearful
What about those of us who have not tested positive for COVID-19 or have not been tested at all. At the heart of the matter in facing the challenges associated with the COVID-19 virus — whether these challenges be financial, vocational or family related–is the stress that inevitably is induced when we think about, feel about and take action about the virus’ threatening nature.
We therefore begin this statement about action to be taken with an excellent presentation by one of our task force members, Christy Lewis:
To begin a cross-cultural reflection on the psychological ramifications of the COVID-19 virus, we offer an essay on the way in which one of our Task Force members, Eliza Wong, Psy.D., works with highly anxious clients in her home country: Singapore.
Dealing with Anxiety during COVID-19 in Singapore
We hope these perspectives on stress and anxiety in the age of the COVID-19 virus invasion provides some guidance for you in better understanding the psychological impact of the virus and identifying actions you can take to help ameliorate this impact.
- Related Articles
- More By William Bergquist
- More In Health / Biology
The Shattered Tin Man Midst the Shock and Awe in Mid-21st Century Societies I: Shattering and Shock
Lay me down to sleep: designing the environment for high quality rest, the wonder of interpersonal relationships via: culprits of division and bach family members as exemplars of relating midst differences, i dreamed i was flying: a developmental representation of competence, snuggling in: what makes us comfortable when we sleep, the intricate and varied dances of friendship i: turnings and types, leadership in the midst of heath care complexity ii: coaching, balancing and moving across multiple cultures, leadership in the midst of heath care complexity i: team operations and design, delivering health care in complex adaptive systems i: the nature of dynamic systems, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
I wish to introduce a quite different interpretation regarding the presence of flight in t…
- Counseling / Coaching
- Health / Biology
- Sleeping/Dreaming
- Personality
- Developmental
- Cognitive and Affective
- Psychobiographies
- Disclosure / Feedback
- Influence / Communication
- Cooperation / Competition
- Unconscious Dynamics
- Intervention
- Child / Adolescent
- System Dynamics
- Organizational Behavior / Dynamics
- Development / Stages
- Organizational Types / Structures
- System Dynamics / Complexity
- Assessment / Process Observation
- Intervention / Consulting
- Cross Cultural
- Behavioral Economics
- Technologies
- Edge of Knowledge
- Organizational
- Laboratories
- Field Stations
- In Memoriam
BRIEF RESEARCH REPORT article
Adjustment to a “new normal:” coping flexibility and mental health issues during the covid-19 pandemic.

- 1 Department of Psychology, The University of Hong Kong, Hong Kong, China
- 2 Department of Psychology, The University of Oslo, Oslo, Norway
- 3 Modum Bad Psychiatric Hospital, Vikersund, Norway
The Coronavirus Disease 2019 (COVID-19) pandemic is an unprecedented health crisis in terms of the scope of its impact on well-being. The sudden need to navigate this “new normal” has compromised the mental health of many people. Coping flexibility, defined as the astute deployment of coping strategies to meet specific situational demands, is proposed as an adaptive quality during this period of upheaval. The present study investigated the associations between coping flexibility and two common mental health problems: COVID-19 anxiety and depression. The respondents were 481 Hong Kong adults (41% men; mean age = 45.09) who took part in a population-based telephone survey conducted from April to May 2020. Self-report data were assessed with the Coping Flexibility Interview Schedule, COVID-19-Related Perception and Anxiety Scale, and Center for Epidemiological Studies Depression Scale. Slightly more than half (52%) of the sample met the criteria for probable depression. Four types of COVID-19 anxiety were identified: anxiety over personal health, others' reactions, societal health, and economic problems. The results consistently revealed coping flexibility to be inversely associated with depression and all four types of COVID-19 anxiety. More importantly, there was a significant interaction between perceived likelihood of COVID-19 infection and coping flexibility on COVID-19 anxiety over personal health. These findings shed light on the beneficial role of coping flexibility in adjusting to the “new normal” amid the COVID-19 pandemic.
Introduction
The emergence of an atypical coronavirus, SARS-CoV-2, instigated a global outbreak of Coronavirus Disease 2019 [COVID-19; e.g., ( 1 )]. Following identification of the earliest cases of COVID-19 in December 2019, the World Health Organization ( 2 ) declared the viral outbreak a health emergency of international concern on January 30, 2020, and then a global pandemic <2 months later. The escalating pandemic has induced anxiety and panic reactions in the general public, and the emotional responses bear some resemblance to those observed amid the severe acute respiratory syndrome (SARS) outbreak in 2003 [e.g., ( 3 , 4 )]. For instance, the panic sell-off of stocks led to a plunge in the global stock market ( 5 ), and long lines for food and the irrational stockpiling of personal protection equipment such as facemasks and hand sanitizers have been widely seen ( 6 , 7 ).
Despite such resemblances, the COVID-19 pandemic is an unprecedented crisis in terms of the scope of its influence on both physical and mental health [e.g., ( 8 , 9 )]. To curb the transmission of this hitherto unknown virus, governments all over the world have enforced strict epidemic-control measures such as nationwide school closures, stay-at-home orders, and physical distancing regulations in public areas ( 10 ). Also, myriad public and private organizations have adopted teleworking policies mandating that their employees work from home ( 11 ). Although employees hold generally favorable attitudes toward home-based teleworking, the sudden drastic change in work mode left many unprepared ( 12 ). Previous research on the office-home transition has revealed major changes in the work environment to induce the most stress and anxiety in employees who feel the least prepared for this alternative work mode ( 13 ). Devastating problems arising from stressful life changes have been documented not only in adults but also in youngsters, with recent studies revealing a significant proportion of children and adolescents to have experienced psychological distress during the school-closure period ( 14 , 15 ). The COVID-19 pandemic has confronted people of all ages with fundamental life changes [e.g., ( 16 , 17 )].
To grapple with the “new normal” and deal with the considerable challenges brought about by the pandemic, individuals need a considerable degree of flexibility. Psychological resilience is a widely recognized mechanism underlying the adjustment process, with coping flexibility a core component [e.g., ( 18 )]. The theory of coping flexibility postulates that effective coping entails (a) sensitivity to the diverse situational demands embedded in an ever-changing environment and (b) variability in deploying coping strategies to meet specific demands ( 19 ). More specifically, psychological adjustment is a function of the extent to which individuals deploy problem-focused coping strategies (e.g., direct action) in controllable stressful situations and emotion-focused coping strategies (e.g., distraction) in uncontrollable ones. Inflexible coping, in contrast, has been linked to psychological symptoms. For example, individuals with heightened anxiety levels are characterized by an illusion of control [e.g., ( 20 , 21 )]. They tend to perceive all events in life as being under their control, and thus predominantly opt for problem-focused coping regardless of the situational characteristics. In contrast, individuals with depression are characterized by a sense of learned helplessness [e.g., ( 22 , 23 )]. They tend to view all events as beyond their control, and thus predominantly deploy emotion-focused coping across stressful events. Coping flexibility has been identified to foster adjustment to stressful life changes, which is indicated by a reduction in symptoms of anxiety and depression commonly experienced in stressful life transitions ( 24 ).
Applying these theories and findings to psychological adjustment during the COVID-19 pandemic, individuals higher in coping flexibility are predicted to experience lower levels of anxiety and depression than those lower in coping flexibility. Clinical trial findings on COVID-19 offer a mixture of promise and disappointment regarding the efficacy of SARS-CoV-2 vaccine candidates [e.g., ( 25 )], and the absence of a thorough understanding of the etiology and treatment of this atypical virus has elicited widespread public panic responses. According to the theory of psychological entropy ( 26 ), uncertainty is a crucial antecedent of anxiety. In accordance with that theory, studies conducted during the pandemic have revealed unusually high prevalence rates of mental health problems such as anxiety and depression, rates ~3-fold higher than both their pre-pandemic prevalence and lifetime prevalence over the past two decades ( 27 , 28 ).
In light of the transactional theory of stress and coping that highlights the importance of primary and secondary appraisals in the coping process ( 29 ), coping flexibility (secondary appraisal) is predicted to explain the association between context-specific health beliefs (primary appraisal) and mental health. Instead of perceiving the COVID-19 pandemic as aversive and uncontrollable, resilient copers tend to espouse a more complex view by recognizing both controllable and uncontrollable aspects of the pandemic. For instance, these individuals tend to take such positive actions as acquiring new information technology and digital skills to meet the demands of home-based teleworking, but engage in meditation to cope with the unpleasant emotions brought about by mandatory stay-at-home orders. Accordingly, coping flexibility is hypothesized to be inversely associated with anxiety and depression during the pandemic.
As individuals high in coping flexibility are characterized by cognitive astuteness in making distinctions in an array of stressful events ( 30 , 31 ), coping flexibility is also predicted to interact with context-specific health beliefs to have a conjoint influence on mental health in the pandemic context. Although COVID-19 shares similar characteristics with other atypical coronaviruses of SARS and Middle East respiratory syndrome (MERS), the case fatality rate of COVID-19 is much lower than the others ( 32 ). Among individuals high in coping flexibility, those who tend to perceive such differences may experience lower COVID-19 anxiety than their counterparts who do not hold this perception. In this respect, mental health experienced during the pandemic is a function of both context-specific health beliefs and coping flexibility.
The present study was conducted during the “second wave” of COVID-19 infections in Hong Kong. Although the first confirmed COVID-19 case was identified on January 23, 2020, with the first death recorded 2 weeks later ( 33 ), Hong Kong remained largely unscathed by the first wave, with only sporadic cases reported and a relatively flat epidemic curve (i.e., fewer than 100 confirmed cases). However, there was a sudden surge in confirmed cases in March, when the viral outbreak swept the globe ( 34 ). The Government of the Hong Kong Special Administrative Region (HKSAR) responded to the health emergency by enacting a travel ban on non-residents, issuing compulsory quarantine orders for residents returning from overseas, and tightening various physical distancing measures in late March and early April [e.g., ( 35 , 36 )]. Special work arrangements for government employees were also implemented, and many organizations followed suit. The psychosocial impact was thus so pervasive that all sectors of society were affected. A population-based survey was therefore deemed the most appropriate method for investigating the psychological reactions to the pandemic among residents of Hong Kong. The method yields heterogeneous community samples, which maximizes representativeness and minimizes sampling errors.
Materials and Methods
Sample size determination and power analysis.
The statistical power analysis showed that the minimum sample size was 276 in order to identify statistically significant associations among the study variables, but a larger sample size was recruited to meet the requirements for conducting principal component analysis (PCA). Considering the general rule of thumb of having at least 50 cases per factor and a maximum number of nine factors to be identified in the PCA, the pre-planned minimum sample size was 450.
Participants and Procedures
The respondents were 481 Hong Kong adults (41% men; mean age = 45.09, SD = 23.42), who were recruited from a population-based telephone survey conducted by a survey research center at the first author's university. Random digit dialing was used for identifying eligible households, and then the most recent birth day method was employed to select a household member. To be eligible for participation, respondents had to be aged 18 or older, a resident of Hong Kong, able to understand Cantonese, and willing to give consent. Participation was voluntary, and all respondents who completed the survey were entered into a lucky draw for a chance to win gift certificates worth 500 Hong Kong dollars (about 65 U.S. dollars).
Trained interviewers conducted the telephone interviews using a structured questionnaire with standard questions. To foster interviewer calibration and minimize measurement bias, the survey was piloted in a small group of respondents from April 2 to 10, 2020. The final set of survey questions was amended to enhance the clarity of a few items, and then the full survey was administered from April 20 to May 19, 2020.
The study was conducted according to the ethical research standards of the American Psychological Association, and the study protocol was reviewed and approved by the human research ethics committee of the first author's university before the survey began (approval number: EA1912046 dated March 4, 2020). All respondents gave verbal consent in accordance with the Declaration of Helsinki.
Instruments
Coping flexibility.
Coping flexibility was assessed by the revised Coping Flexibility Interview Schedule ( 37 ). This interview schedule was originally developed based on clinical samples ( 38 ), and was adjusted for use with heterogeneous non-clinical populations. In the pilot phase, some respondents reported difficulty in understanding the terms of primary and secondary approach coping that was currently used in our interview schedule. The interview questions were revised by combining the terms of primary and secondary approach coping into problem-focused coping and converting the term of avoidant coping style into emotion-focused coping. Problem-focused and emotion-focused coping were originally used in the transactional theory of coping ( 39 ) from which the Coping Flexibility Interview Schedule was derived. The respondents were asked to report their deployment of problem-focused (e.g., information seeking, monitoring) and emotion-focused (e.g., acceptance, relaxation) coping in controllable and uncontrollable stressful situations over the past month.
To obtain a composite score of coping flexibility indicating strategy-situation fit, the individual coping items were subsequently coded by two independent raters according to a coding scheme ( 40 , 41 ) based on coping theories ( 39 , 42 ). One point was given to the deployment of problem-focused coping strategies to handle controllable stressful events and/or the deployment of emotion-focused coping strategies to handle uncontrollable stressful events. Zero points were given otherwise. All of these scores were aggregated, and then averaged to obtain a composite score. Inter-rater agreement was evaluated using Krippendorff alpha coefficients ( 43 ), and the results showed no discrepancies because no subjective codings were required (Krippendorff alpha = 100%).
COVID-19-Related Perceptions
Both perceived likelihood and impact of COVID-19 infection were measured by a modified measure developed and validated during the SARS outbreak ( 44 ). To make this measure relevant to the present pandemic context, the context was altered from “SARS outbreak” to “COVID-19 pandemic.” Respondents gave four-point ratings to indicate their perception of the likelihood of contracting COVID-19 (1 = very unlikely , 4 = very likely ) and the impact of having it (1 = no impact at all , 4 = a large impact ). The measure has been found to display both criterion and predictive validity ( 44 , 45 ).
COVID-19 Anxiety
As the events that have occurred during the COVID-19 pandemic are unprecedented, our team conducted a qualitative study in March 2020 asking participants to list all of the issues that had made them feel anxious during the pandemic. Content analysis of the results revealed 16 distinct themes regarding anxiety-provoking issues experienced amid the pandemic (see Table 1 for details). These items were compiled into a context-specific measure for assessing COVID-19 anxiety. Respondents rated each item on a scale ranging from 1 ( not worried at all ) to 4 ( very worried ).
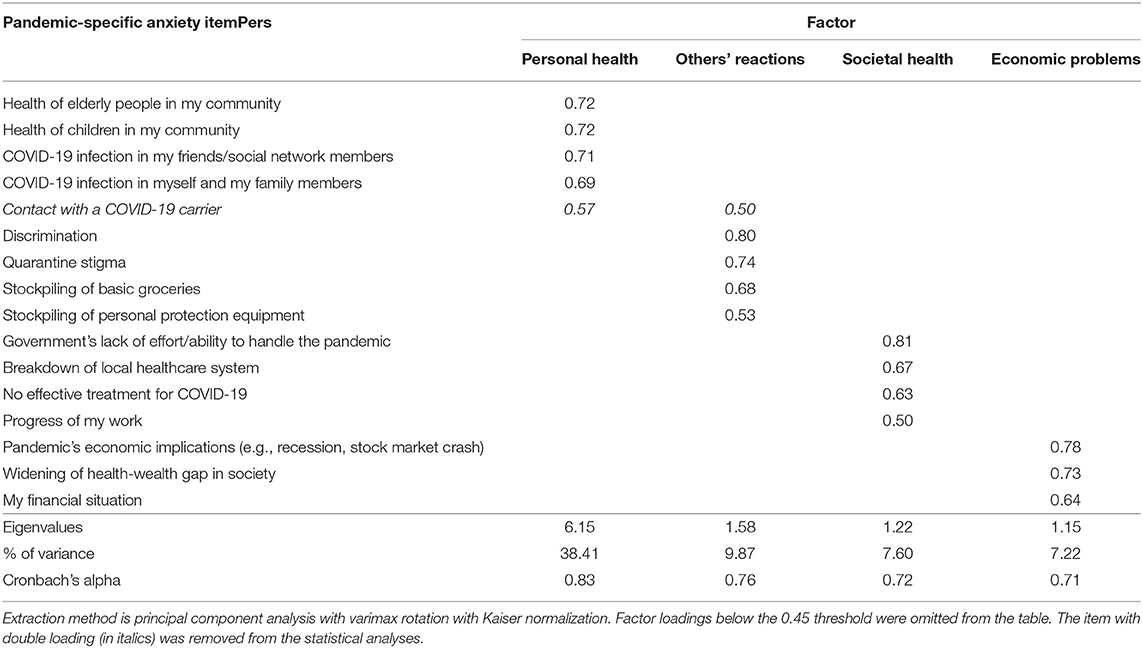
Table 1 . Four-factor promax-rotated factor solution for COVID-19 anxiety ( n = 481).
Depression was measured by the short form of the Center for Epidemiological Studies Depression Scale ( 46 ), which contains 10 items. The translated Chinese version was used in this study ( 47 ). Respondents rated each item on a four-point scale (0 = rarely or none of the time , 3 = most or all of the time ). In this study, we applied the recommended cut-off score of 10 as the classification scheme [e.g., ( 46 , 48 )].
Statistical Analysis
All statistical procedures were conducted using SPSS version 26.0 for Windows (IBM Corporation, 2019, Armonk, NY). Before hypothesis testing, PCA was performed to identify the factorial structure underlying the 16 anxiety-provoking issues. The components were rotated using the varimax method with Kaiser normalization to increase the interpretability of the findings. The number of factors extracted was determined by the Kaiser rule, with factors retained when the eigenvalue exceeded one. The total amount of variance accounted for by the factors needed to exceed 60%, a minimum criterion for factor selection widely adopted in PCA research ( 49 ). Both the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy and Bartlett's test of sphericity were first examined to check the appropriateness for analyzing the dataset, with appropriateness indicated if the KMO index was >0.50 and the test of sphericity was significant. For PCA, items with a factor loading <0.45 or double loading were removed. Cronbach alpha was used to indicate internal consistency for the items within each factor, with an alpha >0.70 considered adequate.
The potential differences among demographic groups were examined. Differences in sex were detected using an independent-samples t -test, and age differences using Pearson zero-order correlation analysis. In addition to testing age as a continuous variable, we also adopted a generational approach proposed by the Pew Research Center that makes comparisons across four age cohorts: (a) Millennials, who were born in 1981 or after; (b) Generation X-ers, who were born between 1965 and 1980; (c) Baby Boomers, who were born between 1946 and 1964; and (d) Silent Gen'ers, who were born before 1946 ( 50 ). A general linear model (GLM) was employed to investigate the differences among the four generations, with post hoc Bonferroni tests conducted if generational differences were found in any of the study variables.
Pearson zero-order correlation analysis was conducted to obtain an overview of the inter-relationships among the study variables. The hypothesized beneficial role of coping flexibility on mental health was then tested using three-step hierarchical regression analysis. First, the two demographic variables (i.e., sex and age) were entered to control for their potential effects on the criterion in question. Second, the variables of perceived likelihood of COVID-19 infection, perceived impact of COVID-19 infection, and coping flexibility were entered simultaneously. Third, the Perceived Likelihood of COVID-19 Infection × Coping Flexibility interaction and the Perceived Impact of COVID-19 Infection × Coping Flexibility interaction were entered. To address the potential multicollinearity problem, all of the variables were centered before conducting these analyses. The procedures were identical for each mental health problem included as the criterion variable. To unpack significant interaction effects, post hoc simple effects analysis was employed to examine the effects of COVID-19-related perception on a criterion at each level of coping flexibility.
PCA was performed because the KMO index was high (.87) and Bartlett's test of sphericity was significant (χ 2 = 3379.31, p < 0.0001). The results with the principal component weights of the 16 anxiety-provoking issues are presented in Table 1 . A four-factor solution was yielded, accounting for 63% of the total variance, with 38% explained by the first factor, personal health issues (e.g., “ COVID-19 infection in myself and my family members ”); 10% by the second factor, other people's undesirable reactions (e.g., “ discrimination ”); 8% by the third factor, societal health issues (e.g., “ government's lack of effort/ability to handle the pandemic ”); and 7% by the fourth factor, economic problems (e.g., “ pandemic's economic implications ”). It is noteworthy that one item (i.e., “ contact with a COVID-19 carrier ”) had a double loading with a difference of <0.10, and was thus discarded. All four factors displayed internal consistency (Cronbach alphas > 0.70), and were thus included in the subsequent analyses as indicators of COVID-19 anxiety.
The GLM results revealed a significant cross-generational difference only for anxiety over societal health, F (3, 477) = 33.92, p < 0.0001, partial eta squared = 0.18. Post hoc Bonferroni tests indicated that Silent Gen'ers aged over 74 ( M = 2.02, SD = 0.62) reported significantly less anxiety over societal health than did Millennials aged 18–39 ( M = 2.87, SD = 0.66) or Generation X-ers aged 40–55 ( M = 2.71, SD = 0.68), p s < 0.0001. However, there were no other differences regarding sex, generation, or the Sex × Generation interaction, p s > 0.05.
The descriptive statistics of and inter-relationships among the study variables are presented in Table 2 . The average depression score was 9.85, which was very close to the cut-off score for probable depression. Adopting the standard cut-off criterion of 10, slightly more than half (52%) of the respondents were categorized as having probable depression. The probable depression group ( M = 2.67, SD = 0.75) generally experienced a higher anxiety level over societal health issues than the no depression group ( M = 2.48, SD = 0.73), t = 2.72, p = 0.007. In addition, the probable depression group ( M = 0.50, SD = 0.21) also reported a generally lower degree of coping flexibility than the no depression group ( M = 0.58, SD = 0.21), t (479) = −3.95, p < 0.0001. However, no other significant differences in depression level were found for sex or generation, p s > 0.21.
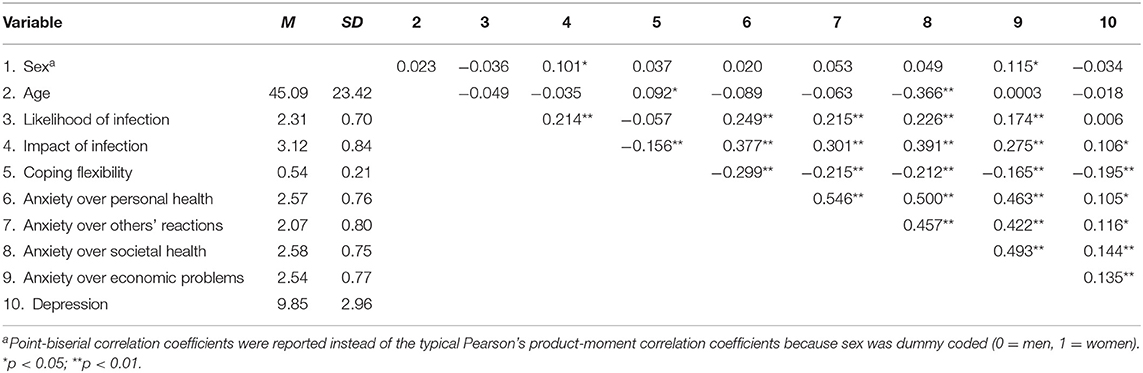
Table 2 . Descriptive statistics of study variables ( n = 481).
Table 3 summarizes the results of hierarchical regression analysis for various mental health problems. As shown in the table, the pattern of results was highly consistent across the four types of COVID-19 anxiety; that is, all four types were positively associated with both the perceived likelihood and impact of COVID-19 infection and inversely associated with coping flexibility. There was also a significant interaction between perceived likelihood of COVID-19 infection and coping flexibility, and the results are presented in Figure 1 . For individuals higher in coping flexibility, those who perceived a lower likelihood of contracting COVID-19 reported less anxiety over their own health than their counterparts who perceived a greater likelihood of such contraction. For individuals lower in coping flexibility, however, such individual differences were absent and they generally reported greater anxiety over their own health than those higher in coping flexibility. In addition, the results revealed depression to also be inversely associated with coping flexibility, although its associations with the two types of COVID-19-related perception were non-significant. In short, these findings provide support for the hypothesized beneficial role of coping flexibility in dealing with mental health issues experienced during the COVID-19 pandemic.
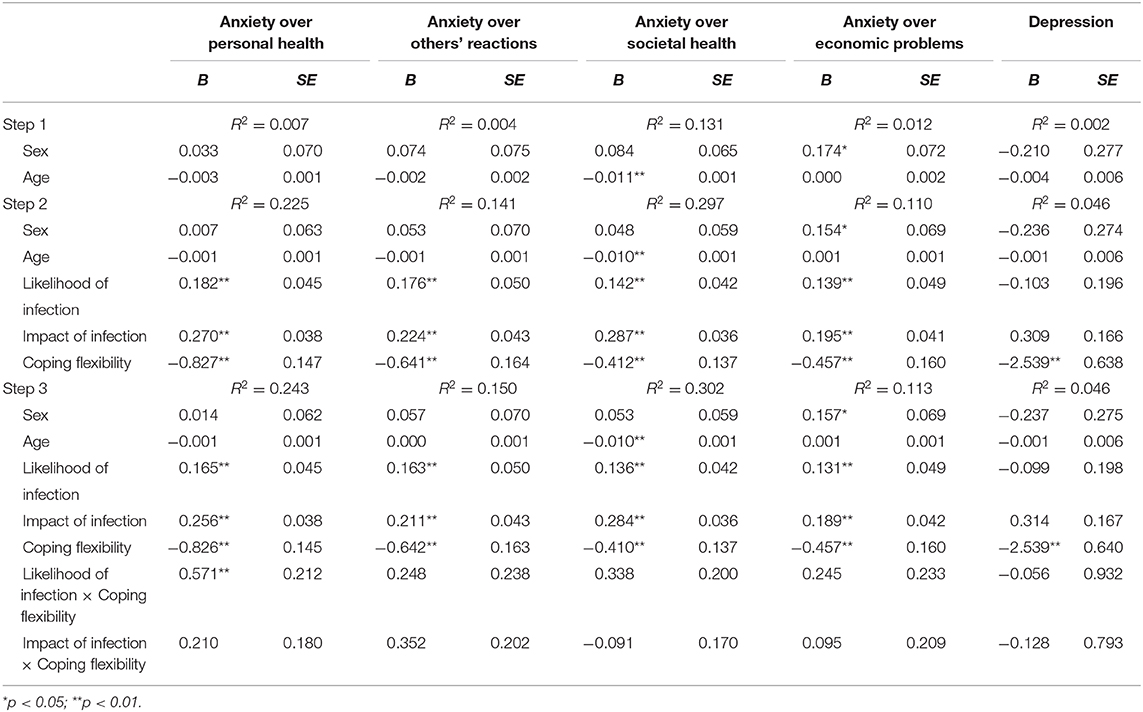
Table 3 . Summary of hierarchical regression analysis by mental health problems ( n = 481).
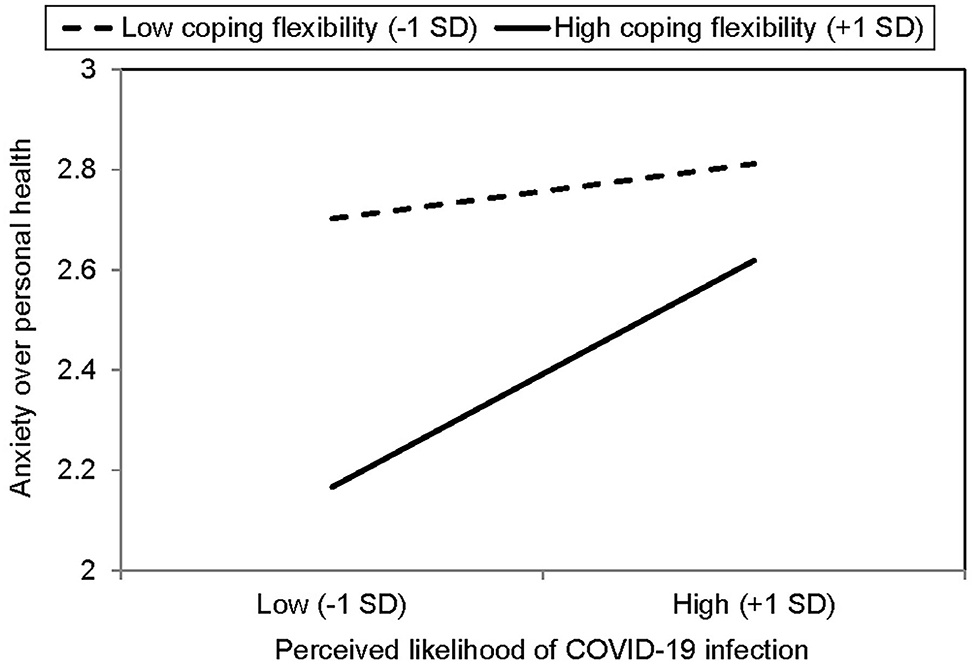
Figure 1 . Simple effects analysis for significant interaction between perceived likelihood of COVID-19 infection and coping flexibility ( n = 481).
In addition to evaluating strategy-situation fit using composite coping flexibility scores, nuanced analysis was conducted to further examine the deployment of individual coping strategies and their associations with mental health problems. Most of the respondents (61%) reported deploying problem-focused coping to handle controllable stressful events during the pandemic, whereas just under half (45%) reported deploying that strategy to deal with uncontrollable stressful events. Fewer respondents said they had used emotion-focused coping to deal with controllable and uncontrollable stressful events (39 and 37%, respectively). Moreover, the deployment of problem-focused coping in controllable stressful events was inversely associated with anxiety over personal health and others' reactions, p s <0.0001, whereas the deployment of emotion-focused coping in controllable stressful events was positively associated with all four types of COVID-19 anxiety and depression, p s < 0.0001. However, neither problem-focused nor emotion-focused coping deployed in uncontrollable stressful events were significantly associated with any of the mental health problems, p s > 0.14.
The present study has investigated coping responses and mental health issues among the general public in Hong Kong amid the second wave of the COVID-19 pandemic. Recent studies have identified high prevalence rates of anxiety and depression among residents of COVID-19-affected regions all over the world [e.g., ( 28 , 51 )]. Our study expands this growing body of research by specifying four major factors of COVID-19 anxiety: personal health, others' reactions, societal health, and economic problems. Although the third factor is characterized primarily by societal health issues, it is interesting to note that a seemingly unrelated item “ progress of my work ” also loaded onto this factor. This perplexing finding may reflect the fact that employees' work progress has been affected more by societal factors (e.g., implementation of prevention and control disease regulations for business and premises, home-based teleworking policy) than personal factors during the pandemic.
A similar phenomenon is found for the fourth factor, economic problems. Most of the items loading onto it involved broad societal issues (e.g., economic recession, widening of health-wealth gap), but an item related to personal financial problems also did so. This finding similarly indicates that individuals' personal financial condition during the pandemic may be influenced to a great extent by the wider economy. Taken together, these interesting findings reflect the intricate interactions between the individual and society in times of crisis, thus attesting to the necessity of identifying anxiety-provoking issues specific to the pandemic in addition to assessing generic mental health issues that are context-free.
In addition to anxiety, our findings also show depression to have been prevalent among Hong Kong adults during the second wave of the pandemic, with slightly more than half the sample identified as having probable depression. Compared with respondents without depression, those with probable depression tended to experience greater anxiety related to societal health issues but not economic problems or personal health issues. These findings indicate that the unusually high prevalence of depression reported during the pandemic is largely related to health-related problems at the societal level (e.g., governmental actions to combat COVID-19, possible breakdown of local healthcare system) rather than personal health issues.
More importantly, the present study is the first to apply the theory of coping flexibility to the context of the COVID-19 pandemic, and the findings provide support for the hypothesized beneficial role of coping flexibility in relieving heightened anxiety and depression when handling the vicissitudes emerged during the pandemic. Astute strategy deployment to meet the specific demands of an ever-changing environment is essential for adjustment to the “new normal,” and a better strategy-situation fit is found to be inversely associated with both COVID-19 anxiety and depression. It is noteworthy that coping flexibility interacts with perceived susceptibility to COVID-19 infection to have a conjoint influence on COVID-19 anxiety. Even within individuals having a higher level of coping flexibility, those tend to experience fewer symptoms of COVID-19 anxiety over personal health if they display cognitive astuteness in assessing their possibility of contracting COVID-19. These novel findings provide support for the notion that the anxiety-buffering role of coping flexibility is highly context-specific ( 24 ), which is confined to infection susceptibility and anxiety over personal health in this stressful encounter. Such context-specificity is not surprising because subjective appraisals of the possibility of contracting a novel virus should be directly linked with concerns over personal health rather than other anxiety-provoking events related to non-health issues or to the society at large. Moreover, these findings further demonstrate that COVID-19 anxiety is not a unidimensional construct and should thus be studied using a multidimensional approach.
We further found the use of problem-focused coping to deal with controllable stressful events to be related to lower levels of anxiety over personal issues (i.e., personal health and others' reactions) rather than broader societal issues (i.e., societal health, economic problems). It is also noteworthy that the use of emotion-focused coping to handle controllable rather than uncontrollable stressful events was related to higher COVID-19 anxiety and depression, a finding consistent with previous studies on clinical samples of depression ( 22 ). Although the unprecedented COVID-19 pandemic is objectively an uncontrollable stressor due to its uncertain nature, the theory of coping flexibility highlights the importance of identifying aspects of life that are controllable and distinguishing these aspects from most other uncontrollable ones in a stressful encounter. For example, when a person high in coping flexibility fails to buy facemasks after visiting many stores, this person still regards the problem as controllable and keeps trying a variety of alternative means (e.g., placing orders in overseas online stores, seeking advice from members of WhatsApp groups). It is the cognitive astuteness in distinguishing between controllable and uncontrollable life aspects that fosters adjustment to stressful life changes.
Such situational differences in coping effectiveness indicate that neither problem-focused nor emotion-focused coping is inherently adaptive or maladaptive. The role of effective coping in mitigating mental health problems depends largely on the extent to which a deployed strategy meets the specific demands of the stressful encounter concerned. For instance, playing online games or browsing social network sites can be stress-relieving during leisure time ( 52 , 53 ), but prolonged gameplay or social media use can impair work or academic performance while working or studying from home ( 54 ). These findings are in line with the theory of coping flexibility, highlighting the beneficial role of flexible coping in soothing mental health problems experienced during the pandemic.
The present findings also have practical implications. Given the beneficial role of coping flexibility, clinicians may work with clients to enhance coping effectiveness with regard to strategy-situation fit. Stress management intervention may involve sharpening clients' skills for (a) distinguishing the key demands stemming from an array of stressful events; (b) assessing whether or not such demands are amendable to a change in effort (i.e., controllable or uncontrollable); (c) applying the meta-cognitive skill of reflection to evaluate strategies that best match the specific demands of diverse stressful situations; and (d) subsequently deploying the most appropriate strategy to handle each stressor. Such flexible coping skills are especially useful for dealing with the psychological distress elicited by a pandemic involving an assortment of stressful events.
Coping flexibility may also be valuable at a broader level because the unpredictable progression of the COVID-19 pandemic across successive waves presents varying challenges for public health authorities worldwide. For instance, the shortage of personal protection equipment aroused immense public anxiety in Hong Kong during the first wave owing to the sudden surge in demand for facemasks and hand sanitizer. After the supply of such equipment had been stabilized, however, new societal problems emerged. For example, during the second wave, public commitment to observing physical distancing measures began to wane owing to “pandemic fatigue” ( 55 ). Public health authorities may need to adopt a certain degree of flexibility in monitoring and identifying emerging issues to allow the timely adjustment of extant disease-control measures or the formulation of new ones to mitigate changing public health threats.
Despite its important findings, several study limitations must be noted. The survey was conducted during the second wave of the pandemic, when the epidemic curve climbed to a high level and then leveled off for a few months before reaching a further peak in the third wave in July and August, 2020 ( 34 ). As the COVID-19 pandemic continues to evolve in an unpredictable manner, some of the anxiety-provoking issues identified in this study may no longer elicit anxiety to the same extent in future waves. The list of issues eliciting COVID-19 anxiety should thus be updated in future research. Given the time sensitivity of these issues, pilot testing is essential to evaluate their relevance in particular phases of the pandemic.
Further, although our findings offer robust support for the hypothesized beneficial role of coping flexibility amid the pandemic, previous meta-analysis indicated that that beneficial role is more prominent in collectivist than individualist regions ( 19 ). A fruitful direction for future research would thus be to replicate the present design in individualist countries, allowing cross-cultural comparisons to be made. In addition to cultural differences, there may also be considerable variations among Chinese adults residing in different regions, as the epidemic trajectory has varied greatly among cities in the Greater Bay Area, such as Guangzhou and Macau ( 56 ). Greater effort can be made to compare the prevalence of psychological disorders and coping processes among Chinese residents of diverse regions.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by the study protocol was reviewed and approved by the Human Research Ethics Committee of the University of Hong Kong (approval number: EA1912046 dated March 4, 2020). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
CC contributed to project design and administration, coordinated the data collection, performed the statistical analysis, and wrote the first draft of the manuscript. H-yW contributed to project design, survey creation, statistical analysis, and data interpretation. OE contributed to data interpretation and writing parts of the manuscript. All authors contributed to the article and approved the submitted version.
This research project was funded by the Public Policy Research Funding Scheme from the Policy Innovation and Co-ordination Office (Project Number: SR2020.A8.019) and General Research Fund (Project Number: 17400714) of the Government of the Hong Kong Special Administrative Region. The funders had no role in study design and administration, statistical analysis or interpretation, manuscript writing, or the decision to submit the paper for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The author would like to thank Sylvia Lam, Sophie Lau, Janice Leung, Yin-wai Li, Stephanie So, Yvonne Tsui, and Kylie Wong for research and clerical assistance.
1. Lai C, Shih T, Ko W, Tang H, Hsueh P. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. (2020) 55:105924. doi: 10.1016/j.ijantimicag.2020.105924
PubMed Abstract | CrossRef Full Text | Google Scholar
2. World Health Organization. Timeline: WHO's COVID-19 Response . (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed October 8, 2020).
Google Scholar
3. Chen R, Chou K, Huang Y, Wang T, Liu S, Ho L. Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. Int J Nurs Stud. (2006) 43:215–25. doi: 10.1016/j.ijnurstu.2005.03.006
4. Cheng C, Tang CS. The psychology behind the masks: psychological responses to the severe acute respiratory syndrome outbreak in different regions. Asian J Soc Psychol. (2004) 7:3–7. doi: 10.1111/j.1467-839X.2004.00130.x
5. Baker SR, Bloom N, Davis SJ, Kost K, Sammon M, Viratyosin T. The unprecedented stock market reaction to COVID-19. Rev Asset Pricing Studies. (2020) raaa008. doi: 10.3386/w26945
CrossRef Full Text | Google Scholar
6. Arafat SY, Kar SK, Marthoenis M, Sharma P, Apu EH, Kabir R. Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. (2020) 289:113061. doi: 10.1016/j.psychres.2020.113061
7. Wong JEL, Leo YS, Tan CC. COVID-19 in Singapore—current experience: critical global issues that require attention and action. JAMA. (2020) 323:1243–4. doi: 10.1001/jama.2020.2467
8. Bressington DT, Cheung TCC, Lam SC, Suen LKP, Fong TKH, Ho HSW. Association between depression, health beliefs, and face mask use during the COVID-19 pandemic. Front Psychiatry. (2020) 11:1075. doi: 10.3389/fpsyt.2020.571179
9. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
10. Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA. (2020) 323:2137–8. doi: 10.1001/jama.2020.5460
11. Belzunegui-Eraso A, Erro-Garcés A. Teleworking in the context of the Covid-19 crisis. Sustainability. (2020) 12:3662. doi: 10.3390/su12093662
12. Persol Research and Development. Survey of Telework in Japan for COVID-19 . Nagoya: Author (2020).
13. Harris L. Home-based teleworking and the employment relationship: managerial challenges and dilemmas. Pers Rev. (2003) 32:422–37. doi: 10.1108/00483480310477515
14. Tang S, Xiang M, Cheung T, Xiang Y. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. (2021) 279:353–60. doi: 10.1016/j.jad.2020.10.016
15. Zhang Z, Zhai A, Yang M, Zhang J, Zhou H, Yang C. Prevalence of depression and anxiety symptoms of high school students in shandong province during the COVID-19 epidemic. Front Psychiatry. (2020) 11:1499. doi: 10.3389/fpsyt.2020.570096
16. Voitsidis P, Gliatas I, Bairachtari V, Papadopoulou K, Papageorgiou G, Parlapani E. Insomnia during the COVID-19 pandemic in a greek population. Psychiatry Res. (2020) 289:113076. doi: 10.1016/j.psychres.2020.113076
17. Cheng C, Ebrahimi OV, Lau Y. Maladaptive coping with the infodemic and sleep disturbance in the COVID-19 pandemic. J Sleep Res. (2020) e13235. doi: 10.1111/jsr.13235
18. Lam CB, McBride-Chang CA. Resilience in young adulthood: the moderating influences of gender-related personality traits and coping flexibility. Sex Roles. (2007) 56:159–72. doi: 10.1007/s11199-006-9159-z
19. Cheng C, Lau HB, Chan MS. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol Bull. (2014) 140:1582–607. doi: 10.1037/a0037913
20. Cheng C, Hui W, Lam S. Psychosocial factors and perceived severity of functional dyspeptic symptoms: a psychosocial interactionist model. Psychosom Med. (2004) 66:85–91. doi: 10.1097/01.PSY.0000106885.40753.C1
21. Sanderson WC, Rapee RM, Barlow DH. The influence of an illusion of control on panic attacks induced via inhalation of 5.5% carbon dioxide-enriched air. Arch Gen Psychiatry. (1989) 46:157–162. doi: 10.1001/archpsyc.1989.01810020059010
22. Gan Y, Zhang Y, Wang X, Wang S, Shen X. The coping flexibility of neurasthenia and depressive patients. Pers Individ Differ. (2006) 40:859–71. doi: 10.1016/j.paid.2005.09.006
23. Zong J, Cao XY, Cao Y, Shi YF, Wang YN, Yan C, et al. Coping flexibility in college students with depressive symptoms. Health Quality Life Outcomes. (2010) 8:1–6. doi: 10.1186/1477-7525-8-66
24. Cheng C, Chau C. When to approach and when to avoid? Funct Flex Key Psychol Inquiry. (2019) 30:125–9. doi: 10.1080/1047840X.2019.1646040
25. Jean S, Lee P, Hsueh P. Treatment options for COVID-19: The reality and challenges. J Microbiol Immunol Infect. (2020) 53:436–43. doi: 10.1016/j.jmii.2020.03.034
26. Hirsh JB, Mar RA, Peterson JB. Psychological entropy: a framework for understanding uncertainty-related anxiety. Psychol Rev. (2012) 119:304–20. doi: 10.1037/a0026767
27. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US Adults before and during the COVID-19 pandemic. JAMA Network Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
28. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
29. Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen RJ. The dynamics of a stressful encounter. In: Higgins ET, Kruglanski AW, editors. Motivational Science: Social and Personality Perspectives . New York, NY: Psychology Press (2000). p. 111–27.
30. Cheng C. Dialectical thinking and coping flexibility: a multimethod approach. J Pers. (2009) 77:471–94. doi: 10.1111/j.1467-6494.2008.00555.x
31. Cheng C, Chiu C, Hong Y, Cheung JS. Discriminative facility and its role in the perceived quality of interactional experiences. J Pers. (2001) 69:765–86. doi: 10.1111/1467-6494.695163
32. Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: are they closely related? Clin Microbiol Infect. (2020) 26:729–34. doi: 10.1016/j.cmi.2020.03.026
33. Centre for Health Protection. Number of Notifiable Infectious Diseases by Month in 2020 . (2020). Available onlone at: https://www.chp.gov.hk/en/statistics/data/10/26/43/6896.html (accessed October 8, 2020).
34. Statista. Number of Novel Coronavirus COVID-19 Cumulative Confirmed, Recovered and Death Cases in Hong Kong from January 30 to October 25, 2020 . (2020). Available online at: https://www.statista.com/statistics/1105425/hong-kong-novel-coronavirus-covid19-confirmed-death-recovered-trend/ (accessed October 28, 2020).
35. The HKSAR and Government (2020). Government Announces Enhancements to Anti-Epidemic Measures in Four Aspects . Available online at: https://www.info.gov.hk/gia/general/202003/24/P2020032400050.htm (accessed October 8, 2020).
36. news.gov.hk. Restrictions on Bars Gazetted . (2020). Available online at: https://www.news.gov.hk/eng/2020/04/20200402/20200402_195740_071.html (accessed October 8, 2020).
37. Atal S, Cheng C. Socioeconomic health disparities revisited: coping flexibility enhances health-related quality of life for individuals low in socioeconomic status. Health Qual Life Outcomes. (2016) 14:1–7. doi: 10.1186/s12955-016-0410-1
38. Cheng C, Hui W, Lam S. Perceptual style and behavioral pattern of individuals with functional gastrointestinal disorders. Health Psychol. (2000) 19:146–54. doi: 10.1037/0278-6133.19.2.146
39. Lazarus RS, Folkman S. The concept of coping. In: Monat A, Lazarus RS, editors. Stress and Coping: An Anthology . New York, NY: Columbia University (1991). p. 189–206
40. Cheng C, Chan NY, Chio JHM, Chan P, Chan AOO, Hui WM. Being active or flexible? Role of control coping on quality of life among patients with gastrointestinal cancer. Psychooncology. (2012) 21:211–8. doi: 10.1002/pon.1892
41. Cheng C, Cheng F, Atal S, Sarwono S. Testing of a dual process model to resolve the socioeconomic health disparities: a tale of two Asian countries. Int J Environ Res Public Health. (2021) 18:717. doi: 10.3390/ijerph18020717
42. Endler NS. Stress, anxiety and coping: the multidimensional interaction model. Can Psychol. (1997) 38:136–53. doi: 10.1037/0708-5591.38.3.136
43. Hayes AF, Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. (2007) 1:77–89. doi: 10.1080/19312450709336664
44. Cheng C, Ng A. Psychosocial factors predicting SARS-preventive behaviors in four major SARS-affected regions. J Appl Soc Psychol. (2006) 36:222–47. doi: 10.1111/j.0021-9029.2006.00059.x
45. Cheng C, Cheung MWL. Psychological responses to outbreak of severe acute respiratory syndrome: a prospective, multiple time-point study. J Pers. (2005) 73:261–85. doi: 10.1111/j.1467-6494.2004.00310.x
46. Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Am J Prev Med. (1994) 10:77–84. doi: 10.1016/S0749-3797(18)30622-6
47. Yang CF. Measures of Personality and Social Psychological Attitudes , Vol. 1. Taipei: Yuan-Liou (1997).
48. Boey KW. Cross-validation of a short form of the CES-D in Chinese elderly. Int J Geriatr Psychiatry. (1999) 14:608–17. doi: 10.1002/(SICI)1099-1166(199908)14:8<608::AID-GPS991>3.0.CO;2-Z
49. Bagozzi RP, Youjae Y. On the evaluation of structural equation models. J Acad Mark Sci. (1988) 16:74–94. doi: 10.1007/BF02723327
50. Wang H, Cheng C. New perspectives on the prevalence and associated factors of gaming disorder in Hong Kong community adults: a generational approach. Comput Hum Behav. (2021) 114:106574. doi: 10.1016/j.chb.2020.106574
51. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. (2020) 16:1–11. doi: 10.1186/s12992-020-00589-w
52. Kardefelt-Winther D. The moderating role of psychosocial well-being on the relationship between escapism and excessive online gaming. Comput Hum Behav. (2014) 38:68–74. doi: 10.1016/j.chb.2014.05.020
53. Young NL, Daria JK, Mark DG, Christina JH. Passive Facebook use, Facebook addiction, and associations with escapism: an experimental vignette study. Comput Hum Behavi. (2017) 71:24–31. doi: 10.1016/j.chb.2017.01.039
54. Cheng C, Lau Y, Luk JW. Social capital–accrual, escape-from-self, and time-displacement effects of internet use during the COVID-19 stay-at-home period: prospective, quantitative survey study. J Med Int Res. (2020) 22:e22740. doi: 10.2196/22740
55. Harvey N. Behavioural fatigue: real phenomenon, naïve construct, or policy contrivance. Front Psychol. (2021) 11:2960. doi: 10.3389/fpsyg.2020.589892
56. Johns Hopkins Coronavirus Resource Center. Coronavirus COVID-19 Global Cases . (2021). Available online at: https://coronavirus.jhu.edu/map.html (accessed January 18, 2021).
Keywords: coronavirus disease, resilience, coping, stress, psychological well-being, adaptation, Chinese, epidemic
Citation: Cheng C, Wang H-y and Ebrahimi OV (2021) Adjustment to a “New Normal:” Coping Flexibility and Mental Health Issues During the COVID-19 Pandemic. Front. Psychiatry 12:626197. doi: 10.3389/fpsyt.2021.626197
Received: 05 November 2020; Accepted: 01 March 2021; Published: 19 March 2021.
Reviewed by:
Copyright © 2021 Cheng, Wang and Ebrahimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cecilia Cheng, ceci-cheng@hku.hk
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- Long-term effects of COVID-19
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
Help transform healthcare
Your donation can make a difference in the future of healthcare. Give now to support Mayo Clinic's research.

- Find a Doctor
- Patients & Visitors
- ER Wait Times
- For Medical Professionals
- Piedmont MyChart

- Medical Professionals
- Find Doctors
- Find Locations
Receive helpful health tips, health news, recipes and more right to your inbox.
Sign up to receive the Living Real Change Newsletter
Managing stress during the ongoing COVID-19 pandemic
Are you feeling stress, fear and anxiety amid the ongoing COVID-19 pandemic ? If so, you’re not alone. The recommendations for masking and social distancing affect nearly every part of our lives, including finances, relationships, transportation, jobs and healthcare.
Some common causes of stress during the coronavirus pandemic are uncertainty, lack of routine and reduced social support, says Mark Flanagan, LMSW, MPH, MA, a social worker at Cancer Wellness at Piedmont .
Routines and COVID-19
As humans, we don’t like uncertainty and tend to thrive in routines , says Flanagan. Routines are essential because they create a sense of normalcy and control in our lives. This sense of control then allows us to manage the challenges that come our way.
“When we don’t have a routine, much of our time is spent trying to establish one,” says Flanagan. “Without a routine, we often pay attention to the things that are most ‘flashy.’ When big news happens, we tend to focus on it more.”
Social support and COVID-19
Not only are our routines currently disrupted, but the routines of everyone around us are as well.
“When something goes wrong in our lives, we can usually rely on others to get a sense of calm,” he says. “But when everyone is experiencing the same sense of uncertainty, there’s no real ‘anchor’ to help manage some of the stress.”
Stress affects your health
Stress management is essential for good physical health , and it’s especially important right now as our world addresses the COVID-19 pandemic .
“While short-term pressures and stress are normal and can help us change in positive ways , chronic stress causes a huge deterioration in our quality of life on a physical level,” says Flanagan. “When we are more pessimistic, depressed or anxious, our immune system goes down and produces more stress hormones, reducing our immunity and increasing inflammation.”
Stress can also put a strain on your mental health, relationships and productivity, he notes.
Stress reduction tips for COVID-19
“Rather than dwell on nervousness, focus on the things you can control,” Flanagan suggests. “When you move the locus of control from something outside yourself to inside yourself, you powerfully reduce anxiety and boost confidence.”
He suggests the following steps to regain control and reduce stress.
Follow the recommended health guidelines. These guidelines include getting the COVID-19 vaccine , frequent hand-washing, wearing a mask in public places, social distancing, practicing respiratory etiquette and cleaning commonly used surfaces. See the latest recommendations from the Centers for Disease Control and Prevention (CDC) . Not only will you protect your health, but you’ll also protect the health of vulnerable people in your community, like older adults and those with serious or underlying health issues.
Create a morning routine. When you’re stuck at home, it can be tempting to let go of basic routines, but Flanagan says a morning routine can help you feel more productive and positive. Consider waking up at the same time each day, exercising, showering, meditating, journaling, tidying your home or having a healthy breakfast as part of your morning ritual.
Check in with loved ones regularly. Staying in touch with family and friends can help reduce stress.
Consider ways to help others. This can include picking up groceries for a neighbor and leaving them at their door, donating to a local charity, or purchasing gift cards from your favorite restaurant. By taking the focus off yourself, you can experience reduced stress and a greater sense of well-being.
Have a daily self-care ritual. Self-care can include exercise, meditation, walking outside, reading, taking a bubble bath, painting, journaling, gardening, cooking a healthy meal or enjoying a favorite hobby. Pick one thing and do it at the same time each day. It will help anchor your day and provide a welcome respite.
Limit news and media consumption. “When we constantly check our newsfeeds and see bad news, it activates our sympathetic nervous system and can send us into fight-or-flight mode,” says Flanagan. He recommends limiting how often you check the news to once or twice a day (ideally not first thing in the morning or after dinner), turning off news alerts, and obtaining information from one or two reputable news outlets.
Set boundaries around social media. “There’s this concept of toxic sociality where we constantly have to be connected, even in superficial ways, and when we’re not, it feels like part of us isn’t being ‘fed,’” he explains. “It’s important to practice social distancing with social media too. We may not think we’re having any effect on our newsfeed, but we can take steps to reduce the ripple effect of panic on social media.” He suggests posting positive messages online and being mindful of your likes, shares and comments.
Meditate. Meditation can help restore your sense of control as you focus on your breath or a positive word or phrase. “ Meditation can help you activate your parasympathetic nervous system, and that’s an antidote to fear,” says Flanagan. “And when you’re more centered, you’re able to create a calm reality around you.” Try this guided meditation to get started.
Encourage others. “Often, when we are scared, it can be tempting to repeat negative messages, but actively encouraging family and friends is really important,” he says. “Chances are, someone is having a harder time than you are. Your words matter and people will respond accordingly. It’s important to realize we are not victims; we are helping to create our environment and change it for the better. By sending positive messages out into the world, you’ll not only affect those around you, but those words will come back to you.”
Hope during the coronavirus pandemic
“It’s important to remember that this will pass sooner or later,” says Flanagan. “The world has gone through many different challenges, like disease outbreaks, war and uncertain times. For better or worse, these times always pass. That doesn’t mean this time isn’t significantly challenging, but if we focus on what we can control and do things that are good for our health and the health of those around us, we will come out of this in perhaps a more whole state and with a renewed perspective. It’s important to look toward the future and begin building for that future. You can always have hope. Hope never leaves us.”
For information on coronavirus (COVID-19), including symptoms, risks and ways to protect yourself, click here.
- coronavirus
- infectious disease
- stress management
Related Stories

Schedule your appointment online
Schedule with our online booking tool
*We have detected that you are using an unsupported or outdated browser. An update is not required, but for best search experience we strongly recommend updating to the latest version of Chrome, Firefox, Safari, or Internet Explorer 11+
Share this story
Download the Piedmont Now app
- Indoor Hospital Navigation
- Find & Save Physicians
- Online Scheduling
Download the app today!
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

The Impact of Different Coping Styles on Psychological Distress during the COVID-19: The Mediating Role of Perceived Stress
1 Graduate School of Education, Fordham University, New York, NY 10023, USA; ude.mahdrof@4gnidy (Y.D.); ude.mahdrof@62gnawhj (J.H.)
2 Beijing Key Laboratory of Applied Experimental Psychology, National Demonstration Center for Experimental Psychology Education, Faculty of Psychology, Beijing Normal University, Beijing 100875, China; moc.361@ysp_cxf (X.F.); moc.361@iewgnohysp (W.H.)
Jacqueline Hwang
3 Teachers’ College, Beijing Union University, Beijing 100874, China; nc.ude.unb.liam@aijgnaw
Associated Data
We do not provide public access to the data set due to protection of the privacy of the participants. Regarding the details of the data, please contact the corresponding author.
The present study aimed to understand the impact of different coping methods endorsed by Chinese college students during COVID-19 through the examination of the mediating role of perceived stress. We recruited a total of 492 undergraduate students to complete an online survey from May to June 2020. The results of structural equation modeling indicated that perceived stress was a significant mediator in the association between different coping styles and psychological distress. Three coping styles, including problem-focused, adaptive emotion-focused, and maladaptive emotion-focused coping styles were all significantly correlated with psychological distress. Perceived stress significantly mediated the association between the three coping styles and psychological distress. The results indicated a full mediation model in which problem-focused coping and adaptive emotion-focused coping affected psychological distress entirely through the mediation of perceived stress. Maladaptive emotion-focused coping positively predicted perceived stress, which in turn positively predicted psychological distress through a partial mediation model. We discuss the implications of these findings and offer suggestions for future research.
1. Introduction
The novel coronavirus behind the current pandemic and disruption of life was given the name of “SARS-CoV-2” and the disease was also named “coronavirus disease 2019” (COVID-19; Centers for Disease Control and Prevention [CDC]) [ 1 ]. Wuhan, in the Hubei province of China, was the first city that reported the first case of COVID-19 in late December 2019. Quickly, the virus spread beyond Hubei Province, and Chinese authorities segregated the affected regions and immediately implemented nationwide mitigation measures according to the severity of the reported cases of COVID-19 [ 2 ]. Although local transmission of the virus was under control by April 2020 in China, COVID-19 had already spread worldwide. The World Health Organization (WHO) characterized COVID-19 as a pandemic (CDC) [ 3 ] on 11 March 2020.
University students have faced numerous challenges during the pandemic. In China, many universities suspended in-person classes and activities in Spring 2021 and through the summer session. Study abroad programs were cut short with universities asking their students to return home. Many university residence halls closed, giving students only a few days’ notice to vacate their dorm rooms [ 4 , 5 , 6 ]. Some academic disciplines did not allow for efficient online courses. Fieldwork, internships, and clinical rotations were suspended. Given the uncertainty of when life would return to normal [ 7 ], students felt uneasy about the course of their academic careers. Due to the effects of COVID-19, many students faced unprecedented stress regarding their living situations, financial burdens, graduation challenges, and job searches [ 8 ]. The present study aimed to examine the mediating role of perceived stress on the associations between three different coping styles and psychological distress during the COVID-19 pandemic through the transactional mode of stress and coping proposed by Lazarus and Folkman [ 9 ].
1.1. Coping Styles
Based on the transactional model of stress and coping developed by Lazarus and Folkman, personal and situational factors influence how one perceives and evaluates encountered situations. Variables within a person and the environment (e.g., beliefs, demands, and constraints) affect stress appraisal and coping strategy use, resulting in physiological and emotional reactions [ 9 ]. Coping could be described as humans’ cognitive and/or behavioral efforts that are used to cope with external and internal demands under a stressful circumstance [ 9 , 10 ].
There are different types of coping strategies. Emotion-focused coping is reactive and refers to attempting to regulate feelings and emotional responses to the stressor (e.g., anger, fear, sadness, anxiety, pressure). Problem-focused coping is proactive and refers to acting on the stressor, the environment, or oneself to address the problem in an attempt to decrease or eliminate the stress [ 10 ]. It was reported that it is more effective to use problem-focused coping in controllable stressful circumstances, but it is more effective to use emotion-focused coping in uncontrollable stressful circumstances [ 11 , 12 ]. A third type of coping, avoidance-focused coping, refers to cognitions and behaviors aimed at avoiding the stressful situation and reactions to it, such as distraction and diversion, and tends to be an initial reaction to stress [ 11 , 13 , 14 , 15 ].
In a study by Kumanova and Karastoyanov that investigated the associations between perceived stress and coping strategies, results showed that people who more often use specific proactive coping strategies, such as reflective coping and strategic planning; specific reactive problem-focused coping strategies, such as effective coping and planning ahead of time; and specific reactive emotion-focused strategies, such as reinterpretation from a positive perspective and growth, experience less stress. Conversely, people who more often use specific reactive emotion-focused coping approaches, such as focusing on emotions, denial, seeking emotional social support, and disengaging, experience more stress [ 16 ].
Different coping strategies also appear in response to different stressful situations. One study examined the relationship between stressors and coping in college students when the 2003 severe acute respiratory syndrome (SARS) epidemic occurred, and researchers found that the active coping was predictive of life satisfaction and the avoidant coping was predictive of psychological symptoms. The results indicated that all types of coping buffered against negative impacts to health. In situations of uncontrollable, large-scale stressors, such as SARS 2003, any type of coping appears to help reduce stress [ 12 ]. In short, there have been mixed findings regarding coping styles and stress.
1.2. Psychological Distress
To slow down and contain the spread of COVID-19, many governments around the world have adopted suppression measures, such as lockdowns, quarantining at home, and bans of social gatherings and public events, which can lead to unintended mental health consequences for the public [ 17 ]. Brooks and colleagues identified some of the factors that might contribute to psychological distress in relation to these measures [ 18 ]. First, ongoing reports of COVID-19 outbreaks in different countries and regions through social media and the press are likely to increase individuals’ anxiety, depression, and fears associated with COVID-19. Second, both valid and invalid information about the negative consequences of COVID-19 might lead to higher levels of anxiety and depression. Third, high-risk individuals, such as the elderly and those with existing medical conditions, might suffer from more severe anxiety and depression.
In China, one of the major suppression measures has been confinement (e.g., staying at home during quarantine, banning of social gatherings). Confinement limits opportunities for social interaction, and it can negatively affect the mental health of vulnerable individuals [ 19 ]. Confinement can lead to increased psychological distress due to limited access to extended family and limited contact with people outside of the home [ 20 ]. Suppression measures have also altered conditions at work and school for many people. Many college students had to immediately transition from in-person instruction to fully virtual instruction, which dramatically increased the hours spent on teleworking for both academic activities and employment activities [ 21 ] and decreased the opportunities for physical activities [ 22 ]. Prolonged hours of teleworking and exclusive virtual learning can lead to mental fatigue and burnout [ 21 ].
1.3. The Mediating Role of Perceived Stress
If an individual perceives that the demands of a situation are beyond their own capabilities to deal with the circumstances, a sense of stress occurs [ 9 ]. The concept of perceived stress highlights that although people might experience the same event (e.g., the COVID-19 pandemic), it is their perception of the event that largely determines their stress response. Unprecedented stressors have affected university students as a consequence of the COVID-19 pandemic [ 5 , 23 ]. The degree to which people find a life situation stressful determines the degree of confidence they have in their ability to cope with that stressful situation. When an individual feels the general stressfulness of their life and realizes that their ability to handle such stress might be limited during specific situations, they perceive stress. In particular, perceived stress consists of factors such as feelings about circumstances that are uncontrollable or unpredictable in one’s life, how much change is occurring, and one’s confidence in one’s ability to deal with the presenting challenges [ 9 , 24 ].
Research has found that perceived stress is associated with self-efficacy, that is, high levels of perceived stress predict low levels of self-efficacy. Additionally, individuals who perceive a stressful situation as a challenge or an opportunity to prove themselves utilize coping skills more effectively and are less likely to think negatively [ 25 , 26 ]. Although all university students have been experiencing the same event, the COVID-19 pandemic, and are likely to cope with the pandemic using different coping styles, it is each student’s perception of the situation that dictates their level of stress, which in turn can affect the onset of psychological distresses, such as mental fatigue, anxiety, and depression.
1.4. Purpose of the Study
Although some previous studies examined copying styles, psychological distress, and perceived stress in numerous circumstances, none of them were conducted during a long-lasting public health crisis such as the COVID-19 which affected the public not only at the individual level, but also at the societal level. In addition, there is no single theory to fully support our theoretical model, which proposed to examine how and to what degree that the perceived stress might mediate the relations between copying styles and psychological distress. In the present study, the focus was to examine the mediating role of perceived stress in the associations between different coping styles and psychological distress among college students during COVID-19. The following questions were proposed: How do problem-focused coping, adaptive emotion-focused coping, and maladaptive emotion-focused coping affect mental health during the COVID-19 pandemic? Are there other potential mediation factors between three coping styles and mental health, such as psychological distress during the COVID-19 pandemic? The findings might provide insights to public health providers and mental health service providers in terms of how to provide prevention and intervention strategies to the public, especially during a public health crisis.
2. Materials and Methods
2.1. participants.
This study was approved by Academic Ethics Committee of the Faculty of Psychology at Beijing Normal University. We recruited 492 Chinese students from two colleges in Beijing who completed the online survey between May and June 2020. The participants comprised 196 (39.8%) males and 296 (60.2%) females. Participants had an average age of 19.51 years (SD = 1.516), with an age range from 17 to 29. Because the public has been through multiple waves of the COVID-19 surges, it is important to explain the social context of the time when the study was implemented. The first COVID-19 case was identified in Wuhan, China in December of 2019. Starting on 3 February 2020, the Chinese authorities closed off Wuhan (a city of 11 million) by canceling planes and trains leaving the city, suspending buses, subways and ferries within it and quarantining the non-essential workers for about two months. After that, sporadic quarantine was conducted in different cities in China, based on the number of COVID-19 cases. Thus, in general, the public was under serious pressure due to uncertainty of the virus and the constantly changing policies enforced by the central or local government. During the time period of data collection, no COVID-19 vaccine was available to the public.
2.2. Measures
2.2.1. coping.
The measure of coping was adapted from the Brief COPE inventory [ 27 ]. This scale initially consisted of 14 subscales and there were two items for each subscale. Yeung and Fung [ 28 ] used one item for each subscale, and there were two categories of the items: problem-focused coping and emotion-focused coping. The categories were separated into adaptive emotion-focused coping (e.g., “I’ve been looking for something positive in what is happening”) and maladaptive emotion-focused coping (e.g., “I’ve been using alcohol or other drugs to make myself feel better”). The Brief COPE consisted of 11 items, including three items for problem-focused coping, two items for adaptive emotion-focused coping, and six items for maladaptive emotion-focused coping. Two items that best fit the pandemic situation to measure adaptive emotion-focused coping were chosen, including “I’ve been looking for something good in what is happening” and “I’ve been accepting the reality of the fact which has happened.” Participants were directed to rate their coping during the peak time of COVID-19, ranging from 1 (none) to 5 (always). Cronbach’s α for the measure of coping was 0.794 in the present study. Cronbach’s α for problem-focused coping, adaptive emotion-focused coping, and maladaptive emotion-focused coping were 0.606, 0.823, and 0.772, respectively.
2.2.2. Perceived Stress
The measure for perceived stress was adapted from the Depression Anxiety Stress Scales [ 29 ]. The sample items were statements such as “Because of COVID-19, I find it difficult to relax.” Participants rated their perceived stress during the peak time of COVID-19, ranging from 1 (strongly disagree) to 5 (strongly agree). The scale consisted of seven items. Cronbach’s α for perceived stress was 0.905 in the present study.
2.2.3. Psychological Distress
We measured psychological distress using the Chinese version of the 10-item Kessler Scale [ 30 ], which was adapted from Kessler et al. [ 31 ]. The scale consisted of 10 items. The sample items were statements such as “I felt so sad that nothing could cheer me up.” Participants were asked to rate their relatedness to presented factors during the peak time of COVID-19, ranging from 1 (strongly disagree) to 5 (strongly agree). Cronbach’s α for psychological distress was 0.959 in the present study.
2.3. Data Analysis
We used SPSS 19.0 (IBM Corp., Armonk, N.Y., USA) to provide descriptive analyses of the variables, including the means, standard deviations, and Pearson correlations. Mplus 7.1 was used to examine the hypothetical model. We used maximum likelihood (ML) to handle the missing data. We used chi-square values (χ 2 ), the comparative fit index (CFI), the Tucker– Lewis fit index (TLI), the root-mean-square error of approximation (RMSEA), and the standardized root-mean-square residual (SRMR) to evaluate the models. In general, an acceptable model fit is indicated by CFI and TLI greater than 0.9 and RMSEA and SRMR less than 0.08.
3.1. Descriptive Statistics and Correlations
This study is all subjective self-reported data. To the validity of the results, we conducted a common method bias test. Harman’s single factor test result showed that the model fit was: χ 2 = 4275.297, CFI = 0.614, TLI = 0.583, RMSEA = 0.000, SRMR = 0.128. This model was unsatisfactory. Thus, this study did not have serious common method bias. We provide the means, standard deviations, and correlation coefficient in Table 1 . Three coping styles, perceived stress, and psychological distress were correlated with each other (r ranging from 0.093 to 0.595). Problem-focused coping was positively correlated with perceived stress and psychological distress. Adaptive emotion-focused coping was negatively correlated with perceived stress and psychological distress. Maladaptive emotion-focused coping was positively correlated with perceived stress and psychological distress.
Means, Standard Deviations, and Correlations Among the Variables.
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| 1 Gender | – | – | – | ||||||
| 2 Age | 19.51 | 1.52 | 0.244 *** | – | |||||
| 3 Problem-focused Coping | 3.19 | 0.76 | −0.050 | −0.046 | – | ||||
| 4 Adaptive Emotion-focused Coping | 2.76 | 0.53 | 0.062 | 0.011 | 0.581 *** | – | |||
| 5 Maladaptive Emotion-focused Coping | 1.84 | 0.65 | −0.161 *** | 0.005 | 0.324 *** | −0.028 | – | ||
| 6 Perceived Stress | 2.07 | 0.73 | 0.081 | 0.056 | 0.154 ** | −0.131 ** | 0.376 *** | – | |
| 7 Psychological Distress | 1.99 | 0.84 | −0.044 | 0.014 | 0.101 * | −0.185 *** | 0.467 *** | 0.595 *** | – |
Note. Gender (1 = male, 2 = female). * p < 0.05. ** p < 0.01. *** p < 0.001. M = Means; SD = Standard Deviations.
3.2. Examination of the Mediation Model
A multiple model (see Figure 1 ) with the three coping styles as independent variables, perceived stress as the mediator, and psychological distress as the dependent variable was established. The SEM results of the mediation model showed an acceptable model fit: χ 2 /df = 3.337, CFI = 0.923, TLI = 0.913, RMSEA = 0.069, SRMR = 0.077. As shown in Figure 1 , maladaptive emotion-focused coping directly and significantly predicted psychological distress. Maladaptive emotion-focused coping positively predicted perceived stress, which in turn positively predicted psychological distress. Similarly, problem-focused coping positively predicted perceived stress, which in turn positively predicted psychological distress. In addition, adaptive emotion-focused coping negatively predicted perceived stress, which in turn positively predicted psychological distress. More importantly, problem-focused coping and adaptive emotion-focused coping did not directly predict psychological distress. The results indicated a full mediation model: problem-focused coping and adaptive emotion-focused coping affected psychological distress entirely through the mediation path.

Mediation model of the association between different coping styles and psychological distress. Note: all the loadings on latent variables were significant ( p < 0.001). *** p < 0.001. Pro = Problem-focused; Ada = Adaptive Emotion-focused Coping; Mal = Maladaptive Emotion-focused Coping; Per = Perceived Stress; Psy = Psychological Distress.
To further examine whether the indirect effects were significant, we used bias-corrected bootstrap tests derived from 1000 samples. As shown in Table 2 , maladaptive emotion-focused coping positively predicted psychological distress, while problem-focused coping and adaptive emotion-focused coping did not predict psychological distress. Perceived stress significantly mediated the association between the three coping styles—problem-focused coping, adaptive emotion-focused coping and maladaptive emotion-focused coping—and psychological distress.
Bias-corrected bootstrap tests on direct and indirect effects.
| Path | Standardized | 95% CI | |
|---|---|---|---|
| (β) | Low | High | |
| Problem-focused Coping → Psychological Distress | 0.069 | −0.196 | 0.035 |
| Problem-focused Coping → Perceived Stress → Psychological Distress | 0.135 | 0.056 | 0.229 |
| Adaptive Emotion-focused Coping → Psychological Distress | −0.143 | −0.405 | 0.077 |
| Adaptive Emotion-focused Coping → Perceived Stress → Psychological Distress | −0.142 | −0.240 | −0.043 |
| Maladaptive Emotion-focused Coping → Psychological Distress | 0.319 | 0.201 | 0.438 |
| Maladaptive Emotion-focused Coping → Perceived Stress → Psychological Distress | 0.161 | 0.098 | 0.223 |
4. Discussion
Although previous studies examined the relations between coping styles, psychological distress, and perceived stress in the public, this study examined such relations in the context of the COVID-19 pandemic in Chinese college students in the country where the first case of COVID-19 was officially reported. First, the results showed that three coping styles were all significantly correlated with psychological distress in Chinese college students during the early stage of the COVID-19 pandemic. Adaptive emotion-focused coping was negatively associated with perceived stress and psychological distress. Maladaptive emotion-focused coping was positively associated with perceived stress and distress. These findings concur with those of Kumanova and Karastoyanov [ 16 ], suggesting that individuals who use specific reactive emotion-focused coping strategies more often, such as focusing on emotions, denial, seeking emotional social support, and disengaging, experience more stress.
Second, perceived stress significantly mediated the association between problem-focused, adaptive emotion-focused, and maladaptive emotion-focused coping and psychological distress. According to Lazarus and Folkman [ 9 ], perceived stress is associated with many psychological factors such as one’s feelings about the unpredictability and uncontrollability of a specific life circumstance, such as the COVID-19 outbreak, and confidence in their abilities to problem solve and cope with the difficulties. Research has suggested that perceived stress can be associated with self-efficacy (i.e., belief about one’s capacities to execute behaviors to achieve certain performance attainments) [ 24 , 32 ]. Previous studies have suggested that individuals who perceived a stressful situation as an opportunity or challenge to prove their abilities tended to utilize their coping skills more effectively and be less likely to have negative thoughts [ 25 , 26 ]. Although the COVID-19 pandemic has had an unprecedented impact on the public, individuals are likely to perceive and interpret the presented situations differently and utilize coping strategies differently, which might contribute to different levels of psychological distress.
Third, problem-focused and adaptive emotion-focused coping affected psychological distress entirely through the mediation path. The findings of the current study suggest that problem-focused and adaptive emotion-focused coping did not directly predict psychological distress. The impacts of problem-focused and adaptive emotion-focused coping on psychological distress were through the mediation role of perceived stress in this study. The associated consequences and effects of the COVID-19 pandemic continue to pose a major challenge to the public. Preventive measures and social distancing requirements have been developed and mandated to contain the spread of the virus and are still ongoing in specific regions [ 33 ]. College students have faced a number of challenges, such as sudden closures of university dormitories, cancellation of all in-person instruction and field placements (e.g., practicums and internships), the loss of off-campus jobs that require in-person contact, lack of in-person social support from peers and instructors, and a dramatic reduction in outdoor physical activities [ 34 ]. According to Lazarus [ 35 ], perceived stress is experienced subjectively by an individual, who might identify an imbalance between the demands placed on them and the available resources to deal such demands. While the rapidly changing societal situations associated with COVID-19 may have appeared to be uncontrollable to some participants, others might have perceived the situation differently, and thus might have subjectively experienced different levels of psychological distress. The findings suggest that mental health providers might want to target strategies and resources that could alleviate perceived stress in the individuals when an uncontrollable pandemic such as the COVID-19 occurs. In other words, individuals might not be able to change the external environment in the context of COVID-19 pandemic, but subjectively changing one’s perception and interpretation of a stressful event might help reduce perceived stress.
The literature has linked exposure to acute stress to both short-term or long-term physical and psychological disorders. Cannon [ 36 ] outlined that the human body copes with acute stressors by utilizing emotional and motivational systems. When encountering stressful situations, the human body’s sympathetic nervous system initiates the “fight or flight response,” such as faster heart rate, rapid breathing rate, and excessive sweating. In turn, the parasympathetic responses are diminished to cope with the stressor. Over time, the human body might become exhausted, and such response eventually leads to physical burnout and psychological distress. According to Melamed et al. [ 37 ], when an individual is emotionally exhausted and does not have the resources to cope with encountered stressors, psychological burnout and distress might occur. Thus, perceived stress experienced by an individual might directly dictate the pervasiveness and severity of the psychological distress of the individual.
Fourth, different coping styles appear to have differentiated impacts on mental health. Based on the transactional theory, stress can be viewed as an interactive process between the stressors, such as environmental circumstances that negatively affects one’s well-being, and one’s psychological responses, such as appraisal, adjustment, and coping [ 9 ]. Based on Lazarus and Folkman (1984), one coping strategy is emotion-focused coping. In the present study, maladaptive emotion-focused coping (e.g., refusal, avoidance, escape, use of alcohol) was separated from adaptive emotion-focused coping (e.g., accepting the reality, or looking for positive aspects in life challenges). Maladaptive emotion-focused coping could lead to passive or avoidant coping. In a stressful situation, it is common that individuals resort to avoidant coping in order to reduce the emotional stress elicited by a challenging situation, rather than directly problem solving and handling the stress at the source [ 38 ]. In a situation where individuals feel that they have little control over the situation, they tend to default to avoidant coping [ 39 ]. In the current study, maladaptive emotion-focused coping positively predicted perceived stress, which in turn positively predicted psychological distress. This finding was consistent with Compas et al. [ 40 ], who suggested that maladaptive emotion-focused coping, such as avoidance coping, has been associated with higher levels of psychological distress and more depressive symptoms. In the current study, adaptive emotion-focused coping negatively predicted perceived stress, which in turn positively predicted psychological distress. This finding suggested that the use of positive emotion-focused coping, such as reappraisal and assigning positive meaning to ordinary events, might help buffer against depressed mood [ 41 ] and acute stress [ 42 ]. In other words, when the external event is uncontrollable such as the COVID-19 pandemic, one could resort to focusing on positive aspects of one’s emotion in order to reduce perceived stress, leading to lower level of psychological distress.
In general, active problem-focused coping has been related to lower psychological distress [ 40 , 43 ]. Surprisingly, problem-focused coping in the present study positively predicted perceived stress, which in turn positively predicted psychological stress. Given the unprecedented severity and pervasiveness of the impact of the COVID-19 pandemic, most individuals have never encountered such a global event. Even when individuals attempt problem-solving approaches, they have little control over the rapidly changing situations related to the COVID-19, such as public health policy changes, school closures, losing a job due to business closure, having no access to public facilities, and staying in an isolated environment for a prolonged period due to quarantine policy. During the COVID-19 pandemic, even when individuals engage in active coping and problem solving, they cannot change the global situation, and infection rates in different regions continue to fluctuate. It is plausible that the more individuals actively engage in problem solving related to COVID-19, the more they ruminate and worry about the situation, leading to higher levels of perceived stress and higher levels of reported psychological distress. Gan and colleagues [ 44 ] examined coping strategies by college students in response to SARS-related stressors. The results showed that participants reported using more avoidant coping with SARS-related stressors that, like COVID-19, were uncontrollable. Such findings suggest that individuals’ coping styles during an unprecedented and sudden COVID-19 pandemic might be different from their coping styles during a typical circumstance, and such difference warrants a differential examination.
There are several limitations of this study that should be noted. First, the study was based on self-reported questionnaires, which might produce potential biases, although our factor analysis results did not indicate a serious common method bias. Second, we recruited undergraduate students exclusively from two universities in Beijing. It is likely that those who responded to the survey were the individuals who wanted to have a voice and were interested in such a research topic. These college students represented highly educated young people in a metropolitan area in China where the societal and public health resources are relatively abundant. Because of this sampling, the findings of this study might not be generalizable to a population with lower educational attainment and more vulnerable occupational status, or to those in other geographical areas. Third, the survey was conducted fully online. Researchers were unable to reach individuals who might not have had internet access during the early stages of the COVID-19 outbreak; such individuals might have been more vulnerable, and might have perceived higher levels of stress associated with COVID-19. Fourth, the present study only focused on the relations between psychological distress, perceived stress, and three types of coping. There might other factors such as subclinical symptoms and emotional difficulties that might affect students’ self-reporting. Such factors should be further explored in future studies.
Future researchers are encouraged to examine a more general population in more diverse regions to capture perceived stress and psychological distress in individuals with different levels of educational attainment, different occupational statuses, and in different regions. Future researchers should consider other measures that could better reflect perceived stress and psychological distress in addition to self-reported questionnaires.
5. Conclusions
The present study was to explore the impact of different coping styles on psychological distress during the COVID-19 outbreak among college students in China. The problem-focused and maladaptive emotion-focused coping styles were positively correlated with perceived stress and psychological distress. The maladaptive emotion-focused coping style was negatively correlated with perceived stress and psychological distress. It appears that adaptive, emotion-focused coping could alleviate the mental discomfort associated with the COVID-19 pandemic. The mediating role of perceived stress between the associations of three coping styles and psychological distress found that problem-focused coping and adaptive emotion-focused coping affected psychological distress entirely through the mediation path, in which perceived stress was the mediator. Perceived stress partially mediated the association between maladaptive emotion-focused coping and psychological distress. The findings underscore the importance of perceived stress and provide insights for future intervention. Our findings suggest that mental health service providers might consider providing strategies to help clients reduce their perceived stress. During uncontrollable public health emergencies, strategies and resources that could alleviate one’s perceived stress appear to buffer psychological distress.
Author Contributions
Conceptualization of ideas, Y.D. and X.F.; methodology, X.F.; use of software, X.F.; validation, Y.D., X.F. and R.L.; data analysis, X.F.; implementation of the survey, X.F. and W.H.; funding resources, R.L.; data curation, X.F.; writing—original manuscript draft preparation, Y.D.; writing—editing and revising, J.H.; visualization, Y.D.; supervision, J.W.; project management, R.L.; funding acquisition, R.L. All authors have read and agreed to the published version of the manuscript.
We thank the funding support from the National Social Science Fund of China, grant number 17BSH102 (awarded to Rude Liu).
Institutional Review Board Statement
This project was approved by the Academic Ethics Committee at Beijing Normal University (approval date: 3 December 2017).
Informed Consent Statement
Subjects involved in the study filled out the informed consent.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Follow U of T News
Some stress-management strategies could pose physical health risks during COVID-19: U of T study

Published: July 14, 2021
By Don Campbell
“Keep Calm and Carry On” may not be the best mantra when it comes to managing stress in the context of COVID-19.
A new study by University of Toronto researchers finds that cognitive reappraisal, a common strategy used to manage the stress of a health threat, may end up creating a greater risk to public health during the pandemic.
To help manage stress, people often employ the coping strategy to lower fear and worry by re-interpreting the situation at hand.

“When you’re feeling stressed about your health, you may try to make yourself think about the situation in a way that helps you stay calm,” says Brett Ford , assistant professor in the department of psychology at U of T Scarborough and one of the study’s authors.
“But there appears to be a trade-off. Those who use coping strategies to deal with a health threat – in this case from COVID-19 – may end up jeopardizing health behaviours.”
While reappraisal can take many forms, in the context of COVID-19, it could mean thinking the pandemic isn’t a big deal – or that it’s a blip that will soon blow over.
“In many circumstances, reappraisal is a valuable tool to help with our mental health,” says Angela Smith , PhD student and lead author of the study. “However, the consequences of using it in the face of a pandemic may result in downplaying the vital importance of taking the necessary health precautions.”
In the study, published in the journal Psychological Science , Smith, Ford and their co-authors used data from two separate surveys taken over a period of three months beginning as the pandemic hit in February 2020. They found that people who successfully reduced fear in the face of COVID-19 were mentally healthier, but less likely to follow public health recommendations such as wearing a mask or social distancing.
“Fear motivates us to take actions that protect our physical health, which is really important during a pandemic – not only for individuals, but also from a community-health perspective,” Ford says.
Ford adds that we are trained to use whatever tools we have available to manage stress, but there’s also the need to understand the downstream consequences of using these tools, especially in the face of a community health threat like COVID-19.
What it also suggests is that health messages aimed at reducing fear, such as “Keep Calm and Carry On,” may actually backfire and promote fewer health behaviours.
“Seeking comfort during times of stress – when comfort is most needed – can pose a challenging dilemma when you need to also prioritize physical health,” says Ford, an expert on the health implications of how people think about and manage their emotions.
The research, which received funding from the Social Sciences and Humanities Research Council of Canada (SSHRC) and a U of T COVID-19 Student Engagement award, did uncover possible alternatives to the drawbacks of using reappraisal to avoid fear. The researchers say that, in the face of COVID-19, people can use reappraisal to cultivate socially-oriented positive emotions such as love, gratitude, compassion or admiration.
“The emotions we feel when we’re feeling good about others, such as having gratitude towards frontline workers, actually provides emotional comfort without jeopardizing behaviours such as social distancing,” says Smith.
“We’re excited about these findings because there are forms of emotion regulation people can use to manage the stress of the pandemic that don’t come at the cost of these vital protective health behaviours.”
As for why these emotions are effective, Smith says it may come down to providing a source of connection to others who are in a tough situation.
“It is undeniable that people are experiencing worry and anxiety as part of this pandemic. We can’t subtract that negativity out of the situation, but we can add some positivity to it – some compassion, some gratitude,” she says.
“By doing this we protect both ourselves and our communities.”
Share this page


Subscribe to The Bulletin Brief
More u of t news.


7 Ways to Manage Stress During the Coronavirus Pandemic
Taking it easy when it feels like the world is on fire..
Posted March 20, 2020 | Reviewed by Ekua Hagan
- What Is Stress?
- Take our Burnout Test
- Find a therapist to overcome stress

As I write this, I am sitting in the living room of an apartment I rented on Airbnb in Nashville, Tennessee. Two weeks ago, my family and I were here for a tango marathon when dancers from across the country flocked to the Music City for a weekend of good times, southern charm, and the warm embrace of Argentine tango. We made new friends, caught up with old ones, and left with nothing but fond memories. When we arrived at our next destination, we learned that just after we left, tornadoes ripped through Nashville and other parts of Tennessee, devastating the city we love and had enjoyed so much. A lot can happen in a day.
The coronavirus was on the news and definitely a topic of conversation, but most of the people we talked to felt optimistic . Two weeks later, and it seems to be all anyone can think about. The stores are empty, stripped clean of essential items like toilet paper and milk, and the bars and restaurants that help make this city so much fun are closed. Face masks are common, and every cough or sneeze causes momentary panic. In other countries, and even in other cities and states, citizens have been ordered to remain in their homes, and all large gatherings of people have been canceled. A lot can happen in a couple of weeks.
We are back in Nashville because of our own cancelations. My partner Sarah is a tango dancer, and I am a touring public speaker, and both of us are self-employed. We were on our way to Memphis for a series of speaking gigs when we started receiving the notifications, one after another after another until our entire tour had been canceled. We live on the road as we work, so a canceled tour also means we need to find somewhere to call home for a bit. Being just a couple of hours shy of Nashville, we decided to hole up here for a few days and plan our next steps.
To say our situation is stressful is an understatement. There are a lot of people who have it worse, but we have lost all our income for the next three months, our housing, and we have a little girl to consider as well. It is a tough spot, and yet both of us are in relatively good spirits. Neither of us has dealt with anything like this before, but we both handle stress well and remain optimistic, even when the global situation seems to get worse and worse. How do we do it?
Drugs. Lots and lots of drugs.
I am joking, of course. Sarah and I are both highly resilient people. In fact, the canceled tour was about stress management , a subject that I have been speaking to audiences about for years. I even wrote a book on the subject, The Art of Taking It Easy , and have been putting those skills to practice all my life. Sarah puts her own stress management skills to test every day by having to deal with me.
The coronavirus pandemic, and the reaction to it, may seem as if the world is on fire. Granted, I have never seen anything like this in my lifetime (which probably overlaps significantly with your lifetime), so it might be on a larger scale, but it is still just another source of stress in a long line of things that cause stress. Stress is stress regardless of the source, and the tools to manage it are the same. Allow me to share a few here.
Before I do, please note that I am discussing how we can manage our stress, anxiety , or worrisome reactions to the pandemic, not the coronavirus itself. Also, if you have been personally affected by the coronavirus, I wish you or your loved ones a healthy recovery. My goal here is to help most of us stay calm or, as I like to put it, take it easy.
1. Assess your threat level. When overwhelmed with worry or fear , it is sometimes helpful to inform yourself of the facts to assess your personal level of threat. For example, earlier in the month, I had a moment of concern and looked up the infection statistics at the time. There were about 120,000 people known to have the virus out of the nearly 8 billion people that live on this planet. Also, most of those cases were in China while my feet were planted firmly in the United States.
Digging even deeper, I found that there were only seven cases in my state and none of them in my area. I assessed my threat level as low and slept easily that night. Now, you might say, “But, Brian, what about all those people that could be spreading the virus without knowing it?” to which I’d answer that I am trying to reduce anxiety, not add to it. Once you have assessed your threat, then it is important to…

2. Identify what you can control. When we encounter stress, any stress, it is important that we ask ourselves if we can do anything about it. If there is some action we can take, then taking that action will help reduce our anxiety. For example, experts emphasize the importance of handwashing to minimize the spread of the virus. Most of us are capable of washing our hands, so wash your damn hands more often than you do.
If the experts say avoid crowded areas, then avoid crowded areas, and live with the comfort of knowing that you are doing all you can to reduce your exposure. However, what if, after a couple of weeks of social isolation , you’ve become a handwashing obsessed hermit, and you still feel anxious? Well…
3. Accept what you cannot control. Focus on what you can do, not what you can’t. There are always going to be variables that are out of your control, and that is part of what makes viruses so frightening. We can never know whether we have been in contact. We can’t control our government’s attempts at containment. We can’t control the loss of income we have experienced or the circumstances that put us back in Nashville.
Sometimes, the healthiest thing we can do is accept that there is nothing we can do. Worrying, complaining, ruminating, and wishing things were different are thoughts we will entertain, but if we focus on them too much, they’ll amplify our stress. Regarding all sorts of stress, I ask people all the time: If there is nothing you can do about it, why are you worried about it? Worrying does nothing but make the problem worse. If you are doing all you can and find that you are still overly focused on things that are outside of your control, you may want to try…
4. Actively changing negative thoughts. Did you know that the only part of your brain you have direct, voluntary control over is the part you think with? If you didn’t, that should be really great news, because it is those very thoughts that are contributing to the anxiety you may be feeling during this pandemic.
What we think influences how we feel, and I often tell people if they don’t like the way they feel to change their thoughts. So, if your brain is too frequently occupied by worries about the virus, anger about social distancing, or sorrow over lost income, then change those thoughts. Simply redirect your attention to a new subject whenever needed. Any new stimulus or activity will help change our thoughts. For example, we could listen to music, do the dishes, read a book, go for a walk, literally anything we can do will help change the channel in our head. This brings me to…
5. Staying active. One thing great about this pandemic is that it is happening during the age of the internet. We may be isolating ourselves physically, but we have an amazing opportunity to connect with others virtually.
Over the last few weeks, I have seen some incredible coping strategies as people in quarantine zones are doing what they can to stay active. I’ve seen videos of opera singers in Italy serenading their neighbors from the windows. There are tango dancers that formed the group “I’m not dancing the tango, so I am doing this instead” to share new hobbies, crafts, and other goofy pursuits. There are people who have started working out or learning to cook.
Painting, making music, or creating art, in general, can be very helpful. A lot of people I know are using this time to catch up on their reading list, and if that sounds appealing, I know a book that would make a great addition to that list. Staying active is great, but we can also work on…
6. Positive thinking . Remember earlier when I mentioned the only part of your brain you have voluntary control over is the part you think with? Another thing worth noting is that you can only hold a few thoughts in mind at any given time. So, if you are having positive, optimistic thoughts, there isn’t much room left for dwelling on negativity.
Monty Python once sang “Always Look on the Bright Side of Life,” and while it may have been played for laughs, but there is truth there. Positive thinking and optimism help us pull through. Not to sound like a blind optimist, but things will absolutely get better. And, speaking of playing things for laughs, don't forget about…
7. Humor . My seminars on stress management are popular because I use a lot of humor in my presentations. In fact, humor is a natural stress-management tool. Coping with and minimizing stress is what humor is for. Laughter relieves anxiety, lowers stress hormones , and helps us to calm down. I can’t tell you how to find humor in your situation, but as much as we can, we need to laugh and just take it easy.
So, work from home if you can, avoid crowds, wash your hands, and try to keep your mind off of the negativity as we all wait this one out. As for us, in the morning, we will be packing up and making our way to stay with family for the next month or so. I don’t know when or if we will be able to tour again, but I am sure we will be OK. Today we hung out with our friend Shawn, who lives in Nashville. Keeping with the protocol of social distancing, Sarah and I refused to talk to him.

Brian King, Ph.D. , trained as a neuroscientist and psychologist and travels the world as a comedian and public speaker. he is the author of The Art of Taking It Easy and The Laughing Cure .
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Coping with Stress
Many of us are facing challenges that can be stressful and overwhelming. Learning to cope with stress in a healthy way will help you, the people you care about, and those around you become more resilient.
Stress can cause the following:
- Feelings of fear, anger, sadness, worry, numbness, or frustration.
- Changes in appetite, energy, desires, and interests.
- Trouble concentrating and making decisions.
- Nightmares or problems sleeping.
- Physical reactions, such as headaches, body pains, stomach problems, or skin rashes.
- Worsening of chronic health problems and mental health conditions.
- Increased use of alcohol , illegal drugs (like heroin , cocaine , or methamphetamine ), and misuse of prescription drugs (like opioids).
- Healthy Ways to Cope with Stress
- If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org
- Disaster Distress Helpline : CALL or TEXT 1-800-985-5990 (press 2 for Spanish)

Here are some ways you can manage stress, anxiety, grief, or worry:
- Take breaks from news stories, including those on social media. It’s good to be informed, but constant information about negative events can be upsetting. Consider limiting news to just a couple times a day and disconnecting from phone, TV, and computer screens for a while.
- Eat healthy. Have fruits and vegetables, lean protein, whole grains, and low-fat or no-fat dairy. Limit foods with unhealthy fats, salt, and added sugars. See Healthy Eating Tips .
- Get enough sleep. Go to bed and wake up at the same time each day to help you sleep better . Adults need 7 or more hours per night.
- Move more and sit less. Every little bit of physical activity helps. Start small and build up to 2 ½ hours a week. You can break it into smaller amounts such as 20 to 30 minutes a day.
- Limit alcohol intake. Choose not to drink, or drink in moderation on days you drink alcohol. Moderation means having 2 drinks or less a day for men or 1 drink or less for women. Find out more at Drink Less, Be Your Best .
- Avoid using illegal drugs or prescription drugs in ways other than prescribed. Don’t take someone else’s prescription. Substance use treatment is available, and recovery starts with asking for help.
- Avoid smoking , vaping, and the use of other tobacco products. People can and do quit smoking for good.
- Continue with regular health appointments, tests, screenings, and vaccinations.
- Take deep breaths, stretch, or meditate .
- Try to do some other activities you enjoy.
- Talk with people you trust about your concerns and how you are feeling.
- Connect with your community-based or faith-based organizations.
For Everyone
- How Right Now — Finding What Helps
- Coping with a Disaster or Traumatic Event
- Suicide Prevention
- I’m So Stressed Out! Fact Sheet (NIMH)
- Mindfulness Coach – PTSD: National Center for PTSD (va.gov)
For Families and Children
- Helping Children Cope with Emergencies
- Adolescent Mental Health
- Tools for Supporting Emotional Wellbeing in Children and Youth
- Open access
- Published: 28 March 2024
Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support
- Helen M West ORCID: orcid.org/0000-0001-8712-5890 1 ,
- Luke Flain ORCID: orcid.org/0000-0001-7296-6304 2 ,
- Rowan M Davies 3 , 4 ,
- Benjamin Shelley 3 , 5 &
- Oscar T Edginton ORCID: orcid.org/0000-0001-5298-9402 3 , 6
BMC Psychology volume 12 , Article number: 179 ( 2024 ) Cite this article
1016 Accesses
2 Citations
Metrics details
A Publisher Correction to this article was published on 26 June 2024
This article has been updated
Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the ‘coping reservoir’ model of wellbeing.
In synchronous interactive pre-recorded webinars, 78 fourth-year medical students in the UK responded to reflective prompts. Participants wrote open-text comments on a Padlet site. Responses were analysed using reflexive thematic analysis.
Analysis identified five themes. COVID-19 exacerbated academic pressures, while reducing the strategies available to cope with stress. Relational connections with family and friends were affected by the pandemic, leading to isolation and reliance on housemates for informal support. Relationships with patients were adversely affected by masks and telephone consultations, however attending placement was protective for some students’ wellbeing. Experiences of formal support were generally positive, but some students experienced attitudinal and practical barriers.
Conclusions
This study used a novel methodology to elicit medical students’ reflections on their mental wellbeing during COVID-19. Our findings reinforce and extend the ‘coping reservoir’ model, increasing our understanding of factors that contribute to resilience or burnout. Many stressors that medical students typically face were exacerbated during COVID-19, and their access to coping strategies and support were restricted. The changes to relationships with family, friends, patients, and staff resulted in reduced support and isolation. Recognising the importance of relational connections upon medical students’ mental wellbeing can inform future support.
Peer Review reports
Medical students are known to experience high levels of stress, anxiety, depression and burnout due to the nature, intensity and length of their course [ 1 ]. Medical students are apprehensive about seeking support for their mental wellbeing due to perceived stigma and concerns about facing fitness to practise proceedings [ 2 ], increasing their vulnerability to poor mental health.
Research has identified that the stressors medical students experience include a demanding workload, maintaining work–life balance, relationships, personal life events, pressure to succeed, finances, administrative issues, career uncertainty, pressure around assessments, ethical concerns, and exposure to patient death [ 3 , 4 ]. In March 2020, the COVID-19 pandemic introduced additional stressors into medical students’ lives. These included sudden alterations to clinical placements, the delivery of online teaching, uncertainty around exams and progression, ambiguity regarding adequate Personal Protective Equipment (PPE), fear of infection, and increased exposure to death and dying [ 5 , 6 ]. Systematic reviews have reported elevated levels of anxiety, depression and stress among medical students during COVID-19 [ 7 ] and that the prevalence of depression and anxiety during COVID-19 was higher among medical students than in the general population or healthcare workers [ 8 ].
While training, medical students are expected to develop awareness of personal mental wellbeing and learn healthy coping strategies for dealing with stress [ 9 ]. Developing adaptive methods of self-care and stress reduction is beneficial both while studying medicine, and in a doctor’s future career. Protecting and promoting psychological wellbeing has the potential to improve medical students’ academic attainment, as well as their physical and mental wellbeing [ 10 ], and it is therefore important for medical educators to consider how mental wellbeing is fostered. Feeling emotionally supported while at medical school reduces the risk of psychological distress and burnout, and is related to whether students contemplate dropping out of medical training [ 11 ]. In their systematic narrative review of support systems for medical students during COVID-19, Ardekani et al. [ 12 ] propose a framework incorporating four levels: policies that promote a supportive culture and environment, active support for students at higher risk of mental health problems, screening for support needs, and provision for students wishing to access support. This emphasis on preventative strategies aligns with discussions of trauma-informed approaches to medical education, which aim to support student learning and prevent harm to mental wellbeing [ 13 ]. Dunn et al. [ 14 ] proposed a ‘coping reservoir’ model to conceptualise the factors that deplete and restore medical students’ mental wellbeing (Fig. 1 ). This reservoir is drained and filled repeatedly, as a student faces demands for their time, energy, and cognitive and emotional resources. This dynamic process leads to positive or negative outcomes such as resilience or burnout.
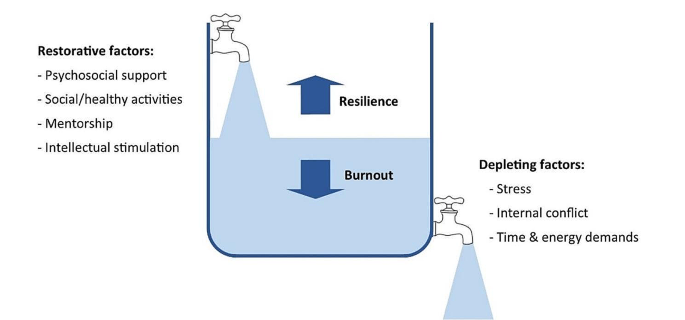
Coping reservoir model– adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
At present we have limited evidence to indicate why medical students’ mental wellbeing was so profoundly affected by COVID-19 and whether students developed coping strategies that enhanced their resilience, as suggested by Kelly et al. [ 15 ]. This study therefore sought to conceptualise the challenges medical students experienced during COVID-19, the coping strategies they developed in response to these stressors, and the supportive measures they valued. The ‘coping reservoir’ model [ 14 ] was chosen as the conceptual framework for this study because it includes both restorative and depleting influences. Understanding the factors that mediate medical students’ mental wellbeing will enable the development of interventions and support that are effective during crises such as the pandemic and more generally.
Methodology
This research study is based on a critical realist paradigm, recognising that our experience of reality is socially located [ 16 ]. Participant responses were understood to represent a shared understanding of that reality, acknowledging the social constructivist position that subjective meanings are formed through social norms and interactions with others, including while participating in this study. It also draws on hermeneutic phenomenology in aiming to interpret everyday experienced meanings for medical students during COVID-19 [ 17 ]. The use of an e-learning environment demonstrates an application of connectivism [ 18 ], a learning theory in which students participate in technological enabled networks. We recognise that meaning is co-constructed by the webinar content, prompts, ‘coping reservoir’ framework and through the process of analysis.
The multidisciplinary research team included a psychologist working in medical education, two medical students, and two Foundation level doctors. The team’s direct experience of the phenomenon studied was an important resource throughout the research process, and the researchers regularly reflected on how their subjective experiences and beliefs informed their interpretation of the data. Reflexive thematic analysis was chosen because it provides access to a socially contextualised reality, encompasses both deductive and inductive orientations so that analysis could be informed by the ‘coping reservoir’ while also generating unanticipated insights, and enables actionable outcomes to be produced [ 19 ].
Ethical approval
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365).
Participants
Fourth-year medical students at the University of Liverpool were invited to participate in the study during an online webinar in their Palliative Medicine placement. During six webinars between November 2020 and June 2021, 78 out of 113 eligible students participated, giving a response rate of 69%. This was a convenience sample of medical students who had a timetabled session on mental wellbeing. At the time, these medical students were attending clinical placements, however COVID-19 measures in the United Kingdom meant that academic teaching and support was conducted online, travel was limited, and contact with family and friends was restricted.
Students were informed about the study prior to the synchronous interactive pre-recorded webinar and had an opportunity to ask questions. Those who consented to participate accessed a Padlet ( www.padlet.com ) site during the webinar that provided teaching on mental wellbeing, self-care and resilience in the context of palliative medicine. Padlet is a collaborative online platform that hosts customisable virtual bulletin boards. During this recording, participants were asked to write anonymous open-text responses to reflective prompts developed from reviewing the literature (Appendix 1 ), and post these on Padlet. The Padlet board contained an Introduction to the webinar, sections for each prompt, links to references, and signposting to relevant support services. Data files were downloaded to Excel and stored securely, in line with the University of Liverpool Research Data Management Policy.
The research team used the six steps of reflexive thematic analysis to analyse the dataset. This process is described in Table 1 , and the four criteria for trustworthiness in qualitative research proposed by Lincoln and Guba [ 20 ] are outlined in Table 2 . We have used the purposeful approach to reporting thematic analysis recommended by Nowell et al. [ 21 ] and SRQR reporting standards [ 22 ] (Appendix 2 ).
Five themes were identified from the analysis:
COVID-19 exacerbated academic pressures.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress.
COVID-19 changed relationships with family and friends, which affected mental wellbeing.
COVID-19 changed interactions with patients, with positive and negative effects.
Formal support was valued but seeking it was perceived as more difficult during COVID-19.
COVID-19 exacerbated academic pressures
‘Every day feels the same, it’s hard to find motivation to do anything.’
Many participants reported feeling under chronic academic pressure due to studying medicine. Specific stressors reported were exams, revision, deadlines, workload, specific course requirements, timetables, online learning, placement, and communication from University. Some participants also reported negative effects on their mental wellbeing from feelings of comparison and competition, feeling unproductive, and overthinking.
Massive amounts of work load that feels unachievable.
COVID-19 exacerbated these academic stresses, with online learning and monotony identified as particularly draining. However, other students found online learning beneficial, due to reduced travelling.
I miss being able to see people face to face and zoom is becoming exhausting. My mental wellbeing hasn’t been great recently and I think the effects of the pandemic are slowly beginning to affect me.
I also prefer zoom as it is less tiring than travelling to campus/placement.
Clinical placements provided routine and social interaction. However, with few social interactions outside placement, this became monotonous. A reduction in other commitments helped some students to focus on their academic requirements.
‘Most social activity only taking place on placement has made every day feel the same’.
Some students placed high value on continuing to be productive and achieve academically despite the disruption of a pandemic, potentially to the detriment of their mental wellbeing. Time that felt unproductive was frustrating and draining.
‘Having a productive day i.e. going for a run and a good amount of work completed in the day’.
‘Unproductive days of revision or on placement’.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress
‘Everyone’s mental well-being decreased as things they used for mental health were no longer available’.
Students often found it difficult to sustain motivation for academic work without the respite of their usual restorative activities challenging.
‘Not being able to balance work and social life to the same extent makes you resent work and placement more’.
The competing demands medical students encounter for their time and energy were repeatedly reported by participants.
‘Sometimes having to go to placement + travel + study + look after myself is really tough to juggle!’
However, removing some of the boundaries around academic contact and structure of extracurricular activities heightened the impact of stressors. Many participants focused on organising and managing their time to cope with this. Students were aware that setting time aside for relaxation, enjoyment, creativity, and entertainment would be beneficial for their wellbeing.
‘Taking time off on the weekends to watch movies’.
However, they found it difficult to prioritise these without feeling guilty or believing they needed to ‘earn’ them, and academic commitments were prioritised over mental wellbeing.
‘Try to stop feeling guilty for doing something that isn’t medicine’. ‘Would like to say I’d do more to increase my mental wellbeing but finals are approaching and that will probably have to take priority for the next few months’.
Medical students were generally aware that multiple factors such as physical activity, time with loved ones, spiritual care, nourishment and hobbies had a positive impact on their mental wellbeing. During COVID-19, many of the coping strategies that students had previously found helpful were unavailable.
‘Initially it improved my mental well-being as I found time to care for myself, but with time I think everyone’s mental well-being decreased as things they used for mental health were no longer available e.g. gym, counselling, seeing friends’.
Participants adapted to use coping strategies that remained available during the pandemic. These included walks and time spent outdoors, exercise, journaling, reflection, nutrition, and sleep.
‘Running’. ‘Yoga’. ‘Fresh air and walks’.
A few students also reported that they tried to avoid unhelpful coping strategies, such as social media and alcohol.
‘Not reading the news, not using social media’.
‘Avoiding alcohol as it leads to poor sleep and time wasted’.
Many participants commented on increased loneliness, anxiety, low mood, frustration, and somatic symptoms.
‘Everyone is worn out and demotivated’. ‘Feel that as I am feeling low I don’t want to bring others down’. ‘Feel a lot more anxious than is normal and also easily annoyed and irritable.’
However, not all students reported that COVID-19 had a negative effect on wellbeing. A small minority responded that their wellbeing had improved in some way.
‘I think covid-19 has actually helped me become more self reliant in terms of well-being’.
COVID-19 changed relationships with family and friends, which affected mental wellbeing
‘Family are a huge support for me and I miss seeing them and the lack of human contact.’
Feeling emotionally supported by family and friends was important for medical students to maintain good mental wellbeing. However, COVID-19 predominantly had a negative impact on these relationships. Restrictions, such as being unable to socialise or travel during lockdowns, led to isolation and poor mental wellbeing.
‘Not being able to see friends or travel back home to see friends/family there’.
Participants frequently reported that spending too much time with people, feeling socially isolated, being unable to see people, or having negative social experiences had an adverse effect on their mental wellbeing. Relationships with housemates were a key source of support for some students. However, the increased intensity in housemate relationships caused tension in some cases, which had a particularly negative effect.
‘Much more difficult to have relationships with peers and began feeling very isolated’. ‘Talk about some of the experiences I’ve had on placement with my housemates’. ‘Added strain on my housemates to be the only ones to support me’.
Knowing that their peers were experiencing similar stressors helped to normalise common difficulties. The awareness that personal contacts were also struggling sometimes curtailed seeking informal support to avoid being a burden.
‘Actually discussing difficulties with friends has been most helpful, as it can sometimes feel like you’re the only one struggling, when actually most people are finding this year really difficult’. ‘Family and friends, but also don’t want to burden them as I know I can feel overwhelmed if people are always coming to me for negative conversations’.
COVID-19 changed interactions with patients, with positive and negative effects
‘With patients there has been limited contact and I miss speaking to patients.’
Some students reported positive effects on relationships with patients, and feeling a sense of purpose in talking to patients when their families were not allowed to visit. Medical students felt a moral responsibility to protect patients and other vulnerable people from infection, which contributed to a reduction in socialising even when not constrained by lockdown.
‘Talking to patients who can’t get visitors has actually made me feel more useful’. ‘Anxiety over giving COVID-19 to patients or elderly relatives’.
Students occasionally reported that wearing PPE made interactions with patients more challenging. Students’ contact with patients changed on some placements due to COVID-19, for example replacing in-person appointments with telephone consultations, and they found this challenging and disappointing.
‘Masks are an impediment to meaningful connections with new people’. ‘GP block when I saw no patients due to it all being on the telephone’.
Formal support was valued but seeking it was perceived as more difficult during COVID-19
‘Feel a burden on academic and clinical staff/in the way/annoying so tend to just keep to myself.’
Many participants emphasised the primary importance of support from family and friends, and their responses indicated that most had not sought formal support. While staff remained available and created opportunities for students to seek support, factors such as online learning and increased clinical workloads meant that some students found it harder to build supportive relationships with academic and placement staff and felt disconnected from them, which was detrimental for wellbeing and engagement.
‘Staff have been really helpful on placement but it was clear that in some cases, staff were overwhelmed with the workload created by COVID’. ‘Even though academic staff are available having to arrange meetings over zoom rather than face to face to discuss any problem is off putting’.
A few students described difficulty knowing what support was available, and identifying when they needed it.
‘It’s difficult to access support when you’re not sure what is available. Also you may feel your problems aren’t as serious as other people’s so hold off on seeking support’.
Formal support provided within the University included meetings with Academic Advisors, the School of Medicine wellbeing team, and University counselling service and mental health advisory team. It was also available from NHS services, such as GPs and psychological therapies. Those who had accessed formal support mostly described positive experiences with services. However, barriers to seeking formal support, such as perceived stigma, practicalities, waiting times for certain services, and concern that it may impact their future career were reported by some participants.
‘It is good that some services offer appointments that are after 5pm- this makes it more accessible to healthcare students’. ‘Had good experience with GPs about mental health personally’. ‘Admitting you need help or asking for help would make you look weak’. ‘Reassurance should be provided to medical students that accessing the wellbeing team is not detrimental to their degree. If anything it should be marketed as a professional and responsible thing to do’.
Some students preferred the convenience of remote access, others found phone or video impersonal and preferred in-person contact.
Students expressed that it was helpful when wellbeing support was integrated with academic systems, for example Academic Advisors or placement supervisors.
‘My CCT [primary-care led small group teaching] makes sure to ask how we are getting on and how our placements are going, so I think small groups of people with more contact with someone are more useful then large groups over zoom’. ‘Someone to speak to on palliative care placement, individual time with supervisor to check how we are doing (wellbeing, mental health) - would be a nice quick checkup’.
Participants typically felt able to share openly in an anonymous forum. Reading peers’ comments helped them to see that other students were having similar experiences and challenged unhealthy comparisons.
‘I definitely shared more than I would have done on a zoom call’. ‘I loved this session as it makes you feel like you’re not alone’. ‘Reassuring to know that there are others going through similar things as you’.
Our findings demonstrate that the COVID-19 pandemic exacerbated the stressors medical students experience, and removed some rewarding elements of learning, while reducing access to pre-existing coping strategies. The results support many aspects of the ‘coping reservoir’ framework [ 14 ]. Findings corroborate the restorative effects of psychosocial support and social/healthy activities such as sleep and physical activity, and the depletion of wellbeing due to time and energy demands, stress, and disruptions relating to the pandemic such as online teaching and limited social interaction. Feeling a sense of purpose, from continuing studying or interactions with patients for example, was restorative for wellbeing. Mentorship and intellectual stimulation were present in the responses, but received less attention than psychosocial support and social/healthy activities. Internal conflict is primarily characterised by Dunn et al. [ 14 ] as ambivalence about pursuing a career in medicine, which was not expressed by participants during the study. However, participants identified that their wellbeing was reduced by feeling unproductive and lacking purpose, feeling guilty about taking time for self-care, competing priorities, and comparison with peers, all of which could be described as forms of internal conflict. Different restorative and draining factors appeared to not be equally weighted by the participants responding to the prompts: some appear to be valued more highly, or rely on other needs being met. Possible explanations are that students may be less likely to find intellectual stimulation and mentorship beneficial if they are experiencing reduced social support or having difficulty sleeping, and internal conflict about pursuing a career in medicine might be overshadowed by more immediate concerns, for example about the pandemic. This prioritisation resembles the relationship between physiological and psychological needs being met and academic success [ 23 ], based on Maslow’s hierarchy of needs [ 24 ]. A revised ‘coping reservoir’ model is shown in Fig. 2 .
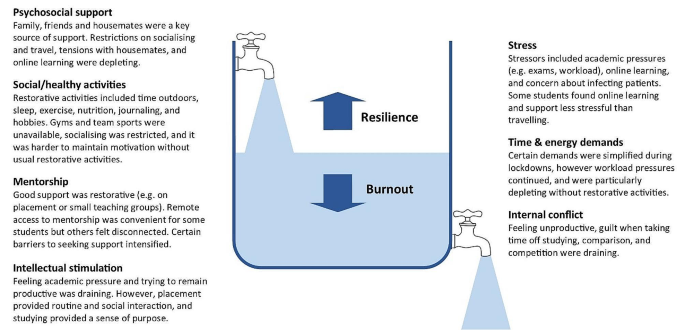
Coping reservoir model - the effects of COVID-19 on restorative and depleting factors for medical students, adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
Relational connections with family, friends, patients, and staff were protective factors for mental wellbeing. Feeling emotionally supported by family and friends is considered especially important for medical students to maintain good mental wellbeing [ 11 ]. These relationships usually mitigate the challenges of medical education [ 25 ], however they were fundamentally affected by the pandemic. Restrictions affecting support from family and friends, and changes to contact with patients on placement, had a negative effect on many participants’ mental wellbeing. Wellbeing support changed during the pandemic, with in-person support temporarily replaced by online consultations due to Government guidelines. Barriers to seeking formal support, such as perceived stigma, practicalities, and concern that it may impact their future career were reported by participants, reflecting previous research [ 26 ]. Despite initiatives to increase and publicise formal support, some students perceived that this was less available and accessible during COVID-19, due to online learning and awareness of the increased workload of clinicians, as described by Rich et al. [ 27 ]. These findings provide further support for the job demand-resources theory [ 28 , 29 ] where key relationships and support provide a protective buffer against the negative effects of challenging work.
In line with previous research, many participants reported feeling under chronic academic pressure while studying medicine [ 3 ]. Our findings indicate that medical students often continued to focus on achievement, productivity and competitiveness, despite the additional pressures of the pandemic. Remaining productive in their studies might have protected some students’ mental wellbeing by providing structure and purpose, however students’ responses primarily reflected the adverse effect this mindset had upon their wellbeing. Some students felt guilty taking time away from studying to relax, which contributes to burnout [ 30 ] , and explicitly prioritised academic achievement over their mental wellbeing.
Students were aware of the factors that have a positive impact on their mental wellbeing, such as physical activity, time with loved ones, spiritual care, nourishment and hobbies [ 31 ]. However, COVID-19 restrictions affected many replenishing factors, such as socialising, team sports, and gyms, and intensified draining factors, such as academic stressors. Students found ways to adapt to the removal of most coping strategies, for example doing home workouts instead of going to the gym, showing how they developed coping strategies that enhanced their resilience [ 15 ]. However, they found it more difficult to mitigate the effect of restrictions on relational connections with peers, patients and staff, and this appears to have had a particularly negative impact on mental wellbeing. While clinical placements provided helpful routine, social interaction and a sense of purpose, some students reported that having few social interactions outside placement became monotonous.
Our findings show that medical students often felt disconnected from peers and academic staff, and reported loneliness, isolation and decreased wellbeing during COVID-19. This corresponds with evidence that many medical students felt isolated [ 32 ], and students in general were at higher risk of loneliness than the general population during COVID-19 lockdowns [ 33 ]. Just as ‘belongingness’ mediates subjective wellbeing among University students [ 34 ], feeling connected and supported acts as a protective buffer for medical students’ psychological wellbeing [ 25 ].
Translation into practice
Based on the themes identified in this study, specific interventions can be recommended to support medical students’ mental wellbeing, summarised in Table 3 . This study provides evidence to support the development of interventions that increase relational connections between medical students, as a method of promoting mental wellbeing and preventing burnout. Our findings highlight the importance of interpersonal relationships and informal support mechanisms, and indicate that medical student wellbeing could be improved by strengthening these. Possible ways to do this include encouraging collaboration over competition, providing sufficient time off to visit family, having a peer mentor network, events that encourage students to meet each other, and wellbeing sessions that combine socialising with learning relaxation and mindfulness techniques. Students could be supported in their interactions with patients and peers by embedding reflective practice such as placement debrief sessions, Schwartz rounds [ 35 ] or Balint groups [ 36 ], and simulated communication workshops for difficult situations.
Experiencing guilt [ 30 ] and competition [ 4 ] while studying medicine are consistently recognised as contributing to distress and burnout, so interventions targeting these could improve mental wellbeing. Based on the responses from students, curriculum-based measures to protect mental wellbeing include manageable workloads, supportive learning environments, cultivating students’ sense of purpose, and encouraging taking breaks from studying without guilt. Normalising sharing of difficulties and regularly including content within the curriculum on self-care and stress reduction would improve mental wellbeing.
In aiming to reduce psychological distress among medical students, it is important that promotion of individual self-care is accompanied by reducing institutional stressors [ 11 , 29 ]. While the exploration of individual factors is important, such as promoting healthy lifestyle habits, reflection, time management, and mindset changes, this should not detract from addressing factors within the culture, learning and work environment that diminish mental wellbeing [ 37 ]. Heath et al. [ 38 ] propose a pro-active, multi-faceted approach, incorporating preventative strategies, organisational justice, individual strategies and organisational strategies to support resilience in healthcare workers. Similarly, trauma-informed medical education practices [ 13 ] involve individual and institutional strategies to promote student wellbeing.
Students favoured formal support that was responsive, individualised, and accessible. For example, integrating conversations about wellbeing into routine academic systems, and accommodating in-person and remote access to support. There has been increased awareness of the wellbeing needs of medical students in recent years, especially since the start of the pandemic, which has led to improvements in many of these areas, as reported in reviews by Ardekani et al. [ 12 ] and Klein and McCarthy [ 39 ]. Continuing to address stigma around mental health difficulties and embedding discussions around wellbeing in the curriculum are crucial for medical students to be able to seek appropriate support.
Strengths & limitations
By using qualitative open-text responses, rather than enforcing preconceived categories, this study captured students’ lived experience and priorities [ 4 , 31 ]. This increased the salience and depth of responses and generated categories of responses beyond the existing evidence, which is particularly important given the unprecedented experiences of COVID-19. Several strategies were used to establish rigour and trustworthiness, based on the four criteria proposed by Lincoln and Guba [ 20 ] (Table 2 ). These included the active involvement of medical students and recent medical graduates in data analysis and the development of themes, increasing the credibility of the research findings.
Potential limitations of the study are that participants may have been primed to think about certain aspects of wellbeing due to data being collected during a webinar delivered by medical educators including the lead author at the start of their palliative medicine placement, and the choice of prompts. Data was collected during the COVID-19 pandemic, and therefore represents fourth year medical students’ views in specific and unusual circumstances. Information on this context is provided to enable the reader to evaluate whether the findings have transferability to their setting. Responses were visible to others in the group, so participants may have influenced each other to give socially acceptable responses. This process of forming subjective meanings through social interactions is recognised as part of the construction of a shared understanding of reality, and we therefore view it as an inherent feature of this methodology rather than a hindrance. Feedback on the webinar indicated that students benefitted from this process of collective meaning-making. Similarly, researcher subjectivity is viewed as a contextual resource for knowledge generation in reflexive thematic analysis, rather than a limitation to be managed [ 19 ]. The study design meant that different demographic groups could not be compared.
Padlet provided a novel and acceptable method of data collection, offering researchers and educators the potential benefits of an anonymous forum in which students can see their peers’ responses. The use of an interactive webinar demonstrated a potential application of connectivist pedagogical principles [ 18 ]. Researchers are increasingly using content from online forums for qualitative research [ 40 ], and Padlet has been extensively used as an educational tool. However, to the authors’ knowledge, Padlet has not previously been used as a data collection platform for qualitative research. Allowing anonymity carried the risk of students posting comments that were inappropriate or unprofessional. However, with appropriate guidance it appeared to engender honesty and reflection, provided a safe and collaborative learning environment, and student feedback was overwhelmingly positive. It would be useful to evaluate the effects of this reflective webinar on medical students’ mental wellbeing, given that it acted as an intervention in addition to a teaching session and research study.
Students were prompted to plan what they would do following the webinar to improve their mental wellbeing. A longitudinal study to determine how students enacted these plans would allow a more detailed investigation of students’ self-care behaviour.
While we hope that the stressors of COVID-19 will not be repeated, this study provides valuable insight into medical students’ mental wellbeing, which can inform support beyond this exceptional time. The lasting impact of the pandemic upon medical education and mental wellbeing remains to be seen. Nevertheless, our findings reinforce and extend the coping reservoir model proposed by Dunn et al. [ 14 ], adding to our understanding of the factors that contribute to resilience or burnout. In particular, it provides evidence for the development of interventions that increase experiences of relational connectedness and belonging, which are likely to act as a buffer against emotional distress among medical students.
Data availability
The datasets generated and analysed during the study are available from the corresponding author on reasonable request.
Change history
26 june 2024.
A Correction to this paper has been published: https://doi.org/10.1186/s40359-024-01813-7
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316(21):2214.
Article PubMed PubMed Central Google Scholar
Awad F, Awad M, Mattick K, Dieppe P. Mental health in medical students: time to act. Clin Teach. 2019;16(4):312–6.
Article PubMed Google Scholar
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. 2021;0:1–7.
Google Scholar
De Andres Crespo M, Claireaux H, Handa AI. Medical students and COVID-19: lessons learnt from the 2020 pandemic. Postgrad Med J. 2021;97(1146):209–10.
Paz DC, Bains MS, Zueger ML, Bandi VR, Kuo VY, Cook K et al. COVID-19 and mental health: a systematic review of international medical student surveys. Front Psychol. 2022;(November):1–13.
Jia Q, Qu Y, Sun H, Huo H, Yin H, You D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front Psychol. 2022;13:846789.
General Medical Council. Outcomes for Graduates. London; 2020 https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates [accessed 13 Feb 2024].
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
McLuckie A, Matheson KM, Landers AL, Landine J, Novick J, Barrett T, et al. The relationship between psychological distress and perception of emotional support in medical students and residents and implications for educational institutions. Acad Psychiatry. 2018;42(1):41–7.
Ardekani A, Hosseini SA, Tabari P, Rahimian Z, Feili A, Amini M. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med Educ. 2021;21:352.
Brown T, Berman S, McDaniel K, Radford C, Mehta P, Potter J, et al. Trauma-informed medical education (TIME): advancing curricular content and educational context. Acad Med. 2021;96(5):661–7.
Dunn LB, Iglewicz A, Moutier C. Promoting resilience and preventing burnout. Acad Psychiatry. 2008;32(1):44–53.
Kelly EL, Casola AR, Smith K, Kelly S, Syl M, Cruz D, De. A qualitative analysis of third-year medical students ’ reflection essays regarding the impact of COVID-19 on their education. BMC Med Educ. 2021;21(481).
Pilgrim D. Some implications of critical realism for mental health research. Soc Theory Heal. 2014;12:1–21.
Article Google Scholar
Henriksson C, Friesen N. Introduction. In: Friesen N, Henriksson C, Saevi T, editors. Hermeneutic phenomenology in education. Sense; 2012. pp. 1–17.
Goldie JGS, Connectivism. A knowledge learning theory for the digital age? Med Teach. 2016;38(10):1064–9.
Braun V, Clarke V. Thematic analysis: a practical guide. SAGE Publications Ltd; 2021.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, California: SAGE; 1985.
Book Google Scholar
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. 2017;16:1–13.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: Acad Med. 2014;89(9):1245–51.
PubMed Google Scholar
Freitas FA, Leonard LJ. Maslow’s hierarchy of needs and student academic success. Teach Learn Nurs. 2011;6(1):9–13.
Maslow AH. Motivation and personality. 3rd ed. New York: Longman; 1954.
MacArthur KR, Sikorski J. A qualitative analysis of the coping reservoir model of pre-clinical medical student well-being: human connection as making it worth it. BMC Med Educ. 2020;20(1):1–11.
Simpson V, Halpin L, Chalmers K, Joynes V. Exploring well-being: medical students and staff. Clin Teach. 2019;16(4):356–61.
Rich A, Viney R, Silkens M, Griffin A, Medisauskaite A. UK medical students’ mental health during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2023;13:e070528.
Bakker AAB, Demerouti E. Job demands-resources theory: taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–85.
Riley R, Kokab F, Buszewicz M, Gopfert A, Van Hove M, Taylor AK et al. Protective factors and sources of support in the workplace as experienced by UK foundation and junior doctors: a qualitative study. BMJ Open. 2021;11(6).
Greenmyer JR, Montgomery M, Hosford C, Burd M, Miller V, Storandt MH, et al. Guilt and burnout in medical students. Teach Learn Med. 2021;34(1):69–77.
Ayala EE, Omorodion AM, Nmecha D, Winseman JS, Mason HRC. What do medical students do for self-care? A student-centered approach to well-being. Teach Learn Med. 2017;29(3):237–46.
Wurth S, Sader J, Cerutti B, Broers B, Bajwa MN, Carballo S, et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: studies, clinical implication, and professional identity. BMC Med Educ. 2021;21(1):620.
Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–4.
Arslan G, Loneliness C, Belongingness. Subjective vitality, and psychological adjustment during coronavirus pandemic: development of the college belongingness questionnaire. J Posit Sch Psychol. 2021;5(1):17–31.
Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E et al. A realist informed mixed-methods evaluation of Schwartz center rounds in England. Heal Serv Deliv Res. 2018;6(37).
Monk A, Hind D, Crimlisk H. Balint groups in undergraduate medical education: a systematic review. Psychoanal Psychother. 2018;8734:1–26.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49.
Heath C, Sommerfield A, Von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020;75(10):1364–71.
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(92).
Smedley RM, Coulson NS. A practical guide to analysing online support forums. Qual Res Psychol. 2021;18(1):76–103.
Download references
Acknowledgements
We would like to thank Dr P Byrne for providing guidance, Mrs A Threlfall and Professor VCT Goddard-Fuller for commenting on drafts, and the medical students who participated in the webinars.
This study was unfunded.
Author information
Authors and affiliations.
Department of Psychology, University of Liverpool, Eleanor Rathbone Building, Bedford Street South, Liverpool, L69 7ZA, UK
Helen M West
Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK
School of Medicine, University of Liverpool, Liverpool, UK
Rowan M Davies, Benjamin Shelley & Oscar T Edginton
Salford Royal NHS Foundation Trust, Manchester, UK
Rowan M Davies
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
Benjamin Shelley
Leeds Teaching Hospitals NHS Foundation Trust, Leeds, UK
Oscar T Edginton
You can also search for this author in PubMed Google Scholar
Contributions
HMW conceptualised the study and collected the data. HMW, LF, RMD, BS and OTE conducted data analysis. HMW, LF, RMD and OTE wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Helen M West .
Ethics declarations
Ethical approval and consent to participate.
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365). Students were fully informed about the study prior to the workshop and had an opportunity to ask questions. Participants provided informed consent, completing an electronic consent form before responding to prompts. The study was conducted in accordance with relevant guidelines and regulations, including the University of Liverpool Research Ethics and Research Data Management Policies, and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
West, H.M., Flain, L., Davies, R.M. et al. Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support. BMC Psychol 12 , 179 (2024). https://doi.org/10.1186/s40359-024-01618-8
Download citation
Received : 12 December 2023
Accepted : 22 February 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s40359-024-01618-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental wellbeing
- Medical student
- Student doctor
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 19.8.2024 in Vol 26 (2024)
This is a member publication of Open University
Prevalence of Health Misinformation on Social Media—Challenges and Mitigation Before, During, and Beyond the COVID-19 Pandemic: Scoping Literature Review
Authors of this article:

- Dhouha Kbaier 1 , PhD ;
- Annemarie Kane 2 , PhD ;
- Mark McJury 3 ;
- Ian Kenny 1 , PhD
1 School of Computing and Communications, The Open University, Milton Keynes, United Kingdom
2 Faculty of Arts and Social Sciences, The Open University, Milton Keynes, United Kingdom
3 School of Physical Sciences, The Open University, Milton Keynes, United Kingdom
Corresponding Author:
Dhouha Kbaier, PhD
School of Computing and Communications
The Open University
Walton Hall
Milton Keynes, MK7 6AA
United Kingdom
Email: [email protected]
Background: This scoping review accompanies our research study “The Experience of Health Professionals With Misinformation and Its Impact on Their Job Practice: Qualitative Interview Study.” It surveys online health misinformation and is intended to provide an understanding of the communication context in which health professionals must operate.
Objective: Our objective was to illustrate the impact of social media in introducing additional sources of misinformation that impact health practitioners’ ability to communicate effectively with their patients. In addition, we considered how the level of knowledge of practitioners mitigated the effect of misinformation and additional stress factors associated with dealing with outbreaks, such as the COVID-19 pandemic, that affect communication with patients.
Methods: This study used a 5-step scoping review methodology following Arksey and O’Malley’s methodology to map relevant literature published in English between January 2012 and March 2024, focusing on health misinformation on social media platforms. We defined health misinformation as a false or misleading health-related claim that is not based on valid evidence or scientific knowledge. Electronic searches were performed on PubMed, Scopus, Web of Science, and Google Scholar. We included studies on the extent and impact of health misinformation in social media, mitigation strategies, and health practitioners’ experiences of confronting health misinformation. Our independent reviewers identified relevant articles for data extraction.
Results: Our review synthesized findings from 70 sources on online health misinformation. It revealed a consensus regarding the significant problem of health misinformation disseminated on social network platforms. While users seek trustworthy sources of health information, they often lack adequate health and digital literacies, which is exacerbated by social and economic inequalities. Cultural contexts influence the reception of such misinformation, and health practitioners may be vulnerable, too. The effectiveness of online mitigation strategies like user correction and automatic detection are complicated by malicious actors and politicization. The role of health practitioners in this context is a challenging one. Although they are still best placed to combat health misinformation, this review identified stressors that create barriers to their abilities to do this well. Investment in health information management at local and global levels could enhance their capacity for effective communication with patients.
Conclusions: This scoping review underscores the significance of addressing online health misinformation, particularly in the postpandemic era. It highlights the necessity for a collaborative global interdisciplinary effort to ensure equitable access to accurate health information, thereby empowering health practitioners to effectively combat the impact of online health misinformation. Academic research will need to be disseminated into the public domain in a way that is accessible to the public. Without equipping populations with health and digital literacies, the prevalence of online health misinformation will continue to pose a threat to global public health efforts.
Introduction
The global adoption of the internet has made health information more accessible, and the development of digital technology has enabled its rapid dissemination. However, the internet has also made possible the dissemination of false and misleading health misinformation and disinformation, with negative consequences, including the potential to exacerbate health inequalities. Health practitioners have found themselves at the forefront of communicating with patients who have taken on board health misinformation in the context of its proliferation on the web. This paper (associated with the study by Ismail et al [ 1 ]) surveyed the current literature concerning online health misinformation to establish the extent and scope of the problem, with special reference to the needs of health practitioners in their efforts to mitigate its impact. Several studies have established useful definitions of the terms misinformation and disinformation and distinctions between them. Misinformation has been defined as information that is not supported by evidence and contradicts the best-supported evidence available [ 2 , 3 ]. Wang et al [ 4 ] made a further distinction between online misinformation and disinformation, in particular on social media platforms. For Wang et al [ 4 ], misinformation is information that is not known to be false and is shared without malice. By contrast, disinformation involves the knowing and sharing of false information with the purpose of causing harm. This paper follows the distinctions of Wang et al [ 4 ] to use the terms misinformation and disinformation as appropriate.
It is important to acknowledge at the outset that digital technology in health and social contexts presents both risks and opportunities for equity among different information audiences [ 5 ]. However, there has recently been a change in the reception and assessment of the role of the internet, social media in particular, among researchers, even predating the COVID-19 pandemic. In the early days of social media, researchers largely identified prosocial and altruistic uses of social media platforms such as Facebook and Twitter by the public. However, considerable disquiet about the impact of social media and its potential for the spread of “fake news” and the amplification of conspiracy theories has displaced the more positive evaluation that was apparent when social media was in its infancy [ 6 ]. In the majority of the current research, there is a view that digital technology, particularly social media, has amplified the problem of health misinformation. The risk most frequently identified, either explicitly or implicitly, is the susceptibility of ordinary users, who may be lacking sophisticated levels of health and digital literacies, to health misinformation. Further risks noted in the literature include disinformation disseminated by organized trolling networks and bots that can be hard to distinguish from human users. The recognition of these risks underpins an emerging policy discourse about the threat of health misinformation, particularly the role of social media in its spread, in which health information and misinformation has become a politicized issue. From one policy perspective, there is an assumption that social media users are vulnerable, even passive, recipients of health misinformation rather than reflective interpreters of the available information. The corollary of this is that correcting misinformation with authoritative knowledge will solve the problem. However, a survey of the literature suggested that neither assumption fully expresses the complexity of how health misinformation is disseminated, received, and used via the internet. This may be because although there is a growing body of evidence on the extent of online health misinformation, there is much less research about what users do with health misinformation, why users consume health misinformation, and why (and which) people believe health misinformation [ 7 - 9 ].
In this scoping review, we reviewed the current state of knowledge regarding the prevalence of online misinformation before and during the COVID-19 pandemic and the impact that has on users’ understanding of health information. We considered this context with special reference to patients’ understanding, health practitioners’ practice in response to that, and policy makers’ concerns. The pressures and distractions that health professionals face in attempting to mitigate the impacts of online health misinformation are discussed in relation to patients’ health and digital literacies and the politicization of health information and misinformation.
Information Sources
We conducted a comprehensive literature search to identify relevant studies that explored health misinformation on social media platforms. The search was conducted across multiple electronic databases, including PubMed, Scopus, Web of Science, and Google Scholar.
The search terms included a combination of relevant keywords and phrases, including “health misinformation,” “social media,” “online health communities,” and “COVID-19 pandemic.” The search was not limited by publication date. Detailed search strategies are provided in Multimedia Appendix 1 .
Study Selection
Our study selection process followed a scoping approach, where we aimed to identify and include studies that provided insights into the prevalence and challenges of health misinformation on social media platforms. Initially, 2 researchers independently screened titles and abstracts of the identified articles to determine their relevance. Articles that did not meet the inclusion criteria were excluded at this stage.
Inclusion Criteria
Articles were included if they discussed health misinformation on social media, addressed the challenges posed by health misinformation, or were relevant to the period before, during, and after the COVID-19 pandemic.
Any disagreements between the 2 researchers were resolved through discussion and consensus. Full-text articles were then retrieved for the remaining studies, and a further assessment of eligibility was conducted based on the same inclusion criteria.
Data Extraction
We gathered information on (1) study objectives, (2) research methods, (3) findings, and (4) key themes related to health misinformation. This process was performed independently by 2 researchers, and any discrepancies were resolved through discussion.
Data Synthesis and Analysis
We adopted a scoping review content analysis approach to analyze the data extracted from the selected articles. The analysis process involved identifying key themes and patterns related to health misinformation on social media. The content analysis allowed us to gain a deeper understanding of the challenges posed by health misinformation and the strategies for its mitigation, both before and during the COVID-19 pandemic.
Results of Search
In our article selection process ( Figure 1 ), we initiated our search by identifying a total of 4563 articles from various databases. Following the removal of duplicates, 1295 articles were excluded, leaving us with 3268 unique articles. Subsequently, these articles underwent an initial screening, which involved evaluating their abstracts and titles, resulting in the exclusion of 2635 articles that did not align with our inclusion criteria. Further scrutiny was applied during full-text screening, which was conducted on 633 articles. Among these, 563 articles were found ineligible due to reasons such as not meeting the inclusion criteria (n=378 articles), being classified as literature reviews, editorials, or letters (n=174 articles), or the full texts being inaccessible (n=11 articles). A total of 70 articles were ultimately included in this scoping review.

Characteristics of Included Documents (n=70)
The majority (65/70, 93%) of documents were published in the last 10 years and originated predominantly in North America (42/70, 60%), Europe (19/70, 27%), and Asia (11/70, 16%). The funding sources were mainly public (61/70, 87%). The documents were classified as original research papers (38/70, 54%), subjective “opinion” articles (editorials, viewpoints, commentaries, and letters to the journal; 11/70, 16%), and knowledge syntheses or reviews (9/70, 13%) which included systematic reviews (n=6), descriptive reviews (n=2), and 1 integrated theoretic review.
Extent and Impact of Health Misinformation Disseminated Across a Range of Outlets
This section will review the literature concerning the extent and impact of the problem of health misinformation, including the spread of antivaccination discourse. In a study by Wood et al [ 10 ] among health practitioners in North Carolina, 94.2% of the respondents reported encounters with patient health misinformation within the previous year. While the sources of this misinformation were not broken down and identified by Wood et al [ 10 ], several other studies linked patient health misinformation to the prevalence of health misinformation on social media sites, identifying the latter as a significant problem [ 4 , 11 - 15 ]. There is a growing consensus among researchers, health professionals, and policy makers about the need to confront, challenge, and even prevent the online dissemination of health misinformation [ 16 ]. Since the emergence of online social networks, users have increasingly sought and shared health information on social media sites. It is estimated that around 70% of adult internet users search health matters on the web. With the emergence of social media platforms, there has been a rise in “peer-to-peer health care,” through which individuals seek and share health information, forming online health communities with others who have similar health concerns [ 3 ]. In addition, health organizations and health professionals are increasingly using social media to disseminate and promote health information and advice. The opportunities for sharing and promoting good health information via the internet are evident, and it is important to acknowledge that in online health communities, users share experiences and receive and give different kinds of support, including emotional support, to cope with specific health conditions. However, the medium has also enabled the dissemination of health misinformation, and the prosocial aspects of sharing are also likely to involve the sharing of misinformation, putting the health of users at risk [ 3 ].
Misinformation Spreads on Social Media
There is a high degree of consensus among researchers that mainly because of the increasing popularity of social media, the internet has become a space for the dissemination and amplification of “fake news,” misleading information, and rumor, including health misinformation and antivaccine conspiracy theories [ 17 ]. The COVID-19 pandemic has heightened these concerns, resulting in a proliferation of recent studies and rapid reviews focusing on the online spread of misinformation. Lee et al [ 18 ] proposed that the proliferation of health misinformation during the COVID-19 pandemic became a major public health issue. At the earliest signs of the emerging COVID-19 pandemic, the director-general of the World Health Organization, Tedros Adhanom Ghebreyesus, speaking at the February 2020 Munich Security Conference, expressed concern about the risk of an infodemic of health misinformation disseminated via social media, identifying “vaccine hesitancy” as 1 of the top 10 global health threats [ 19 ]. Bapaye and Bapaye [ 20 ] agreed that the risks of misinformation on social networking sites constitute a global issue, referring specifically to the COVID-19 infodemic.
However, this is not in itself a new problem; longstanding concerns about “fake news” and misinformation in traditional media have been evident since the early decades of the 20th century [ 21 ], and the prevalence of misinformation on internet platforms certainly predates the COVID-19 pandemic. Therefore, because the COVID-19 pandemic has only intensified the concern regarding health misinformation, it might be more appropriate to see the pandemic as symptomatic of, and crystallizing, the challenges of countering health misinformation in the digital age, as the development of digital technology and the internet have brought about profound changes in the capacity of both misinformation and disinformation to spread globally and amplify rapidly [ 4 ].
Suarez-Lledo and Alvarez-Galvez [ 16 ] undertook a review of 69 studies of health misinformation on social media to identify the main health misinformation topics and their frequency on different social media platforms. The studies surveyed used a variety of research methods, including social network analysis (28%), evaluation of content (26%), evaluation of quality (24%), content/text analysis (16%), and sentiment analysis (6%). Suarez-Lledo and Alvarez-Galvez [ 16 ] concluded that the incidence of health misinformation was highest on Twitter, in particular, regarding the use of tobacco and other drugs, with some studies citing 87% of such posts containing misinformation. However, health misinformation about vaccines was also prevalent, with around 43% of posts containing misinformation, with the human papillomavirus vaccine being the most affected. This review by Suarez-Lledo and Alvarez-Galvez [ 16 ] confirmed many of the findings from earlier surveys. For example, in their survey of 57 articles, Wang et al [ 4 ] found that the most frequently discussed topics were regarding vaccination and infectious diseases, including Ebola and the Zika virus. Other topics such as nutrition, cancer, water fluoridation, and smoking were also prevalent. The studies they surveyed had tended to find that a high degree of misinformation on these topics was being shared and liked on social media.
Lee et al [ 18 ] conducted a cross-sectional online survey in South Korea to examine the prevalence of COVID-19 misinformation and the impact of exposure to COVID-19 misinformation on beliefs and behaviors. They found that exposure to COVID-19 misinformation was associated with misinformation belief, which then resulted in fewer preventive behaviors. Therefore, they highlighted the potential of misinformation to undermine global efforts in disease control and argued that public health strategies are needed to combat the proliferation of misinformation. Bapaye and Bapaye [ 20 ] conducted a cross-sectional online questionnaire survey of 1137 WhatsApp users in India. They noted that most research on the prevalence of misinformation in social media has focused on Twitter and Facebook and on the Global North. Measured by age, researchers found that users aged >65 years were the most vulnerable to accepting the veracity of messages containing health misinformation (K=0.38, 95% CI 0.341-0.419) Respondents aged 19 to 25 years displayed much lower vulnerability (K=0.31, 95% CI 0.301-0.319) than those aged >25 years ( P <.05). Measured by occupational category, users employed in nonprofessional occupations had the highest vulnerability (K=0.38, 95% CI 0.356-0.404); this was significantly higher than those of professionals and students ( P <.05). Notably, the vulnerability of health professionals was not significantly different from those of other occupation groups ( P >.05).
The authors concluded that in a developing country, WhatsApp users aged >65 years and those involved in nonprofessional occupations are the most vulnerable to false information disseminated via WhatsApp. Crucially, they noted that health care workers, who might be expected by laypersons to have expert knowledge, were as likely to be vulnerable to health misinformation as other occupation groups.
Antivaxxer Spread Before, During, and Beyond the COVID-19 Pandemic
Much of the current unease from researchers, understandably, centers on health misinformation about vaccines in the wake of the COVID-19 pandemic. In particular, there is concern about the growth and spread of so-called antivaxxer misinformation and beliefs. In 2019, the United States had its biggest measles outbreak in 30 years, with most cases involving people who had not been vaccinated. Hotez [ 22 ] claimed that much of the reason for the growth of antivaccine beliefs is because of a campaign of misinformation. He argued that social media sites are meeting places for the sharing of antivaccine views. To evade social media platforms’ automated moderation tools, which tend to focus on words, several antivaxxer groups, including one with around 250,000 members, began using visual codes, such as the carrot emoji, to hide antivaxxer content.
However, some of the misinformation has gained credibility because it has come from sources that laypersons would expect to be trustworthy. For example, in 1998, the British medical journal The Lancet published a paper by Dr Andrew Wakefield claiming a link between the measles, mumps, rubella vaccine and the onset of autism spectrum disorder. Wakefield’s paper was later rebutted, and an overwhelming body of evidence now refutes its conclusions [ 23 ]. However, despite long being discredited, Wakefield’s claims have remained a part of the antivaccine discourse. The persistence of the antivaccination narrative demonstrates the power of such discourses even in the face of evidence to challenge them.
Although strong antivaccine beliefs, and the more ambivalent attitude of vaccine hesitancy, have been around as long as there have been vaccines, until recent decades, they were on the margins. However, evidence supports the claim that they have been gaining momentum in the United States and Europe.
A survey by Skafle et al [ 24 ] aimed to synthesize the results from 19 studies in which the effect of social media misinformation on vaccine hesitancy was measured or discussed. The authors noted that the “vast majority” of studies were from industrialized Western countries. Only 1 study contained misinformation about autism as a side effect of COVID-19 vaccines. Nevertheless, the studies implied that information spread on social media had a negative effect on vaccine hesitancy and uptake. The conclusions from Skafle et al [ 24 ] were supported by data from online polling agencies. For example, a US YouGov poll from May 2020 found that only 55% of respondents would definitely take a COVID-19 vaccine if one were to become available, whereas 19% of respondents said that they would refuse and 26% were still undecided [ 25 ].
While much of the research about online vaccine discourse comes from the United States, there is also evidence that vaccine hesitancy has risen elsewhere. For example, in an Ipsos-MORI survey taken in December 2020, only 40% of respondents in France said they would take a COVID-19 vaccine, a figure symptomatic of a steep and swift decline in vaccine confidence in France [ 26 ]. However, interestingly, the same Ipsos-MORI poll indicated a rise in vaccine confidence among respondents in the United States since the earlier YouGov poll, cited earlier, by approximately 10% to 65%, and respondents in the United Kingdom expressed a still higher willingness to take a COVID-19 vaccine at approximately 77%. It is notable that in the United States and United Kingdom, the Ipsos-MORI results came after a period of intermittent lockdowns. The contrast with the results from France is, nevertheless, striking.
Understanding the Challenges Surrounding Health Misinformation
Here, we consider the challenges created by health misinformation on the web: (1) the role played by malicious actors on social media in spreading vaccine disinformation and misinformation and (2) how contextual and cultural issues have different effects on patients’ understanding of what is considered genuine, valid, and authentic health information.
Spread of Health Misinformation on Social Media by Malicious Actors
One strand of research presents the issue of health misinformation as a contest between trolls and bots on the one hand and the voices of trustworthy public health agencies on the other [ 6 ]. This view was supported by Hotez [ 22 ] and Broniatowski et al [ 11 ]. The latter investigated the role of bots and trolls as malicious actors mobilizing vaccination discourse on the web. Their study focused specifically on vaccine-related health messaging on Twitter. Comparing the rates of vaccine-related messages, they found that sophisticated bots and Russian trolls tweeted at higher rates than “average users.” However, the respective content from bots and trolls differed. Whereas bots communicated antivaccine messages, Russian troll accounts provided a seemingly balanced discussion of both provaccination and antivaccination arguments, implying an equivalence between them. The authors argued that amplifying and normalizing a debate is done with the purpose of sowing discord and may lead to undermining public confidence in scientific consensus about the effectiveness of vaccines. Wang et al [ 4 ] acknowledged that it is a challenge to readily distinguish between misinformation and disinformation on the web. They noted that disinformation, such as antivaccine propaganda, can unknowingly be spread by users with genuine concerns [ 4 ], as individuals increasingly seek health and healthy lifestyle information via the internet.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Politicization of the Problem of Health Misinformation
The identification of online trolls, bots, and orchestrated networks as major contributors to the spread of health disinformation and misinformation is now part of mainstream political discourse in the United States. On July 16, 2021, a quarrel broke out between the president of the United States, Joe Biden, and Facebook over the spread of health misinformation on the company’s social media platforms. Speaking to journalists, Biden blamed social media companies for a rise in the number of deaths from COVID-19 among the unvaccinated in the United States. Referring explicitly to Facebook, the president claimed that by allowing the proliferation of health misinformation on its platforms, the company was “killing people” [ 27 ]. Discursive interventions from politicians are never neutral; nevertheless, Biden’s claim about the impact of health misinformation on social media is backed up by many of the studies surveyed for this paper. Facebook immediately rebutted Biden’s accusation by citing their rules, introduced in February 2021, which banned posts that make identifiably false claims about vaccines. Furthermore, Facebook challenged Biden’s claim by asserting that not only has Facebook provided more authoritative information about COVID-19 and vaccines than any other internet site, reaching 2 billion people with such posts, but also that the platform’s vaccine finder tool had been used by more than 3 million Americans.
These figures suggest that although antivaxxer groups find ways to evade detection, their reach may be countered by that of information grounded in current science. A spokesperson for the company said that, far from killing people, “The facts show that Facebook is helping save lives. Period” [ 27 ]. The argument between Biden and Facebook may indeed signal more lay awareness of the problem and echo the concerns of the recent academic research about the dissemination of health misinformation by organized bot and troll networks. Framed as it is, in terms of apportioning the blame for the spread of health misinformation, Biden’s intervention mirrors much of the academic discourse in the United States on the subject. However, it is also symptomatic of the politicization of health misinformation, arguably accelerated by the COVID-19 pandemic, which may thwart evidence-based decision-making. This point was emphasized strongly by Kyabaggu et al [ 5 ]. They framed the problem of pervasive misinformation and disinformation in terms of prime movers and beneficiaries who use it to advance sociopolitical agendas and entrench asymmetrical power, especially in times of uncertainty and threat, such as the COVID-19 pandemic.
Kyabaggu et al [ 5 ] identified government failures to adopt evidence-informed decision-making. They noted that such failures have costs that not only are economic but, crucially, result in poorer health outcomes. They cited as an example the United Kingdom government’s initial prevaccine herd immunity strategy. The intention of this strategy was to allow SARS-CoV-2 to indiscriminately spread to a critical mass to build up population immunity. The authors noted that this was “a particularly concerning example of evidence framing by a government.” Kyabaggu et al [ 5 ] argued that public acceptance of health risk messages and adoption of health-protecting behaviors is highly contingent on the degree to which governments engage in evidence-informed decision-making and communicate this basis effectively. The authors cited several instances of government actors failing to recognize misinformation, disseminating inconsistent or inaccurate information, and not using evidence- and information-based decision-making processes. In recent years, the public policy discourse in the United Kingdom has been veering away from evidence- and information-based decision-making, as politicians have denounced “experts” and their “influence” on policy [ 28 , 29 ].
Finally, Gruzd et al [ 30 ] reported on the impact of coordinated link-sharing behavior to spread and amplify conspiracy-related misinformation. They found a coalition of Facebook accounts that engaged in coordinated link sharing behavior to promote COVID-19 related misinformation. This coalition included US-based pro-Trump, QAnon, and antivaccination accounts.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Health Literacies and Inequality
While the approach of Broniatowski et al [ 11 ], for example, provided a persuasive account of ways in which online health misinformation can be disseminated, there are limitations to this approach, as it did not provide an account of how users respond to the misinformation they encounter. The responses of ordinary users were assumed rather than investigated. Research by Vosoughi et al [ 31 ] provided a caveat to the claim that it is bots that accelerate the spread of misinformation. Their work supported that of Broniatowski et al [ 11 ] in suggesting that bots spread accurate and false information at the same rate. However, Vosoughi et al [ 31 ] also explained that misinformation spreads more rapidly than accurate information because humans, rather than bots, are more likely to spread misinformation [ 31 ]. This claim was further supported by Wang [ 32 ], who suggested that in democracies, where ideas compete for attention in a marketplace, accurate scientific information, which, for the layperson, may be boring or difficult to understand, is easily crowded out by information that is more easily grasped or sensational. Mokhtari and Mirzaei [ 12 ] located this problem specifically in the context of the COVID-19 pandemic. They considered that high mortality from COVID-19, its complexity, and its unknown features resulted in fear, anxiety, and mental pressure among people worldwide. To allay anxiety, people needed health information literacy, defined by the American Library Association as a set of abilities individuals require to recognize when information is needed and to locate, evaluate, and use it effectively [ 33 ]. In addition, Wang [ 32 ] noted that individuals are differentially vulnerable to health misinformation depending on their level of health literacy and that models need to account for this. Mokhtari and Mirzaei [ 12 ] argued that not only information and health literacies but also media literacy are needed. However, studies in the field of health literacy suggest that significant inequalities in health and digital literacies exist.
Researchers have argued that “vastly undervalued and unrecognized” health literacy ought to be considered the best “social vaccine” for preventing COVID-19 in populations [ 5 ]. However, inequalities in health literacy persist. Kyabaggu et al [ 5 ] defined health literacy as encompassing cognitive and social skills that determine individuals’ motivation and ability to access, understand, and use information, including quantitative health risk information, in ways that promote and maintain good health across the life course. They asserted that health literacy is an essential self-management skill and community resource for health, noting that health literacy is positively associated with patients’ involvement in clinical decision-making, willingness to express health concerns, and compliance with clinical guidance. However, despite research demonstrating the importance of health literacy, evidence, even from high-income countries, suggested relatively low levels of health literacy.
Kyabaggu et al [ 5 ] drew a link between health literacy and digital literacy. They suggested that the latter can be understood as health literacy in digital information and technology spaces. They argued that inequalities in health outcomes are exacerbated by a widening digital divide. While digital technology in health and social contexts presents both new risks and opportunities for equity in different information audiences, the ways in which power and privilege operated in the COVID-19 misinformation discourse have not been sufficiently examined. Although socially and economically disadvantaged groups were at a greater risk of exposure to COVID-19, their voices and experiences were often marginalized. In addition, inequalities in access to accurate information are not only related to issues of digital access and literacy but are also situational. For example, disadvantaged individuals may have fewer social connections, and low pay may necessitate longer working hours, militating against individuals having the resources of time and energy to seek out accurate health information and enhance their level of health literacy.
The experiences of specific groups may also go unreported. Quraishi [ 34 ] addressed the impact of misinformation on South Asian students—a fast-growing group in the United States, but one that often receives little media attention. Quraishi [ 34 ] concluded that there is a relationship between the COVID-19 pandemic and students’ academic performance and mental health, as well as an increase in the spread of misinformation regarding COVID-19 public safety guidelines.
Older adults can be a vulnerable group in relation to their comparatively poor digital literacy. Zhou et al [ 35 ] reported on the accuracy of older adults in judging health information credibility. They found that on average, participants only successfully judged 41.38% of health articles. Attractive headlines increased participant credibility judgments on the content, and of the articles shared with others, 62.5% contained falsehoods.
Contextual Factors Influencing the Reception of and Responses to Misinformation: Cultures and Values
Larson and Broniatowski [ 19 ] argued that developing the kinds of literacy advocated by Mokhtari and Mirzaei [ 12 ] and Tully et al [ 2 ] will not address the deep-seated problems they identified. The work by Kyabaggu et al [ 5 ] supported this, and noted that the infodemic crisis is not merely a health and digital literacy issue. Some demographics may be more vulnerable to persuasive communication from broader sociocultural forces. Kyabaggu et al [ 5 ] argued that in considering the social determinants of health, attention must be paid not only to digital and health literacies but also to the ways in which these literacies coexist and interact with other influences. Larson and Broniatowski [ 19 ] suggested that one of the strongest determinants of vaccine confidence or vaccine hesitancy is the level of trust or distrust in the institutions that produce vaccines. A higher level of trust encourages the willingness to accept a high level of risk for a greater benefit. A lower level of trust militates against the acceptance of even a low level of perceived risk. For Larson and Broniatowski [ 19 ], it is not simply the presence of misinformation on social media networks but the social and cultural context of users’ reception of that information that influences responses. Health information operates in a complex and contentious social world. Individuals and communities respond to new information in terms of already developed political, cultural, and social values that influence whether they trust or distrust authority. Populations may be characterized by trust or mistrust of scientific institutions and government. Trust has been eroded through the exposure of fraud, research scandals, and misconduct by major multinational pharmaceutical companies, for example. Communities may be predisposed to distrust the government and its agents depending on their own status or identity. According to Goldenberg [ 36 ], these contexts can make misinformation and health conspiracy theories compelling.
Strategies to Correct Online Misinformation
We address the additional pressures on health professionals in communicating accurate information to mitigate the effects of misinformation, particularly with regard to the additional requirements imposed as a result of the precautions being taken during the pandemic. One area of disagreement in the literature concerns the usefulness of user correction response.
Research Into User Correction Strategies
There is some disagreement as to whether engagement with misinformation by users spreads and reinforces it or even whether extended debates over health misinformation cause users to doubt the possibility of knowable facts. For example, Broniatowski et al [ 11 ] argued that when ordinary users directly confront vaccine-skeptic messages from bots, it only serves to legitimize the “debate.” By contrast, Tully et al [ 2 ] argued that social media users have a role to play in either spreading or stopping the spread of misinformation across platforms. Their research aimed to uncover what factors influenced users’ responses. Tully et al [ 2 ] acknowledged that a range of factors can influence the spread or prevention of misinformation, including the behavior of malicious actors such as bots and trolls; the platform’s terms of service; and content moderation policies. As already noted, while most users are not creators of misinformation, they may spread and amplify it by liking, sharing, or replying. In opposition to the work of Broniatowski et al [ 11 ], Tully et al [ 2 ] argued that the content of engagement is particularly important, as their research suggested that multiple corrections by social media users may be required to reduce misperceptions. However, they claimed that most people simply ignore misinformation when they see it on social media.
Tully et al [ 2 ] noted the promise in mobilizing users to engage in such correction, given the vast numbers of users on these sites, in comparison with professional fact-checkers and health authorities.
They considered whether the tone of a correction would influence perceptions of the credibility of the message. However, despite some mixed evidence, they concluded that overall, the tone was not a significant factor and that neutral, affirmative, and uncivil corrections were all effective at reducing misperceptions. They found that participants were generally unlikely to reply to the misinformation tweet. However, their content analysis of hypothetical replies suggested that when users did reply, they mainly provided correct information, particularly after seeing other corrections. Tully et al [ 2 ] concluded that user corrections offer “untapped potential” in responding to misinformation on social media, but further work is needed to consider how users can be mobilized to provide corrections, given their overall unwillingness to reply. However, a limitation of the experimental approach of Tully et al [ 2 ], acknowledged by the researchers, is that in asking individuals what they would hypothetically do, this may not reflect what they actually do in a real social media setting, especially in relation to an issue they care more strongly about. Although the experiment gauged attitudes, it did not delve into how strongly these attitudes were held. It is also not clear to what degree corrections were effective at reducing misperceptions and how reductions were measured.
By contrast, the results of experimental studies by Ittefaq [ 37 ] and Mourali and Drake [ 38 ] suggested that correcting misinformation is by no means a straightforward proposition. They noted the previous research on rebuttal, which suggested that properly designed corrections can mitigate the effects of misinformation. However, such studies have tended to compare responses to misinformation followed by correction with responses of a control group that receives no correction or receives an alternative correction. Mourali and Drake [ 38 ] argued that this static approach misses the dynamic nature of social media debate. They noted that the correction of misinformation is generally followed up with a rebuke by the original poster, inciting further correction and prolonged back-and-forth debate. Mourali and Drake [ 38 ] cited previous studies showing that exposure to conflicting information about health topics, including mammography, nutrition, and the human papillomavirus vaccine, may increase confusion and negative attitudes toward that particular health topic. The researchers found that initial exposure to misinformation had a negative impact on attitudes and intentions toward masking, consistent with previous studies that concluded that exposure to misinformation negatively impacts attitudes and intentions toward behaviors favored by science. Also consistent with previous research, they found that the first correction of the false claim improved attitudes and intentions toward masking. The authors suggested that this effect is partially explained by a decrease in the perceived strength of the argument underlying the false claim. However, this initial improvement diminished on further exposure to false claims and refutation attempts. This finding confirmed their hypothesis that extended exposure to false claims and refutation attempts appears to weaken belief in the possibility of objective knowledge, leading to less positive reactions toward masking as a science-based behavior. They concluded that the level of exposure to contradictory information needs to reach a certain threshold before it affects perceived truth objectivity. However, although people are more likely to share misinformation when its content is consistent with their existing beliefs or when its message is simple, direct, or sensational, correcting misinformation does reduce its likelihood of being shared on social media, an effect that persists even after multiple exposures.
Mourali and Drake [ 38 ] noted that each social media platform exhibits particular interaction norms, which may impact how users interpret the conversation. As their study was limited to a single platform, Reddit, and the debate was restricted to 4 exchanges between only 2 protagonists, the researchers acknowledged that these aspects limit the generalizability of the results. They suggested that future research could attempt to replicate their findings on different social media platforms, and to include more than 2 protagonists and more than 4 exchanges. They noted further that although extended debates are common on social media, it is not known how frequently they occur, echoing the comments by Suarez-Lledo and Alvarez-Galvez [ 16 ] that the extent of misinformation is not clear.
In contrast to the fairly sanguine view of Tully et al [ 2 ] about the potential of users to spread corrective information, Mourali and Drake [ 38 ] problematized the position, pointing to the potential for more complex and uncertain outcomes, whereas Larson and Broniatowski [ 19 ] argued that although the importance of correcting misinformation, item by item, should not be diminished, only if underlying issues driving misinformation are addressed can, for example, long-term vaccine confidence in populations be sustained. They argue that simply responding to misinformation with factual corrections is not likely to reverse the dissent that has been evident among antivaxxers or to necessarily persuade the more ambivalent vaccine-hesitant individuals. They identified deeper social and cultural issues at play, which have been discussed in this paper in the previous sections.
Research Into Effective Models to Accomplish the Automatic Detection of Health Misinformation in Online Health Communities
Here, we consider examples of research into the automatic detection of health misinformation in online health communities. Zhao et al [ 3 ] began from the premise that there is a vast amount of health misinformation, creating a challenge for health communities in identifying misinformation. Rather than relying on users’ ability to correct misinformation, they proposed that there is a need for an effective model to achieve automatic detection of health misinformation in online health communities. This view was also put forward by Weinzierl and Harabagiu [ 39 ]. Focusing specifically on COVID-19 vaccine misinformation, they argued that automatic detection of misinformation on social media is an essential first step in delivering interventions designed to address vaccine hesitancy.
Zhao et al [ 3 ] identified much of the existing analysis as concentrating on the linguistic features of communications only. They wanted to examine the underresearched area of whether integrating user behavioral features with linguistic features, sentiment features, and topic features could effectively distinguish misinformation from accurate information in online health communities. Their study combined the aforementioned features to build a detection model targeting misinformation in online health communities’ contexts. The behavioral features targeted were discussion initiation, interaction engagement, influential scope, relational mediation, and informational independence. Descriptions of these behavioral features are reproduced in Table 1 .
| Behavioral feature | Measurement | Description |
| Discussion initiation | The number of threads a user created | To reflect the activity of a user in terms of initiating new discussions |
| Interaction engagement | The number of replies and the number of replies to a reply a user created | To reflect the activity of a user in terms of interacting with other users |
| Influential scope | Degree centrality | To reflect the potential communication ability of a user |
| Relational mediation | Betweenness centrality | To assess the potential of a user for the control of communication in the community |
| Informational independence | Closeness centrality | To assess the ability of a user to instantly communicate with others without going through many intermediaries |
The authors tested their detection model on a data set collected from a real online health community, selecting as their data source Zibizheng Ba, an autism forum on the Baidu Tieba online health community site hosted by the Chinese web service Baidu. Baidu Tieba claims to be one of the largest interest-based discussion platforms in China. Users can generate topic-based discussion forums on the platform, share information, and make friends with other users. Posts on Baidu Tieba are indexed by Baidu, China’s most popular search engine, so users can readily find misinformation when searching for health-related information through the search engine. The authors developed a python-based web crawler to collect data from the forum. To train the health misinformation detection model, 5000 records were sampled from the whole data set by stratification according to 3 types of records (ie, thread, reply, and reply to reply) using stratified sampling methods. Therefore, the constituent types of the records (ie, thread, reply, and reply to reply) in the sample data set were consistent with the composition of the whole data set.
The researchers applied the elaboration likelihood model (ELM). The model, originally developed by Petty and Cacioppo [ 40 ] to explain attitude change, has been used extensively in advertising to try to influence consumers.
Overall, 4 types of misinformation were identified through their coding analysis, and the model correctly detected about 85% of the health misinformation. Their results also indicated that behavioral features were more informative than linguistic features in detecting misinformation. The authors concluded that their results not only demonstrated the efficacy of behavioral features in health misinformation detection but also offered both methodological and theoretical contributions to misinformation detection by integrating the features of messages as well as the features of message creators. Others have also highlighted the problems posed by misleading visual information [ 41 ].
It is worth noting that during the pandemic, the UK National Health Service (NHS) began using Twitter to promote provaccine messaging, which closely follows a combination of the features suggested by Zhao et al [ 3 ]. When users searched for the term “vaccine” or related terms, the top post was a message prominently displaying the NHS logo, identifying it as reputable and trustworthy. The tweets contained links to NHS websites providing information about vaccines and COVID-19. The posts differed in linguistic content and visual design. For example, one featured only written text on a white background and stated in bold, “Know the facts.” Another featured a large image of a happy minority ethnic family, washing dishes together, with the message that the COVID-19 vaccine decreases household transmission by up to half. The contrasting designs suggest that the message was targeted specifically to users’ timelines. It was also apparent that elements of ELM were being applied, combining the features identified by Zhao et al [ 3 ] in different ways.
Weinzierl and Harabagiu [ 39 ] adopted a different method than Zhao et al [ 3 ], reversing the more commonly used classification approach. The authors of each study claimed strong results in identifying health misinformation on social media platforms. However, Nabożny et al [ 42 ] argued that the current automatic systems for assessing the credibility of health information are not sufficiently precise to be used without supervision by human medical expert annotators.
Barve and Saini [ 43 ] have reported on their use of automated fact-checking using a coded content similarity measure (CSM). In this approach, the CSM showed improved accuracy (91.06%) compared to the accuracy of the Jaccard similarity measure (74.26%). Further, the algorithmic approach outperformed the feature-based method.
Neither Zhao et al [ 3 ] nor Weinzierl and Harabagiu [ 39 ] recorded what happens when misinformation is detected. Research from Broniatowksi et al [ 44 ] suggested that once detected, steps taken by social media platforms such as content removal or deplatforming may not be effective in stemming the spread of misinformation and may even be counterproductive. Social media platforms use a combination of “hard” and “soft” content remedies to reduce the spread of health misinformation. Soft remedies include warning labels attached to content and downranking of some content in web searches, whereas hard remedies include content removal and deplatforming of accounts. Hard remedies are controversial and have given rise to accusations of censorship. For the authors, short-term evidence for the effectiveness of hard remedies is in any case mixed, and long-term evidence is yet to be examined. Their study focused on Facebook and found that while hard remedies did reduce the number of antivaccine posts, they also produced unintended consequences. Provaccine content was removed, and engagement with the remaining antivaccine content repeatedly recovered to prepolicy levels. Worryingly, this content became more misinformative, more politically polarized, and more likely to be seen in users’ news feeds. The authors explain these results as a product of Facebook’s architecture, which is designed to promote community formation. Members of communities dedicated to vaccine refusal seek out misinformation. To meet this demand, and to circumvent content moderation efforts, antivaccine content producers post links to external sources of misinformative content, such as Bitchute, Rumble, Gab, and Telegram, in lieu of more mainstream platforms that had implemented similar content removal policies (eg, YouTube and Twitter). Broniatowski et al [ 44 ] argued that Facebook’s policy reduced the number of posts in antivaccine venues but was not successful in inducing a sustained reduction in engagement with antivaccine content, including misinformation. The authors noted that alternative platforms often host politically extreme right-wing content. Therefore, they argued that Facebook’s content removal policies may have the unintended consequence of radicalizing their audiences, and their findings suggested the need to address how social media platform architecture enables community formation and mobilization around misinformative topics when managing the spread of online content.
These studies advocate for the automatic detection of health misinformation. However, work that calls into question the ability of automatic detection to operate without human intervention has also been discussed. In addition, there are questions raised in the literature about what should be done when misinformation is detected and concerns about whether content removal or deplatforming of accounts are the most effective ways to reduce the spread of health misinformation or may even be counterproductive.
The Roles of Health Practitioners
The discussion so far has highlighted the complex and multifaceted dimensions of the context of online health misinformation in which health practitioners must operate. As noted in our introduction, a study of health practitioners in North Carolina found that nearly 95% had encountered patient health misinformation within the previous year [ 10 ]. There is very little research on the amount or effectiveness of training received by health professionals to prepare them for engaging with patients about health misinformation. Wood et al [ 10 ] found that most respondents had not received relevant training despite overwhelmingly reporting encountering health misinformation.
Nevertheless, within the literature, there is no shortage of advice from researchers and health professionals addressed to health practitioners on how to approach and correct health misinformation. This advice stems from both original research studies and reviews of best practices featured in peer-reviewed medical and health journals. Such advice centers on the need for health practitioners to understand misinformation and how to address it. Health practitioners are advised of the need to be aware of health myths and urged to dismantle them in providing accurate health guidance [ 45 , 46 ]. Practitioners are further advised that misinformation and pseudoscience are appealing to those seeking certainty because they present information in absolutes, whereas medical science is often ambiguous and contingent. Health practitioners are also encouraged to learn how to message more clearly and to mimic the strategies of misinformation [ 45 ]. One study recommends that “practitioners familiarize themselves with the tools of scientific enquiry and consider the pros and cons of various conspiracy evaluation guidelines” [ 47 ]. Thompson [ 48 ] reports on the activity of health professional influencers and pedagogues in combating misinformation. However, the effectiveness of such social media influencers who are also health professionals remains unclear. At the same time, there is some acknowledgment in this body of literature that misinformation cannot simply be offset with facts, confirming the challenges, discussed earlier, of simply engaging in online refutation. Addressing misinformation also depends on meeting patients’ emotional needs [ 45 , 49 ].
In this context, the one-to-one patient-provider relationship in the practice setting is perceived as paramount [ 45 ]. As suggested by much of the research, source credibility, or trust, is understood to be the strongest driver of effective correction strategies [ 50 ]. It is argued that health care practitioners have the unique opportunity to guide patients toward high-quality, evidence-based medical information [ 10 ]. However, it is also noted that practitioners will need patience in their efforts to persuade patients to abandon strongly held self-beliefs, however harmful. Doing so may mean patients relinquishing membership of online communities that have become integral in their lives and even their identities. As noted earlier, belief in misinformation is often persistent in the face of evidence. Success is more likely when individuals are encouraged to reexamine their information sources, alongside new information providing additional context, rather than simply characterizing the individual’s beliefs as wrong [ 51 ]. Kyabaggu et al [ 5 ] commented that good health communication needs to be tailored to the underlying cause of the misinformation problem, and efforts should be made to take on board inequalities within populations to create accurate, low-barrier, targeted health risk messaging. Skafle et al [ 24 ] contended that to challenge misconceptions, false claims need to be openly addressed and discussed with both cultural and religious awareness in mind. Guidance for practitioners noted that while responding to patient questions about alternative or unproven therapies may become laborious, a strong bond of trust between health practitioner and patient gives a patient a feeling of being supported and increases their adherence to treatment [ 52 ]. Rather than waiting for patients to raise misinformation issues, health care practitioners are advised to anticipate and proactively address potential misinformation and myths with patients. For example, the mortality rate for pediatric cancer has risen during the COVID-19 pandemic because of delayed access to medical care, but misinformation related to COVID-19 may also be a contributing factor [ 53 ]. The literature highlights the challenge of navigating the information and misinformation and the need for health practitioners to communicate with their patients more effectively. However, such efforts are not always successful. Some of the factors that may prevent effective communication of good health information have already been raised in this paper. They are revisited and discussed in the next section, along with other stressors for health practitioners.
Stressors for Health Practitioners
Challenges for health practitioners include time pressures and the additional burdens placed on them during the COVID-19 pandemic. These additional pressures add to the issues health practitioners face in trying to mitigate the impact of misinformation. The following is a brief overview of these issues.
On the one hand, administrative burdens placed on practitioners frequently deny them time for dialogue with their patients [ 52 ]. On the other, in different contexts, practitioners may be coping with a lack of proper facilities; poor infrastructure for patient care; insufficient or ineffective personal protective equipment; lack of awareness among the general population; poor compliance with preventive methods; and the fear of being infected with the virus, as they too are exposed to misinformation. During the COVID-19 pandemic, health practitioners were considered more vulnerable than other workers to developing psychological problems and other stress-related disorders, as they treated patients confirmed with COVID-19 while also dealing with misinformation [ 54 ].
As noted above, practitioners are recommended to invest in developing high levels of patient trust and to proactively correct health misinformation. However, recommendations presuppose that health practitioners necessarily have the resources to do these things well. Some of the materials produced to educate patients are not always reliable or evidence based, resulting ultimately in a loss of trust on the part of patients [ 52 ]. In addition, as noted previously, health practitioners themselves are not necessarily immune from accepting health misinformation as credible. Evidence about the level of knowledge and understanding of COVID-19 among practitioners reveals its unevenness. A study of dentists and oral health practitioners’ knowledge about COVID-19 suggested that their knowledge was at a relatively high level [ 55 ]. By contrast, a study of 310 eye care professionals in Nepal revealed some knowledge but also some acceptance of misinformation. Symptoms of COVID-19 were known to 94% of participants, but only 49% of participants were aware of how the disease is transmitted. More significantly, 41% of participants believed that the consumption of hot drinks helps to destroy the virus, in contradiction to World Health Organization information. The mean overall “knowledge” performance score, as measured by the benchmarks set by the researchers, was 69.65% [ 56 ].
A qualitative study to investigate primary health care practitioners’ perceptions and understanding of the COVID-19 pandemic was conducted in KwaZulu-Natal, South Africa. The study collected data from 15 participants at 2 different clinics situated in rural KwaZulu-Natal. Participants comprised nurses, physiotherapists, pharmacists, community caregivers, social workers, and clinical associates. Data were collected through individual, in-depth face-to-face interviews using a semistructured interview guide. The participants reported prepandemic and pandemic experiences of fear or denial. There was a perception of poor preparation for the COVID-19 outbreak. The findings also revealed participants’ misperceptions regarding the nature of the COVID-19 pandemic. Researchers concluded that respondents’ misunderstandings regarding the pandemic were primarily a result of misinformation found on social media [ 57 ].
The discussion in this section so far has highlighted the significant potential of health practitioners in mitigating the impact of online health misinformation. However, it has also underlined factors that may militate against health practitioners’ ability to do so effectively. Not least of these is the issue of health practitioners’ own knowledge, which coexists with other stressors for health practitioners in combating misinformation. The discussion will now consider health information management (HIM) as a tool for supporting health practitioners’ knowledge base as one element in a multifaceted strategy for combating misinformation on the web.
HIM as a Mitigation Strategy
We have seen there is a need for health practitioners to be supported with evidence-based knowledge that they can share with patients. Kyabaggu et al [ 5 ] argued that the COVID-19 pandemic has demonstrated that in an infectious health crisis, the gathering of accurate and reliable data to assist with the public health response is essential. They highlighted the importance of HIM professionals in supporting contact tracing and syndromic surveillance, as well as in mapping and forecasting health data. They noted that the generation of health information supports the continuum of care and the setting of targets and indicators and aids the planning, monitoring, and evaluation of health programs locally and globally. The health information produced also underpins the development of equitable, efficient, and accessible health care systems, contributing to improving public health initiatives and outcomes. Kyabaggu et al [ 5 ] emphasized the importance of an area of HIM, currently in its early stages, that deals with gathering and identifying evidence about the structural inequalities that underlie the disparities in vulnerability to health misinformation discussed in this paper. The collection of rich, high-quality information, including patient-reported experience, outcome measures, and culturally appropriate identity data, can enable health practitioners and public health advisers serving the most disadvantaged and underrepresented communities to use more tools of advocacy for patients.
The authors noted that advances in technology, including artificial intelligence, have the potential to relieve some of the pressures and constraints on health practitioners working on the front line during crises such as the COVID-19 pandemic, allowing more time for one-to-one engagement with patients. Kyabaggu et al [ 5 ] advocated for the content expertise of health information managers to serve health practitioners by delivering patient-facing information triaging services; constructing user-friendly knowledge representations, such as data visualizations; and developing information interpretation tools, such as decision aids, plain language summaries, and supplementary explanatory information and metadata. Kyabaggu et al [ 5 ] identified the interdisciplinary underpinnings of HIM as essential in contributing to the educational, informational, and decision-making support for addressing current and future infodemic management crises.
Summary of Results
Within the literature, there is a consensus that there exists a significant problem of online health misinformation disseminated via the internet on social network platforms, often by online health communities. It is apparent that while users seek trustworthy sources of health information, they are unequally equipped to assess its credibility. This is partly because some groups lack sufficient levels of health and digital literacies, which may be exacerbated by concomitant social and economic inequalities. Reception of, and response to, online health misinformation is also shaped by users’ cultural contexts, values, and experiences, which may hinder trust in scientific institutions and governments. Evidence suggests that some demographics are more vulnerable to accepting health misinformation as credible and that health practitioners are unevenly prepared in the context of new global health crises, such as the COVID-19 pandemic. Furthermore, the evidence of disparities in positive and negative attitudes toward vaccination highlights a need to pay specific attention to regional and national settings, even in the current global context. Preexisting levels of local trust in vaccine providers may be a significant factor to consider. While the validity and reliability of YouGov polls are limited, nevertheless, the data from an admittedly narrow range of sources suggests that vaccine confidence may have become more fluctuating and potentially vulnerable to destabilization in the digital era.
While online mitigation strategies such as user correction and automatic detection may have their uses, their effectiveness is contested, and some studies suggest they may even be counterproductive. Our analysis of the available literature indicates that the effectiveness of these strategies varies and needs further evaluation [ 42 , 58 ]. The issue of online health misinformation is further complicated by the operation of malicious actors and politicization of the issue, particularly during the COVID-19 pandemic, militating against the equitable and trusted dissemination of evidence-based knowledge. The role of health practitioners in this context is a challenging one. Research suggests that on the one hand, they are still best placed, at the front line of care, to combat health misinformation with science-based knowledge and advice. On the other hand, the stressors identified in this review create barriers to their abilities to do this well. Constraints of time and lack of supporting infrastructure add to the knowledge deficit noted earlier. Our review underlines the complexity of the environment in which health practitioners operate and calls for greater support and resources to enable effective mitigation of health misinformation [ 59 ]. Investment in HIM at local and global levels could address all 3 deficits, creating the potential for health practitioners to enhance their capacity to build trust via knowledgeable one-to-one communication with patients.
Limitations
The limitations of this study are the following: First, the constraints of time and space have necessarily limited the scale and scope of the survey. Second, the study of online health misinformation is a growing field, and inevitably, the nature of the issue means that new evidence is emerging at a rapid rate. In particular, new knowledge and further reflection in the wake of the COVID-19 pandemic will continue to shed new light on the subject. Our study acknowledges these limitations and emphasizes the dynamic nature of the field.
Conclusions
Our survey of the literature on online health misinformation has revealed a complex and multifaceted context in which health practitioners must operate. As the world renormalizes following the pandemic, a collaborative global interdisciplinary effort to provide equitable access to timely, accurate, and complete health information will be needed to support health practitioners in combating the impact of online health misinformation. Academic research will need to be disseminated into the public domain in a way that is accessible to the public to counter misinformation and educate populations concerning how science is carried out. Our conclusions drawn from this review stress the urgency of effective strategies and collaborative efforts to mitigate the prevalence and impact of health misinformation on a global scale. Without strategies for equipping populations with the health and digital literacies required to interpret and use information appropriately, the prevalence of online health misinformation will continue to pose a threat to global public health efforts, disproportionately affecting vulnerable and resource-limited populations. Although social media platforms have a responsibility to correct misinformation, governments will need to engage in evidence-informed decision-making and invest in HIM to support frontline health practitioners in their work, enhance population health literacy, and strengthen evidence-informed decision-making at all levels.
Several issues for further investigation arise from the findings of this review. These include the following:
- The long-term impact of COVID-19 vaccine hesitancy
- Whether the COVID-19 pandemic has intensified or diminished information literacy, and the related question of whether the pandemic will incentivize health information literacy
- The effects of social and cultural differences on the long-term traction of future health misinformation
- Whether social and economic inequalities will become less or more pronounced in the face of a global pandemic
- The comparative effectiveness of strategies to enhance populations’ media and digital literacies to facilitate the mitigation of health misinformation and its effects
- The influence of state actors on the propagation of health misinformation on the web
- The extent to which academic research has been disseminated into the public domain in a way that is accessible to the public, and the effectiveness of strategies to do so to counter misinformation and educate populations concerning how science is carried out
Acknowledgments
This research was funded by the School of Computing and Communications at the Open University. It allowed researchers across several faculties to collaborate and build a research team that focused on the experience of health practitioners with misinformation and its impact on their job practice. The authors would also like to thank Tracie Farrell and Nashwa Ismail for their invaluable suggestions and recommendations, as well as their assistance in the article screening process.
Data Availability
The data analyzed in this study are derived from published articles available on Google Scholar. All articles included in the review are cited in the reference list. No additional data or code were collected or generated as part of this study.
Authors' Contributions
The study was conceptualized by DK; funding acquisition was managed by DK; data were curated by DK, AK, MM, and IK; formal analysis was conducted by DK and MM; the investigation was carried out by AK and MM; the methodology was designed by DK and MM; project administration was overseen by DK; resources were provided by DK; supervision was carried out by DK; validation was conducted by DK, AK, MM, and IK; visualization was handled by DK and MM; writing (original draft preparation) was done by DK; and writing (review and editing) was carried out by DK, AK, and MM. All authors reviewed and approved the final version.
Conflicts of Interest
None declared.
Detailed search strategy.
- Ismail N, Kbaier D, Farrell T, Kane A. The experience of health professionals with misinformation and its impact on their job practice: qualitative interview study. JMIR Form Res. Nov 02, 2022;6(11):e38794. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tully M, Bode L, Vraga EK. Mobilizing users: does exposure to misinformation and its correction affect users’ responses to a health misinformation post? Soc Media Soc. Dec 10, 2020;6(4):205630512097837. [ CrossRef ]
- Zhao Y, Da J, Yan J. Detecting health misinformation in online health communities: Incorporating behavioral features into machine learning based approaches. Inf Process Manage. Jan 2021;58(1):102390. [ CrossRef ]
- Wang Y, McKee M, Torbica A, Stuckler D. Systematic literature review on the spread of health-related misinformation on social media. Soc Sci Med. Nov 2019;240:112552. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kyabaggu R, Marshall D, Ebuwei P, Ikenyei U. Health literacy, equity, and communication in the COVID-19 era of misinformation: emergence of health information professionals in infodemic management. JMIR Infodemiology. 2022;2(1):e35014. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sutton J. Health communication trolls and bots versus public health agencies' trusted voices. Am J Public Health. Oct 2018;108(10):1281-1282. [ CrossRef ] [ Medline ]
- Kim S, Capasso A, Ali SH, Headley T, DiClemente RJ, Tozan Y. What predicts people's belief in COVID-19 misinformation? A retrospective study using a nationwide online survey among adults residing in the United States. BMC Public Health. Nov 18, 2022;22(1):2114. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morgan JC, Cappella JN. The effect of repetition on the perceived truth of tobacco-related health misinformation among U.S. adults. J Health Commun. Mar 04, 2023;28(3):182-189. [ CrossRef ] [ Medline ]
- Nan X, Wang Y, Thier K. Why do people believe health misinformation and who is at risk? A systematic review of individual differences in susceptibility to health misinformation. Soc Sci Med. Dec 2022;314:115398. [ CrossRef ] [ Medline ]
- Wood JL, Lee GY, Stinnett SS, Southwell BG. A pilot study of medical misinformation perceptions and training among practitioners in North Carolina (USA). Inquiry. 2021;58:469580211035742. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Broniatowski DA, Jamison AM, Qi S, AlKulaib L, Chen T, Benton A, et al. Weaponized health communication: Twitter bots and Russian trolls amplify the vaccine debate. Am J Public Health. Oct 2018;108(10):1378-1384. [ CrossRef ] [ Medline ]
- Mokhtari H, Mirzaei A. The tsunami of misinformation on COVID-19 challenged the health information literacy of the general public and the readability of educational material: a commentary. Public Health. Oct 2020;187:109-110. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schmid P, Altay S, Scherer LD. The psychological impacts and message features of health misinformation - a systematic review of randomized controlled trials. Eur Psychol. Jul 2023;28(3):162-172. [ CrossRef ]
- Southwell BG, Otero Machuca J, Cherry ST, Burnside M, Barrett NJ. Health misinformation exposure and health disparities: observations and opportunities. Annu Rev Public Health. Apr 03, 2023;44(1):113-130. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Westberry C, Palmer XL, Potter L. Social media and health misinformation: a literature review. In: Arai K, editor. Proceedings of the Future Technologies Conference (FTC) 2023, Volume 3. FTC 2023. Lecture Notes in Networks and Systems, vol 815. Cham, Switzerland. Springer; 2023.
- Suarez-Lledo V, Alvarez-Galvez J. Prevalence of health misinformation on social media: systematic review. J Med Internet Res. Jan 20, 2021;23(1):e17187. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Borges do Nascimento IJ, Pizarro AB, Almeida J, Azzopardi-Muscat N, Gonçalves MA, Björklund M, et al. Infodemics and health misinformation: a systematic review of reviews. Bull World Health Organ. Sep 01, 2022;100(9):544-561. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee JJ, Kang K, Wang MP, Zhao SZ, Wong JYH, O'Connor S, et al. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J Med Internet Res. Nov 13, 2020;22(11):e22205. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Larson HJ, Broniatowski DA. Why debunking misinformation is not enough to change people's minds about vaccines. Am J Public Health. Jun 2021;111(6):1058-1060. [ CrossRef ] [ Medline ]
- Bapaye JA, Bapaye HA. Demographic factors influencing the impact of coronavirus-related misinformation on WhatsApp: cross-sectional questionnaire study. JMIR Public Health Surveill. Jan 30, 2021;7(1):e19858. [ FREE Full text ] [ CrossRef ] [ Medline ]
- McKernon E. Fake news and the public. Harper's. Oct 1925. URL: https://harpers.org/archive/1925/10/fake-news-and-the-public/ [accessed 2024-07-30]
- Hotez P. The physician-scientist: defending vaccines and combating antiscience. J Clin Invest. Apr 29, 2019;129(6):2169-2171. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dyer C. Lancet retracts Wakefield's MMR paper. BMJ. Mar 02, 2010;340:c696. [ CrossRef ] [ Medline ]
- Skafle I, Nordahl-Hansen A, Quintana DS, Wynn R, Gabarron E. Misinformation about COVID-19 vaccines on social media: rapid review. J Med Internet Res. Aug 04, 2022;24(8):e37367. [ FREE Full text ] [ CrossRef ] [ Medline ]
- New Yahoo News/YouGov coronavirus poll: almost 1 in 5 say they won't get vaccinated. Yahoo News. URL: https://www.yahoo.com/news/new-yahoo-news-you-gov-coronavirus-poll-almost-one-in-five-say-they-wont-get-vaccinated-143852222.html [accessed 2024-08-06]
- Peretti-Watel P, Verger P, Raude J, Constant A, Gautier A, Jestin C, et al. Dramatic change in public attitudes towards vaccination during the 2009 influenza A(H1N1) pandemic in France. Euro Surveill. Oct 31, 2013;18(44):20623. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Reuters. ‘They’re killing people’: Biden slams Facebook for Covid disinformation. The Guardian. Jul 21, 2021. URL: https://www.theguardian.com/media/2021/jul/17/theyre-killing-people-biden-slams-facebook-for-covid-misinformation [accessed 2024-07-30]
- Britain has had enough of experts, says Gove. Financial Times. URL: https://www.ft.com/content/3be49734-29cb-11e6-83e4-abc22d5d108c [accessed 2024-07-30]
- US news roundup: 19-25 August. Research Professional News. Aug 25, 2022. URL: https://www.researchprofessionalnews.com/rr-news-usa-2022-8-us-news-roundup-19-25-august/ [accessed 2024-07-30]
- Gruzd A, Mai P, Soares FB. How coordinated link sharing behavior and partisans' narrative framing fan the spread of COVID-19 misinformation and conspiracy theories. Soc Netw Anal Min. 2022;12(1):118. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. Mar 09, 2018;359(6380):1146-1151. [ CrossRef ] [ Medline ]
- Wang Y. Systematic review on the social mechanism of health misinformation dissemination in the internet era. Eur J Public Health. Nov 2018;28(suppl_4):cky213.194. [ CrossRef ]
- Framework for information literacy for higher education. American Library Association. 2016. URL: http://www.ala.org/acrl/sites/ala.org.acrl/files/content/issues/infolit/framework1.pdf [accessed 2024-07-30]
- Quraishi Z. Addressing mental health, misinformation, and religious tensions among South Asian students across California higher education during the COVID-19 pandemic: A qualitative research study. Heliyon. Jun 2023;9(6):e16396. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhou J, Xiang H, Xie B. Better safe than sorry: a study on older adults' credibility judgments and spreading of health misinformation. Univers Access Inf Soc. Aug 04, 2022;22(3):1-10. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Goldenberg MJ. Vaccine Hesitancy: Public Trust, Expertise, and the War on Science. Pittsburgh, PA. University of Pittsburgh Press; 2021.
- Ittefaq M. "It frustrates me beyond words that I can't fix that": health misinformation correction on Facebook during COVID-19. Health Commun. Nov 12, 2023;12:1-11. [ CrossRef ] [ Medline ]
- Mourali M, Drake C. The challenge of debunking health misinformation in dynamic social media conversations: online randomized study of public masking during COVID-19. J Med Internet Res. Mar 02, 2022;24(3):e34831. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Weinzierl MA, Harabagiu SM. Automatic detection of COVID-19 vaccine misinformation with graph link prediction. J Biomed Inform. Dec 2021;124:103955. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Petty RE, Cacioppo JT. Elaboration likelihood model of persuasion. In: Communication and Persuasion. Springer Series in Social Psychology. New York, NY. Springer; 1986.
- Cowles K, Miller R, Suppok R. When seeing isn't believing: navigating visual health misinformation through library instruction. Med Ref Serv Q. 2024;43(1):44-58. [ CrossRef ] [ Medline ]
- Nabożny A, Balcerzak B, Morzy M, Wierzbicki A, Savov P, Warpechowski K. Improving medical experts' efficiency of misinformation detection: an exploratory study. World Wide Web. 2023;26(2):773-798. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Barve Y, Saini JR. Detecting and classifying online health misinformation with 'Content Similarity Measure (CSM)' algorithm: an automated fact-checking-based approach. J Supercomput. 2023;79(8):9127-9156. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Broniatowski D, Gu J, Jamison AM, Simons JR. Facebook's architecture undermines vaccine misinformation removal efforts. arXiv. Preprint posted online Feb 4, 2022. [ FREE Full text ] [ CrossRef ]
- Russell N. Misinformation during COVID: how should nurse practitioners respond? J Nurse Pract. Jun 2021;17(6):763-764. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wilner T, Holton A. Breast cancer prevention and treatment: misinformation on Pinterest, 2018. Am J Public Health. Oct 2020;110(S3):S300-S304. [ CrossRef ] [ Medline ]
- MacFarlane D, Hurlstone MJ, Ecker UK. Protecting consumers from fraudulent health claims: A taxonomy of psychological drivers, interventions, barriers, and treatments. Soc Sci Med. Aug 2020;259:112790. [ CrossRef ] [ Medline ]
- Thompson JD. Public health pedagogy and digital misinformation: health professional influencers and the politics of expertise. J Sociol. Sep 28, 2022;59(3):646-663. [ CrossRef ]
- Gunter J. Medical misinformation and the internet: a call to arms. Lancet. Jun 08, 2019;393(10188):2294-2295. [ CrossRef ] [ Medline ]
- Sui Y, Zhang B. Determinants of the perceived credibility of rebuttals concerning health misinformation. Int J Environ Res Public Health. Mar 02, 2021;18(3):1345. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Collier R. Containing health myths in the age of viral misinformation. CMAJ. May 14, 2018;190(19):E578. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peterson JS, Swire-Thompson B, Johnson SB. What is the alternative? Responding strategically to cancer misinformation. Future Oncol. Sep 2020;16(25):1883-1888. [ CrossRef ] [ Medline ]
- Guidry JP, Miller CA, Ksinan AJ, Rohan JM, Winter MA, Carlyle KE, et al. COVID-19-related misinformation among parents of patients with pediatric cancer. Emerg Infect Dis. Mar 2021;27(2):650-652. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ali S, Khalid A, Zahid E. Is COVID-19 immune to misinformation? A brief overview. Asian Bioeth Rev. Jun 2021;13(2):255-277. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jafari A, Mohammadpour M, Ghanbarzadegan A, Rossi-Fedele G, Bastani P. Oral health practitioners' knowledge, attitude, and awareness about coronavirus: A systematic review and meta-analysis. J Educ Health Promot. 2021;10:39. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sanyam SD, Sah SK, Chaudhary P, Burton MJ, Hoffman JJ. Knowledge and awareness-based survey of COVID-19 within the eye care profession in Nepal: Misinformation is hiding the truth. PLoS One. 2021;16(7):e0254761. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nxumalo CT, Mchunu GG. A qualitative study to explore primary health care practitioners' perceptions and understanding regarding the COVID-19 pandemic in KwaZulu-Natal, South Africa. Afr J Prim Health Care Fam Med. Nov 26, 2021;13(1):e1-e11. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Abbasi K. Where now in the danse macabre of COVID-19 and misinformation? BMJ. Aug 17, 2023;382:1884. [ CrossRef ]
- Pesko MF, Cummings KM, Douglas CE, Foulds J, Miller T, Rigotti NA, et al. United States public health officials need to correct e-cigarette health misinformation. Addiction. May 2023;118(5):785-788. [ CrossRef ] [ Medline ]
Abbreviations
| content similarity measure |
| elaboration likelihood model |
| health information management |
| National Health Service |
Edited by G Eysenbach, T Leung; submitted 15.04.22; peer-reviewed by G Nneji, S-F Tsao; comments to author 07.06.22; revised version received 29.09.22; accepted 12.07.24; published 19.08.24.
©Dhouha Kbaier, Annemarie Kane, Mark McJury, Ian Kenny. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 19.08.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
COMMENTS
Stress reappraisal and mindset interventions have high potential to assist in stress management during the COVID‐19 pandemic based on their demonstrated efficacy in laboratory and selected applied contexts (Crum et al., 2013, 2017; Keech et al., 2019). Research demonstrating that such interventions are highly translatable and have consistent ...
Abbott (2021) investigated stress caused by the COVID-19 pandemic and its related consequences and found that there is an increase in prevalence of stress, anxiety, and depression in the U.S. population from 11% to 42% due to this pandemic. The surge in stress among people is also during the rise of new COVID-19 covariant cases.
The prevalence of depression, anxiety, physical discomfort, insomnia and post-traumatic stress disorder (PTSD) during the COVID-19 pandemic: Having a childbearing age: During the COVID/19 pandemic, pregnant women had lower scores of symptoms of depression, anxiety, and PTSD (all p < 0.05) compared to non-pregnant women. Sade et al., 2020
Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69 ...
The first step to lower your stress is to keep a daily schedule. Make or maintain healthy habits and routines. This can help boost your mood and energy levels. Make sleep a priority. Get up at about the same time every day. Go to bed at about the same time every day. Make sure that you are getting enough restful sleep.
Play with puzzles, a board game, do a treasure hunt, tackle a project, reorganize something, or start a new book that is unrelated to coronavirus coverage. Connect with others. "I can't stress ...
Background Individuals face increased psychological distress during the COVID-19 pandemic. However, it's unknown whether choice of coping styles are influenced by COVID-19 in addition to known predictors. Methods Data from 26,016 UK adults in the UCL COVID-19 Social Study were analysed from 12/4/2020 15/5/2020. Regression models were used to identify predictors of coping styles (problem ...
The COVID-19 virus knows all about the human psyche. The virus is aware that we experience stress and become anxious when we keep a distance from other people and are forced to isolate ourselves from direct, physical contact with the people we love and cherish. Under conditons of stress and as we become more anxious, our vulnerability also ...
Introduction. The emergence of an atypical coronavirus, SARS-CoV-2, instigated a global outbreak of Coronavirus Disease 2019 [COVID-19; e.g., ()].Following identification of the earliest cases of COVID-19 in December 2019, the World Health Organization declared the viral outbreak a health emergency of international concern on January 30, 2020, and then a global pandemic <2 months later.
Background In the case of people who carry an increased number of anxiety traits and maladaptive coping strategies, psychosocial stressors may further increase the level of perceived stress they experience. In our research study, we aimed to examine the levels of perceived stress and health anxiety as well as coping styles among university students amid the COVID-19 pandemic. Methods A cross ...
Ask others you trust how they have coped with COVID-19 stress. Breathe through COVID-19 stress by inhaling and exhaling slowly and deeply. Soothe COVID-19 stress by protecting time to relax. Share ...
The study addresses a gap in research on media use during the COVID-19 pandemic, focusing on the overlooked role of short video social media platforms in stress management. It builds on transactional stress model and coping flexibility to advance the understanding of the strategy-situation fit, particularly the alignment of coping strategies ...
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
angry during a crisis. Talking to people you trust can help. Contact your friends and family. Don't use smoking, alcohol or other drugs to deal with your emotions. If you feel overwhelmed, talk to a health worker or counsellor. Have a plan, where to go to and how to seek help for physical and mental health needs if required.
COVID-19 pandemic is associated with stress related mental illnesses. Moderate to severe anxiety and depression is present in a considerable proportion. Almost one third of respondents have possibility of posttraumatic stress disorder. Students, young people, single and health care professionals are more vulnerable.
As the pandemic persists, we are increasingly seeing the effects of prolonged stress. Prolonged stress has negative mental, emotional, and physical effects. With awareness and strategic ...
Stress reduction tips for COVID-19. "Rather than dwell on nervousness, focus on the things you can control," Flanagan suggests. "When you move the locus of control from something outside yourself to inside yourself, you powerfully reduce anxiety and boost confidence.". He suggests the following steps to regain control and reduce stress.
The coronavirus disease 2019 (COVID-19) pandemic has placed unprecedented stress on the health care system globally, revealing the interconnectedness and fragility of its ecosystem. The resultant overwhelming burden of illness and mortality has threatened operations of health care institutions worldwide and the physical, emotional, and financial health of their workers.1 Health care workers ...
The sample items were statements such as "Because of COVID-19, I find it difficult to relax." Participants rated their perceived stress during the peak time of COVID-19, ranging from 1 (strongly disagree) to 5 (strongly agree). The scale consisted of seven items. Cronbach's α for perceived stress was 0.905 in the present study.
"Keep Calm and Carry On" may not be the best mantra when it comes to managing stress in the context of COVID-19. A new study by University of Toronto researchers finds that cognitive reappraisal, a common strategy used to manage the stress of a health threat, may end up creating a greater risk to public health during the pandemic. To help manage stress, people often employ the coping ...
Once you have assessed your threat, then it is important to…. 2. Identify what you can control. When we encounter stress, any stress, it is important that we ask ourselves if we can do anything ...
Feelings of fear, anger, sadness, worry, numbness, or frustration. Changes in appetite, energy, desires, and interests. Trouble concentrating and making decisions. Nightmares or problems sleeping. Physical reactions, such as headaches, body pains, stomach problems, or skin rashes. Worsening of chronic health problems and mental health conditions.
Background Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the 'coping reservoir' model of wellbeing. Methods In synchronous ...
Background: This scoping review accompanies our research study "The Experience of Health Professionals With Misinformation and Its Impact on Their Job Practice: Qualitative Interview Study." It surveys online health misinformation and is intended to provide an understanding of the communication context in which health professionals must operate.