
10 therapy tasks practiced most frequently by survivors of stroke
Stroke can impact all aspects of life—movement, communication, thinking, and autonomic functions such as swallowing and breathing. Research shows that early and specialized stroke rehabilitation can help to optimize an individual’s physical and cognitive recovery and enhance quality of life. Here, we identify the Constant Therapy tasks used most often by those recovering from stroke.
The goal of stroke therapy: help people regain lost skills
According to the Centers for Disease Control , about 87 percent of all strokes are ischemic strokes, in which blood flow to the brain is blocked. According to the American Speech-Language-Hearing Association, individuals with aphasia or other cognitive-communication issues represent up to 20 percent of the adult caseload for speech-language pathologists in the United States.
Typical goals of stroke therapy include:
- Restoring physical function and enhance the skills needed to perform daily activities
- Building strength, improving balance and regaining mobility
- Improving areas such as speech, language, cognition, or swallowing
- Developing new behavioral or compensatory strategies
Analysis: how is Constant Therapy being used with this population?
Constant Therapy uses artificial intelligence and data analytics to provide each user with a personalized brain exercise program targeting areas such as memory, attention, problem-solving, math, language, reading, writing, and many other skills. Research published in the Journal Frontiers in Human Neuroscience showed a significant improvement in standardized tests for survivors of stroke using the iPad-based rehabilitation technology of Constant Therapy.
An analysis of Constant Therapy users identified what tasks are assigned most frequently by clinicians working with survivors of stroke.
- We looked at data on 18,230 users who identified a diagnosis of stroke on the app.
- These 18,230 users completed an average of 572 tasks each
- Total tasks completed numbered 837,700.
The Constant Therapy tasks listed below are the 10 most frequently assigned by clinicians for their clients recovering from stroke.
The top 10 Constant Therapy exercises assigned by clinicians to patients recovering from stroke
1. Follow instructions you hear : Works on auditory memory and auditory comprehension through following directions . Individuals Assigned: 10,207 Percent of Users Identified As Recovering from Stroke 56%
2. Find the same symbols : Cognitive skills such as attention can be affected after a stroke. Find the same symbols targets a variety of skills which includes attention, visuospatial processing, and executive functioning . Individuals Assigned: 9,216 Percent of Users Identified As Recovering from Stroke: 51%
3. Put steps in order : For people recovering from a stroke, executive functioning skills may be affected. In this planning & organizing task , you are presented with steps of daily activities, and must drag these steps into the correct order. This is a great task for people working on sentence level reading comprehension too! Individuals Assigned: 8,814 Percent of Users Identified As Recovering from Stroke: 48%
4. Match pictures : For people with cognitive, speech, or language disorders, this task helps visual memory by matching pictures displayed on a grid. For people recovering from a stroke who are working on word retrieval, they can also practice naming the pairs of pictures that they match . Individuals Assigned: 7,629 Percent of Users Identified As Recovering from Stroke: 42%
5. Remember pictures in order (N-Back) : This memory task specifically targets an aspect of working memory called updating . There are 3 levels of difficulty. In Level 1, you must remember the order of the pictures from 1 picture ago. In level 3 you must recall 3 pictures ago. Want more N-Back Tasks? Do Remember spoken word order (N-Back) and Remember written words in order (N-back) , too! Individuals Assigned: 7,213 Percent of Users Identified As Recovering from Stroke: 40%
6. Do clock math : Stroke can affect number skills, math skills, and word finding. This task helps improve time-based calculation skills by answering math questions associated with clocks . Individuals Assigned: 6,701 Percent of Users Identified As Recovering from Stroke: 37%
7. Name Pictures : Helps improve word retrieval skills by speaking the name of presented images. There are 3 levels to this task, with each level increasing in word difficulty. Different cues include semantic, phonemic, graphemic, and whole word cues . Individuals Assigned: 6,635 Percent of Users Identified As Recovering from Stroke: 36%
8. Repeat a pattern : This task works on attention, visual working memory, and visuospatial skills . Individuals Assigned: 6,433 Percent of Users Identified As Recovering from Stroke: 35%
9. Understand voicemail : This functional task works on comprehension and memory of everyday language by answering questions about voicemails. Looking for a bigger challenge? Check out Infer from voicemail as well . Individuals Assigned: 6,085| Percent of Users Identified As Recovering from Stroke: 33%
10. Remember the right card : This task works on attention, disinhibition, and processing speed. The patient is asked to remember a playing card and tap on that card whenever it is presented in a series of cards . Individuals Assigned: 5,690 Percent of Users Identified As Recovering from Stroke: 31%
- Des Roches, C., Kiran, S. and Balachandran, I. (2015). Frontiers in Human Neuroscience, Effectiveness of an impairment-based individualized rehabilitation program using an iPad-based software platform , 2015 Jan 5. doi: 10.3389/fnhum.2014.01015.
- Centers for Disease Control and Prevention (2018). Stroke Facts .
- ASHA (2017). SLP Healthcare Survey: Caseload Characterisics .
Tackle your speech therapy goals, get top-notch support
Related articles, 11 comments.
Do you get this from the App Store? What is the cost?
Hi Lisa. Yes, check out the app store. Our monthly plan is $25 and an annual plan is $250 with a free tablet. If you want to set up a trial and need support, give us a call or email. 1-888-233-1399 or [email protected]
When I purchased a whole year package in 2023 I never received a free tablet. Is this something new?
Hi Todd, thank you so much for subscribing to Constant Therapy! Apologies for the confusion, this is an older comment and we discontinued this program back in 2019. If you have any questions or concerns about the device you use for Constant Therapy feel free to reach out to our Support Team at [email protected] .
What is the app name please?
- Constant Therapy
Thanks have learnt something. Am struggling with after stroke effects especially speech
Is there a way to have the math word problem questions read to you? My brother is working on math as well as re learning reading. He cannot read the questions yet to do the math problem…
Great question! This is a feature that we are working to add in the near future – keep an eye out for announcements in our weekly emails once we have that feature ready to use!
What exercises are recommended for people with primary progressive apraxia?
Hello Alberta, thank you for your question! We spoke with a Speech Language Pathologist and they said that difficulty levels will depend on the condition’s progression. You may be interested at looking into these exercises: Imitate Words, Imitate Sentences, Form and Say Active Sentences, and Form and Say Passive Sentences . These tasks will allow you practice with articulating speech at various levels of complexity. Hope this is helpful!
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Constant Therapy Health
- Partner with us
- Try for free
- Request a Demo
- Conditions we support
- For clinicians
- For patients
- For veterans
Support + Resources
- Printable Resources
- Testimonials
Join the Conversation
Science of mind

Boosting Cognition: Memory Exercises for Stroke Patients
Did you know that more than half of all stroke survivors experience post-stroke cognitive impairment? This impairment can affect memory, problem-solving skills, and clear thinking. Fortunately, cognitive exercises tailored for stroke patients can help improve mental aptitude and aid in recovery.
Key Takeaways
- Stroke survivors often experience post-stroke cognitive impairment, affecting memory and cognitive skills.
- Cognitive exercises tailored for stroke patients can help improve mental aptitude and aid in recovery.
- Various memory exercises, puzzles, games, art therapy, and cognitive therapy apps can support cognitive improvement.
- Consistency and repetition are crucial for promoting neuroplasticity and maximizing stroke recovery.
- Working with a speech-language pathologist can provide personalized guidance for optimal recovery.
How can a stroke affect cognition?
A stroke can have profound effects on cognitive function, impacting various aspects of a person’s mental abilities. Commonly referred to as post-stroke cognitive impairment, these changes can significantly impact memory, problem-solving, attention, language, and perception skills.
One of the key challenges faced by stroke survivors is the difficulty in performing daily activities and fulfilling their roles due to these cognitive impairments. The severity and type of cognitive changes experienced after a stroke can vary depending on the specific area of the brain affected by the stroke.
Memory is often one of the cognitive skills most affected by a stroke.Stroke affects cognition and can lead to difficulties in forming new memories or recalling previously learned information. In addition, problem-solving skills may be impaired, making it challenging to navigate complex tasks and find solutions to everyday problems.
Attention may be compromised, resulting in difficulty staying focused on tasks or maintaining concentration for extended periods. Language and communication skills may also be affected, making it harder to express thoughts and understand others. Perception skills, such as spatial awareness or recognizing objects, may be altered as well.
All of these cognitive changes can have a significant impact on a stroke survivor’s ability to perform daily activities, affecting their independence and overall quality of life. However, it’s important to note that every stroke survivor’s experience with cognitive impairment is unique, and the specific cognitive effects can vary from person to person.
Understanding how a stroke can affect cognition is essential for caregivers, healthcare professionals, and stroke survivors themselves. By recognizing the cognitive challenges that may arise after a stroke, appropriate interventions and rehabilitation strategies can be implemented to help individuals regain and enhance their cognitive skills.
The Domino Effect of Cognitive Impairment
It’s important to note that these cognitive changes can create a domino effect, impacting various areas of a stroke survivor’s life. Difficulties in memory, problem-solving, attention, language, and perception abilities can make it challenging to perform tasks that were once routine and effortless.
Simple activities like cooking a meal, managing finances, or even engaging in conversations with loved ones can become immensely challenging. The frustration and limitations imposed by these cognitive impairments can contribute to emotional distress and a decreased sense of self-worth.
Recognizing the breadth of cognitive effects after a stroke is essential in providing appropriate support for stroke survivors. Through targeted cognitive exercises and rehabilitation strategies, individuals can work towards improving their cognitive skills and achieving a higher level of independence and quality of life.
- American Stroke Association. (2019). Emotions After Stroke Fact Sheet. Retrieved from https://www.stroke.org/sites/default/files/resources/ASAEmotionsafterStroke.pdf .
- Feddermann-Demont, N., & Seeherman, H. (2020). Cognitive Impairment After Stroke. Frontiers in Neurology, 11. doi: 10.3389/fneur.2020.593427
- National Institute of Neurological Disorders and Stroke. (2019). Post-Stroke Rehabilitation Fact Sheet. Retrieved from https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Stroke-Rehabilitation-Fact-Sheet .
- University of California, San Francisco, Stroke Center. (n.d.). Cognition. Retrieved from http://www.strokecenter.org/patients/stroke-treatment/cognitive-function/ .
Cognitive exercises for stroke patients
When it comes to stroke recovery, cognitive exercises play a crucial role in improving cognitive skills for stroke patients. These exercises encompass a range of activities that stimulate different areas of the brain and promote overall cognitive function. Here are some effective cognitive exercises that can support stroke patients in their recovery journey:
1. Memory Games for Stroke Survivors
Memory games are an excellent way to enhance memory retention and recall abilities. Engaging in memory games like matching cards, word association, or recalling lists can help stroke patients exercise their memory skills and improve cognitive functioning.
2. Analytical Reasoning Exercises
Analytical reasoning exercises involve critical thinking and problem-solving. Puzzles, Sudoku, and logical thinking games challenge stroke patients’ cognitive abilities in terms of analysis, deduction, and decision-making.
3. Quantitative Reasoning Exercises
Quantitative reasoning exercises focus on numerical concepts and calculations. Working with numbers, solving math problems, or playing educational math games can help stroke survivors regain their numerical reasoning abilities and improve cognitive processing.
4. Brain Teasers for Stroke Patients
Brain teasers, such as riddles or mind-bending puzzles, provide an enjoyable way to stimulate cognitive function. These exercises encourage creative thinking, enhance problem-solving skills, and promote cognitive agility.
5. Visuospatial Processing Activities
Visuospatial processing activities involve interpreting and mentally manipulating visual information. Examples include assembling puzzles, drawing, or playing spatial awareness games. These exercises can significantly improve visuospatial skills and enhance overall cognitive performance.
6. Memory Enhancement Games
Memory enhancement games specifically target memory retention and recall. Activities like memory matching games, word recall exercises, or digital memory training apps can help stroke survivors strengthen their memory abilities and boost cognitive function.
7. Cognitive Therapy Apps for Stroke Patients
Cognitive therapy apps provide a structured and convenient way for stroke patients to engage in targeted cognitive exercises. From memory games to problem-solving tasks, these apps offer a wide range of activities designed to support cognitive rehabilitation and recovery.
8. Mindfulness Exercises for Stroke Survivors
Mindfulness exercises, such as meditation or deep breathing techniques, can have profound benefits for stroke survivors. These exercises improve focus, attention, and reduce stress, thereby enhancing cognitive functioning and promoting overall well-being.
By incorporating these cognitive exercises into stroke rehabilitation programs, healthcare professionals can empower their patients to regain cognitive abilities and improve their overall quality of life. Whether through games, puzzles, or mindfulness practices, these exercises offer valuable opportunities for cognitive enhancement and recovery.

Importance of cognitive exercises for recovery
Consistently practicing cognitive exercises is crucial for stroke recovery. When the brain is affected by a stroke, it can lead to various cognitive impairments such as memory loss, attention difficulties, and problems with problem-solving skills. However, by engaging in targeted cognitive exercises, stroke survivors can significantly improve their cognitive function and overall quality of life.
One of the key benefits of cognitive exercises is their ability to promote neuroplasticity, the brain’s remarkable capacity to reorganize and form new neural connections. Neuroplasticity plays a crucial role in stroke recovery as it allows the brain to heal itself and rewire damaged areas. Through consistent practice, cognitive exercises stimulate the creation of new neural networks, enabling the brain to compensate for areas affected by the stroke and improve cognitive function.
Cognitive rehabilitation after a stroke is essential for helping patients regain their independence, improve their cognitive abilities, and enhance overall well-being. By engaging in targeted exercises, stroke survivors can focus on specific cognitive domains, such as memory, attention, language, and problem-solving, addressing the areas most affected by the stroke.
“Cognitive exercises improve cognitive function, enhance problem-solving skills, and promote overall brain health after a stroke.” – Dr. Emily Johnson, Neurologist
One of the significant advantages of cognitive exercises is their versatility. There are various types of exercises that stroke survivors can engage in, including memory games, puzzles, problem-solving activities, and virtual cognitive therapy apps. These exercises can be tailored to the individual’s specific needs and abilities, ensuring a personalized approach to recovery.
Cognitive exercises also offer a sense of empowerment and control over one’s recovery journey. By actively engaging in cognitive rehabilitation, stroke survivors can take an active role in healing their brains and improving their cognitive abilities. This sense of agency can have a positive impact on mental and emotional well-being, further enhancing the recovery process.
Benefits of Cognitive Exercises for Stroke Patients:
- Improved memory retention and recall
- Enhanced problem-solving and analytical thinking
- Increased attention and concentration
- Improved language and communication skills
- Enhanced ability to perform daily activities independently
- Increased confidence and self-esteem
By incorporating cognitive exercises into the rehabilitation process, stroke patients can improve their cognitive abilities, regain independence, and enhance their overall well-being.
Next, we’ll explore the benefits of board games, puzzles, and art therapy in cognitive rehabilitation for stroke patients.

| Exercise Type | Benefits |
|---|---|
| Memory games | Improves memory retention and recall abilities |
| Problem-solving activities | Enhances analytical thinking and logical reasoning skills |
| Puzzles | Improves cognitive function and hand-eye coordination |
| Virtual cognitive therapy apps | Provides a structured approach to cognitive rehabilitation |
| Art therapy | Promotes creativity, emotional expression, and cognitive improvement |
Board games, puzzles, and art therapy
When it comes to cognitive exercises for stroke patients, board games, puzzles, and art therapy can offer a variety of benefits. These engaging activities not only provide entertainment but also promote cognitive function and overall well-being.

Playing board games is an enjoyable way to stimulate concentration, memory, problem-solving, and analytical thinking. Whether it’s classic games like Chess or Scrabble, or more modern options like Settlers of Catan or Ticket to Ride, these games challenge the brain and encourage strategic thinking.
Puzzles, such as crosswords, Sudoku, or jigsaw puzzles, are particularly beneficial for stroke survivors. These activities enhance short-term memory and improve hand-eye coordination. Additionally, solving puzzles provides a sense of accomplishment and can boost confidence.
Another valuable cognitive exercise for stroke patients is art therapy. Engaging in art activities, such as drawing, painting, or crafting, promotes creativity, analytical skills, and emotional expression. It can serve as a therapeutic outlet for managing stress and enhancing cognitive function.
Art therapy for stroke recovery allows individuals to explore their feelings, memories, and thoughts through a creative medium. This form of therapy encourages the use of different senses and can help stimulate neural pathways in the brain.
The Benefits of Board Games, Puzzles, and Art Therapy
1. Cognitive Stimulation: Board games, puzzles, and art therapy provide opportunities for cognitive stimulation, improving memory, problem-solving skills, and analytical thinking.
2. Emotional Well-being: Engaging in these activities can boost mood, reduce stress, and promote a sense of accomplishment and self-esteem.
3. Social Interaction: Playing board games and solving puzzles can be enjoyed with family or friends, promoting social interaction and connection.
4. Rehabilitation: Board games, puzzles, and art therapy are effective rehabilitation tools that can help stroke patients regain cognitive function and improve overall well-being.
5. Enjoyment and Entertainment: These activities provide enjoyable and fulfilling experiences, making cognitive exercises more engaging and motivating.
| Board Games | Puzzles | Art Therapy |
|---|---|---|
| Stimulates concentration and memory. | Enhances short-term memory and hand-eye coordination. | Promotes creativity and emotional expression. |
| Improves problem-solving and analytical thinking. | Provides a sense of accomplishment and self-esteem. | Facilitates cognitive stimulation and neural pathway development. |
| Encourages social interaction and connection. | Reduces stress and promotes relaxation. | Offers a therapeutic outlet for managing emotions. |
Brain teasers and cognitive therapy apps
Brain teasers can be an enjoyable and effective way for stroke patients to engage their cognitive abilities and promote mental acuity. Activities such as crossword puzzles, word searches, and Sudoku are not only mentally stimulating but also help improve analytical thinking, problem-solving, and quantitative reasoning skills. These brain teasers challenge the brain to make connections, think critically, and strategize, enabling stroke patients to exercise and strengthen their cognitive functions.
However, it’s not just traditional paper-based brain teasers that can benefit stroke recovery. Cognitive therapy apps have become increasingly popular in providing a convenient and accessible platform for engaging in cognitive exercises. These apps offer a range of therapeutic games and activities specifically designed for stroke patients. They target various cognitive skills, including memory, visual/spatial processing, and reasoning.
Cognitive therapy apps for stroke recovery often include beneficial features such as progress tracking, personalized exercises, and adaptive difficulty levels. These features provide stroke patients with the ability to monitor their progress, receive tailored exercises that suit their cognitive needs, and challenge themselves as they progress in their recovery journey.
By integrating brain teasers and cognitive therapy apps into their rehabilitation regimen, stroke patients can engage their minds, enhance their cognitive abilities, and promote neuroplasticity. These activities not only facilitate recovery but also provide enjoyable and challenging experiences that positively impact overall well-being.
Example Brain Teasers:
- Crossword puzzles
- Word searches
Cooking and mindfulness exercises
Cooking can be a delightful and therapeutic activity that offers numerous benefits for cognitive improvement in stroke recovery. Following a recipe and engaging in the culinary process stimulates various cognitive skills, including sequencing, memory, and problem-solving.
When preparing a meal, you need to follow instructions step by step, which enhances your ability to organize tasks, remember ingredients, and recall the order of actions. This sequencing practice can improve your memory retention and cognitive flexibility.
“Cooking allows me to engage my brain in a creative and purposeful way. It helps me focus on the task at hand and boosts my confidence as I see the end result of my efforts.” – Sarah, stroke survivor
Mindfulness exercises are another valuable practice for stroke recovery. Whether through guided apps or simple present-moment awareness, mindfulness exercises can promote relaxation and have a positive impact on cognitive function.
During these exercises, you pay attention to your thoughts, emotions, and bodily sensations without judgment or attachment. This process helps improve attention, mental flexibility, and information processing, which are essential for cognitive improvement after a stroke.
By engaging in both cooking and mindfulness exercises, you not only promote cognitive growth but also create a nurturing environment for relaxation and well-being.
Benefits of Cooking after a Stroke:
- Enhances sequencing and memory skills
- Improves problem-solving abilities
- Promotes cognitive flexibility
- Boosts confidence and self-esteem
- Provides a creative outlet
- Increases engagement in daily activities
The role of consistency and neuroplasticity in stroke recovery
Consistency is vital when it comes to cognitive exercises for stroke recovery. By consistently practicing cognitive exercises, stroke survivors can promote neuroplasticity, which is the brain’s ability to form new neural pathways and heal from damage. Regular and ongoing engagement in cognitive exercises, both during therapy sessions and at home, can lead to lasting improvements in cognitive function.
Neuroplasticity plays a crucial role in the brain’s ability to heal and adapt after a stroke. Through consistent practice, stroke survivors can stimulate the brain’s natural healing processes and promote the development of new neural connections. This process allows the brain to compensate for the areas affected by the stroke, enabling individuals to regain lost cognitive skills and improve overall functioning.
Repetition is a key component in cognitive exercises for stroke recovery. By repeating specific tasks and exercises, stroke survivors can reinforce and strengthen the neural pathways associated with those skills. This repetition helps the brain to reorganize and rebuild connections, enhancing the recovery process and facilitating the restoration of cognitive abilities.
Working with a speech-language pathologist can provide stroke survivors with personalized guidance and treatment plans for optimal recovery. These professionals can design a tailored cognitive exercise regimen that targets specific areas of improvement and ensures consistency in practice. The speech-language pathologist will monitor progress and make adjustments as needed to maximize the benefits of cognitive exercises and promote neuroplasticity.
Source Links
- https://www.healthline.com/health/stroke-treatment-and-timing/brain-exercises-for-stroke-recovery
- https://www.flintrehab.com/best-cognitive-exercises-for-stroke-patients/
- https://gleneagles.com.my/articles/12-good-brain-exercises-for-stroke-recovery
Similar Posts

How bad can memory loss get with fibromyalgia?

Can BPPV Cause Memory Loss? Understanding Risks

How to talk to someone with short term memory loss?

Exploring Music Therapy for Memory Loss Benefits

Does Mounjaro Cause Memory Loss? My Insights

Why does dory have memory loss?
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Coping With Stroke
Frequently asked questions.
- Next in Stroke Guide Everything You Should Know About Stroke
Everyone has a different way of coping after stroke . While some effects of a stroke may be immediately apparent and, perhaps with therapy, relatively short-lived, others may take months or even years to develop and could be long-lasting.
Having support and getting proper rehabilitation from your care team is essential to making your post-stroke life as good as possible. In addition to physical, occupational, and speech therapy, coping can involve talk therapy with a psychologist or social worker and support groups—online or in-person.
Verywell / Ellen Lindner
Sadness, anxiety, anger, and grief are all common responses to a stroke. This can be due to physical or biochemical changes in the brain as well as the emotional response to post-stroke life.
Talk to your healthcare provider about your emotional health and any changes in mood or behavior, as it may be a serious side effect of the stroke. Medications and treatments may be able to help you. Your practitioner might also recommend that you see a mental health professional for specialized treatment.
Different psychological approaches for treating post-stroke emotional disorders include:
- Solution-focused therapy (SFT)
- Problem-solving therapy (PST)
- Cognitive behavioral therapy (CBT)
- Attitude and commitment therapy (ACT)
- Interpersonal therapy
- Mindfulness therapy, also called mindfulness-based cognitive therapy
Group therapy can also be helpful and many people find the social interaction of a group helps to relieve feelings of isolation following a stroke.
Many people go through a grieving process after a stroke. As you begin to come to terms with new limitations and mourn the loss of your life before stroke, you may experience periods of denial, anger, bargaining, and depression before finally coming to acceptance . This is perfectly normal.
Journaling, talking with a friend, or seeing a therapist can help your emotional healing.
Self-Esteem
The effects of stroke can also challenge your self-esteem. For example, it can be especially hard on you if the stroke has impaired your mobility and limited your independence—affecting, perhaps, what formerly made you feel like a confident individual.
Be gentle with yourself, avoid being self-critical, and try to reframe negative self-talk with positive thoughts.
Behavioral and Personality Changes
After a stroke, new behaviors can include a lack of inhibition, which means that people may behave inappropriately or childlike. Other changes in behavior include a lack of empathy , loss of sense of humor, irrational jealousy , and anger. Talk to your healthcare provider about these changes in behavior, as there may be medications that can help.
Pseudobulbar affect (PBA), also known as emotional lability, reflex crying, and involuntary emotional expression disorder, is more common following a brainstem stroke . In PBA, there is a disconnect between the parts of the brain that control emotions and reflexes.
People with PBA may briefly cry or laugh involuntarily, without an emotional trigger, and in ways that are not appropriate to the situation.
While there are helpful PBA medications and strategies, such as preventing episodes with deep breathing, distractions, or movement, some people find simply alerting those around them in advance can help reduce embarrassment and make it easier to cope.
Depression is common after a stroke, with some studies saying about 25% of stroke survivors become depressed and other estimates putting that number as high as 79%.
Stroke survivors are twice as likely to attempt suicide as the general population. If you are having suicidal thoughts, dial 988 to contact the 988 Suicide & Crisis Lifeline and connect with a trained counselor. If you or a loved one are in immediate danger, call 911 ..
Treating depression with a combination of medication, talk therapy, and group support may improve your mood and also boost physical, cognitive and intellectual recovery.
Clinical Guidelines: Post-Stroke Depression
The American Heart Association and the American Stroke Association jointly recommend periodic reassessment of depression, anxiety, and other psychiatric symptoms in stroke survivors to help improve outcomes. Medications, therapy, and patient education about stroke can all be helpful.
Coping with physical limitations after a stroke can be a struggle. While many of these challenges will improve over time, it can help to know what you can expect during recovery and where to turn for help.
Many long-term physical complications from a stroke can be helped with therapies, while others may be managed with medication or adaptive technologies and other tools that can help improve independence and quality of life.
Most of the time, weakness caused by a stroke affects one side of the body, known as hemiparesis. This commonly affects the face, arm, or leg or a combination of the three. While the weakness may linger long-term, physical therapy can help you to regain strength, and occupational therapy can help you develop alternative strategies for everyday activities.
Many stroke survivors report feeling off-balance, dizzy, light-headed, or as if the room is spinning. These sensations may come and go but may eventually stabilize. Physical therapy is the most effective way to combat balance impairment after a stroke. Your therapist can show you safe, at-home balance exercises or yoga poses to improve balance and combat dizziness.
Vision Changes
Vision problems that may result from a stroke include:
- Double vision (diplopia)
- Visual field loss (hemianopsia )
- Jerking of the eyes (nystagmus)
- Loss of vision
Ophthalmologists and occupational therapists can advise you on the best method to manage vision changes, including therapy to compensate for vision loss, prism lenses, sunglasses, an eye patch, or eye drops.
Communication Problems
Difficulty speaking or understanding words is one of the most well-known results of a stroke and among the most impactful.
Speech-language therapy can help people cope with aphasia (which is trouble speaking or understanding words due to a disease or an injury of the brain) and dysarthria (difficulty articulating words due to muscle weakness or diminished coordination of face and mouth muscles).
Cognitive Deficits
Cognitive changes after a stroke include memory glitches, trouble solving problems, and difficulty understanding concepts. While the severity varies from one stroke survivor to another, research shows cognitive remediation can help significantly.
These interventions include exercises to improve memory, processing speed, and attention, and teaching compensatory strategies, such as making lists and keeping a planner.
Hemispatial Neglect
A stroke on one side of the brain can lead to difficulties with the field of vision or movement on the other side of the body, known as hemispatial neglect. For example, a stroke in the right cerebral cortex can lead to the diminished ability to notice and use the left side of the body.
Depending on the part of the body affected, an optometrist, neuropsychologist, or physical or occupational therapist can help you cope with hemispatial neglect.
Many stroke survivors experience new-onset pain after a stroke. Common locations for post-stroke pain include:
- Muscles (widespread or in a small area)
Rest, physical therapy, and medication can help you to cope with the pain. Post-stroke headaches require special attention from your healthcare provider, but they can improve with the right treatment.
Fatigue and Sleeping Problems
In studies, up to half of stroke survivors report experiencing long-term fatigue following a stroke. For some, this manifests as excessive sleep or the inability to feel rested, while others wake in the middle of the night, have difficulty falling or staying asleep, and nap sporadically throughout the day.
These problems may be due to the stroke itself or a secondary cause, such as depression, pain, or nutritional deficiencies. If you experience fatigue or trouble sleeping, talk to your healthcare provider, who can run additional tests, prescribe medication for insomnia, or offer other strategies to help you cope.
Swallowing Difficulties
A speech and swallow evaluation can identify problems with chewing and swallowing , a common stroke complication known as dysphagia. Most patients see improvement within the first few weeks after a stroke. However, swallowing problems can be quite dangerous.
Choking due to stroke-induced muscle weakness may cause serious illness, such as aspiration pneumonia or even life-threatening breathing obstruction and infection problems. Feeding therapy may help you to regain the ability to swallow safely, although some patients may require a feeding tube to get adequate nutrition.
Trouble With Urination
After a stroke, many stroke survivors experience incontinence , which is urinating when you do not want to. Some stroke survivors also experience bladder retention , which is the inability to urinate on demand. Both of these problems can be managed with medical treatment and physical therapy.
Urination problems can be embarrassing and inconvenient. Discrete bladder-leak protection products like pads for both men and women, disposable underwear, and leak-proof underwear can help you feel more confident going out in public.
Muscle Atrophy
Post-stroke muscle weakness can lead to a lack of movement. A recent stroke patient may need assistance getting up and around in the days following a stroke, and staying in bed too long can result in the muscles shrinking and becoming weaker.
Muscle atrophy can be prevented through pre-emptive post-stroke rehabilitation methods that engage weakened muscles before they shrink. It is difficult to recover from muscle atrophy, but rehabilitation techniques can help improve the situation and slowly rebuild muscle.
Muscle Spasticity
Sometimes weakened muscles become stiff and rigid after a stroke, possibly even jerking on their own. Muscle spasticity and rigidity is often painful and can result in diminished motor control of the already weakened muscles.
Active post-stroke rehabilitation can prevent this, and there are a number of effective medical treatments. Your physical therapy team can provide exercises you can do throughout the day at home to prevent and ease spasticity.
Some people experience post-stroke seizures due to erratic electrical brain activity. Seizure prevention may be part of the post-stroke care program, and seizures are typically managed with medication. Cortical stroke survivors are at especially high risk of developing seizures years later.
Whether your stroke left you with minor physical limitations, speech difficulties, or serious mobility challenges, many people feel isolated after a stroke. Getting back into the stream of life can take time.
Many patients and caregivers find that joining a support group can offer both social engagement and emotional support. Your local hospital or rehabilitation center likely hosts a regular support group, or you can check the American Stroke Foundation's website .
For people with limited mobility, joining an online support group that holds regular online meetings, a Facebook community group, or message boards to talk with other stroke survivors and caregivers can be a lifeline keeping you connected to others. Online support is available through the Stroke Network .
The after-effects of a stroke can present unique individual challenges. Lingering weakness, mobility challenges, difficulty communicating, and visual problems can lead to a lack of independence.

Help With Daily Living
Depending on the degree of your stroke, you may require help with activities of daily living, including cooking, cleaning, and grooming. In some cases, family members step up to help, while others may require a visiting nurse, a part-time aide, or even live-in help like a housekeeper, companion, or nurse.
Some people choose to move to retirement complexes that provide varying levels of care or assisted living facilities.
Getting Around
Some people lose the ability to drive and experience other physical changes that make it difficult to get around. Some stroke survivors find getting a mobility scooter can help them get out in the world independently.
Many communities offer senior or disability buses to help you go shopping or offer car services to bring you to your healthcare provider and therapy appointments. You can also use a ride service like Uber or call a taxi to get from place to place.
Roughly one-quarter of strokes occur in people who have not yet retired. If you are working full-time at the time of your stroke, you should be able to apply for temporary disability until you are able to resume working.
If the stroke has left you with minor impairments, but you can still perform some of your former duties, the American Stroke Association recommends entering into a Reasonable Accommodations Agreement with your employer. If you are unable to work, you may qualify for long-term disability through Social Security .
You may find the quickest improvements happen in the three or four months after the stroke. Recovery may continue for one or two years afterward.
According to the American Stroke Association, 10% of stroke survivors recover almost completely, about 25% recover with minor impairments, and 40% have moderate to severe impairments. Another 10% need care in a long-term care facility.
American Stroke Association. Emotional & behavioral effects of stroke .
Wichowicz HM, Puchalska L, Rybak-Korneluk AM, Gąsecki D, Wiśniewska A. Application of Solution-Focused Brief Therapy (SFBT) in individuals after stroke . Brain Inj . 2017;31(11):1507–1512. doi:10.1080/02699052.2017.1341997
Visser MM, Heijenbrok-Kal MH, Van't Spijker A, Lannoo E, Busschbach JJ, Ribbers GM. Problem-solving therapy during outpatient stroke rehabilitation improves coping and health-related quality of life: Randomized controlled trial . Stroke . 2016;47(1):135–142. doi:10.1161/STROKEAHA.115.010961
Wang SB, Wang YY, Zhang QE, et al. Cognitive behavioral therapy for post-stroke depression: A meta-analysis . J Affect Disord . 2018;235:589–596. doi:10.1016/j.jad.2018.04.011
American Stroke Association. Post stroke mood disorders .
Renner CIe, Outermans J, Ludwig R, Brendel C, Kwakkel G, Hummelsheim H. Group therapy task training versus individual task training during inpatient stroke rehabilitation: A randomised controlled trial . Clin Rehabil . 2016;30(7):637–648. doi:10.1177/0269215515600206
American Stroke Association. Grief and acceptance .
American Stroke Association. Self esteem post stroke .
American Stroke Association. Personality changes post stroke .
American Stroke Association. Pseudobulbar affect (PBA) .
Hadidi NN, Huna Wagner RL, Lindquist R. Nonpharmacological treatments for post-stroke depression: An integrative review of the literature . Res Gerontol Nurs . 2017;10(4):182–195. doi:10.3928/19404921-20170524-02
Mohd Zulkifly MF, Ghazali SE, Che Din N, Singh DK, Subramaniam P. A review of risk factors for cognitive impairment in stroke survivors . Scientific World Journal . 2016;2016:3456943. doi:10.1155/2016/3456943
Winstein CJ, Stein J, Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association . Stroke . 2016 Jun;47(6):e98-e169. doi: 10.1161/STR.0000000000000098.
Stroke Association. Physical effects of stroke .
van Duijnhoven HJ, Heeren A, Peters MA, et al. Effects of exercise therapy on balance capacity in chronic stroke: Systematic review and meta-analysis . Stroke . 2016;47(10):2603–2610. doi:10.1161/STROKEAHA.116.013839
American Stroke Association. Visual disturbances .
Stroke Foundation. Vision loss after stroke fact sheet .
Brady MC, Kelly H, Godwin J, Enderby P, Campbell P. Speech and language therapy for aphasia following stroke . Cochrane Database Syst Rev . 2016;(6):CD000425. doi:10.1002/14651858.CD000425.pub4
Spencer KA, Brown KA. Dysarthria following stroke . Semin Speech Lang . 2018;39(1):15–24. doi:10.1055/s-0037-1608852
Virk S, Williams T, Brunsdon R, Suh F, Morrow A. Cognitive remediation of attention deficits following acquired brain injury: A systematic review and meta-analysis . NeuroRehabilitation . 2015;36(3):367-77. doi:10.3233/NRE-151225
Scholarpedia: The peer-reviewed open-access encyclopedia. Hemineglect .
American Stroke Association. Coping with pain .
Stroke Foundation. Pain after stroke fact sheet .
Paolucci S, Iosa M, Toni D, et al. Prevalence and time course of post-stroke pain: A multicenter prospective hospital-based study . Pain Med . 2016;17(5):924–930. doi:10.1093/pm/pnv019
Harriott AM, Karakaya F, Ayata C. Headache after ischemic stroke: A systematic review and meta-analysis . Neurology . 2019; doi:10.1212/WNL.0000000000008591
Stroke Association. Fatigue after stroke .
González-Fernández M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after stroke: An overview . Curr Phys Med Rehabil Rep . 2013;1(3):187–196. doi:10.1007/s40141-013-0017-y
Rofes L, Arreola V, Almirall J, et al. Diagnosis and management of oropharyngeal dysphagia and its nutritional and respiratory complications in the elderly . Gastroenterol Res Pract . 2011;2011:818979. doi:10.1155/2011/818979
Stroke Foundation. Incontinence after stroke fact sheet .
Scherbakov N, Doehner W. Sarcopenia in stroke-facts and numbers on muscle loss accounting for disability after stroke . J Cachexia Sarcopenia Muscle . 2011;2(1):5–8. doi:10.1007/s13539-011-0024-8
Bethoux F. Spasticity management after stroke . Phys Med Rehabil Clin N Am . 2015;26(4):625–639. doi:10.1016/j.pmr.2015.07.003
Graham NS, Crichton S, Koutroumanidis M, Wolfe CD, Rudd AG. Incidence and associations of poststroke epilepsy: the prospective South London Stroke Register . Stroke . 2013;44(3):605–611. doi:10.1161/STROKEAHA.111.000220
Wang G, Jia H, Chen C, et al. Analysis of risk factors for first seizure after stroke in Chinese patients . Biomed Res Int . 2013;2013:702871. doi:10.1155/2013/702871
American Stroke Association. 15 things caregivers should know after a loved one has had a stroke .
American Stroke Association. Rehab therapy after a stroke .
American Stroke Association. Reasonable accommodations agreement .
Mohd Zulkifly MF, Ghazali SE, Che Din N, Singh DK, Subramaniam P. A Review of risk factors for cognitive impairment in stroke survivors . Scientific World Journal . 2016;2016:3456943. doi:10.1155/2016/3456943
Oh H, Seo W. A comprehensive review of central post-stroke pain . Pain Management Nursing . 2015;16(5):804-18. doi:10.1016/j.pmn.2015.03.002
By Heidi Moawad, MD Dr. Moawad is a neurologist and expert in brain health. She regularly writes and edits health content for medical books and publications.
The effectiveness of problem solving therapy for stroke patients: Study protocol for a pragmatic randomized controlled trial
- BMC Neurology 13(1):67

- Erasmus MC & Rijndam Rehabilitation Center, Rotterdam

- Erasmus University Rotterdam

- Erasmus University MC
Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- HEALTH QUAL LIFE OUT

- Andrew Lloyd
- Vincent Thijs
- Hubert M Wichowicz
- Lidia Puchalska

- Martyna Puchalska
- COCHRANE DB SYST REV

- Katherine Laura Cox

- Chia-Lin Koh

- Debbie V. Summers

- Maria E. A. Armento

- R G Robinson

- David J Moser

- PSYCHOL MED
- THE WHOQOL GROUP
- Roijen van L

- Marianne Donker
- APPL PSYCH MEAS
- Lenore Sawyer Radloff
- Deanne Hawkins

- C.H. Vaartjes
- Frank L J Visseren
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Study protocol
- Open access
- Published: 27 June 2013
The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial
- Marieke M Visser 1 , 2 ,
- Majanka H Heijenbrok-Kal 1 , 2 ,
- Adriaan van ’t Spijker 3 ,
- Gerard M Ribbers 1 , 2 &
- Jan JV Busschbach 3
BMC Neurology volume 13 , Article number: 67 ( 2013 ) Cite this article
6804 Accesses
10 Citations
2 Altmetric
Metrics details
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the cost-effectiveness of the intervention.
Methods/design
We strive to include 200 stroke patients in the outpatient phase of rehabilitation treatment, using a multicenter pragmatic randomized controlled trial with one year follow-up. Patients in the intervention group will receive Problem Solving Therapy in addition to the standard rehabilitation program. The intervention will be provided in an open group design, with a continuous flow of patients. Primary outcome measures are coping style and health-related quality of life. Secondary outcome measures are depression, social participation, health care consumption, and the cost-effectiveness of the intervention.
We designed our study as close to the implementation in practice as possible, using a pragmatic randomized trial and open group design, to represent a realistic estimate of the effectiveness of the intervention. If effective, Problem Solving Therapy is an inexpensive, deliverable and sustainable group intervention for stroke rehabilitation programs.
Trial registration
Nederlands Trial Register, NTR2509
Peer Review reports
Stroke is an increasing public health problem in the Netherlands: every year, 41,000 people suffer from stroke and over 3% of the total health care costs are related to the treatment of stroke and its consequences [ 1 ]. The mortality rate after stroke is 30% and is likely to decrease, which will cause an increase in morbidity [ 2 ]. Almost 50% of stroke survivors experience consequences in daily life that result in a lowered health-related quality of life (HR-QoL) [ 1 ]. The World Health Organization Quality of Life (WHOQOL) Group defines quality of life as “individuals’ perceptions of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns [ 3 ]. HR-QoL refers to the health-related aspects of quality of life. On average, utility scores of HR-QoL after stroke range from 0.47 to 0.68 (a utility score equal to death is 0.0 and full health 1.0), which is substantially lower than the value of a healthy reference population (utility score of 0.93) [ 4 , 5 ]. HR-QoL after stroke is predicted by functional constraints, age, gender, and psychosocial factors, like socioeconomic status, depression, and coping style [ 4 , 6 – 8 ]. Functional constraints, age, gender, and socioeconomic status cannot or are difficult to change, but coping style could be targeted. The question then becomes if HR-QoL after stroke could be improved through a coping style intervention. If this is possible, a secondary question would be how such improvement relates to depression, health care consumption, and costs.
A common definition of coping style is someone’s preferred way of dealing with different situations. Several coping styles can be distinguished, such as active, passive, and avoidant coping. Wolters (2010) shows that in traumatic brain-injured (TBI) patients, higher HR-QoL in the long term is predicted by an increase in active problem-focused coping style and a decrease in passive emotion-focused coping style. Unfortunately, in this population of TBI patients the active coping decreases over time, while passive coping increases [ 9 ]. This suggests that if the decrease of active coping can be stopped, there is room for improvement in HR-QoL. Stroke patients make even less use of active, problem-oriented coping styles compared to other brain damaged patients [ 10 ]. Furthermore, Darlington (2007) shows that in stroke patients, coping becomes more important in determining HR-QoL over time, while the importance of general functioning decreases [ 11 ]. This would mean that long term HR-QoL could benefit from improved coping.
Coping styles can be influenced by several interventions. Backhaus (2010) shows that an intervention aimed at changing maladaptive coping styles positively influenced psychosocial functioning of TBI patients [ 12 ]. However, HR-QoL was not measured in this study. No research is found that investigated an intervention aimed at improving HR-QoL through the change of maladaptive coping styles in stroke patients. We therefore set out to investigate whether Problem Solving Therapy (PST), which aims at active problem-focused coping, might improve HR-QoL in stroke patients. PST has been proved effective in other patient populations [ 13 , 14 ]. In stroke patients, PST has been shown successful for the prevention of post stroke depression [ 15 ]. Effects on coping style and HR-QoL have not been investigated yet.
The primary aim of this study is to investigate whether PST is an effective group intervention for improving active problem-focused coping style and HR-QoL in stroke patients. The secondary aim is to determine the effect of PST on depression, social participation, health care consumption, and the cost-effectiveness of the intervention. The effectiveness of the therapy will be investigated in an open group design, which has not been used in PST research before. PST will be added to the standard care just before the end of the rehabilitation program, as at this moment a relapse in HR-QoL is frequently observed, when patients cannot rely on their therapists anymore [ 16 ]. By teaching patients to actively cope with stressful situations, through adapting and realizing their goals, we expect that patients will use more effective coping styles, which consequently may prevent the relapse in HR-QoL, and possibly increase HR-QoL in the long term. With regard to the secondary aims of this study, we expect the incidence of depression to decrease, social participation to improve, and health care consumption to decrease, resulting in a favorable cost-effectiveness ratio for the intervention.
Study design and procedure
The effectiveness of PST for stroke patients will be evaluated in a multicenter pragmatic randomized controlled trial (RCT) with one year follow-up, with the intervention performed in the daily practice of a sub-acute outpatient stroke rehabilitation program. As such, the potential effects of the intervention have a good external validity, which allows us to calculate the cost-effectiveness of the therapy compared with standard care.
The study will be performed in Rijndam Rehabilitation Center in collaboration with Erasmus MC, both in the Netherlands, and in Ghent University Hospital in Belgium. Patients are invited by their rehabilitation physician to participate in the study. Before the start of the study, patients need to sign the informed consent form. Data will be collected at four time points by one of three research psychologists. T0 is the baseline measurement, performed within three weeks before the start of the intervention phase. T1 will be performed within ten days after the intervention phase, T2 six months and T3 twelve months after the intervention phase (Figure 1 ). The measurements will be performed in the rehabilitation center or at the patients’ home in a face-to-face interview. The study has been approved by the Medical Ethics Committee of Erasmus MC University Medical Center and the Ethics Committee of Ghent University Hospital.
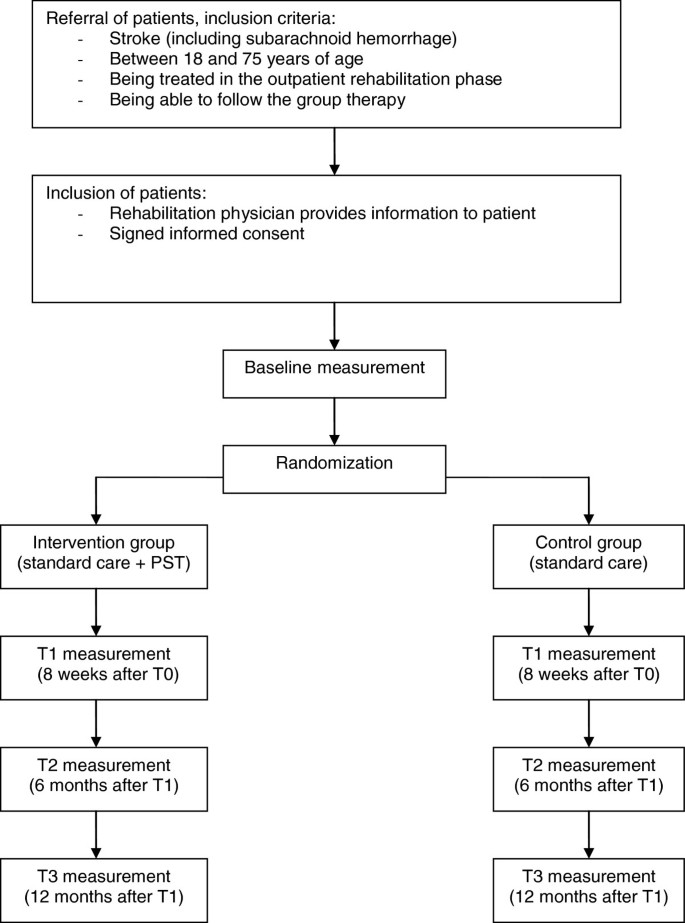
Design of the randomized controlled trial.
Study population
We strive to include 200 stroke patients. Inclusion criteria are: stroke (including subarachnoid hemorrhage), age between 18 and 75 years, being treated in the outpatient rehabilitation phase, and being able to participate in group therapy. Exclusion criteria are: progressive neurological disorders, life expectancy less than one year, insufficient understanding of the Dutch language, excessive drinking or drug abuse, subdural hematomas, moderate and severe aphasia. The same criteria would apply to the implementation of PST in practice, which stresses the pragmatic character of the trial. The inclusion of patients started March 2011 and will end August 2013. The one-year follow-up of all patients will be finished by September 2014.
Randomization
Patients are randomized to the intervention- or control condition using a stratified block randomization procedure with a block size of four. To ensure comparability between the two groups, patients are stratified per rehabilitation center. A member of the research group, who is not involved in the collection of the data, prospectively allocates the patients to the intervention- or control condition in a one-to-one ratio using an online random-number generator. To allow blinded randomization, the allocation information will be put in separate sealed envelopes which are consecutively numbered. At the end of the baseline measurement, the investigator opens the numbered envelop and informs the patient about the condition he or she is assigned to. The research psychologists who perform the baseline and follow-up measurements are blinded for treatment condition. The therapists who provide the intervention are not involved in the collection of the data. The investigator who will analyze the data is not involved in the collection of the follow-up measurements.
Intervention: problem solving therapy
Patients who are assigned to the intervention condition will receive PST in addition to the standard rehabilitation program, which will start during the last eight weeks of outpatient treatment. PST is a widely used and practical intervention method, based on a general model of coping with stress [ 17 , 18 ]. The model states that having a chronic disease causes stressful daily problems, which increase the chance of experiencing psychological stress and depressive feelings. Therefore, the aim of PST is to improve the skills to cope with the stressful daily problems in life after stroke.
The intervention will be provided in an open group design, with a continuous flow of patients, which means that patients can enter the group every week and leave the group after eight sessions (Figure 2 ). The reason for this design is that it studies group therapy in its most feasible form, where patients start and end their programs at different time-points. If we had chosen to study the effect in closed groups, many patients in the similar stage of their programs are necessary. This would only be possible if patients are admitted to large scale rehabilitation centers, which is not the rehabilitation practice in The Netherlands, or patients would have to wait for a long time before entering the group. The open group design has some disadvantages. Patients may feel unsafe when they enter an already existing group. Furthermore, a continuous flow of patients is required to keep a balanced number of patients in the group. Therefore, interventions aimed at rare diseases cannot be studied with an open group design. However, for our population of stroke patients we do expect the design to be suitable and beneficial, because these patients are frequently seen in rehabilitation treatment. An open group design has several benefits as well. Advantages for the patients are that they do not have to wait until they can start with the intervention, they can share their experiences with other ‘experienced’ stroke patients, and there is room for interaction with many fellow patients. Other advantages are that the intervention is relatively easy to organize and implement in the daily practice of the rehabilitation center. This open group design has not been investigated in PST research yet.
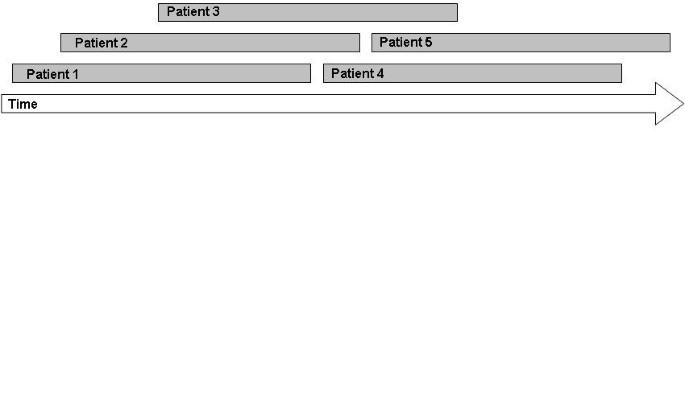
Patient flow in an open group therapy.
The intervention in this study consists of eight group sessions of 1,5 hours a week, with homework exercises after each session. The group consists of a minimum of three and a maximum of six participants. PST is provided by one to three trained neuropsychologists per rehabilitation center. Solving problems will be structured, by dividing the problem solving process in four steps:
Define problem and goal;
Generating multiple solutions;
Considering the possible consequences of the solutions systematically and select the best solution;
Implement the solution and evaluate.
Each session starts with the sharing of experiences from the past week. Then, the model of problem solving will be repeated and explained. If there are some participants who are in the group for a couple of weeks already, they will be asked to explain the model to other new participants. Subsequently, one step of the model will be highlighted every week. With emphasis on this specific step, the model will be applied to one or more examples from the participants. Finally, the participants will be asked to practice the specific step at home by making a homework assignment. During the sessions, inadequate and irrational thoughts will be challenged by common cognitive interventions. A unique aspect of the intervention is the focus on the definition of the problem in the first step of the model. A clear definition of the problem will lead to a better understanding and more solutions to it.
Control condition: standard care
Patients who are assigned to the control condition will receive the standard rehabilitation program, in order to be able to study the additional effect of the intervention to the standard rehabilitation program. This standard rehabilitation program consists of individualized amounts of treatment by a physical therapist, occupational therapist, speech therapist, psychologist, social worker, and rehabilitation physician, depending on the severity of stroke. On average, stroke patients in outpatient rehabilitation receive twelve hours of treatment a week during a nine week rehabilitation program.
Primary outcome measures are changes in task-oriented coping and psychosocial HR-QoL in patients in the intervention group in comparison with the control group. Coping style is measured using the Coping Inventory for Stressful Situations (CISS) and the short version of the Social Problem Solving Inventory-Revised (SPSI-R:SF). The CISS questionnaire consists of 48 questions and contains three subscales; Task-oriented coping, Emotion-oriented coping, and Avoidant coping. The subscale Avoidant coping consists of two subscales; Distraction and Social Diversion [ 18 , 19 ]. Because the PST aims at tasks, ‘Task-oriented coping’ is chosen as a primary endpoint; the other two subscales are used as secondary endpoints. The SPSI-R:SF questionnaire consists of ten questions about problem solving skills regarding daily situations. There are five subscales: Positive Problem Orientation, Rational Problem Solving, Negative Problem Orientation, Impulsivity/Carelessness Style, and Avoidance Style, and all are used as secondary endpoints in this trial [ 20 ].
HR-QoL is measured using the EuroQol (EQ-5D-5L) and the Stroke Specific Quality of Life Scale (SS-QoL-12). The EQ-5D is a generic questionnaire, and consists of five questions regarding mobility, self-care, daily activities, pain/complaints, mood, and a VAS scale. The five dimensions can be combined to one utility scale, representing the societal perspective of the general public [ 21 ]. The SS-QoL-12 is specifically developed for the population of stroke patients [ 22 ]. We will use the abbreviated version containing twelve items, which has been shown valid [ 23 ]. The questionnaire provides a total score and two sub scores: physical and psychosocial, of which the psychosocial sub-score is defined as the primary endpoint. The other HR-QoL scores are used as secondary endpoints.
Other secondary outcome measures are differences in depression, social participation, and health care consumption between patients in the intervention and control group. Additionally, the influence of cognitive functioning, personality characteristics, aphasia, type of stroke, side of stroke, level of functioning, and demographic characteristics on the outcomes will be assessed. Finally, the cost-effectiveness of the intervention will be calculated compared with standard care.
Depression is measured using the Center for Epidemiologic Studies Depression Scale (CES-D). This questionnaire consists of twenty items concerning depression, higher scores indicate more depressive symptoms [ 24 ].
Social participation is measured using the Impact on Participation and Autonomy (IPA). The questionnaire consists of five dimensions; Autonomy indoors, Family role, Autonomy outdoors, Social life and relationships, Work and education [ 25 ].
Health care consumption is measured using the Trimbos Questionnaire for Costs association with Psychiatric Illness (TiC-P). The questionnaire was developed for economic evaluation in mental health care, and measures health care consumption and productivity losses [ 26 ].
Sample size calculation
To determine the sample size for measuring differences between the intervention- and control group in coping style and HR-QoL, we searched for comparable effect sizes in the literature. With regard to coping style, there was no data available for this calculation. With regard to HR-QoL, Studenski (2005) measured an increase in HR-QoL after a physical therapy for stroke patients, with a long term effect size f ranging from 0.06 to 0.18 [ 27 ]. Because of the lack of more comparable data, we used this data and carefully estimated the effect size f to be 0.08. Considering the design of two groups and four repeated measurements, an expected correlation of 0.70, an alpha of 0.05, and a power of 0.80, we calculated a total required sample size of 132 patients based on the F-test. Because potential drop out is estimated at 0.30, we will strive to include 200 patients.
Statistical analyses
Demographic variables will be analyzed with an independent sample T-test for continuous variables, the Mann–Whitney U test for ordinal variables, and the chi-square test for categorical variables. Linear Mixed Models will be used to compare the repeated measurements between treatment groups, taking into account the correlation within and between subjects. We will create models for all the primary and secondary outcome variables, with time, group condition (intervention or control), and the interaction between these variables as predictors. Furthermore, we will control for variables that are accidentally not equally distributed between the two group conditions.
The cost-effectiveness of the intervention will be calculated by counting all the medical and non-medical costs, like productivity losses. The incremental cost-effectiveness ratio will be calculated by dividing the difference in total costs by the difference in quality-adjusted life years (QALYs). These QALYs will be calculated based on the EQ-5D questionnaire. The economic evaluation will be conducted according to the Dutch guidelines [ 28 ] and includes multivariate probabilistic sensitivity analyses. In the base case scenario the time horizon will be one year. If the effect is still present at one year follow up, a Markov model will be made to model a longer time horizon.
This study investigates the effect of PST on coping style and HR-QoL in stroke patients. In addition, the effect on depression, social participation, and health care consumption will be investigated, as well as the cost-effectiveness of the intervention. We will study the effectiveness of PST as close to the implementation in practice as possible, using a pragmatic trial design and an open group therapy. Any pragmatic trial has limitations; MacPherson (2004) argued that a pragmatic trial design cannot be used to determine the specific components of a treatment that caused an effect [ 29 ]. It may be possible that patients in the intervention group show improvement caused by the extra attention they receive and not so much by the assumed effective elements of the therapy; this attention effect may be considered a placebo effect. If we would like to distinguish between this ‘placebo effect’ and the effect of the specific treatment elements, the control group should have received a ‘sham therapy’. Such sham therapy would hinder the estimation of the effect of PST in practice, as in practice such additional effort would not take place. Therefore, one of the advantages of the pragmatic study design is that the external validity is better than using a sham-controlled design; the results will be generalizable to the normal rehabilitation setting [ 30 ]. The study population represents the normal stroke population in the outpatient phase of rehabilitation treatment, and the psychologists will provide the intervention to the patients just as they would do in practice. The results of a pragmatic trial are directly applicable to the usual care setting [ 31 ]. Moreover, if the intervention will prove effective, it will be easy to implement the intervention in the standard rehabilitation program, since it is already in use and the psychologists will already be trained. Other rehabilitation centers can use the therapy manual we developed.
We expect that patients who received PST will use more effective coping styles and experience a higher HR-QoL. Furthermore, we expect that patients after PST will show a decrease in depression score, an increase in social participation, and a decrease in health care consumption, which would lead to a reduction in the health care costs. We expect the intervention to be cost-effective, since the costs of the intervention are relatively low; one psychologist can train three to six patients at the same time. Darlington (2009) estimated the cost-effectiveness of an intervention aimed at coping strategies in stroke patients: the maximum costs for a single patient were 2500 euros, which will be lower if the therapy is provided in a group [ 32 ]. If PST will be proved effective for stroke patients in outpatient rehabilitation, the intervention will be an inexpensive, deliverable and sustainable group intervention that could be added to usual stroke rehabilitation programs.
Abbreviations
Center for Epidemiologic Studies Depression Scale
Coping Inventory for Stressful Situations
- Health-related quality of life
Impact on Participation and Autonomy
- Problem Solving Therapy
Quality-adjusted life years
Randomized controlled trial
Social Problem Solving Inventory-Revised
Stroke Specific Quality of Life Scale
Traumatic brain-injured
Trimbos Questionnaire for Costs association with Psychiatric Illness
World Health Organization Quality of Life.
Evers SM, Engel GL, Ament AJ: Cost of stroke in The Netherlands from a societal perspective. Stroke. 1997, 28 (7): 1375-1381. 10.1161/01.STR.28.7.1375.
Article CAS PubMed Google Scholar
Vaartjes I, van Dis I, Visseren F, Bots M: Hart- en vaatziekten in Nederland 2009, cijfers over leefstijl- en risicofactoren, ziekte en sterfte. 2009, Den Haag: Nederlandse Hartstichting
Google Scholar
Group W, Harper A, Power M: Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998, 28 (3): 551-558.
Article Google Scholar
Sturm JW, Donnan GA, Dewey HM, Macdonell RAL, Gilligan AK, Srikanth V, Thrift AG: Quality of life after stroke - The North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2004, 35 (10): 2340-2345. 10.1161/01.STR.0000141977.18520.3b.
Article PubMed Google Scholar
Mittmann N, Trakas K, Risebrough N, Liu BA: Utility scores for chronic conditions in a community-dwelling population. Pharmaco Economics. 1999, 15 (4): 369-376. 10.2165/00019053-199915040-00004.
Article CAS Google Scholar
Paul SL, Sturm JW, Dewey HM, Donnan GA, Macdonell RAL, Thrift AG: Long-term outcome in the north east Melbourne stroke incidence study - Predictors of quality of life at 5 years after stroke. Stroke. 2005, 36 (10): 2082-2086. 10.1161/01.STR.0000183621.32045.31.
Almborg AH, Ulander K, Thulin A, Berg S: Discharged after stroke - important factors for health-related quality of life. J Clin Nursing. 2010, 19 (15–16): 2196-2206.
Patel MD, Tilling K, Lawrence E, Rudd AG, Wolfe CDA, McKevitt C: Relationships between long-term stroke disability, handicap and health-related quality of life. Age Ageing. 2006, 35 (3): 273-279. 10.1093/ageing/afj074.
Wolters G, Stapert S, Brands I, Van Heugten C: Coping styles in relation to cognitive rehabilitation and quality of life after brain injury. Neuropsychol Rehabil. 2010, 20 (4): 587-600. 10.1080/09602011003683836.
Herrmann M, Curio N, Petz T, Synowitz H, Wagner S, Bartels C, Wallesch CW: Coping with illness after brain diseases - a comparison between patients with malignant brain tumors, stroke, Parkinson's disease and traumatic brain injury. Disabil Rehabil. 2000, 22 (12): 539-546. 10.1080/096382800416788.
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: Coping strategies as determinants of quality of life in stroke patients: A longitudinal study. Cerebrovasc Dis. 2007, 23 (5–6): 401-407.
Backhaus SL, Ibarra SL, Klyce D, Trexler LE, Malec JF: Brain Injury Coping Skills Group: A Preventative Intervention for Patients With Brain Injury and Their Caregivers. Archives Physical Med Rehabil. 2010, 91 (6): 840-848. 10.1016/j.apmr.2010.03.015.
Merlijn V, Hunfeld JAM, van der Wouden JC, Hazebroek-Kampschreur A, van Suijlekom-Smit LWA, Koes BW, Passchier J: A cognitive-behavioural program for adolescents with chronic pain - a pilot study. Patient Educ Counseling. 2005, 59 (2): 126-134. 10.1016/j.pec.2004.10.010.
Hopko DR, Armento MEA, Robertson SMC, Ryba MM, Carvalho JP, Colman LK, Mullane C, Gawrysiak M, Bell JL, McNulty JK, et al: Brief Behavioral Activation and Problem-Solving Therapy for Depressed Breast Cancer Patients: Randomized Trial. J Consult Clin Psychol. 2011, 79 (6): 834-849.
Robinson RG, Jorge RE, Moser DJ, Acion L, Solodkin A, Small SL, Fonzetti P, Hegel M, Arndt S: Escitalopram and problem-solving therapy for prevention of poststroke depression - A randomized controlled trial. Jama-Journal The Am Med Assoc. 2008, 299 (20): 2391-2400. 10.1001/jama.299.20.2391.
Ch'ng AM, French D, McLean N: Coping with the Challenges of Recovery from Stroke Long Term Perspectives of Stroke Support Group Members. J Health Psychology. 2008, 13 (8): 1136-1146. 10.1177/1359105308095967.
Nezu AM, Perri MG, Nezu CM, Berking M: Problem-solving therapy for depression: theory, research, and clinical guidelines. 1989, New York: Wiley
Nezu AM, Nezu CM: Problem Solving Therapy. J Psychother Integr. 2001, 11 (2): 187-205. 10.1023/A:1016653407338.
Endler NS, Parker JDA: Coping inventory for stressful situations (CISS) manual. 1990, Toronto: Multi-Health Systems
Hawkins D, Sofronoff K, Sheffield J: Psychometric Properties of the Social Problem Solving Inventory-Revised Short-Form: Is the Short Form a Valid and Reliable Measure for Young Adults?. Cognitive Therapy Res. 2009, 33 (5): 462-470. 10.1007/s10608-008-9209-7.
Lamers LM, McDonnell J, Stalmeier PF, Krabbe PF, Busschbach JJ: The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ. 2006, 15 (10): 1121-1132. 10.1002/hec.1124.
Williams LS, Weinberger M, Harris LE, Clark DO, Biller J: Development of a stroke-specific quality of life scale. Stroke. 1999, 30 (7): 1362-1369. 10.1161/01.STR.30.7.1362.
Post MWM, Boosman H, van Zandvoort MM, Passier P, Rinkel GJE, Visser-Meily JMA: Development and validation of a short version of the Stroke Specific Quality of Life Scale. J Neurol Neurosurg Psychiatry. 2011, 82 (3): 283-286. 10.1136/jnnp.2009.196394.
Radloff LS: The CES-D Scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977, 1: 385-401. 10.1177/014662167700100306.
Cardol M, de Haan RJ, de Jong BA, van den Bos GAM, de Groot IJM: Psychometric properties of the impact on participation and autonomy questionnaire. Arch Physical Med Rehabil. 2001, 82 (2): 210-216. 10.1053/apmr.2001.18218.
Hakkaart-Van Roijen L: Trimbos/iMTA questionnaire for Costs associated with Psychiatric Illness (TiC-P). Manual. September 2010, Rotterdam: Erasmus University Rotterdam
Studenski S, Duncan PW, Perera S, Reker D, Lai SM, Richards L: Daily functioning and quality of life in a randomized controlled trial of therapeutic exercise for subacute stroke survivors. Stroke. 2005, 36 (8): 1764-1770. 10.1161/01.STR.0000174192.87887.70.
Oosterbrink JB, Bouwmans CAM, Koopmanschap MA, Rutten FFH: Handleiding voor kostenonderzoek, methoden en standaard kostprijzen voor economische evaluaties in de gezondheidszorg. 2004, Diemen: College voor zorgverzekeringen
Macpherson H: Pragmatic clinical trials. Complement Ther Med. 2004, 12 (2–3): 136-140.
Tunis SR, Stryer DB, Clancy CM: Practical clinical trials - Increasing the value of clinical research for decision making in clinical and health policy. Jama-Journal Am Med Assoc. 2003, 290 (12): 1624-1632. 10.1001/jama.290.12.1624.
Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B, Oxman AD, Moher D: Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008, 337: a2390-10.1136/bmj.a2390.
Article PubMed PubMed Central Google Scholar
Darlington ASE, Dippel DWJ, Ribbers GM, van Balen R, Passchier J, Busschbach JJV: A Prospective Study On Coping Strategies And Quality Of Life In Patients After Stroke, Assessing Prognostic Relationships And Estimates Of Cost-Effectiveness. J Rehabil Med. 2009, 41 (4): 237-241. 10.2340/16501977-0313.
Pre-publication history
The pre-publication history for this paper can be accessed here: http://www.biomedcentral.com/1471-2377/13/67/prepub
Download references
Acknowledgements
This study is funded by the National Initiative Brain and Cognition (NIHC 056-11-010), Stichting Coolsingel, and Erasmus MC Cost-Effectiveness Research.
Author information
Authors and affiliations.
Department of Rehabilitation Medicine, Erasmus MC, University Medical Center Rotterdam, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Marieke M Visser, Majanka H Heijenbrok-Kal & Gerard M Ribbers
Rijndam Rehabilitation Center, PO Box 23181, 3001, KD, Rotterdam, The Netherlands
Department of Psychiatry, Erasmus MC, University Medical Center Rotterdam, Section Medical Psychology and Psychotherapy, PO Box 2040, 3000, CA, Rotterdam, The Netherlands
Adriaan van ’t Spijker & Jan JV Busschbach
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Marieke M Visser .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
All authors contributed to the development of the study protocol. AvtS adapted the PST-manual for the population of stroke patients. MMV implemented the therapy in the rehabilitation program. All authors read and corrected the draft version of this manuscript, and approved the final version.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Authors’ original file for figure 2, rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Visser, M.M., Heijenbrok-Kal, M.H., van ’t Spijker, A. et al. The effectiveness of problem solving therapy for stroke patients: study protocol for a pragmatic randomized controlled trial. BMC Neurol 13 , 67 (2013). https://doi.org/10.1186/1471-2377-13-67
Download citation
Received : 23 April 2013
Accepted : 20 June 2013
Published : 27 June 2013
DOI : https://doi.org/10.1186/1471-2377-13-67
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rehabilitation
- Coping style
BMC Neurology
ISSN: 1471-2377
- General enquiries: [email protected]

18 Ways to Improve Cognitive Problems After Stroke
Aug 21, 2019
A Decrease font size. A Reset font size. A Increase font size.
First published on ARNI Institute for Stroke Rehabilitation website
A change in cognitive ability is common after a stroke. Did you know that as many as two-thirds of stroke survivors may experience cognitive impairment as a result of their stroke.? If this is you, or you know someone who seems possibly to be going through such difficulties, here’s 18 steps you can take to try and improve cognition difficulties after stroke:
First, what is cognition?
Put simply, cognition is thinking; it is the processing, organising and storing of information – an umbrella term for all of the mental processes used by your brain to carry you through the day, including perception, knowledge, problem-solving, judgement, language, and memory. The brain’s fantastic complexity means that it can collect vast amounts of information from your senses (sights, sounds, touch, etc) and combine it with stored information from your memory to create thoughts, guide physical actions, complete tasks and understand the world around you.
A stroke can affect the way your brain understands, organises and stores information. This brain injury can result in damage to the areas of the brain that are responsible for perception, memory, association, planning, concentration, etc. The severity and localisation of the stroke will effect the type and level of difficulties experienced by an individual, and will vary from person to person.
It can be difficult to plan and organise daily tasks. The brain is constantly working in the background, allowing us to complete a task based on prior knowledge, experience, and learned behaviour.
You don’t have to consciously think how to boil the kettle, change TV channels or put on your socks before your shoes: you just do it. But damage to the brain can result in problems with these planning and execution mechanisms.
You might not be able to think how to do a simple task, or you may get the sequence wrong (for example, shoes before socks). You might have trouble with orientation, which could include not knowing the date, day of the week, or even who you are with. Problem-solving too can become difficult. Making decisions, solving problems, understanding numbers and managing money can be a challenge.
Good cognitive function also relies on memory. The brain uses 2 types of memory to hold information, the long and short term memory. Short-term memory is the temporary store for small amounts of information. This information is kept readily available and can be recalled quickly. For example, a phone number can be remembered long enough for you to dial it. Long-term memory is where you keep your experiences, thoughts and feelings from the past and things stored here can be stored indefinitely. Memory problems could result in difficulty storing or recalling information. This could include problems remembering appointments, important dates or in the case of short term memory, what you were about to do, or what somebody just said to you.
Problems with concentration are common. Concentration is required for effective cognitive function, as many of your thinking process require concentration. Concentration requires our brain to filter out much of the information coming in from your conscious thinking, so you are not distracted by it.
Stroke can impact on this ability because of damage to the areas of the brain responsible for this, and also because tiredness, pain and emotional problems have an effect of the ability to stay focused and concentrate. This could result in difficulties when trying to follow a television programme, or conduct a conversation with a friend. Multi-tasking too is difficult.
18 Things to try
- Cognitive problems are confusing and frustrating. But, there are some things you can to do help. Most improvements occur in the first 3 months after a stroke, after which they slow down, but the brain will keep creating new neural pathways after this time.
- To help with memory and perception problems, try using a diary, day planner, calendar or notepad. Writing down appointments and creating to-do-lists can help you to remember them.
- Photos and pictures can help to ‘trigger’ your memory.
- Check your calendar, newspaper or diary to help you remember the day and date.
- Make notes of important conversations.
- Use notes, lists and labels around the house and help prompt you to remember. Mobile phones are a great resource. Set alarms, reminders and memos to remind you throughout the day.
- It is important not to overload yourself, finish one task before you start another. Plan your day and prioritise tasks.
- Try slowing the activity down, working through a step at a time.
- Keep instructions clear and short, no more than 5 or 6 words to a sentence, and only 1 or 2 instructions at a time.
Please read the full list here .

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Neurol Neurosurg Psychiatry
- v.77(11); 2006 Nov

Defining and quantifying coping strategies after stroke: a review
The coping strategies that people use after a stroke may influence recovery. Coping measures are generally used to assess the mediating behaviour between a stressor (ie, disease or condition) and the physical or psychological outcome of an individual. This review evaluates measures that quantified coping strategies in studies on psychological adaptation to stroke. The main aspects of the coping measures reviewed were (a) conceptual basis; (b) coping domains assessed; (c) coping strategies used after a stroke; and (d) psychometric properties of coping measures used in studies assessing patients with stroke. Four databases (Medline, CINAHL, PsychINFO and Cochrane Systematic Reviews) were searched to identify studies that used a coping measure in stroke. 14 studies assessed coping strategies in patients after stroke. Ten different coping measures were used, and the studies reviewed had many limitations. Few studies provided definitions of “coping” and the psychometric properties of the coping measures were under‐reported. The need for future studies to more clearly define the coping process and to present data on the reliability and validity of the measures used is emphasised.
A stroke is a sudden and often traumatic major life event that usually occurs with minimal warning and, for many, results in life‐changing consequences with which affected people must cope. Stroke is the first leading cause of disability in adults in Western countries and more than one third of people who survive a stroke will have severe disability. 1 The increasing size of the older population coupled with the increase in the proportion of people surviving acute stroke means that the number of people learning to cope with stroke‐related disability each year is increasing. 2
Research on the use of disability‐specific coping strategies for other conditions has shown better psychosocial adaptation to disability and chronic illness. 3 As neurorehabilitation comprises maximising recovery and adaptation to disability, coping skills may be of importance. Some evidence suggests that coping is likely to predict success in rehabilitation. 4 Rehabilitation after a stroke includes more than functional recovery because, in tandem with physical disability, people often experience a variety of psychological sequelae such as depression, anxiety and emotional lability, which can compromise the rehabilitation process and affect long‐term adjustment. 5 , 6 , 7
Research on stroke is beginning to focus attention on psychological outcomes such as quality of life and subjective well‐being 8 , 9 in addition to survival and functional outcomes. Depression has been most intensively studied, 10 , 11 , 12 , 13 and other psychological problems dealt with include fear of loss of control, 14 fears about death and disfigurement, social isolation, helplessness and worry about loss of social roles. 7 A focus on coping with the emotional and cognitive changes after stroke is critical to understanding the rehabilitation process. 15
Coping has been a major focus of research in psychology for several decades and in particular in the discipline of health psychology. 16 Two of the core theorists in the study of coping, Folkman and Lazarus, 17 , 18 , 19 , 20 defined coping as “the constantly changing cognitive and behavioural efforts to manage the specific external or internal demands that are appraised as taxing or exceeding the resources of the person”. This definition had a profound effect on the conceptualisation of coping 21 and has become widely accepted in the psychological literature. 22 Coping strategies refer to the specific efforts, both behavioural and cognitive, that people use to master, tolerate, reduce or minimise stressful events. Two major categories of coping strategies are widely recognised 16 , 23 , 24 : problem‐solving strategies (efforts to do something active to alleviate stressful circumstances) and emotion‐focused coping strategies (efforts to regulate the emotional consequences of stressful or potentially stressful events). Some authors have argued for a third dimension of avoidance‐oriented coping (efforts to avoid a stressful situation by seeking out other people or by engaging in a substitute task). 24 , 25 , 26 The opposite end of the spectrum to avoidance‐oriented coping is referred to as active approach‐oriented coping. 25 , 26 , 27 A distinction is also made between dispositional and situational approaches to coping. The dispositional approach focuses on relatively stable coping strategies used by people across different stressful situations, whereas the situational approach refers to coping as a dynamic process, showing little consistency both across and within stressful situations. 28
The Transactional Theory of Stress and Coping, developed by Lazarus and Folkman, 17 , 18 , 29 , 30 is the most widely used framework for evaluating the processes of coping with stressful events. 21 , 26 According to this theory, the stressor is initially appraised in terms of personal relevance to the individual and, subsequently, the resources available to deal with the stressor are evaluated. According to de Ridder, 21 the Transactional Theory encouraged the development of instruments in which subjects were asked to reflect on their conscious efforts to cope with adverse conditions. Several self‐report measures of coping now exist—for example, the Ways of Coping Questionnaire (WCQ) 31 and the Coping Orientation for Problem Experiences. 25
Abundant research literature on coping is available in the context of a wide range of illnesses. 32 , 33 , 34 , 35 , 36 , 37 In the context of stroke, some relatively recent attention has been paid to the issue of coping. 38 , 39 To date, however, research findings have not quantified what consistent coping strategies are commonly adopted in the aftermath of stroke. This paper aims to evaluate measures that quantified coping strategies in studies dealing with psychological adaptation to stroke. This review examines the conceptual basis and the specific domains of the coping measures used to assess coping after stroke. It also evaluates the findings in relation to the pattern(s) of coping strategies used in populations with stroke, with a view to identifying whether there is a “typical” profile of coping response in the context of an acute, debilitating condition such as stroke. Psychometric properties of the coping measures will be reviewed with respect to a population affected by stroke, as certain stroke sequelae such as cognitive and language impairments may affect participation in coping assessments or in the process of coping. Identifying adaptive coping strategies that people use after a stroke may facilitate the development of more effective rehabilitation strategies. Coping skills may be considered to be the key psychological resources necessary to rebuild the lives of patients disrupted by the residual deficits of stroke.
Search strategy
A review was conducted of standardised measures of coping used in studies of patients with stroke. A computer search was performed on databases: Medline (1966–February 2006), PsychINFO (1887–February 2006), CINAHL (1967–February 2006) and the Cochrane Systematic Reviews (1993–February 2006). The following keywords were used: “stroke” or “cerebrovascular accident” and “coping” or “adaptation, psychological” or “adaptive behaviours” or “reintegration” or “psychological adjustment”. Selected articles were obtained and reference lists in articles were reviewed by the main author to identify additional citations.
Inclusion criteria
Articles were included in the review if they fulfilled the following criteria:
- They published peer‐reviewed research.
- They used standardised questionnaires and measures in cross‐sectional, longitudinal and intervention studies.
- The sample population comprised or included patients with stroke.
- Data from an instrument quantifying coping were reported.
Analysis of psychometric criteria
Reliability.
Two types of reliability were examined in this review: internal consistency and test–retest. Internal consistency is the most common estimate of reliability reported, estimated using Cronbach's α, which should not fall below 0.7 for research purposes. 40 Although establishing test–retest reliability in the context of research on coping strategies is problematic, because of the inherent potential for variability in coping responses over time, we assessed for the presence (or absence) of data on test–retest reliability: if present, a correlation of ⩾0.7 was considered of value. 40
We reported evidence of construct validity, the extent to which a measure is related to other measures in ways that are consistent with the hypothesised direction. 41 Several different specific categories used to classify types of validity information—for example, correlations with specified variables, correlations with unspecified variables, correlations with other measures, inter‐correlations among parts of a measure, comparison of scores between two or more groups and any type of factor analysis—were used as guidelines to report validity of the coping measures in this review.
Of 102 studies identified, 14 studies met the inclusion criteria. Table 1 1 presents a summary of the studies reviewed. Seven studies were cross‐sectional in design, 42 , 43 , 44 , 45 , 46 , 47 , 48 five were longitudinal studies 39 , 49 , 50 , 51 , 52 and two were intervention studies. 53 , 54 The sample type and size varied in different studies. Six studies conducted research on a population with stroke alongside other patient groups. 42 , 43 , 44 , 51 , 52 , 53 The remaining eight studies examined coping only in patients with stroke. Seven studies were primarily descriptions of the profiles of coping strategies, and a further three examined the stability of this profile over time. 39 , 49 , 50 Five of the studies examined the association of various factors (emotionalism, nursing follow‐up, depression, training of patient and anxiety) with coping behaviour and two investigated coping as a predictor of outcome. Most of the studies had modest sample sizes, ranging from 30 to 76 participants. The timing of assessment of coping after stroke also varied, ranging from 1 week to 3 years. The mean age (average of reported means) was 65 (SD 8.6) years, with two means identified as outliers (38.6 and 78.1). The sample populations in studies in which mean ages were outliers were not constituted entirely of a population with stroke. 42 , 51
| Study reference | Study aim | Coping definition | Coping measure | Study population | Findings |
|---|---|---|---|---|---|
| (a) Sample size | |||||
| (b) Age in years and sex | |||||
| (c) Time of assessment | |||||
| Eccles | To explore psychological characteristics of patients with stroke with emotionalism | ND | MASS | (a) n = 65 patients with stroke(b) Mean age = 71.8; 29 male, 36 female(c) 1 month after stroke | Association between emotionalism and the strategies helplessness/hopelessness and anxiety preoccupation |
| Wahl | To explore changes between predictors (ie, sociodemographics, subjective health, social support, anxiety and coping) and outcome measures (ie, subjective well‐being and autonomy) before and after rehabilitation treatment | ND | Trier Scales on coping with illness | (a) Patient sample n = 34 (stroke), 44 (fractures), 22 (other)(b) Mean age = 78.1(c) Between 1 and 3 months | No findings specific to patients with stroke |
| Fitchett | To investigate the relationship between religion and health outcomes in patients undergoing medical rehabilitation | Positive religious coping provides a sense of meaning that may aid in coping with stressful life events or on a cognitive level, religious beliefs may provide a sense of self‐efficacy in the face of stress or a way to positively reframe negative events. | Brief RCOPE | (a) Patient sample n = 114 (17% stroke, 49% hip and knee joint replacement, 17% amputation, 17% other)(b) Mean age = 65.2(c) Admission, discharge and 4 months follow‐up | No findings specific to patients with stroke |
| Negative religious coping interprets a stressful event as a sign of abandonment or punishment by God | |||||
| King | To describe the natural history of adaptation to stroke and to identify survivor and care giver predictors of depressive symptoms | The coping process, initiated to restore equilibrium (adaptation), includes cognitive appraisal of the importance of the illness, identification of adaptive tasks and coping skills | WCQ | (a) n = 53 patients with stroke(b) Mean age = 58.4; 17 male, 36 female(c) Before discharge, 6–10 weeks, 1 and 2 years after discharge from acute rehabilitation | Less frequent use of finding meaning and more frequent use of avoidance coping correlated with greater depressive symptoms before discharge. Most coping process variables did not change markedly over time |
| Easton | To examine effects of nursing follow‐up on coping strategies used by patients undergoing rehabilitation after discharge | Efforts to master conditions of harm, threat or challenge when a routine or automatic response is not readily available | Jalowiec Coping Scale | (a) n = 46 (stroke), 33 (orthopaedic) and 21 (other)(b) Mean age = 69(c) At discharge and at 4 months after discharge from rehabilitation | No findings specific to patients with stroke |
| Rochette and Desrosiers | To explore type of coping strategies used after stroke; to verify if coping strategies change over time, and are related to age, sex, actualisation of potential, handicap level and depression | Ongoing cognitive and behavioural efforts to manage specific external or internal demands that are appraised as taxing or exceeding the resources of the person | WCQ | (a) n = 76 patients with stroke(b) Mean age = 68.3(c) 2 weeks and 6 months after discharge from rehabilitation | Problem solving and magical thinking were most used and escape avoidance was least used. Women used more coping strategies and obtained higher scores on the magical thinking subscale. Positive‐reappraisal strategies were related to handicap level whereas the magical‐thinking and escape‐avoidance strategies were related to depression levels |
| Sinyor | To examine relationships between depression after stroke, functional status and rehabilitation outcome | ND | Coping Scale (COPE) | (a) n = 64 patients with stroke (30 depressed, 34 non‐depressed)(b) Mean age = 68.8 (depressed group), 65.7 (non‐depressed group); male 53% (depressed), 68% (non‐depressed)(c) Mean days after stroke = 58.6 (depressed group), 55.5 (non‐depressed group) | Patients who were depressed used less behavioural action and rational cognition strategies |
| Herrmann | To describe determining factors of coping strategies and possible related factors in patients with aphasia and their relatives in the first year after stroke | On the basis of results, defined coping as not a form of behaviour specific to the actual situation, but reflects pre‐morbidly acquired attitudes and modes of behaviour (trait rather than state factors) | FQCI | (a) n = 58 patients with stroke(b) Age<75, median = 64(c) 1 week, 1, 6 and 12 months after stroke | 6 months after stroke, active and problem‐oriented styles of coping dominated in aphasic and non‐aphasic patients12 months after stroke, active, problem‐oriented strategies continued to dominate the coping styles of non‐aphasic patients, whereas the strategy “distraction and self reorganisation” dominated as a coping style by aphasic patients |
| Johnson and Pearson | To measure effects of a structured educational course on stroke survivors' response to living with their stroke‐related disabilities and how it can contribute to the rehabilitation process of stroke survivors who have returned to living in the community | ND | WCQ‐CVA | (a) n = 41 community‐dwelling stroke survivors(b) Treatment group (mean age = 64.2; 8 male, 13 female) control group (mean age = 63.9; 10 male, 10 female)(c) Between 6 months and 3 years after stroke | No marked differences before and after intervention in the scores on coping between the treatment and control groupsWomen, subjects ⩽60 years and with deficits in the left hemisphere had higher coping scores |
| Finset and Andersson | To investigate coping strategies in patients with acquired brain injuries | The person's cognitive and behavioural efforts to manage (reduce, minimise, master or tolerate) the internal and external demands of the person–environment transaction that is appraised as taxing or exceeding the resources of the person(Transactional Theory of Stress and Coping) | COPE Questionnaire | (a) Patient sample n = 30 (CVA), 27 (TBI) and 13 (HBI) comparison group n = 71 students(b) Mean age = 38.6 (patient group), 25.2 (student group)(c) Mean time from injury to participation in study = 12.7 months | Approach‐oriented strategies, active coping and positive reinterpretation gained higher scores than strategies expressing avoidance, denial and behavioural disengagement. Association between lack of approach‐oriented coping with apathy and avoidant coping was associated with depression |
| Gillespie | To investigate relationships between after stroke symptoms of anxiety, coping activity and stage of recovery | The function of coping has been taken to be the attenuation of distressing psychological outcomes such as anxiety and depression(Transactional theory of stress and coping) | WCC | (a) n = 44 patients with stroke(b) Mean age = 68.6; male 66%(c) Early group <6.95 months after stroke, late group >6.95 months after stroke | Anxiety was associated with more frequent use of avoidant coping strategies |
| Herrmann | To investigate coping styles in patients with different brain disorders | ND | FQCI | (a) Patient sample n = 21 (MBT), 30 (CVA), 58 (TBI) and 54 (PD)(b) Stroke group mean age = 59(c) Stroke group 12 months after stroke | Patients with stroke used fewer active, problem‐oriented coping than did patients with other brain disorders |
| Herrmann | To investigate coping strategies and psychosocial changes in patients with PD and stroke (CVA) and their relatives | ND | FQCI | (a) Patient sample n = 50 (CVA) and 54 (PD)(b) Mean age: CVA = 61, PD = 64(c) Mean time (months) after onset of illness: CVA = 26, PD = 96 | Active problem‐oriented coping and distraction predominated as coping styles for the stroke group and the degree of motor impairment correlated with a depressive coping style |
| De Sepulveda and Chang | To examine relationships among social support, appraisals of stroke disability, method of coping with disability in the community and effectiveness of coping strategies | Coping behaviour was defined as constantly changing cognitive and behavioural efforts to manage specific external or internal demands that are appraised as taxing or exceeding the resources of the person | WCQ | (a) n = 75 community‐dwelling stroke survivors(b) Age>62, mean = 75(c) Disabled by stroke within the last 3 years | Emotion‐focused coping behaviours were used more often than problem‐focused behaviours. Functional disability reduced coping effectiveness |
| Transactional theory of stress and coping | |||||
Brief RCOPE, Brief Religious Coping Scale; COPE, Coping Orientation for Problem Experiences; CVA, cerebral vascular accident; FQCI, Freiburg Questionnaire of Coping with Illness; HBI, hypoxic brain injury; MASS, Mental Adjustment to Stroke Scale; MBT, malignant brain tumour; ND, no definition of coping; PD, Parkinson's disease; TBI, traumatic brain injury; WCC, Ways of Coping Checklist; WCQ, Ways of Coping Questionnaire; WCQ‐CVA, Ways of Coping—Cardiovascular Accident.
Conceptual basis
Five studies defined the term “coping” 39 , 42 , 45 , 48 , 50 and four made reference to a coping theory or model. 39 , 42 , 45 , 48 The only consistent definition of coping used in three of the studies 42 , 45 , 50 was that by Lazarus and Folkman. 17 , 18 , 20 Two other studies 39 , 48 used definitions that have some resemblance to the Lazarus and Folkman definition. Of the studies that used a model of coping, three 42 , 45 , 48 used the Transactional Theory of Stress and Coping 17 , 18 , 20 and one 39 used the Moos and Tsu 55 model of the crisis of physical illness.
Coping measures and domains
Ten different coping measures were identified in the 14 studies reviewed, with some measures used in more than one study—for example, the WCQ. 31 Table 2 2 presents an overview of the measures used, including the coping domains assessed by each of the coping measures, and the psychometric properties of each measure provided in the studies reviewed. The WCQ was the most commonly used of the coping measures and was used in five studies. The full 66‐item WCQ, 31 however, was used in only one study, 45 with modified versions of the scale used in the remaining three studies reviewed. 39 , 48 , 50 The next most used coping measure in the studies was the Freiburg Questionnaire on Coping with Illness, 37 represented in three of the studies. 43 , 44 , 49 The Freiburg Questionnaire on Coping with Illness is an instrument widely used in German‐speaking countries, in comparison with the internationally used WCQ. Two condition‐specific measures of coping were used in two studies. One study 46 used a modified version of the Mental Adjustment to Cancer Scale 61 and titled their version the Mental Adjustment to Stroke Scale. The second condition‐specific measure was a revised version of the Ways of Coping—Cancer Scale. 36 This revised version was called the Ways of Coping—Cardiovascular Accident 54 Scale.
| Coping scale | Coping domains and strategies | Items | Study reference | Reliability | Validity | |
|---|---|---|---|---|---|---|
| Consistency | Stability | |||||
| Cronbach's α | Test–retest | |||||
| WCQ | ConfrontiveSeeking social supportPlanned problem solving Self‐controlAcceptance of responsibilityEscape‐avoidance behaviourPositive reappraisal | 66 | De Sepulveda and Chang | 0.63 (emotion focused)0.73 (problem focused) | NDI | Emotion‐focused coping correlated with social support (r = 0.20, p = 0.05) and with income (r = 0.22, p = 0.05) |
| A shortened versionWCQ | Finding meaningCompromisingCautiousActive problem solvingSeeking social supportAvoidance | 40 | King | Revised scales ranged from 0.59 (compromising) to 0.72 (avoidance) at T1; 0.60 (active problem solving) to 0.83 (finding meaning) at T4 | NDI | Frequency of seeking social support decreased over time, F(3, 105) = 6.0, p = 0.001Predictors of depression at T1 were less frequent use of finding meaning, r = −0.30, p<0.05 and more frequent use of avoidant coping, r = 0.38, p<0.01 |
| 0.59 (active problem solving), 0.61 (compromising) at T2; and 0.41 (compromising) at T3; 0.62–0.90 for other remaining scales | ||||||
| A shortened versionWCQ | Magical thinkingDistancingSelf‐controllingSeeking social supportEscape avoidancePositive reappraisalProblem solving (confrontive coping excluded) | 28 | Rochette and Desrosiers | Reported internal consistency 0.61–0.79 for the original scale NDI for this 28‐item shortened version | NDI | Sex, correlated with the total coping scale (r = 0.29, p = 0.01) and with magical thinking (r = 0.36, p = 0.002)Actualisation of potential correlated with total coping scale (r = 0.33, p = 0.003); seeking social support (r = 0.31, p = 0.007); positive reappraisal (r = 0.50, p<0.001); and problem solving (r = 0.43, p<0.001)Handicap level correlated with positive reappraisal (r = 0.34, p = 0.003). Depression correlated with magical thinking (r = 0.33, p = 0.004) and escape avoidance (r = 0.45, p<0.001) |
| Modified version of WCC | Acting and distractionDistancingProblem‐solving | 28 | Gillespie | NDI | NDI | Anxiety correlated with the coping strategy “acting out and distraction” in the >6 months after stroke group (r = 0.46, p<0.05) |
| FQCI (short version) | Depressive copingActive, problem‐oriented copingDistraction and self reorganisation | 35 | Gillespie | NDI | NDI | 6 months after stroke, active and problem‐oriented styles of coping dominate in aphasic and non‐aphasic groups, more pronounced in the non‐aphasic group (Mann–Whitney U test; p = 0.014) |
| Religious relief/questfor senseMinimisation and wishful thinking | Only significant change found between 6 and 12 months was an increase of the distraction and self‐reorganisation strategies of the relatives (Wilcoxon matched pairs signed ranks test; p = 0.05). | |||||
| 35 | Herrmann | NDI | NDI | Patients with PD exhibited active strategies (median PD 3.2, CVA 2.4, p<0.05, U test) and religious relief and quest for sense (median PD 3.0, CVA 2.4; p<0.01, U test) more strongly than patients with CVA | ||
| Degree of motor impairment correlated with a depressive coping style only in patients with CVA (r = −0.57, p<0.001) | ||||||
| 35 | Herrmann | NDI | NDI | Active problem‐oriented coping significantly different between study groups (Χ = 11.5, df = 3, p = 0.009), CVA with lowest values. Significant positive correlation between depressive coping and motor impairment in patients with stroke (r = 0.30, p = 0.01) | ||
| Brief RCOPE | Positive religious copingNegative religious coping | 21 | Fitchett | 0.89 (positive religious coping)0.45 (negative religious coping) | Positive and negative religious coping had moderate to high correlations between baseline and the 4‐month follow‐up(r = 0.82 and 0.66, p<0.001) | Positive (r = 0.28, p<0.01) and negative religious coping (r = −0.22, p⩽0.05) at admission correlated with life satisfaction at follow‐up.Positive religious coping correlated with life satisfaction (r = 0.24, p⩽0.05) and negative religious coping correlated with depression (r = 0.21, p⩽0.05) at follow‐up. Patients whose mobility control had not changed or had worsened (n = 30) had higher positive religious coping scores than those whose mobility control had improved (means = 18.41 and 14.57, respectively, t (92) = 2.15, p = 0.03) |
| COPE Questionnaire | Active copingPlanningSuppressionRestraint copingSeeking social support(instrumental and emotional)Positive reinterpretationAcceptance | 52 | Finset and Andersson | The internal reliability of the 12 indexes varied from 0.56 to 0.80, 3 indexes falling below 0.60 | NDI | Significant positive relationship between approach sum score and somatic symptoms score of the MADRS (r = 0.26, p<0.05) in a partial correlation with apathy controlled. Avoidance coping correlated with behavioural/affective apathy (r = 0.34, p<0.01) and with all measures of depression including total depression (r = 0.44, p<0.01). A trend for patients with HBI to have higher avoidance coping than patients with CVA, with patients with TBI in between |
| Focus on emotion | ||||||
| Denial | ||||||
| Behavioural and mental disengagement | ||||||
| Modified version of the COPE | WorrySuppressionBehavioural actionRational cognitionDenial | 19 | Sinyor | NDI | NDI | Depression was associated with less endorsement of both behavioural action (SDS r = −0.26, p<0.05) and rational cognition (CDI r = 0.27, p<0.05) strategies |
| Denial | ||||||
| The Trier Scales on coping with illness | RuminationSearch for meaning in religionThreat minimisation Information seekingSearch for affiliation | 37 | Wahl | 0.74 (rumination), 0.76 (search for affiliation), 0.73 (threat minimisation), 0.84 (information seeking) and 0.80 (search for meaning in religion) | NDI | Information seeking correlated with subjective well‐being at T1 and T2 (r = 0.83 and 0.85, respectively), with autonomy at T1 and T2 (r = 0.87). Search for affiliation correlated with subjective well‐being at T1 and T2 (r = 0.96 and 0.97, respectively) and autonomy at T1 and T2 (r = 0.94 and 0.96, respectively) |
| Jalowiec Coping Scale | ConfrontiveEvasiveOptimisticFatalisticEmotivePalliativeSupportiveSelf‐reliant | 60 | Easton | Coping effectiveness scores at discharge and at 4 months (r = 0.77 and r = 0.93) | NDI | Mean scores for optimistic and fatalistic coping styles were significant (p<0.05) at discharge and for evasive, fatalistic, palliative and supportive coping styles (p<0.05, p<0.01, p<0.001) at 4 months after discharge for experimental group |
| WOC‐CVA | DistancingFocusing on the positiveSeek and use social support | 31 | Johnson and Pearson | NDI | NDI | No significant difference in the score on coping either before (F = 1.34, p<0.55) or after the treatment intervention (F = 1.19, p<0.73). Ways of coping approached significance before and after treatment (t = −2.05, p<0.055) |
| MASS | Fighting spiritHopelessness/helplessnessAnxious preoccupationFatalismAvoidance | 40 | Eccles | NDI | NDI | There was an association between the MASS subscales helplessness/hopelessness (F = 11.71, p = 0.001) and anxious preoccupation (F = 8.05, p = 0.006). The associations with fatalism (F = 14.79, p = 0.052) and avoidance (F = 0.06, p = 0.80) were not significant after adjustment for the General Health Questionnaire |
Brief RCOPE, Brief Religious Coping Scale; CDI, Composite Depression Index; COPE, Coping Orientation for Problem Experiences; CVA, cerebral vascular accident; FQCI, Freiburg Questionnaire on Coping with Illness; HBI, hypoxic brain injury; MASS, Mental Adjustment to Stroke Scale; MADRS, Montgomery and Asberg Depression Rating Scale; MBT, malignant brain tumour; NDI, no data identified; PD, Parkinson's disease; SDS, Zung Self‐rating Depression Scale; T1, time 1; T2, time 2; T3, time 3; T4, time 4; TBI, traumatic brain injury; WCC, Ways of Coping Checklist; WCQ, Ways of Coping Questionnaire; WOC‐CVA, Ways of Coping—Cardiovascular Accident.
Coping strategies used after a stroke
Two studies 42 , 44 reported greater use of active problem‐oriented coping in patients with stroke than in other populations tested, whereas another study 43 reported that patients with stroke used fewer active problem‐oriented coping strategies than participants with other brain disorders. Findings on the use of problem‐focused as opposed to emotion‐focused strategies were conflicting. One study reported greater use of emotion‐focused coping behaviours than problem‐focused coping, 45 whereas another study reported greater use of problem‐focused coping strategies. 50 Avoidance‐type coping strategies were the least used in two of the studies. 42 , 45 The four studies that examined the stability of coping over time found that the coping strategies used did not change markedly at the different time points assessed. 39 , 49 , 50 , 53
On the Mental Adjustment to Stroke Scale, “emotionalism” was found to correlate with helplessness or hopelessness and anxious preoccupation. However, the term “emotionalism” was not defined in the study that used this measure. 46 Anxiety was associated with more frequent use of avoidant coping strategies, 48 whereas patients with stroke who were depressed in comparison with patients with stroke who were not depressed used less behavioural action and fewer rational cognition strategies. 47 Depression was associated with avoidant coping 42 and was specifically associated with greater use of escape avoidance and use of magic thinking coping domains. 50 Training of patients had no effect on coping behaviours on the condition‐specific Ways of Coping—Cardiovascular Accident Scale. 54 Physical ability was associated with coping effectiveness and coping behaviour in two studies. De Sepulveda and Chang 45 reported that functional disability reduced coping effectiveness and Herrmann et al 44 found that the degree of motor impairment correlated with a depressive coping style. Less frequent use of finding meaning and more frequent use of avoidance coping were predictors of depression before discharge from rehabilitation. 39
Psychometric properties
Table 2 2 presents the psychometric properties of the coping scales. Internal consistency data were reported for coping subscales in seven studies. Therefore, in seven studies no psychometric data were reported. One study reported internal consistency values for the original WCQ measure and no data were identified for the modified version of the scale that was used. 50 Where reported, Cronbach's α's ranged from 0.41 to 0.90 (table 2 2). ). Only one coping measure (The Trier Scales on coping with illness) 56 reported internal consistency reliabilities with Cronbach's α of 0.7 or higher for all subscales. Of note, test–retest reliabilities were identified by one study that reported moderate to high correlations of the Brief Religious Coping Scale's coping strategies over time. 52
The main type of validity data reported in nine studies was r‐specified values, where the coping subscales were correlated with other specified variables. In five of these studies, the r values reported were <0.5, indicating that the strength of correlations between variables was generally weak to moderate. One study reported high correlations between the Trier Scales on coping with illness subscales and other variables, with r values >0.8. 51 The coping domains of information seeking and search for affiliation correlated highly with subjective well‐being and autonomy, providing supporting evidence of the validity of this scale. Overall, there was little evidence of construct validity for the coping scales used in the studies reviewed, and the correlations between the subscales of the coping scales and other variables reported were generally weak.
The aim of this paper was to review quantitative coping research in populations of patients with stroke. Overall, a modest number of papers met the search criteria, highlighting the scarcity of quantitative research on the processes of coping and adaptation in the literature on stroke. Although over the past decade psychosocial aspects of recovery in stroke have begun to receive attention, much of the literature continues to focus on physical abilities. Not all studies reviewed had a full complement of patients with stroke, but included other vascular and cerebral diseases, making comparisons between studies complex and reducing the possibility of finding consistencies between studies. A further reason for the small number of studies identified in this review may result from reporting bias, in that only the studies with significant findings could have been published. In addition, given that the median sample size for patients with stroke reported in table 1 1 is 55, the values reported in the current review may be overestimates of the size of relationships between coping strategies and other variables. Routine reporting of confidence intervals for sample correlations would provide greater insight into the plausible range of correlation values and facilitate more definitive conclusions regarding the strength of the relationship between coping strategies and other variables.
This review discussed some of the major conceptual issues that exist in the literature with regard to coping measurement after stroke. These issues include the lack of consistent definitions throughout studies and the deficiency of coping theoretical frameworks. Eight of the studies defined what they meant by the term “coping”, 39 , 42 , 45 , 48 , 49 , 50 , 52 , 53 with a consistent definition used in three of the studies. 42 , 45 , 50 The conceptual shortcoming of inconsistent definitions shares some commonality with the general literature on coping. Only a small number of studies outlined a theoretical framework of coping, the one most often used being the Transactional Model. 20 Moos and Tsu's 55 model of coping with physical illness was also identified in the review, but this model is not quoted as often as the Transactional Theory in the general literature. A large number of coping questionnaires, each proposing different dimensions, exists in the general literature on coping. This was reflected in the current review, where 10 different coping measures were used in the 14 studies reviewed. The heterogeneity of coping measures in the studies reviewed creates challenges for detecting trends or drawing conclusions regarding the use of coping strategies after stroke.
The conceptualisation of the structure of coping to date has been complex and varies in terms of measurement in different studies. A helpful development has been the hierarchical conceptualisation of Skinner et al , 63 in which the structure of coping spans the conceptual space between instances of coping and adaptive processes. This hierarchy operates (from the bottom up) on four levels: (1) instances of coping (eg, “I wore my lucky t‐shirt the day of the exam”); (2) ways of coping (eg, problem‐solving, rumination, venting, escape); (3) dimensions of coping (eg, problem, emotion, avoidance‐focused coping); and (4) strategy of adaptation (ie, continuing to secure adequate information about the environment or escaping from a potentially dangerous transaction). This conceptualisation of the structure of coping organises the various coping items and domains identified by the various coping measures in the literature. It provides category systems for classifying ways of coping. This type of framework may prove useful when assessing coping with various different measures and should allow researchers on the subject of coping after stroke to come to some general consensus, as the levels within this framework provide a clearer categorisation of strategies.
Coping measures, domains and strategies
Little overlap was observed in the measures used in the studies included in this review, and the coping strategies used by patients with stroke varied across studies. Overall, it was not possible to identify conclusively the specific coping strategies used by people in either the acute phase after stroke (ie, within the first 6 months) or in the longer term (after 6 months). However, some general trends were reported, as were some recurrent findings. The use of approach and active problem‐oriented coping strategies were reported more often than were emotion‐focused coping strategies. However, the results did not indicate the coping strategies that were more or less effective in terms of outcome of stroke. In the general literature on coping, most negative life events seem to elicit both types of coping strategies, although people with more personal and environmental resources may rely more on approach and active problem‐oriented coping and less on avoidance emotional coping. 64 A longstanding issue in the perspective on individual differences is whether avoidant or emotional responses or problem‐solving coping methods are superior. 16 Avoidant responses may be more effective for managing short‐term threats, 65 but for long‐term threats problem‐solving coping may manage stress more effectively. It is therefore imperative to examine the coping process over longer durations in patients with stroke to determine the strategies consistently used in the long term. This review suggests that, in fact, strategies do not change over time; with considerable stability in use of coping strategies, longitudinal studies failed to detect significant changes over time (p<0.05). However, this apparent lack of change may simply reflect low levels of statistical power. Future research examining the stability of coping strategies over time could use latent growth analysis to explore this issue.
Combining the findings of this review—that is, that coping strategies adopted by patients in the acute phase after stroke are unlikely to change in the longer term 39 , 49 , 54 —with research indicating higher levels of psychological distress in those using less active, problem‐oriented coping strategies and more avoidance strategies 42 , 47 , 48 suggests that an intervention targeted at coping strategies typically associated with distress may improve patient recovery considerably. The general literature has shown similar findings in a variety of studies on diverse populations where emotion‐oriented coping style has been positively linked, for both men and women, with negative health variables such as anxiety, depression and poor recovery from illness. 28 Evidence on coping and recovery of physical function after stroke is generally lacking in the literature. Studies to date have focused on the relationship between physical function and depression. 15 , 44 , 66 Further studies assessing depression and physical function should incorporate the coping process to identify if there is an important predictive relationship between variables. Furthermore, nearly half of the studies reviewed were of sample populations with brain disorders other than stroke. In some of these studies, no specific inferences could be made in relation to the type of coping strategies relevant to a population with stroke.
In most of the studies reviewed, psychometric properties of the coping measures used were under‐reported or were not reported at all. 43 , 54 The internal consistency reliabilities of the coping subscales, where reported, were generally less than the value considered acceptable (Cronbach's α's⩾0.7) and test–retest reliability was reported in only one of the studies reviewed. 52 One study reported internal consistency coefficients from the original psychometric data of the coping measure and reported no data on the modified version of the scale used in the researchers' own study. 50 Specific concerns exist in the context of stroke, such as stroke sequelae—for example, cognitive, language or visual deficits—that may affect reliable measurement in a population with stroke. Of note, only one study described a cognitive screening method. 67 Many generic measures of coping may be less applicable in a population coping with health problems. Hence, many researchers who use scales such as the WCC or the WCQ have modified the instruments when studying medical populations by dropping or adding items, or by changing the scoring system. 28 Although these modified scales may remove some of the problems associated with inapplicable items, according to Parker and Endler, 27 new inadequacies are produced. These include difficulty with generalising results from one sample or health problem to another and frequent poor reporting of psychometric data on these modified scales. In terms of validity, only one category was represented in the results—that is, correlations of coping subscales with other specified variables (construct validity). This finding is in keeping with that of Hogan and Agnello. 41 In an investigation on current research practice regarding reporting measurement validity evidence, only 55% of research reports included any type of validity evidence, and on those reporting validity information, most reported correlations with other variables. The Behavioral Subscales of the Trier Scales on coping with illness showed very strong correlations (r = 0.83–0.97) with well‐being. 46 However, in general, the correlations between coping subscales and other specified variables reported in table 2 2 are weak (eg, r = 0.2) to moderate (eg, r = 0.5). These methodological limitations, such as the conceptual issues discussed earlier, are similar to deficiencies identified in the general literature on coping. 21 Researchers in the field of coping have described in detail the conceptual and methodological difficulties regarding the measurement of coping. 21 , 30 , 68 , 69
Further directions and conclusions
Literature on measuring coping quantitatively in a population with stroke remains scarce, allowing both researchers and clinicians to draw few inferences on the type of coping strategies people actually use in both the acute and chronic stages after stroke. No unique coping strategies are used at different time points across the adaptive recovery period, but coping strategies seem to remain consistent over time. This is supportive of a dispositional approach, which assumes that people bring to a given context a relatively stable coping “disposition” that is minimally influenced by situational contingencies. 28 Most coping measures used in the studies reviewed have one or more psychometric limitations—for example, weak correlations with other variables or inadequate psychometric reporting of the measures used in the studies and a failure to account for difficulties with measuring due to stroke sequelae, such as communication difficulties or cognitive impairment.
Considerable potential exists for further investigation on this topic, but it is imperative for authors to state their definition and framework of coping. The limited number of follow‐up studies on stroke should encourage more longitudinal studies assessing coping over time, with particular attention to assessment of coping within the initial acute phase of stroke—that is, within the first month—as a marker to determine what people are likely to use in the long term. It remains to be clarified whether maladaptive strategies can be identified by examining associated variables such as quality of life, mood and level of disability—for example, what the patient is able to do for himself or herself outside the clinical setting. Lazarus 70 suggested that within‐subject prospective longitudinal research is required to measure coping, as this allows researchers to identify psychological structures such as stable personality dispositions and changes (or processes) in psychological reactions over time and diverse conditions.
Summary points
- A limited number of studies deal with coping as part of the psychological adaptation process after stroke.
- Definitions of coping are heterogeneous and absent in some studies.
- Theoretical frameworks to support operational coping models are lacking.
- Psychometric properties of coping measures are under‐reported in relation to both reliability and validity.
- The findings identify the scope for further exploration of the coping process after stroke.
From this review, there are no inferences that can be made on the type of coping strategies used in a population with stroke. Further studies are required that consistently use coping measures with similar coping domains to ensure identification of broadly successful and unsuccessful strategies in the context of stroke. Consideration and specification of adaptation models relevant to the adaptation process after stroke will further improve the use of findings from research studies on coping and adaptation after stroke.
This research was supported by a Programme Grant from the Irish Health Research Board (HRB): Professor Hannah McGee (Principal Investigator), Royal College of Surgeons in Ireland (RCSI); Professor Des O'Neill (Trinity College Dublin (TCD)); Dr Tony Fahey (Economic and Social Research Institute (ESRI)); and Professor Bob Stout (Queens University Belfast (QUB) (Co‐Investigators).
Acknowledgements
We thank the other research staff of the Healthy Aging Research Programme (HARP) and Steering Group members who contributed to this review: Ms Maja Barker, Dr Ronan Conroy, Ms Rebecca Garavan, Dr Frances Horgan, Mrs Karen Morgan, Dr Ann O'Hanlon (project coordinator), Dr Emer Shelley (RCSI), Dr Vivienne Crawford, Mr John Dinsmore, and Dr Richard Layte (ESRI).
Abbreviations
WCQ - Ways of Coping Questionnaire
Competing interests: None declared.

Brain Exercises For Stroke Recovery Patients: Improving Cognitive And Memory Functions

Christopher Ravn
Key takeaways.
1. A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. 2. Training and exercising a stroke survivor's brain is known as stroke rehabilitation. 3. Memory exercises are a fundamental part of stroke rehabilitation, helping to retrain the brain and improve cognitive function that may have been affected by the stroke.
Table of Contents
1. What Are The Best Brain Exercises For Stroke Recovery? 2. What Are The Benefits Of Cognitive Exercises For Stroke Patients? 3. How Do You Train And Exercise Your Brain After A Stroke 4. How Effective Are Brain Stroke Recovery Exercises? 5. What Are Cognitive Therapy Activities For Stroke Victims And Survivors? 6. What Cognitive Activities For Adults After Stroke Are Most Effective? 7. How Do Stroke Cognitive Rehabilitation Activities Work? 8. Frequently Asked Questions About Brain Exercises For Stroke Recovery
What Are The Best Brain Exercises For Stroke Recovery?
A stroke is a serious, life-threatening medical condition that happens when the blood supply to part of the brain is cut off. Strokes occur when a blood clot blocks the flow of blood and oxygen to the brain. These blood clots are typically the result of atherosclerosis, or arteries narrowed or blocked over time by fatty deposits. This is the most common type of stroke. Less common are hemorrhagic strokes, where a blood vessel supplying the brain bursts.
People who survive a stroke are often left with long-term problems caused by an injury to their brain . They will face challenges with thinking, reasoning, awareness, and memory. If help is obtained over time, the brain retains some function but needs to reorganize itself. This journey to recovery is arduous and involves relearning skills, improving physical coordination, and maintaining cognitive functions.
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills . These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.
What Does Science Say About Light Therapy?
Find a collection of academic research papers that we, together with top-tier academic research institutions. We are exceedingly proud of our work and incredibly grateful to collaborate with such wonderful research institutions.
What Are The Benefits Of Cognitive Exercises For Stroke Patients?
Cognitive exercises play a crucial role in the rehabilitation of stroke survivors, but they need to be practiced consistently to be most effective. Following a stroke, the brain is busy rewiring new pathways to bypass the affected areas – a process known as neuroplasticity. Functions are being rewired to new, healthy areas of the brain, to compensate for tissue damage sustained in the stroke.
How Do You Train And Exercise Your Brain After A Stroke
Training and exercising a stroke survivor’s brain is known as stroke rehabilitation . These typically are a program of different therapies, designed for the survivor to help them with movement, speech, strength, and daily living skills post-stroke. The aim is to help them regain their independence and quality of life.
What’s involved in stroke rehabilitation is speech and language therapy , focused on improving communication skills affected by the stroke and common post-stroke issues such as swallowing difficulties, otherwise known as dysphagia.
We Believe Prioritizing Brain Health Enhances Your Quality Of Life
Get to know our team, our mission and how our EVY LIGHT® can provide you and your loved ones with a fuller life, letting you breathe a little easier.
How Effective Are Brain Stroke Recovery Exercises?
According to the National Library of Medicine, approximately 40% of patients suffer from functional impairment after stroke onset, and 15–30% experience severe motor, sensory, cognitive, perceptual, and/or language impairments.
Rehabilitation is vital for stroke survivors, and those who undergo consistent and professional rehabilitation tend to recover quickly . Studies have shown that rehabilitation exercise regimens applied soon after a stroke are effective. The programs will need to be tailored to the survivor and how they were affected, so that the correct areas are given the necessary attention.
Cognitive issues are often the most debilitating and difficult-to-address consequences of a stroke. A stroke survivor with memory and attention issues who engages in cognitive therapy, including puzzles and memory games , could experience improvements in their memory and concentration, allowing them to better manage daily tasks and activities.
One may question what the difference is between regular exercises and those intended for stroke patients. The answer lies in their intention. Pre-stroke exercises are typically general and aim to maintain overall health and well-being – cardio, strength training, and muscle toning, for example. In contrast, post-stroke exercises are more targeted, focusing on the rehabilitation and recovery of specific functions affected by the stroke. Post-stroke exercises often involve intensive therapy tailored to individual needs, such as speech therapy, physical therapy, and cognitive exercises.
Studies have shown that brain stroke recovery exercises can be highly effective in improving functional outcomes and quality of life for stroke survivors. Studies published in the Journal of Stroke found that intensive rehabilitation programs significantly improved motor function and activities of daily living in stroke patients. Another study published in the Journal of Neurologic Physical Therapy showed that cognitive rehabilitation can lead to improvements in memory, attention, and executive function in stroke survivors.
What Are Cognitive Therapy Activities For Stroke Victims And Survivors?
Cognitive therapy is designed to improve cognitive functions affected by the stroke, for example, memory, processing speed, problem-solving, language, and executive functions . The aim is to challenge the brain in a supportive way.
Cognitive therapy would include memory exercises, e.g., card games to improve short-term working memory; puzzles, computer games, and reading and summarizing to improve their attention, concentration, and information processing; reading, writing, and conversation practice to help with communication; drawing; navigation tasks to help with visual-spatial orientation, planning, and awareness; and problem-solving tasks to help improve planning and organization skills.
What Cognitive Activities For Adults After Stroke Are Most Effective?
How do stroke cognitive rehabilitation activities work.
A 37-year-old stroke survivor participated in memory-based exercises as part of his rehabilitation program. He regularly played memory games and engaged in storytelling activities with his therapist. Over time, his short-term memory and cognitive function significantly improved . He was able to recall important information, make decisions more confidently, and communicate more effectively with his family and healthcare providers.
Family members can play a crucial role in implementing these activities and supporting stroke rehabilitation. They can be educated on the importance of consistency and patience, as progress may be gradual.
Short-Term Memory Loss Exercises To Train Your Brain After A Stroke
- Repetition: This involves repeating information or tasks multiple times to reinforce memory. For example, repeating a new phone number several times to remember it.
- Association: This technique involves linking new information with existing memories or concepts. For instance, associating a new face with a familiar name or place.
- Visualization: Creating mental images can aid memory recall. For instance, visualizing a grocery list as items in specific locations in your home.
- Chunking: Breaking down information into smaller, manageable chunks can make it easier to remember. For example, remembering a long number by grouping it into smaller sets.
- Memory Games: Playing memory games like matching cards or word recall can be fun and effective. These games challenge the brain and improve memory skills.
Music Stimulation Therapy For Stroke Survivors
Music stimulation therapy can benefit stroke survivors by engaging multiple areas of the brain. Listening to music activates the auditory cortex , which processes sound, while also stimulating areas responsible for memory and emotions. This stimulation can enhance cognitive functions such as memory, attention, and executive function. Additionally, music can evoke emotional responses that may help reduce stress and anxiety, which are common after a stroke.
Some examples of music-based exercises at home include listening to familiar music, such as the stroke survivor’s favorite songs or music from their past. This can evoke memories and emotions, stimulating cognitive function. Caregivers and guardians can sing along to these songs with the patient, to further engage the areas of the brain responsible for these functions.
Enhance your brain performance through the power of light.
Comfortable and easy to use 40Hz light therapy to support and improve your brain function.
Motor Skills Activities For Adults After A Stroke
- Finger Tapping: Tap each finger to your thumb in sequence, then reverse the order. This can improve individual finger movements
- Finger Stretching: Gently stretch your fingers and thumb apart, then bring them back together. Repeat several times to improve flexibility and control.
- Drawing: Encourage drawing simple shapes or patterns, progressing to more complex drawings. This can improve hand-eye coordination and fine motor skills.
- Painting: Use a brush or fingers to paint on paper or canvas. This activity can improve grip strength and coordination.
Practicing Games For Stroke Rehabilitation
- Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like “Train of Thought” and “Memory Matrix” are particularly effective for cognitive exercise.
- Nintendo Wii Fit: Games like “Balance Bubble” and “Table Tilt” can improve balance, coordination, and cognitive function through interactive gameplay.

Other Activities That Help Retrain The Brain After A Stroke
An overall change in daily routines is crucial in stroke recovery to promote brain retraining and maximize rehabilitation outcomes.
The most important are physical activity and cognitive stimulation . Incorporating regular physical activity into daily routines can improve blood flow to the brain, promote neuroplasticity, and enhance overall brain health. Activities like walking, yoga, or tai chi can be beneficial.
As for mentally stimulating activities, these include reading, puzzles, or learning new skills, which can help retrain the brain and improve cognitive function . These activities should be challenging but achievable to promote brain plasticity.
Physical Activities In Cognitive Rehabilitation
- Walking: A safe and effective way to improve cardiovascular fitness and mobility. Start with short distances and gradually increase.
- Balance Exercises: Standing on one leg, heel-to-toe walking, and other balance exercises can improve stability and reduce the risk of falls.
Meditation And Relaxation Techniques For Cognitive Stimulation
- Focused Breathing: Sit comfortably and focus on your breath. Inhale deeply through your nose, hold for a moment, and exhale slowly through your mouth. Repeat for several minutes, focusing only on your breath.
- Guided Meditation: Use audio recordings or apps that guide you through a meditation practice, focusing on relaxation, gratitude, or mindfulness.
Social Participation As A Cognitive Exercise
- Support Groups: Joining a stroke support group allows individuals to connect with others who have experienced similar challenges, provide emotional support, and share coping strategies.
- Book Clubs or Discussion Groups: Participating in a book club or discussion group provides opportunities for intellectual stimulation and social interaction.
- You could also recommend light therapy for depression, as most would be negatively impacted by it.
Technology Aid In Stroke Rehabilitation Exercises
Apps and other digital tools can assist in cognitive rehabilitation post-stroke by providing accessible and engaging ways to improve cognitive functions. These tools can offer personalized exercises, real-time feedback, and progress tracking, making rehabilitation more efficient and effective .
Learn What Others Have Experienced with EVY Light
See how others have achieved a sharper mind by activating their gamma brainwaves in combination with maintaining a healthy lifestyle.
Frequently Asked Questions About Brain Exercises For Stroke Recovery
The best exercises for stroke recovery focus on cognitive rehabilitation, including problem-solving activities like puzzles and board games, which enhance cognitive flexibility and decision-making skills. These exercises play a crucial role in helping individuals regain cognitive functions affected by stroke, such as memory, problem-solving skills, processing speed, and attention span, ultimately aiding in their recovery journey.
What Are Cognitive Therapy Activities For Stroke Patients?
Receive notification when news, blogs, promotions, or other valuable information drops.

How To Use A Light Therapy Lamp Effectively In The Morning, Day, Or Night

Lewy Body Dementia Vs Parkinson: Key Differences, Symptoms & Common Misdiagnosis

Alcohol-related Dementia: Detecting Symptoms, Causes, & Life Expectancy Management Tips

Free Care For Dementia & Alzheimer’s Patients: How To Get Financial Assistance & More

Amnesia Vs Dementia: Differences In Memory Loss & Similarities

What Makes Dementia & Alzheimers Eyes Look Different? How To Tell It’s Coming

How To Care For Someone With Dementia: 10 Helpful Tips

When Should Someone With Dementia & Alzheimer’s Go Into A Care Home? Key Indicators

Alzheimer’s & Dementia Supplements: Best Vitamins & Tips To Slow Down Progression

At What Stage Do Dementia Patients Forget Family Members? What Happens & How To Manage

Dementia Anger: Common Triggers, How To Deal & Handle Fits Of Rage

Why Do Dementia & Alzheimer’s Patients Stop Eating? What To Do And Not Do
How To Get Dementia & Alzheimer Patients To Sleep At Night: Expert Tips To Keep Them In Bed

Xanax And Dementia: Potential Risks Between Benzodiazepines And Dementia

What Stage Of Dementia & Alzheimer’s Is Not Sleeping Very Common? Full Insights

What Age Does Dementia Start? Exploring Causes Of Early Onset Dementia

Senile Vs Dementia: Definitions, Differences & How To Deal With Senility

Parkinson’s Vs Alzheimer’s: Learn The Differences, Similarities & Treatment Insights

Mild Cognitive Impairment (MCI) Vs Dementia: In-Depth Exploration Into These Cognitive Issues

Mild Cognitive Impairment Life Expectancy: How It Differs Across Patients

Melatonin For Dementia & Alzheimer’s: Safe Use For Sleep Improvement In Elderly Patients

How To Deal With Dementia Patients Who Are Aggressive: What To Do And Safety Tips

Does Metformin Cause Dementia & Alzheimer’s? Analyzing The Link Between Metformin And Cognitive Issues

Dementia, Alzheimer And Incontinence: Managing Bladder Control & Different Stages
Activities For Dementia Patients: Recreational Ideas To Keep People With Dementia Active

Alzheimer’s Hallucinations: Identifying Symptoms And Management Strategies

Why Won’t Dementia Patients Take Showers? Understanding The Refusal & How To Assist Bathing Habits

Why Do Dementia Patients Sleep So Much? Reasons Behind Excessive Sleep & How To Prevent It

What Stage Of Dementia Is Sundowning? How To Manage Changes In Behavior & Treat Early Symptoms

What Sleeping Position Is Linked To Dementia? Different Options To Increase Health & How To Prevent Risks

Subjective Cognitive Impairment: Early Diagnose & How To Prevent Other Types Of Cognitive Decline

Mild Cognitive Impairment & Driving: Safety Issues, Abilities Required & Legal Concerns

Light Therapy Lamp Benefits: How To Use For Physical & Mental Conditions, Safety Considerations

Levels Of Cognitive Impairment: How To Determine Four Levels, Evaluation & Management

How To Talk To Someone With Cognitive Impairment: Creative Ways To Encourage Communication & Active Listening

How Long Do The 7 Stages Of Alzheimer’s Last? Duration, Symptoms & Care Needs For Every Stage

Early Signs Of Alzheimer’s In Your 50s: Risks, Symptoms & Testing Methods

Do Light Therapy Lamps Work: How Useful They Are For Different Disorders & How To Maximize Their Benefits

Signs Death Is Near In Alzheimer’s & Dementia: How To Provide Care & Recognize The Symptoms In The Final Stages

How To Deal With A Spouse With Memory Loss: Caring Tips For Living With Memory Loss & First Steps To Take
Mental Exercises For Mild Cognitive Impairment: Ideas For Improving And Preventing Mild Cognitive Decline

How To Help Someone With Cognitive Impairment: Caring & Communication Techniques To Improve The Quality Of Life Of Persons With MCI

How To Deal With Dementia In A Parent: Techniques To Help & Live With Dementia Parents At Home
How To Deal With Fixation In Dementia: Coping With Dementia Behavior Changes & Ideas To Focus Away From Fixation

How to Help Someone with Dementia Remember: A Comprehensive Guide for Caregivers and Families

Is Mild Cognitive Impairment A Disability? Legal Working Rights And Disability Benefits Advice

Living With A Spouse With Mild Cognitive Impairment: Caring Marital Relations To Adapt And Help A Spouse With MCI

How Long Does It Take For Light Therapy To Work: Duration & Frequency For Optimal Results & Benefits

How Long Can A Person With Dementia Live At Home: Setting Up A Safe Home Care Plan, Living Alone & Memory Care Considerations

How Fast Does Mild Cognitive Impairment (MCI) Progress: Turning Into Other Cognitive Decline, Risks Factors & Timeline

How Do Light Therapy Lamps Work? Best Ways To Maximize The Benefits & Timing Sessions

Brain Exercises For Seniors: Fun Ways Of Cognitive Training & How To Improve Mental Health In Older Adults

Sad Light vs Grow Light: How Different Are They?

Gifts for Dementia Patients: What’s a Good Presents Idea for Someone With Alzheimer’s & Memory Loss
Green Light Therapy Treatment & Its Health Benefits
How to Get Guardianship of an Elderly Parent With Dementia: Legal Steps

Meditation Light Therapy: How to Improve All Relaxation Techniques

Music Therapy for Dementia: Helping Patients Memory Functions

Sensory Activities for Dementia Patients: Improving Abilities & Quality of Life

How To Know When To Call Hospice For Dementia: Qualification Considerations

Which Sense Is Most Affected by Alzheimer’s Disease: Early Signs

What Is the Difference Between Memory Care vs Dementia Care?

Best Gifts for Seasonal Depression & Affective Disorder: Top Ideas

Speech Therapy Memory Activities for Adults: Enhancing Cognitive Skills

Light Therapy Treatment For Depression, SAD And Mood Disorders

How To Talk To Someone With Short-Term Memory Loss: Communication Strategies

Green Light Therapy Treatment For Depression, SAD And Mood Disorders

Brain Exercises To Prevent Alzheimer’s And Dementia: Types & The Best Ones

Transforming Lives: Melissa’s Journey with EVY LIGHT®

5 Warning Signs Of Early Alzheimer’s You Can’t Ignore

Crafting a Brain-Boosting Routine
How Learning Impacts The Brain

Thrive Together: Boosting Brain Health with Group Activities

Proactive Brain Health: Aging Gracefully with Science

Support Memory At All Stages of Life

Harnessing the Power of Dopamine for Keeping Mentally Energized

Strategies for Enhanced Focus: Unleash Your Productivity Potential

Move for Mind: The Link Between Exercise and Mental Health

The Vital Connection Between Your Sleep, Body, and Brain

Unlocking the Sunshine: 6 Tips to Banishing Brain Fog

Unveiling the Astonishing Energy Consumption of the Human Brain
Get exclusive content straight from the scientists who are rooting for you and your brain.
Comfortable Daily Use, Drug Free to Promote Focus, Clarity, and Mental Sharpness.
Privacy Preferences
When you visit our website, it may store information through your browser from specific services, usually in the form of cookies. Here you can change your Privacy preferences. It is worth noting that blocking some types of cookies may impact your experience on our website and the services we are able to offer.

COMMENTS
More than half of all stroke survivors experience a post-stroke cognitive impairment. This may affect many functions, including memory, problem solving skills, and the ability to think clearly, among others. However, survivors can often improve their mental aptitude by practicing cognitive exercises for stroke patients.
Percent of Users Identified As Recovering from Stroke: 40%. 6. Do clock math: Stroke can affect number skills, math skills, and word finding. This task helps improve time-based calculation skills by answering math questions associated with clocks. Individuals Assigned: 6,701 Percent of Users Identified As Recovering from Stroke: 37%. 7.
Background and Purpose—This study investigated whether problem-solving therapy (PST) is an effective group intervention for improving coping strategy and health-related quality of life (HRQoL) in patients with stroke. Methods—In this multicenter randomized controlled trial, the intervention group received PST as add-on to standard outpatient rehabilitation, the control group received ...
Your rehabilitation plan will depend on the part of the body or type of ability affected by your stroke. Physical activities might include: Motor-skill exercises. Exercises can help improve muscle strength and coordination throughout the body. These can include muscles used for balance, walking and even swallowing.
Decision making is defined as the process of examining possibilities, risks, uncertainties, and options, comparing them, and choosing a course of action. 1, 2 Decisions based on erroneous assessments may result in incorrect patient and family expectations, and potentially inappropriate advice, treatment, or discharge planning (eg, longer length ...
We developed a unique intervention grounded in stress and coping theory, applying the COPE model to problem-solving for community-dwelling caregivers of veterans with stroke. The nurse-led, active, telehealth format with 4 sessions is a strength because there is a lack of studies combining these three elements.
The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients. The secondary aim is to determine the effect of Problem Solving Therapy on depression, social participation, health care consumption, and to determine the ...
One of the most important relationships you'll have is with your doctor. It's not just about listening to what you're told. You need to ask the right questions — and ask again if you don't get the answers you need. Take part in decisions about your treatment, follow the treatment plan you and your doctor agree on, watch for problems ...
Cognitive therapy apps provide a structured and convenient way for stroke patients to engage in targeted cognitive exercises. From memory games to problem-solving tasks, these apps offer a wide range of activities designed to support cognitive rehabilitation and recovery. 8. Mindfulness Exercises for Stroke Survivors
thinking difficulties. Communication, decision making, and problem solving can become very confusing or overwhelming if these skills are impaired. Many factors can hinder the ability to use deductive reasoning, such as: • Difficulty understanding language or concepts due to aphasia. • Difficulty using convergent and divergent language skills.
Frequently Asked Questions. Next in Stroke Guide. ... Cognitive changes after a stroke include memory glitches, trouble solving problems, and difficulty understanding concepts. ... A recent stroke patient may need assistance getting up and around in the days following a stroke, and staying in bed too long can result in the muscles shrinking and ...
Example strategy games for stroke patients include: Carcassonne: a puzzle-based game that can challenge visuospatial skills and problem-solving. Chess: a traditional game requiring planning, judgement and reasoning. Catan: a building and trading game requiring constant cognitive flexibility and social skills.
problem-solving refers to the "process of finding solutions to specific problems".13 Problem-solving therapy (PST) is an intervention in which patients are taught to increase structure in solving problems and flexibility by using different coping strategies in various situations. In patients with stroke, PST has
The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and health-related quality of life in stroke patients.
Coping style is one of the determinants of health-related quality of life after stroke. Stroke patients make less use of active problem-oriented coping styles than other brain damaged patients. Coping styles can be influenced by means of intervention. The primary aim of this study is to investigate if Problem Solving Therapy is an effective group intervention for improving coping style and ...
Making decisions, solving problems, understanding numbers and managing money can be a challenge. Good cognitive function also relies on memory. The brain uses 2 types of memory to hold information, the long and short term memory. Short-term memory is the temporary store for small amounts of information. ... Stroke can impact on this ability ...
Reactivating the muscles can help stimulate the connection between the brain and muscles, encouraging neuroplasticity. 8. Mirror Therapy. Mirror therapy is another type of stroke intervention that is particularly helpful for survivors with hand paralysis or severe hand impairments.
In this issue of stroke, Ikeme et al 41 conducted a systematic review of acute care services for stroke by race/ethnicity in the United States from January 1, 2010, to April 5, 2021 (n=30 studies). They found that White patients used emergency medical services at a greater rate than Black, Asian, and Hispanic patients.
(a) n = 76 patients with stroke(b) Mean age = 68.3(c) 2 weeks and 6 months after discharge from rehabilitation: Problem solving and magical thinking were most used and escape avoidance was least used. Women used more coping strategies and obtained higher scores on the magical thinking subscale.
The care of patients with stroke begins in the hospital and continues in the community, where recovery, reintegration, and health maintenance take place over the years that follow. 1,2 Primary care clinicians provide most of this long-term care. 3 In a typical primary care practice of 2000 adults, 100 will have a history of stroke, and 5 to 10 will have a new stroke each year. 4-6 The needs ...
The following are some games that are helpful in stroke recovery cognitive exercises. Lumosity: This brain training app offers a variety of games designed to improve memory, attention, and problem-solving skills. Games like "Train of Thought" and "Memory Matrix" are particularly effective for cognitive exercise.
Multicomponent nursing interventions that provide caregivers skills to cope and manage physical, cognitive, emotional, and behavioral stroke-related problems are essential beginning with initial treatment and continuing throughout stroke recovery. 3 Furthermore, caregivers may question how they will manage caregiving long term and report feelings of physical and emotional strain, being worried ...