

How To Implement Effective Strategic Planning In Healthcare

Are you feeling overwhelmed and uncertain about the future?
According to Deloitte , “The global healthcare sector stands at a crossroads in 2024, poised for profound changes. The future of global healthcare is likely to be shaped by innovation, sustainability, social care integration, cost management, and workforce adaptation.”
If you work in the healthcare industry, you know firsthand how quickly things can change. As technology advances, regulations change, the population ages, and new diseases evolve at lightning speed, it can be tough to keep up.
That's why implementing an effective strategic planning process that is execution-ready is so important. It's a tool that helps healthcare organizations prioritize their goals, anticipate potential roadblocks, and quickly adapt to seize new opportunities.
Whether you’re a manager or a top-level executive, this article will provide valuable insights and guidance to help you develop and execute a successful strategic plan.
We'll also show you how Cascade can help you successfully plan, execute, and track your healthcare strategy in one centralized location. Plus, as a bonus, we'll provide a free strategic planning template prefilled with healthcare examples to help you get started.
So, let's dive in and discover how strategic planning can help you navigate the changing landscape of the healthcare environment and achieve your organization’s goals.

Strategic Planning In Healthcare: What Is It?
Strategic planning in healthcare helps you set business goals and decide how to allocate resources to achieve these goals. It involves looking at your organization’s internal and external environments using established strategic tools .
Doing so lets you develop a strategic plan outlining what you want to achieve and an action plan to get there. Think of it like building a roadmap that helps you get to where you want to go.
With a healthcare strategy, you’ll have a framework for improved decision-making that is aligned with your overarching business objectives . This ensures you’re moving towards your long-term goals and objectives, even when making short-term decisions.
Examples Of Strategic Planning In Healthcare
Strategic planning can significantly enhance the operational efficiency and service quality of healthcare organizations. Here are some specific examples of how you can use strategic planning:
- Boosting Patient Care Quality : Tackle specific challenges like lowering the rates of hospital-acquired infections or enhancing the coordination of patient care. By pinpointing these areas, you can implement targeted improvements that directly benefit patient outcomes.
- Optimizing Staff and Resource Management : Utilize data analytics to make evidence-based decisions regarding staffing and resource distribution. This approach ensures that your workforce is optimally aligned with patient needs, and your resource allocation is efficient, contributing to a more effective healthcare system.
- Exploring New Avenues for Growth : Seize opportunities to expand your services and reach by integrating telehealth, offering home healthcare solutions, or developing specialized programs tailored to unique patient demographics. Such strategic initiatives can open new revenue streams and meet the evolving needs of your community.
- Improving Financial Health : Identify strategies for cost reduction and revenue enhancement, such as streamlining supply chain operations or venturing into untapped markets. These measures can bolster your organization's financial stability, allowing for reinvestment in key areas.
- Fostering Partnerships for Comprehensive Care : Establish collaborations with community organizations, other healthcare providers and facilities, or specialists to broaden your service offerings and improve patient care. Partnerships can lead to a more integrated care model that addresses a wide range of patient needs.
📚 Recommended read: Strategy study: The Ramsay Health Care Growth Study
Healthcare Strategic Planning: Why Is It Important?
Strategic planning in healthcare is more than just setting goals; it's about ensuring your organization is on the right track for success.
These are some of the countless benefits of strategic planning in healthcare:
Boost profitability
Strategic planning helps healthcare leaders improve their organization’s financial performance and achieve long-term sustainability. It's about using resources wisely, cutting costs where possible, and smoothing out inefficiencies by streamlining processes and creating better strategic initiatives to increase patient volume and improve experience.
Additionally, strategic planning plays a crucial role in uncovering new opportunities for revenue, enabling healthcare organizations to diversify their sources of income.
Enhance collaboration and engagement
Strategic planning in healthcare goes beyond identifying operational challenges; it's about bringing to light the issues that affect our teams daily, such as the strain of long work hours. When staff feel overburdened, their motivation dips, leading to decreased engagement and higher turnover rates.
By articulating a clear vision for the organization and actively involving employees in the strategic planning process, we can significantly boost morale. It's about making sure everyone feels seen and heard, understanding that their contributions are valued. This inclusive approach not only enhances team engagement but also encourages stronger retention.
Strategic planning also fosters collaboration across different teams and business units within the healthcare organization. By working together towards common goals, departments can better align their efforts, share insights, and support each other in achieving the organization's objectives. This synergy not only improves efficiency but also builds a more cohesive and motivated workforce.
💡Pro Tip : Ensure your vision statement is crystal clear organization-wide for unified strategic alignment.
Increase efficiency
Strategic planning helps you align your operational activities with the organization’s goals. This ensures that every action contributes toward achieving your business objectives. Strategic planning also empowers healthcare leaders, providing them with the insights needed to make resource allocation decisions wisely in the dynamic healthcare landscape.
Improve communication
A good strategic plan should be shared with all stakeholders so they can form a clear picture of how their actions affect a future outcome. This transparency promotes better communication within the organization, as employees align their efforts towards achieving a common goal. The end result is a more collaborative environment where the collective focus is on attaining shared objectives.
Drive alignment and strategy execution
Involving key stakeholders in the strategic planning process is crucial for aligning your healthcare organization's goals with its overarching strategy. This ensures that everyone, from top management to frontline staff, is aligned and moving in the same direction. Achieving this level of strategic harmony across the organization reduces confusion and clarifies the collective mission, paving the way for successful strategy implementation. This collaborative approach not only fosters a unified effort towards common objectives but also enhances the overall effectiveness of the organization's strategic initiatives.
💡Pro Tip : Ensure you balance a top-down and bottom-up for enhanced vertical and horizontal strategic alignment .
5 Strategic Planning Tools For Your Healthcare Strategy
Here’s a list of strategy tools and frameworks that can help you identify gaps in your healthcare strategy, prioritize strategic initiatives, and develop business goals:
1. Balanced Scorecard (BSC)
The Balanced Scorecard translates strategic goals into measurable indicators or metrics to help you balance four critical organizational perspectives: financial, customer, internal processes, and organizational capacity.
Using this tool ensures that your organization aligns with your strategic objectives and that you’re measuring the right KPIs to track progress toward those objectives.
2. Objectives and key results (OKR)
The OKR framework sets specific and measurable objectives and tracks progress toward them using key results. Objectives should be ambitious and challenging but achievable. Meanwhile, key results should be specific and measurable and have defined target values.
This framework promotes accountability and transparency since everyone works toward the same goals.
3. Political, economic, sociocultural, and technological (PEST) analysis
PEST analysis helps you understand the external factors that may impact your operations. By using this tool, you can identify potential opportunities and threats so you can anticipate and respond to changes in the external environment.
For example, PEST can help you identify a shift toward consumer-driven healthcare. Consequently, this enables you to invest in telemedicine and other digital healthcare technologies to meet patients’ changing needs.
4. Strengths, weaknesses, opportunities, threats (SWOT) analysis
SWOT analysis is a simple yet powerful way to identify the internal and external factors that can impact your organization’s success.
For example, if you discover that staffing levels are a weakness, you may decide to invest in staff training or recruitment programs. Or, if you identify an opportunity to expand into a new service area, you may choose to allocate resources for the expansion.
By leveraging your organization's strengths through this analysis, you can craft targeted strategies that address challenges and capitalize on opportunities for sustained success.
5. Theory of change (TOC)
The theory of change is a framework that helps your organization articulate the desired outcomes and specific steps you need to take to achieve them. This model provides a more structured approach to achieving goals by identifying the inputs required for success.
For example, if you want to reduce hospital readmissions, you may use the theory of change to identify the inputs needed (staff training on patient education), activities needed (discharge planning), and desired outcomes (reduction in hospital readmissions). By mapping out this logic model and continuously evaluating the initiative, your organization can adjust its activities to achieve your desired outcomes and improve the quality of care for your patients.
📚 Recommended read: 26 Best Strategy Tools For Your Organization in 2024
How To Implement A Strategic Plan In Healthcare
Implementing a strategic healthcare plan can be challenging. Follow this step-by-step framework to help you get started.
💡Pro Tip : Streamline your healthcare strategy planning, execution, and tracking with Cascade Strategy Execution Platform . It serves as a centralized hub for enhanced decision-making and accelerated results. Unsure of where to begin? Kickstart your strategic planning process with our complimentary pre-filled healthcare strategy template .
1. Establish goals
The first step is to establish clear and measurable goals. These goals should align with your organization’s mission and vision , and be SMART (specific, measurable, achievable, relevant, and time-bound).
Examples of goals in healthcare include reducing hospital readmission rates, improving patient satisfaction scores, or increasing revenue.
👉🏻How Cascade can help? With Cascade's Planner feature , you can simplify the process of constructing your strategies. It provides a structured approach, making it effortless to break down complex high-level initiatives into actionable outcomes.
2. Set milestones and measure progress
Once you establish goals, it’s important to set milestones and measure progress regularly. This allows your organization to track its progress toward achieving its goals, identify areas for improvement, and make necessary adjustments.
Make sure to establish a timeframe for your milestones, whether it's monthly, quarterly, or yearly, depending on the nature of your goal.
👉🏻How Cascade can help? Cascade's Metrics Library offers a centralized repository for your business metrics, allowing you to seamlessly link these metrics to your plan's Key Performance Indicators (KPIs). Integrating core metrics becomes a breeze, whether they originate from your business systems, data lakes, Business Intelligence (BI) tools, or spreadsheets.
3. Develop an execution plan
To successfully achieve your goals, it is essential to have a comprehensive execution plan . This plan should detail all the necessary activities and strategies that will guide you toward success.
An effective execution plan must include a well-structured timeline, a checklist of required resources, and clearly defined responsibilities for each action or project.
👉🏻How Cascade can help? Cascade's Alignment Maps feature empowers you to monitor the interactions between activities by documenting and examining dependencies, blockers, and risks that might arise during your strategic journey. This ensures a smooth path to successful strategy execution.
4. Monitor performance and adapt as needed
Once the plan is in motion, you should monitor its performance regularly and make necessary adjustments when you notice deviations. You must be flexible and willing to change your execution plan as needed.
For example, if the original plan doesn't turn out to be effective, it's important to quickly reevaluate and come up with an alternative strategy.
👉🏻How Cascade can help? Cascade's Dashboards & Reports allow you to gain accurate, real-time insights into your strategic performance, enabling you to easily share this information with your stakeholders.
5. Communicate regularly
Communication is key in implementing a strategic plan . Each stakeholder should understand their role and how their work fits into the big picture. You must inform them of progress toward the established goals, any changes to the execution plan, and other relevant information. This will help you build trust and get buy-in, which are essential for successful strategy execution.
6. Celebrate successes
Celebrating successes helps maintain motivation and momentum. It shows staff and stakeholders that their hard work is paying off. This can be done in various ways, such as recognizing staff members who have contributed significantly to the plan or sharing positive feedback from patients.
Positive reinforcement will motivate employees to keep striving to achieve your organization’s objectives.
📚 Recommended read: How Parker University uses Cascade to help them hold a position as a leader in Patient-Centric Healthcare
Case Study: Perley Health’s Strategic Ambition
Perley Health, a healthcare organization dedicated to improving care for veterans and seniors, faced some significant challenges in their strategic planning and execution processes. These challenges included making assumptions about the stability of the external environment in their long-term planning, inconsistency in how different departments planned and reported, a lack of clarity in how they measured success, and a somewhat fragmented approach to strategic and departmental plans.
Perley Health's journey toward strategic improvement began with the adoption of Cascade, a pivotal decision for them. Initially, they used Cascade to bring together all their strategic plans and initiatives, which brought about greater transparency and alignment with their organizational priorities. This not only made resource allocation more efficient but also provided a standardized way to measure results, making it easier to discuss return on investment (ROI) and track progress systematically.
Empowered by Cascade's capabilities, the management and various teams could now propose forward-thinking initiatives with a clear view of how they aligned with strategic priorities. This sped up decision-making and made funding allocation more precise.
With the right tools in place, Perley Health is now confidently working towards their goal of doubling senior care and establishing themselves as a center of excellence in frailty-informed care. They keep a close eye on their progress using the Cascade platform.
This case underscores the critical importance of strategic planning in navigating the complexities of healthcare, demonstrating a clear path to achieving and surpassing organizational objectives.
📚 Read the complete Perley Health Case Study!
Execute Your Healthcare Strategy With Cascade 🚀
Take the guesswork out of strategic planning in healthcare. With Cascade , you can easily create an execution plan customized to your goals and objectives, including assigning initiatives and setting deadlines for each team member involved.
Take a look at this example of a healthcare strategic plan in Cascade:

You can also leverage easy-to-use dashboards and visualizations that provide real-time data on your progress toward your goals.
Here’s an example of a real-time dashboard:

Cascade lets you collaborate with your team, assign responsibilities, and communicate progress, ensuring everyone is aligned and working toward the same objectives.
Whether you run a small clinic or a large healthcare organization, Cascade will help you make strategic planning in healthcare a breeze. Learn more about Cascade for healthcare !
Looking for a tailored tour of our platform? Book a demo with one of our Strategy Execution experts.
Popular articles

Strategic Initiatives Guide: Types, Development & Execution
.png)
20 Free Strategic Plan Templates (Excel & Cascade) 2024
.png)
How To Write KPIs In 4 Steps + Free KPI Template
.png)
35 Noteworthy Vision Statement Examples (+ Free Template)
Your toolkit for strategy success.

4 Keys to Successful Healthcare Management
By Arial Starks
The business of healthcare continues to grow at an impressive rate , and more healthcare professionals are seeking healthcare management roles that accompany this growth. Healthcare workers aspiring to move into management should take note of a few fundamental keys to success. We sat down with Burch Wood , Director of Healthcare Programs, and Anna Kennedy , Program Coordinator, Health Care, at Vanderbilt Business to learn the keys to successful healthcare management.
1. Gain Business Knowledge

One of the most common reasons healthcare professionals consider returning to school in the middle of their careers is to gain knowledge in areas where they are lacking. This knowledge gap tends to be centered around business concepts that are essential to healthcare management. Wood says in order for a healthcare professional to make the transition to administrative roles, they need to explore pursuing a program like the Master of Management in Health Care (MMHC) where they will gain that core business training.
“That’s why we have the MMHC, to give those who are tasked with the job of running a healthcare organization the business knowledge that will make them effective leaders,” he said.
2. Learn to lead a team/organization

Anna Kennedy
Healthcare professionals can be excellent at what they do, but if they are not able to lead a team or organization, Wood says it could prevent them from reaching their maximum career potential. “In the healthcare field, you have to learn how to manage a very diverse group of people,” he says. “You have to know how to get the most out of them and how to keep them motivated day after day.”
Healthcare management programs like the MMHC teach professionals to work as part of a team and can equip them with the tools they need to effectively lead a group of people. “The MMHC bringing different types of people together, communicating and learning to speak the same (business) language, (that) is part of what you get as the business fundamentals of the program,” says Kennedy.
3. Think and act strategically
One of the essential skills you learn in the Vanderbilt MMHC program is how to approach work with a strategic mindset. Through courses like management and strategy , professionals learn the importance of effective decision-making, which makes them better overall leaders in turn.
“At the end of the day, in order to be a good administrator, you have to understand and be able to answer questions like ‘what’s your 5 and 10 year plan?’ or even ‘how do the people you manage fit into that plan?” says Wood. “I believe part of why Vanderbilt organizes the MMHC program like we do is to give these healthcare professionals a taste of that early on.”
4. Be a life-long learner
A major key to success in any industry, but especially in the ever-changing world of healthcare management, is a commitment to life-long learning. As technology and concepts in healthcare continue to evolve, Kennedy says the ability to learn and adapt sets a person apart from the rest. “That’s what we look for in a candidate for the MMHC program, and it is almost always going to translate to their professional life as well,” she says. “It’s not what you learned 10 years ago, but how you can continue learning over the next 10 years.”
Wood notes that in order to make positive change in your organization, you have to be willing to learn and change as the industry progresses. “You have to have someone who is not only willing to accept change but also be a part of that change,” he says. “The people who are the most successful are the ones who see change coming down the pike and instead of running from it, they harness it and try to make something good out of it.”
Optimal success will look different to everyone in healthcare management, but as Wood says, as long as you are able to make positive change for your organization and in the lives of the people who depend on you as part of that organization, you can consider yourself successful.
To learn more about healthcare management at Vanderbilt Business, click here .
Featured News MMHC News News Press Releases
Other Stories
Want to learn more about MMHC?
The future of healthcare: Value creation through next-generation business models
The healthcare industry in the United States has experienced steady growth over the past decade while simultaneously promoting quality, efficiency, and access to care. Between 2012 and 2019, profit pools (earnings before interest, taxes, depreciation, and amortization, or EBITDA) grew at a compound average growth rate of roughly 5 percent. This growth was aided in part by incremental healthcare spending that resulted from the 2010 Affordable Care Act. In 2020, subsidies for qualified individual purchasers on the marketplaces and expansion of Medicaid coverage resulted in roughly $130 billion 1 Federal Subsidies for Health Insurance Coverage for People Under Age 65: CBO and JCT’s March 2020 Projections, Congressional Budget Office, Washington, DC, September 29, 2020, cbo.gov. 2 Includes adults made eligible for Medicaid by the ACA and marketplace-related coverage and the Basic Health Program. of incremental healthcare spending by the federal government.
The next three years are expected to be less positive for the economics of the healthcare industry, as profit pools are more likely to be flat. COVID-19 has led to the potential for economic headwinds and a rebalancing of system funds. Current unemployment rates (6.9 percent as of October 2020) 3 The employment situation—October 2020 , US Department of Labor, November 6, 2020, bls.gov. indicate some individuals may move from employer-sponsored insurance to other options. It is expected that roughly between $70 billion and $100 billion in funding may leave the healthcare system by 2022, compared with the expected trajectory pre-COVID-19. The outflow is driven by coverage shifts out of employer-sponsored insurance, product buy-downs, and Medicaid rate pressures from states, partially offset by increased federal spending in the form of subsidies and cost sharing in the Individual market and in Medicaid funding.
Underlying this broader outlook are chances to innovate (Exhibit 1). 4 Smit S, Hirt M, Buehler K, Lund S, Greenberg E, and Govindarajan A, “ Safeguarding our lives and our livelihoods: The imperative of our time ,” March 23, 2020, McKinsey.com. Innovation may drive outpaced growth in three categories: segments that are anticipated to rebound from poor performance over recent years, segments that benefit from shifting care patterns that result directly from COVID-19, and segments where growth was expected pre-COVID-19 and remain largely unaffected by the pandemic. For the payer vertical, we estimate profit pools in Medicaid will likely increase by more than 10 percent per annum from 2019 to 2022 as a result of increased enrollment and normalized margins following historical lows. In the provider vertical, the rapid acceleration in the use of telehealth and other virtual care options spurred by COVID-19 could continue. 5 Bestsennyy O, Gilbert G, Harris A, and Rost J, “ Telehealth: A quarter-trillion-dollar post-COVID-19 reality? ” May 29, 2020, McKinsey.com. Growth is expected across a range of sub-segments in the services and technology vertical, as specialized players are able to provide services at scale (for example, software and platforms and data and analytics). Specialty pharmacy is another area where strong growth in profit pools is likely, with between 5 and 10 percent compound annual growth rate (CAGR) expected in infusion services and hospital-owned specialty pharmacy sub-segments.
Strategies that align to attractive and growing profit pools, while important, may be insufficient to achieve the growth that incumbents have come to expect. For example, in 2019, 34 percent of all revenue in the healthcare system was linked to a profit pool that grew at greater than 5 percent per year (from 2017 to 2019). In contrast, we estimate that only 13 percent of revenue in 2022 will be linked to profit pools growing at that rate between 2019 and 2022. This estimate reflects that profit pools are growing more slowly due to factors that include lower membership growth, margin pressure, and lower revenue growth. This relative scarcity in opportunity could lead to increased competition in attractive sub-segments with the potential for profits to be spread thinly across organizations. Developing new and innovative business models will become important to achieve the level of EBITDA growth observed in recent years and deliver better care for individuals. The good news is that there is significant opportunity, and need, for innovation in healthcare.
New and innovative business models across verticals can generate greater value and deliver better care for individuals
Glimpse into profit pool analyses and select sub-segments.
Within the context of these overarching observations, the projections for specific sub-segments are nuanced and tightly connected to the specific dynamics each sub-segment is currently facing:
- Payer—Small Group: Small group has historically seen membership declines and we expect this trend to continue and/or accelerate in the event of an economic downturn. Membership declines will increase competition and put pressure on incumbent market leaders to both maintain share and margin as membership declines, but fixed costs remain.
- Payer—Medicare Advantage: Historic profit pool growth in the Medicare Advantage space has been driven by enrollment gains that result from demographic trends and a long-term trend of seniors moving from traditional Medicare fee-for-service programs to Medicare Advantage plans that have increasingly offered attractive ancillary benefits (for example, dental benefits, gym memberships). Going forward, we expect Medicare members to be relatively insulated from the effects of an economic downturn that will impact employers and individuals in other payer segments.
- Provider—General acute care hospitals: Cancelation of elective procedures due to COVID-19 is expected to lead to volume and revenue reductions in 2019 and 2020. Though volume is expected to recover partially by 2022, growth will likely be slowed due to the accelerated shift from hospitals to virtual care and other non-acute settings. Payer mix shifts from employer-sponsored to Medicaid and uninsured populations in 2020 and 2021 are also likely to exert downward pressure on hospital revenue and EBITDA, possibly driving cost-optimization measures through 2022.
- Provider—Independent labs: COVID-19 testing is expected to drive higher than average utilization growth in independent labs through 2020 and 2021, with more typical utilization returning by 2022. However, labs may experience pressure on revenue and EBITDA growth as the payer mix shifts to lower-margin segments, offsetting some of the gains attributed to utilization.
- Provider—Virtual office visits: Telehealth has helped expand access to care at a time when the pandemic has restricted patients’ ability to see providers in person. Consumer adoption and stickiness, along with providers’ push to scale-up telehealth offerings, are expected to lead to more than 100 percent growth per annum in the segment from 2019 to 2022, going beyond traditional “tele-urgent” to more comprehensive virtual care.
- HST—Medical financing: The medical financing segment may be negatively impacted in 2020 due to COVID-19, as many elective services for which financing is used have been deferred. However, a quick bounce-back is expected as more patients lacking healthcare coverage may need financing in 2021, and as providers may use medical financing as a lever to improve cash reserves.
- HST—Wearables: Looking ahead, the wearables segment is expected to see a slight dip in 2020 due to COVID-19, but is expected to rebound in 2021 and 2022 given consumer interest in personal wellness and for tracking health indicators.
- Pharma services—Pharmacy benefit management: The growth is expected to return to baseline expectations by 2022 after an initial decline in 2020 and 2021 due to the COVID-19-driven decrease in prescription volume.
New and innovative business models are beginning to show promise in delivering better care and generating higher returns. The existence of these models and their initial successes are reflective of what we have observed in the market in recent years: leading organizations in the healthcare industry are not content to simply play in attractive segments and markets, but instead are proactively and fundamentally reshaping how the industry operates and how care is delivered. While the recipe across verticals varies, common among these new business models are greater alignment of incentives typically involving risk bearing, better integration of care, and use of data and advanced analytics.
Payers—Next-generation managed care models
For payers, the new and innovative business models that are generating superior returns are those that incorporate care delivery and advanced analytics to better serve individuals with increasingly complex healthcare needs (Exhibit 2). As chronic disease and other long-term conditions require more continuous management supported by providers (for example, behavioral health conditions), these next-generation managed care models have garnered notice. Nine of the top ten payers have made acquisitions in the care delivery space. Such models intend to reorient the traditional payer model away from an operational focus on financing healthcare and pricing risk, and toward more integrated managed care models that better align incentives and provide higher-quality, better experience, lower-cost, and more accessible care. Payers that deployed next-generation managed care models generate 0.5 percentage points of EBITDA margin above average expectations after normalizing for payer scale, geographical footprint, and segment mix, according to our research.
The evidence for the effectiveness of these next-generation care models goes beyond the financial analysis of returns. We observe that these models are being deployed in those geographies that have the greatest opportunity to positively impact individuals. Those markets with 1) a critical mass of disease burden, 2) presence of compressible costs (the opportunity for care to be redirected to lower-cost settings), and 3) a market structure conducive to shifting to higher-value sites of care, offer substantial ways to improve outcomes and reduce costs. (Exhibit 3).
Currently, a handful of payers—often large national players with access to capital and geographic breadth that enables acquisition of at-scale providers and technologies—have begun to pursue such models. Smaller payers may find it more difficult to make outright acquisitions, given capital constraints and geographic limitations. M&A activity across the care delivery landscape is leaving smaller and more localized assets available for integration and partnership. Payers may need to increasingly turn toward strategic partnerships and alliances to create value and integrate a range of offerings that address all drivers of health.
Providers—reimagining care delivery beyond the hospital
For health systems, through an investment lens, the ownership and integration of alternative sites of care beyond the hospital has demonstrated superior financial returns. Between 2013 and 2018, the number of transactions executed by health systems for outpatient assets increased by 31 percent, for physician practices by 23 percent, and for post-acute care assets by 13 percent. At the same time, the number of hospital-focused deals declined by 6 percent. In addition, private equity investors and payers are becoming more active dealmakers in these non-acute settings. 6 CapitalIQ, Dealogic, and Irving Levin Associates. 7 In 2018, around 40 percent of all post-acute and outpatient deals were completed by an acquirer other than a traditional provider.
As investment is focused on alternative sites of care, we observe that health systems pursuing diversified business models that encompass a greater range of care delivery assets (for example, physician practices, ambulatory surgery centers, and urgent care centers) are generating returns above expectations (Exhibit 4). By offering diverse settings to receive care, many of these systems have been able to lower costs, enhance coordination, and improve patient experience while maintaining or enhancing the quality of the services provided. Consistent with prior research, 8 Singhal S, Latko B, and Pardo Martin C, “ The future of healthcare: Finding the opportunities that lie beneath the uncertainty ,” January 31, 2018, McKinsey.com. systems with high market share tend to outperform peers with lower market share, potentially because systems with greater share have greater ability not only to ensure referral integrity but also to leverage economies of scale that drive efficiency.
The extent of this outperformance, however, varies by market type. For players with top quartile share, the difference in outperformance between acute-focused players and diverse players is less meaningful. Contrastingly, for bottom quartile players, the increase in value provided by presence beyond the acute setting is more significant. While there may be disadvantages for smaller and sub-scale providers, opportunities exist for these players—as well as new entrants and attackers—to succeed by integrating offerings across the care continuum.
These new models and entrants and their non-acute, technology-enabled, and multichannel offerings can offer a different vision of care delivery. Consumer adoption of telehealth has skyrocketed, from 11 percent of US consumers using telehealth in 2019 to 46 percent now using telehealth to replace canceled healthcare visits. Pre-COVID-19, the total annual revenues of US telehealth players were an estimated $3 billion; with the acceleration of consumer and provider adoption and the extension of telehealth beyond virtual urgent care, up to $250 billion of current US healthcare spend could be virtualized. 9 Bestsennyy O, Gilbert G, Harris A, and Rost J, “ Telehealth: A quarter-trillion-dollar post-COVID-19 reality? ” May 29, 2020, McKinsey.com. These early indications suggest that the market may be shifting toward a model of innovative tech-enabled care, one that unlocks value by integrating digital and non-acute settings into a comprehensive, coordinated, and lower-cost offering. While functional care coordination is currently still at the early stages, the potential of technology and other alternative settings raises the question of the role of existing acute-focused providers in a more integrated and digital world.
Would you like to learn more about our Healthcare Systems & Services Practice ?
Healthcare services and technology—innovation and integration across the value chain.
Growth in the healthcare services and technology vertical has been material, as players are bringing technology-enabled services to help improve patient care and boost efficiency. Healthcare services and technology companies are serving nearly all segments of the healthcare ecosystem. These efforts include working with payers and providers to better enable the link between actions and outcomes, to engage with consumers, and to provide real-time and convenient access to health information. Since 2014, a large number and value of deals have been completed: more than 580 deals, or $83 billion in aggregate value. 10 Includes deals over $10 million in value. 11 Analysis from PitchBook Data, Inc. and McKinsey Healthcare Services and Technology domain profit pools model. Venture capital and private equity have fueled much of the innovation in the space: more than 80 percent 12 Includes deals over $10 million in value. of deal volume has come from these institutional investors, while more traditional strategic players have focused on scaling such innovations and integrating them into their core.
Driven by this investment, multiple new models, players, and approaches are emerging across various sub-segments of the technology and services space, driving both innovation (measured by the number of venture capital deals as a percent of total deals) and integration (measured by strategic dollars invested as a percent of total dollars) with traditional payers and providers (Exhibit 5). In some sub-segments, such as data and analytics, utilization management, provider enablement, network management, and clinical information systems, there has been a high rate of both innovation and integration. For instance, in the data and analytics sub-segment, areas such as behavioral health and social determinants of health have driven innovation, while payer and provider investment in at-scale data and analytics platforms has driven deeper integration with existing core platforms. Other sub-segments, such as patient engagement and population health management, have exhibited high innovation but lower integration.
Traditional players have an opportunity to integrate innovative new technologies and offerings to transform and modernize their existing business models. Simultaneously, new (and often non-traditional) players are well positioned to continue to drive innovation across multiple sub-segments and through combinations of capabilities (roll-ups).
Pharmacy value chain—emerging shifts in delivery and management of care
The profit pools within the pharmacy services vertical are shifting from traditional dispensing to specialty pharmacy. Profits earned by retail dispensers (excluding specialty pharmacy) are expected to decline by 0.5 percent per year through 2022, in the face of intensifying competition and the maturing generic market. New modalities of care, new care settings, and new distribution systems are emerging, though many innovations remain in early stages of development.
Specialty pharmacy continues to be an area of outpaced growth. By 2023, specialty pharmacy is expected to account for 44 percent of pharmacy industry prescription revenues, up from 24 percent in 2013. 13 Fein AJ, The 2019 economic report on U.S. pharmacies and pharmacy benefit managers , Drug Channels Institute, 2019, drugchannelsinstitute.com. In response, both incumbents and non-traditional players are seeking opportunities to both capture a rapidly growing portion of the pharmacy value chain and deliver better experience to patients. Health systems, for instance, are increasingly entering the specialty space. Between 2015 and 2018 the share of provider-owned pharmacy locations with specialty pharmacy accreditation more than doubled, from 11 percent in 2015 to 27 percent in 2018, creating an opportunity to directly provide more integrated, holistic care to patients.

Challenges emerge for the US healthcare system as COVID-19 cases rise
A new wave of modalities of care and pharmaceutical innovation are being driven by cell and gene therapies. Global sales are forecasted to grow at more than 40 percent per annum from 2019 to 2024. 14 Evaluate Pharma, February 2020. These new therapies can be potentially curative and often serve patients with high unmet needs, but also pose challenges: 15 Capra E, Smith J, and Yang G, “ Gene therapy coming of age: Opportunities and challenges to getting ahead ,” October 2, 2019, McKinsey.com. upfront costs are high (often in the range of $500,000 to $2,000,000 per treatment), benefits are realized over time, and treatment is complex, with unique infrastructure and supply chain requirements. In response, both traditional healthcare players (payers, manufacturers) and policy makers (for example, the Centers for Medicare & Medicaid Services) 16 Centers for Medicare & Medicaid Services, “Medicaid program; establishing minimum standards in Medicaid state drug utilization review (DUR) and supporting value-based purchasing (VBP) for drugs covered in Medicaid, revising Medicaid drug rebate and third party liability (TPL) requirements,” Federal Register , June 19, 2020, Volume 85, Number 119, p. 37286, govinfo.gov. are considering innovative models that include value-based arrangements (outcomes-based pricing, annuity pricing, subscription pricing) to support flexibility around these new modalities.
Innovations also are accelerating in pharmaceutical distribution and delivery. Non-traditional players have entered the direct-to-consumer pharmacy space to improve efficiency and reimagine customer experience, including non-healthcare players such as Amazon (through its acquisition of PillPack in 2018) and, increasingly, traditional healthcare players as well, such as UnitedHealth Group (through its acquisition of DivvyDose in September 2020). COVID-19 has further accelerated innovation in patient experience and new models of drug delivery, with growth in tele-prescribing, 17 McKinsey COVID-19 Consumer Survey conducted June 8, 2020 and July 14, 2020. a continued shift toward delivery of pharmaceutical care at home, and the emergence of digital tools to help manage pharmaceutical care. Select providers have also begun to expand in-home offerings (for example, to include oncology treatments), shifting the care delivery paradigm toward home-first models.
A range of new models to better integrate pharmaceutical and medical care and management are emerging. Payers, particularly those with in-house pharmacy benefit managers, are using access to data on both the medical and pharmacy benefit to develop distinctive insights and better coordinate across pharmacy and medical care. Technology providers, together with a range of both traditional and non-traditional healthcare players, are working to integrate medical and pharmaceutical care in more convenient settings, such as the home, through access to real-time adherence monitoring and interventions. These players have an opportunity to access a broad range of comprehensive data, and advanced analytics can be leveraged to more effectively personalize and target care. Such an approach may necessitate cross-segment partnerships, acquisitions, and/or alliances to effectively integrate the many components required to deliver integrated, personalized, and higher-value care.
Creating and capturing new value
These materials are being provided on an accelerated basis in response to the COVID-19 crisis. These materials reflect general insight based on currently available information, which has not been independently verified and is inherently uncertain. Future results may differ materially from any statements of expectation, forecasts or projections. These materials are not a guarantee of results and cannot be relied upon. These materials do not constitute legal, medical, policy, or other regulated advice and do not contain all the information needed to determine a future course of action. Given the uncertainty surrounding COVID-19, these materials are provided “as is” solely for information purposes without any representation or warranty, and all liability is expressly disclaimed. References to specific products or organizations are solely for illustration and do not constitute any endorsement or recommendation. The recipient remains solely responsible for all decisions, use of these materials, and compliance with applicable laws, rules, regulations, and standards. Consider seeking advice of legal and other relevant certified/licensed experts prior to taking any specific steps.
Before the COVID-19 pandemic, our research indicated that profits for healthcare organizations were expected to be harder to earn than they have been in the recent past, which has been made even more difficult by COVID-19. New entrants and incumbents who can reimagine their business models have a chance to find ways to innovate to improve healthcare and therefore earn superior returns. The opportunity for incumbents who can reimagine their business models and new entrants is substantial.
Institutions will be expected to do more than align with growth segments of healthcare. The ability to innovate at scale and with speed is expected to be a differentiator. Senior leaders can consider five important questions:
- How does my business model need to change to create value in the future healthcare world? What are my endowments that will allow me to succeed?
- How does my resource (for example, capital and talent) allocation approach need to change to ensure the future business model is resourced differentially compared with the legacy business?
- How do I need to rewire my organization to design it for speed? 18 De Smet A, Pacthod D, Relyea C, and Sternfels B, “ Ready, set, go: Reinventing the organization for speed in the post-COVID-19 era ,” June 26, 2020, McKinsey.com.
- How should I construct an innovation model that rapidly accesses the broader market for innovation and adapts it to my business model? What ecosystem of partners will I need? How does my acquisition, partnership, and alliances approach need to adapt to deliver this rapid innovation?
- How do I prepare my broader organization to adopt and scale new innovations? Are my operating processes and technology platforms able to move quickly in scaling innovations?
There is no question that the next few years in healthcare are expected to require innovation and fresh perspectives. Yet healthcare stakeholders have never hesitated to rise to the occasion in a quest to deliver innovative, quality care that benefits everyone. Rewiring organizations for speed and efficiency, adapting to an ecosystem model, and scaling innovations to deliver meaningful changes are only some of the ways that helping both healthcare players and patients is possible.
Emily Clark is an associate partner in the Stamford office. Shubham Singhal , a senior partner in McKinsey’s Detroit office, is the global leader of the Healthcare, Public Sector and Social Sector practices. Kyle Weber is a partner in the Chicago office.
The authors would like to thank Ismail Aijazuddin, Naman Bansal, Zachary Greenberg, Rob May, Neha Patel, and Alex Sozdatelev for their contributions to this article.
This article was edited by Elizabeth Newman, an executive editor in the Chicago office.
Explore a career with us
Related articles.

The great acceleration in healthcare: Six trends to heed

When will the COVID-19 pandemic end?

Healthcare innovation: Building on gains made through the crisis

Build plans, manage results, & achieve more
Learn about the AchieveIt Difference vs other similar tools
We're more than just a software, we're a true partner
- Strategic Planning
- Business Transformation
- Enterprise PMO
- Project + Program Management
- Operational Planning + Execution
- Integrated Plan Management
- Federal Government
- State + Local Government
- Banks + Credit Unions
- Manufacturing
Best practices on strategy, planning, & execution
Real-world examples of organizations that have trusted AchieveIt
Ready-to-use templates to take planning to the next level
Research-driven guides to help your strategy excel
Pre-recorded & upcoming webinars on everything strategy & planning
- *NEW!* Podcast 🎙️
The Complete Guide to Strategic Planning in Healthcare
RELATED TAGS:
supply chain
Healthcare institutions around the world must adapt their strategies to meet current trends and patient preferences. By using reliable and thoughtful planning, healthcare facilities can initiate patient-centric approaches and boost success.
Strategic healthcare planning consists of creating objectives, setting goals and then creating a plan for achievement. In other words, it’s the process of outlining goals and taking the necessary steps to achieve them. Most healthcare plans also consider government policies and technological advancements that could alter health goals and operations.
Read on to learn more about the importance of planning in healthcare.
In This Article
The Importance of Planning in Healthcare
- New Technologies
- Mass Adoption of Virtual Care
- Continued Management of Cybersecurity Risks
- Evolving Coding Requirements
- Population Health Management
The Benefits of Healthcare Strategic Planning
Questions to ask, partner with achieveit today.

Strategic planning is essential for a healthcare facility’s overall success. Planning allows organizations to adjust to the changing demands of the healthcare industry while supporting goal achievement.
You can also see the importance of strategic healthcare planning in other areas, including:
- Adapting to current trends: Having strong plans in place can help your facility adjust to current trends. By strategically thinking about the future of the field, you can avoid surprises later. For example, a significant change facing the healthcare industry is the rise of hybrid and remote work. Many facilities offer telehealth services or remote appointments for patients. With strategic management in healthcare, institutions can take note of these changes and adjust upcoming hiring policies and staff positions.
- Meeting patient needs: Strategic planning can also aid facilities in meeting patient needs. As technological advancements progress and the number of available providers grows, patients are seeking personalized and high-quality options. Facilities can examine patient demands and use these to craft their upcoming strategy in healthcare. In turn, they can create a patient-centric approach that improves the quality of care and sets them apart from competitors.
- Reduc ing supply chain disruption impacts: The COVID-19 pandemic disrupted the supply chain for all industries, including healthcare. Without the proper tools and equipment, healthcare professionals cannot provide care for all patients. Your strategic plan could help you analyze current supply chain trends and alter ordering decisions in response. For instance, if you notice a specific type of equipment is consistently out of stock, you could order extra quantities for your facility.
- Meeting rising hospital numbers: After the COVID-19 pandemic, the healthcare industry experienced a sudden increase in hospitalizations . Strategic planning allows facilities to allocate necessary resources to meet these trends. They can also become more prepared for other potential health crises.
- Helping with public funding: Strong performance helps healthcare facilities receive more funding from public sources. Most donors use various quality metrics to determine how much funding institutions should gain each year. A strategic plan can boost your facility’s performance on many levels, from care quality to maintaining supplies.
Overall, strategic planning in hospitals and other facilities is essential for institutional success and responding to current trends in the healthcare industry.
Top 5 Strategic Challenges in Healthcare
From the Affordable Care Act’s (ACA) influx of insured patients to the increased strain of COVID-19, healthcare facilities have been constantly adapting. Here are some examples of strategic planning in healthcare today.
1. New Technologies

In the medical field, new technologies seem to appear every day. From remote patient monitoring to robust patient portals, healthcare facilities must consider the evolution of the tools used during day-to-day care. These resources may impact workflows, budgets and the patient experience.
Many new technologies offer benefits like improved efficiency and positive experiences, but they can also create healthcare challenges in the form of new requirements for your IT team and staff training. Remaining flexible can help you accommodate these possibilities, stay ahead of the competition and improve care with modern capabilities.
2. Mass Adoption of Virtual Care

From a cost perspective, one shining light for healthcare systems is the rise of virtual care, commonly referred to as telemedicine. Using internet-enabled services, healthcare providers are able to consult with patients virtually and provide diagnoses, thereby saving time and resources associated with an in-person hospital consult.
As this technology continues to proliferate, and patients become more comfortable with interacting with their doctors over virtual systems, healthcare systems will be able to trim significant expenses across departments, helping to control costs. In creating their strategic plans, healthcare leaders should take a deep look at how they continue managing telemedicine technology to help aid in future cost savings.
3. Continued Management of Cybersecurity Risks
Data security has become a significant challenge across industries, but none more so than the healthcare industry. Due to the extensive nature of personal information inherent in healthcare records, insurance companies and healthcare systems should be cautious regarding the security of their patient records.
As regular security breaches always remind us, healthcare entities should pay special attention to the security of their systems to ensure the privacy of subscribers. Healthcare leadership will need to collaborate extensively with IT, in a strategic sense, to ensure the department has the resources and technology necessary to guarantee data security and HIPAA compliance.
4. Evolving Coding Requirements
The next version of the International Classification of Diseases (ICD) is currently under review in the U.S. If you’ve been in the industry for a while, you might remember the transition to ICD-10 back in 2015. Although we may not see ICD-11 for a while, healthcare strategy must consider this eventual implementation and other potential changes to reporting and documentation requirements. To ensure full reimbursement, organizations may need to upgrade existing systems and train employees accordingly.
5. Population Health Management
Healthcare systems across the country are being confronted with a new paradigm of healthcare delivery: Ensuring the overall health of demographic cohorts within their communities.
Shifts toward value-based care only increase the focus on population health, requiring healthcare leaders to design strategic plans and allocate resources to educate the populations they serve on preventative care. This will require the participation of stakeholders across departments and often will necessitate new programs to be established to help further population health interests.

Committing to a strategic plan can bring many benefits to healthcare facilities, including:
- Establishing a shared vision: A plan requires your facility to focus on specific goals. As you develop these objectives, you and your team can establish the overall purpose of your facility. Then, you can create concrete ways to meet this vision . You can also inform employees, shareholders and other crucial team members of this vision, inspiring members at every level. All members can unite around a shared purpose and find more value in their work, improving overall performance.
- Prioritizing critical issues: By focusing on a strategic plan, you can prioritize vital issues. Every healthcare facility has specific areas for improvement, whether it’s improving collaboration or meeting staffing requirements. Strategic management in healthcare allows you to identify these areas and brainstorm specific ways to address them. You can focus on resolving the most significant issues first, instead of getting overwhelmed with secondary problems.
- Improving team communication: Strategic planning also assists with communication across your facility. Your plan should address key issues and goals, then outline the steps you will take to achieve these. You can share these plans with all institutional members, giving everyone a clear idea of future actions. With everyone on the same page, your facility can collaborate more easily and stay on track with goals.
- Enhancing motivation: A clear vision and plan can motivate employees to work harder. They can feel empowered to make decisions that support institutional goals. As they work toward a shared purpose outlined in a healthcare strategy, they feel more motivated by their daily work and can improve their performance.
- Solidifying leadership: All healthcare facilities rely on strong leadership to lead employees and meet goals. Leaders can use strategic plans to clearly identify goals for employees. They can clarify expected behaviors and encourage employees to work toward their personal best. Passionate leaders and hard-working employees can establish your facility as a leading healthcare option.
Because the purpose of strategic planning in healthcare is to work towards improvement, asking questions can help you. Healthcare institutions should ask a few crucial questions during their planning. By thinking about particular circumstances, you can tailor plans for your needs. These questions can also help you identify goals and develop a shared purpose.
Here are a few examples of questions to ask during strategic planning:
- What is the current financial situation of your institution?
- What are your goals for finances moving forward?
- What areas need more help or growth?
- What are the needs of your facility’s typical population?
- How could these needs change over time?
- What current trends in the healthcare industry or government policies could impede these goals?
- Where would you like to see your organization in five years or ten years?
You can use questions like these to establish objectives and an overall vision. Once you have developed these, you can develop steps for achievement. Structures like SMART goals can help you create measurable and timely actions .

At AchieveIt, we understand the importance of well-defined healthcare goals and addressing the challenges of healthcare strategy. You can move directly toward your shared vision with a strategic plan and clear-cut goals.
Our strategic planning software helps healthcare institutions meet their goals. The technology helps you analyze data to identify specific goals and areas for improvement. Then, we can help you form quantifiable and actionable goals that move you toward your overall purpose.
AchieveIt software also features:
- Integrated reports
- Automated reminders for deadlines and goals
- Real-time data updates
- Speedy set-ups and communication processes
Our expert team of specialists can help your facility through each step of the planning process. We can enhance your plans and offer specific suggestions for improvement. Whether you want to improve physician care or reduce waiting room times, our software can help you meet these goals.
Let’s actually do this. Schedule a demo with AchieveIt today.
Meet the Author Chelsea Damon
Chelsea Damon is the Content Strategist at AchieveIt. When she's not publishing content about strategy execution, you'll likely find her outside or baking bread.
Related Posts

Balanced Strategy: Mastering the Art of Zooming In and Out

Everything You Need to Know About Business Mission and Vision Statements

Excel vs. AchieveIt for Strategic Planning
Hear directly from our awesome customers
See first-hand why the world's best leaders use AchieveIt
See AchieveIt in action
Stay in the know. Join our community of subscribers.
Subscribe for plan execution content sent directly to your inbox.

5 Tips For Strategic Planning Professionals in Healthcare

Enhance your strategic planning with our 5 tips for healthcare professionals. Elevate your planning and contribute to your organization's success now!
Table of Contents
In healthcare, things change quickly. Some hospitals and healthcare organizations believe that’s a reason to avoid strategic planning—because the change lurking just around the bend is sure to derail even the best-laid plans. But the truth is, a strategy can be your best resource in times of change, as long as it’s grounded in your mission and vision.
As a leading strategy management software provider, we’ve helped numerous healthcare organizations plan and execute their goals for the future. Keep reading to get our take on why strategic management in healthcare is critical for succeeding in a volatile world, and learn a few tips that can help you carry out strategic planning more effectively.
Looking for some examples of healthcare strategic plans? Download sample strategy maps created specifically for medical and healthcare organizations like yours.
Strategic management in healthcare: what is it.
Strategic management in healthcare is the process of defining the future of your organization, setting goals that will move you toward that future, and determining the major projects you’ll take on to meet those goals. It also includes sustaining that strategy focus over a period of three to five years.
Why is strategic management important in healthcare?
Like other companies, healthcare organizations benefit from having a plan for the future—one that all employees are aware of and consistently working toward. Strategy should serve as a guidepost for all important decisions to make sure your facility stays on track.
But as we mentioned above, healthcare is even more complex than your average business—and frequently affected by external forces. If asked to describe how strategic management helps your facility control the future, we’d answer with the following:
- The strategic planning process naturally includes assessing changes in the external environment (through exercises like the SWOT analysis) and thus helps your organization stay on top of them.
- It provides focus and direction for daily work even as circumstances (internal or external) may change.
- It provides leaders with a consistent flow of information about organizational performance, promoting better, more timely decision-making. The availability of such data also helps organizations reprioritize or pivot as needed.
5 Tips For Healthcare Strategic Planning Professionals
1. keep your organization’s mission top-of-mind..
Mission and vision are the cornerstones of your organization and provide a foundation for strategic planning. Make sure the priorities and objectives outlined in your plan support those key elements—and reconsider any goals that are not aligned.
2. Narrow your strategy’s focus.
Too many healthcare organizations try to be everything to everyone. As a result, their strategies touch nearly every base imaginable, from being the best at research and innovation to serving as many potential patients as possible to being customer-centric, etc. Narrowing down your strategy requires courage—it may feel as if you’re passing up opportunities to improve. But in reality, you run the risk of not excelling in anything if you’re trying to achieve everything . Home in on the areas you want to pursue and direct your resources and energy to accomplishing those specific goals.
3. Align your plan with in-progress accreditations or certifications.
If you’re pursuing an accreditation or award like PHAB or Baldrige, your strategic plan needs to align with that goal. Make sure your plan points you in the right direction and supports tracking all the data required by the administering body.
4. Do a SWOT analysis.
Periodically analyzing your organization’s strengths and weaknesses, as well as external opportunities and threats, is a useful exercise that can inform your strategic plan. Follow the steps outlined here to complete the analysis, and see some healthcare-specific examples.
5. Communicate.
Strategic plans are only effective if everyone knows about them. Every department head should be charged with explaining how their team fits into the strategy and why it matters. (Read some tips here on how to effectively communicate with employees.) You’ll also need to create tailored presentations for other stakeholders—patients, administrators, community members, etc.
And finally, remember: Don’t overload yourself and your team with goals and metrics right out of the gate—having too many makes it hard to prioritize and makes communication difficult. Ease into it. The first year, start by creating a high-level plan for the organization as a whole; the following year, try to tackle planning for business units, service lines, etc.
Support Your Efforts With ClearPoint Strategy Reporting Software
Understanding why strategic planning is important in healthcare is the first step; however, the strategic planning process is complex.
In fact, creating the strategy is just the tip of the iceberg. Once it’s been launched, you need to know if you’re making progress—and that requires reporting regularly on your results.
Reporting can sink even the best strategy efforts because, without the right tools, strategy management quickly becomes overwhelming. ClearPoint is the only strategy reporting software that helps healthcare organizations effectively manage all the fundamental activities that go into reporting:
- You need to gather data that will help you draw conclusions about your performance. Your data is likely scattered across locations, systems, and services. ClearPoint seamlessly integrates with your on-premise and SaaS software applications to make data collection easy.
- You need to pull together data in a way that helps you make sense of it. In ClearPoint, you can make sense of any data set. Use data aggregations and complex calculations to get your data in any format you need. Then, automatically evaluate your results so it’s easy to tell if you’re on track.
- You need to analyze data to understand the story it is telling. ClearPoint allows you to link projects with strategy objectives to understand how everything you’re doing fits together; it also facilitates the analysis of both quantitative and qualitative data. This allows your organization to spot problems early and make corrections to areas that need the most help.
- You need to create reports that your leadership teams can review and discuss for decision-making purposes. With ClearPoint, you can create beautifully branded reports (and dashboards like the one below) for any audience—your board, your management team, and your individual providers. ClearPoint lets you create reports in a variety of formats and even schedule reports to automatically generate and send.

When it comes down to it, the fundamental challenge of strategic management in healthcare is managing it all—coordinating resources and people to ensure everyone is continuously working toward a common goal, and staying on top of your successes and failures.
How can strategic planning improve the performance of an organization?
Strategic planning improves the performance of an organization by providing a clear direction and framework for decision-making. It aligns resources and efforts with long-term objectives, identifies potential risks and opportunities, and ensures that all departments are working towards common goals. This results in increased efficiency, better resource allocation, and improved overall performance.
Why is strategic planning important in healthcare?
Strategic planning in healthcare is important because it helps organizations navigate the complex and rapidly changing healthcare environment. It ensures that resources are used effectively to improve patient care, meet regulatory requirements, and achieve financial stability. Strategic planning also helps healthcare organizations set priorities, allocate resources, and measure progress towards their goals, ultimately leading to better patient outcomes and organizational sustainability.
Why do strategic plans fail?
Strategic plans fail for several reasons:
- Lack of Clear Objectives: Vague or unrealistic goals can lead to confusion and lack of focus. - Poor Communication: Failure to communicate the plan to all stakeholders can result in lack of alignment and commitment. - Inadequate Resources: Insufficient resources, including time, budget, and personnel, can hinder implementation. - Lack of Flexibility: Inability to adapt the plan to changing circumstances can make it obsolete. - Poor Execution: Failure to translate the plan into actionable steps and monitor progress can lead to poor outcomes.
How is strategic planning done?
Strategic planning is done through a systematic process that includes:
- Defining Vision and Mission: Establishing the organization's purpose and long-term aspirations. - Conducting Analysis: Performing SWOT or PESTEL analyses to understand internal and external factors . - Setting Goals: Defining specific, measurable objectives. - Developing Strategies: Creating broad approaches and initiatives to achieve the goals. - Allocating Resources: Ensuring necessary resources are available and properly allocated. - Implementing Plans: Executing the strategies and action plans. - Monitoring and Evaluating: Continuously tracking progress and making adjustments as needed.
Who does strategic planning?
Strategic planning is typically done by senior leadership and management teams within an organization. This often includes executives, department heads, and key stakeholders. In larger organizations, strategic planning may also involve input from board members, employees, and external consultants to ensure a comprehensive and inclusive approach.

Ted Jackson
Ted is a Founder and Managing Partner of ClearPoint Strategy and leads the sales and marketing teams.

Latest posts

ClearPoint Strategy versus the Status Quo
.webp)
ClearPoint Strategy vs. Envisio: A Comprehensive Comparison
%20(2).webp)
ClearPoint Strategy vs. AchieveIt: Selecting the Optimal Tool for Strategic Management
Strategic Planning In Healthcare: 2024 Guide + Examples

Sara Seirawan
This guide contains new healthcare planning strategies, their benefits, examples, traps to avoid, and all you need to know.
Whether you’re a medical business owner, an executive, or a practitioner, my promise to you is that, by the end of this article, you’ll get a razor-sharp understanding of what strategic planning is and how it can skyrocket your operational efficiency.
Here’s a brief outline of what I’ll cover:
What is strategic planning in healthcare?
- The importance of strategic planning in healthcare
- 3 Common Mistakes when implementing strategies
- The best 8 healthcare planning strategies
- ‘Secret’ to a fruitful healthcare planning campaigns
Strategic planning in healthcare is setting long-term objectives for your medical business and an action plan to hit your target goals. It’s about taking a proactive approach to building a future-proof medical brand.
There are many strategies (which we’re going to look at) to achieve a strategy-driven business model, but before we go deep into the details, let’s check how this can benefit your practice.
The benefit of strategic planning in healthcare
With a good strategic approach comes great advantages for your medical business.
1) It protect your medical business from unforeseen risks
With the Covid-19 situation, healthcare providers no longer can afford to function reactively. And this is where SP (strategic planning) comes into place. SP, by nature, is a proactive approach. It is focused on long-term goals and future-oriented planning.
This not only immune you against any unlooked-for risks but arms you with a well-crafted plan of what should be done in the face of uncertainty.
The Planning Strategy should work as the shatterproof window for your practice.
2) It speeds up your medical business growth
Having a strategy in place holds everyone involved accountable. This means an increased commitment from your team and faster work processes.
Furthermore, according to Parkinson’s Law, any team, when giving a task, will fill whatever time was allocated for its completion. This not only quickens your operational efficiency, but it also skyrockets your work productivity and patient outcomes.
This enhanced workflow will accelerate the rate at which your medical business grows. Resulting in a faster profit cycle.
The next graph illustrates how business growth rate correlates with operational efficiency.
3) It creates a cohesive workplace for your medical business
Medical businesses routinely separate functions to hierarchical levels to achieve efficiencies, However…
These divides lead to confusion, anxiety, and distrust as employees work at cross-purposes, taking refuge in functional silos instead of a collaborative ecosystem.
This makes your medical staff sub-optimizing when you need all parts working together.
Employees go about directionless, without an understanding of their role in delivering the (non-existent) consistent experience for patients.
To combat this, putting a strategic vision for your business ensures cohesiveness and a united workforce.
The bottom line is : the result of having a shared strategic vision is coherence; the result of aimless workflow is wasted resources.
4) It increases your profit margin
Great medical business owners aim for the stars and land on the moon. And this is what makes strategic financial planning great. It forces you to aim high. This kind of planning breaks the chains of the self-limiting beliefs that are preventing you and your staff from achieving a higher rate of profit margins.
Not only that, but it also makes sure that what you’re doing is directed by a strategy and measurable KPIs (key performance indicators) and not by a mere accumulation of tactics that don’t add up together.
This results in a well-tracked process, efficient way of working, and increased profitability.
3 Common mistakes when implementing healthcare strategic planning
Let’s explore common mistakes medical business fall into when implementing strategic planning workshops.
1) Disregarding their branding efforts
Any medical practice can have strategies, but great medical businesses let their brand act as a decisional filter for their planning effort.
Does your strategy align perfectly with your brand’s core attribute? Does this plan solidify your place in the market or does it weaken your brand’s perceived value? If you don’t have a grounded brand in place, your strategy might end up hurting your medical business.
If you’d like to learn more about brand building and how can you build a mouth-watering brand, you can check our free healthcare branding guide .
2) Focusing on too many metrics and KPIs
Getting distracted by too many metrics is the fast lane to a crumbling healthcare plan. Many practices try to implement a strategy but end up focusing on the wrong metrics and getting overwhelmed.
It is best to list out critical KPIs (key performance indicators) for your medical brand before embarking on a strategy.
3) Lack of professional facilitators
Any healthcare strategic plan needs a good facilitator. A facilitator that has a great knowledge of the healthcare industry know-how and its business side of things. Common trap healthcare organizations or practices fall into is trying to implement these strategies in-house. This leads to unproductive workshops and unfruitful results.
We strongly advise you to outsource these strategies to great facilitators that have past-experience running healthcare strategic planning workshops. This will save you time and provide you with the best result for your medical business.
Best Healthcare Planning Strategies (With Examples)
Let’s go through some of the essentials of strategic planning methods in healthcare.
1) S.W.O.T Analysis Strategy
S.W.O.T is a strategic planning technique used to define your healthcare organization’s (or practice’s) Strengths , Weaknesses , Opportunities , and Threats in the competitive landscape.
SWOT Analysis arms you with a clear overview of critical metrics that are key for your performance and the overall success of your medical business.
Let’s see some examples of SWOT Diagrams in healthcare.
Hospital strategic plan: SWOT example
Strategic planning in nursing: swot example, 2) s.w.o.t strategy canvas™.
SWOT Analysis is not enough to measure the success of your efforts.
That’s why our team at unnus developed the SWOT Strategy Canvas™ (SSC), a visual representation graph of the impact SWOT has on your medical brand.
The SSC could be conducted every 6 months to track the efficiency and the effort of SWOT.
SSC graph tracks the Impact Rate of each element of the SWOT (strengths, weaknesses, opportunities, and threats). The goal is to witness a low Impact Rate of weakness and threats and a high Impact Rate of Strengths and Opportunities.
If you’d like to know more about the how-tos and other details of SWOT analysis and SSC, check our step-by-step guide on SWOT here .
3) Brand Vision Strategy
Brand Vision Strategy is a planning method used to define concrete objectives for your medical brand and set up trackable metrics for the overarching vision.
The Brand Vision Strategy has three stages:
- 15 Year Vision Timeline
- Brand Obituary
- Vision Strategy Matrix
Let’s see how the three stages overlap.
#First~ The 15 Year Vision Plan
The 15 Year vision Plan is where we start defining the higher goals and aspirations that your medical business needs to achieve.
The benefit of this stage are threefold:
- It ensures that you know where your medical business is headed
- It works as a pathway to check back against when measuring your progress
- Forces you and your team to aim high and set a bold goals
#Second~ Brand Obituary
What will happen if your practice closes its door tomorrow? Would journalists write headlines heralding your past achievements, or would their stories simply add you to a list of bygones? Would employees wonder how it could have ended, or would they have known it was inevitable? Would patients mourn your passing, or would the demise of your medical brand go unnoticed?
Unlike the 15 Year Vision Plan, this method works as a risk assessment and proactive approach for future commitment.
This exercise will force you to think through some of the key elements that make up your brand.
Here’s an example of this technique from our client, a dental practice Confidental™.
#Third~ Brand Vision Matrix
In this stage, we get strategic by defining a set of metrics to track and check back against your overarching vision. This stage focuses on tracking and measuring your progress towards the final goal of the strategy.
The metrics that we’re going to measure in this stage fall into four categories:
- Some of the most important measures of internal business performance are overall productivity rates, ability to meet deadlines on time, and ability to achieve previously set goals and this category will contain all necessary metrics for that.
- Tracking how your medical staff is growing will help facilitate the overall team goals. You’ll want to keep track of employee morale, how knowledgeable staff is, and how reliably they use the business’s best practices.
- It is critical to capture the efficiency of your stakeholders to gauge the overall performance of your medical business. This section is focused on staff, team, and shareholders.
- Most medical businesses find it useful to measure the business’s progress toward financial goals. Common measures of financial performance include revenues, return on investment, earnings, cost per case, etc.
Each category will contain the following:
- Set of objectives that are relevant to it
- Measurement and matrices
- Progress Record of each target
- Initiatives (what are we doing hit that target)
Here’s an example of a hospital’s Brand Vision Matrix:
4) Brand Cause And Effect Strategy
This strategy helps you pinpoint the root causes of complex problems that are hindering your business growth. The premise of this strategy is to take on a big problem and start dissecting it into categorical components or “sub issues”.
This way you can spot deeply-embedded issues that are causing the main problem. You can think of this strategy as more a way to treat the problem rather than finding it.
The benefits of this strategy are:
- Better visualization of your medical business risks
- Treating the causes rather than the symptoms of the problem
- Gets you out of the tunnel vision trap and provide you with a clear picture of the challenges your business might face
Here’s an example for this strategic planning technique for a hospital
5) Patient Journey Strategy
The patient journey strategy (PJS) is a visual representation strategy of your patient’s experience. It allows you to capture the path that a patient follows when they book an appointment, sign up for a care service membership, or otherwise interact with your medical business.
This strategy focuses on every single touchpoint (places where patients interact with your business) and hone in on what can be improved, fixed, or removed.
Patients are the lifeblood of your business and zero in on your patient’s pain points, challenges, and needs are critical for success.
Some of the benefits of using this strategy are:
- Anticipate multiple patient pathways
- Understand the patient’s perspective
- Inform your staff and employee about what should be improved
- Target patient more closely and increase personalization
- Improve patient experience
- Uncovering easy-to-overlook aspects of your business
Here’s a snapshot of a patient journey of medical practice and how the team identified potential issues and problems
Click here for to larger version .
6) Risk Assessment Matrix Framework
The Risk Assessment Matrix creates a framework where you can assess the urgency and the likelihood of any potential threat that might affect your business.
This strategy also allows you to better allocate your efforts across multiple aspects of your business based on the potential severity of any risk. In addition, it’s a great way to visualize and prioritize where and when should you take action against any business threats.
Risks in this framework should be ranked according to low probability and severity (one- colored green) to the highest possible likelihood (ten-colored red). Ranking them in this way lets your team tackle the biggest threats with a sharp action plan.
Here’s an example of this framework:
You can access the full version here .
7) OKR (Objectives & Key Results) Framework
OKRs stands for Objectives & Key Results. An OKR framework helps medical businesses solve their critical organizational problems. As a framework, OKRs also help healthcare leadership teams discuss how the work of the staff ties back to the overall business strategy.
OKRs should be transparent to everyone: top-down, bottom-up, and cross-functional. When everyone’s looking at the same framework, everyone has the opportunity to work toward the same outcomes.
Objectives are the vaccine to “blue sky thinking” – their goal is to help articulate what you want to accomplish. An objective is significant, concrete, and drives you to get tasks done.
Key results are the way you’re going to get those tasks done. Specific and measurable, these quantitative goals act as benchmarks for how you’ll reach objectives. (Think outcomes or results in real numbers.)
8) Brand Prioritization Framework
The Brand Prioritization Framework (BPF), or priority matrix, helps your medical teams prioritize initiatives or service lines based on their impact on your medical brand and the level of effort needed for success.
With nine “buckets” or areas of interest, your team can decide if an idea or plan is low, medium, or high effort. The team can also accordingly decide if that plan will likely have low, medium, or high impact.
As a visual framework, the Brand Prioritization Framework helps you promptly reach an agreement on quick wins, big projects, filler tasks, or anything that could waste time.
An example of the BPF for might be:
You can access a large resolution here .
The ‘secret’ to a fruitful healthcare strategic plan
A great healthcare strategy is always directed by the brand’s attributes. A strategic plan won’t take any business anywhere if it is not guided by your branding strategy.
A planning strategy could potentially hurt your healthcare brand equity (your perceived worth) if it veers off from your brand’s positioning . If you’d like to learn more about branding in healthcare and how it can overhaul your strategic plan, you can check our guide here .
If you’re busy and looking for great healthcare brand strategy facilitators, contact us here and we’d gladly help you.
- what is strategic planning in healthcare
- the benefit of strategic planning in healthcare
- 3 common mistakes when implementing healthcare strategic planning
- best healthcare planning strategies with examples
- the secret to a fruitful healthcare strategic plan

Sara Seirawan, Head of content, manages unnus's content distribution and marketing efforts. She's also a chief author at unnus Magazine.
- Free course

Become a Member
Strategic Planning for Healthcare Organizations
Judith N. Aburmishan, MBA, CPA, CHBC
Neil Baum, MD
July 1, 2022
Physician Leadership Journal
Volume 9, Issue 4, Pages 40-43
https://doi.org/ 10.55834 / plj.6555794318
A key element in business management is strategic planning, which can move a business/practice that is being buffeted by changing economic forces to one that shapes its own future. It is an organized, step-by-step review of the business, the economy, and the environment in which the business operates.
Physicians and healthcare executives can no longer treat the business of a medical organization as an afterthought. Increased regulation, dominance by government payers, remote and internet delivery systems, and electronic medical records have all entered the industry uninvited and often are met with resistance by current management.
One of the reasons healthcare managers resist change is that many of the individuals who manage medical practices and organizations come from a provider background and have been trained in the science of healthcare, not in the business of healthcare.
Strategic Planning
Choosing Strategies
One of the key elements of strategic planning is evaluating alternative strategies that have been identified as necessary next steps. A conceptually easy method of evaluating alternative strategies is to identify the project or result’s key drivers of success by having a roundtable discussion with all the stakeholders about a completed project or successful result and working backward to identify the elements that created the success.
Examples of the key drivers include:
Time to implement
Cost to implement
Impact on staff
Fiscal impact
Impact on patients
Impact on volume
The next step is to work with the implementation team to identify strategies to establish the project or produce the desired result. One strategy is for the team to develop a grid with the key elements across the top and each strategy along the left side. They then assign each strategy for each key driver a numeric score between 1 and 5, with 5 being the most positive and 1 the least positive. The strategy with the most points can be considered the most promising. For example, Table 1 illustrates that adding morning hours is the best strategy for this organization.

This is a simplified method; the rating scale can be modified to a scale of 1–10 or 1–100. In addition, the topics to consider can be changed based on the key issues that need to be addressed in the medical organization.
Although the process of getting to these strategies may seem like a considerable amount of work, time spent on this process often eliminates costly selection processes. More importantly, it puts the organization in the position of creating its own success. Medical organizations that make researched decisions regarding strategy are more successful than those that simply react to market forces.
Leaders, Teams, and Timelines
After each strategy is ranked and prioritized, the next step is to identify who will be accountable for the strategy’s implementation. In smaller groups, this often falls to one or two individuals, but having several people engaged and supporting the process will make each strategy easier to implement and will improve the chances of long-term success.
The person responsible for the strategy is also responsible for conducting the research and compiling all the relevant information necessary to create a detailed action plan. For example, if the organization plans to add morning hours, an example of a simple step-by-step process is:
Select a launch date.
Designate the earlier hours.
Determine staffing needs for additional hours.
Determine if additional hours can be staffed without increasing overhead.
Identify barriers to access by patients during nonpeak hours (building access and parking).
Develop a provider schedule.
Create a staff schedule and hire additional staff.
Publicize the new hours.
Design marketing materials that announce the new hours (ads, social media).
Develop a budget for marketing and staffing.
Submit a plan for approval by the leadership.
Finalize a launch or go-live date.
During the creation of the detailed implementation plan for any strategy, it’s important to get the feedback and buy-in of the other employees. A plan that doesn’t have employee support will be doomed to failure. Listen and acknowledge objections. It is better to recognize objections before launching the project than to try to solve problems after the launch.
The next step is to identify specific steps and assign a realistic completion date to each (see Table 2 for a simple format). It’s helpful to know how long each of the steps will take to complete so the timeline is reasonable and realistic. For example, placing ads and publicizing the new hours might require 60 minutes to call local media, or it might take weeks as internet posts are updated, websites are changed, and ad rates and other agreements are negotiated.
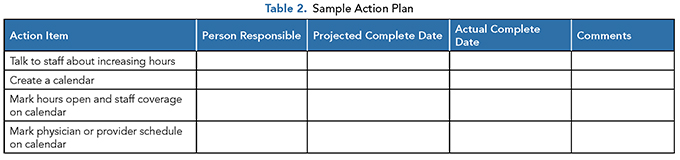
A process for ensuring accountability is also necessary. For a project to proceed in a timely fashion, each team member should have specific dates and times to complete assigned tasks. Often, actions necessary for completing new strategies will require team members to step outside of their comfort zone and accomplish tasks that are not in their job description ( e.g. , negotiating rates for a new ad) or are in addition to a full schedule. If the strategies are to be implemented in a timely fashion, everyone responsible for implementing the strategy must be accountable for completing their assignments on time.
Measurable Results
Just as in any clinical treatment, a strategic plan should measure the results. For example, in measuring the results of expanded hours for a medical organization, factors to be considered might include expenses, net income resulting from the new hours, and the number of new patients per week.
Once these results have been selected as measures of success, the accounting and recordkeeping system must be modified to track the relevant numbers. Most organizations do not measure revenue generated by hour or expenses incurred by hour, and they may not keep track of new patients per week. Therefore, the current bookkeeping systems should be reviewed and additional levels of recordkeeping designed so that the values used in the measurement are tracked properly from the beginning of the project. This is also critical for the start-up expenses that are incurred. Remember, what gets measured gets done!
Many accounting systems can code all income and expenses to a special “class” that can generate its own profit and loss. Depending on the significance of the strategy, accounting records measuring the results may be kept for a few months or a year, or they may become part of the regular monthly reports the accountants provide. The reports should not only cover the results for the current period (week, month, quarter), but also they should be comparable week over week or month over month, so that progress or trends can be identified.
Once the reports are designed and the systems are revised to track the relevant data, the team members accountable for the success of the project should begin receiving weekly reports on results. These reports will give the team regular and ongoing feedback regarding what is working and what is not.
The Final Step
The last step is to have a final meeting with the team members accountable for implementation and other stakeholders who have an interest in the success of the strategy. At this meeting, everyone should raise potential problems and obstacles to overcome if the project is going to be a success. Everyone should envision any obstacles or problems that are likely to occur, assume a worst-case scenario, and list potential issues. Then, put in place solutions that will resolve these problems should they appear.
Another consideration is how the new strategy will affect all areas of the enterprise and what potential problems and obstacles will be created by the new strategy. If the organization adds more hours, this will increase the traffic in the office, which could interfere with patients coming in for early blood draws.
Anticipating potential pitfalls and creating solutions will likely reduce the number of fires that need to be put out in the first few weeks of the implementation of the plan.
Proceeding from Concept to Reality
Almost by definition, a strategy can never be fully implemented because everything that is assumed when formulating it — about customers, technology, regulation, competitors, and so on — is in a constant state of flux.
CEOs and their business unit leaders must continuously evolve their strategies ( i.e., the fundamental choices listed above) if they are to remain relevant and competitive. And if that’s the case, there will always be a gap between where their companies are and what their strategies call for. Closing that gap is “implementation.” Thus, strategy and implementation are running continuously in parallel rather than in sequence, as Ken Favaro describes in his March 2015 Harvard Business Review article, “Defining Strategy, Implementation, and Execution.”
Garnering Support for the Strategy
Implementation consists of taking the actions to create something new and then evaluating the result and constantly modifying the actions until the desired result is achieved. An informal survey of business publications identifies several key elements necessary during the implementation stage of any strategy: acceptance and support for the strategy by the key stakeholders, a clear understanding of the decision-making rights of the staff accountable for implementation, and open and immediate communication from the top down and the bottom up.
Any significant strategy should be communicated to the staff throughout the planning process, and all levels of staff should have been given the opportunity to contribute to the plans. The physicians, providers, and administrators of a medical organization must be 100% in support of the strategy, and it must be clear to their staff, patients, and others that they are excited about the upcoming changes. Any hesitancy or second-guessing must be resolved immediately and not left to spread throughout the organization.
Everyone should be encouraged to bring concerns or problems to the person accountable for the strategy and be acknowledged, not ignored, when they do bring up a problem. Any problem identified is an opportunity to make the strategy more successful.
A critical part of this step is that administrators and staff be given the authority to make decisions at a certain level of operations on the spot and that the owners and higher management will support those decisions if they are within the approved guidelines. This gives each employee the ability to react quickly to unexpected issues that might arise in implementation.
Once the situation is resolved, the decision should be reported to the person accountable for implementation so that any impact of the decision on other areas of the process is identified and accounted for. In this way, the action plan is constantly being updated for new actions and revised dates. The plan should be available to the entire team and be discussed at a weekly meeting.
Declaring Completion
An often-over-looked step in implementation of a strategy or set of strategies is to declare completion when the project is operational, the strategy has been implemented, and the action is complete. Unlike a celebration by the members of an athletic team at the end of a game or match, the completion of a business project is seldom formally celebrated. The acknowledgment of completion is often obscured by day-to-day problems or the dragging out of finishing touches so that the project has been operating for months before all the details are finished.
When developing an action plan, it is always important to include milestones — places where sections of the plan can be declared complete, and the progress to date can be celebrated. At this point, some of the results from the action should be reported, and the entire group can be acknowledged for their contribution to the new reality.
Reaching milestones should be shared with not only the employees, but also all stakeholders in the organization, such as the patients, referring physicians, and hospital staff. By sharing these accomplishments, you are establishing in the minds of these people that you have an organization that is growing and expanding, and it is a great place to be. You are seen as a successful organization, and this alone can increase referrals.
Rewarding Performance
It’s a common axiom in business that what gets measured and reported gets done. This is because it’s a human trait to want to be accepted as a valuable member of the group. It is also important to be aware that direct rewards always affect performance, so we can say that what gets measured, reported on, and rewarded gets done faster.
Therefore, all strategies should have milestones, as discussed above, and along with the celebration of completion, there should be a reward. The reward doesn’t always have to be monetary; it can be recognition through an inexpensive gift, such as a coffee mug, or a prize with another perceived value, such as a coveted parking space. It really doesn’t matter; the real reward is public recognition for a job well done. These little breaks to celebrate completion keep the energy and commitment up for the project and allow the entire staff to feel part of the team.
Evaluating Success
Evaluation is the final step in the strategic management process. Without this step, the organization does not know whether it reached the desired goal and whether that goal was indeed in line with the organization’s mission and vision statements.
Every planned and executed action will produce results. The question is whether the results are what was expected or anticipated — and even whether they are results worth keeping.
The evaluation should take place 6-9 months after the project is complete and operating. By then, results will have been measured for a determined period, and performance month over month can be tracked. The project’s effect on the organization should be clear, as should the results of mid-implementation changes.
Once all the data have been analyzed, management and the implementation team should identify the three most desirable results of the project. One of the desirable items might even be a process that didn’t work well and was eliminated quickly.
The key is to identify what made those results work and then determine how that success can be replicated in any future project. When possible, a complete summary of the steps that led to the success should be documented in memo form and kept in the project resource file.
The team should also identify areas that could have been done better, then determine what led to the problems and how the process could be revised so that a different result might be obtained. These notes should also be kept in the project resource file.
It is important to set up analysis and measurement as an ongoing process. Many of the measurements should be incorporated into the monthly or quarterly reports so that the organization can make sure that the new process or strategy continues to create the success envisioned and continues to align with the mission and vision statements.
The Bottom Line
This process of identification and implementation in a business strategy is detailed and can be time-intensive. A busy organization might take a year to fully identify and implement a strategy; another organization might identify and implement a strategy during a single meeting. Regardless, the process is similar in each case.
When deciding to implement a new strategy, management should consider the time and dollars committed when determining how many of these steps to incorporate. Clearly, when the time and financial commitment are large, the process should be done in its entirety, but if it is a decision as simple as changing the professional staff uniform, some of the steps identified above can be modified and combined.
The bottom line is that for an organization to thrive and not just survive in the current healthcare environment, it needs to be proactive. This is easily accomplished by having a strategic plan to address where the practice is within the market, where it wants to be, and what gap or gaps must be closed for the practice to be operating consistently at the top of the industry.
Strategic Perspective
Critical Appraisal Skills
Differentiation
This article is available to AAPL Members.
Log in to view., career & learning, leadership library, membership & community, for over 45 years..
The American Association for Physician Leadership has helped physicians develop their leadership skills through education, career development, thought leadership and community building.
The American Association for Physician Leadership (AAPL) changed its name from the American College of Physician Executives (ACPE) in 2014. We may have changed our name, but we are the same organization that has been serving physician leaders since 1975.
CONNECT WITH US
Looking to engage your staff.
AAPL providers leadership development programs designed to retain valuable team members and improve patient outcomes.
American Association for Physician Leadership®
formerly known as the American College of Physician Executives (ACPE)
Privacy Policy | Advertising Kit | Press Room
Understanding Business Strategy to Facilitate Health Care Success
Published september 26, 2022, courses mentioned in this post: h ealth care strategy, series mentioned in this post: health care leadership.
When you think of health care organizations, do the terms sustainable advantage or strategic differentiation come to mind?
In an industry with increasing competition and innovation, leaders of U.S. healthcare organizations, or those delivering care, need to understand how the success of their business depends on these key principles. This includes understanding the industry you’re in and market dynamics, the forces that make it easy or difficult to capture value, and how you can successfully compete against rivals.
You must go beyond simply creating value to develop the critical thinking and analytical skills to evaluate the needs of your business, and its constituents, in order to optimize business decisions and inform new or innovative health care ventures.

Taught by Harvard Business School Professor Leemore Dafny , our Health Care Strategy course teaches learners to align business strategy with the challenges and structures of the health care industry in the United States.
This 5-week course explores four main concepts of business strategy that can enable leaders to deal with the unique challenges and structures of health care organizations. These concepts include:
Value Creation and Value Capture
Value is only created if purchasers are willing and able to pay an amount that exceeds the cost of producing a product or service. Additionally, value creation does not automatically result in value capture.
In Health Care Strategy , learners will exercise how to apply a framework that illustrates value creation and value capture. With case studies from Statins and Livongo , you’ll learn how to determine how much value a seller can capture by considering the competitive environment and the value created for different stakeholders.
Industry Analysis
Within the Industry Analysis module of Health Care Strategy , learners will perform a “five forces” analysis and assess the strength of different forces in different industries through a case study with Advanced Fertility Care . Identifying the forces that drive industry profits is a critical first step to defining a business strategy. A successful strategy combats the forces that diminish industry profits.
Developing a strategy requires making tradeoffs. Through a case study with Oak Street Health , learners will evaluate the tradeoffs made by an entrant in elder care, and how this informs decisions about their growth. Learners will better understand how positioning can enable you to succeed in an “unattractive” industry.
Value capture is more challenging when the value of a product or service is divided among different stakeholders, making this an extra challenge within the health care sector.
Competition
Competition among health care providers increases quality, reduces prices, and can increase a provider’s reach. Learners will evaluate the results of a “natural experiment” involving the British National Health Service (NHS) and assess opportunities provided by destination medicine for both providers and employers through a case study with Geisinger Health .
Learners will also analyze business and regulatory moves that reduce and enhance competition in different markets through a case study with the Surgical Institute of Reading .
The Boundaries of the Firm
The last module of Health Care Strategy dissects an organization’s decision to vertically integrate by observing consolidation in Eastern Massachusetts. The decision to vertically integrate depends on several factors, such as the necessity for “relationship specific” investments by upstream and downstream parties, and the degree of difficulty in aligning incentives with arms-length relationships.
Vertically integrated firms may find it more profitable to price their products less than they would if they were not integrated, even if there is no change in production cost from integrating. Learners will assess the effects of vertical integration on pricing under different assumptions.
Lastly, learners will examine the effects of provider-insurer integration on competition, prices, and access for patients through a case study with Civica Rx . Integration can deflect or enhance competition, depending on the industry structure and potential efficiencies created by the merger.
Register for an upcoming Health Care Strategy cohort today to learn how to use business strategy to facilitate health care success.
| Demonstrate that you are committed to your growth by specializing further and pursuing a multi-course certificate program.
The health care sector in the United States is one of the most essential and consequential parts of our economy.
|
|
|
Related Courses
Health care strategy.
Learn from HBS Professor Leemore Dafny how to align the principles of business strategy with the unique challenges and structures of health care organizations to capture value, define your mission, and lead your organization to success.
Health Care Economics
Taught by Harvard Medical School faculty, this course provides insights into the interactions between industries in the US health care sector and teaches what economic forces are shaping health care.
Digital Health
Digital technologies and big data offer tremendous opportunities to improve health care.
HAP Summer Sale | 20% Off
HAP Summer Sale - Order any book now through September 16 and receive a 20% discount off the member and non-member price when you use the promo code SUMMER24 at checkout. This discount excludes any multi-book sets that are already discounted and the Board of Governors Exam flashcards.

Strategic Healthcare Management: Planning and Execution, Third Edition
Stephen l. walston, phd.
- Member Price: $57.40
- Non Member Price: $82.00
- Strategic Planning
- New Release
Book Description
- The growing trend of healthcare data analytics, with emphasis on the importance of data-driven strategic analysis and the instruments used for extracting, manipulating, and visualizing data
- Project management principles to support strategy implementation, with an exploration of tools and techniques such as project charters, communication planning, scope definition, timelines, and Gantt charts.
- Table of Contents (PDF)
- Preface (PDF)
- Book Excerpt (PDF)
- Transition Guide
- Instructor Resource Sample

Futurescan 2018: Healthcare Trends and Implications 2018-2023
Looking Back to Look Forward: AUPHA at 70
-b084e1dd.jpg?w=160)
Management of Healthcare Organizations: An Introduction, Third Edition

Evidence-Based Management in Healthcare: Principles, Cases, and Perspectives, Second Edition
Strategic Healthcare Management: Planning and Execution, Second Edition
Essentials of Strategic Planning in Healthcare, Third Edition

Futurescan 2019–2024: Healthcare Trends and Implications
Exceptional Leadership: 16 Critical Competencies for Healthcare Executives, Second Edition

Futurescan 2022–2027: Health Care Trends and Implications
Marketing Health Services, Fourth Edition

Getting It Done: Experienced Healthcare Leaders Reveal Field-Tested Strategies for Clinical and Financial Success

Why Hospitals Should Fly: The Ultimate Flight Plan to Patient Safety and Quality Care
Transformative Planning: How Your Healthcare Organization Can Strategize for an Uncertain Future
Leadership for Public Health: Theory and Practice
An Insider’s Guide to Working with Healthcare Consultants

Healthcare Strategic Planning, Fourth Edition
Strategic Analysis for Healthcare: Concepts and Practical Applications, Second Edition

Make It Happen: Effective Execution in Healthcare Leadership

The Future of Healthcare: Global Trends Worth Watching
Essentials of Healthcare Management: Cases, Concepts, and Skills, Second Edition
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Strategic planning in healthcare organizations
Affiliation.
- 1 Medtronic Ibérica, Madrid, Spain. [email protected]
- PMID: 22699047
- DOI: 10.1016/j.recesp.2012.04.005
Strategic planning is a completely valid and useful tool for guiding all types of organizations, including healthcare organizations. The organizational level at which the strategic planning process is relevant depends on the unit's size, its complexity, and the differentiation of the service provided. A cardiology department, a hemodynamic unit, or an electrophysiology unit can be an appropriate level, as long as their plans align with other plans at higher levels. The leader of each unit is the person responsible for promoting the planning process, a core and essential part of his or her role. The process of strategic planning is programmable, systematic, rational, and holistic and integrates the short, medium, and long term, allowing the healthcare organization to focus on relevant and lasting transformations for the future.
Copyright © 2012 Sociedad Española de Cardiología. Published by Elsevier Espana. All rights reserved.
PubMed Disclaimer
Similar articles
- Strategic planning processes and financial performance among hospitals in Lebanon. Saleh S, Kaissi A, Semaan A, Natafgi NM. Saleh S, et al. Int J Health Plann Manage. 2013 Jan-Mar;28(1):e34-45. doi: 10.1002/hpm.2128. Epub 2012 Aug 1. Int J Health Plann Manage. 2013. PMID: 22859363
- An exploratory study of healthcare strategic planning in two metropolitan areas. Begun JW, Kaissi AA. Begun JW, et al. J Healthc Manag. 2005 Jul-Aug;50(4):264-74; discussion 274-5. J Healthc Manag. 2005. PMID: 16130809
- Strategic learning in healthcare organizations. O'Sullivan MJ. O'Sullivan MJ. Hosp Top. 1999 Summer;77(3):13-21. doi: 10.1080/00185869909596526. Hosp Top. 1999. PMID: 10787685 Review.
- Strategic cycling: shaking complacency in healthcare strategic planning. Begun J, Heatwole KB. Begun J, et al. J Healthc Manag. 1999 Sep-Oct;44(5):339-51; discussion 351-2. J Healthc Manag. 1999. PMID: 10621138
- Critical success factors for strategic telemedicine planning in New Zealand. Al-Qirim NA. Al-Qirim NA. Telemed J E Health. 2005 Oct;11(5):600-7. doi: 10.1089/tmj.2005.11.600. Telemed J E Health. 2005. PMID: 16250825 Review.
- Healthcare Organizations Management: Analyzing Characteristics, Features and Factors, to Identify Gaps "Scoping Review". Alsaqqa HH. Alsaqqa HH. Health Serv Insights. 2023 May 3;16:11786329231168130. doi: 10.1177/11786329231168130. eCollection 2023. Health Serv Insights. 2023. PMID: 37153880 Free PMC article. Review.
- Health Care Logistics Network Design and Analysis on Pandemic Outbreaks: Insights From COVID-19. Cetinkale Z, Aydin N. Cetinkale Z, et al. Transp Res Rec. 2023 Apr;2677(4):674-703. doi: 10.1177/03611981221099015. Epub 2022 Jun 15. Transp Res Rec. 2023. PMID: 37153192 Free PMC article.
- Strategic planning, components and evolution in zoonotic diseases frameworks: one health approach and public health ethics. Ghanbari MK, Gorji HA, Behzadifar M, Shoghli A, Martini M. Ghanbari MK, et al. J Prev Med Hyg. 2022 Jan 31;62(4):E981-E987. doi: 10.15167/2421-4248/jpmh2021.62.4.2323. eCollection 2021 Dec. J Prev Med Hyg. 2022. PMID: 35603238 Free PMC article. Review.
- Implementing a Clinical Research Department to Support Pediatric Studies: A SWOT Analysis. Thajer A, Sommersguter-Reichmann M, Löffler-Stastka H. Thajer A, et al. Int J Environ Res Public Health. 2020 Aug 27;17(17):6211. doi: 10.3390/ijerph17176211. Int J Environ Res Public Health. 2020. PMID: 32867050 Free PMC article.
- Corporate social responsibility and financial profile of Spanish private hospitals. Creixans-Tenas J, Coenders G, Arimany-Serrat N. Creixans-Tenas J, et al. Heliyon. 2019 Oct 11;5(10):e02623. doi: 10.1016/j.heliyon.2019.e02623. eCollection 2019 Oct. Heliyon. 2019. PMID: 31667425 Free PMC article. Review.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ediciones Doyma, S.L.
- Elsevier Science

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

- Youth Program
- Wharton Online
Business of Healthcare Specialization
Do you fully understand the impact of alternative payment models, particularly bundled payments, on the cost and quality of health care? Do you know how to design, implement, and measure financial and non-financial incentives to drive clinician practice change? Do you know how to use predictive analytics and informatics to improve health care delivery?
The Business of Healthcare Certificate program was designed to help you keep pace with the rapidly changing world of health and health care. Through partnership with Wharton and Penn Medicine, you’ll learn from experts in business acumen, health care management, and health care policy to develop the skills you’ll need to successfully navigate the intersection of business and health care.
By the end of this certificate program, you will have a strong foundational understanding of the American health care system, along with the basic financial and management skills to make better, well-informed decisions that improve the cost and quality of the health care you or your enterprise provides.
Why Take an Online Healthcare Certificate Program?
- Hospital executives say that preparing the enterprise for sustainable cost control is their No.1 concern, followed by innovative approaches to expense reduction at No.2 1
- 72 percent of physicians consider cost data valuable, but only 28 percent receive any such cost information 2
- The employment of medical and health services managers, including healthcare executives, is projected to grow 20 percent through 2026, significantly faster than the average for all occupations 3
Program Details
Start Dates: Immediately
Duration: 4 weeks per course
Commitment: 2-3 hours per week
Program Format: 100% Online
Program Tuition: $79 per month
READY TO START?
Business of healthcare specialization courses.

FINANCIAL ACUMEN FOR NON-FINANCIAL MANAGERS
$79/month Duration: 4 weeks (2-3 hours/week)
Gain a practical understanding of how data is used to assess what drives financial performance and forecast future financial scenarios. Learn about the frameworks of financial reporting, income statements, and cash reporting, and apply different approaches to analyzing financial performance using real-life examples.
Full Course Description

THE ECONOMICS OF HEALTH CARE DELIVERY
This course is designed to help you understand the complex structure of the health care system and health insurance. Through the study and analysis of providers and insurance through an economic lens, you’ll learn how basic economic principles apply to both principles and payment methods.

MANAGEMENT FUNDAMENTALS
People are the most valuable asset of any business, but they are also the most unpredictable, and the most difficult asset to manage. This course will help you develop the skills you need to start motivating, organizing, and rewarding people in your organization.

HEALTH CARE INNOVATION
Designed to help you gain a practical understanding of the theoretical frameworks of behavioral economics and operations management in the health care setting, this course will help you apply these frameworks to assess health care practices and apply innovation while managing risk.
Ready to get started? Enroll Now
Key certificate program takeaways.
In our online healthcare certificate program, participants will learn how to:
- Employ best practices to maximize profit for a healthcare organization
- Calculate the financial viability of a health care provider using key performance indicators
- Evaluate the Iron Triangle of Health Care (quality, cost, and access)
- Make good and timely management decisions and build a higher performing team
- Establish a framework for implementing effective and successful health care interventions
Business of Healthcare Faculty
The Business of Healthcare Specialization program channels the knowledge and insights of experts from Wharton and the Perelman School of Medicine at the University of Pennsylvania.
Learn from and interact with some of the leading experts at the intersection of business and healthcare, including the former special advisor for health policy to the director of the White House Office of Management and Budget and authors of such books as Prescription for the Future: The Twelve Transformational Practices of Highly Effective Medical Organizations . Faculty members hold MBAs, MDs and PhDs from world-class institutions like Harvard University, Harvard Medical School, UCLA, and the University of Chicago, and their work has been published in numerous leadings journals such as The New England Journal of Medicine (NEJM) and The Journal of the American Medical Association (JAMA).
Faculty research interests include:
- Health policy
- Health care reform
- Health care management
- Delivery innovation
- Physician executives
- Operational performance
- Innovation management
- R&D management
Christian Terwiesch, PhD
Andrew M. Heller Professor at the Wharton School; Professor of Operations, Information, and Decisions; Professor of Health Policy, Perelman School of Medicine; Co-Director, Mack Institute of Innovation Management
Research Interests: Analyzing operational performance, innovation management, R&D management
See Faculty Bio
Christopher D. Ittner, PhD
EY Professor of Accounting; Chairperson, Accounting Department, The Wharton School
Research Interests: Cost accounting, intangible assets, performance measurement
Richard Lambert, PhD
Miller-Sherrerd Professor; Professor of Accounting, The Wharton School
Research Interests: Financial reporting, cost analysis, incentive compensation plans
Ezekiel J. Emanuel, MD, PhD
Diane v.S. Levy and Robert M. Levy University Professor; Professor of Health Care Management, The Wharton School; Professor of Medical Ethics and Health Policy, Perelman School of Medicine, University of Pennsylvania
Research Interests: Health policy, health care reform, medical ethics, drug pricing, transformations, bundled payments
Peter Cappelli, DPhil
George W. Taylor Professor of Management; Director, Center for Human Resources, The Wharton School
Research Interests: Human-resource practices, public policy related to employment, talent and performance management
Kevin Volpp, MD, PhD
Janet and John Haas President’s Distinguished Professor, Medical Ethics and Health Policy; Director, Center for Health Incentives and Behavioral Economics, Leonard Davis Institute; Professor of Medicine; Professor of Health Care Management
Research Interests: Behavioral economics, habit formation, wellness incentives, innovation in health delivery
David A. Asch, MD, MBA
Professor of Medicine, Medical Ethics, and Health Policy; Professor of Anesthesiology and Critical Care Medicine; Professor of Health Care Management; Professor of Operations, Information, and Decisions; Executive Director, Center for Health Care Innovation, The Wharton School
Research Interests: Clinician and patient decision making, health care management, health policy, medical ethics, physician executives, technology assessment, behavioral economics
Amol S. Navathe, MD, PhD
Assistant Professor, Health Policy and Medicine, Perelman School of Medicine
Research Interests: Delivery innovation, health IT, organization of healthcare delivery
Guy David, PhD
Gilbert and Shelley Harrison Associate Professor of Health Care Management; Associate Professor, Medical Ethics and Health Policy, Perelman School of Medicine
Research Interests: Applied microeconomics, emergency medical services, health economics, industrial organization, nonprofit organizations, post-acute care, regulation
Roy Rosin, MBA
Leonard David Institute of Health Economics Senior Fellow; Chief Innovation Officer Penn Medicine, Perelman School of Medicine
Research Interests: Access to care, behavioral economics/behavior change, delivery innovation, disease prevention/health promotion, disparities and health equity, bundled payments, health IT, medication adherence, organization of healthcare delivery, risk communication, social media and health
Michael Useem, PhD
William and Jacalyn Egan Professor of Management; Professor of Management; Director, Center for Leadership and Change Management; Editor, Wharton Leadership Digest
Research Interests: Catastrophic and enterprise risk management, corporate change and restructuring, leadership, decision making, governance
The Wharton School is accredited by the International Association for Continuing Education and Training (IACET) and is authorized to issue the IACET CEU.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Planning and Managing Health Systems
Health systems are complex organizations. They are often the largest single employer in a country, with expenditures of public and private money of 4–17 percent of gross domestic product. Overall and individual facility management requires mission statements, objectives, targets, budgets, activities planning, human interaction, services delivery, and quality assurance. Health organization involves a vast complex of stakeholders and participants, suppliers and purchasers, regulators and direct providers, and individual patients, and their decision-making. These include pyramidal and network organizations and ethical decision-making based on public interest, resource allocations, priority selection, and assurance of certain codes of law and ethical conduct. This chapter discusses how complex organizations work, with potential for application in health, and the motivations of workers and of the population being served. Organization theory helps in devising methods to integrate relevant factors to become more effective in defining and achieving goals and missions.
Learning Objectives
Upon completion of this chapter, the student should be able to:
- 1. Define the role of management at all levels of health service and public health organization;
- 2. Apply management theory to health planning and the New Public Health;
- 3. Continue preparation for leadership roles in health service organizations.
Introduction
Health systems are complex organizations and their management is an important concept in the New Public Health. Health is a major sector of any economy and often employs more people in the industrialized countries than any other industry. Health has complex networks of services and provider agencies, including funding through public or private insurance or through national health service systems. Whether insurance is provided by the state or through private and public sources combined, skilled management is required at the macro- or national and the micro- or local level, including the many institutions that make up the system. Management training of public health professionals and clinical services personnel is a requisite and not a luxury.
Planning and management are changing in the era of the New Public Health with advances in prevention and treatment of disease, population health needs, innovative technologies such as genetic engineering, new immunizations that prevent cancers and infectious diseases, prevention of non-communicable diseases, environmental and nutritional health, and health promotion to reduce risk factors and improve healthful living for the individual and the community. Modern and successful public health also must address social, economic, and community determinants of health and the promotion of public policies and individual behaviors for health and well-being. The social capital and norms that promote cooperation among people are the basis of a “civil society” (i.e., the totality of voluntary, civic, and social organizations and institutions of a functioning society alongside the structures of governmental and commercial institutions). Health systems are ideally knowledge- and evidence-based in using technologies available in medicine and the environment to promote the health and well-being of a population, including security against the effects of threatened terrorism, growing social isolation, and inequities in health. Management in health can learn much from concepts of business management that have evolved to address the economic and human resource aspects of a health system at the macrolevel or an individual unit of service at the microlevel.
The New Public Health is not contained within one organization, but rather reflects the collective efforts of national, state, regional, and local governments, many organizations in the public and non-governmental sectors, and finally efforts of individual or group advocates and providers and the public itself. The political level is crucial for adequate funding, legislation, and promotion of health-oriented policy positions and in public health management. The responsibility for health management is shared across all parts of society, including individuals, communities, business, and all levels of government.
The New Public Health identifies and addresses community health risks and needs. Planning is critical to the process of keeping a health system sustainable and adaptable and in creating adequate responses to new health threats. Monitoring, measurement, and documentation of health needs are vital to design and adapt an effective program and to measure impact. Data on the targeted issues must be accessible while protecting individual privacy.
Health is a hugely expensive and expansive complex of services, facilities, and programs provided by a wide range of professional and support service personnel making up one of the largest employers of any sector in a developed country. Services are increasingly delivered by organized groups of providers. But all health systems operate in an environment of economic constraints, imposing a need to seek efficiency in the use of resources. How organizations function is of great importance not only for their economic survival, but also, and equally important, for the well-being of the clients and providers of care.
An organization is two or more people working together to achieve a common goal. Management is the process of defining the goals and making effective use of an organization to attain those goals. Even very small units of a human organization require management. Management of human resources is vital to the success of an organization, whether in a production or service industry. Health systems may vary from a single structure to a network of many organizations. No matter how organizations are financed or operated, they require management.
Management in health care has much to learn from approaches to management in other industries. Elements of theories and practices of profit-oriented sector management can be applied to health services even if they are operated as non-profit enterprises. Physicians, nurses, and other health professionals will very likely be involved in the management of some part of the health care system, whether a hospital department, a managed care system, a clinic, or even a small health care team. At every level, management always means working with people, using resources, providing services, and working towards common objectives.
Health providers require preparation in the theory and practice of management. A management orientation can help providers to understand the wider implications of clinical decisions and their role in helping the health care system to achieve goals and targets. Students and practitioners of public health need preparation in order to recognize that a health care system is more complex than the direct provision of individual services. Similarly, policy and management personnel need to be familiar with both individual and population health needs and related care issues.
Health Policy and Planning as Context
Health has evolved from an individual one-on-one service to complex systems organized within financing arrangements, mostly under government auspices. As a governmental priority, health may be influenced by political ideology, sometimes reflecting societal attitudes of the party in power and sometimes apparently at odds with its general social policy. Following Bismarck’s introduction in Germany in 1881 of national health insurance for workers and their families, funded by both workers and their employers, most countries in the industrialized world introduced variants of this national health plan. Usually, this has been at the initiative of socialist or liberal political leadership, but conservative political parties have preserved national health programs once implemented. Despite the new conservatism since the 1990s with its pre-eminent ideology of market forces, the growing roles for national, state, and local authorities in health have led to a predominantly government role in financing and overall responsibility for health care, even where there is no universal national health system, as in the USA. The UK’s National Health Service (NHS), initiated by a Labour government in 1948, has survived through many changes of government, including the conservative Margaret Thatcher period in which many national industries and services were privatized.
Health policy is a function of national (government) responsibility overall for health, but implementation is formulated and met at state, local, or institutional levels. The division of responsibilities is not always clear cut but needs to be addressed and revised both professionally and politically within constitutional, legal, and financial constraints. Selection of the direction to be taken in organizing health services is usually based on a mix of factors, including the political view of the government, public opinion, and rational assessment of needs as indicated through epidemiological data, cost–benefit analysis, the experience of “good public health practice” from leading countries, and recommendations by expert groups. Lobbying on the part of professional or lay groups for particular interests they wish to promote is part of the process of policy formulation and has an important role in the planning and management of health care systems. There are always competing interests for limited resources of funding, by personnel within the health field itself and in competition with other demands outside the health sector.
The political level is vitally involved in health management in establishing and maintaining national health systems, and in determining the place of health care as a percentage of total governmental budgetary expenditures, in allocating funds among the competing priorities. These competing priorities for government expenditures include defense, roads, education, and many others, as well as those within the health sector itself. Traditionally, there are competing priorities between the hospital and medical sector and the public health and community programs sector. A political commitment to health must be accompanied by allocation of resources adequate to the scope of the task. Thus, health policy is largely determined by societal priorities and is not a prerogative of government, health care providers, or any institution alone.
As a result of long struggles by trade unions, advocacy groups, and political action, well-developed market economies have come to accept health as a national obligation and essential to an economically successful and well-ordered society. This realization has led to the implementation of universal access systems in most of the industrialized countries. Once initiated, national health systems require high levels of resources, because the health system is labor intensive with relatively high salaries for health care professionals. In these countries, health expenditures consume between 7 and nearly 18 percent of gross domestic product (GDP). Some industrialized countries, notably those in the former Soviet bloc, lacking mechanisms for advocacy, including consumer and professional opinion, tended to view health with a political objective of social benefits, and also as a “non-productive” consumer of resources rather than a producer of new wealth. As a result, budget allocations and total expenditures for health as a percentage of GDP were well below those of other industrialized countries ( Figure 12.1 ). Salaries for health personnel in the Semashko system were low compared to industrial workers in the “productive” sectors. Furthermore, industrial policy did not promote modern health-related industries, compared to the military or heavy industrial sectors.

Total health expenditure as percentage of gross domestic product (GDP), World Health Organization estimates.
The former socialist countries of Eastern Europe which have joined the European Union (EU) have gradually increased allocation to health from 5.44 percent of GDP in 1995 to 7.1 percent in 2010, while the pre-2004 members of the EU increased their expenditures from 8.5 percent of GDP to 10.6 percent. The average spend in the Commonwealth of Independent States (Russia, Ukraine, and others) increased from 5.6 percent in 1995 to 5.74 percent in 2010, and in the Central Asian Republics (Kazakhstan, Uzbekistan, and others) from 4.8 percent in 1995 to 5.2 percent in 2010 (WHO Health for All database, January 2013). However, Russian health expenditure in 2011 was still only 6.2 percent of GDP and there is a lingering idea of health being a non-productive investment. The developing countries generally spend under 4 percent of GNP on health, because health is addressed as a relatively low political priority, and they depend very much on international donors for even the most basic of public health programs such as immunization.
Financing of health care and resource allocation requires a balance among primary, secondary, and tertiary care. Economic assessment, monitoring, and evaluation are part of determining the health needs of the population. Regulatory agencies are responsible for defining goals, priorities, and objectives for resulting services. Targets and methods of achieving them provide the basis for implementation and evaluation strategies. Planning requires written plans that include a statement of vision, mission objectives, target strategies, methods, and coordination during the implementation. Designation and evaluation of responsibilities, resources to be committed, and participants and partners in the procedure are part of the continuous process of management.
The dangers of taking a “wrong” direction may be severe, not only in terms of financial costs, but also in terms of high levels of preventable morbidity and mortality. Health policy is often as imprecise a science as medicine itself. The difference is that inappropriate policy can affect the lives and well-being of very large numbers of people, as opposed to an individual being harmed by the mistake of one doctor. There may be no “correct” answer, and there are numerous controversies along the path. Health policy remains more an “art” than the more quantitative and seemingly precise field of health economics. Societal, economic, and cultural factors as well as personal habits have long been accepted as having an important impact on vulnerability to coronary heart disease. But other factors such as the degree of control over one’s life, as suggested in studies of British civil servants, religiosity, and the effects of migration on families left behind are part of the social gradients and inequalities seen in many disease entities, with consequent excess morbidity and mortality in some contexts, such as in Russia and Ukraine.
Health policy, planning, and management are interrelated and interdependent. Any set goal should be accompanied by planning how to attain it. A policy should state the values on which it is based, as well as specify sources of funding, planning, and management arrangements for its implementation. Examination of the costs and benefits of alternative forms of health care helps in making decisions as to the structure and the content of health care services, both internal structures (within one organization) and external linkages (intersectoral cooperation with other organizations). The methods chosen to attain the goals become the applied health policy.
The World Health Organization’s (WHO’s) 1977 Health for All strategy was directed at the political level and intended to increase governmental awareness of health as a key component of overall development. To some degree it succeeded despite its expansive aspirations, and even after nearly 40 years, its objectives remain worthwhile even in well-developed health systems. Within health, primary care was stressed as the most effective investment to improve the health status of the population. In 1993, the World Bank’s World Development Report adopted the Health for All strategy and promoted the view that health is an important investment sector for general economic and social development. However, economic policies promoting privatization and deregulation in the health sector threaten to undermine this larger goal in countries with national health systems.
In the USA, major steps are being taken to increase coverage of health insurance for all as the number of uninsured Americans declined from 50 million people uninsured in 2010 to 48.6 million in 2011, edging down from 16.3 to 15.7 percent of the total population. Further decline in the uninsured population is expected as the Patient Protection and Affordable Care Act (PPACA, or “Obamacare”) comes into effect in the coming years, bringing many millions of Americans into health insurance and meeting federal standards of fair practices such as eliminating exclusion for pre-existing conditions by private insurers. The PPACA comes into effect on 1 January 2014 and will guarantee coverage for pre-existing conditions, and ensure that premiums cannot vary based on gender or medical history. It will subsidize the cost of coverage, and new state-based health insurance exchanges will help consumers to find suitable policies. It will introduce many preventive care measures into public and private insurance plans, and will promote efficiencies in the health systems including reduction in fraudulent claims and wasteful funding systems. All of this will require skilled management in the components of the health system (see Chapters 10 and 13Chapter 10Chapter 13).
In the New Public Health, health promotion, preventive care, and clinical care are all part of public health because the well-being of the individual and the community requires a coordinated effort from all elements of the health spectrum. Establishing and achieving national health goals require planning, management, and coordination at all levels. The achievement of health advances depends on organizations and structured efforts to reach health goals such as those defined above, and more recently by the United Nations (UN) in the Millennium Development Goals (MDGs) (see Chapter 2), and requires some understanding of organizations and how they work.
The Elements of Organizations
The study of organizations developed within sociology, but has gradually become a multidisciplinary activity involving many other professional fields, such as economics, anthropology, individual and group psychology, political science, human resources management, and engineering. Organizations, whether in the public or private sector, exist within an external environment, and utilize their own structure, participants, and technology to achieve goals. For an organization to survive and thrive, it must adapt to the physical, social, cultural, and economic environment.
Organizations participating in health care establish the connection between service providers and consumers, with the goal of better health for the individual and the community. The factors for this include legislation, regulation, professionalism, instrumentation, medications, vaccines, education, and other modalities of intervention for prevention and treatment. The social structure of an organization may be formal (structured stability), natural (groupings reflecting common interests), or open (loosely coupled, interacting, and self-adjusting systems to achieve goals).
Formal systems are deliberately structured for the purposes of the organization. Natural systems are less formal structures where participants work together collaboratively to achieve common goals defined by the organization. Open systems relate elements of the organization to coalitions of partners in the external environment to achieve mutually desirable goals. In the health system, structures should focus on prevention and treatment of disease and improvement in health and well-being of society. The social structure of an organization includes values, norms, and roles governing the behavior of its participants.
Government, business, or service organizations, including health systems, require organizational structures, with a defined mission and set of values, in order to function. An organizational structure needs to be tailored to the size and complexity of the entity and the goals it wishes to achieve. The structure of an organization is the way in which it divides its labor into distinct tasks and coordinates them. The major organizational models, which are not mutually exclusive and may indeed be complementary, are the pyramidal (bureaucratic) and network structures. The bureaucratic model is based on a hierarchical chain of command with clearly defined roles. In contrast, the matrix or network organization brings together professional or technical people to work on specific programs, projects, or tasks. Both are vital to most organizations to meet ongoing responsibilities and to address special challenges.
Scientific Management
Some classic organization theory concepts help to set the base for modern management ideas as applied to the health sector. Scientific management was pioneered by Frederick Winslow Taylor (1856–1915). His work was pragmatic and based on empirical engineering, developed in observational studies carried out for the purpose of increasing worker, and therefore system, efficiency. Taylor’s industrial engineering studies of scientific management were based on the concept that the best way to improve worker productivity was by designing improved techniques or methods used by workers. This theory viewed workers as instruments to be manipulated by management, and assumed that efficient, rationally planned methods would produce better industrial results and industrial peace as the tasks of managers and workers would be better defined.
Time and motion studies analyzed work tasks to seek more efficient methods of work in factories. Motivation of workers was seen to be related to payment by piecework and economic self-interest to maximize productivity. Taylor sought to improve the productivity of each worker and to make management more efficient in order to increase earnings of employers and workers. He found that the worker was more efficient and productive if the worker was goal oriented rather than task oriented. This approach dominated organization theory during the early decades of the twentieth century.
Resistance to Taylor’s ideas came from both management and labor; the former because it seemed to interfere with managerial prerogatives and the latter because it expected the worker to function at top efficiency at all times. However, Taylor’s work had a lasting influence on the theory of work and organizations.
Bureaucratic Pyramidal Organizations
The traditional pyramidal bureaucratic organization is classically seen in the military and civil services, but also in large-scale industry, where discipline, obedience, and loyalty to the organization are demanded, and individuality is minimized. This form of organization was analyzed by sociologist Max Weber between 1904 and 1924. Leadership is assigned by higher authority, and is presumed to have greater knowledge than members lower down in the organization. This form of organization is effective when the external and internal environments, the technology, and functions are relatively well defined, routine, and stable.
The pyramidal system ( Figure 12.2 ) has an apex of policy and executive functions, a middle level of management personnel and support staff, and a base of the people who produce the output of the organization. The flow of information is generally one way, from the bottom to the top level, where decisions are made for the detailed performance of duties at all levels. Lateralizing the information systems so that essential data can be shared to help staff at the middle and field or factory-floor levels of management is generally discouraged because this may promote decentralized rather than centralized management. Even these types of organization have increasingly come to emphasize small-group loyalty, leadership initiative, and self-reliance.

Pyramid structure of organizations.
The bureaucratic organization has the following characteristics:
- • There is a fixed division of labor with a clear jurisdiction and based on assignments, which are subject to change by the leader.
- • There is a hierarchy of offices, with each lower functionary controlled and supervised by a higher one.
- • A documented, stable set of rules governs decisions and actions.
- • Property and rights belong to the office, not the person in the office.
- • Officials are selected on the basis of qualifications; salaries and benefits are based on technical competencies.
- • Employment is viewed as a tenured career for officials, after an initial trial period.
The bureaucratic system, based on formal rationality, structure, and discipline, is widely used in production, service, and governmental agencies, including military and civilian departments and agencies.
Organizations as Energy Systems
Health systems, like other organizations, are dynamic and require continuous management, adjustment, and systems control. Continuous monitoring and feedback, evaluation, and revision help to meet individual and community needs. The input–process–output model ( Figure 12.3 ) depends on feedback systems to make the administrative or educational changes needed to keep moving towards the selected objectives and targets.

Organizations as energy systems.
Organizations use resources or inputs that are processed to achieve desired results or outputs. The resource inputs are money, personnel, information, and supplies. Process is the accumulation of all activities taken to achieve the results intended. Output, or outcome, is the product, its marketing, its reputation and quality, and profit. In a service sector such as health, output or impact can be measured in terms of reduced morbidity and/or mortality, improved health, or number of successfully treated and satisfied patients at affordable costs. The management system provides the resources and organizes the process by which it hopes to achieve the established goals.
Program implementation requires systematic feedback for the process to work effectively. When targets are set and strategy is defined, resources, whether new or existing, are placed at the service of the new program. Management is then responsible for using the resources to achieve the intended targets. The results are the outcome or output measures, which are evaluated and fed back to the input and process levels.
Health systems consist of many subsystems, each with an organization, leaders, goals, targets, and internal information systems. Subsystems need to communicate within themselves, with peer organizations, and with the macro (health) system. Leadership style is central to this process. The surgeon as the leader of the team in the operating room depends on the support and judgment of other crucial people on the team, such as anesthesiologists, operating room nurses, pathologists, radiologists, and laboratory services, all of whom lead their own teams. Hospital and public health directors cannot function without a high degree of decentralized responsibility and a creative team approach to quality development of the facility.
Health systems management includes analysis of service policy, budget, decision-making in policy, as well as operation, regulation, supervision, provision, maintenance, ethical standards, and legislation. Policy formulation involves a set of decisions made in pursuit of a course of action for achieving selected health targets, such as those in the MDGs or continuing to update Healthy People 2020 health targets in the USA (see Chapter 2).
Cybernetics and Management
Cybernetics , a term coined by Norbert Wiener, refers to systems or organizations which are dependent on each other to function, and whose interdependence requires flexibility of response. Cybernetics gained wide credence in engineering in the early 1950s, and feedback systems became part of standard practice of all modern management systems. Its later transformations appeared in operating service systems, as information for management. Application of this concept is entering the health sector. Rapid advances in computer technology, by which personal computers have access to Internet systems and large amounts of data, have already enhanced this process. In mechanistic systems, the behavior of each unit or part is constrained and limited; in organic systems, there is more interaction between parts of the system. The example used in Figure 12.4 is the use of a thermostat to control the temperature and function of a heater according to conditions in the room. This is also described as a feedback system.

Cybernetic feedback control organization.
Cybernetics opens up new vistas on the use of health information for managing the operation of health systems. A database for each health district would allow assessment of current epidemiological patterns, with appropriate comparisons to neighboring districts or regional, state, and national patterns.
Data would need to be processed at state or national levels in comparable forms for a broad range of health status indicators. Furthermore, the data should be prepared for online availability to local districts in the form of current health profiles. Thus, data can be aggregated and disaggregated to meet the management needs of the service, and may be used to generate real targets and measure progress towards meeting them. A geographic information system may demonstrate high rates of a disease in a region due to local population risk factors, and thus become the basis for an intervention program.
In the health field, the development of reporting systems based on specific diseases or categories has been handicapped by a lack of integrative systems and a geographic reporting approach. The technology of computers and the Internet should be used to process data systems in real time and in a more user-friendly manner. This would enable local health authorities and providers to respond to actual health problems of the communities.
Health is a knowledge-based service industry, so that knowledge management and information technology are extremely important parts of the New Public Health, not only in patient care systems in hospitals, but also in public health delivery systems in the community, school, place of work, and home. Mobilization of evidence and experience of best practices for policies and management decision- making is a fundamental responsibility of health leaders. The gap between information and action is wide and presents an ethical as well as a political challenge. Regions with the most severe health problems lack trained personnel in assessment and exploitation of current state-of-the-art practices and technology in many practical public health fields, including immunization policy and in management of risk factors for stroke.
Knowledge and evidence are continuously evolving, but the capacity to access and interpret information is commonly poorly implemented in many countries so that very large numbers of people die of preventable diseases even when there are, overall, sufficient resources to address the challenges. International guidelines are vital to help countries to adopt current standards and make use of the available knowledge for public policy. Political support and openness to international norms are crucial to this process of technology diffusion and building the physical and human resource infrastructure needed to achieve better population health with current best practices. Development of health standards in low-income countries is progressing but is seriously handicapped by low levels of funding, lack of emphasis on training sufficient and appropriate human resource personnel and administrative support to promote measures which can save millions of lives. In high-income countries, the slow adoption of best international health standards can have harsh effects on population health, such as in the long delay in adopting national health insurance in the USA. In the European context, the EU has failed to adopt a harmonized recommended immunization program, which is badly needed for the new and potential members, as well as the older member countries. In countries of the former socialist bloc, mortality rates from stroke and coronary heart disease are slowly declining but remain two to four times higher than in countries of Western Europe (see Chapter 5). Systems management requires access to and the use of knowledge to bridge these gaps.
Adoption and adaptation of knowledge to address local problems are essential in a globalized world, if only to prevent the international spread of threatened pandemics or adoption of unhealthy lifestyles (diet, smoking, and lack of exercise) to middle-income countries, which are developing a growing middle class alongside massive poverty. The application of knowledge and experience that has been successful in leading countries can foster innovation and create experience that may generate a local renewal process. Management is crucial to address the complex “strategy areas for improving performance of health organizations: standards and guidelines, organizational design, education and training, improved process, technology and tool development, incentives, organizational culture, and leadership and management” (Bradley et al., 2012). Managing a knowledge-based service industry or facility relies on leadership, collaboration to realize the potential of technology, professional skills, and social capital to the address the health problems faced by all countries.
Target-Oriented Management
The management of resources to achieve productivity and measurable success has been characterized and accompanied by the development of systems of organizing people to create solutions to problems or to innovate towards defined objectives.
Operations Research
Operations research is a concept developed by British scientists and military personnel in search of solutions for specific problems of warfare during World Wars I and II. The approach was based on the development of multidisciplinary teams of scientists and personnel. The development of the Anti-Submarine Detection Investigation Committee for underwater detection of submarines during World War I characterized and pioneered this form of research. The famous Bletchley Park Enigma code-breaking success in Britain and the Manhattan Project, in which the USA assembled a powerful research and development team which produced the atomic bomb, are prime World War II examples.
Team- and goal-oriented work was very effective in problem solving under the enormous pressure of wartime needs. It also influenced postwar approaches to developmental needs in terms of applied science in such areas as the aerospace and computer industries. The computer hardware and software industries are characterized by innovation conceived and developed through informal working groups with a high level of individual competence, peer group dynamism, and commitment to problem solving. Thus, the “nerds” of Macintosh and Microsoft beat the “suits” of IBM in innovation and introduction of the personal computer. Similar startup groups, such as Google and Facebook, successfully took the Internet to startling new levels of global applications, showing the capacity of innovation from California’s Silicon Valley and its counterparts in other places in the USA and worldwide.
In the health field, innovation in organization developed prepaid group practice which became the health maintenance organization (HMO), and later the managed care organization (MCO), now a major, if controversial, factor in health care provision in the USA. Other examples may be found in multidisciplinary research teams working on vaccines or pharmaceutical research, and in the increasingly multidisciplinary function of hospital departments and especially highly interdependent intensive care or home care teams.
Management by Objectives
The business concept of management by objectives (MBO), pioneered in the 1960s, has become a common theme in health management. MBO is a process whereby managers of an enterprise jointly identify its goals, define each individual’s areas of responsibility in terms of the results expected, and use these measures as guides for operating the unit and assessing the contributions of its members.
The common goals and then the individual unit goals must be established, as well as the organizational structure developed to help achieve these goals. The goals may be established in terms of outcome variables, such as defined targets for reduction of infant or maternal mortality rates. Goals may also be set in terms of intervening or process variables, such as achieving 95 percent immunization coverage, prenatal care attendance, or screening for breast cancer and mammography. Achievements are measured in terms of relevancy, efficiency, impact, and effectiveness.
The MBO approach has been subject to criticism in the field of business management because of its stress on mechanical application of quantitative outcome measures and because it ignores the issue of quality. This approach had great influence on the adoption of the objective of “Health for All” by the WHO, and on the US Department of Health and Human Services’ 1979 health targets for the year 2000, later as Healthy People 2010, and now, based on these experiences and new evidence, renewed as Healthy People 2020. Targeting diseases for eradication may contribute to institution building by developing experience and technical competence to broaden the organizational capacity.
However, categorical programs or target-oriented programs can detract from the development of more comprehensive systems approaches. Addressing the MDGs of reducing child and maternal mortality is at odds to some extent with targeting poliomyelitis for eradication and reliance on national immunization days, which distract planning and resource allocation for the buildup of the essential public health infrastructure for the basic immunization system so fundamental to child health. Immunization and human immunodeficiency virus (HIV) control draw the major part of donor resources in developing countries, while education for strengthening human resources and infrastructure draw less donor attention. A balance between comprehensive and categorical approaches requires very skilled management. The MDGs agreed to by the UN in 2001 as targets for the year 2015 provide a set of measurable objectives and a formula for international aid and for national development planning to help the poorest nations, with the wealthy nations providing aid, education, debt relief, and economic development through fairer trade practices. They are now being reviewed for extension to 2020 based on experience to date, with successes and failures, and recognizing the vital importance of non-communicable diseases as central to the health burden of low- and middle-income countries.
Human Relations Management
Management is the activity of coordinating and integrating organizational resources, including people, money, materials, time, and space. The purpose is to achieve defined/stated objectives as effectively and efficiently as possible. Whether in terms of producing goods and profits or in delivering services effectively, management deals with human motivation and behavior because workers are the key to achieving goals. Knowledge and motivation of the individual client and the community are also essential for achieving good health. Thus, management must take into account the knowledge, attitudes, beliefs, and practices of the consumer as much as or more than those of the people working within the system, as well as the general cultural and knowledge level in the society, as reflected in the media, political opinions, and organizations addressing the issues.
Management, like medicine, is both a science and an art. The application of scientific knowledge and technology in medicine involves both theory and practice. Similarly, management practice involves elements of organizational theory, which, in turn, draws on the behavioral and social sciences and quantitative methodologies. Sociology, psychology, anthropology, political science, history, and ethics contribute to the understanding of psychosocial systems, motivation, status, group dynamics, influence, power, authority, and leadership. Quantitative methods including statistics, epidemiology, survey methods, and economic theory are also basic to development of systems concepts. Comparative institutional analysis helps principles of organization and management to develop, while philosophy, ethics, and law are part of understanding individual and group value systems.
Organizational theory, a relatively new discipline in health, as an academic study of organizations, addresses health-related issues using the methods of economics, sociology, political science, anthropology, and psychology. The application of organizational theory in health care has evolved and become an integral part of training for, and the practice of, health administration. Related practical disciplines include human resources, and industrial and organizational psychology. Translation of organizational theory into management practice requires knowledge, planning, organization, mobilization of professional and other staff support for evidence-based best practices, assembly of resources, motivation, monitoring and control. Health organizations have become more complex and costly over time, especially in their mix of specializations in science, technology, and professional services.
Organization and management are particularly crucial for successful application of the principles of the New Public Health, as it involves integration of traditionally separate health services. Delegation of responsibilities in health systems, such as in intensive care units, is fundamental to success in patient care, with nurses taking increasing responsibility for the management of the severely ill patient suffering from multiple system failure. Delegation or devolution of health care responsibilities to non-medical practitioners has been an ongoing development affecting nurse practitioners, physician assistants, paramedics, community health workers and others, as discussed in Chapter 14. It is a vital process to provide needs not met by physicians because of shortages and inappropriate location or specialty preferences that leave primary care or other medical specialties unable to meet community and patient needs.
The Hawthorne Effect
Elton Mayo of the Harvard School of Business carried out a series of observational studies at the Hawthorne, Illinois, plant of the Western Electric Company between 1927 and 1932. Mayo and his industrial engineer, along with psychologist colleagues, made a major contribution to the development of management theory. Mayo began with industrial engineering studies of the effect of increased lighting on production at an assembly line. This was followed by other improvements in working conditions, including reduced length of the working day, longer rest periods, better illumination, color schemes, background music, and other factors in the physical environment. These studies showed that production increased with each of these changes and improvements. However, the researchers discovered, to their surprise, that production continued to increase when the improvements were withdrawn. Furthermore, in a control group where conditions remained the same, productivity also grew during the study period. These results led Mayo to conclude that the performance of workers improved because of a sense that management was interested in them, and that worker participation contributes to improved production.
Traditionally, industrial management viewed employees as mechanistic components of a production system. Previous theory was that productivity was a function of working conditions and monetary incentives. What came to be known as the Hawthorne effect showed the importance of social and psychological factors on productivity. Formal and informal social organizations among management and employees were recognized as key elements in productivity, now called industrial humanism . Research methods adapted from the behavioral sciences contributed to scientific studies in industrial management. Traditional theories of the bureaucratic model of organization and management were modified by the behavioral sciences. This led to the emergence of the systems approach, or scientific analysis to analyze complex structures or organizations, taking into account the mutually interdependent elements of activities, interactions, and interpersonal relationships between management and workers.
Some revisits to the Hawthorne studies suggest that the data do not support the conclusions, and offer a different interpretation. One is that informal groups such as workers on a production line themselves set standards for work which assert an informal social control outside the authority system of the organization. The informal cohesive group can thus control the norms of the amount of work acceptable to the group, i.e., not “too much” and not “too little”. Others point out that the effects were temporary and that there were extraneous factors, but the added value of the Hawthorne effect remains part of the history of and had a culture-changing effect on management theory.
The Hawthorne effect in management is in some ways comparable to the placebo effect in clinical research and health care practice. It is also applied to clinical practice, whereby medical care provided by doctors is measured for specific “tracer conditions” to assess completeness of care according to current clinical guidelines. Review of clinical records has been shown to be a factor in improving performance by doctors in practice, such as in treatment of acute myocardial infarction, management of hypertension, or completeness of carrying out preventive procedures such as screening for cancer of the cervix, breast, or colon (see Chapters 3 and 15Chapter 3Chapter 15). Awareness of being studied is a factor in improved performance or response to an intervention. Studies of clinical practice-based research or public health interventions need to consider whether different types of studies and outcomes are more or less susceptible to the Hawthorne effect (Fernald et al., 2012).
Maslow’s Hierarchy of Needs
Abraham Maslow’s hierarchy of human needs made an important contribution to management theory. Maslow (1908–1970) was an American psychologist, considered “the father of humanism” in psychology. Maslow defined a prioritization of human needs ( Figure 12.5 ), starting with those of basic physical survival; at higher levels, human needs include social affiliation, self-esteem, and self-fulfillment. Others in the hierarchy include socialization and self-realization; later revisions include cognitive needs.

Maslow’s hierarchy of needs.
The survival needs of an employee include a base salary and benefits, including health insurance and pension; the safety and security needs include protection from injury, toxic exposure or excess stress; social needs at work include an identity, pride, friendships, union solidarity, company social activities and benefits; esteem and recognition include job titles, awards, and financial rewards for achievement by individuals, groups, or all employees; and self-actualization includes promotion to more challenging jobs with benefits, both financial and in terms of recognition.
This concept is important in terms of management because it identifies human needs beyond those of physical and economic well-being. It relates them to the social context of the work environment with needs of recognition, satisfaction, self-esteem, and self-fulfillment. Maslow’s conclusions opened many positive areas of management research, not only in the motivation of workers in production and service industries, but also in the motivation of consumers.
Maslow’s hierarchy of human needs contributed to the idea that workers’ sense of well-being is important to management. His theories played an important role in application of sociological theory to client behavior, just as the topic of personal lifestyle in health became a central part of public health and clinical management of many conditions, such as in risk factor reduction for cardiovascular diseases. This concept fits well with the epidemiological studies referred to in the Introduction, such as those showing strong relationships with sociopolitical factors as well as socioeconomic conditions.
Theory X –Theory Y
Theory X –Theory Y ( Table 12.1 ), developed by clinical psychologist and professor of management Douglas McGregor in the 1960s, examined two extremes in management assumptions about human nature that ultimately affect the operations of organizations. Organizations with centralized decision-making, a hierarchical pyramid, and external control are based on certain concepts of human nature and motivation. McGregor’s theory, drawing on Maslow’s hierarchy of needs, describes an alternative set of assumptions that credit most people with the capacity for self-direction.
| Theory | Theory |
|---|---|
| Work is inherently distasteful to people | Work is as natural as play in favorable conditions |
| Most people are not ambitious, have little desire for responsibility, and prefer to be directed | Self-control is indispensable in achieving goals |
| Most people have little capacity for creatively solving organizational problems | The capacity for creativity in solving organizational problems is widely distributed in the population |
| Motivation occurs only at physiological and safety levels | Motivation exists at the social, esteem, and self-actualization levels, as well as the physiological and security levels |
| Most people must be closely controlled and often coerced to achieve organizational objectives | People can be self-directed and creative at work if properly encouraged |
Traditional approaches to organization and management stress direction and external control. Theory X assumes that workers are lazy, unambitious, uncreative, and motivated only by basic physiological needs or fear. Theory Y places stress on integration and self-control. This model provides a more optimistic leadership model, emphasizing management development programs and promoting human potential, assuming that, if properly motivated, people can be self-directed and creative at work, and that the role of management is to unleash this potential in workers with performance appraisal. Many other theories of motivation and management have been developed to explain human behavior and how to utilize inherent skills to produce a more creative work environment, reduce resistance to change, reduce unnecessary disputes, and ultimately create a more effective organization.
Variants of the human motivation approach in management carried the concept further by examining industrial organization to determine the effects of management practices on individual behavior and personal growth within the work environment. They describe two contrasting models of workforce motivation. Theory X assumes that management produces immature responses on the part of the worker: passivity, dependence, erratically shallow interests, short-term perspective, subordination, and lack of self-awareness. In contrast, at the other end of the immaturity–maturity spectrum was the mature worker, with an active approach, an independent mind capable of a broad range of responses, deeper and stronger interests, a long-term perspective, and a high level of awareness and self-control. This model has been tested in a variety of industrial settings, showing that giving workers the opportunity to grow and mature on the job helps them to satisfy more than basic survival needs and allows them to use more of their potential in accomplishing organizational goals. This model became widely influential in human resource management theory of organizational behavior, organizational communication, and organizational development, and in the practical management of business and service enterprises.
In The Motivation to Work (1959), US clinical psychologist Frederick Herzberg wrote of his motivation–hygiene theory. He developed this theory after extensive studies of engineers and accountants, examining what he called hygiene factors (i.e., administrative, supervisory, monetary, security, and status issues in work settings). His motivating factors included achievement, recognition of accomplishment, challenging work, and increased responsibility with personal and collective growth and development. He proved that the motivating factors had a substantial positive effect on job satisfaction.
These human resource theories of management helped to change industrial approaches to motivation from “job enrichment” to a more fundamental and deliberate upgrading of responsibility, scope, and challenge of work, by letting workers develop their own ways of achieving objectives. Even when the theories were applied to apparently unskilled workers, such as plant janitors, the workers changed from an apathetic, poorly performing group into a cohesive, productive team, taking pride in their work and appearance. This approach gave members of the team the opportunity to meet their human self-actualization needs by taking greater responsibility for problem solving, and it resulted in less absenteeism, higher morale, and greater productivity with improved quality.
Rensis Likert, with McDougal and Herzberg, helped to pioneer the “Human Relations School” in the 1960s, applying human resource theory to management systems and styles. Likert classified his theory into four different systems, as follows.
- • System 1 – Management has no confidence or trust in subordinates, and avoids involving them in decisions and goal setting, which are made from the top down. Management is task oriented, highly structured, and authoritarian. Fear, punishment, threats, and occasional rewards are the principal methods of motivation. Worker–management interaction is based on fear and mistrust. Informal organizations within the system often develop that lead to passive resistance of management and are destructive to the goals of the formal organization.
- • System 2 – Management has a condescending relationship with subordinates, with some degree of trust and confidence. Most decisions are centralized, but some decentralization is permitted. Rewards and punishments are used for motivation. Informal organizations become more important in the overall structure.
- • System 3 – Management places a greater degree of trust and confidence in subordinates, who are given a greater degree of decision-making powers. Broad policy remains a centralized function.
- • System 4 – Management is seen as having complete confidence in subordinates. Decision-making is dispersed, and communication flows upward, downward, and laterally. Economic rewards are associated with achieving goals and improving methods. Relationships between management and subordinates are frequent and friendly, with a sense of teamwork and a high degree of mutual respect.
Case studies showed that a shift in management from Likert system 1 towards system 4 radically changed the performance of production, cut manufacturing costs, reduced staff turnover, and increased staff morale. Furthermore, workers and managers both shared a concern for the quality of the product or service and the competitiveness and success of their business. The health industry includes highly trained professionals and paraprofessional workers who function as a team with a high degree of cohesion, mutual dependence, and autonomy, such as a surgical or an emergency department team.
Network Organization
The network, or task-oriented working group, is basically a more democratic and participatory form of organization meant to elicit free interchange of concerns and ideas. This is a more organic form of organization, best suited to be effective for adaptation when the environment is complex and dynamic, when the workforce is largely professional, and when the technology and system functions change rapidly. Complexities and technological change require information, expertise, flexibility, and innovation, strengths best promoted in free exchange of ideas in a mutually stimulating environment.
In a network organization, leadership may be formal or informal, assigned to a particular function, which may be temporary, medium term, or permanent, to achieve a single defined task or develop an intersectoral program. The task force is usually for a short-term specific assignment; a working group, often for a medium-term project, such as integrating services of a region; and a committee for permanent tasks such as monitoring an immunization program.
Significant advantages of this form of organization are the challenge and the sharing of information and responsibility, which give professionals responsibility and job satisfaction by providing the opportunity to demonstrate their creativity. Members of the task force may each report within their own pyramidal structure, but as a group they work to achieve the assigned objective. They may also be interdisciplinary or interagency working groups to review the state of the art in this particular issue as documented in reports and professional literature, and to coordinate activities, review previous work, or plan common future activities.
An ongoing network organization may be a government cabinet committee to coordinate government policy and the work of various government departments, or a joint chiefs of staff to coordinate the various armed services. This approach is commonly used for task groups wherein interdisciplinary teams of professionals meet to coordinate functions of a department in a hospital, or where a multidisciplinary group of experts is established with the specified task of a technical nature.
Network organizational activity is part of the regular functions of a health professional. Informal networking is a day-to-day activity of a physician in consultations with colleagues and also a part of more formalized network groups. The hospital department must, to a large extent, function as a network organization with different professionals working as a team more effectively than would be possible in a strictly authoritarian pyramidal model. A ministry of health may need to develop a joint working group with the ministry of transport, the police, and those responsible for standards of motor vehicles to seek ways to reduce road accident deaths and injuries. If a measles eradication project is envisioned, a multidisciplinary and multiorganizational team, or a network, should be established to plan and carry out the complex of tasks needed to achieve the target ( Figure 12.6 ).

Network organization structure.
Note: The letters represent the participation by individuals or organizations as a task group to achieve a defined goal, as set out in terms of reference and a time-frame.
In a public health context, a task group to determine how to reduce obesity rates in school-aged children, or to eradicate measles locally, might be chaired by the deputy chief medical officer or senior health promotion person; if the project is reduction of obesity among school children, the lead agency may be the department of education, perhaps jointly with the local department of health; if reduction in road traffic deaths is the topic, the lead may be the police department with participation of emergency transportation and hospital emergency room lead personnel. Members may include the chief district nurse, an administrative and budget officer, a pharmacist, the chief of the pediatric department of the district hospital, a primary school administrator, a health educator, a medical association representative, the director of laboratories, the director of the supply department, a representative of the department of education, representatives of voluntary organizations interested in the topic, and others as appropriate.
Most organizational structures are mixed, combining elements of both the formal pyramidal and the less structured network structure with a task-oriented mandate. It is often difficult for a rigid pyramidal structure to deal with parallel bodies in a structured way, so the network approach is necessary to establish working relations with outside bodies to achieve common goals. A network is a democratic functional grouping of those professionals and organizations needed to achieve a defined target, sometimes involving people from many different organizations. The terms of reference of the working group are crucial to its function as well as its composition, time-frame, and access to relevant information. The application of this concept is increasingly central in health care organization as multilevel health systems evolve in the form of managed care or district health systems. These are vertically integrated management systems involving highly professional teams and units whose interdependence for patient care and financial responsibility are central elements of the New Public Health.
Total Quality Management
In the USA during World War II, W. Edwards Deming, a physicist and statistician, developed a system of economic and statistical methods of quality control in production industries. Following the war, Deming was invited to teach in Japan and moved from the university to the level of industrial management. Japanese industrialists adopted his principles of management and introduced quality management into all industries, with astonishingly successful results within a decade. The concept, later called total quality management (TQM), has since been adopted widely in production and service industries.
In the Deming approach to company management, quality is the top priority and is the key responsibility of management, not of the workers. If management sets the tone and involves the workers, quality goes up, costs come down, and both customer satisfaction and loyalty increase. Having their ideas listened to, and avoiding a punitive inspection approach, enhances the pride of the workers. It is the responsibility of leadership to remove fear and build mutual participation and common interest. Training is one of the most important investments of the organization. The differences between traditional management and the TQM approach are shown in BOX 12.1 , BOX 12.2 . In societies with growing economies, the role of an educated workforce becomes greater as information technology and services, such as health, become larger parts of the economy and require professionalism and self-motivating workers.
Traditional Management Theory
- • Quality is expensive.
- • Inspection is the key to quality, and control experts and inspectors can assure this.
- • Systems are designed by outside experts – no input is needed from workers.
- • Work standards, quotas, and targets can help productivity.
- • People may be hired when needed and laid off when not needed.
- • Rewards and punishments will lead to greater productivity and creativity.
- • Buy at the lowest cost.
- • Change suppliers frequently, based on price alone.
- • Profits are based on keeping costs down and revenue high.
- • Profit is the most important indicator of a company.
- • Quality leads to lower costs and less waste.
- • Inspection is after the damage is done; worker involvement in quality services eliminates defects.
- • Quality is determined by management.
- • Most defects are caused by the system, not the worker.
- • Eliminate work standards and quotas in industry as sole criteria of performance.
- • Fear leads to disaster.
- • Make workers feel secure in their jobs.
- • Judgment, punishment, and reward for above- or below-average performance destroy teamwork essential for quality production.
- • Work with suppliers to improve quality and costs.
- • Profits are generated by loyal customers – running a company for profit alone is like driving a car by looking in the rearview mirror.
The TQM approach integrates the scientific management and human relations approaches by giving workers credit for intellectual capacity and expects them to use it to analyze and improve the tasks they perform. Even more, this approach expects workers at all levels to contribute to better quality in the process of design, manufacture, and even marketing of the product or the service.
The TQM ideas were revolutionary and successful when applied in business management in production industries. The TQM concept is much in discussion in the service industries. The WHO has adapted TQM to a model called continuous quality improvement (CQI), with the stress on mutual responsibilities throughout a health system for quality of care. The application of TQM and CQI approaches is discussed in Chapter 15, including the external regulatory and self-development TQM approaches.
In the health sector, issues such as prevention of health facility-acquired infections require staff dedicated to promoting a culture of cleaning, frequent and thorough hand washing, sterilization, isolation techniques, intravenous and intratracheal catheter and tube care technique, and immunization of hospital personnel. These and many other cross-disciplinary measures promote patient safety and prevent the costly and frequently deadly effects of serious respiratory or urinary tract injection acquired in hospitals or other health care facilities.
Changing Human Behavior
Human behavior is individual but takes place in a social context. Changes to individual behavior are needed to reduce risk factors for many diseases. Change can be threatening; it requires alteration, substitution, transformation, or modification of purposes, procedures, methods, or style. The implementation of plans usually requires some change, which often meets resistance. The resistance to change may be professional, technical, psychological, political, emotional, or a mix of all of these. The manager of a health facility or service has to cope with change and gather the support of those involved to participate in creating or implementing the change effectively.
The behavior of the worker in a production or service industry is vital to the success of the organization. Equally important is the behavior of the purchaser or consumer of the product or service. Diagnosing organizational problems is an important skill to bring to leadership in health systems. Even more important is the ability to identify and alter the variables that require change and adaptation to improve the performance of the organization. High expectations are essential to produce high performance and improved standards of service or productivity. Conversely, low expectations not only lead to low performance, but produce a downward spiraling effect. This applies not only within the organization, but to the individuals and community served, whether in terms of purchase of goods produced or in terms of health-related behavior.
People often resist change because of fear of the unknown. Participation in the process of defining problems, formulating objectives, and identifying alternatives is needed to bring about changes. Change in organizational performance is complex, and this is the test of leadership. Similarly, change at the individual level is essential to achieve the goals of the group, whether this is in terms of the functioning of a health care service unit, such as a hospital, or whether it is an individual’s decision to change from smoking to non-smoking status. The health of both an individual and a population depends on the individual health team member’s motivation and experience.
The behavior of the individual is important to his or her personal and community health. Even small steps in the direction of a desirable change in behavior should be rewarded as soon as possible (i.e., reinforcing positive performance in increments). Behavior modification is based on the concept that change of behavior starts with the feelings and attitudes within the individual, but can be influenced by knowledge, peer pressure, media coverage, and legislative standards. Change involves a number of elements to define a current or previous starting point:
- • Knowledge – What is the level of adequate health information?
- • Attitudes – What is the person’s perception of that information?
- • Behavior of the individual – What does the individual actually do?
- • Behavior of the group – What are the social norms and acts?
- • Behavior of the organization – What does the health system do to change these factors?
- • Behavior of society – What do legislation, regulations, and enforcement say about harmful acts endangering individuals and the public?
- • Preparation for emergencies – What organizations are in place and organized to meet local or national emergencies, and how are public perception and participation affected by messages from authorities, such as in evacuation of hurricane or tsunami danger zones?
- • Behavior of the media – How do the media convey public health messages and warnings, and how does this affect behavior or responses?
Change in behavior is vital in the health field: in the organization, in the community, in individual behavior, and in societal regulation and norms. The health belief model (Chapter 2) is widely influential in psychology and health promotion. The belief intervention approach involves programs meant to reduce risk factors for a public health problem. It may require change in the law and in organizational behavior, with involvement and feedback to the people who determine policy, those who manage services, and the community being served.
Obesity in school-aged children is being fought by many measures including healthier menus and banning the sale of high sugar drinks on school property. High cholesterol is being fought on many fronts including dietary change and banning the use of transfats in food processing. Deaths from bulimia are not uncommon and may stem from teenage identification of beauty with ultrathin body image. Banning television and modeling agencies from using models with a very low body mass index is an intervention in advertising which encourages harmful practices that are a danger to health and life. Banning cigarette advertising and smoking in public places promotes behavioral change, as does raising the taxes on cigarettes. Gun control laws are meant to prevent disturbed individuals or political fanatics having easy access to firearms to commit mass murder. Strict enforcement of drinking and driving laws can prevent drunk driving and reduce road traffic deaths (see Chapter 15).
Empowerment
In the 1980s, major industries in the USA were unable to compete successfully with the Japanese in the consumer electronics and automobile industries. Management theory began to place greater emphasis on empowerment as a management tool. The TQM approach stresses teamwork and involvement of the worker in order to achieve better quality of production. Comparatively, empowerment went further to involve the worker in operation, quality assessment, and even planning of the design and production process. Results in production industries were remarkable, with increased efficiency, less absenteeism, and greater searching for ideas to improve quality and quantity of production, with the worker as a participant in the management and production process.
The concept of empowerment entered the service industries with the same rationale. The rationale is that improvements in quality and effectiveness of service require the active physical and emotional participation of the worker. Participation in decision-making is the key to empowerment. This requires management to adopt new methods that allow the worker, whether professional or manual, to be an active participant. Successful application of the empowerment principles in health care extends to the patient, the family, and the community, emphasizing patients’ rights to informed participation in decisions affecting their medical care, and the protection of privacy and dignity.
Diffusion of powers occurs when management of services is decentralized. Delegation of powers to professional groups, non-governmental organizations (NGOs), and advocacy organizations is part of empowerment in health care organizations. Governmental powers to govern or promote areas such as licensure, accreditation, training, research, and service can be devolved to local authorities or NGOs by delegation of authority or transfer of funds. Organizational change may involve decentralization. Institutional changes such as amalgamation of hospitals, long-term care facilities, home care programs, day surgery, ambulatory care, and public health services are needed to produce a more effective use of resources. Integration of services under community leadership and management should encourage transfer of funds within a district health network from institutional care to community-based care. Such changes are a test of leadership skills to achieve cultural change within an organization, which requires behavioral change and involvement of health workers in policy and management of the change process.
Strategic Management of Health Systems
Strategic management emphasizes the importance of positioning the organization in its environment in relation to its mission, resources, consumers, and competitors. It requires development of a plan of action or implementation of a strategy to achieve the mission or goal of the organization within acceptable ethical and legal guidelines. Articulation of these is a key role of the management level of an organization. Defining the mission and goals of the organization must take into account the external and internal environment, resources, and operational needs to implement and evaluate the adequacy of the outcomes. The strategy of the organization matches its internal approach with external factors, such as consumer attitudes and competing organizations. Strategy is a set of methods and skills of the health care manager to attain the objectives of a health organization, including:
- • providing high-quality care at current professional standards
- • innovating to avoid obsolescence
- • developing good internal and external professional relationships
- • utilizing human resources effectively
- • ensuring accountability and accreditation within the local and national environment
- • promoting the service to improve market share
- • managing financial, human, and other resources efficiently
- • promoting the public and professional reputation of the institution.
Policy is the formulation of objectives and priorities. Strategy refers to long-range plans to achieve stated objectives, indicating the problems to be expected and how to deal with them. Strategy does not identify all actions to be taken, but it includes evaluation of progress made towards a stated goal. While the term has traditionally been used in a military context, it has become an essential concept in management, whether of industry, business, or health care. Tactics are the methods used to fulfill the strategy. Thus, strategic MBO is applicable to the health system, incorporating definitions of goals and targets, and the methods to achieve them ( Box 12.3 ).
The Strategic Management Process
- (a) Define mission, goals, and objectives.
- (b) Undertake surveillance.
- (c) Analyze external environment.
- (d) Analyze internal environment.
- (e) Assess capabilities.
- (f) Evaluate strategic choices, short-range.
- (g) Develop strategic planning, long-range.
- (h) Guide the implementation process.
- (i) Communicate policy direction.
- (a) Motivate: clearly communicate the goals and plans of the organization.
- (b) Differentiate between short- and long-term goals.
- (c) Ensure that staff understand their responsibilities.
- (d) Ensure provision of adequate resources.
- (e) Promote sense of staff involvement.
- (f) Modify structure to meet needs.
- (g) Delegate authority, assign responsibility.
- (h) Promote interdepartmental coordination and interpersonal relations.
- (i) Promote capacity to deal with change.
- (j) Review policies in keeping with progress towards goals.
- (k) Promote understanding of change and resistance to change.
- (a) Evaluate effectiveness.
- (b) Evaluate outcome, lessons learned.
- (c) Revise strategic plan.
- (d) Redeploy resources in keeping with lessons learned.
Change in health organizations may involve a substantial alteration in the size or relationships between existing, well-established facilities and programs ( Table 12.2 ). A strategic plan for health reform in response to the need for cost containment, redefined health targets, or dissatisfaction with the status quo requires a model or a vision for the future and a well-managed program. Opposition to change may occur for psychological, social, and economic reasons, or because of fear of loss of jobs or changes in assignments, salary, authority, benefits, or status. Downsizing in the hospital sector, with buildup of community health services, is one of the major issues in health reforms in many countries. It can be accomplished over time by naturally occurring vacancies or attrition due to retirement, or by retraining and reassignment, all of which require skilled leadership.
Transformation of Health Care Paradigms
| Old Paradigm | New Paradigm |
|---|---|
| Emphasis on inpatient care | Emphasis on continuum of care |
| Emphasis on treating illness | Emphasis on maintaining and promoting wellness |
| Responsibility for the individual patient | Accountable for defined population |
| Specialists rewarded more than generalists | Greater economic parity between providers |
| Surgery rewarded more than medical services | Prevention rewarded versus surgery |
| Goal to fill beds | Provision of care at appropriate level of care |
| Separate organization, funding of hospital and other services | Integrate health delivery system |
| Managers run an organization or a department | Managers promote market share |
| Managers coordinate services | Managers promote intersectoral cooperation |
The introduction of new categories of health workers in hospitals such as phlebotomists, hospitalist doctors, and technicians of all kinds has improved hospital efficiency and safety. Community health has benefited from home care and in many situations community health workers to assist and supervise patient care in remote rural villages and in urban centers, even in high-income countries, with health guides trained to help people to function with chronic illnesses and dementias (see Chapter 14).
Health System Organization Models
The New Public Health is an integration or coordination of many participating health care facilities and health-promoting programs. It is evolving in various forms in different places as networks with administrative and financial interaction between participating elements. Each organization provides its own specific services or groups of services. How they function internally and how they interact functionally and financially are important aspects of the management and outcomes of health systems. The health system functions as a network with formal and informal relationships; it may be very broad and loosely connected as in a highly decentralized system, with many lines of communication, payment, regulation, standards setting, and levels of authority.
The relationship and interchange between different health care providers have functional and economic elements. As an example, an educated adult woman is more likely than an uneducated woman to prepare herself for the requirements of pregnancy by smoking and alcohol or drug cessation, folic acid intake, healthful diet, and attending professional antenatal care. A pregnant woman who is healthy and prepared for pregnancy physically and emotionally, and who receives comprehensive prenatal care, is less likely than a woman whose health is neglected to develop complications and require prolonged hospital care as a result of childbirth. The cost of good prenatal care is a fraction of the economic cost of treating the potential complications and damage to her health or that of the newborn. A health system is responsible for ensuring that a woman of reproductive age takes folic acid tablets orally before becoming pregnant, has had access to family planning services so that the pregnancy is a desired one, ensures that the space between pregnancies is adequate for her health and that of her baby, and receives adequate prenatal care. An obstetrics department should be involved in assuring or providing the prenatal care, especially for high-risk cases, and delivery should be in hygienic and professionally supervised settings.
Similarly, for children and elderly people, there is a wide range of public health and personal care services that make up an adequate and cost-effective set of services and programs. The economic burden of caring for the sick child falls on the hospital. When there is a per capita grant to a district, the hospital and the primary care service have a mutual interest in reducing morbidity and hence mortality. This is the principle of the HMOs and district health systems discussed elsewhere. It is also a fundamental principle of the New Public Health.
Health care organizations differ according to size, complexity, ownership, affiliations, types of services, and location. Traditionally, a health care organization provides a single type of service, such as an acute care hospital providing episodic inpatient care, or a home health care agency. In present-day health reforms, health care organizations, such as an HMO or a district health system, provide a population-based, comprehensive service program. Each organization must have or develop a structure suited to meet its goals, in both the internal and external environments. The common elements that each organization must deal with include governance of policy, production or service, maintenance, financing, relating to the external environment, and adapting to changing conditions.
Functional Model
A functional model of an organization perhaps best suited to the smaller hospital is the division of labor into specific functional departments; for example, medical, nursing, administration, pharmacy, maintenance, and dietary, each reporting through a single chain of command to the chief executive officer (CEO) ( Figure 12.7 ). The governing agency, which may be a local non-profit board or a national health system, has overall legal responsibility for the operation and financial status of the hospital, as well as raising capital for improvements.

Functional model of organization.
The medical staff may be in private practice and work in the hospital with their own patients by application for this right as “attending physician”, according to their professional qualifications, or the medical staff may be employed by the hospital in a similar way to the rest of the staff. Salaried medical staff may include physicians in administration, pathology, anesthesia, and radiology, so that even in a private practice market system many medical staff members are hospital employees. Increasingly, hospitals are employing “hospitalists”, who are full- or part-time physicians whose work is in the health facility, to provide continuity of inpatient and emergency department services, augmenting the services of senior or attending staff or private practice physicians. This shift is in part related to the increasing numbers of female physicians who run their homes and families as well as practice medicine and who find this mode of work more attractive than full-time private practice.
This model is the common arrangement in North American hospitals. The governing board of a “voluntary”, non-governmental, not-for-profit organization with municipal and community representatives may be appointed by a sponsoring religious, municipal, or fraternal organization.
Corporate Model
The corporate model in health care organization ( Figure 12.8 ) is often used in larger hospitals or where mergers with other hospitals or health facilities are taking place. The CEO delegates responsibility to other members of the senior management team who have operational responsibility for major sectors of the hospital’s functioning.

Corporate model of health care organization.
A variation of the corporate model is the divisional model of a health care organization based on the individual service divisions allowing middle management a high degree of autonomy ( Figure 12.9 ). There is often departmental budgeting for each service, which operates as an economic unit; that is, balancing income and expenditures. Each division is responsible for its own performance, with powers of strategic and operational decision-making authority. This model is used widely in private corporations, and in many hospitals in the USA. With increasing complexity of services, it is also employed in corporate health systems in the USA, with regional divisions.

Divisional model of health care organization.
Matrix Model
The matrix model of a health care organization is based on a combination of pyramidal and network organization. This model is suited to a public health department in a state, county, or city. Individual staff people report in the pyramidal chain of command, but also function in multidisciplinary teams to work on specific programs or projects. A nutritionist in the geriatric department is responsible to the chief of nutrition services but is functionally a member of the team on the geriatric unit. In a laterally integrated health maintenance organization or district health system, specialized staff may serve in both institutional (i.e., hospital) and community health roles ( Figure 12.10 ).

Matrix model of health care organization.
The organizational structure appropriate to one set of circumstances may not be suitable for all. Whether the payment system is by norm (i.e., by predetermined numbers of staff, their salaries, and fixed costs for all services), per diem (i.e., payment of a daily rate times the number of days of stay), historical budget, or per capita in a regional or district health system structure (see Chapters 10 and 11Chapter 10Chapter 11), the internal operation of a hospital will require a model of organization appropriate to it. Hospitals need to modify their organizational structure as they evolve, and as the economics of health care change.
Skills for Management
Leadership in an organization requires the ability to define the goals or mission of the organization and to develop a strategy and define steps needed to achieve these goals. It requires an ability to motivate and engender enthusiasm for this vision by working with others to gain their ideas, their support, and their participation in the effort. In health care as in other organizations, it is easier to formulate plans than to implement them. Change requires the ability not only to formulate the concept of change, but also to modify the organizational structure, the budgeted resources, the operational policies and, perhaps most importantly, the corporate culture of the organization.
Management involves skills that are not automatically part of a health professional’s training. Skilled clinicians often move into positions requiring management skills in order to build and develop the health care infrastructure. In some countries, hospital managers must be physicians, often senior surgeons. Clinical capability does not transfer automatically into management skills to deal with personnel, budgets, and resources. Therefore, training in management is vital for the health professional.
The manager needs training for investigations and fact-finding as well as the ability to evaluate personnel, programs, and issues, and set priorities for dealing with the short- and long-term issues. Negotiating with staff and outside agencies is a constant activity of the manager, ranging from the trivial to major decisions with wide implications. Perhaps the most crucial skill of the manager is communication: the ability to convey verbal, written, or unwritten messages that are received and understood and to assess the responses as an equal part of the exchange.
Interpersonal skills are a part of management practice. The capable manager can relate to personnel at all levels in an open and equal manner. This skill is essential to help foster a sense of pride and involvement of all personnel in working towards the same goals and objectives, and to show that each member of the team is important to meeting the objectives of the organization. At the same time, the manager needs to communicate information, especially as to how the organization is doing in achieving its objectives.
The manager is responsible for organizing, planning, controlling, directing, and motivating. Managers assume multiple roles. A role is an organized set of behaviors. Henry Mintzberg described the roles needed by all managers: informational, interpersonal, and decisional roles. Robert Katz (1974) identified three managerial skills that are essential to successful management: technical, human, and conceptual: “Technical skill involves process or technique knowledge and proficiency. Managers use the processes, techniques and tools of a specific area. Human skill involves the ability to interact effectively with people. Managers interact and cooperate with employees. Conceptual skill involves the formulation of ideas. Managers understand abstract relationships, develop ideas, and solve problems creatively”. Technical skill deals with things, human skill concerns people, and conceptual skill has to do with ideas. The distribution of these skills between the levels of management is shown in Figure 12.11 .

Distribution of skills within an organization.
The Chief Executive Officer of Health Organizations
Hospital directors in the past were often senior physicians, often called superintendents , without training in health management. The business manager CEO has become common in hospital management in the USA. During the 1950s, the CEO was called an administrator , and worked under the direction of a board of trustees who raised funds, set policies, and were often involved in internal administration.
Where the CEO was a non-physician, the usual case in North American hospitals, a conflict often existed with the clinical staff of the hospital. In some settings, this led to appointment of a parallel structure with a full-time chief of medical staff with a focus on clinical and qualitative matters. In European hospitals, the CEO is usually a physician, often by law, and the integration of the management function with the role of clinical chief is the prevalent model.
Over time, as the cost and complexity of the health system have increased, the CEO role has changed to one of a “coordinator”. The CEO is now more involved in external relations and less in the day-to-day operation of the facility. The CEO is a leader/partner but primus inter pares , or first among equals, in a management team that shares information and works to define objectives and solve problems. This de-emphasizes the authoritarian role and stresses the integrative function.
The CEO is responsible for the financial management of operational and capital budgets of the facility, which is integral to the planning and future development of the facility. Budgets include four main factors: income, fixed or regular overhead, variable or unpredictable overhead, and capital or development costs, all essential to the survival and development of the organization.
The key role of top management is to develop a vision, goals, and targets for the institution, to maintain an atmosphere and systems to promote the quality of care, financial solidity, and to represent the institution to the public. The overall responsibility for the function and well-being of the program is with the CEO and the governing board of directors.
Community Participation
Community participation in management of health facilities has a long-standing and constructive tradition. The traditional hospital board has served as a mechanism for community participation and leadership in promoting health facility development and management at the community level. The role of hospital boards evolved from primarily a philanthropic and fund-raising one to a greater overall responsibility for policy and planning function working closely with management and senior professional staff. This change occurred as operational costs increased rapidly, as government insurance schemes were implemented, and as court decisions defined the liability of hospitals and reinforced the broadened role of governing boards in malpractice cases and quality assurance. Centrally developed health systems such as the UK’s NHS have promoted district and county health systems with high degrees of community participation and management, both at the district level and for services or facilities.
The role of local authorities, as well as state and national governments, is crucial to the functioning of public health in its traditional issues such as safe water supply, sanitation, business licensing, social welfare, and many others, as discussed in Chapter 10. These functions have not diminished with the greater roles of state and federal or national governments in health. In healthful living environments the local authority functions are of continuing and indeed expanding importance, as in urban planning and transportation, promoting easy access to commercial facilities for shopping and healthy food sources for poorer sections as well as those available to prosperous members of the community.
Advocacy has always been an important part of public health. An illustration of this is seen in Box 12.4 in changing the law banning birth control in Massachusetts in the 1960s. The issue of birth control still casts a heavy burden on women globally owing to religious objections, so this example from the 1960s is still relevant as a political issue both in the USA and in many other countries.
Changing the Law Banning Birth Control in Massachusetts: The Role of Advocacy
In 1942 and 1948, referenda were held on a Massachusetts law which banned dissemination of birth control devices and information; both were defeated. Massachusetts and Connecticut alone of all the states continued to ban birth control. But with the advent of the birth control pill in the 1960s, the issue was reopened. Richard Cardinal Cushing, head of the Archdiocese of Boston, no longer opposed a change in the state law, although still opposed the practice of birth control.
Some Catholic doctors, including Dr John Rock, the gynecologist who conducted the key clinical studies of the birth control pill, favored a change in the law. An article published by a young Catholic doctor, later specializing in public health, in the prestigious New England Journal of Medicine in 1964, called for changing the Massachusetts birth control law. This drew the ire of some of the hierarchy of the Church.
However, the article served to stimulate the Legislature to revisit the law, leading to its repeal in 1966, thus allowing use of all methods of birth control. The controversy subsided and women were free to control their own fertility as a result of this advocacy.
Community participation can be crucial to the success of an intervention to promote community health. Sensitivity to local, religious, or ethnic concerns is part of planning any study or intervention in public health. This does not mean that the national, state, and local health authorities must continuously canvass public opinion, but there is advantage in holding referenda on some issues compared to governmental fiat. The USA has higher rates of fluoridation than most countries, and this is implemented after referenda in each municipality (see Chapter 7). In Portland, Oregon, the City Council profluoridation vote in 2012 ( New York Times , 12 September 2012) was later rejected in the public referendum. Portland is the only major American city without fluoridation ( Portland Tribune , 21 May 2013).
Integration: Lateral and Vertical
Rationalization of health facilities increasingly means organizational linkages between previously independent facilities. Mergers of health facilities are common events in many health systems. In the USA, there are frequent mergers between hospitals, or between facilities linked to HMOs or managed care systems. Health reform in many countries is based on similar linkages. Governmental approval and alteration to financing systems are needed to promote linkages between services to achieve greater efficiency and improve patient care (see Chapters 10 and 11Chapter 10Chapter 11).
Lateral integration is the term used for amalgamation among similar facilities. Like a chain of hotels, in health care this involves two or more hospitals, usually meant to achieve cost savings, improve financing and efficiency, and reduce duplication of services. Urban hospitals, both not-for-profit as well as for-profit, often respond to competition by purchasing or amalgamating with other hospitals to increase market share in competitive environments. This is often easier for hospital-oriented CEOs and staff to comprehend and manage, but it avoids the issues of downsizing and integration with community-based services.
Vertical integration describes organizational linkages between different kinds of health care facilities to form integrated, comprehensive health service networks. This permits a shift of emphasis and resources from inpatient care to long-term, home, and ambulatory care, and is known as the managed care or district health system model. Community interest is a factor in promoting change to integrate services, which can be a major change for the management culture, especially of the hospital.
The survival of a health care facility may depend on integration with appropriate changes in concepts of management. In the 1990s, a large majority of California residents moved to managed care programs because of the high cost of fee-for-service indemnity health insurance and because of federal waivers to promote managed care for Medicare and Medicaid beneficiaries. Independent community hospitals without a strong connection to managed care organizations (MCOs) were in danger of losing their financial base.
Hospital bed supplies were reduced in the USA from 4.5 beds per 1000 population in 1980 to 2.9 in 2000 and 2.6 in 2009. Occupancy rates also fell, from 75 percent in 1980 to 64 percent in 2000 and rose slightly to 66 percent in 2009. Hospital discharges also fell during these years, from 173 per 1000 population in 1980 to 113 in 2005 and 112 in 2007, while days of care fell from 1297 to 558 and 540, respectively (Health United States, 2011). These data are monitored by the National Hospital Discharge Survey and the Centers for Disease Control and Prevention’s (CDC’s) National Center for Health Statistics. The lower hospital bed supply and utilization since the 1980s and 1990s reflect the adoption of insurance system payments by diagnosis-related group (DRG), rather than on a per diem basis. Similar trends are seen in European countries, although in the Commonwealth of Independent States the number of hospital beds declined between 1990 and 2005-2011 but stabilized at high and inefficient levels (8 beds per 1000 population) compared to the number in Western Europe, which fell from 5 beds per 1000 in 1990 to 3.4 in 2011, and in some countries to 2 per 1000 population despite increased longevity and aging of the population.
There was a shift to stronger ambulatory care, as occurred throughout the industrialized countries despite an aging of the population. These trends were largely due to greater emphasis on ambulatory surgery and other care, and major medical centers responded with strategic plans to purchase community hospitals and develop affiliated medical groups and contract relationships with managed care organizations to strengthen their “market share” service population base for the future. The new payment environment and managed care also promoted hospital mergers (lateral integration) and linkages between different levels of service, such as teaching hospitals with community hospitals and primary community care services (vertical integration).
Vertical integration not only is important in urban areas, but can serve as a basis for developing rural health care in both developed and developing countries. The district hospital and primary care center operating as an integrated program can provide a high-quality program. Hospital-centered health care, common in industrialized countries, has traditionally channeled a high percentage of total health expenditures into hospital services. Over recent years, there has been a reduction in hospital bed supply in most industrialized countries, with shorter length of stay, more emphasis on ambulatory care, improved diagnostic facilities, and improved outcomes of care (see Chapter 3).
Expenditures on the hospital component of care have come down to between 40 and 45 percent of total health expenditures in many countries, with a growing proportion going to ambulatory and primary care, and increased percentages to public health. This shift in priorities has been an evolutionary process that will continue, but requires skilled management leadership, grounded in health systems management training and epidemiological knowledge, and skilled negotiating skills to foster primary care and health promotion approaches both within the organization and in relation to outside services, especially preventive services. This shift in policy direction will be fostered in implementation of the PPACA (Obamacare), discussed in Chapters 10 and 13Chapter 10Chapter 13. Managed care systems or accountable care organizations (ACOs) will integrate hospital and community care and try to limit hospital care by strengthening ambulatory and primary care, and especially preventive care. This will have both economic and epidemiological benefits, but will depend on skilled management to understand and lead in their implementation.
Much of the rationale for these changes is discussed in the literature and summarized in a 2012 report from the US Institute of Medicine, entitled “Best care at lower cost”. This report calls for overhauling the health system in a continuous evolution based on evidence and lessons learned from decades of innovative care systems and research into their workings. The health system needs to relate to other community services with a shared population orientation ( Institute of Medicine, 2012 ).
Norms and Performance Indicators
Norms are useful to promote efficient use of resources and promote high standards of care, if based on empirical standards proved by experience, trial and error, and scientific observation. Norms may be needed even without adequate evidence, but should be tested in the reality of observation, experience, and experiment. This process requires data for selected health indicators and trained observers free to examine, report, and publish their findings for open discussion among colleagues and peers in proceedings open to the media and the general public.
Normative standards of planning are the determination of a number per unit of population that is deemed to be suitable for population needs; for example, the number of beds or doctors per 1000 population or length of stay in hospital. Many organizations based on the bureaucratic model used norms as the basis for planning and allocation of resources including funding (see Chapter 11). This led to payment systems which encouraged greater use of that resource. If a factory is paid by the number of workers and not the number and quality of the cars produced, then management will have no incentive to introduce efficiency or quality improvement measures. If a district or a hospital is paid by the number of beds, or by days of care in the hospital, there is no incentive to introduce alternative services such as same-day or outpatient surgery and home care.
Performance indicators are measures of completion of specific functions of preventive care such as immunization, mammography, Pap smears, and diabetes and hypertension screening. They are indirect measures of economy, efficiency, and effectiveness of a service and are being adopted as better methods of monitoring and paying for a service, such as by paying a premium. General practitioners in the UK receive additional payments for full immunization coverage of the children registered in their practices. A block grant or per capita sum may be tied to indicators that reflect good standards of care or prevention, such as low infant, child, and maternal mortality. Incentive payments to hospitals can promote ambulatory services as alternatives to admissions and reduce lengths of stay. Limitations of financial resources in the industrialized countries and even more so in the developing countries make the use of appropriate performance indicators of great importance in the management of resources.
Pay-for-performance is a system of paying for health services developed in the UK for paying general practitioners, with apparently satisfactory results. It is now widely used in the USA. It is defined as “a strategy to improve health care delivery that relies on the use of market or purchaser power. Agency for Healthcare Research and Quality (AHRQ) Resources on Pay for Performance (P4P), depending on the context, refers to financial incentives that reward providers for the achievement of a range of payer objectives, including delivery efficiencies, submission of data and measures to payer, and improved quality and patient safety” ( Agency for Healthcare Research and Quality, 2012 ). More than half of commercial HMOs are using pay-for-performance. Recent legislation requires the Medicare and Medicaid programs to adopt this approach for beneficiaries and providers. As commercial programs have evolved during the past 5 years, the categories of providers (clinicians, hospitals, and other health care facilities), number of measures, and dollar amounts at risk have increased. This method of payment is likely to be promoted in the Affordable Care Act implementation to improve quality and control cost increases in US health care (see Chapters 10, 11, and 13Chapter 10Chapter 11Chapter 13). Pay-for-performance has also been adopted in other countries trying to improve quality of care, such as Macedonia (Lazarevik and Kasapinov, 2012).
Health Promotion and Advocacy
Social marketing is the systematic application of marketing alongside other concepts and techniques to achieve specific behavioral goals for a social good. Initially focused on commercial goals in the 1970s, the concept became part of health promotion activities to address health issues where there was no current biomedical approach, such as in smoking reduction and in safe sex practices to prevent the spread of HIV.
Social marketing was based initially on commercial marketing techniques but now integrates a full range of social sciences and social policy approaches using the strong customer understanding and insight approach to inform and guide effective policy and strategy development. It has become part of public health practice and policy setting to achieve both strategic and operational targets. A classic example of the success is seen with tobacco reduction strategies in many countries using education, taxation, and legislative restrictions. Other challenges in this field include risk behavior such as alcohol abuse through binge drinking, unsafe sex practices, and dietary practices harmful to health.
Philanthropy and Volunteerism
Philanthropy and volunteerism have long been important elements of health systems through building hospitals, mission houses, and food provision, and other prototype initiatives on a demonstration basis. This approach has been instrumental in such areas as improved care and prevention of HIV, immunization in underdeveloped countries, global health strategies, and maternal and child health services.
During the late twentieth and early twenty-first centuries, a new “social entrepreneurship” was initiated and developed by prominent reform-minded former US President Bill Clinton, Microsoft’s Bill Gates, and the Open Society Institute of George Soros. The Rotary Club International has been a major factor in funding and promoting the global campaign to eradicate poliomyelitis. This has promoted integration and consortia for the promotion of acquired immunodeficiency syndrome (AIDS) prevention and malaria control in many developing countries. The Global Alliance for Vaccine and Immunization (GAVI) is a US-based organization which links international public and private organizations and resources to extend access to immunization globally. It includes the United Nations Children’s Fund (UNICEF), WHO, bilateral donor countries, the vaccine industry, the Gates Foundation, and other major donors. GAVI has made an important contribution to advancing vaccine coverage and adding important new vaccines in many developing countries and regions. These organizations focus funds and activities on promoting improved care and prevention of HIV, tuberculosis, and malaria, along with improved vaccination for children, reproductive health, global health strategies, technologies, and advocacy. These programs generate publicity and raise consciousness at political levels where resource allocations are made. A central feature of these programs is the promotion of “civil society” as active partners in a globalized world of free trade, democracy, and peace.
Specific initiatives included promoting improved large-scale marketing of antiretroviral drugs for the treatment of HIV infection, including price reduction so that developing countries can offer antiretroviral treatment, especially to reduce mother-to-infant transmission. Programs have branched out into the distribution of malaria-preventing bed nets, provision of low-cost pharmaceuticals, marketing drugs for the poor, desalination plants, solar roof units, low-cost small loans, and cell phones, mainly in Africa.
Another form of social entrepreneurship that has gained support in the private sector is proactiveness in environmental consciousness to address issues raised by the environmental movement, and public interest for environmental accountability. The automobile industry is facing both public concern and federal legal mandates for improved gas mileage as opposed to public demand for larger cars. Hybrid cars using less fuel have been successfully introduced into the market for low-emission, fuel-efficient cars, and electric cars are gradually entering the field. Public opinion is showing signs of moving towards promoting environmentally friendly design, marketing, and purchasing practices in energy consumption, conservation practices, and public policy. Public opinion and the price of fuel will play a major part in driving governments to legislate energy and conservation policies to address global warming and damage to the environment, with their many negative health consequences. However, such changes must work with public opinion because of the sensitivity of consumers to the price of fuel. In addition, when food crops, such as corn, are used to produce ethanol for energy to replace oil, then food prices rise and consumers suffer and respond vigorously.
Corporations adopt policies of environmental responsibility in part because of public relations and partly because of potential liability claims. Much of the planning and financial costs of offshore petroleum and gas drilling is spent on safety measures to protect the environment. The explosion in 2010 at a British Petroleum site in the Gulf of Mexico, off the coast of Texas and Louisiana, caused massive pollution and environmental damage, and resulted in the US government being awarded US$4.5 billion against BP for cleanup and damages. The reputation of the corporation suffered and some executive officers lost their positions. Thus, corporate social responsibility can be seen as self-interest.
New Organizational Models
New models of health care organization are emerging and developing rapidly in many countries. This is partly a result of a search for more economical methods of delivering health care and partly the result of the target-oriented approach to health planning that seeks the best way to define and achieve health objectives. The developed countries seek ways to restrain cost increases, and the developing countries seek effective ways to quickly and inexpensively raise health standards for their populations. New organizational models that try to meet these objectives include district health systems, managed care organizations (MCOs) and accountable care organizations (ACOs), described in greater detail in Chapter 11. Critical and basic elements of a health system organization are shown in Figure 12.12 .

Basic elements of an organizational system.
New Projects and their Evaluation
New initiatives are part of the growth and development of any organization or health service system, as needs, technologies, resources, and public demand change. Identification of issues and decisions to launch new endeavors or projects to advance the state of the art, to address unmet needs, or to meet competition are part of organizational responsibility, in the public sector to meet needs, and in the private sector to remain competitive.
In developing and developed countries, many NGOs provide funding from abroad for essential services that a government may be unable to provide. Such projects focus on issues directed from the head offices in the USA or Europe of the funding source or management offices for specific vertical programs which are often not fully integrated with national priorities and programs. However, these need coordination and approval by the local national government agency responsible for that sector of public service. New projects run by NGOs may run in parallel to each other, or to state health services as uncoordinated activities. Governmental public health agencies have responsibility for oversight of health systems and can play a leadership and regulatory role in coordinating activities and directing new programs to areas of greatest national need.
The public health agency may also seek funding to launch new pilot or specific needs programs. The agency may introduce a new vaccine into a routine immunization program in phases, pending government approval and funding to incorporate it as a routine immunization program based on evaluation of the initial phase. An example is the introduction of Haemophilus influenzae type b vaccine in Albania in 2006, which was funded by GAVI for 5 years based on a study and proposal including a cost-effectiveness study (Bino S, Ginsberg G, personal communication, 2007).
Proposals for health projects by NGOs or private agencies need to be prepared in keeping with the vision, mission, and objectives of the responsible governmental agency, with ethics review and community participation. A project proposal should include why the project is important, its specific goals and objectives, available or new resources, and the time-frame required to achieve success ( Box 12.5 ). It should describe the means proposed to accomplish the goals, and how the proposed program will impact the community, providing recommendations for follow-up and/or further action.
Program Evaluation Information Needs
The following utility standards ensure that an evaluation will serve the information needs of intended users:
- • Identify and engage stakeholders, including relevant government agencies, people or communities involved in or affected by the evaluation, so that their needs and concerns can be addressed.
- • Develop and describe the program.
- • Focus the evaluation design with ethical standards and review requirements respected.
- • Gather credible evidence – The people conducting the evaluation should be trustworthy and competent in performing the evaluation for findings to achieve maximum credibility and acceptance. Information collected should address pertinent questions regarding the program and be responsive to the needs and interests of clients and other specified stakeholders.
- • Justify the conclusions – The perspectives, procedures, and rationale used to interpret the findings should be carefully described so that the bases for value judgments are clear.
- • Ensure sharing and use of information and lessons learned – Evaluation reports should clearly describe the program being evaluated, including its context and the purposes, procedures, and findings of the evaluation so that essential information is provided and easily understood. Substantial interim findings and evaluation reports should be disseminated to intended users so that they can be used in a timely fashion to encourage follow-through by stakeholders, to increase the likelihood of the evaluation being used.
- • Standards of a project should focus on scientific justification, utility, feasibility, propriety, and accuracy.
- – direct service interventions
- – community mobilization efforts
- – research initiatives
- – surveillance systems
- – policy development activities
- – outbreak investigations
- – laboratory diagnostics
- – communication campaigns
- – infrastructure building projects
- – training and education services
- – administrative systems and others.
The introduction of the project proposal outlines the current state of the problem and the case for action. It should describe existing programs which address that issue, with proposed collaboration, and expansion or improvement of programs, but avoiding duplication of services. Background information needs to relate the project to the priorities of the prospective funding organization. The objectives should follow the acronym “SMART”: specific, measurable, achievable, relevant, and time-based. This term, originally used for computer disc self-management, has been adapted as a current form of MBO from the 1950s and 1960s.
The project objectives should be feasible and the expected results of the project should be based on the stated objectives. The funding organization will want to know what will be the expected product of the program in measurable process (e.g., immunization coverage) or outcome indicators (e.g., reduced child mortality). Projections will be based on the intended activities and known outcomes of other past programs with similar goals in the same or other countries (environmental scan), and should be supported by a review of local and international literature on the topic. The activities section of a proposal should include a timeline of the intended actions and a description of activities based on best practices. The expected outcomes, monitoring and evaluation, and justification are all part of the presentation ( Box 12.6 ).
Project Proposal Summary
- • Title page – Name of project; principal people and implementing organizations; contact person(s); time-frame; country (state, region); target group of project; estimated project cost; date of submission.
- • Introduction – Provides project background including the health issue(s) to be addressed, a situational analysis of the health problem, the at-risk and target populations, and existing programs in the community; includes an international and national literature review of the topic with references.
- • Aim of the project – Intended accomplishment of the project; what will be evaluated (i.e., what is “the program” and in what context does it exist?); what aspects of the program and evidence will be used to indicate how the program has performed?
- • Objectives – Specific, measurable, achievable, relevant, and time-based (SMART).
- • Expected results – Based on the objectives: what will be produced and delivered.
- • Activities – Actions and time-frame in keeping with the objectives and expected results.
- • Work plan – Timeline of all activities, including preparation, training, pilot, and implementation stages.
- • Budget – Estimated cost of expenditures, including human resources, activities, running costs, and overheads for project and evaluation.
- • Monitoring and evaluation – What evidence will be used to indicate how the program has performed? What plan is recommended for periodic follow-up of project activities (including timeline and measures) to implement lessons learned from positive or negative outcomes, and use of resources? How efficient and effective is the project?
- • Conclusions – What conclusions regarding program performance may be drawn? What conclusions regarding program performance are justified by comparing the available evidence to the selected standards?
- • Reporting – Report the project to the key stakeholders and public bodies; publication in peer-reviewed journal if possible.
- • Justification – Why is this project important and timely, and how will implementation benefit health of the community?
The proposed funding agency expects convincing evidence of how this program will be effective, efficient, practical, and realistic. This information is presented in the activities section, which also needs to address the resources that will be needed to implement the program such as the budget for staff, supervison, training, management, materials (vaccines, syringes, equipment, ongoing supplies and others), transportation, and costs of premises. After completing the activities section, a realistic and achievable work plan and time-frame are required.
Well-planned projects have monitoring and evaluation criteria. Monitoring follows the performance of the program, documenting successes, failures, and lessons learned, as well as expenditures. Evaluation guidelines of the program define the methods used to assess the impact of the project and whether the project was carried out in an effective and efficient manner, and may be required periodically throughout the life of the project.
The most difficult issue is sustainability. A project funded by an NGO is usually time limited to 3–4 years and the survival of the program usually depends on its acceptability and the capacity of government to continue it. Thus, evaluation becomes even more crucial for the follow-up of even successful short-term projects. Harm reduction programs include tackling HIV in drug users, reducing maternal–child HIV transmission, tobacco control programs, and reducing levels of obesity in schoolchildren. Sustainability and diffusion of positive findings to wider application are important challenges, especially to global health. Even in high-income countries, diffusion of best practices is often slow and fraught with controversy and inertia. Examples of this slow or non-diffusion of evidence-based public health include the failure of most European countries to harmonize salt fortification with iodine or total indifference to flour fortification with folic acid to prevent neural tube defects (see Chapters 6 and 8Chapter 6Chapter 8).
Public health work within departments or ministries of health or local health authorities operates at a disadvantage in comparison with other health activities, especially hospitals, pharmaceuticals, diagnostics, and medical care. The competition for resources in a centrally funded system is intense, and the political and bureaucratic battles for funds may pit new immunization agents or health promotion programs against new cancer treatment drugs or scanners, and this is very often a difficult struggle. The presentation of program proposals for new public health interventions requires skill, professionalism, good timing, and the help of informed public and professional opinion. Allocation of resources is decided at the political level in a tax-based universal system, while even in a social security (Bismarckian) system where funding is through an employee–employer payroll deduction, additional funding from government is essential to keep up with the continuing flow of new modalities of treatment or prevention.
Public health is handicapped in portraying the costs and benefits of important interventions, leaving new programs with insufficient resources, including the staffing and administrative costs (e.g., office space, phone service, transportation costs), which are essential parts of any public health program. Portraying the cost of the new proposed program should be based on the total population served, not just the specific target population for a new program; that is, it should be represented as a per capita cost. Similarly, projected benefits should extrapolate the results from other areas, such as pandemic or avian flu or severe acute respiratory syndrome (SARS), and the likely impact on the target geographic area and its population.
Competencies in Health Policy and Management
Public health has prime responsibility for monitoring the health status of the population as well as in preventing infectious and non-communicable diseases and injuries, preparing for disasters, and many other functions. This role requires an adequate multidisciplinary workforce with high levels of competencies. This topic is discussed extensively in Chapter 14.
Canada’s experience with the SARS epidemic in 2003 led to a reappraisal of public health preparedness and standards. This, in turn, led to the establishment of the national Public Health Agency of Canada, which is mandated to develop standards and practices to raise the quality of public health in the country and especially to prepare for possible pandemics. The Agency issued standards of competency for public health personnel and fostered the development of regional laboratories, and schools of public health were developed across Canada. Core competencies for program planning implementation and evaluation are seen in Box 12.7 .
Core Competencies for Program Planning, Implementation and Evaluation
Core competencies are essential knowledge, skills, and attitudes necessary for the practice of public health. They transcend the boundaries of specific disciplines and are independent of program and topic. They are the building blocks for effective public health practice, and the use of an overall public health approach.
Generic core competencies provide a baseline for what is required to fulfill public health system core functions. These include population health assessment, surveillance, disease and injury prevention, health promotion, and health protection.
The core competencies are needed to effectively choose options, and to plan, implement, and evaluate policies and/or programs in public health, including the management of incidents such as outbreaks and emergencies.
A public health practitioner is able to:
- • describe selected policy and program options to address a specific public health issue
- • describe the implications of each option, especially as they apply to the determinants of health and recommend or decide on a course of action
- • develop a plan to implement a course of action taking into account relevant evidence, legislation, emergency planning procedures, regulations, and policies
- • implement a policy or program and/or take appropriate action to address a specific public health issue
- • demonstrate the ability to implement effective practice guidelines
- • evaluate an action, a policy, or a program
- • demonstrate an ability to set and follow priorities, to maximize outcomes based on available resources
- • demonstrate the ability to fulfill functional roles in response to a public health emergency.
Health care systems throughout the world are being scrutinized because of their growing costs in relation to national wealth. At the same time, techniques for evaluating health care with respect to appropriateness, quality, and resource allocation are being developed. These techniques are multifactorial since they must relate to all aspects of health care, including the characteristics of the population being served; available health care resources; measures of the process and utilization of care; measures of health care outcomes; peer review, including quality assessment of health care providers; consumer attitudes, knowledge, and compliance; care provided for “tracer” or sample conditions; and economic cost–benefit studies.
Evaluation in health care assumes that a health care system and the providers of health care within that system are responsible and accountable for the health status of the population. It must, however, recognize that health services are not the sole determinants of health status; social, economic, and cultural factors also play key roles. A comprehensive approach to evaluation in health care is described in Chapter 3. Many of the components that are available in health care systems exist, while others that remain to be developed are discussed. Evaluation is an integral part of a comprehensive health care system, in that the components of evaluation must be built into any national system. As long as rationality is expected of health care, evaluation is an essential element of the overall system (Tulchinsky, 1982) (see Chapter 3).
Systems Approach and National Planning
The purpose of management in health is the improvement of health, and not merely the maintenance of an institution. Separate management of a variety of health facilities serving a community has derived from different historical development and funding systems. In competition for public attention and political support, public health suffers in comparison to hospitals, new technology and drugs, and other competitors for limited resources. The experience of successes in reducing mortality from both non-infectious and infectious conditions comes largely from public health interventions. Medical care is also an essential part of public health, so that management and resource allocation within the total health sector are interactive and mutually dependent. The New Public Health looks at all services as part of a network of interdependent services, each contributing to health needs, whether in hospital care or in enforcing public health law regarding; for example, motor vehicle safety and smoking restriction in public places.
Separate management and budgeting of a complex of services results in disproportionate funds, staff, and attention being directed towards high-cost services such as hospitals, and fails to redirect resources to more cost-effective and patient-sensitive kinds of services, such as home and preventive care. However, reducing the supply of hospital beds and implementing payment systems with resources for early diagnosis and incentives for short stays have changed this situation quite dramatically in recent decades. The effects of incentives and disincentives built into funding systems are central issues in determining how management approaches problem solving and program planning, and are therefore important considerations in promoting health.
The management approach to resolving this dilemma is professional vision and leadership to promote the broader New Public Health. Thus, managers of hospitals and other health facilities need broad-based training in a New Public Health in order to understand the interrelationships of services, funding, and population health. Managers who continue to work with an obsolescent paradigm with the traditional emphasis, regardless of the larger picture, may find the hospital non-competitive in a new climate where economic incentives promote downsizing institutions and upgrading health promotion. Defensive, internalized management will become obsolete, while forward-looking management will be the pioneers of the New Public Health. This may be seen as a systems approach to improve population and individual health, based on strategic planning for immediate needs and adaptation of health systems in the longer term issues in health.
Examples of national planning that cut across health and social services include national insurance policies and the provision of new services to meet rising needs, as shown for Alzheimer’s disease, in France since 2001 ( Box 12.8 ) and in the USA since 2011 ( Box 12.9 ).
France – National Dementia Plans 2001–2012
First national dementia plan 2001–2005.
An estimated 600,000 French people lived with dementia; half were diagnosed and one-third were receiving treatment; 75 percent of people with Alzheimer’s disease were living at home; 50 percent of all nursing home residents lived with some form of dementia; a day’s care cost 荤60 while full-time residency in a nursing home ranged between 荤3000 and 荤4600.
- • Identify the early symptoms of dementia and refer people to specialists.
- • Create a network of “memory centers” to enable earlier diagnosis.
- • Produce ethical guidelines for families and care homes.
- • Provide financial support for people with dementia.
- • Establish day care centers and create local dementia information centers.
- • Build new residential care homes and improve existing homes.
- • Provide support for research and clinical studies.
Second Alzheimer Plan 2005–2007
By 2004 nearly 800,000 French people lived with dementia; a growing proportion of women and 18 percent of all people over 75; over 165,000 new cases of dementia diagnosed annually with an associated life expectancy of 8 years; Alzheimer’s disease now recognized as a chronic disease by the French social security system, with the need for continuing support.
- • Eligibility of dementia for 100 percent insurance coverage.
- • Identify and support the needs of younger people with dementia.
- • Provide training and support to professional and volunteer workers.
- • Develop emergency housing resources.
Third Alzheimer Plan 2008–2012
- • The growing need is clear.
- • Improve diagnosis.
- • Strengthen coordination between providers.
- • Provide better treatment and support for caregivers.
- • Provide supportive home help more effectively.
- • Speed up research.
- • Provide public information.
Fourth Alzheimer Plan
- • Pan European.
- • In preparation.
US National Alzheimer’s Disease Project Act
Vision statement.
“For millions of Americans, the heartbreak of watching a loved one struggle with Alzheimer’s disease is a pain they know all too well. Alzheimer’s disease burdens an increasing number of our Nation’s elders and their families, and it is essential that we confront the challenge it poses to our public health.” US President Barack Obama
Action Plan
On 4 January 2011, President Barack Obama signed into law the National Alzheimer’s Project Act (NAPA), requiring the Secretary of the US Department of Health and Human Services (HHS) to establish the National Alzheimer’s Project to:
- • Create and maintain an integrated national plan to overcome Alzheimer’s disease (AD).
- • Coordinate Alzheimer’s disease research and services across all federal agencies.
- • Accelerate the development of treatments to prevent, halt, or reverse the course of AD.
- • Improve early diagnosis and coordination of care and treatment of AD.
- • Improve outcomes for ethnic and racial minority populations that are at higher risk for AD.
- • Coordinate with international bodies to fight AD globally.
The law also establishes the Advisory Council on Alzheimer’s Research, Care, and Services and requires the Secretary of HHS, in collaboration with the Advisory Council, to create and maintain a national plan to overcome AD.
Goals and Strategies for 2025
Research funds are being allocated towards that end. Education for health providers, strengthening of the workforce, for direct care and for public health guidelines for management of AD, education and support for caring families, addressing special housing needs for AD patients and many other initiatives are proposed in this comprehensive approach to a growing public health problem. Enhancing public awareness is crucial to achieve the goals set out in this plan.
Health care is one of the largest and most important industries in any country, consuming anywhere from 3 to nearly 18 percent of GNP, and still growing. It is a service, not a production industry, and is vital to the health and well-being of the individual, the population, and the economy. Because health care employs large numbers of skilled professionals and many unskilled people, it is often vital to the economic survival of small communities, as well as for a sense of community well-being.
Management includes planning, leading, controlling, organizing, motivating, and decision-making. It is the application of resources and personnel towards achieving targets. Therefore, it involves the study of the use of resources, and the motivation and function of the people involved, including the producer or provider of service, and the customer, client, or patient. This cannot take place in a vacuum, but is based on the continuous monitoring of information and its communication to all parties involved. These functions are applicable at all levels of management, from policy to operational management of a production or a service system. Creative management of health systems is vital to the functioning of the system at the macrolevel, as well as in the individual department or service. This implies effective use of resources to achieve objectives, and community, provider, and consumer satisfaction. These are formidable challenges, not only when money is available in abundance, but even more so when resources are limited and difficult choices need to be made.
Modern management includes knowledge and skills in identifying and measuring community health needs and health risks. Critical needs are addressed in strategic planning with measurable impacts and targets. Public health managers should have skills gained in marketing, networking, data management, managing human resources and finance, engaging community partners, and communicating public health messages.
Many of the methods of management and organization theory developed as part of the business world have become part of public health. These include defining the mission, values and objectives of the organization, strategic planning and management, MBO, human resource management (recognizing individual and professional values), incentives–disincentives, regulation, education, and economic resources. The ultimate mission of public health is the saving of human life and improving its quality, and achieving this efficiently with high standards of professionalism and community involvement.
The scope of the New Public Health is broad. It includes the traditional public health programs, but equally must concern itself with managing and planning comprehensive service systems and measuring their function. The selection of targets and priorities is often determined by the feasible rather than the ideal. The health manager, either at the macrolevel of health or managing a local clinic, needs to be able to conceptualize the possibilities of improving the health of individuals and the population in his or her service responsibility with current and appropriate methods. Good management means designing objectives based on a balance between the feasible and the desirable. Public health has benefited greatly from its work with the social sciences and assistance from management and systems sciences to adapt and absorb the new challenges and technologies in applied public health. The New Public Health is not only a concept; it is a management approach to improve the health of individuals and the population.
For a complete bibliography and guidance for student reviews and expected competencies please see companion web site at http://booksite.elsevier.com/9780124157668
Bibliography
Electronic resources.
- Agency for Healthcare Research and Quality http://www.ahrq.gov/ (accessed 28.12.12) [ PubMed ]
- American College of Healthcare Executives http://www.ache.org/ (accessed 28.12.12)
- American College of Medical Quality http://www.acmq.org/ (accessed 28.12.12)
- American Hospital Association http://www.aha.org/ (accessed 28.12.12)
- Centers for Disease Control and Prevention Management and Analysis Services Office. http://www.cdc.gov/maso/ (accessed 28.12.12)
- Glossary of Managed Care Terms http://www.pohly.com/terms.html http://www.thci.org/other_resources/glossary.htm and. (accessed 28.12.12)
- Joint Commission http://www.jointcommission.org/ Updated 27 December 2012 at: (accessed 28.12.12)
- National Association of Public Hospitals and Health Systems. http://www.naph.org/ (accessed 28.12.12)
- National Center for Health Statistics Centers for Disease Control and Prevention. http://www.cdc.gov/nchs/ (accessed 28.12.12)
- World Health Organization The health manager’s website. http://www.who.int/management/en/ (accessed 28.12.12)
Recommended Reading
- Agency for Healthcare Research and Quality Pay for performance (P4P): AHRQ resources. 2012. http://www.ahrq.gov/professionals/quality-patient-safety/quality-resources/tools/pay4per.html AHRQ, Rockville, MD. Available at: (accessed 02.01.14)
- Aguayo R. Simon & Schuster; New York: 1990. Dr. Deming: the American who taught the Japanese about quality. http://www.amazon.com/Dr-Deming-American-Japanese-Quality/dp/0671746219 Available at: (accessed 02.01.14) [ Google Scholar ]
- American College of Physicians Health and Public Policy Committee. Achieving a high performance health care system with universal access: what the United States can learn from other countries. Ann. Intern. Med. 2008; 148 :55–75. http://annals.org/article.aspx?articleid=738556 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Bar-Yam Y. Improving the effectiveness of health care and public health: a multi-scale complex systems analysis. Am. J. Public Health. 2006; 96 :459–466. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1470498/ Available at: (accessed 02.01.14) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention Framework for program evaluation in public health. MMWR Recomm. Rep. 1999; 48 (RR-11):1–40. http://www.cdc.gov/mmwr/pdf/rr/rr4811.pdf Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention Biological and chemical terrorism: strategic plan for preparedness and response. Recommendations of the CDC strategic planning workgroup. MMWR Recomm. Rep. 2000; 49 (RR-04):1–14. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr4904a1.htm Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Centers for Disease Control and Prevention . CDC; Atlanta, GA: 12 September 2012. A framework for program evaluation. Office of the Associate Director for Program – Program Evaluation. http://www.cdc.gov/eval/framework/index.htm Available at: (accessed 30.12.12) [ Google Scholar ]
- CEO online Developing leadership skills. http://www.ceoonline.com/expert_talk/leadership_management/leadership_skill.aspx Available at: (accessed 24.12.12)
- Dutton D.B. Patterns of ambulatory health care in five different delivery systems. Med. Care. 1979; 17 :221–243. http://journals.lww.com/lww-medicalcare/toc/1979/03000 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Ettelt S., Nolte E., Thomson S., Mays N. WHO, on behalf of the European Observatory on Health Systems and Policies; Copenhagen: 2008. Capacity planning in health care: a review of the international experience. http://www.euro.who.int/__data/assets/pdf_file/0003/108966/E91193.pdf Available at: (accessed 02.01.14) [ Google Scholar ]
- Ginter P.M., Duncan W.J.P., Swayne L.E. 7th edition; Jossey-Bass: 2013. Strategic management of health care organizations. http://ca.wiley.com/WileyCDA/WileyTitle/productCd-1118466462.html Available at: (accessed 02.01.14) [ Google Scholar ]
- Heldman A.B., Schindelar J., Weaver J.B., III Social media engagement and public health communication: implications for public health organizations being truly “social” Public Health Reviews. 2013:35. http://www.publichealthreviews.eu/show/a/129 epub ahead of print. (accessed 04.01.13) [ Google Scholar ]
- Institute of Medicine . National Academies Press; Washington, DC: 2001. Crossing the quality chasm: a new health system for the twenty-first century. http://www.nap.edu/catalog.php?record_id=10027 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Institute of Medicine . National Academies Press; Washington, DC: 2003. Future of the public’s health in the 21st century. http://www.nap.edu/catalog.php?record_id=10548 Available at: (accessed 02.01.14) [ Google Scholar ]
- Institute of Medicine . National Academies Press; Washington, DC: 2012. Best care at lower cost: the path to continuously learning health care in America. http://www.nap.edu/download.php?record_id=13444 Available at: (accessed 13.07.13) [ PubMed ] [ Google Scholar ]
- Johnson W.D., Diaz R.M., Flanders W.D., Goodman M., Hill A.N., Holtgrave D. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst. Rev. 2008;(3):CD001230. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD001230.pub2/abstract;jsessionid=2CEB240AD4112A2A5696505CD03A7CDD.f04t04 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Katzenbach J.R., Smith D.K. Harvard Business School Press; Cambridge, MA: 1993. The wisdom of teams: creating the high-performance organization. http://www.amazon.com/The-Wisdom-Teams-High-Performance-Organization/dp/0060522003 Available at: (accessed 02.01.14) [ Google Scholar ]
- Lee N.R., Kotler P.A. Sage; Thousand Oaks, CA: 2011. Social marketing: Influencing behaviors for good [fourth edition] http://www.amazon.com/Social-Marketing-Influencing-Behaviors-Good/dp/1412981492 Available at: (accessed 01.02.14) [ Google Scholar ]
- Levesque, J.-F., Breton, M., Senn, N., Levesque, P., Bergeron, P., Roy, D.A., MD, 2013. The interaction of public health and primary care: functional roles and organizational models that bridge individual and population perspectives. Public Health Reviews, 35: epub ahead of print. http://www.publichealthreviews.eu/show/a/130 (accessed 04.01.13).
- Maynard A. The powers and pitfalls of the payment for performance. Health Econ. 2012; 21 :3–12. http://avym.com/wp-content/uploads/2013/07/Powers-and-Pitfalls-of-Fee-For-Service-payment-models.pdf Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Molinsky A.L., Davenport T.H., Iyer B., Davidson C. Three skills every 21st-century manager needs. Harv. Bus. Rev. 2012 (January–February) http://hbr.org/2012/01/three-skills-every-21st-century-manager-needs Available at: (accessed 23.12.12) [ PubMed ] [ Google Scholar ]
- Powel T.C. Total quality management as competitive advantage: a review and empirical study. Strateg. Manage. J. 1995; 16 :15–37. http://www.thomaspowell.co.uk/article_pdfs/TQM_as_CA.pdf Available at: (accessed 02.01.14) [ Google Scholar ]
- Ryan A., Blustein J. Making the best of hospital pay for performance. N. Engl. J. Med. 2012; 366 :1557–1559. http://www.nejm.org/doi/pdf/10.1056/NEJMp1202563 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Satcher D., Higginbotham E.J. The public health approach to eliminating disparities in health. Am. J. Public Health. 2008; 98 :400–403. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2253560/ Available at: (accessed 02.01.14) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Scutchfield F.D., Ingram R.C. Public health systems and services research: building the evidence base to improve public health practice. Public Health Reviews. 2013:35. http://www.publichealthreviews.eu/show/a/126 epub ahead of print. (accessed 04.01.13) [ Google Scholar ]
- Shortell S.M., Gillies R., Wu F. United States innovations in healthcare delivery. Public Health Rev. 2011; 32 :190–212. http://www.publichealthreviews.eu/show/f/26 Available at: (accessed 02.01.14) [ Google Scholar ]
- Smith J.M., Topol E. A call to action: lowering the cost of health care. Am. J. Prev. Med. 2013; 44 (1S1):S54–S57. http://www.ajpmonline.org/article/S0749-3797(12)00637-X/fulltext Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Sutton M., Nikolova S., Boaden R., Lester H., McDonald R., Roland M. Reduced mortality with hospital pay for performance in England. N. Engl. J. Med. 2012; 367 :1821–1828. http://www.nejm.org/doi/full/10.1056/NEJMsa1114951 Available at: (accessed 02.01.14) [ PubMed ] [ Google Scholar ]
- Trochim W.M., Cabrera D.A., Milstein B., Gallagher R.S., Leischow S.L. Practical challenges of systems thinking and modeling in public health. Am. J. Public Health. 2006; 96 :538–546. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1470516/ Available at: (accessed 02.01.14) [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Turnock B.J. second ed. Jones and Bartlett; Sudbury, MA: 2012. Public health: essentials of public health. http://www.amazon.com/Essentials-Of-Public-Health-Essential/dp/1449600220 Available at: (accessed 02.01.14) [ Google Scholar ]
- US Department of Health and Human Services . DHHS; Washington, DC: 2011. Health United States, 2011, with chartbook on trends in the health of Americans. http://www.cdc.gov/nchs/data/hus/hus11.pdf Available at: (accessed 02.01.14) [ Google Scholar ]
| You might be using an unsupported or outdated browser. To get the best possible experience please use the latest version of Chrome, Firefox, Safari, or Microsoft Edge to view this website. |
- Financial Advisor
Financial Planning Basics

Updated: Jun 26, 2024, 4:51pm

No matter the size or scope of your financial goals, a financial plan can help make them a reality.
Financial planning is the process of looking at the current state of your finances and making a step-by-step plan to get it where you want it to be. That may mean devising a plan to become debt-free or figuring out how to save enough money for a down payment on a new home.
This process can include many aspects of personal finance, including investing, debt repayment, building savings, planning for retirement and even purchasing insurance.
Anyone can engage in financial planning—it’s not just for the wealthy. You can get started on making financial goals on your own, and if you choose, you can work with a financial professional to help devise the smartest plan to make those goals a reality.
Advertisement
Datalign advisory.
Access to thousands of financial advisors.
Match with a pre-screened financial advisor that is right for you.
Connect with your match for a free, no-obligation call.
5 Steps to Create a Financial Plan
A financial plan is devised of smaller goals or tasks that will help support you along your financial journey. Create a financial plan with these five steps:
1. Identify Your Financial Goals
By identifying your financial goals, you’ll have a clear idea of what you need to accomplish to make them happen. Your goals should be realistic and actionable and include a timeline of when you want to accomplish them.
Making a goal to pay off credit card debt by a certain date, for example, would be an appropriate financial goal that will set you up for success.
2. Set a Budget
Having a clear picture of your finances will make it easier to achieve any financial goals. A budget can help you understand where your money is going each month. It can also help you identify where you may be overspending, giving you opportunities to cut back and allocate that money elsewhere.
One of the easiest budgets to start with is the 50/30/20 budget . This budget plan allocates your monthly income into three buckets: mandatory expenses (50%), savings and debt repayment (20%) and discretionary spending (30%). This is just one of many types of budgeting plans out there.
A budget should be a guide to help you understand your monthly finances and devise smaller goals that will bring you closer to your long-term financial goals. You likely won’t always follow your budget down to every single penny; keeping this in mind will help you stay on track, rather than get discouraged and give up on budgeting altogether.
There are apps out there that make budgeting much easier by helping you visualize your spending and savings choices each month. Some budgeting apps even give you the option to enter your financial goals directly into their platform to help you stay on track. A fully featured budgeting app allows you to track spending, manage recurring bill payments, set savings goals and manage your monthly cash flow.
3. Build an Emergency Fund
Building an emergency fund will help make sure that a financial emergency doesn’t become a catastrophic financial event.
Experts usually recommend having six months’ worth of living expenses saved to cushion you, should the unfortunate unexpected happen, such as losing a job. But six months’ worth of money can be unattainable for those who may be struggling financially, or those living in tight financial means each month.
You can start building an emergency fund by setting a few dollars aside each paycheck. You can start with a small fund goal of $100 to $200 to establish your fund. From there, you can create other smaller goals that will add up to a larger financial cushion. Some budgeting and savings apps also give you the option of rounding up to the nearest dollar in transactions and funnel that spare change toward your savings.
4. Reduce Your Debt
Having to make debt payments each month means you’ll have less money to allocate toward your purchase goals. Plus, carrying credit card debt can be expensive; every month, you’re accruing interest on your balance, which can make it take longer to pay off.
There are a variety of debt payoff methods out there. Two of the most popular include the debt snowball and debt avalanche methods . With the snowball method, you’ll pay off your smallest balance debts first, then make your way to the ones with the higher balances. The debt avalanche, on the other hand, starts with higher interest rate debts first.
5. Invest for the Future
Although risky, investing can help grow your money, even if you’re not wealthy. You can get started with investing by enrolling in your company’s 401(k) plan or opening a low-or-no fee account through an online broker .
Keep in mind that investing always involves some risk; you could end up losing the money you invest. There are also robo-advisors that automatically recommend investments based on your goals and risk tolerance.
Looking For A Financial Advisor?
Get In Touch With A Pre-screened Financial Advisor In 3 Minutes
Via Datalign Advisory
Bottom Line
A financial plan is composed of a series of smaller goals that will help you achieve a larger financial goal, such as purchasing a home or retiring comfortably. A solid financial plan includes identifying your goals, creating a budget, building an emergency fund, paying off high interest debt and investing.

7 Life-Changing Events a Financial Advisor Can Help With
How To Become A Financial Advisor
What You Need to Know About Independent Financial Advisors
Financial Advisor Vs. Financial Planner: What’s The Difference?

What Is FINRA?
Fee-Only Financial Planner vs. Fee-Based: What’s the Difference?
Jordan Tarver has spent seven years covering mortgage, personal loan and business loan content for leading financial publications such as Forbes Advisor. He blends knowledge from his bachelor's degree in business finance, his experience as a top performer in the mortgage industry and his entrepreneurial success to simplify complex financial topics. Jordan aims to make mortgages and loans understandable.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
17 Team-Building Activities for In-Person, Remote, and Hybrid Teams
- Rebecca Knight

Employees with strong relationships at work are more creative, collaborative, and likely to stay with their organization.
Managers sometimes turn to team-building activities to build connections between colleagues. But which activities and practices would work best for your team? And how can you put them into action most effectively? In this article, the author offers advice and recommendations from three experts. Their activity suggestions are intended to inspire ideas that you can then tailor to your team’s size, sensibilities, and circumstances. These activities don’t need to be extravagant or overly structured — what matters is being intentional about making team building happen. Stay attentive to your team members’ needs, involve colleagues in planning, and show sincere interest in getting to know them. By doing so, you’ll help build a positive, inclusive team culture that tackles loneliness and helps everyone succeed together.
In the era of remote work and scattered teams, managers face a key challenge: fostering connections among employees, no matter where they happen to be located.
- RK Rebecca Knight is a journalist who writes about all things related to the changing nature of careers and the workplace. Her essays and reported stories have been featured in The Boston Globe, Business Insider, The New York Times, BBC, and The Christian Science Monitor. She was shortlisted as a Reuters Institute Fellow at Oxford University in 2023. Earlier in her career, she spent a decade as an editor and reporter at the Financial Times in New York, London, and Boston.
Partner Center

IMAGES
COMMENTS
Explore key strategies for healthcare executives in our in-depth guide on strategic planning, covering essential techniques, phases, and success tips.
Strategic management is becoming increasingly important for sustainable management in healthcare. The reasons for this can be seen in the increasing complexity, dynamics and uncertainty of the system's regimes and the resulting need for strategic ...
Uncover the top seven strategic planning models revolutionizing healthcare, how they work, and how they contribute to the success of organizations.
Understand business strategy to facilitate health care success In this course, Harvard Business School faculty teach learners to align business strategy with the challenges and structures of the health care industry in the United States.
Learn why strategic planning is essential for coding managers and compliance directors and how to create a plan for your organization. Strategic planning is an important part of any business and is becoming ever more critical in our evolving healthcare environment. Strategic planning involves setting goals, determining actions to achieve those goals, and mobilizing resources to efficiently ...
Unlock effective healthcare strategic planning with insights, a free template, and tips for adapting to rapid industry changes.
Vanderbilt MMHC leaders break down 4 keys to successful healthcare management and how to manage growth in the industry.
The future of healthcare: Value creation through next-generation business models. The healthcare industry in the United States has experienced steady growth over the past decade while simultaneously promoting quality, efficiency, and access to care. Between 2012 and 2019, profit pools (earnings before interest, taxes, depreciation, and ...
Learn about the importance & benefits of strategic planning in healthcare, the top 5 strategic challenges and questions healthcare institutions should ask.
Enhance your strategic planning with our 5 tips for healthcare professionals. Elevate your planning and contribute to your organization's success now!
Starting with an examination of leadership's role in strategic planning and the impact of organizational culture, the book then explores the essential techniques, tools, and data for developing a strategic plan and recommends strategic planning initiatives across the continuum of healthcare services.
Strategic Planning In Healthcare: 2024 Guide + Examples. This guide contains new healthcare planning strategies, their benefits, examples, traps to avoid, and all you need to know. Whether you're a medical business owner, an executive, or a practitioner, my promise to you is that, by the end of this article, you'll get a razor-sharp ...
Strategic planning is a crucial process for health care organizations because the environment is continuously changing, with new technologies, regulations, and patient expectations emerging. By engaging in strategic planning, health care organizations can stay ahead of these changes and be better prepared for the future.
Strategic Planning A key element in business management is strategic planning, which can move a business/practice that is being buffeted by changing economic forces to one that shapes its own future. It is an organized, step-by-step review of the business, the economy, and the environment in which the business operates. Strategic Planning for Healthcare Organizations
Taught by Harvard Business School Professor Leemore Dafny, our Health Care Strategy course teaches learners to align business strategy with the challenges and structures of the health care industry in the United States. This 5-week course explores four main concepts of business strategy that can enable leaders to deal with the unique challenges ...
Strategic Healthcare Management: Planning and Execution provides a thorough overview of strategic principles and the competencies needed to apply them, such as communication, decision making, positioning, goal setting, data analyses, project management, and financial analysis.
Strategic planning is a completely valid and useful tool for guiding all types of organizations, including healthcare organizations. The organizational level at which the strategic planning process is relevant depends on the unit's size, its complexity, and the differentiation of the service provided. A cardiology department, a hemodynamic unit ...
The Business of Healthcare Certificate program was designed to help you keep pace with the rapidly changing world of health and health care. Through partnership with Wharton and Penn Medicine, you'll learn from experts in business acumen, health care management, and health care policy to develop the skills you'll need to successfully navigate the intersection of business and health care.
7 Steps to Strategic Planning. anning: Step 1 - Review/Develop Vision & MissionAlthough many organizations have created vision, mission, goals and objectives, thes. elements need to be reviewed on a continuous basis. The reason lies in the ever-changing environment and business constraints forced upon organizations through government, payo.
IntroductIon Strategic planning brings leaders and stakeholders together to position their organization for success in an environment of uncertainty. A healthcare organization engages in strategic planning to reduce costs, improve quality and service, and ensure access to care.
Keywords: health promotion, health systems management, human behavior, knowledge-based service industry, management skills, network organization, organization theory, planning and policy in health, strategic management, systems approach Learning Objectives Upon completion of this chapter, the student should be able to: 1.
Track and manage all the aspects of work with healthcare project management software. From planning to execution, these tools will help you achieve successful outcomes every time.
Financial planning is the process of looking at the current state of your finances and making a step-by-step plan to get them to where you want them to be.
Health Plan member's EPSDT SC to notify UHC C&S Louisiana Health Plan CM/CC of specific member needs, request assistance with obtaining needed services and/or to serve as notification of activity related to member services, such as prior authorization for service request that are due for renewal.
Improve patient care by embracing our 5G Advanced Network Solutions for healthcare. See how organizations like Boston Children's Hospital use our 5G network to meet some of the industry's biggest challenges and opportunities.
Creating a good healthcare risk management plan is very important to make sure patients, the team and organization are safe and doing well. This type of strategy helps in finding out, evaluating and lessening possible risks that might affect the care's quality plus how smoothly it operates. A properly organized risk management plan doesn't just […]
Managers sometimes turn to team-building activities to build connections between colleagues. But which activities and practices would work best for your team? And how can you put them into action ...
The 2024 list of interior design firms is another reflection of our city's resilience in midst of changing times. Companies represented include multidiscipline firms and boutique agencies.
The ORR Unaccompanied Children Bureau Policy Guide is a summary of ORR policies for the placement, release and care of unaccompanied children in ORR custody. The guide is for members of the public and other stakeholders and is organized into three main sections.
Oversees computerized maintenance management system (CMMS) and the capital planning software including data entry, data storage, dashboard and query creation, report generation, and managing work requests and work completion processes.