Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
Methodology
- How to Write a Literature Review | Guide, Examples, & Templates

How to Write a Literature Review | Guide, Examples, & Templates
Published on January 2, 2023 by Shona McCombes . Revised on September 11, 2023.
What is a literature review? A literature review is a survey of scholarly sources on a specific topic. It provides an overview of current knowledge, allowing you to identify relevant theories, methods, and gaps in the existing research that you can later apply to your paper, thesis, or dissertation topic .
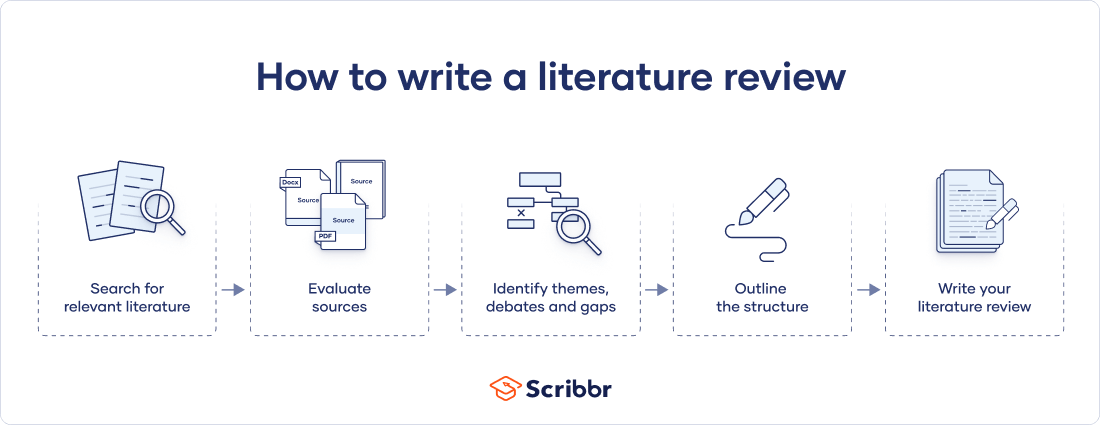
There are five key steps to writing a literature review:
- Search for relevant literature
- Evaluate sources
- Identify themes, debates, and gaps
- Outline the structure
- Write your literature review
A good literature review doesn’t just summarize sources—it analyzes, synthesizes , and critically evaluates to give a clear picture of the state of knowledge on the subject.
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is the purpose of a literature review, examples of literature reviews, step 1 – search for relevant literature, step 2 – evaluate and select sources, step 3 – identify themes, debates, and gaps, step 4 – outline your literature review’s structure, step 5 – write your literature review, free lecture slides, other interesting articles, frequently asked questions, introduction.
- Quick Run-through
- Step 1 & 2
When you write a thesis , dissertation , or research paper , you will likely have to conduct a literature review to situate your research within existing knowledge. The literature review gives you a chance to:
- Demonstrate your familiarity with the topic and its scholarly context
- Develop a theoretical framework and methodology for your research
- Position your work in relation to other researchers and theorists
- Show how your research addresses a gap or contributes to a debate
- Evaluate the current state of research and demonstrate your knowledge of the scholarly debates around your topic.
Writing literature reviews is a particularly important skill if you want to apply for graduate school or pursue a career in research. We’ve written a step-by-step guide that you can follow below.
Don't submit your assignments before you do this
The academic proofreading tool has been trained on 1000s of academic texts. Making it the most accurate and reliable proofreading tool for students. Free citation check included.

Try for free
Writing literature reviews can be quite challenging! A good starting point could be to look at some examples, depending on what kind of literature review you’d like to write.
- Example literature review #1: “Why Do People Migrate? A Review of the Theoretical Literature” ( Theoretical literature review about the development of economic migration theory from the 1950s to today.)
- Example literature review #2: “Literature review as a research methodology: An overview and guidelines” ( Methodological literature review about interdisciplinary knowledge acquisition and production.)
- Example literature review #3: “The Use of Technology in English Language Learning: A Literature Review” ( Thematic literature review about the effects of technology on language acquisition.)
- Example literature review #4: “Learners’ Listening Comprehension Difficulties in English Language Learning: A Literature Review” ( Chronological literature review about how the concept of listening skills has changed over time.)
You can also check out our templates with literature review examples and sample outlines at the links below.
Download Word doc Download Google doc
Before you begin searching for literature, you need a clearly defined topic .
If you are writing the literature review section of a dissertation or research paper, you will search for literature related to your research problem and questions .
Make a list of keywords
Start by creating a list of keywords related to your research question. Include each of the key concepts or variables you’re interested in, and list any synonyms and related terms. You can add to this list as you discover new keywords in the process of your literature search.
- Social media, Facebook, Instagram, Twitter, Snapchat, TikTok
- Body image, self-perception, self-esteem, mental health
- Generation Z, teenagers, adolescents, youth
Search for relevant sources
Use your keywords to begin searching for sources. Some useful databases to search for journals and articles include:
- Your university’s library catalogue
- Google Scholar
- Project Muse (humanities and social sciences)
- Medline (life sciences and biomedicine)
- EconLit (economics)
- Inspec (physics, engineering and computer science)
You can also use boolean operators to help narrow down your search.
Make sure to read the abstract to find out whether an article is relevant to your question. When you find a useful book or article, you can check the bibliography to find other relevant sources.
You likely won’t be able to read absolutely everything that has been written on your topic, so it will be necessary to evaluate which sources are most relevant to your research question.
For each publication, ask yourself:
- What question or problem is the author addressing?
- What are the key concepts and how are they defined?
- What are the key theories, models, and methods?
- Does the research use established frameworks or take an innovative approach?
- What are the results and conclusions of the study?
- How does the publication relate to other literature in the field? Does it confirm, add to, or challenge established knowledge?
- What are the strengths and weaknesses of the research?
Make sure the sources you use are credible , and make sure you read any landmark studies and major theories in your field of research.
You can use our template to summarize and evaluate sources you’re thinking about using. Click on either button below to download.
Take notes and cite your sources
As you read, you should also begin the writing process. Take notes that you can later incorporate into the text of your literature review.
It is important to keep track of your sources with citations to avoid plagiarism . It can be helpful to make an annotated bibliography , where you compile full citation information and write a paragraph of summary and analysis for each source. This helps you remember what you read and saves time later in the process.
To begin organizing your literature review’s argument and structure, be sure you understand the connections and relationships between the sources you’ve read. Based on your reading and notes, you can look for:
- Trends and patterns (in theory, method or results): do certain approaches become more or less popular over time?
- Themes: what questions or concepts recur across the literature?
- Debates, conflicts and contradictions: where do sources disagree?
- Pivotal publications: are there any influential theories or studies that changed the direction of the field?
- Gaps: what is missing from the literature? Are there weaknesses that need to be addressed?
This step will help you work out the structure of your literature review and (if applicable) show how your own research will contribute to existing knowledge.
- Most research has focused on young women.
- There is an increasing interest in the visual aspects of social media.
- But there is still a lack of robust research on highly visual platforms like Instagram and Snapchat—this is a gap that you could address in your own research.
There are various approaches to organizing the body of a literature review. Depending on the length of your literature review, you can combine several of these strategies (for example, your overall structure might be thematic, but each theme is discussed chronologically).
Chronological
The simplest approach is to trace the development of the topic over time. However, if you choose this strategy, be careful to avoid simply listing and summarizing sources in order.
Try to analyze patterns, turning points and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred.
If you have found some recurring central themes, you can organize your literature review into subsections that address different aspects of the topic.
For example, if you are reviewing literature about inequalities in migrant health outcomes, key themes might include healthcare policy, language barriers, cultural attitudes, legal status, and economic access.
Methodological
If you draw your sources from different disciplines or fields that use a variety of research methods , you might want to compare the results and conclusions that emerge from different approaches. For example:
- Look at what results have emerged in qualitative versus quantitative research
- Discuss how the topic has been approached by empirical versus theoretical scholarship
- Divide the literature into sociological, historical, and cultural sources
Theoretical
A literature review is often the foundation for a theoretical framework . You can use it to discuss various theories, models, and definitions of key concepts.
You might argue for the relevance of a specific theoretical approach, or combine various theoretical concepts to create a framework for your research.
Like any other academic text , your literature review should have an introduction , a main body, and a conclusion . What you include in each depends on the objective of your literature review.
The introduction should clearly establish the focus and purpose of the literature review.
Depending on the length of your literature review, you might want to divide the body into subsections. You can use a subheading for each theme, time period, or methodological approach.
As you write, you can follow these tips:
- Summarize and synthesize: give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: don’t just paraphrase other researchers — add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically evaluate: mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: use transition words and topic sentences to draw connections, comparisons and contrasts
In the conclusion, you should summarize the key findings you have taken from the literature and emphasize their significance.
When you’ve finished writing and revising your literature review, don’t forget to proofread thoroughly before submitting. Not a language expert? Check out Scribbr’s professional proofreading services !
This article has been adapted into lecture slides that you can use to teach your students about writing a literature review.
Scribbr slides are free to use, customize, and distribute for educational purposes.
Open Google Slides Download PowerPoint
If you want to know more about the research process , methodology , research bias , or statistics , make sure to check out some of our other articles with explanations and examples.
- Sampling methods
- Simple random sampling
- Stratified sampling
- Cluster sampling
- Likert scales
- Reproducibility
Statistics
- Null hypothesis
- Statistical power
- Probability distribution
- Effect size
- Poisson distribution
Research bias
- Optimism bias
- Cognitive bias
- Implicit bias
- Hawthorne effect
- Anchoring bias
- Explicit bias
A literature review is a survey of scholarly sources (such as books, journal articles, and theses) related to a specific topic or research question .
It is often written as part of a thesis, dissertation , or research paper , in order to situate your work in relation to existing knowledge.
There are several reasons to conduct a literature review at the beginning of a research project:
- To familiarize yourself with the current state of knowledge on your topic
- To ensure that you’re not just repeating what others have already done
- To identify gaps in knowledge and unresolved problems that your research can address
- To develop your theoretical framework and methodology
- To provide an overview of the key findings and debates on the topic
Writing the literature review shows your reader how your work relates to existing research and what new insights it will contribute.
The literature review usually comes near the beginning of your thesis or dissertation . After the introduction , it grounds your research in a scholarly field and leads directly to your theoretical framework or methodology .
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
McCombes, S. (2023, September 11). How to Write a Literature Review | Guide, Examples, & Templates. Scribbr. Retrieved July 29, 2024, from https://www.scribbr.com/dissertation/literature-review/
Is this article helpful?
Shona McCombes
Other students also liked, what is a theoretical framework | guide to organizing, what is a research methodology | steps & tips, how to write a research proposal | examples & templates, "i thought ai proofreading was useless but..".
I've been using Scribbr for years now and I know it's a service that won't disappoint. It does a good job spotting mistakes”
Purdue Online Writing Lab Purdue OWL® College of Liberal Arts
Writing a Literature Review

Welcome to the Purdue OWL
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice.
Copyright ©1995-2018 by The Writing Lab & The OWL at Purdue and Purdue University. All rights reserved. This material may not be published, reproduced, broadcast, rewritten, or redistributed without permission. Use of this site constitutes acceptance of our terms and conditions of fair use.
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays). When we say “literature review” or refer to “the literature,” we are talking about the research ( scholarship ) in a given field. You will often see the terms “the research,” “the scholarship,” and “the literature” used mostly interchangeably.
Where, when, and why would I write a lit review?
There are a number of different situations where you might write a literature review, each with slightly different expectations; different disciplines, too, have field-specific expectations for what a literature review is and does. For instance, in the humanities, authors might include more overt argumentation and interpretation of source material in their literature reviews, whereas in the sciences, authors are more likely to report study designs and results in their literature reviews; these differences reflect these disciplines’ purposes and conventions in scholarship. You should always look at examples from your own discipline and talk to professors or mentors in your field to be sure you understand your discipline’s conventions, for literature reviews as well as for any other genre.
A literature review can be a part of a research paper or scholarly article, usually falling after the introduction and before the research methods sections. In these cases, the lit review just needs to cover scholarship that is important to the issue you are writing about; sometimes it will also cover key sources that informed your research methodology.
Lit reviews can also be standalone pieces, either as assignments in a class or as publications. In a class, a lit review may be assigned to help students familiarize themselves with a topic and with scholarship in their field, get an idea of the other researchers working on the topic they’re interested in, find gaps in existing research in order to propose new projects, and/or develop a theoretical framework and methodology for later research. As a publication, a lit review usually is meant to help make other scholars’ lives easier by collecting and summarizing, synthesizing, and analyzing existing research on a topic. This can be especially helpful for students or scholars getting into a new research area, or for directing an entire community of scholars toward questions that have not yet been answered.
What are the parts of a lit review?
Most lit reviews use a basic introduction-body-conclusion structure; if your lit review is part of a larger paper, the introduction and conclusion pieces may be just a few sentences while you focus most of your attention on the body. If your lit review is a standalone piece, the introduction and conclusion take up more space and give you a place to discuss your goals, research methods, and conclusions separately from where you discuss the literature itself.
Introduction:
- An introductory paragraph that explains what your working topic and thesis is
- A forecast of key topics or texts that will appear in the review
- Potentially, a description of how you found sources and how you analyzed them for inclusion and discussion in the review (more often found in published, standalone literature reviews than in lit review sections in an article or research paper)
- Summarize and synthesize: Give an overview of the main points of each source and combine them into a coherent whole
- Analyze and interpret: Don’t just paraphrase other researchers – add your own interpretations where possible, discussing the significance of findings in relation to the literature as a whole
- Critically Evaluate: Mention the strengths and weaknesses of your sources
- Write in well-structured paragraphs: Use transition words and topic sentence to draw connections, comparisons, and contrasts.
Conclusion:
- Summarize the key findings you have taken from the literature and emphasize their significance
- Connect it back to your primary research question
How should I organize my lit review?
Lit reviews can take many different organizational patterns depending on what you are trying to accomplish with the review. Here are some examples:
- Chronological : The simplest approach is to trace the development of the topic over time, which helps familiarize the audience with the topic (for instance if you are introducing something that is not commonly known in your field). If you choose this strategy, be careful to avoid simply listing and summarizing sources in order. Try to analyze the patterns, turning points, and key debates that have shaped the direction of the field. Give your interpretation of how and why certain developments occurred (as mentioned previously, this may not be appropriate in your discipline — check with a teacher or mentor if you’re unsure).
- Thematic : If you have found some recurring central themes that you will continue working with throughout your piece, you can organize your literature review into subsections that address different aspects of the topic. For example, if you are reviewing literature about women and religion, key themes can include the role of women in churches and the religious attitude towards women.
- Qualitative versus quantitative research
- Empirical versus theoretical scholarship
- Divide the research by sociological, historical, or cultural sources
- Theoretical : In many humanities articles, the literature review is the foundation for the theoretical framework. You can use it to discuss various theories, models, and definitions of key concepts. You can argue for the relevance of a specific theoretical approach or combine various theorical concepts to create a framework for your research.
What are some strategies or tips I can use while writing my lit review?
Any lit review is only as good as the research it discusses; make sure your sources are well-chosen and your research is thorough. Don’t be afraid to do more research if you discover a new thread as you’re writing. More info on the research process is available in our "Conducting Research" resources .
As you’re doing your research, create an annotated bibliography ( see our page on the this type of document ). Much of the information used in an annotated bibliography can be used also in a literature review, so you’ll be not only partially drafting your lit review as you research, but also developing your sense of the larger conversation going on among scholars, professionals, and any other stakeholders in your topic.
Usually you will need to synthesize research rather than just summarizing it. This means drawing connections between sources to create a picture of the scholarly conversation on a topic over time. Many student writers struggle to synthesize because they feel they don’t have anything to add to the scholars they are citing; here are some strategies to help you:
- It often helps to remember that the point of these kinds of syntheses is to show your readers how you understand your research, to help them read the rest of your paper.
- Writing teachers often say synthesis is like hosting a dinner party: imagine all your sources are together in a room, discussing your topic. What are they saying to each other?
- Look at the in-text citations in each paragraph. Are you citing just one source for each paragraph? This usually indicates summary only. When you have multiple sources cited in a paragraph, you are more likely to be synthesizing them (not always, but often
- Read more about synthesis here.
The most interesting literature reviews are often written as arguments (again, as mentioned at the beginning of the page, this is discipline-specific and doesn’t work for all situations). Often, the literature review is where you can establish your research as filling a particular gap or as relevant in a particular way. You have some chance to do this in your introduction in an article, but the literature review section gives a more extended opportunity to establish the conversation in the way you would like your readers to see it. You can choose the intellectual lineage you would like to be part of and whose definitions matter most to your thinking (mostly humanities-specific, but this goes for sciences as well). In addressing these points, you argue for your place in the conversation, which tends to make the lit review more compelling than a simple reporting of other sources.
Writing a Critical Review of Literature: A Practical Guide for English Graduate Students
- December 2018
- III(I):136-153
- This person is not on ResearchGate, or hasn't claimed this research yet.

- COMSATS University Islamabad

Abstract and Figures

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations

- S D Lukea Bhiwajee
- Nizar Ibnus

- REV EDUC RES
- M D Lecompte
- J K Klinger
- S A Campbell
- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- UConn Library
- Literature Review: The What, Why and How-to Guide
- Introduction
Literature Review: The What, Why and How-to Guide — Introduction
- Getting Started
- How to Pick a Topic
- Strategies to Find Sources
- Evaluating Sources & Lit. Reviews
- Tips for Writing Literature Reviews
- Writing Literature Review: Useful Sites
- Citation Resources
- Other Academic Writings
What are Literature Reviews?
So, what is a literature review? "A literature review is an account of what has been published on a topic by accredited scholars and researchers. In writing the literature review, your purpose is to convey to your reader what knowledge and ideas have been established on a topic, and what their strengths and weaknesses are. As a piece of writing, the literature review must be defined by a guiding concept (e.g., your research objective, the problem or issue you are discussing, or your argumentative thesis). It is not just a descriptive list of the material available, or a set of summaries." Taylor, D. The literature review: A few tips on conducting it . University of Toronto Health Sciences Writing Centre.
Goals of Literature Reviews
What are the goals of creating a Literature Review? A literature could be written to accomplish different aims:
- To develop a theory or evaluate an existing theory
- To summarize the historical or existing state of a research topic
- Identify a problem in a field of research
Baumeister, R. F., & Leary, M. R. (1997). Writing narrative literature reviews . Review of General Psychology , 1 (3), 311-320.
What kinds of sources require a Literature Review?
- A research paper assigned in a course
- A thesis or dissertation
- A grant proposal
- An article intended for publication in a journal
All these instances require you to collect what has been written about your research topic so that you can demonstrate how your own research sheds new light on the topic.
Types of Literature Reviews
What kinds of literature reviews are written?
Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified. The review ends with a conclusion section which summarizes the findings regarding the state of the research of the specific study, the gaps identify and if applicable, explains how the author's research will address gaps identify in the review and expand the knowledge on the topic reviewed.
- Example : Predictors and Outcomes of U.S. Quality Maternity Leave: A Review and Conceptual Framework: 10.1177/08948453211037398
Systematic review : "The authors of a systematic review use a specific procedure to search the research literature, select the studies to include in their review, and critically evaluate the studies they find." (p. 139). Nelson, L. K. (2013). Research in Communication Sciences and Disorders . Plural Publishing.
- Example : The effect of leave policies on increasing fertility: a systematic review: 10.1057/s41599-022-01270-w
Meta-analysis : "Meta-analysis is a method of reviewing research findings in a quantitative fashion by transforming the data from individual studies into what is called an effect size and then pooling and analyzing this information. The basic goal in meta-analysis is to explain why different outcomes have occurred in different studies." (p. 197). Roberts, M. C., & Ilardi, S. S. (2003). Handbook of Research Methods in Clinical Psychology . Blackwell Publishing.
- Example : Employment Instability and Fertility in Europe: A Meta-Analysis: 10.1215/00703370-9164737
Meta-synthesis : "Qualitative meta-synthesis is a type of qualitative study that uses as data the findings from other qualitative studies linked by the same or related topic." (p.312). Zimmer, L. (2006). Qualitative meta-synthesis: A question of dialoguing with texts . Journal of Advanced Nursing , 53 (3), 311-318.
- Example : Women’s perspectives on career successes and barriers: A qualitative meta-synthesis: 10.1177/05390184221113735
Literature Reviews in the Health Sciences
- UConn Health subject guide on systematic reviews Explanation of the different review types used in health sciences literature as well as tools to help you find the right review type
- << Previous: Getting Started
- Next: How to Pick a Topic >>
- Last Updated: Sep 21, 2022 2:16 PM
- URL: https://guides.lib.uconn.edu/literaturereview
The Sheridan Libraries
- Write a Literature Review
- Sheridan Libraries
- Find This link opens in a new window
- Evaluate This link opens in a new window
What Will You Do Differently?
Please help your librarians by filling out this two-minute survey of today's class session..
Professor, this one's for you .
Introduction
Literature reviews take time. here is some general information to know before you start. .
- VIDEO -- This video is a great overview of the entire process. (2020; North Carolina State University Libraries) --The transcript is included --This is for everyone; ignore the mention of "graduate students" --9.5 minutes, and every second is important
- OVERVIEW -- Read this page from Purdue's OWL. It's not long, and gives some tips to fill in what you just learned from the video.
- NOT A RESEARCH ARTICLE -- A literature review follows a different style, format, and structure from a research article.
| Reports on the work of others. | Reports on original research. | |
| To examine and evaluate previous literature. | To test a hypothesis and/or make an argument. May include a short literature review to introduce the subject. |
Steps to Completing a Literature Review

- Next: Find >>
- Last Updated: Sep 26, 2023 10:25 AM
- URL: https://guides.library.jhu.edu/lit-review

How To Write An A-Grade Literature Review
3 straightforward steps (with examples) + free template.
By: Derek Jansen (MBA) | Expert Reviewed By: Dr. Eunice Rautenbach | October 2019
Quality research is about building onto the existing work of others , “standing on the shoulders of giants”, as Newton put it. The literature review chapter of your dissertation, thesis or research project is where you synthesise this prior work and lay the theoretical foundation for your own research.
Long story short, this chapter is a pretty big deal, which is why you want to make sure you get it right . In this post, I’ll show you exactly how to write a literature review in three straightforward steps, so you can conquer this vital chapter (the smart way).
Overview: The Literature Review Process
- Understanding the “ why “
- Finding the relevant literature
- Cataloguing and synthesising the information
- Outlining & writing up your literature review
- Example of a literature review
But first, the “why”…
Before we unpack how to write the literature review chapter, we’ve got to look at the why . To put it bluntly, if you don’t understand the function and purpose of the literature review process, there’s no way you can pull it off well. So, what exactly is the purpose of the literature review?
Well, there are (at least) four core functions:
- For you to gain an understanding (and demonstrate this understanding) of where the research is at currently, what the key arguments and disagreements are.
- For you to identify the gap(s) in the literature and then use this as justification for your own research topic.
- To help you build a conceptual framework for empirical testing (if applicable to your research topic).
- To inform your methodological choices and help you source tried and tested questionnaires (for interviews ) and measurement instruments (for surveys ).
Most students understand the first point but don’t give any thought to the rest. To get the most from the literature review process, you must keep all four points front of mind as you review the literature (more on this shortly), or you’ll land up with a wonky foundation.
Okay – with the why out the way, let’s move on to the how . As mentioned above, writing your literature review is a process, which I’ll break down into three steps:
- Finding the most suitable literature
- Understanding , distilling and organising the literature
- Planning and writing up your literature review chapter
Importantly, you must complete steps one and two before you start writing up your chapter. I know it’s very tempting, but don’t try to kill two birds with one stone and write as you read. You’ll invariably end up wasting huge amounts of time re-writing and re-shaping, or you’ll just land up with a disjointed, hard-to-digest mess . Instead, you need to read first and distil the information, then plan and execute the writing.

Step 1: Find the relevant literature
Naturally, the first step in the literature review journey is to hunt down the existing research that’s relevant to your topic. While you probably already have a decent base of this from your research proposal , you need to expand on this substantially in the dissertation or thesis itself.
Essentially, you need to be looking for any existing literature that potentially helps you answer your research question (or develop it, if that’s not yet pinned down). There are numerous ways to find relevant literature, but I’ll cover my top four tactics here. I’d suggest combining all four methods to ensure that nothing slips past you:
Method 1 – Google Scholar Scrubbing
Google’s academic search engine, Google Scholar , is a great starting point as it provides a good high-level view of the relevant journal articles for whatever keyword you throw at it. Most valuably, it tells you how many times each article has been cited, which gives you an idea of how credible (or at least, popular) it is. Some articles will be free to access, while others will require an account, which brings us to the next method.
Method 2 – University Database Scrounging
Generally, universities provide students with access to an online library, which provides access to many (but not all) of the major journals.
So, if you find an article using Google Scholar that requires paid access (which is quite likely), search for that article in your university’s database – if it’s listed there, you’ll have access. Note that, generally, the search engine capabilities of these databases are poor, so make sure you search for the exact article name, or you might not find it.
Method 3 – Journal Article Snowballing
At the end of every academic journal article, you’ll find a list of references. As with any academic writing, these references are the building blocks of the article, so if the article is relevant to your topic, there’s a good chance a portion of the referenced works will be too. Do a quick scan of the titles and see what seems relevant, then search for the relevant ones in your university’s database.
Method 4 – Dissertation Scavenging
Similar to Method 3 above, you can leverage other students’ dissertations. All you have to do is skim through literature review chapters of existing dissertations related to your topic and you’ll find a gold mine of potential literature. Usually, your university will provide you with access to previous students’ dissertations, but you can also find a much larger selection in the following databases:
- Open Access Theses & Dissertations
- Stanford SearchWorks
Keep in mind that dissertations and theses are not as academically sound as published, peer-reviewed journal articles (because they’re written by students, not professionals), so be sure to check the credibility of any sources you find using this method. You can do this by assessing the citation count of any given article in Google Scholar. If you need help with assessing the credibility of any article, or with finding relevant research in general, you can chat with one of our Research Specialists .
Alright – with a good base of literature firmly under your belt, it’s time to move onto the next step.
Need a helping hand?
Step 2: Log, catalogue and synthesise
Once you’ve built a little treasure trove of articles, it’s time to get reading and start digesting the information – what does it all mean?
While I present steps one and two (hunting and digesting) as sequential, in reality, it’s more of a back-and-forth tango – you’ll read a little , then have an idea, spot a new citation, or a new potential variable, and then go back to searching for articles. This is perfectly natural – through the reading process, your thoughts will develop , new avenues might crop up, and directional adjustments might arise. This is, after all, one of the main purposes of the literature review process (i.e. to familiarise yourself with the current state of research in your field).
As you’re working through your treasure chest, it’s essential that you simultaneously start organising the information. There are three aspects to this:
- Logging reference information
- Building an organised catalogue
- Distilling and synthesising the information
I’ll discuss each of these below:
2.1 – Log the reference information
As you read each article, you should add it to your reference management software. I usually recommend Mendeley for this purpose (see the Mendeley 101 video below), but you can use whichever software you’re comfortable with. Most importantly, make sure you load EVERY article you read into your reference manager, even if it doesn’t seem very relevant at the time.
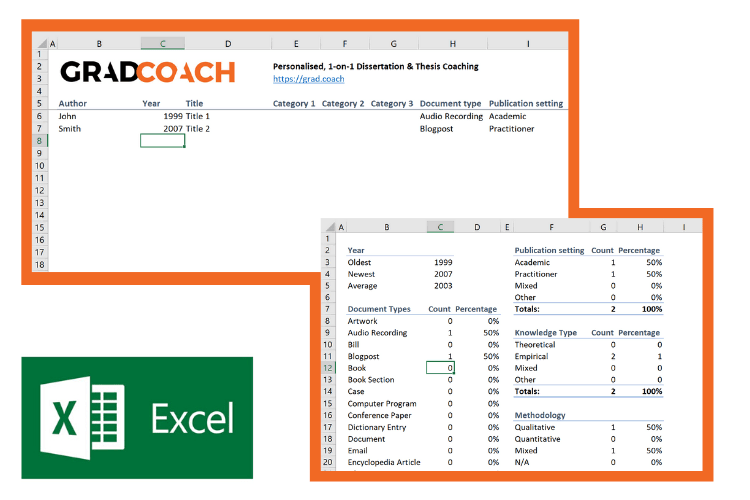
2.2 – Build an organised catalogue
In the beginning, you might feel confident that you can remember who said what, where, and what their main arguments were. Trust me, you won’t. If you do a thorough review of the relevant literature (as you must!), you’re going to read many, many articles, and it’s simply impossible to remember who said what, when, and in what context . Also, without the bird’s eye view that a catalogue provides, you’ll miss connections between various articles, and have no view of how the research developed over time. Simply put, it’s essential to build your own catalogue of the literature.
I would suggest using Excel to build your catalogue, as it allows you to run filters, colour code and sort – all very useful when your list grows large (which it will). How you lay your spreadsheet out is up to you, but I’d suggest you have the following columns (at minimum):
- Author, date, title – Start with three columns containing this core information. This will make it easy for you to search for titles with certain words, order research by date, or group by author.
- Categories or keywords – You can either create multiple columns, one for each category/theme and then tick the relevant categories, or you can have one column with keywords.
- Key arguments/points – Use this column to succinctly convey the essence of the article, the key arguments and implications thereof for your research.
- Context – Note the socioeconomic context in which the research was undertaken. For example, US-based, respondents aged 25-35, lower- income, etc. This will be useful for making an argument about gaps in the research.
- Methodology – Note which methodology was used and why. Also, note any issues you feel arise due to the methodology. Again, you can use this to make an argument about gaps in the research.
- Quotations – Note down any quoteworthy lines you feel might be useful later.
- Notes – Make notes about anything not already covered. For example, linkages to or disagreements with other theories, questions raised but unanswered, shortcomings or limitations, and so forth.
If you’d like, you can try out our free catalog template here (see screenshot below).
2.3 – Digest and synthesise
Most importantly, as you work through the literature and build your catalogue, you need to synthesise all the information in your own mind – how does it all fit together? Look for links between the various articles and try to develop a bigger picture view of the state of the research. Some important questions to ask yourself are:
- What answers does the existing research provide to my own research questions ?
- Which points do the researchers agree (and disagree) on?
- How has the research developed over time?
- Where do the gaps in the current research lie?
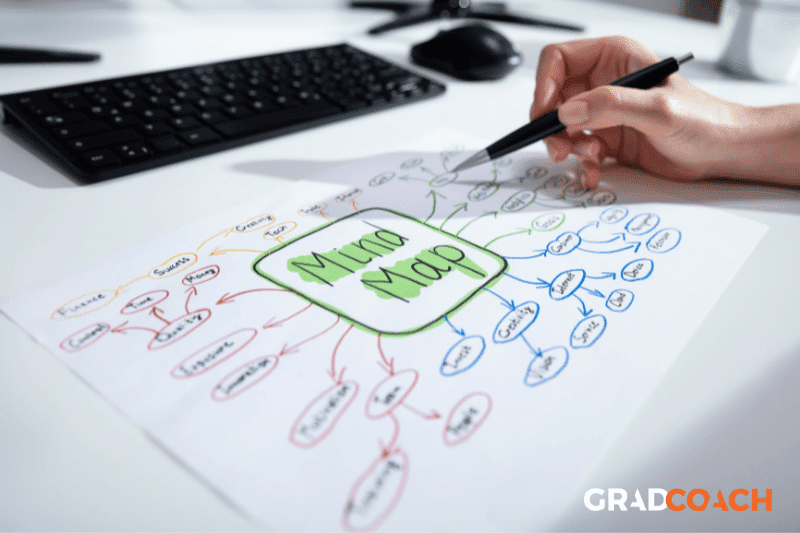
To help you develop a big-picture view and synthesise all the information, you might find mind mapping software such as Freemind useful. Alternatively, if you’re a fan of physical note-taking, investing in a large whiteboard might work for you.
Step 3: Outline and write it up!
Once you’re satisfied that you have digested and distilled all the relevant literature in your mind, it’s time to put pen to paper (or rather, fingers to keyboard). There are two steps here – outlining and writing:
3.1 – Draw up your outline
Having spent so much time reading, it might be tempting to just start writing up without a clear structure in mind. However, it’s critically important to decide on your structure and develop a detailed outline before you write anything. Your literature review chapter needs to present a clear, logical and an easy to follow narrative – and that requires some planning. Don’t try to wing it!
Naturally, you won’t always follow the plan to the letter, but without a detailed outline, you’re more than likely going to end up with a disjointed pile of waffle , and then you’re going to spend a far greater amount of time re-writing, hacking and patching. The adage, “measure twice, cut once” is very suitable here.
In terms of structure, the first decision you’ll have to make is whether you’ll lay out your review thematically (into themes) or chronologically (by date/period). The right choice depends on your topic, research objectives and research questions, which we discuss in this article .
Once that’s decided, you need to draw up an outline of your entire chapter in bullet point format. Try to get as detailed as possible, so that you know exactly what you’ll cover where, how each section will connect to the next, and how your entire argument will develop throughout the chapter. Also, at this stage, it’s a good idea to allocate rough word count limits for each section, so that you can identify word count problems before you’ve spent weeks or months writing!
PS – check out our free literature review chapter template…
3.2 – Get writing
With a detailed outline at your side, it’s time to start writing up (finally!). At this stage, it’s common to feel a bit of writer’s block and find yourself procrastinating under the pressure of finally having to put something on paper. To help with this, remember that the objective of the first draft is not perfection – it’s simply to get your thoughts out of your head and onto paper, after which you can refine them. The structure might change a little, the word count allocations might shift and shuffle, and you might add or remove a section – that’s all okay. Don’t worry about all this on your first draft – just get your thoughts down on paper.

Once you’ve got a full first draft (however rough it may be), step away from it for a day or two (longer if you can) and then come back at it with fresh eyes. Pay particular attention to the flow and narrative – does it fall fit together and flow from one section to another smoothly? Now’s the time to try to improve the linkage from each section to the next, tighten up the writing to be more concise, trim down word count and sand it down into a more digestible read.
Once you’ve done that, give your writing to a friend or colleague who is not a subject matter expert and ask them if they understand the overall discussion. The best way to assess this is to ask them to explain the chapter back to you. This technique will give you a strong indication of which points were clearly communicated and which weren’t. If you’re working with Grad Coach, this is a good time to have your Research Specialist review your chapter.
Finally, tighten it up and send it off to your supervisor for comment. Some might argue that you should be sending your work to your supervisor sooner than this (indeed your university might formally require this), but in my experience, supervisors are extremely short on time (and often patience), so, the more refined your chapter is, the less time they’ll waste on addressing basic issues (which you know about already) and the more time they’ll spend on valuable feedback that will increase your mark-earning potential.
Literature Review Example
In the video below, we unpack an actual literature review so that you can see how all the core components come together in reality.
Let’s Recap
In this post, we’ve covered how to research and write up a high-quality literature review chapter. Let’s do a quick recap of the key takeaways:
- It is essential to understand the WHY of the literature review before you read or write anything. Make sure you understand the 4 core functions of the process.
- The first step is to hunt down the relevant literature . You can do this using Google Scholar, your university database, the snowballing technique and by reviewing other dissertations and theses.
- Next, you need to log all the articles in your reference manager , build your own catalogue of literature and synthesise all the research.
- Following that, you need to develop a detailed outline of your entire chapter – the more detail the better. Don’t start writing without a clear outline (on paper, not in your head!)
- Write up your first draft in rough form – don’t aim for perfection. Remember, done beats perfect.
- Refine your second draft and get a layman’s perspective on it . Then tighten it up and submit it to your supervisor.

Psst… there’s more!
This post is an extract from our bestselling short course, Literature Review Bootcamp . If you want to work smart, you don't want to miss this .
38 Comments
Thank you very much. This page is an eye opener and easy to comprehend.
This is awesome!
I wish I come across GradCoach earlier enough.
But all the same I’ll make use of this opportunity to the fullest.
Thank you for this good job.
Keep it up!
You’re welcome, Yinka. Thank you for the kind words. All the best writing your literature review.
Thank you for a very useful literature review session. Although I am doing most of the steps…it being my first masters an Mphil is a self study and one not sure you are on the right track. I have an amazing supervisor but one also knows they are super busy. So not wanting to bother on the minutae. Thank you.
You’re most welcome, Renee. Good luck with your literature review 🙂
This has been really helpful. Will make full use of it. 🙂
Thank you Gradcoach.
Really agreed. Admirable effort
thank you for this beautiful well explained recap.
Thank you so much for your guide of video and other instructions for the dissertation writing.
It is instrumental. It encouraged me to write a dissertation now.
Thank you the video was great – from someone that knows nothing thankyou
an amazing and very constructive way of presetting a topic, very useful, thanks for the effort,
It is timely
It is very good video of guidance for writing a research proposal and a dissertation. Since I have been watching and reading instructions, I have started my research proposal to write. I appreciate to Mr Jansen hugely.
I learn a lot from your videos. Very comprehensive and detailed.
Thank you for sharing your knowledge. As a research student, you learn better with your learning tips in research
I was really stuck in reading and gathering information but after watching these things are cleared thanks, it is so helpful.
Really helpful, Thank you for the effort in showing such information
This is super helpful thank you very much.
Thank you for this whole literature writing review.You have simplified the process.
I’m so glad I found GradCoach. Excellent information, Clear explanation, and Easy to follow, Many thanks Derek!
You’re welcome, Maithe. Good luck writing your literature review 🙂
Thank you Coach, you have greatly enriched and improved my knowledge
Great piece, so enriching and it is going to help me a great lot in my project and thesis, thanks so much
This is THE BEST site for ANYONE doing a masters or doctorate! Thank you for the sound advice and templates. You rock!
Thanks, Stephanie 🙂
This is mind blowing, the detailed explanation and simplicity is perfect.
I am doing two papers on my final year thesis, and I must stay I feel very confident to face both headlong after reading this article.
thank you so much.
if anyone is to get a paper done on time and in the best way possible, GRADCOACH is certainly the go to area!
This is very good video which is well explained with detailed explanation
Thank you excellent piece of work and great mentoring
Thanks, it was useful
Thank you very much. the video and the information were very helpful.
Good morning scholar. I’m delighted coming to know you even before the commencement of my dissertation which hopefully is expected in not more than six months from now. I would love to engage my study under your guidance from the beginning to the end. I love to know how to do good job
Thank you so much Derek for such useful information on writing up a good literature review. I am at a stage where I need to start writing my one. My proposal was accepted late last year but I honestly did not know where to start
Like the name of your YouTube implies you are GRAD (great,resource person, about dissertation). In short you are smart enough in coaching research work.
This is a very well thought out webpage. Very informative and a great read.
Very timely.
I appreciate.
Very comprehensive and eye opener for me as beginner in postgraduate study. Well explained and easy to understand. Appreciate and good reference in guiding me in my research journey. Thank you
Thank you. I requested to download the free literature review template, however, your website wouldn’t allow me to complete the request or complete a download. May I request that you email me the free template? Thank you.
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly

Library Guides
Literature reviews: criticality.
- Criticality
Express Critical Analysis
The literature review of a dissertation should include critical analysis. You cannot simply juxtapose the literature you find: you have to evaluate and draw conclusions from it.
Paragraph level
Try expressing your voice in each paragraph of your literature review. Write strong paragraphs. In strong paragraphs your voice can be heard in the topic sentence, development (where you analyse and compare/contrast the sources, sometimes as individual pieces, sometimes in a synthesis) and, even more easily, in the concluding sentence, where you present the "therefore" of the paragraph.
How to express criticality at the paragraph level:
Identify the significance of the sources, and why the points they are making are relevant
Make connections between the sources
Compare and contrast sources, literatures
Accept/adopt points made by the sources, with reasons
Reject the points made by the sources, with reasons (e.g., limitations in the methodology; out of date; limited scope; geographical delimitation)
Indicate the position you are taking in your own work on the theories and concepts presented by the sources
Show how limitations in the existing literature create a research gap for you
Organise the materials, synthesising them in an original way, that sheds new light on the topic.
To find out more about paragraph writing, check out the Assignment Writing Guides.
Literature review level
Try to take ownership of the literature review. Remember the purposes of the review (providing background on the subject you are researching and identifying a gap in the existing literature on this subject). Thus, throughout the review:
Identify the key themes relevant to your subject matter
Identify the most logical and effective order for your themes
Relate the sources back to the dissertation's research question
Shed new light on the topic
Draw conclusions on the existing literature
Identify gaps in the literature
Your literature review should present an argument (which you can recap in the concluding paragraph of the literature review). For instance,
"The literature says/illustrates/reveals that... there are debates in the literature as of... it can be understood from the literature that... however, there are gaps in the literature... the literature does not specifically address (specific sector/location/population)... there is a lack of independent/recent studies on... therefore in order to answer the research question(s) (you can repeat the question) this dissertation uses method xyz, as illustrated in the next section (if applicable)".
Manchester University’s academic phrase bank is a great resource for learning new words and phrases.
Extra Resources
For extra help with all aspects of study skills including how to undertake literature reviews, appointments are available with learning advisors on Engage.
Appointments are also available with an Academic Engagement Librarian to discuss any issues you might be having with research.
- << Previous: Synthesis
- Last Updated: Nov 18, 2023 10:56 PM
- URL: https://libguides.westminster.ac.uk/literature-reviews
CONNECT WITH US
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Lau F, Kuziemsky C, editors. Handbook of eHealth Evaluation: An Evidence-based Approach [Internet]. Victoria (BC): University of Victoria; 2017 Feb 27.

Handbook of eHealth Evaluation: An Evidence-based Approach [Internet].
Chapter 9 methods for literature reviews.
Guy Paré and Spyros Kitsiou .
9.1. Introduction
Literature reviews play a critical role in scholarship because science remains, first and foremost, a cumulative endeavour ( vom Brocke et al., 2009 ). As in any academic discipline, rigorous knowledge syntheses are becoming indispensable in keeping up with an exponentially growing eHealth literature, assisting practitioners, academics, and graduate students in finding, evaluating, and synthesizing the contents of many empirical and conceptual papers. Among other methods, literature reviews are essential for: (a) identifying what has been written on a subject or topic; (b) determining the extent to which a specific research area reveals any interpretable trends or patterns; (c) aggregating empirical findings related to a narrow research question to support evidence-based practice; (d) generating new frameworks and theories; and (e) identifying topics or questions requiring more investigation ( Paré, Trudel, Jaana, & Kitsiou, 2015 ).
Literature reviews can take two major forms. The most prevalent one is the “literature review” or “background” section within a journal paper or a chapter in a graduate thesis. This section synthesizes the extant literature and usually identifies the gaps in knowledge that the empirical study addresses ( Sylvester, Tate, & Johnstone, 2013 ). It may also provide a theoretical foundation for the proposed study, substantiate the presence of the research problem, justify the research as one that contributes something new to the cumulated knowledge, or validate the methods and approaches for the proposed study ( Hart, 1998 ; Levy & Ellis, 2006 ).
The second form of literature review, which is the focus of this chapter, constitutes an original and valuable work of research in and of itself ( Paré et al., 2015 ). Rather than providing a base for a researcher’s own work, it creates a solid starting point for all members of the community interested in a particular area or topic ( Mulrow, 1987 ). The so-called “review article” is a journal-length paper which has an overarching purpose to synthesize the literature in a field, without collecting or analyzing any primary data ( Green, Johnson, & Adams, 2006 ).
When appropriately conducted, review articles represent powerful information sources for practitioners looking for state-of-the art evidence to guide their decision-making and work practices ( Paré et al., 2015 ). Further, high-quality reviews become frequently cited pieces of work which researchers seek out as a first clear outline of the literature when undertaking empirical studies ( Cooper, 1988 ; Rowe, 2014 ). Scholars who track and gauge the impact of articles have found that review papers are cited and downloaded more often than any other type of published article ( Cronin, Ryan, & Coughlan, 2008 ; Montori, Wilczynski, Morgan, Haynes, & Hedges, 2003 ; Patsopoulos, Analatos, & Ioannidis, 2005 ). The reason for their popularity may be the fact that reading the review enables one to have an overview, if not a detailed knowledge of the area in question, as well as references to the most useful primary sources ( Cronin et al., 2008 ). Although they are not easy to conduct, the commitment to complete a review article provides a tremendous service to one’s academic community ( Paré et al., 2015 ; Petticrew & Roberts, 2006 ). Most, if not all, peer-reviewed journals in the fields of medical informatics publish review articles of some type.
The main objectives of this chapter are fourfold: (a) to provide an overview of the major steps and activities involved in conducting a stand-alone literature review; (b) to describe and contrast the different types of review articles that can contribute to the eHealth knowledge base; (c) to illustrate each review type with one or two examples from the eHealth literature; and (d) to provide a series of recommendations for prospective authors of review articles in this domain.
9.2. Overview of the Literature Review Process and Steps
As explained in Templier and Paré (2015) , there are six generic steps involved in conducting a review article:
- formulating the research question(s) and objective(s),
- searching the extant literature,
- screening for inclusion,
- assessing the quality of primary studies,
- extracting data, and
- analyzing data.
Although these steps are presented here in sequential order, one must keep in mind that the review process can be iterative and that many activities can be initiated during the planning stage and later refined during subsequent phases ( Finfgeld-Connett & Johnson, 2013 ; Kitchenham & Charters, 2007 ).
Formulating the research question(s) and objective(s): As a first step, members of the review team must appropriately justify the need for the review itself ( Petticrew & Roberts, 2006 ), identify the review’s main objective(s) ( Okoli & Schabram, 2010 ), and define the concepts or variables at the heart of their synthesis ( Cooper & Hedges, 2009 ; Webster & Watson, 2002 ). Importantly, they also need to articulate the research question(s) they propose to investigate ( Kitchenham & Charters, 2007 ). In this regard, we concur with Jesson, Matheson, and Lacey (2011) that clearly articulated research questions are key ingredients that guide the entire review methodology; they underscore the type of information that is needed, inform the search for and selection of relevant literature, and guide or orient the subsequent analysis. Searching the extant literature: The next step consists of searching the literature and making decisions about the suitability of material to be considered in the review ( Cooper, 1988 ). There exist three main coverage strategies. First, exhaustive coverage means an effort is made to be as comprehensive as possible in order to ensure that all relevant studies, published and unpublished, are included in the review and, thus, conclusions are based on this all-inclusive knowledge base. The second type of coverage consists of presenting materials that are representative of most other works in a given field or area. Often authors who adopt this strategy will search for relevant articles in a small number of top-tier journals in a field ( Paré et al., 2015 ). In the third strategy, the review team concentrates on prior works that have been central or pivotal to a particular topic. This may include empirical studies or conceptual papers that initiated a line of investigation, changed how problems or questions were framed, introduced new methods or concepts, or engendered important debate ( Cooper, 1988 ). Screening for inclusion: The following step consists of evaluating the applicability of the material identified in the preceding step ( Levy & Ellis, 2006 ; vom Brocke et al., 2009 ). Once a group of potential studies has been identified, members of the review team must screen them to determine their relevance ( Petticrew & Roberts, 2006 ). A set of predetermined rules provides a basis for including or excluding certain studies. This exercise requires a significant investment on the part of researchers, who must ensure enhanced objectivity and avoid biases or mistakes. As discussed later in this chapter, for certain types of reviews there must be at least two independent reviewers involved in the screening process and a procedure to resolve disagreements must also be in place ( Liberati et al., 2009 ; Shea et al., 2009 ). Assessing the quality of primary studies: In addition to screening material for inclusion, members of the review team may need to assess the scientific quality of the selected studies, that is, appraise the rigour of the research design and methods. Such formal assessment, which is usually conducted independently by at least two coders, helps members of the review team refine which studies to include in the final sample, determine whether or not the differences in quality may affect their conclusions, or guide how they analyze the data and interpret the findings ( Petticrew & Roberts, 2006 ). Ascribing quality scores to each primary study or considering through domain-based evaluations which study components have or have not been designed and executed appropriately makes it possible to reflect on the extent to which the selected study addresses possible biases and maximizes validity ( Shea et al., 2009 ). Extracting data: The following step involves gathering or extracting applicable information from each primary study included in the sample and deciding what is relevant to the problem of interest ( Cooper & Hedges, 2009 ). Indeed, the type of data that should be recorded mainly depends on the initial research questions ( Okoli & Schabram, 2010 ). However, important information may also be gathered about how, when, where and by whom the primary study was conducted, the research design and methods, or qualitative/quantitative results ( Cooper & Hedges, 2009 ). Analyzing and synthesizing data : As a final step, members of the review team must collate, summarize, aggregate, organize, and compare the evidence extracted from the included studies. The extracted data must be presented in a meaningful way that suggests a new contribution to the extant literature ( Jesson et al., 2011 ). Webster and Watson (2002) warn researchers that literature reviews should be much more than lists of papers and should provide a coherent lens to make sense of extant knowledge on a given topic. There exist several methods and techniques for synthesizing quantitative (e.g., frequency analysis, meta-analysis) and qualitative (e.g., grounded theory, narrative analysis, meta-ethnography) evidence ( Dixon-Woods, Agarwal, Jones, Young, & Sutton, 2005 ; Thomas & Harden, 2008 ).
9.3. Types of Review Articles and Brief Illustrations
EHealth researchers have at their disposal a number of approaches and methods for making sense out of existing literature, all with the purpose of casting current research findings into historical contexts or explaining contradictions that might exist among a set of primary research studies conducted on a particular topic. Our classification scheme is largely inspired from Paré and colleagues’ (2015) typology. Below we present and illustrate those review types that we feel are central to the growth and development of the eHealth domain.
9.3.1. Narrative Reviews
The narrative review is the “traditional” way of reviewing the extant literature and is skewed towards a qualitative interpretation of prior knowledge ( Sylvester et al., 2013 ). Put simply, a narrative review attempts to summarize or synthesize what has been written on a particular topic but does not seek generalization or cumulative knowledge from what is reviewed ( Davies, 2000 ; Green et al., 2006 ). Instead, the review team often undertakes the task of accumulating and synthesizing the literature to demonstrate the value of a particular point of view ( Baumeister & Leary, 1997 ). As such, reviewers may selectively ignore or limit the attention paid to certain studies in order to make a point. In this rather unsystematic approach, the selection of information from primary articles is subjective, lacks explicit criteria for inclusion and can lead to biased interpretations or inferences ( Green et al., 2006 ). There are several narrative reviews in the particular eHealth domain, as in all fields, which follow such an unstructured approach ( Silva et al., 2015 ; Paul et al., 2015 ).
Despite these criticisms, this type of review can be very useful in gathering together a volume of literature in a specific subject area and synthesizing it. As mentioned above, its primary purpose is to provide the reader with a comprehensive background for understanding current knowledge and highlighting the significance of new research ( Cronin et al., 2008 ). Faculty like to use narrative reviews in the classroom because they are often more up to date than textbooks, provide a single source for students to reference, and expose students to peer-reviewed literature ( Green et al., 2006 ). For researchers, narrative reviews can inspire research ideas by identifying gaps or inconsistencies in a body of knowledge, thus helping researchers to determine research questions or formulate hypotheses. Importantly, narrative reviews can also be used as educational articles to bring practitioners up to date with certain topics of issues ( Green et al., 2006 ).
Recently, there have been several efforts to introduce more rigour in narrative reviews that will elucidate common pitfalls and bring changes into their publication standards. Information systems researchers, among others, have contributed to advancing knowledge on how to structure a “traditional” review. For instance, Levy and Ellis (2006) proposed a generic framework for conducting such reviews. Their model follows the systematic data processing approach comprised of three steps, namely: (a) literature search and screening; (b) data extraction and analysis; and (c) writing the literature review. They provide detailed and very helpful instructions on how to conduct each step of the review process. As another methodological contribution, vom Brocke et al. (2009) offered a series of guidelines for conducting literature reviews, with a particular focus on how to search and extract the relevant body of knowledge. Last, Bandara, Miskon, and Fielt (2011) proposed a structured, predefined and tool-supported method to identify primary studies within a feasible scope, extract relevant content from identified articles, synthesize and analyze the findings, and effectively write and present the results of the literature review. We highly recommend that prospective authors of narrative reviews consult these useful sources before embarking on their work.
Darlow and Wen (2015) provide a good example of a highly structured narrative review in the eHealth field. These authors synthesized published articles that describe the development process of mobile health ( m-health ) interventions for patients’ cancer care self-management. As in most narrative reviews, the scope of the research questions being investigated is broad: (a) how development of these systems are carried out; (b) which methods are used to investigate these systems; and (c) what conclusions can be drawn as a result of the development of these systems. To provide clear answers to these questions, a literature search was conducted on six electronic databases and Google Scholar . The search was performed using several terms and free text words, combining them in an appropriate manner. Four inclusion and three exclusion criteria were utilized during the screening process. Both authors independently reviewed each of the identified articles to determine eligibility and extract study information. A flow diagram shows the number of studies identified, screened, and included or excluded at each stage of study selection. In terms of contributions, this review provides a series of practical recommendations for m-health intervention development.
9.3.2. Descriptive or Mapping Reviews
The primary goal of a descriptive review is to determine the extent to which a body of knowledge in a particular research topic reveals any interpretable pattern or trend with respect to pre-existing propositions, theories, methodologies or findings ( King & He, 2005 ; Paré et al., 2015 ). In contrast with narrative reviews, descriptive reviews follow a systematic and transparent procedure, including searching, screening and classifying studies ( Petersen, Vakkalanka, & Kuzniarz, 2015 ). Indeed, structured search methods are used to form a representative sample of a larger group of published works ( Paré et al., 2015 ). Further, authors of descriptive reviews extract from each study certain characteristics of interest, such as publication year, research methods, data collection techniques, and direction or strength of research outcomes (e.g., positive, negative, or non-significant) in the form of frequency analysis to produce quantitative results ( Sylvester et al., 2013 ). In essence, each study included in a descriptive review is treated as the unit of analysis and the published literature as a whole provides a database from which the authors attempt to identify any interpretable trends or draw overall conclusions about the merits of existing conceptualizations, propositions, methods or findings ( Paré et al., 2015 ). In doing so, a descriptive review may claim that its findings represent the state of the art in a particular domain ( King & He, 2005 ).
In the fields of health sciences and medical informatics, reviews that focus on examining the range, nature and evolution of a topic area are described by Anderson, Allen, Peckham, and Goodwin (2008) as mapping reviews . Like descriptive reviews, the research questions are generic and usually relate to publication patterns and trends. There is no preconceived plan to systematically review all of the literature although this can be done. Instead, researchers often present studies that are representative of most works published in a particular area and they consider a specific time frame to be mapped.
An example of this approach in the eHealth domain is offered by DeShazo, Lavallie, and Wolf (2009). The purpose of this descriptive or mapping review was to characterize publication trends in the medical informatics literature over a 20-year period (1987 to 2006). To achieve this ambitious objective, the authors performed a bibliometric analysis of medical informatics citations indexed in medline using publication trends, journal frequencies, impact factors, Medical Subject Headings (MeSH) term frequencies, and characteristics of citations. Findings revealed that there were over 77,000 medical informatics articles published during the covered period in numerous journals and that the average annual growth rate was 12%. The MeSH term analysis also suggested a strong interdisciplinary trend. Finally, average impact scores increased over time with two notable growth periods. Overall, patterns in research outputs that seem to characterize the historic trends and current components of the field of medical informatics suggest it may be a maturing discipline (DeShazo et al., 2009).
9.3.3. Scoping Reviews
Scoping reviews attempt to provide an initial indication of the potential size and nature of the extant literature on an emergent topic (Arksey & O’Malley, 2005; Daudt, van Mossel, & Scott, 2013 ; Levac, Colquhoun, & O’Brien, 2010). A scoping review may be conducted to examine the extent, range and nature of research activities in a particular area, determine the value of undertaking a full systematic review (discussed next), or identify research gaps in the extant literature ( Paré et al., 2015 ). In line with their main objective, scoping reviews usually conclude with the presentation of a detailed research agenda for future works along with potential implications for both practice and research.
Unlike narrative and descriptive reviews, the whole point of scoping the field is to be as comprehensive as possible, including grey literature (Arksey & O’Malley, 2005). Inclusion and exclusion criteria must be established to help researchers eliminate studies that are not aligned with the research questions. It is also recommended that at least two independent coders review abstracts yielded from the search strategy and then the full articles for study selection ( Daudt et al., 2013 ). The synthesized evidence from content or thematic analysis is relatively easy to present in tabular form (Arksey & O’Malley, 2005; Thomas & Harden, 2008 ).
One of the most highly cited scoping reviews in the eHealth domain was published by Archer, Fevrier-Thomas, Lokker, McKibbon, and Straus (2011) . These authors reviewed the existing literature on personal health record ( phr ) systems including design, functionality, implementation, applications, outcomes, and benefits. Seven databases were searched from 1985 to March 2010. Several search terms relating to phr s were used during this process. Two authors independently screened titles and abstracts to determine inclusion status. A second screen of full-text articles, again by two independent members of the research team, ensured that the studies described phr s. All in all, 130 articles met the criteria and their data were extracted manually into a database. The authors concluded that although there is a large amount of survey, observational, cohort/panel, and anecdotal evidence of phr benefits and satisfaction for patients, more research is needed to evaluate the results of phr implementations. Their in-depth analysis of the literature signalled that there is little solid evidence from randomized controlled trials or other studies through the use of phr s. Hence, they suggested that more research is needed that addresses the current lack of understanding of optimal functionality and usability of these systems, and how they can play a beneficial role in supporting patient self-management ( Archer et al., 2011 ).
9.3.4. Forms of Aggregative Reviews
Healthcare providers, practitioners, and policy-makers are nowadays overwhelmed with large volumes of information, including research-based evidence from numerous clinical trials and evaluation studies, assessing the effectiveness of health information technologies and interventions ( Ammenwerth & de Keizer, 2004 ; Deshazo et al., 2009 ). It is unrealistic to expect that all these disparate actors will have the time, skills, and necessary resources to identify the available evidence in the area of their expertise and consider it when making decisions. Systematic reviews that involve the rigorous application of scientific strategies aimed at limiting subjectivity and bias (i.e., systematic and random errors) can respond to this challenge.
Systematic reviews attempt to aggregate, appraise, and synthesize in a single source all empirical evidence that meet a set of previously specified eligibility criteria in order to answer a clearly formulated and often narrow research question on a particular topic of interest to support evidence-based practice ( Liberati et al., 2009 ). They adhere closely to explicit scientific principles ( Liberati et al., 2009 ) and rigorous methodological guidelines (Higgins & Green, 2008) aimed at reducing random and systematic errors that can lead to deviations from the truth in results or inferences. The use of explicit methods allows systematic reviews to aggregate a large body of research evidence, assess whether effects or relationships are in the same direction and of the same general magnitude, explain possible inconsistencies between study results, and determine the strength of the overall evidence for every outcome of interest based on the quality of included studies and the general consistency among them ( Cook, Mulrow, & Haynes, 1997 ). The main procedures of a systematic review involve:
- Formulating a review question and developing a search strategy based on explicit inclusion criteria for the identification of eligible studies (usually described in the context of a detailed review protocol).
- Searching for eligible studies using multiple databases and information sources, including grey literature sources, without any language restrictions.
- Selecting studies, extracting data, and assessing risk of bias in a duplicate manner using two independent reviewers to avoid random or systematic errors in the process.
- Analyzing data using quantitative or qualitative methods.
- Presenting results in summary of findings tables.
- Interpreting results and drawing conclusions.
Many systematic reviews, but not all, use statistical methods to combine the results of independent studies into a single quantitative estimate or summary effect size. Known as meta-analyses , these reviews use specific data extraction and statistical techniques (e.g., network, frequentist, or Bayesian meta-analyses) to calculate from each study by outcome of interest an effect size along with a confidence interval that reflects the degree of uncertainty behind the point estimate of effect ( Borenstein, Hedges, Higgins, & Rothstein, 2009 ; Deeks, Higgins, & Altman, 2008 ). Subsequently, they use fixed or random-effects analysis models to combine the results of the included studies, assess statistical heterogeneity, and calculate a weighted average of the effect estimates from the different studies, taking into account their sample sizes. The summary effect size is a value that reflects the average magnitude of the intervention effect for a particular outcome of interest or, more generally, the strength of a relationship between two variables across all studies included in the systematic review. By statistically combining data from multiple studies, meta-analyses can create more precise and reliable estimates of intervention effects than those derived from individual studies alone, when these are examined independently as discrete sources of information.
The review by Gurol-Urganci, de Jongh, Vodopivec-Jamsek, Atun, and Car (2013) on the effects of mobile phone messaging reminders for attendance at healthcare appointments is an illustrative example of a high-quality systematic review with meta-analysis. Missed appointments are a major cause of inefficiency in healthcare delivery with substantial monetary costs to health systems. These authors sought to assess whether mobile phone-based appointment reminders delivered through Short Message Service ( sms ) or Multimedia Messaging Service ( mms ) are effective in improving rates of patient attendance and reducing overall costs. To this end, they conducted a comprehensive search on multiple databases using highly sensitive search strategies without language or publication-type restrictions to identify all rct s that are eligible for inclusion. In order to minimize the risk of omitting eligible studies not captured by the original search, they supplemented all electronic searches with manual screening of trial registers and references contained in the included studies. Study selection, data extraction, and risk of bias assessments were performed independently by two coders using standardized methods to ensure consistency and to eliminate potential errors. Findings from eight rct s involving 6,615 participants were pooled into meta-analyses to calculate the magnitude of effects that mobile text message reminders have on the rate of attendance at healthcare appointments compared to no reminders and phone call reminders.
Meta-analyses are regarded as powerful tools for deriving meaningful conclusions. However, there are situations in which it is neither reasonable nor appropriate to pool studies together using meta-analytic methods simply because there is extensive clinical heterogeneity between the included studies or variation in measurement tools, comparisons, or outcomes of interest. In these cases, systematic reviews can use qualitative synthesis methods such as vote counting, content analysis, classification schemes and tabulations, as an alternative approach to narratively synthesize the results of the independent studies included in the review. This form of review is known as qualitative systematic review.
A rigorous example of one such review in the eHealth domain is presented by Mickan, Atherton, Roberts, Heneghan, and Tilson (2014) on the use of handheld computers by healthcare professionals and their impact on access to information and clinical decision-making. In line with the methodological guidelines for systematic reviews, these authors: (a) developed and registered with prospero ( www.crd.york.ac.uk/ prospero / ) an a priori review protocol; (b) conducted comprehensive searches for eligible studies using multiple databases and other supplementary strategies (e.g., forward searches); and (c) subsequently carried out study selection, data extraction, and risk of bias assessments in a duplicate manner to eliminate potential errors in the review process. Heterogeneity between the included studies in terms of reported outcomes and measures precluded the use of meta-analytic methods. To this end, the authors resorted to using narrative analysis and synthesis to describe the effectiveness of handheld computers on accessing information for clinical knowledge, adherence to safety and clinical quality guidelines, and diagnostic decision-making.
In recent years, the number of systematic reviews in the field of health informatics has increased considerably. Systematic reviews with discordant findings can cause great confusion and make it difficult for decision-makers to interpret the review-level evidence ( Moher, 2013 ). Therefore, there is a growing need for appraisal and synthesis of prior systematic reviews to ensure that decision-making is constantly informed by the best available accumulated evidence. Umbrella reviews , also known as overviews of systematic reviews, are tertiary types of evidence synthesis that aim to accomplish this; that is, they aim to compare and contrast findings from multiple systematic reviews and meta-analyses ( Becker & Oxman, 2008 ). Umbrella reviews generally adhere to the same principles and rigorous methodological guidelines used in systematic reviews. However, the unit of analysis in umbrella reviews is the systematic review rather than the primary study ( Becker & Oxman, 2008 ). Unlike systematic reviews that have a narrow focus of inquiry, umbrella reviews focus on broader research topics for which there are several potential interventions ( Smith, Devane, Begley, & Clarke, 2011 ). A recent umbrella review on the effects of home telemonitoring interventions for patients with heart failure critically appraised, compared, and synthesized evidence from 15 systematic reviews to investigate which types of home telemonitoring technologies and forms of interventions are more effective in reducing mortality and hospital admissions ( Kitsiou, Paré, & Jaana, 2015 ).
9.3.5. Realist Reviews
Realist reviews are theory-driven interpretative reviews developed to inform, enhance, or supplement conventional systematic reviews by making sense of heterogeneous evidence about complex interventions applied in diverse contexts in a way that informs policy decision-making ( Greenhalgh, Wong, Westhorp, & Pawson, 2011 ). They originated from criticisms of positivist systematic reviews which centre on their “simplistic” underlying assumptions ( Oates, 2011 ). As explained above, systematic reviews seek to identify causation. Such logic is appropriate for fields like medicine and education where findings of randomized controlled trials can be aggregated to see whether a new treatment or intervention does improve outcomes. However, many argue that it is not possible to establish such direct causal links between interventions and outcomes in fields such as social policy, management, and information systems where for any intervention there is unlikely to be a regular or consistent outcome ( Oates, 2011 ; Pawson, 2006 ; Rousseau, Manning, & Denyer, 2008 ).
To circumvent these limitations, Pawson, Greenhalgh, Harvey, and Walshe (2005) have proposed a new approach for synthesizing knowledge that seeks to unpack the mechanism of how “complex interventions” work in particular contexts. The basic research question — what works? — which is usually associated with systematic reviews changes to: what is it about this intervention that works, for whom, in what circumstances, in what respects and why? Realist reviews have no particular preference for either quantitative or qualitative evidence. As a theory-building approach, a realist review usually starts by articulating likely underlying mechanisms and then scrutinizes available evidence to find out whether and where these mechanisms are applicable ( Shepperd et al., 2009 ). Primary studies found in the extant literature are viewed as case studies which can test and modify the initial theories ( Rousseau et al., 2008 ).
The main objective pursued in the realist review conducted by Otte-Trojel, de Bont, Rundall, and van de Klundert (2014) was to examine how patient portals contribute to health service delivery and patient outcomes. The specific goals were to investigate how outcomes are produced and, most importantly, how variations in outcomes can be explained. The research team started with an exploratory review of background documents and research studies to identify ways in which patient portals may contribute to health service delivery and patient outcomes. The authors identified six main ways which represent “educated guesses” to be tested against the data in the evaluation studies. These studies were identified through a formal and systematic search in four databases between 2003 and 2013. Two members of the research team selected the articles using a pre-established list of inclusion and exclusion criteria and following a two-step procedure. The authors then extracted data from the selected articles and created several tables, one for each outcome category. They organized information to bring forward those mechanisms where patient portals contribute to outcomes and the variation in outcomes across different contexts.
9.3.6. Critical Reviews
Lastly, critical reviews aim to provide a critical evaluation and interpretive analysis of existing literature on a particular topic of interest to reveal strengths, weaknesses, contradictions, controversies, inconsistencies, and/or other important issues with respect to theories, hypotheses, research methods or results ( Baumeister & Leary, 1997 ; Kirkevold, 1997 ). Unlike other review types, critical reviews attempt to take a reflective account of the research that has been done in a particular area of interest, and assess its credibility by using appraisal instruments or critical interpretive methods. In this way, critical reviews attempt to constructively inform other scholars about the weaknesses of prior research and strengthen knowledge development by giving focus and direction to studies for further improvement ( Kirkevold, 1997 ).
Kitsiou, Paré, and Jaana (2013) provide an example of a critical review that assessed the methodological quality of prior systematic reviews of home telemonitoring studies for chronic patients. The authors conducted a comprehensive search on multiple databases to identify eligible reviews and subsequently used a validated instrument to conduct an in-depth quality appraisal. Results indicate that the majority of systematic reviews in this particular area suffer from important methodological flaws and biases that impair their internal validity and limit their usefulness for clinical and decision-making purposes. To this end, they provide a number of recommendations to strengthen knowledge development towards improving the design and execution of future reviews on home telemonitoring.
9.4. Summary
Table 9.1 outlines the main types of literature reviews that were described in the previous sub-sections and summarizes the main characteristics that distinguish one review type from another. It also includes key references to methodological guidelines and useful sources that can be used by eHealth scholars and researchers for planning and developing reviews.
Typology of Literature Reviews (adapted from Paré et al., 2015).
As shown in Table 9.1 , each review type addresses different kinds of research questions or objectives, which subsequently define and dictate the methods and approaches that need to be used to achieve the overarching goal(s) of the review. For example, in the case of narrative reviews, there is greater flexibility in searching and synthesizing articles ( Green et al., 2006 ). Researchers are often relatively free to use a diversity of approaches to search, identify, and select relevant scientific articles, describe their operational characteristics, present how the individual studies fit together, and formulate conclusions. On the other hand, systematic reviews are characterized by their high level of systematicity, rigour, and use of explicit methods, based on an “a priori” review plan that aims to minimize bias in the analysis and synthesis process (Higgins & Green, 2008). Some reviews are exploratory in nature (e.g., scoping/mapping reviews), whereas others may be conducted to discover patterns (e.g., descriptive reviews) or involve a synthesis approach that may include the critical analysis of prior research ( Paré et al., 2015 ). Hence, in order to select the most appropriate type of review, it is critical to know before embarking on a review project, why the research synthesis is conducted and what type of methods are best aligned with the pursued goals.
9.5. Concluding Remarks
In light of the increased use of evidence-based practice and research generating stronger evidence ( Grady et al., 2011 ; Lyden et al., 2013 ), review articles have become essential tools for summarizing, synthesizing, integrating or critically appraising prior knowledge in the eHealth field. As mentioned earlier, when rigorously conducted review articles represent powerful information sources for eHealth scholars and practitioners looking for state-of-the-art evidence. The typology of literature reviews we used herein will allow eHealth researchers, graduate students and practitioners to gain a better understanding of the similarities and differences between review types.
We must stress that this classification scheme does not privilege any specific type of review as being of higher quality than another ( Paré et al., 2015 ). As explained above, each type of review has its own strengths and limitations. Having said that, we realize that the methodological rigour of any review — be it qualitative, quantitative or mixed — is a critical aspect that should be considered seriously by prospective authors. In the present context, the notion of rigour refers to the reliability and validity of the review process described in section 9.2. For one thing, reliability is related to the reproducibility of the review process and steps, which is facilitated by a comprehensive documentation of the literature search process, extraction, coding and analysis performed in the review. Whether the search is comprehensive or not, whether it involves a methodical approach for data extraction and synthesis or not, it is important that the review documents in an explicit and transparent manner the steps and approach that were used in the process of its development. Next, validity characterizes the degree to which the review process was conducted appropriately. It goes beyond documentation and reflects decisions related to the selection of the sources, the search terms used, the period of time covered, the articles selected in the search, and the application of backward and forward searches ( vom Brocke et al., 2009 ). In short, the rigour of any review article is reflected by the explicitness of its methods (i.e., transparency) and the soundness of the approach used. We refer those interested in the concepts of rigour and quality to the work of Templier and Paré (2015) which offers a detailed set of methodological guidelines for conducting and evaluating various types of review articles.
To conclude, our main objective in this chapter was to demystify the various types of literature reviews that are central to the continuous development of the eHealth field. It is our hope that our descriptive account will serve as a valuable source for those conducting, evaluating or using reviews in this important and growing domain.
- Ammenwerth E., de Keizer N. An inventory of evaluation studies of information technology in health care. Trends in evaluation research, 1982-2002. International Journal of Medical Informatics. 2004; 44 (1):44–56. [ PubMed : 15778794 ]
- Anderson S., Allen P., Peckham S., Goodwin N. Asking the right questions: scoping studies in the commissioning of research on the organisation and delivery of health services. Health Research Policy and Systems. 2008; 6 (7):1–12. [ PMC free article : PMC2500008 ] [ PubMed : 18613961 ] [ CrossRef ]
- Archer N., Fevrier-Thomas U., Lokker C., McKibbon K. A., Straus S.E. Personal health records: a scoping review. Journal of American Medical Informatics Association. 2011; 18 (4):515–522. [ PMC free article : PMC3128401 ] [ PubMed : 21672914 ]
- Arksey H., O’Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005; 8 (1):19–32.
- A systematic, tool-supported method for conducting literature reviews in information systems. Paper presented at the Proceedings of the 19th European Conference on Information Systems ( ecis 2011); June 9 to 11; Helsinki, Finland. 2011.
- Baumeister R. F., Leary M.R. Writing narrative literature reviews. Review of General Psychology. 1997; 1 (3):311–320.
- Becker L. A., Oxman A.D. In: Cochrane handbook for systematic reviews of interventions. Higgins J. P. T., Green S., editors. Hoboken, nj : John Wiley & Sons, Ltd; 2008. Overviews of reviews; pp. 607–631.
- Borenstein M., Hedges L., Higgins J., Rothstein H. Introduction to meta-analysis. Hoboken, nj : John Wiley & Sons Inc; 2009.
- Cook D. J., Mulrow C. D., Haynes B. Systematic reviews: Synthesis of best evidence for clinical decisions. Annals of Internal Medicine. 1997; 126 (5):376–380. [ PubMed : 9054282 ]
- Cooper H., Hedges L.V. In: The handbook of research synthesis and meta-analysis. 2nd ed. Cooper H., Hedges L. V., Valentine J. C., editors. New York: Russell Sage Foundation; 2009. Research synthesis as a scientific process; pp. 3–17.
- Cooper H. M. Organizing knowledge syntheses: A taxonomy of literature reviews. Knowledge in Society. 1988; 1 (1):104–126.
- Cronin P., Ryan F., Coughlan M. Undertaking a literature review: a step-by-step approach. British Journal of Nursing. 2008; 17 (1):38–43. [ PubMed : 18399395 ]
- Darlow S., Wen K.Y. Development testing of mobile health interventions for cancer patient self-management: A review. Health Informatics Journal. 2015 (online before print). [ PubMed : 25916831 ] [ CrossRef ]
- Daudt H. M., van Mossel C., Scott S.J. Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O’Malley’s framework. bmc Medical Research Methodology. 2013; 13 :48. [ PMC free article : PMC3614526 ] [ PubMed : 23522333 ] [ CrossRef ]
- Davies P. The relevance of systematic reviews to educational policy and practice. Oxford Review of Education. 2000; 26 (3-4):365–378.
- Deeks J. J., Higgins J. P. T., Altman D.G. In: Cochrane handbook for systematic reviews of interventions. Higgins J. P. T., Green S., editors. Hoboken, nj : John Wiley & Sons, Ltd; 2008. Analysing data and undertaking meta-analyses; pp. 243–296.
- Deshazo J. P., Lavallie D. L., Wolf F.M. Publication trends in the medical informatics literature: 20 years of “Medical Informatics” in mesh . bmc Medical Informatics and Decision Making. 2009; 9 :7. [ PMC free article : PMC2652453 ] [ PubMed : 19159472 ] [ CrossRef ]
- Dixon-Woods M., Agarwal S., Jones D., Young B., Sutton A. Synthesising qualitative and quantitative evidence: a review of possible methods. Journal of Health Services Research and Policy. 2005; 10 (1):45–53. [ PubMed : 15667704 ]
- Finfgeld-Connett D., Johnson E.D. Literature search strategies for conducting knowledge-building and theory-generating qualitative systematic reviews. Journal of Advanced Nursing. 2013; 69 (1):194–204. [ PMC free article : PMC3424349 ] [ PubMed : 22591030 ]
- Grady B., Myers K. M., Nelson E. L., Belz N., Bennett L., Carnahan L. … Guidelines Working Group. Evidence-based practice for telemental health. Telemedicine Journal and E Health. 2011; 17 (2):131–148. [ PubMed : 21385026 ]
- Green B. N., Johnson C. D., Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. Journal of Chiropractic Medicine. 2006; 5 (3):101–117. [ PMC free article : PMC2647067 ] [ PubMed : 19674681 ]
- Greenhalgh T., Wong G., Westhorp G., Pawson R. Protocol–realist and meta-narrative evidence synthesis: evolving standards ( rameses ). bmc Medical Research Methodology. 2011; 11 :115. [ PMC free article : PMC3173389 ] [ PubMed : 21843376 ]
- Gurol-Urganci I., de Jongh T., Vodopivec-Jamsek V., Atun R., Car J. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database System Review. 2013; 12 cd 007458. [ PMC free article : PMC6485985 ] [ PubMed : 24310741 ] [ CrossRef ]
- Hart C. Doing a literature review: Releasing the social science research imagination. London: SAGE Publications; 1998.
- Higgins J. P. T., Green S., editors. Cochrane handbook for systematic reviews of interventions: Cochrane book series. Hoboken, nj : Wiley-Blackwell; 2008.
- Jesson J., Matheson L., Lacey F.M. Doing your literature review: traditional and systematic techniques. Los Angeles & London: SAGE Publications; 2011.
- King W. R., He J. Understanding the role and methods of meta-analysis in IS research. Communications of the Association for Information Systems. 2005; 16 :1.
- Kirkevold M. Integrative nursing research — an important strategy to further the development of nursing science and nursing practice. Journal of Advanced Nursing. 1997; 25 (5):977–984. [ PubMed : 9147203 ]
- Kitchenham B., Charters S. ebse Technical Report Version 2.3. Keele & Durham. uk : Keele University & University of Durham; 2007. Guidelines for performing systematic literature reviews in software engineering.
- Kitsiou S., Paré G., Jaana M. Systematic reviews and meta-analyses of home telemonitoring interventions for patients with chronic diseases: a critical assessment of their methodological quality. Journal of Medical Internet Research. 2013; 15 (7):e150. [ PMC free article : PMC3785977 ] [ PubMed : 23880072 ]
- Kitsiou S., Paré G., Jaana M. Effects of home telemonitoring interventions on patients with chronic heart failure: an overview of systematic reviews. Journal of Medical Internet Research. 2015; 17 (3):e63. [ PMC free article : PMC4376138 ] [ PubMed : 25768664 ]
- Levac D., Colquhoun H., O’Brien K. K. Scoping studies: advancing the methodology. Implementation Science. 2010; 5 (1):69. [ PMC free article : PMC2954944 ] [ PubMed : 20854677 ]
- Levy Y., Ellis T.J. A systems approach to conduct an effective literature review in support of information systems research. Informing Science. 2006; 9 :181–211.
- Liberati A., Altman D. G., Tetzlaff J., Mulrow C., Gøtzsche P. C., Ioannidis J. P. A. et al. Moher D. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Annals of Internal Medicine. 2009; 151 (4):W-65. [ PubMed : 19622512 ]
- Lyden J. R., Zickmund S. L., Bhargava T. D., Bryce C. L., Conroy M. B., Fischer G. S. et al. McTigue K. M. Implementing health information technology in a patient-centered manner: Patient experiences with an online evidence-based lifestyle intervention. Journal for Healthcare Quality. 2013; 35 (5):47–57. [ PubMed : 24004039 ]
- Mickan S., Atherton H., Roberts N. W., Heneghan C., Tilson J.K. Use of handheld computers in clinical practice: a systematic review. bmc Medical Informatics and Decision Making. 2014; 14 :56. [ PMC free article : PMC4099138 ] [ PubMed : 24998515 ]
- Moher D. The problem of duplicate systematic reviews. British Medical Journal. 2013; 347 (5040) [ PubMed : 23945367 ] [ CrossRef ]
- Montori V. M., Wilczynski N. L., Morgan D., Haynes R. B., Hedges T. Systematic reviews: a cross-sectional study of location and citation counts. bmc Medicine. 2003; 1 :2. [ PMC free article : PMC281591 ] [ PubMed : 14633274 ]
- Mulrow C. D. The medical review article: state of the science. Annals of Internal Medicine. 1987; 106 (3):485–488. [ PubMed : 3813259 ] [ CrossRef ]
- Evidence-based information systems: A decade later. Proceedings of the European Conference on Information Systems ; 2011. Retrieved from http://aisel .aisnet.org/cgi/viewcontent .cgi?article =1221&context =ecis2011 .
- Okoli C., Schabram K. A guide to conducting a systematic literature review of information systems research. ssrn Electronic Journal. 2010
- Otte-Trojel T., de Bont A., Rundall T. G., van de Klundert J. How outcomes are achieved through patient portals: a realist review. Journal of American Medical Informatics Association. 2014; 21 (4):751–757. [ PMC free article : PMC4078283 ] [ PubMed : 24503882 ]
- Paré G., Trudel M.-C., Jaana M., Kitsiou S. Synthesizing information systems knowledge: A typology of literature reviews. Information & Management. 2015; 52 (2):183–199.
- Patsopoulos N. A., Analatos A. A., Ioannidis J.P. A. Relative citation impact of various study designs in the health sciences. Journal of the American Medical Association. 2005; 293 (19):2362–2366. [ PubMed : 15900006 ]
- Paul M. M., Greene C. M., Newton-Dame R., Thorpe L. E., Perlman S. E., McVeigh K. H., Gourevitch M.N. The state of population health surveillance using electronic health records: A narrative review. Population Health Management. 2015; 18 (3):209–216. [ PubMed : 25608033 ]
- Pawson R. Evidence-based policy: a realist perspective. London: SAGE Publications; 2006.
- Pawson R., Greenhalgh T., Harvey G., Walshe K. Realist review—a new method of systematic review designed for complex policy interventions. Journal of Health Services Research & Policy. 2005; 10 (Suppl 1):21–34. [ PubMed : 16053581 ]
- Petersen K., Vakkalanka S., Kuzniarz L. Guidelines for conducting systematic mapping studies in software engineering: An update. Information and Software Technology. 2015; 64 :1–18.
- Petticrew M., Roberts H. Systematic reviews in the social sciences: A practical guide. Malden, ma : Blackwell Publishing Co; 2006.
- Rousseau D. M., Manning J., Denyer D. Evidence in management and organizational science: Assembling the field’s full weight of scientific knowledge through syntheses. The Academy of Management Annals. 2008; 2 (1):475–515.
- Rowe F. What literature review is not: diversity, boundaries and recommendations. European Journal of Information Systems. 2014; 23 (3):241–255.
- Shea B. J., Hamel C., Wells G. A., Bouter L. M., Kristjansson E., Grimshaw J. et al. Boers M. amstar is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. Journal of Clinical Epidemiology. 2009; 62 (10):1013–1020. [ PubMed : 19230606 ]
- Shepperd S., Lewin S., Straus S., Clarke M., Eccles M. P., Fitzpatrick R. et al. Sheikh A. Can we systematically review studies that evaluate complex interventions? PLoS Medicine. 2009; 6 (8):e1000086. [ PMC free article : PMC2717209 ] [ PubMed : 19668360 ]
- Silva B. M., Rodrigues J. J., de la Torre Díez I., López-Coronado M., Saleem K. Mobile-health: A review of current state in 2015. Journal of Biomedical Informatics. 2015; 56 :265–272. [ PubMed : 26071682 ]
- Smith V., Devane D., Begley C., Clarke M. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. bmc Medical Research Methodology. 2011; 11 (1):15. [ PMC free article : PMC3039637 ] [ PubMed : 21291558 ]
- Sylvester A., Tate M., Johnstone D. Beyond synthesis: re-presenting heterogeneous research literature. Behaviour & Information Technology. 2013; 32 (12):1199–1215.
- Templier M., Paré G. A framework for guiding and evaluating literature reviews. Communications of the Association for Information Systems. 2015; 37 (6):112–137.
- Thomas J., Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. bmc Medical Research Methodology. 2008; 8 (1):45. [ PMC free article : PMC2478656 ] [ PubMed : 18616818 ]
- Reconstructing the giant: on the importance of rigour in documenting the literature search process. Paper presented at the Proceedings of the 17th European Conference on Information Systems ( ecis 2009); Verona, Italy. 2009.
- Webster J., Watson R.T. Analyzing the past to prepare for the future: Writing a literature review. Management Information Systems Quarterly. 2002; 26 (2):11.
- Whitlock E. P., Lin J. S., Chou R., Shekelle P., Robinson K.A. Using existing systematic reviews in complex systematic reviews. Annals of Internal Medicine. 2008; 148 (10):776–782. [ PubMed : 18490690 ]
This publication is licensed under a Creative Commons License, Attribution-Noncommercial 4.0 International License (CC BY-NC 4.0): see https://creativecommons.org/licenses/by-nc/4.0/
- Cite this Page Paré G, Kitsiou S. Chapter 9 Methods for Literature Reviews. In: Lau F, Kuziemsky C, editors. Handbook of eHealth Evaluation: An Evidence-based Approach [Internet]. Victoria (BC): University of Victoria; 2017 Feb 27.
- PDF version of this title (4.5M)
- Disable Glossary Links
In this Page
- Introduction
- Overview of the Literature Review Process and Steps
- Types of Review Articles and Brief Illustrations
- Concluding Remarks
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 9 Methods for Literature Reviews - Handbook of eHealth Evaluation: An Ev... Chapter 9 Methods for Literature Reviews - Handbook of eHealth Evaluation: An Evidence-based Approach
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
How to Write Critical Reviews
When you are asked to write a critical review of a book or article, you will need to identify, summarize, and evaluate the ideas and information the author has presented. In other words, you will be examining another person’s thoughts on a topic from your point of view.
Your stand must go beyond your “gut reaction” to the work and be based on your knowledge (readings, lecture, experience) of the topic as well as on factors such as criteria stated in your assignment or discussed by you and your instructor.
Make your stand clear at the beginning of your review, in your evaluations of specific parts, and in your concluding commentary.
Remember that your goal should be to make a few key points about the book or article, not to discuss everything the author writes.
Understanding the Assignment
To write a good critical review, you will have to engage in the mental processes of analyzing (taking apart) the work–deciding what its major components are and determining how these parts (i.e., paragraphs, sections, or chapters) contribute to the work as a whole.
Analyzing the work will help you focus on how and why the author makes certain points and prevent you from merely summarizing what the author says. Assuming the role of an analytical reader will also help you to determine whether or not the author fulfills the stated purpose of the book or article and enhances your understanding or knowledge of a particular topic.
Be sure to read your assignment thoroughly before you read the article or book. Your instructor may have included specific guidelines for you to follow. Keeping these guidelines in mind as you read the article or book can really help you write your paper!
Also, note where the work connects with what you’ve studied in the course. You can make the most efficient use of your reading and notetaking time if you are an active reader; that is, keep relevant questions in mind and jot down page numbers as well as your responses to ideas that appear to be significant as you read.
Please note: The length of your introduction and overview, the number of points you choose to review, and the length of your conclusion should be proportionate to the page limit stated in your assignment and should reflect the complexity of the material being reviewed as well as the expectations of your reader.
Write the introduction
Below are a few guidelines to help you write the introduction to your critical review.
Introduce your review appropriately
Begin your review with an introduction appropriate to your assignment.
If your assignment asks you to review only one book and not to use outside sources, your introduction will focus on identifying the author, the title, the main topic or issue presented in the book, and the author’s purpose in writing the book.
If your assignment asks you to review the book as it relates to issues or themes discussed in the course, or to review two or more books on the same topic, your introduction must also encompass those expectations.
Explain relationships
For example, before you can review two books on a topic, you must explain to your reader in your introduction how they are related to one another.
Within this shared context (or under this “umbrella”) you can then review comparable aspects of both books, pointing out where the authors agree and differ.
In other words, the more complicated your assignment is, the more your introduction must accomplish.
Finally, the introduction to a book review is always the place for you to establish your position as the reviewer (your thesis about the author’s thesis).
As you write, consider the following questions:
- Is the book a memoir, a treatise, a collection of facts, an extended argument, etc.? Is the article a documentary, a write-up of primary research, a position paper, etc.?
- Who is the author? What does the preface or foreword tell you about the author’s purpose, background, and credentials? What is the author’s approach to the topic (as a journalist? a historian? a researcher?)?
- What is the main topic or problem addressed? How does the work relate to a discipline, to a profession, to a particular audience, or to other works on the topic?
- What is your critical evaluation of the work (your thesis)? Why have you taken that position? What criteria are you basing your position on?
Provide an overview
In your introduction, you will also want to provide an overview. An overview supplies your reader with certain general information not appropriate for including in the introduction but necessary to understanding the body of the review.
Generally, an overview describes your book’s division into chapters, sections, or points of discussion. An overview may also include background information about the topic, about your stand, or about the criteria you will use for evaluation.
The overview and the introduction work together to provide a comprehensive beginning for (a “springboard” into) your review.
- What are the author’s basic premises? What issues are raised, or what themes emerge? What situation (i.e., racism on college campuses) provides a basis for the author’s assertions?
- How informed is my reader? What background information is relevant to the entire book and should be placed here rather than in a body paragraph?
Write the body
The body is the center of your paper, where you draw out your main arguments. Below are some guidelines to help you write it.
Organize using a logical plan
Organize the body of your review according to a logical plan. Here are two options:
- First, summarize, in a series of paragraphs, those major points from the book that you plan to discuss; incorporating each major point into a topic sentence for a paragraph is an effective organizational strategy. Second, discuss and evaluate these points in a following group of paragraphs. (There are two dangers lurking in this pattern–you may allot too many paragraphs to summary and too few to evaluation, or you may re-summarize too many points from the book in your evaluation section.)
- Alternatively, you can summarize and evaluate the major points you have chosen from the book in a point-by-point schema. That means you will discuss and evaluate point one within the same paragraph (or in several if the point is significant and warrants extended discussion) before you summarize and evaluate point two, point three, etc., moving in a logical sequence from point to point to point. Here again, it is effective to use the topic sentence of each paragraph to identify the point from the book that you plan to summarize or evaluate.
Questions to keep in mind as you write
With either organizational pattern, consider the following questions:
- What are the author’s most important points? How do these relate to one another? (Make relationships clear by using transitions: “In contrast,” an equally strong argument,” “moreover,” “a final conclusion,” etc.).
- What types of evidence or information does the author present to support his or her points? Is this evidence convincing, controversial, factual, one-sided, etc.? (Consider the use of primary historical material, case studies, narratives, recent scientific findings, statistics.)
- Where does the author do a good job of conveying factual material as well as personal perspective? Where does the author fail to do so? If solutions to a problem are offered, are they believable, misguided, or promising?
- Which parts of the work (particular arguments, descriptions, chapters, etc.) are most effective and which parts are least effective? Why?
- Where (if at all) does the author convey personal prejudice, support illogical relationships, or present evidence out of its appropriate context?
Keep your opinions distinct and cite your sources
Remember, as you discuss the author’s major points, be sure to distinguish consistently between the author’s opinions and your own.
Keep the summary portions of your discussion concise, remembering that your task as a reviewer is to re-see the author’s work, not to re-tell it.
And, importantly, if you refer to ideas from other books and articles or from lecture and course materials, always document your sources, or else you might wander into the realm of plagiarism.
Include only that material which has relevance for your review and use direct quotations sparingly. The Writing Center has other handouts to help you paraphrase text and introduce quotations.
Write the conclusion
You will want to use the conclusion to state your overall critical evaluation.
You have already discussed the major points the author makes, examined how the author supports arguments, and evaluated the quality or effectiveness of specific aspects of the book or article.
Now you must make an evaluation of the work as a whole, determining such things as whether or not the author achieves the stated or implied purpose and if the work makes a significant contribution to an existing body of knowledge.
Consider the following questions:
- Is the work appropriately subjective or objective according to the author’s purpose?
- How well does the work maintain its stated or implied focus? Does the author present extraneous material? Does the author exclude or ignore relevant information?
- How well has the author achieved the overall purpose of the book or article? What contribution does the work make to an existing body of knowledge or to a specific group of readers? Can you justify the use of this work in a particular course?
- What is the most important final comment you wish to make about the book or article? Do you have any suggestions for the direction of future research in the area? What has reading this work done for you or demonstrated to you?

Academic and Professional Writing
This is an accordion element with a series of buttons that open and close related content panels.
Analysis Papers
Reading Poetry
A Short Guide to Close Reading for Literary Analysis
Using Literary Quotations
Play Reviews
Writing a Rhetorical Précis to Analyze Nonfiction Texts
Incorporating Interview Data
Grant Proposals
Planning and Writing a Grant Proposal: The Basics
Additional Resources for Grants and Proposal Writing
Job Materials and Application Essays
Writing Personal Statements for Ph.D. Programs
- Before you begin: useful tips for writing your essay
- Guided brainstorming exercises
- Get more help with your essay
- Frequently Asked Questions
Resume Writing Tips
CV Writing Tips
Cover Letters
Business Letters
Proposals and Dissertations
Resources for Proposal Writers
Resources for Dissertators
Research Papers
Planning and Writing Research Papers
Quoting and Paraphrasing
Writing Annotated Bibliographies
Creating Poster Presentations
Writing an Abstract for Your Research Paper
Thank-You Notes
Advice for Students Writing Thank-You Notes to Donors
Reading for a Review
Critical Reviews
Writing a Review of Literature

Scientific Reports
Scientific Report Format
Sample Lab Assignment
Writing for the Web
Writing an Effective Blog Post
Writing for Social Media: A Guide for Academics

The Guide to Literature Reviews

- What is a Literature Review?
- The Purpose of Literature Reviews
- Guidelines for Writing a Literature Review
- How to Organize a Literature Review?
- Software for Literature Reviews
- Using Artificial Intelligence for Literature Reviews
- How to Conduct a Literature Review?
- Common Mistakes and Pitfalls in a Literature Review
- Methods for Literature Reviews
When to conduct a systematic review?
How do systematic literature reviews differ from other reviews, how to conduct a systematic literature review.
- What is a Narrative Literature Review?
- What is a Descriptive Literature Review?
- What is a Scoping Literature Review?
- What is a Realist Literature Review?
- What is a Critical Literature Review?
- Meta Analysis vs. Literature Review
- What is an Umbrella Literature Review?
- Differences Between Annotated Bibliographies and Literature Reviews
- Literature Review vs. Theoretical Framework
- How to Write a Literature Review?
- How to Structure a Literature Review?
- How to Make a Cover Page for a Literature Review?
- How to Write an Abstract for a Literature Review?
- How to Write a Literature Review Introduction?
- How to Write the Body of a Literature Review?
- How to Write a Literature Review Conclusion?
- How to Make a Literature Review Bibliography?
- How to Format a Literature Review?
- How Long Should a Literature Review Be?
- Examples of Literature Reviews
- How to Present a Literature Review?
- How to Publish a Literature Review?
What is a Systematic Literature Review?
A systematic literature review is a structured, organized and transparent process for identifying, selecting, and critically appraising relevant research studies to answer a specific research question . Systematic reviews apply predefined criteria for selecting studies, assessing their quality, and synthesizing their findings. This rigorous methodology ensures that a literature review is exhaustive and reproducible.

At the heart of a systematic review lies a well-defined protocol that guides the entire process, from the formulation of research questions to the selection and appraisal of relevant studies. This systematic approach contrasts with other literature reviews, which may be conducted more flexibly.
The methods in a systematic literature review are designed to offer a comprehensive textual summary and synthesis of existing research, providing context and background information critical to understanding the broader research landscape. Systematic reviews are essential for informing evidence-based practices and policy decisions, as they consolidate findings from numerous studies and offer a high level of evidence.
A systematic review often follows specific guidelines such as the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Page et al., 2020). The guidelines ensure that reviews are conducted rigorously and reported clearly. This facilitates the replication of findings and the assessment of conclusions; while PRISMA primarily focuses on quantitative research , it has extensions like PRISMA-ScR that can apply to qualitative research . Researchers also use the Cochrane Handbook for Systematic Literature Reviews (Higgins et al., 2023) which focuses on detailed guidelines for doing systematic reviews of healthcare interventions.
Systematic reviews are often used in evidence-based research and practice, particularly in environmental science, healthcare, and social sciences. Researchers undertake these reviews to identify gaps in current evidence and suggest areas for further investigation. They are essential in developing guidelines and informing policies by providing nuanced and detailed evaluations of experiences, perceptions, and contextual factors.
Qualitative systematic reviews support grant applications by demonstrating the current state of qualitative knowledge and the need for further exploration. Organizations employ a systematic review methodology to improve practices and interventions. Public health professionals rely on qualitative systematic reviews to assess the effectiveness of interventions and shape strategies that consider the socio-cultural contexts. Regularly updating these reviews ensures that the synthesized qualitative evidence remains current, aiding in more informed and effective decision-making in various disciplines.
Systematic literature reviews differ from other types of reviews in their methodology, scope, and rigour. They follow a structured approach with clear research questions, predefined criteria, comprehensive search strategies, and systematic data extraction. Other reviews, like narrative reviews , are more flexible and less structured, often lacking predefined criteria and systematic searches.
Systematic reviews aim to cover all relevant studies on a specific question. In contrast, other reviews may focus on a narrower study scope and include studies selectively, reflecting the author's perspective. Systematic reviews also employ a systematic search strategy to cover multiple databases and grey literature sources such as government or technical reports, reducing the risk of cherry-picking studies.
Rigor is another key difference. Systematic reviews critically appraise the quality of included studies and often use statistical methods (in the case of quantitative research ) or thematic analysis to synthesize findings. Other reviews do not usually include formal quality assessments and rely more on narrative synthesis.
Reproducibility is a hallmark of systematic reviews. They document their process in detail, allowing others to replicate the study. Other reviews often lack this detailed methodology, making replication difficult and leading to potential inconsistencies.
Transparency is crucial in systematic reviews, with published protocols, documented search strategies, and clear study selection processes. Guidelines like the PRISMA checklist (Page et. al 2020) ensure thorough reporting. Other reviews do not usually follow strict guidelines and may not fully disclose their methods and criteria.
The primary objective of systematic reviews is to provide high-quality evidence, informing clinical practice, policy-making, and further research. Other reviews aim to offer overviews or summaries of the literature, providing insights and perspectives rather than systematic evidence synthesis.
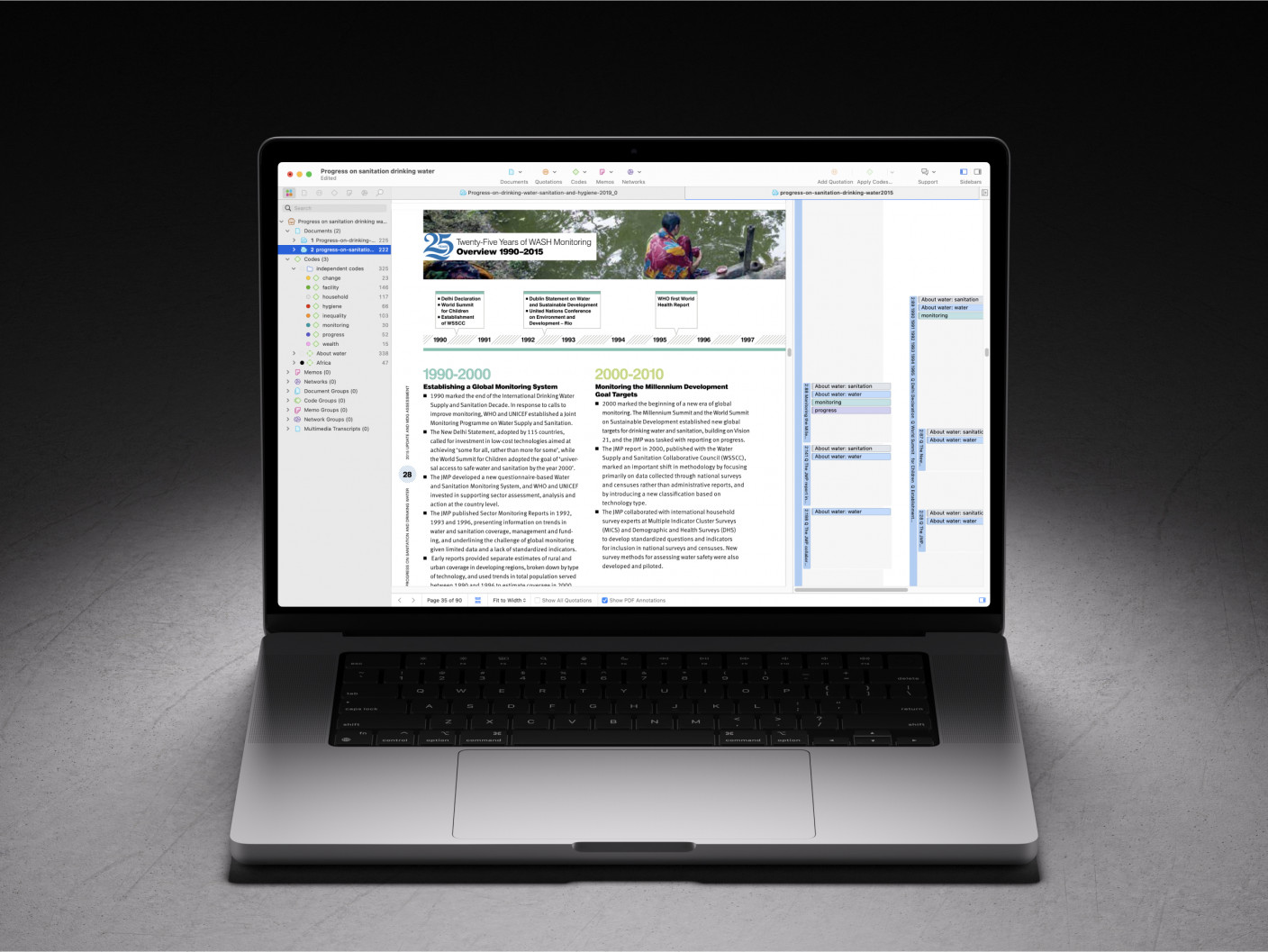
Quality literature reviews start with ATLAS.ti
ATLAS.ti is there for you at every step, from searching articles to reference managing. See how with a free trial.
To effectively conduct a systematic literature review, it is crucial to follow a structured set of instructions that encompass comprehensive planning, rigorous methodology, and meticulous documentation. The following steps are recommended when conducting a systematic literature review:
Define the research question : Clearly state the research question(s) you intend to answer, ensuring it is specific, open-ended, and suitable for detailed exploration. This will guide all subsequent steps. For example, "How do adolescents perceive the impact of social media on their mental health?" Break down the main question into sub-questions, such as: What are the positive and negative perceptions of social media among adolescents? How do adolescents describe their emotional responses to social media interactions? What coping strategies do adolescents use to manage social media-induced stress?
Develop a protocol : Outline the methodology and criteria for your review in a detailed protocol to ensure transparency. Include background information, rationales, and clearly stated objectives. Define inclusion and exclusion criteria based on the study population, context, data collection methods, and outcomes of interest. Identify and list the databases you will search, such as PubMed , PsycINFO , and Scopus . Develop keywords and search strings using Boolean operators. Create a data extraction form to capture relevant data from each study. Optionally, register your protocol with a platform like PROSPERO for enhanced transparency.
Conduct a comprehensive literature search : Perform a thorough search across identified databases using developed keywords and search strategy. Document the search process meticulously, including search dates, databases searched, and the number of records retrieved. This ensures a comprehensive capture of relevant studies related to your research question.
Screen and select studies : Apply the inclusion and exclusion criteria to filter studies. Start with an initial screening of titles and abstracts, followed by a full-text review of remaining studies for final inclusion. Document reasons for exclusion at each stage to ensure transparency and consistency.
Assess the quality of studies : Use standardized tools, such as the Critical Appraisal Skills Programme (CASP) for qualitative studies to assess the quality of qualitative studies . Evaluate aspects like credibility, transferability, dependability, and confirmability. Ensure consistency and document the process and outcomes.
Extract data : Develop a data extraction form to systematically capture relevant data from each included study, such as study design, participant characteristics, data collection methods, themes, and findings. Use qualitative data analysis software such as ATLAS.ti for coding and theme identification.
Analyze and synthesize data : Identify and synthesize key themes and patterns across studies. Conduct a meta-synthesis to integrate findings and provide a comprehensive understanding of the research question. Ensure a thorough synthesis to highlight variations and commonalities across studies.
Report findings : Follow a structured format including an introduction, methods, results, discussion, and conclusion. Adhere to PRISMA guidelines (Page et. al 2020) for transparent reporting. Use tables, figures, and flow diagrams to illustrate findings and the study selection process.
Discuss implications : Interpret the findings within the context of existing literature, acknowledging limitations and suggesting areas for future research. Provide recommendations based on gathered evidence.
Update and maintain the review : Consider periodic updates as new studies become available to ensure findings remain current. Set up database alerts to stay informed about new research.

A systematic literature review rigorously answers specific research questions by evaluating and synthesizing evidence from multiple studies, providing comprehensive context and background information. Unlike other literature reviews, systematic review protocols follow a structure with predefined criteria, ensuring exhaustive and reproducible results. They adhere to guidelines like PRISMA (Page et. al 2020) for thorough reporting and trustworthy conclusions. Systematic reviews are essential in healthcare and social sciences because they help identify evidence gaps and inform policies. Regular updates keep the evidence current, supporting effective decision-making across various disciplines.
Page M J, McKenzie J E, Bossuyt P M, Boutron I, Hoffmann T C, Mulrow C D et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews BMJ 2021; 372 :n71 doi:10.1136/bmj.n71
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.4 (updated August 2023). Cochrane, 2023.
Develop powerful literature reviews with ATLAS.ti
Use our intuitive data analysis platform to make the most of your literature review. Get started with a free trial.
- Link to facebook
- Link to linkedin
- Link to twitter
- Link to youtube
- Writing Tips
Critical Analysis in a Literature Review
- 3-minute read
- 29th June 2015
A literature review is vital to any in-depth research , providing a foundation your work will build upon. Familiarizing yourself with the existing literature allows you to identify current debates in the field, ensuring that your work is up-to-date and addresses significant questions.
But a good literature review will require reading critically. This means deciding whether you agree or disagree with certain viewpoints, arguments and theories, rather than simply describing them.
It also requires being able to spot the flaws and strengths of particular studies, which can in turn help when developing your own ideas. To make sure you do this effectively, it’s worth looking for the following things.
1. Overgeneralizations
One common issue in research is the scope of its application, especially when dealing with limited sample sizes or when a study is generalized too broadly.
The conclusions of a psychological study conducted with all male participants, for instance, may not be applicable in the same way to female subjects.
2. Methodological Limitations
When writing a literature review, ask yourself whether the methods used for particular studies were appropriate.
For example, whether the study used a quantitative, qualitative or mixed-methods research design can make a big difference to the conclusions reached.
3. How Well Explained is the Research?
When reading for a critical literature review, it is important to consider how well written the studies you examine are.
Find this useful?
Subscribe to our newsletter and get writing tips from our editors straight to your inbox.
Does the author explain their methods? Is enough detail provided for any experiments to be replicated? Are sampling, data collection and analysis techniques clearly identified? Does the conclusion follow from the results?
Asking these and similar questions will help you discern between good and bad research.
4. Identify Biases
Another important factor is to consider whether implicit biases might have influenced the research.
The term “confirmation bias,” for example, refers to the tendency to focus on evidence which supports one’s existing beliefs, which can lead to overlooking alternative hypotheses.
5. Challenge Your Own Assumptions
If you come across a study which seems to oppose your hypothesis, consider whether it presents good counterarguments to your own position. If it does, ask yourself whether this affects how you conduct the rest of your research.
The final point here is important because conducting a literature review serves two purposes . The finished literature review will help your reader to understand the background of your research, so critical analysis helps to clarify what your work contributes to the debate.
But comparing different studies and theories for a literature review will also help you to develop a research approach. The better your critical analysis, then, the better prepared you’ll be.
Share this article:
Post A New Comment
Got content that needs a quick turnaround? Let us polish your work. Explore our editorial business services.
6-minute read
How to Write a Nonprofit Grant Proposal
If you’re seeking funding to support your charitable endeavors as a nonprofit organization, you’ll need...
9-minute read
How to Use Infographics to Boost Your Presentation
Is your content getting noticed? Capturing and maintaining an audience’s attention is a challenge when...
8-minute read
Why Interactive PDFs Are Better for Engagement
Are you looking to enhance engagement and captivate your audience through your professional documents? Interactive...
7-minute read
Seven Key Strategies for Voice Search Optimization
Voice search optimization is rapidly shaping the digital landscape, requiring content professionals to adapt their...
4-minute read
Five Creative Ways to Showcase Your Digital Portfolio
Are you a creative freelancer looking to make a lasting impression on potential clients or...
How to Ace Slack Messaging for Contractors and Freelancers
Effective professional communication is an important skill for contractors and freelancers navigating remote work environments....

Make sure your writing is the best it can be with our expert English proofreading and editing.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Ontology in hybrid intelligence: a concise literature review.

Share and Cite
Pileggi, S.F. Ontology in Hybrid Intelligence: A Concise Literature Review. Future Internet 2024 , 16 , 268. https://doi.org/10.3390/fi16080268
Pileggi SF. Ontology in Hybrid Intelligence: A Concise Literature Review. Future Internet . 2024; 16(8):268. https://doi.org/10.3390/fi16080268
Pileggi, Salvatore Flavio. 2024. "Ontology in Hybrid Intelligence: A Concise Literature Review" Future Internet 16, no. 8: 268. https://doi.org/10.3390/fi16080268
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Open access
- Published: 25 July 2024
Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review
- Ali Mohammad Mosadeghrad 1 ,
- Mahnaz Afshari 2 ,
- Parvaneh Isfahani 3 ,
- Farahnaz Ezzati 4 ,
- Mahdi Abbasi 4 ,
- Shahrzad Akhavan Farahani 4 ,
- Maryam Zahmatkesh 5 &
- Leila Eslambolchi 4
BMC Health Services Research volume 24 , Article number: 841 ( 2024 ) Cite this article
193 Accesses
Metrics details
Primary Health Care (PHC) systems are pivotal in delivering essential health services during crises, as demonstrated during the COVID-19 pandemic. With varied global strategies to reinforce PHC systems, this scoping review consolidates these efforts, identifying and categorizing key resilience-building strategies.
Adopting Arksey and O'Malley's scoping review framework, this study synthesized literature across five databases and Google Scholar, encompassing studies up to December 31st, 2022. We focused on English and Persian studies that addressed interventions to strengthen PHC amidst COVID-19. Data were analyzed through thematic framework analysis employing MAXQDA 10 software.
Our review encapsulated 167 studies from 48 countries, revealing 194 interventions to strengthen PHC resilience, categorized into governance and leadership, financing, workforce, infrastructures, information systems, and service delivery. Notable strategies included telemedicine, workforce training, psychological support, and enhanced health information systems. The diversity of the interventions reflects a robust global response, emphasizing the adaptability of strategies across different health systems.
Conclusions
The study underscored the need for well-resourced, managed, and adaptable PHC systems, capable of maintaining continuity in health services during emergencies. The identified interventions suggested a roadmap for integrating resilience into PHC, essential for global health security. This collective knowledge offered a strategic framework to enhance PHC systems' readiness for future health challenges, contributing to the overall sustainability and effectiveness of global health systems.
Peer Review reports
The health system is a complex network that encompasses individuals, groups, and organizations engaged in policymaking, financing, resource generation, and service provision. These efforts collectively aim to safeguard and enhance people health, meet their expectations, and provide financial protection [ 1 ]. The World Health Organization's (WHO) framework outlines six foundational building blocks for a robust health system: governance and leadership, financing, workforce, infrastructure along with technologies and medicine, information systems, and service delivery. Strengthening these elements is essential for health systems to realize their objectives of advancing and preserving public health [ 2 ].
Effective governance in health systems encompasses the organization of structures, processes, and authority, ensuring resource stewardship and aligning stakeholders’ behaviors with health goals [ 3 ]. Financial mechanisms are designed to provide health services without imposing financial hardship, achieved through strategic fund collection, management and allocation [ 4 , 5 ]. An equitable, competent, and well-distributed health workforce is crucial in delivering healthcare services and fulfilling health system objectives [ 2 ]. Access to vital medical supplies, technologies, and medicines is a cornerstone of effective health services, while health information systems play a pivotal role in generating, processing, and utilizing health data, informing policy decisions [ 2 , 5 ]. Collectively, these components interact to offer quality health services that are safe, effective, timely, affordable, and patient-centered [ 2 ]
The WHO, at the 1978 Alma-Ata conference, introduced primary health care (PHC) as the fundamental strategy to attain global health equity [ 6 ]. Subsequent declarations, such as the one in Astana in 2018, have reaffirmed the pivotal role of PHC in delivering high-quality health care for all [ 7 ]. PHC represents the first level of contact within the health system, offering comprehensive, accessible, community-based care that is culturally sensitive and supported by appropriate technology [ 8 ]. Essential care through PHC encompasses health education, proper nutrition, access to clean water and sanitation, maternal and child healthcare, immunizations, treatment of common diseases, and the provision of essential drugs [ 6 ]. PHC aims to provide protective, preventive, curative, and rehabilitative services that are as close to the community as possible [ 9 ].
Global health systems, however, have faced significant disruptions from various shocks and crises [ 10 ], with the COVID-19 pandemic being a recent and profound example. The pandemic has stressed health systems worldwide, infecting over 775 million and claiming more than 7.04 million lives as of April 13th, 2024 [ 11 ]. Despite the pandemic highlighting the critical role of hospitals and intensive care, it also revealed the limitations of specialized medicine when not complemented by a robust PHC system [ 12 ].
The pandemic brought to light the vulnerabilities of PHC systems, noting a significant decrease in the use of primary care for non-emergency conditions. Routine health services, including immunizations, prenatal care, and chronic disease management, were severely impacted [ 13 ]. The challenges—quarantine restrictions, fears of infection, staffing and resource shortages, suspended non-emergency services, and financial barriers—reduced essential service utilization [ 14 ]. This led to an avoidance of healthcare, further exacerbating health inequalities and emphasizing the need for more resilient PHC systems [ 15 , 16 , 17 ].
Resilient PHC systems are designed to predict, prevent, prepare, absorb, adapt, and transform when facing crises, ensuring the continuity of routine health services [ 18 ]. Investing in the development of such systems can not only enhance crisis response but also foster post-crisis transformation and improvement. This study focuses on identifying global interventions and strategies to cultivate resilient PHC systems, aiding policymakers and managers in making informed decisions in times of crisis.
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents. Unlike systematic reviews, it typically does not require a quality assessment of the included literature, making it well-suited for rapidly gathering a wide scope of evidence [ 19 ]. Our goal was to uncover the breadth of solutions aimed at bolstering the resilience of the PHC system throughout the COVID-19 crisis. The outcomes of this review are intended to inform the development of a model that ensures the PHC system's ability to continue delivering not just emergency services but also essential care during times of crisis.
We employed Arksey and O'Malley's methodological framework, which consists of six steps: formulating the research question, identifying relevant studies, selecting the pertinent studies, extracting data, synthesizing and reporting the findings, and, where applicable, consulting with stakeholders to inform and validate the results [ 20 ]. This comprehensive approach is designed to capture a wide range of interventions and strategies, with the ultimate aim of crafting a robust PHC system that can withstand the pressures of a global health emergency
Stage 1: identifying the research question
Our scoping review was guided by the central question: "Which strategies and interventions have been implemented to enhance the resilience of primary healthcare systems in response to the COVID-19 pandemic?" This question aimed to capture a comprehensive array of responses to understand the full scope of resilience-building activities within PHC systems.
Stage 2: identifying relevant studies
To ensure a thorough review, we conducted systematic searches across multiple databases, specifically targeting literature up to December 31st, 2022. The databases included PubMed, Web of Science, Scopus, Magiran, and SID. We also leveraged the expansive reach of Google Scholar. Our search strategy incorporated a bilingual approach, utilizing both English and Persian keywords that encompassed "PHC," "resilience," "strategies," and "policies," along with the logical operators AND/OR to refine the search. Additionally, we employed Medical Subject Headings (MeSH) terms to enhance the precision of our search. The results were meticulously organized and managed using the Endnote X8 citation manager, facilitating the systematic selection and review of pertinent literature.
Stage 3: selecting studies
In the third stage, we meticulously vetted our search results to exclude duplicate entries by comparing bibliographic details such as titles, authors, publication dates, and journal names. This task was performed independently by two of our authors, LE and MA, who rigorously screened titles and abstracts. Discrepancies encountered during this process were brought to the attention of a third author, AMM, for resolution through consensus.
Subsequently, full-text articles were evaluated by four team members—LE, MA, PI, and SHZ—to ascertain their relevance to our research question. The selection hinged on identifying articles that discussed strategies aimed at bolstering the resilience of PHC systems amidst the COVID-19 pandemic Table 1 .
We have articulated the specific inclusion and exclusion criteria that guided our selection process in Table 2 , ensuring transparency and replicability of our review methodology
Stage 4: charting the data
Data extraction was conducted by a team of six researchers (LE, MA, PI, MA, FE, and SHZ), utilizing a structured data extraction form. For each selected study, we collated details including the article title, the first author’s name, the year of publication, the country where the study was conducted, the employed research methodology, the sample size, the type of document, and the PHC strengthening strategies described.
In pursuit of maintaining rigorous credibility in our study, we adopted a dual-review process. Each article was independently reviewed by pairs of researchers to mitigate bias and ensure a thorough analysis. Discrepancies between reviewers were addressed through discussion to reach consensus. In instances where consensus could not be reached, the matter was escalated to a third, neutral reviewer. Additionally, to guarantee thoroughness, either LE or MA conducted a final review of the complete data extraction for each study.
Stage 5: collating, summarizing and reporting the results
In this stage, authors LE, MZ, and MA worked independently to synthesize the data derived from the selected studies. Differences in interpretation were collaboratively discussed until a consensus was reached, with AMM providing arbitration where required.
We employed a framework thematic analysis, underpinned by the WHO's health system building blocks model, to structure our findings. This model categorizes health system components into six foundational elements: governance and leadership; health financing; health workforce; medical products, vaccines, and technologies; health information systems; and service delivery [ 2 ]. Using MAXQDA 10 software, we coded the identified PHC strengthening strategies within these six thematic areas.
Summary of search results and study selection
In total, 4315 articles were found by initial search. After removing 397 duplicates, 3918 titles and abstracts were screened and 3606 irrelevant ones were deleted. Finally, 167 articles of 312 reviewed full texts were included in data synthesis (Fig. 1 ). Main characteristics of included studies are presented in Appendix 1.

PRISMA Flowchart of search process and results
Characteristics of studies
These studies were published in 2020 (18.6%), 2021 (36.5%) and 2022 (44.9%). They were conducted in 48 countries, mostly in the US (39 studies), the UK (16 studies), Canada (11 studies), Iran (10 studies) and Brazil (7 studies) as shown in Fig. 2 .

Distribution of reviewed studies by country
Although the majority of the reviewed publications were original articles (55.1 %) and review papers (21 %), other types of documents such as reports, policy briefs, analysis, etc., were also included in this review (Fig. 3 ).
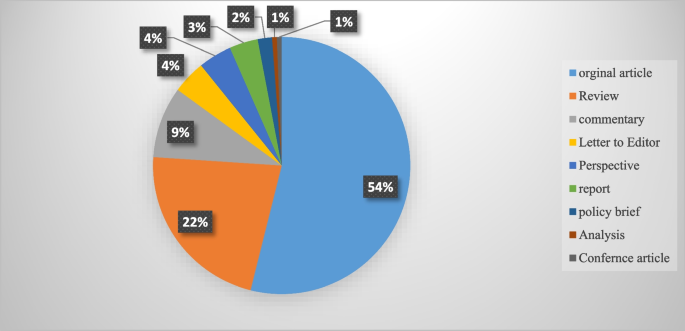
An overview of the publication types
Strengthening interventions to build a resilient PHC system
In total, 194 interventions were identified for strengthening the resilience of PHC systems to respond to the COVID-19 pandemic. They were grouped into six themes of PHC governance and leadership (46 interventions), PHC financing (21 interventions), PHC workforce (37 interventions), PHC infrastructures, equipment, medicines and vaccines (30 interventions), PHC information system (21 interventions) and PHC service delivery (39 interventions). These strategies are shown in Table 3 .
This scoping review aimed to identify and categorize the range of interventions employed globally to strengthen the resilience of primary healthcare (PHC) systems in the face of the COVID-19 pandemic. Our comprehensive search yielded 194 distinct interventions across 48 countries, affirming the significant international efforts to sustain healthcare services during this unprecedented crisis. These interventions have been classified according to the WHO’s six building block model of health systems, providing a framework for analyzing their breadth and depth. This review complements and expands upon the findings from Pradhan et al., who identified 28 interventions specifically within low and middle-income countries, signaling the universality of the challenge and the myriad of innovative responses it has provoked globally [ 178 ].
The review highlights the critical role of governance and leadership in PHC resilience. Effective organizational structure changes, legal reforms, and policy development were crucial in creating adaptive healthcare systems capable of meeting the dynamic challenges posed by the pandemic. These findings resonate with the two strategies of effective leadership and coordination emphasized by Pradhan et al. (2023), and underscore the need for clear vision, evidence-based policy, and active community engagement in governance [ 178 ]. The COVID-19 pandemic posed significant challenges for PHC systems globally. A pivotal response to these challenges was the active involvement of key stakeholders in the decision-making process. This inclusivity spanned across the spectrum of general practitioners, health professionals, health managers, and patients. By engaging these vital contributors, it became possible to address their specific needs and to design and implement people-centered services effectively [ 41 , 42 , 43 ].
The development and implementation of collaborative, evidence-informed policies and national healthcare plans were imperative. Such strategies required robust leadership, bolstered by political commitment, to ensure that the necessary changes could be enacted swiftly and efficiently [ 41 , 45 ]. Leaders within the health system were called upon to foster an environment of good governance. This entailed promoting increased participation from all sectors of the healthcare community, enhancing transparency in decision-making processes, and upholding the principles of legitimacy, accountability, and responsibility within the health system [ 10 ]. The collective aim was to create a more resilient, responsive, and equitable healthcare system in the face of the pandemic's demands.
In the wake of the COVID-19 pandemic, governments were compelled to implement new laws and regulations. These were designed to address a range of issues from professional accreditation and ethical concerns to supporting the families of healthcare workers. Additionally, these legal frameworks facilitated the integration of emerging services such as telemedicine into the healthcare system, ensuring that these services were regulated and standardized [ 38 , 40 , 61 ]. A key aspect of managing the pandemic was the establishment of effective and transparent communication systems for patients, public health authorities, and the healthcare system at large [ 60 , 61 ]. To disseminate vital information regarding the pandemic, vaccination programs, and healthcare services, authorities leveraged various channels. Public media, local online platforms, and neighborhood networks were instrumental in keeping the public informed about the ongoing situation and available services [ 53 , 60 , 86 ]. For health professionals, digital communication tools such as emails and WhatsApp groups, as well as regular meetings, were utilized to distribute clinical guidelines, government directives, and to address any queries they might have had. This ensured that healthcare workers were kept up-to-date with the evolving landscape of the pandemic and could adapt their practices accordingly [ 60 , 144 ].
Healthcare facilities function as complex socio-technical entities, combining multiple specialties and adapting to the ever-changing landscape of healthcare needs and environments [ 179 ]. To navigate this dynamic, policy makers must take into account an array of determinants—political, economic, social, and environmental—that influence health outcomes. Effective management of a health crisis necessitates robust collaboration across various sectors, including government bodies, public health organizations, primary healthcare systems, and hospitals. Such collaboration is not only pivotal during crisis management but also during the development of preparedness plans [ 63 ]. Within the health system, horizontal collaboration among departments and vertical collaboration between the Ministry of Health and other governmental departments are vital. These cooperative efforts are key to reinforce the resilience of the primary healthcare system. Moreover, a strong alliance between national pandemic response teams and primary healthcare authorities is essential to identifying and resolving issues within the PHC system [ 29 ]. On an international scale, collaborations and communications are integral to the procurement of essential medical supplies, such as medicines, equipment, and vaccines. These international partnerships are fundamental to ensuring that health systems remain equipped to face health emergencies [ 63 ].
To ensure the PHC system's preparedness and response capacity was at its best, regular and effective monitoring and evaluation programs were put in place. These included rigorous quarterly stress tests at the district level, which scrutinized the infrastructure and technology to pinpoint the system’s strengths and areas for improvement [ 43 ]. Furthermore, clinical audits were conducted to assess the structure, processes, and outcomes of healthcare programs, thereby enhancing the quality and effectiveness of the services provided [ 63 ]. These evaluation measures were crucial for maintaining a high standard of care and for adapting to the ever-evolving challenges faced by the PHC system.
Financial strategies played a critical role in enabling access to essential health services without imposing undue financial hardship. Various revenue-raising, pooling, and purchasing strategies were implemented to expand PHC financing during the pandemic, illustrating the multifaceted approach needed to sustain healthcare operations under strained circumstances [ 9 , 19 ].
In response to the COVID-19 pandemic, the Indian government took decisive action to bolster the country's healthcare infrastructure. By enhancing the financial capacity of states, the government was able to inject more funds into the Primary Health Care (PHC) system. This influx of resources made it possible to introduce schemes providing free medications and diagnostic services [ 50 ]. The benefits of increased financial resources were also felt beyond India's borders, enabling the compensation of health services in various forms. In Greece, it facilitated the monitoring and treatment of COVID-19 through in-person, home-based, and remote health services provided by physicians in private practice. Similarly, in Iran, the financial boost supported the acquisition of basic and para-clinical services from the private sector [ 21 , 65 ]. These measures reflect a broader international effort to adapt and sustain health services during a global health crisis.
The COVID-19 pandemic presented a formidable challenge to the PHC workforce worldwide. Healthcare workers were subjected to overwhelming workloads and faced significant threats to both their physical and mental well-being. To build resilience in the face of this crisis, a suite of interventions was implemented. These included recruitment strategies, training and development programs, enhanced teamwork, improved protective measures, comprehensive performance appraisals, and appropriate compensation mechanisms, as documented in Table 3 . To address staffing needs within PHC centers, a range of professionals including general practitioners, nurses, community health workers, and technical staff were either newly employed or redeployed from other healthcare facilities [ 63 ]. Expert practitioners were positioned on the frontlines, providing both in-person services and telephone consultations, acting as gatekeepers in the health system [ 49 , 63 ]. Support staff with technological expertise played a crucial role as well, assisting patients in navigating patient portals, utilizing new digital services, and conducting video visits [ 102 ]. Furthermore, the acute shortage of healthcare workers was mitigated by recruiting individuals who were retired, not currently practicing, or in training as students, as well as by enlisting volunteers. This strategy was key to bolstering the workforce and ensuring continuity of care during the pandemic [ 109 ].
During the pandemic, new training programs were developed to prepare healthcare staff for the evolving demands of their roles. These comprehensive courses covered a wide array of critical topics, including the correct use of personal protective equipment (PPE), the operation of ventilators, patient safety protocols, infection prevention, teamwork, problem-solving, self-care techniques, mental health support, strategies for managing stress, navigating and applying reliable web-based information, emergency response tactics, telemedicine, and direct care for COVID-19 patients [ 74 , 95 , 100 , 108 , 110 , 112 , 117 ].
Acknowledging the psychological and professional pressures faced by the primary healthcare workforce, health managers took active measures to safeguard both the physical and mental well-being of their employees during this challenging period [ 124 ]. Efforts to protect physical health included monitoring health status, ensuring vaccination against COVID-19, and providing adequate PPE [ 63 , 72 ]. To address mental health, a variety of interventions were deployed to mitigate anxiety and related issues among frontline workers. In Egypt, for instance, healthcare workers benefited from psychotherapy services and adaptable work schedules to alleviate stress [ 126 ]. Singapore employed complementary strategies, such as yoga, meditation, and the encouragement of religious practices, to promote relaxation among staff [ 133 ]. In the United States, the Wellness Hub application was utilized as a tool for employees to enhance their mental health [ 132 ]. In addition to health and wellness initiatives, there were financial incentives aimed at motivating employees. Payment protocols were revised, and new incentives, including scholarship opportunities and career development programs, were introduced to foster job satisfaction and motivation among healthcare workers [ 63 ].
The resilience of PHC systems during the pandemic hinged on several key improvements. Enhancing health facilities, supplying medicines and diagnostic kits, distributing vaccines, providing medical equipment, and building robust digital infrastructure were all fundamental elements that contributed to the strength of PHC systems, as outlined in Table 3 . Safe and accessible primary healthcare was facilitated through various means. Wheelchair routes were created for patients to ensure their mobility within healthcare facilities. , dedicated COVID-19 clinics were established, mass vaccination centers were opened to expedite immunization, and mobile screening stations were launched to extend testing capabilities [ 23 , 33 , 63 , 140 ].
In Iran, the distribution and availability of basic medicines were managed in collaboration with the Food and Drug Organization, ensuring that essential medications reached those in need [ 89 ]. During the outbreak, personal protective equipment (PPE) was among the most critical supplies. Access to PPE was prioritized, particularly for vulnerable groups and healthcare workers, to provide a layer of safety against the virus [ 63 ]. Vaccines were made available at no cost, with governments taking active measures to monitor their safety and side effects, to enhance their quality, and to secure international approvals. Furthermore, effective communication strategies were employed to keep the public informed about vaccine-related developments [ 32 , 83 ].
These comprehensive efforts underscored the commitment to maintaining a resilient PHC system in the face of a global health every individual in the community could access healthcare services. To facilitate this, free high-speed Wi-Fi hotspots were established, enabling patients to engage in video consultations and utilize a range of e-services without the barrier of internet costs crisis. Significant enhancements were made to the digital infrastructure. This expansion was critical in ensuring that [ 30 , 54 ]. Complementing these measures, a variety of digital health tools were deployed to further modernize care delivery. Countries like Nigeria and Germany, for instance, saw the introduction of portable electrocardiograms and telemedical stethoscopes. These innovations allowed for more comprehensive remote assessments and diagnostics, helping to bridge the gap between traditional in-person consultations and the emerging needs for telemedicine [ 141 , 180 ].
Throughout the COVID-19 pandemic, targeted interventions were implemented to bolster information systems and research efforts, as outlined in Table 3 . Key among these was the advancement of a modern, secure public health information system to ensure access to health data was not only reliable and timely but also transparent and accurate [ 33 , 45 , 49 ]. The "Open Notes" initiative in the United States exemplified this effort, guaranteeing patient access to, and editorial control over, their health records [ 141 ]. Management strategies also promoted the "one-health" approach, facilitating the exchange of health data across various departments and sectors to enhance public health outcomes [ 10 ].
In addition to these information system upgrades, active patient surveillance and early warning systems were instituted in collaboration with public health agencies. These systems played a pivotal role in detecting outbreaks, providing precise reports on the incidents, characterizing the epidemiology of pathogens, tracking their spread, and evaluating the efficacy of control strategies. They were instrumental in pinpointing areas of concern, informing smart lockdowns, and improving contact tracing methods [ 33 , 63 , 72 ]. The reinforcement of these surveillance and warning systems had a profound impact on shaping and implementing a responsive strategy to the health crisis [ 10 ].
To further reinforce the response to the pandemic, enhancing primary healthcare (PHC) research capacity became crucial. This enabled healthcare professionals and policymakers to discern both facilitators and barriers within the system and to devise fitting strategies to address emerging challenges. To this end, formal advisory groups and multidisciplinary expert panels, which included specialists from epidemiology, clinical services, social care, sociology, policy-making, and management, were convened. These groups harnessed the best available evidence to inform decision-making processes [ 30 ]. Consequently, research units were established to carry out regular telephone surveys and to collect data on effective practices, as well as new diagnostic and therapeutic approaches [ 31 , 89 ]. The valuable insights gained from these research endeavors were then disseminated through trusted channels to both the public and policymakers, ensuring informed decisions at all levels [ 36 ].
The COVID-19 pandemic acted as a catalyst for the swift integration of telemedicine into healthcare systems globally. This period saw healthcare providers leverage telecommunication technologies to offer an array of remote services, addressing medical needs such as consultations, diagnosis, monitoring, and prescriptions. This transition was instrumental in ensuring care continuity and mitigating infection risks for both patients and healthcare workers, highlighting an innovative evolution in healthcare delivery [ 170 , 181 ].
Countries adapted to this new model of healthcare with varied applications: Armenia established telephone follow-ups and video consultations for remote patient care, while e-pharmacies and mobile health tools provided immediate access to medical information and services [ 29 ]. In France and the United States, tele-mental health services and online group support became a means to support healthy living during the pandemic [ 147 , 158 ] . New Zealand introduced the Aroha chatbot, an initiative to assist with mental health management [ 139 ].
The implementation and effectiveness of these telehealth services were not limited by economic barriers, as underscored by Pradhan et al. (2023), who noted the key role of telemedicine in low and middle-income countries. These countries embraced the technology to maintain health service operations, proving its global applicability and utility [ 178 ]. The widespread adoption of telemedicine, therefore, represents a significant and perhaps lasting shift in healthcare practice, one that has redefined patient care in the face of a global health crisis and may continue to shape the future of healthcare delivery [ 170 , 178 , 181 ].
The study highlighted PHC strengthening strategies in COVID-19 time . Notably, the adaptations and reforms spanned across governance, financing, workforce management, information system, infrastructural readiness, and service delivery enhancements. These interventions collectively contributed to the robustness of health systems against the sudden surge in demand and the multifaceted challenges imposed by the pandemic and resulted.
Significantly, the findings have broader implications for health policy and system design worldwide. The pandemic has highlighted the critical need for resilient health systems that are capable of not only responding to health emergencies but also maintaining continuity in essential services. The strategies documented in this review serve as a template for countries to fortify their health systems by embedding resilience into their PHC frameworks (Fig. 4 ). Future health crises can be better managed by learning from these evidenced responses, which emphasize the necessity of integrated, well-supported, and dynamically adaptable health care structures.
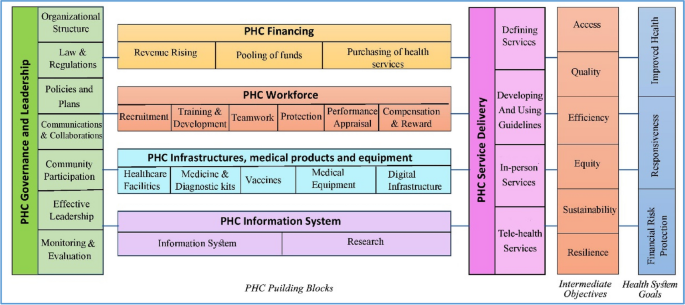
A model for strengthening the resilience of the primary health care system
Looking ahead, realist reviews could play a pivotal role in refining PHC resilience strategies. By understanding the context in which specific interventions succeed or fail, realist reviews can help policymakers and practitioners design more effective health system reforms, as echoed in the need for evidence-based planning in health system governance [ 9 ] . These reviews offer a methodological advantage by focusing on the causality between interventions and outcomes, aligning with the importance of effective health system leadership and management [ 50 , 182 ] . They take into account the underlying mechanisms and contextual factors, thus providing a nuanced understanding that is crucial for tailoring interventions to meet local needs effectively [ 28 , 86 ] , ultimately leading to more sustainable health systems globally. This shift towards a more analytical and context-sensitive approach in evaluating health interventions, as supported by WHO's framework for action [ 2 , 10 ] , will be crucial for developing strategies that are not only effective in theory but also practical and sustainable in diverse real-world settings.
Limitations and future research
In our comprehensive scoping review, we analyzed 167 articles out of a dataset of 4,315, classifying 194 interventions that build resilience in primary healthcare systems across the globe in response to pandemics like COVID-19. While the review's extensive search provides a sweeping overview of various strategies, it may not capture the full diversity of interventions across all regions and economies. Future research should focus on meta-analyses to evaluate the effectiveness of these interventions in greater detail and employ qualitative studies to delve into the specific challenges and successes, thus gaining a more nuanced understanding of the context. As the review includes articles only up to December 31, 2022, it may overlook more recent studies. Regular updates, a broader linguistic range, and the inclusion of a more diverse array of databases are recommended to maintain relevance and expand the breadth of literature, ultimately guiding more focused research that could significantly enhance the resilience of PHC systems worldwide.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
Primary Health Care
World Health Organization
Sustainable Development Goals
Universal Health Coverage
Personal Protective Equipment
General Practitioner
Mosadeghrad AM. A practical model for health policy making and analysis. Payesh. 2022;21(1):7–24 ([in Persian]).
Article Google Scholar
World Health Organization. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes. WHO’s Framework for Action. Geneva: World Health Organization; 2007.
Google Scholar
Khosravi MF, Mosadeghrad AM, Arab M. Health System Governance Evaluation: A Scoping Review. Iran J Public Health. 2023;52(2):265.
PubMed PubMed Central Google Scholar
Mosadeghrad AM, Abbasi M, Abbasi M, Heidari M. Sustainable health financing methods in developing countries: a scoping review. J of School Public Health Inst Public Health Res. 2023;20(4):358–78 ([in Persian]).
Mosadeghrad AM. Health strengthening plan, a supplement to Iran health transformation plan: letter to the editor. Tehran Univ Med J. 2019;77(8):537–8 ([in Persian]).
World Health Organization. Declaration of alma-ata. Copenhagen: Regional Office for Europe; 1978. p. 1–4.
Rasanathan K, Evans TG. Primary health care, the Declaration of Astana and COVID-19. Bull World Health Organ. 2020;98(11):801.
Article PubMed PubMed Central Google Scholar
World Health Organization, UNICEF. Operational framework for primary health care: transforming vision into action. Geneva: World Health Organization and the United Nations Children’s Fund; 2020.
Mosadeghrad AM, Heydari M, Esfahani P. Primary health care strengthening strategies in Iran: a realistic review. J School Public Health Inst Public Health Res. 2022;19(3):237–58 ([in Persian]).
Sagan A, Webb E, Azzopardi-Muscat N, de la Mata I, McKee M, Figueras J. Health systems resilience during COVID-19: Lessons for building back better. Regional Office for Europe: World Health Organization; 2021.
World Health Organization, Coronavirus (COVID-19) map. Available at https://covid19.who.int/ /. Access date 14/04/2024.
Plagg B, Piccoliori G, Oschmann J, Engl A, Eisendle K. Primary health care and hospital management during COVID-19: lessons from lombardy. Risk Manag Healthc Policy. 2021:3987–92.
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
Mosadeghrad AM, Jajarmizadeh A. Continuity of essential health services during the COVID-19 pandemic. Tehran Univ Med J. 2021;79(10):831–2 ([in Persian]).
Splinter MJ, Velek P, Ikram MK, Kieboom BC, Peeters RP, Bindels PJ, Ikram MA, Wolters FJ, Leening MJ, de Schepper EI, Licher S. Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med. 2021;18(11):e1003854.
Article CAS PubMed PubMed Central Google Scholar
Wangmo S, Sarkar S, Islam T, Rahman MH, Landry M. Maintaining essential health services during the pandemic in Bangladesh: the role of primary health care supported by routine health information system. WHO South East Asia J Public Health. 2021;10(3):93.
Kumpunen S, Webb E, Permanand G, Zheleznyakov E, Edwards N, van Ginneken E, Jakab M. Transformations in the landscape of primary health care during COVID-19: Themes from the European region. Health Policy. 2022;126(5):391–7.
Article PubMed Google Scholar
Ezzati F, Mosadeghrad AM, Jaafaripooyan E. Resiliency of the Iranian healthcare facilities against the Covid-19 pandemic: challenges and solutions. BMC Health Serv Res. 2023;23(207):1–16.
Mosadeghrad AM, Isfahani P, Eslambolchi L, Zahmatkesh M, Afshari M. Strategies to strengthen a climate-resilient health system: a scoping review. Global Health. 2023;19(1):62.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005;8(1):19–32.
Akrami F, Riazi-Isfahani S, Mahdavi hezaveh A, Ghanbari Motlagh A, Najmi M, Afkar M, et al. Iran’s Status of NCDs Prevention and Management Services during COVID-19 Pandemic at PHC Level. SJKU. 2021;26(5):50–68.
Etienne CF, Fitzgerald J, Almeida G, Birmingham ME, Brana M, Bascolo E, Cid C, Pescetto C. COVID-19: transformative actions for more equitable, resilient, sustainable societies and health systems in the Americas. BMJ Global Health. 2020;5(8):e003509.
Tabrizi JS, Raeisi A, Namaki S. Primary health care and COVID-19 Pandemic in the Islamic Republic of Iran. Depict Health. 2022;13(Suppl 1):S1-10.
Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, Wouters E, Van Olmen J. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21:1–6.
Goodyear-Smith F, Kidd M, Oseni TIA, Nashat N, Mash R, Akman M, Phillips RL, van Weel C. Internationalexamples of primary care COVID-19 preparedness and response: a comparison of four countries. Fam MedCommunity Health. 2022;10(2):e001608.
Kinder K, Bazemore A, Taylor M, Mannie C, Strydom S, George J, Goodyear-Smith F. Integrating primary care and public health to enhance response to a pandemic. Prim Health Care Res Dev. 2021;22:e27.
De Maeseneer J. Prim Health Care Res Dev. 2021;22:e73.
Westfall JM, Liaw W, Griswold K, Stange K, Green LA, Phillips R, Bazemore A, Jaén CR, Hughes LS, DeVoe J, Gullett H. Uniting public health and primary care for healthy communities in the COVID-19 era and beyond. J Am Board Fam Med. 2021;34(Supplement):S203-9.
Johansen AS, Shriwise A, Lopez-Acuna D, Vracko P. Strengthening the primary health care response to COVID-19: an operational tool for policymakers. Prim Health Care ResDev. 2021;22:e81.
Reath J, Lau P, Lo W, Trankle S, Brooks M, Shahab Y, Abbott P. Strengthening learning and research in health equity–opportunities for university departments of primary health care and general practice. Aust J Prim Health. 2022;29(2):131–6.
Ferenčina J, Tomšič V. COVID-19 clinic as a basis of quality primary health care in the light of the pandemic - an observational study. Med Glas (Zenica). 2022;19(1). https://doi.org/10.17392/1437-21 .
Mosadeghrad AH. Promote COVID-19 vaccination uptake: a letter to editor. Tehran Univ Med Sci J. 2022;80(2):159–60.
Chaiban L, Benyaich A, Yaacoub S, Rawi H, Truppa C, Bardus M. Access to primary and secondary health care services for people living with diabetes and lower-limb amputation during the COVID-19 pandemic in Lebanon: a qualitative study. BMC Health Serv Res. 2022;22(1):593.
Džakula A, Banadinović M, Lovrenčić IL, Vajagić M, Dimova A, Rohova M, Minev M, Scintee SG, Vladescu C, Farcasanu D, Robinson S. A comparison of health system responses to COVID-19 in Bulgaria, Croatia and Romania in 2020. Health Policy. 2022;126(5):456–64.
Ghazi Saeedi M, Tanhapour M. Telemedicine System: A Mandatory Requirement in Today’s World. Payavard. 2022;15(5):490–507.
Ferorelli D, Nardelli L, Spagnolo L, Corradi S, Silvestre M, Misceo F, Marrone M, Zotti F, Mandarelli G, Solarino B, Dell’Erba A. Medical legal aspects of telemedicine in Italy: application fields, professional liability and focus on care services during the COVID-19 health emergency. J Prim CareCommun Health. 2020;11:2150132720985055.
CAS Google Scholar
Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS. Actualizing better health and health care for older adults: commentary describes six vital directions to improve the care and quality of life for all older Americans. Health Aff. 2021;40(2):219–25.
Hernández Rincón EH, Pimentel González JP, Aramendiz Narváez MF, Araujo Tabares RA, Roa González JM. Description and analysis of primary care-based COVID-19 interventions in Colombia. Medwave. 2021;21(3):e8147.
Giannopoulou I, Tsobanoglou GO. COVID-19 pandemic: challenges and opportunities for the Greek health care system. Irish J Psychol Med. 2020;37(3):226–30.
Chow C, Goh SK, Tan CS, Wu HK, Shahdadpuri R. Enhancing frontline workforce volunteerism through exploration of motivations and impact during the COVID-19 pandemic. Int J Disaster Risk Reduct. 2021;1(66):102605.
Alboksmaty A, Kumar S, Parekh R, Aylin P. Management and patient safety of complex elderly patients in primary care during the COVID-19 pandemic in the UK—Qualitative assessment. PLoS One. 2021;16(3):e0248387.
Savoy A, Patel H, Shahid U, Offner AD, Singh H, Giardina TD, Meyer AN. Electronic Co-design (ECO-design) Workshop for Increasing Clinician Participation in the Design of Health Services Interventions: Participatory Design Approach. JMIR Hum Fact. 2022;9(3):e37313.
Tumusiime P, Karamagi H, Titi-Ofei R, Amri M, Seydi AB, Kipruto H, Droti B, Zombre S, Yoti Z, Zawaira F, Cabore J. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the Fifth Health Sector Directors’ Policy and Planning Meeting for the WHO African Region. BMC Proc. 2020;14:1–8 (BioMed Central).
Atoofi MK, Rezaei N, Kompani F, Shirzad F, Sh D. Requirements of mental health services during the COVID-19 outbreak: a systematic review. Iran J Psychiatry Clin Psychol. 2020;26(3):264–79.
Mosadeghrad AM, Taherkhani T, Shojaei S, Jafari M, Mohammadi S, Emamzadeh A, Akhavan S. Strengthening primary health care system resilience in COVID-19 pandemic: a scoping review. sjsph 2022;20(1):13-24.
Fotokian Z, Mohammadkhah F. Primary health care as a strategy to fight COVID-19 pandemic: letter to the editor. J Isfahan Med School. 2021;39(630):470–4. https://doi.org/10.22122/jims.v39i630.14016 .
Li D, Howe AC, Astier-Peña MP. Primary health care response in the management of pandemics: Learnings from the COVID-19 pandemic. Atención Primaria. 2021;1(53):102226.
Chua AQ, Tan MMJ, Verma M, Han EKL, Hsu LY, Cook AR, et al. BMJ Global Health. 2020;5(9):e003317.
Eisele M, Pohontsch NJ, Scherer M. Strategies in primary care to face the SARS-CoV-2/COVID-19 pandemic: an online survey. Front Med. 2021;2(8):613537.
Lamberti-Castronuovo A, Valente M, Barone-Adesi F, Hubloue I, Ragazzoni L. Primary health care disaster preparedness: a review of the literature and the proposal of a new framework. Int J Dis Risk Reduct. 2022;2:103278.
Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, Burey S, Feldman M, Morris SK. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario Canada. Vaccine. 2021;39(31):4373–82.
Saxenian H, Alkenbrack S, Freitas Attaran M, Barcarolo J, Brenzel L, Brooks A, Ekeman E, Griffiths UK, Rozario S, Vande Maele N, Ranson MK. Sustainable financing for Immunization Agenda 2030. Vaccine. 2024;42 Suppl 1:S73-S81. https://doi.org/10.1016/j.vaccine.2022.11.037 .
Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint—the immunising pregnant women and infants network. Vaccines. 2020;8(3):556.
Sagan A, Thomas S, McKee M, Karanikolos M, Azzopardi-Muscat N, de la Mata I, Figueras J, World Health Organization. COVID-19 and health systems resilience: lessons going forwards. Eurohealth. 2020;26(2):20–4.
Celuppi IC, Meirelles BH, Lanzoni GM, Geremia DS, Metelski FK. Management in the care of people with HIV in primary health care in times of the new coronavirus. Revista de Saúde Pública. 2022;1(56):13.
Denis JL, Potvin L, Rochon J, Fournier P, Gauvin L. On redesigning public health in Québec: lessons learned from the pandemic. Can J Public Health= Revue Canadienne de Sante Publique. 2020;111(6):912.
PubMed Google Scholar
Wilson G, Windner Z, Dowell A, Toop L, Savage R, Hudson B. Navigating the health system during COVID-19: primary care perspectives on delayed patient care. N Z Med J. 2021;134(1546):17–27 (PMID: 34855730).
Zhang N, Yang S, Jia P. Cultivating resilience during the COVID-19 pandemic: a socioecological perspective. Annu Rev Psychol. 2022;4(73):575–98. https://doi.org/10.1146/annurev-psych-030221-031857 . (Epub 2021 Sep 27 PMID: 34579547).
Al Ghafri T, Al Ajmi F, Al Balushi L, Kurup PM, Al Ghamari A, Al Balushi Z, Al Fahdi F, Al Lawati H, Al Hashmi S, Al Manji A, Al Sharji A. Responses to the pandemic covid-19 in primary health care in oman: muscat experience. Oman Med J. 2021;36(1):e216.
Adler L, Vinker S, Heymann AD, Van Poel E, Willems S, Zacay G. The effect of the COVID-19 pandemic on primary care physicians in Israel, with comparison to an international cohort: a cross-sectional study. Israel J Health Policy Res. 2022;11(1):1.
Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur RE, Walley J. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10(12):e041622.
Hussein ES, Al-Shenqiti AM, Ramadan RM. Applications of medical digital technologies for noncommunicable diseases for follow-up during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(19):12682.
Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. 2021;38(6):811–25.
Sandhu HS, Smith RW, Jarvis T, O’Neill M, Di Ruggiero E, Schwartz R, Rosella LC, Allin S, Pinto AD. Early impacts of the COVID-19 pandemic on public health systems and practice in 3 Canadian provinces from the perspective of public health leaders: a qualitative study. J Public Health Manag Pract. 2022;28(6):702–11.
Farsalinos K, Poulas K, Kouretas D, Vantarakis A, Leotsinidis M, Kouvelas D, Docea AO, Kostoff R, Gerotziafas, Antoniou MN, Polosa R. Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicol Rep. 2021;8:1–9.
Article CAS PubMed Google Scholar
Fitzpatrick K, Sehgal A, Montesanti S, Pianarosa E, Barnabe C, Heyd A, Kleissen T, Crowshoe L. Examining the role of Indigenous primary healthcare across the globe in supporting populations during public health crises. Global Public Health. 2022;24:1–29.
Liaw ST, Kuziemsky C, Schreiber R, Jonnagaddala J, Liyanage H, Chittalia A, Bahniwal R, He JW, Ryan BL, Lizotte DJ, Kueper JK. Primary care informatics response to Covid-19 pandemic: adaptation, progress, and lessons from four countries with high ICT development. Yearbook Med Inform. 2021;30(01):044–55.
Djalante R, Shaw R, DeWit A. Progress in disaster. Science. 2020;6:100080.
Fatima R, Akhtar N, Yaqoob A, Harries AD, Khan MS. Building better tuberculosis control systems in a post-COVID world: learning from Pakistan during the COVID-19 pandemic. Int J Infect Dis. 2021;1(113):S88-90.
Shin WY, Kim C, Lee SY, Lee W, Kim JH. Role of primary care and challenges for public–private cooperation during the coronavirus disease 2019 pandemic: An expert Delphi study in South Korea. Yonsei Med J. 2021;62(7):660.
Thompson RN, et al. Key questions for modelling COVID-19exit strategies. Proc R Soc B. 2020;287:20201405. https://doi.org/10.1098/rspb.2020.1405 .
Baral P. Health systems and services during COVID-19: lessons and evidence from previous crises: a rapid scoping review to inform the United Nations research roadmap for the COVID-19 recovery. Int J Health Serv. 2021;51(4):474–93.
Daou M, Helou S, El Helou J, El Hachem C, El Helou E. Ensuring care continuity in extreme crises: A participatory action research approach. InMEDINFO 2021: One World, One Health–Global Partnership for Digital Innovation 2022 (pp. 937-941). IOS Press.
Besigye IK, Namatovu J, Mulowooza M. Coronavirus disease-2019 epidemic response in Uganda: the need to strengthen and engage primary healthcare. Afr J Prim Health Care Fam Med. 2020;12(1):1–3.
Silva MJ, Santos P. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: a cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5421. https://doi.org/10.3390/ijerph18105421 . (PMID:34069438;PMCID:PMC8159089).
Sultana A, Bhattacharya S, Hossain MM. COVID-19 and primary care: a critical need for strengthening emergency preparedness across health systems. J Fam Med Primary Care. 2021;10(1):584–5.
Xu RH, Shi LS, Xia Y, Wang D. Associations among eHealth literacy, social support, individual resilience, and emotional status in primary care providers during the outbreak of the SARS-CoV-2 Delta variant. Digit Health. 2022;25(8):20552076221089788. https://doi.org/10.1177/20552076221089789 . (PMID:35355807;PMCID:PMC8958311).
Bajgain BB, Jackson J, Aghajafari F, Bolo C, Santana MJ. Immigrant Healthcare Experiences and Impacts During COVID-19: A Cross-Sectional Study in Alberta Canada. J Patient Exp. 2022;9:23743735221112708.
Kim AY, Choi WS. Considerations on the implementation of the telemedicine system encountered with stakeholders’ resistance in COVID-19 pandemic. Telemed e-Health. 2021;27(5):475–80.
Tayade MC. Strategies to tackle by primary care physicians to mental health issues in India in COVId-19 pandemic. J Fam Med Prim Care. 2020;9(11):5814–5.
Thomas C. Resilient health and care: Learning the lessons of Covid-19 in the English NHS, IPPR. 2020. http://www.ippr.org/research/publications/resilient-health-and-care .
Saab MM, O’Driscoll M, FitzGerald S, Sahm LJ, Leahy-Warren P, Noonan B, Kilty C, Lyons N, Burns HE, Kennedy U, Lyng Á. Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study. BMC Prim Care. 2022;23(1):1–5.
Ma L, Han X, Ma Y, Yang Y, Xu Y, Liu D, Yang W, Feng L. Decreased influenza vaccination coverage among Chinese healthcare workers during the COVID-19 pandemic. Infect Dis Pov. 2022;11(05):63–73.
Ismail SA, Lam ST, Bell S, Fouad FM, Blanchet K, Borghi J. Strengthening vaccination delivery system resilience in the context of protracted humanitarian crisis: a realist-informed systematic review. BMC Health Serv Res. 2022;22(1):1–21.
Litke N, Weis A, Koetsenruijter J, Fehrer V, Koeppen M, Kuemmel S, Szecsenyi J, Wensing M. Building resilience in German primary care practices: a qualitative study. BMC Prim Care. 2022;23(1):1–4.
Den Broeder L, South J, Rothoff A, Bagnall AM, Azarhoosh F, Van Der Linden G, Bharadwa M, Wagemakers A. Community engagement in deprived neighbourhoods during the COVID-19 crisis: perspectives for more resilient and healthier communities. Health promotion international. 2022;37(2):daab098.
Sundararaman T, Muraleedharan VR, Ranjan A. Pandemic resilience and health systems preparedness: lessons from COVID-19 for the twenty-first century. J Soc Econ Dev. 2021;23(Suppl 2):1–11. https://doi.org/10.1007/s40847-020-00133-x . (Epub ahead of print. PMID: 34720480; PMCID: PMC7786882).
Ferreira NN, Garibaldi PM, Moraes GR, Moura JC, Klein TM, Machado LE, Scofoni LF, Haddad SK, Calado RT, Covas DT, Fonseca BA. The impact of an enhanced health surveillance system for COVID-19 management in Serrana, Brazil. Public Health Pract. 2022;1(4):100301.
Harzheim E, Martins C, Wollmann L, Pedebos LA, Faller LD, Marques MD, Minei TS, Cunha CR, Telles LF, Moura LJ, Leal MH. Federal actions to support and strengthen local efforts to combat COVID-19: Primary Health Care (PHC) in the driver’s seat. Ciência Saúde Coletiva. 2020;5(25):2493–7.
Smaggus A, Long J, Ellis LA, Clay-Williams R, Braithwaite J. Government actions and their relation to resilience in healthcare during the COVID-19 pandemic in New South Wales, Australia and Ontario, Canada. Int J Health Policy Manag. 2022;11(9):1682–94. https://doi.org/10.34172/ijhpm.2021.67 .
Tselebis A, Pachi A. Primary mental health care in a New Era. Healthcare (Basel). 2022;10(10):2025. https://doi.org/10.3390/healthcare10102025 . (PMID:36292472;PMCID:PMC9601948).
Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, Mathijssen E, Smit LC, Stalpers D, Schoonhoven L, Veldhuizen JD, Trappenburg JC. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11(1):e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Basu P, Alhomoud S, Taghavi K, Carvalho AL, Lucas E, Baussano I. Cancer screening in the coronavirus pandemic era: adjusting to a new situation. JCO Global Oncol. 2021;7(1):416–24.
Rieckert A, Schuit E, Bleijenberg N, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11:e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Shaikh BT. Strengthening health system building blocks: configuring post-COVID-19 scenario in Pakistan. Prim Health Care Res Dev. 2021;22:e9 Cambridge University Press.
Franzosa E, Gorbenko K, Brody AA, Leff B, Ritchie CS, Kinosian B, Ornstein KA, Federman AD. “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2021;69(2):300–6.
Adhikari B, Mishra SR, Schwarz R. Transforming Nepal’s primary health care delivery system in global health era: addressing historical and current implementation challenges. Global Health. 2022;18(1):1–2.
Mas Bermejo P, Sánchez Valdés L, Somarriba López L, Valdivia Onega NC, Vidal Ledo MJ, Alfonso Sánchez I, et al. Equity and the Cuban National Health System's response to COVID-19. Rev Panam Salud Publica. 2021;45:e80. https://doi.org/10.26633/RPSP.2021.80 .
Gong F, Hu G, Lin H, Sun X, Wang W. Integrated Healthcare Systems Response Strategies Based on the Luohu Model During the COVID-19 Epidemic in Shenzhen, China. Int J Integr Care. 2021;21(1):1. https://doi.org/10.5334/ijic.5628 .
Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(Supplement):S61-70.
Teng K, Russo F, Kanuch S, Caron A. Virtual Care Adoption-Challenges and Opportunities From the Lens of Academic Primary Care Practitioners. J Public Health Manag Pract. 2022;28(6):599–602. https://doi.org/10.1097/PHH.0000000000001548 . (Epub 2022 Aug 27. PMID: 36037465; PMCID: PMC9555588).
Anaya YB, Mota AB, Hernandez GD, Osorio A, Hayes-Bautista DE. Post-pandemic telehealth policy for primary care: an equity perspective. J Am Board Fam Med. 2022;35(3):588–92.
Florea M, Lazea C, Gaga R, Sur G, Lotrean L, Puia A, Stanescu AM, Lupsor-Platon M, Florea H, Sur ML. Lights and shadows of the perception of the use of telemedicine by Romanian family doctors during the COVID-19 pandemic. Int J Gen Med. 2021;14:1575.
Selick A, Durbin J, Hamdani Y, Rayner J, Lunsky Y. Accessibility of Virtual Primary Care for Adults With Intellectual and Developmental Disabilities During the COVID-19 Pandemic: Qualitative Study. JMIR Form Res 2022;6(8):e38916. https://formative.jmir.org/2022/8/e38916 . https://doi.org/10.2196/38916 .
Frost R, Nimmons D, Davies N. Using remote interventions in promoting the health of frail older persons following the COVID-19 lockdown: challenges and solutions. J Am Med Direct Assoc. 2020;21(7):992.
Suija K, Mard LA, Laidoja R, et al. Experiences and expectation with the use of health data: a qualitative interview study in primary care. BMC Prim Care. 2022;23:159. https://doi.org/10.1186/s12875-022-01764-1 .
Sullivan EE, McKinstry D, Adamson J, Hunt L, Phillips RS, Linzer M. Burnout Among Missouri Primary Care Clinicians in 2021: Roadmap for Recovery? Mo Med. 2022;119(4):397–400 (PMID: 36118800; PMCID: PMC9462904).
Tang C, Chen X, Guan C, Fang P. Attitudes and Response Capacities for Public Health Emergencies of Healthcare Workers in Primary Healthcare Institutions: A Cross-Sectional Investigation Conducted in Wuhan, China, in 2020. Int Environ Res Public Health. 2022;19(19):12204. https://doi.org/10.3390/ijerph191912204 .
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T, Tan SM, Bartos M, Mabuchi S, Bonk M, McNab C, Werner GK, Panjabi R, Nordström A, Legido-Quigley H. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964-80. https://doi.org/10.1038/s41591-021-01381-y .
Berger Z, De Jesus VA, Assoumou SA, Greenhalgh T. Long COVID and health inequities: the role of primary care. Milbank Q. 2021;99(2):519.
Haldane V, Dodd W, Kipp A, Ferrolino H, Wilson K, Servano D, Lau LL, Wei X. Extending health systems resilience into communities: a qualitative study with community-based actors providing health services during the COVID-19 pandemic in the Philippines. BMC Health Serv Res. 2022;22(1):1–2.
Haun JN, Cotner BA, Melillo C, Panaite V, Messina W, Patel-Teague S, Zilka B. Proactive integrated virtual healthcare resource use in primary care. BMC Health Serv Res. 2021;21(1):1–4.
Kelly F, Uys M, Bezuidenhout D, Mullane SL, Bristol C. Improving Healthcare Worker Resilience and Well-Being During COVID-19 Using a Self-Directed E-Learning Intervention. Front Psychol. 2021;12:748133. https://doi.org/10.3389/fpsyg.2021.748133 .
Thekkur P, Fernando M, Nair D, Kumar AMV, Satyanarayana S, Chandraratne N, Chandrasiri A, Attygalle DE, Higashi H, Bandara J, Berger SD, Harries AD. Primary Health Care System Strengthening Project in Sri Lanka: Status and Challenges with Human Resources, Information Systems, Drugs and Laboratory Services. Healthcare. 2022;10(11):2251. https://doi.org/10.3390/healthcare10112251 .
Balogun M, Banke-Thomas A, Gwacham-Anisiobi U, Yesufu V, Ubani O, Afolabi BB. Actions and AdaptationsImplemented for Maternal, Newborn and Child Health Service Provision During the Early Phase of the COVID-19 Pandemic in Lagos, Nigeria: Qualitative Study of Health Facility Leaders. Ann Glob Health. 2022;88(1):13. https://doi.org/10.5334/aogh.3529 .
Llamas S, MP AP, Felipe P. Patient safety training and a safe teaching in primary care. Aten Primaria. 2021;53 Suppl 1(Suppl 1):102199.
Eze-Emiri C, Patrick F, Igwe E, Owhonda G. Retrospective study of COVID-19 outcomes among healthcare workers in Rivers State, Nigeria. BMJ Open. 2022;12(11):e061826.
Golechha M, Bohra T, Patel M, Khetrapal S. Healthcare worker resilience during the COVID-19 pandemic: a qualitative study of primary care providers in India. World Med Health Policy. 2022;14(1):6–18.
Gómez-Restrepo C, Cepeda M, Torrey WC, Suarez-Obando F, Uribe-Restrepo JM, Park S, Acosta MP, Camblor PM, Castro SM, Aguilera-Cruz J, González L. Perceived access to general and mental healthcare in primary care in Colombia during COVID-19: A cross-sectional study. Frontiers in Public Health. 2022;10:896318.
Nejat N, Borzabadi Farahani Z. COVID-19 pandemic: opportunities for continuing nursing professional development. J Med Educ Dev. 2022;14(44):1–2.
DeVoe JE, Cheng A, Krist A. JAMA Health Forum. 2020;1(4):e200423.
Hoeft TJ, Hessler D, Francis D, Gottlieb LM. Applying lessons from behavioral health integration to social care integration in primary care. Ann Fam Med. 2021;19(4):356–61.
Silsand L, Severinsen GH, Berntsen G. Preservation of Person-Centered care through videoconferencing for patient follow-up during the COVID-19 pandemic: case study of a multidisciplinary care team. JMIR Format Res. 2021;5(3):e25220.
Sullivan E, Phillips R.S. Sustaining primary care teams in the midst of a pandemic. Isr J Health Policy Res. 2020; 9. 77. https://doi.org/10.1186/s13584-020-00434-w .
Abd El Kader AI, Faramawy MA. COVID-19 anxiety and organizational commitment among front line nurses: Perceived role of nurse managers' caring behavior. Nurs Pract Today. 2022;9(1):X.
Croghan IT, Chesak SS, Adusumalli J, Fischer KM, Beck EW, Patel SR, Ghosh K, Schroeder DR, Bhagra A. Stress, resilience, and coping of healthcare workers during the COVID-19 pandemic. J Prim Care Commun Health. 2021;12:21501327211008450.
Aragonès E, del Cura-González I, Hernández-Rivas L, Polentinos-Castro E, Fernández-San-Martín MI, López-Rodríguez JA, Molina-Aragonés JM, Amigo F, Alayo I, Mortier P, Ferrer M. Psychological impact of the COVID-19 pandemic on primary care workers: a cross-sectional study. Br J Gen Pract. 2022;72(720):e501-10.
Franck E, Goossens E, Haegdorens F, Geuens N, Portzky M, Tytens T, Dilles T, Beeckman K, Timmermans O, Slootmans S, Van Rompaey B. Role of resilience in healthcare workers’ distress and somatization during the COVID-19 pandemic: a cross-sectional study across Flanders Belgium. Nurs Open. 2022;9(2):1181–9.
DeTore NR, Sylvia L, Park ER, Burke A, Levison JH, Shannon A, et al. J Psychiatr Res. 2022;146:228–33.
Shi LS, Xu RH, Xia Y, Chen DX, Wang D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: the mediating effects of social support and resilience. Front Psychol. 2022;21(12):800183. https://doi.org/10.3389/fpsyg.2021.800183 . (PMID:35126252;PMCID:PMC8814425).
Golden EA, Zweig M, Danieletto M, Landell K, Nadkarni G, Bottinger E, Katz L, Somarriba R, Sharma V, Katz CL, Marin DB. A resilience-building app to support the mental health of health care workers in the COVID-19 era: Design process, distribution, and evaluation. JMIR Format Res. 2021;5(5):e26590.
Chan AY, Ting C, Chan LG, Hildon ZJ. “The emotions were like a roller-coaster”: a qualitative analysis of e-diary data on healthcare worker resilience and adaptation during the COVID-19 outbreak in Singapore. Hum Resour Health. 2022;20(1):60.
Ashley C, James S, Williams A, Calma K, Mcinnes S, Mursa R, Stephen C, Halcomb E. The psychological well-being of primary healthcare nurses during COVID-19: a qualitative study. J Adv Nurs. 2021;77(9):3820–8.
Carmona LE, Nielfa MD, Alvarado AL. The Covid-19 pandemic seen from the frontline. Int Braz J Urol. 2020;27(46):181–94.
Delobelle PA, Abbas M, Datay I, De Sa A, Levitt N, Schouw D, Reid S. Non-communicable disease care and management in two sites of the Cape Town Metro during the first wave of COVID-19: A rapid appraisal. Afr J Prim Health Care Fam Med. 2022;14(1):e1-e7. https://doi.org/10.4102/phcfm.v14i1.3215 .
Luciani S, Agurto I, Caixeta R, Hennis A. Prioritizing noncommunicable diseases in the Americas region in the era of COVID-19. Rev Panam Salud Publica. 2022;46:e83. https://doi.org/10.26633/RPSP.2022.83 .
Cabral IE, Pestana-Santos M, Ciuffo LL, Nunes YDR, Lomba MLLF. Child health vulnerabilities during the COVID-19 pandemic in Brazil and Portugal. Rev Lat Am Enfermagem. 2021;29:e3422. https://doi.org/10.1590/1518-8345.4805.3422 . (Published 2021 Jul 2).
Ludin N, Holt-Quick C, Hopkins S, Stasiak K, Hetrick S, Warren J, Cargo T. A Chatbot to support young people during the COVID-19 Pandemic in New Zealand: evaluation of the real-world rollout of an open trial. J Med Internet Res. 2022;24(11):e38743.
Breton M, Deville-Stoetzel N, Gaboury I, Smithman MA, Kaczorowski J, Lussier MT, Haggerty J, Motulsky A, Nugus P, Layani G, Paré G. Telehealth in primary healthcare: a portrait of its rapid implementation during the COVID-19 pandemic. Healthcare Policy. 2021;17(1):73.
Knop M, Mueller M, Niehaves B. Investigating the use of telemedicine for digitally mediated delegation in team-based primary care: mixed methods study. J Med Internet Res. 2021;23(8):e28151.
Zamiela C, Hossain NUI, Jaradat R. Enablers of resilience in the healthcare supply chain: A case study of U.S healthcare industry during COVID-19 pandemic. Res Transport Econ. 2022;93:101174. https://doi.org/10.1016/j.retrec.2021.101174 . Epub 2021 Dec 24. PMCID: PMC9675944.
Lukong AM, Jafaru Y. Covid-19 pandemic challenges, coping strategies and resilience among healthcare workers: a multiple linear regression analysis. Afr J Health Nurs Midwifery. 2021;4:16–27.
Hearnshaw S, Serban S, Mohammed I, Zubair A, Jaswal D, Grant S. A local dental network approach to the COVID-19 pandemic: innovation through collaboration. Prim Dental J. 2021;10(1):33–9.
Haase CB, Bearman M, Brodersen J, Hoeyer K, Risor T. ‘You should see a doctor’, said the robot: Reflections on a digital diagnostic device in a pandemic age. Scand J Public Health. 2021;49(1):33–6.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobilehealth tools to support COVID-19 training and surveillance in Ogun State Nigeria. Frontiers in Sustainable Cities. 2021;3:638278:1-9.
Ibragimov K, Palma M, Keane G, Ousley J, Crowe M, Carreño C, Casas G, Mills C, Llosa A. Shifting to Tele-Mental Health in humanitarian and crisis settings: an evaluation of Médecins Sans Frontières experience during the COVID-19 pandemic. Conflict Health. 2022;16(1):1–5.
Wherton J, Greenhalgh T, Hughes G, Shaw SE. The role of information infrastructures in scaling up video consultations during COVID-19: mixed methods case study into opportunity, disruption, and exposure. J Med Internet Res. 2022;24(11):e42431. https://doi.org/10.2196/42431 . (PMID:36282978;PMCID:PMC9651004).
Jonnagaddala J, Godinho MA, Liaw ST. From telehealth to virtual primary care in Australia? a rapid scoping review. Int J Med Inform. 2021;1(151):104470.
Tanemura N, Chiba T. The usefulness of a checklist approach-based confirmation scheme in identifying unreliable COVID-19-related health information: a case study in Japan. Humanit Soc Sci Commun. 2022;9(1):270. https://doi.org/10.1057/s41599-022-01293-3 . (Epub 2022 Aug 15. PMID: 35990766; PMCID: PMC9376898).
Zaroushani V. Occupational safety and health and response to COVID-19 using the fourth industrial revolution technologies. J Health Saf Work. 2020;10(4):329–48.
Binagwaho A, Hirwe D, Mathewos K. Health System Resilience: Withstanding Shocks and Maintaining Progress. Glob Health Sci Pract. 2022;10(Suppl 1):e2200076. https://doi.org/10.9745/GHSP-D-22-00076 .
Freed SL, Thiele D, Gardner M, Myers E. COVID-19 evaluation and testing strategies in a federally qualified health center. Am J Public Health. 2022;112(S3):S284-7.
Levy P, McGlynn E, Hill AB, Zhang L, Korzeniewski SJ, Foster B, Criswell J, O’Brien C, Dawood K, Baird L, Shanley CJ. From pandemic response to portable population health: a formative evaluation of the Detroit mobile health unit program. Plos One. 2021;16(11):e0256908.
Corwin C, Sinnwell E, Culp K. A mobile primary care clinic mitigates an early COVID-19 outbreak among migrant farmworkers in Iowa. J Agromed. 2021;26(3):346–51.
Mills WR, Buccola JM, Sender S, Lichtefeld J, Romano N, Reynolds K, Price M, Phipps J, White L, Howard S. Home-based primary care led-outbreak mitigation in assisted living facilities in the first 100 days of coronavirus disease 2019. J Am Med Direct Assoc. 2020;21(7):951–3.
Sigurdsson EL, Blondal AB, Jonsson JS, Tomasdottir MO, Hrafnkelsson H, Linnet K, Sigurdsson JA. How primary healthcare in Iceland swiftly changed its strategy in response to the COVID-19 pandemic. BMJ Open. 2020;10(12):e043151. https://doi.org/10.1136/bmjopen-2020-043151 . (PMID:33293329;PMCID:PMC7722808).
Mirsky JB, Thorndike AN. Virtual group visits: hope for improving chronic disease management in primary care during and after the COVID-19 pandemic. Am J Health Promot. 2021;35(7):904–7.
Lauriola P, Martín-Olmedo P, Leonardi GS, Bouland C, Verheij R, Dückers ML, Van Tongeren M, Laghi F, Van Den Hazel P, Gokdemir O, Segredo E. On the importance of primary and community healthcare in relation to global health and environmental threats: lessons from the COVID-19 crisis. BMJ Global Health. 2021;6(3):e004111.
Stengel S, Roth C, Breckner A, et al. Resilience of the primary health care system – German primary care practitioners’ perspectives during the early COVID-19 pandemic. BMC Prim Care. 2022;23:203. https://doi.org/10.1186/s12875-022-01786-9 .
Adu PA, Stallwood L, Adebola SO, Abah T, Okpani AI. The direct and indirect impact of COVID-19 pandemic on maternal and child health services in Africa: a scoping review. Global Health Res Policy. 2022;7(1):1–4.
Segal M, Giuffrida P, Possanza L, Bucciferro D. The critical role of health information technology in the safe integration of behavioral health and primary care to improve patient care. J Behav Health Serv Res. 2022;49(2):221–30. https://doi.org/10.1007/s11414-021-09774-0 . (Epub 2021 Oct 19. PMID: 34668115; PMCID: PMC8525847).
Gallardo-Rincón H, Gascon JL, Martínez-Juárez LA, Montoya A, Saucedo-Martínez R, Rosales RM, Tapia-Conyer R. MIDO COVID: A digital public health strategy designed to tackle chronic disease and the COVID-19 pandemic in Mexico. Plos One. 2022;17(11):e0277014.
Shah SS, Safa A, Johal K, et al. A prospective observational real world feasibility study assessing the role of app-based remote patient monitoring in reducing primary care clinician workload during the COVID pandemic. BMC Fam Pract. 2021;22:248. https://doi.org/10.1186/s12875-021-01594-7 .
Lu M, Liao X. Access to care through telehealth among US Medicare beneficiaries in the wake of the COVID-pandemic. Front Public Health. 2022;10:946944.
Reges O, Feldhamer I, Wolff Sagy Y, Lavie G. Factors associated with using telemedicine in the primary care clinics during the COVID-19 pandemic in Israel. Int J Environ Res Public Health. 2022;19(20):13207.
Neves AL, Li E, Gupta PP, Fontana G, Darzi A. Virtual primary care in high-income countries during the COVID-19 pandemic: Policy responses and lessons for the future. Eur J Gen Pract. 2021;27(1):241–7.
Fadul N, Regan N, Kaddoura L, Swindells S. A midwestern academic HIV clinic operation during the COVID-19 pandemic: implementation strategy and preliminary outcomes. J International Assoc Provid AIDS Care (JIAPAC). 2021;2(20):23259582211041424.
Gray C, Ambady L, Chao S PharmD, Smith W MPH, Yoon J. Virtual Management of Chronic Conditions During the COVID-19 Pandemic: Insights From Primary Care Providers and Clinical Pharmacists. Mil Med. 2023;188(7-8):e2615-e2620. https://doi.org/10.1093/milmed/usac277 .
Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Commun Health. 2020;11:2150132720980612.
Calvo-Paniagua J, Díaz-Arribas MJ, Valera-Calero JA, et al. A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: A quasi-experimental study. PLoS One. 2022;17(8):e0271802. https://doi.org/10.1371/journal.pone.0271802 . (Published 2022 Aug 4).
Chen K, Davoodi NM, Strauss DH, Li M, Jiménez FN, Guthrie KM, et al. J Appl Gerontol. 2022;41(11):2282–95.
Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, Lewis R, Iyer G, Macleod J, Horwood J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. 2021;71(704):e166-77.
Maria AR, Serra H, Heleno B. Teleconsultations and their implications for health care: a qualitative study on patients’ and physicians’ perceptions. Int J Med Inform. 2022;1(162):104751.
Liddy C, Singh J, Mitchell R, Guglani S, Keely E. How one eConsult service is addressing emerging COVID-19 questions. J Am Board Fam Med. 2022;35(3):601–4.
Schow DC, Thomson A, Trusty WT, Buchi-Fotre L. Use of a research as intervention approach to explore telebehavioral health services during the COVID-19 pandemic in Southeastern Idaho. J Prim Care Commun Health. 2022;13:21501319211073000.
Bruns BE, Lorenzo-Castro SA, Hale GM. Controlling blood pressure during a pandemic: The impact of telepharmacy for primary care patients. J Pharm Pract. 2022;27:08971900221136629.
Pradhan NA, Samnani AA, Abbas K, Rizvi N. Resilience of primary healthcare system across low-and middle-income countries during COVID-19 pandemic: a scoping review. Health Res Policy Syst. 2023;21(1):98.
Esfahani P, Mosadeghrad AM, Akbarisari A. The success of strategic planning in health care organizations of Iran. Int J Health Care Qual Assur. 2018;31(6):563–74.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobile health tools to support COVID-19 training and surveillance in Ogun State Nigeria. Front Sustain Cities. 2021;5(3):638278.
Ndayishimiye C, Lopes H, Middleton J. A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. 2023;13(2):273–84.
Ghiasipour M, Mosadeghrad AM, Arab M, Jaafaripooyan E. Leadership challenges in health care organizations: The case of Iranian hospitals. Med J Islam Repub Iran. 2017;31(1):560–7.
Download references
Acknowledgments
We would like to thank Dr. Arshad Altaf for his invaluable comments on the earlier drafts of this work.
Funding for this project was provided by the World Health Organization Eastern Mediterranean Region.
Author information
Authors and affiliations.
Health policy and management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Ali Mohammad Mosadeghrad
Health policy, School of Nursing and Midwifery, Saveh University of Medical Sciences, Saveh, Iran
Mahnaz Afshari
Health management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran
Parvaneh Isfahani
Health services management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Farahnaz Ezzati, Mahdi Abbasi, Shahrzad Akhavan Farahani & Leila Eslambolchi
Health Management, School of Business and Management, Royal Holloway University of London, London, UK
Maryam Zahmatkesh
You can also search for this author in PubMed Google Scholar
Contributions
LE, MA, MZ and AMM participated in the design of the study. LE, AMM, MA, MZ, PI, FE, MA and SHA undertook the literature review process. All authors drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Leila Eslambolchi .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Tehran University of Medical Science (Approval ID: IR.TUMS.SPH.REC.1401.0979).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mosadeghrad, A.M., Afshari, M., Isfahani, P. et al. Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review. BMC Health Serv Res 24 , 841 (2024). https://doi.org/10.1186/s12913-024-11278-4
Download citation
Received : 14 January 2024
Accepted : 03 July 2024
Published : 25 July 2024
DOI : https://doi.org/10.1186/s12913-024-11278-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care system
- Strengthening strategies
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Tacit Knowledge Transfer in Safety-Critical Systems: A Systematic Literature Review
27 Pages Posted: 25 Jul 2024 Publication Status: Under Review
Rikard Eklund
Chalmers University of Technology
Anna-Lisa Osvalder
The departure of experienced individuals from an organization can result in a significant decline in productivity, efficiency, and safety due to the loss of specialized knowledge and skills. The intuitive understanding and experience derived from operational safety, procedural adherence, and the management of non-normal situations, accumulated over long-term employment, are often unspoken, experience-based, and challenging to document, thus constituting tacit knowledge. Addressing the transfer of such tacit knowledge necessitates the implementation of various strategies. This systematic literature review, conducted as applicable in accordance with the PRISMA [41] statement, aims to explore and compile existing methodologies for transferring tacit knowledge within safety-critical systems. A total of 22 empirical and non-empirical studies across sectors including nuclear power production, offshore operations, aerospace, control rooms, maritime, and railways were systematically examined. The findings were assessed, classified, and presented using the SECI model [1]. The review identified the importance of knowledge management and the necessity of deploying methods to manage knowledge effectively. It furthermore identified that personal interactions founded on mutual trust within social communities, such as apprenticeships, are commonly employed for knowledge transfer. However, these methodologies have generally been inconsistently documented. Informal interactions also play a significant role in enabling tacit knowledge transfer. In safety-critical system environments, however, informal organizational entities pose challenges, as informal channels may become undetectable and lead to the use of non-standard procedures compared to established standard operating procedures (SOPs). Furthermore, the review highlights inconsistencies in the definition and operationalization of tacit knowledge, which complicate the design of research instruments. In summary, this systematic literature review provides a comprehensive overview of research on tacit knowledge transfer methods in safety-critical systems, highlighting prevalent practices and identifying gaps in documentation and research consistency.
Keywords: Tacit knowledge, knowledge transfer, Safety-critical Systems, Systematic Literature Review, PRISMA, SECI model
Suggested Citation: Suggested Citation
Rikard Eklund (Contact Author)
Chalmers university of technology ( email ), do you have a job opening that you would like to promote on ssrn, paper statistics.
- Open access
- Published: 25 July 2024
Effect of post-storage filters vs. pre-storage filters for leukoreduction of blood components on clinical outcomes: a systematic review and meta-analysis
- Natasha Dejigov Monteiro da Silva ORCID: orcid.org/0000-0002-2718-3885 1 ,
- Youko Nukui 1 ,
- Juliana Takahashi 2 ,
- Diná de Almeida Lopes Monteiro da Cruz 2 &
- Lilia de Souza Nogueira 2
Systematic Reviews volume 13 , Article number: 196 ( 2024 ) Cite this article
Leukoreduction has been used to limit the risk of adverse events. The most commonly used methodology is filtration (pre- or post-storage). However, whether pre-storage filtration is better than post-storage filtration needs to be clearly defined, particularly for countries that still use post-storage filtration. This study aimed to synthesize the best available evidence on the effectiveness of pre-storage filters compared with post-storage filters for transfusion reactions, for the occurrence of infections, for the length of hospital stay, and for the death of patients undergoing leukoreduced transfusion.
We searched the MEDLINE (PubMed), CINAHL (EBSCO), PsycINFO (APA), Scopus (Elsevier), The Cochrane Library (J. Wiley), Web of Science Core Collection (Clarivate Analytics), Embase (Elsevier), and LILACS (VHL) databases and gray literature for eligible studies in August 2020 and updated the search in October 2023. The Joanna Briggs Institute critical assessment tools were applied to analyze the quality appraisal of the studies. GRADE was used to determine the certainty of the evidence.
The meta-analysis showed that pre-storage filtration was a protective factor for the occurrence of febrile non-hemolytic transfusion reaction in red blood cells (RR 0.49, 95% CI 0.41–0.59) and platelet concentrate transfusions (RR 0.16, 95% CI 0.12–0.22). The same did not occur for post-surgical infection after platelet concentrate transfusions (RR 0.82, 95% CI 0.65–1.04). Only one study analyzed the length of hospital stay and showed no significant difference between patients who received leukoreduced transfusions according to the type of filter used. According to the GRADE criteria, the certainty of the evidence for febrile non-hemolytic transfusion reactions was low for red blood cells and very low for platelet concentrate due to the high risk of bias. Infection was a low risk due to imprecision.
Conclusions
The results of this review showed that the certainty of recommending the best type of filter (pre- or post-storage) for the benefit of the outcomes analyzed is still fragile; therefore, more robust evidence is needed.
Systematic review registration
PROSPERO CRD42020192202.
Peer Review reports
Transfusion is a relevant therapy for treating patients, especially those in critical condition, to obtain biological responses such as increased tissue oxygenation or to prevent or cease bleeding [ 1 , 2 , 3 , 4 ]. Alloantigens and metabolically active cells capable of proliferating and producing response modifiers that affect the recipient are introduced during transfusion. In addition, inflammatory mediators, such as cytokines, interleukins [ 1 , 2 , 3 , 4 , 5 , 6 ], and tumor necrosis factor, are released by the degradation of leukocytes as blood components are collected, processed, and stored. At the same time, the recipient will respond to transfusion by producing immunological mediators that further influence the recipient’s clinical response [ 5 ].
Despite advances in transfusion medicine, this therapy can still cause adverse events due to the risks related to the procedure, such as failures during the blood cycle due to incorrect indication of the need for transfusion, inappropriate use of blood components, or aspects inherent to the receiver itself [ 1 , 2 , 3 , 4 ]. Transfusion reactions (TRs) are among the main adverse events related to using blood products. According to the Agence Nationale de Sécurité du Médicament et des Produits de Santé (ANSM), it is estimated that the expected TR rate is three to five reactions per 1000 transfusions performed [ 6 ]. Moreover, red blood cell (RBC) and platelet concentrate (PC) transfusions are responsible for most TRs [ 7 , 8 ]. The main TR associated with the presence of mediators released by leukocyte degradation is the febrile non-hemolytic transfusion reaction (FNHTR). In addition, alloimmunization (ALO), transfusion-related acute lung injury (TRALI), graft versus host disease (GVHD), and communicable diseases, including cytomegalovirus (CMV), have been found in the literature; however, these infections occur less frequently [ 6 , 7 , 8 , 9 ]. Transfusional immunomodulation can also cause adverse events, such as increased bacterial infections in the postoperative period and the recurrence of malignancies (i.e., intestinal neoplasia); the reactivation of latent and asymptomatic infections; and increased morbidity and mortality [ 10 , 11 , 12 ].
Leukoreduction is one of the procedures used to remove leukocytes through filters to avoid TRs and transfusion-related immunomodulation (TRIM). The pre-storage filter is used during donation (in-line) or to separate blood components (bench) within 48 h after collection. A post-storage filter is used at the bedside during transfusion.
Several studies suggest other clinical benefits of reducing leukocyte counts, such as decreasing the length of hospital stay and the use of antibiotics, in addition to improving the efficiency of platelet transfusion [ 10 , 13 , 14 ]. European countries such as Germany, the United Kingdom, Ireland, and Portugal have adopted leukoreduction since 1990 to prevent complications such as TRs and Creutzfeldt‒Jakob Disease Variant transmission [ 15 , 16 ]. Canada has implemented the same method to avoid TRIM [ 17 ]. Leukoreduction is not widely used in Brazil, especially in public health services. Brazilian legislation guides prioritization in recommending leukoreduction for some groups of patients but does not determine the filtration time, whether pre or post-storage [ 18 ].
Although the benefits of leukoreduction are recognized, pre-storage leukoreduction has advantages over post-storage, including preventing the accumulation of cytokines that are synthesized during cell storage, preventing RBC hemolysis, and interruption of filtration by cell debris resulting from the storage of RBCs and ensuring quality control of the leukoreduction of products intended for transfusion [ 6 , 10 , 19 ].
Some studies comparing the use of blood components subjected to pre and post-storage filtration have shown that pre-storage leukoreduction is more advantageous for reducing TRs, infection, and postoperative mortality, especially in patients with cancer, transplants, or hematological diseases [ 19 , 20 , 21 ]. However, other studies have not shown a difference between the filtration time (before and after storage) and the clinical outcome of transfusion patients [ 22 , 23 ]. This controversy justifies the need for this review.
Preliminary searches performed in PROSPERO, the Cochrane Library, and the Joanna Briggs Institute (JBI) Evidence Synthesis did not identify reviews that compared pre and post-storage leukoreduction filters on patient outcomes. Considering the knowledge gap about the ideal filter (pre- or post-storage) for performing leukoreduction, it is essential to find the best available evidence about this filter, which in turn will contribute to clinical decisions that promote safety for patients who need transfusions and will also help elaborate public policies on the subject. Therefore, this systematic review aimed to synthesize the best available evidence on the effectiveness of pre-storage filters compared with post-storage filters on the following clinical outcomes: TRs, the occurrence of infections, length of hospital stay, and hospital death in patients receiving leukoreduced transfusion.
This systematic review had the protocol published a priori [ 24 ] and registered in the PROSPERO database (CRD42020192202). Considering that the post-storage filter (bedside) has been the oldest and most widely used technology for decades, the PICO structure presented in the review protocol [ 24 ] was changed with regard to the intervention and the comparator by consensus among the authors of this review. Thus, the pre-storage filter (bench or inline) was considered for intervention, and the post-storage filter (bedside) was considered for the comparator.
Information sources and search strategy
The sources included were MEDLINE (PubMed), CINAHL (EBSCO), PsycINFO (APA), Scopus (Elsevier), The Cochrane Library (Wiley), the Web of Science Core Collection (Clarivate Analytics), Embase (Elsevier) and LILACS (VHL). The search for unpublished studies (gray literature) included regulatory bodies such as the National Health Surveillance Agency ( Agência Nacional de Vigilância Sanitária-Anvisa ) of Brazil, the Pan American Health Organization (PAHO) and the World Health Organization (WHO); representative entities, such as the Brazilian Association of Hematology, Hemotherapy and Cell Therapy (Associação Brasileira de Hematologia, Hemoterapia e Terapia Celular-ABHH); and the American Association of Blood Banks (AABB), as well as records from the Digital Library of Theses and Dissertations and All Trials and Restoring Invisible and Abandoned Trials (RIAT). The full search strategy is provided in Additional file 1: Appendix 1 and the structured searches were conducted in August 2020 and updated in October 2023.
These references were grouped and imported into EndNote, a web version (Clarivate Analytics, PA, USA), and duplicate articles were removed. The Rayyan platform ( https://rayyan.qcri.org/ ) was used for study screening and selection. The titles and abstracts of the studies were examined, and those relevant to the review question were selected for full-text retrieval. The evaluation was based on the inclusion criteria and was independently conducted by pairs of reviewers (NDMS and LSN, YN and DALMC; JT and NDMS; LSN and YN). Any divergences between reviewers in the study selection process were resolved by consensus or consultation with a third reviewer.
Eligibility criteria
Participants.
Patients of any age, sex, or race who received a leukoreduced blood transfusion.
Intervention(s)
Pre-storage filter of any brand and type to remove leukocytes.
Comparator(s)
Post-storage filter of any brand and type to remove leukocytes.
TRs, infections, length of hospital stay, and hospital death. The length of hospital stay was regarded as the number of days the patient stayed there. TRs were considered by the type of reaction and by the diagnosis of the confirmed reaction (ALO, FNHTR, or TRALI), according to internationally adopted definitions. Infections were considered those confirmed by laboratory examination and not associated with contamination of the blood component. In-hospital death was identified as the patient’s death during hospitalization from any cause after receiving a leukoreduced transfusion.
Types of studies
Experimental or quasi-experimental studies, including randomized or nonrandomized clinical trials; observational cohort, prospective or retrospective, case–control and cross-sectional studies; and case reports or case series. Studies published in Portuguese, English, or Spanish were included. No time limit was considered for the review.
Quality assessment
Pairs of reviewers (NDMS and LSN; YN and DALMC; JT and NDMS; LSN and YN) assessed eligible studies for methodological quality using standardized JBI critical appraisal tools [ 25 ] for quasi-experimental studies and randomized controlled trials after they had been imported into the JBI System for the Unified Management, Assessment, and Review of Information (JBI SUMARI) software [ 26 ]. The purpose of the critical appraisal tool is to assess the methodological quality of a study and to determine the extent to which a study has addressed the possibility of bias in its design, conduct, and analysis [ 25 ]. Answers rated as “yes”, “no”, “unclear” or “not applicable” were assigned for each question (13 for randomized controlled trial studies and 9 for quasi-experimental studies). Any disagreements between reviewers were resolved by consensus among all the reviewers. No studies were excluded based on methodological quality.
Data extraction and statistical analysis
The JBI template form was used for data extraction and is presented in Additional file 2: Appendix 2. The extracted data included the study location, participant details, storage filters used, and relevant results for the review question. The studies included reported RBC units or PC pools. We converted units and pools into the number of transfusions. For RBC, we considered one unit equal to one transfusion. For PC, we considered one pool (4 to 5 units of PC) equal to one transfusion. The frequency of outcomes was absolute in some studies and percentages in others. It was possible to calculate the quantity of the outcomes in absolute numbers in all cases. Two independent reviewers (DALMC and LSN) performed these calculations, and even if they agreed, they were redone and confirmed by all the reviewers. Any disagreements were resolved by consensus among all the reviewers. It was necessary to contact the main author [ 22 , 23 ] to request additional information in two cases.
The study results were pooled in a meta-analysis using the JBI SUMARI [ 26 ] to estimate a summarized mean effect according to the selected outcomes. Effect sizes are expressed as relative risk (RR) for dichotomous data, with a 95% confidence interval (CI). The random effect model was used due to clinical and methodological variability between studies. Statistical heterogeneity was assessed by visual inspection of the forest plot distribution, Pearson’s chi-squared test pattern, and I 2 statistics. We chose to present the results of the meta-analysis, regardless of the degree of heterogeneity, to facilitate follow-up of the interpretations.
A funnel plot was not performed to assess publication bias due to the low number of studies included in each meta-analysis, but a sensitivity analysis was conducted.
Assessing certainty in the findings
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) [ 27 ] approach to assessing evidence was followed, and a summary of the findings was presented with the following information: absolute effect for the pre and post-storage groups, relative effect estimates considering the RR and 95% CI (dichotomous variables: occurrence of FNHTR and infection) or mean (continuous variable: length of hospital stay). The evidence quality was classified according to the design, execution, and publication limitations (risks of bias), directivity, heterogeneity, and precision of the included studies, as established by GRADE [ 27 ].
Results of the search and selection process
The initial literature search identified 1286 records, totaling 821 records after removing duplicates. A total of 796 records were excluded from screening the titles and abstracts because they were clearly ineligible for review. The remaining 26 reports were read in full to confirm their relevance for the review, and 17 were excluded for failing to meet the inclusion criteria [ 22 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ]; thus, nine studies [ 19 , 20 , 21 , 23 , 44 , 45 , 46 , 47 , 48 ] were included in this review.
The selection results are presented as a flowchart (Fig. 1 ), as recommended by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [ 49 ].
Additional file 3:Appendix 3 provides the list of studies excluded after reading the full texts and the reasons for their exclusion.

PRISMA study selection and inclusion criteria.
Characteristics of the included studies
One of the included studies was a randomized clinical trial [ 23 ], and the others were quasi-experimental [ 19 , 20 , 21 , 44 , 45 , 46 , 47 , 48 ]. The characteristics and primary results of the studies are reported in Additional file 2: Appendix 2.
Of the studies included in the review, five (55.6%) [ 20 , 21 , 23 , 47 , 48 ] were conducted in Europe, three (33.3%) in North America [ 19 , 44 , 46 ] and one (11.1%) in Asia [ 45 ]. Most of the publications (n = 7; 77.8%) occurred between 2000 and 2018 [ 19 , 20 , 21 , 44 , 45 , 46 , 47 ], mainly between 2000 and 2005 (n = 4; 44.4%) [ 20 , 44 , 46 , 47 ], with the most recent and oldest studies dating from 2018 [ 45 ] and 1998 [ 23 ], respectively. The most common outcome was TR, mainly FNHTR (n = 7; 77.8%) [ 19 , 20 , 44 , 45 , 46 , 47 , 48 ]. The study participants were diverse: they were immunocompromised [ 44 , 45 ] or had oncological [ 19 , 20 , 21 , 46 , 48 ], hematological [ 19 , 48 ] or cardiac diseases [ 19 , 23 ]; had undergone different transplants [ 45 ] or had an indication for colorectal resection [ 21 ]; were candidates for long-term transfusion therapy [ 47 ]; or had already presented FNHTR in previous transfusions [ 19 , 45 , 46 ]. The population included in the two studies was any patient who underwent allogeneic transfusion [ 44 , 47 ].
Importantly, four studies [ 20 , 44 , 46 , 47 ] analyzed data from patients who were transfused before and after universal leukoreduction was adopted. All transfused patients who received filtered blood components before universal leukoreduction were selectively indicated, and the predominant type of filtration was post-storage. In the universal leukoreduction phase, all patients received transfusions pre-storage filtered [ 20 , 44 , 46 , 47 ]. Therefore, it can be assumed that patients who received post-storage filtered transfusions had a greater risk of reactions than did those who received pre-storage filtered blood components, leading to the risk of equivocally increasing the benefit of pre-storage filtration according to the results of these studies [ 20 , 44 , 46 , 47 ], which contributed 78% (269,537 of 345,750) of the transfusions analyzed.
The patient sample sizes described in 6 studies ranged from 32 to 17,475 transfused patients [ 20 , 21 , 23 , 45 , 46 , 48 ], in which the blood components used were RBC and PC. The total number of transfusions (RBC and PC) in the included studies was 345,750 (180,655 pre; 165,095 post-storage filtered), ranging from 161 to 174,856 transfusions [ 19 , 20 , 23 , 44 , 45 , 46 , 47 , 48 ]. Some studies did not present demographic data (age and sex) from the samples [ 19 , 44 , 46 , 47 ]; others only presented the age group [ 20 , 48 ]. The follow-up time of the patients was reported in only 5 studies and ranged from 1 h to 60 days after transfusion [ 20 , 23 , 45 , 47 , 48 ]. Notably, FNHTRs were identified in RBC [ 20 , 44 , 45 , 46 , 47 ] transfusions in 5 studies and in patients treated with PC in four studies [ 19 , 45 , 46 , 48 ]. Most of the studies evaluated other TRs in addition to FNHTRs, such as allergic reactions [ 19 , 20 , 44 , 45 , 46 , 47 ]. One patient can receive more than one transfusion, but only two studies [ 20 , 23 ] have reported the mean number of transfusions per patient. Only two studies evaluated infection [ 21 , 23 ], and one analyzed the length of hospital stay [ 23 ]. Although one study evaluated mortality [ 23 ] within 60 days after transfusion, it was unclear whether death occurred during hospitalization. The main author did not return contact information upon request.
Methodological quality
At least 60% of the studies had positive responses to the applicable questions of the critical evaluation tools. The results of specific scores for each study included in this review using the evaluation criteria associated with the type of study design are provided in Tables 1 and 2 .
The greater the number of “yes” responses on the evaluation forms used in this review, the lower the risk of bias. Table 1 shows that the total number of positive responses was 84.6%, with questions 4 and 6 indicating a possible risk of bias considering that there was no information about the blinding of participants and outcome raters. Table 2 shows that the minimum percentage of positive responses in each study was 62.5%, the maximum was 87.5%, and questions 1, 4, 7, 8, and 9 had positive responses in all the included studies. The answers to questions 2 and 3 show the most frequent risk of bias among the studies. The characteristics of the samples of patients in both groups were not presented in six of the eight studies included [ 19 , 20 , 44 , 46 , 47 , 48 ], which limited the evaluation of the risk of selection bias relevant to question 2. It is important to note that the risk of selection bias is important in studies that analyzed data from before and after the adoption of pre-storage leukoreduction in all transfusions since the sample of patients who received transfusions with post-storage leukoreduction was more restricted and had a higher risk of TR, as already mentioned [ 20 , 44 , 46 , 47 ]. The answers to question 6 were unclear in four studies [ 19 , 21 , 44 , 46 ], as there was no report on the follow-up time for evaluating the outcomes. Question 5 was considered not applicable to the quasi-experimental studies of interest for this review because TRs are only transfusional if they occur after the intervention (transfusion), and there is no reason to evaluate them before transfusions.
Review findings and certainty of the evidence
The studies included in this review provided evidence of the effectiveness of the type of filtration of RBCs or PCs on FNHTR [ 19 , 20 , 44 , 45 , 46 , 47 , 48 ] infection [ 21 , 23 ] and length of hospital stay [ 23 ]. The evidence could be synthesized in meta-analysis for FNHTRs (RBCs and PCs) and infection (PCs). The length of hospital stay was only reported in one study for patients who underwent PC transfusions [ 23 ].
A meta-analysis synthesizing evidence on the occurrence of FNHTRs showed that pre-storage filtration was a protective factor against RBC (0.49, 95% CI 0.41 to 0.59) and PC transfusions (RR 0.16, 95% CI, 0.12 to 0.22) (Figs. 2 and 3 ). However, the heterogeneity between the studies included in the meta-analysis was noteworthy. The I 2 was 66% in the meta-analysis for RBC and 93% for PC (Figs. 2 and 3 ). The heterogeneity was reduced (I 2 = 0) after repeating the analysis and excluding a very large study [ 46 ] to establish how much it dominated the results, and the effect continued to be favorable for the prestorage filter (Fig. 4 ). Moreover, the effect size increased and the 95% CI increased (from RR = 0.16 [95%CI 0.12–0.22]) to RR = 0.54 [95%CI 0.36–0.82].

Forest plot for the occurrence of FNHTRs after RBC transfusions according to the type of filter (pre or post-storage). CI: Confidence interval; M-H: Mantel–Haenszel

Forest plot for the occurrence of FNHTRs after PC transfusions according to the type of filter (pre or post-storage). CI: Confidence interval; M-H: Mantel–Haenszel

Forest plot for the occurrence of FNHTRs after PC transfusions according to the type of filter (pre or post-storage), excluding one large study. CI: Confidence interval; M-H: Mantel–Haenszel
The findings on the role of filtration type in preventing infection (Fig. 5 ) after PC transfusion are inconclusive. Although the RR (0.82) suggested a protective effect of the pre-storage filtration, this estimate was not statistically significant (95% CI 0.65 to 1.04), and the I 2 statistic was 75%. The only study identified for which the length of hospital stay was an outcome showed no statistically significant difference between patients who received leukoreduced PC transfusion according to the filter type used. The certainty in the final set of evidence was low due to the risk of bias, sample size, heterogeneity, and imprecision reflected in the wide CI. A summary of the findings is reported in Additional file 4: Appendix 4.

Forest plot for the occurrence of infection after PC transfusions according to the type of filter (pre or post-storage). CI: Confidence interval; M-H: Mantel–Haenszel
The results showed that the certainty of recommending one type of filter or another is still fragile. The limited number of robust studies evaluating relevant outcomes for this review contributed to this fragility.
Most studies [ 19 , 20 , 21 , 44 , 45 , 46 , 47 , 48 ] included in the review were quasi-experimental studies designed as time series to evaluate the impact of adopting universal leukoreduction. In these studies, the outcomes of patients who received leukoreduced blood components before universal leukoreduction were compared to those of all transfused patients after universal leukoreduction. The data sources included existing data from blood centers and patients' health records. Despite the advantages of using existing data [ 50 ], controlling for extraneous factors in this kind of data source is not possible, as is the case for randomized controlled trials, increasing the risk of bias in such studies [ 51 ]. In studies using existing data sources, changes in clinical practices, professionals involved, or filter models with varying filtration capacities over time cannot be strictly controlled.
Although ALO and TRALI are also related to the presence of inflammatory mediators and have been relevant outcomes in studies that compared leukoreduced and nonleukoreduced transfusions [ 6 , 7 , 8 ], only FNHTRs were found in this review. An allergic reaction was found in 75% of the studies analyzed [ 19 , 20 , 45 , 46 , 47 ], but it was not considered an outcome in this review because leukoreduction is not an indication for preventing it since its pathophysiology is different from that of FNHTRs and is related to the presence of anti-IgE antibodies in the receptor [ 4 ]. Two studies [ 21 , 23 ] analyzed the presence of postsurgical infection for immunomodulation, but one study showed that surgery had a high potential for contamination (colorectal resection) [ 21 ].
An important aspect to be discussed is the lack of identification of recent primary studies and the greater frequency of studies carried out in developed countries. Most of the included studies were published between 1998 and 2005 [ 19 , 20 , 23 , 44 , 46 , 47 , 48 ] and originated in Europe and North America. Universal leukoreduction, which presupposes the exclusive use of the pre-storage filter, is adopted in some countries in these regions [ 15 , 16 , 17 ]. It can be admitted that, in this case, the use of the pre-storage filter is more appropriate from a practical point of view than the post-storage filter is, which would explain the lack of more recent studies comparing pre and post-storage filtration and, therefore, the possible lack of relevance of this review question for these contexts. However, in contexts with limitations of any nature for adopting universal leukoreduction and in which selective leukoreduction is considered, answering the central question of this review is important to support the recommendations on the type of filter to use. Although it may seem implicit in this comment that universal leukoreduction is based on robust evidence, this is not the case. A systematic review evaluating the use of leukoreduction did not find robust evidence to support or reject the routine use of leukoreduction in all patients transfused with RBCs to prevent TRALI, death, infection, non-infection complications, or other adverse events because the quality of evidence was also very low [ 52 ]. As with this review, the different scenarios and the high heterogeneity between studies contributed to the high risk of bias, inconsistency, and imprecision.
The characteristics of the population/sample, blood components, filters, and follow-up time according to the outcomes impacted the assessment of methodological quality and synthesis of the results. These characteristics deserve to be discussed so that they can be considered in primary studies. Some studies presented information about people’s illnesses but lacked demographic data, such as sex or age [ 19 , 20 , 44 , 46 , 47 ], making it impossible to compare the studied samples. In addition, there was little information, such as a previous history of TR or concomitant use of other nonleukoreduced blood components, constituting factors that may mask the results found since alloimmunized patients have an increased risk of developing TR and because the simultaneous use of a nonleukoreduced blood component leads to a greater chance of developing TR.
Another impacting factor was the length of follow-up of the patients, which was reported in only 5 studies [ 20 , 23 , 45 , 47 , 48 ]; this factor is relevant for determining whether the time interval was sufficient for the occurrence of the assessed outcome. Notably, only one study raised the issue of premedication, in this case, for anesthetized patients, and discarded premedication in patients with a history of previous reactions [ 20 ]. TR identification is more complicated in anesthetized patients, mainly due to the possibility of developing an adverse reaction to the drugs used [ 53 ] and even hypothermia associated with exposure during surgical procedures [ 54 , 55 ]. Pre-transfusion medication to minimize some TR symptoms is still used but is controversial and may mask the side effects of transfusion [ 56 , 57 ].
A lack of information on storage time regarding blood components and the average number of transfused bags per patient was identified. It is known that bags with longer storage times have a greater number of leukocyte degradation components, increasing the chance of developing adverse events. Additionally, the risk of TR and other adverse events is directly proportional to the number of transfusions received [ 58 ]. We know that type of filter equipment may differ between studies and impact the results. Few studies have presented relevant information about the filters used in leukoreduction processes and their filtration capacity. In some cases, it was possible to retrieve data from catalogs available on the internet, but in others, the information was incomplete. These methodological limitations impacted the results of this review and need to be overcome in further primary studies on the effectiveness of pre and post-storage leukoreduction filters. These characteristics of the reports are probably associated with the times of their publication, as consensuses for reports of primary studies did not exist or were not so widespread, such as the CONSORT [ 59 ].
Given the points highlighted above and the reduced number of studies found, the certainty of recommending using the pre-storage filter is weak. In addition, this review identified the need for primary studies that comparatively evaluate pre and post-storage leukoreduction filters in the overall population, which limits the recommendation of the best type of filter to prevent the analyzed outcomes. Even so, this review provides essential information for clinical, managerial, and political decisions about the types of filters to be used when leukoreduction of blood components is desired, especially in countries with medium or low income or in situations where universal leukoreduction is not yet an option. Notably, the choice to adopt pre-storage leukoreduction should also consider other factors not discussed in this review, such as logistics, human resources involved, and the restructuring process. According to van de Watering et al. [ 60 ], “universal leukoreduction is a step toward maximum safety, but it goes beyond ideal safety”.
The results of this systematic review revealed that although the meta-analysis indicated that using a pre-storage filter is a protective factor against FNHTR after RBC and PC transfusions, there was great statistical heterogeneity among the studies. The results for infection were inconclusive. We identified only one study that analyzed the length of hospital stay and none that investigated hospital death. Therefore, the results showed that there needs to be more robust evidence to recommend the best type of filter (pre or post-storage) to prevent the analyzed outcomes.
Availability of data and materials
The data we used for this study are available within the review and its additional files.
Abbreviations
Alloimmunization
Agence Nationale de Sécurité du Médicament et des Produits de Santé
Confidence interval
Cytomegalovirus
Febrile nonhemolytic transfusion reaction
Grading of Recommendations Assessment, Development and Evaluation
Graft versus host disease
Mantel–Haenszel
Platelet concentrate
Preferred Reporting Items for Systematic Reviews and Meta-analyses
Red blood cells
Relative risk
Transfusion reaction
Transfusion-related acute lung injury
Transfusion-related immunomodulation
Tobian AAR, Heddle NM, Wiegmann TL, Carson JL. Red blood cell transfusion: 2016 clinical practice guidelines from AABB. Transfusion. 2016;56(10):2627–30.
Article PubMed Google Scholar
Brasil. Ministério da Saúde. Portaria n° 158, de 4 de fevereiro de 2016. [Redefining the technical regulation of blood therapy procedures]. Diário Oficial da União, Brasília, DF, 05 fev. 2016. [citado em: 2020 Fev 20]. Disponível em: https://bvsms.saude.gov.br/bvs/saudelegis/gm/2016/prt0158_04_02_2016.html
Carson JL, Gyyatt G, Heddle NM, Grossman BJ, Cohn CS, Fung MK, et al. Clinical practice guidelines from the AABB: red blood cell transfusion thresholds and storage. JAMA. 2016;16(19):2025–35.
Article Google Scholar
Fung MK, editor. Technical manual. 19th ed. American Association of Blood Banks: Bethesda, MD; 2017.
Google Scholar
Kunkel SL. An introduction to cytokine biology. In: Davenport RD, Sinyder EL, editors. Cytokines in transfusion medicine: a primer Chapter 1. Bethesda: MD: AAB Press; 1997. p. 1–17.
Agence Nationale de Sécurité du Médicament et des Produits de Santé. [2013 Haemovigilance activity report]. Saint-Denis; 2014. [cité 2020 Jun. 17]. Disponible en: http://hemovigilance-cncrh.fr/www2/votre_region/rhone-alpes/rapport_d_activite_ra_2013.pdf
Politis C, Wiersum JC, Richardson C, Robillard P, Jorgensen J, Renaudier P, et al. The international haemovigilance network database for the surveillance of adverse reactions and events in donors and recipients of blood components: technical issues and results. Vox Sang. 2016;111(4):409–17.
Article CAS PubMed Google Scholar
Harvey AR, Basavaraju SV, Chung KW, Kuehnert MJ. Transfusion-related adverse reactions reported to the National Healthcare Safety Network Hemovigilance Module, United States, 2010 to 2012. Transfusion. 2015;55(4):709–18.
Hall S, Danby R, Osman H, Peniket A, Rocha V, Craddock C, et al. Transfusion in CMV seronegative T-depleted allogeneic stem cell transplant recipients with CMV-unselected blood components results in zero CMV transmissions in the era of universal leukocyte reduction: a UK dual center experience. Transfus Med. 2015;25(6):418–23.
Lannan K, Sahler J, Spinelli SL, Phipps RP, Blumberg N. Transfusion immunomodulation—the case for leukoreduced and (perhaps) washed transfusions. Blood Cells Mol Dis. 2013;50(1):61–8.
Gilliss BM, Looney MR, Gropper MA. Reducing noninfectious risks of blood transfusion. Anesthesiology. 2011;115(3):635–49.
Alberti LR, Vasconcellos LS, Petroianus A. Influence of blood transfusion on development of infection in patients with malignant neoplasms of the digestive system. Arq Gastroenterol. 2006;43(3):168–72.
Holbro A, Andreas, Infantia L, Sigleb J, Busera A. Platelet transfusion: basic aspects. Swiss Med Wkly. 2013;49:1–10.
Hébert PC, Fergusson D, Blajchman MA, Wells GA, Kmetic A, Coyle D, et al. Clinical outcomes following institution of the Canadian universal leukoreduction program for red blood cell transfusions. JAMA. 2003;289(15):1941–9.
Enright H, Davis K, Gernsheimer T, McCullough JJ, Woodson R, Slichter SJ. Factors influencing moderate to severe reactions to PLT transfusions: experience of the TRAP multicenter clinical trial. Transfusion. 2003;43(11):1545–52.
Heim D, Passweg J, Gregor M, Buser A, Theocharides A, Arber C, et al. Patient and product factors affecting platelet transfusion results. Transfusion. 2008;48(4):681–7.
Vamvakas EC. The abandoned controversy surrounding universal white blood cell reduction. Blood Transfus. 2014;12(2):143–5.
PubMed PubMed Central Google Scholar
Brasil. Agência Nacional de Vigilância Sanitária. Resolução (RDC) n⁰ 34, de 11 de junho de 2014. Dispõe sobre as boas práticas no ciclo do sangue. Diário Oficial da União, Brasília, DF, 16 jun. 2014. Available from: http://portal.anvisa.gov.br/documents/10181/2867975/%281%29RDC_34_2014_COMP.pdf/ddd1d629-50a5-4c5b-a3e0-db9ab782f44a
Wang RR, Triulzi DJ, Qu L. Effects of prestorage vs poststorage leukoreduction on the rate of febrile nonhemolytic transfusion reactions to platelets. Am J Clin Path. 2012;138(2):255–9.
Da Ponte A, Bidoli E, Talamini R, Steffan A, Abbruzzese L, Toffola RT, et al. Pre-storage leucocyte depletion and transfusion reaction rates in cancer patients. Transfus Med. 2005;15(1):37–43.
Garancini M, Degrate L, Carpinelli MR, Maternini M, Uggeri F, Giordano L, et al. Impact of pre-storage and bedside filtered leukocyte-depleted blood transfusions on infective morbidity after colorectal resection: a single-center analysis of 437 patients. Surg Infect. 2013;14(4):374–80.
Politis C, Stamoulis K, Grouzi E, Baka M, Apostolidou I, Baliaga S, et al. Adverse reaction associated with the transfusion of blood components processed with different methods: The impact of automated pre-storage leukocyte depletion. Transfus Med Rev. 2022;32(1):10–1.
van de Watering LMG, Hermans J, Houbiers JG, van den Broek PJ, Bouter H, Boer F, et al. Beneficial effects of leukocyte depletion of transfused blood on postoperative complications in patients undergoing cardiac surgery: a randomized clinical trial. Circulation. 1998;97:562–8.
Silva NDM, Nukui Y, Takahashi J, Cruz DALM, Nogueira LS. Effect of post-storage filters vs. pre-storage filters for leukoreduction of blood components on clinical outcomes: a systematic review protocol. JBI Evid Synth. 2021;19(9):2382–8. https://doi.org/10.11124/JBIES-20-00353 .
Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: Systematic reviews of effectiveness. In: Aromataris E, Munn Z (Editors). JBI Manual for Evidence Synthesis. JBI, 2020 [cited 2020 Jul 14] Available from https://synthesismanual.jbi.global . https://doi.org/10.46658/JBIMES-20-04
Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). Int J Evid Based Healthc. 2019;17(1):36–43.
Grade Working Group. The Grading of Recommendations Assessment, Development and Evaluation. 2004–2020 [cited 2020 Jun 17]. Available from: http://www.gradeworkinggroup.org/ .
Mishima Y, Tsuno NH, Matsuhashi M, Yoshizato T, Sato T, Ikeda T, et al. Effects of universal vs bedside leukoreductions on the alloimmunization to platelets and the platelet transfusion refractoriness. Transfus Apher Sci. 2015;52(1):112–21.
Vamvakas EC, Blajchman MA. Prestorage versus poststorage white cell reduction for the prevention of the deleterious immunomodulatory effects of allogeneic blood transfusion. Transfus Med Rev. 2000;14(1):23–33.
Abbasi M, Abbasi T, Ghodarzi MT, Mohammadi A. Comparison of the side effects of blood transfusion between pre-storage filtration and post-storage filtration methods in thalassemia patients. Sci Jf Kurdistan Univ Med Sci. 2013;18(1):85–93.
Klüter H, Bubel S, Kirchner H, Wilhelm D. Febrile and allergic transfusion reactions after the transfusion of white cell-poor platelet preparations. Transfusion. 1999;39(11):1179–84.
Kwon JH, Han S, Jang JS, Lee KW, Ahn JH, Kim K, et al. Decrease in the risk of post-transplant hepatocellular carcinoma recurrence after the conversion to prestorage leukoreduction for transfused red blood cells. Transplantation. 2021;105(3):577–85.
Müller-Steinhardt M, Schlenke P, Wagner T, Klüter H. Transfusion of platelet concentrates from pooled buffy-coats: comparison of bedside vs. prestorage leukofiltration. Transf Med. 2000;10(1):59–65.
Ohto H, Nomizu T, Kuroda F, Hoshi T, Rokkaku Y. HLA alloimmunization of surgical patients by transfusion with bedside leukoreduced blood components. Fukushima J Med Sci. 2003;49(1):45–54.
Say B, Sari FN, Oguz SS, Degirmencioglu H, Arayici S, KadiogluSimsek G, et al. Interleukin-6 and C-reactive protein load in pre-storage and post-storage white blood cell-filtered red blood cell transfusions in premature infants. Transf Med. 2015;25(3):170–3.
Article CAS Google Scholar
Sprogøe-Jakobsen U, Saetre AM, Georgsen J. Preparation of white cell-reduced red cells by filtration: comparison of a bedside filter and two blood bank filter systems. Transfusion. 1995;35(5):421–6.
Bilgin YM, Van De Watering LMG, Eijsman L, Versteegh MIM, Van Oers MHJ, Brand A. Is increased mortality associated with post-operative infections after leukocytes containing red blood cell transfusions in cardiac surgery? An extended analysis Transf Med. 2007;17(4):304–11.
CAS Google Scholar
Glenister KM, Sparrow RL. Level of platelet-derived cytokines in leukoreduced red blood cells is influenced by the processing method and type of leukoreduction filter. Transfusion. 2010;50(1):185–9.
Llewelyn CA, Taylor RS, Todd AA, Stevens W, Murphy MF, Williamson LM. The effect of universal leukoreduction on postoperative infections and length of hospital stay in elective orthopedic and cardiac surgery. Transfusion. 2004;44(4):489–500.
Mortensen FV, Jensen LS, Sørensen HT, Pedersen L. Cause-specific mortality associated with leukoreduced, buffy coat–depleted, or no blood transfusion after elective surgery for colorectal cancer: a posttrial 15-year follow-up study. Transfusion. 2011;51(2):259–63.
Seftel MD, Growe GH, Petraszko T, Benny WB, Le A, Lee C-Y, et al. Universal prestorage leukoreduction in Canada decreases platelet alloimmunization and refractoriness. Blood. 2004;103(1):333–9.
Skånberg J, Lundholm K, Haglind E. Effects of blood transfusion with leucocyte depletion on length of hospital stay, respiratory assistance and survival after curative surgery for colorectal cancer. Acta Oncol. 2007;46(8):1123–30.
Federowicz I, Barrett BB, Andersen JW, Urashima M, Popovsky MA, Anderson KC. Characterization of reactions after transfusion of cellular blood components that are white cell reduced before storage. Transfusion. 1996;36(1):21–8.
Uhlmann EJ, Isgriggs E, Wallhermfechtel M, Goodnough LT. Prestorage universal WBC reduction of RBC units does not affect the incidence of transfusion reactions. Transfusion. 2001;41(8):997–1000.
Chang CC, Lee TC, Su MJ, Lin HC, Cheng FY, Chen YT, Yen TH, Chu FY. Transfusion-associated adverse reactions (TARRs) and cytokine accumulations in the stored blood components: the impact of prestorage versus poststorage leukoreduction. Oncotarget. 2018;9(4):4385–94.
Paglino JC, Pomper GJ, Fisch GS, Champion MH, Snyder EL. Reduction of febrile but not allergic reactions to RBCs and platelets after conversion to universal prestorage leukoreduction. Transfusion. 2004;44(1):16–24.
Pruss A, Kalus U, Radtke H, Koscielny J, Baumann-Baretti B, Balzer D, et al. Universal leukodepletion of blood components results in a significant reduction of febrile non-hemolytic but not allergic transfusion reactions. Transfu Apher Sci. 2004;30(1):41–6.
Chalandon Y, Mermillod B, Beris Ph, Doucet A, Chapuis B, Roux-Lombard P, Dayer JM. Benefit of prestorage leukocyte depletion of single-donor platelet concentrates. Vox Sang. 1999;76(1):27–37.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71):1–9.
Wickham RJ. Secondary Analysis Research. J Adv Pract Oncol. 2019;10(4):395–400. https://doi.org/10.6004/jadpro.2019.10.4.7 . Epub 2019 Mar 1. PMID: 33343987; PMCID: PMC7520737.
Fergusson D, Hebert P, Shapiro S. The before/after study design in transfusion medicine: methodologic considerations. Transfus Med Rev. 2002;16(4):296–303. https://doi.org/10.1053/tmrv.2002.35211 .
Simancas-Racines D, Osorio D, Martí-Carvajal AJ, Arevalo-Rodriguez I. Leukoreduction for the prevention of adverse reactions from allogeneic blood transfusion. Cochrane Database Syst Rev. 2015;12:CD009745.
Faria E. Anafilaxia a agentes anestésicos. Rev Port Imunoalergologia. 2018;26(4):239–54.
Moola S, Lockwood C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. Int J Evid Based Health. 2011;94:337–45.
Sappenfield JW, Hong CM, Galvagno SM. Perioperative temperature measurement and management: moving beyond the Surgical Care Improvement Project. J Anesthesiol Clin Sci. 2013 [cited 2022 Out 17] Available from: http://www.hoajonline.com/journals/pdf/20149-9752-2-8.pdf .
Duran J. Effects of leukoreduction and premedication with acetaminophen. J Pediatr Oncol Nurs. 2014;31:223–9.
Marti-Carvajal AJ, Sola I, Gonzalez LE, Leon de Gonzalez G, Rodriguez-Malagon N. Pharmacological interventions for the prevention of allergic and febrile non-haemolytic transfusion reactions. Cochrane Database Syst Rev. 2010;6:CD007539.
Johnson DJ, Scott AV, Barodka VM, Park S, Wasey JO, Ness PM, et al. Morbidity and mortality after high-dose transfusion. Anesthesiology. 2016;124(2):387–95.
Merkow RP, Kaji AH, Itani KMF. The CONSORT Framework. JAMA Surg. 2021;156(9):877–8.
Article PubMed PubMed Central Google Scholar
van der Watering LMG. What has universal leucodepletion given us: evidence from clinical trials? Vox Sang. 2004;87(Suppl 2):139–44.
Download references
Acknowledgements
We appreciate the support provided by the Brazilian Centre for Evidence-based Healthcare. A JBI Centre of Excellence.
The authors received no specific funding for this work. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior — Brasil ( CAPES )-Finance Code 001.
Author information
Authors and affiliations.
HCFMUSP: Universidade de São Paulo Hospital das Clínicas, Av. Dr. Ovídio Pires de Campos 225, Cerqueira César, São Paulo (SP), Brazil
Natasha Dejigov Monteiro da Silva & Youko Nukui
Universidade de São Paulo Escola de Enfermagem, São Paulo, Brazil
Juliana Takahashi, Diná de Almeida Lopes Monteiro da Cruz & Lilia de Souza Nogueira
You can also search for this author in PubMed Google Scholar
Contributions
All the authors: study conception and protocol, literature search, title/abstract and full-text screening, data extraction, quality assessment, statistical analyses, data interpretation, and manuscript writing. DALMC, LSN, and YN: supervision. All the authors read and approved the final manuscript.
Corresponding author
Correspondence to Natasha Dejigov Monteiro da Silva .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1. search strategy., additional file 2: appendix 2. characteristics of included studies., additional file 3: appendix 3. studies ineligible following full-text review., additional file 4: appendix 4. summary of findings., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Dejigov Monteiro da Silva, N., Nukui, Y., Takahashi, J. et al. Effect of post-storage filters vs. pre-storage filters for leukoreduction of blood components on clinical outcomes: a systematic review and meta-analysis. Syst Rev 13 , 196 (2024). https://doi.org/10.1186/s13643-024-02615-z
Download citation
Received : 30 December 2023
Accepted : 12 July 2024
Published : 25 July 2024
DOI : https://doi.org/10.1186/s13643-024-02615-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Effectiveness
- Post-storage filter
- Pre-storage filter
- Leukoreduction
- Meta-analysis
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- DOI: 10.1097/NNA.0000000000001454
- Corpus ID: 271291044
Supporting Time-Critical Decision Making: The Creation of a Nurse-Led Rapid Literature Review Service.
- Lisa Morse , L. Apen , +1 author C. Crawford
- Published in Journal of Nursing… 1 July 2024
25 References
Chatgpt: friend or foe, paper 1: demand-driven rapid reviews for health policy and systems decision-making: lessons from lebanon, ethiopia, and south africa on researchers and policymakers’ experiences, paper 4: a review of reporting and disseminating approaches for rapid reviews in health policy and systems research, rapid reviews for health policy and systems decision-making: more important than ever before, using artificial intelligence methods for systematic review in health sciences: a systematic review, building the science to guide nursing administration and leadership decision making, systematic versus rapid versus scoping reviews., nursing leadership and covid-19:, rapid reviews: the pros and cons of an accelerated review process., evidence-based nursing management: basing organizational practices on the best available evidence, related papers.
Showing 1 through 3 of 0 Related Papers

IMAGES
VIDEO
COMMENTS
Step 1 - Search for relevant literature. Step 2 - Evaluate and select sources. Step 3 - Identify themes, debates, and gaps. Step 4 - Outline your literature review's structure. Step 5 - Write your literature review. Free lecture slides.
The Critical Literature Review Q: What is a literature review? Stated most simply, it is an overview of published and unpublished materials which help answer two fundamental questions: 1. What are the current theoretical or policy issues and debates related to your topic? 2. What is the current state of knowledge about these issues and problems?
Critically reviewing the literature is an indispensible skill which is used throughout a research career. This article demystifies the processes involved in systematically and critically reviewing the literature to demonstrate knowledge, identify research ideas, position research and develop theory. Although aimed primarily at research students ...
A literature review is a document or section of a document that collects key sources on a topic and discusses those sources in conversation with each other (also called synthesis ). The lit review is an important genre in many disciplines, not just literature (i.e., the study of works of literature such as novels and plays).
A formal literature review is an evidence-based, in-depth analysis of a subject. There are many reasons for writing one and these will influence the length and style of your review, but in essence a literature review is a critical appraisal of the current collective knowledge on a subject. Rather than just being an exhaustive list of all that ...
These steps includ e; a) critical reading and note-taking, b) writing. a s ummary of the reviewed literature, c) organization of literature review, and d) the use of a synthesis matrix. The last ...
WRITING A TARGETED LITERATURE REVIEW a targeted literature review is NOT: ¡ a sophisticated evaluation of the entire literature or literatures related to your topic ¡ a set of thinly connected summaries of important related works haphazardly selected from many subfields a targeted literature review IS: ¡ a carefully curated set of sources from a small number of subfield literatures
In addition to critical thinking, a literature review needs consistency, for example in the choice of passive vs. active voice and present vs. past tense. Rule 7: Find a Logical Structure. Like a well-baked cake, a good review has a number of telling features: it is worth the reader's time, timely, systematic, well written, focused, and ...
he simplest thing of all—structure. Everything you write has three components: a beginning, a middle and an e. d and each serves a different purpose. In practice, this means your review will have an introduction, a main body where you review the literature an. a conclusion where you tie things up.
What kinds of literature reviews are written? Narrative review: The purpose of this type of review is to describe the current state of the research on a specific topic/research and to offer a critical analysis of the literature reviewed. Studies are grouped by research/theoretical categories, and themes and trends, strengths and weakness, and gaps are identified.
Abstract. Critically reviewing the literature is an indispensible skill which is used throughout a research career. This demystifies the processes involved in systematically and critically reviewing the literature to demonstrate knowledge, identify research ideas and questions, position research and develop theory.
Steps to Completing a Literature Review. Find. Conduct searches for relevant information. Evaluate. Critically review your sources. Summarize. Determine the most important and relevant information from each source, theories, findings, etc. Synthesize. Create a synthesis matrix to find connections between resources, and ensure your sources ...
As mentioned above, writing your literature review is a process, which I'll break down into three steps: Finding the most suitable literature. Understanding, distilling and organising the literature. Planning and writing up your literature review chapter. Importantly, you must complete steps one and two before you start writing up your chapter.
A formal literature review is an evidence-based, in-depth analysis of a subject. There are many reasons for writing one and these will influence the length and style of your review, but in essence a literature review is a critical appraisal of the current collective knowledge on a subject.
As mentioned previously, there are a number of existing guidelines for literature reviews. Depending on the methodology needed to achieve the purpose of the review, all types can be helpful and appropriate to reach a specific goal (for examples, please see Table 1).These approaches can be qualitative, quantitative, or have a mixed design depending on the phase of the review.
A literature review is a type of critical review in which you analyze and evaluate many sources on a specific topic. The purpose is to provide your reader with an overview of the research that has been done on your topic, and to evaluate the sources you are reviewing. You will probably include less
Express Critical Analysis. The literature review of a dissertation should include critical analysis. You cannot simply juxtapose the literature you find: you have to evaluate and draw conclusions from it. Paragraph level. Try expressing your voice in each paragraph of your literature review. Write strong paragraphs.
Literature reviews play a critical role in scholarship because science remains, first and foremost, a cumulative endeavour (vom Brocke et al., 2009). As in any academic discipline, rigorous knowledge syntheses are becoming indispensable in keeping up with an exponentially growing eHealth literature, assisting practitioners, academics, and graduate students in finding, evaluating, and ...
More and more students are required to perform a critical literature review as part of their undergraduate or postgraduate studies. Whilst most of the latest research methods textbooks advise how to do a literature search, very few cover the literature review. This paper covers two types of review: a critical literature review and a systematic ...
Types of Literature Review are as follows: Narrative literature review: This type of review involves a comprehensive summary and critical analysis of the available literature on a particular topic or research question. It is often used as an introductory section of a research paper. Systematic literature review: This is a rigorous and ...
To write a good critical review, you will have to engage in the mental processes of analyzing (taking apart) the work-deciding what its major components are and determining how these parts (i.e., paragraphs, sections, or chapters) contribute to the work as a whole. Analyzing the work will help you focus on how and why the author makes certain ...
What is a Critical Literature Review? ... The methods in a systematic literature review are designed to offer a comprehensive textual summary and synthesis of existing research, providing context and background information critical to understanding the broader research landscape. Systematic reviews are essential for informing evidence-based ...
Critical Analysis in a Literature Review. A literature review is vital to any in-depth research, providing a foundation your work will build upon. Familiarizing yourself with the existing literature allows you to identify current debates in the field, ensuring that your work is up-to-date and addresses significant questions. ...
In the context of the constant evolution and proliferation of AI technology, hybrid intelligence is gaining popularity in reference to a balanced coexistence between human and artificial intelligence. The term has been extensively used over the past two decades to define models of intelligence involving more than one technology. This paper aims to provide (i) a concise and focused overview of ...
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents.
Addressing the transfer of such tacit knowledge necessitates the implementation of various strategies. This systematic literature review, conducted as applicable in accordance with the PRISMA [41] statement, aims to explore and compile existing methodologies for transferring tacit knowledge within safety-critical systems.
Critical Review is indexed or abstracted in: ABC-Clio , Book Review Index, CIAO (Columbia International Affairs Online), Current Contents/Social & Behavioral Sciences, Economic Literature Index on DIALOG , EconLit on CD-ROM , Hoover's, Index to Book Reviews in the Humanities, International Bibliography of Book Reviews, International Bibliography of Periodical Literature, International ...
The greater the number of "yes" responses on the evaluation forms used in this review, the lower the risk of bias. Table 1 shows that the total number of positive responses was 84.6%, with questions 4 and 6 indicating a possible risk of bias considering that there was no information about the blinding of participants and outcome raters. Table 2 shows that the minimum percentage of positive ...
This article treats critical literature reviews as a distinct review type, and presents a critique of author-labeled critical literature reviews in Organization and Management Studies. We identify and problematize 275 review articles that claim to critically review a body of literature and find that most to not deliver on this claim.
This article describes a nurse-led rapid review service implemented at a large academic medical center and provides a reproducible process to guide other healthcare organizations in developing similar programs. Due to shifting priorities and unforeseen challenges, nurse leaders often lack sufficient time and resources to systematically review and appraise the available literature in search of ...