COVID-19: Stress and Anxiety
[Additional essays and videocasts regarding psychological ramifications of the COVID-19 virus outbreak can be found at: https://communitiescollaborating.com/[
The COVID-19 virus knows all about the human psyche. The virus is aware that we experience stress and become anxious when we keep a distance from other people and are forced to isolate ourselves from direct, physical contact with the people we love and cherish. Under conditons of stress and as we become more anxious, our vulnerability also increases — leaving us even more anxious. A vicious cycle . . . and a cycle that we need to stop!!
This essay includes material prepared by members of the Global Psychology Task Force–a group of experienced professional psychologists from around the world who have come together to address the psychological ramifications of the COVID-19 virus. They have prepared a website (www.communities collaborating.com) that incorporates essays, video clips and links to other references that address these ramifications. This essay is derived from the content of this website.

Stress Ruts, Lions and Lumens
We start with a brief video presentation by Dr. William Bergquist, a member of the Global Psychology Task Force. He has titled his presentation: “Stress Ruts, Lions and Lumens in the Age of the Pandemic”:
Reducing the Stress and Anxiety
This essay concerns the way to reduce the stress and anxiety. In addressing this psychological dynamic we turn to both the anxiety aroused by those who have tested positive for the virus and those who have not been tested or have been tested and are negative but still worry about the physical and psychological health of other people in their life, as well as their own economic health and the economic and societal health of their community and country.
https://www.vox.com/identities/2020/3/21/21188362/manage-anxiety-pandemic
We turn now to someone who have been infected by COVID-19
Managing the Anxiety as Someone Who Has Been Infected
The anxiety associated with any major illness is quite understandable and is not in any way a sign of weakness. There are many ways in which to address this anxiety–such as looking to loved ones for support (even if they can’t be physically present), reducing other sources of stress in one’s life, identifying daily plans for dealing with the virus–and most importantly taking actions that enable you to feel less powerless and victimized.
It is perhaps best to turn from these general recommendations to the insights offered by someone who has been infected and struggled for a lengthy period of time with the infestation and related fever and isolation. This person is Dr. Suzanne Brennen-Nathan, one or our Global Psychology Task Force members. Suzanne is a highly experienced psychotherapist who has specialized in the treatment of trauma in her clinical practice. Who better to reflect on the illness and offer recommendations then someone “who has been there” and has expertise in the traumatizing impact of a major illness like COVID-19. Suzanne has been interviewed by Dr. William Bergquist, another member of the Task Force:
Managing the Anxiety as Someone Who Hasn’t Been Tested or Is Negative But Still Fearful
What about those of us who have not tested positive for COVID-19 or have not been tested at all. At the heart of the matter in facing the challenges associated with the COVID-19 virus — whether these challenges be financial, vocational or family related–is the stress that inevitably is induced when we think about, feel about and take action about the virus’ threatening nature.
We therefore begin this statement about action to be taken with an excellent presentation by one of our task force members, Christy Lewis:
To begin a cross-cultural reflection on the psychological ramifications of the COVID-19 virus, we offer an essay on the way in which one of our Task Force members, Eliza Wong, Psy.D., works with highly anxious clients in her home country: Singapore.
Dealing with Anxiety during COVID-19 in Singapore
We hope these perspectives on stress and anxiety in the age of the COVID-19 virus invasion provides some guidance for you in better understanding the psychological impact of the virus and identifying actions you can take to help ameliorate this impact.
- Related Articles
- More By William Bergquist
- More In Health / Biology
The Shattered Tin Man Midst the Shock and Awe in Mid-21st Century Societies I: Shattering and Shock
Lay me down to sleep: designing the environment for high quality rest, the wonder of interpersonal relationships via: culprits of division and bach family members as exemplars of relating midst differences, i dreamed i was flying: a developmental representation of competence, snuggling in: what makes us comfortable when we sleep, the intricate and varied dances of friendship i: turnings and types, leadership in the midst of heath care complexity ii: coaching, balancing and moving across multiple cultures, leadership in the midst of heath care complexity i: team operations and design, delivering health care in complex adaptive systems i: the nature of dynamic systems, leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
I wish to introduce a quite different interpretation regarding the presence of flight in t…
- Counseling / Coaching
- Health / Biology
- Sleeping/Dreaming
- Personality
- Developmental
- Cognitive and Affective
- Psychobiographies
- Disclosure / Feedback
- Influence / Communication
- Cooperation / Competition
- Unconscious Dynamics
- Intervention
- Child / Adolescent
- System Dynamics
- Organizational Behavior / Dynamics
- Development / Stages
- Organizational Types / Structures
- System Dynamics / Complexity
- Assessment / Process Observation
- Intervention / Consulting
- Cross Cultural
- Behavioral Economics
- Technologies
- Edge of Knowledge
- Organizational
- Laboratories
- Field Stations
- In Memoriam
- COVID-19 and your mental health
Worries and anxiety about COVID-19 can be overwhelming. Learn ways to cope as COVID-19 spreads.
At the start of the COVID-19 pandemic, life for many people changed very quickly. Worry and concern were natural partners of all that change — getting used to new routines, loneliness and financial pressure, among other issues. Information overload, rumor and misinformation didn't help.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020.
Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19. And you're not alone if you've coped with the stress in less than healthy ways, such as substance use.
But healthier self-care choices can help you cope with COVID-19 or any other challenge you may face.
And knowing when to get help can be the most essential self-care action of all.
Recognize what's typical and what's not
Stress and worry are common during a crisis. But something like the COVID-19 pandemic can push people beyond their ability to cope.
In surveys, the most common symptoms reported were trouble sleeping and feeling anxiety or nervous. The number of people noting those symptoms went up and down in surveys given over time. Depression and loneliness were less common than nervousness or sleep problems, but more consistent across surveys given over time. Among adults, use of drugs, alcohol and other intoxicating substances has increased over time as well.
The first step is to notice how often you feel helpless, sad, angry, irritable, hopeless, anxious or afraid. Some people may feel numb.
Keep track of how often you have trouble focusing on daily tasks or doing routine chores. Are there things that you used to enjoy doing that you stopped doing because of how you feel? Note any big changes in appetite, any substance use, body aches and pains, and problems with sleep.
These feelings may come and go over time. But if these feelings don't go away or make it hard to do your daily tasks, it's time to ask for help.
Get help when you need it
If you're feeling suicidal or thinking of hurting yourself, seek help.
- Contact your healthcare professional or a mental health professional.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline , available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
If you are worried about yourself or someone else, contact your healthcare professional or mental health professional. Some may be able to see you in person or talk over the phone or online.
You also can reach out to a friend or loved one. Someone in your faith community also could help.
And you may be able to get counseling or a mental health appointment through an employer's employee assistance program.
Another option is information and treatment options from groups such as:
- National Alliance on Mental Illness (NAMI).
- Substance Abuse and Mental Health Services Administration (SAMHSA).
- Anxiety and Depression Association of America.
Self-care tips
Some people may use unhealthy ways to cope with anxiety around COVID-19. These unhealthy choices may include things such as misuse of medicines or legal drugs and use of illegal drugs. Unhealthy coping choices also can be things such as sleeping too much or too little, or overeating. It also can include avoiding other people and focusing on only one soothing thing, such as work, television or gaming.
Unhealthy coping methods can worsen mental and physical health. And that is particularly true if you're trying to manage or recover from COVID-19.
Self-care actions can help you restore a healthy balance in your life. They can lessen everyday stress or significant anxiety linked to events such as the COVID-19 pandemic. Self-care actions give your body and mind a chance to heal from the problems long-term stress can cause.
Take care of your body
Healthy self-care tips start with the basics. Give your body what it needs and avoid what it doesn't need. Some tips are:
- Get the right amount of sleep for you. A regular sleep schedule, when you go to bed and get up at similar times each day, can help avoid sleep problems.
- Move your body. Regular physical activity and exercise can help reduce anxiety and improve mood. Any activity you can do regularly is a good choice. That may be a scheduled workout, a walk or even dancing to your favorite music.
- Choose healthy food and drinks. Foods that are high in nutrients, such as protein, vitamins and minerals are healthy choices. Avoid food or drink with added sugar, fat or salt.
- Avoid tobacco, alcohol and drugs. If you smoke tobacco or if you vape, you're already at higher risk of lung disease. Because COVID-19 affects the lungs, your risk increases even more. Using alcohol to manage how you feel can make matters worse and reduce your coping skills. Avoid taking illegal drugs or misusing prescriptions to manage your feelings.
Take care of your mind
Healthy coping actions for your brain start with deciding how much news and social media is right for you. Staying informed, especially during a pandemic, helps you make the best choices but do it carefully.
Set aside a specific amount of time to find information in the news or on social media, stay limited to that time, and choose reliable sources. For example, give yourself up to 20 or 30 minutes a day of news and social media. That amount keeps people informed but not overwhelmed.
For COVID-19, consider reliable health sources. Examples are the U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO).
Other healthy self-care tips are:
- Relax and recharge. Many people benefit from relaxation exercises such as mindfulness, deep breathing, meditation and yoga. Find an activity that helps you relax and try to do it every day at least for a short time. Fitting time in for hobbies or activities you enjoy can help manage feelings of stress too.
- Stick to your health routine. If you see a healthcare professional for mental health services, keep up with your appointments. And stay up to date with all your wellness tests and screenings.
- Stay in touch and connect with others. Family, friends and your community are part of a healthy mental outlook. Together, you form a healthy support network for concerns or challenges. Social interactions, over time, are linked to a healthier and longer life.
Avoid stigma and discrimination
Stigma can make people feel isolated and even abandoned. They may feel sad, hurt and angry when people in their community avoid them for fear of getting COVID-19. People who have experienced stigma related to COVID-19 include people of Asian descent, health care workers and people with COVID-19.
Treating people differently because of their medical condition, called medical discrimination, isn't new to the COVID-19 pandemic. Stigma has long been a problem for people with various conditions such as Hansen's disease (leprosy), HIV, diabetes and many mental illnesses.
People who experience stigma may be left out or shunned, treated differently, or denied job and school options. They also may be targets of verbal, emotional and physical abuse.
Communication can help end stigma or discrimination. You can address stigma when you:
- Get to know people as more than just an illness. Using respectful language can go a long way toward making people comfortable talking about a health issue.
- Get the facts about COVID-19 or other medical issues from reputable sources such as the CDC and WHO.
- Speak up if you hear or see myths about an illness or people with an illness.
COVID-19 and health
The virus that causes COVID-19 is still a concern for many people. By recognizing when to get help and taking time for your health, life challenges such as COVID-19 can be managed.
- Mental health during the COVID-19 pandemic. National Institutes of Health. https://covid19.nih.gov/covid-19-topics/mental-health. Accessed March 12, 2024.
- Mental Health and COVID-19: Early evidence of the pandemic's impact: Scientific brief, 2 March 2022. World Health Organization. https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1. Accessed March 12, 2024.
- Mental health and the pandemic: What U.S. surveys have found. Pew Research Center. https://www.pewresearch.org/short-reads/2023/03/02/mental-health-and-the-pandemic-what-u-s-surveys-have-found/. Accessed March 12, 2024.
- Taking care of your emotional health. Centers for Disease Control and Prevention. https://emergency.cdc.gov/coping/selfcare.asp. Accessed March 12, 2024.
- #HealthyAtHome—Mental health. World Health Organization. www.who.int/campaigns/connecting-the-world-to-combat-coronavirus/healthyathome/healthyathome---mental-health. Accessed March 12, 2024.
- Coping with stress. Centers for Disease Control and Prevention. www.cdc.gov/mentalhealth/stress-coping/cope-with-stress/. Accessed March 12, 2024.
- Manage stress. U.S. Department of Health and Human Services. https://health.gov/myhealthfinder/topics/health-conditions/heart-health/manage-stress. Accessed March 20, 2020.
- COVID-19 and substance abuse. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/covid-19-substance-use#health-outcomes. Accessed March 12, 2024.
- COVID-19 resource and information guide. National Alliance on Mental Illness. https://www.nami.org/Support-Education/NAMI-HelpLine/COVID-19-Information-and-Resources/COVID-19-Resource-and-Information-Guide. Accessed March 15, 2024.
- Negative coping and PTSD. U.S. Department of Veterans Affairs. https://www.ptsd.va.gov/gethelp/negative_coping.asp. Accessed March 15, 2024.
- Health effects of cigarette smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/index.htm#respiratory. Accessed March 15, 2024.
- People with certain medical conditions. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed March 15, 2024.
- Your healthiest self: Emotional wellness toolkit. National Institutes of Health. https://www.nih.gov/health-information/emotional-wellness-toolkit. Accessed March 15, 2024.
- World leprosy day: Bust the myths, learn the facts. Centers for Disease Control and Prevention. https://www.cdc.gov/leprosy/world-leprosy-day/. Accessed March 15, 2024.
- HIV stigma and discrimination. Centers for Disease Control and Prevention. https://www.cdc.gov/hiv/basics/hiv-stigma/. Accessed March 15, 2024.
- Diabetes stigma: Learn about it, recognize it, reduce it. Centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html. Accessed March 15, 2024.
- Phelan SM, et al. Patient and health care professional perspectives on stigma in integrated behavioral health: Barriers and recommendations. Annals of Family Medicine. 2023; doi:10.1370/afm.2924.
- Stigma reduction. Centers for Disease Control and Prevention. https://www.cdc.gov/drugoverdose/od2a/case-studies/stigma-reduction.html. Accessed March 15, 2024.
- Nyblade L, et al. Stigma in health facilities: Why it matters and how we can change it. BMC Medicine. 2019; doi:10.1186/s12916-019-1256-2.
- Combating bias and stigma related to COVID-19. American Psychological Association. https://www.apa.org/topics/covid-19-bias. Accessed March 15, 2024.
- Yashadhana A, et al. Pandemic-related racial discrimination and its health impact among non-Indigenous racially minoritized peoples in high-income contexts: A systematic review. Health Promotion International. 2021; doi:10.1093/heapro/daab144.
- Sawchuk CN (expert opinion). Mayo Clinic. March 25, 2024.
Products and Services
- A Book: Endemic - A Post-Pandemic Playbook
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- A Book: Future Care
- Antibiotics: Are you misusing them?
- COVID-19 and vitamin D
- Convalescent plasma therapy
- Coronavirus disease 2019 (COVID-19)
- COVID-19: How can I protect myself?
- Herd immunity and respiratory illness
- COVID-19 and pets
- COVID-19 antibody testing
- COVID-19, cold, allergies and the flu
- COVID-19 tests
- COVID-19 drugs: Are there any that work?
- COVID-19 in babies and children
- Coronavirus infection by race
- COVID-19 travel advice
- COVID-19 vaccine: Should I reschedule my mammogram?
- COVID-19 vaccines for kids: What you need to know
- COVID-19 vaccines
- COVID-19 variant
- COVID-19 vs. flu: Similarities and differences
- COVID-19: Who's at higher risk of serious symptoms?
- Debunking coronavirus myths
- Different COVID-19 vaccines
- Extracorporeal membrane oxygenation (ECMO)
- Fever: First aid
- Fever treatment: Quick guide to treating a fever
- Fight coronavirus (COVID-19) transmission at home
- Honey: An effective cough remedy?
- How do COVID-19 antibody tests differ from diagnostic tests?
- How to measure your respiratory rate
- How to take your pulse
- How to take your temperature
- How well do face masks protect against COVID-19?
- Is hydroxychloroquine a treatment for COVID-19?
- Long-term effects of COVID-19
- Loss of smell
- Mayo Clinic Minute: You're washing your hands all wrong
- Mayo Clinic Minute: How dirty are common surfaces?
- Multisystem inflammatory syndrome in children (MIS-C)
- Nausea and vomiting
- Pregnancy and COVID-19
- Safe outdoor activities during the COVID-19 pandemic
- Safety tips for attending school during COVID-19
- Sex and COVID-19
- Shortness of breath
- Thermometers: Understand the options
- Treating COVID-19 at home
- Unusual symptoms of coronavirus
- Vaccine guidance from Mayo Clinic
- Watery eyes
Related information
- Mental health: What's normal, what's not - Related information Mental health: What's normal, what's not
- Mental illness - Related information Mental illness
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.

Stress and decision-making during the pandemic

More than 18 months into the coronavirus pandemic, Americans remain in limbo between lives once lived and whatever the post-pandemic future holds. For many, the current reality encompasses a daily web of risk assessment, upended routines and endless news about the state of COVID-19 in the world, America and our individual communities.
October 26, 2021
A new survey conducted by The Harris Poll on behalf of the American Psychological Association found that stress levels are holding steady from recent years, and despite many struggles, U.S. adults retain a positive outlook. Most (70%) were confident that everything will work out after the coronavirus pandemic ends, and more than three-quarters (77%) said, all in all, they are faring well during the coronavirus pandemic.
However, behind this professed optimism about the future, day-to-day struggles are overwhelming many. Prolonged effects of stress and unhealthy behavior changes are common. Daily tasks and decision-making have become more difficult during the pandemic, particularly for younger adults and parents. As each day can bring a new set of decisions about safety, security, growth, travel, work, and other life requirements, people in the United States seem to be increasingly wracked with uncertainty.
U.S. adults are struggling with daily decisions, especially millennials
For many, the pandemic has imposed the need for constant risk assessment, with routines upended and once trivial tasks recast in light of the pandemic. Many people ask, “What is the community transmission in my area today and how will this affect my choices? What is the vaccination rate? Is there a mask mandate here?” When the factors influencing a person’s decisions are constantly changing, no decision is routine. And this is proving to be exhausting.
According to the survey, nearly one-third of adults (32%) said sometimes they are so stressed about the coronavirus pandemic that they struggle to make basic decisions, such as what to wear or what to eat. Millennials (48%) were particularly likely to struggle with this when compared with other groups (Gen Z adults: 37%, Gen Xers: 32%, Boomers: 14%, older adults: 3%).

View a full-sized version of the image available for download.
View a full-sized version of the image with a description.
More than one-third said it has been more stressful to make day-to-day decisions (36%) and major life decisions (35%) compared with before the coronavirus pandemic. Younger adults were more likely to feel these decisions are more stressful now (daily decisions: 40% of Gen Z adults, 46% of millennials, and 39% of Gen Xers vs. 24% of boomers, and 14% of older adults; major decisions: 50% of Gen Z adults and 45% of millennials vs. 33% of Gen Xers, 24% of boomers, and 6% of older adults). And slightly more than three in five (61%) agreed the coronavirus pandemic has made them rethink how they were living their life.
More than three in five (63%) agreed that uncertainty about what the next few months will be like causes them stress, and around half (49%) said that the coronavirus pandemic has made planning for their future feel impossible.
When it comes to overall stress, it is not surprising to find that younger generations, who were more likely to say they struggle with basic decisions, also reported generally high stress levels. Gen Z adults (5.6 out of 10 ), millennials (5.7), and Gen Xers (5.2) reported higher average stress levels over the past month related to the coronavirus pandemic than boomers (4.3) and older adults (2.9). This pattern was mirrored in the groups’ respective ability to manage stress; around half of Gen Z adults (45%) and millennials (50%) said they do not know how to manage the stress they feel due to the coronavirus pandemic, compared with 32% of Gen Xers, 21% of boomers, and 12% of older adults.
1 On a scale of one to 10 where one means “little to no stress” and 10 means “a great deal of stress.”
More dependents, more decisions—pandemic parenting stress persists
Decision-making fatigue is having a disproportionate impact on parents, given changes to work, school, and everyday routines during the pandemic. Many are struggling to manage households divided by vaccination status, with one set of rules for vaccinated adults and kids over age 12 and another for younger unvaccinated children—not to mention varying health conditions that may exist.
The ongoing uncertainty and changes seem to be compounding struggles for parents, especially for those with younger children. For instance, parents with children under age 18 were more likely than those without children to say that both day-to-day decisions and major life decisions are more stressful than they were pre-pandemic (daily: 47% vs. 30%; major: 44% vs. 31%), with 54% of those with young children ages zero to four reporting that day-to-day decisions have become more stressful.
Moreover, almost half of parents reported that sometimes they are so stressed about the coronavirus pandemic that they struggle to make basic decisions (e.g., what to wear, what to eat) (47% vs. 24% of non-parents). Meanwhile, the majority made at least one major life decision during the coronavirus pandemic (62% vs. 35% of non-parents), illustrating a decision-making paradox that seems to have emerged: despite uncertainty and decision difficulty, major life changes still occur.
All of this is wearing on parents as the pandemic persists. And while most parents said they are faring well during the coronavirus pandemic, they were less likely to say so than non-parents (71% vs. 80%). Further, compared with 2020, parents were:
- More likely to say family responsibilities (75% vs. 70% of parents in 2020) and relationships (68% vs. 64%) are significant sources of stress in their lives.
- More likely to feel they could have used more emotional support than they received over the past year (79% vs. 71%).
- Less likely to feel they are doing enough to manage their stress (58% vs. 67%).
- More likely to nap (35% vs. 30%) to manage their stress but less likely to spend time with friends or family (35% vs. 42%).
- Less likely to say their mental health is very good or excellent (47% vs. 52%).

Pandemic stress among people of color is still elevated, especially for Hispanic adults
Hispanic and Black adults were less likely to say they are faring well during the coronavirus pandemic than non-Hispanic White adults, though the levels still speak to an overall positive outlook (81% of non-Hispanic White adults vs. 68% of Hispanic adults and 72% of Black adults). Still, in line with the overall survey findings, this optimistic finding stands in contrast to the reality of compounding pandemic-related stressors bearing down on marginalized communities, especially Hispanic adults.
For example, Hispanic adults were more likely than non-Hispanic White adults to say decision-making has become more stressful compared with before the pandemic (day-to-day decisions: 44% vs. 34%; major decisions: 40% vs. 32%), and Hispanic and Black adults were more likely than non-Hispanic White adults to say sometimes they are so stressed about the coronavirus pandemic that they struggle to make even basic decisions (e.g., what to wear, what to eat, etc.) (38% and 36% vs. 29%, respectively).
Hispanic adults reported the highest levels of stress, on average, over the past month related to the coronavirus pandemic (5.6 vs. Black adults: 5.1; Asian adults: 5.1; non-Hispanic White adults: 4.8). Moreover, Hispanic adults were most likely to say they are struggling with the ups and downs of the coronavirus pandemic (61% vs. 51% of non-Hispanic White adults and 51% of Black adults) and that they don’t know how to manage the stress they feel due to the pandemic (43% vs. 33% and 34%, respectively).
This unequal burden of stress on Hispanic adults was not surprising, considering findings from the survey that shine a light on racial and ethnic disparities in relation to the impact of the pandemic. Specifically, Hispanic adults were more likely than non-Hispanic White adults to know someone who had been sick with or died of COVID-19 (sick: 64% vs. 46%; died: 42% vs. 25%).

Stress levels remain higher than pre-pandemic levels, work- and housing costs-related stress on the rise
The average reported level of stress during the past month among all adults was 5.0, which has held steady from 2020. Still, this level is slightly elevated from pre-pandemic levels (2021: 5.0; 2020: 5.0; 2019: 4.9; 2018: 4.9; 2017: 4.8; 2016: 4.8).
And while a year over year comparison of significant sources of stress shows a downward trend across most factors, work- and housing costs-related stress slightly increased from 2020. Additionally, all sources of stress remain somewhat higher than pre-pandemic levels, with the economy, housing costs, personal safety, and discrimination representing more dramatic spikes.
Significant sources of stress: 2019–2021

Many are suffering from the impacts of stress, younger adults and parents continue to bear the brunt
As a result of stress, nearly three-quarters of U.S. adults (74%) have experienced various impacts in the last month, such as headaches (34%), feeling overwhelmed (34%), fatigue (32%), or changes in sleeping habits (32%). Again, younger adults and parents were more likely to report this, with 86% of millennials reporting impacts of stress, closely followed by Gen Z adults (84%) and Gen Xers (77%); only 59% of boomers and 57% of older adults said the same. Parents were also more likely than non-parents to report experiencing impacts of stress in the last month (83% vs. 69%).
Further, the majority of adults (59%) said they have experienced behavior changes as a result of stress in the past month. Most commonly, the changes had been avoiding social situations (24%), altering eating habits (23%), procrastinating or neglecting responsibilities (22%), or altering physical activity levels (22%). In conjunction with changes in eating habits and physical activity, more than one-third said they eat to manage their stress, which remains elevated after increasing during the first year of the pandemic (25% in 2019, 37% in 2020, and 35% in 2021).
- Gen Z adults: 79%; millennials: 74%; Gen Xers: 64% versus boomers: 37%; older adults: 17%
- Parents: 75% vs. non-parents: 50%

Resilience among populations varies, some are faring better than others
Generally speaking, U.S. adults are adjusting through the pandemic, but some show fewer signs of resiliency than others. More than half of U.S. adults (53%) agreed they are struggling with the ups and downs of the coronavirus pandemic. Further, slightly more than one-quarter (26%) have low resilience, as determined by a score of 1.00 to 2.99 on the Brief Resilience Scale. Fifty-eight percent had average resilience (a score of 3.00 to 4.30) and 16% had high resilience (a score of 4.31 to 5.00), the survey found.
Younger adults, parents, and those with an annual household income of less than $50K were more likely than their respective counterparts to have a low resilience score. Those with low resilience scores were more likely than those with average or high resilience to say:
- Their stress level, on average, over the past month related to the pandemic has been higher (average: 6.3 vs. 4.9 and 3.3).
- The level of stress in their life increased compared with before the pandemic (53% vs. 43% and 24%).
- Making decisions has become more stressful compared with before the pandemic (day-to-day decisions: 55% vs. 33% and 16%; major decisions: 54% vs. 32% and 13%).
- Sometimes they are so stressed about the coronavirus pandemic that they struggle to make even basic decisions (50% vs. 31% and 5%).
Further, those with low resilience scores were around three times as likely to have experienced negative impacts of stress in the last month (94% vs. 75% and 38%), particularly feeling overwhelmed (57% vs. 29% and 12%) and behavior changes as a result of stress (85% vs. 56% and 25%), particularly avoiding social situations (41% vs. 20% and 10%).
Speaking to the struggles of this group, those with low resilience scores were more likely to be taking actions to manage their stress (98% vs. 92% and 80%), but also to feel they could have used more emotional support than they received over the past year (88% vs. 60% and 25%).
Methodology
The August/COVID Resilience Survey was conducted online within the United States by The Harris Poll on behalf of the American Psychological Association between August 11 and August 23, 2021, among 3,035 adults age 18+ who reside in the United States.
Interviews were conducted in English and Spanish. Data were weighted to reflect their proportions in the population based on the 2020 Current Population Survey (CPS) by the U.S. Census Bureau. Weighting variables included age by gender, race/ethnicity, education, region, and household income. Hispanic adults were also weighted for acculturation, taking into account respondents’ household language as well as their ability to read and speak in English and Spanish. Country of origin (United States/non-United States) was also included for Hispanic and Asian subgroups. Weighting variables for Gen Z adults (ages 18 to 24) included education, age by gender, race/ethnicity, region, household income, and size of household, based on the 2019 CPS. Propensity score weighting was used to adjust for respondents’ propensity to be online.
Parents are defined as U.S. adults ages 18+ who have at least one person under the age of 18 living in their household at least 50% of the time for whom they are the parent or guardian.
Generational definitions are as follows: Gen Z adults (ages 18 to 24), millennials (ages 25 to 42), Gen Xers (ages 43 to 56), boomers (ages 57 to 75), and older adults (ages 76+).
Related resources
- Report document (PDF, 4.48MB)
- Survey questions (PDF, 222KB)
- Press release: Pandemic impedes basic decision-making ability
- Contact : Sophie Bethune ( email ) Telephone: (202) 336-6134
- 2021 Work and Well-being Survey report
- 2021 COVID-19 Practitioner Survey report
- Parental burnout: How to recognize and overcome it
- Stress and uncertainty
- What's the difference between stress and anxiety?
- Stress's effects on the body
- More stress information and topics
View the Stress in America TM press room.

- Find a Doctor
- Patients & Visitors
- ER Wait Times
- For Medical Professionals
- Piedmont MyChart

- Medical Professionals
- Find Doctors
- Find Locations
Receive helpful health tips, health news, recipes and more right to your inbox.
Sign up to receive the Living Real Change Newsletter
Managing stress during the ongoing COVID-19 pandemic
Are you feeling stress, fear and anxiety amid the ongoing COVID-19 pandemic ? If so, you’re not alone. The recommendations for masking and social distancing affect nearly every part of our lives, including finances, relationships, transportation, jobs and healthcare.
Some common causes of stress during the coronavirus pandemic are uncertainty, lack of routine and reduced social support, says Mark Flanagan, LMSW, MPH, MA, a social worker at Cancer Wellness at Piedmont .
Routines and COVID-19
As humans, we don’t like uncertainty and tend to thrive in routines , says Flanagan. Routines are essential because they create a sense of normalcy and control in our lives. This sense of control then allows us to manage the challenges that come our way.
“When we don’t have a routine, much of our time is spent trying to establish one,” says Flanagan. “Without a routine, we often pay attention to the things that are most ‘flashy.’ When big news happens, we tend to focus on it more.”
Social support and COVID-19
Not only are our routines currently disrupted, but the routines of everyone around us are as well.
“When something goes wrong in our lives, we can usually rely on others to get a sense of calm,” he says. “But when everyone is experiencing the same sense of uncertainty, there’s no real ‘anchor’ to help manage some of the stress.”
Stress affects your health
Stress management is essential for good physical health , and it’s especially important right now as our world addresses the COVID-19 pandemic .
“While short-term pressures and stress are normal and can help us change in positive ways , chronic stress causes a huge deterioration in our quality of life on a physical level,” says Flanagan. “When we are more pessimistic, depressed or anxious, our immune system goes down and produces more stress hormones, reducing our immunity and increasing inflammation.”
Stress can also put a strain on your mental health, relationships and productivity, he notes.
Stress reduction tips for COVID-19
“Rather than dwell on nervousness, focus on the things you can control,” Flanagan suggests. “When you move the locus of control from something outside yourself to inside yourself, you powerfully reduce anxiety and boost confidence.”
He suggests the following steps to regain control and reduce stress.
Follow the recommended health guidelines. These guidelines include getting the COVID-19 vaccine , frequent hand-washing, wearing a mask in public places, social distancing, practicing respiratory etiquette and cleaning commonly used surfaces. See the latest recommendations from the Centers for Disease Control and Prevention (CDC) . Not only will you protect your health, but you’ll also protect the health of vulnerable people in your community, like older adults and those with serious or underlying health issues.
Create a morning routine. When you’re stuck at home, it can be tempting to let go of basic routines, but Flanagan says a morning routine can help you feel more productive and positive. Consider waking up at the same time each day, exercising, showering, meditating, journaling, tidying your home or having a healthy breakfast as part of your morning ritual.
Check in with loved ones regularly. Staying in touch with family and friends can help reduce stress.
Consider ways to help others. This can include picking up groceries for a neighbor and leaving them at their door, donating to a local charity, or purchasing gift cards from your favorite restaurant. By taking the focus off yourself, you can experience reduced stress and a greater sense of well-being.
Have a daily self-care ritual. Self-care can include exercise, meditation, walking outside, reading, taking a bubble bath, painting, journaling, gardening, cooking a healthy meal or enjoying a favorite hobby. Pick one thing and do it at the same time each day. It will help anchor your day and provide a welcome respite.
Limit news and media consumption. “When we constantly check our newsfeeds and see bad news, it activates our sympathetic nervous system and can send us into fight-or-flight mode,” says Flanagan. He recommends limiting how often you check the news to once or twice a day (ideally not first thing in the morning or after dinner), turning off news alerts, and obtaining information from one or two reputable news outlets.
Set boundaries around social media. “There’s this concept of toxic sociality where we constantly have to be connected, even in superficial ways, and when we’re not, it feels like part of us isn’t being ‘fed,’” he explains. “It’s important to practice social distancing with social media too. We may not think we’re having any effect on our newsfeed, but we can take steps to reduce the ripple effect of panic on social media.” He suggests posting positive messages online and being mindful of your likes, shares and comments.
Meditate. Meditation can help restore your sense of control as you focus on your breath or a positive word or phrase. “ Meditation can help you activate your parasympathetic nervous system, and that’s an antidote to fear,” says Flanagan. “And when you’re more centered, you’re able to create a calm reality around you.” Try this guided meditation to get started.
Encourage others. “Often, when we are scared, it can be tempting to repeat negative messages, but actively encouraging family and friends is really important,” he says. “Chances are, someone is having a harder time than you are. Your words matter and people will respond accordingly. It’s important to realize we are not victims; we are helping to create our environment and change it for the better. By sending positive messages out into the world, you’ll not only affect those around you, but those words will come back to you.”
Hope during the coronavirus pandemic
“It’s important to remember that this will pass sooner or later,” says Flanagan. “The world has gone through many different challenges, like disease outbreaks, war and uncertain times. For better or worse, these times always pass. That doesn’t mean this time isn’t significantly challenging, but if we focus on what we can control and do things that are good for our health and the health of those around us, we will come out of this in perhaps a more whole state and with a renewed perspective. It’s important to look toward the future and begin building for that future. You can always have hope. Hope never leaves us.”
For information on coronavirus (COVID-19), including symptoms, risks and ways to protect yourself, click here.
- coronavirus
- infectious disease
- stress management
Related Stories

Schedule your appointment online
Schedule with our online booking tool
*We have detected that you are using an unsupported or outdated browser. An update is not required, but for best search experience we strongly recommend updating to the latest version of Chrome, Firefox, Safari, or Internet Explorer 11+
Share this story
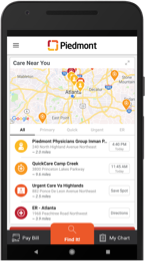
Download the Piedmont Now app
- Indoor Hospital Navigation
- Find & Save Physicians
- Online Scheduling
Download the app today!

7 Ways to Manage Stress During the Coronavirus Pandemic
Taking it easy when it feels like the world is on fire..
Posted March 20, 2020 | Reviewed by Ekua Hagan
- What Is Stress?
- Take our Burnout Test
- Find a therapist to overcome stress

As I write this, I am sitting in the living room of an apartment I rented on Airbnb in Nashville, Tennessee. Two weeks ago, my family and I were here for a tango marathon when dancers from across the country flocked to the Music City for a weekend of good times, southern charm, and the warm embrace of Argentine tango. We made new friends, caught up with old ones, and left with nothing but fond memories. When we arrived at our next destination, we learned that just after we left, tornadoes ripped through Nashville and other parts of Tennessee, devastating the city we love and had enjoyed so much. A lot can happen in a day.
The coronavirus was on the news and definitely a topic of conversation, but most of the people we talked to felt optimistic . Two weeks later, and it seems to be all anyone can think about. The stores are empty, stripped clean of essential items like toilet paper and milk, and the bars and restaurants that help make this city so much fun are closed. Face masks are common, and every cough or sneeze causes momentary panic. In other countries, and even in other cities and states, citizens have been ordered to remain in their homes, and all large gatherings of people have been canceled. A lot can happen in a couple of weeks.
We are back in Nashville because of our own cancelations. My partner Sarah is a tango dancer, and I am a touring public speaker, and both of us are self-employed. We were on our way to Memphis for a series of speaking gigs when we started receiving the notifications, one after another after another until our entire tour had been canceled. We live on the road as we work, so a canceled tour also means we need to find somewhere to call home for a bit. Being just a couple of hours shy of Nashville, we decided to hole up here for a few days and plan our next steps.
To say our situation is stressful is an understatement. There are a lot of people who have it worse, but we have lost all our income for the next three months, our housing, and we have a little girl to consider as well. It is a tough spot, and yet both of us are in relatively good spirits. Neither of us has dealt with anything like this before, but we both handle stress well and remain optimistic, even when the global situation seems to get worse and worse. How do we do it?
Drugs. Lots and lots of drugs.
I am joking, of course. Sarah and I are both highly resilient people. In fact, the canceled tour was about stress management , a subject that I have been speaking to audiences about for years. I even wrote a book on the subject, The Art of Taking It Easy , and have been putting those skills to practice all my life. Sarah puts her own stress management skills to test every day by having to deal with me.
The coronavirus pandemic, and the reaction to it, may seem as if the world is on fire. Granted, I have never seen anything like this in my lifetime (which probably overlaps significantly with your lifetime), so it might be on a larger scale, but it is still just another source of stress in a long line of things that cause stress. Stress is stress regardless of the source, and the tools to manage it are the same. Allow me to share a few here.
Before I do, please note that I am discussing how we can manage our stress, anxiety , or worrisome reactions to the pandemic, not the coronavirus itself. Also, if you have been personally affected by the coronavirus, I wish you or your loved ones a healthy recovery. My goal here is to help most of us stay calm or, as I like to put it, take it easy.
1. Assess your threat level. When overwhelmed with worry or fear , it is sometimes helpful to inform yourself of the facts to assess your personal level of threat. For example, earlier in the month, I had a moment of concern and looked up the infection statistics at the time. There were about 120,000 people known to have the virus out of the nearly 8 billion people that live on this planet. Also, most of those cases were in China while my feet were planted firmly in the United States.
Digging even deeper, I found that there were only seven cases in my state and none of them in my area. I assessed my threat level as low and slept easily that night. Now, you might say, “But, Brian, what about all those people that could be spreading the virus without knowing it?” to which I’d answer that I am trying to reduce anxiety, not add to it. Once you have assessed your threat, then it is important to…

2. Identify what you can control. When we encounter stress, any stress, it is important that we ask ourselves if we can do anything about it. If there is some action we can take, then taking that action will help reduce our anxiety. For example, experts emphasize the importance of handwashing to minimize the spread of the virus. Most of us are capable of washing our hands, so wash your damn hands more often than you do.
If the experts say avoid crowded areas, then avoid crowded areas, and live with the comfort of knowing that you are doing all you can to reduce your exposure. However, what if, after a couple of weeks of social isolation , you’ve become a handwashing obsessed hermit, and you still feel anxious? Well…
3. Accept what you cannot control. Focus on what you can do, not what you can’t. There are always going to be variables that are out of your control, and that is part of what makes viruses so frightening. We can never know whether we have been in contact. We can’t control our government’s attempts at containment. We can’t control the loss of income we have experienced or the circumstances that put us back in Nashville.
Sometimes, the healthiest thing we can do is accept that there is nothing we can do. Worrying, complaining, ruminating, and wishing things were different are thoughts we will entertain, but if we focus on them too much, they’ll amplify our stress. Regarding all sorts of stress, I ask people all the time: If there is nothing you can do about it, why are you worried about it? Worrying does nothing but make the problem worse. If you are doing all you can and find that you are still overly focused on things that are outside of your control, you may want to try…
4. Actively changing negative thoughts. Did you know that the only part of your brain you have direct, voluntary control over is the part you think with? If you didn’t, that should be really great news, because it is those very thoughts that are contributing to the anxiety you may be feeling during this pandemic.
What we think influences how we feel, and I often tell people if they don’t like the way they feel to change their thoughts. So, if your brain is too frequently occupied by worries about the virus, anger about social distancing, or sorrow over lost income, then change those thoughts. Simply redirect your attention to a new subject whenever needed. Any new stimulus or activity will help change our thoughts. For example, we could listen to music, do the dishes, read a book, go for a walk, literally anything we can do will help change the channel in our head. This brings me to…
5. Staying active. One thing great about this pandemic is that it is happening during the age of the internet. We may be isolating ourselves physically, but we have an amazing opportunity to connect with others virtually.
Over the last few weeks, I have seen some incredible coping strategies as people in quarantine zones are doing what they can to stay active. I’ve seen videos of opera singers in Italy serenading their neighbors from the windows. There are tango dancers that formed the group “I’m not dancing the tango, so I am doing this instead” to share new hobbies, crafts, and other goofy pursuits. There are people who have started working out or learning to cook.
Painting, making music, or creating art, in general, can be very helpful. A lot of people I know are using this time to catch up on their reading list, and if that sounds appealing, I know a book that would make a great addition to that list. Staying active is great, but we can also work on…
6. Positive thinking . Remember earlier when I mentioned the only part of your brain you have voluntary control over is the part you think with? Another thing worth noting is that you can only hold a few thoughts in mind at any given time. So, if you are having positive, optimistic thoughts, there isn’t much room left for dwelling on negativity.
Monty Python once sang “Always Look on the Bright Side of Life,” and while it may have been played for laughs, but there is truth there. Positive thinking and optimism help us pull through. Not to sound like a blind optimist, but things will absolutely get better. And, speaking of playing things for laughs, don't forget about…
7. Humor . My seminars on stress management are popular because I use a lot of humor in my presentations. In fact, humor is a natural stress-management tool. Coping with and minimizing stress is what humor is for. Laughter relieves anxiety, lowers stress hormones , and helps us to calm down. I can’t tell you how to find humor in your situation, but as much as we can, we need to laugh and just take it easy.
So, work from home if you can, avoid crowds, wash your hands, and try to keep your mind off of the negativity as we all wait this one out. As for us, in the morning, we will be packing up and making our way to stay with family for the next month or so. I don’t know when or if we will be able to tour again, but I am sure we will be OK. Today we hung out with our friend Shawn, who lives in Nashville. Keeping with the protocol of social distancing, Sarah and I refused to talk to him.

Brian King, Ph.D. , trained as a neuroscientist and psychologist and travels the world as a comedian and public speaker. he is the author of The Art of Taking It Easy and The Laughing Cure .
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
- Open access
- Published: 17 May 2022
Stress management in nurses caring for COVID-19 patients: a qualitative content analysis
- Mahboobeh Hosseini Moghaddam ORCID: orcid.org/0000-0002-3381-4559 1 ,
- Zinat Mohebbi ORCID: orcid.org/0000-0003-2995-0264 1 &
- Banafsheh Tehranineshat ORCID: orcid.org/0000-0002-2066-5689 2
BMC Psychology volume 10 , Article number: 124 ( 2022 ) Cite this article
8688 Accesses
9 Citations
2 Altmetric
Metrics details
Being in the frontline of the battle against COVID-19, nurses need to be capable of stress management to maintain their physical and psychological well-being in the face of a variety of stressors. The present study aims to explore the challenges, strategies, and outcomes of stress management in nurses who face and provide care to COVID-19 patients.
The present study is a qualitative descriptive work that was conducted in teaching hospitals affiliated with Shiraz University of Medical Sciences, Iran, from June 2020 to March 2021. Sixteen nurses who were in practice in units assigned to COVID-19 patients were selected via purposeful sampling. Data were collected through semi-structured, individual interviews conducted online. The collected data were analyzed using MAXQDA 10 according to the conventional content analysis method suggested by Graneheim and Lundman.
The data collected in the interviews resulted in 14 subcategories under 4 main categories: providing care with uncertainty and anxiety, facing psychological and mental tension, creating a context for support, and experiencing personal-professional growth.
Conclusions
The nurses caring for COVID-19 patients needed the support of their authorities and families to stress management. Providing a supportive environment through crisis management training, providing adequate equipment and manpower, motivating nurses to achieve psychological growth during the pandemic can help them manage stress.
Peer Review reports
Introduction
Today, COVID-19 is a life-threatening disease all over the world and has become an international concern and a global emergency [ 1 ]. Following the spread of the infection to more than 150 countries and its reaching pandemic proportions, the healthcare personnel, especially nurses, have been in the frontline of providing care to the infected [ 2 ]. The nature of healthcare professions, nursing in particular, involves working in highly stressful conditions [ 3 ]. The results of several studies show that prolonged exposure to stress can cause nurses and other healthcare personnel to suffer such consequences as a reduction in their physical and psychological health, lower job satisfaction, reduced efficiency and quality of care, and an increase in the rate of job burnout [ 2 , 4 ].
The members of healthcare teams, especially nurses, are exposed to many occupational hazards and experience high levels of stress as a result. According to a study, the nurses who cared for severe acute respiratory syndrome (SARS) patients suffered from high levels of psychological distress [ 5 ]. At the height of SARS and Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic, nurses and medical students in Taiwan and Saudi Arabia who cared for the infected showed signs of psychological issues, including anxiety, stress and aggressiveness [ 6 ]. Fear and anger were other distressful emotions experienced by nurses who provided care to MERS-CoV patients in Saudi Arabia [ 7 ].
The results of recent studies show that the healthcare personnel have experienced high levels of anxiety since the outbreak of the COVID-19 pandemic [ 1 , 8 ]. The pandemic also affected the psychological health of a considerable number of healthcare professionals in Spain, so much so that their resilience was at risk in case of another wave of the infection. Severe stress was often caused by fear of being infected and infecting one’s loved ones. These difficult conditions resulted in care providers’ lack of empathy with COVID-19 patients and inconsistency in caring for the patients [ 9 ]. According to another study in South America, many healthcare professionals experienced lack of personal protective equipment (PPE), including gowns, masks, and face shields, during the pandemic. Concern about lack of equipment and fear of being infected were greater in the personnel who were involved in procedures in which aerosols were produced. Some care providers had to use their gowns and N95 masks several times because there was a shortage of protective equipment [ 10 ]. A study by Zhang et al. (2020) in China showed that, in the early stages of caring for COVID-19 patients, nurses were divided between their professional commitment and fear of being infected. The nurses who had been isolated for 1–2 weeks suffered emotional exhaustion; they were able to adapt psychologically after 3–4 weeks of working in isolated wards [ 11 ].
According to studies in Iran, the causes of care providers’ heightened anxiety in caring for COVID-19 patients are fear of being infected, the difficulty of controlling the pandemic and lack of medical equipment [ 1 , 12 , 13 ], death anxiety, the little-known nature of the infection, lack of time, spread of bad news, obsessive thoughts and the public’s disregard for preventive measures [ 14 ]. Another study in Iran reported administrative issues to be the most significant source of stress for nurses who provide care to COVID-19 patients [ 15 ].
Long working hours and work overload, exposure to infection and close contact with COVID-19 patients, the stigma of being a potential carrier of the infection, social media pressures, and increase in the number of death cases lead to fatigue, despair, and helplessness in the nurses and undermine the quality and quantity of nursing care [ 12 ]. Other consequences of job fatigue in nurses are absence, delay, job burnout, and concentration disorders, with adverse effects on patient safety [ 16 , 17 ].
Compared to the other professionals in the healthcare system, nurses spend more time with patients and play a key role in controlling and treating emerging diseases [ 18 ]. Research shows that nurses have experienced higher levels of occupational and psychological stress during the COVID-19 pandemic [ 8 , 17 ]. Nurses’ psychological health correlates with the quality of healthcare services, and occupational stress is one of the most influential factors in the psychological health of this population [ 19 ]. Accordingly, it is necessary to evaluate nurses’ mental health and stress management skills in facing and caring for COVID-19 patients and to identify barriers to their stress management during the current pandemic. Considering the above-mentioned points and the fact that the researchers could not find any studies which investigated nurses’ stress management at the height of the COVID-19 pandemic, a qualitative study could provide an in-depth understanding of the subject in question. Accordingly, the present study uses a qualitative approach to explore the challenges, strategies, and outcomes of stress management in nurses who face and provide care to COVID-19 patients.
Materials and methods
The present study is a qualitative descriptive work of research with a content analysis design which was conducted from June 2020 to March 2021 in teaching hospitals affiliated with Shiraz University of Medical Sciences. The participants of the study were nurses who were in practice in hospitals dedicated to the treatment of COVID-19 patients or back-up hospitals. As the pandemic continued, all the hospitals in Iran had to admit COVID-19 patients; thus, in every hospital, certain wards, including surgical and internal wards, were assigned to the care and treatment of the infected.
In total, 16 nurses who were in practice in special care, internal, surgical and emergency departments were selected via purposeful sampling [ 20 ]. Sampling continued until the data was saturated, i.e. no new knowledge could be obtained and the categories were saturated in terms of characteristics and dimensions. The researchers reached data saturation after 14 interviews. However, two more interviews were conducted to verify data saturation. Analysis of the last two interviews did not yield any new codes. The research team and two qualitative research experts examined the codes to verify that the data were saturated.
The inclusion criteria were: having a bachelor’s degree in nursing, having at least six months’ experience of full-time practice as a clinical nurse, having at least 2 weeks’ experience of caring for COVID-19 patients, and willingness to share one’s experiences with the researchers. The subjects who were not willing to be interviewed or continue their participation in the study were excluded. Data were collected through 16 in-depth, semi-structured, individual interviews which were conducted by the third author.
The participants were interviewed by video calls with “WhatsApp”, in workplace (one of the classes at school of nursing and midwifery), after arrangements about the time of the interviews had been made with them. Each interview lasted from 40 to 60 min and began with a general question: “Can you describe your experiences of a work shift in which you faced or cared for a COVID-19 patient?” Subsequently, the interviewer asked more specific questions: “What are your experiences of the challenges and barriers to stress management when you faced and cared for COVID-19 patients?”, “What factors improve stress management when nurses face and care for COVID-19 patients?”, “What factors undermine stress management when nurses face and care for COVID-19 patients?”, “How did you feel when/if you could not manage your stress when you faced and cared for COVID-19 patients?”, “What stress management strategies can help nurses who face and care for COVID-19 patients?” and “What are the outcomes of stress management for nurses who face and care for COVID-19 patients?” Moreover, follow-up questions were asked to obtain more details about the objective of the study (Additional file 1 : Interview Guide). The participants' voices were recorded using a Sony Voice Recorder ICD-TX650.
The present study used the conventional content analysis method suggested by Graneheim and Lundman (2004). Frequently used in studies related to nursing, this method allows for collecting new, rich information and mental analysis of the content of textual data through systematic categorization, codification and theme making or developing known paradigms [ 21 , 22 ]. Each interview was transcribed in full immediately after it was completed. To immerse in the data and obtain a general idea of the participants’ answers, the researchers read the transcripts several times. Words, phrases and paragraphs which carried significance with regard to the challenges, strategies and outcomes of stress management in the COVID-19 crisis were selected as meaning units. Similar initial codes were classified into broader categories based on their similarities and differences and categories were thus developed. To ensure that the codes were consistent, the researchers reviewed the categories and compared them to the data again. Afterward, through deep and accurate contemplation and comparison of the categories against each other, the themes emerged [ 23 ]. The data were organized using MAXQDA 2010 distributed by VERBI.
The trustworthiness of the collected data was ensured using Lincoln and Guba’s criteria [ 24 ]. Credibility was achieved through prolonged engagement with the data, member checking, peer debriefing, maximum variation sampling, and searching for contrasting evidence. To ensure dependability and confirmability, the researchers relied on audit trial which consists of using proper techniques to conduct interviews, making accurate transcripts and having the data reviewed by one’s co-researchers. To enhance the transferability of the results, the researchers provided accurate and thorough descriptions of the subject under study, the participants’ characteristic, methods of data collection and analysis, along with documented examples of the participants’ statements [ 25 ].
The participants’ ages ranged from 25 to 48 years, with the mean being 34.93 years. The majority of the participants were female (Table 1 ). Analyses of the data resulted in 510 initial codes, 14 subcategories and four main categories, namely: providing care with uncertainty and anxiety, facing psychological and mental tension, creating a context for support, and experiencing personal-professional growth (Table 2 ). Table 3 presents an example of meaning units, coding, and development of sub-categories and categories. Providing care with uncertainty and anxiety and facing psychological and mental tension were the challenges which the nurses in the present study experienced when they faced and cared for patients with COVID-19.
Providing care with uncertainty and anxiety
One of the findings of the present study was providing care with uncertainty and anxiety. This category consisted of the subcategories of providing care as a professional duty, concern over transmitting the infection to one’s family, fear of the unknown aspects of the disease, and concern over making wrong decisions.
Providing care as a professional duty
According to the participants’ experiences, despite a lack of facilities and personal protective equipment, there was a dominant sense of commitment among nurses to perform their professional duties in the COVID-19 pandemic. From the nurses’ point of view, working in difficult and dangerous conditions is part of a nurse’s job which must be maintained during the pandemic of an emerging disease.
“… anyway, it’s my job to give care in all circumstances and I had to do it at that time …” (P1).
According to another participant:
“…I volunteered to work in the COVID-19 ward … I thought to myself, ‘This is my job and my duty …” (P15).
Concern over transmitting the infection to one’s family
Despite their commitment to perform their professional duties, the nurses in the present study were worried about transmitting the infection to their families and their concern acted as a barrier to their stress management. The participants also mentioned that when their colleagues were infected, the fear of contracting the disease in the near future was a barrier to their stress management.
“… I was really worried that I could be the source of infection to my 60-year-old parents …” (P6).
Fear of the unknown aspects of the disease
One of the major barriers to stress management in the face of COVID-19 was lack of knowledge about the nature of the infection. Fear of the personnel arising from the unknown aspects of the disease was a main source of stress.
“… We didn’t know anything about it. The disease was completely unknown to us …” (P 3).
Concern over making wrong decisions
Some of the nurses were working in COVID-19 units voluntarily; however, they admitted that they had felt doubtful about their decision to provide voluntary care to COVID-19 patients in the first few days.
“… I kept wondering if my decision was right or not …” (P 4).
Another nurse stated that:
“…Maybe the decision I made was a step to fulfill my personal commitment …” (P 2).
Facing psychological and mental tension
Many of the nurses who were working in COVID-19 units declared that they had experienced a variety of psychological issues during their practice in these units which prevented them from managing their stress. This category consisted of the sub-categories of families’ insistence on quitting one’s job, working in difficult conditions, lack of personal protective equipment, and feeling rejected.
Families’ insistence on quitting one’s job
One of the sources of psychological tension for the nurses was the insistence of some of their family members that they should quit their profession as nurses during the pandemic.
“…My dad was strongly against me staying in this profession at those critical times …” (P 3).
Working in difficult conditions
Many of the participants described working in personal protective gear as very difficult. They also referred to work fatigue and physical exhaustion due to work overload as barriers to stress management.
“…When your shift is over, you can barely breathe; with a high PaCO2, it’s hard to breathe … it’s hard to eat in this coverall, you can’t drink any water through your shift … the fatigue …. Working in such conditions won’t let you manage stress…” (P 12).
According to another nurse:
“…Our workload has increased at these stressful times caused by the pandemic; my life and my family’s life have been affected … it’s not easy to work with all this protective gear on … Such things as fogging of my face shield interfered with my job … I was exhausted, both physically and emotionally…” (P16).
Lack of personal protective equipment
The participants stated that one of the major barriers to stress management was lack of personal protective equipment and coveralls, especially in the first few days of the pandemic. According to one of the nurses:
“…When the epidemic started, we didn’t have access to special gear for COVID-19 protection and had to care for the infected with minimum equipment, in regular masks and uniforms …” (P 5).
Feeling rejected
Another barrier to stress management in COVID-19 units was being treated inappropriately and rejected by the personnel in non-COVID-19 units. One of the participating nurses stated that:
“…When I got on the hospital shuttle, I felt so nervous. All the other staff that didn’t work in COVID-19 units would protest and tell the driver that he shouldn’t let me get on board … I should get off ….” (P 7).
Some of the participants had experienced rejection by their family members and relatives, which made it more difficult for them to manage stress.
“…Once, when one of my relatives saw me, she took her son’s hand and walked away from me …” (P 3).
Creating a context of support
In the present study, the participants believed that creating a context of support is an important stress management strategy in facing and caring for COVID-19 patients. This category consists of the subcategories of proper intradepartmental management, support of the authorities, and effective communication skills.
Proper intradepartmental management
The participants’ experiences showed that proper intradepartmental management, e.g. planning according to the personnel’s conditions, replacing COVID-19 personnel with volunteers, avoiding discrimination, playing soft music in the units, and using effective interpersonal communication skills, including empathy, humor and spreading positive thinking, can contribute to the personnel’s stress management. During the COVID-19 crisis, the unit managers tried to make plans according to the personnel’s conditions in order to reduce the personnel’s stress.
“…The husband of one of my staff here could spend two weeks a month with his wife …. I arranged her shifts so she didn’t have to work or worked less when her husband was with her so she wouldn’t be so worried about infecting her husband …” (P 1).
To reduce nurses’ direct contact with COVID-19 patients, the unit managers put the overstressed nurses in charge of recording patients’ history in their files in order to reduce stress in them.
“…One of my staff was stressed out …. I made her the shift supervisor so she would be busy with the patients’ files and have less direct contact with the patients …” (P 8).
Support of the authorities
In order to support the nurses by helping them manage their stress, the unit and hospital authorities arranged certain hours for the nurses to meet with the hospital counselor or for the counselor to see the nurses.
“…Whenever the personnel felt they were suffering from psychological tension and needed counseling, they could visit the hospital counselors ….” (P 11).
Another strategy used by the authorities to help the nurses manage their stress was setting up workshops to inform the nurses about the pathophysiology of COVID-19, how the infection is transmitted, the correct use of personal protective equipment, and regimens that boost the immune system. This information proved very influential in reducing stress in the nurses.
“…We didn’t have any preparation from before; education is really important; once we learned more about the disease, we could protect ourselves better …. We were less stressed …” (P 12).
According to the participants, continuing education was integral to enabling them to manage the stress caused by being in contact with COVID-19 patients. Even though the presence of the supervisors and the other members of the treatment team in the environment could communicate a sense of support and hope to the nurses, some of the supervisors refused to be present in the places where the patients were being cared for.
“…Our supervisor won’t even enter the unit to see for herself what kind of issues we are dealing with here …” (P 9).
Effective communication skills
The head nurses’ use of effective communication skills in their interactions with the staff was found to be a successful approach to stress management in those critical times. In addition, through empathy, the unit personnel tried to connect to their colleagues’ inner worlds and have a mutual understanding of their emotions and concerns, thereby coping with the stress caused by the COVID-19 crisis. The participants stated that in an empathetic relationship, they could experience a sense of support.
Showing appreciation and giving rewards were found to be effective stress management strategies which could raise the personnel’s spirits and improve interpersonal relationships. According to one of the participants:
“…One of the main issues for the nurses who are doing a good job in these units is not receiving any appreciation or rewards. There is a limit to any person’s tolerance. Some turn to spirituality for strength, but not everyone is spiritual. In short, there is a lack of appreciation …” (P 5).
Other behaviors which contributed to the nurses’ stress management were exchanging friendly banters with each other, spreading positive thinking, and remaining optimistic about the future.
Experiencing personal-professional growth
The participants referred to experiencing personal-professional growth as one of the outcomes of working in the very difficult conditions created by the spread of COVID-19. Caring for COVID-19 patients was a constructive experience which could prove instrumental in coping with problems in the future. Making an effort to use various stress management skills in the face of COVID-19 improved nurses’ empowerment and gave them a chance for personal growth. Compared to the time before the emergence of COVID-19, nurses can focus on their problems better and manage stress and stressors more effectively. This category consists of the subcategories of improved learning, perception of positive feelings at the end of a crisis, and self-transformation.
Improved learning
The participants believed that, despite all the difficulties, working during the pandemic had resulted in their gaining useful knowledge. Their experiences showed that providing care during the COVID-19 pandemic had helped them develop time management skills, learn to make optimal use of the available equipment and deal with deficiencies, improve their medication knowledge, increase their knowledge of emerging diseases, and learn to make effective use of infection control strategies.
“…I had read a few things about emerging diseases, but working in this pandemic has given me the chance to gain hands-on experience of caring for these patients …” (P 7).
Perception of positive feelings at the end of a crisis
While providing care to COVID-19 patients, the participants had experienced such positive feelings and emotions as elevated self-confidence, personal satisfaction, the opportunity to prove their competence, and the good feeling of overcoming the difficulties and challenges of caring for COVID-19 patients.
“…Working in these conditions created a positive sense of being useful to others in me … which made me feel happy and lively and physical fatigue could not take away my happiness …” (P 6).
Many of the participants mentioned feeling good about solving problems and happiness about serving one’s fellowmen to be among other outcomes of working in the COVID-19 crisis.
“…Having been put on the path to serve my fellowmen was the positive feeling that I experienced …” (P 4).
Another participant stated:
“…I feel happy now that I could live through the problems I had at the time …” (P 12).
Self-transformation
The results of the study showed that the experience of caring for COVID-19 patients in difficult conditions had strengthened relationships between colleagues and between friends at work. Many of the participants had come to have higher regard for the meaning and value of their lives and what they had. The participants compared working in the COVID-19 crisis to fighting in a war which had transformed them by making them braver in the face of critical conditions and more empowered in managing difficult times.
“…Working during the current pandemic has helped me discover my abilities …. Now I know how to act in war conditions …” (P 7).
The present study was conducted to identify the challenges, strategies and outcomes of stress management for nurses who come into contact with and provide care to COVID-19 patients. Analyses of the collected data showed that the nurses’ experiences could be classified into four categories: providing care with uncertainty and anxiety, facing psychological and mental tension, creating a context for support, and experiencing personal-professional growth.
One of the findings of the present study was nurses’ feelings of uncertainty and anxiety in providing care. The nurses were worried about transmitting the infection to their family members, were not adequately aware of the nature of the disease, and were in fear of making wrong decisions about caring for COVID-19 patients; yet, they deemed it their professional duty to provide care to those patients. In another study, the nurses were worried about facing patients with COVID-19, contracting the infection and transmitting it to their loved ones. The nurses were also concerned about the unknown aspects of the disease and its potentially dangerous nature, uncertainty about the end of the pandemic, and the impact of the pandemic on their job security and other working conditions [ 26 ]. Another study reported that the healthcare personnel suffered psychosocial issues, e.g. depression, anxiety, and stress, as a result of having inadequate knowledge about COVID-19, continuously caring for the infected, work overload, frequent exposure to distressful events, such as death, and fear of infecting their families [ 27 ]. In yet another study, the nurses suffered from stress due to caring for the infected and work overload, which resulted in their experiencing burnout, emotional fatigue, and despair [ 28 ]. De Kock et al. found that, the COVID-19 crisis had an impact on the nurses’ mental health and increased their anxiety, stress, and sleep difficulties. The occupational, psychosocial, and environmental risk factors associated with adverse mental health outcomes during the COVID-19 pandemic identified through their study [ 29 ]. The frontline healthcare workers commonly reported increased workloads, which impacted on their psychosocial health. The healthcare workers reported increased hours and weekend shifts, additional time taken to manage PPE and staff shortages as frequent sources of stress. However, because of staff shortages, some nurses described feeling guilty for taking time off to rest [ 30 ].
Several studies suggest long-distance psychological interventions, including video conferencing, online programs, applications, and even telephone calls, to help care providers cope with their anxiety [ 31 , 32 ]. In China, Internet-based programs are used to screen and identify individuals who are prone to psychological disorders and to provide self-learning protocols and guidelines to the healthcare personnel and the general public in the form of videos and pamphlets [ 33 ]. During a pandemic, digital interventions should be used to address anxiety, depression, self-torture, and suicide, as well as to gather information, perform triage and introduce medical interventions via online applications or phone calls and text messaging for those with limited access to digital sources [ 34 , 35 ]. Measures, such as workshops and counseling with a psychologist, should be taken to decrease stress and anxiety in nurses who are directly involved in caring for COVID-19 patients as prolonged anxiety can lead to psychological distress, depression and other psychological issues.
Another finding of the present study was nurses’ exposure to mental and psychological tension which originated from the insistence of their families that they should quit their jobs, feeling rejected, witnessing the death of their colleagues and friends, fear of infecting their families, lack of medical equipment, and fatigue. According to one study, the major contributory factors in the psychological pain of nurses, doctors, therapists and other healthcare professionals were the emotional efforts and physical fatigue that they experienced in caring for COVID-19 patients whose conditions were deteriorating quickly. Seeing and caring for colleagues who were severely infected or lost their lives to COVID-19, lack of ventilators and other medical equipment needed to care for patients in critical conditions, and anxiety due to new clinical roles and work overload were other causes of psychological distress [ 36 ].
As a result of social stigmatization, the nurses suffered from social dejection and loneliness. They preferred to be isolated because they were afraid that they might transmit the infection to others [ 37 ]. Another study reported that frequent changes in the hospital policies, routines, and guidelines which were updated confused the nurses [ 38 ]. In another study, the participants reported work overload as a result of lack of medical protective equipment: the nurse managers had to reduce the number of care providers to ensure that all the personnel had access to protective equipment by conserving it. Moreover, to avoid going to break rooms during working hours, the healthcare professionals did not eat anything, and they experienced severe emotional distress and grief if their patients passed away [ 39 ]. During the COVID-19 pandemic, nurses were exposed to so many psychological issues that they sometimes had to resign [ 40 ].
According to Maslow's hierarchy of needs, physiological and safety needs are two of the basic and essential needs of mankind. If these needs are satisfied in them, nurses can experience self-esteem, love and self-actualization and, consequently, meet other individuals’ needs without feelings of exhaustion or burnout. Thus, authorities and governments should decrease the physical and mental pressure caused by the COVID-19 pandemic by creating an appropriate work environment, supplying adequate PPE, managing work shifts effectively, and considering the physical and mental health of nurses [ 12 ]. Support interventions, including informing the public about the pandemic and self-quarantine, providing enough resources to meet the basic needs of nurses in quarantine, and giving nurses easy access to social media so that they can be in touch with their friends and families can encourage nurses to stay in their jobs [ 37 ]. Also, counseling the personnel and preparing them for the challenges in their profession and giving a clear picture of what they are going to face can prove helpful [ 41 ].
Research findings show that mental health interventions for the time of the pandemic, including crisis management, education in resilience, improvement in quality of life and life satisfaction, confrontational strategies, education via guidelines and protocols, screening programs and long-distance Internet-based interventions, are effective methods to manage the psychological consequences of the pandemic for nurses [ 42 , 43 ]. Strategic support and planning across the country and arranging for psychological first aid during crises which are potentially offered by telemedicine are among the interventions which must be employed. In addition, comprehensive plans should be developed to reduce mental pressure on nurses through prevention and intervention, e.g. screening and purposeful visits, to avoid further mental health issues in this population [ 44 , 45 ]. Educational programs about death anxiety can result in better nursing care in critical situations. Educational workshops are effective in reducing death anxiety [ 14 ]. Giving nurses active guidance and motivating them to achieve psychological growth during the pandemic can contribute to their psychological adaptation [ 46 ].
Another finding of the present study was the role of creating a context of support. The participants’ experiences showed that intradepartmental management, support of the authorities, and effective communication skills are effective ways to support nurses in the stressful conditions caused by the pandemic. A context of support will reduce nurses’ anxiety and help them continue to provide quality healthcare services in the crisis. According to one study, personal resilience protects nurses from anxiety by enabling them to adapt to irritating, stressful conditions. In addition, public support for nurses plays a significant role in their achieving positive emotional states in stressful times, such as the outbreak of a disease [ 47 ]. In another study, the nurses practiced self-isolation as a protection strategy [ 38 ]. The nurses believed that one of the greatest challenges in their workplace during the pandemic was lack of a crisis management plan on the management and ministry of healthcare levels [ 48 ]. In Billings et al. study working with coworkers during the pandemic was considered to provide an important source of mutual support and opportunities to learn from each other. The employees reported feeling supported by their organizations when there was a clear alliance and shared decision making between senior managers and frontline healthcare workers [ 30 ].
The experiences of the nurses and doctors in another study showed that one way to prevent the physical and emotional exhaustion caused by working in special care units is using educational interventions to develop resilience in the personnel. Also, regular and systematic educational programs designed to improve the healthcare personnel’s preparation and efficacy in crisis management seemed essential [ 49 ]. Healthcare professionals were also found to rely on self-management mechanisms. They preferred to focus on their work rather than listen to rumors about COVID-19. Some of the other personnel engaged in relaxation activities, including seeing movies, taking showers, and reading. They also stressed the significance of good nutrition and adequate rest and sleep [ 39 ].
Moreover, stress management approaches, including relaxation, biofeedback, cognitive strategies, interventions focused on eliminating or decreasing stressful working conditions, such as job redefinition and clear job description, formation of joint personnel committees, and increasing the personnel’s participation in organizational decisions are essential to controlling stressful conditions [ 50 ]. One support strategy for the personnel in the frontline of caring for patients with COVID-19 is providing them with online psychological support services which enable the personnel to express their needs. Access to mental health care is possible through telemedicine managed by mental health experts, mobile phone applications, online sources, and virtual peer support. Online psychological care networks are useful in dealing with the stress and concerns of healthcare professionals and their families and relatives and other individuals [ 51 ]. One study classifies nurse managers’ experiences of management of the nursing workforce during the COVID-19 crisis into management of workforce recruitment (volunteers and non-volunteers) and management of workforce (via motivational measures and psychological support). Successful crisis management depends on using flexible and situation-based principles of management toward recruiting adequate workforce and retaining the current workforce [ 52 ]. By creating a pleasant work environment, encouraging colleague support, and raising trust in the personnel, nurse managers can improve nurses’ stress management skills. Nurse managers play a key role in the promotion of inter-professional relationships in clinical environments, which can contribute to nurses’ mental health [ 11 ]. Providing a supportive environment through crisis management training, providing adequate equipment and manpower, and developing resilience skills in staff helps nurses manage stress.
Another finding of the present study was the nurses’ experiencing personal and professional growth. This theme consisted of the subcategories of improved learning, perception of positive feelings at the end of a crisis, and self-transformation. According to a study, one of the psychological experiences of the nurses who cared for COVID-19 patients was perception of growth under pressure and appreciation of life. The nurses declared that, in the pandemic, the picture of the nursing profession had improved, nurses had realized their potential, and nurses’ ability to cope with difficulties in life had elevated [ 46 ]. Another study reported an increase in nurses’ self- esteem and sense of responsibility during the pandemic [ 39 ]. One of the significant experiences of new nurses was learning during the pandemic. The nurses stated that caring for COVID-19 patients gave them a chance to develop their clinical skills, gain hands-on clinical experience, and learn how to adapt to critical conditions. They also learned methods of protecting themselves, using the equipment needed in caring for COVID-19 patients, time management, and providing care in the shortest possible time to minimize contact with the infected [ 53 ]. Another study reported an increase in nurses’ awareness about the value of the nursing profession and their sense of achievement and pride. Moreover, the nurses had a better perception of their professional and social identity and established stronger relationships with their colleagues. Many of the nurses had a greater appreciation of life and everything which they had. The pandemic had given them a chance to realize their full potential, which, in turn, increased their self-confidence. In addition, by self-reflection, the nurses discovered their weaknesses and tried to develop their knowledge and skills. They appreciated the support of their friends, colleagues and the society and developed a more positive perspective on the significance of life and family health [ 54 ].
Appreciating life and experiencing increased self-power are the characteristics of post-traumatic growth which may emerge in individuals following a stressful experience. As a result of cognitive reconstruction after trauma, individuals experience personal vulnerability and come to believe that they are not capable of predicting and controlling certain events in life. In response to the unstable nature of life, individuals reconsider the little things in life which used to be important or unimportant to them, which in turn, results in their changing their priorities in life and having a deeper apperception of life [ 55 ]. The results of studies show that projecting a positive image of the nursing profession in the society helps nurses find their potential, improves nurses’ professional knowledge and skills in the epidemic of emerging diseases, and increases nurses’ awareness of their personal and professional growth and professional identity by extension.
As the main strength of this study, we conducted one of the qualitative studies that explored strategies and outcomes of stress management based on experiences of the nurses who provide directly care to COVID-19 patients. One of the limitations of the present study was the fact that, because of the COVID-19 pandemic, the interviews were not conducted on a face-to-face basis. However, the researchers tried to have a better interaction with the participants by making video calls to them. Another limitation of the study was that the interviews were conducted individually. Focus group interviews allow for the collection of richer information.
Despite the fact that the nurses in the present study regarded caring for COVID-19 patients as their professional duty, they needed the support of their superiors, families, and friends. Authorities can create an effective context of support through proper intradepartmental management, providing adequate equipment, giving positive feedback, and organizing continuing workshops. In addition, effective communication skills, receiving positive feedback and easy access to counselors can contribute to nurses’ stress management and adaptation. The outcomes of stress management on the part of nurses were found to include understanding the meaning of life and experiencing personal and professional growth. It is suggested that future studies address the causes of barriers to nurses’ stress management in the COVID-19 crisis and the strengths and weaknesses of the healthcare system in dealing with this pandemic. It is also suggested that future research address the lived experiences of change in the performance and behaviors of care providers who care for COVID-19 patients.

Availability of data and materials
The dataset generated and/or analysed during the current study are not publicly available due to promises of participant anonymity and confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
Coronavirus infection disease-19
Severe Acute Respiratory Syndrome
Middle East respiratory syndrome coronavirus
Personal protective equipment
Khoshnood Z, Mehdipour-Rabori R, Nazari Robati F, Helal Birjandi M, Bagherian S. Patients’ experiences of living with coronavirus disease 2019: a qualitative study. Evid Based Care J. 2021;11(1):44–50.
Google Scholar
Fathi Ashtiani A, Pirzadi H, Shokoohi-Yekta M, Tavallai S. The influence of teaching program of stress management and communication skills on improvement of mental health of nurses and hospital staff: an experimental study. Iran J Nurs. 2014;27(90):1–13. https://doi.org/10.29252/ijn.27.90.91.1 .
Article Google Scholar
Rose S, Hartnett J, Pillai S. Healthcare worker’s emotions, perceived stressors and coping mechanisms during the COVID-19 pandemic. PLoS One. 2021;16(7):e0254252.
Li X, Jiang T, Sun J, Shi L, Liu J. The relationship between occupational stress, job burnout and quality of life among surgical nurses in Xinjiang, China. BMC Nurs. 2021;20(1):1–1. https://doi.org/10.1186/s12912-021-00703-2 .
Park J-S, Lee E-H, Park N-R, Choi YH. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: a cross-sectional study. Arch Psychiatr Nurs. 2018;32(1):2–6. https://doi.org/10.1016/j.apnu.2017.09.006 .
Article PubMed PubMed Central Google Scholar
Al-Rabiaah A, Temsah MH, Al-Eyadhy AA, Hasan GM, Al-Zamil F, Al-Subaie S, Alsohime F, Jamal A, Alhaboob A, Al-Saadi B, Somily AM. Middle East Respiratory Syndrome-Corona Virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J Infect Public Health. 2020;13(5):687–91. https://doi.org/10.1016/j.jiph.2020.01.005 .
Abolfotouh MA, AlQarni AA, Al-Ghamdi SM, Salam M, Al-Assiri MH, Balkhy HH. An assessment of the level of concern among hospital-based health-care workers regarding MERS outbreaks in Saudi Arabia. BMC Infect Dis. 2017;17(1):1–10. https://doi.org/10.1186/s12879-016-2096-8 .
Mohammadi F, Farjam M, Gholampour Y, Tehranineshat B, Oshvandi K, Bijani M. Health professionals’ perception of psychological safety in patients with coronavirus (COVID-19). Risk Manag Healthc Policy. 2020;13:785. https://doi.org/10.2147/RMHP.S261410 .
Mira JJ, et al. Acute stress of the healthcare workforce during the COVID-19 pandemic evolution: a cross-sectional study in Spain. BMJ Open. 2020;10(11):e042555. https://doi.org/10.1136/bmjopen-2020-042555 .
Article PubMed Google Scholar
Martin-Delgado J, Viteri E, Mula A, Serpa P, Pacheco G, Prada D, de Andrade C, Lourenção D, Campos Pavan Baptista P, Ramirez G, Mira JJ. Availability of personal protective equipment and diagnostic and treatment facilities for healthcare workers involved in COVID-19 care: a cross-sectional study in Brazil, Colombia, and Ecuador. PLoS One. 2020;15(11):e0242185. https://doi.org/10.1371/journal.pone.0242185 .
Zhang Y, Wei L, Li H, Pan Y, Wang J, Li Q, Wu Q, Wei H. The psychological change process of frontline nurses caring for patients with COVID-19 during its outbreak. Issues Ment Health Nurs. 2020;41(6):525–30. https://doi.org/10.1080/01612840.2020.1752865 .
Ahmadidarrehsima S, Salari N, Dastyar N, Rafati F. Exploring the experiences of nurses caring for patients with COVID-19: a qualitative study in Iran. BMC Nurs. 2022;21(1):1–7. https://doi.org/10.1186/s12912-022-00805-5 .
Mohammadi F, Tehranineshat B, Bijani M, Khaleghi AA. Management of COVID-19-related challenges faced by EMS personnel: a qualitative study. BMC Emerg Med. 2021;21(1):1–9. https://doi.org/10.1186/s12873-021-00489-1 .
Galehdar N, Kamran A, Toulabi T, Heydari H. Exploring nurses’ experiences of psychological distress during care of patients with COVID-19: a qualitative study. BMC Psychiatry. 2020;20(1):1–9. https://doi.org/10.1186/s12888-020-02898-1 .
Raesi R, Abbasi Z, Saghari S, Bokaie S, Raei M, Hushmandi K. Evaluation of factors affecting job stress in nurses caring for COVID-19 patients. J Mar Med. 2021;3(4):80–8.
Sikaras C, Ilias I, Tselebis A, Pachi A, Zyga S, Tsironi M, Gil AP, Panagiotou A. Nursing staff fatigue and burnout during the COVID-19 pandemic in Greece. AIMS public health. 2022;9(1):94. https://doi.org/10.3934/publichealth.2022008 .
Amiri A, Rashnuodi P, Mousavi S, Shadian KL. Investigating the level of job stress in nurses exposed to COVID-19 in educational hospitals in Ahvaz. J Occup Hyg Eng. 2021;8(2):58–65.
Abbaszadeh A, Ehsani SR. Nurse perceptions of caring of emerging avian influenza disease. Nurs Midwifery J. 2015;12(11):973–81.
Sultan S, Bashar A, Nomani I, Tabassum A, Iqbal MS, Fallata EO, Sindi RA, Almasoudi NM, Rheem S. Impact of COVID-19 pandemic on psychological health of a sample of the health care workers in the western region of Kingdom of Saudi Arabia. Middle East Curr Psychiatry. 2022;29(1):1–11. https://doi.org/10.1186/s43045-022-00174- .
Holloway I, Galvin K. Qualitative research in nursing and healthcare. New York: Wiley; 2016.
Krippendorff K. Content analysis: an introduction to its methodology. Thousand Oaks: Sage Publications; 2018.
Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. https://doi.org/10.1111/j.1365-2648.2007.04569.x .
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. https://doi.org/10.1016/j.nedt.2003.10.001 .
Grove SK, Gray JR. Understanding nursing research e-book: building an evidence-based practice. Amsterdam: Elsevier Health Sciences; 2018.
Speziale HS, Streubert HJ, Carpenter DR. Qualitative research in nursing: advancing the humanistic imperative. Philadelphia: Lippincott Williams & Wilkins; 2011.
Arnetz JE, Goetz CM, Arnetz BB, Arble E. Nurse reports of stressful situations during the COVID-19 pandemic: qualitative analysis of survey responses. Int J Environ Res. 2020;17(21):8126. https://doi.org/10.3390/ijerph17218126 .
Carbajal AB, Boluarte AS, Boluarte AR, Soto CM. Working conditions and emotional impact in healthcare workers during COVID-19 pandemic. J Healthc Qual. 2020. https://doi.org/10.1016/j.jhqr.2020.08.002 .
Ali H, et al. Major stressors and coping strategies of frontline nursing staff during the outbreak of coronavirus disease 2020 (COVID-19) in Alabama. J Multidiscip Healthc. 2020;2020(13):2057. https://doi.org/10.2147/JMDH.S285933 .
De Kock JH, Latham HA, Leslie SJ, Grindle M, Munoz SA, Ellis L, Polson R, O’Malley CM. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):1–8. https://doi.org/10.1186/s12889-020-10070-3 .
Billings J, Ching BC, Gkofa V, Greene T, Bloomfield M. Experiences of frontline healthcare workers and their views about support during COVID-19 and previous pandemics: a systematic review and qualitative meta-synthesis. BMC Health Serv Res. 2021;21(1):1–7. https://doi.org/10.1186/s12913-021-06917-z .
Priede A, López-Álvarez I, Carracedo-Sanchidrián D, González-Blanch C. Mental health interventions for healthcare workers during the first wave of COVID-19 pandemic in Spain. Rev Psiquiatr Salud Ment. 2021;14(2):83–9. https://doi.org/10.1016/j.rpsm.2021.01.005 .
Article PubMed Central Google Scholar
Lai J, Ma S, Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976–e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 .
Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, Cheung T, Xiang YT. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. 2020;16(10):1732. https://doi.org/10.7150/ijbs.45120 .
Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, Ballard C, Christensen H, Silver RC, Everall I, Ford T. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–60. https://doi.org/10.1016/S2215-0366(20)30168-1 .
Shahed Hagh Ghadam H, Fathi Ashtiani A, Rahnejat AM, Ahmadi Tahour Soltani M, Taghva A, Ebrahimi MR, et al. Psychological consequences and interventions during the COVID-19 pandemic: narrative review. J Mar Med. 2020;2(1):1–11.
Ayanian JZ. Mental health needs of health care workers providing frontline COVID-19 care. JAMA Health Forum. 2020;1(4):e200397–e200397. https://doi.org/10.1001/jamahealthforum.2020.0397 .
Kackin O, Ciydem E, Aci OS, Kutlu FY. Experiences and psychosocial problems of nurses caring for patients diagnosed with COVID-19 in Turkey: a qualitative study. Int J Soc Psychiatry. 2020. https://doi.org/10.1177/0020764020942788 .
Lam KK, Hung SYM. Perceptions of emergency nurses during the human swine influenza outbreak: a qualitative study. Int Emerg Nurs. 2013;21(4):240–6. https://doi.org/10.1016/j.ienj.2012.08.008 .
Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, et al. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health. 2020;8(6):e790–8. https://doi.org/10.1016/S2214-109X(20)30204-7 .
Ohue T, Togo E, Ohue Y, Mitoku K. Mental health of nurses involved with COVID-19 patients in Japan, intention to resign, and influencing factors. Medicine. 2021. https://doi.org/10.1097/MD.0000000000026828 .
Chandra A, Vanjare H. Coping by the healthcare workers during COVID-19 pandemic in developing countries—a review. Pain Intensive Care. 2020;24(3):346–53.
Bozdağ F, Ergün N. Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychol Rep. 2021;124(6):2567–86. https://doi.org/10.1177/0033294120965477 .
Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, Zhuang Q. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med Sci Monit. 2020;26:e924171–81. https://doi.org/10.12659/MSM.924171 .
Sarboozi Hosein Abadi T, Askari M, Miri K, Namazi Nia M. Depression, stress and anxiety of nurses in COVID-19 pandemic in Nohe-Dey Hospital in Torbat-e-Heydariyeh city, Iran. Mil Med. 2020;22(6):526–33.
Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, Smith AC. The role of telehealth in reducing the mental health burden from COVID-19. Telemed E-Health. 2020;26(4):377–9. https://doi.org/10.1089/tmj.2020.0068 .
Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control. 2020;48(6):592–8. https://doi.org/10.1016/j.ajic.2020.03.018 .
Labrague LJ, De Los Santos JAA. COVID-19 anxiety among front-line nurses: predictive role of organisational support, personal resilience and social support. J Nurs Manag. 2020;28(7):1653–61. https://doi.org/10.1111/jonm.13121 .
Koh Y, Hegney D, Drury V. Nurses’ perceptions of risk from emerging respiratory infectious diseases: a Singapore study. Int J Nurs Pract. 2012;18(2):195–204. https://doi.org/10.1111/j.1440-172X.2012.02018.x .
Zakeri MA, Dehghan M. The role of continuing education in protecting nurses against COVID-19 infection. J Occup Health. 2021;10(2):64–6.
Roberts RK, Grubb PL. The consequences of nursing stress and need for integrated solutions. Rehab Nurs. 2014;39(2):62–9. https://doi.org/10.1002/rnj.97 .
Teixeira CFDS, Soares CM, Souza EA, Lisboa ES, Pinto ICDM, Andrade LRD, et al. The health of healthcare professionals coping with the Covid-19 pandemic. Cien Saude Colet. 2020;25:3465–74. https://doi.org/10.1590/1413-81232020259.19562020 .
Poortaghi S, Shahmari M, Ghobadi A. Exploring nursing managers’ perceptions of nursing workforce management during the outbreak of COVID-19: a content analysis study. BMC Nurs. 2021;20(1):1–10. https://doi.org/10.1186/s12912-021-00546-x .
Casafont C, Fabrellas N, Rivera P, Olivé-Ferrer MC, Querol E, Venturas M, et al. Experiences of nursing students as healthcare aid during the COVID-19 pandemic in Spain: a phemonenological research study. Nurse Educ Today. 2021;97:104711. https://doi.org/10.1016/j.nedt.2020.104711 .
Cui S, Zhang L, Yan H, Shi Q, Jiang Y, Wang Q, et al. Experiences and psychological adjustments of nurses who voluntarily supported COVID-19 patients in Hubei Province, China. Psychol Res Behav Manag. 2020;13:1135. https://doi.org/10.2147/PRBM.S283876 .
Tehranineshat B, Torabizadeh C. Posttraumatic growth: an analysis of the concept based on Rodgers’ concept development. J Relig Health. 2021;60(4):2728–44. https://doi.org/10.1007/s10943-020-01144-y .
Download references
Acknowledgements
The present article is the result of a research project registered at Shiraz University of Medical Sciences (No. 19757). The authors would like to thank the authorities and nurses of the hospitals affiliated with Shiraz University of Medical Sciences who participated in the study.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and affiliations.
Department of Nursing, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran
Mahboobeh Hosseini Moghaddam & Zinat Mohebbi
Community Based Psychiatric Care Research Center, School of Nursing and Midwifery, Shiraz University of Medical Sciences, Shiraz, Iran
Banafsheh Tehranineshat
You can also search for this author in PubMed Google Scholar
Contributions
MHM has made a substantial contribution to the study design, analysis, interpretation of data, and revised the article critically. ZM has made a substantial contribution to the concept, design, data analysis, interpretation of data, revised the article critically and approved the version to be published. BT is responsible for the acquisition of data, study design, analysis, interpretation of data, drafted, and revised the article critically and approved the version to be published. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Banafsheh Tehranineshat .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the World Medical Association’s Declaration of Helsinki. The present study was approved by the ethics committee of Shiraz University of Medical Sciences and registered at IR.SUMS.REC.1399.416. The study materials (interview questions and informed consent form) were approved by the ethics committee of the university. Before the interviews, the participants were informed by phone about the objective of the study, the voluntary basis of participation, the methods of data collection and the reason for recording the interviews. Also, the role of the researchers and the participants, and the confidentiality and anonymity of information were explained. Then the subjects who were willing to participate were asked to complete the informed consent form by Porsline. The participants were also informed that they were free to withdraw from the study at any point.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest for the research, authorship, and/or publication of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hosseini Moghaddam, M., Mohebbi, Z. & Tehranineshat, B. Stress management in nurses caring for COVID-19 patients: a qualitative content analysis. BMC Psychol 10 , 124 (2022). https://doi.org/10.1186/s40359-022-00834-4
Download citation
Received : 15 October 2021
Accepted : 10 May 2022
Published : 17 May 2022
DOI : https://doi.org/10.1186/s40359-022-00834-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.

Trusted Health Information from the National Institutes of Health
How have you managed stress during COVID-19?
Readers share their stories and suggestions.

Readers, including the Srikonda family, Alyssa and Kevin Gbolie, and Ed Piscitelli, share their pandemic takeaways.
During this global pandemic, we have all had to make changes to our daily lives. We asked readers to tell us how they kept connected and took care of their mental health over the last year. Here are some of their stories.
They embraced the extra time with family

"Since my son's music lessons are now virtual, I can hover nearby pretending to be busy and savor the moments listening to him play. Bringing a pandemic puppy into the family has also been so good for all of us. We've shared lots of laughs and spent time together instead of in our separate corners of the house."
Susan L. P. Srikonda Marketing Communications Columbus, OH

"Significantly limiting our news intake allowed us to focus on key issues while avoiding repetitive stories. Many people were heading to the water as a means of escape, so we had to find new fly-fishing spots that pushed us out of our comfort zone but was ultimately very rewarding."
Ed Piscitelli , Retired Janice Piscitelli , Executive with Empower Retirement Parker, CO

"As a nurse in a hospital that was hit hard, I try to decompress on days off with my young sons. I find myself continually reframing negative situations for them. Instead of focusing on the places we can't go because of COVID, we find a cool new place to explore each weekend. Instead of focusing on the time away from school, we focus on the extra family time. Focus on gratitude, not the things we are missing."
Ashley Fitzpatrick Nursing Manager, Cardiac Lab Closter, NJ
They stayed involved with their communities

"I send greeting cards to members of my church to keep in touch … and to dozens of strangers each month. On every card, I hand-write an inspiring message to brighten the days of people whose lives might be more depressed than what I sometimes think mine is. Happiness is like jam . . . You can't spread even a little without getting some on yourself!"
Raymond Herzog Retired Electronics Engineer Middleburg Heights, OH

"As a collegiate athlete, the loss of spring lacrosse has been very tough. I knew that so many other people my age were struggling to adapt to this new and crazy life. I created the Survive Your Mind podcast so everyone could talk about their mental health."
Paul Macrina Student Drexel University
They kept in touch online

"From the time my alarm goes off in the morning until I get into bed at night, I'm communicating with [my teaching colleagues] and I can't imagine doing this year without them."
Nicole Sheehan Grade 3 Teacher Norfolk, MA
"My friends and I would have regular board game nights once a month. Luckily, we have the technology to take that online. We get together over a video call, play some games, talk, and enjoy some snacks and drinks 'together' for a few hours. It's a nice escape from the news cycle."
Kevin Gbolie Community Manager Washington, DC
They started new routines and hobbies
"I meditate 10 minutes every day before work. Getting outdoors, with all the visuals and sounds, gets me to unplug, which has been key to my mental health. I also print out inspirational quotes and tape them anonymously on teacher's doors. Some days you just need a little love."
Robyn Hunt Vogel High School Aide John's Creek, GA

"Routine and structure, such as keeping bedtime the same each night, were important, along with being grateful for good food."
Kathy Ramsay Retired Latham, NY

"I focused on improving my Irish language skills. It made me not miss siblings and an elderly parent back home as I don't know when I can travel to them."
Aine Lutes Banking executive San Diego, CA
July 05, 2021
Health Fast Facts
Depression can happen at any age, but often symptoms begin in the teens or early 20s or 30s .
Explore More on MedlinePlus.gov
You may also like.

Commonly prescribed antidepressants and how they work
Antidepressants are among the most searched-for medications online. But there is a lot of information out there to sift through....

How to cope with the stress of social isolation
Social isolation, or being physically separated from others, can lead to loneliness and increased stress, especially during a pandemic. Loneliness...

How to help someone with anxiety
Wondering how you can help a friend, family member, or co-worker who is overwhelmed by anxiety? We spoke to David...
Trusted health information delivered to your inbox
Enter your email below
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
How does the psychological impact of covid-19 affect the management strategies of individuals with type 1 and type 2 diabetes a mixed-method study.

1. Introduction
Aims of the study, 2. materials and methods, 2.1. study design, setting, and participants, 2.2. measurements, 2.2.1. phase i, quantitative phase, 2.2.2. phase ii, qualitative phase, data analysis, 3.1. quantitative analysis, 3.1.1. demographic characteristics, 3.1.2. clinical variables, 3.1.3. correlation between depression, anxiety, and insomnia, 3.1.4. predictive factors associated with depression, anxiety, and insomnia, 3.2. qualitative analysis, 3.2.1. proactive self-management, diet and sleeping pattern, physical activity, medication and follow-up, covid-19 vaccination, 3.2.2. contextual challenges to self-care management strategies, digital transformation, the ambiguity surrounding hybrid immunity and the end of the pandemic, the burden of work and family responsibilities during and after the pandemic, 4. discussion, 5. conclusions, institutional review board statement, informed consent statement, data availability statement, acknowledgments, conflicts of interest, abbreviations.
| KSA | Kingdom of Saudi Arabia |
| HADS | Hospital Anxiety and Depression Scale |
| ISI | Insomnia Severity Index |
| Topic/Themes and Subthemes Covered | Questions Asked |
|---|---|
| Understanding how does the COVID-19 pandemic and its trajectory impact diet and sleeping patterns? | |
| Understanding how the COVID-19 pandemic and its trajectory impact performing exercise and physical activity | |
| Understanding how the COVID-19 pandemic and its trajectory impact the utilization of healthcare services and medication adherence. | |
| Understanding the patient’s experiences and perceptions regarding the COVID-19 vaccinations and booster dose | |
| Understanding the patient’s digital transformation experiences, including challenges, barriers, and issues. | |
| Understanding the patient’s experiences and perceptions about hybrid immunity and the end of the pandemic. | |
| Understanding the impact of environmental factors such as work and family obligations on patients’ physical and psychological well-being |
| Depression | Anxiety | Insomnia | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | OR (95% CI) | p | |
| Other Comorbidities | ||||||
| None (Only Diabetic) | 0.29 (0.08–0.96) | 0.04 | ||||
| Depression | 0.45 (0.23–0.9) | 0.02 | ||||
| Anxiety | 0.47 (0.23–0.94) | 0.03 | 0.31 (0.17–0.56) | 0.00 | ||
| Insomnia | 0.31 (0.17–0.58) | 0.00 |
- Kreider, K.E. Diabetes distress or major depressive disorder? A practical approach to diagnosing and treating psychological comorbidities of diabetes. Diabetes Ther. 2017 , 8 , 1–7. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Martino, G.; Caputo, A.; Bellone, F.; Quattropani, M.C.; Vicario, C.M. Going beyond the visible in type 2 diabetes mellitus: Defense mechanisms and their associations with depression and health-related quality of life. Front. Psychol. 2020 , 11 , 267. [ Google Scholar ] [ CrossRef ]
- Vilafranca Cartagena, M.; Tort-Nasarre, G.; Romeu-Labayen, M.; Vidal-Alaball, J. The experiences of patients with diabetes and strategies for their management during the first COVID-19 lockdown: A qualitative study. BMC Nurs. 2022 , 21 , 124. [ Google Scholar ] [ CrossRef ]
- Mphasha, M.H.; Mothiba, T.M.; Skaal, L. Family support in managing diabetes patients’ perspectives from Limpopo province in South Africa. BMC Public Health 2022 , 22 , 2421. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mukona, D.M.; Zvinavashe, M. Self-management of diabetes mellitus during the COVID-19 pandemic: Recommendations for a resource limited setting. Diabetes Metab. Syndr. Clin. Res. Rev. 2020 , 14 , 1575–1578. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Grabowski, D.; Overgaard, M.; Meldgaard, J.; Johansen, L.B.; Willaing, I. Disrupted self-management and adaption to new diabetes routines: A qualitative study of how people with diabetes managed their illness during the COVID-19 lockdown. Diabetology 2021 , 2 , 1–15. [ Google Scholar ] [ CrossRef ]
- Al-Daghri, N.M.; Almiman, A.A.; Wani, K.; Khattak, M.N.; Aljohani, N.J.; Alfawaz, H.; Sabico, S. COVID-19 lockdown and lifestyle changes in Saudi adults with types 1 and 2 diabetes. Front. Public Health 2022 , 10 , 912816. [ Google Scholar ] [ CrossRef ]
- Lombardo, F.; Salzano, G.; Bombaci, B.; Basile, P.; Lucania, G.; Alibrandi, A.; Passanisi, S. Has COVID-19 lockdown improved glycaemic control in pediatric patients with type 1 diabetes? An analysis of continuous glucose monitoring metrics. Diabetes Res. Clin. Pract. 2021 , 178 , 108988. [ Google Scholar ] [ CrossRef ]
- Aragona, M.; Rodia, C.; Bertolotto, A.; Campi, F.; Coppelli, A.; Giannarelli, R.; Bianchi, C.; Dardano, A.; Del Prato, S. Type 1 diabetes and COVID-19: The “lockdown effect”. Diabetes Res. Clin. Pract. 2020 , 170 , 108468. [ Google Scholar ] [ CrossRef ]
- Raosoft. Raosoft Sample Size Calculator , Raosoft, Inc.: Seattle, WA, USA, 2004. Available online: http://www.raosoft.com/samplesize.html (accessed on 10 September 2021).
- Gerrish, K.; Lacey, A. The Research Process in Nursing ; John Wiley & Sons: Hoboken, NJ, USA, 2010. [ Google Scholar ]
- Squires, A. Methodological challenges in cross-language qualitative research: A research review. Int. J. Nurs. Stud. 2009 , 46 , 277–287. [ Google Scholar ] [ CrossRef ]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983 , 67 , 361–370. [ Google Scholar ] [ CrossRef ]
- Terkawi, A.S.; Tsang, S.; AlKahtani, G.J.; Al-Mousa, S.H.; Musaed, A.; AlZoraigi, S.U.S.; Altirkawi, K.A. Development and validation of Arabic version of the Hospital Anxiety and Depression Scale. Saudi J. Anaesth. 2017 , 11 (Suppl. S1), S11–S18. [ Google Scholar ] [ CrossRef ]
- Morin, C.M.; Belleville, G.; Bélanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011 , 34 , 601–608. [ Google Scholar ] [ CrossRef ]
- Suleiman, K.H.; Yates, B.C. Translating the insomnia severity index into Arabic. J. Nurs. Scholarsh. 2011 , 43 , 49–53. [ Google Scholar ] [ CrossRef ]
- Burn, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006 , 33 , 77–101. [ Google Scholar ] [ CrossRef ]
- Creswell, J.W. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches ; Sage Publications: Thousand Oaks, CA, USA, 2013. [ Google Scholar ]
- Al-Sofiani, M.E.; Albunyan, S.; Alguwaihes, A.M.; Kalyani, R.R.; Golden, S.H.; Alfadda, A. Determinants of mental health outcomes among people with and without diabetes during the COVID-19 outbreak in the Arab Gulf Region. J. Diabetes 2021 , 13 , 339–352. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Garcia-Lara, R.A.; Gomez-Urquiza, J.L.; Membrive-Jiménez, M.J.; Velando-Soriano, A.; Granados-Bolivar, M.E.; Romero-Bejar, J.L.; Suleiman-Martos, N. Anxiety, distress and stress among patients with diabetes during COVID-19 pandemic: A systematic review and meta-analysis. J. Pers. Med. 2022 , 12 , 1412. [ Google Scholar ] [ CrossRef ]
- Moradian, S.; Teufel, M.; Jahre, L.; Musche, V.; Fink, M.; Dinse, H.; Schweda, A.; Weismüller, B.; Dörrie, N.; Tan, S.; et al. Mental health burden of patients with diabetes before and after the initial outbreak of COVID-19: Predictors of mental health impairment. BMC Public Health 2021 , 21 , 2068. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Alkhormi, A.H.; Mahfouz, M.S.; Alshahrani, N.Z.; Hummadi, A.; Hakami, W.A.; Alattas, D.H.; Alhafaf, H.Q.; Kardly, L.E.; Mashhoor, M.A. Psychological health and diabetes self-management among patients with type 2 diabetes during COVID-19 in the Southwest of Saudi Arabia. Medicina 2022 , 58 , 675. [ Google Scholar ] [ CrossRef ]
- Al-Mamun, F.; Hasan, M.; Quadros, S.; Kaggwa, M.M.; Mubarak, M.; Sikder, M.T.; Hossain, M.S.; Muhit, M.; Moonajilin, M.S.; Gozal, D.; et al. Depression among Bangladeshi diabetic patients: A cross-sectional, systematic review, and meta-analysis study. BMC Psychiatry 2023 , 23 , 369. [ Google Scholar ] [ CrossRef ]
- Parlapani, E.; Holeva, V.; Nikopoulou, V.A.; Sereslis, K.; Athanasiadou, M.; Godosidis, A.; Stephanou, T.; Diakogiannis, I. Intolerance of Uncertainty and Loneliness in Older Adults during the COVID-19 Pandemic. Front. Psychiatry 2020 , 11 , 842. [ Google Scholar ] [ CrossRef ]
- Abdu, Y.; Naja, S.; Mohamed Ibrahim, M.I.; Abdou, M.; Ahmed, R.; Elhag, S.; Saleh, A.O.; Yassin, M.; Bougmiza, I. Sleep Quality Among People with Type 2 Diabetes Mellitus During COVID-19 Pandemic: Evidence from Qatar’s National Diabetes Center. Diabetes Metab. Syndr. Obes. 2023 , 16 , 2803–2812. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Al Maqbali, M. Impact of insomnia on mental status among chronic disease patients during COVID-19 pandemic. Ethics Med. Public Health 2023 , 27 , 100879. [ Google Scholar ] [ CrossRef ]
- Fisher, L.; Polonsky, W.; Asuni, A.; Jolly, Y.; Hessler, D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. J. Diabetes Its Complicat. 2020 , 34 , 107748. [ Google Scholar ] [ CrossRef ]
- Alessi, J.; de Oliveira, G.B.; Franco, D.W.; Brino do Amaral, B.; Becker, A.S.; Knijnik, C.P.; Kobe, G.L.; de Carvalho, T.R.; Telo, G.H.; Schaan, B.D.; et al. Mental health in the era of COVID-19: Prevalence of psychiatric disorders in a cohort of patients with type 1 and type 2 diabetes during the social distancing. Diabetol. Metab. Syndr. 2020 , 12 , 76. [ Google Scholar ] [ CrossRef ]
- de Carvalho Alencar, D.; dos Santos Ribeiro, L.M.; Carvalho, L.; Rocha, G.S.; de Sousa, E.O.; de Sousa Ibiapina, A.R. Mental health of people with diabetes during the COVID-19 pandemic period: Integrative review. Rev. Eletr. Enferm. 2022 , 24 , 67537. [ Google Scholar ] [ CrossRef ]
- Sinuraya, B.; Armini, N.K.A.; Santosa, D.A.; Acob, J.R. Sleep problems in patients with diabetes mellitus during the pandemic COVID-19: A systematic review. Int. J. Health Sci. 2022 , 6 (Suppl. S2), 14624–14635. [ Google Scholar ] [ CrossRef ]
- Sisman, P.; Polat, I.; Aydemir, E.; Karsi, R.; Gul, O.O.; Cander, S.; Ersoy, C.; Erturk, E. How the COVID-19 outbreak affected patients with diabetes mellitus? Int. J. Diabetes Dev. Ctries 2021 , 42 , 53–61. [ Google Scholar ] [ CrossRef ]
- Jahan, I.; Hasan, A.N.; Sharif, A.B.; Akter, S. Changes in dietary habit and physical activity among the diabetic patients of Bangladesh during COVID-19: A cross-sectional study. PLoS Glob. Public Health 2023 , 3 , e0002096. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fatani, B.; Alfhaed, N.K.; Alkhemshi, A.A.; Alomireeni, A.A.; Albarrak, M.S.; Alquhayz, M.F.; Alzahrani, S.G. Behavioral Changes in Patients With Diabetes During the COVID-19 Pandemic in Saudi Arabia: A Cross-Sectional Study. Cureus 2023 , 15 , e34956. [ Google Scholar ] [ CrossRef ]
- Bala, R.; Srivastava, A.; Potsangbam, T.; Anal, L.; Ningthoujam, G.D. Self care practices and psychological distress among diabetic patients in Manipur during COVID-19: A scenario from the North East. Diabetes Metab. Syndr. Clin. Res. Rev. 2021 , 15 , 93–98. [ Google Scholar ] [ CrossRef ]
- Utli, H.; Doğru, B.V. The effect of the COVID-19 pandemic on self-management in patients with type 2 diabetics. Prim. Care Diabetes 2021 , 15 , 799–805. [ Google Scholar ] [ CrossRef ]
- Olesen, K.; Joensen, L.E.; Madsen, K.P.; Willaing, I. How has the COVID-19 Pandemic Affected Diabetes Self-Management in People With Diabetes?-A One-Year Follow-Up Study. Front. Clin. Diabetes Healthc. 2022 , 3 , 867025. [ Google Scholar ] [ CrossRef ]
- Özdemir, S.Ç.; Eren, M.G.; Sert, H.; Öztürk, F.C. Experiences of Patients With Type 2 Diabetes Who Recovered From COVID-19 in the Pandemic Period: A Qualitative Study. Clin. Nurs. Res. 2023 , 32 , 983. [ Google Scholar ] [ CrossRef ]
- Yu, L.; Guo, S.; Ji, W.; Sun, H.; Lee, S.; Zhang, D. Intervention Effects of Physical Activity on Type 2 Diabetic Patients Potentially Infected with COVID-19. Medicina 2023 , 59 , 1772. [ Google Scholar ] [ CrossRef ]
- WHO. Statement on the Fifteenth Meeting of the IHR (2005) Emergency Committee on the COVID-19 Pandemic. 2023. Available online: https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic (accessed on 23 November 2023).
- Amsah, N.; Md Isa, Z.; Ahmad, N.; Abdul Manaf, M.R. Impact of COVID-19 Pandemic on Healthcare Utilization among Patients with Type 2 Diabetes Mellitus: A Systematic Review. Int. J. Environ. Res. Public Health 2023 , 20 , 4577. [ Google Scholar ] [ CrossRef ]
- Yang, Y.; Huang, L. Neurological Disorders Following COVID-19 Vaccination. Vaccines 2023 , 11 , 1114. [ Google Scholar ] [ CrossRef ]
- Yasmin, F.; Najeeb, H.; Naeem, U.; Moeed, A.; Atif, A.R.; Asghar, M.S.; Waqar, F. Adverse events following COVID-19 mRNA vaccines: A systematic review of cardiovascular complication, thrombosis, and thrombocytopenia. Immun. Inflamm. Dis. 2023 , 11 , e807. [ Google Scholar ] [ CrossRef ]
- Li, H.; Ping, F.; Li, X.; Wang, Z.; Xiao, J.; Jiang, H.; Xiao, X. COVID-19 vaccine coverage, safety, and perceptions among patients with diabetes mellitus in China: A cross-sectional study. Front. Endocrinol. 2023 , 14 , 1172089. [ Google Scholar ] [ CrossRef ]
- den Hartog, G.; Andeweg, S.P.; Hoeve, C.E.; Smits, G.; Voordouw, B.; Eggink, D.; Knol, M.J.; van Binnendijk, R.S. Assessment of hybrid population immunity to SARS-CoV-2 following breakthrough infections of distinct SARS-CoV-2 variants by detecting antibodies to nucleoprotein. Sci. Rep. 2023 , 13 , 18394. [ Google Scholar ] [ CrossRef ]
- Lasrado, N.; Barouch, D.H. SARS-CoV-2 hybrid immunity: The best of both worlds. J. Infect. Dis. 2023 , 228 , 1311–1313. [ Google Scholar ] [ CrossRef ]
- Rick, A.M.; Laurens, M.B.; Huang, Y.; Yu, C.; Martin, T.C.; Rodriguez, C.A.; Rostad, C.A.; Maboa, R.M.; Baden, L.R.; El Sahly, H.M.; et al. Risk of COVID-19 after natural infection or vaccination. EBioMedicine 2023 , 96 , 104799. [ Google Scholar ] [ CrossRef ]
- Duan, L.; Wang, Y.; Dong, H.; Song, C.; Zheng, J.; Li, J.; Xu, J. The COVID-19 vaccination behavior and correlates in diabetic patients: A health belief model theory-based cross-sectional study in China, 2021. Vaccines 2022 , 10 , 659. [ Google Scholar ] [ CrossRef ]
- Sun, C.A.; Shenk, Z.; Renda, S.; Maruthur, N.; Zheng, S.; Perrin, N.; Levin, S.; Han, H.R. Experiences and perceptions of telehealth visits in diabetes care during and after the COVID-19 pandemic among adults with type 2 diabetes and their providers: Qualitative study. JMIR Diabetes 2023 , 8 , e44283. [ Google Scholar ] [ CrossRef ]
- Sakur, F.; Ward, K.; Khatri, N.N.; Lau, A.Y. Self-care behaviors and technology used during COVID-19: Systematic review. JMIR Hum. Factors 2022 , 9 , e35173. [ Google Scholar ] [ CrossRef ]
- Papazafiropoulou, A. Telemedicine and diabetes during the COVID-19 era. Arch. Med. Sci. Atheroscler. Dis. 2022 , 7 , e131. [ Google Scholar ] [ CrossRef ]
- Megasari, L.A.; Mas’ udah, S.; Febrianto, P.T. The Impact of the COVID-19 Pandemic and Work From Home Policy on Poor Communities and Women in Rural Area. Society 2021 , 9 , 522–538. [ Google Scholar ] [ CrossRef ]
- Pleym, K.; Iversen, M.M.; Broström, A. Experiences and actions related to living with type 1 diabetes during the COVID-19 pandemic in Norway: A qualitative study conducted from July to December 2020. BMJ Open 2022 , 12 , e056027. [ Google Scholar ] [ CrossRef ]
- Lambert, C.; Jomeen, J.; McSherry, W. Reflexivity: A review of the literature in the context of midwifery research. Br. J. Midwifery 2010 , 18 , 321–326. [ Google Scholar ] [ CrossRef ]
- Hibbert, P.; Coupland, C.; MacIntosh, R. Reflexivity: Recursion and relationality in organizational research processes. Qual. Res. Organ. Manag. Int. J. 2010 , 5 , 47–62. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Depression (n = 155, 37.1%) | Non-Depression (n = 263, 62.9%) | Anxiety (n = 247, 59.1%) | Non-Anxiety (n = 171, 40.9%) | Insomnia (n = 277, 66.3%) | Non-Insomnia (n = 141, 33.7%) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p | n | % | n | % | p | n | % | n | % | p | |
| 0.008 ** | 0.13 | 0.04 | |||||||||||||||
| Male | 170 | 40.7 | 76 | 49 | 94 | 35.7 | 93 | 37.7 | 77 | 45 | 103 | 37.2 | 67 | 47.5 | |||
| Female | 248 | 59.3 | 79 | 51 | 263 | 64.3 | 154 | 62.3 | 94 | 55 | 174 | 62.8 | 74 | 52.5 | |||
| 0.26 | 0.02 * | 0.41 | |||||||||||||||
| 18–30 | 172 | 41.1 | 60 | 38.7 | 112 | 42.6 | 114 | 46.2 | 58 | 33.9 | 122 | 44 | 50 | 35.5 | |||
| 31–40 | 57 | 13.6 | 21 | 13.5 | 36 | 13.7 | 25 | 10.1 | 32 | 18.7 | 34 | 12.3 | 23 | 16.3 | |||
| 41–50 | 84 | 20.1 | 26 | 16.8 | 58 | 22.1 | 52 | 21.1 | 32 | 18.7 | 55 | 19.9 | 29 | 20.6 | |||
| 51–60 | 57 | 13.6 | 25 | 16.1 | 32 | 12.2 | 30 | 12.1 | 27 | 15.8 | 34 | 12.3 | 23 | 16.3 | |||
| More than 60 | 48 | 11.5 | 23 | 14.8 | 25 | 9.5 | 26 | 10.5 | 22 | 12.9 | 32 | 11.6 | 16 | 11.3 | |||
| 0.38 | 0.06 | 0.26 | |||||||||||||||
| Married | 236 | 56.5 | 94 | 60.6 | 142 | 54 | 129 | 52.2 | 107 | 62.6 | 151 | 54.5 | 85 | 60.3 | |||
| Single | 155 | 37.1 | 51 | 32.9 | 104 | 39.5 | 103 | 41.7 | 52 | 30.4 | 110 | 39.7 | 45 | 31.9 | |||
| Others | 27 | 6.5 | 10 | 6.5 | 17 | 6.5 | 15 | 6.1 | 12 | 7 | 16 | 5.8 | 11 | 7.8 | |||
| 0.79 | 0.24 | 0.55 | |||||||||||||||
| Basic | 74 | 17.7 | 25 | 16.1 | 49 | 18.6 | 40 | 16.2 | 34 | 19.9 | 47 | 17 | 27 | 19.1 | |||
| Secondary | 151 | 36.1 | 58 | 37.4 | 93 | 35.4 | 97 | 39.3 | 54 | 31.6 | 105 | 37.9 | 46 | 32.6 | |||
| Degree | 193 | 46.2 | 72 | 46.5 | 121 | 46 | 110 | 44.5 | 83 | 48.5 | 125 | 45.1 | 68 | 48.2 | |||
| 0.001 ** | 0.25 | 0.11 | |||||||||||||||
| Employed | 128 | 30.6 | 42 | 27.1 | 86 | 32.7 | 69 | 27.9 | 59 | 34.5 | 76 | 27.4 | 52 | 36.9 | |||
| Retired | 65 | 15.6 | 37 | 23.9 | 28 | 10.6 | 37 | 15 | 28 | 16.4 | 43 | 15.5 | 22 | 15.6 | |||
| Unemployed | 225 | 53.8 | 76 | 49 | 149 | 56.7 | 141 | 57.1 | 84 | 49.1 | 158 | 57 | 67 | 47.5 | |||
| 0.33 | 0.43 | 0.04 | |||||||||||||||
| Type 1 | 214 | 51.2 | 79 | 51 | 135 | 51.3 | 131 | 53 | 83 | 48.5 | 148 | 53.4 | 66 | 46.8 | |||
| Type 2 | 139 | 33.3 | 47 | 30.3 | 92 | 35 | 76 | 30.8 | 63 | 36.8 | 81 | 29.2 | 58 | 41.1 | |||
| Others | 65 | 15.6 | 29 | 18.7 | 36 | 13.7 | 40 | 16.2 | 25 | 14.6 | 48 | 17.3 | 17 | 12.1 | |||
| 0.10 | 0.10 | 0.03 | |||||||||||||||
| Hypertensive/Heart failure | 96 | 23 | 39 | 25.2 | 57 | 21.7 | 61 | 24.7 | 35 | 20.5 | 68 | 24.5 | 28 | 19.9 | |||
| Others | 15 | 3.6 | 6 | 3.9 | 9 | 3.4 | 11 | 4.5 | 4 | 2.3 | 13 | 4.7 | 2 | 1.4 | |||
| Asthma | 25 | 6 | 12 | 7.7 | 13 | 4.9 | 18 | 7.3 | 7 | 4.1 | 18 | 6.5 | 7 | 5 | |||
| None (Only Diabetic) | 250 | 59.8 | 81 | 52.3 | 169 | 64.3 | 135 | 54.7 | 115 | 67.3 | 152 | 54.9 | 98 | 69.5 | |||
| More than two Comorbidities | 32 | 7.7 | 17 | 11 | 15 | 5.7 | 22 | 8.9 | 10 | 5.8 | 26 | 9.4 | 6 | 4.3 | |||
| 0.10 | 0.44 | 0.43 | |||||||||||||||
| Yes | 126 | 30.1 | 54 | 34.8 | 72 | 27.4 | 78 | 31.6 | 48 | 28.1 | 87 | 31.4 | 39 | 27.7 | |||
| No | 292 | 69.9 | 101 | 65.2 | 191 | 72.6 | 169 | 68.4 | 123 | 71.9 | 190 | 68.6 | 102 | 72.3 | |||
| 0.75 | 0.49 | 0.94 | |||||||||||||||
| Yes, one Dose | 123 | 29.4 | 43 | 27.7 | 80 | 30.4 | 72 | 29.1 | 51 | 29.8 | 83 | 30 | 40 | 28.4 | |||
| Yes, two doses | 274 | 65.6 | 103 | 66.5 | 171 | 65 | 160 | 64.8 | 114 | 66.7 | 180 | 65 | 94 | 66.7 | |||
| No | 21 | 5 | 9 | 5.8 | 12 | 4.6 | 15 | 6.1 | 6 | 3.5 | 14 | 5.1 | 7 | 5 | |||
| Depression | Anxiety | Insomnia | |
|---|---|---|---|
| Depression | 1 | 0.579 ** | 0.452 ** |
| Anxiety | 1 | 0.461 ** | |
| Insomnia | 1 |
| Overarching Theme | Interpretative Theme | Participants’ Quotes |
|---|---|---|
| “Thank Allah we have plenty of food, but I could not eat that much. I was alone, and I lost my appetite. I used to eat with my son and grandchildren; they lived close to me next door. After this pandemic, we could not be together. As usual, they brought food to my room. It is too lonely and sad. (P3, F)” | ||
| “ I am old and have other comorbidities, so I have a restricted diet. We used to eat with my daughter and grandchildren; after this pandemic, she could not do that as before. She does what she can but has become busy with her children, their distance learning, and her work. The quality of my food has changed. I eat less and do not enjoy my food anymore… I do not want to put an extra burden on her. (P5, M)” | ||
| “ I am a teacher, and I used to work with children and have a good daily routine. I worked from home after the lockdown and school suspension, and my daily routine changed. I felt depressed and became irritable and anxious. Being at home 24 h is horrible. I started to eat more. My diet is not as healthy as before. I sleep fewer hours and gain more weight. I could not control myself, and my blood sugar level was fluctuating. (P7, F)” | ||
| “I could not retrieve my normal sleeping pattern and peace; the home environment became more noisy and crowded, had more tensions, negative news, stress and tasks or obligations, and not enough personal space, you know, disruption in our daily lives and the lockdown..etc. I could not sleep enough or sleep fewer hours, having more sleeping disruptions and becoming a night person, being exhausted all of the time, and it is difficult to control my blood glucose level, weight, and my eating patterns as well. (P9, M)” | ||
| “I am an old man, and one physiotherapist used to come to me daily. My kids hired him after my right foot was amputated as I had gangrene. I cannot perform the exercise without help; my muscles are too weak. He helped me to perform the exercise. | ||
| “After this pandemic and lockdown, he could no longer work for me as he has worked at the hospital. He might have transmitted the virus to me. I try to perform exercises without help but fail; it is painful, and I feel frustrated. My son helps me during the bath, but I have not performed exercise for a long time. I feel better with exercise. I become more worried, stressed, and irritable since I stopped exercising. I have muscle and bone pain and feel helpless and upset. (P12, M)” | ||
| “I used to perform the exercise at home when my children were at school and my husband was at work. I have a daily routine of doing yoga, performing exercises, having online Zumba classes, taking care of myself, and having peace out of everything. After COVID-19, lockdown, and school suspension, I cannot do that anymore; I cannot find peace and a good time. I have tried to perform exercises, but they do not let me do what I want. It is annoying that they are becoming demanding, asking, and disrupting. I have five children and a husband at home; there is much tension and stress. I cannot be alone and have time for myself as before. I cannot control my blood sugar, and I gain more weight. All daily routines are disrupted, including physical activity, diet, and sleeping patterns. I feel depressed and stressed. (M10, F)” | ||
| “I used to go to the beach, taking advantage of the public exercise machines, breathing fresh air, and enjoying the view. After this pandemic, it is too difficult. The lockdown has started, and it is not allowed to go out. In addition, it is not safe, and I cannot use the machines there. It is unsterilized. It is for public use. I could not touch or use them anymore. I lived in a small apartment and did not have enough space to exercise. I also have limited income and cannot pay for exercise machines. I feel chained between the room walls and depressed. I did not perform an exercise, and my blood sugar is not controlled. After three years, I felt stuck and could not retrieve my normal life. (P2, M)” | ||
| “I try not to go to the GP as much as possible; I do not want to be with others; they might have COVID-19, so it is better to be home. My daughter collects my monthly medicine and brings it to me. I have my medication as usual; there is no change. I take my pills every day before breakfast and before dinner. I do not think it needs to be changed. (P15, M)” | ||
| “My youngest daughter used to check my blood sugar before having insulin injections, but she cannot visit me and do that regularly due to the lockdown and the COVID-19 consequences. I have tremors and cataracts in my left eye. I cannot do blood sugar tests for myself. I remember not taking my insulin when my blood sugar was low, but I did not know that. Insulin lowers my blood sugar, and I was fainting. My Allah helped me; I could have died at that moment. I feel alone and frustrated. I do not want to die alone or with the wrong insulin dose. This idea makes me more anxious and depressed. My Allah, mercy us. (P16, F)” | ||
| “I could not control myself, and my blood sugar level was fluctuating. I was on oral antidiabetic, but recently, the physician prescribed insulin for me. (P13, F)” | ||
| “ COVID-19 was horrible and scary. I kept asking about COVID-19 and what was happening, but no one answered. I was sick during the first wave of this pandemic; I went to the hospital with my son. The nurse in the triage room asked me to come back home immediately and not sit on the chair; he told me sorry, COVID-19 patients were everywhere, and we could not protect or serve you right now. He was frustrated and shouting at my son to run away from the hospital. (P11, M)” | ||
| “Many options are available for COVID-19 vaccinations, but which is the best for me? How was it developed so quickly? What are the real risks and side effects? We have heard a lot about its side effects. Some people die after having vaccinations, and some have strokes. What are the side effects in the long term? We do not know the truth about it. (P1, M)” | ||
| “I am not sure about COVID-19 vaccination. In the beginning, I was keen to receive vaccination, and I think it is an impressive blessing to save people, get rid of this pandemic, and retrieve our normal life. After having the first dose, I was sick for ten days. Two months later, I was infected and experienced severe symptoms. I think there is no point in having a booster dose. (P4, F).” | ||
| “While I had the COVID-19 vaccine, I was infected with COVID-19. I had severe symptoms, and I was hospitalized for a while. Until now, I am still struggling with the long-term effects of chest pain, shortness of breath, fatigue, joint pain..etc. I do not think the COVID-19 vaccine is effective, and I do not think it makes any difference. I think its side effects and complications more than benefits. I know some people had strokes and blood clotting issues after being vaccinated. It is unsuitable for people like us with diabetes. (P13, F)” | ||
| “ Most medical services and communication channels have moved to the online world. I am an old man who is not good at technology. My daughters tried to teach me, but I could not. I think this makes our life more sophisticated. I could not talk freely online; I felt like I was in prison. I am alone with this mobile. (P5, M)” | ||
| “As a mother, this digital technology makes our life horrible, burdens us with more work, and increases the pressure on mothers. I must care for my children’s health and education; distance learning kills me in addition to demanding and depressed husbands, working all the time at home without a break, and tolerating their psychological distress. How could I find time and space to care for myself and look after my health? I am exhausted and cannot control my blood sugar or lifestyle. (P6, F)” | ||
| “While digital technology gives us more opportunity to access free and paid online applications such as fitness, exercise, meditation, weight loss, and healthy diet, etc., We could not take advantage of this technology for many reasons, the environmental challenges at home, family and work obligation and unfished online work tasks.” | ||
| “Everyone talks about hybrid immunity; I do not think this is real for us. My aunt passed away due to COVID-19 when she was 59 years old and had the COVID-19 vaccine three times. She was diabetic like me, and while she survived the first time having a COVID-19 infection, she passed away the second time having this infection. (P14, M)” | ||
| “See, around you, nobody is strict with social distancing or wearing masks, even your family members who already know about your medical case, while we hear every time about new variants of COVID-19, how we could have a hybrid community. I do not think this is real. Vaccinations do not work, people are not strict with personal protective measures, and new variants are emerging between time and time, and we feel insecure and safe.” | ||
| “I had a healthy lifestyle and quit life. Overnight, we are forced to change our lifestyle and priorities due to COVID-19. Work hard without having a good and clear plan. All our programs were destroyed. Over time, we lose the passion and support to look after ourselves. All the circumstances around me put pressure on me, putting my healthy habits at the bottom of the priorities list. (P1, M)” | ||
| “Even now, after lifting precautionary and preventive measures, we still cannot control our lifestyle habits and manage our life patterns to be healthier. I think regaining a lifestyle is not impossible. I used to walk and take advantage of public exercise, but how could I trust it again while we always hear that new variants of COVID have been discovered? We all lost peace somehow in our home and soul (P2, M).” | ||
| “During the lockdown, we also lost our boundaries with family members and our space. They became more demanding and complaining and expected a lot from me. This was tough on me as a diabetic patient on Insulin. While the lockdown was over, we all returned to work or school; I could not retrieve my boundaries to have my own space, care for my health, and look after my health as before the pandemic. (P7, F)” |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Madkhali, N.A.B. How Does the Psychological Impact of COVID-19 Affect the Management Strategies of Individuals with Type 1 and Type 2 Diabetes? A Mixed-Method Study. Healthcare 2024 , 12 , 1710. https://doi.org/10.3390/healthcare12171710
Madkhali NAB. How Does the Psychological Impact of COVID-19 Affect the Management Strategies of Individuals with Type 1 and Type 2 Diabetes? A Mixed-Method Study. Healthcare . 2024; 12(17):1710. https://doi.org/10.3390/healthcare12171710
Madkhali, Norah Abdullah Bazek. 2024. "How Does the Psychological Impact of COVID-19 Affect the Management Strategies of Individuals with Type 1 and Type 2 Diabetes? A Mixed-Method Study" Healthcare 12, no. 17: 1710. https://doi.org/10.3390/healthcare12171710
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

- Request Information

Aug 11, 2020 11:34:39 AM | Stress Managment During COVID-19 | achs.edu
Feeling stressed? We created a webinar series designed to help you slow down, take a moment to breathe, and learn some helpful tools to support you.

Image copyright: pexels.com
All of us around the world may be experiencing stress more often or more intensely because of the COVID-19 pandemic. Because of this, we have found that stress management is a much-needed topic during these times. With that in mind, we’ve created a week-long stress management webinar series designed to help you slow down, take a moment to breathe, and learn some new and helpful tools to support you.
Stress Management Webinar Series
The series features a new presenter each day of the week from August 24 to 28.
- We all know what it’s like to feel stressed, but what IS stress exactly and how does it tend to affect us mentally and physically? Learn some basic ways to identify stress and also get some tips to manage it.
- Qi Gong focuses our intent on one breath at a time, one movement at a time, which trains our mind to stay in the moment. The Iron Shirt Qi Gong series helps to strengthen our immune system as each movement enhances the associated meridian channel, thereby bringing our body into a relaxed state and into homeostasis.
- A conversation about setting boundaries, expectations and routines that will allow you to thrive during chaotic times.
- What if every time we encountered a problem, we took less fault personally, and instead, adopted a lens that promoted growth and commitment to our goals? In this webinar, we will discuss practicing Resiliency ABC's, focusing on progress rather than goals, acquiring an adaptive mindset, and learning to perceive obstacles as challenges rather than dealbreakers. Join us to learn how to cultivate a mindset that fosters success, happiness, and resiliency.
- Enjoy a simple and easy practice that will lift your spirits, clear your mind, and increase your focus at work, home, or during your educational studies. Jennifer is a 15 year yoga and wellness professional earning her Master's in the Science of Aromatherapy at ACHS, and is looking forward to giving you valuable tips to get you through your semester and life practices.

Aromatherapy To Support Calm
During this crazy time, when everything feels out of our control, it feels good to tackle the things you can control such as your stress level. Our Calm is Contagious DIY Blend will help take the edge off and give you that tranquil vibe that is eluding us all right now. Diffuse it or add to a nasal inhaler and inhale deeply, or try combining Calm is Contagious Blend with your favorite carrier oil for a luxurious moisturizing rub after a bath. If you prefer you can even add this carrier oil blend to your bath and enjoy a de-stress soak. Another effective way to use it is to add it to argan oil which is great for hair health and give yourself a deep scalp massage and leave on overnight. De-stress and healthy hair!
Now breathe and enjoy ……...
Disclosure of Material Connection: This blog may contain affiliate links. I am disclosing this in accordance with the Federal Trade Commission’s 16 CFR, Part 255: “Guides Concerning the Use of Endorsements and Testimonials in Advertising.”
This article is for informational purposes only. It is not intended to treat, diagnose, cure, or prevent disease. This article has not been reviewed by the FDA. Always consult with your primary care physician or naturopathic doctor before making any significant changes to your health and wellness routine.
About American College of Healthcare Sciences

This commitment to our students and graduates reflects in our current survey results that reflect 98% of our students would recommend ACHS to a friend or family member.
We believe education is the most powerful tool for changing an individual and the world around us.
When a person enrolls as ACHS, it is vitally important that they graduate with tools they need to forge their own holistic and sustainable missions, build up their communities confidently and changing the face of healthcare with knowledge.

Written By: American College of Healthcare Sciences
You may also like.
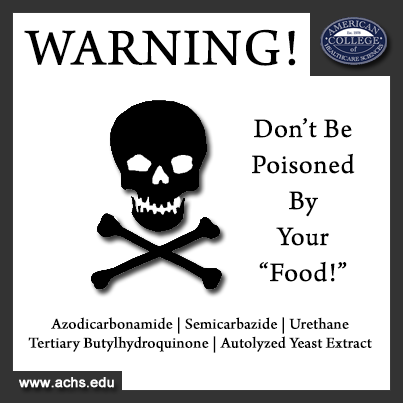
Mar 1, 2014 6:00:00 AM | holistic nutrition Top 5 Most Dangerous Restaurants For Your Health | achs.edu

Mar 8, 2018 12:20:00 PM | environmental sustainability Why We Care About Environmental Wellness | achs.edu

Jul 17, 2018 7:34:00 AM | 5 Seeds that Support Healthy Digestion | achs.edu
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

College students’ stress and health in the COVID-19 pandemic: The role of academic workload, separation from school, and fears of contagion
Chunjiang yang.
School of Economics and Management, Yanshan University, Qinhuangdao, Hebei, China
Yashuo Chen
Associated data.
All relevant data are within the manuscript and its Supporting Information files. In addition, all data are available form the OSF database. The link is https://osf.io/ajfhw/ and the DOI is 10.17605/OSF.IO/AJFHW .
The COVID-19 pandemic has unhinged the lives of people across the globe. In particular, more than 30 million Chinese college students are home-schooling, yet there is little understanding of how academic workload, separation from school, and fears of contagion lead to a decrease in their health. This study examined the relationships between Chinese college students’ three critical stressors and two types of health in the COVID‐19 pandemic context. We used a three-wave lagged design with a one-week interval. All the constructs were assessed by self-report in anonymous surveys during the COVID‐19 pandemic. College students were asked to report their demographic information, academic workload, separation from school, fears of contagion, perceived stress, and health. The results of this study showed that academic workload, separation from school, and fears of contagion had negative effects on college students’ health via perceived stress. In the COVID-19 crisis, multiple prevention and control measures focusing on college students may lead them to have different degrees of stress and health problems. Our results enrich the literature on stress and health and offer novel practical implications for all circles of the society to ensure students’ health under the context of the COVID-19 epidemic.
Introduction
Compared with other student groups, such as primary school students and middle school students, the traditional view is that college students bear more pressure and have more serious physical and mental health problems [ 1 ]. In previous research, there is a strongly held consensus that dealing with intimate relationships, financial difficulties, and fulfilling responsibilities and roles are the main sources of stress for college students. Due to the recent social changes in the education domain (e.g., the sharing of educational resources and advances in communication technology), the use of distance education is more and more, which changes the communication patterns between teachers and students, increases the isolation and independence of students, and thus becomes an important source of pressure for students [ 2 ]. Today, the spread of coronavirus disease 2019 (COVID-19) is becoming unstoppable, having infected more than 12 million people [ 3 ]. In response to this unprecedented challenge, the Chinese government has ordered a nationwide school closure as an emergency measure to prevent the spreading of the infection among teachers and students. As a consequence, 30.315 million Chinese college students are trapped at home, learning online courses through the internet to complete the required academic tasks. So far, the new virtual semester has been going on for nearly three months, and various courses are offered online in a well-organized manner. Although these decisive actions and efforts are highly commendable and necessary, there are also reasons to worry that drawn-out school suspension, home confinement, and distance learning may have adverse effects on college students’ physical and mental health [ 4 ]. In addition, a series of issues, such as fear of contagion, frustration and boredom, inadequate information, and lack of private space at home, would continue to emerge and increase during the COVID-19 outbreak [ 4 ]. However, previous research failed to give enough attention to college students in the epidemic context. For example, some studies have shown that large-scale isolation measures and loss of income have led to mental health problems among migrant workers during COVID-19 outbreaks [ 5 ]. Chen et al. [ 6 ] have discussed the problems in psychological intervention services of medical workers. The present study aimed to fill the void by focusing on college students to explore the influence of several important stressors on their health during the COVID-19 outbreak. Specifically, we identified three important stressors among college students—academic workload, separation from school, and fear of contagion and further explored the mechanism behind the relationships between three stressors and mental and physical health.
Academic stressors refer to any academic demands (e.g., environmental, social, or internal demands) that cause a student to adjust his or her behavior. Learning and examination, performance competition, especially mastering much knowledge in a short time, would lead to different degrees of academic pressure [ 7 ]. Although all planned courses have been affected by the COVID-19 epidemic, online learning still leaves college students with the same academic burden as usual. In addition, previous evidence shows that separation anxiety disorder of adults is similar to that of children and adolescents in phenomenology. College students who are attached to their classmates may experience separation anxiety after leaving school. Emerging problems during the COVID-19 outbreak, such as conflicting family schedules, changes in eating and sleeping habits, separation from classmates, and loneliness, may have adverse effects on college students [ 8 ]. Seligman and Wuyek suggested that college students may experience separation anxiety when they go home for the holidays [ 9 ]. Finally, the COVID-19 pandemic has projected humanity into an unprecedented era characterized by feelings of helplessness and loss of control. As Sontag [ 10 ] noted, unknown diseases cannot be totally controlled and thus are often considered more threatening than factual evidence. During this period, populations remained almost entirely susceptible to COVID-19, causing the natural spread of infections to exhibit almost perfect exponential growth [ 11 ]. Therefore, feelings of fear and apprehension about having or contracting COVID-19 may be a significant stressor for college students. Considering the actual situation of college students during an outbreak of COVID-19, the first aim of the study is to identify academic workload, separation from school, and fears of contagion, which are the three important stressors of college students.
Moreover, previous studies demonstrated that diseases (e.g., SARS) [ 12 ], academic (e.g., academic expectations) [ 13 ], and attachments (e.g., attachment to parents) [ 14 ] are closely associated with students’ health. However, it is still not fully understood how these stressors lead to health-related outcomes. In particular, we know little about the mechanism through which these stressors affect physical and mental health in the context of the COVID-19 outbreak. Brewster et al. [ 15 ] have suggested that further research is needed to establish the different mechanisms through which stressors impact health in order to have a profound understanding of the nature of stress. In response to these calls for further research, the second aim of this study thus was to examine the potential mediating roles of perceived stress in the relationships between the three stressors and physical and psychological health.
Overall, the current study focuses on college students and presents an integrated framework to investigate whether and how three types of stressors influence physical and mental health. Our study contributes to the current literature on stress and health in three unique ways. First, to the best of our knowledge, this study is the first to explore home-schooling college students’ physical and mental health during the COVID-19 outbreak. It makes up for the lack of understanding of the situations of college students who are ongoing home-schooling during the COVID-19 outbreak. Second, we discovered that academic stressors, interpersonal stressors, and environmental stressors of college students are critical factors that influence their health. This investigation not only overcomes the previous analysis focusing primarily on the effect of a single stressor on college students’ health but also enlarges the scope of current research on students’ stress and health by shifting the locus of theorizing away from campus domain to family domain. Third, by examining the mediating role of perceived stress, we exposed the “black box” in the relationship between stressors and health.
Three stressors among college students during the COVID-19 outbreak
College students’ stressors have been typically grouped into three major categories: academic pressure [ 16 – 19 ], social and interpersonal pressure [ 20 , 21 ], and environmental pressure [ 22 , 23 ]. Specifically, this study focuses on academic workload (representing academic pressure), separation from school (representing social and interpersonal pressure), and fear of contagion (representing environment pressure).
Academic workload
Academic problems have been regarded as the most common stressor for college students [ 24 , 25 ]. For example, in Schafer’s [ 26 ] investigation, students reported that the most significant daily hassles were academics-related stressors such as constant study, writing papers, preparing for exams, and boring teachers. The academic pressure easily comes from taking and preparing for exams, grade level competition, and acquiring a large amount of knowledge in a short period of time [ 7 ]. Perceived stress is a response to stressors, referring to the state of physical or psychological arousal [ 27 ]. College students experience adverse physical and psychological outcomes when they perceive excessive or negative stress. Excessive stress may induce physical impairments, including lack of energy, loss of appetite, headaches, or gastrointestinal problems [ 28 ]. Numerous studies have evaluated academic stress associated with various adverse outcomes, such as poor health [ 29 , 30 ], anxiety [ 31 ], depression [ 32 ], and poor academic performance [ 33 , 34 ]. In particular, Hystad et al. [ 35 ] found significant associations between academic stress and health, both psychological and physical.
Separation from school
Previous studies have shown that students view the transition from high school to college as a source of some degree of stress and emotional dissonance [ 36 ]. College students’ adaptability is closely related to their attachment with different people, such as parents and friends. Indeed, extant research on attachment has four research directions. First, the most systematic studies have focused on adolescents’ psychological separation from parents, suggesting that the healthy development of adolescents depends largely on psychological separation from parents [ 37 ]. The second field focuses on the attachment relationship between parents and adolescents, assuming that attachment to parents is a necessary prerequisite for adolescents’ adaptive function [ 38 , 39 ]. The third research stream emphasized the importance of psychological separation and attachment. According to this point of view, a balanced parent-child relationship between psychological separation and parental attachment is the best choice for students’ development [ 37 , 40 ]. Finally, a fourth research stream focuses on attachment to a group or group members in a campus environment and suggests that this attachment may influence students’ affective and behavioral outcomes [ 41 ]. From the above-mentioned research fields, we can discover that the existing literature mainly focuses on the effects of attachment on college students in their campus life. Of course, it is undeniable that the campus is the primary field for college students, while the family field becomes more important for college students during the weekends, holidays, and internships. Unfortunately, there is a dearth of research on the influence of attachment on college students in their family life. According to the literature on attachment and separation, attachment relationships between college students and their classmates may affect their stress and health when they are at home.
Social cohesion theorists believed group formation was entirely a function of individual relationships among the group members: As individuals were attracted to one another, they were consequently attracted to the group as a whole. Furthermore, group formation can occur independently of interpersonal attraction [ 42 ]. Based on the social identity theorists’ research, in minimal groups, people formed group attachment without having any contact or even knowing the other members in their group [ 41 ]. Thus, whether or not there is a close relationship with group members, one can feel the attachment to the group to which he belongs. However, some scholars reasoned that students with a stronger and healthier sense of themselves as individuals would be better equipped to handle the demands for independent functioning that accompany the college transition. An investigation among medical students shows that students with greater group cohesion reported less stress [ 43 ]. Separation anxiety begins with separation from parents, peers, and other significant persons. The national mandate force college students to separate from school in the COVID-19 pandemic, leading to separate from their peers and thus may cause their stress.
Fears of contagion
Fears of contagion reflect feelings of apprehension about having or contracting COVID-19. The literature on health anxiety [ 44 ] suggests that threatening events—such as a global pandemic—trigger high levels of stress. Although previous studies have described the pressures triggered by large-scale events, such as natural disasters [ 44 ] and terrorist attacks [ 45 ], the outbreak of infectious diseases (the COVID-19 pandemic) worldwide is different from other large-scale events [ 46 ]. Update to 1 May 2020 , the COVID-19 pandemic has resulted in 3175207 confirmed cases and 224172 deaths [ 3 ]. To prevent the spread of infectious diseases, Chines schools have been closed nationwide, collective activities have been canceled, public transportation has been suspended, and family imprisonment has been strictly enforced in some epidemic areas. The outbreak of COVID-19 has a seriously destructive impact on people’s lives all over the world. The effects of COVID-19 are multifaceted, affecting both physical health (e.g., pneumonia, liver, and renal injury) and psychological well-being (e.g., fear of contracting an infectious disease, avoid exposure to others to reduce the risk of being infected). Although national preventive measures can slow the spread of the epidemic, individuals cannot ensure that they are not infected with the disease. According to Chinese data, a large number of transmissions, both in nosocomial and community settings, occurred through human-to-human contact with individuals showing no or mild symptoms [ 47 ]. The COVID-19 pandemic is an immediate threat, it is unclear how long it will persist, and there are a multitude of unanswered questions regarding its impact. Several anecdotal reports by health care professionals note the COVID-19 pandemic triggers individuals’ anxiety and stress, particularly surrounding the uncertainties brought by COVID-19 [ 48 ]. Therefore, we suggest that fear of having or contracting COVID-19 may lead to college students’ stress and health problems.
Transactional models of stress and coping
Lazarus and Folkman [ 49 ] defined stress as a particular relationship between the person and the environment that is appraised by the person as taxing or exceeding his or her resources and endangering his or her well-being. The Transactional Model of Stress provides a basic framework for explaining the processes of individuals coping with stressful events. A core tenet of this model is that the interaction between the person and the environment creates an individual’s feeling of stress. When faced with a stressor, two appraisals were triggered, an individual evaluates potential threats or harms (primary appraisal), as well as the ability to change the situation and control negative emotional reactions (secondary appraisal). Primary appraisal is an individual’s estimate of the significance of an event as stressful, negative, positive, controllable, challenging, friendly, or irrelevant. The secondary appraisal is a judgment of an individual’s coping resources and choices [ 50 ]. The response described in the transaction model starts after the primary and secondary appraisals [ 49 ]. There are two kinds of coping efforts strongly related to a person’s cognitive appraisal. One is referred to as problem-focused coping, and the other is referred to as emotion-focused coping. The former coping strategy has been shown to be more commonly used in a person’s causal analysis, suggesting that some measures can be taken to change the negative situation. For example, Folkman and Lazarus [ 51 ] show that students will adopt a problem-based coping style before the examination. The latter coping strategy predominates when people assess that they have no options or lack resources to alter the situation, stressors have to be accepted [ 52 ]. Students have reported they often use escape/avoidance ways to cope with stressors. The problem-solving efforts try to change the situation actively, while the emotion-centric coping style will only change the individual’s interpretation of the stressors. Based on these arguments, we suggest that college students who feel stressed (e.g., regard their stress as an environmental source or lack of ability to alter) would adopt emotion-focused coping as a means of reappraising an uncontrollable situation. Thus, perceived stress plays a central role in the attribution–secondary appraisal coping relationship.
The present study
Our primary aim in the study was to examine the influence of stressors on college students’ stress and health during the COVID-19 outbreak. Specifically, we empirically examine the influence of academic workload, separation from school, and fears of contagion on college students’ psychology and physiology health that included perceived stress as a mediator. Based on the literature review, we hypothesized:
H1a: Academic workload is positively correlated with perceived stress.
H1b: Academic workload is negatively correlated with physical and mental health.
H2a: Separation from school is positively correlated with perceived stress.
H2b: Separation from school is negatively correlated with physical and mental health.
H3a: Fears of contagion are positively correlated with perceived stress.
H3b: Fears of contagion are negatively correlated with physical and mental health.
H4: Perceived stress is negatively correlated with physical and mental health.
- H5: Perceived stress mediates the relationship between academic workload and physical and mental health.
- H6: Perceived stress mediates the relationship between separation from school and physical and mental health.
- H7: Perceived stress mediates the relationship between fears of contagion and physical and mental health.
The hypothesized model is presented in Fig 1 .

Ethics statement
All participants were treated following the American Psychological Association ethical guidelines, and the study protocol was approved by the Yanshan University Institutional Review Board (Approval no. 20-03-01). Each participant got an introduction and a link to a questionnaire via WeChat, a widely used instant communication tool in China. In the introduction, anonymity, the aim of the survey, and information on whether participants agreed to participate in the survey were all illustrated in detail. We explained that if you want to participate in the survey, please open the questionnaire link and fill in your true feelings. Some college students expressed their intention to participate in written form through WeChat, and other college students directly participated in the survey with tacit approval according to the instructions. Therefore, all participants completed the questionnaire voluntarily. In addition, participants were undergraduate students recruited from four public universities in China. Thus, participants are adults and not minors, and we do not need to obtain consent from parents or guardians.
Procedure and participants
Our work is situated within an environmental context the COVID-19 pandemic. All variables were assessed with participants’ self-reports in three anonymous online surveys. Data were collected in three waves to minimize common method bias [ 53 ]. In the first-wave survey (Time 1), participants were asked to report their academic workload, separation from school, fears of contagion, and necessary demographic information. In Time 1, 1072 completed questionnaires were returned. One week later (Time 2), students evaluated their level of perceived stress. Time 2 questionnaires were distributed to the 1072 students, with 945 completed questionnaires being returned. Finally, one week after the second-wave survey (Time 3), students evaluated their physical and psychological health. At Time 3, 867 complete questionnaires were returned.
The average age of college undergraduates was 20.17 years, with 69 percent female. There are 348 freshmen, accounting for 40.1%; 200 sophomores, accounting for 23.1%; 305 junior students, accounting for 35.2%; 14 senior students, accounting for 1.6%. The average number of online courses is 8.41. Only 29.2% of the students rated the quality of online courses as good or very good. Nearly half of the participants said they wanted or very much wanted the school to start soon (49.2%). Of the 867 college students who had participated, 56.2% of them were concerned or very concerned about the possibility of contracting COVID-19 after the semester began. The demographic profile of the survey participants is presented in Table 1 .
| Variables | Frequency | Percentage |
|---|---|---|
| 17–20 | 534 | 61.6% |
| 21–24 | 328 | 37.8% |
| 24–30 | 5 | 0.6% |
| Female | 598 | 69.0% |
| Male | 269 | 31.0% |
| Freshman year | 348 | 40.1% |
| Sophomore year | 200 | 23.1% |
| Junior year | 305 | 35.2% |
| Senior year | 14 | 1.6% |
| 1–5 | 89 | 10.3% |
| 6–10 | 599 | 69.1% |
| 11–15 | 171 | 19.8% |
| 16–20 | 7 | 0.8% |
We translated the measures from English to Chinese following the commonly used translation/back-translation procedure. All measures are reported in S1 Appendix . Unless otherwise noted, participants responded to all items on a 7-point scale (from 1 = strongly disagree to 7 = strongly agree).
It was measured using the three-item scale developed by Hystad et al. [ 35 ]. Items included: “I am spending a lot of time thinking about how this semester’s grades could negatively affect my educational and career goals,” “I am worrying a great deal about the effect this semester’s grades will have on my future,” and “I find myself very concerned about the grades I am likely to receive this semester.” Cronbach’s alpha in their study was .85, which suggests that this scale has good reliability. In the current study, Cronbach’s α of this variable is .883.
Separation from school was measured using the attachment avoidance scale developed by Smith et al. [ 54 ]. The scale has fifteen-item. An example of a reworded scale item is “I find it difficult to allow myself to depend on my group.” Factor analytic results in their research suggested that the scale has good reliability. In our current study, we reworded to refer to participants’ classmates rather than their social group. An example of a reworded scale item is “I find it difficult to allow myself to depend on my classmates.” Cronbach’s α of this variable is .929.
We developed a six-item scale to assess participants’ fears of COVID-19 infection. Six items included “In public, I don’t care about touching the door handle without protection,” “In public, I don’t mind sitting in a chair that has just been sat on,” “In an elevator, I don’t mind pushing a button without protection,” “When I’m in a crowded place, I don’t worry about coronavirus from other people,” “I don’t worry about infection if other people don’t wear masks,” “Wearing a mask would make me feel safe.” In the current study, Cronbach’s α of this variable is .842. The results of confirmatory factor analysis are shown that χ2 = 74.424; df = 8; RMSEA = .098; CFI = .982; TLI = .966; SRMR = .043. Thus, this scale has acceptable reliability and validity.
Perceived stress
The 10-item Perceived Stress Scale [ 55 ] was used to measure the student’s stress level in the past month. Participants responded to the items on a 5-point scale (from1 = never to 5 = very often). A sample item is “In the last month, how often have you felt nervous and “stressed”?” In our research, Cronbach’s α of this variable is .792.
Physical and psychological health
The CHQ-12 of the Chinese version was used to measure physical and psychological health. The CHQ-12 has been widely used in Chinese populations. The 12 items included headaches, heart palpitations, chest pain or tightening, trembling or pins and needles, sleeplessness, nervousness, and hopelessness. Participants responded to the items on a 4-point scale (1 = not at all, 4 = more than usual). A higher score represented a more severe psychosocial impairment. In our research, Cronbach’s α of this variable is .895.
Control variables
We controlled students’ age, gender, grade, and the number of online courses in the study.
Analysis strategy
First, we conducted a series of confirmatory factor analyses ( CFA ) in order to test the discriminant validity of the five prime constructs (academic workload, separation from school, fears of contagion, perceived stress, and health). CFA, as an empirical research technology, is affiliated with structural equation modeling. Therefore, it is necessary to judge the fitting situation according to the fitting indexes from the structural equation model. Common fitting indexes include chi-square( χ2 ), degree of freedom ( df ), CFI , TLI , RMSEA , and S RMR . Specifically, if the ratio of chi square to degree of freedom is less than 5, the model is generally acceptable. When CFI and TLI are higher than 0.9, the model fits well. The smaller the RMSEA and SRMR , the better the result, and in particular, when it is below 0.08, the model is acceptable. Second, we performed Harman’s single-factor test to explore the potential influence of common method variance. No single factor accounting for more than 50% of the variance of all the relevant items indicates that the results are acceptable. Third, we calculated Pearson’s correlation coefficient using SPSS Version 21, which reflects the effect of change in one variable when the other variable changes. Fourth, we tested our hypotheses using a path analysis in Mplus Version 8.3. To examine mediation (Hypothesis 5,6, and 7), we used a bootstrap simulation with 1,000 replications to create our bias-corrected 95% confidence intervals (CIs) around our indirect effects. The bootstrap approach is a more robust strategy than the causal step procedure for small samples for assessing indirect effects and a useful method for avoiding power problems relating to a non-normal sampling of the indirect effect. When the 95% confidence interval of the path coefficient does not contain zero, the mediating effect is significant.
Confirmatory factor analyses
Table 2 presents the CFA results. As shown, the baseline five-factor model fitted the data well ( χ2 = 3020.006; df = 965; RMSEA = .050; CFI = .920; TLI = .914; SRMR = .064). Against this baseline five-factor model, we tested four alternative models: model 1 was a four-factor model with academic workload merged with perceived stress to form a single factor ( χ2 = 5405.203; df = 969; RMSEA = .073; CFI = .827; TLI = .815; SRMR = .112); model 2 was three-factor model with separation from school merged with academic workload and perceived stress to form a single factor ( χ2 = 6756.895; df = 972; RMSEA = .083; CFI = .774; TLI = .760; SRMR = .096); model 3 was a two-factor model, with fears of contagion merged with separation from school, academic workload, and perceived stress to form a single factor ( χ2 = 9752.729; df = 974; RMSEA = .102; CF I = .658; TLI = .636; SRMR = .110) and model 4 was a one-factor model with five constructs merged with one factor ( χ2 = 13665.328; df = 975; RMSEA = .123; CFI = .505; TLI = .475; SRMR = .143). As Table 2 shows, the fit indexes supported the hypothesized five-factor model, providing evidence of the construct distinctiveness of fears of contagion, separation from school, academic workload, and perceived stress and health.
| Model | Factors | χ | df | Δχ | RMSEA | CFI | TLI | SRMR |
|---|---|---|---|---|---|---|---|---|
| Baseline model | Five factors | 3020.006 | 965 | 0.050 | 0.920 | 0.914 | 0.064 | |
| Model 1 | Four factors | 5405.203 | 969 | 2385.197** | 0.073 | 0.827 | 0.815 | 0.112 |
| Model 2 | Three factors | 6756.895 | 972 | 3736.889** | 0.083 | 0.774 | 0.760 | 0.096 |
| Model 3 | Two factors | 9752.729 | 974 | 6732.723** | 0.102 | 0.658 | 0.636 | 0.110 |
| Model 4 | One factor | 13665.328 | 975 | 10645.322** | 0.123 | 0.505 | 0.475 | 0.143 |
Note: AW = academic workload; SFS = separation from school; FOC = fears of contagion; PS = perceived stress; Two factors = AW+SFS+FOC+PS, Health; Three factors = AW+SFS+PS, FOC, Health; Four factors = AW+PS, SFS, FOC, Health.
Tests for common method variance
Because we collected student’s self-report of fears of contagion, separation from school, academic workload, and perceived stress and health in the study, common method variance (CMV) may present as a problem. Therefore, we measured different constructs at different time points to decrease common method variance as much as possible [ 56 ] and showed high respect for the security, anonymity, and privacy of research objects and informants. In addition, the results of Harman’s single-factor test suggest that an exploratory factor analysis of all items explained 68.86% of the total variance, and the largest factor accounted for only 24.73% of the variance.
Descriptive statistics
The bivariate Pearson Correlation produces a sample correlation coefficient, which measures the strength and direction of linear relationships between pairs of continuous variables. Reported in Table 3 are the means, standard deviations and bivariate correlations of variables. Academic workload, separation from school, fears of contagion, and perceived stress were all negatively correlated with health ( r = -.121, p < .01; r = -.289, p < .01; r = -.242, p < 0.01; r = -.225, p < 0.01, respectively). Academic workload, separation from school, and fear of contagion, were all positively correlated with perceived stress ( r = .152, p < .01; r = .207, p < .01; r = .133, p < 0.01, respectively). It appears that these findings preliminarily provided support for our hypotheses.
| Variables | M | SD | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|---|
| 1. Age | 20.170 | 1.393 | ||||||
| 2. Number of online courses | 8.410 | 2.804 | .368 | |||||
| 3. Academic workload | 4.900 | 1.363 | .013 | .047 | ||||
| 4. Fears of contagion | 3.093 | 1.237 | -.040 | -.064 | .009 | |||
| 5. Separation from school | 3.358 | 1.059 | -.040 | .053 | .014 | .171 | ||
| 6. Perceived stress | 3.064 | .455 | -.013 | .014 | .152 | .133 | .207 | |
| 7. Health | 3.075 | .547 | -.011 | .015 | -.121 | -.242 | -.289 | -.225 |
** = p < 0.01
* = p < 0.05.
Hypothesis testing
We performed structural equation modeling (SEM) to test the proposed hypotheses and summarized the standardized values of the path coefficients and their significance levels in Fig 2 . The results showed significant positive path coefficients from academic workload to perceived stress ( β = .211, SE = .040, p < .01), providing empirical evidence in support of H1a. Furthermore, academic workload was shown to have a negative effect on health ( β = -.053, SE = .037, n . s .), not providing empirical support for H1b. We also demonstrated that separation from school had a positive association with perceived stress ( β = .324, SE = .043, p < .01) and had a negative association with health ( β = -.252, SE = .039, p < .01), providing empirical evidence in support of H2a and H2b. Moreover, our results showed that fears of contagion were significantly related to perceived stress ( β = .121, SE = .039, p < 0.01) and were significantly related to health ( β = -.088, SE = .035, p < .05), providing empirical evidence in support of H3a and H3b. Perceived stress had a negative effect on health ( β = -.240, SE = .050, p < .01), providing empirical evidence in support of H4.

We further examined the mediating role of perceived stress with nonparametric bootstrapping procedures. As shown in Table 4 , the influence of academic workload on health was mediated by perceived stress because the indirect influence of academic workload on health registered the value of b at -.051 ( SE = .016, p = .001), with the 95% CI [-.081, -.028]. Therefore, H5 was supported. Similarly, the influence of separation from school on health was mediated by perceived stress because the indirect influence of separation from school on health registered the value of b at -.078 ( SE = .020, p = .000), with the 95% CI [-.113, -.049]. Therefore, H6 was supported. The influence of fear of contagion on health was mediated by perceived stress because the indirect influence of fear of contagion on health registered the value of b at -.029 ( SE = .012, p = .014), with the 95% CI [-.053, -.013]. Therefore, H7 was supported.
| Indirect paths | Effects | SE | Lower 5% | Upper 5% | Results | |
|---|---|---|---|---|---|---|
| AW→Perceived stress→ Health | -0.051 | 0.016 | 0.001 | -0.081 | -0.028 | Supported |
| SFS→Perceived stress→ Health | -0.078 | 0.020 | 0.000 | -0.113 | -0.049 | Supported |
| FOC→Perceived stress→Health | -0.029 | 0.012 | 0.014 | -0.053 | -0.013 | Supported |
Note: AW = academic workload; SFS = separation from school; FOC = fears of contagion; We report the 95% confidence intervals (CIs) calculated using 1,000 bootstrap samples, with lower and upper limits in brackets.
The spread of COVID-19 is becoming unstoppable and has already influenced people and countries all over the world. Holmes et al. [ 57 ] called for that multidisciplinary science research must be central to the international response to the COVID-19 pandemic and provide evidence-based guidance on responding to promoting people’s health and wellbeing during the COVID-19 pandemic. To answer this call, we focus on college students getting home-schooling to explore their stress and health problems. Although the COVID-19 is still spreading rapidly and widely worldwide, it has been effectively controlled in China. What has happened in China shows that quarantine, social distancing, and isolation of infected populations can contain the epidemic. Whereas individual coping strategies are possible (e.g., social distancing), the spread of the virus at a state level is still beyond any given individual’s control. The continuous spread of the epidemic, strict isolation measures, and delays in starting schools, colleges, and universities across the country are expected to influence college students. Considering stress and anxiety associated with the current COVID-19 pandemic for college students [ 49 ], it is urgent for the society and management departments to understand the actual situation of college students timely and accurately. Based on the Transactional Model of Stress and coping [ 49 ], this study explored the influence of academic workload, separation from school, and fears of contagion on college students’ physical and physiological health, as well as the mediating effect of perceived stress in those relationships.
The current study contributes to the existing literature. First, the present study goes beyond previous literature on college students’ health during the epidemic by integrating three types of stressors from different fields in the proposed model. As highlighted in previous research on college students’ academic stress, preparing exams, courses, and papers should exhibit a negative effect on individual health. During the COVID-19 outbreak, Chinese college students’ learning was not suspended, but they attend the various courses offered online follow the regular schedule. While those measures of the virtual semester ensure regular study, they also cause stress on students. In addition, given the importance of social groups to an individual’s identity and self-worth, we found that college students were separated from their classmates during the COVID-19 epidemic, which brought them stress and anxiety. Previous evidence suggests that college students usually keep attachment relationships with their social group [ 12 , 58 ]. Attachment figures are usually parents, but may also be siblings, grandparents, or group. Unlike most previous studies that focused on separation from parents [ 9 ], this study focused on the influence of departure from school and schoolmates, which is particularly relevant to the epidemic situation. For college students attached to their school or classmates, school-closure is a kind of separation experience, which may be different from their experience when they leave home. Considering the relatively new separation (separation from school) caused by the outbreak of COVID-19, our findings suggest that separation from school was positively related to college students’ perceived stress during home-schooling. Finally, we found that exposure to a potentially infectious environment would lead to people’s stress, which is in line with previous research that pointed out the negative correlation between the risk of infection and life satisfaction [ 58 ]. Similar results have been found in the study of College Students’ psychological adjustment during SARS. For example, Main et al. [ 12 ] found that the experience of SARS-related stressors was positively associated with psychological symptoms for Chinese college students during the outbreak. Thus, we supposed that during an acute large-scale epidemic such as the SARS and COVID-19 epidemic, even among persons who were not directly contaminated with the disease, the psychological influence of the outbreak on them was significant. In doing so, we identified three important stressors for college students in the COVID-19 pandemic, providing essential inspiration for college students to maintain their physical and mental health during the current epidemic.
Second, based on a transactional model view, we provide a plausible mechanism for explaining the association between academic workload, separation from school, and fears of contagion and health. The transactional model posits that stress responses emerge from appraisal processes that begin when individuals experience a stressor. During primary appraisal, perceptions of elements of the focal stressor are used to determine the degree of threat or harm that this stressor represents; during secondary appraisal, individuals consider if and how they can resolve the underlying stressor. COVID-19, a contagious respiratory illness, is an ongoing, global health crisis, and the greatest challenge we have faced since World War II [ 59 ]. The COVID-19 pandemic is a grim but illustrative anxiety-inducing stressor; an uncertain and ongoing threat that cannot be resolved via individual efforts. When individuals have few resources, ways, or abilities at their disposal to deal with the stressors, they generate stress and anxiety and ultimately lead to negative consequences. Thus, perceived stress may be a mediator, transmitting the effects of academic workload, separation from school, and fears of contagion on health-related outcomes. These findings suggest that academic workload, separation from school, and fears of contagion may contribute to youth’s general perceived stress, which in turn, may negatively influence their physical and psychological health. Our findings supported Lorenzo-Blanco and Unger’s [ 60 ] and Sariçam’s [ 61 ] proposition that perceived stress plays an important role in influencing psychological well-being.
The results of the current study are of significance to practice and policy. First, the administrative department needs to raise the awareness of potential physical and mental health influences of home-schooling during the outbreak. While taking effective prevention measures, the government should guide the mass media to spread positive information and control rumors. Communication can serve as an important resource in dealing with the difficulties of family matters. For instance, parents can share their life experiences with their children and advocate for them to develop good living habits and enjoy a healthy lifestyle. Psychologists can communicate with students by social media platforms to help them cope with mental health issues caused by domestic conflicts, tension with parents, and anxiety from becoming infected. In addition, schools play an important role not only in providing students with educational materials but also in providing students with opportunities to interact with teachers and students. Schools should also provide guidelines and principles for effective online learning and ensure that content meets educational requirements. Nevertheless, it is also important not to overburden students.
Limitations
Despite the potential contribution that the present study makes to the mental health field, limitations of the study should be noted. First, a potential limitation is that all measures came from the same source, raising the potential for same-source measurement biases. However, we used a variety of means to reduce this issue, including varying our response scales and separating our measures in time. Further, as we were interested in how college students have dealt with the pandemic over time, focusing on self-reported experiences was appropriate. Another potential limitation of our study is concerned with causality. Hence, future research should conduct the experimental design or utilize the longitudinal data to ensure the conclusion reflects causation. Finally, our research reflects only the impact of the COVID-19 pandemic for college students, and much work is needed to gain a complete understanding of the implications of this crisis for students. Future research could consider how individual factors, such as self-concept, and contextual factors, such as social support, may influence college students’ response to perceived stress. Moreover, research focused on within-person fluctuations of perceived stress during this time would also be instructive, as there is no doubt that individuals have experienced considerable variability on a daily basis during the pandemic.
Conclusions
Confronting the COVID-19 outbreak and variously rigorous measures to prevent the spreading of the infection, college students may feel stress and have more or fewer health problems. Academic workload, psychological separation from school, and fear of contagion were positively associated with the perceived stress and negatively associated with physical and psychological health. In addition, perceived stress is a key mechanism in the relationships between three stressors and two forms of health. This study makes not only unique theoretical contributions to the stress and health literature during the COVID-19 outbreak but also offers novel practical implications for joint efforts from all circles of society to ensure students’ health.
Supporting information
S1 appendix, funding statement.
National Natural Science Foundation of China (71572170). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2021; 16(2): e0246676.
Decision Letter 0
30 Dec 2020
PONE-D-20-32875
College students’ stress and health during the COVID-19 outbreak: the effects of academic workload, separation from school, and fears of contagion
Dear Dr. Yang,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
==============================
One expert in this field has carefully reviewed your submission and he pointed out some merits in your work. However, a major concern regarding the sampling should be tackled in the revision. That says, the samples seemed to be different across time points and the authors should provide clear rationale and how they take care of the methodology issues if they really used different samples. This is a fatal point for me to judge whether the revision can be accepted.
Please submit your revised manuscript by Feb 13 2021 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: http://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols
We look forward to receiving your revised manuscript.
Kind regards,
Chung-Ying Lin
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please ensure that you include a title page within your main document.
We do appreciate that you have a title page document uploaded as a separate file, however, as per our author guidelines ( http://journals.plos.org/plosone/s/submission-guidelines#loc-title-page ) we do require this to be part of the manuscript file itself and not uploaded separately.
Could you therefore please include the title page into the beginning of your manuscript file itself, listing all authors and affiliations.
3. Please provide additional details regarding participant consent.
In the ethics statement in the Methods and online submission information, please ensure that you have specified (i) whether consent was informed and (ii) what type you obtained (for instance, written or verbal, and if verbal, how it was documented and witnessed). If your study included minors, state whether you obtained consent from parents or guardians. If the need for consent was waived by the ethics committee, please include this information.
If you are reporting a retrospective study of medical records or archived samples, please ensure that you have discussed whether all data were fully anonymized before you accessed them and/or whether the IRB or ethics committee waived the requirement for informed consent. If patients provided informed written consent to have data from their medical records used in research, please include this information.
4. Please include additional information regarding the survey or questionnaire used in the study and ensure that you have provided sufficient details that others could replicate the analyses.
For instance, if you developed a questionnaire as part of this study and it is not under a copyright more restrictive than CC-BY, please include a copy, in both the original language and English, as Supporting Information, or include a citation if it has been published previously.
5. In the Methods, please discuss whether and how the questionnaire was validated and/or pre-tested. If these did not occur, please provide the rationale for not doing so.
6. We note that you have indicated that data from this study are available upon request. PLOS only allows data to be available upon request if there are legal or ethical restrictions on sharing data publicly. For more information on unacceptable data access restrictions, please see http://journals.plos.org/plosone/s/data-availability#loc-unacceptable-data-access-restrictions .
In your revised cover letter, please address the following prompts:
a) If there are ethical or legal restrictions on sharing a de-identified data set, please explain them in detail (e.g., data contain potentially sensitive information, data are owned by a third-party organization, etc.) and who has imposed them (e.g., an ethics committee). Please also provide contact information for a data access committee, ethics committee, or other institutional body to which data requests may be sent.
b) If there are no restrictions, please upload the minimal anonymized data set necessary to replicate your study findings as either Supporting Information files or to a stable, public repository and provide us with the relevant URLs, DOIs, or accession numbers. For a list of acceptable repositories, please see http://journals.plos.org/plosone/s/data-availability#loc-recommended-repositories .
We will update your Data Availability statement on your behalf to reflect the information you provide
7. Your ethics statement should only appear in the Methods section of your manuscript. If your ethics statement is written in any section besides the Methods, please delete it from any other section.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Partly
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #1: Yes
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: No
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: In general, this is a good study considering the concept backed by a sound theoretical framework. However, authors need to improve the study’s write-up in several sections of the manuscript especially the English language. I will strongly recommend a native English Language speaker to edit it.
Knowing that we cannot make a causal inference from this study, it will be more prudent to use associate/relate rather than affect.
Page 8: Procedure and Participants
Can authors justify why they used different samples for each Time wave and how they resolve the confounding issues arising from this method?
Also, there seems to be a typo in the number of data collected for wave one.
Authors should start a sentence with words and not figures as did with 49.2% and 56.2%.
Authors may want to revise this section incorporating the number of items per scale, the original developer (author) of each scale, original psychometric property, and how it was scored in this study. Much more importantly, the psychometric properties of these measures for this study.
Data analysis
Authors may end the method section with the above sub-title. This section may detail the types of analytic tools used and the purposes for using them. Cut-off or other criteria related to these analytic tools may be written here.
Tests for common method variance: The first sentence under this sub-section seems incomplete.
Table 3: for bivariate relationships, authors may take out categorical variables from the results as it does not make meaning.
Table 4: Authors may add further details to the table as effect and CI are not enough to get a better picture of the analysis/data.
Page 14: “Given the ongoing COVID -19 epidemic to inducing panic, and anxiety [49], therefore, timely and…” this sentence is difficult to understand, please revise.
Authors may try to relate the theory to the findings thoroughly.
Explaining the “SFS” with separation anxiety disorder is too far-fetched (exaggerated and unconvincing). Besides, these are students above 17 year old. SFS have a role to play in the lives of students but not from the angle of separation anxiety but probably as a supporting/coping strategy.
The way the authors reported the procedure of the data collection did not reflect a cross-sectional design. Hence, it will make readers doubt the authenticity/validity of this study.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
13 Jan 2021
A Point-by-Point Response to Editor Comments
Your comment:
One expert in this field has carefully reviewed your submission and he pointed out some merits in your work. However, a major concern regarding the sampling should be tackled in the revision. That says, the samples seemed to be different across time points and the authors should provide clear rationale and how they take care of the methodology issues if they really used different samples. This is a fatal point for me to judge whether the revision can be accepted.
Our response:
Thank you for giving us the opportunity to revise our paper. We hope that you find this revised manuscript significantly improved and up to your expectation.
Thank you for your question. Indeed, although the numbers of participants are different across time points, we didn’t use different samples in our research.
First, we explain what the time-lagged design is and why it is used in our research.
The time-lagged design is a type of research design in which the same person reports information or data of different variables at different time points, which has been widely used in science research (e.g., Laschinger & Fida, 2014; SPENCE LASCHINGER & Finegan, 2008; Kilroy et al., 2017). The time-lagged design can ensure the constructs we concerned would be less influenced by common method bias (e.g., Podsakoff et al. 2003). Generally, the independent variables (IV) are first collected at Time-1, and then the mediation variables (mediators) at Time-2, and finally the dependent variables (DV) at Time-3 from the same person. In our research, academic workload, separation from school, and fears of contagion are independent variables, perceived stress is a mediator, and health is a dependent variable. Thus, we used the time-lagged design and these data of different variables were collected at three time points with one-week interval.
Second, we describe how to conduct the collection of data and explain that we didn’t use different samples in our study.
In the first-wave survey (Time 1), participants were asked to report their academic workload, separation from school, fears of contagion, and necessary demographic information, and we got 1072 questionnaires. One week later (Time 2), perceived stress needs to be measured, and we distributed questionnaires to the 1,072 people who had participated in the first-wave survey. However, 127 participants quit the survey and we got 945 questionnaires at Time 2 (valid response rate: 945/1072=88.15%). One week after the second-wave survey (Time 3), physical and psychological health needs to be measured, and we distributed questionnaires to the 945 people who had participated in both the first-wave and second-wave survey. However, 78 participants quit the survey, and we got 867 questionnaires at Time 3(valid response rate: 867/945=91.95%). That is, we got completed data, including the data of all variables used in our research from 867 participants who participated in three surveys. In the data analysis, we used data from only 867 participants. Because some participants did not participate fully in the three surveys, their data was incomplete and thus could not be included in the study. That is, because some participants dropped out of the survey during the data collection process, the number of participants varied at different time points, as shown in Figure 1.
Podsakoff, P. M., MacKenzie, S. B., Lee, J. Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. Journal of applied psychology, 88(5), 879.
Laschinger, H. K. S., & Fida, R. (2014). A time-lagged analysis of the effect of authentic leadership on workplace bullying, burnout, and occupational turnover intentions. European Journal of Work and Organizational Psychology, 23(5), 739-753.
SPENCE LASCHINGER, H. K., & Finegan, J. (2008). Situational and dispositional predictors of nurse manager burnout: a time‐lagged analysis. Journal of Nursing Management, 16(5), 601-607.
Kilroy, S., Flood, P. C., Bosak, J., & Chênevert, D. (2017). Perceptions of high‐involvement work practices, person‐organization fit, and burnout: A time‐lagged study of health care employees. Human Resource Management, 56(5), 821-835.
A Point-by-Point Response to Reviewer Comments
Reviewer #1: Partly
Thank you very much. Following your suggestions, we carefully revised the manuscript. All changes were marked in blue text. Below please see our point-to-point response to your comments. We hope that you find this revised manuscript significantly improved and up to your expectation.
Reviewer #1: Yes
Thank you very much for your recognition and support!
Reviewer #1: No
Thank you very much. We would like to provide and share the data we used in our research.
Reviewer #1: In general, this is a good study considering the concept backed by a sound theoretical framework. However, authors need to improve the study’s write-up in several sections of the manuscript especially the English language. I will strongly recommend a native English Language speaker to edit it.
Thank you very much for your recognition and support! We have had a professional copy editor with English as her first language to thoroughly go through the draft. We are confident that the writing has been improved and hope that the revised manuscript will meet your requirements. All changes were marked in blue in the revised manuscript.
Thank you very much. Following your suggestion, we use associate/relate rather than affect in the revised manuscript. All changes were marked in blue text.
Page 2 Line 44-Page 8 Line 208:
Page 8 Line 210-Page 9 Line 220:
Thank you very much for your advice. We have corrected the typo in the number of data collected for wave one. In addition, we have started the sentence with words and not figures.
Please see Page 9 Line 245- Line 247:
In the first-wave survey (Time 1), participants were asked to report their academic workload, separation from school, fears of contagion, and necessary demographic information. In Time 1, 1072 completed questionnaires were returned.
Please see Page 10 Line 254- Line 256:
Nearly half of the participants said they wanted or very much wanted the school to start soon (49.2%). Of the 867 college students who had participated, 56.2% of them were concerned or very concerned about the possibility of contracting COVID-19 after the semester began.
Thank you very much. We carefully revised this section. In the revised manuscript, we described the number of items per scale, the original developer of each scale, the reliability of the original scale, and the reliability of scale in our research. All items we used in the research has been provided in Appendix. In addition, we described that participants responded to items on a 7-point scale or 5-point scale. Specifically, the scale of physical and psychological health has its Chinese version, and thus we can directly use it in our research. The scales of academic workload, separation from school, and perceived stress have their English version, and thus we followed the translation/back-translation procedure to translate English to Chinese. Finally, we developed the scale of fears of contagion, and test its reliability and validity. Based on the results of Cronbach's α, we found that the psychometric properties of these measures for this study are acceptable.
Please see Page 10 Line 259- Page 12 Line 294:
We translated the measures from English to Chinese following the commonly used translation/back-translation procedure. All measures are reported in Appendix A. Unless otherwise noted, participants responded to all items on a 7-point scale (from 1=strongly disagree to 7=strongly agree).
It was measured using the three-item scale developed by Hystad et al. [35]. Items included: “I am spending a lot of time thinking about how this semester’s grades could negatively affect my educational and career goals,” “I am worrying a great deal about the effect this semester’s grades will have on my future,” and “I find myself very concerned about the grades I am likely to receive this semester.” Cronbach’s alpha in their study was .85, which suggests that this scale has good reliability. In the current study, Cronbach's α of this variable is .883.
Separation from school was measured using the attachment avoidance scale developed by Smith et al. [54]. The scale has fifteen-item. An example of a reworded scale item is “I find it difficult to allow myself to depend on my group.” Factor analytic results in their research suggested that the scale has good reliability. In our current study, we reworded to refer to participants' classmates rather than their social group. An example of a reworded scale item is “I find it difficult to allow myself to depend on my classmates.” Cronbach's α of this variable is
We developed a six-item scale to assess participants’ fears of COVID-19 infection. Six items included “In public, I don't care about touching the door handle without protection,” “In public, I don’t mind sitting in a chair that has just been sat on,” “In an elevator, I don’t mind pushing a button without protection,” “When I’m in a crowded place, I don’t worry about coronavirus from other people,” “I don't worry about infection if other people don't wear masks,” “Wearing a mask would make me feel safe.” In the current study, Cronbach's α of this variable is .842. The results of confirmatory factor analysis are shown that χ2 = 74.424; df = 8; RMSEA = .098; CFI =.982; TLI = .966; SRMR = .043. Thus, this scale has acceptable reliability and validity.
The 10-item Perceived Stress Scale [55] was used to measure the student’s stress level in the past month. Participants responded to the items on a 5-point scale (from1=never to 5=very often). A sample item is “In the last month, how often have you felt nervous and “stressed”?” In our research, Cronbach's α of this variable is .792.
The CHQ-12 of the Chinese version was used to measure physical and psychological health. The CHQ-12 has been widely used in Chinese populations. The 12 items included headaches, heart palpitations, chest pain or tightening, trembling or pins and needles, sleeplessness, nervousness, and hopelessness. Participants responded to the items on a 4-point scale (1= not at all, 4=more than usual). A higher score represented a more severe psychosocial impairment. In our research, Cronbach's α of this variable is .895.
Please see Page 24 Line 622- Page 26 Line 677:
1. I am spending a lot of time thinking about how this semester’s grades could negatively affect my educational and career goals.
2. I am worrying a great deal about the effect this semester’s grades will have on my future.
3. I find myself very concerned about the grades I am likely to receive this semester.
1. I find it difficult to allow myself to depend on my group.
2. I sometimes worry that I will be hurt if I allow myself to become too close to my group.
3. I am nervous when my group gets too close.
4. My desire to feel completely at one sometimes scares my group away.
5. I prefer not to depend on my group or to have my group depend on me.
6. I often worry that my group does not really accept me.
7. I am comfortable not being close to my group.
8. I often worry my group will not always want me as a member.
9. I am somewhat uncomfortable being close to my group.
10. My group is never there when I need it.
11. I find it difficult to completely trust my group.
12. I find my group is reluctant to get as close as I would like.
13. I am not sure that I can always depend on my group to be there when I need it.
14. I sometimes worry that my group doesn't value me as much as I value my group.
15. I want to be emotionally close with my group, but I find it difficult to trust my group completely or to depend on my group.
1. In public, I don't care about touching the door handle without protection.
2. In public, I don’t mind sitting in a chair that has just been sat on.
3. In an elevator, I don’t mind pushing a button without protection.
4. When I’m in a crowded place, I don't worry about coronavirus from other people.
5. I don't worry about infection if other people don't wear masks.
6. Wearing a mask would make me feel safe.
1. In the last month, how often have you been upset because of something that happened unexpectedly?
2. In the last month, how often have you felt that you were unable to control the important things in your life?
3. In the last month, how often have you felt nervous and “stressed”?
4. In the last month, how often have you felt confident about your ability to handle your personal problems?
5. In the last month, how often have you felt that things were going your way?
6. In the last month, how often have you found that you could not cope with all the things that you had to do?
7. In the last month, how often have you been able to control irritations in your life?
8. In the last month, how often have you felt that you were on top of things?
9. In the last month, how often have you been angered because of things that were outside of your control?
10. In the last month, how often have you felt difficulties were piling up so high that you could not overcome them?
Have you recently...
1. been suffering from headache or pressure in your head?
2. had palpitation and worried that you might have heart trouble?
3. had discomfort or a feeling of pressure in your chest?
4. been suffering from shaking or numbness of your limbs?
5. lost much sleep through worry?
6. been taking things hard?
7. been getting along well with your family or friends?
8. been losing confidence in yourself?
9. been feeling nervous and strung-up all the time?
10. been feeling hopeful about your future?
11. been worried about your family or close friends?
12. felt that life is entirely hopeless?
Thank you very much for your advice. Following your suggestion, we have added the sub-title and provide more details about the types of analytic tools used, the purposes for using them and so on.
Please see Page 12 Line 297- Line 314:
First, we conducted a series of confirmatory factor analyses (CFA) in order to test the discriminant validity of the five prime constructs (academic workload, separation from school, fears of contagion, perceived stress, and health). CFA, as an empirical research technology, is affiliated with structural equation modeling. Therefore, it is necessary to judge the fitting situation according to the fitting indexes from the structural equation model. Common fitting indexes include chi-square(χ2), degree of freedom (df), CFI, TLI, RMSEA, and SRMR. Specifically, if the ratio of chi square to degree of freedom is less than 5, the model is generally acceptable. When CFI and TLI are higher than 0.9, the model fits well. The smaller the RMSEA and SRMR, the better the result, and in particular, when it is below 0.08, the model is acceptable. Second, we performed Harman’s single-factor test to explore the potential influence of common method variance. No single factor accounting for more than 50% of the variance of all the relevant items indicates that the results are acceptable. Third, we calculated Pearson’s correlation coefficient using SPSS Version 21, which reflects the effect of change in one variable when the other variable changes. Fourth, we tested our hypotheses using a path analysis in Mplus Version 8.3. To examine mediation (Hypothesis 5,6, and 7), we used a bootstrap simulation with 1,000 replications to create our bias-corrected 95% confidence intervals (CIs) around our indirect effects. The bootstrap approach is a more robust strategy than the causal step procedure for small samples for assessing indirect effects and a useful method for avoiding power problems relating to a non-normal sampling of the indirect effect. When the 95% confidence interval of the path coefficient does not contain zero, the mediating effect is significant.
Thank you very much for your advice. First, we revised the first sentence under this sub-section and make it complete. Second, we deleted the section of categorical variables in Table 3. Third, we provide more details about the analysis/data.
Please see Page 13 Line 332- Line 338:
Tests for Common Method Variance
Because we collected student’s self-report of fears of contagion, separation from school, academic workload, and perceived stress and health in the study, common method variance (CMV) may present as a problem. Therefore, we measured different constructs at different time points to decrease common method variance as much as possible [56] and showed high respect for the security, anonymity, and privacy of research objects and informants. In addition, the results of Harman’s single-factor test suggest that an exploratory factor analysis of all items explained 68.86% of the total variance, and the largest factor accounted for only 24.73% of the variance.
Please see Page 14 Line 348- Line 349:
Please see Page 15 Line 372- Line 374:
Thank you very much for your advice. We have revised this confused sentence.
Please see Page 15 Line 375- Line 388:
The spread of COVID-19 is becoming unstoppable and has already influenced people and countries all over the world. Holmes et al. [57] called for that multidisciplinary science research must be central to the international response to the COVID-19 pandemic and provide evidence-based guidance on responding to promoting people’s health and wellbeing during the COVID-19 pandemic. To answer this call, we focus on college students getting home-schooling to explore their stress and health problems. Although the COVID-19 is still spreading rapidly and widely worldwide, it has been effectively controlled in China. What has happened in China shows that quarantine, social distancing, and isolation of infected populations can contain the epidemic. Whereas individual coping strategies are possible (e.g., social distancing), the spread of the virus at a state level is still beyond any given individual’s control. The continuous spread of the epidemic, strict isolation measures, and delays in starting schools, colleges, and universities across the country are expected to influence college students. Considering stress and anxiety associated with the current COVID-19 pandemic for college students [49], it is urgent for the society and management departments to understand the actual situation of college students timely and accurately.
Thank you very much for your advice. Following your suggestion, we integrated theory with our findings thoroughly in the revised manuscript.
Please see Page 15 Line 375- Page 17 Line 432:
The spread of COVID-19 is becoming unstoppable and has already influenced people and countries all over the world. Holmes et al. [57] called for that multidisciplinary science research must be central to the international response to the COVID-19 pandemic and provide evidence-based guidance on responding to promoting people’s health and wellbeing during the COVID-19 pandemic. To answer this call, we focus on college students getting home-schooling to explore their stress and health problems. Although the COVID-19 is still spreading rapidly and widely worldwide, it has been effectively controlled in China. What has happened in China shows that quarantine, social distancing, and isolation of infected populations can contain the epidemic. Whereas individual coping strategies are possible (e.g., social distancing), the spread of the virus at a state level is still beyond any given individual’s control. The continuous spread of the epidemic, strict isolation measures, and delays in starting schools, colleges, and universities across the country are expected to influence college students. Considering stress and anxiety associated with the current COVID-19 pandemic for college students [49], it is urgent for the society and management departments to understand the actual situation of college students timely and accurately. Based on the Transactional Model of Stress and coping [49], this study explored the influence of academic workload, separation from school, and fears of contagion on college students’ physical and physiological health, as well as the mediating effect of perceived stress in those relationships.
The current study contributes to the existing literature. First, the present study goes beyond previous literature on college students’ health during the epidemic by integrating three types of stressors from different fields in the proposed model. As highlighted in previous research on college students’ academic stress, preparing exams, courses, and papers should exhibit a negative effect on individual health. During the COVID-19 outbreak, Chinese college students’ learning was not suspended, but they attend the various courses offered online follow the regular schedule. While those measures of the virtual semester ensure regular study, they also cause stress on students. In addition, given the importance of social groups to an individual’s identity and self-worth, we found that college students were separated from their classmates during the COVID-19 epidemic, which brought them stress and anxiety. Previous evidence suggests that college students usually keep attachment relationships with their social group [12,58]. Attachment figures are usually parents, but may also be siblings, grandparents, or group. Unlike most previous studies that focused on separation from parents [9], this study focused on the influence of departure from school and schoolmates, which is particularly relevant to the epidemic situation. For college students attached to their school or classmates, school-closure is a kind of separation experience, which may be different from their experience when they leave home. Considering the relatively new separation (separation from school) caused by the outbreak of COVID-19, our findings suggest that separation from school was positively related to college students’ perceived stress during home-schooling. Finally, we found that exposure to a potentially infectious environment would lead to people’s stress, which is in line with previous research that pointed out the negative correlation between the risk of infection and life satisfaction [58]. Similar results have been found in the study of College Students’ psychological adjustment during SARS. For example, Main et al. [12] found that the experience of SARS-related stressors was positively associated with psychological symptoms for Chinese college students during the outbreak. Thus, we supposed that during an acute large-scale epidemic such as the SARS and COVID-19 epidemic, even among persons who were not directly contaminated with the disease, the psychological influence of the outbreak on them was significant. In doing so, we identified three important stressors for college students in the COVID-19 pandemic, providing essential inspiration for college students to maintain their physical and mental health during the current epidemic.
Second, based on a transactional model view, we provide a plausible mechanism for explaining the association between academic workload, separation from school, and fears of contagion and health. The transactional model posits that stress responses emerge from appraisal processes that begin when individuals experience a stressor. During primary appraisal, perceptions of elements of the focal stressor are used to determine the degree of threat or harm that this stressor represents; during secondary appraisal, individuals consider if and how they can resolve the underlying stressor. COVID-19, a contagious respiratory illness, is an ongoing, global health crisis, and the greatest challenge we have faced since World War II [59]. The COVID-19 pandemic is a grim but illustrative anxiety-inducing stressor; an uncertain and ongoing threat that cannot be resolved via individual efforts. When individuals have few resources, ways, or abilities at their disposal to deal with the stressors, they generate stress and anxiety and ultimately lead to negative consequences. Thus, perceived stress may be a mediator, transmitting the effects of academic workload, separation from school, and fears of contagion on health-related outcomes. These findings suggest that academic workload, separation from school, and fears of contagion may contribute to youth’s general perceived stress, which in turn, may negatively influence their physical and psychological health. Our findings supported Lorenzo-Blanco and Unger’s [60] and Sariçam’s [61] proposition that perceived stress plays an important role in influencing psychological well-being.
Thank you very much for your advice. Following your suggestion, we explained “SFS” from the point of attachment in the revised manuscript. From a supporting/coping strategy, we provided some advice to help college students keep healthy when they separate from school.
Please see Page 16 Line 397- Line 406:
In addition, given the importance of social groups to an individual’s identity and self-worth, we found that college students were separated from their classmates during the COVID-19 epidemic, which brought them stress and anxiety. Previous evidence suggests that college students usually keep attachment relationships with their social group [12,58]. Attachment figures are usually parents, but may also be siblings, grandparents, or group. Unlike most previous studies that focused on separation from parents [9], this study focused on the influence of departure from school and schoolmates, which is particularly relevant to the epidemic situation. For college students attached to their school or classmates, school-closure is a kind of separation experience, which may be different from their experience when they leave home. Considering the relatively new separation (separation from school) caused by the outbreak of COVID-19, our findings suggest that separation from school was positively related to college students’ perceived stress during home-schooling.
Thank you very much for your advice. We revised this point in the revised manuscript. Although we used a time-lagged design to collect data at different times, future research can conduct the experimental design or utilize the longitudinal data to ensure the conclusion reflects causation.
Please see Page 18 Line 445- Page 18 Line 458:
Submitted filename: Response to Reviewers.DOCX
Decision Letter 1
25 Jan 2021
College students’ stress and health in the COVID-19 pandemic: the role of academic workload, separation from school, and fears of contagion
PONE-D-20-32875R1
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Dear authors,
Thank you for addressing the reviewer's comments. There is only on minor issue remains and I believe that you can deal with it during the proof stage.
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #1: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #1: The authors have comprehensively revised the manuscript to my satisfaction. A minor comment though.
Authors should make sure that all p-values are exact (e.g., p=.032) than stating it as "p<.05".
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Acceptance letter
Dear Dr. Yang:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Chung-Ying Lin

IMAGES
COMMENTS
Abbott (2021) investigated stress caused by the COVID-19 pandemic and its related consequences and found that there is an increase in prevalence of stress, anxiety, and depression in the U.S. population from 11% to 42% due to this pandemic. The surge in stress among people is also during the rise of new COVID-19 covariant cases.
Stress reappraisal and mindset interventions have high potential to assist in stress management during the COVID‐19 pandemic based on their demonstrated efficacy in laboratory and selected applied contexts (Crum et al., 2013, 2017; Keech et al., 2019). Research demonstrating that such interventions are highly translatable and have consistent ...
The prevalence of depression, anxiety, physical discomfort, insomnia and post-traumatic stress disorder (PTSD) during the COVID-19 pandemic: Having a childbearing age: During the COVID/19 pandemic, pregnant women had lower scores of symptoms of depression, anxiety, and PTSD (all p < 0.05) compared to non-pregnant women. Sade et al., 2020
Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24-30, 2020. MMWR Morb Mortal Wkly Rep 2020;69 ...
The COVID-19 virus knows all about the human psyche. The virus is aware that we experience stress and become anxious when we keep a distance from other people and are forced to isolate ourselves from direct, physical contact with the people we love and cherish. Under conditons of stress and as we become more anxious, our vulnerability also ...
The first step to lower your stress is to keep a daily schedule. Make or maintain healthy habits and routines. This can help boost your mood and energy levels. Make sleep a priority. Get up at about the same time every day. Go to bed at about the same time every day. Make sure that you are getting enough restful sleep.
Worldwide surveys done in 2020 and 2021 found higher than typical levels of stress, insomnia, anxiety and depression. By 2022, levels had lowered but were still higher than before 2020. Though feelings of distress about COVID-19 may come and go, they are still an issue for many people. You aren't alone if you feel distress due to COVID-19.
Background Individuals face increased psychological distress during the COVID-19 pandemic. However, it's unknown whether choice of coping styles are influenced by COVID-19 in addition to known predictors. Methods Data from 26,016 UK adults in the UCL COVID-19 Social Study were analysed from 12/4/2020 15/5/2020. Regression models were used to identify predictors of coping styles (problem ...
Play with puzzles, a board game, do a treasure hunt, tackle a project, reorganize something, or start a new book that is unrelated to coronavirus coverage. Connect with others. "I can't stress ...
Making decisions has become more stressful compared with before the pandemic (day-to-day decisions: 55% vs. 33% and 16%; major decisions: 54% vs. 32% and 13%). Sometimes they are so stressed about the coronavirus pandemic that they struggle to make even basic decisions (50% vs. 31% and 5%).
Investigating the Prevalence of COVID-19-Related Sleep Disorders Among Individuals Recovering from COVID-19: A Cross-Sectional Analytical Study, Jundishapur Journal of Health Sciences, 15, 4 ...
Stress reduction tips for COVID-19. "Rather than dwell on nervousness, focus on the things you can control," Flanagan suggests. "When you move the locus of control from something outside yourself to inside yourself, you powerfully reduce anxiety and boost confidence.". He suggests the following steps to regain control and reduce stress.
During the acute phase of the pandemic, in the background of an increased level of stress and anxiety in the society due to COVID-19, it is essential that any emergency response should consider the component of mental health crisis management (Assari and Habibzadeh, 2020). This is relevant not only for patients showing COVID-19 symptoms, but ...
Higher COVID-19 related stress exposure led to an average increase of anxiety, depression, and general discomfort in children's and adolescents' lives4. Youth who were exposed to greater pandemic-related stressors exhibited higher rates of internalizing and externalizing psychopathology during stay-at-home orders and even six months later6.
The coronavirus disease 2019 (COVID-19) pandemic has placed unprecedented stress on the health care system globally, revealing the interconnectedness and fragility of its ecosystem. The resultant overwhelming burden of illness and mortality has threatened operations of health care institutions worldwide and the physical, emotional, and financial health of their workers.1 Health care workers ...
Once you have assessed your threat, then it is important to…. 2. Identify what you can control. When we encounter stress, any stress, it is important that we ask ourselves if we can do anything ...
Background Being in the frontline of the battle against COVID-19, nurses need to be capable of stress management to maintain their physical and psychological well-being in the face of a variety of stressors. The present study aims to explore the challenges, strategies, and outcomes of stress management in nurses who face and provide care to COVID-19 patients. Methods The present study is a ...
angry during a crisis. Talking to people you trust can help. Contact your friends and family. Don't use smoking, alcohol or other drugs to deal with your emotions. If you feel overwhelmed, talk to a health worker or counsellor. Have a plan, where to go to and how to seek help for physical and mental health needs if required.
COVID‐19 can also result in increased stress, anxiety, and depression among elderly people already dealing with mental health issues. Family members may witness any of the following changes to the behavior of older relatives 11 ; Irritating and shouting behavior. Change in their sleeping and eating habits.
I find myself continually reframing negative situations for them. Instead of focusing on the places we can't go because of COVID, we find a cool new place to explore each weekend. Instead of focusing on the time away from school, we focus on the extra family time. Focus on gratitude, not the things we are missing." Ashley Fitzpatrick.
(1) Background: During and after the pandemic, individuals with type 1 and type 2 diabetes struggled to maintain a healthy lifestyle due to psychological distress and the struggle to accommodate contextual challenges and changes in their family and work obligations and expectations. This study aims to explore the long-term impacts of the pandemic on proactive self-management behaviors and ...
This increased nurses' motivation to work during the COVID-19 crisis [21, 43] however contrary to that, some studies identified that nurses also witnessed social panic due to unrealistic reporting, termed as an infodemic, causing nurses' increased stress and anxiety in caring role [20, 23, 40, 81].
All of us around the world may be experiencing stress more often or more intensely because of the COVID-19 pandemic. Because of this, we have found that stress management is a much-needed topic during these times. With that in mind, we've created a week-long stress management webinar series designed to help you slow down, take a moment to ...
Academic workload . Academic problems have been regarded as the most common stressor for college students [24, 25].For example, in Schafer's [] investigation, students reported that the most significant daily hassles were academics-related stressors such as constant study, writing papers, preparing for exams, and boring teachers.The academic pressure easily comes from taking and preparing ...