- Research article
- Open access
- Published: 15 August 2015

A systematic review of the predictors of disease progression in patients with autosomal dominant polycystic kidney disease
- Claire Woon 1 ,
- Ashleigh Bielinski-Bradbury 1 ,
- Karl O’Reilly 2 &
- Paul Robinson 2
BMC Nephrology volume 16 , Article number: 140 ( 2015 ) Cite this article
6388 Accesses
32 Citations
8 Altmetric
Metrics details
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disorder characterised by progressive renal cyst formation leading to renal failure in the majority of patients. The likelihood and rate of ADPKD progression is difficult to predict and there is a clear need to identify prognostic indicators that could be used to anticipate ADPKD progression, to aid the management of patients in clinical practice.
A systematic literature review was conducted to identify publications detailing the natural history of ADPKD, including diagnosis, prognosis and progression. Publications were identified and filtered, and data were extracted, based on a predefined research protocol.
The review identified 2799 journal articles and 444 conference abstracts; 254 articles, including observational studies, clinical trials and reviews, proceeded to data extraction. Disease progression was associated with a variety of prognostic indicators, most commonly age and total kidney volume (TKV). In the identified clinical trials, the absence of a consistent measure of disease progression led to variation in the primary endpoints used. Consequently, there was difficulty in consistently and effectively demonstrating and comparing the efficacy of investigational treatments across studies. More consistency was found in the observational studies, where disease progression was most frequently measured by TKV and glomerular filtration rate.
Conclusions
This systematic review identified age and TKV as the most commonly cited prognostic indicators in the published ADPKD literature. It is envisaged that this review may inform future research, trial design and predictive models of ADPKD natural history, helping to optimise patient care.
Peer Review reports
Polycystic kidney disease (PKD) is the most common genetic disorder leading to end stage renal disease (ESRD). Autosomal dominant polycystic kidney disease (ADPKD) is caused by germline mutations in PKD1 (85 % of cases) and PKD2 (15 % of cases), and is typically diagnosed later in life than autosomal recessive polycystic kidney disease [ 1 – 4 ].
ADPKD is characterised by the progressive development of multiple bilateral renal cysts and has a prevalence of less than five patients per 10,000 of the population in the EU [ 5 – 7 ]. ADPKD is a systemic disease, with extra-renal manifestations including liver cysts, intracranial aneurysms and hypertension [ 3 , 8 ]. Approximately 70 % of patients with ADPKD will progress to ESRD at a median age of 56 years [ 9 , 10 ]. Patients with ADPKD may experience chronic pain, which may be debilitating, in addition to increased morbidity due to enlarged kidneys, which can lead to poor health-related quality of life (HRQoL) and reduced social interaction [ 3 , 11 ].
ADPKD is associated with a high degree of clinical variability between patients, both within and between families, especially in terms of the likelihood and rate of progression towards ESRD. In the early stages of ADPKD, before renal function is significantly compromised, progression can be difficult to detect as patients are often asymptomatic. Currently, there is a lack of consensus in the published literature regarding the optimal factors for prediction of renal outcomes and the ideal variables that should be measured in order to monitor disease progression, especially in the early stages of the disease. This has led to difficulties in identifying patients at high risk of ESRD and in defining appropriate primary endpoints to consistently measure and compare the efficacy of therapies in development.
There is a requirement for greater understanding of the predictors of disease progression in ADPKD in order to optimise clinical trial design, treatment and patient care. The objective of this systematic review was to identify publications that detail the natural history of ADPKD, considering the indicators of early- and late-stage progression. It was envisaged that this review would aid clinical practice by informing future research and the development of a predictive model to estimate the likely rate of progression and ultimate long-term outcomes in patients with ADPKD.
Systematic literature search
A systematic review of the literature was conducted to identify publications that detail the natural history of ADPKD, including diagnosis, prognosis and progression. In the absence of a definitive measure of disease progression, all measures linked to the progression of ADPKD were considered, although it was anticipated that those linked to cyst development/renal enlargement and renal function would be the most relevant.
The systematic review was conducted and reported according to the principles in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [ 12 ] (Additional file 1 ). A search was conducted in the following electronic databases:
MEDLINE and MEDLINE In-Process
Cochrane Central Register of Controlled Trials (CENTRAL)
The Cochrane Database of Systematic Reviews (CDSR)
NHS Economic Evaluation Database (NHS EED)
Health Economic Evaluations Database (HEED)
Electronic databases were searched on 7th April 2014 using a structured search string, including terms for ADPKD and study type (Additional file 2 ). The search was restricted to publications from the previous 10 years in all databases except BIOSIS, which was limited to the past 3 years. Publications in the field of ADPKD have become significantly more numerous in recent years; therefore, it was considered that a sufficient number of relevant articles would be identified and that any earlier studies containing key information would be identified through reference explosion. In addition, diagnostic and prognostic techniques have progressed with the advancement of technology, with earlier publications often relying on subjective measures of progression, including kidney palpation.
‘Grey literature’ searches of relevant congresses, limited to the past 3 years, were also conducted (World Congress of Nephrology, American Society of Nephrology, American Academy of Nephrology, British Renal Society, European Renal Association and International Society for Pharmacoeconomics and Outcomes Research). Reference lists of systematic reviews and meta-analyses identified by the search were reviewed to identify additional relevant articles that were not identified in the systematic search due to study type restrictions.
Studies meeting the following criteria were considered for inclusion in the review:
Study types: clinical trials, observational studies, systematic reviews, meta-analyses and non-systematic reviews
Population: human, adults (≥18 years of age) with PKD, or ADPKD specifically
Outcomes: diagnosis or prognosis
Language: English.
Study selection
Identified articles were screened by one reviewer, according to the criteria specified above. Articles were filtered using a positive exclusion method, whereby articles with insufficient information to warrant their exclusion remained in the review [ 13 ].
Initially, titles and abstracts of identified articles were reviewed (title/abstract screening) according to a checklist; full-text papers of the publications remaining after title/abstract screening were reviewed according to the same checklist (full text screening). Papers assessing HRQoL were excluded at full text screening if they did not report data on the progression of ADPKD.
Publications that included assessment of the link between ADPKD progression and genetic markers were only included in the review if they assessed the link with genotype ( PKD1 / PKD2 ). Publications assessing genetic markers at a molecular level, i.e. studies assessing specific single nucleotide polymorphisms, were excluded because this level of detail is not readily available to nephrologists in clinical evaluations. An independent reviewer checked a random selection of articles (10 %) at both title/abstract and full text screening to ensure consistency and accuracy.
Data extraction
Data were extracted from studies that met the inclusion criteria. If more than one article was found to present data from the same study population, results were collated as appropriate.
Extracted data consisted of:
Study characteristics, such as study design, duration and location
Patient characteristics (see ‘ Definitions ’)
Clinical characteristics and outcomes linked to disease progression (see ‘ Definitions ’)
Information regarding ESRD in the patient populations, such as age at ESRD onset and length of time on dialysis.
Definitions
For the purposes of this review, ‘patient characteristics’ were demographic data and ‘clinical characteristics’ were defined as baseline clinical parameters, baseline measures of renal size and function, and characteristics that were not influenced by changing renal parameters, e.g. genotype (Table 1 ). ‘Outcomes’ were defined as any measures or markers of disease progression, such as parameters reported over a time period, or measurements taken at both baseline and end of the study. The reporting of symptoms of ADPKD, such as pain, may have been considered as patient characteristics if only reported at baseline, but may also have been considered as outcomes if reported over time.
Glomerular filtration rate (GFR) was a recognised measure of renal function, and was either estimated based on serum creatinine concentration using equations such as the Modification of Diet in Renal Disease (MDRD) equation or the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation (estimated GFR [eGFR]), or measured by creatinine clearance (measured GFR [mGFR]). For simplicity, we used the term ‘GFR’ to refer to studies that used either eGFR or mGFR or both, or where methods of determining GFR were not defined. Change in GFR was used as a measure of renal function and change in total kidney volume (TKV) was used for renal volume in this review.
Figure 1 shows the selection process for articles included in the systematic review. A total of 2799 articles were identified in the original literature search, with a further 444 relevant conference abstracts identified. A total of 254 articles proceeded to the data extraction stage. Of the 254 papers that progressed to data extraction, 160 were observational studies, 33 were clinical trials and 61 were reviews.
PRISMA diagram of the systematic review. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Observational studies
The majority of the identified studies were observational studies (63.0 %), including case studies, registry reviews and patient surveys with durations ranging from 6 months to more than 40 years. The studies employed a range of different objectives, with many aiming to increase understanding of ADPKD. Most studies reported baseline patient characteristics, including average age and gender (65 and 58.8 % of studies, respectively), while symptoms of ADPKD frequently reported at baseline included hypertension and proteinuria (21.3 and 10.6 % studies, respectively). The most commonly reported measure of renal function, described in 66 (41.3 %) observational studies, was GFR. The most frequent measure of renal size was TKV (34 studies, 21.3 %).
Of the 38 (23.8 %) publications that reported outcomes of ADPKD measured over time, disease progression was measured in 32 studies (84.2 %) by GFR, estimated most commonly by the MDRD equation (41.6 %). Change in TKV was reported as a measure of disease progression in 12 studies (31.6 %), with 11 publications using magnetic resonance imaging (MRI) and one publication using computed tomography. Renal enlargement over time as a surrogate marker of disease progression was also measured by total cyst volume (TCV) (five studies) [ 14 – 18 ], volume of each kidney (four studies) [ 19 – 22 ], and total renal volume (TRV) (three studies) [ 19 , 22 , 23 ].
In total, 19 studies reported patient and clinical characteristics of patients with ESRD. Of these studies, 18 reported age at ESRD and 11 reported the number of ADPKD patients reaching ESRD. Baseline characteristics of patients in each of the study groups were not reported in eight studies [ 24 – 31 ], but others reported a number of parameters including age (seven studies) [ 32 – 37 ], serum creatinine (four studies) [ 37 – 40 ], GFR (three studies) [ 33 , 35 , 38 ], TKV (three studies) [ 33 , 36 , 40 ], hypertension (one study) [ 41 ] and PKD mutation (one study) [ 42 ].
Publications were identified that measured GFR decline or increase in TKV (disease progression) and assessed the associated patient and clinical characteristics, defined in Table 1 . If the association with patient and clinical characteristics was significant, these were then defined as prognostic indicators in the prediction of disease progression (Table 2 ).
TKV and age at baseline were the two factors most commonly cited as significantly associated with a faster rate of ADPKD progression, each cited in ten studies (Table 3 ). A wide range of prognostic indicators (a total of 26) were reported, many of which were only reported by one study, indicating a lack of consensus in the literature on the parameters implicated in ADPKD progression.
Seventeen publications from the Consortium for Radiologic Imaging Studies in Polycystic Kidney Disease (CRISP) study were identified by the systematic review [ 15 – 17 , 43 – 56 ]. CRISP is a prospective, long-term observational study, including 241 ADPKD patients with normal renal function who were considered at high risk of renal insufficiency. The study was initiated to increase the knowledge and understanding of ADPKD prognosis by establishing reliable measures of disease progression [ 2 ]. Patients were diagnosed due to a positive family history (asymptomatic family screening) or based on signs and symptoms related to the disease. The study includes patients with defined hypertension diagnosed before the age of 35 years; ADPKD diagnosed in utero or in the first year of life; 24-h urinary protein excretion greater than 300 mg/day; or an episode of gross haematuria in men before the age of 30 years (CRISP I population) [ 57 ]. A range of measurements have thus far been reported, and patients have been stratified by several different criteria across the CRISP publications, demonstrating the relevance of a number of prognostic factors, such as gender and age at diagnosis (Table 2 ). CRISP has identified the importance of TKV as a key prognostic indicator, particularly in the early stages of ADPKD where significant renal enlargement can occur prior to the loss of renal function [ 2 , 46 ]. The CRISP study is ongoing, with 203 patients having been re-enrolled in CRISP II from July 2007 [ 15 ].
Patients were stratified by rate of ADPKD progression, and groups defined as fast or slow progressors (large or small annual decline in GFR, respectively), in four observational studies (Additional file 3 ) [ 56 , 58 – 60 ]. Although this concept is important in the clinical setting, there is no definitive conclusion in the literature as to how the rate of progression should be measured or stratified. Across the four studies, a range of prognostic indicators were reported, including initial GFR, high blood pressure, age at diagnosis and TKV at a given time point.
Disease severity was correlated with HRQoL in a single study [ 11 ]. In general, for patients with a lower GFR, Short Form-36 health survey scores were lower, indicating reduced HRQoL [ 11 ].
A research group in Brest, France, conducted an observational study assessing 26 clinical, biological and genetic variables (not specified) for use in a prognostic model. The model was based on data from 1017 patients with ADPKD, and was tested in a sub-population of 255 patients who had either reached ESRD or were aged over 60 years [ 41 ]. The presence of hypertension along with at least one urologic complication, or the presence of a truncating PKD1 mutation was reported to be associated with poorest renal outcome [ 41 ].
Clinical trials
The 33 clinical trial publications were reviewed to ensure the same data were not extracted from multiple reports of the same study. Of these 33, 24 unique reports were identified. The trials assessed the efficacy of three main drug types to slow the progression of ADPKD:
Mammalian target of rapamycin inhibitors, e.g. sirolimus, everolimus and tacrolimus [ 61 – 67 ].
Somatostatin analogues, e.g. somatostatin, lanreotide and octreotide [ 68 – 73 ].
The vasopressin v2 receptor antagonist, tolvaptan [ 74 – 80 ].
Further drugs were:
Eicosapentaenoic acid, an anti-inflammatory omega-3 fatty acid [ 81 ].
Pravastatin, a statin [ 82 ].
Anti-hypertensives, e.g. angiotensin-converting enzyme inhibitors (ACEIs) (enalapril or ramipril) [ 83 , 84 ] or the beta-blocker metoprolol [ 84 ].
In the clinical trials assessing treatments to halt or slow the development of ADPKD, efficacy was assessed using measures of disease progression. Change in TKV or renal function, measured by GFR or serum creatinine concentration, were the most commonly used primary endpoints in the identified trials.
Other primary endpoints considered in studies of disease-modifying interventions in patients with ADPKD included change in liver volume, change in TCV and change in urinary fatty acid-binding protein. The number of different primary endpoints used in the identified trials demonstrated inconsistencies in the measurement of efficacy due to the paucity of data on the progression of ADPKD.
In the 21 publications that reported data at multiple time points, the most frequently reported outcomes were TKV (14 reports, 66.7 %), eGFR (12 reports, 57.1 %), serum creatinine (7 reports, 33.3 %) and systolic blood pressure (9 reports, 42.9 %). Of these, 12 studies reported data at two time points and eight studies reported data at three or four time points. Data were recorded at baseline and after 6 months in six studies [ 62 , 65 , 68 , 71 – 73 ], at baseline and after 12 months in one study [ 70 ], at baseline and after 24 months in three studies [ 61 , 66 , 82 ], and at baseline and after 36 months in two studies [ 83 , 84 ].
Due to the short study duration and lack of suitable sub-analyses or patient level data, disease progression data from these trials were not appropriate for the assessment of the prognostic potential of the variables measured at baseline.
Hypertension was targeted as a manifestation of ADPKD in the Halt Progression of Polycystic Kidney Disease (HALT-PKD) study, a clinical trial studying the intensive blockade of the renin-angiotensin system with combination ACEIs and angiotensin receptor blockers (ARBs). The study aimed to test the hypothesis that rigorous blood pressure control was more effective in slowing progression of renal disease in early ADPKD than moderate blood pressure control, by comparing the combination treatment to ACEI monotherapy alone. The primary endpoint was annual change in TKV, which was lower with rigorous blood pressure control than with moderate blood pressure control ( P = 0.006). The rate of change in GFR was similar for the two treatment groups [ 85 , 86 ].
The 61 non-systematic and systematic reviews and meta-analyses identified were mainly focussed around new and potential treatment options, as well as reviews of the genetics, pathophysiology and manifestations of the disease. In general, the identified reviews acknowledged and discussed a range of different prognostic indicators, but did not provide conclusive agreement on these factors.
Our review demonstrated that, as a result of the extensive clinical variability associated with ADPKD, a range of biological, genetic and clinical characteristics have been reported in the published literature for both the prediction and measurement of ADPKD progression. Currently, therapeutic options for ADPKD focus on management of the symptoms and complications of the disease since there is no available treatment to slow ADPKD progression. Stratification of patients based on their predicted rate of progression could improve symptom management. The uncertainty surrounding the clinical progression of the disease has also contributed to a paucity of clinical trials investigating potential interventions.
Due to the variability in the rate of ADPKD progression and the length of time taken for patients to reach ESRD, progression to ESRD is a poor candidate endpoint for use in clinical trials. Instead, predictors/indicators of time to disease progression have been used to assess the efficacy of treatments; however, a variety of different endpoints have been employed. This has led to problems in demonstrating conclusive efficacy and in comparing treatments across trials. As a result, no consensus has been reached regarding the optimal endpoints to assess the progression of ADPKD and the efficacy of potential therapies. A range of observational studies have attempted to address this, but there is inconsistency in the parameters reported and in the assessment of disease progression.
Studies evaluating ADPKD have generally been conducted in relatively small study populations, because the slow rate of progression and the lengthy period during which GFR is within the normal range limits the size of the population available for analysis. The CRISP observational study is a rich data source that has assessed several prognostic indicators in a relatively large cohort of patients with ADPKD, selected in order to study the clinical and radiological features of perceived fast progressors over a long follow-up period (6 years) [ 15 , 46 ]. To assess the relationship between baseline TKV and renal growth over time, the cohort was stratified; a greater baseline TKV at a younger age was associated with a more rapid increase in TKV [ 46 ].
CRISP also illustrated that, although GFR does not typically change until the fourth or fifth decade of life, renal enlargement progresses significantly in the early stages of the disease, identifying large TKV as a key indicator of early disease progression [ 2 , 46 ]. This provides evidence that early treatment may be important to slow or halt the progression of ADPKD before cyst development causes irreversible damage [ 46 ]. Other prognostic indicators of relevance included hypertension, gender and age at diagnosis, some of which correlate with those identified by other studies [ 2 ]. It is anticipated that these prognostic indicators will be used in the future evaluation of treatments that aim to slow the progression of ADPKD and will lead to improvement and standardisation of trial design [ 2 ]. However, the CRISP study also has limitations in that, compared with the general ADPKD population, CRISP enrolled a younger cohort with well-preserved renal function. Further analyses are required to validate these findings in the wider ADPKD population with a broader range of renal function and volumes.
Since the searches were conducted, three abstracts from the PKD Outcomes Consortium (PKDOC) have been presented [ 87 – 89 ]. The PKDOC dataset is the largest ADPKD dataset currently available and includes data from CRISP in addition to other study populations from the Mayo Clinic, Emory University and the University of Colorado [ 89 ]. These abstracts validate the use of TKV as an important prognostic indicator, identifying baseline TKV and baseline eGFR as prognostic biomarkers for both eGFR decline and progression to ESRD.
Our systematic review has identified a wide range of prognostic indicators that have been proposed or assessed in observational studies and clinical trials, but there is currently no agreement within the literature. The absence of long term patient level data from the identified clinical trials prevented correlations between variables measured at baseline and the rate of disease progression. In observational studies, age and TKV at baseline were the two factors most commonly cited as significantly associated with a faster rate of ADPKD progression. However, further research is required to validate these factors as true indicators of disease progression. Reported prognostic indicators may be complications of ADPKD that are exacerbated by disease progression, rather than factors driving the underlying progression of the disease, or may exhibit a cause-effect association, in which they both exacerbate and are worsened by the progression of the disease.
The specific genotype of patients with ADPKD has also generated interest as a potential indicator of disease progression rate. Although it is generally agreed in the literature that patients with PKD1 mutations have larger kidneys and worse renal function compared to patients with PKD2 mutations, few papers report the use of GFR and/or TKV to measure disease progression in patients stratified by genotype. Therefore, despite the large number of potential prognostic indicators identified, there may be an interaction between some, possibly enabling the collapse of several prognostic indicators into fewer key factors that are most informative. The two most commonly reported prognostic indicators identified by this review were age and TKV at baseline, which may encapsulate other factors such as PKD gene mutation, renal blood flow and baseline GFR.
Due to inter-patient heterogeneity in renal size and genetic profile, current diagnostic practices based on renal ultrasound and family histories are suboptimal. Recently, urinary proteomic and microRNA biomarkers have been identified that could be used as a non-invasive method of diagnosing patients with ADPKD [ 90 , 91 ]. Long-term studies are ongoing to determine whether such markers also serve as prognostic indicators in ADPKD [ 90 ]. However, initial results are promising as a correlation was observed between the urinary peptide profile and height-adjusted TKV in patients with ADPKD [ 91 ].
The identification of prognostic indicators is of great importance in the drive to improve the management of ADPKD, as a better understanding of patients’ clinical prognosis may lead to improved symptom management that can be tailored to individuals, depending on their predicted rate of progression. This knowledge will also aid the stratification and selection of patients for disease-modifying treatments, as well as providing a basis for improved clinical trial design with standard endpoints to evaluate and compare treatments. A more thorough understanding of the natural history of ADPKD may be beneficial in terms of optimising treatment. The construction of a disease progression model to predict the progression of ADPKD, incorporating the identified prognostic indicators, could be informative for the future management of the disease.
There has previously been little clinical consensus regarding the prognostic indicators associated with disease progression in ADPKD, especially in the early stages of the disease. As a result, ADPKD progression has been assessed using a wide range of patient and clinical characteristics. A systematic review of the literature has identified age and TKV as the two factors most commonly cited as significantly associated with a faster rate of ADPKD progression, particularly in the early stages of the disease. By identifying these prognostic indicators it is hoped there is an opportunity to improve trial design and conduct further research, including a predictive model of ADPKD natural history, in order to provide clinicians with a clearer understanding of factors influencing disease progression, thereby helping to optimise patient care.
Abbreviations
Angiotensin-converting enzyme inhibitor
- Autosomal dominant polycystic kidney disease
Angiotensin receptor blocker
Cochrane database of systematic reviews
Cochrane central register of controlled trials
Chronic kidney disease epidemiology collaboration
Consortium for radiologic imaging studies in polycystic kidney disease
Estimated glomerular filtration rate
- End stage renal disease
Glomerular filtration rate
Halt progression of polycystic kidney disease
Health economic evaluations database
Health-related quality of life
Modification of diet in renal disease
Measured glomerular filtration rate
Magnetic resonance imaging
NHS economic evaluation database
Polycystic kidney disease
Polycystic kidney disease outcomes consortium
Preferred reporting items for systematic reviews and meta-analyses
Total cyst volume
Total kidney volume
Total renal volume
Nahm AM, Henriquez DE, Ritz E. Renal cystic disease (ADPKD and ARPKD). Nephrol Dial Transplant. 2002;17:311–4.
Article PubMed Google Scholar
Chapman AB. Approaches to testing new treatments in autosomal dominant polycystic kidney disease: insights from the CRISP and HALT-PKD studies. Clin J Am Soc Nephrol. 2008;3:1197–204.
Article CAS PubMed Google Scholar
Luciano RL, Dahl NK. Extra-renal manifestations of autosomal dominant polycystic kidney disease (ADPKD): considerations for routine screening and management. Nephrol Dial Transplant. 2014;29:247–54.
Chapal M, Debout A, Dufay A, Salomon R, Roussey G, Burtey S, et al. Kidney and liver transplantation in patients with autosomal recessive polycystic kidney disease: a multicentric study. Nephrol Dial Transplant. 2012;27:2083–8.
Heidland A, Bahner U, Deetjen A, Gotz R, Heidbreder E, Schafer R, et al. Mass-screening for early detection of renal disease: benefits and limitations of self-testing for proteinuria. J Nephrol. 2009;22:249–54.
PubMed Google Scholar
Neumann HP, Jilg C, Bacher J, Nabulsi Z, Malinoc A, Hummel B, et al. Epidemiology of autosomal-dominant polycystic kidney disease: an in-depth clinical study for south-western Germany. Nephrol Dial Transplant. 2013;28:1472–87.
Patch C, Charlton J, Roderick PJ, Gulliford MC. Use of antihypertensive medications and mortality of patients with autosomal dominant polycystic kidney disease: a population-based study. Am J Kidney Dis. 2011;57:856–62.
Torres VE, Rossetti S, Harris PC. Update on autosomal dominant polycystic kidney disease. Minerva Med. 2007;98:669–91.
CAS PubMed Google Scholar
Shaw C, Simms RJ, Pitcher D, Sandford R. Epidemiology of patients in England and Wales with autosomal dominant polycystic kidney disease and end-stage renal failure. Nephrol Dial Transplant. 2014;29:1910–8.
Spithoven EM, Kramer A, Meijer E, Orskov B, Wanner C, Caskey F, et al. Analysis of data from the ERA-EDTA Registry indicates that conventional treatments for chronic kidney disease do not reduce the need for renal replacement therapy in autosomal dominant polycystic kidney disease. Kidney Int. 2014;86:1244–52.
Miskulin DC, Abebe KZ, Chapman AB, Perrone RD, Steinman TI, Torres VE, et al. Health-related quality of life in patients with autosomal dominant polycystic kidney disease and CKD stages 1–4: a cross-sectional study. Am J Kidney Dis. 2014;63:214–26.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9. W64.
Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration. 2011. http://www.cochrane-handbook.org . Accessed 15 Jan 15 A.D.
Chen D, Ma Y, Wang X, Yu S, Li L, Dai B, et al. Clinical characteristics and disease predictors of a large Chinese cohort of patients with autosomal dominant polycystic kidney disease. PLoS One. 2014;9, e92232.
Article PubMed PubMed Central Google Scholar
Torres VE, Grantham JJ, Chapman AB, Mrug M, Bae KT, King BF, et al. Potentially modifiable factors affecting the progression of autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2011;6:640–7.
Article CAS PubMed PubMed Central Google Scholar
Torres VE, King BF, Chapman AB, Brummer ME, Bae KT, Glockner JF, et al. Magnetic resonance measurements of renal blood flow and disease progression in autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2007;2:112–20.
Harris PC, Bae KT, Rossetti S, Torres VE, Grantham JJ, Chapman AB, et al. Cyst number but not the rate of cystic growth is associated with the mutated gene in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2006;17:3013–9.
Irazabal-Mira MV, Torres VE, Hogan MC, Glockner J, King BF, Ofstie TG, et al. Short-term effects of tolvaptan on renal function and volume in patients with autosomal dominant polycystic kidney disease (ADPKD). J Am Soc Nephrol. 2010;21 Suppl:528A–9. abstract F-PO1824.
Google Scholar
Ulusoy S, Ozkan G, Kosucu P, Kaynar K, Eyuboglu I. A comparison of the effects of losartan and ramipril on blood pressure, renal volume and progression in polycystic kidney disease: A 5-Year follow-up. Hippokratia. 2012;16:143–8.
CAS PubMed PubMed Central Google Scholar
Peces R, Cuesta-Lopez E, Peces C, Perez-Duenas V, Vega-Cabrera C, Selgas R. Octreotide reduces hepatic, renal and breast cystic volume in autosomal-dominant polycystic kidney disease. Int U Nephrol. 2011;43:565–9.
Article Google Scholar
Rim H, Jung GS, Jung YS. Transcatheter arterial embolization using ethanol in a dialysis patient for contracting enlarged polycystic kidneys. Korean J Radiol. 2010;11:574–8.
Ulusoy S, Ozkan G, Orem C, Kaynar K, Kosucu P, Kiris A. A comparison of the effects of ramipril and losartan on blood pressure control and left ventricle hypertrophy in patients with autosomal dominant polycystic kidney disease. Ren Fail. 2010;32:913–7.
Azurmendi PJ, Fraga AR, Valdez MG, Arrizurieta E, Martin RS. Early progression markers in autosomal dominant polycystic kidney disease. A longitudinal study in patients with normal GFR. J Am Soc Nephrol. 2011;22 Suppl:301A. abstract TH-PO819.
Dicks E, Ravani P, Langman D, Davidson WS, Pei Y, Parfrey PS. Incident renal events and risk factors in autosomal dominant polycystic kidney disease: a population and family-based cohort followed for 22 years. Clin J Am Soc Nephrol. 2006;1:710–7.
Helal I, Gitomer BY, McFann K, Yan XD, Brosnahan GM, Schrier RW. Serum uric acid and renal disease progression in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2011;22 Suppl:300A. abstract TH-PO816.
Helal I, Gitomer BY, McFann K, Tkachenko OO, Yan XD, Schrier RW. Changing pattern of end-stage renal disease treatment in autosomal dominant polycystic kidney disease patient over time. J Am Soc Nephrol. 2012;23 Suppl:702A. abstract SA-PO288.
Nishimura H, Ubara Y, Nakamura M, Nakanishi S, Sawa N, Hoshino J, et al. Renal cell carcinoma in autosomal dominant polycystic kidney disease. Am J Kidney Dis. 2009;54:165–8.
Orskov B, Christensen KB, Feldt-Rasmussen B, Strandgaard S. Low birth weight is associated with earlier onset of end-stage renal disease in Danish patients with autosomal dominant polycystic kidney disease. Kidney Int. 2012;81:919–24.
Orskov B, Sorensen V, Feldt-Rasmussen B, Strandgaard S. Changes in causes of death and risk of cancer in Danish patients with autosomal dominant polycystic kidney disease and end-stage renal disease. Nephrol Dial Transplant. 2012;27:1607–13.
Spithoven EM, Kramer A, Wanner C, Jager KJ, Gansevoort RT. Incidence of renal replacement therapy for ADPKD in Europe. J Am Soc Nephrol. 2013;24 Suppl:691A–2. abstract SA-PO279.
Yoo DJ, Agodoa L, Yuan CM, Abbott KC, Nee R. Risk of intracranial hemorrhage associated with autosomal dominant polycystic kidney disease in patients with end stage renal disease. BMC Nephrol. 2014;15:39.
Barua M, Cil O, Paterson AD, Wang K, He N, Dicks E, et al. Family history of renal disease severity predicts the mutated gene in ADPKD. J Am Soc Nephrol. 2009;20:1833–8.
Chang MY, Chen HM, Jenq CC, Lee SY, Chen YM, Tian YC, et al. Novel PKD1 and PKD2 mutations in Taiwanese patients with autosomal dominant polycystic kidney disease. J Hum Genet. 2013;58:720–7.
Cornec-Le Gall E, Treguer L, Sawadogo T, Benarbia S, Le Meur Y. Clinical factors predicting renal outcome in autosomal dominant polycystic kidney disease (ADPKD): results of the GENKYST registry. Nephrol Dial Transplant. 2013;28 Suppl 1:i81–4.
Haynes R, Staplin N, Emberson J, Herrington G, Tomson C, Agodoa L, et al. Evaluating the contribution of the cause of kidney disease to prognosis in CKD: results from the study of heart and renal protection (SHARP). Am J Kidney Dis. 2014;64:40–8.
Helal I, McFann K, Reed B, Yan XD, Schrier RW, Fick-Brosnahan GM. Serum uric acid, kidney volume and progression in autosomal-dominant polycystic kidney disease. Nephrol Dial Transplant. 2013;28:380–5.
Nunes ACF, Milani V, Porsch DB, Rossato LB, Mattos CB, Roisenberg I, et al. Frequency and clinical profile of patients with polycystic kidney disease in southern Brazil. Ren Fail. 2008;30:169–73.
Fary Ka E, Seck SM, Niang A, Cisse MM, Diouf B. Patterns of autosomal dominant polycystic kidney diseases in black Africans. Saudi J Kidney Dis Transpl. 2010;21:81–6.
Romao EA, Moyses Neto M, Teixeira SR, Muglia VF, Vieira-Neto OM, Dantas M. Renal and extrarenal manifestations of autosomal dominant polycystic kidney disease. Braz J Med Biol Res. 2006;39:533–8.
Schrier RW, McFann KK, Johnson AM. Epidemiological study of kidney survival in autosomal dominant polycystic kidney disease. Kidney Int. 2003;63:678–85.
Cornec-Le Gall E, Hourmant M, Morin MP, Perrichot R, Charasse C, Siohan P, et al. A new algorithm to predict renal outcome in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2013;24 Suppl:59A. abstract FR-OR98.
Cornec-Le Gall E, Audrezet MP, Hourmant M, Morin MP, Grall-Jezequel A, Renaudineau E, et al. PKD1 mutation type, but not the mutation location, influences renal outcome in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2012;23 Suppl:49A. abstract FR-OR085.
Boertien WE, Meijer E, Li J, Bost JE, Struck J, Flessner MF, et al. Relationship of copeptin, a surrogate marker for arginine vasopressin, with change in total kidney volume and GFR decline in autosomal dominant polycystic kidney disease: results from the CRISP cohort. Am J Kidney Dis. 2013;61:420–9.
Chapman AB, Bost JE, Torres VE, Mrug M, Bae KT, Grantham JJ. Cyst-dependent renal complications in autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2010;21 Suppl:384A. abstract F-PO1198.
Chapman AB, Bost JE, Torres VE, Guay-Woodford L, Bae KT, Landsittel D, et al. Kidney volume and functional outcomes in autosomal dominant polycystic kidney disease. Clin J Am Soc Nephrol. 2012;7:479–86.
Grantham JJ, Torres VE, Chapman AB, Guay-Woodford LM, Bae KT, King Jr BF, et al. Volume progression in polycystic kidney disease. N Engl J Med. 2006;354:2122–30.
Grantham JJ, Torres VE, Chapman AB, Bae KT, Tao C, Guay-Woodford LM, et al. Urinary monocyte chemotactic protein-1 (MCP1) predicts progression in autosomal dominant polycystic kidney disease (ADPKD). J Am Soc Nephrol. 2010;21 Suppl:526A. abstract F-PO1814.
Irazabal MV, Boertien WE, Landsittel D, Li J, Struck J, Flessner MF, et al. Urine sodium excertion and plasma proANP as markers of disease progression in ADPKD. J Am Soc Nephrol. 2012;23 Suppl:246A. abstract TH-PO642.
Marier JF, Gosselin NH, Chittenden JT, Czerwiec FS, Levy DI, Chapman AB, et al. Total kidney volume is a prognostic biomarker for worsening of kidney function in patients with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2013;24 Suppl:686A. abstract SA-PO259.
Marier JF, Mouksassi M, Jonsson F, Czerwiec FS, Levy DI, Chapman AB, et al. Total kidney volume is a prognostic biomerker for the progression to end-stage renal disease in patients with autosomal dominant polycystic kidney disease over 10 years. J Am Soc Nephrol. 2013;24 Suppl:686A–7. abstract SA-PO260.
Mrug M, Mrug S, Guay-Woodford LM, Torres VE, Bae KT, Harris PC, et al. Prediction of renal function trajectories in early autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2012;23 Suppl:66A. abstract SA-OR005.
Mrug M, Mrug S, Landsittel D, Torres VE, Bae KT, Harris PC, et al. Prediction of GFR endpoints in early autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2013;24 Suppl:59A. abstract FR-OR97.
Parikh CR, Dahl NK, Chapman AB, Bost JE, Edelstein CL, Comer DM, et al. Evaluation of urine biomarkers of kidney injury in polycystic kidney disease. Kidney Int. 2012;81:784–90.
Rule AD, Torres VE, Chapman AB, Grantham JJ, Guay-Woodford LM, Bae KT, et al. Comparison of methods for determining renal function decline in early autosomal dominant polycystic kidney disease: the consortium of radiologic imaging studies of polycystic kidney disease cohort. J Am Soc Nephrol. 2006;17:854–62.
Torres VE, Chapman AB, King BF, Martin DR, Grantham JJ, Mrug M, et al. Renal blood flow (RBF) is an underestimated tool to monitor the progression of autosomal dominant polycystic kidney disease (ADPKD). J Am Soc Nephrol. 2010;21 Suppl:527A. abstract F-PO1818.
Warner JD, Irazabal MV, Erickson BJ, King BF, Bae KT, Grantham JJ, et al. A new metric to predict autosomal dominant polycystic kidney disease (ADPKD) progression: cyst parenchyma surface area (CPSA). J Am Soc Nephrol. 2012;23 Suppl:704A–5. abstract SA-PO296.
Chapman AB, Guay-Woodford LM, Grantham JJ, Torres VE, Bae KT, Baumgarten DA, et al. Renal structure in early autosomal-dominant polycystic kidney disease (ADPKD): The Consortium for Radiologic Imaging Studies of Polycystic Kidney Disease (CRISP) cohort. Kidney Int. 2003;64:1035–45.
Griveas I, Bishop K, World M. Adult polycystic kidney disease: who needs hospital follow-up? Artif Organs. 2012;36:594–9.
Ozkok A, Akpinar TS, Tufan F, Kanitez NA, Uysal M, Guzel M, et al. Clinical characteristics and predictors of progression of chronic kidney disease in autosomal dominant polycystic kidney disease: a single center experience. Clin Exp Nephrol. 2013;17:345–51.
Panizo N, Goicoechea M, Garcia de Vinuesa S, Arroyo D, Yuste C, Rincon A, et al. Chronic kidney disease progression in patients with autosomal dominant polycystic kidney disease. Nefrologia. 2012;32:197–205.
Mora FP, Codianni P, Liern M, Grammatico D, Vallejo G. Use of rapamycin to reduce the pathologic kidney volume growth in autosomal polycystic kidney disease. Pediatr Nephrol. 2013;28:1492.
Perico N, Antiga L, Caroli A, Ruggenenti P, Fasolini G, Cafaro M, et al. Sirolimus therapy to halt the progression of ADPKD. J Am Soc Nephrol. 2010;21:1031–40.
Qian Q, Du H, King BF, Kumar S, Cosio FG, Torres VE. Sirolimus reduces polycystic liver volume in ADPKD patients after renal transplantation. J Am Soc Nephrol. 2007;18:365A.
Serra AL, Poster D, Kistler AD, Krauer F, Raina S, Young J, et al. Sirolimus and kidney growth in autosomal dominant polycystic kidney disease. N Engl J Med. 2010;363:820–9.
Soliman AR, Ismail E, Zamil S, Lotfy A. Sirolimus therapy for patients with adult polycystic kidney disease: a pilot study. Transplant Proc. 2009;41:3639–41.
Stallone G, Infante B, Grandaliano G, Bristogiannis C, Macarini L, Mezzopane D, et al. Rapamycin for treatment of type I autosomal dominant polycystic kidney disease (RAPYD-study): a randomized, controlled study. Nephrol Dial Transplant. 2012;27:3560–7.
Walz G, Budde K, Mannaa M, Nurnberger J, Wanner C, Sommerer C, et al. Everolimus in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2010;363:830–40.
Caroli A, Antiga L, Cafaro M, Fasolini G, Remuzzi A, Remuzzi G, et al. Reducing polycystic liver volume in ADPKD: effects of somatostatin analogue octreotide. Clin J Am Soc Nephrol. 2010;5:783–9.
Caroli A, Perico N, Perna A, Antiga L, Brambilla P, Pisani A, et al. Effect of longacting somatostatin analogue on kidney and cyst growth in autosomal dominant polycystic kidney disease (ALADIN): a randomised, placebo-controlled, multicentre trial. Lancet. 2013;382:1485–95.
Chrispijn M, Nevens F, Gevers TJG, Vanslembrouck R, van Oijen MGH, Coudyzer W, et al. The long-term outcome of patients with polycystic liver disease treated with lanreotide. Aliment Pharmacol Ther. 2012;35:266–74.
Gevers TJG, Hol JC, Monshouwer R, Dekker H, Wetzels JF, Drenth JPH. Lanreotide halts polycystic liver and kidney growth in patients with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2013;24 Suppl:60A–1. abstract FR-OR102.
Ruggenenti P, Remuzzi A, Ondei P, Fasolini G, Antiga L, Ene-Iordache B, et al. Safety and efficacy of long-acting somatostatin treatment in autosomal-dominant polycystic kidney disease. Kidney Int. 2005;68:206–16.
van Keimpema L, Nevens F, Vanslembrouck R, van Oijen MG, Hoffmann AL, Dekker HM, et al. Lanreotide reduces the volume of polycystic liver: a randomized, double-blind, placebo-controlled trial. Hepatology. 2009;50 Suppl 4:328A.
Boertien WE, Meijer E, de Jong PE, Bakker SJL, Czerwiec FS, Struck J, et al. Short-term renal hemodynamic effects of tolvaptan in subjects with autosomal dominant polycystic kidney disease at various stages of chronic kidney disease. Kidney Int. 2013;84:1278–86.
Czerwiec FS, Chapman AB, Devuyst O, Gansevoort RT, Higashihara E, Krasa HB, et al. Clinical outcomes in ADPKD: results from the TEMPO 3:4 trial. J Am Soc Nephrol. 2013;24 Suppl:61A. abstract FR-OR103.
Horie S, Higashihara E, Muto S, Nutahara K, Iino Y, Narita I, et al. Effects of tolvaptan in ADPKD: subanalysis of Japanese patients from the TEMPO 3:4 trial. J Am Soc Nephrol. 2013;24 Suppl:688A. abstract SA-PO266.
Perrone RD, Chapman AB, Czerwiec FS, Devuyst O, Gansevoort RT, Grantham JJ, et al. Correlation of total kidney volume and eGFR in patients with ADPKD: results from the TEMPO 3:4 trial. J Am Soc Nephrol. 2013;24 Suppl:687A. abstract SA-PO263.
Torres VE, Grantham JJ, Chapman AB, Watnick T, Kedzierski K, Ouyang JJ, et al. Phase 2 open-label study to determine safety, tolerability and efficacy of split-dose tolvaptan in ADPKD [abstract no:SA-PO077]. J Am Soc Nephrol. 2007;18 Suppl:361A–2. abstract SA-PO077.
Torres VE, Chapman AB, Grantham JJ, Watnick TJ, Ouyang J, Krasa HB, et al. TEMPO 2/4 update: changes in ADPKD total kidney volume and eGFR with 3 years of tolvaptan and after withdrawal. J Am Soc Nephrol. 2010;21 Suppl:528A. abstract F-PO1822.
Torres VE, Chapman AB, Devuyst O, Gansevoort RT, Grantham JJ, Higashihara E, et al. Tolvaptan in patients with autosomal dominant polycystic kidney disease. N Engl J Med. 2012;367:2407–18.
Higashihara E, Nutahara K, Horie S, Muto S, Hosoya T, Hanaoka K, et al. The effect of eicosapentaenoic acid on renal function and volume in patients with ADPKD. Nephrol Dial Transplant. 2008;23:2847–52.
Fassett RG, Coombes JS, Packham D, Fairley KF, Kincaid-Smith P. Effect of pravastatin on kidney function and urinary protein excretion in autosomal dominant polycystic kidney disease. Scand J Urol Nephrol. 2010;44:56–61.
van Dijk MA, Breuning MH, Duiser R, van Es LA, Westendorp RG. No effect of enalapril on progression in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2003;18:2314–20.
Zeltner R, Poliak R, Stiasny B, Schmieder RE, Schulze BD. Renal and cardiac effects of antihypertensive treatment with ramipril vs metoprolol in autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2008;23:573–9.
Schrier RW, Abebe KZ, Perrone RD, Torres VE, Braun WE, Steinman TI, et al. Blood pressure in early autosomal dominant polycystic kidney disease. N Engl J Med. 2014;371:2255–66.
Torres VE, Abebe KZ, Chapman AB, Schrier RW, Braun WE, Steinman TI, et al. Angiotensin blockade in late autosomal dominant polycystic kidney disease. N Engl J Med. 2014;371:2267–76.
Perrone R, Marier JF, Mouksassi M, Romero K, Dennis EH, Miskulin D, et al. Baseline total kidney volume is associated with worsening of kidney function independently of baseline glomerular filtration rate in patients with autosomal dominant polycystic kidney disease. In: Abstract 318 presented at the National Kidney Foundation Spring Clinical Meeting, Las Vegas, Nevada, USA, 22–26 Apr 2014. 2014.
Perrone R, Marier JF, Mouksassi M, Czerwiec FS, Romero K, Dennis EH, et al. End-stage renal disease in patients with autosomal dominant polycystic kidney disease is dependent on baseline total kidney volume and baseline glomerular filtration rate. In: Abstract 319 presented at the National Kidney Foundation Spring Clinical Meeting, Las Vegas, Nevada, USA, 22–26 Apr 2014. 2014.
Perrone R, Marier JF, Mouksassi M, Czerwiec FS, Romero K, Dennis EH, et al. Qualification of total kidney volume as a prognostic biomarker for use in clinical trials evaluating patients with autosomal dominant polycystic kidney disease. In: Abstract 428 presented at the National Kidney Foundation Spring Clinical Meeting, Las Vegas, Nevada, USA, 22–26 Apr 2014. 2014.
Ben-Dov IZ, Tan YC, Morozov P, Wilson PD, Rennert H, Blumenfeld JD, et al. Urine microRNA as potential biomarkers of autosomal dominant polycystic kidney disease progression: description of miRNA profiles at baseline. PLoS One. 2014;9, e86856.
Kistler AD, Serra AL, Siwy J, Poster D, Krauer F, Torres VE, et al. Urinary proteomic biomarkers for diagnosis and risk stratification of autosomal dominant polycystic kidney disease: a multicentric study. PLoS One. 2013;8, e53016.
Kistler AD, Poster D, Krauer F, Weishaupt D, Raina S, Senn O, et al. Increases in kidney volume in autosomal dominant polycystic kidney disease can be detected within 6 months. Kidney Int. 2009;75:235–41.
Boertien WE, Meijer E, Jie L, Bost JE, Struck J, Flessner MF, et al. Copeptin, a surrogate marker for vasopressin, is associated with disease progression in the CRISP cohort of ADPKD patients. J Am Soc Nephrol. 2011;22 Suppl:59A. abstract FR-OR245.
Boertien WE, Meijer E, Zittema D, van Dijk MA, Rabelink TJ, Breuning MH, et al. Copeptin, a surrogate marker for vasopressin, is associated with kidney function decline in subjects with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 2012;27:4131–7.
Kurashige M, Hanaoke K, Kawaguchi Y, Hasegawa T, Imamura M, Maeda S, et al. Genetic and phenotypic characteristics of subjects with autosomal dominant polycystic kidney disease in the Japanese. J Am Soc Nephrol. 2012;23 Suppl:701A. abstract SA-PO280.
Kurashige M, Hanaoka K, Imamura M, Kawaguchi Y, Hasegawa E, Hosoya T, et al. A comprehensive mutation search within the PKD1/2 for Japanese subjects with autosomal dominant polycystic kidney disease. J Am Soc Nephrol. 2013;24 Suppl:694A. abstract SA-PO290.
Hwang JH, Park HC, Jeong JC, Ha Baek S, Han MY, Bang K, et al. Chronic asymptomatic pyuria precedes overt urinary tract infection and deterioration of renal function in autosomal dominant polycystic kidney disease. BMC Nephrol. 2013;14:1.
Lacquaniti A, Chirico V, Lupica R, Buemi A, Loddo S, Caccamo C, et al. Apelin and copeptin: two opposite biomarkers associated with kidney function decline and cyst growth in autosomal dominant polycystic kidney disease. Peptides. 2013;49:1–8.
Spithoven EM, Meijer E, Boertien WE, Sinkeler SJ, Tent H, de Jong PE, et al. Tubular secretion of creatinine in autosomal dominant polycystic kidney disease: consequences for cross-sectional and longitudinal performance of kidney function estimating equations. Am J Kidney Dis. 2013;62:531–40.
Thong KM, Ong ACM. The natural history of autosomal dominant polycystic kidney disease: 30-year experience from a single centre. QJM. 2013;106:639–46.
Higashihara E, Nutahara K, Okegawa T, Shishido T, Tanbo M, Kobayasi K, et al. Kidney volume and function in autosomal dominant polycystic kidney disease. Clin Exp Nephrol. 2014;18:157–65.
Download references
Acknowledgements
The authors would like to thank ACM Ong, B Ørskov, R Sandford and G Walz for their advice and collaboration. The authors also acknowledge J Moorhouse (Double Helix Consulting) for assistance with the filtering of records and revision of the manuscript. This study was funded by Otsuka Pharmaceutical Europe Ltd.
Author information
Authors and affiliations.
Double Helix Consulting, Complete House, Macclesfield, Cheshire, UK
Claire Woon & Ashleigh Bielinski-Bradbury
Otsuka Pharmaceutical Europe Ltd, Wexham, UK
Karl O’Reilly & Paul Robinson
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Paul Robinson .
Additional information
Competing interests.
Otsuka Pharmaceutical Europe Ltd, who funded this review and employ KOR and PR, produce tolvaptan, which is now approved for use in Europe, Canada and Japan.
Authors’ contributions
CW and ABB participated in the study design, database searching, filtering of records, data analysis and preparation of the article. KOR and PR participated in the study design, data analysis and preparation of the article. All authors read and approved the final manuscript.
Additional files
Additional file 1:.
PRISMA 2009 checklist. A checklist of items to be reported in systematic reviews and meta-analyses (DOCX 18 kb)
Additional file 2:
General search string. General search string used to interrogate databases and identify potential studies of interest. (DOCX 17 kb)
Additional file 3:
Definitions of fast and slow progression. Definitions of fast and slow progression of ADPKD used in observational studies. (DOCX 18 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Woon, C., Bielinski-Bradbury, A., O’Reilly, K. et al. A systematic review of the predictors of disease progression in patients with autosomal dominant polycystic kidney disease. BMC Nephrol 16 , 140 (2015). https://doi.org/10.1186/s12882-015-0114-5
Download citation
Received : 29 January 2015
Accepted : 20 July 2015
Published : 15 August 2015
DOI : https://doi.org/10.1186/s12882-015-0114-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Disease progression
- Systematic review
- Prognostic indicators
BMC Nephrology
ISSN: 1471-2369
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 15 July 2024
Overview of clinical status, treatment, and long-term outcomes of pediatric autosomal-dominant polycystic kidney disease: a nationwide survey in Taiwan
- Chia-Yi Chin 1 , 2 ,
- Wan-Ting Huang 3 ,
- Jen-Hung Wang 3 ,
- Je-Wen Liou 4 ,
- Hao-Jen Hsu 5 &
- Ming-Chun Chen 1 , 2
Scientific Reports volume 14 , Article number: 16280 ( 2024 ) Cite this article
384 Accesses
Metrics details
This retrospective study investigated the incidence, medication use, and outcomes in pediatric autosomal-dominant polycystic kidney disease (ADPKD) using Taiwan's National Health Insurance Research Database (NHIRD). A 1:4 matched control group of individuals included in the NHIRD during the same period was used for comparative analyses. A total of 621 pediatric patients were identified from 2009 to 2019 (mean age, 9.51 ± 6.43 years), and ADPKD incidence ranged from 2.32 to 4.45 per 100,000 individuals (cumulative incidence, 1.26–1.57%). The incidence of newly developed hypertension, anti-hypertensive agent use, nephrolithiasis, and proteinuria were significantly higher in the ADPKD group than the non-ADPKD group (0.7 vs. 0.04, 2.26 vs. 0.30, 0.4 vs. 0.02, and 0.73 vs. 0.05 per 100 person-years, respectively). The adjusted hazard ratios for developing hypertension, proteinuria, nephrolithiasis and anti-hypertensive agent use in cases of newly-diagnosed pediatric ADPKD were 12.36 (95% CI 4.92–31.0), 13.49 (95% CI 5.23–34.79), 13.17 (95% CI 2.48–69.98), and 6.38 (95% CI 4.12–9.89), respectively. The incidence of congenital cardiac defects, hematuria, urinary tract infections, gastrointestinal diverticulosis, dyslipidemia, and hyperuricemia were also higher in the ADPKD group. Our study offers valuable insights into the epidemiology of pediatric ADPKD in Taiwan and could help in formulating guidelines for its appropriate management.
Similar content being viewed by others

Implications of early diagnosis of autosomal dominant polycystic kidney disease: A post hoc analysis of the TEMPO 3:4 trial

Autosomal-dominant polycystic kidney disease: tolvaptan use in adolescents and young adults with rapid progression
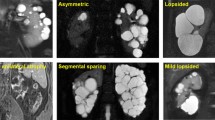
Atypical Polycystic Kidney Disease as defined by Imaging
Introduction.
Autosomal-dominant polycystic kidney disease (ADPKD), a ciliopathy characterized by diffuse cyst formation, is the most prevalent hereditary renal disease, with an estimated prevalence ranging from 1 in 500 to 2,500 individuals worldwide 1 , 2 . ADPKD accounts for 5% of all cases of end-stage renal disease and 10% of cases in individuals under 65 years of age 3 . Loss of function mutations in PKD1 (chromosome 16p13.3) and PKD2 (chromosome 4q21)—which encode for polycystin-1 (PC1) and polycystin-2 (PC2), respectively—are responsible for approximately 95% of all ADPKD cases 3 , 4 . These mutations disrupt the molecular pathways that control cellular proliferation, tubulogenesis, and fluid secretion, eventually leading to the development of fluid-filled cysts 4 .
A high incidence of cardiovascular, renal, and gastrointestinal complications has been reported among patients with ADPKD 5 , including children and adolescents 6 . Approximately 3% of children with ADPKD-causing mutations develop progressive structural kidney disease at an unusually early age or at an accelerated rate, with the disease even manifesting in utero in some cases 7 . Thus, early childhood interventions to mitigate the progression of ADPKD to chronic renal failure could significantly impact individual and public health and medical resource requirements in the long term 6 .
The incidence of ADPKD and associated complications vary geographically, ethnically, and methodologically 1 , 2 , 6 . However, there are no reports on the epidemiology and current characteristics of the pediatric ADPKD population in Taiwan. Moreover, there is a lack of long-term follow-up data on medication use, clinical outcomes, comorbidities, and complications, and most previously published reports relied on small, single-center cohorts.
The National Health Insurance Research Database (NHIRD) provides access to 99.8% of healthcare data in Taiwan, facilitating population-based epidemiological research and evaluation of disease incidence and healthcare burdens 8 . This study utilized NHIRD data to investigate nation-wide trends in pediatric ADPKD incidence, medication use, and disease outcomes and complications in Taiwan.
Setting and data sources
Over 90% of hospitals and clinics in Taiwan are included under the government-sponsored Taiwan National Health Insurance program. Our population-based retrospective study used the Health and Welfare Data Science Center (HWDC) datasets extracted from the Taiwan NHIRD, which contains healthcare details and vital status data of 99.8% of Taiwan’s 23 million residents ( https://nhird.nhri.org.tw/en/index.html) 8 , 9 , to identify patients with incident ADPKD among all individuals registered during the period spanning January 2009 to December 2019, as disclosed by the Collaboration Center of Health Information Application of Taiwan. The diagnosis codes were based on the 9 th and 10 th revisions of the International Classification of Diseases, Clinical Modification codes (ICD-9-CM for 2009 to 2015 and ICD-10-CM 2016 onwards). Incidence rates were calculated using public national birth data from the Taiwanese Ministry of the Interior as the denominator.
Ethics approval and patient selection
The study was conducted in accordance with the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the Protection of Human Subjects Institutional Review Board of Tzu Chi Hospital (approval no: IRB111-023-B, approved on April 21, 2022); the requirement for informed consent was waived due to the retrospective nature of the study. The ADPKD cohort comprised patients with at least one hospitalization or two outpatient visit records for ADPKD (ICD-9-CM codes: 753.12, 753.13; ICD-10 codes: Q61.2, Q61.3). The first date of diagnosis was used as the index date 9 . Patients with invalid or missing personal data were excluded from the analysis. Subjects with comorbidities reported before the index date were included in baseline disease analysis but excluded from further ADPKD-related complication analyses in this study 8 . Control subjects, matched 1:4 to the ADPKD group by sex, age, and index date (between 2009 and 2019), were selected from the remaining NHIRD cohort and using the same exclusion criteria.
Evaluation of ADPKD-related complications
Several cardiovascular, renal, and gastrointestinal complications are associated with of ADPKD 3 , 5 . We analyzed ADPKD-related complications for patients and controls who had at least one hospitalization or two outpatient visits, identified by the relevant ICD-9 or ICD-10 codes, with a minimum interval of 30 days from the index date, as detailed in Table XXX2. In assessing the clinical outcomes of children with very-early onset (VEO) ADPKD, diagnosed within the first 1.5 years of life, we conducted a subgroup analysis focusing on ADPKD patients younger than 1.5 years, as presented in Table XXX4.
Evaluation of ADPKD-related medication use
To analyze the use of anti-hypertensive medications in newly diagnosed ADPKD patients, the Anatomical Therapeutic Chemical Classification (ATC) system was used to analyze medication use. Previously reported medications for symptomatic ADPKD control, including statins (ATC codes: C10AA, C10BX03) and anti-hypertensive agents (ATC codes: C02–C04, C07–C09) were assessed 5 , 6 . Common anti-hypertensive agents used for blood pressure control were grouped into six categories: (1) angiotensin-converting enzyme inhibitors (ACEis) and angiotensin receptor blockers (ARBs), (2) beta blockers, (3) calcium channel blockers (CCBs), (4) diuretics, (5) aldosterone blockers, and (6) others 10 , 11 . Individuals who had used above medications for more than 30 days in the year prior to the index date were excluded. Therefore, the medications we refer to are those newly initiated after the diagnosis of ADPKD. Only medications used > 30 days after the index date were included in the analysis.
Statistical analysis
Annual incidence rates based on age and sex were calculated by dividing the number of new cases in the ADPKD and non-ADPKD groups based on the corresponding age- and sex-specific population data for the study period obtained from the Taiwanese Ministry of the Interior. Descriptive statistics data are presented in terms of absolute numbers and percentages. Comparison of two incidences was performed using the Chi2-statistic. Univariable and multivariable Cox proportional hazards models were used to estimate the risk of different complication for two groups. SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. Statistical significance was set at P < 0.05.
Demographic information of pediatric patients with ADPKD
A total of 21,555 patients were diagnosed with ADPKD (Fig. 1 ) between 2008 and 2019 in Taiwan according to the National Health Research Institute (NHRI) data. Patients over 18 years of age (n = 16,831), with missing information regarding sex (n = 230), and first diagnosed before 2009 (n = 3823) were excluded. To ensure a minimum follow-up period of 1 year for the study population, children diagnosed with ADPKD in 2019 (n = 50) were excluded from the outcome analysis.

Flowchart of patient selection for the pediatric ADPKD group and the matched non-ADPKD group. ADPKD, autosomal-dominant polycystic kidney disease.
Finally, this study included and analyzed 621 pediatric patients newly diagnosed with ADPKD between January 1, 2009 and December 31, 2018 and 2484 controls. Patients were followed-up from the index date until the occurrence of an event, death, or the end of the study on December 31, 2019.
The prevalence of ADPKD in the pediatric population between 2008 and 2019 was 2.32 to 4.45 per 100,000 persons. The cumulative incidence rate of pediatric ADPKD from 2009 to 2019 was 1.26–1.57% (Fig. 2 ).

Incidence rates in the ADPKD population by gender from 2009 to 2019.
The characteristics and common comorbidities of patients with ADPKD in our cohort are shown in Table 1 . The mean age was 9.51 ± 6.43 years, and male sex was more common (53.8%). Ten percent of patients had urinary tract infections before being diagnosed with ADPKD, and 3.87% and 2.24% children newly diagnosed with ADPKD already had hematuria and proteinuria/albuminuria, respectively. Chronic kidney disease (CKD) was already diagnosed in 1.2% of children with ADPKD. Approximately 2% of patients had hypertension and congenital heart defects and nearly 5% had already used anti-hypertensive drugs before being diagnosed with ADPKD.
Complications in pediatric ADPKD
Details regarding the patterns of various complications and the corresponding characteristics of pediatric patients with ADPKD in Taiwan are presented in Tables 2 and 3 and Fig. 3 .

Kaplan–Meier curves for the assessed events in the ADPKD and non-ADPKD groups.
Cardiovascular system
The incidence of newly developed hypertension was significantly higher among children with ADPKD from 2009 to 2018 (Table 2 ) than that among children without ADPKD (0.7 versus 0.04 per 100 person-years, P < 0.001; incidence rate ratio [IRR], approximately 17.8). The incidences of congenital cardiac defects (0.3 versus 0.17 per 100 person-years, P = 0.067) and mitral valve prolapse (0.2 versus 0.08 per 100 person-years, P = 0.198) were higher among children with ADPKD. However, these differences did not reach statistical significance.
The cumulative incidence of hypertension (Fig. 3 a) was significantly higher among children with ADPKD than in those without ADPKD (log-rank test, P < 0.001). The hazard ratio (HR) of developing hypertension (Table 3 ) was 17.19 (95% confidence interval [CI]: 7.08 to 41.77) and the adjusted HR (aHR) was 12.36 (95% CI: 4.92 to 31.0) in children newly diagnosed with ADPKD. The HR and aHR of newly diagnosed congenital cardiac defect were 1.97 (95% CI 0.98–3.93) and 2.34 (95% CI 1.11–4.90), respectively. The HR for newly diagnosed mitral valve prolapse was not statistically significant (Table 3 ). In children aged 1.5 years and younger, as documented in Table 4 , the incidence of hypertension was 0.39 per 100 person-year. The incidence of congenital cardiac defects was higher among children with ADPKD (0.81 vs. 0.42 per 100 person-years, P = 0.179), although this difference did not achieve statistical significance.
Renal system
The incidence of nephrolithiasis among children with ADPKD was 0.4 per 100 person-years, which was significantly higher than that among children without ADPKD in (0.02 per 100 person-years, P < 0.001; IRR, 20.5). The incidence of proteinuria/albuminuria and hematuria were also significantly higher in children with ADPKD compared to those without ADPKD (0.73 versus 0.05 per 100 person-years, P < 0.001; IRR, 13.9 for proteinuria/albuminuria and 0.93 versus 0.16 per 100 person-years, P < 0.001; IRR: 5.9 for hematuria).
The cumulative incidence of proteinuria or albuminuria, hematuria, and urinary tract or cystic infection were significantly higher in children with ADPKD (Fig. 3 b–d). The HR for developing renal system disorders among children newly diagnosed with ADPKD are shown in Table 3 . The HR and aHR for developing proteinuria or albuminuria were 13.50 (95% CI 6.13–29.71) and 13.49 (95% CI 5.23–34.79), respectively. The HR and aHR for developing nephrolithiasis during follow-up were 19.71 (95% CI 5.70–68.11) and 13.17 (95% CI 2.48–69.98), respectively. The risk of hematuria and urinary tract or cystic infection were also significantly higher among children with ADPKD. There were 23 CKD events in the ADPKD group and the incidence ratio was 0.62 per 100 person-years. No CKD event was documented in children without ADPKD. In children aged 1.5 years and younger, as outlined in Table 4 , the incidence rates for proteinuria/albuminuria and CKD were 0.26 and 0.52 per 100 person-year, respectively. The incidence of hematuria and urinary tract or cystic infection was also significantly elevated in children with ADPKD, with rates of 0.65 compared to 0.12 per 100 person-years ( P = 0.006; IRR: 5.18 for hematuria) and 5.22 versus 1.67 per 100 person-years ( P < 0.001; IRR: 3.12 for urinary tract or cystic infection).
Other systems
Specific diseases associated with ADPKD in adults, specifically diverticulum in the colon or intestine, , dyslipidemia, and hyperuricemia, was significantly higher among children with ADPKD than among children without ADPKD (0.2 versus 0.03, 0.4 versus 0.14, and 0.2 versus 0.03 per 100 person-years, all P < 0.001).
ADPKD children had higher inguinal hernia rates, but not significantly different from non-ADPKD (0.13 vs 0.11, P = 0.645).
The cumulative incidence of dyslipidemia (Fig. 3 e) was significantly higher in children with ADPKD than in those without ADPKD (log-rank test, P < 0.001). The HR and aHR of developing dyslipidemia (Table 3 ) were 2.83 (95% CI 1.46–5.50) and 3.66 (95% CI 1.77–7.59) and those for hyperuricemia were 7.0 (95% CI 2.05–23.91) and 8.0 (95% CI 2.0–31.99), respectively. The HR and aHR of developing diverticulum in the colon or intestine during follow-up were 3.33 (95% CI 1.02–10.92) and 3.89 (95% CI 1.12–13.44). The risk of developing inguinal hernia was not statistically significant.
Medication use
The incidence of anti-hypertensive agent (2.26 vs 0.30 per 100 person-years, P < 0.001) and statin (0.21 vs 0.02 per 100 person-years, P < 0.001) use in ADPKD children (Table 2 ) were significantly higher than those among non-ADPKD children (IRR for anti-hypertensive agent and statin use, 7.55 and 10.87, respectively). A higher incidence of anti-hypertensive agent use was also found in age 1.5 years or younger (1.52 versus 0.13 per 100 person-years, P < 0.001) (Table 4 ). The cumulative incidence of anti-hypertensive medication use (Fig. 3 f) was significantly higher in children with ADPKD than in those without ADPKD (log-rank test, P < 0.001). The HR and aHR for using anti-hypertensive medications among children newly diagnosed with ADPKD (Table 3 ) were 8.01 (95% CI 5.37–11.94) and 6.38 (95% CI 4.12–9.89). Furthermore, the risk of statin use was significantly higher among children with ADPKD (HR: 10.67 [95% CI 2.83–40.20]. aHR: 8.66 [95% CI 1.64–45.64]). With regard to the anti-hypertensive medication categories, ACEis and ARBs accounted for 55%, beta-blockers for 22%, aldosterone antagonists for 8%, diuretics for 6%, calcium channel blockers for 5%, and others for 4%, respectively (Fig. 4 ).

Distribution of anti-hypertensive medications used in the ADPKD population. ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers.
This nationwide retrospective cohort study used the NHRI database to assess the incidence, comorbidities, and medication patterns of ADPKD in the pediatric population in Taiwan. In our cohort, the prevalence of pediatric ADPKD was 2.32–4.45 per 100,000 persons, which was lower than the ADPKD prevalence among adults (9.3–47.6 per 100,000 persons) 1 , 2 , 12 ; the cumulative incidence rate was 1.26% to 1.57%. The prevalence of hypertension in pediatric ADPKD was reported as approximately 20–35% in cohort studies conducted two to three decades ago 13 , 14 , 15 , 16 , whereas a meta-analysis conducted in 2016 reported a prevalence of 20% 17 . In our cohort, we observed a prevalence of approximately 2.4% among individuals who already had hypertension before or at the time of ADPKD diagnosis. However, it is important to note that the actual prevalence might be higher, as 4.8% of the cohort were already using anti-hypertensive medications prior to the diagnosis of ADPKD. This discrepancy could be attributed to the lack of ICD code data documentation at the time of prescribing medications, as well as the use of anti-hypertensive agents for renal protection by patients with proteinuria.
In children newly diagnosed with ADPKD, the observed incidence of hypertension was approximately 0.7 per 100 person-years. Hypertension in ADPKD is a progressive condition caused primarily by the growth of cysts in the kidneys, which disrupt the normal kidney architecture and compress renal blood vessels and tubules 14 , 16 , 18 . As the size and number of renal cysts increase, local ischemia can occur, leading to renin–angiotensin–aldosterone system (RAAS) activation, which in turn results in an increased production of vasoconstrictors and further contributes to elevated blood pressure 18 , 19 . Furthermore, the prevalence of hypertension in ADPKD owing to the progressive growth of kidney cysts tends to increase over time, regardless of normal or stable kidney function and proteinuria 20 . There is clear evidence of the benefits of controlling hypertension in children, especially those with chronic kidney disease 21 , as well as evidence supporting the efficacy and safety of ACEis and ARBs in pediatric patients, particularly in the context of renal hypertension. Moreover, Wright et al. have demonstrated their superiority over other anti-hypertensive drug classes, particularly in patients with proteinuria 22 . In our cohort, we observed that ACEis or ARBs were the most commonly prescribed anti-hypertensive medications, accounting for 55% of cases. When considering the addition of aldosterone blockers to the treatment regimen, medications targeting the RAAS blockade constituted approximately 63% of the prescribed medications for hypertension management. This suggests that RAAS inhibitors, including ACEis and ARBs, were the preferred choice for blood pressure control in our cohort.
The second most commonly prescribed anti-hypertensive medication category in our cohort was beta blockers, accounting for 22% of cases. Diuretics and CCBs accounted for 6% and 5% of the prescribed medications, respectively. These findings indicate that beta blockers were the next most frequently used anti-hypertensive agents, whereas diuretics and CCBs were less commonly employed for blood pressure management in our cohort of children with ADPKD. In adults with ADPKD, the evidence regarding the comparative efficacy of RAAS inhibitors versus beta-blockers or CCBs for blood pressure control is less conclusive 23 , 24 . Dual RAAS inhibitor therapy does not offer additional benefits in terms of blood pressure control compared with the use of an ACEi or ARB alone in adults with ADPKD 25 . Diuretics should be used cautiously in ADPKD, as they appear to have detrimental effects on the estimated glomerular filtration rate (eGFR) than when compared to ACEis 26 . Direct comparisons of anti-hypertensive medications in pediatric patients with ADPKD are limited. However, based on studies conducted in adult patients, RAAS inhibitors can be considered a reasonable choice for blood pressure control and slowing the decline in renal function compared with other anti-hypertensive agents. Further research is required to better understand the specific effects of optimal treatment approaches for hypertension in pediatric patients with ADPKD.
ADPKD is primarily caused by pathogenic mutations in the PKD1 or PKD2 genes, which encode for PC-1 and PC-2, respectively. These proteins play crucial roles in cardiac development and function, as evidenced in animal model studies. Moreover, there is an association between ADPKD and congenital heart defects with an overall prevalence of 1.84% reported in a large ADPKD cohort 27 . Notably, mitral valve prolapse has been reported in approximately 26% of patients with ADPKD due to PKD1 mutations 28 . In our cohort, approximately 2.5% of patients had congenital cardiac defects and 0.45% had mitral valve prolapse before or at ADPKD diagnosis. Over a follow-up period of at least one year, the incidence rate was 0.3 per 100 person-year for congenital cardiac defects and 0.2 per 100 person-year for mitral valve prolapse. These rates were higher than those observed in non-ADPKD patients, although the differences were not statistically significant. However, the HR for newly diagnosed congenital cardiac defects was elevated in children with ADPKD. These findings emphasize the importance of routine screening for congenital cardiac defects in patients newly diagnosed with ADPKD. Based on our observations, patients with ADPKD are at an increased risk of congenital cardiac defects; therefore, incorporating routine screening for congenital heart diseases (CHDs) as part of the diagnostic workup for ADPKD is necessary to ensure the early detection and appropriate management of these cardiac complications.
Previous cohort studies revealed an increased incidence of renal and cyst infections (by up to 15–25%) among ADPKD-diagnosed children 5 . In this study, UTI was the most prevalent urinary system diseases (10.7%), and the aHR of newly diagnosed UTI was 3.50 in the pediatric ADPKD population compared to that in the non-ADPKD population. Hematuria, as spontaneous, nephrolithiasis-related or after an abdominal trauma, occurs in 42% of patients with ADPKD, and approximately 10–14% of patients have microscopic or gross hematuria before the age of 16 years 3 . In a previous epidemiological study, isolated hematuria rates in Taiwanese elementary and junior high-school children were 0.13% and 0.18%, respectively 29 . Children with ADPKD also have a higher incidence of nephrolithiasis than that in the general population, which is attributable to anatomical and metabolic abnormalities. In our study, hematuria and nephrolithiasis were markedly more prevalent (aHRs, 5.55 and 13.17, respectively) among children with ADPKD than those without ADPKD, emphasizing the need for routine monitoring of these complications in pediatric patients with ADPKD.
Proteinuria, an indicator of CKD, causes glomerular hypertrophy and worsens tubulointerstitial damage and fibrosis 5 . Notably, a systematic review found a proteinuria prevalence of 20% in children with ADPKD 17 , whereas our cohort exhibited a lower prevalence, and only 2.2% of patients presented with proteinuria prior to ADPKD diagnosis. However, the IRR and aHR for developing proteinuria were 13.9 and 13.5, respectively. Cumulatively, pediatric patients with ADPKD had a significantly higher proteinuria incidence than non-ADPKD patients during follow-up. The cumulative incidence of proteinuria significantly surpassed those in both pediatric ADPKD and non-ADPKD patients over the follow-up period. Overt proteinuria correlates with advanced kidney structural issues and escalates with age in patients with ADPKD. Owing to its therapeutic and prognostic importance, proteinuria monitoring should be the standard in pediatric ADPKD care 5 . We found that 1.2% of children newly diagnosed with ADPKD already had CKD; furthermore, during the course of follow-up, 23 CKD events were documented among the 613 children with ADPKD, signifying a notably higher occurrence compared with that in the non-ADPKD group, which had no CKD events during the same period. A previous meta-analysis 30 conducted in adults demonstrated that the use of ACEis or ARBs to reduce proteinuria significantly enhanced renal survival in patients with CKD. Although randomized controlled trials in the pediatric population are lacking, it is prudent to consider ACEis or ARBs as primary treatment options for children with ADPKD presenting with proteinuria.
In a previous study, colonic diverticular disease was found to be associated with ADPKD 31 . In this study, there was nearly fourfold higher risk of developing diverticular disease in the intestine or colon after ADPKD was diagnosed. Statins (HMG-CoA reductase inhibitors) not only lower cholesterol, but also enhance renal blood flow and attenuate vascular inflammation through vascular and glomerular nitric oxide production 32 . In our cohort, statin use was approximately tenfold higher among children with ADPKD compared to that in the control group. The incidence of dyslipidemia was also 2.9-fold higher in the ADPKD group, which indicated that statins are used not only used for cholesterol control but also for renal protection in Taiwan. Interestingly, the incidence of hyperuricemia was notably higher in the pediatric ADPKD cohort than that in the non-ADPKD group. A previous study indicated that while hyperuricemia was not an independent factor for renal progression in adult ADPKD, it correlated with reduced eGFR, suggesting that correcting hyperuricemia might slow renal function decline in some patients with ADPKD 33 . The role of hyperuricemia in ADPKD progression remains unclear, necessitating further studies to validate the impact of hyperuricemia control in the ADPKD population.
Approximately 3% of children with ADPKD-causing mutations show very-early onset (VEO) or rapid disease progression 5 . Previous studies have described VEO ADPKD as having a higher risk of developing hypertension and a decline in glomerular filtration rates 34 , 35 . In our subgroup analysis of ADPKD patients younger than 1.5 years, the incidence rate of hypertension was 0.39 per 100 person-years, compared to none in the non-ADPKD group. ADPKD patients also had significant complications in hematuria (IRR: 5.18, P = 0.006) and urinary tract or cyst infections (IRR: 3.12, P < 0.001), suggesting the need for careful monitoring these younger patients.
Our large-scale, nationwide, population-based cohort study had several strengths and limitations. Our study used a large population to provide sufficient sample size and statistical power to evaluate the clinical characteristics of ADPKD in the pediatric population. Additionally, it used ICD-9 and ICD-10 codes for case selection, which avoided the need for questionnaires, minimized selection bias via multi-institutional follow-up linkage, and enabled the long-term follow-up of records. However, this study also has some limitations. First, ADPKD often remains asymptomatic in childhood. These patients come to medical attention due to presence of clinical symptoms such as hematuria, proteinuria and hypertension, or diagnosis inferred from family history. However, detailed clinical, disease severity, laboratory, radiographic data and family history were not available from the NHIRD. In addition, the accuracy of the medical codes may have affected the validity of the data. To minimize diagnostic miscoding errors, we only recruited patients with at least one inpatient claim or two outpatient claims for ADPKD and related complications at least 30 days after the index date of ADPKD diagnosis 36 . However, the true incidence and complication rates of ADPKD may have been underestimated because of our strict inclusion criteria or patients not seeking medical care. Future studies might explore the incorporation of additional diagnostic criteria, such as family history or genetic screening results, to provide a more comprehensive assessment of ADPKD incidence. Second, data on personal habits, such as lifestyle habits, smoking, and alcohol use, are not available in the NHIRD. These factors are important and can influence the propensity for cardiovascular and other complications. Finally, the impact of medications such as vasopressin antagonists (tolvaptan) on patients with ADPKD was not analyzed in the present study.
In conclusion, our study provides valuable information on the epidemiology of pediatric ADPKD in Taiwan, including data regarding its national incidence, typical medication use, and associated complications. These findings could be crucial for policymakers in developing clinical guidelines for better ADPKD management. Further prospective studies are also warranted to assess long-term outcomes in our ADPKD population.
DataAvailability
All data generated or analyzed during this study are included in this published article.
Solazzo, A. et al. The prevalence of autosomal dominant polycystic kidney disease (ADPKD): A meta-analysis of European literature and prevalence evaluation in the Italian province of Modena suggest that ADPKD is a rare and underdiagnosed condition. PLoS ONE 13 , e0190430 (2018).
Article PubMed PubMed Central Google Scholar
Lanktree, M. B. et al. Prevalence estimates of polycystic kidney and liver disease by population sequencing. J. Am. Soc. Nephrol. 29 , 2593–2600 (2018).
Article CAS PubMed PubMed Central Google Scholar
Reddy, B. V. & Chapman, A. B. The spectrum of autosomal dominant polycystic kidney disease in children and adolescents. Pediatr. Nephrol. 32 , 31–42 (2017).
Article PubMed Google Scholar
Olesen, E. T. B. & Fenton, R. A. Aquaporin 2 regulation: Implications for water balance and polycystic kidney diseases. Nat. Rev. Nephrol. 17 , 765–781 (2021).
Article CAS PubMed Google Scholar
Gimpel, C. et al. International consensus statement on the diagnosis and management of autosomal dominant polycystic kidney disease in children and young people. Nat. Rev. Nephrol. 15 , 713–726 (2019).
Cadnapaphornchai, M. A. Autosomal dominant polycystic kidney disease in children. Curr. Opin. Pediatr. 27 , 193–200 (2015).
Audrézet, M. P. et al. Comprehensive PKD1 and PKD2 mutation analysis in prenatal autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 27 , 722–729 (2016).
Chen, M. C., Chen, J. H., Chen, Y., Tsai, Y. H. & Lee, C. H. Low and decreased prevalence of congenital abdominal wall defect in Taiwan. J. Pediatr. Surg. 54 , 1958–1964 (2019).
Hsiao, Y. C., Wang, J. H., Chang, C. L., Hsieh, C. J. & Chen, M. C. Association between constipation and childhood nocturnal enuresis in Taiwan: A population-based matched case-control study. BMC Pediatr. 20 , 35 (2020).
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140 , e20171904 (2017).
Lurbe, E. et al. 2016 European Society of Hypertension guidelines for the management of high blood pressure in children and adolescents. J. Hypertens. 34 , 1887–1920 (2016).
Willey, C. J. et al. Prevalence of autosomal dominant polycystic kidney disease in the European Union. Nephrol. Dial. Transplant. 32 , 1356–1363 (2017).
PubMed Google Scholar
Kelleher, C. L., McFann, K. K., Johnson, A. M. & Schrier, R. W. Characteristics of hypertension in young adults with autosomal dominant polycystic kidney disease compared with the general US population. Am. J. Hypertension. 17 , 1029–1034 (2004).
Article Google Scholar
Fick, G. M. et al. The spectrum of autosomal dominant polycystic kidney disease in children. J. Am. Soc. Nephrol. 4 , 1654–1660 (1994).
Sedman, A. et al. Autosomal dominant polycystic kidney disease in childhood: A longitudinal study. Kidney Int. 31 , 1000–1005 (1987).
Seeman, T. et al. Ambulatory blood pressure correlates with renal volume and number of renal cysts in children with autosomal dominant polycystic kidney disease. Blood Press. Monit. 8 , 107–110 (2003).
Marlais, M. et al. Hypertension in autosomal dominant polycystic kidney disease: A meta-analysis. Arch. Dis. Child. 101 , 1142–1147 (2016).
Cadnapaphornchai, M. A. Hypertension in children with autosomal dominant polycystic kidney disease (ADPKD). Curr. Hypertens. Rev. 9 , 21–26 (2013).
Chapman, A. B., Johnson, A., Gabow, P. A. & Schrier, R. W. The renin–angiotensin–aldosterone system and autosomal dominant polycystic kidney disease. N. Eng. J. Med. 323 , 1091–1096 (1990).
Article CAS Google Scholar
Seeman, T., Jansky, P., Filip, F., Bláhová, K. & Jaroš, A. Increasing prevalence of hypertension during long-term follow-up in children with autosomal dominant polycystic kidney disease. Pediatr. Nephrol. 36 , 3717–3723 (2021).
Group, E. T. Strict blood-pressure control and progression of renal failure in children. N. Eng. J. Med . 361 , 1639–1650 (2009).
Wright, J. T. Jr. et al. Effect of blood pressure lowering and antihypertensive drug class on progression of hypertensive kidney disease: Results from the AASK trial. JAMA. 288 , 2421–2431 (2002).
Zeltner, R., Poliak, R., Stiasny, B., Schmieder, R. E. & Schulze, B. D. Renal and cardiac effects of antihypertensive treatment with ramipril vs metoprolol in autosomal dominant polycystic kidney disease. Nephrol. Dial. Transplant. 23 , 573–579 (2008).
Ecder, T. et al. Effect of antihypertensive therapy on renal function and urinary albumin excretion in hypertensive patients with autosomal dominant polycystic kidney disease. Am. J. Kidney Dis. 35 , 427–432 (2000).
Torres, V. E. et al. Angiotensin blockade in late autosomal dominant polycystic kidney disease. N. Engl. J. Med. 371 , 2267–2276 (2014).
Ecder, T. et al. Diuretics versus angiotensin-converting enzyme inhibitors in autosomal dominant polycystic kidney disease. Am. J. Nephrol. 21 , 98–103 (2001).
Chedid, M. et al. Congenital heart disease in adults with autosomal dominant polycystic kidney disease. Am. J. Nephrol. 53 , 316–324 (2022).
Lumiaho, A. et al. Mitral valve prolapse and mitral regurgitation are common in patients with polycystic kidney disease type 1. Am. J. Kidney Dis. 38 , 1208–1216 (2001).
Lin, C. C., Chiang, C. C., Jen, J. J. & Kao, S. M. The developments of mass urinary screening in Taiwan. Acta Paediatr. Taiwan. 42 , 130–133 (2001).
CAS PubMed Google Scholar
Heerspink, H. J. L., Kröpelin, T. F., Hoekman, J. & De Zeeuw, D. Drug-induced reduction in albuminuria is associated with subsequent renoprotection: A meta-analysis. J. Am. Soc. Nephrol. 26 , 2055 (2015).
Duarte-Chavez, R. et al. Colonic diverticular disease in autosomal dominant polycystic kidney disease: Is there really an association? A nationwide analysis. Int. J. Colorectal Dis. 36 , 83–91 (2021).
McFarlane, S., Muniyappa, R., Francisco, R. & Sowers, J. Pleiotropic effects of statins: Lipid reduction and beyond. J. Clin. Endocrinol. Metab. 87 , 1451–1458 (2002).
Han, M. et al. Hyperuricemia and deterioration of renal function in autosomal dominant polycystic kidney disease. BMC Nephrol. 15 , 63 (2014).
MacDermot, K. D., Saggar-Malik, A. K., Economides, D. L. & Jeffery, S. Prenatal diagnosis of autosomal dominant polycystic kidney disease (PKD1) presenting in utero and prognosis for very early onset disease. J Med Genet. 35 , 13–16 (1998).
Nowak, K. L., Cadnapaphornchai, M. A., Chonchol, M. B., Schrier, R. W. & Gitomer, B. Long-term outcomes in patients with very-early onset autosomal dominant polycystic kidney disease. Am J Nephrol. 44 , 171–178 (2016).
Chen, S. M., Huang, J. Y., Wu, M. C. & Chen, J. Y. The risk of developing constipation after neonatal necrotizing enterocolitis. Front. Pediatr. 8 , 120 (2020).
Article ADS CAS PubMed PubMed Central Google Scholar
Download references
Acknowledgements
This research was funded by the Buddhist Compassion Relief Tzu Chi Foundation (grant number: TCU-B02 (TCCF110195A)). The authors would like to thank Editage ( www.editage.com.tw ) for English language editing.
Buddhist Compassion Relief Tzu Chi Foundation (grant number:TCU-B02 (TCCF110195A)).
Author information
Authors and affiliations.
Department of Pediatrics, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, 97004, Taiwan
Chia-Yi Chin & Ming-Chun Chen
School of Medicine, Tzu Chi University, Hualien, 97004, Taiwan
Epidemiology and Biostatistics Center, Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Hualien, 97004, Taiwan
Wan-Ting Huang & Jen-Hung Wang
Department of Biochemistry, School of Medicine, Tzu Chi University, Hualien, 97004, Taiwan
Je-Wen Liou
Department of Biomedical Sciences and Engineering, Tzu Chi University, Hualien, 97004, Taiwan
Hao-Jen Hsu
You can also search for this author in PubMed Google Scholar
Contributions
M. C. C., J. W. L., and H. J. H. conceived and designed the study. W.-T.H. and J.-H.W. prepared the materials and collected the data. C.-Y.C., W.-T.H., J.-H.W., and M.-C.C. analyzed and interpreted the patient data. C.-Y.C. and M.-C.C. wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Ming-Chun Chen .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Chin, CY., Huang, WT., Wang, JH. et al. Overview of clinical status, treatment, and long-term outcomes of pediatric autosomal-dominant polycystic kidney disease: a nationwide survey in Taiwan. Sci Rep 14 , 16280 (2024). https://doi.org/10.1038/s41598-024-67250-z
Download citation
Received : 28 March 2024
Accepted : 09 July 2024
Published : 15 July 2024
DOI : https://doi.org/10.1038/s41598-024-67250-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autosomal-dominant polycystic kidney disease
- Complication
- Population-based cohort study
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
What Is Autosomal Dominant Polycystic Kidney Disease?
- 1 Division of Nephrology, McGill University Health Centre, Montreal, Quebec, Canada
- 2 University of Brest, Inserm, UMR 1078, GGB, CHU Brest, Brest, France
- 3 Division of Nephrology, Tufts University Medical Center, Boston, Massachusetts
- Original Investigation Exome Sequencing of a Clinical Population for Autosomal Dominant Polycystic Kidney Disease Alexander R. Chang, MD; Bryn S. Moore, MS; Jonathan Z. Luo, MS; Gino Sartori, MD; Brian Fang, BS; Steven Jacobs, MD; Yoosif Abdalla, MD; Mohammed Taher, MD; David J. Carey, PhD; William J. Triffo, MD, PhD; Gurmukteshwar Singh, MD; Tooraj Mirshahi, PhD JAMA
Autosomal dominant polycystic kidney disease is the most common genetic cause of kidney failure.
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disease in which individuals have a 50% chance of inheriting an ADPKD gene variant if one of their parents has ADPKD. However, in about 15% of patients, ADPKD arises from a genetic variant that was not inherited from either parent. ADPKD affects between 1 in 1000 and 1 in 2500 people worldwide and involves progressive growth of fluid-filled cysts in the kidneys.
People with ADPKD may also have cysts in their liver and pancreas, abdominal hernias, and cardiac valve abnormalities. Between 9% and 12% of patients with ADPKD have brain blood vessel abnormalities (aneurysms). Very rarely, these brain aneurysms can burst, which may result in permanent neurological damage or death.
Common Signs and Symptoms of ADPKD
In the early stages of disease, many individuals with ADPKD have no symptoms, although most have high blood pressure. As the kidney cysts increase in size, patients may develop abdominal pain or pressure, blood in the urine, kidney infections, and kidney stones. Over time, more than half of people with ADPKD develop kidney failure and need treatment with dialysis or kidney transplant. Onset of kidney failure is usually after age 50 years but may occur earlier.
Diagnosis of ADPKD
The recommended imaging test to diagnose ADPKD is ultrasound, which reveals cysts in the kidneys. Other imaging tests that may be considered are magnetic resonance imaging (MRI) or contrast-enhanced computed tomography (CT). Presence of kidney cysts confirms the diagnosis of ADPKD in people with a family history of ADPKD. If the diagnosis of ADPKD is uncertain based on imaging, genetic testing should be performed to confirm the diagnosis.
ADPKD Factors for Higher Risk of Kidney Failure
In ADPKD, certain categories of genetic variants are associated with more mild or severe disease. However, people with the same genetic variant may have different rates of progression to kidney failure. Kidney volume (adjusted for height and age) may help determine whether people with ADPKD are at a high risk of kidney failure because enlarged kidneys are associated with loss of kidney function.
Treatment of and Screening for ADPKD
Although there is currently no cure for ADPKD, treatments are available to improve outcomes. Medications to decrease blood pressure help slow the progression of kidney disease. Individuals with ADPKD should maintain an optimal weight, engage in regular physical exercise, have high water intake, limit salt to 5 grams per day, avoid smoking, and limit use of nonsteroidal anti-inflammatory drugs such as ibuprofen. A medication called tolvaptan may be taken by patients with ADPKD who are at higher risk of kidney failure but should be prescribed only by a physician experienced with this treatment.
Asymptomatic children of a parent with ADPKD should be closely monitored for high blood pressure but do not require screening before adulthood. Prior to being tested for ADPKD, adults with a family history of ADPKD should receive diagnostic counseling about the benefits of screening (timely initiation of treatment if ADPKD is diagnosed or reassurance if ADPKD is ruled out) and risks (potential problems with insurance and psychological aspects of being diagnosed with a genetic disease).
For More Information
National Institute of Diabetes and Digestive and Kidney Diseases
Published Online: March 17, 2023. doi:10.1001/jama.2023.2161
Conflict of Interest Disclosures: Dr Alam reported receiving personal fees from Otsuka Canada, Bayer, and AstraZeneca and grants from Otsuka Canada. Dr Perrone reported consulting for Otsuka (paid to institution); receiving grants from Sanofi, Palladiobio, Kadmon, and Reata; steering committee activity for Sanofi and Palladiobio (paid to institution); and receiving personal fees from Navitor, Carraway, UpToDate, Haymarket, and Reata. No other disclosures were reported.
Source: Cornec-Le Gall E, Alam A, Perrone RD. Autosomal dominant polycystic kidney disease. Lancet . 2019;393(10174):919-935. doi:10.1016/S0140-6736(18)32782-X
See More About
Alam A , Cornec-Le Gall E , Perrone RD. What Is Autosomal Dominant Polycystic Kidney Disease? JAMA. 2023;329(13):1128. doi:10.1001/jama.2023.2161
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Compliance with a healthful plant-based diet is associated with kidney function in patients with autosomal dominant polycystic kidney disease.

1. Introduction
2. materials and methods, 2.1. study participants, 2.2. clinical variables, 2.3. dietary assessment and pdis, 2.4. statistical analysis, 3.1. general characteristics of the study participants by egfr, 3.2. pdis according to the egfr and the correlation between pdis and kidney function, 3.3. associations between pdis and kidney function, 3.4. dietary intakes of study participants according to the median values of pdis, 4. discussion, supplementary materials, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Nobakht, N.; Hanna, R.M.; Al-Baghdadi, M.; Ameen, K.M.; Arman, F.; Nobahkt, E.; Kamgar, M.; Rastogi, A. Advances in Autosomal Dominant Polycystic Kidney Disease: A Clinical Review. Kidney Med. 2020 , 2 , 196–208. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Willey, C.J.; Blais, J.D.; Hall, A.K.; Krasa, H.B.; Makin, A.J.; Czerwiec, F.S. Prevalence of autosomal dominant polycystic kidney disease in the European Union. Nephrol. Dial. Transplant. 2017 , 32 , 1356–1363. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lanktree, M.B.; Haghighi, A.; Guiard, E.; Iliuta, I.A.; Song, X.; Harris, P.C.; Paterson, A.D.; Pei, Y. Prevalence Estimates of Polycystic Kidney and Liver Disease by Population Sequencing. J. Am. Soc. Nephrol. 2018 , 29 , 2593–2600. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chebib, F.T.; Torres, V.E. Autosomal Dominant Polycystic Kidney Disease: Core Curriculum 2016. Am. J. Kidney Dis. 2016 , 67 , 792–810. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chebib, F.T.; Zhou, X.; Garbinsky, D.; Davenport, E.; Nunna, S.; Oberdhan, D.; Fernandes, A. Tolvaptan and Kidney Function Decline in Older Individuals with Autosomal Dominant Polycystic Kidney Disease: A Pooled Analysis of Randomized Clinical Trials and Observational Studies. Kidney Med. 2023 , 5 , 100639. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chapman, A.B.; Devuyst, O.; Eckardt, K.U.; Gansevoort, R.T.; Harris, T.; Horie, S.; Kasiske, B.L.; Odland, D.; Pei, Y.; Perrone, R.D.; et al. Autosomal-dominant polycystic kidney disease (ADPKD): Executive summary from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2015 , 88 , 17–27. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ikizler, T.A.; Burrowes, J.D.; Byham-Gray, L.D.; Campbell, K.L.; Carrero, J.J.; Chan, W.; Fouque, D.; Friedman, A.N.; Ghaddar, S.; Goldstein-Fuchs, D.J.; et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am. J. Kidney Dis. 2020 , 76 , S1–S107. [ Google Scholar ] [ CrossRef ]
- Pickel, L.; Iliuta, I.A.; Scholey, J.; Pei, Y.; Sung, H.K. Dietary Interventions in Autosomal Dominant Polycystic Kidney Disease. Adv. Nutr. 2022 , 13 , 652–666. [ Google Scholar ] [ CrossRef ]
- Capelli, I.; Lerario, S.; Aiello, V.; Provenzano, M.; Di Costanzo, R.; Squadrani, A.; Vella, A.; Vicennati, V.; Poli, C.; La Manna, G.; et al. Diet and Physical Activity in Adult Dominant Polycystic Kidney Disease: A Review of the Literature. Nutrients 2023 , 15 , 2621. [ Google Scholar ] [ CrossRef ]
- Hemler, E.C.; Hu, F.B. Plant-Based Diets for Personal, Population, and Planetary Health. Adv. Nutr. 2019 , 10 , S275–S283. [ Google Scholar ] [ CrossRef ]
- Satija, A.; Hu, F.B. Plant-based diets and cardiovascular health. Trends Cardiovasc. Med. 2018 , 28 , 437–441. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Thompson, A.S.; Candussi, C.J.; Tresserra-Rimbau, A.; Jennings, A.; Bondonno, N.P.; Hill, C.; Sowah, S.A.; Cassidy, A.; Kühn, T. A healthful plant-based diet is associated with lower type 2 diabetes risk via improved metabolic state and organ function: A prospective cohort study. Diabetes Metab. 2023 , 50 , 101499. [ Google Scholar ] [ CrossRef ]
- Samtiya, M.; Aluko, R.E.; Dhewa, T.; Moreno-Rojas, J.M. Potential Health Benefits of Plant Food-Derived Bioactive Components: An Overview. Foods 2021 , 10 , 839. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, H.; Caulfield, L.E.; Garcia-Larsen, V.; Steffen, L.M.; Grams, M.E.; Coresh, J.; Rebholz, C.M. Plant-Based Diets and Incident CKD and Kidney Function. Clin. J. Am. Soc. Nephrol. 2019 , 14 , 682–691. [ Google Scholar ] [ CrossRef ]
- Carrero, J.J.; González-Ortiz, A.; Avesani, C.M.; Bakker, S.J.; Bellizzi, V.; Chauveau, P.; Clase, C.M.; Cupisti, A.; Espinosa-Cuevas, A.; Molina, P.; et al. Plant-based diets to manage the risks and complications of chronic kidney disease. Nat. Rev. Nephrol. 2020 , 16 , 525–542. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.; Castro III, A.F.; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009 , 150 , 604–612. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Satija, A.; Bhupathiraju, S.N.; Rimm, E.B.; Spiegelman, D.; Chiuve, S.E.; Borgi, L.; Willett, W.C.; Manson, J.E.; Sun, Q.; Hu, F.B. Plant-Based Dietary Patterns and Incidence of Type 2 Diabetes in US Men and Women: Results from Three Prospective Cohort Studies. PLoS Med. 2016 , 13 , e1002039. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moloudpour, B.; Jam, S.A.; Darbandi, M.; Janati, A.; Gholizadeh, M.; Najafi, F.; Pasdar, Y. Association Between Plant-based Diet and Kidney Function in Adults. J. Ren. Nutr. 2024 , 34 , 125–132. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Heo, G.Y.; Koh, H.B.; Kim, H.J.; Kim, K.W.; Jung, C.Y.; Kim, H.W.; Chang, T.I.; Park, J.T.; Yoo, T.H.; Kang, S.W.; et al. Association of Plant Protein Intake with Risk of Incident CKD: A UK Biobank Study. Am. J. Kidney Dis. 2023 , 82 , 687–697.e1. [ Google Scholar ] [ CrossRef ]
- Li, P.; Xia, C.; Liu, P.; Peng, Z.; Huang, H.; Wu, J.; He, Z. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in evaluation of inflammation in non-dialysis patients with end-stage renal disease (ESRD). BMC Nephrol. 2020 , 21 , 511. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ahbap, E.; Sakacı, T.; Kara, E.; Sahutoglu, T.; Koc, Y.; Basturk, T.; Sevınc, M.; Akgol, C.; Kayalar, A.; Ucar, Z.; et al. Neutrophil-to-lymphocyte ratio and platelet-tolymphocyte ratio in evaluation of inflammation in end-stage renal disease. Clin. Nephrol. 2016 , 85 , 199–208. [ Google Scholar ] [ CrossRef ]
- Khan, M.A.; Kassianos, A.J.; Hoy, W.E.; Alam, A.K.; Healy, H.G.; Gobe, G.C. Promoting Plant-Based Therapies for Chronic Kidney Disease. J. Evid.-Based Integr. Med. 2022 , 27 , 1–16. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ranganathan, N.; Anteyi, E. The Role of Dietary Fiber and Gut Microbiome Modulation in Progression of Chronic Kidney Disease. Toxins 2022 , 14 , 183. [ Google Scholar ] [ CrossRef ]
- Sirich, T.L.; Plummer, N.S.; Gardner, C.D.; Hostetter, T.H.; Meyer, T.W. Effect of increasing dietary fiber on plasma levels of colon-derived solutes in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2014 , 9 , 1603–1610. [ Google Scholar ] [ CrossRef ]
- Xie, L.M.; Ge, Y.Y.; Huang, X.; Zhang, Y.Q.; Li, J.X. Effects of fermentable dietary fiber supplementation on oxidative and inflammatory status in hemodialysis patients. Int. J. Clin. Exp. Med. 2015 , 8 , 1363–1369. [ Google Scholar ]
- Krishnamurthy, V.M.; Wei, G.; Baird, B.C.; Murtaugh, M.; Chonchol, M.B.; Raphael, K.L.; Greene, T.; Beddhu, S. High dietary fiber intake is associated with decreased inflammation and all-cause mortality in patients with chronic kidney disease. Kidney Int. 2012 , 81 , 300–306. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sakaguchi, Y.; Kaimori, J.Y.; Isaka, Y. Plant-Dominant Low Protein Diet: A Potential Alternative Dietary Practice for Patients with Chronic Kidney Disease. Nutrients 2023 , 15 , 1002. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kramers, B.J. Salt, but not protein intake, is associated with accelerated disease progression in autosomal dominant polycystic kidney disease. Kidney Int. 2020 , 98 , 989–998. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chebib, F.T.; Nowak, K.L.; Chonchol, M.B.; Bing, K.; Ghanem, A.; Rahbari-Oskoui, F.F.; Dahl, N.K.; Mrug, M. Polycystic Kidney Disease Diet: What is Known and What is Safe. Clin. J. Am. Soc. Nephrol. 2024 , 19 , 664–682. [ Google Scholar ] [ CrossRef ]
- Elmadfa, I.; Meyer, A.L. Animal Proteins as Important Contributors to a Healthy Human Diet. Annu. Rev. Anim. Biosci. 2017 , 5 , 111–131. [ Google Scholar ] [ CrossRef ]
- Alvirdizadeh, S.; Yuzbashian, E.; Mirmiran, P.; Eghtesadi, S.; Azizi, F. A prospective study on total protein, plant protein and animal protein in relation to the risk of incident chronic kidney disease. BMC Nephrol. 2020 , 21 , 489. [ Google Scholar ] [ CrossRef ] [ PubMed ]
Click here to enlarge figure
| Plant Food Groups | PDI | hPDI | uPDI | |
|---|---|---|---|---|
| Whole grains | Whole-grain breakfast cereal, other cooked breakfast cereal, cooked oatmeal, dark bread, brown rice, other grains, bran, wheat germ, popcorn | Positive | Positive | Reverse |
| Fruits | Raisins or grapes, prunes, bananas, cantaloupe, watermelon, fresh apples or pears, oranges, grapefruit, strawberries, blueberries, peaches or apricots or plums | Positive | Positive | Reverse |
| Vegetables | Tomatoes, tomato juice, tomato sauce, broccoli, cabbage, cauliflower, Brussels sprouts, carrots, mixed vegetables, yellow or winter squash, eggplant or zucchini, yams or sweet potatoes, spinach cooked, spinach raw, kale or mustard or chard greens, iceberg or head lettuce, romaine or leaf lettuce, celery, mushrooms, beets, alfalfa sprouts, garlic, corn | Positive | Positive | Reverse |
| Nuts | Nuts, peanut butter | Positive | Positive | Reverse |
| Legumes | String beans, tofu or soybeans, beans or lentils, peas or lima beans | Positive | Positive | Reverse |
| Vegetable oils | Oil-based salad dressing, vegetable oil used for cooking | Positive | Positive | Reverse |
| Tea and coffee | Tea, coffee, decaffeinated coffee | Positive | Positive | Reverse |
| Fruit juices | Apple cider (non-alcoholic) or juice, orange juice, grapefruit juice, other fruit juice | Positive | Reverse | Positive |
| Refined grains | Refined-grain breakfast cereal, white bread, English muffins or bagels or rolls, muffins or biscuits, white rice, pancakes or waffles, crackers, pasta | Positive | Reverse | Positive |
| Potatoes | French fries, baked or mashed potatoes, potato or corn chips | Positive | Reverse | Positive |
| Sugar-sweetened beverages | Colas with caffeine and sugar, colas without caffeine but with sugar, other carbonated beverages with sugar, non-carbonated fruit drinks with sugar | Positive | Reverse | Positive |
| Sweets and desserts | Chocolates, candy bars, candy without chocolate, cookies (home-baked and ready-made), brownies, doughnuts, cake (home-baked and ready-made), sweet rolls (home-baked and ready-made), pies (home-baked and ready-made), jams or jellies or preserves or syrup or honey | Positive | Reverse | Positive |
| Animal fat | Butter added to food, butter or lard used for cooking | Reverse | Reverse | Reverse |
| Dairy | Skimmed low-fat milk, whole milk, cream, sour cream, sherbet, ice cream, yogurt, cottage or ricotta cheese, cream cheese, other cheese | Reverse | Reverse | Reverse |
| Egg | Eggs | Reverse | Reverse | Reverse |
| Fish or seafood | Canned tuna, dark meat fish, other fish, shrimp or lobster or scallops | Reverse | Reverse | Reverse |
| Meat | Chicken or turkey with skin, chicken or turkey without skin, bacon, hot dogs, processed meats, liver, hamburger, beef or pork or lamb mixed dish, beef or pork or lamb main dish | Reverse | Reverse | Reverse |
| Miscellaneous animal-based foods | Pizza, chowder or cream soup, mayonnaise or other creamy salad dressing | Reverse | Reverse | Reverse |
| Early CKD (eGFR ≥ 60 mL/min/1.73 m ; n = 69) | Advanced CKD (eGFR < 60 mL/min/1.73 m ; n = 37) | p | |
|---|---|---|---|
| Age (y) | 49.80 ± 12.39 | 60.00 ± 9.10 | |
| Sex (M/F) | 33/36 | 20/17 | 0.541 |
| Height (cm) | 164.37 ± 8.70 | 165.23 ± 8.02 | 0.618 |
| Body weight (kg) | 63.08 ± 11.49 | 62.51 ± 10.91 | 0.805 |
| BMI (kg/m ) | 23.25 ± 3.06 | 22.76 ± 2.81 | 0.428 |
| Anemia, n (%) | 5 (7.2) | 12 (32.4) | |
| Diabetes, n (%) | 2 (2.9) | 3 (8.1) | 0.340 |
| Dyslipidemia, n (%) | 20 (29.0) | 20 (54.1) | |
| Gout, n (%) | 1 (1.4) | 2 (5.4) | 0.278 |
| Hypertension, n (%) | 43 (62.3) | 35 (94.6) | |
| Hyperuricemia, n (%) | 2 (2.9) | 4 (10.8) | 0.180 |
| SBP (mmHg) | 127.34 ± 13.72 | 126.91 ± 11.35 | 0.876 |
| DBP (mmHg) | 82.10 ± 10.30 | 81.15 ± 9.67 | 0.653 |
| ESR (mm/h) | 16.92 ± 18.73 | 21.94 ± 18.04 | 0.359 |
| Neutrophil–lymphocyte ratio | 1.80 ± 0.90 | 1.88 ± 0.72 | 0.662 |
| Platelet–lymphocyte ratio | 126.29 ± 43.00 | 128.67 ± 42.91 | 0.789 |
| Serum albumin (g/dL) | 4.33 ± 0.32 | 4.21 ± 0.22 | 0.039 |
| Hemoglobin (g/dL) | 13.43 ± 1.55 | 12.05 ± 1.48 | |
| Hematocrit (%) | 40.57 ± 4.13 | 37.26 ± 3.97 | |
| eGFR (mL/min/1.73 m ) | 89.48 ± 16.18 | 33.80 ± 13.57 | |
| BUN (mg/dL) | 14.12 ± 3.40 | 30.54 ± 14.20 | |
| Serum creatinine (mg/dL) | 0.88 ± 0.19 | 2.13 ± 0.81 | |
| Serum calcium (mg/dL) | 9.25 ± 0.33 | 9.20 ± 0.34 | 0.454 |
| Serum phosphorus (mg/dL) | 3.51 ± 0.51 | 3.60 ± 0.53 | 0.395 |
| Serum potassium (mmol/L) | 4.25 ± 0.28 | 4.59 ± 0.41 | |
| Serum sodium (mmol/L) | 140.67 ± 1.66 | 141.27 ± 2.28 | 0.122 |
| PDI | hPDI | uPDI | |
|---|---|---|---|
| SBP (mmHg) | 0.0003 | −0.088 | 0.015 |
| DBP (mmHg) | 0.134 | −0.039 | −0.030 |
| ESR (mm/h) | −0.182 | −0.237 | −0.061 |
| Neutrophil–lymphocyte ratio | −0.130 | 0.123 | |
| Platelet–lymphocyte ratio | 0.035 | 0.083 | |
| Serum albumin (g/dL) | −0.050 | 0.007 | −0.004 |
| Hemoglobin (g/dL) | −0.054 | 0.034 | −0.058 |
| Hematocrit (%) | −0.066 | 0.022 | −0.008 |
| eGFR (mL/min/1.73 m ) | 0.179 | ||
| BUN (mg/dL) | −0.106 | ||
| Serum creatinine (mg/dL) | |||
| Serum calcium (mg/dL) | −0.024 | −0.037 | 0.020 |
| Serum phosphorus (mg/dL) | −0.0002 | −0.040 | 0.063 |
| Serum potassium (mmol/L) | 0.008 | −0.014 | |
| Serum sodium (mmol/L) | 0.085 | 0.122 |
| PDI (Median Score = 54) | hPDI (Median Score = 57) | uPDI (Median Score = 54) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Low PDI (n = 50) | High PDI (n = 56) | p | Low hPDI (n = 52) | High hPDI (n = 54) | p | Low uPDI (n = 48) | High uPDI (n = 58) | p | |
| SBP (mmHg) | 124.94 ± 8.84 | 129.13 ± 15.41 | 0.103 | 129.08 ± 12.20 | 125.45 ± 13.43 | 0.157 | 125.31 ± 11.66 | 128.87 ± 13.84 | 0.166 |
| DBP (mmHg) | 80.30 ± 8.12 | 83.05 ± 11.38 | 0.169 | 81.24 ± 9.48 | 82.28 ± 10.63 | 0.605 | 80.65 ± 8.84 | 82.80 ± 11.01 | 0.283 |
| ESR (mm/h) | 19.83 ± 11.27 | 17.52 ± 22.55 | 0.654 | 21.00 ± 19.92 | 16.65 ± 17.46 | 0.397 | 16.41 ± 17.97 | 20.92 ± 19.16 | 0.377 |
| NLR | 1.90 ± 0.88 | 1.77 ± 0.78 | 0.411 | 2.08 ± 0.93 | 1.60 ± 0.65 | 1.78 ± 0.90 | 1.87 ± 0.78 | 0.576 | |
| PLR | 121.98 ± 38.23 | 132.12 ± 46.55 | 0.233 | 137.92 ± 44.67 | 116.38 ± 38.25 | 124.33 ± 46.39 | 129.47 ± 39.83 | 0.548 | |
| Serum albumin (g/dL) | 4.31 ± 0.27 | 4.27 ± 0.31 | 0.492 | 4.28 ± 0.31 | 4.30 ± 0.27 | 0.820 | 4.27 ± 0.27 | 4.31 ± 0.31 | 0.494 |
| Hemoglobin (g/dL) | 12.94 ± 1.74 | 12.94 ± 1.59 | 0.991 | 13.02 ± 1.46 | 12.86 ± 1.84 | 0.629 | 13.08 ± 1.60 | 12.83 ± 1.70 | 0.435 |
| Hematocrit (%) | 39.44 ± 4.57 | 39.37 ± 4.19 | 0.931 | 39.66 ± 3.90 | 39.15 ± 4.78 | 0.555 | 39.62 ± 4.17 | 39.23 ± 4.52 | 0.646 |
| eGFR (mL/min/1.73 m ) | 65.22 ± 30.47 | 74.35 ± 30.57 | 0.127 | 62.94 ± 33.20 | 76.89 ± 26.68 | 84.09 ± 25.00 | 58.42 ± 30.33 | ||
| BUN (mg/dL) | 21.26 ± 12.49 | 18.59 ± 11.05 | 0.245 | 22.88 ± 14.21 | 16.93 ± 7.89 | 15.60 ± 6.45 | 23.36 ± 13.90 | ||
| Serum creatinine (mg/dL) | 1.45 ± 0.83 | 1.20 ± 0.72 | 0.104 | 1.57 ± 0.91 | 1.07 ± 0.53 | 0.97 ± 0.37 | 1.61 ± 0.90 | ||
| Serum calcium (mg/dL) | 9.24 ± 0.35 | 9.22 ± 0.31 | 0.819 | 9.24 ± 0.35 | 9.22 ± 0.31 | 0.847 | 9.19 ± 0.29 | 9.27 ± 0.36 | 0.226 |
| Serum phosphorus (mg/dL) | 3.56 ± 0.54 | 3.53 ± 0.49 | 0.797 | 3.54 ± 0.54 | 3.55 ± 0.49 | 0.968 | 3.49 ± 0.45 | 3.59 ± 0.56 | 0.285 |
| Serum potassium (mmol/L) | 4.36 ± 0.38 | 4.37 ± 0.36 | 0.834 | 4.34 ± 0.38 | 4.39 ± 0.36 | 0.555 | 4.27 ± 0.33 | 4.45 ± 0.39 | |
| Serum sodium (mmol/L) | 140.78 ± 2.15 | 140.96 ± 1.68 | 0.622 | 140.58 ± 1.96 | 141.17 ± 1.83 | 0.113 | 140.65 ± 1.87 | 141.07 ± 1.94 | 0.258 |
| PDI (Median Score = 54) | hPDI (Median Score = 57) | uPDI (Median Score = 54) | ||||
|---|---|---|---|---|---|---|
| Low PDI (n = 50) | High PDI (n = 56) | Low hPDI (n = 52) | High hPDI (n = 54) | Low uPDI (n = 48) | High uPDI (n = 58) | |
| Model 1 Odds ratio (95% CI) | 1.00 (Ref) | 0.654 (0.293–1.459) p = 0.300 | 1.00 (Ref) | = 0.002 | 1.00 (Ref) | < 0.001 |
| Model 2 Odds ratio (95% CI) | 1.00 (Ref) | 0.462 (0.185–1.153) p = 0.098 | 1.00 (Ref) | < 0.001 | 1.00 (Ref) | < 0.001 |
| PDI (Median Score = 54) | hPDI (Median Score = 57) | uPDI (Median Score = 54) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Low PDI (n = 50) | High PDI (n = 56) | p | Low hPDI (n = 52) | High hPDI (n = 54) | p | Low uPDI (n = 48) | High uPDI (n = 58) | p | |
| Energy (kcal) | 1791.74 ± 435.05 | 1883.89 ± 494.47 | 0.313 | 1912.23 ± 490.23 | 1771.28 ± 437.90 | 0.121 | 1888.69 ± 543.46 | 1800.48 ± 394.27 | 0.336 |
| Carbohydrate (g) | 255.91 ± 56.79 | 285.50 ± 78.82 | 276.62 ± 70.29 | 266.66 ± 71.15 | 0.470 | 267.29 ± 77.51 | 275.06 ± 64.74 | 0.575 | |
| Fiber (g) | 21.60 ± 8.52 | 25.51 ± 9.80 | 20.60 ± 8.89 | 26.62 ± 8.96 | 25.69 ± 8.61 | 21.99 ± 9.73 | |||
| Protein (g) | 70.13 ± 21.29 | 71.47 ± 21.17 | 0.747 | 73.39 ± 23.35 | 68.38 ± 18.65 | 0.224 | 75.97 ± 22.95 | 66.59 ± 18.66 | |
| Animal protein (g) | 36.13 ± 17.10 | 34.31 ± 15.94 | 0.572 | 38.70 ± 18.22 | 31.77 ± 13.86 | 40.07 ± 17.44 | 31.11 ± 14.50 | ||
| Plant protein (g) | 32.50 ± 9.09 | 35.38 ± 10.06 | 0.126 | 32.85 ± 9.19 | 35.15 ± 10.08 | 0.222 | 34.58 ± 10.58 | 33.56 ± 8.93 | 0.590 |
| Fat (g) | 50.13 ± 20.12 | 47.99 ± 20.08 | 0.584 | 52.36 ± 21.35 | 45.76 ± 18.29 | 0.090 | 54.18 ± 22.99 | 44.71 ± 16.20 | |
| Cholesterol (mg) | 293.67 ± 151.40 | 294.44 ± 220.81 | 0.983 | 295.27 ± 128.13 | 292.93 ± 236.62 | 0.950 | 309.90 ± 140.30 | 280.98 ± 223.91 | 0.439 |
| SFAs (g) | 10.48 ± 5.69 | 10.87 ± 7.74 | 0.770 | 11.38 ± 6.65 | 10.01 ± 6.97 | 0.301 | 10.65 ± 5.03 | 10.71 ± 8.05 | 0.968 |
| MUFAs (g) | 12.41 ± 7.09 | 12.98 ± 9.52 | 0.728 | 13.01 ± 7.84 | 12.43 ± 9.02 | 0.724 | 12.83 ± 5.05 | 12.62 ± 10.47 | 0.900 |
| PUFAs (g) | 12.31 ± 5.89 | 13.75 ± 7.08 | 0.261 | 12.12 ± 6.44 | 13.99 ± 6.59 | 0.143 | 14.61 ± 7.00 | 11.79 ± 5.92 | |
| ω-6 PUFAs (g) | 4.77 ± 4.39 | 5.08 ± 4.53 | 0.727 | 4.43 ± 4.52 | 5.42 ± 4.36 | 0.252 | 5.54 ± 4.71 | 4.43 ± 4.19 | 0.201 |
| ω-3 PUFAs (g) | 1.04 ± 1.17 | 1.25 ± 2.14 | 0.534 | 0.92 ± 1.19 | 1.37 ± 2.14 | 0.185 | 1.55 ± 2.28 | 0.82 ± 1.05 | |
| Vit A (µg RAE) | 418.40 ± 216.31 | 499.70 ± 405.25 | 0.208 | 430.39 ± 321.43 | 491.16 ± 340.17 | 0.347 | 530.11 ± 354.74 | 404.44 ± 301.18 | 0.051 |
| Vit D (µg) | 3.91 ± 3.64 | 5.30 ± 9.79 | 0.343 | 4.89 ± 9.35 | 4.41 ± 5.33 | 0.746 | 5.65 ± 5.50 | 3.81 ± 8.85 | 0.212 |
| Vit E (mg α-TE) | 14.98 ± 4.96 | 18.60 ± 7.51 | 15.66 ± 5.30 | 18.08 ± 7.61 | 0.061 | 18.87 ± 7.85 | 15.25 ± 4.98 | ||
| Vit K (µg) | 151.54 ± 122.15 | 162.10 ± 108.17 | 0.638 | 141.76 ± 116.22 | 171.91 ± 111.99 | 0.177 | 158.71 ± 112.81 | 155.80 ± 116.92 | 0.897 |
| Vit B (mg) | 1.54 ± 0.50 | 1.67 ± 0.59 | 0.206 | 1.59 ± 0.51 | 1.63 ± 0.59 | 0.670 | 1.74 ± 0.62 | 1.50 ± 0.47 | |
| Vit B (mg) | 1.35 ± 0.45 | 1.33 ± 0.39 | 0.781 | 1.36 ± 0.45 | 1.32 ± 0.39 | 0.671 | 1.51 ± 0.45 | 1.20 ± 0.33 | |
| Niacin (mg NE) | 12.30 ± 4.42 | 13.57 ± 5.39 | 0.193 | 12.68 ± 4.99 | 13.25 ± 4.99 | 0.556 | 14.55 ± 5.38 | 11.66 ± 4.22 | |
| Vit B (mg) | 1.78 ± 1.13 | 1.90 ± 1.20 | 0.605 | 1.68 ± 0.91 | 1.99 ± 1.35 | 0.174 | 2.13 ± 1.36 | 1.60 ± 0.91 | |
| Folate (µg DFE) | 417.99 ± 127.67 | 451.09 ± 155.11 | 0.236 | 409.39 ± 141.37 | 460.60 ± 141.56 | 0.065 | 474.61 ± 145.80 | 403.09 ± 133.60 | |
| Vit B (µg) | 8.48 ± 5.81 | 8.19 ± 5.27 | 0.788 | 8.29 ± 6.26 | 8.36 ± 4.72 | 0.946 | 9.33 ± 5.03 | 7.49 ± 5.78 | 0.086 |
| Vit C (mg) | 96.98 ± 63.33 | 115.45 ± 72.17 | 0.167 | 92.82 ± 64.72 | 120.15 ± 69.85 | 116.27 ± 71.83 | 98.86 ± 65.10 | 0.194 | |
| Calcium (mg) | 461.22 ± 226.49 | 520.54 ± 219.48 | 0.174 | 481.35 ± 245.21 | 503.35 ± 202.66 | 0.615 | 535.82 ± 206.30 | 456.76 ± 232.89 | 0.070 |
| Phosphorus (mg) | 1006.38 ± 300.32 | 1063.32 ± 327.60 | 0.355 | 1027.47 ± 324.48 | 1045.13 ± 308.06 | 0.774 | 1134.14 ± 320.80 | 955.63 ± 288.18 | |
| Sodium (mg) | 2925.43 ± 941.94 | 3308.05 ± 1174.16 | 0.069 | 3058.52 ± 1178.10 | 3194.06 ± 989.55 | 0.522 | 3440.21 ± 989.24 | 2868.83 ± 1097.04 | |
| Potassium (mg) | 2518.73 ± 930.76 | 2906.80 ± 1081.18 | 0.052 | 2530.87 ± 1059.40 | 2909.49 ± 968.21 | 0.057 | 2974.40 ± 950.56 | 2516.31 ± 1049.15 | |
| PDI (Median Score = 54) | hPDI (Median Score = 57) | uPDI (Median Score = 54) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Low PDI (n = 50) | High PDI (n = 56) | p | Low hPDI (n = 52) | High hPDI (n = 54) | p | Low uPDI (n = 48) | High uPDI (n = 58) | p | |
| Protein intake (g/kg BW) | |||||||||
| Normal (≥0.8 g/kg BW) | 39 (78.0%) | 52 (92.9%) | 40 (76.9%) | 51 (94.4%) | 45 (93.75%) | 46 (79.3%) | |||
| Reduced (<0.8 g/kg BW) | 11 (22.0%) | 4 (7.1%) | 12 (23.1%) | 3 (5.6%) | 3 (6.25%) | 12 (20.7%) | |||
| Dietary Fiber | Dietary Protein | Dietary Animal Protein | Dietary Plant Protein | |
|---|---|---|---|---|
| SBP (mmHg) | −0.095 | −0.021 | 0.041 | −0.105 |
| DBP (mmHg) | 0.066 | 0.017 | 0.021 | 0.005 |
| ESR (mm/h) | −0.115 | −0.057 | 0.021 | −0.192 |
| Neutrophil–lymphocyte ratio | −0.101 | 0.003 | ||
| Platelet–lymphocyte ratio | −0.135 | −0.140 | −0.046 | |
| Serum albumin (g/dL) | 0.078 | 0.121 | 0.111 | 0.041 |
| Hemoglobin (g/dL) | 0.132 | 0.165 | 0.092 | |
| Hematocrit (%) | 0.126 | 0.148 | 0.076 | 0.191 |
| eGFR (mL/min/1.73 m ) | 0.118 | |||
| BUN (mg/dL) | −0.104 | |||
| Serum creatinine (mg/dL) | −0.180 | −0.158 | ||
| Serum calcium (mg/dL) | 0.055 | −0.043 | −0.059 | 0.023 |
| Serum phosphorus (mg/dL) | −0.029 | −0.015 | 0.003 | −0.073 |
| Serum potassium (mmol/L) | −0.047 | −0.013 | −0.018 | −0.001 |
| Serum sodium (mmol/L) | 0.046 | −0.154 | −0.143 | −0.067 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Heo, S.; Han, M.; Ryu, H.; Kang, E.; Kim, M.; Ahn, C.; Yang, S.J.; Oh, K.-H. Compliance with a Healthful Plant-Based Diet Is Associated with Kidney Function in Patients with Autosomal Dominant Polycystic Kidney Disease. Nutrients 2024 , 16 , 2749. https://doi.org/10.3390/nu16162749
Heo S, Han M, Ryu H, Kang E, Kim M, Ahn C, Yang SJ, Oh K-H. Compliance with a Healthful Plant-Based Diet Is Associated with Kidney Function in Patients with Autosomal Dominant Polycystic Kidney Disease. Nutrients . 2024; 16(16):2749. https://doi.org/10.3390/nu16162749
Heo, Sumin, Miyeun Han, Hyunjin Ryu, Eunjeong Kang, Minsang Kim, Curie Ahn, Soo Jin Yang, and Kook-Hwan Oh. 2024. "Compliance with a Healthful Plant-Based Diet Is Associated with Kidney Function in Patients with Autosomal Dominant Polycystic Kidney Disease" Nutrients 16, no. 16: 2749. https://doi.org/10.3390/nu16162749
Article Metrics
Supplementary material.
ZIP-Document (ZIP, 162 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Case Report
- Open access
- Published: 14 August 2024
Tubal mesosalpinx cysts combined with adnexal torsion in adolescents: a report of two cases and review of the literature
- Junzhuo Chen 1 ,
- Changjun Li 2 ,
- He Zhang 3 ,
- Dongqi Li 2 &
- Wei Wang 1
BMC Pediatrics volume 24 , Article number: 525 ( 2024 ) Cite this article
65 Accesses
Metrics details
Tubal mesosalpinx cysts are paratubal cysts, that account for approximately 10% of adnexal masses, and the presence of these cysts combined with adnexal torsion is a rare acute abdominal condition, with few cases reported in the literature. We reported two cases of adolescent tubal mesosalpinx cysts combined with adnexal torsion and reviewed the literature to help improve the diagnosis of the disease.
Case reports
The first patient was an 11-year-old girl with left lower abdominal pain for 5 days and fever with nausea and vomiting for 3 days, who was found to have a cystic pelvic mass on preoperative imaging and was diagnosed intraoperatively and postoperatively on pathology as having a left tubal mesosalpinx cyst combined with adnexal torsion. The second patient was a 13-year-old girl with right lower abdominal pain for 16 h and a palpable mass in the lower and middle abdomen on examination, which was hard and tender to palpate. Preoperative imaging revealed a large cystic mass in the right adnexal region, and intraoperative and postoperative pathology revealed a right tubal mesosalpinx cyst combined with adnexal torsion.
Conclusions
Tubal mesosalpinx cysts combined with adnexal torsion are rare causes of acute lower abdominal pain. Early diagnosis and timely surgery are necessary to ensure ovarian and tubal function. Accurate preoperative imaging diagnosis is challenging, and MRI is a beneficial supplement to ultrasound and CT examinations, providing more objective imaging information and reducing the incidence of adverse outcomes.
Peer Review reports
Tubal mesosalpinx cysts are paratubal cysts, that mostly occur in women of childbearing age and are rare in children and adolescent women [ 1 ]. It may lead to acute complications, such as rare adnexal torsion, which is more difficult to diagnose preoperatively. Adnexal torsion is the twisting of the adnexa around the infundibulopelvic ligament and the ovarian ligament. It is one of the gynecological acute abdominal conditions [ 2 , 3 ]. Adnexal torsion carries certain risks to future fertility, so early diagnosis and immediate intervention are necessary to ensure ovarian and tubal function in young female patients with adnexal torsion. However, due to the lack of specificity of its clinical manifestations, preoperative diagnosis of this disease is extremely difficult and it is often misdiagnosed, leading to delayed treatment [ 4 ]. We reported two cases of adolescent girls who were diagnosed with tubal mesosalpinx cysts combined with adnexal torsion and reviewed the literature to help improve the diagnosis of the disease.
An 11-year-old girl was admitted to the hospital with “left lower abdominal pain for 5 days and fever with nausea and vomiting for 3 days”. On physical examination, the abdomen appeared flat, the abdominal wall was soft, and there was tenderness and rebound pain in the left lower abdomen. Laboratory examination revealed a leukocyte count of 1.8 × 10 4 /L with no other abnormalities. The adolescent had her menarche half a month ago and experienced no menstrual pain.
Ultrasound revealed a cystic echo approximately 6.88cmx5.03 cm in the left adnexal region, with clear borders and regular morphology, and an enlarged and twisted ovary in front of the lesion on the same side, which is closely related to the cystic lesion, and the “ovarian crescent sign” [ 5 ] can be seen. CDFI showed no blood flow signal(Fig. 1 a). CT revealed a cystic lesion on the left side of the pelvis, measuring approximately 6.80 cm x 5.07 cm with a CT value of roughly 10 HU (Fig. 1 b and c). On MRI, the lesion displayed a low signal on T1WI and a high signal on T2WI. The boundary between the lesion and the left ovary was unclear. The left ovary exhibited swollen morphology and uneven density. The uterus showed external compressive changes and had a clear boundary with the cystic lesion (Fig. 1 d).

Imaging examination. ( a ) Ultrasound revealed a cystic echo (short arrow), poorly demarcated from the left ovary (slender arrow). ( b and c ) CT showed a round-like cystic lesion (short arrow) closely related to the left ovary (slender arrow), and the uterus (yellow arrow) showed extrinsic compressive changes. ( d ) The MRI sagittal view showed a round-like high signal (short arrow), and the lesion was poorly demarcated from the left ovary (slender arrow)
Surgery: Laparoscopic surgery was performed under general anesthesia. Intraoperatively, two trocars are placed lateral to the left rectus abdomins muscles, 2 cm above and 2 cm medial to the anterior superior iliac spine, respectively. Then, another trocar was placed at the right reverse McBurney’s point. It was found that the left adnexa was significantly enlarged with purplish-blue ischemic changes, and a cyst with a diameter of approximately 8 cm was observed in the left tubal tract area. The left fallopian tube and ovary twisted 2 turns along the infundibulopelvic ligament (Fig. 2 a and b). We repositioned the left adnexa, restored its blood supply. The ovary and the cyst were completely separated, and the cyst was completely stripped.
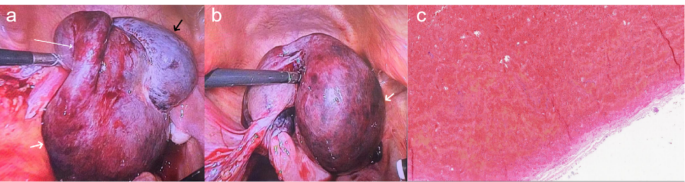
Operative findings during laparoscopy and postoperative pathological microscopic findings. ( a and b ) The left ovary appeared enlarged and purplish-blue (black arrow). The left fallopian tube (slender arrow) and ovary (black arrow) twisted 2 turns along the pelvic funnel ligament. A mesenteric cyst (short arrow) was observed adjacent to the left fallopian tube. ( c ) Postoperative pathological microscopic findings
Postoperative pathological microscopic findings: The specimen exhibited cystic wall-like tissue without clear overlying epithelium and significant hemorrhage within the wall, consistent with a cyst (Fig. 2 c).
A 13-year-old girl was admitted to the hospital with a complaint of “16 hours of pain in the lower right abdomen.” On physical examination, there was tenderness and rebound pain in the lower right abdomen, along with the detection of a mass measuring approximately 15.00 cm x 12.00 cm in the middle and lower abdomen. The mass exhibited a hard texture, tenderness, and mobility. The adolescent had her menarche one year ago and experienced no menstrual pain.
Ultrasound revealed a large cystic mass measuring approximately 16.00 cm x 10.00 cm in the right adnexal region, which was well demarcated from the ovary, and the ovarian crescent sign was visible. Torsion of the ovary secondary to pulling by the lesion. An enlarged ischemic right ovary measuring approximately 8.40 cm x 3.80 cm was detected next to the twisted tip, with no clear blood flow signal.
CT revealed a giant cystic occupancy on the right side of the pelvis, measuring approximately 16.50 cm x 11.84 cm. The fluid in the capsule was uniform in density, with a CT value of approximately 4 HU, and the wall of the capsule was slightly hyperdense. Its upper border extended to the lower border of the liver, and its lower border adjoined the right ovary and the right horn of the uterus. The uterus was shifted to the right side. The boundary between the cyst and the ovary was still clear, and there was a close local relationship. In addition, it can be observed that the right fallopian tube has thickened and twisted (Fig. 3 a and b, and 3 c).

( a )The CT coronal view showed a large cystic mass (slender arrow) in the pelvis, whose upper border reached the inferior border of the liver. ( b )The lower border of the large mass (slender arrow) pulled the right ovary (short arrow) and the right horn of the uterus (bold arrow). ( c )The CT sagittal view showed the lower edge of the large mass (slender arrow) pulled the ovary (short arrow), causing it to deform and shift. ( d ) Postoperative pathological microscopic findings
Surgery: Laparoscopic surgery was performed under general anesthesia. Intraoperatively, the pneumoperitoneum was first estalished. Two trocars were placed lateral to the left rectus abdomins muscles, 2 cm above and 2 cm medial to the anterior superior iliac spine, respectively. A drainage needle was used to extract some of the cystic fluid to reduce the volume of the cyst and facilitate subsequent operations. Then, another trocar was placed at the right reverse McBurney’s point. Laparoscopy showed the cyst originated from the right tubal mesosalpinx, approximately 16 cm in diameter. The cyst, together with the right adnexa, was twisted for 2 turns along the infundibulopelvic ligament. The right ovary was ischemic and swollen, with a purplish-blue color, and the right adnexa was reset to restore its blood supply. The ovary and the cyst were completely separated. Then, the cyst was completely stripped away.
Postoperative pathological microscopic findings: The specimen showed a fibrous tissue capsule wall, lined with columnar epithelium, vascular dilatation and congestion, and plasma exudation in the capsule (Fig. 3 d).
Tubal mesosalpinx cysts are independent of the fallopian tubes and ovaries. They originate from the broad ligament between the fallopian tube and the ovary and are easily confused with cystic masses originating from the ovary. They are histologically derived mainly from mesonephric duct remnant tissue, and their pathologic types include paratubal cysts, mesonephric duct cysts, and mesothelial cysts [ 6 , 7 ].
Most tubal mesosalpinx cysts are small in size and have no obvious clinical symptoms. Painful symptoms occur only when the cyst becomes larger and compresses the abdominal organs and tissues, but complications such as hemorrhage, torsion, or rupture are also rare [ 6 ]. When the diameter of the cyst is larger than 5 cm, the weight of the distal end of the fallopian tube increases, and the center of gravity changes, which may lead to torsion of the mesangial root and/or ovary [ 8 , 9 ]. Blockage of the blood supply artery can cause venous reflux obstruction, and in severe cases, it may cause ischemic necrosis of the ipsilateral fallopian tubes and ovaries [ 3 ]. Tubal mesosalpinx cysts in adolescent females and pregnant women tend to increase suddenly in size. It has been suggested that it may be due to the elevated hormone levels in adolescent females and pregnant women, which cause increased secretion of epithelial cells within the cysts. Therefore, the accumulation of secretions within the cyst leads to an increase in its volume, and it easily merges with the self-torsion or accessory torsion of the cyst [ 10 , 11 ]. In this paper, both girls experienced tubal mesosalpinx cysts with adnexal torsion shortly after menarche, which may also be related to increased hormone levels leading to cyst enlargement, consistent with the above literature.
Tubal mesosalpinx cysts are mostly benign, while junctional or malignant cysts are rare. They usually present as unilocular cystic lesions with thin smooth walls. If there is a papillary protrusion inside the cyst that is larger than 5 cm, the risk of malignancy increases [ 6 , 12 ].
The fact that it is challenging to diagnose paratubal and parovarian cysts. Multiple studies have shown that only 30–44% of paratubal tube cysts are accurately diagnosed preoperatively [ 3 , 13 , 14 ]. Ultrasound is the preferred examination for detecting adnexal masses. If torsion is suspected, a color Doppler examination should be added [ 13 ]. Tubal mesosalpinx cysts are often located on one side of the adnexal region or next to the uterorectal fossa. When the cyst is larger, it may be located in the anterior upper part of one side of the uterus, appearing circular or elliptical. The wall of the capsule is mostly thin and smooth, and the capsule is characterized by anechoic liquid dark areas. There may be divisions within the cystic mass, and when combined with bleeding, weak echoes of small light spots can be observed inside the cyst, even presenting as a cystic solid or as a fluid-filled plane. If combined with tubal torsion, a thickened, twisted, and locally dilated anechoic tubular structure can be seen next to the cyst, and the torsion may display a “vortex sign”. The dilated tubes are located on the inner side of the affected ovary and gradually become thinner towards both ends, forming " beak signs” [ 3 , 6 , 15 , 16 ]. If further ovarian torsion occurs, it will manifest as significant enlargement of the affected ovary, enhanced or reduced echogenicity, and disappearance of blood flow signals within the ovary. It should be noted that the presence of blood flow signals in the ovary does not exclude the possibility of torsion [ 13 ]. However, when the boundary between the mesosalpinx cyst and surrounding tissues is unclear, ultrasound is prone to missing diagnosis. The “ovarian crescent sign(OCS)” is a marker used in ultrasound to identify the nature of adnexal masses. This phenomenon is that normal ovarian tissue can be seen next to the adnexal mass, which is of great value for preoperative differentiation of benign or malignant adnexal masses. It can help to exclude invasive ovarian malignant tumors to some extent [ 5 , 17 , 18 ]. We reviewed the ultrasound images of two patients in this study and found the presence of OCS. Unfortunately, the primary diagnosis doctor, due to the lack of experience and specialized training on how to evaluate OCS, did not accurately identify this sign. In the second case, ultrasound revealed a large cystic mass in the right adnexal region pulling the ovary secondary to torsion, and an enlarged ischemic right ovary was detected next to the torsion tip. This patient was diagnosed by ultrasound with concomitant accessory torsion.
CT manifestations of mesosalpinx cysts are mainly circular or quasi-circular cystic masses near the uterus, with a few resembling sausages or serpentine cystic shadows. Cysts are often solitary and thin-walled with smooth margins and localized thickening of the cyst wall on enhancement scans. The capsule has a homogeneous water density with no enhancement; the density may increase when infection or bleeding occurs. The typical sign of tubal mesosalpinx cysts is the " holding ball” sign of the broad ligament of the uterus. When the cyst is large, it can compress and displace the abdominal organs. The larger the cyst, the more prone it is to pedicle torsion and rotation around the vascular pedicle axis. The most direct sign is the thickening and twisting of the fallopian tubes. Multiplanar reconstruction is particularly helpful for assessing the relative positions of the ovary and uterus, with the uterus typically pulled toward the side of torsion [ 3 , 6 , 19 ]. In addition, CT can help rule out other causes of lower abdominal pain, such as appendicitis [ 13 ]. In this report, both CT scans revealed cystic masses in the pelvic cavity, but the origin of the masses was difficult to determine and it was difficult to distinguish on imaging whether the masses originated from the ovary, fallopian tubes, or mesosalpinx.
MRI, with its advantages of high soft-tissue resolution, and multidirectional and multisequence imaging, can detect smaller lesions that are insensitive to ultrasound and can initially determine the benign or malignant nature of the lesions. Tubal mesosalpinx cysts on MRI mainly appear as round or round-like cystic lesions with a watery signal that is low on T1WI and high on T2WI. After enhanced scanning, the cyst wall shows enhancement, but there is no enhancement inside the cyst [ 20 ]. Compared with ultrasound and CT, MRI can more clearly display signs such as dilated tubes, beak signs, and twisted pedicles [ 8 ]. Especially if the patient is obese and the cyst is large, it is difficult for the ultrasound to determine its position relative to the ovary. In this case, MRI compensates for the shortcomings of ultrasound with a larger field of view showing the location of the cyst to the ovary, and it is also easier to show the relative positions of the uterus and ovary, with the uterus shifted to the side of the abnormality in the event of torsion [ 3 , 21 ]. Moreover, if there is no enhancement of the ovary on MRI enhancement scans, it is strongly suspected that torsion has caused ischemic necrosis of the ovary. In the first patient of this report, preoperative MRI revealed the enlarged ovary and upward flipping of the adnexa, which ultrasound failed to clearly show. MR can compensate for missed ultrasound findings. Unfortunately, the second patient did not undergo MR examination.
The main imaging features of adnexal torsion include twisted and thickened fallopian tubes, accompanied by ovarian enlargement and displacement, and pulling of the uterus to move towards the affected ovary side [ 3 , 22 , 23 ]. In this paper, the preoperative MRI of the first case showed enlarged ovaries with upward flipping of the adnexa. The second case showed the thickened and twisted fallopian tube. The lower edge of the large cyst pulled the ovary and the right horn of the uterus, causing deformation and displacement of the ovary, and pulling the uterus towards the twisted side. Both cases in this paper were adnexal torsion due to tubal mesosalpinx cysts, with the tubal thickening and torsion being more pronounced.
Diseases predisposing to adnexal torsion include hydrosalpinx, paratubal cysts, ovarian teratomas, and cysts [ 8 , 13 ]. Preoperative imaging to identify ovarian and tubal mesosalpinx cysts is challenging. When complications such as torsion or rupture occur, a clear diagnosis is rare before surgery, and surgery and pathology are required to make a clear diagnosis. In addition, the torsion of the hematosalpinx in patients with Mayer-Rokitanskt-Kuster-Hauser (MRKH) Syndrome is rare but still possible [ 24 ]. Therefore, adolescents with adnexal torsion should be aware of the presence of MRKH syndrome.
Tubal mesosalpinx cysts combined with adnexal torsion are rare acute abdominal conditions, and improving the accuracy of preoperative imaging diagnosis is crucial. MRI, as a supplement to ultrasound and CT, provides a broader field of view and effective information, aiding in comprehensive diagnosis and treatment, and reducing adverse outcomes. Imaging examinations should be timely, convenient, and precise, facilitating rapid diagnosis and guiding treatment to avoid delays. Nonetheless, laparoscopic exploration remains the gold standard for diagnosis and treatment. Immediate surgery can prevent damage to the ovaries and fallopian tubes, preserving reproductive function.

Data availability
Data is provided within the manuscript.
Zvizdic Z, Bukvic M, Murtezic S, Skenderi F, Vranic S. Giant Paratubal Serous Cystadenoma in an adolescent female: Case Report and Literature Review. J Pediatr Adolesc Gynecol. 2020;33(4):438–40. https://doi.org/10.1016/j.jpag.2020.03.010
Article PubMed Google Scholar
Alpendre F, Pedrosa I, Silva R, Batista S, Tapadinhas P. Giant paratubal cyst presenting as adnexal torsion: a case report. Case Rep Womens Health. 2020;27:e00222. https://doi.org/10.1016/j.crwh.2020.e00222
Article PubMed PubMed Central Google Scholar
Dawood MT, Naik M, Bharwani N, Sudderuddin SA, Rockall AG, Stewart VR. Adnexal Torsion: review of Radiologic appearances. Radiographics. 2021;41(2):609–24. https://doi.org/10.1148/rg.2021200118
Barloon TJ, Brown BP, Abu-Yousef MM, Warnock NG. Paraovarian and paratubal cysts: preoperative diagnosis using transabdominal and transvaginal sonography. J Clin Ultrasound. 1996;24(3):117–22. https://doi.org/10.1002/(SICI)1097-0096(199603)24:3%3C;117::AID-JCU2%3E;3.0.CO;2-K
Article CAS PubMed Google Scholar
Hillaby K, Aslam N, Salim R, Lawrence A, Raju KS, Jurkovic D. The value of detection of normal ovarian tissue (the ‘ovarian crescent sign’) in the differential diagnosis of adnexal masses. Ultrasound Obstet Gynecol. 2004;23(1):63–7. https://doi.org/10.1002/uog.946
Kiseli M, Caglar GS, Cengiz SD, Karadag D, Yılmaz MB. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet. 2012;285(6):1563–9. https://doi.org/10.1007/s00404-012-2304-8
Gupta A, Gupta P, Manaktala U, Khurana N. Clinical, radiological, and histopathological analysis of paraovarian cysts. J -Life Health. 2016;7(2):78. https://doi.org/10.4103/0976-7800.185337
Article Google Scholar
Qian L, Wang X, Li D, Li S, Ding J. Isolated fallopian tube torsion with paraovarian cysts: a case report and literature review. BMC Womens Health. 2021;21(1):345. https://doi.org/10.1186/s12905-021-01483-2
Breitowicz B, Wiebe BM, Rudnicki M. Torsion of bilateral paramesonephric cysts in young girls: Torsion of bilateral paramesonephric cysts. Acta Obstet Gynecol Scand. 2005;84(2):199–200. https://doi.org/10.1111/j.0001-6349.2005.0255c.x
Muolokwu E, Sanchez J, Bercaw JL, et al. Paratubal cysts, obesity, and hyperandrogenism. J Pediatr Surg. 2011;46(11):2164–7. https://doi.org/10.1016/j.jpedsurg.2011.07.011
Devouassoux-Shisheboran M, Silver SA, Tavassoli FA. Wolffian adnexal tumor, so-called female adnexal tumor of probable wolffian origin (FATWO). Hum Pathol. 1999;30(7):856–63. https://doi.org/10.1016/S0046-8177(99)90148-X
Thanasa A, Thanasa E, Xydias EM, et al. Pueperal Paratubal Cyst Torsion and secondary fallopian tube torsion without ovarian involvement: a Case Report. Cureus Published Online March. 2023;22. https://doi.org/10.7759/cureus.36540
Thakore SS, Chun MJ, Fitzpatrick K. Recurrent ovarian torsion due to Paratubal cysts in an adolescent female. J Pediatr Adolesc Gynecol. 2012;25(4):e85–7. https://doi.org/10.1016/j.jpag.2011.10.012
Darwish AM, Amin AF, Mohammad SA. Laparoscopic management of paratubal and paraovarian cysts. JSLS. 2003;7(2):101–6.
PubMed PubMed Central Google Scholar
Gross M, Blumstein SL, Chow LC. Isolated fallopian tube torsion: a rare twist on a common theme. Am J Roentgenol. 2005;185(6):1590–2. https://doi.org/10.2214/AJR.04.1646
Narayanan S, Bandarkar A, Bulas DI. Fallopian tube torsion in the Pediatric Age Group: radiologic evaluation. J Ultrasound Med. 2014;33(9):1697–704. https://doi.org/10.7863/ultra.33.9.1697
Stankovic ZB, Bjelica A, Djukic MK, Savic D. Value of ultrasonographic detection of normal ovarian tissue in the differential diagnosis of adnexal masses in pediatric patients. Ultrasound Obstet Gynecol. 2010;36(1):88–92. https://doi.org/10.1002/uog.7557
Van Holsbeke C, Van Belle V, Leone FPG, et al. Prospective external validation of the ‘ovarian crescent sign’ as a single ultrasound parameter to distinguish between benign and malignant adnexal pathology. Ultrasound Obstet Gynecol. 2010;36(1):81–7. https://doi.org/10.1002/uog.7625
Low S, Ong C, Lam S, Beh S. Paratubal cyst complicated by tubo-ovarian torsion: computed tomography features. Australas Radiol. 2005;49(2):136–9. https://doi.org/10.1111/j.1440-1673.2005.01405.x
Kishimoto K, Ito K, Awaya H, Matsunaga N, Outwater EK, Siegelman ES. Paraovarian cyst: MR imaging features. Abdom Imaging. 2002;27(6):685–9. https://doi.org/10.1007/s00261-002-0014-6
Stefanopol IA, Baroiu L, Neagu AI, et al. Clinical, imaging, histological and Surgical aspects regarding Giant Paraovarian cysts: a systematic review. Ther Clin Risk Manag. 2022;18:513–22. https://doi.org/10.2147/TCRM.S361476
Rha SE, Byun JY, Jung SE, et al. CT and MR Imaging features of Adnexal Torsion. Radiographics. 2002;22(2):283–94. https://doi.org/10.1148/radiographics.22.2.g02mr02283
Jung SI, Park HS, Yim Y, et al. Added Value of using a CT coronal reformation to diagnose Adnexal Torsion. Korean J Radiol. 2015;16(4):835. https://doi.org/10.3348/kjr.2015.16.4.835
Naem A, Sleiman Z. Unusual torsion of Hematosalpinx in a case of MRKH Syndrome. J Minim Invasive Gynecol. 2023;30(2):85–6. https://doi.org/10.1016/j.jmig.2022.11.010
Download references
No funding.
Author information
Authors and affiliations.
Department of Radiology, Beijing Youan Hospital, Capital Medical University, No. 8 Xitoutiao, Youanmen Street, Fengtai District, Beijing, 100069, China
Junzhuo Chen & Wei Wang
Department of Radiology, Linzhou People’s Hospital, Linzhou, China
Changjun Li & Dongqi Li
Department of Gynecology, Henan Provincial People’s Hospital, Zhengzhou, China
You can also search for this author in PubMed Google Scholar
Contributions
J.C. contributed to the investigation, data curation, and writing the original draft; C.L. contributed to preparing and image analysis; H.Z. contributed to surgical management and revising the work; D.L. contributed to the investigation and data curation; and W.W. contributed to the conceptualization, methodology, validation, reviewing and editing the article, and project administration. All the authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Wei Wang .
Ethics declarations
Ethics approval and consent to participate.
This is not applicable, as this is a case report.
Consent for publication
Informed consent was obtained from the patient’s parents for publication of clinical information and photographs. The parents of the two patients have signed the written informed consent forms.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Chen, J., Li, C., Zhang, H. et al. Tubal mesosalpinx cysts combined with adnexal torsion in adolescents: a report of two cases and review of the literature. BMC Pediatr 24 , 525 (2024). https://doi.org/10.1186/s12887-024-05001-9
Download citation
Received : 07 May 2024
Accepted : 08 August 2024
Published : 14 August 2024
DOI : https://doi.org/10.1186/s12887-024-05001-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Tubal mesosalpinx cysts
- Paratubal cysts
- Adnexal torsion
BMC Pediatrics
ISSN: 1471-2431
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Part 1. Overview Information
National Institutes of Health ( NIH )
U24 Resource-Related Research Projects – Cooperative Agreements
- April 4, 2024 - Overview of Grant Application and Review Changes for Due Dates on or after January 25, 2025. See Notice NOT-OD-24-084 .
- August 31, 2022 - Implementation Changes for Genomic Data Sharing Plans Included with Applications Due on or after January 25, 2023. See Notice NOT-OD-22-198 .
- August 5, 2022 - Implementation Details for the NIH Data Management and Sharing Policy. See Notice NOT-OD-22-189 .
Only one application per institution is allowed, as defined in Section III. 3. Additional Information on Eligibility .
This Notice of Funding Opportunity (NOFO) requests applications for the Central Coordinating Site for the Polycystic Kidney Disease (PKD) Core Centers. The Central Coordinating Site is expected to work collaboratively with the PKD Core Centers as part of the PKD Research Resource Consortium (PKD RRC) and serve as a national resource for the larger research community. The Central Coordinating Site will provide central administrative and communications support, and oversee data sharing for the PKD RRC. The Central Coordinating Site will also administer a Pilot and Feasibility Award program. All activities within the PKD RRC are expected to address the overall goal of improving our understanding of the pathogenesis, progression, prevention and clinical course of PKD through enhanced sharing of resources and establishment of a robust national research community. This NOFO is a companion announcement to RFA-DK-25-016: Polycystic Kidney Disease Core Centers (U54).
This Notice of Funding Opportunity (NOFO) requires a Plan for Enhancing Diverse Perspectives (PEDP).
October 14, 2024
| Application Due Dates | Review and Award Cycles | ||||
|---|---|---|---|---|---|
| New | Renewal / Resubmission / Revision (as allowed) | AIDS - New/Renewal/Resubmission/Revision, as allowed | Scientific Merit Review | Advisory Council Review | Earliest Start Date |
| November 14, 2024 | November 14, 2024 | Not Applicable | March 2025 | May 2025 | July 2025 |
All applications are due by 5:00 PM local time of applicant organization.
Applicants are encouraged to apply early to allow adequate time to make any corrections to errors found in the application during the submission process by the due date.
Not Applicable
It is critical that applicants follow the instructions in the Research (R) Instructions in the How to Apply - Application Guide , except where instructed to do otherwise (in this NOFO or in a Notice from NIH Guide for Grants and Contracts ).
Conformance to all requirements (both in the How to Apply - Application Guide and the NOFO) is required and strictly enforced. Applicants must read and follow all application instructions in the How to Apply - Application Guide as well as any program-specific instructions noted in Section IV. When the program-specific instructions deviate from those in the How to Apply - Application Guide , follow the program-specific instructions.
Applications that do not comply with these instructions may be delayed or not accepted for review.
There are several options available to submit your application through Grants.gov to NIH and Department of Health and Human Services partners. You must use one of these submission options to access the application forms for this opportunity.
- Use the NIH ASSIST system to prepare, submit and track your application online.
- Use an institutional system-to-system (S2S) solution to prepare and submit your application to Grants.gov and eRA Commons to track your application. Check with your institutional officials regarding availability.
- Use Grants.gov Workspace to prepare and submit your application and eRA Commons to track your application.
Part 2. Full Text of Announcement
Section i. notice of funding opportunity description.
Understanding and ameliorating autosomal dominant PKD and autosomal recessive PKD are central to the mission of NIDDK. The clinical course of these diseases is highly variable: some patients develop only a modest number of renal cysts, while others develop a massive number of renal cysts and renal failure at an early age. The diseases have extra-renal manifestations, including liver and systemic vasculature, with variable penetrance. Despite important advances in elucidating causative genetic defects, many challenges remain in determining the mechanisms of cyst development and enlargement, and the progressive loss of renal function in PKD that could potentially be targeted for therapeutic interventions.
In 2020, a national PKD Research Resource Consortium (PKD RRC, https://www.pkd-rrc.org ) was established with NIDDK funding with the goal of creating a framework for collaboration that develops and broadly shares research resources, core services and expertise to support innovation in research related to PKD. At present the PKD RRC consists of three national Research and Translation Core Centers and a Central Coordinating Site that collaborate to offer research resources, including cell and animal models, antibodies, and human PKD biological samples to the broader research community upon request. The PKD RRC has also developed a multi-center, longitudinal observational cohort of adults and children with PKD with linked biospecimens. In addition, the PKD RRC has developed a Genome browser which serves as a repository of variants across the exomes and targeted panel sequencing of individuals with PKD. These resources are available to the broader research community upon request. Through this NOFO, NIDDK aims to continue to support the development and sharing of existing resources while encouraging innovation of new and valuable resources to the PKD research community.
The present NOFO is issued to support a Central Coordinating Site to provide centralized administrative support to the PKD Core Centers. Applicants for the PKD Core Centers (requested through RFA-DK-25-016) are expected to work collaboratively with the Central Coordinating Site as part of the PKD RRC.
The expected outcome from this next phase of the PKD RRC will be:
- A broad-based effort to advance PKD research.
- Successful sharing of unique and relevant resources, data, tools, technologies, services, and expertise that address fundamental challenges in PKD research.
- A lowering of barriers to entry for new investigators and those who are from fields not traditionally involved in PKD research.
- Identification of emerging areas of science and anticipation of how these areas can be useful to PKD research.
- Periodic evaluation of the usefulness of shared resources and emphasis/deemphasis as appropriate.
- A broadening of the PKD research workforce to include more diverse perspectives.
- Incorporation of PKD patient perspectives into the work of the PKD RRC.
NIDDK recognizes that diverse teams working together and capitalizing on innovative ideas and distinct perspectives outperform homogeneous teams. There are many benefits that flow from a diverse scientific workforce, including: fostering scientific innovation, enhancing global competitiveness, contributing to robust learning environments, improving the quality of the research, advancing the likelihood that underserved populations participate in, and benefit from research, and enhancing public trust. NIDDK recognizes that many investigators share these values and endeavor to incorporate diverse perspectives into their projects and change the culture in science.
Objectives and Scope
The overall goal of the Central Coordinating Site is to organize and facilitate the activities of the PKD RRC, under the direction of the PKD RRC Steering Committee, to achieve the following objectives:
- Facilitate sharing of resources and data within the PKD RRC and with the wider PKD research community.
- Develop and implement multipronged outreach strategies and communication plans for disseminating information about the research resources and methods offered through the PKD Core Centers to the wider PKD research community. As part of the outreach strategy, the Central Coordinating Site is expected to plan and support an annual scientific symposium that brings together the PKD research community as a whole and highlights the resources offered by the PKD RRC. The symposium may be held either in person, virtually or a hybrid format.
- Plan and support an annual in-person Steering Committee meeting of the PKD RRC.
- Manage (or subcontract for the management of) a database of longitudinal clinical characteristics and imaging to allow sharing of de-identified data from patient participants from the PKD Core Centers and other willing institutions.
- Manage (or subcontract for the management of) other databases developed and contributed to by the PKD Core Centers (e.g. clinical database, Genome browser).
- Convene standing scientific working groups to discuss opportunities and emerging needs in PKD research, as well as metrics and benchmarking approaches to evaluate existing and potential novel technologies. As needed, the Central Coordinating Site may establish working groups (standing or ad hoc) around topics of interest to the PKD field as identified by program recipients or the wider research community, in consultation with NIDDK staff.
- Coordinate with the PKD Core Centers to solicit and incorporate PKD patient perspectives into the work of the PKD RRC.
- Manage and administer a Pilot and Feasibility Award Program to support early and innovative pilot projects in priority areas aligned with the goals of the PKD RRC. These may include early-stage, proof-of-principle studies that could generate preliminary data for larger studies; activities to advance dissemination of methods or tools; or the development and validation of standard processes and materials that may aid new technology evaluation. The program may enable new partnerships by encouraging collaborative projects. Funds for this program will be provided as part of the Central Coordinating Site and disbursed to successful applicants through a process jointly overseen by the PKD RRC Steering Committee and NIDDK.
- Develop, support, manage, and continually enhance a well-organized, user-friendly, intuitive, interactive PKD RRC website for internal and external communication.
- Plan, organize and support at least one annual face-to-face Steering Committee meeting for the PKD RRC investigator to be held in the Bethesda area or a location decided by the PKD RRC Steering Committee.
- Provide centralized administrative support, including coordination of Material Transfer Agreements and Data Use Agreements across the Consortium and with outside users,
- Schedule and coordinate web-based conference calls and webinars.
- Develop and implement a consortium-wide Plan for Enhancing Diverse Perspectives (PEDP).
Project Organization:
The PKD RRC will consist of approximately four PKD Core Centers and a single Central Coordinating Site. Applications for PKD Core Centers are solicited through a separate, companion NOFO (RFA-DK-25-016). The Central Coordinating Site will coordinate communications between the PKD RRC and the greater research community, organize and facilitate the education and outreach activities of the PKD RRC, and support and administer the Pilot and Feasibility Program. Investigators with appropriate expertise may apply to both this announcement (RFA-DK-25-015) and RFA-DK-25-016. An applicant without expertise in PKD research should include a co-investigator (or any other justified title) in the PKD field as Associate Director. The coordinated efforts of the PKD Core Centers and the Central Coordinating Site will be overseen by PKD RRC Steering Committee composed of PKD Core Centers Director(s), the Central Coordinating Site Director(s), and NIDDK program staff. The PKD Core Centers will meet at minimum once yearly for a face-to-face Steering Committee meeting in the Bethesda, MD area that will be coordinated by the Central Coordinating Site. The first meeting will be held on September 29, 2025, and all PKD Core Center Director(s), including the Biomedical Resource Core Director(s), Resource Development Core Director(s), and the Central Coordinating Site Director(s) are required to attend. The NIDDK may engage an External Experts Panel to advise the Institute on the progress of the PKD RRC.
See Section VIII. Other Information for award authorities and regulations.
Plan for Enhancing Diverse Perspectives (PEDP) The NIH recognizes that teams comprised of investigators with diverse perspectives working together and capitalizing on innovative ideas and distinct viewpoints outperform homogeneous teams. There are many benefits that flow from a scientific workforce rich with diverse perspectives, including: fostering scientific innovation, enhancing global competitiveness, contributing to robust learning environments, improving the quality of the research, advancing the likelihood that underserved populations participate in, and benefit from research, and enhancing public trust. To support the best science, the NIH encourages inclusivity in research guided by the consideration of diverse perspectives. Broadly, diverse perspectives can include but are not limited to the educational background and scientific expertise of the people who perform the research; the populations who participate as human subjects in research studies; and the places where research is done. This NOFO requires a Plan for Enhancing Diverse Perspectives (PEDP), which will be assessed as part of the scientific and technical peer review evaluation. Assessment of applications containing a PEDP are based on the scientific and technical merit of the proposed project. Consistent with federal law, the race, ethnicity, or sex (including gender identify, sexual orientation, or transgender status) of a researcher, award participant, or trainee will not be considered during the application review process or when making funding decisions. Applications that fail to include a PEDP will be considered incomplete and will be administratively withdrawn before review. The PEDP will be submitted as Other Project Information as an attachment (see Section IV). Applicants are strongly encouraged to read the NOFO instructions carefully and view the available PEDP guidance materials .
Section II. Award Information
Cooperative Agreement: A financial assistance mechanism used when there will be substantial Federal scientific or programmatic involvement. Substantial involvement means that, after award, NIH scientific or program staff will assist, guide, coordinate, or participate in project activities. See Section VI.2 for additional information about the substantial involvement for this NOFO.
The OER Glossary and the How to Apply - Application Guide provide details on these application types. Only those application types listed here are allowed for this NOFO.
Not Allowed: Only accepting applications that do not propose clinical trials.
Need help determining whether you are doing a clinical trial?
NIDDK intends to commit approximately $1.1 million in FY 2025 to fund one Central Coordinating Site award.
Application budgets are anticipated to be approximately $350,000 in direct costs per year. The applicant(s) may ask for $600,000 or more per year for an Opportunity Pool to support the Pilot and Feasibility Program. All Opportunity Pool costs are inclusive of F&A for the Central Coordinating Site and the subawardees. As such, the Central Coordinating Site should not calculate F&A on the Opportunity Pool set aside.
Application budgets should reflect the actual needs of the project.
The scope of the proposed project should determine the project period. The maximum project period is 5 years.
NIH grants policies as described in the NIH Grants Policy Statement will apply to the applications submitted and awards made from this NOFO.
Section III. Eligibility Information
1. eligible applicants eligible organizations higher education institutions public/state controlled institutions of higher education private institutions of higher education the following types of higher education institutions are always encouraged to apply for nih support as public or private institutions of higher education: hispanic-serving institutions historically black colleges and universities (hbcus) tribally controlled colleges and universities (tccus) alaska native and native hawaiian serving institutions asian american native american pacific islander serving institutions (aanapisis) nonprofits other than institutions of higher education nonprofits with 501(c)(3) irs status (other than institutions of higher education) nonprofits without 501(c)(3) irs status (other than institutions of higher education) for-profit organizations small businesses for-profit organizations (other than small businesses) local governments state governments county governments city or township governments special district governments indian/native american tribal governments (federally recognized) indian/native american tribal governments (other than federally recognized) federal governments eligible agencies of the federal government u.s. territory or possession other native american tribal organizations (other than federally recognized tribal governments) faith-based or community-based organizations regional organizations foreign organizations non-domestic (non-u.s.) entities (foreign organizations) are not eligible to apply. non-domestic (non-u.s.) components of u.s. organizations are not eligible to apply. foreign components, as defined in the nih grants policy statement , are allowed. required registrations applicant organizations applicant organizations must complete and maintain the following registrations as described in the how to apply - application guide to be eligible to apply for or receive an award. all registrations must be completed prior to the application being submitted. registration can take 6 weeks or more, so applicants should begin the registration process as soon as possible. failure to complete registrations in advance of a due date is not a valid reason for a late submission, please reference nih grants policy statement section 2.3.9.2 electronically submitted applications for additional information system for award management (sam) – applicants must complete and maintain an active registration, which requires renewal at least annually . the renewal process may require as much time as the initial registration. sam registration includes the assignment of a commercial and government entity (cage) code for domestic organizations which have not already been assigned a cage code. nato commercial and government entity (ncage) code – foreign organizations must obtain an ncage code (in lieu of a cage code) in order to register in sam. unique entity identifier (uei) - a uei is issued as part of the sam.gov registration process. the same uei must be used for all registrations, as well as on the grant application. era commons - once the unique organization identifier is established, organizations can register with era commons in tandem with completing their grants.gov registrations; all registrations must be in place by time of submission. era commons requires organizations to identify at least one signing official (so) and at least one program director/principal investigator (pd/pi) account in order to submit an application. grants.gov – applicants must have an active sam registration in order to complete the grants.gov registration. program directors/principal investigators (pd(s)/pi(s)) all pd(s)/pi(s) must have an era commons account. pd(s)/pi(s) should work with their organizational officials to either create a new account or to affiliate their existing account with the applicant organization in era commons. if the pd/pi is also the organizational signing official, they must have two distinct era commons accounts, one for each role. obtaining an era commons account can take up to 2 weeks. eligible individuals (program director/principal investigator) any individual(s) with the skills, knowledge, and resources necessary to carry out the proposed research as the program director(s)/principal investigator(s) (pd(s)/pi(s)) is invited to work with their organization to develop an application for support. individuals from diverse backgrounds, including individuals from underrepresented racial and ethnic groups, individuals with disabilities, and women are always encouraged to apply for nih support. see, reminder: notice of nih's encouragement of applications supporting individuals from underrepresented ethnic and racial groups as well as individuals with disabilities , not-od-22-019 and notice of nih's interest in diversity, not-od-20-031 . for institutions/organizations proposing multiple pds/pis, visit the multiple program director/principal investigator policy and submission details in the senior/key person profile (expanded) component of the how to apply - application guide . the central coordinating site director is required to have experience relevant to the oversight and outreach functions described in this nofo but is not required to have a background in pkd research. an applicant without expertise in pkd research should include a co-investigator (or any other justified title) in the pkd field as associate director. the central coordinating site director is expected to work closely with the pkd core centers and the niddk, including through participation on the pkd rrc steering committee, regular teleconference calls, and at relevant meetings and workshops supporting the pkd rrc goals. an associate director may be named, if adequately justified. 2. cost sharing.
This NOFO does not require cost sharing as defined in the NIH Grants Policy Statement NIH Grants Policy Statement Section 1.2 Definition of Terms.
3. Additional Information on Eligibility
Number of Applications
Applicant organizations may submit more than one application, provided that each application is scientifically distinct.
The NIH will not accept duplicate or highly overlapping applications under review at the same time, per NIH Grants Policy Statement Section 2.3.7.4 Submission of Resubmission Application . This means that the NIH will not accept:
- A new (A0) application that is submitted before issuance of the summary statement from the review of an overlapping new (A0) or resubmission (A1) application.
- A resubmission (A1) application that is submitted before issuance of the summary statement from the review of the previous new (A0) application.
- An application that has substantial overlap with another application pending appeal of initial peer review (see NIH Grants Policy Statement 2.3.9.4 Similar, Essentially Identical, or Identical Applications ).
Section IV. Application and Submission Information
1. requesting an application package.
The application forms package specific to this opportunity must be accessed through ASSIST, Grants.gov Workspace or an institutional system-to-system solution. Links to apply using ASSIST or Grants.gov Workspace are available in Part 1 of this NOFO. See your administrative office for instructions if you plan to use an institutional system-to-system solution.
2. Content and Form of Application Submission
It is critical that applicants follow the instructions in the Research (R) Instructions in the How to Apply - Application Guide except where instructed in this notice of funding opportunity to do otherwise. Conformance to the requirements in the How to Apply - Application Guide is required and strictly enforced. Applications that are out of compliance with these instructions may be delayed or not accepted for review.
Letter of Intent
Although a letter of intent is not required, is not binding, and does not enter into the review of a subsequent application, the information that it contains allows IC staff to estimate the potential review workload and plan the review.
By the date listed in Part 1. Overview Information , prospective applicants are asked to submit a letter of intent that includes the following information:
- Descriptive title of proposed activity
- Name(s), address(es), and telephone number(s) of the PD(s)/PI(s)
- Names of other key personnel
- Participating institution(s)
- Number and title of this funding opportunity
The letter of intent should be sent to:
John F. Connaughton, Ph.D. Chief, Scientific Review Branch National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Telephone: 301-594-7797 Email: [email protected]
Page Limitations
All page limitations described in the How to Apply – Application Guide and the Table of Page Limits must be followed.
The following section supplements the instructions found in the How to Apply – Application Guide and should be used for preparing an application to this NOFO.
SF424(R&R) Cover
All instructions in the How to Apply - Application Guide must be followed.
SF424(R&R) Project/Performance Site Locations
Sf424(r&r) other project information.
Other Attachments:
Statement of Willingness: Please title this attachment "Willingness to Participate" and provide a statement indicating a willingness to:
- Work with NIDDK and the PKD RRC to participate in the initial and annual meetings thereafter during the course of the grant award;
- Cooperatively interact with NIDDK and PKD RRC in support of the projects and activities;
- Work collaboratively with the PKD Core Centers to develop and execute Material Transfer Agreements and Data Use Agreements to permit sharing of resources, biological specimens and de-identified patient data;
- Actively seek input from NIDDK and the PKD RRC regarding resource or expertise needs that may arise during the performance of the project; and
- Participate in monthly conference calls.
Plan for Enhancing Diverse Perspectives (PEDP)
- In an "Other Attachment" entitled "Plan for Enhancing Diverse Perspectives," all applicants must include a summary of actionable strategies to advance the scientific and technical merit of the proposed project through expanded inclusivity.
- Applicants should align their proposed strategies for PEDP with the research strategy section, providing a holistic and integrated view of how enhancing diverse perspectives and inclusivity are buoyed throughout the application.
- The PEDP will vary depending on the scientific aims, expertise required, the environment and performance site(s), as well as how the project aims are structured.
- Actionable strategies using defined approaches for the inclusion of diverse perspectives in the project;
- Description of how the PEDP will advance the scientific and technical merit of the proposed project;
- Anticipated timeline of proposed PEDP activities;
- Evaluation methods for assessing the progress and success of PEDP activities.
Examples of items that advance inclusivity in research and may be appropriate for a PEDP can include, but are not limited to:
- Partnerships with different types of institutions and organizations (e.g., research-intensive; undergraduate-focused; HBCUs; emerging research institutions; community-based organizations).
- Project frameworks that enable communities and researchers to work collaboratively as equal partners in all phases of the research process.
- Outreach and planned engagement activities to enhance recruitment of individuals from diverse groups as human subjects in clinical trials, including those from underrepresented backgrounds.
- Description of planned partnerships that may enhance geographic and regional diversity.
- Outreach and recruiting activities intended to diversify the pool of applicants for research training programs, such as outreach to prospective applicants from groups underrepresented in the biomedical sciences, for example, individuals from underrepresented racial and ethnic groups, those with disabilities, those from disadvantaged backgrounds, and women.
- Plans to utilize the project infrastructure (i.e., research and structure) to enhance the research environment and support career-advancing opportunities for junior, early- and mid-career researchers.
- Transdisciplinary research projects and collaborations among researchers from fields beyond the biological sciences, such as physics, engineering, mathematics, computational biology, computer and data sciences, as well as bioethics.
Examples of items that are not appropriate in a PEDP include, but are not limited to:
- Selection or hiring of personnel for a research team based on their race, ethnicity, or sex (including gender identify, sexual orientation, or transgender status).
- A training or mentorship program limited to certain researchers based on their race, ethnicity, or sex (including gender identify, sexual orientation, or transgender status).
For further information on the Plan for Enhancing Diverse Perspectives (PEDP), please see PEDP guidance materials .
SF424(R&R) Senior/Key Person Profile
The CCS Director is required to have a record of accomplishment in oversight, organizational facilitation, and outreach as specified in this NOFO but is not required to have a background in PKD research. An Associate Director may be named, if adequately justified.
R&R Budget
The Director of the Central Coordinating Site will facilitate the activities and outreach strategies of the PKD RRC. The minimum level of effort for the Central Coordinating Site Director is 1.2 person months (10% effort). An Associate Director may be named as well, but the total, combined Directorship efforts may not exceed 2.4 person months. The Central Coordinating Site may also include administrative assistant(s) and specialized support personnel (e.g. website developer, database manager) and must be adequately justified.
The overall budget must include funds to support for the annual PKD RRC face-to-face Steering Committee meeting and travel for the Central Coordinating Site Director to attend the meeting. In addition, the budget should include funds to support the annual scientific symposium of the PKD RRC. A Professional Enrichment Program may be proposed to support travel of PKD RRC investigators to learn new laboratory techniques, develop new collaborations, or engage in scientific information exchange as described in Section I. The Central Coordinating Site budget will include a separate Opportunity Pool of approximately $600,000 total costs per year to fund the Pilot and Feasibility Program (which is inclusive of Facilities and Administration costs). The Pilot and Feasibility projects may include voucher programs or full grants for up to two years.
Budget Justification: Describe the specific functions of all key personnel, consultants, collaborators, and support staff. For years 2-5 of support requested, justify any significant increase or decrease in any category over the initial budget period. Identify such changes with asterisks against the appropriate amounts.
PEDP implementation costs: Applicants may include allowable costs associated with PEDP implementation (as outlined in the Grants Policy Statement section 7): https://grants.nih.gov/grants/policy/nihgps/html5/section_7/7.1_general.htm.
R&R Subaward Budget
Phs 398 cover page supplement, phs 398 research plan.
All instructions in the How to Apply - Application Guide must be followed, with the following additional instructions:
Specific Aims: The specific aims should reflect an integrated approach to reach the goal of the PKD RRC as described in Section I.
Research Strategy: The overall goal of the Central Coordinating Site is to facilitate the efforts of the PKD RRC with particular emphasis on outreach to the widest possible research community. The Central Coordinating Site will work with the PKD Core Centers and the PKD RRC Steering Committee. The Central Coordinating Site should provide a plan for administrative coordination of the PKD RRC activities including the elements below:
- Provide an overview of how the Central Coordinating Site will be structured and how that structure will facilitate the objectives of the PKD RRC. Describe previous experience in facilitating collaborations and in coordination of large, complex research efforts. Include a description of the expertise and the staffing and management structure planned, without duplicating information from the biosketches.
- Describe how the proposed Central Coordinating Site will organize, track, and facilitate the sharing of PKD RRC resources within and outside of the PKD RRC.
- Describe how the Central Coordinating Site will develop, support, manage, and continually enhance a well-organized, user-friendly, intuitive, interactive PKD RRC website for internal and external communication.
- Describe how the Central Coordinating Site will coordinate with the PKD Core Centers to solicit and incorporate PKD patient perspectives into the work of the PKD RRC.
- Describe how the Central Coordinating Site will develop a transparent method to track requests for models, cells, molecules, genes, data, and expert consultations regarding tools provided by PKD RRC investigators.
- Propose plans for coordinating working groups as described in the Research Objectives in Section I. Describe how the Central Coordinating Site will facilitate collaborative Consortium-wide discussions that identify emerging areas of science and anticipate the needs of the PKD research community. Include strategies for consensus building, development of recommendations, and promotion of group outcomes, as well as approaches for facilitating interactions with investigators within and outside of the PKD RRC. Propose and justify any other activities relevant to facilitating collaborations and coordinating scientifically focused discussion groups. The Central Coordinating Site will organize regular web-based conference calls of the PKD RRC Steering Committee, subcommittees, and working groups. The Central Coordinating Site should provide a plan to organize and support an annual, face-to-face meeting of the PKD RRC Steering Committee in the vicinity of Bethesda MD.
Communication and Outreach
- Propose innovative and multipronged communication strategies to ensure that the resources of the PKD RRC are widely known and effectively utilized within and outside the PKD RRC. Provide an overview of target audience(s) and methods. Describe how the Central Coordinating Site will utilize all relevant avenues and modes of communication across the wider research community to ensure that a broad range of investigators are aware of and are encouraged to use the resources of the PKD RRC.
- Provide plans to facilitate and promote educational activities for the PKD RRC. The educational activities should aim to expand the pool of investigators who utilize the PKD RRC resources and who are drawn into the field of PKD research. It is expected that this program would provide outreach to a larger research community and provide a means for inclusion of new disciplines into PKD research. The educational activities may also include, but are not limited to, web-based lecture series by experts with scientific backgrounds that are not traditionally involved in PKD research; or workshops that educate PKD Core Centers members and the wider research community on how to use available databases or resources.
Database development and support
- Describe how the Central Coordinating Site will support, maintain, enhance, and further develop a shareable longitudinal database of deidentified clinical variables and imaging from patient–participants at those PKD Core Centers that include a clinical/translational core as a Biomedical Core and from any other institution that wish to contribute deidentified data to the database. Describe how sharing of the database will be accomplished. The database development and management may be done by staff at the Central Coordinating Site or subcontracted where expertise is available.
- Describe how the Central Coordinating Site will support, maintain, enhance, and further develop a shareable Genome browser that the PKD RRC has developed and is being shared via the PKD RRC website. Describe how sharing of the database will be accomplished. The database development and management may be done by staff at the Central Coordinating Site or subcontracted where expertise is available.
Pilot and Feasibility Projects Program
- Describe a plan to manage the open solicitation, rigorous review, and unbiased selection of projects to be funded under the Pilot and Feasibility Program designed to enrich and grow the PKD research community. The Central Coordinating Site will be responsible for award subcontracts and provide fiscal oversight for Pilot and Feasibility Projects. The Pilot and Feasibility projects are intended for (a) junior investigators or (b) established investigators not previously involved in PKD research. The Pilot and Feasibility Program is not intended to support or supplement ongoing research of an established PKD investigator. Pilot and Feasibility project proposals will be assessed by unbiased independent content experts selected by the Central Coordinating Site and approved by the PKD RRC Steering Committee. These experts will provide comments on scientific merit for submitted Pilot and Feasibility applications to the PKD RRC Steering Committee and NIDDK. The PKD RRC Steering Committee will make final award decisions based on review, the availability of funds, and the PKD RRC program priorities, in consultation with NIDDK.
Letters of Support: Include all assurance letters including institutional commitments and outside collaborations, if such plans are listed in application. The Letters of Support attachment should begin with a table of letter authors, their institutions, and the type of each letter (institutional commitment or resources; collaboration or role in the project; potential or current user of a resource or service proposed in the application).
Resource Sharing Plan : Individuals are required to comply with the instructions for the Resource Sharing Plans as provided in the How to Apply - Application Guide .
Other Plan(s):
All instructions in the How to Apply - Application Guide must be followed, with the following additional instructions:
- All applicants planning research (funded or conducted in whole or in part by NIH) that results in the generation of scientific data are required to comply with the instructions for the Data Management and Sharing Plan. All applications, regardless of the amount of direct costs requested for any one year, must address a Data Management and Sharing Plan.
Appendix: Only limited Appendix materials are allowed. Follow all instructions for the Appendix as described in the How to Apply - Application Guide .
- No publications or other material, with the exception of blank questionnaires or blank surveys, may be included in the Appendix.
PHS Human Subjects and Clinical Trials Information
When involving human subjects research, clinical research, and/or NIH-defined clinical trials (and when applicable, clinical trials research experience) follow all instructions for the PHS Human Subjects and Clinical Trials Information form in the How to Apply - Application Guide , with the following additional instructions:
If you answered “Yes” to the question “Are Human Subjects Involved?” on the R&R Other Project Information form, you must include at least one human subjects study record using the Study Record: PHS Human Subjects and Clinical Trials Information form or Delayed Onset Study record.
Study Record: PHS Human Subjects and Clinical Trials Information
Delayed Onset Study
Note: Delayed onset does NOT apply to a study that can be described but will not start immediately (i.e., delayed start). All instructions in the How to Apply - Application Guide must be followed.
PHS Assignment Request Form
3. unique entity identifier and system for award management (sam).
See Part 2. Section III.1 for information regarding the requirement for obtaining a unique entity identifier and for completing and maintaining active registrations in System for Award Management (SAM), NATO Commercial and Government Entity (NCAGE) Code (if applicable), eRA Commons, and Grants.gov
4. Submission Dates and Times
Part I. contains information about Key Dates and times. Applicants are encouraged to submit applications before the due date to ensure they have time to make any application corrections that might be necessary for successful submission. When a submission date falls on a weekend or Federal holiday , the application deadline is automatically extended to the next business day.
Organizations must submit applications to Grants.gov (the online portal to find and apply for grants across all Federal agencies). Applicants must then complete the submission process by tracking the status of the application in the eRA Commons , NIH’s electronic system for grants administration. NIH and Grants.gov systems check the application against many of the application instructions upon submission. Errors must be corrected and a changed/corrected application must be submitted to Grants.gov on or before the application due date and time. If a Changed/Corrected application is submitted after the deadline, the application will be considered late. Applications that miss the due date and time are subjected to the NIH Grants Policy Statement Section 2.3.9.2 Electronically Submitted Applications .
Applicants are responsible for viewing their application before the due date in the eRA Commons to ensure accurate and successful submission.
Information on the submission process and a definition of on-time submission are provided in the How to Apply – Application Guide .
5. Intergovernmental Review (E.O. 12372)
This initiative is not subject to intergovernmental review.
6. Funding Restrictions
All NIH awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Pre-award costs are allowable only as described in the NIH Grants Policy Statement Section 7.9.1 Selected Items of Cost .
Applications must be submitted electronically following the instructions described in the How to Apply - Application Guide . Paper applications will not be accepted.
Applicants must complete all required registrations before the application due date. Section III. Eligibility Information contains information about registration.
For assistance with your electronic application or for more information on the electronic submission process, visit How to Apply – Application Guide . If you encounter a system issue beyond your control that threatens your ability to complete the submission process on-time, you must follow the Dealing with System Issues guidance. For assistance with application submission, contact the Application Submission Contacts in Section VII .
Important reminders:
All PD(s)/PI(s) must include their eRA Commons ID in the Credential field of the Senior/Key Person Profile form . Failure to register in the Commons and to include a valid PD/PI Commons ID in the credential field will prevent the successful submission of an electronic application to NIH. See Section III of this NOFO for information on registration requirements.
The applicant organization must ensure that the unique entity identifier provided on the application is the same identifier used in the organization’s profile in the eRA Commons and for the System for Award Management. Additional information may be found in the How to Apply - Application Guide .
See more tips for avoiding common errors.
Applications must include a PEDP submitted as Other Project Information as an attachment. Applications that fail to include a PEDP will be considered incomplete and will be administratively withdrawn before review.
Upon receipt, applications will be evaluated for completeness and compliance with application instructions by the Center for Scientific Review and responsiveness by the National Institute of Diabetes and Digestive and Kidney Diseases, NIH. Applications that are incomplete, non-compliant and/or nonresponsive will not be reviewed.
Use of Common Data Elements in NIH-funded Research
Many NIH ICs encourage the use of common data elements (CDEs) in basic, clinical, and applied research, patient registries, and other human subject research to facilitate broader and more effective use of data and advance research across studies. CDEs are data elements that have been identified and defined for use in multiple data sets across different studies. Use of CDEs can facilitate data sharing and standardization to improve data quality and enable data integration from multiple studies and sources, including electronic health records. NIH ICs have identified CDEs for many clinical domains (e.g., neurological disease), types of studies (e.g. genome-wide association studies (GWAS)), types of outcomes (e.g., patient-reported outcomes), and patient registries (e.g., the Global Rare Diseases Patient Registry and Data Repository). NIH has established a “Common Data Element (CDE) Resource Portal" ( http://cde.nih.gov/ ) to assist investigators in identifying NIH-supported CDEs when developing protocols, case report forms, and other instruments for data collection. The Portal provides guidance about and access to NIH-supported CDE initiatives and other tools and resources for the appropriate use of CDEs and data standards in NIH-funded research. Investigators are encouraged to consult the Portal and describe in their applications any use they will make of NIH-supported CDEs in their projects.
Recipients or subrecipients must submit any information related to violations of federal criminal law involving fraud, bribery, or gratuity violations potentially affecting the federal award. See Mandatory Disclosures, 2 CFR 200.113 and NIH Grants Policy Statement Section 4.1.35 .
Send written disclosures to the NIH Chief Grants Management Officer listed on the Notice of Award for the IC that funded the award and to the HHS Office of Inspector Grant Self Disclosure Program at [email protected] .
Post Submission Materials
Applicants are required to follow the instructions for post-submission materials, as described in the policy
Section V. Application Review Information
1. criteria.
Only the review criteria described below will be considered in the review process. Applications submitted to the NIH in support of the NIH mission are evaluated for scientific and technical merit through the NIH peer review system.
Reviewers will provide an overall impact score to reflect their assessment of the likelihood for the project to exert a sustained, powerful influence on the research field(s) involved, in consideration of the following review criteria and additional review criteria (as applicable for the project proposed).As part of the overall impact score, reviewers should consider and indicate how the Plan to Enhance Diverse Perspectives affects the scientific merit of the project.
Reviewers will consider each of the review criteria below in the determination of scientific merit and give a separate score for each. An application does not need to be strong in all categories to be judged likely to have major scientific impact. For example, a project that by its nature is not innovative may be essential to advance a field.
Does the proposed Center address the needs of the consortium that it will coordinate and administer? Is the scope of activities proposed for the Center appropriate to meet those needs? Will successful completion of the aims bring unique advantages or capabilities to the consortium?
Specific to this NOFO : Evaluate the appropriateness of the proposed plan to provide effective administrative support and project management to the entire Consortium, and thus contribute to a nation-wide effort to advance PKD research. Determine if the plans to develop a central portal for investigators to request and access the Consortium resources are appropriate.
Are the PD(s)/PI(s) and other personnel are well suited to their roles in the Center? Do the investigators demonstrate significant experience with coordinating collaborative basic or clinical research? If the Center is multi-PD/PI, do the investigators have complementary and integrated expertise and skills; are their leadership approach, governance, plans for conflict resolution, and organizational structure appropriate for the Center? Does the applicant have experience overseeing selection and management of subawards, if needed?
Specific to this NOFO: Evaluate the PD(s)/PI(s)'s experience in managing and coordinating a highly collaborative Consortium. Evaluate the PD(s)/PI(s)'s experience and approach to guiding working groups and gaining consensus among investigators from diverse scientific backgrounds.
Does the application propose novel organizational concepts or management strategies in coordinating the consortium the Center will serve? Are the concepts or strategies novel to one type of research program or applicable in a broad sense? Is a refinement, improvement, or new application of organizational concepts or management strategies proposed?
Specific to this NOFO : Evaluate the proposed strategies to lead collaborative Consortium-wide discussions that successfully identify emerging areas of science and anticipate the needs of the PKD research community to determine if they are innovative and appropriate to the Consortium. Determine the appropriateness of plans to identify and incorporate patient representatives and ensure that their viewpoints, priorities, and preferences are included in the decision-making processes of the Consortium?
Are the overall strategy, operational plan, and organizational structure well-reasoned and appropriate to accomplish the goals of the consortium the Center will serve? Will the investigators promote strategies to ensure a robust and unbiased scientific approach across the consortium, as appropriate for the work proposed? Are potential problems, alternative strategies, and benchmarks for success presented? If the consortium is in the early stages of operation, does the proposed strategy adequately establish feasibility and manage the risks associated with the activities of the consortium? Are an appropriate plan for work-flow and a well-established timeline proposed?
Specific to this NOFO : Evaluate the appropriateness and potential impact of the proposed plans to establish and implement a multifaceted communication strategy to maximize Consortium outreach and impact. Evaluate the plans to develop, support, manage, and continually enhance a well-organized, user-friendly, intuitive, interactive PKD RRC website for internal and external communication. Evaluate the plans to support, develop, manage, and enhance clinical and genomic databases within the PKD-RRC. Evaluate the proposed strategies to facilitate collaborative Consortium-wide discussions and build consensus to anticipate the needs of the PKD research community. Determine the appropriateness of the proposed plan for administering a Pilot and Feasibility program that includes organization of the process of solicitation, review, selection, and monitoring of these projects.
Will the institutional environment in which the Center will operate contribute to the probability of success in facilitating the consortium it serves? Are the institutional support, equipment and other physical resources available to the investigators adequate for the Center proposed? Will the Center benefit from unique features of the institutional environment, infrastructure, or personnel? Are resources available within the scientific environment to support electronic information handling?
Specific to this NOFO : Evaluate the institutional record of leading, coordinating, managing, and harmonizing highly collaborative endeavors to determine if it is appropriate to the needs of the Consortium. Evaluate the institutional record of fostering an inclusive research environment and giving a voice to people with PKD.
As applicable for the project proposed, reviewers will evaluate the following additional items while determining scientific and technical merit, and in providing an overall impact score, but will not give separate scores for these items.
For research that involves human subjects but does not involve one of the categories of research that are exempt under 45 CFR Part 46, the committee will evaluate the justification for involvement of human subjects and the proposed protections from research risk relating to their participation according to the following five review criteria: 1) risk to subjects, 2) adequacy of protection against risks, 3) potential benefits to the subjects and others, 4) importance of the knowledge to be gained, and 5) data and safety monitoring for clinical trials.
For research that involves human subjects and meets the criteria for one or more of the categories of research that are exempt under 45 CFR Part 46, the committee will evaluate: 1) the justification for the exemption, 2) human subjects involvement and characteristics, and 3) sources of materials. For additional information on review of the Human Subjects section, please refer to the Guidelines for the Review of Human Subjects .
When the proposed project involves human subjects and/or NIH-defined clinical research, the committee will evaluate the proposed plans for the inclusion (or exclusion) of individuals on the basis of sex/gender, race, and ethnicity, as well as the inclusion (or exclusion) of individuals of all ages (including children and older adults) to determine if it is justified in terms of the scientific goals and research strategy proposed. For additional information on review of the Inclusion section, please refer to the Guidelines for the Review of Inclusion in Clinical Research .
The committee will evaluate the involvement of live vertebrate animals as part of the scientific assessment according to the following three points: (1) a complete description of all proposed procedures including the species, strains, ages, sex, and total numbers of animals to be used; (2) justifications that the species is appropriate for the proposed research and why the research goals cannot be accomplished using an alternative non-animal model; and (3) interventions including analgesia, anesthesia, sedation, palliative care, and humane endpoints that will be used to limit any unavoidable discomfort, distress, pain and injury in the conduct of scientifically valuable research. Methods of euthanasia and justification for selected methods, if NOT consistent with the AVMA Guidelines for the Euthanasia of Animals, is also required but is found in a separate section of the application. For additional information on review of the Vertebrate Animals Section, please refer to the Worksheet for Review of the Vertebrate Animals Section.
Reviewers will assess whether materials or procedures proposed are potentially hazardous to research personnel and/or the environment, and if needed, determine whether adequate protection is proposed.
Not applicable.
For Renewals, the committee will consider the progress made in the last funding period.
As applicable for the project proposed, reviewers will consider each of the following items, but will not give scores for these items, and should not consider them in providing an overall impact score.
Reviewers will assess the information provided in this section of the application, including 1) the Select Agent(s) to be used in the proposed research, 2) the registration status of all entities where Select Agent(s) will be used, 3) the procedures that will be used to monitor possession use and transfer of Select Agent(s), and 4) plans for appropriate biosafety, biocontainment, and security of the Select Agent(s).
Reviewers will comment on whether the Resource Sharing Plan(s) (e.g., Sharing Model Organisms ) or the rationale for not sharing the resources, is reasonable.
For consortia involving key biological and/or chemical resources, reviewers will comment on the brief plans proposed for identifying and ensuring the validity of those resources.
Reviewers will consider whether the budget and the requested period of support are fully justified and reasonable in relation to the proposed research.
2. Review and Selection Process Applications will be evaluated for scientific and technical merit by (an) appropriate Scientific Review Group(s) convened by the NIDDK in accordance with NIH peer review policy and procedures , using the stated review criteria . Assignment to a Scientific Review Group will be shown in the eRA Commons. As part of the scientific peer review, all applications will receive a written critique. Applications may undergo a selection process in which only those applications deemed to have the highest scientific and technical merit (generally the top half of applications under review) will be discussed and assigned an overall impact score. Appeals of initial peer review will not be accepted for applications submitted in response to this NOFO. Applications will be assigned on the basis of established PHS referral guidelines to the appropriate NIH Institute or Center. Applications will compete for available funds with all other recommended applications submitted in response to this NOFO. Following initial peer review, recommended applications will receive a second level of review by the appropriate national Advisory Council or Board. The following will be considered in making funding decisions: Scientific and technical merit of the proposed project, including the PEDP, as determined by scientific peer review Availability of funds. Relevance of the proposed project to program priorities. Evidence that the applicant and investigators are committed to policies as established by the PKD Research Consortium Steering Committee including with regard to sharing of information and resources and cooperative interaction. Please note that reviewers will not consider race, ethnicity, age, or sex (including gender identity, sexual orientation or transgender status) of a researcher, award participant, or trainee, even in part, in providing critiques, scores, or funding recommendations. NIH will not consider such factors in making its funding decisions. If the application is under consideration for funding, NIH will request "just-in-time" information from the applicant as described in the NIH Grants Policy Statement Section 2.5.1. Just-in-Time Procedures . This request is not a Notice of Award nor should it be construed to be an indicator of possible funding. Prior to making an award, NIH reviews an applicant’s federal award history in SAM.gov to ensure sound business practices. An applicant can review and comment on any information in the Responsibility/Qualification records available in SAM.gov. NIH will consider any comments by the applicant in the Responsibility/Qualification records in SAM.gov to ascertain the applicant’s integrity, business ethics, and performance record of managing Federal awards per 2 CFR Part 200.206 “Federal awarding agency review of risk posed by applicants.” This provision will apply to all NIH grants and cooperative agreements except fellowships. 3. Anticipated Announcement and Award Dates
After the peer review of the application is completed, the PD/PI will be able to access his or her Summary Statement (written critique) via the eRA Commons . Refer to Part 1 for dates for peer review, advisory council review, and earliest start date.
Information regarding the disposition of applications is available in the NIH Grants Policy Statement Section 2.4.4 Disposition of Applications .
Section VI. Award Administration Information
1. award notices.
A Notice of Award (NoA) is the official authorizing document notifying the applicant that an award has been made and that funds may be requested from the designated HHS payment system or office. The NoA is signed by the Grants Management Officer and emailed to the recipient’s business official.
In accepting the award, the recipient agrees that any activities under the award are subject to all provisions currently in effect or implemented during the period of the award, other Department regulations and policies in effect at the time of the award, and applicable statutory provisions.
Recipients must comply with any funding restrictions described in Section IV.6. Funding Restrictions . Any pre-award costs incurred before receipt of the NoA are at the applicant's own risk. For more information on the Notice of Award, please refer to the NIH Grants Policy Statement Section 5. The Notice of Award and NIH Grants & Funding website, see Award Process.
Institutional Review Board or Independent Ethics Committee Approval: Recipient institutions must ensure that protocols are reviewed by their IRB or IEC. To help ensure the safety of participants enrolled in NIH-funded studies, the recipient must provide NIH copies of documents related to all major changes in the status of ongoing protocols.
2. Administrative and National Policy Requirements
The following Federal wide and HHS-specific policy requirements apply to awards funded through NIH:
- The rules listed at 2 CFR Part 200 , Uniform Administrative Requirements, Cost Principles, and Audit Requirements for Federal Awards.
- All NIH grant and cooperative agreement awards include the NIH Grants Policy Statement as part of the terms and conditions in the Notice of Award (NoA). The NoA includes the requirements of this NOFO. For these terms of award, see the NIH Grants Policy Statement Part II: Terms and Conditions of NIH Grant Awards, Subpart A: General and Part II: Terms and Conditions of NIH Grant Awards, Subpart B: Terms and Conditions for Specific Types of Grants, Recipients, and Activities .
- HHS recognizes that NIH research projects are often limited in scope for many reasons that are nondiscriminatory, such as the principal investigator’s scientific interest, funding limitations, recruitment requirements, and other considerations. Thus, criteria in research protocols that target or exclude certain populations are warranted where nondiscriminatory justifications establish that such criteria are appropriate with respect to the health or safety of the subjects, the scientific study design, or the purpose of the research. For additional guidance regarding how the provisions apply to NIH grant programs, please contact the Scientific/Research Contact that is identified in Section VII under Agency Contacts of this NOFO.
All federal statutes and regulations relevant to federal financial assistance, including those highlighted in NIH Grants Policy Statement Section 4 Public Policy Requirements, Objectives and Other Appropriation Mandates.
Recipients are responsible for ensuring that their activities comply with all applicable federal regulations. NIH may terminate awards under certain circumstances. See 2 CFR Part 200.340 Termination and NIH Grants Policy Statement Section 8.5.2 Remedies for Noncompliance or Enforcement Actions: Suspension, Termination, and Withholding of Support .
NATIONAL INSTITUTE OF DIABETES AND DIGESTIVE AND KIDNEY DISEASES TERMS AND CONDITIONS OF COOPERATIVE AGREEMENT AWARDS RESEARCH PROJECT APPLICATIONS FOR NON-CLINICAL STUDIES.
The following special terms of award are in addition to, and not in lieu of, otherwise applicable U.S. Office of Management and Budget (OMB) administrative guidelines, U.S. Department of Health and Human Services (HHS) grant administration regulations at 2 CFR Part 200, and other HHS, PHS, and NIH grant administration policies.
The administrative and funding instrument used for this program will be the cooperative agreement, an "assistance" mechanism (rather than an "acquisition" mechanism), in which substantial NIH programmatic involvement with the recipients is anticipated during the performance of the activities. Under the cooperative agreement, the NIH purpose is to support and stimulate the recipients' activities by involvement in and otherwise working jointly with the recipients in a partnership role; it is not to assume direction, prime responsibility, or a dominant role in the activities. Consistent with this concept, the dominant role and prime responsibility resides with the recipients for the project as a whole, although specific tasks and activities may be shared among the recipients and NIH as defined below.
The PD(s)/PI(s) will have the primary responsibility for:
- Recipient(s) will be primarily responsible for defining the objectives and approaches, planning, conduct, analysis, and publication of results, interpretations, and conclusions of studies conducted under the terms and conditions of the cooperative agreement award.
- The Program Director/Principal Investigator (PD/PI) will assume responsibility and accountability to the applicant organization officials and to the NIH for the performance and proper conduct of the research supported under this Funding Opportunity Announcement (NOFO) in accordance with the terms and conditions of award, as well as all pertinent laws, regulations and policies.
- Recipient(s) will retain custody of and have primary rights to the data and software developed under these awards, subject to Government policies regarding rights of access consistent with current DHHS, PHS, and NIH policies.
- PD/PI’s will be responsible for providing, at least annually, reports on progress regarding the Plan for Enhancing Diverse Perspectives (PEDP).
- Recipients are responsible for their staff in maintaining confidentiality of the information as developed by the network/consortium, including, without limitation, study protocols, data analysis, conclusions, etc. per policies approved by the Steering Committee (SC) as well as any confidential information received by third party collaborators.
- Recipients must analyze, publish and/or publicly release and disseminate results, data and other products of the study in a timely manner, concordant with the approved plan for making quality-assured data and materials available to the scientific community and the NIH, consistent with NIH policies and achieving the goals of the NOFO.
- Data Management and Sharing Plan: In accordance with the NIH Policy for Data Management and Sharing (NIH NOT-OD-21-013), the NIDDK approved plan will become a term and condition of award, be routinely monitored during the award period, and compliance may factor into future funding decisions. By the end of the funding or proprietary period, a recipient or study group may not continue to exclusively use or share study generated resources until those resources are available to the public via a NIDDK approved repository per the NIDDK approved plan.
- Recipient(s) will be required to participate in a cooperative and interactive manner with members of the network/consortium including designated NIH staff (e.g., Program Official, Project Scientist, Project Coordinator).
- Recipient(s) agree to establish agreements amongst themselves that address the following issues: (1) procedures for data sharing among network/consortium members and data sharing with industry partners; (2) procedures for safeguarding confidential information, including without limitation, any data generated by the network/consortium as well as information and/or data received from external collaborators; (3) procedures for addressing ownership of intellectual property that result from aggregate multi-party data; (4) procedures for sharing bio-specimens under an overarching Material Transfer Agreement (MTA) amongst network/consortium members that operationalizes material transfer in an efficient and expeditious manner; (5) procedures for reviewing publications, determining authorship, and industry access to publications.
- Any third-party collaboration (including but not limited to interactions with organizations from industry, academia, and nonprofit institutions) should be governed by a research collaboration agreement (e.g., Clinical Trial Agreement, Research Collaborative Agreement, etc.) or any third-party contract mechanism(s) with terms that ensure the collaboration is conducted in accordance with the Cooperative Agreement, applicable NIH/NIDDK policies and procedures, applicable network/consortium policies, and with written approval from NIDDK Program staff. Any relevant proposed third-party agreements related to the network/consortium studies between grantee and third-party will be provided to the NIDDK Program staff and NIDDK Technology Advancement Office for review, comment, and approval to assure compliance with NIH/NIDDK policies and network/consortium policies. Further, at the request of the NIDDK Program staff, any other network/consortium-relevant third-party agreements must be shared with NIDDK. Failure to comply with this term may prompt action in accordance with NIH Grants Policy Statement, Section 8.5 titled: “Special Award Conditions and Remedies for Noncompliance (Special Award Conditions and Enforcement Actions)”, and Section 8.5.2, titled: “Remedies for Noncompliance or Enforcement Actions: Suspension, Termination, and Withholding Support”, noncompliance with the terms and conditions of award will be considered by the funding IC for future funding and support decisions and may result in termination of the award.
- Any involvement of a third-party (including but not limited to industry, academia, and nonprofit institutions) in the study and network/consortium activities that includes access to any network/consortium generated resources (i.e., data and biosamples), or study results that are not publicly available, or using the name of the network/consortium or study or the name of the NIH or NIDDK, is permitted only after written permission by the NIDDK Program staff who will consult with others at NIH and NIDDK Technology Advancement Office.
- Recipients must agree to comply with the processes and goals as delineated within the NOFO.
- Recipient(s) agree to the governance of the study through a Steering Committee:
- The PD/PI, or contact PD/PI in the case of multi-PD/PI awards, will serve as a voting member of the Steering Committee and will attend all meetings of the Steering Committee.
- Each full member will have one vote.
- The Recipient will be responsible for accepting and implementing the goals, priorities, procedures, protocols, and policies agreed upon by the Steering Committee and subcommittees.
- Recipients must serve on Subcommittees as needed. Subcommittees will report progress at Steering Committee Meetings and/or lead discussions at the Annual PKD RRC meeting.
- Recipients must share data, materials, models, methods, information and unique research resources that are generated by the projects in concordance with Network/Consortium policies in order to facilitate progress. When appropriate, and in accordance with NIH policies, as well as NIDDK policies, Recipients will be expected to collaborate; share novel reagents, biomaterials, methods and models and resources; and share both positive and negative results that would help guide the research activities of other members.
- Provide updates at least annually on progress in PEDP implementation.
- Upon completion or termination of the research project(s), the Recipients are responsible for making all study materials and procedures broadly available (e.g., putting them into the public domain) or making them accessible to the research community according to the NIH-approved plan submitted for each project, for making all study materials and procedures available to the scientific community and the NIH for the conduct of research. The Data Management and Sharing Plan should include a plan to accomplish aforementioned at the end of the study.
NIH staff have substantial programmatic involvement that is above and beyond the normal stewardship role in awards, as described below:
The IC Project Scientist/Coordinator/Collaborator’s scientific-programmatic involvement (i.e., the NIH partner) will participate in discussions and decision-making regarding the development and sharing of resources, the planning of annual meetings, and the awarding of Pilot and Feasibility grants during the conduct of the activity. Staff involvement must reflect that the dominant role and prime responsibility for the activity reside with the Recipient(s) for the project as a whole, but not necessarily for each task. The NIDDK will designate program staff, including a Program Official and a Grants Management Specialist to provide normal program stewardship and administrative oversight of the cooperative agreement. The Program Official and Grants Management Specialist will be named in the Notice of Grant Award (NOA).
An NIH IC Project Scientist will be substantially involved in this project above and beyond the normal stewardship of an NIH IC Program Official as follows:
1. Serve as the contact point for all facets of the scientific interaction with the recipient(s). As required for the coordination of activities and to expedite progress, NIDDK may designate additional NIDDK staff to provide advice to the recipient on specific scientific and/or analytic issues.
2. For multi-center studies, participate in the Steering Committee that oversees study conduct. The NIDDK Project Scientist will be a full participant and voting member of the Steering Committee and, if applicable, subcommittees.
3. Serve as a resource to study investigators with respect to other ongoing NIDDK activities that may be relevant to the study to facilitate compatibility with the NIDDK missions and avoid unnecessary duplication of effort.
4. Have substantial involvement assisting in the design and coordination of research activities for Recipients as elaborated below:
a. Assisting by providing advice in the management and technical performance of the investigations, coordinating required regulatory clearances for investigational agents used in the study, which are held by NIDDK. The NIDDK may reserve the right to cross file or independently file an Investigational New Drug Application or an Investigational Device Exemption form with the FDA.
b. The NIDDK Project Scientist or Project Coordinator may coordinate activities among recipients by assisting in the design, development, and coordination of a common research or clinical protocol and statistical evaluations of data; in the preparation of questionnaires and other data recording forms; and in the publication of results.
c. Reviewing procedures for assessing data quality and study performance monitoring.
d. The NIDDK Project Scientist or Project Coordinator may be co-authors on study publications. In general, to warrant co-authorship, NIDDK staff must have contributed to the following areas: (a) design of the concepts or experiments being tested; (b) performance of significant portions of the activity; (c) participation in analysis and interpretation of study results and (d) preparation and authorship of pertinent manuscripts.
The NIDDK Program Official identified in the Notice of Award will :
1. Interact with the Program Director(s)/Principal Investigator(s) on a regular basis to monitor study progress. Monitoring may include regular communications with the Program Director/Principal Investigator and staff, periodic site visits, observation of field data collection and management techniques, quality control, fiscal review, and other relevant matters; as well as attendance at Steering Committee, data safety and monitoring board, and related meetings. The NIDDK retains, as an option, periodic review of progress by researchers not involved with the study.
2. Review and approve protocols prior to implementation to ensure they are within the scope of peer review, for safety considerations, as required by federal regulations.
3. The NIDDK Program Official will monitor protocol progress, and may request that a protocol study be closed to accrual for reasons including: (a) accrual rate insufficient to complete study in a timely fashion; (b) accrual goals met early; (c) poor protocol performance; (d) participant safety and regulatory concerns; (e) study results that are already conclusive; (f) low likelihood of showing a benefit of the intervention (futility); and (g) emergence of new information that diminishes the scientific importance of the study question. The NIDDK will not permit further expenditures of NIDDK funds for a study after requesting closure except as specifically approved by the NIDDK.
4. Make recommendations for continued funding based on: a) overall study progress, including sufficient patient and/or data accrual; b) cooperation in carrying out the research (e.g., attendance at Steering Committee meetings, implementation of group decisions, compliance with the terms of award and reporting requirements); and/or c) maintenance of a high quality of research, which will allow pooling of data and comparisons across multiple cooperative agreement awards for common data elements.
5. Appoint an independent Data and Safety Monitoring Board (DSMB) as appropriate for Phase III clinical trials or other high-risk studies, or an Observational Study Monitoring Board (OSMB) for observational/epidemiologic studies; these Boards will review study progress, safety data, and interim results, as appropriate, and provide guidance to the NIDDK. The NIDDK Program Official or their Project Coordinator will serve as the Executive Secretary and/or NIDDK program representative on the DSMB/OSMB.
Areas of Joint Responsibility include:
PD/PI(s) and NIH staff will jointly participate in the discussions and the operations of committees, such as a Steering Committee and other central coordinating components in which there is substantial scientific-programmatic involvement.
Through the Recipient, Steering Committee and NIH staff, the study members will cooperatively develop and implement processes to submit information and data to the Central Coordinating Site, determine criteria and processes for quality control of information and data to be posted for the research community, refine scientific objectives, and implement research advances to facilitate the goals of the study, consistent with NIH policies and achieving the goals of the program as described in the NOFO.
The following bullets are examples of responsibilities that Program Staff may wish to include (bullets can be deleted or modified if they do not apply):
- Steering Committee
A Steering Committee organized by the study investigator(s) will be the main governing body of the study. The Steering Committee has primary responsibility to design research activities, establish priorities, develop common protocols and manuals, questionnaires and other data recording forms, establish and maintain quality control among recipients, review progress, monitor patient accrual, coordinate and standardize data management, and cooperate on the publication of results. Major scientific decisions regarding the core data will be determined by the Steering Committee. The Steering Committee will document progress in written reports to the NIDDK Program Official and will provide periodic supplementary reports upon request
The Steering Committee will be composed of all Program Director(s)/Principal Investigator(s), (including those of data coordinating/statistical centers, if any) and co-investigator(s) as deemed necessary, and the NIDDK Project Scientist. The final structure of the Steering Committee and voting procedures will be established at the first meeting. The NIDDK Project Scientist will have voting membership on the Steering Committee, and as appropriate, its subcommittees. The frequency of Steering Committee meetings will be dictated by a vote of the members of the Steering Committee. The NIDDK Program Official may serve as a non-voting member on the Steering Committee. A Chairperson of the Steering Committee will be selected and voted on by the Steering Committee members. The Chairperson provides leadership to the Committee by conducting the Steering Committee meetings and by interacting closely with the recipients during protocol development and implementation. The NIDDK Project Scientist may not serve as Chairperson. The NIDDK program official will review the Committee’s selection for potential bias, conflicts of interest, or lack of required expertise. If the Program Official has concerns regarding selection of the Chairperson which are not satisfactorily resolved, the Program Official may withhold concurrence if approved by the Director, Division of Extramural Activities, NIDDK based on written justification. In cases where Program Official concurrence is withheld, the Steering Committee will be required to make another selection.
- External Consultants
An independent panel of External Consultants may be established by the Steering Committee. The External Consultants may periodically review interim progress of the project(s) and provide reports to the Steering Committee. Members of the panel of External Consultants may be asked, on an ad hoc basis, to participate in the peer review of applications for new research initiatives that utilize special “opportunity pool” funds. The NIDDK Program Official will review the Committee’s selections for potential bias, conflicts of interest, or lack of required expertise. If the NIDDK Program Official has concerns regarding selection of one or more External Consultants which are not satisfactorily resolved, the NIDDK Program Official may withhold concurrence if approved by the Director of NIDDK Division of Extramural Activities based on written justification. In cases where NIDDK Program Official concurrence is withheld, the Steering Committee will be required to make another selection.
Dispute Resolution:
Any disagreements that may arise in scientific or programmatic matters (within the scope of the award) between recipients and NIH may be brought to Dispute Resolution. A Dispute Resolution Panel composed of three members will be convened: a designee of the Steering Committee chosen without NIH staff voting, one NIH designee, and a third designee with expertise in the relevant area who is chosen by the other two; in the case of individual disagreement, the first member may be chosen by the individual recipient. This special dispute resolution procedure does not alter the recipient's right to appeal an adverse action that is otherwise appealable in accordance with PHS regulation 42 CFR Part 50, Subpart D and HHS regulation 45 CFR Part 16.
3. Data Management and Sharing
Consistent with the 2023 NIH Policy for Data Management and Sharing, when data management and sharing is applicable to the award, recipients will be required to adhere to the Data Management and Sharing requirements as outlined in the NIH Grants Policy Statement . Upon the approval of a Data Management and Sharing Plan, it is required for recipients to implement the plan as described.
4. Reporting
When multiple years are involved, recipients will be required to submit the Research Performance Progress Report (RPPR) annually and financial statements as required in the NIH Grants Policy Statement Section 8.4.1 Reporting. To learn more about post-award monitoring and reporting, see the NIH Grants & Funding website, see Post-Award Monitoring and Reporting .
- Recipients will provide updates at least annually on implementation of the PEDP.
A final RPPR, invention statement, and the expenditure data portion of the Federal Financial Report are required for closeout of an award, as described in the NIH Grants Policy Statement Section 8.6 Closeout . NIH NOFOs outline intended research goals and objectives. Post award, NIH will review and measure performance based on the details and outcomes that are shared within the RPPR, as described at 2 CFR Part 200.301.
Section VII. Agency Contacts
We encourage inquiries concerning this funding opportunity and welcome the opportunity to answer questions from potential applicants.
eRA Service Desk (Questions regarding ASSIST, eRA Commons, application errors and warnings, documenting system problems that threaten submission by the due date, and post-submission issues)
Finding Help Online: https://www.era.nih.gov/need-help (preferred method of contact) Telephone: 301-402-7469 or 866-504-9552 (Toll Free)
General Grants Information (Questions regarding application instructions, application processes, and NIH grant resources) Email: [email protected] (preferred method of contact) Telephone: 301-480-7075
Grants.gov Customer Support (Questions regarding Grants.gov registration and Workspace) Contact Center Telephone: 800-518-4726 Email: [email protected]
Christine Maric-Bilkan, Ph.D. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Telephone: 301-435-0486 Email: [email protected]
Susan R. Mendley, M.D. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Telephone: 301-827-1861 Email: [email protected]
Xiaodu Guo, M.D., Ph.D. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Telephone: 301-594-4719 Email: [email protected]
Krystle Nicholson National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Telephone: 301-594-8860 Email: [email protected]
Section VIII. Other Information
Recently issued trans-NIH policy notices may affect your application submission. A full list of policy notices published by NIH is provided in the NIH Guide for Grants and Contracts . All awards are subject to the terms and conditions, cost principles, and other considerations described in the NIH Grants Policy Statement .
Awards are made under the authorization of Sections 301 and 405 of the Public Health Service Act as amended (42 USC 241 and 284) and under Federal Regulations 42 CFR Part 52 and 2 CFR Part 200.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Outcome of polycystic kidney disease patients on peritoneal dialysis: Systematic review of literature and meta-analysis
Vincent dupont.
1 Division of Nephrology, University Hospital of Reims, Reims, France
Lukshe Kanagaratnam
2 Department of Research and Innovation, University Hospital of Reims, Reims, France
Mickaël Sigogne
Clémence bechade.
3 Division of Nephrology, University hospital of Caen, Caen, France
Thierry Lobbedez
Jose portoles.
4 Division of Nephrology, University Hospital of Puerta de Hierro, Madrid, Spain
Philippe Rieu
5 Laboratory of Nephrology, UMR CNRS URCA 7369 (Matrice Extracellulaire et Dynamique Cellulaire, MEDyC), Reims, France
Moustapha Drame
Fatouma touré, associated data.
All relevant data are within the paper.
Polycystic kidney disease (PKD) is the most frequent hereditary cause of chronic kidney disease. Peritoneal dialysis (PD) is often avoided for patients with PKD because of the suspected risk of mechanical and infectious complications. Only a few studies have analyzed the outcome of PKD patients on PD with sometimes conflicting results. The purpose of this meta-analysis was to investigate outcomes of patients with PKD treated by PD.
A systematic review and meta-analysis were performed examining all studies which included “Polycystic kidney disease” and “Peritoneal dialysis” in their titles, excluding commentaries, letters to the authors and abstracts. PubMed, Embase, Google scholar and Scopus were searched to December 31 st 2017. The primary outcome was overall patient survival. Additional outcomes were PD technique survival, incidence of peritonitis and incidence of abdominal wall hernia.
9 studies published between 1998 and 2016 were included for analysis with a total of 7,197 patients including 882 PKD patients. Overall survival of PKD patients was found to be better compared to non-PKD patients (HR = 0.70 [95% CI, 0.54–0.92]). There were no statistical differences between PKD and non-PKD patients in terms of peritonitis (OR = 0.86 [95% CI, 0.66–1.12]) and technical survival (HR = 0.98 [95% CI, 0.83–1.16]). There was an increased risk of hernia in PKD patients (OR = 2.28 [95% CI, 1.26–4.12]).
Conclusions
PKD is associated with a better global survival, an increased risk of abdominal hernia, but no differences in peritonitis rate or technical survival were found. PD is a safe dialysis modality for PKD patients. Properly designed controlled studies are needed to determine whether all PKD patients are eligible for PD or whether some specific criteria should be determined.
Introduction
Polycystic kidney disease (PKD) is the most frequent hereditary cause of chronic kidney disease. [ 1 , 2 ]. Peritoneal dialysis (PD) is often avoided for PKD patients when it comes to the choice of renal replacement therapy. Indeed, enlarged kidneys and liver may reduce the peritoneal extensibility, leading to increased intraperitoneal pressure [ 3 , 4 ]. Higher prevalence of abdominal wall hernia, leaks, and diverticulitis-related peritonitis have been reported with PD administration in PKD patients [ 5 ]. These complications may directly impact on PD technique survival and on patients’ outcomes. However, only a small number of studies have been designed to analyze the incidence of these events and their relation with PD technical survival or global patient survival. The purpose of this review and meta-analysis was to investigate the outcome of patients with PKD treated by PD.
Study design
This systematic review with meta-analysis was conducted according to a prespecified protocol and was reported using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [ 6 ].
Search strategy and selection criteria
A bibliographic search was performed from the inception to December 31 st 2017 in the following databases: Pubmed, Embase, Google scholar and Scopus. We also screened references of included articles to identify other potential studies. The search strategy, on the article title, was as follows: "polycystic kidney"[title] OR "polycystic kidney disease"[title] OR ADPKD[title] or "autosomic dominant polycystic kidney disease"[title]) AND "peritoneal dialysis"[title]. One author (VD) performed the full search strategy and removed duplicates.
Study selection and data extraction
After eliminating duplicates, two authors (VD, MS) independently reviewed the titles and abstracts of all articles. Disagreements were resolved by consensus. Agreement between the two authors was assessed using the Kappa coefficient. After agreement, the full text of all articles designated for inclusion was obtained. Two authors (VD, MS) checked to ensure that all articles met the criteria for inclusion in this analysis, and then independently extracted the data into a standardized form. Extracted data were: study design, country, number of subject included, percentage of male, age, comorbidity (Charlson index, diabetes mellitus and hypertension), percentage of patients treated by automated peritoneal dialysis, transfer to hemodialysis, access to kidney transplantation, dialysis adequacy, hemoglobinemia, albuminemia, overall survival, PD technique survival defined as permanent cessation of PD therapy due to PD related complications, and occurrence of peritonitis or abdominal hernia. Study authors were contacted to obtain missing data. Studies were included if they presented at least two of the following parameters: overall survival, PD technique survival, incidence of peritonitis, and incidence of abdominal hernia. Studies were excluded if they presented any one or more of the following criteria: case report, case series, abstracts, commenters or letter to the editor, language other than French or English.
Risk-of-Bias assessment
The quality of included studies was assessed independently by two researchers (VD, MS) using the Newcastle-Ottawa scale (NOS) for cohort studies [ 7 ]. The NOS consists of three quality parameters, namely selection, comparability, and outcome assessment. The NOS assigns a maximum of four points for selection, two points for comparability and three points for outcome. NOS scores of ≥7 were considered as high quality studies and 5–6 as moderate quality [ 8 ]. Disagreement was resolved by joint review of the manuscript to reach consensus. Publication bias was assessed using funnel plots and the Egger’s regression test if there were up to 10 eligible studies included in the meta-analysis [ 9 , 10 ].
Statistical analysis
The primary outcome was overall survival. Secondary outcomes were: 1/ PD technique survival defined as permanent cessation of PD therapy due to PD related complications, (considering any other outcome as censored data), 2/ percentage of peritonitis and 3/ frequency of abdominal hernias. Extracted data were presented as number and percentage for qualitative variables, and as mean and standard deviation (or median and range) for quantitative variables. Heterogeneity between studies was assessed using the Cochran Q statistic and I 2 test. A random effects model was used independently of the existence or absence of heterogeneity between the results of the studies because results of studies with different design and patients’ characteristics were pooled. For time to event outcomes, when hazard ratios (HR) were not specified, they were estimated according to the information presented in the paper [ 11 ]. PKD and non PKD patients were compared through random effects models weighted by the inverse-variance method to estimate pooled HR and odds ratios (OR) with 95% confidence intervals (CIs). Sensitivity analyses were performed. All analyses were performed using R version 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria).
Study characteristics
Using the search strategy ( Fig 1 ), we identified 9 eligible studies [ 12 – 20 ] presenting at least two outcome of interest. The agreement in selection of studies between the reviewers was excellent (κ = 1). All the studies included in the meta-analysis were considered as high quality studies (details showed in Table 1 ). Publication bias, using funnel plot and the Egger’s regression test, was not assessed as the number of studies included in this meta-analysis was less than 10 studies [ 9 , 10 ].

| Study, Year | Selection | Comparability | Outcome | NOS |
|---|---|---|---|---|
| **** | ** | *** | 9 | |
| **** | ** | *** | 9 | |
| **** | *** | 7 | ||
| **** | ** | *** | 9 | |
| **** | *** | 7 | ||
| **** | *** | 7 | ||
| **** | *** | 7 | ||
| **** | *** | 7 | ||
| **** | *** | 7 |
NOS, Newcastle-Ottawa Scale score ; the number of stars (*) corresponds to the number of complete items (maximum 4 items of Selection , 2 items for Comparability and 3 items for Outcome)
General characteristics of the studies included in the meta-analysis are presented in Table 2 . A total of 7,197 patients were included for analysis, including 882 PKD patients. Seven of the 9 studies were retrospective. In two of the 9 studies [ 14 , 20 ], PKD patients were significantly younger than non PKD.
| Study, Year | Country | Study Design | n | n | Mean Age | Male (%) | Follow up (M) | Adjusted variables | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PKD+ | PKD- | PKD+ | PKD- | PKD+ | PKD- | |||||||
| Poland | Prospective cohort | 1712 | 106 | 1606 | 62 (55–72) | 60 (47–71) | 0.04 | 42.5 | 53.3 | 32 | Age, sex, diabetes, hypertension | |
| Spain | Prospective matched cohort | 318 | 106 | 212 | 54.28 (±11.92) | 53.43 (±16.43) | 0.6 | 60 | 61.4 | 21 | Age, CIS | |
| Taiwan | Retrospective propensity-score matched cohort | 556 | 139 | 417 | 53.4 (±14.7) | 53.8 (±14.7) | 0.78 | 51.8 | 54.9 | 32 | - | |
| France | Retrospective cohort | 4162 | 344 | 3818 | 56.2 (47.1–67.9) | 71.1 (52.4–80.7) | - | 48 | 59 | 17 | Age, sex, CIS, center, type of assistance | |
| China | Retrospective matched cohort | 126 | 42 | 84 | 57.3 (±12.0) | 56.0 (±11.9) | 0.6 | 64.2 | 46.4 | 42 | ||
| England | Retrospective matched cohort | 112 | 56 | 56 | 50.8 (±11.6) | 50.3 (±11.5) | NS | 45 | 45 | 37 | ||
| China | Retrospective matched cohort | 60 | 30 | 30 | 52.5 (±11.0) | 52.6 (±11.1) | 0.962 | 60 | 60 | 27 | ||
| Sweden | Retrospective cohort | 52 | 26 | 26 | 57 (±11) | 53 (±14) | 0.002 | 65 | 73 | 18 | ||
| Turkey | Retrospective cohort | 99 | 33 | 66 | 35.4 (±13.1) | 46 (±16.8) | - | 39.4 | 53 | 150 | ||
n, number of subjects ; PKD+, Patients with polycystic kidney disease ; PKD-, Patients without polycystic kidney disease ; M, Months (median) ; CIS, Charlson Index Score
*, p<0.05
Clinical characteristics of patients included are summarized in Table 3 . Patients did not differ between the PKD and non PKD groups in terms of hypertension, access to kidney transplantation and transfer to hemodialysis. In one of the 9 studies [ 14 ], Charlson index was found to be higher in non PKD patients. Most of the patients were treated by continuous ambulatory peritoneal dialysis while only Yang et al. reported a higher prevalence of automated peritoneal dialysis in the PKD group [ 12 ].
| Outcome | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study, Year | Hypertension (%) | CIS | APD (%) | Kidney transplantation (%) | Transfer to hemodialysis (%) | ||||||||||
| PKD+ | PKD- | PKD+ | PKD- | PKD+ | PKD- | PKD+ | PKD- | PKD+ | PKD- | ||||||
| 83 | 83.9 | 0.9 | - | - | - | 45.3 | 44.4 | 0.9 | 26.4 | 18.6 | 0.04 | 18.9 | 21.4 | 0.5 | |
| 14.7 | 23 | 0.21 | 4.27 (±1.58) | 5.27 (±2.5) | <0.001 | 43.4 | 33.7 | 0.1 | 47.2 | 30.7 | 0.004 | 17 | 20.3 | NS | |
| 71.2 | 73.1 | 0.66 | 2.9 (±1.4) | 3.0 (±1.4) | 0.5 | 46.8 | 37.6 | 0.03 | 9.4 | 9.8 | 0.87 | 24.5 | 22.5 | 0.64 | |
| - | - | - | 3 (3–5) | 6 (3–7) | - | 54.9 | 34.5 | - | 52 | 30 | - | 32 | 30 | - | |
| 95.2 | 91.7 | 0.5 | 4.6 (±1.6) | 4.1 (±1.8) | 0.1 | - | - | - | 9.5 | 11.9 | - | 9.5 | 11.9 | - | |
| - | - | - | - | - | - | 18.5 | 17.8 | - | 39 | 37 | NS | 30 | 25 | NS | |
| 100 | 93.3 | 0.152 | 3.3 (±1.1) | 3.1 (±1.0) | 0.351 | - | - | - | 16.7 | 16.7 | 1 | 16.7 | 20 | 0.506 | |
| - | - | - | - | - | 0 | 0 | - | 60 | 41.2 | - | 25 | 29.4 | - | ||
| - | - | - | - | - | - | 42.4 | 47 | 0.36 | 30.3 | 16.6 | - | 30.3 | 28.8 | - | |
PKD+, Patients with Polycystic Kidney Disease; PKD-, Patients without Polycystic Kidney Disease; CIS, Charlson Index Score; APD, Automated Peritoneal Dialysis
Biological characteristics of patients included are shown in Table 4 . There was no difference in serum albumin level and dialysis adequacy in term of total weekly Kt/V urea between PKD and non PKD patients. In two studies [ 14 , 17 ], hemoglobin level was higher in PKD patients.
| Study, Year | Hemoglobinemia [g/dL] | Albuminemia [g/L] | Kt/V | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PKD+ | PKD- | PKD+ | PKD- | PKD+ | PKD- | ||||
| 11.4 (±1.5) | 11.2 (±1.7) | 0.2 | 37.3 (±6.0) | 36.0 (±7.3) | 0.1 | 2.22 (±0.59) | 2.33 (±0.71) | 0.2 | |
| 12.63 (±1.44) | 11.96 (±1.49) | 0.001 | - | - | - | 2.68 (±0.65) | 2.52 (±0.80) | 0.1 | |
| - | - | - | - | - | - | - | - | - | |
| - | - | - | - | - | - | - | - | - | |
| 10.4 (±1.7) | 9.0 (±1.3) | <0.001 | 32.0 (±5.9) | 33.0 (±5.0) | 0.4 | 1.93 (±0.39) | 1.99 (±0.37) | 0.4 | |
| 11.0 (±1.5) | 10.6 (±1.9) | NS | 39.8 (±3.9) | 38.1 (±4.9) | NS | 2.3 (±0.50) | 2.1 (±0.4) | NS | |
| 8.1 (±1.6) | 8.0 (±1.5) | 0.957 | 41.0 (±5.2) | 39.0 (±6.4) | 0.182 | 2.11 (±0.53) | 2.08 (±0.56) | 0.328 | |
| - | - | - | - | - | - | - | - | - | |
| 10.7 (±2.0) | 10.3 (±2.0) | 0.38 | 38.6 (±5.1) | 35.6 (±6.6) | 0.03 | 2.15 (±0.40) | 2.03 (±0.60) | 0.47 | |
PKD+, Patients with Polycystic Kidney Disease ; PKD-, Patients without Polycystic Kidney Disease; Kt/V, Total weekly Kt/V urea
Overall survival
There were 5 studies that reported hazard ratios for PKD and non PKD patient survival. 6,378 patients from Europe and China were included in the meta-analysis. PKD status was associated with a better global survival with a Hazard Ratio of 0.70 [95% CI, 0.54–0.92] ( Fig 2 ).

HR, Hazard ratio ; CI, Confidence interval .
PD technique survival
Seven studies reported hazard ratios for PD technique survival in both groups, which included a total of 7,046 patients from Europe, China and Taiwan. There was no difference between PKD and non PKD groups in terms of PD technique survival (HR = 0.98 [95% CI, 0.83–1.16]) as shown in Fig 3 .

Infectious complications
Seven studies reported odds ratios for the incidence of infectious peritonitis episodes in PKD and non PKD patients treated by PD. 6,767 patients from Europe, China, Taiwan and Turkey were included in the meta-analysis ( Fig 4 ). There was no statistical difference in occurrence of infectious peritonitis between PKD and non PKD patients (OR = 0.86 [95% CI, 0.66–1.12]) as shown in Fig 4 .

OR, Odds ratio ; CI, Confidence interval .
Abdominal wall hernias
There were 7 studies that reported odds ratios for the incidence of abdominal wall hernias in PKD and non PKD patients treated by PD, including a total of 2,923 patients from Europe, China, Taiwan and Turkey ( Fig 5 ). PKD patients were found to have an increased risk of abdominal hernia with an Odds Ratio of 2.28 [95% CI, 1.26–4.12] as shown in Fig 5 .

Sensitivity analysis
Because the large weight of the study by Lobbedez et al. among the included studies might affect the entire analysis, we performed sensitivity analysis to check the stability of the previous results without including the study by Lobbedez et al. (except for abdominal wall hernias because this study was not included in analysis for this outcome). Results are summarized on Table 5 . Hazard ratios and Odds ratios showed a great stability even in the absence of the study by Lobbedez et al. The only observed change in the absence of the study by Lobbedez et al. was the absence of statistical relevance in the analysis of overall survival.
| Hazard ratio or Odds Ratio | Confidence interval | Hazard ratio or Odds Ratio w/o Lobbedez et al. | Confidence interval w/o Lobbedez et al. | |
|---|---|---|---|---|
| HR = 0.70 | 0.54–0.92 | HR = 0.74 | 0.5–1.09 | |
| HR = 0.98 | 0.83–1.16 | HR = 1.00 | 0.79–1.27 | |
| OR = 0.86 | 0.66–1.12 | OR = 0.87 | 0.59–1.28 |
w/o, without ; HR, Hazard ratio ; OR, Odds ratio
To our knowledge this is the first meta-analysis designed to study the outcome of PKD patients on PD. We found that compared to non PKD patients, PKD patients on PD had i) better global survival, ii) no difference in PD technique survival, iii) no difference in peritonitis rate but increased risk of abdominal hernias. Our results should reassure nephrologists managing PKD patients regarding the choice of PD as renal replacement therapy.
We found that PKD patients had better survival compared with non PKD patients. This difference could be explained by lower comorbidities reported in PKD patients: younger age [ 14 , 20 ], lower Charlson index [ 14 ] and higher hemoglobinemia [ 14 , 17 ]. On the other hand, patients with this hereditary disease are usually diagnosed earlier and monitored with a better nephrology care and a planned access to PD in optimized conditions. Only one study reports this factor but it could certainly explain at least in part the good clinical outcome for PD group in other studies [ 14 ].In addition, PKD patients have less comorbidities and may therefore have better outcome and a relatively lower risk of death or transfer to hemodialysis because of a higher competing risk of being transplanted ( Table 3 ). Lastly, in one study, diabetes mellitus was found to be the only predictor of all-cause mortality independently from PKD status [ 13 ].
Furthermore, the meta-analysis strategy allowed us to include 7,046 patients for the analysis of PD technique survival. PD technique survival did not differ according to PKD status. Moreover, there were no statistical difference between PKD and non PKD patients in terms of access to kidney transplantation or transfer to hemodialysis. Koc et al. reported that causes of death and transfer to hemodialysis were not different between PKD and non PKD patients (p = 0.35 and 0.36, respectively) [ 16 ]. In the study of Kumar et al, in multivariate analysis [ 18 ], hypoalbuminemia at initiation of PD was found to be the main risk factor for PD therapy cessation independently from PKD status.
Previous reports have suggested an increased incidence of mechanical complications in PKD patients treated with PD, such as abdominal leak or hernia [ 5 , 12 ]. In these studies, abdominal hernias were not associated with an increased risk of PD discontinuation. In the present meta-analysis, we confirm that episodes of abdominal hernia appeared statistically more often in PKD patients treated with PD. However, abdominal wall complications have been found to be more frequent in PKD patients at all stages of kidney disease including before end stage renal disease. As a consequence, it is likely that hernias may not be directly related to increased intraperitoneal pressure but may be related to collagen defects and thus be observed in PKD patients treated with other renal replacement therapies [ 21 ]. Increased risk of abdominal hernias was not associated with a decrease in technique survival. This suggests that for these patients, the therapeutic intervention such as reducing intraabdominal pressure (reduced volume infused of peritoneal solution or using automated peritoneal dialysis) is successful for maintaining them on PD therapy. In addition, studies included in this meta-analysis did not show any difference in term of fluid leak episode incidence [ 13 , 14 , 18 , 20 ].
Some reports indicate that PKD may be associated with an increased risk of diverticulitis, leading to greater risk of peritoneal infection in patients treated with PD [ 5 ]. In the present meta-analysis, including 6,767 patients, we found that PKD was not associated with a higher risk of occurrence of peritoneal infection. Furthermore, incidence of peritonitis episode requiring catheter removal did not differ between groups in Kumar et al. and Xie et al. (25% in PKD group vs 21% in non PKD group and 6,7% in PKD group vs 3,3% in non PKD group respectively) [ 18 , 19 ]. Staphylococcus spp was the main causative micro-organism in both groups while gram-negative organisms incidence did not differ between PKD and non PKD patients [ 14 , 15 , 17 , 18 , 19 ].
PD treatment offers numerous advantages [ 22 , 23 ], however only 7 to 10% of end-stage renal disease patients are treated with PD [ 2 ]. This reflects, at least in part, the clinicians’ fear of technical failure [ 24 ]. PKD patients are probably more concerned by this issue, because of the common misconception that these patients will develop infectious and mechanical complications if treated with PD, due to increased intraperitoneal pressure and a higher incidence of diverticulitis. Our results suggest that PD is a safe renal replacement modality for PKD patients. To the best of our knowledge, there is no available study designed to assess the impact of different PD modalities (continuous ambulatory peritoneal dialysis or automated peritoneal dialysis) on PKD patients’ outcomes.
First limitation of our study is related to the small number of publications on this subject. Additionally, all the studies included in the meta-analysis are retrospective or registry based studies. Indeed, there is no randomized clinical trial available on this subject. Therefore, a potential selection bias may limit the relevance of our conclusions for the entire PKD population. However, we collected all the study available (ie 9) and a total of 7,197 patients across the 9 studies (n = 2,923 to 7,046 patients for each outcome). This was a sufficient prerequisite to perform a meta-analysis. Another limitation is related to the relative importance of the study by Lobbedez et al. among the included studies due to the large number of patients included (n = 4162) accounting for almost half of the total population and Furthermore the design of the Lobbedez study, was different it was the only one including survival analysis after exclusion of the diabetic patients. However our results show strong stability when analyzed with or without Lobbedez’s study.
In conclusion, this meta-analysis showed that PKD patients treated with PD seem to have an increased survival and an increased rate of abdominal hernia, without any impact on PD technique survival. There was no statistical difference in peritonitis rate between PKD and no PKD patients. Therefore, our data suggest that peritoneal dialysis is a safe modality to treat end stage renal disease of PKD patients and should be offered to these patients. However, properly designed controlled studies are needed to determine whether all PKD patients are eligible for PD or whether some specific criteria should be determined. A particular attention should be given to the impact of total kidney volume and liver size in the feasibility of PD.
Supporting information
S1 checklist, funding statement.
The authors received no specific funding for this work.
Data Availability
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Definitions of and Instruments for Disease Activity, Remission, and Relapse in Polymyalgia Rheumatica: A Systematic Literature Review
Affiliations.
- 1 Department of Rheumatology, Sint Maartenskliniek, Ubbergen, The Netherlands.
- 2 Radboud Institute for Health Sciences, Radboud university medical center, Nijmegen, The Netherlands.
- 3 Department of Rheumatology and Immunology, Medical University of Graz, Graz, Austria.
- 4 School of Health and Related Research, University of Sheffield, United Kingdom.
- 5 Department of Rheumatology, Austin Health, Heidelberg, Victoria, Australia.
- 6 Department of Medicine, The University of Melbourne, Parkville, Victoria, Australia.
- 7 Centre for epidemiology, Norwich Medical School, Norwich, United Kingdom.
- 8 Department of Rheumatology, Norfolk and Norwich University Hospital, United Kingdom.
- 9 Leeds Institute for Rheumatic and Musculoskeletal Medicine, University of Leeds, Leeds, United Kingdom.
- 10 Leeds Biomedical Research Centre, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom.
- 11 Department of Rheumatology, Hospital of Brunico (SABES-ASDAA), Italy.
- 12 Department of Rheumatology, Teaching Hospital of the Paracelsus Medical University, Brunico, Italy.
- PMID: 39133187
- DOI: 10.1093/rheumatology/keae428
Objective: To perform a systematic literature review on definitions and instruments used to measure remission, relapse, and disease activity in polymyalgia rheumatica (PMR), to inform an OMERACT project to endorse instruments for these outcomes.
Methods: A search of Pubmed/MEDLINE, EMBASE, CINAHL, Cochrane, and Epistemonikos was performed May 2021 and updated August 2023. Qualitative and quantitative studies published in English were included if they recruited people with isolated PMR regardless of treatment. Study selection and data extraction was performed independently by two investigators and disagreement was resolved through discussion. Data extracted encompassed definitions of disease activity, remission and relapse, and details regarding the instruments used to measure these outcomes.
Results: From the 5,718 records, we included 26 articles on disease activity, 36 on remission, and 53 on relapse; 64 studies were observational and 15interventional, and none used qualitative methods. Some heterogeneity was found regarding definitions and instruments encompassing the domains pain, stiffness, fatigue, laboratory markers (mainly acute phase reactants), and patient and physician global assessment of disease activity. However, instruments for clinical signs were often poorly described. Whilst measurement properties of the polymyalgia rheumatica activity score (PMR-AS) have been assessed, data to support its use for measurement of remission and relapse is limited.
Conclusion: Remission, relapse, and disease activity have been defined heterogeneously in clinical studies. Instruments to measure these disease states still need to be validated. Qualitative research is needed to better understand the concepts of remission and relapse in PMR.
Review registration: PROSPERO identification: CRD42021255925.
Keywords: Polymyalgia rheumatica; disease activity; outcome measurement; relapse; remission; systematic literature review.
© The Author(s) 2024. Published by Oxford University Press on behalf of the British Society for Rheumatology. All rights reserved. For permissions, please email: [email protected].
PubMed Disclaimer
Similar articles
- Definition of remission and relapse in polymyalgia rheumatica: data from a literature search compared with a Delphi-based expert consensus. Dejaco C, Duftner C, Cimmino MA, Dasgupta B, Salvarani C, Crowson CS, Maradit-Kremers H, Hutchings A, Matteson EL, Schirmer M; International Work Group for PMR and GCA. Dejaco C, et al. Ann Rheum Dis. 2011 Mar;70(3):447-53. doi: 10.1136/ard.2010.133850. Epub 2010 Nov 19. Ann Rheum Dis. 2011. PMID: 21097803 Free PMC article. Review.
- Outcomes Measured in Polymyalgia Rheumatica and Measurement Properties of Instruments Considered for the OMERACT Core Outcome Set: A Systematic Review. Twohig H, Owen C, Muller S, Mallen CD, Mitchell C, Hider S, Hill C, Shea B, Mackie SL. Twohig H, et al. J Rheumatol. 2021 Jun;48(6):883-893. doi: 10.3899/jrheum.200248. Epub 2020 Aug 1. J Rheumatol. 2021. PMID: 32739892
- Polymyalgia Rheumatica (PMR) Special Interest Group at OMERACT 11: outcomes of importance for patients with PMR. Mackie SL, Arat S, da Silva J, Duarte C, Halliday S, Hughes R, Morris M, Pease CT, Sherman JW, Simon LS, Walsh M, Westhovens R, Zakout S, Kirwan JR. Mackie SL, et al. J Rheumatol. 2014 Apr;41(4):819-23. doi: 10.3899/jrheum.131254. Epub 2014 Feb 1. J Rheumatol. 2014. PMID: 24488422 Review.
- Folic acid supplementation and malaria susceptibility and severity among people taking antifolate antimalarial drugs in endemic areas. Crider K, Williams J, Qi YP, Gutman J, Yeung L, Mai C, Finkelstain J, Mehta S, Pons-Duran C, Menéndez C, Moraleda C, Rogers L, Daniels K, Green P. Crider K, et al. Cochrane Database Syst Rev. 2022 Feb 1;2(2022):CD014217. doi: 10.1002/14651858.CD014217. Cochrane Database Syst Rev. 2022. PMID: 36321557 Free PMC article.
- Development of a Provisional Core Domain Set for Polymyalgia Rheumatica: Report from the OMERACT 12 Polymyalgia Rheumatica Working Group. Helliwell T, Brouwer E, Pease CT, Hughes R, Hill CL, Neill LM, Halls S, Simon LS, Mallen CD, Boers M, Kirwan JR, Mackie SL. Helliwell T, et al. J Rheumatol. 2016 Jan;43(1):182-6. doi: 10.3899/jrheum.141179. Epub 2015 Nov 15. J Rheumatol. 2016. PMID: 26568595 Review.
Related information
Linkout - more resources, full text sources.
- Silverchair Information Systems
Research Materials
- NCI CPTC Antibody Characterization Program

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
COMMENTS
Polycystic kidney disease (PKD) is a multiorgan disorder resulting in fluid-filled cyst formation in the kidneys and other systems. The replacement of kidney parenchyma with an ever-increasing volume of cysts eventually leads to kidney failure. Recently, increased understanding of the pathophysiology of PKD and genetic advances have led to new ...
Autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic cause of renal failure worldwide. ADPKD is a multisystem and progressive inherited disorder with renal cyst formation, kidney enlargement, and extrarenal organ involvement (eg, liver, pancreas, spleen, cardiac, and arachnoid membranes).
Autosomal dominant polycystic kidney disease (PKD) and autosomal recessive PKD are progressive cilia-related disorders that often lead to chronic kidney disease and end-stage renal disease. This ...
Autosomal dominant polycystic kidney disease (ADPKD) is an inherited multisystem disorder, characterized by renal and extra-renal fluid-filled cyst formation and increased kidney volume that eventually leads to end-stage renal disease. ADPKD is considered the fourth leading cause of end-stage renal disease in the United States and globally.
Autosomal dominant polycystic kidney disease is a common cause of end stage kidney disease. It is a progressive and unfortunately incurable condition that can lead to significant morbidity and kidney failure. Many more patients are diagnosed with this disease without any symptoms as the population is increasingly undergoing imaging for other ...
Background Autosomal dominant polycystic kidney disease (ADPKD) is a genetic disorder characterised by progressive renal cyst formation leading to renal failure in the majority of patients. The likelihood and rate of ADPKD progression is difficult to predict and there is a clear need to identify prognostic indicators that could be used to anticipate ADPKD progression, to aid the management of ...
Autosomal dominant polycystic kidney disease (ADPKD) is the most common genetic cause of end-stage renal disease (ESRD), affecting an estimated 1 in 1,000 people 1. Mutations in either PKD1 or ...
Women. Women with autosomal dominant polycystic kidney disease may have massive cystic enlargement of the liver, 1 a complication attributed to the role of estrogens in promoting the growth of ...
The prevalence of autosomal dominant polycystic kidney disease (ADPKD): A meta-analysis of European literature and prevalence evaluation in the Italian province of Modena suggest that ADPKD is a ...
Autosomal dominant polycystic kidney disease (ADPKD) is characterized by cysts in the kidneys and, in many cases, is associated with cysts in the liver and pancreas that can be helpful in confirming the diagnosis. In addition, patients may have a variety of other abnormalities, many of which are consistent with a generalized defect in ...
INTRODUCTION Polycystic kidney disease (PKD) includes inherited diseases that cause an irreversible decline in kidney function. PKD is most commonly encountered as an autosomal dominant disease, while the rare autosomal recessive form represents a different entity. The autosomal dominant form (autosomal dominant PKD [ADPKD]) is the most common genetic cause of chronic kidney disease (CKD) [ 1 ...
Autosomal dominant polycystic kidney disease (ADPKD) is a slowly progressive kidney disease, and the effect of interventions on hard outcomes such as onset of end-stage kidney disease (ESKD) may be challenging to ascertain given the short duration of most clinical trials, where the statistical power may be low.1 We previously demonstrated a "legacy effect" of target BP interventions in ...
This JAMA Patient Page describes autosomal dominant polycystic kidney disease, its signs and symptoms, diagnosis, and treatment options.
Autosomal dominant polycystic kidney disease (ADPKD) is generally a late-onset multisystem disorder characterized by bilateral kidney cysts, liver cysts, and an increased risk of intracranial aneurysms. Other manifestations include: cysts in the pancreas, seminal vesicles, and arachnoid membrane; dilatation of the aortic root and dissection of the thoracic aorta; mitral valve prolapse; and ...
Abstract. Autosomal polycystic kidney disease is the most common inherited kidney disease determining 5% of all end-stage kidney disease. The only therapy approved for this condition is Tolvaptan, which, with its aquaretic effect, has a strong effect on patients' daily life. Recently, the literature has been enriched with new works that analyze ...
Methods: A systematic review and meta-analysis were performed examining all studies which included "Polycystic kidney disease" and "Peritoneal dialysis" in their titles, excluding commentaries, letters to the authors and abstracts.
BACKGROUND Polycystic renal disease is a frequent congenital anomaly of the kidneys, but research using chromosomal microarray analysis and exome sequencing in fetuses with polycystic renal disease remains sparse, with most studies focusing on the multisystem or genitourinary system.
Introduction: Polycystic kidney diseases are common disorders and are considered as common causes of end stage renal disease, both in children and in adults. General surgeons, neonatologists, pediatric urologists, nephrologists and general physicians frequently encounter patients with polycystic kidney diseases.
Polycystic kidney disease (PKD) is a multiorgan disorder resulting in fluid-filled cyst formation in the kidneys and other systems. The replacement of kidney parenchyma with an ever-increasing volume of cysts eventually leads to kidney failure. Recently, increased understanding of the pathophysiology of PKD and genetic advances have led to new approaches of treatment targeting physiologic ...
Cystic kidneys are common causes of end-stage renal disease, both in children and in adults. Autosomal dominant polycystic kidney disease (ADPKD) and autosomal recessive polycystic kidney disease (ARPKD) are cilia-related disorders and the two main forms ...
Autosomal dominant polycystic kidney disease (ADPKD) is a genetic kidney disorder with multiple cyst formation that progresses to chronic kidney disease (CKD) and end-stage kidney disease. Plant-based diets have attracted considerable attention because they may prevent CKD development. This study investigated whether adherence to a plant-based diet is associated with kidney function in ...
The clinical manifestations of autosomal recessive polycystic kidney disease are multiple renal cyst, cyst of liver and liver fibrosis, intrahepatic bile duct dilatation. Two mutations (c.4274T > G, c.7973T > A) in PKHD1 gene may be pathogenic.
Tubal mesosalpinx cysts are paratubal cysts, that account for approximately 10% of adnexal masses, and the presence of these cysts combined with adnexal torsion is a rare acute abdominal condition, with few cases reported in the literature. We reported two cases of adolescent tubal mesosalpinx cysts combined with adnexal torsion and reviewed the literature to help improve the diagnosis of the ...
A literature review and meta-analysis of available data were performed from January 2000 to September 2023 to identify reported data of prevalence, clinical manifestation, and genetics anomalies of patients with polycystic kidney disease in the continent.
Adult polycystic kidney disease (APKD) is a frequent disease (1/1000) responsible for about 10% of chronic renal failure. It is an autosomic dominant disease due to mutation of one out of three genes: PKD1 (on the 16th chromosome), PKD2 (on the 4th chromosome) and PKD3 (still unmapped). In the past APKD diagnosis was normally done in fourteen ...
NIH Funding Opportunities and Notices in the NIH Guide for Grants and Contracts: Central Coordinating Site for the Polycystic Kidney Disease Research Core Centers (U24 Clinical Trial Not Allowed) RFA-DK-25-015. NIDDK
A systematic review and meta-analysis were performed examining all studies which included "Polycystic kidney disease" and "Peritoneal dialysis" in their titles, excluding commentaries, letters to the authors and abstracts. PubMed, Embase, Google scholar and Scopus were searched to December 31 st 2017.
Objective: To perform a systematic literature review on definitions and instruments used to measure remission, relapse, and disease activity in polymyalgia rheumatica (PMR), to inform an OMERACT project to endorse instruments for these outcomes.