What is Problem-Solving in Nursing? (With Examples, Importance, & Tips to Improve)

Whether you have been a nurse for many years or you are just beginning your nursing career, chances are, you know that problem-solving skills are essential to your success. With all the skills you are expected to develop and hone as a nurse, you may wonder, “Exactly what is problem solving in nursing?” or “Why is it so important?” In this article, I will share some insight into problem-solving in nursing from my experience as a nurse. I will also tell you why I believe problem-solving skills are important and share some tips on how to improve your problem-solving skills.

What Exactly is Problem-Solving in Nursing?
5 reasons why problem-solving is important in nursing, reason #1: good problem-solving skills reflect effective clinical judgement and critical thinking skills, reason #2: improved patient outcomes, reason #3: problem-solving skills are essential for interdisciplinary collaboration, reason #4: problem-solving skills help promote preventative care measures, reason #5: fosters opportunities for improvement, 5 steps to effective problem-solving in nursing, step #1: gather information (assessment), step #2: identify the problem (diagnosis), step #3: collaborate with your team (planning), step #4: putting your plan into action (implementation), step #5: decide if your plan was effective (evaluation), what are the most common examples of problem-solving in nursing, example #1: what to do when a medication error occurs, how to solve:, example #2: delegating tasks when shifts are short-staffed, example #3: resolving conflicts between team members, example #4: dealing with communication barriers/lack of communication, example #5: lack of essential supplies, example #6: prioritizing care to facilitate time management, example #7: preventing ethical dilemmas from hindering patient care, example #8: finding ways to reduce risks to patient safety, bonus 7 tips to improve your problem-solving skills in nursing, tip #1: enhance your clinical knowledge by becoming a lifelong learner, tip #2: practice effective communication, tip #3: encourage creative thinking and team participation, tip #4: be open-minded, tip #5: utilize your critical thinking skills, tip #6: use evidence-based practices to guide decision-making, tip #7: set a good example for other nurses to follow, my final thoughts, list of sources used for this article.

- Faye Abdellah: 21 Nursing Problems Theory

Faye Abdellah is a celebrated nurse theorist, military nurse, and leader in nursing research. Get to know the major concepts of her “ 21 Nursing Problems ” nursing theory, its application, and its impact on nursing.
Table of Contents
Early life of faye abdellah, as an educator, as a researcher, established nursing standards, military nursing service, abdellah’s typology of 21 nursing problems, awards and honors, assumptions, nursing problems, problem solving, basic needs, sustenal care needs, remedial care needs, restorative care needs, patient-centered approaches to nursing, 21 nursing problems and the nursing process, recommended resources, external links, biography of faye glenn abdellah.
Faye Glenn Abdellah (March 13, 1919 – present) is a nursing research pioneer who developed the “Twenty-One Nursing Problems.” Her nursing model was progressive for the time in that it refers to a nursing diagnosis during a time in which nurses were taught that diagnoses were not part of their role in health care.
She was the first nurse officer to rank a two-star rear admiral, the first nurse, and the first woman to serve as a Deputy Surgeon General.
On March 13, 1919, Faye Abdellah was born in New York to a father of Algerian heritage and a Scottish mother. Her family subsequently moved to New Jersey, where she attended high school.
Years later, on May 6, 1937, the German hydrogen-fueled airship Hindenburg exploded over Lakehurst.

Abdellah and her brother witnessed the explosion, destruction, and fire after the ignited hydrogen killed many people. That incident became the turning point in Abdellah’s life. It was that time when she realized that she would never again be powerless to assist when people were in such a dire need of assistance. It was at that moment she vowed that she would learn to nurse and become a professional nurse.
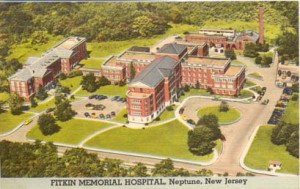
Faye Abdellah earned a nursing diploma from Fitkin Memorial Hospital’s School of Nursing, now known as Ann May School of Nursing.
It was sufficient to practice nursing during her time in the 1940s, but she believed that nursing care should be based on research, not hours of care.
Abdellah went on to earn three degrees from Columbia University: a bachelor of science degree in nursing in 1945, a master of arts degree in physiology in 1947, and a doctor of education degree in 1955.

With her advanced education, Abdellah could have chosen to become a doctor. However, as she explained in one of her interviews that she wanted to be an M.D. because she could do all she wanted to do in nursing, which is a caring profession.
Career and Appointments
In her early twenties, Faye Abdellah worked as a health nurse at a private school, and her first administrative position was on the faculty of Yale University from 1945-1949. At that time, she was required to teach a class called “120 Principles of Nursing Practice,” using a standard nursing textbook published by the National League for Nursing. The book included guidelines that had no scientific basis, which challenged Abdellah to explain everything she called the “brilliant” students.

After a year, Abdellah became so frustrated that she gathered her colleagues in the Yale courtyard and burned the textbooks. The next morning the school’s dean told her she would have to pay for the destroyed texts. It took a year for Abdellah to settle the debt, but she never regretted her actions because it started her on the long road to pursue the scientific basis of the nursing practice .
In 1949, she met Lucile Petry Leone, the first Nurse Officer, and decided to join the Public Health Service. Her first assignment was with the division of nursing that focused on research and studies. They performed studies with numerous hospitals to improve nursing practice .
Abdellah was an advocate of degree programs for nursing. Diploma programs, she believes, were never meant to prepare nurses at the professional level. Nursing education, she argued, should be based on research; she herself became among the first in her role as an educator to focus on theory and research. Her first studies were qualitative; they simply described situations. As her career progressed, her research evolved to include physiology, chemistry, and behavioral sciences.
In 1957, Abdellah spearheaded a research team in Manchester, Connecticut, that established the groundwork for what became known as progressive patient care . In this framework, critical care patients were treated in an intensive care unit, followed by a transition to immediate care and then home care. The first two segments of the care program proved very popular within the caregiver profession. Abdellah is also credited with developing the first nationally tested coronary care unit as an outgrowth of her work in Manchester.

Home care, which is the third phase of the progressive patient care equation, was not widely accepted in the mid-twentieth century. Abdellah explained that people at the time kept saying home care would mean having a maid or a nurse in everyone’s home. They could not figure out that home care with nurses teaching self-care would help patients regain independent function. Forty years later, home care had become an essential part of long-term health care.
In another innovation within her field, Abdellah developed the Patient Assessment of Care Evaluation (PACE), a system of standards used to measure the relative quality of individual health-care facilities that were still used in the healthcare industry into the 21st century. She was also one of the first people in the healthcare industry to develop a classification system for patient care and patient-oriented records.

Classification systems have evolved in different ways within the health-care industry, and Abdellah’s work was foundational in developing the most widely used form: Diagnostic related groups, or DRGs. DRGs, which became the standard coding system used by Medicare, categorize patients according to particular primary and secondary diagnoses. This system keeps health-care costs down because each DRG code includes the maximum amount Medicare will payout for a specific diagnosis or procedure while also taking into account patient age and length of stay in a healthcare facility. Providers are given an incentive to keep costs down because they only realize a profit if costs are less than the amount specified by the relevant DRG category.

During her 40-year career as a Commissioned Officer in the U.S. Public Health Service from 1949 to 1989, Abdellah was assigned to work with the Korean people during the Korean War. As a senior officer, she was alternatively assigned to Japan, China , Russia, Australia, and the Scandinavian countries to identify the Public Health Service’s role in dealing with various health problems. She was able to assist and initiate, in an advisory role, numerous studies in those countries.
She served as Chief Nurse Officer from 1970 to 1987 and was the first nurse to achieve the rank of a two-star Flag Officer named by U.S. Surgeon General C. Everett Koop as the first woman and nurse Deputy Surgeon General from 1982 to 1989. After retirement, Abdellah founded and served as the first dean in the Graduate School of Nursing, GSN, Uniformed Services University of the Health Sciences (USUHS).
Faye Abdellah is well known for developing the “Twenty-One Nursing Problems Theory” that has interrelated the concepts of health, nursing problems, and problem-solving.
She views nursing as an art and a science that molds the attitude, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help individuals cope with their health needs, whether they are ill or well.
She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems.
Faye Abdellah’s theory is further discussed below.
As a consultant and educator, Faye Abdellah shared her nursing theories with caregivers around the world. She led seminars in France, Portugal, Israel, Japan, China, New Zealand, Australia, and the former Soviet Union. She also served as a research consultant to the World Health Organization. From her global perspective, Abdellah learned to appreciate nontraditional and complementary medical treatments and developed the belief such non-Western treatments deserved scientific research.

Also, she has been active in professional nursing associations and is a prolific author, with more than 150 publications. Her publications include Better Nursing Care Through Nursing Research and Patient-Centered Approaches to Nursing . She also developed educational materials in many areas of public health, including AIDS , hospice care , and drug addiction.
Abdellah considers her greatest accomplishment being able to “play a role in establishing a foundation for nursing research as a science.” Her book, Patient-Centered Approaches to Nursing , emphasizes nursing science and has elicited changes throughout nursing curricula. Her work, which is based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome.

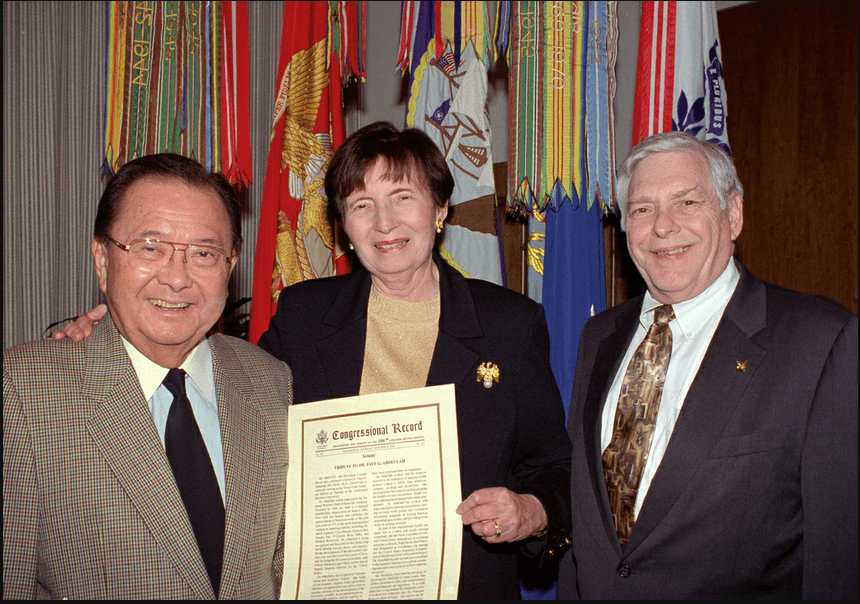
Faye Abdellah is recognized as a leader in nursing research and nursing as a profession within the Public Health Service (PHS) and as an international expert on health problems. She was named a “living legend” by the American Academy of Nursing in 1994 and was inducted into the National Women’s Hall of Fame in 2000 for a lifetime spent establishing and leading essential health care programs for the United States. In 2012, Abdellah was inducted into the American Nurses Association Hall of Fame for a lifetime of contributions to nursing.
Her contributions to nursing and public health have been recognized with almost 90 professional and academic honors, such as the Allied Signal Achievement Award for pioneering research in aging and Sigma Theta Tau’s Lifetime Achievement Award.
Abdellah’s leadership , her publications, and her lifelong contributions have set a new standard for nursing and health care. Her legacy of more than 60 years of extraordinary accomplishments lives nationally and globally.
Aside from being the first nurse and the first woman to serve as a Deputy Surgeon General, Faye Glenn Abdellah also made a name in the nursing profession to formulate her “21 Nursing Problems Theory.” Her theory changed the focus of nursing from disease-centered to patient-centered and began to include the care of families and the elderly in nursing care. The Patient Assessment of Care Evaluation developed by Abdellah is now the standard used in the United States.
Abdellah’s 21 Nursing Problems Theory
According to Faye Glenn Abdellah’s theory, “Nursing is based on an art and science that molds the attitudes, intellectual competencies, and technical skills of the individual nurse into the desire and ability to help people, sick or well, cope with their health needs.”
The patient-centered approach to nursing was developed from Abdellah’s practice, and the theory is considered a human needs theory. It was formulated to be an instrument for nursing education , so it most suitable and useful in that field. The nursing model is intended to guide care in hospital institutions but can also be applied to community health nursing, as well.
The assumptions Abdellah’s “21 Nursing Problems Theory” relate to change and anticipated changes that affect nursing; the need to appreciate the interconnectedness of social enterprises and social problems; the impact of problems such as poverty, racism, pollution, education, and so forth on health and health care delivery; changing nursing education ; continuing education for professional nurses; and development of nursing leaders from underserved groups.
- Learn to know the patient.
- Sort out relevant and significant data.
- Make generalizations about available data concerning similar nursing problems presented by other patients.
- Identify the therapeutic plan.
- Test generalizations with the patient and make additional generalizations.
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting this behavior.
- Explore the patient’s and family’s reaction to the therapeutic plan and involve them in the plan.
- Identify how the nurse feels about the patient’s nursing problems.
- Discuss and develop a comprehensive nursing care plan .
Major Concepts of 21 Nursing Problems Theory
The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
She describes nursing recipients as individuals (and families), although she does not delineate her beliefs or assumptions about the nature of human beings.
Health, or the achieving of it, is the purpose of nursing services. Although Abdellah does not define health, she speaks to “total health needs” and “a healthy state of mind and body.”
Health may be defined as the dynamic pattern of functioning whereby there is a continued interaction with internal and external forces that results in the optimal use of necessary resources to minimize vulnerabilities.
Society is included in “ planning for optimum health on local, state, and international levels.” However, as Abdellah further delineates her ideas, the focus of nursing service is clearly the individual.
The client’s health needs can be viewed as problems, overt as an apparent condition, or covert as a hidden or concealed one.
Because covert problems can be emotional, sociological, and interpersonal in nature, they are often missed or misunderstood. Yet, in many instances, solving the covert problems may solve the overt problems as well.
Quality professional nursing care requires that nurses be able to identify and solve overt and covert nursing problems. The problem-solving process can meet these requirements by identifying the problem, selecting pertinent data, formulating hypotheses, testing hypotheses through collecting data, and revising hypotheses when necessary based on conclusions obtained from the data.
Subconcepts
The following are the subconcepts of Faye Abdellah’s “21 Nursing Problems” theory and their definitions.
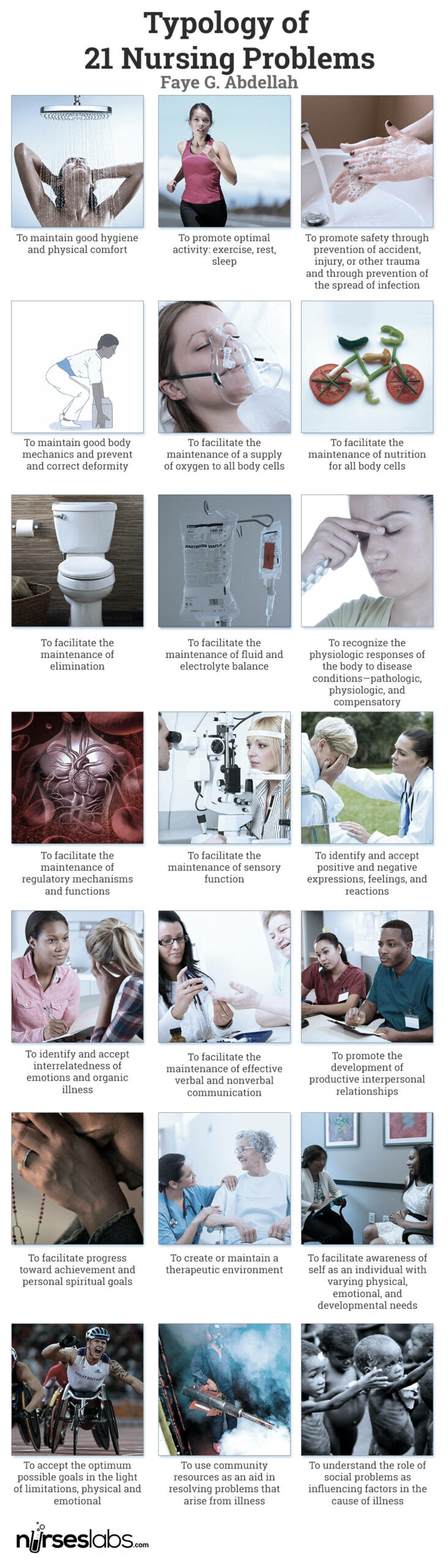
The 21 nursing problems fall into three categories: physical, sociological, and emotional needs of patients; types of interpersonal relationships between the patient and nurse; and common elements of patient care . She used Henderson’s 14 basic human needs and nursing research to establish the classification of nursing problems. Abdellah’s 21 Nursing Problems are the following:
- To maintain good hygiene and physical comfort .
- To promote optimal activity: exercise, rest, sleep
- To promote safety by preventing accidents, injuries, or other trauma and preventing the spread of infection .
- To maintain good body mechanics and prevent and correct the deformity.
- To facilitate the maintenance of a supply of oxygen to all body cells.
- To facilitate the maintenance of nutrition for all body cells.
- To facilitate the maintenance of elimination.
- To facilitate the maintenance of fluid and electrolyte balance.
- To recognize the physiologic responses of the body to disease conditions—pathologic, physiologic, and compensatory.
- To facilitate the maintenance of regulatory mechanisms and functions.
- To facilitate the maintenance of sensory function.
- To identify and accept positive and negative expressions, feelings, and reactions.
- To identify and accept interrelatedness of emotions and organic illness.
- To facilitate the maintenance of effective verbal and nonverbal communication .
- To promote the development of productive interpersonal relationships.
- To facilitate progress toward achievement and personal spiritual goals.
- To create or maintain a therapeutic environment.
- To facilitate awareness of self as an individual with varying physical, emotional, and developmental needs.
- To accept the optimum possible goals in the light of limitations, physical and emotional.
- To use community resources as an aid in resolving problems that arise from an illness.
- To understand the role of social problems as influencing factors in the cause of illness.
Moreover, patients’ needs are further divided into four categories: basic to all patients , sustenance care needs , remedial care needs , and restorative care needs .
The basic needs of an individual patient are to maintain good hygiene and physical comfort ; promote optimal health through healthy activities, such as exercise, rest, and sleep ; promote safety through the prevention of health hazards like accidents, injury , or other trauma and the prevention of the spread of infection; and maintain good body mechanics and prevent or correct deformity.
Sustenal care needs to facilitate the maintenance of a supply of oxygen to all body cells; facilitate the maintenance of nutrition of all body cells; facilitate the maintenance of elimination; facilitate the maintenance of fluid and electrolyte balance; recognize the physiological responses of the body to disease conditions; facilitate the maintenance of regulatory mechanisms and functions, and facilitate the maintenance of sensory function.
Remedial care needs to identify and accept positive and negative expressions, feelings, and reactions; identify and accept the interrelatedness of emotions and organic illness; facilitate the maintenance of effective verbal and non- verbal communication ; promote the development of productive interpersonal relationships; facilitate progress toward achievement of personal spiritual goals; create and maintain a therapeutic environment; and facilitate awareness of the self as an individual with varying physical, emotional, and developmental needs.
Restorative care needs include the acceptance of the optimum possible goals in light of limitations, both physical and emotional; the use of community resources as an aid to resolving problems that arise from an illness; and the understanding of the role of social problems as influential factors in the case of illness.
Abdellah’s work, based on the problem-solving method, serves as a vehicle for delineating nursing (patient) problems as the patient moves toward a healthy outcome. The theory identifies ten steps to identify the patient’s problem and 11 nursing skills to develop a treatment typology.

The ten steps are:
- Validate the patient’s conclusions about his nursing problems.
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting his or her behavior.
- Explore the patient and their family’s reactions to the therapeutic plan and involve them in the plan.
- Identify how the nurses feel about the patient’s nursing problems.
The 11 nursing skills are:
- observation of health status
- skills of communication
- application of knowledge
- the teaching of patients and families
- planning and organization of work
- use of resource materials
- use of personnel resources
- problem-solving
- the direction of work of others
- therapeutic uses of the self
- nursing procedure
Abdellah also explained nursing as a comprehensive service, which includes:
- Recognizing the nursing problems of the patient
- Deciding the appropriate course of action to take in terms of relevant nursing principles
- Providing continuous care of the individual’s total needs
- Providing continuous care to relieve pain and discomfort and provide immediate security for the individual
- Adjusting the total nursing care plan to meet the patient’s individual needs
- Helping the individual to become more self- directing in attaining or maintaining a healthy state of body and mind
- Instructing nursing personnel and family to help the individual do for himself that which he can within his limitations
- Helping the individual to adjust to his limitations and emotional problems
- Working with allied health professions in planning for optimum health on local, state, national, and international levels
- Carrying out continuous evaluation and research to improve nursing techniques and to develop new techniques to meet people’s health needs
Faye Abdellah’s work is a set of problems formulated in terms of nursing-centered services used to determine the patient’s needs. The nursing-centered orientation to client care appears to be contradicting the client-centered approach that Abdellah professes to support. This can be observed by her desire to move away from a disease-centered orientation.
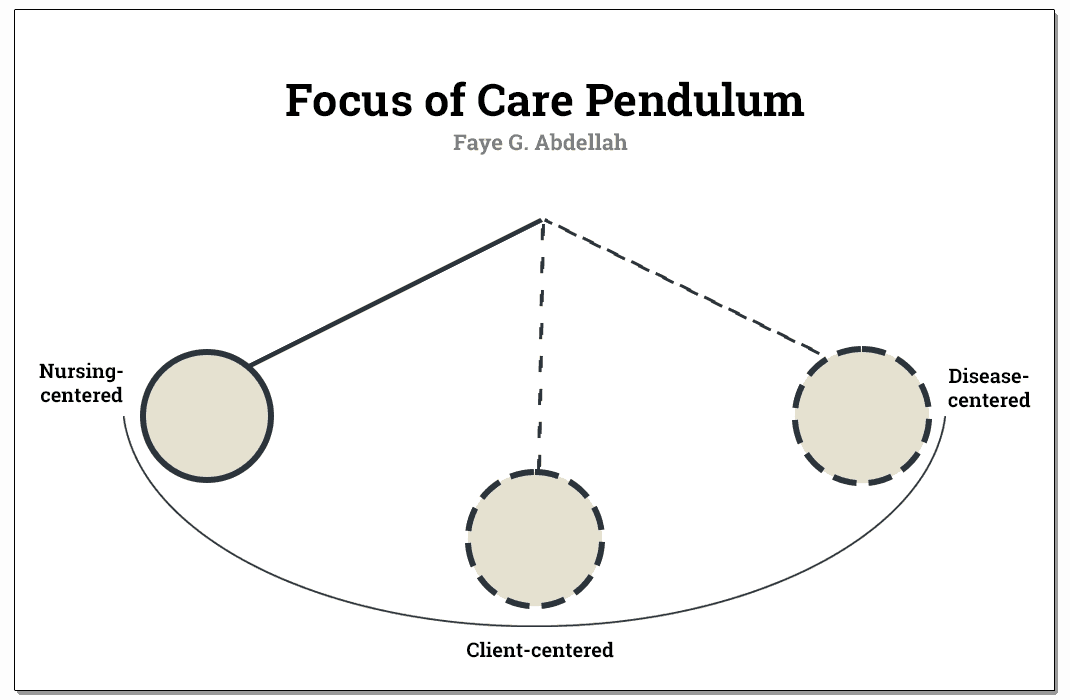
In her attempt to bring the nursing practice to its proper relationship with restorative and preventive measures for meeting total client needs, she seems to swing the pendulum to the opposite pole, from the disease orientation to nursing orientation, while leaving the client somewhere in the middle.
The nursing process in Abdellah’s theory includes assessment , nursing diagnosis , planning, implementation , and evaluation.
In the assessment phase , the nursing problems implement a standard procedure for data collection . A principle underlying the problem-solving approach is that for each identified problem, pertinent data is collected. The overt or covert nature of problems necessitates a direct or indirect approach, respectively.
The outcome of the collection of data in the first phase concludes the patient’s possible problems, which can be grouped under one or more of the broader nursing problems. This will further lead to the nursing diagnosis .
After formulating the diagnosis, a nursing care plan is developed, and appropriate nursing interventions are determined. The nurse now sets those interventions in action, which complete the implementation phase of the nursing process .
The evaluation takes place after the interventions have been carried out. The most convenient evaluation would be the nurse’s progress or lack of progress toward achieving the goals established in the planning phase.
With Faye Abdellah’s aim in formulating a clear categorization of patient’s problems as health needs, she rather conceptualized nurses’ actions in nursing care, which is contrary to her aim. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
The problem-solving approach introduced by Abdellah has the advantage of increasing the nurse’s critical and analytical thinking skills since the care to be provided would be based on sound assessment and validation of findings.
One can identify that the framework is strongly applied to individuals as the focus of nursing care. The inclusion of an aggregate of people such as the community or society would make the theory of Abdellah more generalizable since nurses do not only provide one-person service, especially now that the community healthcare level is sought to have higher importance than curative efforts in the hospital.
The following are the strengths of Faye Abdellah’s “21 Nursing Problems” theory.
- The problem-solving approach is readily generalizable to the client with specific health needs and specific nursing problems.
- With the model’s nature, healthcare providers and practitioners can use Abdellah’s problem-solving approach to guide various activities within the clinical setting. This is true when considering a nursing practice that deals with clients with specific needs and specific nursing problems.
- The language of Faye Abdellah’s framework is simple and easy to comprehend.
- The theoretical statement greatly focuses on problem-solving, an activity that is inherently logical in nature.
The following are the limitations of Faye Abdellah’s “21 Nursing Problems” theory.
- The major limitation to Abdellah’s theory and the 21 nursing problems is their robust nurse-centered orientation. She rather conceptualized nurses’ actions in nursing care which is contrary to her aim.
- Another point is the lack of emphasis on what the client is to achieve was given in client care.
- The framework seems to focus quite heavily on nursing practice and individuals. This somewhat limits the generalizing ability, although the problem-solving approach is readily generalizable to clients with specific health needs and specific nursing.
- Also, Abdellah’s framework is inconsistent with the concept of holism. The nature of the 21 nursing problems attests to this. As a result, the client may be diagnosed with numerous problems leading to fractionalized care efforts. Potential problems might be overlooked because the client is not deemed to be in a particular illness stage.
Abdellah’s typology of 21 nursing problems is a conceptual model mainly concerned with patient’s needs and nurses’ role in problem identification using a problem analysis approach.
According to the model, patients are described as having physical, emotional, and sociological needs. People are also the only justification for the existence of nursing. Without people, nursing would not be a profession since they are the recipients of nursing.
Patient-centered approaches to nursing health are described as a state mutually exclusive of illness. Abdellah does not define health but speaks to “total health needs” and “a healthy state of mind and body” in her nursing description.
However, Abdellah rather conceptualized nurses’ actions in nursing care, contrary to her aim of formulating a clear categorization of patients’ problems as health needs. Nurses’ roles were defined to alleviate the problems assessed through the proposed problem-solving approach.
As a whole, the theory is intended to guide care not just in the hospital setting but can also be applied to community nursing, as well. The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature.
Furthermore, the 21 nursing problems progressed to a second-generation development referred to as patient problems and patient outcomes . Abdellah educated the public on AIDS , drug addiction, violence, smoking, and alcoholism. Her work is a problem-centered approach or philosophy of nursing.
Recommended books and resources to learn more about nursing theory:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
- Nursing Theorists and Their Work (10th Edition) by Alligood Nursing Theorists and Their Work, 10th Edition provides a clear, in-depth look at nursing theories of historical and international significance. Each chapter presents a key nursing theory or philosophy, showing how systematic theoretical evidence can enhance decision making, professionalism, and quality of care.
- Knowledge Development in Nursing: Theory and Process (11th Edition) Use the five patterns of knowing to help you develop sound clinical judgment. This edition reflects the latest thinking in nursing knowledge development and adds emphasis to real-world application. The content in this edition aligns with the new 2021 AACN Essentials for Nursing Education.
- Nursing Knowledge and Theory Innovation, Second Edition: Advancing the Science of Practice (2nd Edition) This text for graduate-level nursing students focuses on the science and philosophy of nursing knowledge development. It is distinguished by its focus on practical applications of theory for scholarly, evidence-based approaches. The second edition features important updates and a reorganization of information to better highlight the roles of theory and major philosophical perspectives.
- Nursing Theories and Nursing Practice (5th Edition) The only nursing research and theory book with primary works by the original theorists. Explore the historical and contemporary theories that are the foundation of nursing practice today. The 5th Edition, continues to meet the needs of today’s students with an expanded focus on the middle range theories and practice models.
- Strategies for Theory Construction in Nursing (6th Edition) The clearest, most useful introduction to theory development methods. Reflecting vast changes in nursing practice, it covers advances both in theory development and in strategies for concept, statement, and theory development. It also builds further connections between nursing theory and evidence-based practice.
- Middle Range Theory for Nursing (4th Edition) This nursing book’s ability to break down complex ideas is part of what made this book a three-time recipient of the AJN Book of the Year award. This edition includes five completely new chapters of content essential for nursing books. New exemplars linking middle range theory to advanced nursing practice make it even more useful and expand the content to make it better.
- Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice This book offers balanced coverage of both qualitative and quantitative research methodologies. This edition features new content on trending topics, including the Next-Generation NCLEX® Exam (NGN).
- Nursing Research (11th Edition) AJN award-winning authors Denise Polit and Cheryl Beck detail the latest methodologic innovations in nursing, medicine, and the social sciences. The updated 11th Edition adds two new chapters designed to help students ensure the accuracy and effectiveness of research methods. Extensively revised content throughout strengthens students’ ability to locate and rank clinical evidence.
Recommended site resources related to nursing theory:
- Nursing Theories and Theorists: The Definitive Guide for Nurses MUST READ! In this guide for nursing theories, we aim to help you understand what comprises a nursing theory and its importance, purpose, history, types or classifications, and give you an overview through summaries of selected nursing theories.
Other resources related to nursing theory:
- Betty Neuman: Neuman Systems Model
- Dorothea Orem: Self-Care Deficit Theory
- Dorothy Johnson: Behavioral System Model
- Florence Nightingale: Environmental Theory
- Hildegard Peplau: Interpersonal Relations Theory
- Ida Jean Orlando: Deliberative Nursing Process Theory
- Imogene King: Theory of Goal Attainment
- Jean Watson: Theory of Human Caring
- Lydia Hall: Care, Cure, Core Nursing Theory
- Madeleine Leininger: Transcultural Nursing Theory
- Martha Rogers: Science of Unitary Human Beings
- Myra Estrin Levine: The Conservation Model of Nursing
- Nola Pender: Health Promotion Model
- Sister Callista Roy: Adaptation Model of Nursing
- Virginia Henderson: Nursing Need Theory
- Abdellah, F.G. The federal role in nursing education. Nursing outlook. 1987, 35(5),224-225.
- Abdellah, F.G. Public policy impacting on nursing care of older adults. In E.M. Baines (Ed.), perspectives on gerontological nursing. Newbury, CA: Sage publications. 1991.
- Abdellah, F.G., & Levine, E. Preparing nursing research for the 21st century. New York: Springer. 1994.
- Abdellah, F.G., Beland, I.L., Martin, A., & Matheney, R.V. Patient-centered approaches to nursing (2nd ed.). New York: Mac Millan. 1968.
- Abdellah, F.G. Evolution of nursing as a profession: perspective on manpower development. International Nursing Review, 1972); 19, 3..
- Abdellah, F.G.). The nature of nursing science. In L.H. Nicholl (Ed.), perspectives on nursing theory. Boston: Little, Brown, 1986.
- Craddock, J. (2013). Encyclopedia of world biography supplement. Detroit, Mich.: Gale. https://www.encyclopedia.com/doc/1G2-3435000010.html
- Better Patient Care Through Nursing Research
- Preparing Nursing Research for the 21st Century: Evolution, Methodologies, Challenges
With contributions by Wayne, G. (for Biography), Vera, M.
6 thoughts on “Faye Abdellah: 21 Nursing Problems Theory”
Thank you for sharing Angelo
I mean no disrespect to RADM Abdellah’s service to our nation, but the USPHS is not part of the military. It is part of the Uniformed Services, but not in the Dept of Defense.
Oh! Good to know! Thanks for clarifying :)
An insightful information 👌
I was a brand new lieutenant US Army and just graduated from college to become a nurse. I had used Faye Abdellah’s Theories as the rationale for nursing care plans in school papers, so I was very familiar. A big professional regret was I had the opportunity to meet Faye at a nursing conference in Germany. I was a timid young nurse and somewhat shy and saw her in one of the conference sessions sitting by herself. I wish I introduced myself and talked to her. I really respected her as a pioneer in nursing theory.
thanks for sharing.
Leave a Comment Cancel reply

ANA Nursing Resources Hub
Search Resources Hub

Critical Thinking in Nursing: Tips to Develop the Skill
4 min read • February, 09 2024
Critical thinking in nursing helps caregivers make decisions that lead to optimal patient care. In school, educators and clinical instructors introduced you to critical-thinking examples in nursing. These educators encouraged using learning tools for assessment, diagnosis, planning, implementation, and evaluation.
Nurturing these invaluable skills continues once you begin practicing. Critical thinking is essential to providing quality patient care and should continue to grow throughout your nursing career until it becomes second nature.
What Is Critical Thinking in Nursing?
Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Reflection comes next. Carefully consider whether your actions led to the right solution or if there may have been a better course of action.
Remember, there's no one-size-fits-all treatment method — you must determine what's best for each patient.
How Is Critical Thinking Important for Nurses?
As a patient's primary contact, a nurse is typically the first to notice changes in their status. One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. By applying critical-thinking skills to anticipate and understand your patients' needs, you can positively impact their quality of care and outcomes.
Elements of Critical Thinking in Nursing
To assess situations and make informed decisions, nurses must integrate these specific elements into their practice:
- Clinical judgment. Prioritize a patient's care needs and make adjustments as changes occur. Gather the necessary information and determine what nursing intervention is needed. Keep in mind that there may be multiple options. Use your critical-thinking skills to interpret and understand the importance of test results and the patient’s clinical presentation, including their vital signs. Then prioritize interventions and anticipate potential complications.
- Patient safety. Recognize deviations from the norm and take action to prevent harm to the patient. Suppose you don't think a change in a patient's medication is appropriate for their treatment. Before giving the medication, question the physician's rationale for the modification to avoid a potential error.
- Communication and collaboration. Ask relevant questions and actively listen to others while avoiding judgment. Promoting a collaborative environment may lead to improved patient outcomes and interdisciplinary communication.
- Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most appropriate one. Besides assessing patient conditions, you can apply these skills to other challenges, such as staffing issues .

How to Develop and Apply Critical-Thinking Skills in Nursing
Critical-thinking skills develop as you gain experience and advance in your career. The ability to predict and respond to nursing challenges increases as you expand your knowledge and encounter real-life patient care scenarios outside of what you learned from a textbook.
Here are five ways to nurture your critical-thinking skills:
- Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice . That knowledge helps you make informed decisions in stressful moments.
- Practice reflection. Allow time each day to reflect on successes and areas for improvement. This self-awareness can help identify your strengths, weaknesses, and personal biases to guide your decision-making.
- Open your mind. Don't assume you're right. Ask for opinions and consider the viewpoints of other nurses, mentors , and interdisciplinary team members.
- Use critical-thinking tools. Structure your thinking by incorporating nursing process steps or a SWOT analysis (strengths, weaknesses, opportunities, and threats) to organize information, evaluate options, and identify underlying issues.
- Be curious. Challenge assumptions by asking questions to ensure current care methods are valid, relevant, and supported by evidence-based practice .
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills.
Images sourced from Getty Images
Related Resources

Item(s) added to cart
- Research article
- Open access
- Published: 07 October 2020
Impact of social problem-solving training on critical thinking and decision making of nursing students
- Soleiman Ahmady 1 &
- Sara Shahbazi ORCID: orcid.org/0000-0001-8397-6233 2 , 3
BMC Nursing volume 19 , Article number: 94 ( 2020 ) Cite this article
31k Accesses
28 Citations
1 Altmetric
Metrics details
The complex health system and challenging patient care environment require experienced nurses, especially those with high cognitive skills such as problem-solving, decision- making and critical thinking. Therefore, this study investigated the impact of social problem-solving training on nursing students’ critical thinking and decision-making.
This study was quasi-experimental research and pre-test and post-test design and performed on 40 undergraduate/four-year students of nursing in Borujen Nursing School/Iran that was randomly divided into 2 groups; experimental ( n = 20) and control (n = 20). Then, a social problem-solving course was held for the experimental group. A demographic questionnaire, social problem-solving inventory-revised, California critical thinking test, and decision-making questionnaire was used to collect the information. The reliability and validity of all of them were confirmed. Data analysis was performed using SPSS software and independent sampled T-test, paired T-test, square chi, and Pearson correlation coefficient.
The finding indicated that the social problem-solving course positively affected the student’ social problem-solving and decision-making and critical thinking skills after the instructional course in the experimental group ( P < 0.05), but this result was not observed in the control group ( P > 0.05).
Conclusions
The results showed that structured social problem-solving training could improve cognitive problem-solving, critical thinking, and decision-making skills. Considering this result, nursing education should be presented using new strategies and creative and different ways from traditional education methods. Cognitive skills training should be integrated in the nursing curriculum. Therefore, training cognitive skills such as problem- solving to nursing students is recommended.
Peer Review reports
Continuous monitoring and providing high-quality care to patients is one of the main tasks of nurses. Nurses’ roles are diverse and include care, educational, supportive, and interventional roles when dealing with patients’ clinical problems [ 1 , 2 ].
Providing professional nursing services requires the cognitive skills such as problem-solving, decision-making and critical thinking, and information synthesis [ 3 ].
Problem-solving is an essential skill in nursing. Improving this skill is very important for nurses because it is an intellectual process which requires the reflection and creative thinking [ 4 ].
Problem-solving skill means acquiring knowledge to reach a solution, and a person’s ability to use this knowledge to find a solution requires critical thinking. The promotion of these skills is considered a necessary condition for nurses’ performance in the nursing profession [ 5 , 6 ].
Managing the complexities and challenges of health systems requires competent nurses with high levels of critical thinking skills. A nurse’s critical thinking skills can affect patient safety because it enables nurses to correctly diagnose the patient’s initial problem and take the right action for the right reason [ 4 , 7 , 8 ].
Problem-solving and decision-making are complex and difficult processes for nurses, because they have to care for multiple patients with different problems in complex and unpredictable treatment environments [ 9 , 10 ].
Clinical decision making is an important element of professional nursing care; nurses’ ability to form effective clinical decisions is the most significant issue affecting the care standard. Nurses build 2 kinds of choices associated with the practice: patient care decisions that affect direct patient care and occupational decisions that affect the work context or teams [ 11 , 12 , 13 , 14 , 15 , 16 ].
The utilization of nursing process guarantees the provision of professional and effective care. The nursing process provides nurses with the chance to learn problem-solving skills through teamwork, health management, and patient care. Problem-solving is at the heart of nursing process which is why this skill underlies all nursing practices. Therefore, proper training of this skill in an undergraduate nursing program is essential [ 17 ].
Nursing students face unique problems which are specific to the clinical and therapeutic environment, causing a lot of stresses during clinical education. This stress can affect their problem- solving skills [ 18 , 19 , 20 , 21 ]. They need to promote their problem-solving and critical thinking skills to meet the complex needs of current healthcare settings and should be able to respond to changing circumstances and apply knowledge and skills in different clinical situations [ 22 ]. Institutions should provide this important opportunity for them.
Despite, the results of studies in nursing students show the weakness of their problem-solving skills, while in complex health environments and exposure to emerging diseases, nurses need to diagnose problems and solve them rapidly accurately. The teaching of these skills should begin in college and continue in health care environments [ 5 , 23 , 24 ].
It should not be forgotten that in addition to the problems caused by the patients’ disease, a large proportion of the problems facing nurses are related to the procedures of the natural life of their patients and their families, the majority of nurses with the rest of health team and the various roles defined for nurses [ 25 ].
Therefore, in addition to above- mentioned issues, other ability is required to deal with common problems in the working environment for nurses, the skill is “social problem solving”, because the term social problem-solving includes a method of problem-solving in the “natural context” or the “real world” [ 26 , 27 ]. In reviewing the existing research literature on the competencies and skills required by nursing students, what attracts a lot of attention is the weakness of basic skills and the lack of formal and systematic training of these skills in the nursing curriculum, it indicates a gap in this area [ 5 , 24 , 25 ]. In this regard, the researchers tried to reduce this significant gap by holding a formal problem-solving skills training course, emphasizing the common social issues in the real world of work. Therefore, this study was conducted to investigate the impact of social problem-solving skills training on nursing students’ critical thinking and decision-making.
Setting and sample
This quasi-experimental study with pretest and post-test design was performed on 40 undergraduate/four-year nursing students in Borujen nursing school in Shahrekord University of Medical Sciences. The periods of data collection were 4 months.
According to the fact that senior students of nursing have passed clinical training and internship programs, they have more familiarity with wards and treatment areas, patients and issues in treatment areas and also they have faced the problems which the nurses have with other health team personnel and patients and their families, they have been chosen for this study. Therefore, this study’s sampling method was based on the purpose, and the sample size was equal to the total population. The whole of four-year nursing students participated in this study and the sample size was 40 members. Participants was randomly divided in 2 groups; experimental ( n = 20) and control (n = 20).
The inclusion criteria to take part in the present research were students’ willingness to take part, studying in the four-year nursing, not having the record of psychological sickness or using the related drugs (all based on their self-utterance).
Intervention
At the beginning of study, all students completed the demographic information’ questionnaire. The study’s intervening variables were controlled between the two groups [such as age, marital status, work experience, training courses, psychological illness, psychiatric medication use and improving cognitive skills courses (critical thinking, problem- solving, and decision making in the last 6 months)]. Both groups were homogeneous in terms of demographic variables ( P > 0.05). Decision making and critical thinking skills and social problem solving of participants in 2 groups was evaluated before and 1 month after the intervention.
All questionnaires were anonymous and had an identification code which carefully distributed by the researcher.
To control the transfer of information among the students of two groups, the classification list of students for internships, provided by the head of nursing department at the beginning of semester, was used.
Furthermore, the groups with the odd number of experimental group and the groups with the even number formed the control group and thus were less in contact with each other.
The importance of not transferring information among groups was fully described to the experimental group. They were asked not to provide any information about the course to the students of the control group.
Then, training a course of social problem-solving skills for the experimental group, given in a separate course and the period from the nursing curriculum and was held in 8 sessions during 2 months, using small group discussion, brainstorming, case-based discussion, and reaching the solution in small 4 member groups, taking results of the social problem-solving model as mentioned by D-zurilla and gold fried [ 26 ]. The instructor was an assistant professor of university and had a history of teaching problem-solving courses. This model’ stages are explained in Table 1 .
All training sessions were performed due to the model, and one step of the model was implemented in each session. In each session, the teacher stated the educational objectives and asked the students to share their experiences in dealing to various workplace problems, home and community due to the topic of session. Besides, in each session, a case-based scenario was presented and thoroughly analyzed, and students discussed it.
Instruments
In this study, the data were collected using demographic variables questionnaire and social problem- solving inventory – revised (SPSI-R) developed by D’zurilla and Nezu (2002) [ 26 ], California critical thinking skills test- form B (CCTST; 1994) [ 27 , 28 ] and decision-making questionnaire.
SPSI-R is a self - reporting tool with 52 questions ranging from a Likert scale (1: Absolutely not – 5: very much).
The minimum score maybe 25 and at a maximum of 125, therefore:
The score 25 and 50: weak social problem-solving skills.
The score 50–75: moderate social problem-solving skills.
The score higher of 75: strong social problem-solving skills.
The reliability assessed by repeated tests is between 0.68 and 0.91, and its alpha coefficient between 0.69 and 0.95 was reported [ 26 ]. The structural validity of questionnaire has also been confirmed. All validity analyses have confirmed SPSI as a social problem - solving scale.
In Iran, the alpha coefficient of 0.85 is measured for five factors, and the retest reliability coefficient was obtained 0.88. All of the narratives analyzes confirmed SPSI as a social problem- solving scale [ 29 ].
California critical thinking skills test- form B(CCTST; 1994): This test is a standard tool for assessing the basic skills of critical thinking at the high school and higher education levels (Facione & Facione, 1992, 1998) [ 27 ].
This tool has 34 multiple-choice questions which assessed analysis, inference, and argument evaluation. Facione and Facione (1993) reported that a KR-20 range of 0.65 to 0.75 for this tool is acceptable [ 27 ].
In Iran, the KR-20 for the total scale was 0.62. This coefficient is acceptable for questionnaires that measure the level of thinking ability of individuals.
After changing the English names of this questionnaire to Persian, its content validity was approved by the Board of Experts.
The subscale analysis of Persian version of CCTST showed a positive high level of correlation between total test score and the components (analysis, r = 0.61; evaluation, r = 0.71; inference, r = 0.88; inductive reasoning, r = 0.73; and deductive reasoning, r = 0.74) [ 28 ].
A decision-making questionnaire with 20 questions was used to measure decision-making skills. This questionnaire was made by a researcher and was prepared under the supervision of a professor with psychometric expertise. Five professors confirmed the face and content validity of this questionnaire. The reliability was obtained at 0.87 which confirmed for 30 students using the test-retest method at a time interval of 2 weeks. Each question had four levels and a score from 0.25 to 1. The minimum score of this questionnaire was 5, and the maximum score was 20 [ 30 ].
Statistical analysis
For analyzing the applied data, the SPSS Version 16, and descriptive statistics tests, independent sample T-test, paired T-test, Pearson correlation coefficient, and square chi were used. The significant level was taken P < 0.05.
The average age of students was 21.7 ± 1.34, and the academic average total score was 16.32 ± 2.83. Other demographic characteristics are presented in Table 2 .
None of the students had a history of psychiatric illness or psychiatric drug use. Findings obtained from the chi-square test showed that there is not any significant difference between the two groups statistically in terms of demographic variables.
The mean scores in social decision making, critical thinking, and decision-making in whole samples before intervention showed no significant difference between the two groups statistically ( P > 0.05), but showed a significant difference after the intervention ( P < 0.05) (Table 3 ).
Scores in Table 4 showed a significant positive difference before and after intervention in the “experimental” group ( P < 0.05), but this difference was not seen in the control group ( P > 0.05).
Among the demographic variables, only a positive relationship was seen between marital status and decision-making skills (r = 0.72, P < 0.05).
Also, the scores of critical thinking skill’ subgroups and social problem solving’ subgroups are presented in Tables 5 and 6 which showed a significant positive difference before and after intervention in the “experimental” group (P < 0.05), but this difference was not seen in the control group ( P > 0.05).
In the present study conducted by some studies, problem-solving and critical thinking and decision-making scores of nursing students are moderate [ 5 , 24 , 31 ].
The results showed that problem-solving skills, critical thinking, and decision-making in nursing students were promoted through a social problem-solving training course. Unfortunately, no study has examined the effect of teaching social problem-solving skills on nursing students’ critical thinking and decision-making skills.
Altun (2018) believes that if the values of truth and human dignity are promoted in students, it will help them acquire problem-solving skills. Free discussion between students and faculty on value topics can lead to the development of students’ information processing in values. Developing self-awareness increases students’ impartiality and problem-solving ability [ 5 ]. The results of this study are consistent to the results of present study.
Erozkan (2017), in his study, reported there is a significant relationship between social problem solving and social self-efficacy and the sub-dimensions of social problem solving [ 32 ]. In the present study, social problem -solving skills training has improved problem -solving skills and its subdivisions.
The results of study by Moshirabadi (2015) showed that the mean score of total problem-solving skills was 89.52 ± 21.58 and this average was lower in fourth-year students than other students. He explained that education should improve students’ problem-solving skills. Because nursing students with advanced problem-solving skills are vital to today’s evolving society [ 22 ]. In the present study, the results showed students’ weakness in the skills in question, and holding a social problem-solving skills training course could increase the level of these skills.
Çinar (2010) reported midwives and nurses are expected to use problem-solving strategies and effective decision-making in their work, using rich basic knowledge.
These skills should be developed throughout one’s profession. The results of this study showed that academic education could increase problem-solving skills of nursing and midwifery students, and final year students have higher skill levels [ 23 ].
Bayani (2012) reported that the ability to solve social problems has a determining role in mental health. Problem-solving training can lead to a level upgrade of mental health and quality of life [ 33 ]; These results agree with the results obtained in our study.
Conducted by this study, Kocoglu (2016) reported nurses’ understanding of their problem-solving skills is moderate. Receiving advice and support from qualified nursing managers and educators can enhance this skill and positively impact their behavior [ 31 ].
Kashaninia (2015), in her study, reported teaching critical thinking skills can promote critical thinking and the application of rational decision-making styles by nurses.
One of the main components of sound performance in nursing is nurses’ ability to process information and make good decisions; these abilities themselves require critical thinking. Therefore, universities should envisage educational and supportive programs emphasizing critical thinking to cultivate their students’ professional competencies, decision-making, problem-solving, and self-efficacy [ 34 ].
The study results of Kirmizi (2015) also showed a moderate positive relationship between critical thinking and problem-solving skills [ 35 ].
Hong (2015) reported that using continuing PBL training promotes reflection and critical thinking in clinical nurses. Applying brainstorming in PBL increases the motivation to participate collaboratively and encourages teamwork. Learners become familiar with different perspectives on patients’ problems and gain a more comprehensive understanding. Achieving these competencies is the basis of clinical decision-making in nursing. The dynamic and ongoing involvement of clinical staff can bridge the gap between theory and practice [ 36 ].
Ancel (2016) emphasizes that structured and managed problem-solving training can increase students’ confidence in applying problem-solving skills and help them achieve self-confidence. He reported that nursing students want to be taught in more innovative ways than traditional teaching methods which cognitive skills training should be included in their curriculum. To this end, university faculties and lecturers should believe in the importance of strategies used in teaching and the richness of educational content offered to students [ 17 ].
The results of these recent studies are adjusted with the finding of recent research and emphasize the importance of structured teaching cognitive skills to nurses and nursing students.
Based on the results of this study on improving critical thinking and decision-making skills in the intervention group, researchers guess the reasons to achieve the results of study in the following cases:
In nursing internationally, problem-solving skills (PS) have been introduced as a key strategy for better patient care [ 17 ]. Problem-solving can be defined as a self-oriented cognitive-behavioral process used to identify or discover effective solutions to a special problem in everyday life. In particular, the application of this cognitive-behavioral methodology identifies a wide range of possible effective solutions to a particular problem and enhancement the likelihood of selecting the most effective solution from among the various options [ 27 ].
In social problem-solving theory, there is a difference among the concepts of problem-solving and solution implementation, because the concepts of these two processes are different, and in practice, they require different skills.
In the problem-solving process, we seek to find solutions to specific problems, while in the implementation of solution, the process of implementing those solutions in the real problematic situation is considered [ 25 , 26 ].
The use of D’zurilla and Goldfride’s social problem-solving model was effective in achieving the study results because of its theoretical foundations and the usage of the principles of cognitive reinforcement skills. Social problem solving is considered an intellectual, logical, effort-based, and deliberate activity [ 26 , 32 ]; therefore, using this model can also affect other skills that need recognition.
In this study, problem-solving training from case studies and group discussion methods, brainstorming, and activity in small groups, was used.
There are significant educational achievements in using small- group learning strategies. The limited number of learners in each group increases the interaction between learners, instructors, and content. In this way, the teacher will be able to predict activities and apply techniques that will lead students to achieve high cognitive taxonomy levels. That is, confront students with assignments and activities that force them to use cognitive processes such as analysis, reasoning, evaluation, and criticism.
In small groups, students are given the opportunity to the enquiry, discuss differences of opinion, and come up with solutions. This method creates a comprehensive understanding of the subject for the student [ 36 ].
According to the results, social problem solving increases the nurses’ decision-making ability and critical thinking regarding identifying the patient’s needs and choosing the best nursing procedures. According to what was discussed, the implementation of this intervention in larger groups and in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students, in the future, is recommended.
Social problem- solving training by affecting critical thinking skills and decision-making of nursing students increases patient safety. It improves the quality of care because patients’ needs are better identified and analyzed, and the best solutions are adopted to solve the problem.
In the end, the implementation of this intervention in larger groups in different levels of education by teaching other cognitive skills and examining their impact on other cognitive skills of nursing students in the future is recommended.
Study limitations
This study was performed on fourth-year nursing students, but the students of other levels should be studied during a cohort from the beginning to the end of course to monitor the cognitive skills improvement.
The promotion of high-level cognitive skills is one of the main goals of higher education. It is very necessary to adopt appropriate approaches to improve the level of thinking. According to this study results, the teachers and planners are expected to use effective approaches and models such as D’zurilla and Goldfride social problem solving to improve problem-solving, critical thinking, and decision-making skills. What has been confirmed in this study is that the routine training in the control group should, as it should, has not been able to improve the students’ critical thinking skills, and the traditional educational system needs to be transformed and reviewed to achieve this goal.
Availability of data and materials
The datasets used and analyzed during the present study are available from the corresponding author on reasonable request.
Abbreviations
California critical thinking skills test
Social problem-solving inventory – revised
Pesudovs L. Medical/surgical nursing in the home. Aust Nurs Midwifery J. 2014;22(3):24.
PubMed Google Scholar
Szeri C, et al. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4).
Friese CR, et al. Pod nursing on a medical/surgical unit: implementation and outcomes evaluation. J Nurs Adm. 2014;44(4):207–11.
Article Google Scholar
Lyneham J. A conceptual model for medical-surgical nursing: moving toward an international clinical specialty. Medsurg Nurs. 2013;22(4):215–20 263.
Altun I. The perceived problem solving ability and values of student nurses and midwives. Nurse Educ Today. 2003;23(8):575–84.
Deniz Kocoglu R, et al. Problem solving training for first line nurse managers. Int J Caring Sci. 2016;9(3):955.
Google Scholar
Mahoney C, et al. Implementing an 'arts in nursing' program on a medical-surgical unit. Medsurg Nurs. 2011;20(5):273–4.
Pardue SF. Decision-making skills and critical thinking ability among associate degree, diploma, baccalaureate, and master's-prepared nurses. J Nurs Educ. 1987;26(9):354–61.
Article CAS Google Scholar
Kozlowski D, et al. The role of emotion in clinical decision making: an integrative literature review. BMC Med Educ. 2017;17(1):255.
Kuiper RA, Pesut DJ. Promoting cognitive and metacognitive reflective reasoning skills in nursing practice: self-regulated learning theory. J Adv Nurs. 2004;45(4):381–91.
Huitzi-Egilegor JX, et al. Implementation of the nursing process in a health area: models and assessment structures used. Rev Lat Am Enfermagem. 2014;22(5):772–7.
Lauri S. Development of the nursing process through action research. J Adv Nurs. 1982;7(4):301–7.
Muller-Staub M, de Graaf-Waar H, Paans W. An internationally consented standard for nursing process-clinical decision support Systems in Electronic Health Records. Comput Inform Nurs. 2016;34(11):493–502.
Neville K, Roan N. Challenges in nursing practice: nurses' perceptions in caring for hospitalized medical-surgical patients with substance abuse/dependence. J Nurs Adm. 2014;44(6):339–46.
Rabelo-Silva ER, et al. Advanced nursing process quality: comparing the international classification for nursing practice (ICNP) with the NANDA-international (NANDA-I) and nursing interventions classification (NIC). J Clin Nurs. 2017;26(3–4):379–87.
Varcoe C. Disparagement of the nursing process: the new dogma? J Adv Nurs. 1996;23(1):120–5.
Ancel G. Problem-solving training: effects on the problem-solving skills and self-efficacy of nursing students. Eurasian J Educ Res. 2016;64:231–46.
Fang J, et al. Social problem-solving in Chinese baccalaureate nursing students. J Evid Based Med. 2016;9(4):181–7.
Kanbay Y, Okanli A. The effect of critical thinking education on nursing students' problem-solving skills. Contemp Nurse. 2017;53(3):313–21.
Lau Y. Factors affecting the social problem-solving ability of baccalaureate nursing students. Nurse Educ Today. 2014;34(1):121–6.
Terzioglu F. The perceived problem-solving ability of nurse managers. J Nurs Manag. 2006;14(5):340–7.
Moshirabadi, Z., et al., The perceived problem solving skill of Iranian nursing students . 2015.
Cinar N. Problem solving skills of the nursing and midwifery students and influential factors. Revista Eletrônica de Enfermagem. 2010;12(4):601–6.
Moattari M, et al. Clinical concept mapping: does it improve discipline-based critical thinking of nursing students? Iran J Nurs Midwifery Res. 2014;19(1):70–6.
PubMed PubMed Central Google Scholar
Elliott TR, Grant JS, Miller DM. Social Problem-Solving Abilities and Behavioral Health. In Chang EC, D'Zurilla TJ, Sanna LJ, editors. Social problem solving: Theory, research, and training. American Psychological Association; 2004. p. 117–33.
D'Zurilla TJ, Maydeu-Olivares A. Conceptual and methodological issues in social problem-solving assessment. Behav Ther. 1995;26(3):409–32.
Facione PA. The California Critical Thinking Skills Test--College Level. Technical Report# 1. Experimental Validation and Content Validity; 1990.
Khalili H, Zadeh MH. Investigation of reliability, validity and normality Persian version of the California Critical Thinking Skills Test; Form B (CCTST). J Med Educ. 2003;3(1).
Mokhberi A. Questionnaire, psychometrics, and standardization of indicators of social problem solving ability. Educ Measurement. 2011;1(4):1–21.
Heidari M, Shahbazi S. Effect of training problem-solving skill on decision-making and critical thinking of personnel at medical emergencies. Int J Crit Illn Inj Sci. 2016;6(4):182–7.
Kocoglu D, Duygulu S, Abaan S, Akin B. Problem Solving Training for First Line Nurse Managers. Int J Caring Sci. 2016;9(13):955–65.
Erozkan A. Analysis of social problem solving and social self-efficacy in prospective teachers. Educational Sciences: Theory and Practice. 2014;14(2):447–55.
Bayani AA, Ranjbar M, Bayani A. The study of relationship between social problem-solving and depression and social phobia among students. J Mazandaran Univ Med Sci. 2012;22(94):91–8.
Kashaninia Z, et al. The effect of teaching critical thinking skills on the decision making style of nursing managers. J Client-Centered Nurs Care. 2015;1(4):197–204.
Kirmizi FS, Saygi C, Yurdakal IH. Determine the relationship between the disposition of critical thinking and the perception about problem solving skills. Procedia Soc Behav Sci. 2015;191:657–61.
Hung CH, Lin CY. Using concept mapping to evaluate knowledge structure in problem-based learning. BMC Med Educ. 2015;15:212.
Download references
Acknowledgments
This article results from research project No. 980 approved by the Research and Technology Department of Shahrekord University of Medical Sciences. We would like to appreciate to all personnel and students of the Borujen Nursing School. The efforts of all those who assisted us throughout this research.
‘Not applicable.
Author information
Authors and affiliations.
Department of Medical Education, Virtual School of Medical Education and Management, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Soleiman Ahmady
Virtual School of Medical Education and management, Shahid Beheshty University of Medical Sciences, Tehran, Iran
Sara Shahbazi
Community-Oriented Nursing Midwifery Research Center, Shahrekord University of Medical Sciences, Shahrekord, Iran
You can also search for this author in PubMed Google Scholar
Contributions
SA and SSH conceptualized the study, developed the proposal, coordinated the project, completed initial data entry and analysis, and wrote the report. SSH conducted the statistical analyses. SA and SSH assisted in writing and editing the final report. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sara Shahbazi .
Ethics declarations
Ethics approval and consent to participate.
This study was reviewed and given exempt status by the Institutional Review Board of the research and technology department of Shahrekord University of Medical Sciences (IRB No. 08–2017-109). Before the survey, students completed a research consent form and were assured that their information would remain confidential. After the end of the study, a training course for the control group students was held.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ahmady, S., Shahbazi, S. Impact of social problem-solving training on critical thinking and decision making of nursing students. BMC Nurs 19 , 94 (2020). https://doi.org/10.1186/s12912-020-00487-x
Download citation
Received : 11 March 2020
Accepted : 29 September 2020
Published : 07 October 2020
DOI : https://doi.org/10.1186/s12912-020-00487-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Social problem solving
- Decision making
- Critical thinking
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Nurse leaders as problem-solvers
Addressing lateral and horizontal violence.
Anthony, Michelle R. PhD, RN; Brett, Anne Liners PhD, RN
Michelle R. Anthony is a program coordinator at Columbia (S.C.) VA Health Care System. Anne Liners Brett is doctoral faculty at the University of Phoenix in Tempe, Ariz.
Acknowledgment: The authors acknowledge the support of the University of Phoenix Center for Educational and Instructional Technology Research.
The contents of this article do not represent the views of the US Department of Veterans Affairs or the United States Government.
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
For more than 126 additional continuing-education articles related to management topics, go to NursingCenter.com/CE .
Earn CE credit online: Go to http://nursing.ceconnection.com and receive a certificate within minutes .
Read about a qualitative, grounded theory study that looked to gain a deeper understanding of nurse leaders' perceptions of their role in addressing lateral and horizontal violence, and the substantive theory developed from the results.

The issue of lateral and horizontal violence (LHV) has plagued the nursing profession for more than 3 decades, yet solutions remain elusive. The significance of LHV isn't lost on nurse leaders because it creates an unhealthy work environment. Research literature worldwide has continued to report the prevalence of disruptive behaviors experienced by nursing students, novice nurses, and seasoned nurses in the workforce. The World Health Organization, International Council of Nurses, and Public Services International have recognized this issue as a major global public health priority. 1
LHV, also called nurse-on-nurse aggression, disruptive behavior, or incivility, undermines a culture of safety and negatively impacts patient care. 2,3 This experience, known to nurses as “eating their young,” isn't only intimidating and disruptive, it's also costly and demoralizing to the nursing profession and healthcare organizations. 4,5 Although the impact of LHV can be dreadful for both the institution and its staff, little is known about the reasons for these behaviors among nursing professionals. 2
LHV encompasses all acts of meanness, hostility, disruption, discourtesy, backbiting, divisiveness, criticism, lack of unison, verbal or mental abuse, and scapegoating. 6 The sole intent of bullying behaviors is to purposefully humiliate and demean victims. Bullying behaviors also taint healthcare organizations; cause irreparable harm to workplace culture; breakdown team communication; and severely impact the quality of the care provided, thereby jeopardizing patient safety. 7,8 Researchers have reported that acts of LHV are used to demonstrate power, domination, or aggression; for retribution; to control others; and to enhance self-image. 9-12
Previous studies have shown that the frequency of LHV in healthcare organizations is quite severe, with about 90% of new nurses surveyed reporting acts of incivility by their coworkers. 13 Sixty-five percent of nurses in one survey reported witnessing incidents of despicable acts, whereas another 46% of coworkers in the same survey reported the issue as “very serious” and “somewhat serious.” 13
LHV poses a significant challenge for nurse leaders who are legally and morally responsible for providing a safe working environment. 2,6 The purpose of this qualitative, grounded theory study was to gain a deeper understanding of nurse leaders' perceptions of their role in addressing LHV and develop a substantive theory from the results.
Literature review
A paucity of evidence exists in the literature regarding how nurse leaders perceive their role in addressing LHV. 14 Studies have shown that this phenomenon is attributed to heavy workloads, a stressful work environment, and lack of workgroup cohesiveness, as well as organizational factors such as misuse of authority and the lack of organizational policies and procedures for addressing LHV behaviors. 15
In one study, one-third of the nurses reported that they had observed emotional abuse during several of their work shifts. 16 Another study indicated that 30% of survey respondents (n = 2,100) stated LHV occurs weekly. 17 A third study revealed that 25% of participants noted LHV happened monthly, and a fourth study of ED nurses reported that about 27.3% of the nurses had experienced LHV perpetrated by nursing leadership (managers, supervisors, charge nurses, and directors), physicians, or peers in the last 6 months. 18
In a survey completed by members of the Washington State Emergency Nurses Association, 27% of respondents experienced acts of bullying in the past 6 months. 19 Another study reported that 27% to 85% of nurse respondents had experienced some form of uncivil behavior. 20 Other data have shown that those more vulnerable to violent, disruptive, and intimidating behaviors are newly licensed nurses beginning their careers. 21
Although nurse leaders can be perpetrators of LHV, they play an essential role in addressing LHV behaviors and creating a safe work environment. 22 The literature suggests that, in many cases, a lack of awareness and response by nurse leaders adds to the prevalence of LHV. 23 This may be due, in part, to nurse leaders being aligned with the perpetrators who are creating the toxic work environment. 6 The literature suggests that an environment where staff members feel safe to practice results in a culture that decreases burnout and promotes nurse retention and quality outcomes. 24,25
This qualitative, grounded theory study focused on nurse leaders' perception of their role in breaking the cycle of LHV for staff members whom they supervise. Two research questions guided the study: 1. How do nurse leaders perceive their role in addressing LHV among nursing staff members under their supervision? 2. What substantive theory may emerge from the data collected during interviews with nurse leaders?
A grounded theory methodology was used to explore the nurse leader's role in addressing LHV with the intent of developing a substantive theory through the meaningful organization of data themes to provide a framework to address the phenomenon of LHV. Purposive sampling was used to recruit a total of 14 participants for this study from a large healthcare system in the Southeastern US. The participants were chosen because of their experience with LHV and their ability to discuss and reflect on those experiences. Informed consent was obtained before the start of the study, which included explaining the reason for the study and what to expect. In addition, permission was obtained from the Institutional Review Board.
Data collection and analysis
Demographic data collected to describe the sample included gender, age range, number of years holding a management position, supervisory responsibility, and highest degree obtained. (See Table 1 .)

Semistructured, in-depth interviews were the primary mode of data collection. The recorded interviews were conducted face-to-face and lasted about 60 minutes. Data collection continued until saturation was achieved. Data saturation occurred when no new descriptive codes, categories, or themes were emerging from the analyzed data. The interviews were transcribed verbatim and verified through a member check process.
During the data analysis process, themes and patterns were identified. Data from each participant's interview were examined to determine if the responses were aligned with the identified themes. Analysis of the data included coding at increasingly abstract levels and constant comparison. Qualitative software assisted in coding the information and uncovering subtle trends.
Four themes emerged from core categories developed during the qualitative data coding process.
Theme 1: Understanding/addressing LHV . In question one, participants were asked to describe their understanding of LHV. Five subthemes emerged from the data collected with this question. (See Table 2 .)

Theme 2: Experience addressing LHV . In the second question, participants were asked about their experience with addressing incidents of LHV. Six subthemes were identified. (See Table 3 .)

Theme 3: Role perception in addressing LHV . In the third question, participants were asked what they perceive their role to be in addressing LHV. Six subthemes resulted from this question. (See Table 4 .)

Theme 4: Organizational impediment to addressing LHV . In question four, participants were asked to describe the factors within the organization that influence or impede their role in addressing LHV. This question yielded nine subthemes. (See Table 5 .)

Substantive theory
As a result of the themes that emerged from the data, a substantive theory was developed. This is especially important for the nursing profession to develop as a scientifically based practice. Theories help guide research and provide the expansion, generation, and validation of the science of nursing knowledge. 26 The substantive theory will help nurse leaders become more cognizant of the role that effective leadership plays in preventing or intervening in incidents of LHV in the workplace. The analysis revealed that nurse leaders are aware that the quality of patient care and staff well-being can be adversely affected by the impact of LHV.
Data themes were used to formulate the following theory: Nurse leaders address LHV affecting their staff members by solving problems, creating a safe work environment, and reducing institutional barriers that impede addressing LHV in a timely fashion. Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28
The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment. Figure 1 shows the interrelatedness of the themes to the resultant substantive theory.


Discussion and implications
The study results have several implications for both the nursing profession and nurse leaders. The nursing profession requires decisive and robust leadership, and the role of the nurse leader is to be a combination of nurturer, investigator, and judge to examine incidents of LHV. 26,29-32 Nurse leaders are responsible for setting the tone and expectations for a safe work environment. This includes modeling the expected ethical behaviors; for example, doing the right things for the right reasons, being collegial toward each other, and being respectful of other's differences. One participant remarked, “This is a different world based on how I was raised. I was raised to be respectful to people.”
In addition, nurse leaders are responsible for enforcing policies created to address disruptive behaviors and working with the administration as soon as an incident occurs. Past research indicates that a healthy and collaborative work environment fosters nurse engagement and patient safety. 25,30 Staff members and patients need a leader to protect them when necessary; thus, the nurse leader needs to “walk the walk” in providing a safe environment for all. Nurse leaders engaged in these kinds of behaviors are providing strong leadership and practicing strong decision-making, thus ensuring the continued robustness of their organizations.
Recommendations and limitations
Future research could replicate this study in a different geographic region to explore the causes of LHV by soliciting the views of nursing students, new graduate nurses, and nurse educators from unionized and nonunionized hospital systems and comparing the results to further understand this phenomenon. Additionally, developing a tool to test the substantive theory could substantiate the nurse leader's role as a problem-solver to address incidence of LHV in the workplace.
The decision to conduct this study in one type of healthcare organization limits the ability to compare the interviewed nurse leaders' experiences with nurse leaders in other healthcare organizations. The experiences of nurses in other healthcare organizations may be different; thus, overall generalizability of the study may be limited.
Say “no” to the status quo
The results of this study support the findings of previous researchers. 23,31,33,34 Accepting the status quo is unacceptable and can cause irreparable harm to organizational well-being if LHV isn't addressed. Collaboration between nurse leaders and administrators is essential to successfully reduce institutional obstacles that prevent the timely handling of LHV incidents. The role of the nurse leader as a problem-solver should be clear, defined, and well supported to seek resolutions to toxic behaviors that are hurting the work environment. But we must remember that creating a policy doesn't equal change. Every employee from the lowest level in the organization to the highest ranks of administration must model civil behaviors.
INSTRUCTIONS Nurse leaders as problem-solvers: Addressing lateral and horizontal violence
Test instructions.
- Read the article. The test for this CE activity is to be taken online at http://nursing.ceconnection.com .
- You'll need to create (it's free!) and login to your personal CE Planner account before taking online tests. Your planner will keep track of all your Lippincott Professional Development online CE activities for you.
- There's only one correct answer for each question. A passing score for this test is 14 correct answers. If you pass, you can print your certificate of earned contact hours and access the answer key. If you fail, you have the option of taking the test again at no additional cost.
- For questions, contact Lippincott Professional Development: 1-800-787-8985 .
- Registration deadline is June 3, 2022 .
PROVIDER ACCREDITATION
Lippincott Professional Development will award 1.5 contact hours for this continuing nursing education activity.
Lippincott Professional Development is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center's Commission on Accreditation.
This activity is also provider approved by the California Board of Registered Nursing, Provider Number CEP 11749 for 1.5 contact hours, and the District of Columbia, Georgia, and Florida CE Broker #50-1223.
Payment: The registration fee for this test is $17.95.
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Leadership strategies to promote frontline nursing staff engagement, nurse leader competencies: a toolkit for success, keeping the peace: conflict management strategies for nurse managers, principles for sustaining shared/professional governance in nursing, workplace incivility: nurse leaders as change agents.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Management and Professional Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022.

Nursing Management and Professional Concepts [Internet].
- About Open RN
Chapter 6 – Ethical Practice
6.1. ethical practice introduction, learning objectives.
• Recognize ethical dilemmas and take appropriate action
• Practice in a manner consistent with a code of ethics for nurses
• Compare and contrast theories of ethical decision-making
• Examine resources to resolve ethical dilemmas
• Examine competent practice within the legal/ethical/regulatory framework of health care
• Defend the course of action or give a rationale for the action
• Apply the ANA Code of Ethics to diverse situations in health care
• Analyze the impact of cultural diversity in ethical decision-making
• Identify advocacy as part of the nursing role when responding to ethical dilemmas
The nursing profession is guided by a code of ethics. As you practice nursing, how will you determine “right” from “wrong” actions? What is the difference between morality, values, and ethical principles? What additional considerations impact your ethical decision-making? What are ethical dilemmas and how should nurses participate in resolving them? This chapter answers these questions by reviewing concepts related to ethical nursing practice and describing how nurses can resolve ethical dilemmas. By the end of this chapter, you will be able to describe how to make ethical decisions using the Code of Ethics established by the American Nurses Association.
6.2. BASIC ETHICAL CONCEPTS
The American Nurses Association (ANA) defines morality as “personal values, character, or conduct of individuals or groups within communities and societies,” whereas ethics is the formal study of morality from a wide range of perspectives.[ 1 ] Ethical behavior is considered to be such an important aspect of nursing the ANA has designated Ethics as the first Standard of Professional Performance. The ANA Standards of Professional Performance are “authoritative statements of the actions and behaviors that all registered nurses, regardless of role, population, specialty, and setting, are expected to perform competently.” See the following box for the competencies associated with the ANA Ethics Standard of Professional Performance[ 2 ]:
Competencies of ANA’s Ethics Standard of Professional Performance[ 3 ]
• Uses the Code of Ethics for Nurses with Interpretive Statements as a moral foundation to guide nursing practice and decision-making.
• Demonstrates that every person is worthy of nursing care through the provision of respectful, person-centered, compassionate care, regardless of personal history or characteristics (Beneficence).
• Advocates for health care consumer perspectives, preferences, and rights to informed decision-making and self-determination (Respect for autonomy).
• Demonstrates a primary commitment to the recipients of nursing and health care services in all settings and situations (Fidelity).
• Maintains therapeutic relationships and professional boundaries.
• Safeguards sensitive information within ethical, legal, and regulatory parameters (Nonmaleficence).
• Identifies ethics resources within the practice setting to assist and collaborate in addressing ethical issues.
• Integrates principles of social justice in all aspects of nursing practice (Justice).
• Refines ethical competence through continued professional education and personal self-development activities.
• Depicts one’s professional nursing identity through demonstrated values and ethics, knowledge, leadership, and professional comportment.
• Engages in self-care and self-reflection practices to support and preserve personal health, well-being, and integrity.
• Contributes to the establishment and maintenance of an ethical environment that is conducive to safe, quality health care.
• Collaborates with other health professionals and the public to protect human rights, promote health diplomacy, enhance cultural sensitivity and congruence, and reduce health disparities.
• Represents the nursing perspective in clinic, institutional, community, or professional association ethics discussions.
Reflective Questions
1. What Ethics competencies have you already demonstrated during your nursing education?
2. What Ethics competencies are you most interested in mastering?
3. What questions do you have about the ANA’s Ethics competencies?
The ANA’s Code of Ethics for Nurses with Interpretive Statements is an ethical standard that guides nursing practice and ethical decision-making.[ 4 ] This section will review several basic ethical concepts related to the ANA’s Ethics Standard of Professional Performance, such as values, morals, ethical theories, ethical principles, and the ANA Code of Ethics for Nurses .
Values are individual beliefs that motivate people to act one way or another and serve as guides for behavior considered “right” and “wrong.” People tend to adopt the values with which they were raised and believe those values are “right” because they are the values of their culture. Some personal values are considered sacred and moral imperatives based on an individual’s religious beliefs.[ 5 ] See Figure 6.1 [ 6 ] for an image depicting choosing right from wrong actions.
In addition to personal values, organizations also establish values. The American Nurses Association (ANA) Professional Nursing Model states that nursing is based on values such as caring, compassion, presence, trustworthiness, diversity, acceptance, and accountability. These values emerge from nursing practice beliefs, such as the importance of relationships, service, respect, willingness to bear witness, self-determination, and the pursuit of health.[ 7 ] As a result of these traditional values and beliefs by nurses, Americans have ranked nursing as the most ethical and honest profession in Gallup polls since 1999, with the exception of 2001, when firefighters earned the honor after the attacks on September 11.[ 8 ]
The National League of Nursing (NLN) has also established four core values for nursing education: caring, integrity, diversity, and excellence[ 9 ]:
- Caring: Promoting health, healing, and hope in response to the human condition.
- Integrity: Respecting the dignity and moral wholeness of every person without conditions or limitations.
- Diversity: Affirming the uniqueness of and differences among persons, ideas, values, and ethnicities.
- Excellence: Cocreating and implementing transformative strategies with daring ingenuity.
View the McCombs School of Business Values video on YouTube. [ 10 ]
Morals are the prevailing standards of behavior of a society that enable people to live cooperatively in groups. “Moral” refers to what societies sanction as right and acceptable. Most people tend to act morally and follow societal guidelines, and most laws are based on the morals of a society. Morality often requires that people sacrifice their own short-term interests for the benefit of society. People or entities that are indifferent to right and wrong are considered “amoral,” while those who do evil acts are considered “immoral.”[ 11 ]
Ethical Theories
There are two major types of ethical theories that guide values and moral behavior referred to as deontology and consequentialism.
Deontology is an ethical theory based on rules that distinguish right from wrong. See Figure 6.2 [ 12 ] for a word cloud illustration of deontology. Deontology is based on the word deon that refers to “duty.” It is associated with philosopher Immanuel Kant. Kant believed that ethical actions follow universal moral laws, such as, “Don’t lie. Don’t steal. Don’t cheat.”[ 13 ] Deontology is simple to apply because it just requires people to follow the rules and do their duty. It doesn’t require weighing the costs and benefits of a situation, thus avoiding subjectivity and uncertainty.[ 14 ],[ 15 ],[ 16 ]
The nurse-patient relationship is deontological in nature because it is based on the ethical principles of beneficence and maleficence that drive clinicians to “do good” and “avoid harm.”[ 17 ] Ethical principles will be discussed further in this chapter.
View the McCombs School of Business Deontology video on YouTube. [ 18 ]
Consequentialism is an ethical theory used to determine whether or not an action is right by the consequences of the action. See Figure 6.3 [ 19 ] for an illustration of weighing the consequences of an action in consequentialism. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do. One type of consequentialism is utilitarianism. Utilitarianism determines whether or not actions are right based on their consequences with the standard being achieving the greatest good for the greatest number of people.[ 20 ],[ 21 ],[ 22 ] For this reason, utilitarianism tends to be society-centered. When applying utilitarian ethics to health care resources, money, time, and clinician energy are considered finite resources that should be appropriately allocated to achieve the best health care for society.[ 23 ]
Consequentialism
Utilitarianism can be complicated when accounting for values such as justice and individual rights. For example, assume a hospital has four patients whose lives depend upon receiving four organ transplant surgeries for a heart, lung, kidney, and liver. If a healthy person without health insurance or family support experiences a life-threatening accident and is considered brain dead but is kept alive on life-sustaining equipment in the ICU, the utilitarian framework might suggest the organs be harvested to save four lives at the expense of one life.[ 24 ] This action could arguably produce the greatest good for the greatest number of people, but the deontological approach could argue this action would be unethical because it does not follow the rule of “do no harm.”
Watch McCombs School of Business Consequentialism video on YouTube. [ 25 ] Read more about Decision making on organ donation: The dilemmas of relatives of potential brain dead donors.
Interestingly, deontological and utilitarian approaches to ethical issues may result in the same outcome, but the rationale for the outcome or decision is different because it is focused on duty (deontologic) versus consequences (utilitarian).
Societies and cultures have unique ethical frameworks that may be based upon either deontological or consequentialist ethical theory. Culturally-derived deontological rules may apply to ethical issues in health care. For example, a traditional Chinese philosophy based on Confucianism results in a culturally-acceptable practice of family members (rather than the client) receiving information from health care providers about life-threatening medical conditions and making treatment decisions. As a result, cancer diagnoses and end-of-life treatment options may not be disclosed to the client in an effort to alleviate the suffering that may arise from knowledge of their diagnosis. In this manner, a client’s family and the health care provider may ethically prioritize a client’s psychological well-being over their autonomy and self-determination.[ 26 ] However, in the United States, this ethical decision may conflict with HIPAA Privacy Rules and the ethical principle of patient autonomy. As a result, a nurse providing patient care in this type of situation may experience an ethical dilemma. Ethical dilemmas are further discussed in the “ Ethical Dilemmas ” section of this chapter.
See Table 6.2 comparing common ethical issues in health care viewed through the lens of deontological and consequential ethical frameworks.
Ethical Issues Through the Lens of Deontological or Consequential Ethical Frameworks
View in own window
| Ethical Issue | Deontological View | Consequential View |
|---|---|---|
| Abortion | Abortion is unacceptable based on the rule of preserving life. | Abortion may be acceptable in cases of an unwanted pregnancy, rape, incest, or risk to the mother. |
| Bombing an area with known civilians | Killing civilians is not acceptable due to the loss of innocent lives. | The loss of innocent lives may be acceptable if the bombing stops a war that could result in significantly more deaths than the civilian casualties. |
| Stealing | Taking something that is not yours is wrong. | Taking something to redistribute resources to others in need may be acceptable. |
| Killing | It is never acceptable to take another human being’s life. | It may be acceptable to take another human life in self-defense or to prevent additional harm they could cause others. |
| Euthanasia/physician- assisted suicide | It is never acceptable to assist another human to end their life prematurely. | End-of-life care can be expensive and emotionally upsetting for family members. If a competent, capable adult wishes to end their life, medically supported options should be available. |
| Vaccines | Vaccination is a personal choice based on religious practices or other beliefs. | Recommended vaccines should be mandatory for everyone (without a medical contraindication) because of its greater good for all of society. |
Ethical Principles and Obligations
Ethical principles are used to define nurses’ moral duties and aid in ethical analysis and decision-making.[ 27 ] Although there are many ethical principles that guide nursing practice, foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), fidelity (keep promises), and veracity (tell the truth).
The ethical principle of autonomy recognizes each individual’s right to self-determination and decision-making based on their unique values, beliefs, and preferences. See Figure 6.4 [ 28 ] for an illustration of autonomy. The American Nurses Association (ANA) defines autonomy as the “capacity to determine one’s own actions through independent choice, including demonstration of competence.”[ 29 ] The nurse’s primary ethical obligation is client autonomy.[ 30 ] Based on autonomy, clients have the right to refuse nursing care and medical treatment. An example of autonomy in health care is advance directives. Advance directives allow clients to specify health care decisions if they become incapacitated and unable to do so.
Autonomy and Self-Determination
Read more about advance directives and determining capacity and competency in the “ Legal Implications ” chapter.
NURSES AS ADVOCATES: SUPPORTING AUTONOMY
Nurses have a responsibility to act in the interest of those under their care, referred to as advocacy. The American Nurses Association (ANA) defines advocacy as “the act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.”[ 31 ] See Figure 6.5 [ 32 ] for an illustration of advocacy.
Advocacy includes providing education regarding client rights, supporting autonomy and self-determination, and advocating for client preferences to health care team members and family members. Nurses do not make decisions for clients, but instead support them in making their own informed choices. At the core of making informed decisions is knowledge. Nurses serve an integral role in patient education. Clarifying unclear information, translating medical terminology, and making referrals to other health care team members (within their scope of practice) ensures that clients have the information needed to make treatment decisions aligned with their personal values.
At times, nurses may find themselves in a position of supporting a client’s decision they do not agree with and would not make for themselves or for the people they love. However, self-determination is a human right that honors the dignity and well-being of individuals. The nursing profession, rooted in caring relationships, demands that nurses have nonjudgmental attitudes and reflect “unconditional positive regard” for every client. Nurses must suspend personal judgement and beliefs when advocating for their clients’ preferences and decision-making.[ 33 ]
Beneficence
Beneficence is defined by the ANA as “the bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.”[ 34 ] See Figure 6.6 [ 35 ] for an illustration of beneficence. Put simply, beneficence is acting for the good and welfare of others, guided by compassion. An example of beneficence in daily nursing care is when a nurse sits with a dying patient and holds their hand to provide presence.
Nursing advocacy extends beyond direct patient care to advocating for beneficence in communities. Vulnerable populations such as children, older adults, cultural minorities, and the homeless often benefit from nurse advocacy in promoting health equity. Cultural humility is a humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.[ 36 ] Nurses, the largest segment of the health care community, have a powerful voice when addressing community beneficence issues, such as health disparities and social determinants of health, and can serve as the conduit for advocating for change.
Nonmaleficence
Nonmaleficence is defined by the ANA as “the bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.”[ 37 ] An example of doing no harm in nursing practice is reflected by nurses checking medication rights three times before administering medications. In this manner, medication errors can be avoided, and the duty to do no harm is met. Another example of nonmaleficence is when a nurse assists a client with a serious, life-threatening condition to participate in decision-making regarding their treatment plan. By balancing the potential harm with potential benefits of various treatment options, while also considering quality of life and comfort, the client can effectively make decisions based on their values and preferences.
Justice is defined by the ANA as “a moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.”[ 38 ] The principle of justice requires health care to be provided in a fair and equitable way. Nurses provide quality care for all individuals with the same level of fairness despite many characteristics, such as the individual’s financial status, culture, religion, gender, or sexual orientation. Nurses have a social contract to “provide compassionate care that addresses the individual’s needs for protection, advocacy, empowerment, optimization of health, prevention of illness and injury, alleviation of suffering, comfort, and well-being.”[ 39 ] An example of a nurse using the principle of justice in daily nursing practice is effective prioritization based on client needs.
Read more about prioritization models in the “ Prioritization ” chapter.
Other Ethical Principles
Additional ethical principles commonly applied to health care include fidelity (keeping promises) and veracity (telling the truth). . An example of fidelity in daily nursing practice is when a nurse tells a client, “I will be back in an hour to check on your pain level.” This promise is kept. An example of veracity in nursing practice is when a nurse honestly explains potentially uncomfortable side effects of prescribed medications. Determining how truthfulness will benefit the client and support their autonomy is dependent on a nurse’s clinical judgment, self-reflection, knowledge of the patient and their cultural beliefs, and other factors.[ 40 ]
A principle historically associated with health care is paternalism. Paternalism is defined as the interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[ 41 ] Paternalism is the basis for legislation related to drug enforcement and compulsory wearing of seatbelts.
In health care, paternalism has been used as rationale for performing treatment based on what the provider believes is in the client’s best interest. In some situations, paternalism may be appropriate for individuals who are unable to comprehend information in a way that supports their informed decision-making, but it must be used cautiously to ensure vulnerable individuals are not misused and their autonomy is not violated.
Nurses may find themselves acting paternalistically when performing nursing care to ensure client health and safety. For example, repositioning clients to prevent skin breakdown is a preventative intervention commonly declined by clients when they prefer a specific position for comfort. In this situation, the nurse should explain the benefits of the preventative intervention and the risks if the intervention is not completed. If the client continues to decline the intervention despite receiving this information, the nurse should document the education provided and the client’s decision to decline the intervention. The process of reeducating the client and reminding them of the importance of the preventative intervention should be continued at regular intervals and documented.
Care-Based Ethics
Nurses use a client-centered, care-based ethical approach to patient care that focuses on the specific circumstances of each situation. This approach aligns with nursing concepts such as caring, holism, and a nurse-client relationship rooted in dignity and respect through virtues such as kindness and compassion.[ 42 ],[ 43 ] This care-based approach to ethics uses a holistic, individualized analysis of situations rather than the prescriptive application of ethical principles to define ethical nursing practice. This care-based approach asserts that ethical issues cannot be handled deductively by applying concrete and prefabricated rules, but instead require social processes that respect the multidimensionality of problems.[ 44 ] Frameworks for resolving ethical situations are discussed in the “ Ethical Dilemmas ” subsection of this chapter.
Nursing Code of Ethics
Many professions and institutions have their own set of ethical principles, referred to as a code of ethics , designed to govern decision-making and assist individuals to distinguish right from wrong. The American Nurses Association (ANA) provides a framework for ethical nursing care and guides nurses during decision-making in its formal document titled Code of Ethics for Nurses With Interpretive Statements (Nursing Code of Ethics) . The Nursing Code of Ethics serves the following purposes[ 45 ]:
- It is a succinct statement of the ethical values, obligations, duties, and professional ideals of nurses individually and collectively.
- It is the profession’s nonnegotiable ethical standard.
- It is an expression of nursing’s own understanding of its commitment to society.
The preface of the ANA’s Nursing Code of Ethics states, “Individuals who become nurses are expected to adhere to the ideals and moral norms of the profession and also to embrace them as a part of what it means to be a nurse. The ethical tradition of nursing is self-reflective, enduring, and distinctive. A code of ethics makes explicit the primary goals, values, and obligations of the profession.”[ 46 ]
The Nursing Code of Ethics contains nine provisions. Each provision contains several clarifying or “interpretive” statements. Read a summary of the nine provisions in the following box.
Nine Provisions of the ANA Nursing Code of Ethics
- Provision 1: The nurse practices with compassion and respect for the inherent dignity, worth, and unique attributes of every person.
- Provision 2: The nurse’s primary commitment is to the patient, whether an individual, family, group, community, or population.
- Provision 3: The nurse promotes, advocates for, and protects the rights, health, and safety of the patient.
- Provision 4: The nurse has authority, accountability, and responsibility for nursing practice; makes decisions; and takes action consistent with the obligation to promote health and to provide optimal care.
- Provision 5: The nurse owes the same duties to self as to others, including the responsibility to promote health and safety, preserve wholeness of character and integrity, maintain competence, and continue personal and professional growth.
- Provision 6: The nurse, through individual and collective effort, establishes, maintains, and improves the ethical environment of the work setting and conditions of employment that are conducive to safe, quality health care.
- Provision 7: The nurse, in all roles and settings, advances the profession through research and scholarly inquiry, professional standards development, and the generation of both nursing and health policy.
- Provision 8 : The nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce health disparities.
- Provision 9: The profession of nursing, collectively through its professional organizations, must articulate nursing values, maintain the integrity of the profession, and integrate principles of social justice into nursing and health policy.
Read the free, online full version of the ANA’s Code of Ethics for Nurses With Interpretive Statements.
In addition to the Nursing Code of Ethics, the ANA established the Center for Ethics and Human Rights to help nurses navigate ethical conflicts and life-and-death decisions common to everyday nursing practice.
Read more about the ANA Center for Ethics and Human Rights .
Specialty Organization Code of Ethics
Many specialty nursing organizations have additional codes of ethics to guide nurses practicing in settings such as the emergency department, home care, or hospice care. These documents are unique to the specialty discipline but mirror the statements from the ANA’s Nursing Code of Ethics. View ethical statements of various specialty nursing organizations using the information in the following box.
Ethical Statements of Selected Specialty Nursing Organizations
• American College of Nurse-Midwives
• Emergency Nurses Association
• National Association for Home Care & Hospice
• National Association of Neonatal Nurses
6.3. ETHICAL DILEMMAS
Nurses frequently find themselves involved in conflicts during patient care related to opposing values and ethical principles. These conflicts are referred to as ethical dilemmas. An ethical dilemma results from conflict of competing values and requires a decision to be made from equally desirable or undesirable options.
An ethical dilemma can involve conflicting patient’s values, nurse values, health care provider’s values, organizational values, and societal values associated with unique facts of a specific situation. For this reason, it can be challenging to arrive at a clearly superior solution for all stakeholders involved in an ethical dilemma. Nurses may also encounter moral dilemmas where the right course of action is known but the nurse is limited by forces outside their control. See Table 6.3a for an example of ethical dilemmas a nurse may experience in their nursing practice.
Examples of Ethical Issues Involving Nurses
| Workplace | Organizational Processes | Client Care |
|---|---|---|
Read more about Ethics Topics and Articles on the ANA website.
According to the American Nurses Association (ANA), a nurse’s ethical competence depends on several factors[ 1 ]:
- Continuous appraisal of personal and professional values and how they may impact interpretation of an issue and decision-making
- An awareness of ethical obligations as mandated in the Code of Ethics for Nurses With Interpretive Statements [ 2 ]
- Knowledge of ethical principles and their application to ethical decision-making
- Motivation and skills to implement an ethical decision
Nurses and nursing students must have moral courage to address the conflicts involved in ethical dilemmas with “the willingness to speak out and do what is right in the face of forces that would lead us to act in some other way.”[ 3 ] See Figure 6.7[ 4 ] for an illustration of nurses’ moral courage.

Figure 6.12
Moral Courage
Nurse leaders and organizations can support moral courage by creating environments where nurses feel safe and supported to speak up.[ 5 ] Nurses may experience moral conflict when they are uncertain about what values or principles should be applied to an ethical issue that arises during patient care. Moral conflict can progress to moral distress when the nurse identifies the correct ethical action but feels constrained by competing values of an organization or other individuals. Nurses may also feel moral outrage when witnessing immoral acts or practices they feel powerless to change. For this reason, it is essential for nurses and nursing students to be aware of frameworks for solving ethical dilemmas that consider ethical theories, ethical principles, personal values, societal values, and professionally sanctioned guidelines such as the ANA Nursing Code of Ethics.
Moral injury felt by nurses and other health care workers in response to the COVID-19 pandemic has gained recent public attention. Moral injury refers to the distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.[ 6 ] Health care workers may not have the time or resources to process their feelings of moral injury caused by the pandemic, which can result in burnout. Organizations can assist employees in processing these feelings of moral injury with expanded employee assistance programs or other structured support programs.[ 7 ] Read more about self-care strategies to address feelings of burnout in the “ Burnout and Self-Care ” chapter.
Frameworks for Solving Ethical Dilemmas
Systematically working through an ethical dilemma is key to identifying a solution. Many frameworks exist for solving an ethical dilemma, including the nursing process, four-quadrant approach, the MORAL model, and the organization-focused PLUS Ethical Decision-Making model.[ 8 ] When nurses use a structured, systematic approach to resolving ethical dilemmas with appropriate data collection, identification and analysis of options, and inclusion of stakeholders, they have met their legal, ethical, and moral responsibilities, even if the outcome is less than ideal.
Nursing Process Model
The nursing process is a structured problem-solving approach that nurses may apply in ethical decision-making to guide data collection and analysis. See Table 6.3b for suggestions on how to use the nursing process model during an ethical dilemma.[ 9 ]
Using the Nursing Process in Ethical Situations[ 10 ]
| Nursing Process Stage | Considerations |
|---|---|
| Assessment/Data Collection | |
| Assessment/Analysis | , or another ethical framework model. |
| Diagnosis | |
| Outcome Identification | |
| Planning | |
| Implementation | |
| Evaluation |
Four-Quadrant Approach
The four-quadrant approach integrates ethical principles (e.g., beneficence, nonmaleficence, autonomy, and justice) in conjunction with health care indications, individual and family preferences, quality of life, and contextual features.[ 11 ] See Table 6.3c for sample questions used during the four-quadrant approach.
Four-Quadrant Approach[ 12 ]
|
|
|
|
MORAL Model
The MORAL model is a nurse-generated, decision-making model originating from research on nursing-specific moral dilemmas involving client autonomy, quality of life, distributing resources, and maintaining professional standards. The model provides guidance for nurses to systematically analyze and address real-life ethical dilemmas. The steps in the process may be remembered by using the mnemonic MORAL. See Table 6.3d for a description of each step of the MORAL model.[ 13 ],[ 14 ]
| M: Massage the dilemma | Collect data by identifying the interests and perceptions of those involved, defining the dilemma, and describing conflicts. Establish a goal. |
|---|---|
| O: Outline options | Generate several effective alternatives to reach the goal. |
| R: Review criteria and resolve | Identify moral criteria and select the course of action. |
| A: Affirm position and act | Implement action based on knowledge from the previous steps (M-O-R). |
| L: Look back | Evaluate each step and the decision made. |
PLUS Ethical Decision-Making Model
The PLUS Ethical Decision-Making model was created by the Ethics and Compliance Initiative to help organizations empower employees to make ethical decisions in the workplace. This model uses four filters throughout the ethical decision-making process, referred to by the mnemonic PLUS:
- P: Policies, procedures, and guidelines of an organization
- L: Laws and regulations
- U: Universal values and principles of an organization
- S: Self-identification of what is good, right, fair, and equitable[ 15 ]
The seven steps of the PLUS Ethical Decision-Making model are as follows[ 16 ]:
- Define the problem using PLUS filters
- Seek relevant assistance, guidance, and support
- Identify available alternatives
- Evaluate the alternatives using PLUS to identify their impact
- Make the decision
- Implement the decision
- Evaluate the decision using PLUS filters
6.4. ETHICS COMMITTEES
In addition to using established frameworks to resolve ethical dilemmas, nurses can also consult their organization’s ethics committee for ethical guidance in the workplace. Ethics committees are typically composed of interdisciplinary team members such as physicians, nurses, allied health professionals, administrators, social workers, and clergy to problem-solve ethical dilemmas. See Figure 6.8 [ 1 ] for an illustration of an ethics committee. Hospital ethics committees were created in response to legal controversies regarding the refusal of life-sustaining treatment, such as the Karen Quinlan case.[ 2 ] Read more about the Karen Quinlan case and controversies surrounding life-sustaining treatment in the “ Legal Implications ” chapter.
Ethics Committee
After the passage of the Patient Self-Determination Act in 1991, all health care institutions receiving Medicare or Medicaid funding are required to form ethics committees. The Joint Commission (TJC) also requires organizations to have a formalized mechanism of dealing with ethical issues. Nurses should be aware of the process for requesting guidance and support from ethics committees at their workplace for ethical issues affecting patients or staff.[ 3 ]
Institutional Review Boards and Ethical Research
Other types of ethics committees have been formed to address the ethics of medical research on patients. Historically, there are examples of medical research causing harm to patients. For example, an infamous research study called the “Tuskegee Study” raised concern regarding ethical issues in research such as informed consent, paternalism, maleficence, truth-telling, and justice.
In 1932 the Tuskegee Study began a 40-year study looking at the long-term progression of syphilis. Over 600 Black men were told they were receiving free medical care, but researchers only treated men diagnosed with syphilis with aspirin, even after it was discovered that penicillin was a highly effective treatment for the disease. The institute allowed the study to go on, even when men developed long-stage neurological symptoms of the disease and some wives and children became infected with syphilis. In 1972 these consequences of the Tuskegee Study were leaked to the media and public outrage caused the study to shut down.[ 4 ]
Potential harm to patients participating in research studies like the Tuskegee Study was rationalized based on the utilitarian view that potential harm to individuals was outweighed by the benefit of new scientific knowledge resulting in greater good for society. As a result of public outrage over ethical concerns related to medical research, Congress recognized that an independent mechanism was needed to protect research subjects. In 1974 regulations were established requiring research with human subjects to undergo review by an institutional review board (IRB) to ensure it meets ethical criteria. An IRB is group that has been formally designated to review and monitor biomedical research involving human subjects.[ 5 ] The IRB review ensures the following criteria are met when research is performed:
- The benefits of the research study outweigh the potential risks.
- Individuals’ participation in the research is voluntary.
- Informed consent is obtained from research participants who have the ability to decline participation.
- Participants are aware of the potential risks of participating in the research.[ 6 ]
View a YouTube video discussing Henrietta Lacks, the Tuskegee Experiment, ethics and research. [ 7 ]
6.5. ETHICS AND THE NURSING STUDENT
Nursing students may encounter ethical dilemmas when in clinical practice settings. Read more about research regarding ethical dilemmas experienced by students as described in the box.
Nursing Students and Ethical Dilemmas [ 1 ]
An integrative literature review performed by Albert, Younas, and Sana in 2020 identified ethical dilemmas encountered by nursing students in clinical practice settings. Three themes were identified:
1. Applying learned ethical values vs. accepting unethical practice
Students observed unethical practices of nurses and physicians, such as breach of patient privacy, confidentiality, respect, rights, duty to provide information, and physical and psychological mistreatment, that opposed the ethical values learned in nursing school. Students experienced ethical conflict due to their sense of powerlessness, low status as students, dependence on staff nurses for learning experiences, and fear of offending health care providers.
2. Desiring to provide ethical care but lacking autonomous decision-making
Students reported a lack of moral courage in questioning unethical practices. The hierarchy of health care environments left students feeling disregarded, humiliated, and intimidated by professional nurses and managers. Students also reported a sense of loss of identity in feeling forced to conform their personal identity to that of the clinical environment.
3. Whistleblowing vs. silence regarding patient care and neglect
Students observed nurses performing unethical nursing practices, such as ignoring client needs, disregarding pain, being verbally abusive, talking inappropriately about clients, and not providing a safe or competent level of care. Most students reported remaining silent regarding these observations due to a lack of confidence, feeling it was not their place to report, or the fear of negative consequences. Organizational power dynamics influenced student confidence in reporting unethical practices to faculty or nurse managers.
The researchers concluded that nursing students feel moral distress when experiencing these kinds of conflicts:
- Providing ethical care as learned in their program of study or accepting unethical practices
- Staying silent about patient care neglect or confronting it and reporting it
- Providing quality, ethical care or adapting to organizational culture due to lack of autonomous decision-making
These ethical conflicts can be detrimental to students’ professional learning and mental health. Researchers recommended that nurse educators should develop educational programs to support students as they develop ethical competence and moral courage to confront ethical dilemmas.[ 2 ]
Read more about ethics education in nursing in the ANA’s Online Journal of Issues in Nursing article .
COVID-19 and the Nursing Profession
The COVID-19 pandemic has highlighted the importance of nurses’ foundational knowledge of ethical principles and the Nursing Code of Ethics . Scarce resources in an overwhelmed health care system resulted in ethical dilemmas and moral injury for nurses involved in balancing conflicting values, rights, and ethical principles. Many nurses were forced to weigh their duty to patients and society against their duty to themselves and their families. Challenging ethical issues occurred related to the ethical principle of justice, such as fair distribution of limited ICU beds and ventilators, and ethical dilemmas related to end-of-life issues such as withdrawing or withholding life-prolonging treatment became common.[ 3 ]
Regardless of their practice setting or personal contact with clients affected by COVID-19, nurses have been forced to reflect on the essence of ethical professional nursing practice through the lens of personal values and morals. Nursing students must be knowledgeable about ethical theories, ethical principles, and strategies for resolving ethical dilemmas as they enter the nursing profession that will continue to experience long-term consequences as a result of COVID-19.[ 4 ]
6.6. SPOTLIGHT APPLICATION
A True Story of a New Nurse’s Introduction to Ethical Dilemmas
A new nurse graduate meets Mary, a 70-year-old woman who was living alone at home with Amyotrophic Lateral Sclerosis (ALS or also referred to as “Lou Gehrig’s disease”). Mary’s husband died many years ago and they did not have children. She had a small support system including relatives who lived out of state and friends with whom she had lost touch since her diagnosis. Mary was fiercely independent and maintained her nutrition and hydration through a gastrostomy tube to avoid aspiration.
As Mary’s disease progressed, the new nurse discussed several safety issues related to Mary living alone. As the new nurse shared several alternative options related to skilled nursing care with Mary, Mary shared her own plan. Mary said her plan included a combination of opioids, benzodiazepines, and a plastic bag to suffocate herself and be found by a nurse during a scheduled visit. In addition to safety issues and possible suicide ideation, the new nurse recognized she was in the midst of an ethical dilemma in terms of the treatment plan, her values and what she felt was best for Mary, and Mary’s preferences.
Applying the MORAL Ethical Decision-Making Model to Mary’s Case
| Massage the Dilemma | Mary lives alone and does not want to go to a nursing home. She lacks social support. She has a progressive and incurable disease that affects her ability to swallow, talk, walk, and eventually breathe. She has made statements to staff indicating she prefers to die rather than leave her home to receive total care in a long-term care setting. According to the deontological theory, suicide is always wrong. According to the consequentialism ethical theory, an action’s morality depends on the consequences of that action. Mary has a progressive, incurable illness that requires total care that will force her to leave the home. She wishes to stay in her home until she dies. To honor Mary’s dignity and respect her autonomy in making treatment decisions. For Mary to experience a “good” death as she defines it, and neither hasten nor prolong her dying process through illegal or amoral interventions. |
|---|---|
| Outline the Options | |
| Review Criteria and Resolve | Mary was assessed to be rational and capable of decision-making by a psychiatrist. Mary defined a “good” death as one occurring in her home and not in a hospital or long-term care setting. Mary did not want her life to be prolonged through the use of technology such as a ventilator. Mary elected to discontinue tube feeding and limit hydration to only that necessary for medication to provide comfort care and symptom management. |
| Affirm Position and Act | Although some health care members did not personally believe in discontinuing food and fluids through the g-tube based on their interpretation of the deontological ethical theory, Mary’s decision was acceptable both legally and ethically, based on the consequentialism ethical theory that the decision best supported Mary’s goals and respected her autonomy. Daily visits were scheduled with hospice staff, including the nurse, nursing assistant, social worker, chaplain, and volunteers. Hired caregivers supplemented visits and in the last couple of days were scheduled around the clock. Mary died comfortably in her bed seven days after implementation of the agreed-upon plan. |
| Look Back | The health care team evaluated what happened during Mary’s situation and what could be learned from this ethical dilemma and applied to future patient-care scenarios. |
6.7. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activities are provided as immediate feedback.)
Ethical Application & Reflection Activity
Filmmaker Lulu Wang first shared a story about her grandmother on This American Life podcast and later turned it into the 2019 movie The Farewell starring Awkwafina. Both share the challenges of a Chinese-born but U.S.-raised woman returning to China and a family who has chosen to not disclose that the grandmother has been given a Stage IV lung cancer diagnosis and three months to live. Listen to the podcast and then answer the following questions:
585: In Defense of Ignorance Act One: What You Don’t Know
1. Reflect on the similarities and differences of your family culture with that of the Billi family. Consider things such as what family gatherings, formal and informal, look like and spoken and unspoken rules related to communication and behavior.
2. The idea of “good” lies and “bad” lies is introduced in the podcast. Nai Nai’s family supports the decision to not tell her about her Stage IV lung cancer, stage a wedding as the excuse to visit and say their goodbyes, and even alter a medical report as good lies necessary to support her mental health, well-being, and happiness. Is the family applying deontological or utilitarian ethics to the situation? Defend your response.
3. Define the following ethical principles and identify examples from this story:
• Autonomy
• Beneficence
• Nonmaleficence
• Paternalism
4. Imagine this story is happening in the United States rather than China and you are the nurse admitting Nai Nai to an inpatient oncology unit. Using the ethical problem-solving model of your choice, identify and support your solution to the ethical dilemma posed when her family requests that Nai Nai not be told that she has cancer.
You are caring for a 32-year-old client who has been in a persistent vegetative state for many years. There is an outdated advanced directive that is confusing on the issue of food and fluids, though clear about not wanting to be on a ventilator if she were in a coma. Her husband wants the feeding tube removed but is unable to say that it would have been the client’s wish. He says that it is his decision for her. Her two adult siblings and parents reject this as a possibility because they say that “human life is sacred” and that the daughter believed this. They say their daughter is alive and should receive nursing care, including feeding. The health care team does not know what to do ethically and fear being sued by either the husband, siblings, or the parents. What do you need to know about this clinical situation? What are the values and obligations at stake in this case? What values or obligations should be affirmed and why? How might that be done?
1. Define the problem.
2. List what facts/information you have.
3. What are the stakeholders’ positions?
• Patient:
• Spouse:
• Family:
• Health Care Team:
• Facility:
• Community:
4. How might the stakeholders’ values differ?
5. What are your values in this situation?
6. Do your values conflict with those of the patient? Describe.

VI. GLOSSARY
The act or process of pleading for, supporting, or recommending a cause or course of action. Advocacy may be for persons (whether an individual, group, population, or society) or for an issue, such as potable water or global health.[ 1 ]
The capacity to determine one’s own actions through independent choice, including demonstration of competence.[ 2 ]
The bioethical principle of benefiting others by preventing harm, removing harmful conditions, or affirmatively acting to benefit another or others, often going beyond what is required by law.[ 3 ]
A set of ethical principles established by a profession that is designed to govern decision-making and assist individuals to distinguish right from wrong.
An ethical theory used to determine whether or not an action is right by the consequences of the action. For example, most people agree that lying is wrong, but if telling a lie would help save a person’s life, consequentialism says it’s the right thing to do.
A humble and respectful attitude towards individuals of other cultures and an approach to learning about other cultures as a lifelong goal and process.
An ethical theory based on rules that distinguish right from wrong.
Conflict resulting from competing values that requires a decision to be made from equally desirable or undesirable options.
Principles used to define nurses’ moral duties and aid in ethical analysis and decision-making.[ 4 ] Foundational ethical principles include autonomy (self-determination), beneficence (do good), nonmaleficence (do no harm), justice (fairness), and veracity (tell the truth).
The formal study of morality from a wide range of perspectives.[ 5 ]
A formal committee established by a health care organization to problem-solve ethical dilemmas.
An ethical principle meaning keeping promises.
A group that has been formally designated to review and monitor biomedical research involving human subjects.
A moral obligation to act on the basis of equality and equity and a standard linked to fairness for all in society.[ 6 ]
The distressing psychological, behavioral, social, and sometimes spiritual aftermath of exposure to events that contradict deeply held moral beliefs and expectations.
Personal values, character, or conduct of individuals or groups within communities and societies.[ 7 ]
The prevailing standards of behavior of a society that enable people to live cooperatively in groups.[ 8 ]
Feelings occurring when an individual is uncertain about what values or principles should be applied to an ethical issue.[ 9 ]
The willingness of an individual to speak out and do what is right in the face of forces that would lead us to act in some other way.[ 10 ]
Feelings occurring when correct ethical action is identified but the individual feels constrained by competing values of an organization or other individuals.[ 11 ]
Feelings occurring when an individual witnesses immoral acts or practices they feel powerless to change.[ 12 ]
The bioethical principle that specifies a duty to do no harm and balances avoidable harm with benefits of good achieved.[ 13 ]
The interference by the state or an individual with another person, defended by the claim that the person interfered with will be better off or protected from harm.[ 14 ]
A type of consequentialism that determines whether or not actions are right based on their consequences, with the standard being achieving the greatest good for the greatest number of people.
Individual beliefs that motivate people to act one way or another and serve as a guide for behavior.[ 15 ]
An ethical principle meaning telling the truth.
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Management and Professional Concepts [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022. Chapter 6 – Ethical Practice.
- PDF version of this title (18M)
In this Page
- ETHICAL PRACTICE INTRODUCTION
- BASIC ETHICAL CONCEPTS
- ETHICAL DILEMMAS
- ETHICS COMMITTEES
- ETHICS AND THE NURSING STUDENT
- SPOTLIGHT APPLICATION
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 6 – Ethical Practice - Nursing Management and Professional Concepts Chapter 6 – Ethical Practice - Nursing Management and Professional Concepts
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
An integrated ethical decision-making model for nurses
Affiliation.
- 1 Department of Nursing, Kyungwon University, San 65 Bokjeong-Dong, Gyeonggi-Do, Korea. [email protected]
- PMID: 22156941
- DOI: 10.1177/0969733011413491
The study reviewed 20 currently-available structured ethical decision-making models and developed an integrated model consisting of six steps with useful questions and tools that help better performance each step: (1) the identification of an ethical problem; (2) the collection of additional information to identify the problem and develop solutions; (3) the development of alternatives for analysis and comparison; (4) the selection of the best alternatives and justification; (5) the development of diverse, practical ways to implement ethical decisions and actions; and (6) the evaluation of effects and development of strategies to prevent a similar occurrence. From a pilot-test of the model, nursing students reported positive experiences, including being satisfied with having access to a comprehensive review process of the ethical aspects of decision making and becoming more confident in their decisions. There is a need for the model to be further tested and refined in both the educational and practical environments.
PubMed Disclaimer
Similar articles
- How do children's nurses make clinical decisions? Two preliminary studies. Twycross A, Powls L. Twycross A, et al. J Clin Nurs. 2006 Oct;15(10):1324-35. doi: 10.1111/j.1365-2702.2006.01453.x. J Clin Nurs. 2006. PMID: 16968437
- Nursing students' experience of ethical problems and use of ethical decision-making models. Cameron ME, Schaffer M, Park HA. Cameron ME, et al. Nurs Ethics. 2001 Sep;8(5):432-47. doi: 10.1177/096973300100800507. Nurs Ethics. 2001. PMID: 16004097
- [A model for ethical decision-making in nursing]. Botes A. Botes A. Curationis. 1994 Dec;17(4):66-70. Curationis. 1994. PMID: 7697793 Afrikaans.
- Risk management frameworks for human health and environmental risks. Jardine C, Hrudey S, Shortreed J, Craig L, Krewski D, Furgal C, McColl S. Jardine C, et al. J Toxicol Environ Health B Crit Rev. 2003 Nov-Dec;6(6):569-720. doi: 10.1080/10937400390208608. J Toxicol Environ Health B Crit Rev. 2003. PMID: 14698953 Review.
- The use of critical reflection in baccalaureate nursing education. Butler KM. Butler KM. Nurs Leadersh Forum. 2004 Summer;8(4):138-45. Nurs Leadersh Forum. 2004. PMID: 15495761 Review.
- Non-Maleficence toward Young Kidney Donors: A Call for Stronger Ethical Standards and Associated Factors in Multidisciplinary Nephrology Teams. Tarabeih M, Na'amnih W. Tarabeih M, et al. Nurs Rep. 2024 Aug 19;14(3):1998-2013. doi: 10.3390/nursrep14030149. Nurs Rep. 2024. PMID: 39189279 Free PMC article.
- Examination of Ethical Decision-Making Models Across Disciplines: Common Elements and Application to the Field of Behavior Analysis. Suarez VD, Marya V, Weiss MJ, Cox D. Suarez VD, et al. Behav Anal Pract. 2022 Nov 29;16(3):657-671. doi: 10.1007/s40617-022-00753-1. eCollection 2023 Sep. Behav Anal Pract. 2022. PMID: 37680335 Free PMC article. Review.
- Multi-professional ethical competence in healthcare - an ethical practice model. Koskinen C, Kaldestad K, Rossavik BD, Ree Jensen A, Bjerga G. Koskinen C, et al. Nurs Ethics. 2022 Jun;29(4):1003-1013. doi: 10.1177/09697330211062986. Epub 2022 Feb 25. Nurs Ethics. 2022. PMID: 35212250 Free PMC article.
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- Ovid Technologies, Inc.

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.

IMAGES
VIDEO
COMMENTS
Problem-solving in nursing is the act of utilizing critical thinking and decision-making skills to identify, analyze, and address problems or challenges encountered by nurses in the healthcare setting. Problem-solving in nursing can be related to specific patient needs or may be related to staff issues.
Conclusion The influencing factors of clinical nurses' problem-solving dilemma are diverse. Hospital managers and nursing educators should pay attention to the problem-solving of clinical nurses, carry out a series of training and counselling of nurses by using the method of situational simulation, optimize the nursing management mode, learn to use new media technology to improve the ...
Problem solving for nurses is essential to quality patient care. Explore problem-solving examples in nursing and devise effective strategies.
This study was intended to confirm the structural relationship between clinical nurse communication skills, problem-solving ability, understanding of patients' conditions, and nurse's perception of professionalism. Due to changes in the ...
s, and problem-solving, which requires analysis. Decision-makingfree flow of ideas is essential to problem-solving and decision-making becaus. it helps prevent preconceived ideas from controlling the process. Many decisions in healthcare are arrived at by group or teams rather than by the in. vidual, and this type of decision-making requ.
The model has interrelated concepts of health and nursing problems and problem-solving, which is inherently logical in nature. Furthermore, the 21 nursing problems progressed to a second-generation development referred to as patient problems and patient outcomes.
Review methods A random-effects model was used to generate pooled standardized mean differences (SMD) for critical thinking, problem-solving, and self-confidence. The heterogeneity of each variable in the pooled estimate was determined using a random-effects model.
Abstract This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted ...
What Is Critical Thinking in Nursing? Critical thinking in nursing involves identifying a problem, determining the best solution, and implementing an effective method to resolve the issue using clinical decision-making skills.
Abstract The COVID-19 pandemic made creative problem-solving, a skill that nurses have long possessed, more observable and valued. This article presents a new professional practice model for nursing innovation that facilitates practice improvements and leverages skills, strengths, and values that are integral to nursing.
Problem-based learning (PBL) is a student-centered approach to teaching that has been applied in medical and nursing education. The effectiveness of PBL in promoting critical thinking in nursing students has been studied extensively with mixed results.
Critical thinking is applied by nurses in the process of solving problems of patients and decision-making process with creativity to enhance the effect. It is an essential process for a safe, efficient and skillful nursing intervention. Critical thinking according to Scriven and Paul is the mental active process and subtle perception, analysis ...
The results showed that structured social problem-solving training could improve cognitive problem-solving, critical thinking, and decision-making skills. Considering this result, nursing education should be presented using new strategies and creative and different ways from traditional education methods.
This paper reviews the literature surrounding the research on how individuals solve problems. The purpose of the review is to heighten awareness amongst nurses in general, and nurse academics in particular about the theories developed, approaches taken and conclusions reached on how clinicians problem-solve.
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28 The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
As such, I offer the following more nursing-centered and practical definition: EBP for nursing is a way of entering the situation with curiosity and engagement that follows the nursing process by responding to the issue or problem using the best available evidence.
Problem-solving ability is an important competency for nursing students to enable them to solve various problems that occur in dynamic clinical settings. The purpose of this cross-sectional study was to identify the factors that affect the problem-solving ...
Abstract. This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills. It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in ...
1. Background The nursing process is a widely recognized theoretical model in nursing education playing a central role in the nurse's competence. This process serves as a theoretical problem-solving model (Fertelli, 2019) in nurse's clinical decision-making, leading to individually adapted patient-safe care (Alfaro-LeFevre, 2013).
Strategies for Problem Solving Nursing students will be expected to have or develop strong problem-solving skills. Problem solving is centered on your ability to identify critical issues and create or identify solutions. Well-developed problem solving skills is a characteristic of a successful student. Remember, problems are a part of everyday life and your ability to resolve problems will ...
The knowledge-driven model emphasizes the organization and availability of relevant content knowledge stored in memory as the prime determinant of clinical problem solving. This contention is discussed in relation to the development of a clinical problem-solving task for nursing students and its implications for nursing curricula.
The nursing process is a structured problem-solving approach that nurses may apply in ethical decision-making to guide data collection and analysis. See Table 6.3b for suggestions on how to use the nursing process model during an ethical dilemma.
Methods. A quasi-experimental design was used. Participants were 161 undergraduate nursing students from two levels of a university, 88 subjects in the experimental group were taught using Simulation with problem-based learning and 73 subjects in the control group were taught using Problem-based learning.
Abstract. The study reviewed 20 currently-available structured ethical decision-making models and developed an integrated model consisting of six steps with useful questions and tools that help better performance each step: (1) the identification of an ethical problem; (2) the collection of additional information to identify the problem and ...