
- Previous Article
- Next Article

Case Presentation
Case study: a patient with diabetes and weight-loss surgery.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Sue Cummings; Case Study: A Patient With Diabetes and Weight-Loss Surgery. Diabetes Spectr 1 July 2007; 20 (3): 173–176. https://doi.org/10.2337/diaspect.20.3.173
Download citation file:
- Ris (Zotero)
- Reference Manager
A.W. is a 65-year-old man with type 2 diabetes who was referred by his primary care physician to the weight center for an evaluation of his obesity and recommendations for treatment options, including weight-loss surgery. The weight center has a team of obesity specialists, including an internist, a registered dietitian (RD), and a psychologist, who perform a comprehensive initial evaluation and make recommendations for obesity treatment. A.W. presented to the weight center team reluctant to consider weight-loss surgery;he is a radiologist and has seen patients who have had complications from bariatric surgery.
Pertinent medical history. A.W.'s current medications include 30 and 70 units of NPH insulin before breakfast and before or after dinner, respectively, 850 mg of metformin twice daily, atorvastatin,lisinopril, nifedipine, allopurinol, aspirin, and an over-the-counter vitamin B 12 supplement. He has sleep apnea but is not using his continuous positive airway pressure machine. He reports that his morning blood glucose levels are 100–130 mg/dl, his hemoglobin A 1c (A1C) level is 6.1%, which is within normal limits, his triglyceride level is 201 mg/dl, and serum insulin is 19 ulU/ml. He weighs 343 lb and is 72 inches tall, giving him a BMI of 46.6 kg/m 2 .
Weight history. A.W. developed obesity as a child and reports having gained weight every decade. He is at his highest adult weight with no indication that medications or medical complications contributed to his obesity. His family history is positive for obesity; his father and one sister are also obese.
Dieting history. A.W. has participated in both commercial and medical weight-loss programs but has regained any weight lost within months of discontinuing the programs. He has seen an RD for weight loss in the past and has also participated in a hospital-based, dietitian-led, group weight-loss program in which he lost some weight but regained it all. He has tried many self-directed diets, but has had no significant weight losses with these.
Food intake. A.W. eats three meals a day. Dinner, his largest meal of the day, is at 7:30 p . m . He usually does not plan a mid-afternoon snack but will eat food if it is left over from work meetings. He also eats an evening snack to avoid hypoglycemia. He reports eating in restaurants two or three times a week but says his fast-food consumption is limited to an occasional breakfast sandwich from Dunkin'Donuts. His alcohol intake consists of only an occasional glass of wine. He reports binge eating (described as eating an entire large package of cookies or a large amount of food at work lunches even if he is not hungry) about once a month, and says it is triggered by stress.
Social history. Recently divorced, A.W. is feeling depressed about his life situation and has financial problems and stressful changes occurring at work. He recently started living with his girlfriend, who does all of the cooking and grocery shopping for their household.
Motivation for weight loss. A.W. says he is concerned about his health and wants to get his life back under control. His girlfriend, who is thin and a healthy eater, has also been concerned about his weight. His primary care physician has been encouraging him to explore weight-loss surgery; he is now willing to learn more about surgical options. He says that if the weight center team's primary recommendation is for weight-loss surgery,he will consider it.
Does A.W. have contraindications to weight-loss surgery, and, if not, does he meet the criteria for weight-loss surgery?
What type of weight-loss surgery would be best for A.W.?
Roles of the obesity specialist team members
The role of the physician as an obesity specialist is to identify and evaluate obesity-related comorbidities and to exclude medically treatable causes of obesity. The physician assesses any need to adjust medications and,if possible, determines if the patient is on a weight-promoting medication that may be switched to a less weight-promoting medication.
The psychologist evaluates weight-loss surgery candidates for a multitude of factors, including the impact of weight on functioning, current psychological symptoms and stressors, psychosocial history, eating disorders,patients' treatment preferences and expectations, motivation, interpersonal consequences of weight loss, and issues of adherence to medical therapies.
The RD conducts a nutritional evaluation, which incorporates anthropometric measurements including height (every 5 years), weight (using standardized techniques and involving scales in a private location that can measure patients who weigh > 350 lb), neck circumference (a screening tool for sleep apnea), and waist circumference for patients with a BMI < 35 kg/m 2 . Other assessments include family weight history,environmental influences, eating patterns, and the nutritional quality of the diet. A thorough weight and dieting history is taken, including age of onset of overweight or obesity, highest and lowest adult weight, usual weight, types of diets and/or previous weight-loss medications, and the amount of weight lost and regained with each attempt. 1
Importance of type of obesity
Childhood- and adolescent-onset obesity lead to hyperplasic obesity (large numbers of fat cells); patients presenting with hyperplasic and hypertrophic obesity (large-sized fat cells), as opposed to patients with hypertrophic obesity alone, are less likely to be able to maintain a BMI < 25 kg/m 2 , because fat cells can only be shrunk and not eliminated. This is true even after weight-loss surgery and may contribute to the variability in weight loss outcomes after weight loss surgery. Less than 5% of patients lose 100% of their excess body weight. 2 , 3
Criteria and contraindications for weight-loss surgery
In 1998, the “Clinical Guidelines on the Identification, Evaluation,and Treatment of Overweight and Obesity in Adults: The Evidence Report” 4 recommended that weight-loss surgery be considered an option for carefully selected patients:
with clinically severe obesity (BMI ≥ 40 kg/m 2 or ≥ 35 kg/m 2 with comorbid conditions);
when less invasive methods of weight loss have failed; and
the patient is at high risk for obesity-associated morbidity or mortality.
Contraindications for weight-loss surgery include end-stage lung disease,unstable cardiovascular disease, multi-organ failure, gastric verices,uncontrolled psychiatric disorders, ongoing substance abuse, and noncompliance with current regimens.
A.W. had no contraindications for surgery and met the criteria for surgery,with a BMI of 46.6 kg/m 2 . He had made numerous previous attempts at weight loss, and he had obesity-related comorbidities, including diabetes,sleep apnea, hypertension, and hypercholesterolemia.
Types of procedures
The roux-en-Y gastric bypass (RYGB) surgery is the most common weight-loss procedure performed in the United States. However, the laparoscopic adjustable gastric band (LAGB) procedure has been gaining popularity among surgeons. Both procedures are restrictive, with no malabsorption of macronutrients. There is,however, malabsorption of micronutrients with the RYGB resulting from the bypassing of a major portion of the stomach and duodenum. The bypassed portion of the stomach produces the intrinsic factor needed for the absorption of vitamin B 12 . The duodenum is where many of the fat-soluble vitamins, B vitamins, calcium, and iron are absorbed. Patients undergoing RYGB must agree to take daily vitamin and mineral supplementation and to have yearly monitoring of nutritional status for life.
Weight loss after RYGB and LAGB
The goal of weight-loss surgery is to achieve and maintain a healthier body weight. Mean weight loss 2 years after gastric bypass is ∼ 65% of excess weight loss (EWL), which is defined as the number of pounds lost divided by the pounds of overweight before surgery. 5 When reviewing studies of weight-loss procedures, it is important to know whether EWL or total body weight loss is being measured. EWL is about double the percentage of total body weight loss; a 65% EWL represents about 32% loss of total body weight.
Most of the weight loss occurs in the first 6 months after surgery, with a continuation of gradual loss throughout the first 18–24 months. Many patients will regain 10–15% of the lost weight; a small number of patients regain a significant portion of their lost weight. 6 Data on long-term weight maintenance after surgery indicate that if weight loss has been maintained for 5 years, there is a > 95% likelihood that the patient will keep the weight off over the long term.
The mean percentage of EWL for LAGB is 47.5%. 3 Although the LAGB is considered a lower-risk surgery, initial weight loss and health benefits from the procedure are also lower than those of RYGB.
Weight-loss surgery and diabetes
After gastric bypass surgery, there is evidence of resolution of type 2 diabetes in some individuals, which has led some to suggest that surgery is a cure. 7 Two published studies by Schauer et al. 8 and Sugarman et al. 9 reported resolution in 83 and 86% of patients, respectively. Sjoström et al. 10 published 2-and 10-year data from the Swedish Obese Subjects (SOS) study of 4,047 morbidly obese subjects who underwent bariatric surgery and matched control subjects. At the end of 2 years, the incidence of diabetes in subjects who underwent bariatric surgery was 1.0%, compared to 8.0% in the control subjects. At 10 years, the incidence was 7.0 and 24.0%, respectively.
The resolution of diabetes often occurs before marked weight loss is achieved, often days after the surgery. Resolution of diabetes is more prevalent after gastric bypass than after gastric banding (83.7% for gastric bypass and 47.9% for gastric banding). 5 The LAGB requires adjusting (filling the band through a port placed under the skin),usually five to six times per year. Meta-analysis of available data shows slower weight loss and less improvement in comorbidities including diabetes compared to RYGB. 5
A.W. had diabetes; therefore, the weight center team recommended the RYGB procedure.
Case study follow-up
A.W. had strong medical indications for surgery and met all other criteria outlined in current guidelines. 4 He attended a surgical orientation session that described his surgical options,reviewed the procedures (including their risks and possible complications),and provided him the opportunity to ask questions. This orientation was led by an RD, with surgeons and post–weight-loss surgical patients available to answer questions. After attending the orientation, A.W. felt better informed about the surgery and motivated to pursue this treatment.
The weight center evaluation team referred him to the surgeon for surgical evaluation. The surgeon agreed with the recommendation for RYGB surgery, and presurgical appointments and the surgery date were set. The surgeon encouraged A.W. to try to lose weight before surgery. 11
Immediately post-surgery. The surgery went well. A.W.'s blood glucose levels on postoperative day 2 were 156 mg/dl at 9:15 a . m . and 147 mg/dl at 11:15 a . m . He was discharged from the hospital on that day on no diabetes medications and encouraged to follow a Stage II clear and full liquid diet( Table 1 ). 12
Diet Stages After RYBG Surgery

On postoperative day 10, he returned to the weight center. He reported consuming 16 oz of Lactaid milk mixed with sugar-free Carnation Instant Breakfast and 8 oz of light yogurt, spread out over three to six meals per day. In addition, he was consuming 24 oz per day of clear liquids containing no sugar, calories, or carbonation. A.W.'s diet was advanced to Stage III,which included soft foods consisting primarily of protein sources (diced,ground, moist meat, fish, or poultry; beans; and/or dairy) and well-cooked vegetables. He also attended a nutrition group every 3 weeks, at which the RD assisted him in advancing his diet.
Two months post-surgery. A.W. was recovering well; he denied nausea, vomiting, diarrhea, or constipation. He was eating without difficulty and reported feeling no hunger. His fasting and pre-dinner blood glucose levels were consistently < 120 mg/dl, with no diabetes medications. He continued on allopurinol and atorvastatin and was taking a chewable daily multivitamin and chewable calcium citrate (1,000 mg/day in divided doses) with vitamin D (400 units). His weight was 293 lb, down 50 lb since the surgery. A pathology report from a liver biopsy showed mild to moderate steatatosis without hepatitis.
One year post-surgery. A.W.'s weight was 265 lb, down 78 lb since the surgery, and his weight loss had significantly slowed, as expected. He was no longer taking nifedipine or lisinipril but was restarted at 5 mg daily to achieve a systolic blood pressure < 120 mmHg. His atorvastatin was stopped because his blood lipid levels were appropriate (total cholesterol 117 mg/dl, triglycerides 77 mg/dl, HDL cholesterol 55 mg/dl, and LDL cholesterol 47 mg/dl). His gastroesophageal reflux disease has been resolved, and he continued on allopurinol for gout but had had no flare-ups since surgery. Knee pain caused by osteoarthritis was well controlled without anti-inflammatory medications, and he had no evidence of sleep apnea. Annual medical follow-up and nutritional laboratory measurements will include electrolytes, glucose,A1C, albumin, total protein, complete blood count, ferritin, iron, total iron binding capacity, calcium, parathyroid hormone, vitamin D, magnesium, vitamins B 1 and B 12 , and folate, as well as thyroid, liver, and kidney function tests and lipid measurements.
In summary, A.W. significantly benefited from undergoing RYBP surgery. By 1 year post-surgery, his BMI had decreased from 46.6 to 35.8 kg/m 2 ,and he continues to lose weight at a rate of ∼ 2 lb per month. His diabetes, sleep apnea, and hypercholesterolemia were resolved and he was able to control his blood pressure with one medication.
Clinical Pearls
Individuals considering weight loss surgery require rigorous presurgical evaluation, education, and preparation, as well as a comprehensive long-term postoperative program of surgical, medical, nutritional, and psychological follow-up.
Individuals with diabetes should consider the RYBP procedure because the data on resolution or significant improvement of diabetes after this procedure are very strong, and such improvements occur immediately. Resolution in or improvement of diabetes with the LAGB procedure are more likely to occur only after excess weight has been lost.
Individuals with diabetes undergoing weight loss surgery should be closely monitored; an inpatient protocol should be written regarding insulin regimens and sliding-scale use of insulin if needed. Patients should be educated regarding self-monitoring of blood glucose and the signs and symptoms of hypoglycemia. They should be given instructions on stopping or reducing medications as blood glucose levels normalize.
Patient undergoing RYGB must have lifetime multivitamin supplementation,including vitamins B 1 , B 12 , and D, biotin, and iron, as well as a calcium citrate supplement containing vitamin D (1,000–1,500 mg calcium per day). Nutritional laboratory measurements should be conducted yearly and deficiencies repleted as indicated for the duration of the patient's life.
Sue Cummings, MS, RD, LDN, is the clinical programs coordinator at the MGH Weight Center in Boston, Mass.
Email alerts
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- Case Report
- Open access
- Published: 06 January 2021
Efficacy of laparoscopic sleeve gastrectomy for patient with morbid obesity and type 1 diabetes mellitus: a case report
- Hidetaka Ichikawa 1 ,
- Hirofumi Imoto ORCID: orcid.org/0000-0003-2037-4643 1 ,
- Naoki Tanaka 1 ,
- Hiroaki Musha 1 ,
- Shojiro Sawada 2 , 4 ,
- Takeshi Naitoh 1 , 3 ,
- Takashi Kamei 1 &
- Michiaki Unno 1
Surgical Case Reports volume 7 , Article number: 7 ( 2021 ) Cite this article
1937 Accesses
3 Citations
Metrics details
Bariatric surgery is effective for the treatment of patients with morbid obesity and type 2 diabetes mellitus (T2DM), for body weight loss and glycemic control. However, in Japan, there has been no previous report of the effectiveness bariatric surgery in a case of morbid obesity associated with acute onset type 1 diabetes mellitus (T1DM), in which pancreatic β-cells were destroyed and endogenous insulin was depleted.
Case presentation
A 36-year-old woman with morbid obesity and T1DM, diagnosed when she was 6 years, was admitted for bariatric surgery. At her first consultation, she had a body weight of 106.7 kg and a body mass index of 42.2 kg/m 2 . Her HbA1c level was 9.0%, with a required daily insulin dose of 75 units. She underwent laparoscopic sleeve gastrectomy. At 1 year after surgery, her body weight had decreased to 81.0 kg and her body mass index to 32.2 kg/m 2 . In addition, her daily required dose of insulin had decreased to 24 units, with an improvement in her HbA1c level to 7.7%.
Conclusions
Although further evidence needs to be accumulated, including long-term outcomes, laparoscopic sleeve gastrectomy may provide an effective treatment for patients with morbid obesity and T1DM for body weight loss, improvement in HbA1c level, and insulin dose reduction.
Bariatric surgery for morbid obesity is widely performed around the world [ 1 ], with demonstrated effectiveness in improving type 2 diabetes mellitus (T2DM) [ 2 , 3 ]. Furthermore, the improvement effect on glycemic control after this surgery are observed prior to body weight loss, with the metabolic effects being markedly greater than can be explained by the loss of body weight alone. In recent years, "Metabolic Surgery" has been introduced as a new concept. However, it is not clear how this concept might apply differently to type 1 diabetes mellitus (T1DM) compared to T2DM.
T1DM is a disease in which pancreatic β-cells are destroyed and insulin secretion becomes impaired. Almost in the same way as T2DM, failure of glycemic control in the chronic phase of T1DM can lead to microangiopathy (retinopathy, nephropathy, neuropathy) and macroangiopathy (atherosclerosis), which can worsen the prognostic outcomes of patients. The main treatment for T1DM is insulin therapy. In recent years, the number of patients with morbid obesity and T1DM has increased. Bae et al. reported that analyzed electronic health records in the United States estimated that 47.8% of patients with T1DM are obese [ 4 ]. Several studies on the usefulness of bariatric surgery for these cases having emerged [ 5 , 6 , 7 , 8 , 9 ]. In Japan, only two studies have described the effect of bariatric surgery on slowly progressive insulin-dependent diabetes mellitus (SPIDDM), which is included in T1DM [ 10 , 11 ], and no studies on bariatric surgery for patients with severe obesity and T1DM with insulin secretion deficiency. In this case report, we describe the effectiveness of laparoscopic sleeve gastrectomy (LSG), by reducing the size of the stomach, in a patient with morbid obesity and T1DM, without endogenous insulin, achieving weight loss, a marked reduction in insulin requirement, and improved glycemic control.
A 36-year-old Japanese female was referred to our hospital with morbid obesity and T1DM. She was diagnosed with T1DM at the age of 6 years, thereafter, treatment with multiple daily insulin was started. By the age of 20 years, she had a body weight of 70 kg, increasing to > 100 kg at the age of 34 years. Her required daily dose of insulin increased as a function of her body weight. At her initial assessment, she required 45 units of insulin aspart and 30 units of insulin glargine per day. Although a temporary weight loss and reduction in daily insulin dose was achieved with an in-hospital treatment, her weight rebounded shortly after discharge and the patient experienced difficulty in controlling her body weight. The patient expressed her intention for surgical treatment for weight loss, and she was referred to our department.
At the time of admission, her height was 159 cm and her weight 106.7 kg, BMI of 42.2 kg/m 2 . Blood analyses indicated HbA1c of 9.0%, and blood C-peptide levels were undetectable (< 0.01 ng/mL), suggesting her insulin secretion capacity was completely depleted. With medication, her blood lipid levels were within normal range. On computed tomography (CT) examination, the calculated visceral fat area was 162.6 cm 2 , with a subcutaneous fat area of 527.9 cm 2 , measured at level of the umbilicus (Fig. 1 a, b). Upper gastrointestinal endoscopy revealed no abnormalities in the esophagus, stomach, or duodenum.
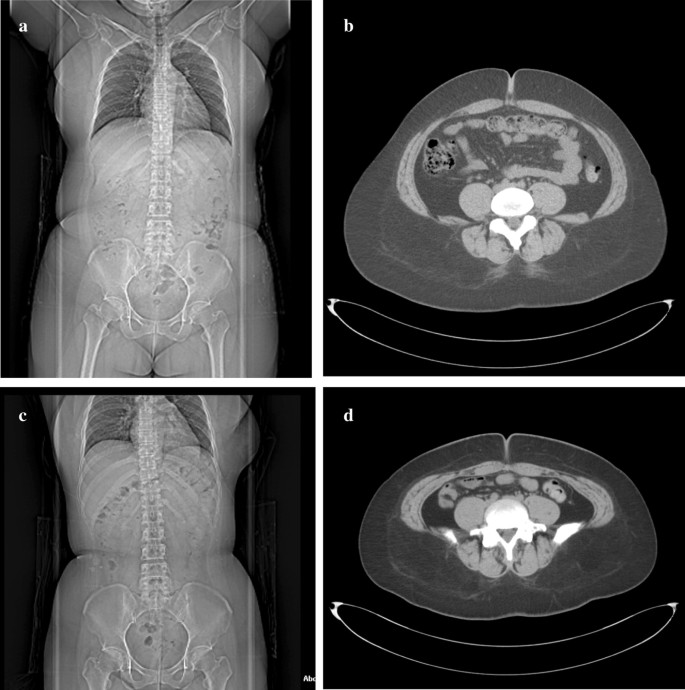
Computed tomography images. a Overall image before surgery, showing b a preoperative visceral fat area of 162.6 cm 2 and subcutaneous fat area of 527.9 cm 2 . c Overall image, 1-year after the surgical procedure, showing a decrease in d the visceral fat area to 44.8 cm 2 and the subcutaneous fat area to 408.8 cm 2
To prevent complications associated with rapid postoperative blood glucose improvement, she was admitted to our hospital 2 weeks before operation for strict glycemic control, dietary restrictions, and exercise therapy. As a result, preoperative HbA1c was reduced to 7.8% and body weight was reduced to 101.1 kg.
We performed a laparoscopic sleeve gastrectomy (LSG) [ 12 ], using five ports,, as shown in Fig. 2 a. The blood vessel along the wall of the greater curvature of the stomach was first dissected. We then inserted a 36 Fr (12 mm) bougie into the stomach and resected the greater curvature of the stomach, from a point, on the oral side, 4 cm from the pylorus to the His angle, using a linear stapler. The staple line was reinforced with continuous seromuscular sutures using non-absorbable stitches (Fig. 2 b, c).
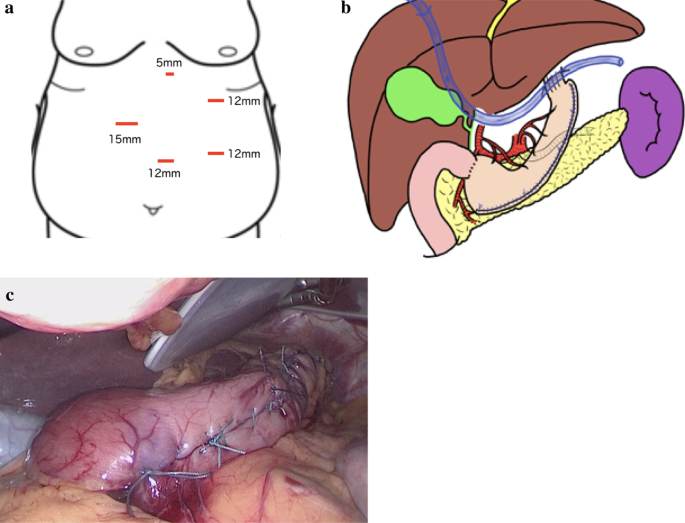
Surgical schema and gastric tube. a Schema of skin incisions (red lines), with the layout and size of ports shown. b Surgical schema, showing a drain placed below the left diaphragm. c Intraoperative photograph, with the complete gastric tube shown
After the operation, a unit of insulin aspart was mixed with 5 g of glucose contained in the infusion solution and sliding scale insulin was added as needed. From postoperative day 2, insulin glargine was administered. Sliding scale insulin was added depending on fasting blood sugar level and oral intake and her daily insulin dose was determined accordingly.
There were no postoperative complications, including severe hypoglycemic episodes. One year after the procedure, her body weight had decreased to 81.0 kg, with a BMI of 32.2 kg/m 2 , with this decrease being mainly due to a decrease in the body fat mass. Her HbA1c level improved to 7.7%, and her daily required insulin dose had been reduced to 24 units (10 units of insulin aspart and 14 units of insulin glargine per day: Fig. 3 a–d). On abdominal CT images, the visceral fat area, measured at level of the umbilicus, was 44.8 cm 2 , with a subcutaneous fat area of 408.8 cm 2 (Fig. 1 c, d). Therefore, there was a marked decrease in both visceral and subcutaneous fat.

Postoperative changes. The change, from preoperative to 12 months postoperatively, in a body weight, body mass index (BMI); b skeletal muscle mass and body fat mass; c HbA1c; and d insulin dose/day. At 1-year after the procedure, the patient’s body weight had decreased to 81 kg and her BMI to 32.2 kg/m 2 , mainly due to a decrease in body fat mass, with the skeletal muscle mass being maintained. The HbA1c level improved to 7.7%, and the daily insulin dose required reduced to 24 units
According to the International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO), about 340,000 bariatric surgeries were performed, worldwide, in 2008, with this number doubling by 2016 to over 680,000, most of which were performed laparoscopically [ 1 ]. In Japan, only LSG has been covered by national insurance since 2014, with the number of LSG procedures performed having increased every year since then. It is well known that bariatric surgery is effective for weight-loss effect, as well as improving T2DM for a prolonged period after surgery [ 2 , 3 ] and lowering the risk for obesity-related diseases, such as cardiovascular disorders [ 13 ]. However, there are few reports of the therapeutic effect of LSG in patients with T1DM, and it has not yet been elucidated and remains controversial.
T1DM is caused by the destruction of pancreatic β cells due to the interaction between genetic factors, environmental factors, and autoimmune mechanisms. According to a survey of the incidence of childhood T1DM in countries around the world, the age-adjusted incidence is high in Europe and in the United States, and low in Japan, at about 2.37 per 10,000 individuals [ 14 , 15 ]. T1DM presents with a variety of clinical features and is classified into three types, according to the mode of onset: typical acute-onset type; SPIDDM, which presents with T2DM pathology at the time of diagnosis and endogenous insulin secretion gradually decreases, with progression to insulin dependence; and fulminant type, characterized by a rapid destruction of pancreatic β cells, leading to severe hyperglycemia which can sometimes be fatal. For all three types of T1DM, insulin therapy is the main treatment. Poor glycemic control over a prolonged period of time causes microangiopathy (retinopathy, nephropathy, neuropathy) and macroangiopathy (atherosclerosis), as with T2DM, with a significant negative impact on patient prognosis.
The cause of poor glycemic control in T2DM is mainly due to obesity and insulin resistance. This is important to note as the rate of obesity among adults with T1DM has been increasing. In recent years, the concept of “double diabetes” [ 16 , 17 ] has been proposed. This is a new expression of the disease in children and adolescents, with the characteristics of a mixture of the two types of diabetes as patients with T1DM diagnosed in infancy acquire the T2DM factor from adolescence to adulthood. This mixed presentation induces obesity and insulin resistance, which leads to poor glycemic control and an increase in the amount of required daily insulin.
There have been a few reports on the efficacy of bariatric surgery in patients with morbid obesity and T1DM [ 5 , 6 , 7 , 8 , 9 ]. The systematic review by Chow et al. summarizes the outcomes of bariatric surgery in 86 patients with T1DM [ 5 ]. Before surgery, the average BMI was 42.5 ± 2.65 kg/m 2 , with an average HbA1c level of 8.46 ± 0.78% and average required insulin dose of 98 ± 26 IU/day. One year after surgery, the BMI had decreased to 29.55 ± 1.76 kg/m 2 , the HbA1c level to 7.95 ± 0.55%, and the required insulin dose to 36 ± 15 IU/day. Furthermore, the risk for obesity-related diseases had also been reduced after surgery [ 8 , 9 ].
In Japan, bariatric surgery for T1DM has been reported only for cases of SPIDDM [ 10 , 11 ]; in these cases, it was possible to reduce or discontinue insulin preparations and oral glycemic drugs after surgery. As an explanatory mechanism, the authors proposed that postoperative weight loss improved insulin resistance, resulting in a protective effect on residual pancreatic β cells. However, there has been no previous report of the effectiveness bariatric surgery in a case of morbid obesity associated with typical acute-onset T1DM, in which pancreatic β-cells were destroyed and endogenous insulin was depleted. This is the first case report of typical acute-onset T1DM with endogenous insulin depletion in Japan. In this case, weight loss and improved glycemic control were achieved in the postoperative follow up period, especially the amount of daily insulin requirement was decreased more dramatically than the weight reduction. This suggests that the observed metabolic effect is not just as a result of the restrictive effect of the surgery or due to the loss in body weight alone. In considering this mechanism of improvement, the concept of “double diabetes” [ 16 , 17 ] is thought to be useful. In other words, it is presumed that the effectiveness of the bariatric surgery is mediated by an improvement in the T2DM factor among patients with double diabetes. Ashrafian et al. reported that after bariatric surgery, β cell dysfunction persisted and, thus, patient still required baseline insulin therapy, although the overall insulin requirement was reduced [ 7 ]. Incretin hormones may also play an important role. In T2DM, change in the dynamics of incretin hormone secretion, such as glucagon-like peptide-1 (GLP-1), after gastric bypass surgery, contributes to the postoperative improvement in glycemic control [ 18 ]. It is plausible that incretin hormones may also contribute to the improvement of glucose metabolism in patients with T1DM after bariatric surgery through an inhibition of glucagon secretion via α cells, even in patients without residual β cells [ 19 ]. However, the underlying mechanisms remain to be elucidated.
Our case shows the possible usefulness of bariatric surgery for the treatment of patients with morbid obesity and T1DM, without endogenous insulin, to achieve postoperative weight loss and to improve glycemic control 1 year after surgery. On the other hand, Vilarrasa et al. described that HbA1c, which had improved in the first year after surgery, returned to the preoperative baseline after 5 years [ 6 ]; therefore, our case also requires long-term strict follow-up. Accumulation of more cases and evaluation of long-term results are warranted to improve our understanding of the role of bariatric surgery for patients with obesity and T1DM.
In the short term, LSG would provide an effective treatment strategy for patients with morbid obesity and T1DM to achieve body weight loss, improve HbA1c level, and reduce the required daily insulin dose.
Availability of data and materials
The dataset supporting the conclusions of this article is included within the article.
Abbreviations
Type 2 diabetes mellitus
- Type 1 diabetes mellitus
- Laparoscopic sleeve gastrectomy
Computed tomography
Slow progressive insulin dependent diabetes mellitus
Glucagon-like peptide-1
Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, et al. IFSO worldwide survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
Article Google Scholar
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, et al. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–133.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Brethauer SA, Navaneethan SD, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376:641–51.
Bae JP, Lage MJ, Mo D, Nelson DR, Hoogwerf BJ. Obesity and glycemic control in patients with diabetes mellitus: Analysis of physician electronic health records in the US from 2009–2011. J Diabetes Complications. 2016;30:212–20.
Article CAS Google Scholar
Chow A, Switzer NJ, Dang J, Shi X, de Gara C, Birch DW, et al. A systematic review and meta-analysis of outcomes for type 1 diabetes after bariatric surgery. J Obes. 2016;2016:6170719.
Vilarrasa N, Rubio MA, Miñambres I, Flores L, Caixàs A, Ciudin A, et al. Long-term outcomes in patients with morbid obesity and type 1 diabetes undergoing bariatric surgery. Obes Surg. 2017;27:856–63.
Ashrafian H, Harling L, Toma T, Athanasiou C, Nikiteas N, Efthimiou E, et al. Type 1 diabetes mellitus and bariatric surgery: a systematic review and meta-analysis. Obes Surg. 2016;26:1697–704.
Brethauer SA, Aminian A, Rosenthal RJ, Kirwan JP, Kashyap SR, Schauer PR. Bariatric surgery improves the metabolic profile of morbidly obese patients with type 1 diabetes. Diabetes Care. 2014;37:E51–E5252.
Robert M, Belanger P, Hould FS, Marceau S, Tchernof A, Biertho L. Should metabolic surgery be offered in morbidly obese patients with type I diabetes? Surg Obes Relat Dis. 2015;11:798–805.
Hironaka JY, Kitahama S, Sato H, Inoue M, Takahashi T, Tamori Y. Sleeve gastrectomy induced remission of slowly progressive type 1 diabetes in a morbidly obese Japanese patient. Intern Med. 2019;58:675–8.
Uno K, Seki Y, Kasama K, Wakamatsu K, Hashimoto K, Umezawa A, et al. Mid-term results of bariatric surgery in morbidly obese Japanese patients with slow progressive autoimmune diabetes. Asian J Endosc Surg. 2018;11:238–43.
Gumbs AA, Gagner M, Dakin G, Pomp A. Sleeve gastrectomy for morbid obesity. Obes Surg. 2007;17:962–9.
Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–93.
DIAMOND Project Group. Incidence and trends of childhood type 1diabetes worldwide 1990–1999. Diabet Med. 2006;23:857–66.
Onda Y, Sugihara S, Ogata T, Yokoya S, Yokoyama T, Tajima N, et al. Incidence and prevalence of childhood-onset type 1 diabetes in Japan: the T1D study. Diabet Med. 2017;34:909–15.
Pozzilli P, Buzzetti R. A new expression of diabetes: double diabetes. Trends Endocrinol Metab. 2007;18:52–7.
Libman IM, Becker DJ. Coexistence of type 1 and type 2 diabetes mellitus: “double” diabetes? Pediatr Diabetes. 2003;4:110–3.
Laferrère B. Diabetes remission after bariatric surgery: is it just the incretins? Int J Obes Suppl. 2011;35:22–5.
Kirwan JP, Aminian A, Kashyap SR, Burguera B, Brethauer SA, Schauer PR, et al. Bariatric surgery in obese patients with type 1 diabetes. Diabetes Care. 2016;39:941–8.
Download references
Acknowledgements
We would like to thank Editage ( https://www.editage.jp ) for English language editing.
The authors declare that they have no funding.
Author information
Authors and affiliations.
Department of Surgery, Tohoku University Graduate School of Medicine, Seiryo-machi, Aoba-ku, Sendai, 980-8574, Japan
Hidetaka Ichikawa, Hirofumi Imoto, Naoki Tanaka, Hiroaki Musha, Takeshi Naitoh, Takashi Kamei & Michiaki Unno
Department of Metabolism and Diabetes, Tohoku University Graduate School of Medicine, 1-1, Seiryo-machi, Aoba-ku, Sendai, 980-8574, Japan
Shojiro Sawada
Department of Colorectal Surgery, Kitasato University School of Medicine, 1-15-1, Kitasato, Minami-ku, Sagamihara, 252-0374, Japan
Takeshi Naitoh
Department of Diabetes and Metabolism, Tohoku Medical and Pharmaceutical University, Fukumuro, Miyagino-ku, Sendai, 983-8512, Japan
You can also search for this author in PubMed Google Scholar
Contributions
HI contributed to drafting the manuscript and study design and concept. HI, HI, NT, HM, SS, TN, TK, and MU performed critical revision of the manuscript. MU provided final approval of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Hirofumi Imoto .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Ichikawa, H., Imoto, H., Tanaka, N. et al. Efficacy of laparoscopic sleeve gastrectomy for patient with morbid obesity and type 1 diabetes mellitus: a case report. surg case rep 7 , 7 (2021). https://doi.org/10.1186/s40792-020-00989-5
Download citation
Received : 11 June 2020
Accepted : 18 September 2020
Published : 06 January 2021
DOI : https://doi.org/10.1186/s40792-020-00989-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Morbid obesity
- Metabolic surgery
An official website of the United States government The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
Save citation to fileEmail citation, add to collections.
Add to My BibliographyYour saved search, create a file for external citation management software, your rss feed.
Long-term systemic effects of metabolic bariatric surgery: A multidisciplinary perspectiveAffiliations.
Background: Obesity is a global health crisis with profound implications on various body systems, contributing to a series of comorbidities. Metabolic Bariatric Surgery (MBS) has emerged as an effective treatment option for severe obesity, with significant weight reduction and potential systemic physiological alterations. Objectives: This narrative review aims to provide a comprehensive analysis of the long-term effects of MBS on a wide array of body systems, including the heart, liver, kidneys, reproductive system, skin, lungs, digestive tract, pancreas, and blood, as well as related cancers of these organs. Methods: A systematic search was conducted in academic databases (PubMed, ISI Web of Science, and Scopus) for observational studies and reviews published between July 2000 and December 2023, investigating the association between MBS and the subsequent function of different organ systems. High-quality studies were prioritized to ensure reliable evidence synthesis. Results: MBS has demonstrated favorable outcomes in reducing cardiovascular disease risk, improving cardiac function, and alleviating heart failure symptoms. It has also been associated with improved respiratory function, remission of obstructive sleep apnea, and reduced cancer incidence and mortality. Additionally, MBS has shown benefits in managing gastrointestinal disorders, enhancing glycemic control, and promoting pancreatic beta-cell regeneration in type 2 diabetes mellitus. However, some methods of MBS are associated with a higher risk of cholelithiasis, GERD, and pancreatic exocrine insufficiency. Conclusion: MBS has far-reaching systemic effects beyond weight loss, offering potential long-term benefits for various organ systems and comorbidities associated with obesity. For many patients with severe obesity, the potential benefits of Metabolic and Bariatric Surgery (MBS) can outweigh the associated risks. However, careful evaluation by a qualified healthcare professional is crucial to determine candidacy and ensure a successful outcome. Further research is needed to fully elucidate the long-term impacts and tailor personalized treatment approaches. Keywords: Bariatric surgery; Cardiovascular system; Digestive system; Kidney; Liver; Long-term care; Metabolic diseases; Neoplasms; Obesity; Organ systems. © 2024 The Authors. PubMed Disclaimer Conflict of interest statementThe authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Summary of the long-term effects… Summary of the long-term effects of MBS on various body organs and diseases. Similar articles
Publication types
LinkOut - more resourcesFull text sources.

NCBI Literature Resources MeSH PMC Bookshelf Disclaimer The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited. CASE REPORT articleClinical challenge: patient with severe obesity bmi 46 kg/m 2. 
Obesity causes and exacerbates many disease processes and affects every organ system. Thus it is not surprising that clinical providers are often overwhelmed with the multitude of symptomatology upon initial presentation in patients with obesity. However, despite a “complicated medical history,” a systematic, organized approach in obesity medicine utilizes a personalized-tailored treatment strategy coupled with understanding of the disease state, presence of comorbidities, contraindications, side effects, and patient preferences. Here, we present the case of a young patient with Class 3b severe obesity, several obesity-related complications, and extensive psychological history. Through synergistic and additive treatments (behavioral/nutritional therapy combined with anti-obesity pharmacotherapy and concurrent enrollment in our bariatric surgery program), the patient was able to achieve significant −30.5% total body weight loss with improvement of metabolic parameters. Though these results are not typical of all patients, we must emphasize the need to encompass all available anti-obesity therapies (lifestyle, pharmacotherapy, medical devices, bariatric surgery in monotherapy or combination) in cases of refractory or severe obesity, as we do similarly for other disease modalities such as refractory hypertension or poorly controlled Type 2 diabetes that requires robust escalation in therapy. Clinical ChallengeA 31 year old patient with a past medical history of Class 3 obesity BMI 46 kg/m 2 , Type 2 diabetes mellitus (A1c <5.7%, well controlled on metformin), polycystic ovarian syndrome, non-alcoholic steatosis of the liver, pulmonary and neurosarcoidosis on infliximab and methotrexate, and chronic worsening pain presents for weight management evaluation. She had a history of opioid use disorder due to the chronic pain, though in remission. She had been on several weight-promoting pain medications for symptom control, including gabapentin, duloxetine and nortriptyline. Contributing factors over the years to her weight gain also included her diagnosis of Bipolar Disorder with antipsychotic medication-induced weight gain (previously trialed aripiprazole, responded to lurasidone with decreasing efficiency, and now finally stable on paliperidone though weight gain promoting). Her highest adult weight was her current weight of 295 pounds with a lowest adult weight of 140 lbs. that pre-dated her Bipolar and sarcoidosis diagnoses several years ago. She had stable eating patterns, and often chose healthy meals such as hummus, vegetables, Greek salads, and lean meats, though had a weakness for sweet cravings. She engaged in structured gym exercise for 30 minutes three times per week despite the chronic pain. Recent stressors included her close aunt who had been diagnosed with cancer. She also suffered from insomnia and had been evaluated closely with sleep therapists and sleep hygiene specialists. Her polysomnogram was negative for sleep apnea. What Would You Do Next?A. Offer more aggressive intensive lifestyle therapy intervention B. Trial of anti-obesity medication if option A above becomes ineffective C. Metabolic and bariatric surgery only as anti-obesity medication would be contraindicated given her history of opioid use D. Trial of anti-obesity medication for 3 months with concurrent referral to bariatric surgery The patient depicted in the case has chronic, debilitating severe obesity classification with several inflammatory obesity-related comorbidities and other contributing etiology to her weight gain. In regards to lifestyle intervention, the patient was started on a healthy low fat high fiber diet with increased consumption of vegetables, while minimizing intake of processed foods, added sugar, trans fats, and refined flours ( 1 ). Nutrient-dense whole foods prepared at home were encouraged. Acceptable macronutrient distribution range is 45–65% carbohydrates, 20–35% total fat of which <10% should be polyunsaturated fats, and 10–35% protein and amino acids 1 . However, obesity-related comorbidities such as type 2 diabetes mellitus, polycystic ovarian syndrome, and non-alcoholic steatosis of the liver suggesting features of insulin resistance need to be taken into consideration when implementing dietary modifications specific to this case. The patient's daily carbohydrate intake should be reduced to 40–50% to combat insulin resistance. Several studies have shown improvement in metabolic parameters and more rapid weight loss when a low carbohydrate diet was implemented initially in the first 3–6 months ( 2 , 3 ). At presentation, the patient's calculated daily protein intake was <20% of total daily intake and increasing her protein intake to 30% reduced her sweet cravings and increased satiety. In addition, she would benefit from at least 150 min per week of structured moderately intensive exercise as tolerated as recommended by The American College of Sports Medicine ( 4 ). Of note, the patient is also under significant stressors. Stress has been very strongly linked to hyperphagia, binging, and obesity ( 5 , 6 ). Stress management would also provide long-term strategies for emotional/stress eating should they arise. Her sleep has been adequately addressed by a specialist multidisciplinary team. Further, the patient was already under intense behavioral therapy given her underlying psychiatric illness. Early behavioral therapy intervention should be strongly considered in patients with adverse psychological factors, eating disorders and underlying psychiatric conditions that would otherwise impede their overall progress toward health goals. However, it may be difficult to promote more aggressive lifestyle intervention alone, especially in a patient with an advanced obesity disease staging who is already making strides to eat healthy and undergoing behavioral therapy. Furthermore, the patient also meets criteria for initiation of anti-obesity pharmacotherapy (AOM): BMI >27 kg/m 2 plus the presence of one obesity-related comorbidity and/or BMI >30 kg/m 2 in conjunction with lifestyle intervention ( 7 , 8 ). Though the patient has a history of opioid use disorder, it is in remission and there is no active contraindication to AOM. The patient also does not have underlying heart disease, end-stage-renal disease, or acute angle glaucoma that would negate use of several AOM such as phentermine/topiramate, lorcaserin, and naltrexone/bupropion. Liraglutide 3.0 mg would be a first option given its double benefits in patients with severe obesity and diabetes ( 7 ) and other obesity-related comorbidities such as fatty liver ( 9 ) and polycystic ovarian disease ( 10 ). The medication is also generally well-tolerated and safe. Because anti-obesity medications can exert central effects in a patient with Bipolar Disorder, close monitoring and communication with the patient's psychiatrist would be critical. Because her BMI is already very elevated, clinically, both lifestyle changes and pharmacological treatment would be implemented together, rather than separately. Moreover, based on her current body mass index alone of 40 kg/m 2 , the patient meets National Institutes of Health consensus criteria for metabolic and bariatric surgery ( 11 ): BMI 35 kg/m 2 in the presence of at least one obesity-related comorbidity or BMI 40 kg/m 2 . Therefore, it would be prudent to discuss bariatric surgery in this patient given her disease severity. The correct answer is D. The patient was actually started on AOM with concurrent referral to the institution's bariatric surgery program. Since the patient's insurance did not provide coverage for liraglutide 3.0 mg, she was alternatively prescribed a combination anti-obesity medication therapy (phentermine/topiramate) after discussion with her psychiatrist and other specialists. AOM were instrumental in improving the patient's overall hunger drive, cravings, and satiety. Despite being the best option for her at presentation, the patient was unwilling to undergo the bariatric procedure. Oftentimes, this may be the case in many patients until they consent to surgical intervention or have weight regain on non-surgical therapy. Future guidelines may need to be more definitive about earlier referral to bariatric surgery. The patient continued AOM long-term, having lost 90 pounds over a 2 year time period ( Figure 1 ). Her BMI now is 28.7 kg/m 2 , weight 205 lbs. (reversed from Class 3 obesity, BMI 46 kg/m 2 , weight 295 lbs.) with improvement in quality of life and obesity-related comorbidities. Liver transaminases that were previously elevated in the context of fatty liver disease normalized along with return of regular menstrual cycles. In the process of losing weight with related attenuation in disease comorbidity and metabolic profile improvement, the patient's neurosarcoidosis continued to show remarkable recovery with stabilization of her mental health conditions and disability. Her specialists reported that this was the best she had been in many years. The patient lost −30.5% of her total body weight, which is typical weight loss achieved by metabolic and bariatric surgery means, through non-surgical intervention. 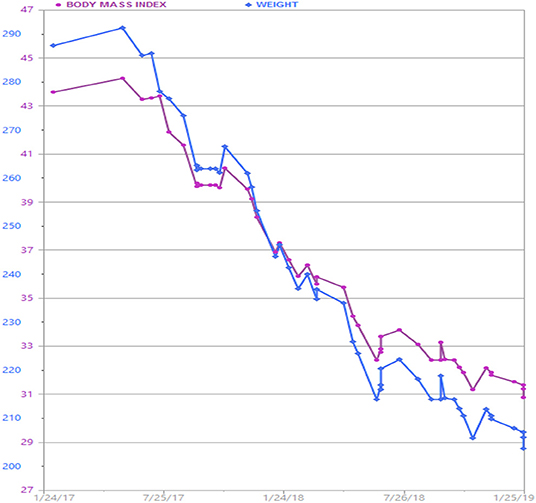 Figure 1 . Patient's weight graph derived from the electronic health record. The patient lost a total of 90 lbs. over a 2 year time period with adjunctive anti-obesity pharmacotherapy (phentermine/topiramate) in combination with behavioral and lifestyle intervention. Though these results may not be usual for all patients, it is important to note that all treatment modalities (behavioral, lifestyle, pharmacological, and/or surgical whether as monotherapy or in combination) must be utilized for patients suffering with severe obesity and its devastating consequences on overall health and quality of life. Many of these patients present with complicated disease states and multiple comorbidities. Thus, important health targets include not only weight loss but treatment-enhanced double benefits leading to improvement of comorbidities. Data Availability StatementAll datasets for this study were directly generated from the patient's electronic health record and are available upon request. Informed ConsentWritten informed consent to publish this case report was obtained from the patient. Author ContributionsGS and CA contributed and edited the contents of this manuscript. No external funding was provided for the creation of this manuscript. Conflict of InterestGS served as a consultant for Johnson and Johnson and advisor for Rhythm Pharmaceuticals. CA reports grants from Aspire Bariatrics, Myos, the Vela Foundation, the Dr. Robert C. and Veronica Atkins Foundation, Coherence Lab, Energesis, NIH, and PCORI, grants and personal fees from Orexigen, GI Dynamics, Takeda, personal fees from Nutrisystem, Zafgen, Sanofi-Aventis, NovoNordisk, Scientific Intake, Xeno Biosciences, Rhythm Pharmaceuticals, Eisai, EnteroMedics, Bariatrix Nutrition, and other from Science-Smart LLC, outside the submitted work. AcknowledgmentsWe would like to thank the patient for permission to publish. 1. ^ http://www.nationalacademies.org/hmd/~/media/Files/ActivityFiles/Nutrition/DRI-Tables/8_MacronutrientSummary.pdf?la=en (accessed April 2, 2019). 1. Gardner CD, Trepanowski JF, Del Gobbo LC, Hauser ME, Rigdon J, Ioannidis JPA, et al. Effect of low-fat vs low-carbohydrate diet on 12-month weight loss in overweight adults and the association with genotype pattern or insulin secretion: the DIETFITS randomized clinical trial. JAMA . (2018) 319:667–79. doi: 10.1001/jama.2018.0245 PubMed Abstract | CrossRef Full Text | Google Scholar 2. Meng Y, Bai H, Wang S, Li Z, Wang Q, Chen L. Efficacy of low carbohydrate diet for type 2 diabetes mellitus management: a systematic review and meta-analysis of randomized controlled trials. Diabetes Res Clin Pract. (2017) 131:124–31. doi: 10.1016/j.diabres.2017.07.006 3. Jang EC, Jun DW, Lee SM, Cho YK, Ahn SB. Comparison of efficacy of low-carbohydrate and low-fat diet education programs in non-alcoholic fatty liver disease: A randomized controlled study. Hepatol Res. (2018) 48:E22–9. doi: 10.1111/hepr.12918 4. Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. (2011) 43:1334–59. doi: 10.1249/MSS.0b013e318213fefb 5. Manna P, Jain SK. Obesity, oxidative stress, adipose tissue dysfunction, and the associated health risks: causes and therapeutic strategies. Metab Syndr Relat Disord. (2015) 13:423–44. doi: 10.1089/met.2015.0095 6. Razzoli M, Pearson C, Crow S, Bartolomucci A. Stress, overeating, and obesity: Insights from human studies and preclinical models. Neurosci Biobehav Rev. (2017) 76:154–62. doi: 10.1016/j.neubiorev.2017.01.026 7. Srivastava G, Apovian CM. Current pharmacotherapy for obesity. Nat Rev Endocrinol. (2018) 14:12–24. doi: 10.1038/nrendo.2017.122 8. Apovian CM, Aronne LJ, Bessesen DH, McDonnell ME, Murad MH, Pagotto U, et al. Pharmacological management of obesity: an endocrine Society clinical practice guideline. J Clin Endocrinol Metab. (2015) 100:342–62. doi: 10.1210/jc.2014-3415 9. Khoo J, Hsiang JC, Taneja R, Koo SH, Soon GH, Kam CJ, et al. Randomized trial comparing effects of weight loss by liraglutide with lifestyle modification in non-alcoholic fatty liver disease. Liver Int. (2019) 39:941–9. doi: 10.1111/liv.14065 10. Nylander M, Frossing S, Clausen HV, Kistorp C, Faber J, Skouby SO. Effects of liraglutide on ovarian dysfunction in polycystic ovary syndrome: a randomized clinical trial. Reprod Biomed Online. (2017) 35:121–7. doi: 10.1016/j.rbmo.2017.03.023 11. Clinical guidelines on the identification evaluation and treatment of overweight and obesity in adults–the evidence report. National Institutes of Health. Obes Res. (1998) 6(Suppl.2):51S–209S. Google Scholar Keywords: anti-obesity medications, weight loss drugs, combination therapy, bariatric surgery, lifestyle intervention Citation: Srivastava G and Apovian CM (2019) Clinical Challenge: Patient With Severe Obesity BMI 46 kg/m 2 . Front. Endocrinol. 10:635. doi: 10.3389/fendo.2019.00635 Received: 30 April 2019; Accepted: 03 September 2019; Published: 02 October 2019. Reviewed by: Copyright © 2019 Srivastava and Apovian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms. *Correspondence: Gitanjali Srivastava, geet5sri@gmail.com Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher. Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Epidemiology and Population Health Evidence from big data in obesity research: international case studies
International Journal of Obesity volume 44 , pages 1028–1040 ( 2020 ) Cite this article 976 Accesses 4 Citations 8 Altmetric Metrics details
Background/objectiveObesity is thought to be the product of over 100 different factors, interacting as a complex system over multiple levels. Understanding the drivers of obesity requires considerable data, which are challenging, costly and time-consuming to collect through traditional means. Use of ‘big data’ presents a potential solution to this challenge. Big data is defined by Delphi consensus as: always digital , has a large sample size, and a large volume or variety or velocity of variables that require additional computing power (Vogel et al. Int J Obes. 2019). ‘Additional computing power’ introduces the concept of big data analytics. The aim of this paper is to showcase international research case studies presented during a seminar series held by the Economic and Social Research Council (ESRC) Strategic Network for Obesity in the UK. These are intended to provide an in-depth view of how big data can be used in obesity research, and the specific benefits, limitations and challenges encountered. Methods and resultsThree case studies are presented. The first investigated the influence of the built environment on physical activity. It used spatial data on green spaces and exercise facilities alongside individual-level data on physical activity and swipe card entry to leisure centres, collected as part of a local authority exercise class initiative. The second used a variety of linked electronic health datasets to investigate associations between obesity surgery and the risk of developing cancer. The third used data on tax parcel values alongside data from the Seattle Obesity Study to investigate sociodemographic determinants of obesity in Seattle. ConclusionsThe case studies demonstrated how big data could be used to augment traditional data to capture a broader range of variables in the obesity system. They also showed that big data can present improvements over traditional data in relation to size, coverage, temporality, and objectivity of measures. However, the case studies also encountered challenges or limitations; particularly in relation to hidden/unforeseen biases and lack of contextual information. Overall, despite challenges, big data presents a relatively untapped resource that shows promise in helping to understand drivers of obesity. This is a preview of subscription content, access via your institution Access optionsSubscribe to this journal Receive 12 print issues and online access 251,40 € per year only 20,95 € per issue Buy this article
Prices may be subject to local taxes which are calculated during checkout Similar content being viewed by others Non-traditional data sources in obesity research: a systematic review of their use in the study of obesogenic environments Trends in the prevalence of adult overweight and obesity in Australia, and its association with geographic remoteness Cross-sectional evidence of the cardiometabolic health benefits of urban liveability in AustraliaDavison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–71. Article CAS PubMed PubMed Central Google Scholar Egger G, Swinburn B. An “ecological” approach to the obesity pandemic. BMJ. 1997;315:477–80. Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J, et al. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: the six-Cs model. Child Dev Perspect. 2011;5:50–8. Article Google Scholar Butland B, Jebb S, Kopelman P, McPherson K, Thomas S, Mardell J et al. Foresight. Tackling obesities: future choices—project report. Government Office for Science; 2007. Rutter HR, Bes-Rastrollo M, de Henauw S, Lahti-Koski M, Lehtinen-Jacks S, Mullerova D, et al. Balancing upstream and downstream measures to tackle the obesity epidemic: a position statement from the European association for the study of obesity. Obes Facts. 2017;10:61–3. Article PubMed PubMed Central Google Scholar Mittelstadt BD, Floridi L. The ethics of big data: current and foreseeable issues in biomedical contexts. Sci Eng Ethics. 2016;22:303–41. Article PubMed Google Scholar Kaisler S, Armour F, Espinosa JA, Money W. Big data: issues and challenges moving forward. In: Proceedings of the 46th Hawaii International Conference on System Sciences. Association for Computing Machinery Digital Library; 2013. p. 995–1004. Herland M, Khoshgoftaar TM, Wald R. A review of data mining using big data in health informatics. J Big Data. 2014;1: https://doi.org/10.1186/2196-1115-1-2 . Vogel C, Zwolinsky S, Griffiths C, Hobbs M, Henderson E, Wilkins E. A Delphi study to build consensus on the definition and use of big data in obesity research. Int J Obes. 2019. https://doi.org/10.1038/s41366-018-0313-9 . Morris M, Birkin M. The ESRC strategic network for obesity: tackling obesity with big data. Int J Obes. 2018;42:1948–50. Timmins K, Green M, Radley D, Morris M, Pearce J. How has big data contributed to obesity research? A review of the literature. Int J Obes. 2018;42:1951–62. Monsivais P, Francis O, Lovelace R, Chang M, Strachan E, Burgoine T. Data visualisation to support obesity policy: case studies of data tools for planning and transport policy in the UK. Int J Obes. 2018;42:1977–86. Morris M, Wilkins E, Timmins K, Bryant M, Birkin M, Griffiths C. Can big data solve a big problem? Reporting the obesity data landscape in line with the Foresight obesity system map. Int J Obes. 2018;42:1963–76. Vayena E, Salathé M, Madoff LC, Brownstein JS. Ethical challenges of big data in public health. PLOS Comput Biol. 2015;11:e1003904. Article PubMed PubMed Central CAS Google Scholar Silver LD, Ng SW, Ryan-Ibarra S, Taillie LS, Induni M, Miles DR, et al. Changes in prices, sales, consumer spending, and beverage consumption one year after a tax on sugar-sweetened beverages in Berkeley, California, US: a before-and-after study. PLoS Med. 2017;14:e1002283. Gore RJ, Diallo S, Padilla J. You are what you tweet: connecting the geographic variation in america’s obesity rate to Twitter content. PLoS ONE. 2015;10:e0133505. Nguyen QC, Li D, Meng H-W, Kath S, Nsoesie E, Li F, et al. Building a national neighborhood dataset from geotagged Twitter data for indicators of happiness, diet, and physical activity. JMIR Public Health Surveill. 2016;2:e158. Hirsch JA, James P, Robinson JR, Eastman KM, Conley KD, Evenson KR, et al. Using MapMyFitness to place physical activity into neighborhood context. Front Public Health. 2014;2:1–9. Althoff T, Hicks JL, King AC, Delp SL, Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547:336–9. Kerr NL. HARKing: hypothesizing after the results are known. Pers Soc Psychol Rev. 1998;2:196–217. Article CAS PubMed Google Scholar Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–29. Bennett JE, Li G, Foreman K, Best N, Kontis V, Pearson C, et al. The future of life expectancy and life expectancy inequalities in England and Wales: Bayesian spatiotemporal forecasting. Lancet. 2015;386:163–70. World Health Organisation. Report of the Commission on ending childhood obesity. Geneva, Switzerland: World Health Organisation; 2016. Centers for Disease Control and Prevention. Recommended community strategies and measurements to prevent obesity in the United States. Atlanta, GA, U.S.: Centers for Disease Control and Prevention; 2009. Local Government Association. Building the foundations: tackling obesity through planning and development. London, UK: Local Government Association; 2016. Burgoine T, Alvanides S, Lake AA. Creating ‘obesogenic realities’; Do our methodological choices make a difference when measuring the food environment? Int J Health Geogr. 2013;12. https://doi.org/10.1186/1476-072X-12-33 . Wilkins E, Morris M, Radley D, Griffiths C. Methods of measuring associations between the Retail Food Environment and weight status: Importance of classifications and metrics. SSM Popul Health. 2019. https://doi.org/10.1016/j.ssmph.2019.100404 . Bardou M, Barkun AN, Martel M. Obesity and colorectal cancer. Gut. 2013;62:933–47. Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64:104–17. Derogar M, Hull MA, Kant P, Östlund M, Lu Y, Lagergren J. Increased risk of colorectal cancer after obesity surgery. Ann Surg. 2013;258:983–8. Kant P, Hull MA. Excess body weight and obesity—the link with gastrointestinal and hepatobiliary cancer. Nat Rev Gastroenterol Hepatol. 2011;8:224–38. Östlund MP, Lu Y, Lagergren J. Risk of obesity-related cancer after obesity surgery in a population-based cohort study. Ann Surg. 2010;252:972–6. Sainsbury A, Goodlad RA, Perry SL, Pollard SG, Robins GG, Hull MA. Increased colorectal epithelial cell proliferation and crypt fission associated with obesity and roux-en-Y gastric bypass. Cancer Epidemiol Biomark Prev. 2008;17:1401–10. Article CAS Google Scholar Aravani A, Downing A, Thomas JD, Lagergren J, Morris EJA, Hull MA. Obesity surgery and risk of colorectal and other obesity-related cancers: an English population-based cohort study. Cancer Epidemiol. 2018;53:99–104. Openshaw S. The modifiable areal unit problem. In: Concepts and techniques in modern geography. Norwich: Geo Books; 1984. p. 1–41. Kwan M-P. The uncertain geographic context problem. Ann Assoc Am Geogr. 2012;102:958–68. Di Zhu X, Yang Y, Liu X. The importance of housing to the accumulation of household net wealth. Harvard, USA: Joint Center for Housing Studies, Harvard University; 2003. Rehm CD, Moudon AV, Hurvitz PM, Drewnowski A. Residential property values are associated with obesity among women in King County, WA, USA. Soc Sci Med. 2012;75:491–5. Drewnowski A, Buszkiewicz J, Aggarwal A. Soda, salad, and socioeconomic status: findings from the Seattle Obesity Study (SOS). SSM Popul Health. 2019;7:e100339. Birkin M, Morris MA, Birkin TM, Lovelace R. Using census data in microsimulation modelling. In: Stillwell J, Duke-Williams O, editors. The Routledge handbook of census resources, methods and applications. 1st ed. Routledge: IJO publication; 2018. Jiao J, Drewnowski A, Moudon AV, Aggarwal A, Oppert J-M, Charreire H, et al. The impact of area residential property values on self-rated health: a cross-sectional comparative study of Seattle and Paris. Prev Med Rep. 2016;4:68–74. Nguyen DM, El-Serag HB. The epidemiology of obesity. Gastroenterol Clinics. 2010;39:1–7. Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Commun Health. 2001;55:111–22. Timperio A, Salmon J, Telford A, Crawford D. Perceptions of local neighbourhood environments and their relationship to childhood overweight and obesity. Int J Obes. 2005;29:170–5. Roda C, Charreire H, Feuillet T, Mackenbach JD, Compernolle S, Glonti K, et al. Mismatch between perceived and objectively measured environmental obesogenic features in European neighbourhoods. Obes Rev. 2016;17 S1:31–41. Drewnowski A, Arterburn D, Zane J, Aggarwal A, Gupta S, Hurvitz PM, et al. The Moving to Health (M2H) approach to natural experiment research: a paradigm shift for studies on built environment and health. SSM Popul Health. 2019;7:100345. Bourassa SC, Cantoni E, Hoesli M. Predicting house prices with spatial dependence a comparison of alternative methods. J Real Estate Res. 2010;32:139–60. Google Scholar Wilkins EL, Radley D, Morris MA, Griffiths C. Examining the validity and utility of two secondary sources of food environment data against street audits in England. Nutr J. 2017;16:1–13. Nevalainen J, Erkkola M, Saarijarvi H, Nappila T, Fogelholm M. Large-scale loyalty card data in health research. Digit Health. 2018;4:2055207618816898. PubMed PubMed Central Google Scholar Aiello L, Schifanello R, Quercia D, Del Prete L. Large-scale and high-resolution analysis of food purchases and health outcomes. EPJ Data Sci. 2019;8:14. Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35:1381–95. Zwolinsky S, McKenna J, Pringle A, Widdop P, Griffiths C, Mellis M, et al. Physical activity and sedentary behavior clustering: segmentation to optimize active lifestyles. J Phys Act Health. 2016;13:921–8. Bauman A, Ainsworth BE, Sallis JF, Hagströmer M, Craig CL, Bull FC, et al. The descriptive epidemiology of sitting: a 20-country comparison using the International Physical Activity Questionnaire (IPAQ). Am J Prev Med. 2011;41:228–35. Guerin PB, Diiriye RO, Corrigan C, Guerin B. Physical activity programs for refugee somali women: working out in a new country. Women & Health. 2003;38:83–99. Pope L, Harvey J. The efficacy of incentives to motivate continued fitness-center attendance in college first-year students: a randomized controlled trial. J Am Coll Health. 2014;62:81–90. Cetateanu A, Jones A. Understanding the relationship between food environments, deprivation and childhood overweight and obesity: evidence from a cross sectional England-wide study. Health Place. 2014;27:68–76. Harrison F, Burgoine T, Corder K, van Sluijs EM, Jones A. How well do modelled routes to school record the environments children are exposed to? A cross-sectional comparison of GIS-modelled and GPS-measured routes to school. Int J Health Geogr. 2014;13:5. Ells LJ, Macknight N, Wilkinson JR. Obesity surgery in England: an examination of the health episode statistics 1996–2005. Obes Surg. 2007;17:400–5. Nielsen JDJ, Laverty AA, Millett C, Mainous AG, Majeed A, Saxena S. Rising obesity-related hospital admissions among children and young people in England: National time trends study. PLoS ONE. 2013;8:e65764. Smittenaar C, Petersen K, Stewart K, Moitt N. Cancer incidence and mortality projections in the UK until 2035. Br J Cancer. 2016;115:1147–55. Wallington M, Saxon EB, Bomb M, Smittenaar R, Wickenden M, McPhail S, et al. 30-day mortality after systemic anticancer treatment for breast and lung cancer in England: a population-based, observational study. The Lancet Oncol. 2016;17:1203–16. Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: Linked national database study. BMJ. 2012;344:d8059. Hanratty B, Lowson E, Grande G, Payne S, Addington-Hall J, Valtorta N, et al. Transitions at the end of life for older adults–patient, carer and professional perspectives: A mixed-methods study. Health Serv Deliv Res. 2014. https://doi.org/10.3310/hsdr02170 . Aggarwal A, Monsivais P, Cook AJ, Drewnowski A. Does diet cost mediate the relation between socioeconomic position and diet quality? Eur J Clin Nutr. 2011;65:1059–66. Drewnowski A, Aggarwal A, Tang W, Moudon AV. Residential property values predict prevalent obesity but do not predict 1-year weight change. Obesity. 2015;23:671–6. Download references AcknowledgementsThe ESRC Strategic Network for Obesity was funded via ESRC grant number ES/N00941X/1. The authors would like to thank all of the network investigators ( https://www.cdrc.ac.uk/research/obesity/investigators/ ) and members ( https://www.cdrc.ac.uk/research/obesity/network-members/ ) for their participation in network meetings and discussion which contributed to the development of this paper. Author informationAuthors and affiliations. Leeds Institute for Data Analytics and School of Medicine, University of Leeds, Leeds, UK Emma Wilkins, Ariadni Aravani, Amy Downing & Michelle A. Morris Center for Public Health Nutrition, University of Washington, Seattle, WA, USA Adam Drewnowski School of Sport, Leeds Beckett University, Leeds, UK Claire Griffiths & Stephen Zwolinsky Leeds Institute for Data Analytics and School of Geography, University of Leeds, Leeds, UK
Engineering and Environment, Northumbria University, Newcastle, UK Seraphim Alvanides GESIS—Leibniz Institute for the Social Sciences, Cologne, Germany You can also search for this author in PubMed Google Scholar Corresponding authorCorrespondence to Michelle A. Morris . Ethics declarationsConflict of interest. The authors declare that they have no conflict of interest. Additional informationPublisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsReprints and permissions About this articleCite this article. Wilkins, E., Aravani, A., Downing, A. et al. Evidence from big data in obesity research: international case studies. Int J Obes 44 , 1028–1040 (2020). https://doi.org/10.1038/s41366-020-0532-8 Download citation Received : 23 May 2019 Revised : 20 December 2019 Accepted : 07 January 2020 Published : 27 January 2020 Issue Date : May 2020 DOI : https://doi.org/10.1038/s41366-020-0532-8 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative This article is cited by
International Journal of Obesity (2023) Creating a long-term future for big data in obesity research
International Journal of Obesity (2019) Quick links
Advertisement Five-Year Changes in Weight and Diabetes Status After Bariatric Surgery for Craniopharyngioma-Related Hypothalamic Obesity: a Case–Control Study
Cite this article
637 Accesses 4 Citations 1 Altmetric Explore all metrics Craniopharyngiomas are tumors located in the hypothalamic region which leads to obesity in about 50% of cases. Long-term efficacy and safety of bariatric surgery are lacking in this peculiar population. The aim of this study is to determine the 5-year weight loss and resolution of type 2 diabetes (T2D) after bariatric surgery in patients operated on craniopharyngioma who had developed hypothalamic obesity. Materials and MethodsThis is a multicenter french retrospective case–control study. Subjects with craniopharyngioma ( n = 23) who underwent sleeve gastrectomy (SG) ( n = 9) or Roux-en-Y gastric bypass (RYGB) ( n = 14) (median age 35 years [25;43] and BMI 44.2 kg/m 2 [40.7; 51.0]; 8/23 with T2D) were individually matched to 2 subjects with common obesity for age, gender, preoperative body mass index, T2D, and type of surgery. TWL% after 1 and 5 years was lower in the craniopharyngioma group than in the control group: 23.1 [15.4; 31.1] (23/23) vs 31.4 [23.9; 35.3] at 1 year ( p = 0.008) (46/46) and 17.8 [7.1; 21.9] (23/23) vs 26.2 [18.9; 33.9] at 5 years ( p = 0.003) (46/46). After RYGB, TWL% was lower in the craniopharyngioma group compared to the control group ( p < 0.001) and comparable after SG both at 1 and 5 years. No difference between the two groups was observed in T2D remission rate and in early and late adverse events. No hormonal deficiency-related acute disease was reported. ConclusionsBariatric surgery induced a significant weight loss in the craniopharyngioma group at 1 and 5 years, but less than in common obesity. SG may be more effective than RYGB but this remains to be demonstrated in a larger cohort. Graphical Abstract This is a preview of subscription content, log in via an institution to check access.  Access this articleSubscribe and save.
Price includes VAT (Russian Federation) Instant access to the full article PDF. Rent this article via DeepDyve Institutional subscriptions  Similar content being viewed by others Efficacy and safety of bariatric surgery for craniopharyngioma-related hypothalamic obesity: a matched case–control study with 2 years of follow-up Impact of Baseline BMI and Adherence to Follow-Up on the Outcome of Sleeve Gastrectomy in Treatment of Adolescent Obesity Long-term Outcomes of Sleeve Gastrectomy in Adolescent Patients: The Effect of Weight Loss in Younger Years to Outcomes in AdulthoodWang KW, et al. The effectiveness of interventions to treat hypothalamic obesity in survivors of childhood brain tumours: a systematic review. Obes Rev. 2017;18(8):899–914. Article Google Scholar van Iersel L, et al. Pathophysiology and individualized treatment of hypothalamic obesity following craniopharyngioma and other suprasellar tumors: a systematic review. Endocr Rev. 2019;40(1):193–235. Bretault M, et al. Management of hypothalamic obesity during transition from childhood to adulthood. Endocr Dev. 2018;33:57–67. Lustig RH, et al. Octreotide therapy of pediatric hypothalamic obesity: a double-blind, placebo-controlled trial. J Clin Endocrinol Metab. 2003;88(6):2586–92. Article CAS Google Scholar Mason PW, Krawiecki N, Meacham LR. The use of dextroamphetamine to treat obesity and hyperphagia in children treated for craniopharyngioma. Arch Pediatr Adolesc Med. 2002;156(9):887–92. Lomenick JP, Buchowski MS, Shoemaker AH. A 52-week pilot study of the effects of exenatide on body weight in patients with hypothalamic obesity. Obesity (Silver Spring). 2016;24(6):1222–5. Zoicas F, et al. GLP-1 analogues as a new treatment option for hypothalamic obesity in adults: report of nine cases. Eur J Endocrinol. 2013;168(5):699–706. Castro-Dufourny I, Carrasco R, Pascual JM. Hypothalamic obesity after craniopharyngioma surgery: treatment with a long acting glucagon like peptide 1 derivated. Endocrinol Diabetes Nutr. 2017;64(3):182–4. Thondam SK, et al. A glucagon-like peptide-1 (GLP-1) receptor agonist in the treatment for hypothalamic obesity complicated by type 2 diabetes mellitus. Clin Endocrinol (Oxf). 2012;77(4):635–7. Bretault M, Carette C, Zaharia R, et al. Liraglutide 3mg as a weight-loss strategy after failed bariatric surgery in a patient with hypothalamic obesity following craniopharyngioma. Diabetes Metab. 2020;46(6):514–5. Arterburn DE, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324(9):879–87. Wijnen M, et al. Efficacy and safety of bariatric surgery for craniopharyngioma-related hypothalamic obesity: a matched case-control study with 2 years of follow-up. Int J Obes (Lond). 2017;41(2):210–6. Bretault M, et al. Clinical review: Bariatric surgery following treatment for craniopharyngioma: a systematic review and individual-level data meta-analysis. J Clin Endocrinol Metab. 2013;98(6):2239–46. Garrez I, Lapauw B, Van Nieuwenhove Y. Bariatric surgery for treatment of hypothalamic obesity after craniopharyngioma therapy: a matched case-control study. Obes Surg. 2020;30(6):2439–44. Page-Wilson G, et al. Hypothalamic obesity in patients with craniopharyngioma: treatment approaches and the emerging role of gastric bypass surgery. Pituitary. 2012;15(1):84–92. Rottembourg D, et al. Outcome after bariatric surgery in two adolescents with hypothalamic obesity following treatment of craniopharyngioma. J Pediatr Endocrinol Metab. 2009;22(9):867–72. Trotta M, et al. Sleeve gastrectomy leads to easy management of hormone replacement therapy and good weight loss in patients treated for craniopharyngioma. Updates Surg. 2017;69(1):95–9. Inge TH, et al. Gastric bypass surgery for treatment of hypothalamic obesity after craniopharyngioma therapy. Nat Clin Pract Endocrinol Metab. 2007;3(8):606–9. van Santen SS, Wolf P, Kremenevski N, et al. Bariatric surgery for hypothalamic obesity in craniopharyngioma patients: a retrospective, matched case-control study. J Clin Endocrinol Metab. 2021;106(11):e4734–45. Fried M, et al. Interdisciplinary European Guidelines on metabolic and bariatric surgery. Obes Facts. 2013;6(5):449–68. Buse JB, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133–5. Pickering L, et al. Sleep-wake and melatonin pattern in craniopharyngioma patients. Eur J Endocrinol. 2014;170(6):873–84. Muller HL. Increased daytime sleepiness in patients with childhood craniopharyngioma and hypothalamic tumor involvement: review of the literature and perspectives. Int J Endocrinol. 2010;2010: 519607. Jayaraj P, et al. Does beta-catenin have a role in pathogenesis of sebaceous cell carcinoma of the eyelid? Br J Ophthalmol. 2011;95(2):284–7. Weismann D, et al. Bariatric surgery for morbid obesity in craniopharyngioma. Clin Endocrinol (Oxf). 2013;78(3):385–90. Papamargaritis D, le Roux CW. Do gut hormones contribute to weight loss and glycaemic outcomes after bariatric surgery? Nutrients. 2021;13(3):762. Castellana M, et al. Roux-en-Y gastric bypass vs sleeve gastrectomy for remission of type 2 diabetes. J Clin Endocrinol Metab. 2021;106(3):922–33. Wijnen M, et al. Excess morbidity and mortality in patients with craniopharyngioma: a hospital-based retrospective cohort study. Eur J Endocrinol. 2018;178(1):93–102. Trivin C, et al. Childhood craniopharyngioma: greater hypothalamic involvement before surgery is associated with higher homeostasis model insulin resistance index. BMC Pediatr. 2009;9:24. Arterburn D, et al. Comparative effectiveness and safety of bariatric procedures for weight loss: a PCORnet cohort study. Ann Intern Med. 2018;169(11):741–50. Brethauer SA, et al. Can diabetes be surgically cured? Long-term metabolic effects of bariatric surgery in obese patients with type 2 diabetes mellitus. Ann Surg. 2013;258(4):628–36. discussion 636-7. Debedat J, et al. Long-term relapse of type 2 diabetes after Roux-en-Y gastric bypass: prediction and clinical relevance. Diabetes Care. 2018;41(10):2086–95. Download references AcknowledgementsThe authors express their thanks to Florence Marchelli and Valentine Lemoine of the CRNH and the Institute of Cardiometabolism and Nutrition, Pitié-Salpêtrière Hospital, Paris, France, for assistance with control recruitment and data management. We thank Dr David Marsh for English editing. Author informationAuthors and affiliations. Nutrition Department, French Reference Center for Prader-Willi Syndrome, Pitié-Salpêtrière Hospital, Assistance Publique-Hôpitaux de Paris, INSERM UMRS NutriOmics, Sorbonne University, 75013, Paris, France Pauline Faucher & Christine Poitou Service de Nutrition, Hôpital Pitié Salpêtrière, 47-83 Bd de l’hôpital, 75671, Paris Cedex 13, France Pauline Faucher Assistance Publique-Hôpitaux de Paris, Centre-Université de Paris, Service de Nutrition, Hôpital Européen Georges Pompidou, Centre Spécialisé Obésité Ile-de-France Sud, 75015, Paris, France Claire Carette & Sébastien Czernichow Université de Paris, 75015, Paris, France Claire Carette, Anne-Sophie Jannot, Alexis Van Straaten & Sébastien Czernichow Assistance Publique-Hôpitaux de Paris, Centre-Université de Paris, Service d’informatique Médicale, Santé Publique Et Biostatistiques, Hôpital Européen Georges Pompidou, 75015, Paris, France Anne-Sophie Jannot & Alexis Van Straaten Department of Endocrinology, Diabetology, and Metabolic Diseases (B.G.), Haut Leveque Hospital, Pessac, University of Bordeaux, 33076, Bordeaux, France Blandine Gatta-Cherifi Centre Hospitalier Universitaire Caen Normandie, Service d’Hépato-gastro-entérologie Nutrition et Chirurgie digestive, Centre Spécialisé de L’Obésité du CHU Caen Normandie, 14000, Caen, France Marie-Astrid Piquet Fédération d’endocrinologie, Centre de Référence Des Maladies Rares Hypophysaires, Groupement Hospitalier Est, 8 av Doyen Lepine, 69677, Hospices Civils de LyonBron Cedex, France Gerald Raverot & Maud Alligier INSERM U1052, CNRS UMR5286, Cancer Research Center of Lyon, 69372, Lyon, France Gerald Raverot F-CRIN/FORCE Network, Human Nutrition Research Center, Lyon, France Maud Alligier Centre Hospitalier Régional Universitaire Nancy Brabois, Centre Spécialisé de L’Obésité du CHRU Nancy Brabois, 54500, Vandoeuvre-Les-Nancy, France Thibault Batisse Specialized Obesity Center and Department of Endocrinology, Diabetology, Nutrition, CHRU-Nancy, Brabois Hospital, Université de Lorraine, 54500, Vandoeuvre-Les-Nancy, France Olivier Ziegler Department of Endocrinology, L’Institut Du Thorax, Centre Hospitalier Universitaire de Nantes, 44093, Nantes, France Delphine Drui Assistance Publique-Hôpitaux de Paris, Hôpital Ambroise Paré, Service d’Endocrinologie Diabétologie Nutrition, 92100, Boulogne-Billancourt, France Marion Bretault Service Nutrition Clinique, Centre Hospitalier Universitaire de Clermont Ferrand, 63003, Clermont Ferrand, France Nicolas Farigon Department of Visceral Surgery, CHU Clermont-Ferrand, 63003, Clermont Ferrand, France Department of Hepato-Biliary and Pancreatic Surgery, Pitié-Salpêtrière University Hospital, Assistance Publique-Hôpitaux de Paris (AP-HP), Sorbonne Université, 47-83 Boulevard de l’Hôpital, 75013, Paris, France Laurent Genser Assistance Publique-Hôpitaux de Paris (AP-HP), Service de chirurgie digestive, Hôpital Européen Georges Pompidou, 75015, Paris, France Tigran Poghosyan Department of Surgery and Oncology, Ambroise Paré Hospital, AP-HP, 92100, Boulogne-Billancourt, France Karina Vychnevskaia Clinique de Chirurgie Digestive Et Endocrinienne (CCDE), CHU de Nantes, 44093, Nantes Cedex 1, France Claire Blanchard L’institut Du Thorax, Université de Nantes, CHU Nantes, CNRS, INSERM, 44000, Nantes, France Department of Digestive Surgery, Center of Bariatric Surgery, Hopital Edouard Herriot, Hospices Civils de Lyon, 69437, Lyon, France Maud Robert Fédération Hospitalo-Universitaire DO-IT, Centre Intégré Et Spécialisé de L’Obésité de Lyon, CRNH-RA, Hospices Civils de Lyon, Lyon, France Oeso-Gastric Surgery Unit, Magellan University Hospital, Bordeaux, France Caroline Gronnier Bordeaux Medicine University, 33076, Bordeaux, France You can also search for this author in PubMed Google Scholar ContributionsC.P, C.C, S.C, P.F, and A-S.J conceived the original idea and designed the study. All authors gathered and/or delivered data for subjects with craniopharyngioma. M.A. supervised the project. C.P and P.F recruited the subjects of the control group. All authors provided critical feedback. A-S.J. and A.V.S performed the statistical analysis. P.F. drafted the manuscript. All authors approved the final version, had access to the full data in the study, and accept responsibility to submit for publication. P.F., C.P., C.C, and S.C. are guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Corresponding authorCorrespondence to Pauline Faucher . Ethics declarationsEthics approval. For this type of study, formal consent is not required. Conflict of InterestThe authors declare no competing interests. Informed ConsentInformed consent does not apply. Additional informationPublisher's note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. • TWL% after 5 years is 18% in craniopharyngioma group vs 26% in controls • No difference in type 2 diabetes remission rate at 5 years • No hormonal deficiency-related acute disease reported Supplementary InformationBelow is the link to the electronic supplementary material. Supplementary file1 Figure: Flowchart of case-control retrospective study. (PPTX 51 KB)Rights and permissions. Reprints and permissions About this articleFaucher, P., Carette, C., Jannot, AS. et al. Five-Year Changes in Weight and Diabetes Status After Bariatric Surgery for Craniopharyngioma-Related Hypothalamic Obesity: a Case–Control Study. OBES SURG 32 , 2321–2331 (2022). https://doi.org/10.1007/s11695-022-06079-9 Download citation Received : 03 February 2022 Revised : 14 April 2022 Accepted : 20 April 2022 Published : 06 May 2022 Issue Date : July 2022 DOI : https://doi.org/10.1007/s11695-022-06079-9 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
Data Sharing Statement
See More AboutSelect your interests. Customize your JAMA Network experience by selecting one or more topics from the list below.
Others Also Liked
Sodhi M , Rezaeianzadeh R , Kezouh A , Etminan M. Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss. JAMA. 2023;330(18):1795–1797. doi:10.1001/jama.2023.19574 Manage citations:© 2024
Risk of Gastrointestinal Adverse Events Associated With Glucagon-Like Peptide-1 Receptor Agonists for Weight Loss
Glucagon-like peptide 1 (GLP-1) agonists are medications approved for treatment of diabetes that recently have also been used off label for weight loss. 1 Studies have found increased risks of gastrointestinal adverse events (biliary disease, 2 pancreatitis, 3 bowel obstruction, 4 and gastroparesis 5 ) in patients with diabetes. 2 - 5 Because such patients have higher baseline risk for gastrointestinal adverse events, risk in patients taking these drugs for other indications may differ. Randomized trials examining efficacy of GLP-1 agonists for weight loss were not designed to capture these events 2 due to small sample sizes and short follow-up. We examined gastrointestinal adverse events associated with GLP-1 agonists used for weight loss in a clinical setting. We used a random sample of 16 million patients (2006-2020) from the PharMetrics Plus for Academics database (IQVIA), a large health claims database that captures 93% of all outpatient prescriptions and physician diagnoses in the US through the International Classification of Diseases, Ninth Revision (ICD-9) or ICD-10. In our cohort study, we included new users of semaglutide or liraglutide, 2 main GLP-1 agonists, and the active comparator bupropion-naltrexone, a weight loss agent unrelated to GLP-1 agonists. Because semaglutide was marketed for weight loss after the study period (2021), we ensured all GLP-1 agonist and bupropion-naltrexone users had an obesity code in the 90 days prior or up to 30 days after cohort entry, excluding those with a diabetes or antidiabetic drug code. Patients were observed from first prescription of a study drug to first mutually exclusive incidence (defined as first ICD-9 or ICD-10 code) of biliary disease (including cholecystitis, cholelithiasis, and choledocholithiasis), pancreatitis (including gallstone pancreatitis), bowel obstruction, or gastroparesis (defined as use of a code or a promotility agent). They were followed up to the end of the study period (June 2020) or censored during a switch. Hazard ratios (HRs) from a Cox model were adjusted for age, sex, alcohol use, smoking, hyperlipidemia, abdominal surgery in the previous 30 days, and geographic location, which were identified as common cause variables or risk factors. 6 Two sensitivity analyses were undertaken, one excluding hyperlipidemia (because more semaglutide users had hyperlipidemia) and another including patients without diabetes regardless of having an obesity code. Due to absence of data on body mass index (BMI), the E-value was used to examine how strong unmeasured confounding would need to be to negate observed results, with E-value HRs of at least 2 indicating BMI is unlikely to change study results. Statistical significance was defined as 2-sided 95% CI that did not cross 1. Analyses were performed using SAS version 9.4. Ethics approval was obtained by the University of British Columbia’s clinical research ethics board with a waiver of informed consent. Our cohort included 4144 liraglutide, 613 semaglutide, and 654 bupropion-naltrexone users. Incidence rates for the 4 outcomes were elevated among GLP-1 agonists compared with bupropion-naltrexone users ( Table 1 ). For example, incidence of biliary disease (per 1000 person-years) was 11.7 for semaglutide, 18.6 for liraglutide, and 12.6 for bupropion-naltrexone and 4.6, 7.9, and 1.0, respectively, for pancreatitis. Use of GLP-1 agonists compared with bupropion-naltrexone was associated with increased risk of pancreatitis (adjusted HR, 9.09 [95% CI, 1.25-66.00]), bowel obstruction (HR, 4.22 [95% CI, 1.02-17.40]), and gastroparesis (HR, 3.67 [95% CI, 1.15-11.90) but not biliary disease (HR, 1.50 [95% CI, 0.89-2.53]). Exclusion of hyperlipidemia from the analysis did not change the results ( Table 2 ). Inclusion of GLP-1 agonists regardless of history of obesity reduced HRs and narrowed CIs but did not change the significance of the results ( Table 2 ). E-value HRs did not suggest potential confounding by BMI. This study found that use of GLP-1 agonists for weight loss compared with use of bupropion-naltrexone was associated with increased risk of pancreatitis, gastroparesis, and bowel obstruction but not biliary disease. Given the wide use of these drugs, these adverse events, although rare, must be considered by patients who are contemplating using the drugs for weight loss because the risk-benefit calculus for this group might differ from that of those who use them for diabetes. Limitations include that although all GLP-1 agonist users had a record for obesity without diabetes, whether GLP-1 agonists were all used for weight loss is uncertain. Accepted for Publication: September 11, 2023. Published Online: October 5, 2023. doi:10.1001/jama.2023.19574 Correction: This article was corrected on December 21, 2023, to update the full name of the database used. Corresponding Author: Mahyar Etminan, PharmD, MSc, Faculty of Medicine, Departments of Ophthalmology and Visual Sciences and Medicine, The Eye Care Center, University of British Columbia, 2550 Willow St, Room 323, Vancouver, BC V5Z 3N9, Canada ( [email protected] ). Author Contributions: Dr Etminan had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Sodhi, Rezaeianzadeh, Etminan. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Sodhi, Rezaeianzadeh, Etminan. Critical review of the manuscript for important intellectual content: All authors. Statistical analysis: Kezouh. Obtained funding: Etminan. Administrative, technical, or material support: Sodhi. Supervision: Etminan. Conflict of Interest Disclosures: None reported. Funding/Support: This study was funded by internal research funds from the Department of Ophthalmology and Visual Sciences, University of British Columbia. Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Data Sharing Statement: See Supplement .
Featured TopicsFeatured series. A series of random questions answered by Harvard experts. Explore the GazetteRead the latest.  Implantable device responds to opioid overdose Study detects ‘hidden consciousness’ in brain injury patients Shingles may increase risk of cognitive declineExamining new weight-loss drugs, pediatric bariatric patients.  AP Photo/David J. Phillip Samantha Laine Perfas Harvard Staff Writer Researcher says study found variation in practices, discusses safety concerns overall for younger usersDrugs like Ozempic and Wegovy, known as GLP-1 receptor agonists, have surged in popularity as treatment for weight loss and management. The increase involves not only adults but also adolescents, along with bariatric surgery patients . Michael Kochis, Ed.M. ’19, M.D. ’20, a resident in the Department of Surgery at Massachusetts General Hospital, realized that little research had been done regarding the use of these drugs on adolescent bariatric surgery patients. Kochis and his team examined practice patterns across the nation, and he spoke to the Gazette about the group’s recent study as well as safety issues for youth generally. This interview has been edited for length and clarity. Have these drugs been found to be safe, both for adults and adolescents? There is increasing evidence that these can be safely used, especially in adults but more recently in pediatrics. Studies happen before drugs get licensed to make sure that they’re safe enough to go to market, and that factors into FDA approval. After approval, they’re still monitored. And I think it’s important to note that safety can mean different things to different people. And so while there are no glaring problems that would withdraw these drugs from the market — which has happened in the past with other medications related to obesity — there are side effects that aren’t well-tolerated by everyone, like nausea or feeling like you’re full all the time. They’re not a “cure all” drug with all benefits and no risk. For pediatrics specifically, there’s far less data on their use in children and young adults because they’re not as frequently prescribed in the first place. It’s harder to get studies where we can collect tons of data on adolescents. One of the areas that this research is highlighting is the fact that these drugs are being used in the pediatric population. It’s really important that we collect data to make sure there’s nothing different about the drugs’ use in this population, compared to what we know from adults. For your study, why did you choose to look at bariatric surgery patients as opposed to just general adolescents who might be using these drugs? Our research group has a specialty in bariatric surgery. We’re hearing more and more and more about these drugs and that sparked our interest. But secondly, the use of these medications in the context of pediatric bariatric surgery has a few unique considerations beyond safety. Those relate to the many physiologic changes that happen as a result of bariatric surgery, not just to weight loss. The surgeries themselves change the body’s metabolism and hormone balances. It’s unknown how the changes from surgery might relate to the hormone balances that these medications affect. And so the questions are relevant before surgery, during surgery, and after surgery in regard to the effects of these medications on patients. We asked questions in all three domains. “More likely than not, you’re doing things differently than your colleagues. So why don’t we start talking about it and sharing our experiences to try to come to the best practices?” Michael Kochis What did your study find in terms of the usage of these medications? There were two really big-picture findings. One is that, yes, these medications are being used for adolescents with obesity who are undergoing bariatric surgery. So essentially the cat’s out of the bag, it’s already happening. And then the second finding is that there’s a lot of uncertainty and variation in the exact practice patterns across institutions. There’s a recognition that we’re doing it this way at our place, and they’re doing it that way at that place. And no one really knows what the right answer or the best answer is. We’re in uncharted territories. That creates an opportunity for deliberate convening amongst these different groups and data-sharing so we can try to establish best practices. That can be based on consensus regarding what experts think the best approach is or hopefully — in time — an evidence-based approach. But that might take time. What are the benefits and potential dangers of realizing there’s so much variation? I think overall, it’s sparking discussion and increasing awareness. A lot of these pediatric bariatric centers have to be really good at what they do. We specifically looked at the larger centers throughout the country, which are often reference points for entire regions. My hunch is that people come to their practices based on what they think is going to be helpful for their patients, not realizing that other places do it differently. This study highlights that and will hopefully spark a discussion so different providers will start talking with their peers and asking questions. More likely than not, you’re doing things differently than your colleagues. So why don’t we start talking about it and sharing our experiences to try to come to the best practices? The problem with this is there might be the recognition that one approach is better than others. If you have variety, the implication is that there might be variations in the quality of care. Once we do have a better understanding of optimal use of these medications in the pre-op, peri-op, and post-op setting, there will be opportunities for standardization of care. What do we still need to learn? Above all, there’s a need for more data. I also hope this highlighted an opportunity for different institutions to come together and collaborate. We’re working on both of those things. Pediatric surgery in general is relatively small; fortunately, a lot of times kids and adolescents don’t need operations as frequently as adults do. So it’s a great space for collaboration and gathering knowledge. There are a couple collaboratives of pediatric hospitals and surgeon networks throughout the country; we at Mass General are currently working to establish another collaborative specifically focused on pediatric metabolic and bariatric surgery. We’re working on creating databases where we can pool all of our data from our separate institutions — about how we treat these patients before they’re getting surgery, what we do during the surgical context, and then how they do after surgery — to get on the same page about what data we’re collecting and how we can assess it in the long term. We can ask some really good research questions that we would never be able to get the answers to (with as much level of detail and discernment) if any one of our institutions did that exact same study alone. More efforts like that will be helpful in providing the high-level evidence we need to make informed decisions about the optimal care for patients. Is there anything that parents should be aware of when considering these medications for their children? I’m glad you brought that up. One of the findings from the study is that some providers’ practices — in the absence of strict guidelines or criteria — were informed partially by patients or families. The use of these medications should be a multidisciplinary discussion with the patient’s pediatrician, primary care doctor, obesity medicine physician, and potentially with a surgeon, if that’s applicable. Every patient has unique circumstances. So I would say to parents that if they see advertisements for this on the news or see these medications on social media, it’s great that they can be informed about what’s out there. But then bring that background knowledge to an informed discussion with your doctors. Understand that just because you heard some celebrities have used them and had certain experiences it does not mean that they are for everybody or should be applied in your circumstance. You can really only discern that based on a comprehensive discussion with your doctors. Share this articleYou might like. Without assistance, it allows for precise administration of naloxone at the moment it is needed  25% of participants with severe brain injury followed instructions covertly  Availability of vaccine offers opportunity to reduce burden of shingles and possible dementia John Manning named next provostHis seven-year tenure as Law School dean noted for commitments to academic excellence, innovation, collaboration, and culture of free, open, and respectful discourse Loving your pup may be a many splendored thingNew research suggests having connection to your dog may lower depression, anxiety Good genes are nice, but joy is betterHarvard study, almost 80 years old, has proved that embracing community helps us live longer, and be happier Warning: The NCBI web site requires JavaScript to function. more... An official website of the United States government The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site. The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health. Lunt N, Smith RD, Mannion R, et al. Implications for the NHS of inward and outward medical tourism: a policy and economic analysis using literature review and mixed-methods approaches. Southampton (UK): NIHR Journals Library; 2014 Jan. (Health Services and Delivery Research, No. 2.2.)  Implications for the NHS of inward and outward medical tourism: a policy and economic analysis using literature review and mixed-methods approaches.Chapter 10 bariatric surgery case study. An area that has seen rapid growth in the numbers of patients travelling abroad, as well as patients in the UK undergoing surgery, is bariatric or weight loss surgery. 194 The UK, like many other countries globally, has seen a rapid increase in the numbers of overweight and obese patients, with the Department of Health estimating that one-quarter of the UK population is now clinically obese, that is, with a body mass index (BMI) of ≥ 30 kg/m 2 . 195 Obesity has several long-term health effects including an increased incidence of diabetes and cardiovascular disease. In addition to behavioural interventions such as exercise, counselling and pharmacological interventions (appetite suppressants), several surgical procedures are available to assist weight loss. The two most common procedures are a gastric band and a gastric bypass. A ‘band’ is the less invasive procedure. It limits food intake by placing a restrictive string around the top end of the stomach. This band has to be regularly adjusted to allow patients to consume food while maintaining weight loss. When a band is too tight it can prevent patients from eating, whereas a loose band means that patients can eat as much as they wish. The bypass is a much more invasive procedure in which part of the patient’s stomach is partitioned and his or her capacity to absorb food is limited. As a result of a bypass, patients need to monitor their food intake carefully to ensure that they receive the nutrition that they require. Given the body’s reduced capacity to absorb nutrients and specific vitamins and minerals, supplements have to be taken by patients for the rest of their lives to ensure adequate nutrition. 196 In the UK, bariatric surgery is a relatively new field of surgery. It is available as treatment on the NHS and National Institute for Health and Care Excellence (NICE) guidelines 197 recommend or make available bariatric surgery in individuals with a BMI > 40 kg/m 2 . However, the implementation and interpretation of the guidelines depend on the PCT and on the assessment by a GP. Research has indicated a reluctance by GPs to prescribe such surgery. 195 In this research, 13 in-depth interviews were conducted with patients who travelled abroad for bariatric surgery. These discussed the themes explored in the patient interviews described in Chapter 9 , for example patients’ experiences of the NHS before and after treatment, and how they identified the treatment provider abroad. In addition, three professionals from organisations working in bariatric surgery in the UK were interviewed to gain further understanding.
Although many issues identified across our sample of patients were common to bariatric patients’ motivation to travel (such as issues relating to distance and eligibility), there were also clear differences within each subtheme identified that were specific to bariatric tourism. These hold important lessons when trying to understand and address the specific factors determining bariatric patients’ travel and follow-up needs. Motivation for travelling abroad for bariatric surgery: an emerging field of expertise in the UKAs with many other medical tourists, bariatric surgery patients were keen to stress that cost had not been the only factor in them choosing to travel for surgery, and only 2 of the 13 patients interviewed cited this as their sole motivation. More than for any other group interviewed, expertise (in bariatric surgery) was the biggest pull factor. In total, 11 out of the 13 had travelled to Belgium, which was perceived to be more advanced in the field of bariatric surgery at the time that the patients interviewed had undertaken treatment (between 2004 and 2009). In several cases patients specifically described how the surgery that they had opted for had not been available to them within the NHS, or that surgeons in the UK had conducted only a small number of procedures, or that there was only limited expertise in these areas. Of the 13 patients interviewed, half reported that the surgeon having conducted the procedure many times before was a key factor in their decision-making. The experience of the surgeon was contrasted in some cases with a general distrust of the NHS: [My motivation for travel was] mainly the cost but also because the surgeon was very highly recommended. Also in general all-round the whole experience. I mean, there’s quite a big issue with MRSA [methicillin-resistant Staphylococcus aureus ] which they didn’t have at all abroad. BT4 AvailabilitySeveral issues relating to the availability of treatment were factors in the decision of where to seek treatment. This relates to bariatric surgery specifically, as it is a comparatively new field in the UK (see also p. 69). For example, two patients from Northern Ireland reported that, at the time of their surgery, it was not available in the province and surgery would have required them to travel (to mainland Britain) in any case. Similarly, a patient from Scotland reported that she would have had to travel to England to receive the procedure under the NHS. Patients also mentioned that they had seen a NHS doctor and had been judged eligible but that the waiting time for the operation had put them off having it done on the NHS. In some cases this appeared to be the actual reported waiting times; in others it was unclear if the patient had just anticipated the long wait. Eligibility on the NHS: a ‘postcode lottery’?As in other cases, such as fertility surgery, several patients reported that they had been found to be ineligible for treatment on the NHS. Although NICE guidelines exist that recommend or make available bariatric surgery for individuals with a BMI > 40 kg/m 2 , 197 the implementation and interpretation of these guidelines depends on the PCT and on assessment by the GP. Several patients interviewed referred to the resulting inequities and the sense of a ‘postcode lottery’. In some cases this was because people were deemed to have a BMI considered too low to qualify for surgery, or patients were considered healthy despite having a very high BMI and fearing for their long-term health. This may in part be the result of GPs looking at bariatric surgery as a ‘last resort’ and an expense rather than a cost-saving treatment. A recent survey of GPs conducted by the Office of Health Economics 195 found that the vast majority try to avoid prescribing surgery for obesity, regardless of BMI. Distance: Belgium, a perceived centre of expertiseAs with other patients, distance played a key role in decision-making. Specific to bariatric patients was that Belgium, as a centre of expertise in bariatric surgery at the time that interviewees had travelled (between 2004 and 2009), was easily accessible via Eurostar. Ten of the 13 people interviewed had travelled to Belgium: several mentioned its proximity, including specifically the ease of access by Eurostar. This has particular relevance for weight loss surgery, as some patients are cautioned against flying following the procedure. Based on this analysis, the decision by patients to travel for weight loss surgery was rarely the result of a single motivating factor; rather, it was a combination of cost, expertise, availability and distance, with different patients giving different weight to each of these. Unique to this group was the specific emphasis given to the experience of the surgeon. This was a direct result of bariatric surgery being a newer field of investigation in the UK; as expertise grows in the UK it is likely that these differences will disappear or become less pronounced. A representative of a Royal College working on these issues highlighted that bariatric surgery had been a very new field in the UK in 2004, but that the field was rapidly growing now with increasing expertise in the UK. Treatment pathway and experience: high rate of complicationsThe treatment pathway for bariatric patients did not vary greatly from the general model set out in Chapter 9 , with most patients describing the use of the internet to identify and research providers. What did set the experience of bariatric patients somewhat apart from the general experience was the level of complications and aftercare required for most procedures. Of the 13 patients interviewed, four experienced complications directly relating to the surgery and had to be resubmitted to hospital for additional surgery while still abroad. Many of the patients interviewed experienced long-term health problems relating to the surgery undertaken or the longer-term care needs resulting from these. However, what resonated across accounts of immediate complications and longer-term issues was the responsibility that patients took for the health outcomes of their procedures. This again seemed to be specific to bariatric patients in the study sample. Follow-up and aftercareThe most common procedures for which patients travelled abroad, gastric banding and gastric bypass, both require lifelong follow-up care and maintenance. In the case of a gastric band, this has to be adjusted to ensure that patients continue to lose weight while being able to consume enough food to obtain the nutrition that they require to survive. The gastric band is an elastic band filled with fluid that can be adjusted to tighten or loosen it. People with a gastric band are required to have the band adjusted at regular intervals. In the case of a gastric bypass, although the procedures may vary, a part of a person’s gut is removed and his or her capacity to absorb minerals and vitamins is limited. Therefore, patients who have undergone a gastric bypass have to rely on supplements to avoid malnutrition and patients have to undergo regular blood tests to monitor this. A professional interviewed for this research referred to the ‘maintenance’ that patients require following bariatric surgery and how this is a lifelong condition. Aftercare and follow-up from bariatric surgery can be divided into the needs immediately following surgery and the ongoing maintenance of the results achieved from the procedure. Several patients reported complications with their bands. One patient had a ‘faulty’ band emptied and removed because of the problems that she experienced with it; this interviewee reported that the replacement was also problematic. Two patients reported more severe long-term health consequences. One (who had had a gastric bypass) reported having been hospitalised for 2 years following a life-threatening complication and was still unable to work. Although the patient had returned to the original surgeon abroad to have the complication dealt with, she was now unable to afford further follow-up visits to him. Despite the complication arising from the original surgery, the patient retained a greater trust in the original surgeon’s abilities than in the NHS as he had been able to resolve the issue whereas the NHS had been unable to: Now, unfortunately two years down the line and I’m still not 100 per cent. I’m still on morphine every day and I’m still underweight. So I still have long-term problems so I don’t know if that will ever be sorted out. BT6 The other described how the long-term consequences of a bypass had led to severe health issues, including tears and fistulas. Continuity of care emerged as a clear challenge for all patients. However, in bariatric surgery this differed between the complications resulting from the surgery and the long-term care needs resulting from the surgery. Some of the complications experienced were severely debilitating, while the need for aftercare and ‘maintenance’ of a gastric band make continuity of care more important than for some of the other areas of surgery for which people travelled and which are reviewed here. The specific clinical requirements of aftercare for bariatric treatment also led to specificities in the industry models. Many of the Belgian providers offered aftercare services to English patients (such as the filling of bands) in London or other UK locations at an additional cost. This was specific to providers of bariatric services. National Health ServiceUnlike other groups of patients, all patients interviewed had been in contact with the NHS (specifically their GP) in relation to their weight before and after the surgery. Six patients specifically recounted the refusal by their GP to refer them for surgery; two of these explicitly mentioned that they were eligible for the surgery according to NICE guidelines but that their GP had told them that no funding was available. Overall, the vast majority of patients reported limited support from GPs. This was more common than in other groups of patients interviewed. In many cases patients reported that this may be based on limited knowledge. One interviewee summed it up as follows: The GP that was here just used to look at me blank if I mentioned my obesity. They didn’t offer anything at all, no support whatsoever [. . .] It’s not that they’re not supportive they just don’t know what to do. They don’t know anything about them. BT7 Interviewees also reported a difference in attitude between surgeons and GPs, which they felt was mainly due to surgeons’ greater knowledge of bariatric surgery. Moreover, all patients interviewed reported that insufficient services were provided within the remit of the NHS for overweight and obese patients. There was a clear sense that the approach by NHS staff had been cautious in relation to surgery and that as a result the patients interviewed for the research felt that the treatment that they required was unavailable to them. Compared with the overall sample of medical tourists, there were several distinct aspects to bariatric tourism. Three key factors were uncommon compared with other patients’ experiences. First, all bariatric patients interviewed had been in contact with the NHS before making their decision to travel for treatment. Second, the lack of expertise within the NHS was a greater factor for motivating bariatric patients than for motivating other medical tourists. Third, the need for aftercare and the high level of complications experienced by bariatric surgery patients set this group apart. It underlines the need for better information and a full understanding of risk amongst this group of medical tourists before they travel. This has also led to specific industry developments by providers, with follow-up consultations in London, and equally specific requirements of the NHS when maintenance is not provided by the original clinic. Bariatric surgery outcomes have long-term consequences; as this is a comparatively ‘young field’ some of these and the effects of treatment abroad will likely emerge only in the future. The SurgiCal Obesity Treatment Study (SCOTS) at the University of Glasgow (a longitudinal study of bariatric surgery patients) 198 will in the future provide important results in this respect. Across the interviews there was a sense that patients felt that they lacked the entitlement for surgery on the NHS as their weight was a result of their own ‘behaviour’. Some of the patients addressed this explicitly and described how their interactions with the NHS had left them feeling this way; most patients had had some contact with the NHS about weight loss and felt abandoned, with the NHS not recognising the value of weight loss surgery. Even when patients described this negative experience as an example of policy that had to change, they were equally keen to convey a sense of responsibility that they had taken on through their actions, that is, choosing to travel and have surgery to address a health issue, which all of them felt would have become worse otherwise. In addition, even in cases in which weight loss surgery may be inadvisable from a medical perspective, the fact that patients felt compelled to travel indicated that current approaches to overweight and obesity by the NHS are not working. Many patients reported a sense of frustration as they felt that they had saved the NHS substantive future health-care expenditure related to being overweight and obese. Patients had a sense of being judged for being overweight or obese.
Included under terms of UK Non-commercial Government License .
In this PageOther titles in this collection.
Recent Activity
Your browsing activity is empty. Activity recording is turned off. Turn recording back on Connect with NLM National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894 Web Policies FOIA HHS Vulnerability Disclosure Help Accessibility Careers
Emergency robotic surgery: the experience of a single center and review of the literature
World Journal of Emergency Surgery volume 19 , Article number: 28 ( 2024 ) Cite this article 185 Accesses 1 Altmetric Metrics details BackgroundsLaparoscopic surgery is widely used in abdominal emergency surgery (AES), and the possibility of extending this approach to the more recent robotic surgery (RS) arouses great interest. The slow diffusion of robotic technology mainly due to high costs and the longer RS operative time when compared to laparoscopy may represent disincentives, especially in AES. This study aims to report our experience in the use of RS in AES assessing its safety and feasibility, with particular focus on intra- and post-operative complications, conversion rate, and surgical learning curve. Our data were also compared to other experiences though an extensive literature review. We retrospectively analysed a single surgeon series of the last 10 years. From January 2014 to December 2023, 36 patients underwent urgent or emergency RS. The robotic devices used were Da Vinci Si (15 cases) and Xi (21 cases). 36 (4.3%) out of 834 robotic procedures were included in our analysis: 20 (56.56%) females. The mean age was 63 years and 30% of patients were ≥ 70 years. 2 (5.55%) procedures were performed at night. No conversions to open were reported in this series. According to the Clavien-Dindo classification, 2 (5.5%) major complications were collected. Intraoperative and 30-day mortality were 0%. ConclusionsOur study demonstrates that RS may be a useful and reliable approach also to AES and intraoperative laparoscopic complications when performed in selected hemodynamically stable patients in very well-trained robotic centers. The technology may increase the minimally invasive use and conversion rate in emergent settings in a completely robotic or hybrid approach. IntroductionAbdominal Emergency Surgery (AES) can be defined as a procedure requiring to deal with an acute threat to life, organ, trauma, acute disease process, acute exacerbation of a chronic disease process, or complication of a surgical or other interventional procedure, normally within hours of decision to operate [ 1 , 2 ]. Further, “expedited surgery” refers to the clinical situation exemplified by a patient in need of prompt treatment but not in imminent danger to life or organ survival; this procedure often takes place a few days after the decision to operate [ 3 ]. Nowadays, minimally invasive laparoscopic approach to urgent abdominal surgery (cholecystitis, acute appendicectomies, bowel perforation or obstruction, etc.) represents the standard of care in many cases and recent guidelines recommend it [ 4 , 5 , 6 , 7 ]. Nevertheless, after more than 20 years from clinical introduction, Robotic Surgery (RS) represents the most important technological evolution and a revolutionary concept of computer-assisted technology in minimally invasive surgery [ 8 ]. It allows to overcome many limits of conventional laparoscopy and to expand the use of minimally invasive approaches. Its peculiar features include a three-dimensional high-definition view, articulated instruments, tremor eradication, and improved ergonomics for surgeons, enable the performance of extremely accurate procedures (micro-sutures, fine dissections, etc.) with consequently lowering conversion rates and postoperative complications, particularly in case of challenging surgical procedures [ 9 , 10 , 11 ]. In addition, compared to traditional laparoscopic surgery, RS demonstrated shorter learning curves for several complex procedures [ 12 , 13 ]. On the other hand, the main drawbacks of robotic technology are linked to its limited diffusion also due to expensive costs [ 14 , 15 , 16 , 17 , 18 , 19 , 20 ]. Nevertheless, robotic surgical technologies have expanded and evolved over the past 20 years, bringing new devices, and improving the most established ones [ 21 , 22 ]. The spreading of robotic platforms and their easier management led to increased RS applications in all abdominal surgical specialities including upper gastrointestinal surgery [ 15 , 23 , 24 , 25 ], colorectal surgery [ 26 , 27 , 28 ], HBP surgery [ 14 , 18 , 29 , 30 , 31 ], abdominal wall surgery and many others [ 7 ]. Despite the huge diffusion of RS in all surgical fields, its application in urgent scenarios has never been investigated representing a new field of interest, with limited literature experiences [ 32 ]. So considering that our experience in RS has been implemented since 2002 and it raised from general to major complex surgery [ 33 , 34 , 35 , 36 , 37 , 38 ], we aim to set the state of art of Robotic Emergency Surgery sharing our experience through the analysis of our peri-operative outcomes and indications in RS. Furthermore, due to the limited evidence available, we have as a secondary endpoint an extensive analysis of previous literature experiences. Study design and patient selectionWe retrospectively reviewed a prospectively collected database of patients undergoing RS at General and Robotic Surgery Unit of San Giovanni Battista Hospital (Foligno, Italy) and General Surgery Unit of San Donato Hospital (Arezzo, Italy) from January 2014 to December 2023. The patients’ data were analyzed according to Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [ 39 ]. All patients signed an informed consent allowing the anonymous scientific use of clinical data and images. The study was carried out according to the Declaration of Helsinki guidelines and was approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: May 12, 2021). In all participating centres, data were prospectively collected from electronic patient records. We selected 834 consecutive robotic procedures for abdominal surgery performed by both centres. Patients were divided into two cohorts: elective surgery and urgent or emergency surgery groups. Urgent surgery was defined as a condition requiring surgery within 72 h in stable patients, but not suitable for discharge. Moreover, emergency surgery was defined as a clinical scenario requiring within 24 h in stable patients, with a low risk of deterioration. All patients < 18 years old and affected by hemodynamical instability were excluded. Criteria adopted to assess baseline characteristics of patients, surgical issues and technologies that allow to benefit of RS in urgent and emergency settings are summarized in Table 1 . Furthermore, to analyze the diagnosis and intraoperative data we carried out a specialities classification as reported in Table 2 . Implementation of the robotic surgery program and learning curve completionOur experience with RS started in September 2002 with the da Vinci S ® platform (Intuitive Surgical, Sunnyvale, California, USA), and over time, its application in abdominal surgery grew as well as platform technologies. During the study period, the da Vinci Si ® platform (Intuitive Surgical, Sunnyvale, California, USA) and, since 2017, da Vinci Xi ® (Intuitive Surgical, Sunnyvale, California, USA) were available at our institutions. Beginning from colorectal surgery, hiatal hernia repairs and cholecystectomies, our surgical team have gradually selected more challenging procedures by carrying out liver and pancreatic resections, oesophageal benign and malignant disorders, bariatric surgery, abdominal wall hernia repairs and nephrectomies [ 14 , 15 , 25 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. All procedures were performed by a well-trained surgeon in minimally invasive surgery (G.C.) with 10 years of previous experience in RS. 36 (4.3%) out of 834 robotic procedures were included in our analysis and treated as urgent or emergent procedures. All patients signed an informed consent allowing the anonymous scientific use of clinical data and images. The study was carried out according to the Declaration of Helsinki guidelines and was approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: 12 May 2021). The collected data included demographic characteristics such as age, sex, and preoperative comorbidities classified according to the Charlson comorbidity Index (CCI) [ 48 ]. The anesthetic risk assessment was performed thanks to the American Society of Anesthesiologists (ASA) score [ 49 ]. We reviewed pre-operative diagnosis, main and associated surgical procedures, operative time and intraoperative complications, and conversion to open rate. Postoperative complications were stratified according to the Clavien-Dindo classification [ 50 ] and were considered severe when ≥ 3. Patients were monitored until their 30th postoperative day. Categorical variables were expressed as frequencies and percentages, while quantitative data were collected as means or medians and interquartile ranges. Literature reviewWe performed literature research on the PubMed Dataset (US National Library of Medicine, http://www.ncbi.nlm.nih.gov/PubMed ), using the subsequent keywords: “robotic surgery”, “urgent surgery”, and “emergency surgery”. We selected only English studies. Original articles, case reports and case series were included, while editorials, letters, and reviews were excluded. Number of treated patients does not represent an exclusion criterion. Articles were first evaluated by title and abstract examination, then a full-text read was performed. More than 50 studies described RS in AES. An extensive analysis was performed to summarize similarities and differences among RS approaches according to abdominal surgery specialities. Pre-, intra- e post-operative outcomes36 (4.3%) out of 834 robotic procedures were included in our analysis. Baseline characteristics of patients are listed in Table 3 . According to surgical procedures, Fig. 1 shows AES performed thanks to RS compared to elective surgery. Over the cohort of 36 patients treated, 16 (44.44%) were males while 20 (56.56%) were females. The mean age was 63.20 years (range: 43–88 years): 30.55% [ 11 ] of patients were ≥ 70 years. The mean Body Mass Index was 26.68 kg/m 2 (range: 23–42). According to the ASA score, 8 (22.22%) patients were classified as ASA 3. No ASA 4 was treated. Patients’ CCI are listed in Table 3 . The da Vinci Si platform was used for the first 15 (41.67%) cases, while Xi for the last 21 (58.33%). 2 (5.55%) procedures were performed at night. No conversions to open were reported in this series. According to Clavien-Dindo grade, 2 (5.55%) major complication was collected: 1 after urgent surgery and 1 after emergency setting. Two minor complications requiring conservative treatments were observed: both complications were related to primary disorders and not to RS. Intraoperative and 30-day mortality were 0%. The mean length of stay was 4.92 days (range: 1–21). The mean follow-up was 26.53 months (range: 7–68). 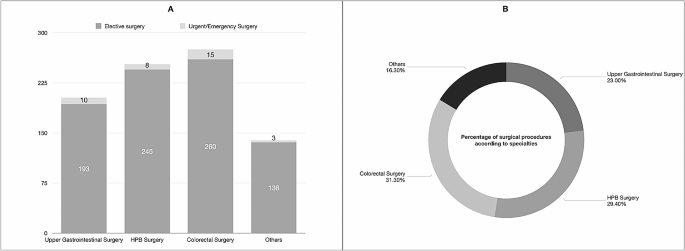 Number of elective and urgent/emergency procedures ( A ) and percentage of overall surgical procedures performed in emergency settings ( B ) according to abdominal surgery specialities. Abbreviations: HPB, Hepatopancreatic and Biliary Surgery; Our experience demonstrates the safety and feasibility of RS also in urgent and emergency abdominal settings in patients not affected by hemodynamic instability. To date, the minimally invasive approaches in emergency scenarios are mainly validated for laparoscopy, as reported by several literature experiences included in the last WSES review [ 51 ]. Despite the diagnostic role of MIS, authors demonstrated several benefits of laparoscopic approaches in hemodynamically stable patients undergone AES, including trauma. However, patient selection, surgeons’ expertise as well as specific surgical training represent crucial key points [ 51 ]. In literature, RS in AES studies is related to high-volume centres, and well-trained surgeons’ experiences and their optimal outcomes should encourage further applications and Randomized Clinical Trials [ 32 , 52 ]. We further analyzed short- and long-term outcomes of RS in AES according to specialties (Table 4 ). Robotic surgery in emergency settingIn the literature, RS in the emergency setting is reported by a limited number of experiences, especially case reports and case series. The urologist experience described by Capibaribe et al. [ 53 ] demonstrated the safety and efficacy of robotic treatment in the case of vesicourethral anastomotic stenosis after open radical prostatectomy, providing better continence results, without pubectomy. Globally, the major barrier to RS adoption is due to limited device access resulting from a shared use policy by several surgical teams (gynaecologists, general surgeons, thoracic surgeons, and urologists). Furthermore, the lack of dedicated teams (surgeons, nurses, and anaesthesiologists) during the night shift might further limit RS. On the other hand, in emergency settings, the “time-sparing” concept is largely known. Commonly, to avoid useless costs due to waste disposable instruments, a hybrid approach should be discussed by the whole surgical team: before robotic docking, a laparoscopic exploration could be the first surgical step to verify clinical environments for doing RS. A crucial issue is represented by frequent operating table position changes, especially during explorative steps (tilting, Trendelenburg, or reverse-Trendelenburg positions) and rapid conversion to open surgery when necessary [ 54 ]. It could be underlined that quick and safe docking and undocking are performed by skilled teams and well-trained surgeons in elective procedures [ 54 , 55 ]. In the last years, the RS technologies have also impacted operative time [ 56 ]: The Xi robot represents a radical evolution from the Si robot. Literature experiences demonstrated better docking ability during Da Vinci Xi surgery when compared to previous robotic systems (Da Vinci S, Si, X) [ 57 , 58 ]. These features were due to laser targeting and improved cannula mounts that resulted in a simplified “linear” port configuration and an abbreviated docking time. Besides, the ability to exchange the robotic camera from port-to-port increased versatility for multi-quadrant surgeries thanks to the smaller 8 mm camera [ 59 , 60 ]. The multi-quadrant operations represent challenges due to the axis of visualization shift up to 360°. This procedure requires undocking the robot and rotating it on the axis. It is crucial for many colorectal surgeries that require access to the entire abdomen such as subtotal colectomy and total proctocolectomy. Furthermore, it was reported that the Xi system’s better fluency is also due to thinner robotic arms that reduce their collisions during surgery and synchronous movements with the operating Table [ 56 ]. In addition, Da Vinci Xi integrates the Indocyanine-Green technology that could be easily used to better identify bile duct during cholecystectomy in patients affected by acute cholecystitis, to assess organ vascularization during their resections and anastomosis, as reported in our experience. Bianchi et al. [ 61 ] performed an extensive comparison of Da Vinci Si and Xi systems to define their advantages and disadvantages. 89 patients (64 in the Si system vs. 25 in the Xi system group) who underwent liver surgery were included. The Si system group experienced a greater total incisional length (+ 8.99 mm; p < 0.0001) due to a higher number of robotic/laparoscopic ports. Nevertheless, no differences were described regarding operative time, conversion rate, estimated blood loss, postoperative complications, mortality, use of analgesics, and costs. The authors concluded that da Vinci Xi represents an effective technological advancement. Hill et al. [ 62 ] hypothesized that Da Vinci Xi will allow for greater efficiency and result in shorter operative times if compared to Da Vinci Si. To validate their hypothesis, the authors performed a retrospective review of patients undergoing sigmoid colon resection or Low Anterior Rectal resection. A total of 93 patients underwent sigmoid resection thanks to RS (Si, n = 52 vs. Xi, n = 41). The Xi group had significantly shorter surgical times for Low Anterior Rectal and sigmoid resection (162 vs. 238 min, p = 0.0001). Nowadays, no data are available on the Da Vinci Si and Xi comparison in AES. However, according to the type of procedures, the mean operative times of Da Vinci Xi were superimposable to the Si group in our experience. The robotic technology in hemodynamically stable patients could potentially reduce the conversion to open rate (0% in our short series), thanks to high-definition view and accuracy of dissection and fine micro-sutures. In 2022, the World Society of Emergency Surgery (WSES) published a position paper on RS in AES after the literature evaluation by a steering committee and an international expert panel [ 32 ]. Ten studies (3 case reports, 3 case series, and 4 retrospective comparative cohort articles) were found and 6 statements were proposed. Experts concluded that RS can be considered safe, and feasible in selected cases represented by hemodynamically stable patients. It should be emphasized that the WSES team reported some RS drawbacks: it is mandatory to perform dedicated surgical training, RS showed longer operative times, higher costs and difficult availability and accessibility represent the main issues during night shifts [ 32 ]. These aspects probably may change in the future with RS diffusion and new robotic devices in the health market. In our experience, the mean age of patients was 63 years. Therefore, more than 30% of patients were older than 70 years (range: 43–88 years) and it is in line with RS literature experiences that showed good outcomes also in the elderly population [ 28 , 41 ]. Nevertheless, operative time represents a crucial point in this frail cohort. Despite RS showing longer operative time when compared to open and laparoscopic surgery, this disadvantage may be offset by lower postoperative complication rates, shorter hospital stays, and lower conversion rates [ 28 , 41 , 63 , 64 , 65 ]. Another key aspect is represented by enhanced vision through near-infrared imaging. It may be useful in AES in case of tissue perfusion evaluations or biliary tree identification in challenging procedures. This feature is not routinely available in laparoscopic surgery [ 66 , 67 ]. Figure 2 shows an emergency scenario due to splenic artery aneurysm repair thanks to RS. 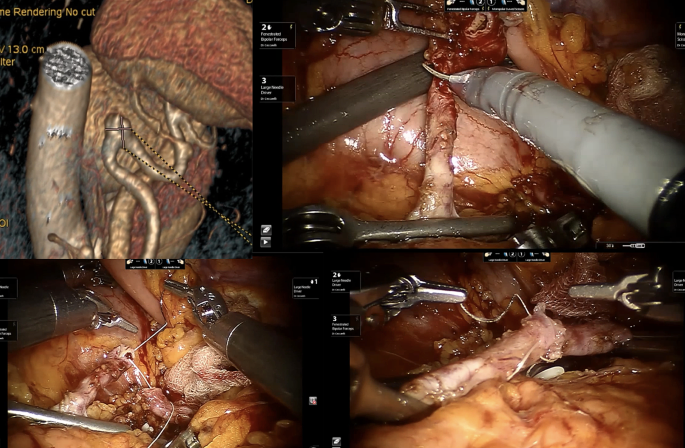 The robotic approach during Emergency Setting for patients affected by splenic artery aneurysms using a vessel resection and end-to-end vascular anastomosis Robotics in emergency upper-GI and bariatric surgeryOne of the earliest studies on RS in AES was published in 2012 [ [ 68 ]]: Sudan et al. experience in complex bariatric surgery involved 2 patients affected by a stomach stricture and an acute abdomen due to perforation with biliary peritonitis after biliopancreatic diversion, respectively. The perforation was treated through an initial laparoscopic investigation followed by a handsewn robotic stitch reparation of duodenal stump dehiscence. In 2020, Cubas et al. [ 69 ] presented an RS procedure for incarcerated Morgagni Hernia in a 29-year-old male. The hernia defect (reported as 10 × 7 cm) was corrected via mesh placement. Patient discharge was possible on POD 5. No recurrence was detected at 1-year follow-up. During the same year, Ceccarelli et al. [ 45 ] published a series of 5 patients affected by strangulated Giant Hiatal Hernia: 3 (60%) patients experienced RS while 2 (40%) laparoscopic approach. The authors described an easier incarcerated stomach management thanks to RS, maybe due to better surgeon ergonomic position and more accurate dissection preserving pleural integrity and vagus nerve. Kim et al. [ 70 ] reported a case of robotic transthoracic repair of a right-sided traumatic diaphragmatic rupture in a 45-year-old male with a history of chronic obstructive pulmonary disease presented as a restrained driver in a low-speed motor vehicle collision. The patient was effectively operated after a 48-hour observation. In 2021, 300 USA hospitals were involved in retrospective data collection of adult patients affected by Hiatal Hernia and treated in elective and urgent/emergency scenarios from 2015 to 2017 [ 71 ]. Data analysis revealed that laparoscopy (64%) was the most frequent approach used during AES, followed by open surgery (30%). A limited number of patients (6%) experienced RS. After cost evaluations and outcomes analysis, authors declared the technical feasibility of minimally invasive approaches when compared to open surgery due to lower cost, lower length of hospital stay, complications, and mortality. Robinson et al. [ 72 ], in 2021, performed a statistical analysis of “in-room-to-surgery-start time” in a retrospective cohort study of 44 patients affected by emergent perforated gastrojejunal ulcers. The comparison between RS and laparoscopic (24 and 20 cases respectively) showed encouraging results for RS (25 versus 31 min, p = 0.01). Furthermore, no statistical differences were observed in terms of intra- and post-operative outcomes (operative time, complication rate, complication severity, hospital length of stay, discharge to home, and 30-day readmission). Despite RS showing higher surgical costs, authors concluded that emergency gastric perforation could be safely approached thanks to RS. No complications were reported in all studies reported in our review [ 69 , 70 , 71 , 72 ]. Robotics in emergency colorectal surgery and appendectomiesNowadays, emergency laparoscopy represents a safe and valid approach to colorectal disorders such as perforated diverticulitis with generalized peritonitis [ 73 ], iatrogenic colonoscopy perforations [ 74 ], bowel obstructions and anastomotic leaks management [ 75 , 76 , 77 ]. In 2012, Pedraza et al. [ 78 ] showed successful robotic colectomy due to iatrogenic colon perforation following colonoscopy. Two years later, Felli et al. [ 79 ] described a case of an 86-year-old woman admitted to the emergency unit for massive intestinal bleeding due to ascending colon cancer. After patient resuscitation thanks to blood transfusions, surgeons carried out a robotic right colectomy. The postoperative period was uneventful. Several series compared laparoscopic and robotic outcomes in patients who underwent elective colorectal surgery [ 80 , 81 , 82 ], suggesting the potential role of RS in this surgical field. Nevertheless, an interesting analysis was performed by Beltzer et al. [ 83 ] in 2019. 106 patients were treated for uncomplicated, complicated, or recurrent diverticulitis. The authors concluded that RS achieves better outcomes when compared to laparoscopic surgery in challenging cases (abscess or relapsing diverticulitis). Three monocentric experiences reported by Kudsi et al. [ 84 , 85 , 86 ] showed the effectiveness of urgent RS for the treatment of obstructive transverse colon cancer, bleeding sigmoid diverticulosis and caecal volvulus. However, RS could represent a crucial approach also in colorectal autoimmune diseases. Concerning this field, Anderson et al. [ 87 ] in 2020 reported a matched case-control study of 6 patients treated by urgent subtotal colectomy for ulcerative colitis using the robotic platform. In addition, authors compared patients who underwent RS to laparoscopic urgent procedures (6 versus 13 cases) concluding that no differences in perioperative outcomes were observed. According to Yang et al. [ 88 ] estimation, more than 17 millions of patients were affected by appendicitis in 2019, making it the most common surgical emergency worldwide. Nevertheless, regarding urgent robotic appendectomies, only 5 literature experiences reported robotic approaches [ 89 , 90 , 91 , 92 , 93 ]. A total of 11 patients were collected and 3 (27.27%) required an appendix stump suture. No complications or conversions were reported. Moreover, Hüttenbrink et al. [ 94 ] described incidental appendicectomy during robotic prostatectomy. Figure 3 shows our experience during RS for complicated sigmoid diverticulitis with sigmoid-bladder fistula. Lunardi et al. [ 95 ] presented an interesting analysis of temporal trends in the use of minimally invasive surgery in Abdominal Emergency and Urgent Settings. The authors compared 89,098 emergency colectomies performed between 2013 and 2021. The increase per year for robotic colectomy was 0.9% (from 1.4% of total procedures in 2013 to 8.8% in 2021). As a result of this increase, a 0.7% decrease was registered for the open approach. Furthermore, patients who underwent RS were older, had more comorbidities and had higher BMI when compared to laparoscopic and open groups. Intraoperative outcomes were encouraging for RS: after Propensity Score Matching, a conversion rate of 25.5% (860/3,375 patients) was registered during laparoscopic surgery, while in 11.2% (379/3,375 patients) of RS cases, a conversion to open was required ( p < 0.001). After Propensity Score Marching of patients underwent Emergency surgery only, RS demonstrated advantages in terms of conversion to open (27.5% vs. 12% in laparoscopic and robotic groups respectively, p < 0.001) and post-operative LOS (7.12 vs. 6.85 days respectively, p = 0.001). In conclusion, conventional open surgery should be recommended for unstable and frail patients who require time-critical surgery. Nevertheless, it could be underlined that stable and frail patients may benefit from an enhanced recovery after surgery associated with RS in the acute setting when compared to open surgery. 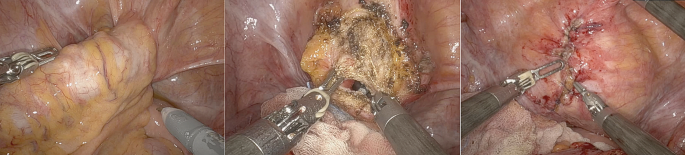 Robotic approach during emergency setting for patients affected by complicated sigmoid diverticulitis with sigmoid-bladder fistula. We performed a fistula resection and bladder suture in double-layer barbed suture Robotics in acute cholecystitis and biliary tree diseasesAnother interesting field of application in AES may be the biliary tree and gallbladder diseases including cholecystitis, Mirizzi syndromes, biliary fistulas, iatrogenic diseases and common bile duct stones. In 2016, Kubat et al. [ 96 ] published a retrospective series of 150 consecutive robotic single-site cholecystectomies (74 versus 76 cases treated in emergency scenarios and elective settings respectively). The mean operative time for ES cohort was significantly longer (95.0 ± 4.4 versus 71.9 ± 2.6 min; p < 0.001). Both cohorts required 1 conversion to open (1.35% for the emergency group and 1.31% for the elective group). One bile duct injury (0.7%) was reported in patients treated in emergency conditions. The authors concluded that robotic single-site cholecystectomy can be performed safely and effectively in both elective and urgent scenarios with a learning curve of about 48 cases to reach acceptable perioperative outcomes. Mirizzi syndrome represents one of the most challenging complications of cholelithiasis [ 97 , 98 , 99 ]. In 2014, Lee et al. [ 97 ] evaluated the outcomes of five patients treated by endoscopic biliary stent placement and subsequent robotic partial cholecystectomy due to Mirizzi syndrome. No conversion to open was reported and all patients experienced an uneventful postoperative course. In 2017 Magge et al. [ 98 ] reported a 6-patient series. All cases were treated performing a combined endoscopic and robotic approaches. In 3 cases (50%) a Roux-en-Y hepatico-jejunostomy was carried out. In these challenging scenarios, RS showed relevant benefits when compared to laparoscopy, facilitating complex dissections, and reducing conversion to open rate. The most representative cohort of patients was described by Gangemi et al. [ 100 ] in 2017. Authors compared a large series of 676 patients receiving a robotic cholecystectomy with 284 treated by conventional laparoscopy: data analysis showed a significantly lower conversion to open in RS group, especially in patients affected by acute or gangrenous cholecystitis. A 3-patient experience was described by Milone et al. [ 101 ] in 2019, achieving good perioperative outcomes in acute cholecystitis treatment. Major bile duct injuries after cholecystectomy require complex surgical repairs that are usually performed with a conventional open approach [ 102 ]. This field may represent an interesting application of RS to safety perform biliary anastomosis. Cubisino et al. presented a systematic review of 13 literature experiences on minimally invasive biliary anastomosis after iatrogenic bile duct injury [ 103 ]. 198 patients were included. 135 patients (63.1%) underwent laparoscopic biliary anastomosis, while 73 (36.1%) received an analogue robotic procedure. According to Strasberg’s classification [ 104 ], all Bile Duct Injuries were types D and E (E1–E5). No conversions occurred in the RS series, while 4 patients required conversion to open surgery among the laparoscopic ones. Postoperative complications were superimposable (18.7% and 19.7% in laparoscopic and robotic approaches, respectively). Nevertheless, the overall reoperation rate was 4.4%, 5.5% in laparoscopic and 2.6% in robotic repairs. During the follow-up period (median 24.6 months), 9 patients developed an anastomotic stricture: 5 (3.70%) in laparoscopic and 4 (5.48%) in robotic series that required a redo-anastomosis in 60% and 25% respectively. When compared to open and laparoscopic cholecystectomy in AES, RS showed an increase of 0.7% per year in Lunardi et al. cohort of 793’800 cholecystectomies [ 95 ], ranging from 2.5 to 8.8% between 2013 and 2021. It could be underlined that conversion rate and LOS were statistically lower in RS group ( p < 0.001). Despite these findings, laparoscopic cholecystectomy yet represents the preferred approach in AES. Robotics emergencies in hernia and abdominal wall surgeryOnly a few studies analyzed urgent hernia operations treated using robotic surgery. In 2020, Bou-Ayash et al. [ 105 ] published a retrospective series of 19 patients (including 23 surgical procedures) affected by inguinal hernia, treated from 2013 to 2020. The authors concluded that the robotic approach represents a safe procedure in selected patients, with a short length of stay and a low complication rate compared to open and laparoscopic surgery. In 2021, Kudsi et al. [ 106 ] described perioperative outcomes of RS in a 34-patient cohort treated between 2013 and 2019. All patients experienced robotic ventral and incisional hernia repair in an emergency setting. 20% of patients were classified as Clavien-Dindo I or II, while about 11% Clavien-Dindo III and IV. Only 3% of the population experienced a recurrence. Muysoms et al. [ 107 ] performed an extensive analysis of robotic cost. They retrospective evaluate laparoscopic (272 procedures of which 6 were emergency cases) and robotic (404 procedures of which 8 were emergency cases) inguinal hernia repairs. As reported in other literature experiences, authors concluded that Robotic inguinal hernia repair was significantly ( p < 0.001) more expensive if compared to laparoscopic surgery (mean cost €2612 versus €1963, respectively). Nevertheless, in the robotic group, a larger number of patients were treated as outpatients with lower postoperative complications. Regarding inguinal and ventral hernia repair, the analysis conducted by Lunardi et al. [ 95 ] showed encouraging data for RS approach: from 2013 to 2021 RS increased of 1.9% per year and 1.1% per year respectively. After propensity score matching, authors reported superimposable data in terms of CCI and BMI, comparing laparoscopic and robotic approaches. Nonetheless, RS showed benefits also in these fields: lower conversion rates were reported both in inguinal hernia repairs (18.1% vs. 3.8%, p < 0.001) and in ventral hernia repair (16.2% vs. 4.8%, p < 0.001). In addition, a statistically significant shorter postoperative LOS was registered in the RS group (the mean LOS in the inguinal hernia group was 3.34 vs. 3 days in laparoscopic and robotic approaches respectively, and the mean LOS in the ventral hernia group was 3.87 vs. 3.73 days, respectively). Other abdominal emergency surgery and future perspectivesA rare indication for urgent RS was post-traumatic splenic bleeding reported by Giulianotti et al. [ 108 ]. Until now, no reports of RS in adhesive intestinal obstruction have been published. A possible and useful application of RS is represented by telementoring and telesurgery [ 32 , 109 , 110 , 111 ]. The original aim of RS and the recent COVID-19 pandemic gave an important incentive in these directions. The advantage of telementoring and telepresence of an expert surgeon in a virtual way is nowadays possible and may be improved thanks to the modern and future highspeed internet connection (5G networks) as well as the telesurgery in ultra-remote countries, in low-volume centers and in an emergent civil or battlefield surgical scenarios [ 112 , 113 , 114 ]. The development of new modular robotic platforms may contribute to increase RS applications in emergency settings. Nowadays, several different robotic platforms are approved for human use, such as CMR Versius (Cambridge Medical Robotics, Cambridge, UK), Distalmotion Dexter (Distalmotion, Epalinges, Switzerland) and Medtronic Hugo (Medtronic Inc., Minneapolis, USA). Most of them share the opportunity of switching from a conventional laparoscopic setting to a robot-assisted one. LimitationsThe main bias of our study was represented by hospital organisations: RS devices are available in the same building as the General Surgery Unit at San Donato Hospital (Arezzo, Italy) facilitating emergency surgical procedures. On the other hand, Da Vinci Xi is situated in a separate building specifically dedicated to RS at the General and Robotic Surgery Unit of San Giovanni Battista Hospital (Foligno, Italy). Furthermore, these findings represented a limit when the surgeons’ team wanted to perform a laparoscopic exploration to validate a minimally invasive robotic approach in emergency scenarios. In our experience, it should also underline that the COVID-19 era has contributed to limiting RS adoption. Future shreds of evidence from randomized clinical trials with long-term follow-up are required to define the potential role of RS in AES. Nevertheless, the unavailable data on the cost-effectiveness of RS in AES are linked to lower use of robotic devices if compared to laparoscopic approaches. Our experience suggested that RS costs are superimposable to laparoscopic surgery if we analyse LOS and conversion rate data. To optimize the delivery of robotic technology in AES, a well-coordinated effort among health systems, clinicians, payers, and policymakers and dedicated training program for robotic teams are imperative. Our study demonstrates that RS may be an useful and reliable approach also to emergency surgical procedures, especially when performed in selected patients in very well trained robotic centers allowing a safe managing of surgical challenging procedures as main indications for this technology, reducing the conversion rate when compared to laparoscopy. As for laparoscopy the patient selection for robotic approach need hemodinamically stable condition and require a sharing of the surgical strategy by all the team: surgeons, nurses and anaesthesiologists. All the staff need to be trained in laparoscopic and robotic elective surgery, including technology functioning. The hybrid use of robotic/laparoscopic technology may be taken into consideration (a laparoscopic exploration may be the first step) to decide the following approach. The robotic approach may be reserved to challenging steps of the operation (suture/microsuture/dissections). The availability of the device is the sine qua non condition for emergent and of course urgent use. The current organization in which the platform is shared by different teams, represent for the diffusion of its use in the emergent setting. The cost reduction of platforms and instruments, together with new robotic devices in the health market, may represent a future perspective for emergencies use of robotic technology. So, the robotic technology may be one of the tools available in every operating theatre, to use in selected cases according to patient condition and surgical team experience. Data availabilityNo datasets were generated or analysed during the current study. Surlin V. Emergency and trauma surgery. Chirurgia (Bucur). 2021;116:643–4. Article PubMed Google Scholar E. U. o. M. S. S. o. S. a. E. B. o. Surgery. (2024), vol. 2024. De Simone B, et al. The new timing in acute care surgery (new TACS) classification: a WSES Delphi consensus study. World J Emerg Surg. 2023;18:32. Article PubMed PubMed Central Google Scholar Crepaz L, et al. Minimally invasive approach to incisional hernia in elective and emergency surgery: a SICE (Italian Society of endoscopic surgery and new technologies) and ISHAWS (Italian society of hernia and abdominal wall surgery) online survey. Updates Surg. 2023;75:1671–80. Coletta D, Patriti A. in Updates Surg . Italy. 2023;75:2047–2048. Wakabayashi G, et al. Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:73–86. Gorter RR, et al. Diagnosis and management of acute appendicitis. Surg Endosc. 2016;30:4668–90. EAES consensus development conference 2015. Jara RD, Guerrón AD, Portenier D. Complications of robotic surgery. Surg Clin North Am. 2020;100:461–8. Rocca A, et al. Robotic surgery for colorectal liver metastases resection: a systematic review. Int J Med Robot. 2021;17:e2330. Martins RS, et al. Quality of life after robotic versus conventional minimally invasive cancer surgery: a systematic review and meta-analysis. J Robot Surg. 2024;18:171. Gomez Ruiz M, et al. Robotic surgery for locally advanced T4 rectal cancer: feasibility and oncological quality. Updates Surg. 2023;75:589–97. Chatterjee S, Das S, Ganguly K, Mandal D. Advancements in robotic surgery: innovations, challenges and future prospects. J Robot Surg. 2024;18:28. Minamimura K, et al. Current status of robotic gastrointestinal surgery. J Nippon Med Sch. 2023;90:308–15. Rocca A, et al. Robotic versus open resection for colorectal liver metastases in a referral centre Hub&Spoke learning program. A multicenter propensity score matching analysis of perioperative outcomes. Heliyon. 2024;10:e24800. Ceccarelli G, et al. Robotic revision surgery after failed Nissen anti-reflux surgery: a single center experience and a literature review. J Robot Surg. 2023;17:1517–24. Knitter S, et al. Robotic versus laparoscopic versus open major hepatectomy - an analysis of costs and postoperative outcomes in a single-center setting. Langenbecks Arch Surg. 2023;408:214. Liu R, Liu Q, Wang Z. Worldwide diffusion of robotic approach in general surgery. Updates Surg. 2021;73:795–7. Daskalaki D, et al. Financial impact of the robotic approach in liver surgery: a comparative study of clinical outcomes and costs between the robotic and open technique in a single institution. J Laparoendosc Adv Surg Tech A. 2017;27:375–82. de’Angelis N, et al. Robotic versus laparoscopic gastric resection for primary gastrointestinal stromal tumors > 5 cm: a size-matched and location-matched comparison. Surg Laparosc Endosc Percutan Tech. 2017;27:65–71. van Dam P et al. Are costs of robot-assisted surgery warranted for gynecological procedures? Obstet Gynecol Int. 2011;2011:973830. Vicente E, Quijano Y, Ferri V, Caruso R. Robot-assisted cholecystectomy with the new HUGO™ robotic-assisted system: first worldwide report with system description, docking settings, and video. Updates Surg. 2023;75:2039–42. Leal Ghezzi T, Campos Corleta O. 30 years of robotic surgery. World J Surg. 2016;40:2550–7. Sarkaria IS et al. Early operative outcomes and learning curve of robotic assisted giant paraesophageal hernia repair. Int J Med Robot. 2017;13. Felder SI, et al. Robotic gastrointestinal surgery. Curr Probl Surg. 2018;55:198–246. Ceccarelli G et al. Minimally invasive approach to gastric GISTs: analysis of a multicenter robotic and laparoscopic experience with literature review. Cancers (Basel). 2021;13. Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Robot-assisted laparoscopic surgery of the colon and rectum. Surg Endosc. 2012;26:1–11. Yeo HL, Isaacs AJ, Abelson JS, Milsom JW, Sedrakyan A. Comparison of open, laparoscopic, and robotic colectomies using a large national database: outcomes and trends related to surgery center volume. Dis Colon Rectum. 2016;59:535–42. de’Angelis N, et al. Robotic versus laparoscopic colorectal cancer surgery in elderly patients: a propensity score match analysis. J Laparoendosc Adv Surg Tech A. 2018;28:1334–45. Cheung TT, et al. Robotic versus laparoscopic liver resection for huge (≥ 10 cm) liver tumors: an international multicenter propensity-score matched cohort study of 799 cases. Hepatobiliary Surg Nutr. 2023;12:205–15. Cillo U, D’Amico FE, Furlanetto A, Perin L, Gringeri E. Robotic hepatectomy and biliary reconstruction for perihilar cholangiocarcinoma: a pioneer western case series. Updates Surg. 2021;73:999–1006. Giulianotti PC, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003;138:777–84. de’Angelis N, et al. Robotic surgery in emergency setting: 2021 WSES position paper. World J Emerg Surg. 2022;17:4. Solaini L, et al. Open versus laparoscopic versus robotic gastric gastrointestinal stromal tumour resections: a multicentre cohort study. Int J Med Robot. 2021;17:e2198. Wei D, Johnston S, Goldstein L, Nagle D. Minimally invasive colectomy is associated with reduced risk of anastomotic leak and other major perioperative complications and reduced hospital resource utilization as compared with open surgery: a retrospective population-based study of comparative effectiveness and trends of surgical approach. Surg Endosc. 2020;34:610–21. Giovannetti A, et al. Laparoendoscopic single-site (LESS) versus robotic redo hiatal hernia repair with fundoplication: which approach is better? Am Surg. 2019;85:978–84. Colvin J, et al. A comparison of robotic versus laparoscopic adrenalectomy in patients with primary hyperaldosteronism. Surg Laparosc Endosc Percutan Tech. 2017;27:391–3. Tolboom RC, Draaisma WA, Broeders IA. Evaluation of conventional laparoscopic versus robot-assisted laparoscopic redo hiatal hernia and antireflux surgery: a cohort study. J Robot Surg. 2016;10:33–9. Kim HI, et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann Surg. 2016;263:103–9. Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–24. Ceccarelli G, et al. Intraoperative and postoperative outcome of robot-assisted and traditional laparoscopic Nissen fundoplication. Eur Surg Res. 2009;43:198–203. Article CAS PubMed Google Scholar Ceccarelli G, et al. Robot-assisted surgery in elderly and very elderly population: our experience in oncologic and general surgery with literature review. Aging Clin Exp Res. 2017;29:55–63. Ceccarelli G, et al. A new robot-assisted Billroth-I reconstruction: details of the technique and early results. Surg Laparosc Endosc Percutan Tech. 2018;28:e33–9. Ceccarelli G, et al. Robot-assisted liver surgery in a general surgery unit with a referral centre hub&spoke learning program. Early outcomes after our first 70 consecutive patients. Minerva Chir. 2018;73:460–8. Ceccarelli G, et al. Robot-assisted Toupet fundoplication and associated cholecystectomy in symptomatic giant hiatal hernia with situs viscerum inversus-A case report and literature review. Int J Surg Case Rep. 2019;60:371–5. Ceccarelli G, et al. Minimally invasive laparoscopic and robot-assisted emergency treatment of strangulated giant hiatal hernias: report of five cases and literature review. World J Emerg Surg. 2020;15:37. Ceccarelli G, et al. Minimally invasive robotic-assisted combined colorectal and liver excision surgery: feasibility, safety and surgical technique in a pilot series. Updates Surg. 2021;73:1015–22. Costa G, et al. Clinico-pathological features of colon cancer patients undergoing emergency surgery: a comparison between elderly and non-elderly patients. Open Med (Wars). 2019;14:726–34. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49:239–43. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. Sermonesi G, et al. Cesena guidelines: WSES consensus statement on laparoscopic-first approach to general surgery emergencies and abdominal trauma. World J Emerg Surg. 2023;18:57. Reinisch A, Liese J, Padberg W, Ulrich F. Robotic operations in urgent general surgery: a systematic review. J Robot Surg. 2023;17:275–90. Capibaribe DM, Avilez ND, Sacomani CAR, Lucena A, Reis LO. Robotic approach to vesicourethral anastomotic stenosis and resection of remaining prostate after radical prostatectomy. Int Braz J Urol. 2023;49:158–60. Huser AS, et al. Simulated life-threatening emergency during robot-assisted surgery. J Endourol. 2014;28:717–21. Ballas DA, Cesta M, Gothard D, Ahmed R. Emergency undocking curriculum in robotic surgery. Cureus. 2019;11:e4321. PubMed PubMed Central Google Scholar van der Schans EM, Hiep MAJ, Consten ECJ, Broeders I. From Da Vinci Si to Da Vinci Xi: realistic times in draping and docking the robot. J Robot Surg. 2020;14:835–9. Alfieri S, et al. Short-term and long-term outcomes after robot-assisted versus laparoscopic distal pancreatectomy for pancreatic neuroendocrine tumors (pNETs): a multicenter comparative study. Langenbecks Arch Surg. 2019;404:459–68. Abdel Raheem A, et al. Da Vinci Xi and Si platforms have equivalent perioperative outcomes during robot-assisted partial nephrectomy: preliminary experience. J Robot Surg. 2017;11:53–61. Yuh B, et al. Use of a mobile tower-based robot–the initial Xi robot experience in surgical oncology. J Surg Oncol. 2016;113:5–7. Hollandsworth HM, et al. Multiquadrant surgery in the robotic era: a technical description and outcomes for Da Vinci Xi robotic subtotal colectomy and total proctocolectomy. Surg Endosc. 2020;34:5153–9. Bianchi G, et al. Short-term outcomes of Da Vinci Xi versus Si robotic systems for minor hepatectomies. Acta Biomed. 2022;93:e2022223. Hill A, McCormick J. In experienced hands, does the robotic platform impact operative efficiency? Comparison of the Da Vinci Si versus Xi robot in colorectal surgery. J Robot Surg. 2020;14:789–92. Oldani A, Bellora P, Monni M, Amato B, Gentilli S. Colorectal surgery in elderly patients: our experience with DaVinci Xi ® system. Aging Clin Exp Res. 2017;29:91–9. Gallotta V, et al. Robotic surgery in elderly and very elderly gynecologic cancer patients. J Minim Invasive Gynecol. 2018;25:872–7. Buchs NC, et al. Safety of robotic general surgery in elderly patients. J Robot Surg. 2010;4:91–8. Barberio M, et al. Quantitative fluorescence angiography versus hyperspectral imaging to assess bowel ischemia: a comparative study in enhanced reality. Surgery. 2020;168:178–84. Liot E, et al. Does near-infrared (NIR) fluorescence angiography modify operative strategy during emergency procedures? Surg Endosc. 2018;32:4351–6. Sudan R, Desai SS. Emergency and weekend robotic surgery are feasible. J Robot Surg. 2012;6:263–6. Cubas R, Garcia M, Mukherjee K. Robotic repair of incarcerated morgagni hernia in an adult on the acute care surgery service. Rev Fac Cien Med Univ Nac Cordoba. 2021;78:91–4. Kim JK, Desai A, Kunac A, Merchant AM, Lovoulos C. Robotic Transthoracic Repair of a Right-Sided Traumatic Diaphragmatic Rupture. Surg J (N Y). 2020;6(3):e164–e166. Hosein S, Carlson T, Flores L, Armijo PR, Oleynikov D. Minimally invasive approach to hiatal hernia repair is superior to open, even in the emergent setting: a large national database analysis. Surg Endosc. 2021;35:423–8. Robinson TD, et al. Emergent robotic versus laparoscopic surgery for perforated gastrojejunal ulcers: a retrospective cohort study of 44 patients. Surg Endosc. 2022;36:1573–7. Sartelli M, et al. 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg. 2020;15:32. de’Angelis N, et al. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg. 2018;13:5. Marano A, Giuffrida MC, Giraudo G, Pellegrino L, Borghi F. Management of peritonitis after minimally invasive colorectal surgery: can we stick to laparoscopy? J Laparoendosc Adv Surg Tech A. 2017;27:342–7. Wind J, et al. Laparoscopic reintervention for anastomotic leakage after primary laparoscopic colorectal surgery. Br J Surg. 2007;94:1562–6. Vennix S, et al. Emergency laparoscopic sigmoidectomy for perforated diverticulitis with generalised peritonitis: a systematic review. Dig Surg. 2016;33:1–7. Pedraza R, Ragupathi M, Martinez T, Haas EM. Robotic-assisted laparoscopic primary repair of acute iatrogenic colonic perforation: case report. Int J Med Robot. 2012;8:375–8. Felli E, et al. Robotic right colectomy for hemorrhagic right colon cancer: a case report and review of the literature of minimally invasive urgent colectomy. World J Emerg Surg. 2014;9:32. Chen ZL, Du QL, Zhu YB, Wang HF. A systematic review and meta-analysis of short-term outcomes comparing the efficacy of robotic versus laparoscopic colorectal surgery in obese patients. J Robot Surg. 2024;18:167. Alkhamis A, et al. Outcomes in robotic-assisted compared to laparoscopic-assisted colorectal surgery in a newly established colorectal tertiary center: a retrospective comparative cohort study. J Robot Surg. 2024;18:152. de Almeida Leite RM et al. Surgical and medical outcomes in robotic compared to laparoscopic colectomy global prospective cohort from the American college of surgeons national surgical quality improvement program. Surg Endosc. 2024. Beltzer C, et al. Robotic versus laparoscopic sigmoid resection for diverticular disease: a single-center experience of 106 cases. J Laparoendosc Adv Surg Tech A. 2019;29:1451–5. Kudsi OY, Gokcal F. Urgent robotic mesocolic excision for obstructing proximal transverse colon cancer - a video vignette. Colorectal Dis. 2019;21:1093–4. Kudsi OY, Bou-Ayash N. Bleeding sigmoid diverticulosis - urgent stapleless totally robotic sigmoidectomy-a video vignette. Colorectal Dis. 2020;22:1205. Kudsi OY, Bou-Ayash N. Caecal volvulus - urgent totally robotic right colectomy - a video vignette. Colorectal Dis. 2020;22:1448–9. Anderson M, et al. Early experience with urgent robotic subtotal colectomy for severe acute ulcerative colitis has comparable perioperative outcomes to laparoscopic surgery. J Robot Surg. 2020;14:249–53. Yang Y, et al. The global burden of appendicitis in 204 countries and territories from 1990 to 2019. Clin Epidemiol. 2022;14:1487–99. Cadière GB, et al. Feasibility of robotic laparoscopic surgery: 146 cases. World J Surg. 2001;25:1467–77. Kelkar D, Borse MA, Godbole GP, Kurlekar U, Slack M. Interim safety analysis of the first-in-human clinical trial of the versius surgical system, a new robot-assisted device for use in minimal access surgery. Surg Endosc. 2021;35:5193–202. Kibar Y, Yalcin S, Kopru B, Kaya E, Topuz B, Ebiloglu T. Robot-Assisted Laparoscopic Repair of Spontaneous Appendicovesical Fistula. J Endourol Case Rep. 2016;2(1):111–3. Yi B, et al. The first clinical use of domestically produced Chinese minimally invasive surgical robot system micro hand S. Surg Endosc. 2016;30:2649–55. Yi B, et al. Domestically produced Chinese minimally invasive surgical robot system micro hand S is applied to clinical surgery preliminarily in China. Surg Endosc. 2017;31:487–93. Hüttenbrink C, et al. Incidental appendectomy during robotic laparoscopic prostatectomy-safe and worth to perform? Langenbecks Arch Surg. 2018;403:265–9. PubMed Google Scholar Lunardi N, et al. Robotic technology in emergency general surgery cases in the era of minimally invasive surgery. JAMA Surg. 2024;159:493–9. Kubat E, Hansen N, Nguyen H, Wren SM, Eisenberg D. Urgent and elective robotic single-site cholecystectomy: analysis and learning curve of 150 consecutive cases. J Laparoendosc Adv Surg Tech A. 2016;26:185–91. Lee KF, et al. A minimally invasive strategy for Mirizzi syndrome: the combined endoscopic and robotic approach. Surg Endosc. 2014;28:2690–4. Magge D, et al. Performing the difficult cholecystectomy using combined endoscopic and robotic techniques: how I do it. J Gastrointest Surg. 2017;21:583–9. Valderrama-Treviño AI, et al. Updates in Mirizzi syndrome. Hepatobiliary Surg Nutr. 2017;6:170–8. Gangemi A, Danilkowicz R, Bianco F, Masrur M, Giulianotti PC. Risk factors for open conversion in minimally invasive cholecystectomy. Jsls. 2017;21. Milone M, et al. Robotic cholecystectomy for acute cholecystitis: three case reports. Med (Baltim). 2019;98:e16010. Article CAS Google Scholar Giuliante F, et al. Bile duct injury after cholecystectomy: timing of surgical repair should be based on clinical presentation. The experience of a tertiary referral center with Hepp-Couinaud hepatico-jejunostomy. Updates Surg. 2023;75:1509–17. Cubisino A, Dreifuss NH, Cassese G, Bianco FM, Panaro F. Minimally invasive biliary anastomosis after iatrogenic bile duct injury: a systematic review. Updates Surg. 2023;75:31–9. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–25. CAS PubMed Google Scholar Bou-Ayash N, Gokcal F, Kudsi OY. Robotic inguinal hernia repair for incarcerated hernias. J Laparoendosc Adv Surg Tech A. 2021;31:926–30. Kudsi OY, Bou-Ayash N, Chang K, Gokcal F. Perioperative and midterm outcomes of emergent robotic repair of incarcerated ventral and incisional hernia. J Robot Surg. 2021;15:473–81. Muysoms F et al. Economic assessment of starting robot-assisted laparoscopic inguinal hernia repair in a single-centre retrospective comparative study: the EASTER study. BJS Open. 2021;5. Giulianotti PC, et al. Robot-assisted treatment of splenic artery aneurysms. Ann Vasc Surg. 2011;25:377–83. Smith AL, et al. Dual-console robotic surgery: a new teaching paradigm. J Robot Surg. 2013;7:113–8. Thomas A, et al. Effective implementation and adaptation of structured robotic colorectal programme in a busy tertiary unit. J Robot Surg. 2021;15:731–9. Panteleimonitis S, et al. Implementation of robotic rectal surgery training programme: importance of standardisation and structured training. Langenbecks Arch Surg. 2018;403:749–60. Zheng J, et al. 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc. 2020;34:5172–80. Mohan A, Wara UU, Arshad Shaikh MT, Rahman RM, Zaidi ZA. Telesurgery and robotics: an improved and efficient era. Cureus. 2021;13:e14124. Anvari M, Manoharan B, Barlow K. From telementorship to automation. J Surg Oncol. 2021;124:246–9. Giulianotti PC, Quadri P, Durgam S, Bianco FM. Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? Short clinical report. Ann Surg. 2018;267:e7–9. Cuendis-Velázquez A, et al. A new era of bile duct repair: robotic-assisted versus laparoscopic hepaticojejunostomy. J Gastrointest Surg. 2019;23:451–9. Marino MV, Mirabella A, Guarrasi D, Lupo M, Komorowski AL. Robotic-assisted repair of iatrogenic common bile duct injury after laparoscopic cholecystectomy: surgical technique and outcomes. Int J Med Robot. 2019;15:e1992. Sucandy I, et al. Robotic versus open extrahepatic biliary reconstruction for iatrogenic bile duct injury. Am Surg. 2022;88:345–7. D’Hondt M, Wicherts DA. Robotic biliary surgery for benign and malignant bile duct obstruction: a case series. J Robot Surg. 2023;17:55–62. Download references This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Author informationAuthors and affiliations. Department of General Surgery, “San Giovanni Battista” Hospital, USL Umbria 2, Foligno, Perugia, Italy Graziano Ceccarelli, Fabio Rondelli & Michele De Rosa Division of General Surgery, Bufalini Hospital, Cesena, Italy Fausto Catena Department of General Surgery and Hepatobiliary and Pancreatic Surgery Unit, Pineta Grande Hospital, Castel Volturno, Caserta, Italy Pasquale Avella & Aldo Rocca Department of Medicine and Health Science “V. Tiberio”, University of Molise, Campobasso, Italy Pasquale Avella, Germano Guerra & Aldo Rocca Department of General Surgery, Singapore General Hospital, Singapore, Singapore Brian WCA Tian You can also search for this author in PubMed Google Scholar ContributionsG.C.: study conception and design, literature search, data acquisition, interpretation and analysis; drafting and critically revising the article for important intellectual content; final approval of the version to be published. P.A.: literature search, data acquisition, interpretation and analysis; drafting and critically revising the article for important intellectual content; final approval of the version to be published. F.C.: drafting and critically revising the article for important intellectual content; final approval of the version to be published. B.W.T.: data acquisition, interpretation and analysis; final approval of the version to be published. F.R.: study conception and design, literature search, data acquisition, interpretation and analysis; final approval of the version to be published. All authors: data acquisition, interpretation, and analysis; final approval of the version to be published. A.R.: supervision, drafted and critically revised the article for important intellectual content; final approval of the version to be published. Corresponding authorCorrespondence to Pasquale Avella . Ethics declarationsHuman ethics and consent to participate. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. An informed consent for treating personal and sensible data was obtained from all patients before the data collection and evaluation. The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of the University of Molise (protocol number 10/21, approved date: May 12, 2021). Consent to publishPatients signed informed consent regarding publishing their data and photographs. Competing interestsThe authors declare no competing interests. Additional informationPublisher’s note. Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. Rights and permissionsOpen Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data. Reprints and permissions About this articleCite this article. Ceccarelli, G., Catena, F., Avella, P. et al. Emergency robotic surgery: the experience of a single center and review of the literature. World J Emerg Surg 19 , 28 (2024). https://doi.org/10.1186/s13017-024-00555-6 Download citation Received : 14 May 2024 Accepted : 22 July 2024 Published : 17 August 2024 DOI : https://doi.org/10.1186/s13017-024-00555-6 Share this articleAnyone you share the following link with will be able to read this content: Sorry, a shareable link is not currently available for this article. Provided by the Springer Nature SharedIt content-sharing initiative
World Journal of Emergency SurgeryISSN: 1749-7922
Obesity Drug Case Study Links Man's Heart Problems With Extreme Weight Loss A case study of a 62-year-old man in the US provides a prime example of why it's so important to keep a close eye on rapid weight loss while juggling medications. At 132 kg (291 lbs), the man qualified as obese, a factor that may have contributed to his development of type 2 diabetes and may have been linked closely with another of his conditions, an underactive thyroid gland. Consequently his family doctor prescribed him with daily insulin injections, as well as a daily dose of a thyroid hormone replacement drug called levothyroxine . He was also told to take a weekly dose of the diabetes and weight loss drug tirzepatide (sold under the brand name Zepbound). Tirzepatide is one of a growing number of popular weight loss drugs that mimic the hormones GLP-1 (glucagon-like peptide-1) and GIP (gastric inhibitory polypeptide) to manage blood sugar levels and appetite. The treatment was so effective the man's weight dropped by 39 kg (86 lbs), or almost 30 percent of his body weight, in just six months. Unfortunately, his weight loss came with a sting in the tail. Shortly after, the man presented himself to an emergency department suffering from "palpitations, excessive sweating, confusion, fever , and hand tremors", according to the case study written up by a team from the University of Colorado. After getting checked out, it was revealed that the palpitations were a sign of atrial fibrillation ; an irregular heartbeat condition that can trigger strokes and heart attacks. Further tests showed this had been brought on by thyrotoxicosis , which is an overabundance of a hormone produced by the thyroid. Or, in this case, a medication designed to look just like it. Dosages for many medications are weight based. So as the man lost weight, the relative dosage of levothyroxine crept higher. At his initial weight he was takening 1.5 μg per kilogram of his weight. By the end that had inadvertantly jumped to 2.15 μg per kilogram. All of this could have been prevented if the man had adjusted his other medications in relation to his changing weight. The levothyroxine should have been adjusted as his weight changed to avoid the thyrotoxicosis and atrial fibrillation, according to the case study authors. The man also missed a scheduled follow-up appointment with his doctor due to traveling, which may have played a part in this lapse in monitoring. Losing a lot of weight quickly does come with potential risks , as well as all the health benefits, and previous studies have shown it's important to maintain good health in other areas while trying to shed the pounds. Tirzepatide has proved very effective in tackling obesity – but when it comes to any extreme weight loss strategy, patients (and their existing medications) need to be closely monitored to prevent other health problems from arising. "With the increasing use of tirzepatide and other GLP-1 analogues for the treatment of patients with obesity, we recommend evaluating patients using tirzepatide closely (every 4 to 6 weeks initially) for assessment of therapy response, adverse events, and possible dose adjustment of other concomitant medications," write the case study authors. The research has been published in JAMA Internal Medicine .  |
IMAGES
COMMENTS
The 12-year results of this controlled, prospective study show that Roux-en-Y gastric bypass offered long-term durability of weight loss and was associated with fewer obesity-related coexisting ...
Sjoström et al. 10 published 2-and 10-year data from the Swedish Obese Subjects (SOS) study of 4,047 morbidly obese subjects who underwent bariatric surgery and matched control subjects. At the end of 2 years, the incidence of diabetes in subjects who underwent bariatric surgery was 1.0%, compared to 8.0% in the control subjects.
Bariatric surgery results in weight loss and health improvements in adults and adolescents. However, whether outcomes differ according to the age of the patient at the time of surgery is unclear. W...
Substantial short- and long-term weight loss after bariatric surgery was a notable outcome in this study. Consistent with previous meta-analyses on weight reduction after bariatric surgery, our findings showed that RYGB and SG offer superior weight reduction outcomes compared to GB or MT [30,31,32]. Long-term outcomes showed that RYGB was the ...
In this multicenter, prospective study of bariatric surgery in adolescents, we found significant improvements in weight, cardiometabolic health, and weight-related quality of life at 3 years after ...
The patient was evaluated by the bariatric multidisciplinary team at Sibley Memorial Hospital and approved for surgery. The patient underwent a minimally invasive Roux-en-Y gastric bypass using the latest camera technology. After her procedure, a new technique was used to test the gastro-jejunal anastomosis for any signs of a leak.
Participants in our study had a pre-surgical mean BMI of 52 kg/m 2. Patients with a pre-surgical BMI of ≥ 50 kg/m 2 are more likely to regain weight, while a lower pre-surgical BMI has been associated with more successful weight loss outcomes 12 to 36 months after surgery [ 48 ]. These findings and the fact that our sample had a mean BMI > 50 ...
Obesity Surgery is a premier interdisciplinary and international forum for the dissemination of research and clinical knowledge on all aspects of bariatric/metabolic surgery.. Welcomes papers from all disciplines involved in the surgical treatment and care of patients suffering from severe obesity. With our focus on promoting inclusiveness, we aim to increase awareness of obesity and ...
The results found in this meta-analysis indicated that the highest prevalence of WR was observed in cross-sectional studies and case-control studies compared to cohort studies (52% versus 48%) with high overall ... Weight regain after bariatric surgery—a Multicentre study of 9617 patients from Indian bariatric surgery outcome reporting group. ...
A Detailed Case Study of Bariatric Surgery in Kaiser Permanente Southern California. Pouya Shafipour, MS, MD, Jack K Der-Sarkissian, ... generally referred to as bariatric surgery. Most bariatric surgery studies have shown excellent weight-loss rates for up to two years after surgery, with patients losing an average of 61 % of their excess ...
The purpose of this Evidence Analysis Library systematic review is to provide an evidence-based summary of nutrition-related practices in bariatric surgery. The systematic review methodology of the Academy of Nutrition and Dietetics was applied. A total of 27 research studies were included, analyzed, and assessed for risk of bias by trained ...
Bariatric surgery is effective for the treatment of patients with morbid obesity and type 2 diabetes mellitus (T2DM), for body weight loss and glycemic control. However, in Japan, there has been no previous report of the effectiveness bariatric surgery in a case of morbid obesity associated with acute onset type 1 diabetes mellitus (T1DM), in which pancreatic β-cells were destroyed and ...
Purpose: Craniopharyngiomas are tumors located in the hypothalamic region which leads to obesity in about 50% of cases. Long-term efficacy and safety of bariatric surgery are lacking in this peculiar population. The aim of this study is to determine the 5-year weight loss and resolution of type 2 diabetes (T2D) after bariatric surgery in patients operated on craniopharyngioma who had developed ...
CASE STUDY. B. L. is a 15-year-old male adolescent who was referred to the weight clinic with a body mass index (BMI) of 50. He was referred based on his history of severe obesity and nonalcoholic fatty liver disease for a discussion of weight loss surgery. B. L. has experienced obesity since childhood. B.
By 2030, the number of overweight adults is projected to be 2.16 billion, with 1.12 billion obese individuals if recent trends continue, represent-ing more than 86% of adults (Kelly, Yang, Chen, Reynolds, & He, 2008). The high prevalence of obesity is associated with an increase in the prevalence of obesity comorbidities.
Background: Obesity is a global health crisis with profound implications on various body systems, contributing to a series of comorbidities. Metabolic Bariatric Surgery (MBS) has emerged as an effective treatment option for severe obesity, with significant weight reduction and potential systemic physiological alterations.
Other options for individual weight control include bariatric surgery and drugs. The release of semaglutide (brand name Wegovy) has rekindled interest in drug therapy for obesity (Wilding et al., 2021). A prospective study of 1,961 adults followed by Wilding and colleagues for more than a year showed that a weekly injection of semaglutide reduced
The patient continued AOM long-term, having lost 90 pounds over a 2 year time period ( Figure 1 ). Her BMI now is 28.7 kg/m 2, weight 205 lbs. (reversed from Class 3 obesity, BMI 46 kg/m 2, weight 295 lbs.) with improvement in quality of life and obesity-related comorbidities. Liver transaminases that were previously elevated in the context of ...
Observational studies have shown improvement in patients with type 2 diabetes mellitus after bariatric surgery. In this randomized, nonblinded, single-center trial, we evaluated the efficacy of int...
Case Study 2 used highly robust data from the NHS, Public Health England and ONS, which importantly included objective data on obesity diagnoses, surgery, cancer incidences and deaths.
Purpose Craniopharyngiomas are tumors located in the hypothalamic region which leads to obesity in about 50% of cases. Long-term efficacy and safety of bariatric surgery are lacking in this peculiar population. The aim of this study is to determine the 5-year weight loss and resolution of type 2 diabetes (T2D) after bariatric surgery in patients operated on craniopharyngioma who had developed ...
The 2008 AACE/ASMBS/TOS guidelines for bariatric surgery identify a lack of comprehension of risks, benefits, expected outcomes, alternatives, and lifestyle changes required with bariatric surgery as a contraindication [1] and the updated 2013 guidelines focus on the need for informed consent [2]. Such contraindications were also noted, in part, by the National Institutes of Health consensus ...
"Bariatric surgery is an effective treatment for people with severe and complex obesity, but is definitely not an easy option, ... Case Study: Maritza Cruz Rivera, 64.
To examine this possibility, investigators retrospectively compared outcomes between nearly 1000 adults with moderate-to-severe OSA who underwent bariatric surgery for a body-mass index (BMI) of 35-70 kg/m 2 and nearly 13,000 patients with OSA and obesity who did not undergo surgery. The primary endpoint was the first occurrence of MACE ...
Glucagon-like peptide 1 (GLP-1) agonists are medications approved for treatment of diabetes that recently have also been used off label for weight loss. 1 Studies have found increased risks of gastrointestinal adverse events (biliary disease, 2 pancreatitis, 3 bowel obstruction, 4 and gastroparesis 5) in patients with diabetes. 2-5 Because such patients have higher baseline risk for ...
Drugs like Ozempic and Wegovy, known as GLP-1 receptor agonists, have surged in popularity as treatment for weight loss and management. The increase involves not only adults but also adolescents, along with bariatric surgery patients.Michael Kochis, a resident in the Department of Surgery at Massachusetts General Hospital, realized that little research had been done regarding the use of these ...
An area that has seen rapid growth in the numbers of patients travelling abroad, as well as patients in the UK undergoing surgery, is bariatric or weight loss surgery.194 The UK, like many other countries globally, has seen a rapid increase in the numbers of overweight and obese patients, with the Department of Health estimating that one-quarter of the UK population is now clinically obese ...
Robotics in emergency upper-GI and bariatric surgery. One of the earliest studies on RS in AES was published in 2012 [ ]: Sudan et al. experience in complex bariatric surgery involved 2 patients affected by a stomach stricture and an acute abdomen due to perforation with biliary peritonitis after biliopancreatic diversion, respectively. The ...
A case study of a 62-year-old man in the US provides a prime example of why it's so important to keep a close eye on rapid weight loss while juggling medications.. At 132 kg (291 lbs), the man qualified as obese, a factor that may have contributed to his development of type 2 diabetes and may have been linked closely with another of his conditions, an underactive thyroid gland.
Type 2 diabetes and obesity, particularly when they occur together, carry the long-term risk of cardiovascular disease. Studies have shown that losing at least 15% of a person's body weight can ...