Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.

Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is a gay male, not currently sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound

How To Present a Patient: A Step-To-Step Guide
Last Updated on June 24, 2022 by Laura Turner
Updated and verified by Dr. Lee Burnett on March 19, 2022.
The ability to deliver oral case presentations is a core skill for any physician. Effective oral case presentations help facilitate information transfer among physicians and are essential to delivering quality patient care. Oral case presentations are also a key component of how medical students and residents are assessed during their training.
At its core, an oral case presentation functions as an argument. It is the presenter’s job to share the pertinent facts of a patient’s case with the other members of the medical care team and establish a clear diagnosis and treatment plan. Thus, the presenter should include details to support the proposed diagnosis, argue against alternative diagnoses, and exclude extraneous information. While this task may seem daunting at first, with practice, it will become easier. That said, if you are unsure if a particular detail is important to your patient’s case, it is probably best to be safe and include it.
Now, let’s go over how to present a case. While I will focus on internal medicine inpatients, the following framework can be applied to patients in any setting with slight modifications.
Oral case presentations are generally made to a medical care team, which can be composed of medical and pharmacy students, residents, pharmacists, medical attendings, and others. As the presenter, you should strive to deliver an interesting presentation that keeps your team members engaged. Here are a few things to keep in mind:
- Be confident: Speak clearly at the loudest volume appropriate to protect patient privacy, vary your tone to emphasize the most important details, and maintain eye contact with members of your team.
- Don’t fidget : Stand up straight and avoid unnecessary, distracting movements.
- Use your notes : You may glance at your notes from time to time while presenting. However, while there is no need to memorize your presentation, there is no better way to lose your team’s attention than to read your notes to them.
- Be honest: Given the importance of presentations in guiding medical care, never guess or report false information to the team. If you are unsure about a particular detail, say so.
The length of your presentation will depend on various factors, including the complexity of your patient, your audience, and your specialty. I have found that new internal medicine inpatients generally take 5-10 minutes to present. Internal medicine clerkship directors seem to agree. In a 2009 survey , they reported a range of 2-20 minutes for the ideal length of student inpatient presentations, with a median of 7 minutes.
While delivering oral case presentations is a core skill for trainees, and there have been attempts to standardize the format , expectations still vary among attending physicians. This can be a frustrating experience for trainees, and I would recommend that you clarify your attending’s expectations at the beginning of each new rotation. However, I have found that these differences are often stylistic, and content expectations are generally quite similar. Thus, developing a familiarity with the core elements of a strong oral case presentation is essential.
How to Present a Patient
You should begin every oral presentation with a brief one-liner that contains the patient’s name, age, relevant past medical history, and chief complaint. Remember that the chief complaint is why the patient sought medical care in his or her own words. An example of an effective opening is as follows: “Ms. X is a 78-year-old female with a past medical history of chronic obstructive pulmonary disease who presents to the hospital after she felt short of breath at home.”
Following the opener, elaborate on why the patient sought medical care. Describe the events that preceded the patient’s presentation in chronological order. A useful mnemonic to use when deciding what to report is OPQRST , which includes: • The Onset of the patient’s symptoms • Any Palliative or Provoking factors that make the symptoms better or worse, respectively • The Quality of his or her symptoms (how he or she describes them) • The Region of the body where the patient is experiencing his or her symptoms and (if the symptom is pain) whether the patient’s pain Radiates to another location or is well-localized • The Severity of the symptoms and any other associated Symptoms • The Time course of the symptoms (how they have changed over time and whether the patient has experienced them before) Additionally, include any other details here that may support your final diagnosis or rule out alternative diagnoses. For example, if you are concerned about a pulmonary embolism and your patient recently completed a long-distance flight, that would be worth mentioning.
The review of systems is sometimes included in the history of present illness, but it may also be separated. Given the potential breadth of the review of systems (a comprehensive list of questions that may be asked can be found here ), when presenting, only report information that is relevant to your patient’s condition.
The past medical history comes next. This should include the following information: • The patient’s medical conditions, including any that were not highlighted in the opener • Any past surgeries the patient has had and when they were performed • The timing of and reasons for past hospitalizations • Any current medications, including dosages and frequency of administration
The next section should detail the patient’s relevant family history. This should include: • Any relevant conditions that run in the patient’s family, with an emphasis on first-degree relatives
After the family history comes the social history. This section should include information about the patient’s: • Living situation • Occupation • Alcohol and tobacco use • Other substance use You may also include relevant details about the patient’s education level, recent travel history, history of animal and occupational exposures, and religious beliefs. For example, it would be worth mentioning that your anemic patient is a Jehovah’s Witness to guide medical decisions regarding blood transfusions.
Once you have finished reporting the patient’s history, you should transition to the physical exam. You should begin by reporting the patient’s vital signs, which includes the patient’s: • Temperature • Heart rate • Blood pressure • Respiratory rate • Oxygen saturation (if the patient is using supplemental oxygen, this should also be reported) Next, you should discuss the findings of your physical exam. At the minimum, this should include: • Your general impressions of the patient, including whether he or she appears “sick” or not • The results of your: • Head and neck exam • Eye exam • Respiratory exam • Cardiac exam • Abdominal exam • Extremity exam • Neurological exam Additional relevant physical examination findings may be included, as well. Quick note: resist the urge to report an exam as being “normal.” Instead, report your findings. For example, for a normal abdominal exam, you could report that “the patient’s abdomen is soft, non-tender, and non-distended, with normoactive bowel sounds.”
This section includes the results of any relevant laboratory testing, imaging, or other diagnostics that were obtained. You do not have to report the results of every test that was ordered. Before presenting, consider which results will further support your proposed diagnosis and exclude alternatives.
The emergency department (ED) course is classically reported towards the end of the presentation. However, different attendings may prefer to hear the ED course earlier, usually following the history of present illness. When unsure, report the ED course after the results of diagnostic testing. Be sure to include initial ED vital signs and any administered treatments.
You should conclude your presentation with the assessment and plan. This is the most important part of your presentation and allows you to show your team how much you really know. You should include: • A brief summary (1-2 lines) of the patient, the reason for admission, and your likely diagnosis. This should also include information regarding the patient’s clinical stability. While it can be similar to your opener, it should not be identical. An example could be: “Ms. X is a 78-year-old female with a past medical history of chronic obstructive pulmonary disease who presents with shortness of breath in the setting of an upper respiratory tract infection who is now stable on two liters of supplemental oxygen delivered via nasal cannula. Her symptoms are thought to be secondary to an acute exacerbation of chronic obstructive pulmonary disease.” • A differential diagnosis . For students, this should consist of 3-5 potential diagnoses. You should explain why you think each diagnosis is or is not the final diagnosis. Be sure to rule out potentially life-threatening conditions (unless you think your patient has one). For our fictional patient, Ms. X, for example, you could explain why you think she does not have a pulmonary embolism or acute coronary syndrome. For more advanced trainees, the differential can be more limited in scope. • Your plan . On regular inpatient floors, this should include a list of the patient’s medical problems, ordered by acuity, followed by your proposed plan for each. After going through each active medical problem, be sure to mention your choice for the patient’s diet and deep vein thrombosis prophylaxis, the patient’s stated code status, and the patient’s disposition (whether you think they need to remain in the hospital). In intensive care units, you can organize the patient’s medical problems by organ system to ensure that no stone is left unturned (if there are no active issues for an organ system, you may say so).
Presenting Patients Who Have Been in the Hospital for Multiple Days
After the initial presentation, subsequent presentations can be delivered via SOAP note format as follows:
- The Subjective section includes details about any significant overnight events and any new complaints the patient has.
- In the Objective section, report your physical exam (focus on any changes since you last examined the patient) and any significant new laboratory, imaging, or other diagnostic results.
- The Assessment and Plan are typically delivered as above. For the initial patient complaint, you do not have to restate your differential diagnosis if the diagnosis is known. For new complaints, however, you should create another differential and argue for or against each diagnosis. Be sure to update your plan every day.
Presenting Patients in Different Specialties
Before you present a patient, consider your audience. Every specialty presents patients differently. In general, surgical and OB/GYN presentations tend to be much quicker (2-3 minutes), while pediatric and family medicine presentations tend to be similar in length to internal medicine presentations. Tailor your presentations accordingly.
Presenting Patients in Outpatient Settings
Outpatients may be presented similarly to inpatients. Your presentation’s focus, however, should align with your outpatient clinic’s specialty. For example, if you are working at a cardiology clinic, your presentation should be focused on your patient’s cardiac complaints.
If your patient is returning for a follow-up visit and does not have a stated chief complaint, you should say so. You may replace the history of present illness with any relevant interval history since his or her last visit.
And that’s it! Delivering oral case presentations is challenging at first, so remember to practice. In time, you will become proficient in this essential medical skill. Good luck!
Kunal Sindhu, MD, is an assistant professor in the Department of Radiation Oncology at the Icahn School of Medicine at Mount Sinai and New York Proton Center. Dr. Sindhu specializes in treating cancers of the head, neck, and central nervous system.
2 thoughts on “How To Present a Patient: A Step-To-Step Guide”
To clarify, it should take 5-10 minutes to present (just one) new internal medicine inpatient? Or if the student had 4 patients to work up, it should take 10 minutes to present all 4 patients to the preceptor?
Good question. That’s per case, but with time you’ll become faster.
Comments are closed.

How to Give an Excellent Medical Presentation
- By Sulaiman Ahmad
- July 22, 2019
- Medical Student , Pre-med
- Self-improvement
In medicine, we are constantly learning from each other. Professors stand in front of lecture halls to teach the fundamental knowledge needed to pass board exams and to treat our patients. Outside of the classroom, medical students, researchers, and physicians attend conferences to communicate ideas and update their colleagues with oral and poster presentations. In the clinic, students and resident physicians relay pertinent patient information to the physician in charge. Eventually, you will find yourself in front of an audience listening to your talk or an attending grading your clinical presentation. First, I will discuss what it takes to make an excellent presentation. I will then finish this topic by providing guidelines for perfecting different types of presentations.
Critical Elements of an Excellent Presentation
do some research.
Your audience will consider you an expert on the information you deliver. It is your job to achieve the expected level of comprehension of the topic. After choosing a topic, gather enough background information from diverse but appropriate sources (e.g., journals articles, relevant chapters in textbooks, personal discussion with subject matter experts, online videos). Your research should provide you with a thorough understanding of the topic and a list of the important facts supporting your take-home message . Any gaps in your knowledge will become evident during your presentation. The goal is to develop confidence in your understanding of the topic and ability to share what you know.
Know Your Audience
Before putting your presentation together, take a moment to assess the baseline understanding of your expected audience . Ultimately your audience should walk away having learned something new. Try to figure out their collective interest, reasons for attending, and prior experience with the topic. Knowing your audience will allow you to focus on information that will keep them engaged and interested. For example, premed students have a different understanding of medical topics than medical students. A presentation on the same subject should be different for both groups. If your listeners have different levels of expertise, take a moment to explain the fundamental concept, then build up the language and complexity to allow everyone to benefit from the information shared. Your audience is the reason why you are presenting.
Tell a Story
The human brain is wired to remember stories , especially if presented logically. A presentation is about the information shared, but it should also include the presenters’ passion, excitement, and personal style. All topics can be formatted to include characters, a description of the setting, plot, conflict, and a resolution. The story should allow the audience to take a journey with you. The hardest part is identifying the start and endpoint of your story and which details are needed. Make every word count by checking if it adds value to your narrative. Consider using metaphors, real examples, and descriptions that give life to your words .
Practicing your presentation is a vital step in developing an excellent presentation. You can memorize a script. However, memorization can reduce your connection with the audience. But in certain situations, scripts are quick and effective means of communicating important facts. Another approach is drafting bullet points of the main ideas and practicing the natural flow of information . This method allows your personality to shine on stage. To become comfortable speaking, start by practicing on your own . You can also record yourself with a cellphone or tablet and review the recording to evaluate your performance. Next, find a small group to present in front of and ask for their honest assessment . Eventually, your presentation will feel natural, and your stage presence will aid in communicating your main idea.
Q&A Session
Usually, your presentation does not end until after a question and answer session. Most presentations should include approximately five minutes in the end for the audience to ask questions . This part of the presentation allows you to clarify or further explain any part of your presentation. A question can also lead to expanding your presentation beyond what you originally planned to discuss . It is important for you to understand what is being asked and address the specific question directly. And if you do not have an answer, it is okay to admit that you do not know . Questions will force you to be creative and truly test your knowledge of the topic.
Different Types of Presentations
Presentations have many different forms, each with different goals; thus, each form requires a unique approach. In medicine, professors and clinician often provide students with lecture objectives and PowerPoint presentations that guide the students in their hour-long lecture. Conferences are a researcher’s platform to share their lab’s progress and conclusions. The last presentation I will go into is the clinical presentation a student typically performs for the physician in charge.
The main purpose of the lecture is to educate the attendees. We all have had great professors captivate our attention and other experiences that were a complete waste of time. But what makes some lectures better than others? The lecturer’s knowledge on the topic becomes obvious, and their stage presence confirms how comfortable they are with the topic. If you are tasked with lecturing on a topic or a series, ensure that you have a solid understanding and address your learning objectives in the time allotted . The main concepts should be repeated multiple times throughout the lecture, followed by examples . Your PowerPoint slides should be limited to only main points and images that support your talking points. After difficult concepts are covered, ask questions to gauge your audience’s understanding . It is better to reemphasize a concept before building up to more complex learning objectives.
Research Presentation
Attending a conference is exciting, especially if you are representing your lab with an oral presentation. It is an opportunity to share your research story, from the point of identifying a question to the process of reaching a conclusion. Realize your audience will include Primary Investigators, post-docs, and Ph.D. students that are also experts in the field . Attempt to grab the audience’s attention from the beginning by providing them with a reason to care. Then continue to explain how your study relates to the published work . After building up the background, address how you arrived at your research question. The most exciting part of your presentation should be explaining your conclusions and the path you took to get there. Finish up strong by discussing the implications of your findings and how they will have an impact in the field . The natural flow of information will come with practice and a deep understanding of your research topic. Presenting as a student usually leads to networking with professors and clinicians that can help you progress in your career.
Patient Presentation
Medical students learn how to take a patient’s history and perform a physical exam, but it is more challenging to reason through your clinical findings and subsequently present to an attending . Your clinical presentation style will change depending on the environment, medical department, and supervising physician . Upon joining a medical team, discuss the expectations and preference with each physician . It may be a good idea to draft a script that can get you started on organizing your patient presentation. The success of your presentation is correlated to your knowledge of the basic sciences and ability to critically assess the patient’s history and physical exam; the more you learn and read, the easier decision making and producing a plan becomes. Another important element is practicing your presentation style until it comes out naturally . Take the time to listen to your peers and experienced colleagues; learn from their mistakes and strengths . After concluding your presentation, ask for feedback and practice implementing the suggestions. You will be the eyes and ears for the physicians in charge, perfecting your patient presentation will help get the care the patients need while making everyone’s job a little easier.
Final remarks
There are some basic steps to achieving an excellent presentation: know the topic well, understand who you’re presenting to, develop a memorable story, and practice until it comes out naturally. A career in medicine is very versatile; you can be at the forefront of the next generation of physicians sharing your experiences or updating the science community with your research conclusions. At the minimum, you will be presenting the patient in the clinic. Thus, presenting is a skill every physician must master.
Sulaiman Ahmad

How to Improve Your Public Speaking as a Student
If public speaking scares you, you are far from alone. We break down 6 strategies for improving your public speaking.

Anatomy of a Successful Medical Student — 5 Critical Traits
Those who thrive in med school—landing in top residency programs without costing their wellbeing—are different from the pack. This is how they do it.

6 Lifestyle Factors That Are Killing Your Focus
Successful students take a holistic approach to their studying and lifestyle. Here are 6 simple tactics that will help you develop laser focus.
Leave a Reply Cancel reply

Join the Insider Newsletter
Receive regular exclusive MSI content, news, and updates! No spam. One-click unsubscribe.
Customer Note Premed Preclinical Med Student Clinical Med Student
You have Successfully Subscribed!
Presentation Skills Toolkit for Medical Students
New section.
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic meetings and conferences. In this toolkit, you’ll find helpful resources on developing and delivering formal lectures and presentations, poster and oral abstract presentations, patient presentations, and leading small group sessions.
Please note: Availability of resources may change over time. To suggest edits or updates, email [email protected] .
On this page:
Formal lectures and presentations, posters and abstracts, patient presentations.
- Leading Small Groups
Traditional academic presentations in medicine and the biomedical sciences are necessarily dense with complex content. Thus, slides tend to be wordy, and presenters may use their slides as cue cards for themselves rather than as tools to facilitate learning for their audience. With the necessary resources, medical students (and presenters at all levels) can better identify appropriate learning objectives and develop presentations that help learners meet those objectives. Organization of content, clarity of slide design, and professional delivery are all essential components to designing and giving effective formal presentations.
Achieving all of these elements can make creating and delivering a formal presentation challenging. The strategies and resources below can help you develop a successful formal presentation.

View long description of infographic .
Strategies for success
- Define the objectives of the presentation. Always define learning objectives for each of your lectures to make it clear what knowledge or skills the audience should acquire from your presentation. The best learning objectives define specific, measurable, or observable knowledge or skill gains. Furthermore, consider how to communicate the importance of the topic to your audience and how information should be arranged to best communicate your key points.
- Design an effective slide set. You should begin creating your slides only after defining your objectives and key points. The slides should support your talk but not be your talk. Keep slides simple. The audience should be able to review a slide and grasp key points quickly. Avoid lengthy text and distracting decorative fonts, clip art, graphs, and pictures. If additional wording or images are necessary, consider handouts or alternative methods of sharing this information. Lastly, design your slide deck to emphasize the key points, revisiting your outline as necessary, and summarize concepts at regular intervals throughout your presentation to strengthen knowledge gains.
- Practice your performance. Effective public speaking starts with preparation and practice. Ensure there is enough time to create your lecture and a supporting slide deck. Know your lecture material and slides without prompts! Understand the audience and learning climate (the size and knowledge level of your audience) and be prepared for the venue (virtual, in-person, or both, lecture hall or classroom). Think about what effective audience engagement may look like and how to incorporate audience response systems, polling, etc., into the lecture.
- Create a positive learning environment. Anticipate questions and allocate sufficient time to answer them. Always repeat the questions being asked for the audience’s benefit and to ensure your understanding. Some questions may be challenging, so be prepared and answer honestly. It is acceptable not to know an answer.
- Demonstrate professionalism in presenting. Exhibit professionalism by being punctual and having appropriate time management. Remember that mistakes happen; be kind to yourself and remain calm and collected. Be enthusiastic: If you can enjoy the experience, so will your audience. Finally, be open to feedback following your presentation.
Additional resources
Below is a collection of resources that further address the elements of creating and delivering a formal presentation. Each resource addresses a specific presentation skill or set of skills listed above and can be used to develop your understanding further.
- Healthy Presentations: How to Craft Exceptional Lectures in Medicine, the Health Professions, and the Biomedical Sciences (requires purchase, book). This illustrated book is a practical guide for improving scientific presentations. It includes specific, practical guidance on crafting a talk, tips on incorporating interactive elements to facilitate active learning, and before-and-after examples of improved slide design. (Skills addressed: 1-3)
- American College of Physicians: Giving the Podium Presentation (freely available, website). This guide includes recommendations related to presentation delivery, including tips on what to wear, how to prepare, answering questions, and anticipating the unexpected. (Skills addressed: 3-5)
- The 4 Ps of Giving a Good Presentation (freely available, PDF). This simple guide on public speaking from the University of Hull covers such topics as positive thinking, preparing, practice, and performing. (Skills addressed: 3-5)
- Zoom Guides (freely available, website). This website from the University of California, San Francisco is one of many great resources created by universities for presenting on a virtual platform, specifically Zoom. (Skills addressed: 3-5)
- Writing Learning Objectives (freely available, PDF). This excellent resource from the AAMC defines Bloom’s Taxonomy and provides verbiage for creating learning objectives. (Skill addressed: 1)
- Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83 (freely available, article). This AMEE Guide explains and explores the more commonly used adult learning theories and how they can be used to enhance learning. It presents a model that combines many of the theories into a flow diagram that can be followed by those planning a presentation. (Skill addressed: 1)
- Assertion-Evidence Approach (freely available, website). This approach to slide design incorporates clear messaging and the strategic combination of text and images. (Skill addressed: 2)
- Multimedia Learning (requires purchase, book). This book outlines the learning theories that should guide all good slide design. It is an accessible resource that will help presenters of all levels create slide decks that best facilitate learning. (Skill addressed: 2)
- Collaborative Learning and Integrated Mentoring in the Biosciences (CLIMB) (freely available, website). This website from Northwestern University shares slide design tips for scientific presentations. Specific tips include simplifying messages and annotating images and tables to facilitate learning. (Skill addressed: 2)
- Clear and to the Point (freely available, online book). This book describes 8 psychological principles for constructing compelling PowerPoint presentations. (Skill addressed: 2)
Return to top ↑
Presenting the results of the research projects, innovations, and other work you have invested in at regional and national meetings is a tremendous opportunity to advance heath care, gain exposure to thought leaders in your field, and put your evidence-based medicine and communication skills into practice in a different arena. Effective scientific presentations at meetings also provide a chance for you to interact with an engaged audience, receive valuable feedback, be exposed to others’ projects, and expand your professional network. Preparation and practice are integral to getting the most out of these experiences.
The strategies and resources below will help you successfully present both posters and abstracts at scientific meetings.
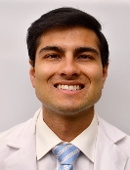
Strategies for success
- Identify a poster’s/abstract’s purpose and key points . Determine the purpose of sharing your work (feedback vs. sharing a new methodology vs. disseminating a novel finding) and tailor the information in your poster or abstract to meet that objective. Identify one to three key points. Keep in mind the knowledge and expertise of the intended audience; the amount of detail that you need to provide at a general vs. specialized meeting may vary.
- Design an effective poster . Design your poster to follow a logical flow and keep it uncluttered. The methods and data should support your conclusions without extraneous information; every chart or image should serve a purpose. Explicitly outline the key takeaways at the beginning or end.
- Present in a conversational, informal style . Imagine you are explaining your project to a colleague. The purpose of your work and key points should guide your presentation, and your explanation of the methods and data should link to your conclusions. Be prepared to discuss the limitations of your project, outline directions for future research, and receive feedback from your audience. Treat feedback as an opportunity to improve your project prior to producing a manuscript.
Additional resources
These resources support the development of the skills mentioned above, guiding you through the steps of developing a poster that frames your research in a clear and concise manner. The videos provide examples that can serve as models of effective poster and abstract presentations.
- How to design an outstanding poster (freely available, article). This article outlines key items for laying out an effective poster, structuring it with the audience in mind, practicing your presentation, and maximizing your work’s impact at meetings. (Skills addressed: 1-3)
- Giving an Effective Poster Presentation (freely available, video). This video shows medical students in action presenting their work and shares strategies for presenting your poster in a conversational style, preparing for questions, and engaging viewers. (Skills addressed: 2,3)
- Better Scientific Poster (freely available, toolkit). This toolkit includes strategies and templates for creating an effective and visually interesting scientific poster. Virtual and social media templates are also available. (Skill addressed: 2)
As with all presentations, it can be very helpful to practice with colleagues and/or mentors before the meeting. This will allow you to get feedback on your project, style, and poster design prior to sharing it with others outside of your institution. It can also help you prepare for the questions you may get from the audience.
Patient presentation skills are valuable for medical students in the classroom and in the care of patients during clinical rotations. Patient presentations are an integral part of medical training because they combine communication skills with knowledge of disease manifestations and therapeutic strategies in a clinical scenario. They are used during active learning in both the preclinical and clinical phases of education and as students advance in training and interact with diverse patients.
Below are strategies for delivering effective patient presentations.

- Structure the presentation appropriately . The structure of your narrative is important; a concise, logical presentation of the relevant information will create the most impact. In the clinical setting, preferences for presentation length and style can vary between specialties and attendings, so understanding expectations is vital.
- Synthesize information from the patient encounter . Synthesis of information is integral for effective and accurate delivery that highlights relevant points. Being able to select pertinent information and present it in an efficient manner takes organization and practice, but it is a skill that can be learned.
- Deliver an accurate, engaging, and fluent oral presentation . In delivering a patient presentation, time is of the essence. The overall format for the presentation is like a written note but usually more concise. Succinctly convey the most essential patient information in a way that tells the patient’s story. Engage your listeners by delivering your presentation in an organized, clear, and professional manner with good eye contact. Presentations will go more smoothly with careful crafting and practice.
- Adjust presentations to meet team, patient, and setting needs . Adaptability is often required in the clinical setting depending on attending preferences, patient needs, and location, making it imperative that you are mindful of your audience.
The resources below provide samples of different types of patient presentations and practical guides for structuring and delivering them. They include tips and tricks for framing a case discussion to deliver a compelling story. Resources that help with adjusting patient presentations based on the setting, such as bedside and outpatient presentations, are also included.
- A Guide to Case Presentations (freely available, document). This practical guide from the Ohio State University discusses basic principles of presentations, differences between written and oral communication of patient information, organization, and common pitfalls to avoid. (Skills addressed: 1-3)
- Verbal Case Presentations: A Practical Guide for Medical Students (freely available, PDFs). This resource from the Augusta University/University of Georgia Medical Partnership provides a practical guide to crafting effective case presentations with an explanation of the goals of each section and additional tips for framing the oral discussion. It also provides a full sample initial history and physical examination presentation. (Skills addressed: 1-4)
- Patient Presentations in Emergency Medicine (freely available, video). This training video for medical students from the Society for Academic Emergency Medicine demonstrates how to tell a compelling story when presenting a patient’s case. The brief video offers handy dos and don'ts that will help medical students understand how best to communicate in the emergency department efficiently and effectively. These skills can also be applied to patient presentations in other specialties. (Skills addressed: 1-4)
Additional information and support on effectively constructing and delivering a case presentation can be found through various affinity support and mentorship groups, such as the Student National Medical Association (SNMA), Latino Medical Student Association (LMSA), and Building the Next Generation of Academic Physicians (BNGAP).
Leading Small Groups
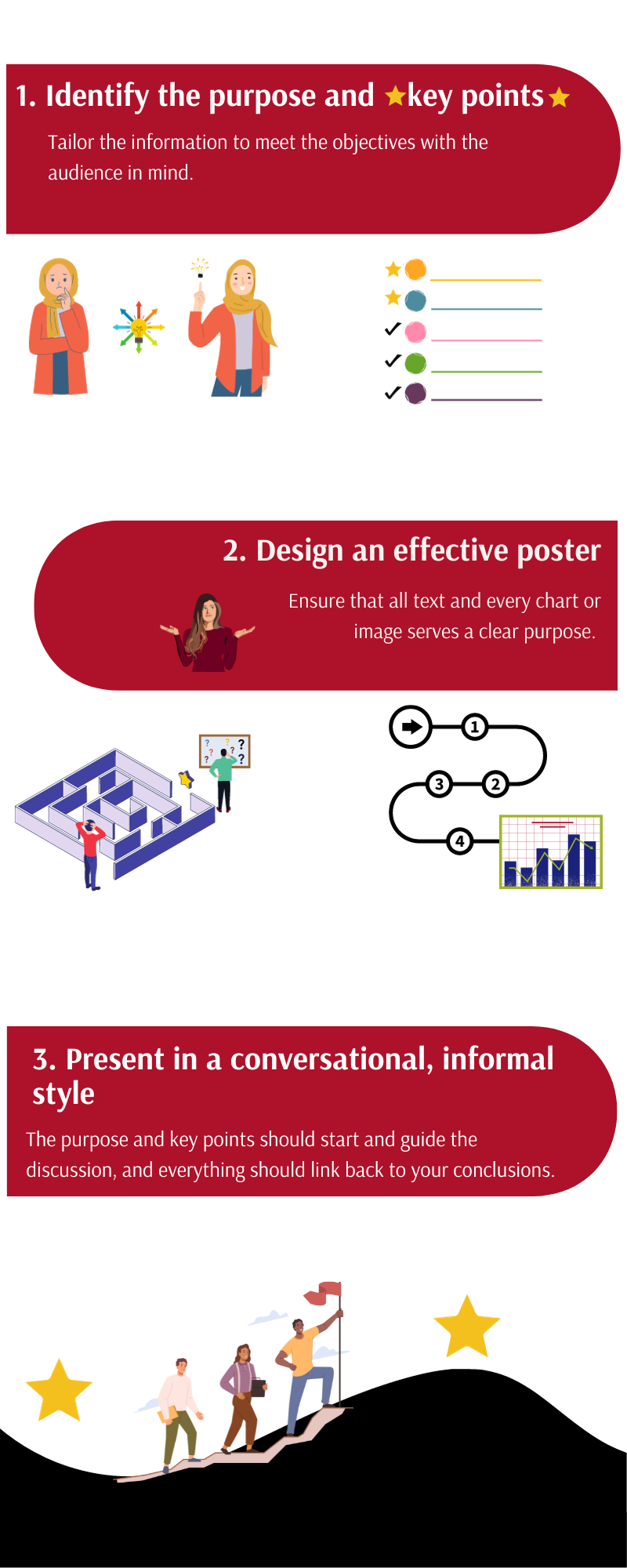
For physicians, working within and leading small groups is an everyday practice. Undergraduate medical education often includes small group communication as well, in the form of problem-based learning groups, journal clubs, and study groups. Having the skills to form, maintain, and help small groups thrive is an important tool for medical students.
Below are strategies to provide effective small group leadership.
- Outline goals/outcomes . Delineating the goals of a meeting ensures that everyone understands the outcome of the gathering and can help keep conversations on track. Listing goals in the agenda will help all participants understand what is to be accomplished.
- Establish ground rules . Establishing explicit procedural and behavioral expectations serves to solidify the framework in which the conversation will take place. These include items such as attendance and how people are recognized as well as the way group members should treat each other.
- Create an inclusive environment . In addition to setting expectations, group leaders can take steps to help all participants feel that their perspectives are valuable. Setting up the room so that everyone sits around a table can facilitate conversations. Having individuals introduce themselves can let the group understand everyone’s background and expertise. In addition, running discussions in a “round-robin style” (when possible) may help every person have an opportunity to express themselves.
- Keep discussions constructive, positive, and on task . As meetings evolve, it can be easy for conversations to drift. Reminding the group of goals and frequently summarizing the discussion in the context of the planned outcomes can help redirect meetings when needed.
- Manage virtual meetings . Online meetings present their own challenges. Adequate preparation is key, particularly working through technological considerations in advance. Explicitly discussing goals and ground rules is even more important in the virtual environment. Group leaders should be more patient with members’ response times and be especially diligent that all participants have an opportunity to be heard.
The resources listed below outline additional helpful points, expanding on the skills described above and providing additional perspectives on managing small group meetings of different types.
- Communication in the Real World: Small Group Communication (freely available, online module). This chapter includes an overview of managing small groups, including understanding the types and characteristics, group development, and interpersonal dynamics. (Skills addressed: 3,4)
- Conversational Leadership (freely available, online book chapter). This short online resource provides guidance for determining group size and seating to best facilitate participation by all group members. (Skill addressed: 4)
- Tips on Facilitating Effective Group Discussion (freely available, PDF). This resource from Brown University provides tips for effective group facilitation, creating an environment conducive for discussions, keeping conversations positive, and managing common problems. Also included is a valuable list of references for further exploration. (Skills addressed: 1-4)
- Facilitating Effective Discussions: Self-Checklist (freely available, online checklist). This checklist from Brown University provides an easy-to-use, practical framework for preparing for, performing, and reflecting on small group facilitation. (Skills addressed: 1-4)
- Sample Guidelines for Classroom Discussion Agreements (freely available, PDF). These guidelines from Brown University give useful tips for managing classroom discussions, including when disagreements occur among group participants. (Skill addressed: 2)
- Fostering and assessing equitable classroom participation (freely available, online article). This online resource from Brown University includes methods to maximize group members’ participation in discussions and to communicate expectations. Also included is a valuable list of references for further exploration. (Skill addressed: 3)
- Facilitating small group learning in the health professions (freely available, online article). The aim of this paper published in BMC Medical Education is to provide students involved in peer/near peer teaching with an overview of practical approaches and tips to improve learner engagement when facilitating small groups. It includes a discussion of the roles of facilitators, strategies for fostering interactions among the group, and methods for resolving common problems. (Skills addressed: 1-4)
- Facilitating a Virtual Meeting (freely available, PDF). This infographic from the University of Nebraska Medical Center includes key points to consider when facilitating an online meeting, including technical considerations, preparation, and follow-up. (Skill addressed: 5)
- Most universities have a communication department with faculty who specialize in small group communication. You may also find that these individuals are a valuable resource.
This toolkit was created by a working group of the Undergraduate Medical Education (UME) Section of the Group on Educational Affairs (GEA).
Working Group Members
- Geoffrey Talmon, MD, University of Nebraska Medical Center
- Jason Kemnitz, EdD, University of South Dakota Sanford School of Medicine
- Lisa Coplit, MD, Frank H. Netter School of Medicine at Quinnipiac University
- Rikki Ovitsh, MD, SUNY Downstate College of Medicine
- Susan Nofziger, MD, Northeast Ohio Medical University
- Amy Moore, MEd, Cleveland Clinic Lerner College of Medicine
- Melissa Cellini, MD, New York Medical College
- Richard Haspel, MD, Harvard Medical School
- Christine Phillips, MD, Boston University School of Medicine
- Arvind Suresh, Geisel School of Medicine at Dartmouth
- Emily Green, PhD, MA, Warren Alpert Medical School of Brown University
- Holly Meyer, PhD, MS, Uniformed Services University of the Health Sciences
- Karina Clemmons, EdD, University of Arkansas for Medical Sciences
- Shane Puckett, EdD, University of South Florida
- Angela Hairrell, PhD, Burnett School of Medicine at Texas Christian University
- Arkene Levy Johnston, PhD, Kiran C. Patel College of Allopathic Medicine
- Sarah Collins, PhD, UT Southwestern Medical Center
- Patrick Fadden, MD, Virginia Commonwealth University School of Medicine
- Lia Bruner, MD, Augusta University - University of Georgia Medical Partnership
- Jasna Vuk, MD, PhD, University of Arkansas for Medical Sciences
- Pearl Sutter, University of Connecticut School of Medicine
- Kelly Park, Baylor University Medical Center
Presentation Skills for Clinicians: Making Your Next Presentation Go Better than Your Last

WHY IS PRESENTING IMPORTANT FOR HEALTHCARE PROFESSIONALS?
Why is it crucial for you to present yourself and your material well? Well, the point is our careers depend heavily on the way we present ourselves and our material. If you do this well, doors swing open. If you don't, they usually find somebody else. So, this could be a career-maker or a career breaker.
Now, how did I get involved in this? Well, a number of years ago, I was elected to be our speaker at high school graduation. And it didn't go very well. And I couldn't quite figure out why. I thought it must have been the microphone or whatever. But I went off to college, Rice University. While at Rice University, I listened to one of the greatest speakers I've ever heard, and that was Muhammad Ali, who spoke in front of the campus and commanded the audience. He almost didn't graduate high school. I figured if he could do this well, I could get better.
I read books, I took courses, and it's from what I learned the hard way, I want to share with you some of the tips and tools that we've learned. One of the things that we have done is a workshop where we videotape learner colleagues, and we go together and group critique what goes well and what could be improved. And I've been doing this for about 20 years now.
So, let's go through some of the important lessons. The goal today is I want your buy-in that this is important and teach you a few things. But I really want to motivate you to think about put in your presentations together a little differently than you've done in the past. And I'll try to demonstrate some of these skills as best I can to you today.
16 TIPS AND TOOLS FOR GIVING A BETTER PRESENTATION
- BODY LANGUAGE
Body language is very important. You've probably seen TED talks in the past. Ted speakers speak with what we call open body language . What does that mean? It means nothing between you and your audience so they don't stand behind lecterns and hold on to the lectern. They don't have their hands clasped or arms folded. They're out in front, full-body hand gestures going, and it creates a real impression with the audience, and it makes everything go better.
- ALWAYS INCLUDE YOUR EMAIL IN THE PRESENTATION
So, a couple of basics. If you're speaking formally, always include an email address on a slide, on a whiteboard, or on a handout. You might ask, what does this tell your audience? It says you're approachable. If they have questions or want to contact you, they can.
Now, one of the questions I often get from people is, “Oh, won't you get a lot of spam doing that?” I get spam, but it's never, never abused in a professional audience. I might get an invitation to speak in Hawaii. I might get a referral, I might get some constructive critiquing. But rarely do you get anything. It just makes you look good.
- WRITE YOUR OWN INTRODUCTION
Again, if it's a formal presentation, write your own introduction. In the Bible, it might say the meek shall inherit the earth. Not when you're wanting to write your own introduction, you need to give yourself credibility on the topic to which you are speaking. And this is important – only you know the credibility you have. And if you send a 40-page curriculum vitae to somebody, nobody reads it, and they might pull out things that you don't feel are important.
- THE NAME BADGE
And then what have I learned about the name badge? Well, first of all, when you are presenting formally, lose the badge because if you have a badge on your body, it looks stupid, it flops around, and anything on your person that is distracting will detract from your presentation.
But if you are going to use the badge, put it on the upper right of your lapel. Why? Because when we meet and greet and shake hands, or bump fists, or hit elbows, it's on the upper right side and people can glance and see your name without looking over your torso embarrassingly to try to remember what your name was.
- POWERPOINT – WHAT NOT TO DO
In medical presentations, lots of PowerPoints are still used, and it can be your friend, but it can often be your enemy. A college professor surveyed a thousand students and asked, “What do you all find most annoying sitting through PowerPoint presentations?” And they could answer more than once, but let me just share a few of the things they found most annoying,
No. 1 was the speaker reading verbatim, word by word, your slides. Next, having tiny point type in the slides. Well, if you have 17 lines on a slide, you have to have tiny lettering to be seen. So, if you've heard of the rule of five or six, that's something to think about – no more than five or six lines per slide and no more than five or six words per slide. And watch out for hard-to-see colors, flying techs, and complex charts.
Let's get to the meat of this talk and talk about how you best connect with an audience and the number one tip, know who's in your audience and meet their needs.
- KNOW WHO'S YOUR AUDIENCE AND WHAT THEY WANT & NEED
What do they want to know? What do they need to know? Not, what do you want to talk about? If you can do that, your evaluations will go sky-high. And that's hard for some people to connect with. But it also takes a lot of baggage off of your shoulders. You don't have to talk about everything about a topic, you don't have to cover from front end to back end. You just have to think about what's this audience wants to know or needs to know.
And you will meet their needs because they are tuned in to an FM radio station whenever you and I speak called WIIFM – What's in it for me? If you answer that question early, you've hooked them. They want to hear more. We'll talk a little about hooks further on.
- ORGANIZATION AND HOOKS
The other important point is the organization of your presentation. An audience will give us somewhere between 5 and 30 seconds before they make a judgment of us and our material, and if you don't hook them, out come the iPhones and they’re reading their email. So, in that opening statement, you need to hook the audience. You can do that with a story, medical stories are cases, or the word imagine. And I'll give you an example.
So, let's say that you're the chief resident is giving a discussion with the residents about diarrhea. And he starts out by saying, “Good morning. Today, we're going to speak about diarrhea. Diarrhea was first described by Dr. Dye and Dr. Rhea in 1898,” and in the audience is going, “Oh, lord, get me out of this. Now, this is going to be terrible.”
But what if the same chief resident started with something like this? “Good morning. You pick up the chart of your first patient. She's a 39-year-old woman who's complaining of three weeks of watery diarrhea. Your heart sinks. You think, ‘What do I need to ask historically? Is there anything on the exam I need to pay attention to? What about testing? Do I need to do testing or order stool studies, or could I empirically treat her and see if she gets better?’ Great questions we’ll answer all these in this presentation. So if she's your first patient, you'll be ready.”
That's a hook, starting with a case. Now, they feel they need to know or want to know more about diarrhea, when before, they weren't interested in a bunch of facts.
- LESS INFORMATION IS MORE
Speaking of facts, it has been shown that after a typical gland rounds presentation, when the learners walk out of the room, and they're asked to recite any facts they recall from the presentation, the average number is zero to three. Zero to three! Why in the world would we give presentations if they don't remember everything we say?
Unfortunately, if your goal is 25 facts in 25 minutes, you'll fail every time, but you can do a lot with a presentation. You can get the learners interested in your topic, so they learn more and want to read more about it. You can get funding for your research. You can get a promotion. You can change somebody's career. You can teach a procedure. But if your goal is 25 facts in 25 minutes, you'll fail every time.
- STRONG FINISH
“Oh, we're done today,” is not a strong closing, nor is a picture of your family, the new baby, or a sunset. If people are going to remember anything out of your presentation. It's usually the last five percent. So I like to teach, say, these two words: In Summary . People awaken. If they've got a pencil, they'll start writing down whatever you say next. If you say, “And if you only remember three things from today,” that's probably what they'll remember.
- GOOD DELIVERY AND SPEEDood Delivery and Speech
Concentrate on the delivery – face your audience, not your screen or your slides. Avoid monotone. You don't know what you sound like unless you've listened to your presentation, and your voice.
Pace is important too. Many speakers talk very fast because after all, they only gave me 15 minutes to go through all this material, and I've got about 40 minutes of material but if I talk really fast, I can get through most of it. And I don't know about you, but I get a little nervous in front of an audience, so the faster I speak, the quicker I sit down.
What's the trouble at that pace? It’s hard to listen and hard to understand, so you lose a sentence or two, and again, out come the iPhones and your into your email.
And the most important speech technique you can master is pausing. To a speaker to pause seems eternal – to the audience, it's a short break. And for those of us that have filler, sounds like, “um, ah, so, uh, you know, etc.” knowing that you make those sounds and learning to replace them with a pause instead is the key here.
- MAKE YOUR PRESENTATION A PERFORMANCE
Now, this is a hard thing sometimes for medical presenters, but you need to make your presentation a performance. Now, when I say performance, you don't have to tell jokes or sing and dance, but you have to connect with your audience. And the easiest way to connect right off the bat is to remember to smile. The audience wants you to succeed. They want you to feel that they can approach you after the presentation, ask you a question.
Yet many of us are actually kind of frowning and looking off-putting because we're trying to think about that 23rd fact that nobody cares about anyway. If you cannot show enthusiasm for your own topic, how is your audience going to care?
- HAND GESTURES
Hand gestures are important. We talked about open postures, so they're not together and grabbing, but along with open posture, you can have purposeful gestures. Do you know they're making pacemakers now at the size of a postage stamp? They can be tucked right under the clavicle. Can't even be seen anymore. Stories are better than facts, but a fact tied to a story will be remembered. And in medicine, our stories are wonderful. We have patient cases stories. We have lots of cases, and we can illustrate a teaching point that will probably be remembered because it's part of a story.
- YOU WON'T LOOK NERVOUS, EVEN IF YOU FEEL NERVOUS
One of the biggest fears of people is public speaking, and I've heard from so many learners that they feel petrified and nervous if they have to speak in front of a large group. In fact, tongue in cheek, I heard once from a friend that there was an article published that showed, at a funeral, 80 percent of the congregation would feel more comfortable in the casket than delivering the eulogy. But public speaking can be a little frightening.
The beauty is most anxiety doesn't show. In our videotaped workshops, we always videotape colleagues and then we ask them, were you nervous during this? “Oh, yes, very nervous.” Then we ask the group of other learners, “Did he or she look nervous?” “Absolutely not.” Most audiences will rate the speaker looking cool and calm, even though the speaker feels uncomfortable. The biggest fear of the speaker is looking nervous, biggest fear of the audience is being bored.
- DRINK WATER
Sometimes, your voice can get a little dry. I think the parasympathetic can kick in. So, it's OK to have a little water to sip on while you're speaking. You probably don't want to slam down a big drink of diet cola before you speak. Not just the caffeine, but the bubbles could come up at the wrong time and embarrass you. So sipping on a little water is fine.
- MAKE EYE CONTACT WITH AT LEAST ONE PERSON
Eye contact. If you're starting out, and you're a little nervous, make eye contact with somebody who is nodding and affirming, and that gives you a little more confidence. And then you can move around the room and make eye contact with others.
I'm asking a lot about humor. If humor is part of your personality, like you can probably tell it's part of mine, it's OK to use it, but don't feel forced. And if you use humor, the safest humor to use is self-deprecating humor. I spoke poorly at my high school graduation. I'm sharing with you what I learned the hard way. That's a lot more acceptable than putting the humor on somebody else.
We've covered a lot of ground. But in summary, if you only remember a few facts from this presentation: meet the needs of the audience, organize the presentation, start with a hook, limited facts, a strong summary, make it a performance, smile, hand gestures, purposeful gestures.
And finally, your presentation skills are extremely important. And let me prove this to you. Think of a person that you have heard present in the last year or two that if he or she were presenting again, you'd make an effort to attend, get a face in your mind. I'll give you a moment now to yourself answer this question. How many facts do you remember the last time he or she spoke?
I usually know the answer, but you remember the person. They were either friendly, approachable, very knowledgeable, funny, an expert in their field. All the stuff on slides isn't remembered, but you remember them for a long time as a great speaker. And colleagues, I want you to be that person that is remembered for a long time as a great speaker. So, I hope these tips have been valuable to you. And I appreciate you reading.
ABOUT GIBLIB
GIBLIB is the premier streaming service with a vast catalog of unrivaled continuing medical education content covering surgical videos, medical lectures, courses, and transcripts. Learn from the world’s best doctors, from the top leading institutions, including Mayo Clinic, UCSF, Cedars-Sinai, Keck Medicine of USC, and many more.
View recent posts

GIBLIB Update
CME Summary when downloading multiple CME activities
Tracking and submitting your CME just got even easier with our new CME summary function. Simply select the completed CME activities that you wish to download the certificates for, and we will consolidate them into a single PDF, which includes a summary of your activities.

Trending Topics
Addressing and Preventing Sexual Harassment in Healthcare
Sexual harassment in health care can have lasting effects on victims, including doctors, nurses and patients. The #MeToo movement has reestablished the need for changes in policy to increase prevention.

State CME Requirements
South Dakota CME Requirements 2022
South Dakota MD and DO physicians, you can fulfill your state CME requirements today by watching the GIBLIB videos listed here.
Institution
Download our mobile app.


- Tips & Tricks
- PowerPoint Templates
- Training Programs
- Free E-Courses
Ultimate Guide to Medical Presentations: Templates, Tutorials, Tips and Resources
About medical presentations.
Medical presentations are fundamentally different from other presentation types. In fact, they are one of the toughest type of presentations to design.
Medical slides have research facts, data charts, diagrams and illustrations that demand a totally different approach to design. You need a slide creation method that considers the unique problems you face as a medical presenter. In this guide, you will Tips, Tutorials and resources to get your started with making over your Medical slides.
We will start with some general tips and tricks on creating medical slides and then proceed to step by step tutorials.

Quick Navigation
Tips to create Medical Presentations
PowerPoint Tutorials for Medical Slides
How to Present Lists & Text
How To Showcase Pictures Creatively
How to use animations effectively, creative morph transition ideas, making medical slides easy to understand, powerpoint delivery tips, powerpoint tips & tricks, issue with typical medical slides, medical slides makeover examples, medical powerpoint templates, free medical & healthcare icons, free medical presentation images, more resources for medical presentations, tips to create medical presentations, how to avoid overwhelming audience in technical presentations.
Do you want to improve how you explain concepts in a technical presentation? In this article, you will find a powerful technique called ‘Telescopic explanation’ to make your technical presentations much clearer and more memorable for your audience. To know more, read this post over on PrezoTraining.com

Tips to present Scientific Information
There are two major facets to a presentation: the content and how you present it. Let’s face it, no matter how great the content, no one will get it if they stop paying attention.
Here are some pointers on how to create clear, concise content for scientific presentations – and how to deliver your message in a dynamic way. Find the tips over on Elsevier connect .
Preparing a Research Presentation
If you have never presented a paper at a scientific meeting, or would like to polish your research presentations, this post contains information that will improve your presentation.
This article contains a set of guides and checklists to help you in the preparation of your presentation. Read this post on ACP .
10 Tips for Medical Presentations
Whether you are presenting an audit or a case report at a local meeting, presenting a paper at a conference, presenting a business case to your Trust, or even presenting on a hot topic at your medical interview, you will need to know how to prepare medical slides which attract your audience rather than distract it. This post on ISC Medical provides 10 tips for Medical presentations.
For a 5-Part series on how to make your Medical Slides Clear and Visual , sign up for our Free E-course.
In the following sections, you'll find step by step PowerPoint tutorials & Makeover Ideas to help you makeover different parts of your presentation.
How To Present Lists and Text
Information presentations use a lot of text and bullet list. In this section, you will find some creative ways to design these type of slides.
PowerPoint Tip: How to Present Long Lists on One Slide
If you have a Long Lists of items on One Slide here is a one-click trick on how to do this. Watch the video below to know more.
PowerPoint Trick to Convert Text to Graphics
Find a useful PowerPoint SmartArt Trick to convert Bullet Point Text to Graphics quickly and easily. Learn how to take the graphics to the next level with some creative ideas from Ramgopal.
For a 5-Part series on how to make your Medical Slides Clear and Visual , sign up for our Free e-course.
Get access to exclusive members-only e-courses & downloads.
Medical presentations usually have a lot of pictures. Especially the training and informational slides. Here are some ways in which you can present the pictures in your presentations in a creative way.
Right Way to Showcase Pictures
Learn the benefit of showcasing pictures using SmartArt tool in PowerPoint. In the video below we start with a typical picture Showcase slide used by presenters. Though the slide looks quite attractive in the first glance, there are some issues that makes the slide ineffective. Watch the video below to know more:
Cropping Pictures in PowerPoint
Learn a super easy trick to crop a picture in PowerPoint in a step by step way. This trick will help you crop a picture in the shape you want, in a single click.
A PowerPoint slide with too much content can be overwhelming for the audience. If you learn to sequence the way you present your information, you make it easy for your audience to understand your presentation.
Here are different ways you can use Custom Animations and Morph Transition effects to sequence information.
Animation for Process with Pictures
In this tutorial, you will find how to create a useful and practical slide with pictures and text to show a process or a timeline diagram. Learn how to create and present it to make an impact.
Animation for Highlighting Pictures
Learn to create an Animated Picture Reveal Effect in PowerPoint. Present your important picture with this effect. Watch the video to preview the effect and learn how to create it:
Sequential Fading technique in PowerPoint
This trick is super useful for medical presentations where you need to present an image step by step. Since it is an image you cannot break it up and present it in parts. However with this useful technique you can highlight one part of an image at a time with animation.

For a 5-Part series on how to make your Medical Slides Clear and Visual , sign up for our Free e-course. Get access to exclusive members-only e-courses & downloads.
In PowerPoint for Office 365, Microsoft introduced the Morph Transition. It is an effective way to create animations fast. Here are some ideas on how you can use this feature to create your slides.
Pros & Cons with Morph Transition
Learn how to create an easy animated scales diagram with Morph Transition Effect. This effect is available in PowerPoint for Office 365. You can also sign up & download the original PowerPoint file over at our website .
Morph Transition To Present Pictures
In this video you will find how to use PowerPoint Morph Transition to replace Custom Animations. See how this can be done with this example of a slide with multiple pictures with text.
Convert your boring text-based slides, blog articles or research papers into clear & beautiful visual slides - even if you have zero Design skills, zero PowerPoint skills & very little time - using our ‘4-step Neuro Slide Design System for Medical Presentations’
Watch the video below to learn more:
Ideas to Present Data
Medical presentations also usually contain a component of data. This could be related to statistics or research. In this section, you will find some easy ways to makeover your slides with numbers.
Creating Pie & Donut Charts
Learn how to create a Pie chart in PowerPoint with this step by step tutorial. This video also covers how to adjust the Pie chart settings and also how to add Donut charts.
How to Animate a PowerPoint Table
Learn a trick to Animate a PowerPoint Table. PowerPoint does not have the feature of animating parts of a table.
[Advanced] Conditional Formatting for Charts
Learn to create a PowerPoint conditional formatting chart that changes color and direction of bar chart automatically for negative values. The positive values are displayed in green color and the negative values in red color.
Here are some tips for when you are actually delivering your presentation. Present confidently with these ideas!
Use Presenter View in PowerPoint like a PRO
How to use Presenter View in PowerPoint to present your slides like a PRO (Presentation Delivery Tips). This view is for the presenter only - when the slideshow This requires 2 monitors (your laptop and the projector screen). Even if you want to use Presenter View in 1 monitor it is possible. Learn how with this video.
Use Hidden Slides to Present Confidently
In this video, you will find a PowerPoint Tip on how to use Hidden slides to present confidently. This feature is especially useful when creating business presentations.
PowerPoint Slideshow Shortcuts
Here are some useful PowerPoint Slideshow Shortcuts you can use when delivering your next presentation. Hope you find these PowerPoint tips useful.
If you wish to improve the quality of your medical slides in a reliable way, take a look at the first video over on this page .
Here are some tips and tricks to reduce time taken to create your slides.
Setting Up Quick Access Toolbar
In this PowerPoint tips tutorial, you will find how to set up the Quick Access Toolbar. It is a great time-saving tool for any version of PowerPoint.
Autocorrect Trick to Save Time
Learn this trick to use PowerPoint Auto-correct option to save time and effort in creating your presentations. Write complex medical terminology accurately & easily in PowerPoint!
Get access to exclusive members-only e-courses & offers.
Many of the medical slides you may see may look like this:

These slides are taken from various sources online like Slideshare and YouTube and represent various types of presentations. The common issues with such slides include:
- Issue with readability - due to poor color choices and font sizes
- Unprofessional design - with overlapping content, hard to read diagrams etc.
- Too much content - that overwhelms the audience
It is quite common to see well researched medical content being totally ignored by the audience - because the presentation slides look busy and boring. And… You can’t blame your audience for tuning out of your presentation.
The quality of your slides makes or breaks your medical presentations.
In this section, we'll makeover usual text filled PowerPoint slides into a visual and interesting slides.
The original slides are taken from various sources online like Slideshare and YouTube and represent various types of presentations.
Medical Title Slide
Original title slide:

Title slide after makeover:

Medical Training Presentation Slide
Original training slide:

Training slide after makeover:

Medical Slide With Quote
Original slide with quote:

Quote slide after makeover:

Health and Safety Training Slide

Slide after makeover:

In the Medical Presentations Bundle with Neuro Slide Design Training, you can watch me make over Text-based slides, a Blog article, a Wikipedia article and a 11-page Research paper. I go through each of the 4 steps to transform these text-based documents to clear and beautiful visual slides.
The Bundle includes 900 Fully Editable PowerPoint Templates. Go over and checkout the bundle .
One of the ways to quickly improve the quality of your slides is to use good quality templates create with the needs of medical presenters in mind. Here are some resources...
Free Medical Title Templates
Leawo website provides free medical title templates for download. These templates are suitable for different type of medical presentations. You can preview and download them here .

FPPT website provides similar free title templates for use as well. You can find title templates related to medical and health fields over here on FPPT .

Premium Medical PowerPoint Templates
While free medical PowerPoint Templates are good enough for student or non-critical presentations, if you are consultant or specialist, you may prefer to use high-quality PowerPoint Templates.
Preview Medical PowerPoint Templates Bundle
Create Medical Slides You Feel Proud to Present Using the Breakthrough Slide Design System created using proven Brain research principles. You can preview templates from our Medical Templates Bundle below:
Browse more templates and know more about the Medical PowerPoint Templates Bundle here .
Icons are useful to represent ideas on slides. Here are some useful links for downloading Healthcare and Medical Icons online.
ICONFINDER : This website has a good collection of vector icons without too many ads or links to other websites.. You can search iconfinder by keyword and specifically look for free to use icons. You can also search by types of icons like glyphs, outline, flat, filled outline, 3D and more.
VECTEEZY : This website provides both free and premium icons. The license may require you to provide attribution to the author. There are lot of popups and ads, and the focus in on their premium icons.
POWERPOINT : If you are using Office 365, you can find a lot of free icons right in PowerPoint. There are icons for people, technology and electronics, communication, business, analytics, commerce, education, signs and symbols, arrows, medical and much more. You can edit the fill colors of these icons to customize them.
Make your own icons in PowerPoint
Make your slides look professional and visual with these icons. Icons make it easy for your audience to remember the information you are presenting. Learn the secret to finding icons for free right within PowerPoint.
300+ Editable Icons for PowerPoint

The Medical Presentations Bundle includes 300+ Medical Icons for PowerPoint. You can break these icons into individual components, mix and match them to create custom icons that meet your specific needs. As one of the doctors using this Bundle said, it is a “ ONE STOP SHOP” for every busy medical practitioner.
Medical presentations can be made more interesting and engaging by the addition of relevant images. If you are looking for high-quality free images, here are some suggestions:
FREEIMAGES.COM : Images on this website are free for use for personal and commercial purposes. You can find a range of generic medical and healthcare images here.

PICJUMBO.COM : This site provides free and interesting images for backgrounds.

WIKIPEDIA is a great source for free images and illustrations. However, there are a couple of things to keep in mind when you use images from Wikipedia.
1) Please check the copyright terms for each image. You may need to provide attribution as per their terms.
2) Images may be of different formats, sizes, color schemes and quality.
Here is a collection of images from Wikipedia related to Brain:

150+ Medical Illustrations | 170+ Medical Photos | 150+ Silhouettes

In the Medical Presentations Bundle we have already done the hard work of putting together a large collection of high quality Medical, Pharma and Science photos & editable illustrations to use in your presentations.
Remember, these are not the usual photos of smiling Doctors and pretty handshakes. These are practical medical photos you can use in your medical slides to illustrate your ideas. As one of the doctors using this Bundle said, it is a “ONE STOP SHOP” for every busy medical practitioner.
For a 5-Part series on how to make your Medical Slides Clear and Visual , sign up for our Free e-course. Get access to exclusive members-only e-courses & downloads.
PowerPoint Skills for Medical Professionals Learn the 14 essential PowerPoint techniques that every medical professional needs to know to design clear medical slides. This training is part of Medical Presentations Bundle .
Advanced PowerPoint Video Tutorials Enhance your presentations with these ideas. In this section you will find extensive video tutorials for 2D and 3D Diagrams, Models, Picture Effects, Animations and More… Click here to browse
Enter your text here...
Liked it? Share:
Get 25 Creative PowerPoint Ideas Mini Course & Members-only tips & offers. Sign up for free below:
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to …
Log in using your username and password
BMA Member Log In
If you have a subscription to The BMJ, log in:
- Need to activate
- Log in via institution
- Log in via OpenAthens
Log in through your institution
Subscribe from £184 *.
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for: £50 / $60/ €56 ( excludes VAT )
You can download a PDF version for your personal record.
Buy this article
Tools for the Patient Presentation
The formal patient presentation.
- Posing the Clinical Question
- Searching the Medical Literature for EBM
Sources & Further Reading
First Aid for the Wards
Lingard L, Haber RJ. Teaching and learning communications in medicine: a rhetorical approach . Academic Medicine. 74(5):507-510 1999 May.
Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format . Academic Medicine. 74(10):S124-S127.
The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) http://meded.ucsd.edu/clinicalmed/oral.htm
"Classically, the formal oral presentation is given in 7 minutes or less. Although it follows the same format as a written report, it is not simply regurgitation. A great presentation requires style as much as substance; your delivery must be succinct and smooth. No time should be wasted on superfluous information; one can read about such matters later in your admit note. Ideally, your presentation should be formulated so that your audience can anticipate your assessment and plan; that is, each piece of information should clue the listener into your thinking process and your most likely diagnosis." [ Le, et al, p. 15 ]
Types of Patient Presentations
New Patient
New patients get the traditional H&P with assessment and plan. Give the chief complaint and a brief and pertinent HPI. Next give important PMH, PSH, etc. The ROS is often left out, as anything important was in the HPI. The PE is reviewed. Only give pertinent positives and negatives. The assessment and plan should include what you think is wrong and, briefly, why. Then, state what you plan to do for the patient, including labs. Be sure to know why things are being done: you will be asked.
The follow-up presentation differs from the presentation of a new patient. It is an abridged presentation, perhaps referencing major patient issues that have been previously presented, but focusing on new information about these issues and/or what has changed. Give the patient’s name, age, date of admission, briefly review the present illness, physical examination and admitting diagnosis. Then report any new finding, laboratory tests, diagnostic procedures and changes in medications.
The attending physician will ask the patient’s permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may offer input or ask questions at any point. When presenting at bedside the student should try to involve the patient.
Preparing for the Presentation
There are four things you must consider before you do your oral presentation
- Occasion (setting and circumstances)
Ask yourself what do you want the presentation to do
- Present a new patient to your preceptor : the amount of detail will be determined by your preceptor. It is also likely to reflect your development and experience, with less detail being required as you progress.
- Present your patient at working or teaching rounds : the amount of detail will be determined by the customs of the group. The focus of the presentation will be influenced by the learning objectives of working responsibilities of the group.
- Request a consultant’s advice on a clinical problem : the presentation will be focused on the clinical question being posed to the consultant.
- Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
- Enlist cooperation required for patient care : a short presentation focusing on the impact your audience can have in addressing the patient’s issues.
Preparation
- Patient evaluation : history, physical examination, review of tests, studies, procedures, and consultants’ recommendations.
- Selected reading : reference texts; to build a foundational understanding.
- Literature search : for further elucidation of any key references from selected reading, and to bring your understanding up to date, since reference text information is typically three to seven years old.
- Write-up : for oral presentation, just succinct notes to serve as a reminder or reference, since you’re not going to be reading your presentation.
Knowledge (Be prepared to answer questions about the following)
- Pathophysiology
- Complications
- Differential diagnosis
- Course of conditions
- Diagnostic tests
- Medications
- Essential Evidence Plus
Template for Oral Presentations
Chief Complaint (CC)
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it. For ongoing care, give a one sentence recap of the history.
History of Present Illness (HPI)
This will be very similar to your written HPI. Present the most important problem first. If there is more than one problem, treat each separately. Present the information chronologically. Cover one system before going onto the next. Characterize the chief complaint – quality, severity, location, duration, progression, and include pertinent negatives. Items from the ROS that are unrelated to the present problem may be mentioned in passing unless you are doing a very formal presentation. When you do your first patient presentation you may be expected to go into detail. For ongoing care, present any new complaints.
Review of Systems (ROS)
Most of the ROS is incorporated at the end of the HPI. Items that are unrelated to the present problem may be briefly mentioned. For ongoing care, present only if new complaints.
Past Medical History (PMH)
Discuss other past medical history that bears directly on the current medical problem. For ongoing care, have the information available to respond to questions.
Past Surgical History
Provide names of procedures, approximate dates, indications, any relevant findings or complications, and pathology reports, if applicable. For ongoing care, have the information available to respond to questions.
Allergies/Medications
Present all current medications along with dosage, route and frequency. For the follow-up presentation just give any changes in medication. For ongoing care, note any changes.
Smoking and Alcohol (and any other substance abuse)
Note frequency and duration. For ongoing care, have the information available to respond to questions.
Social/Work History
Home, environment, work status and sexual history. For ongoing care, have the information available to respond to questions.
Family History Note particular family history of genetically based diseases. For ongoing care, have the information available to respond to questions.
Physical Exam/Labs/Other Tests
Include all significant abnormal findings and any normal findings that contribute to the diagnosis. Give a brief, general description of the patient including physical appearance. Then describe vital signs touching on each major system. Try to find out in advance how thorough you need to be for your presentation. There are times when you will be expected to give more detail on each physical finding, labs and other test results. For ongoing care, mention only further positive findings and relevant negative findings.
Assessment and Plan
Give a summary of the important aspects of the history, physical exam and formulate the differential diagnosis. Make sure to read up on the patient’s case by doing a search of the literature.
- Include only the most essential facts; but be ready to answer ANY questions about all aspects of your patient.
- Keep your presentation lively.
- Do not read the presentation!
- Expect your listeners to ask questions.
- Follow the order of the written case report.
- Keep in mind the limitation of your listeners.
- Beware of jumping back and forth between descriptions of separate problems.
- Use the presentation to build your case.
- Your reasoning process should help the listener consider a differential diagnosis.
- Present the patient as well as the illness .
- << Previous: Home
- Next: Posing the Clinical Question >>
- Last Updated: Jul 19, 2023 10:52 AM
- URL: https://rowanmed.libguides.com/tools
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- GMS J Med Educ
- v.34(1); 2017

Language: English | German
Accepted standards on how to give a Medical Research Presentation: a systematic review of expert opinion papers
Anerkannte standards zum halten medizinischer vorträge: eine systematische Übersicht publizierter experteneinschätzungen, christine blome.
1 University Medical Center Hamburg-Eppendorf (UKE), Institute for Health Services Research in Dermatology and Nursing (IVDP), German Center for Health Services Research in Dermatology (CVderm), Hamburg, Germany
Hanno Sondermann
Matthias augustin.
Background: This systematic review aimed to extract recommendations from expert opinion articles on how to give a medical research presentation on a scientific conference and to determine whether the experts agree on what makes an effective or poor presentation.
Methods: Presentation-related terms were searched within article titles listed in PubMed, restricting the search to English-language articles published from January 1975 to July 2015. Recommendations were extracted from the articles, grouped by content, and analyzed for frequency. Ninety-one articles were included. Among 679 different recommendations, 29 were given in more than 20% of articles each. The five most frequent recommendations were to keep slides simple, adjust the talk to the audience, rehearse, not read the talk from slides or a manuscript, and make eye contact.
Results: No article gave advice that was the complete opposite of the 29 most frequent recommendations with the exception of whether a light or dark background should be used for slides.
Conclusions: Researchers should comply with these widely accepted standards to be perceived as effective presenters.
Zusammenfassung
Hintergrund: Ziel dieser systematischen Übersichtsarbeit war es, aus publizierten Expertenstellungnahmen Empfehlungen zur Vorgehensweise bei medizinischen Präsentationen auf wissenschaftlichen Fachtagungen zu extrahieren und abzuleiten, ob Experten in der Frage übereinstimmen, was eine gute oder schlechte Präsentation ausmacht.
Methoden: Präsentationsbezogene Schlagwörter wurden in den Titeln englischsprachiger, in PubMed geführter und zwischen Januar 1975 und Juli 2015 erschienener Artikel gesucht. Aus den gefundenen Expertenartikeln wurden Empfehlungen extrahiert, inhaltlich gruppiert und nach Häufigkeit ausgewertet. Einundneunzig Artikel wurden eingeschlossen. Von insgesamt 679 unterschiedlichen Empfehlungen fanden sich 29 jeweils in mindestens 20% der Artikel. Die fünf häufigsten Empfehlungen lauteten: Einfache Folien verwenden; die Zuhörerschaft kennen; Augenkontakt halten; die Präsentation üben; nicht von Folien oder Manuskript ablesen.
Ergebnisse: In keinem Artikel wurde eine Empfehlung gegeben, die das klare Gegenteil einer der 29 häufigsten Empfehlungen darstellten, bis auf die Frage, ob ein heller oder dunkler Folienhintergrund verwendet werden sollte.
Schlussfolgerung: Wissenschaftler sollten sich an die hier gefundenen, weithin akzeptierten Empfehlungen halten, damit ihre Präsentationen positiv wahrgenommen werden.
1. Introduction
Some presentations at medical conferences are easy to follow, engaging, and even inspire changes in the way patients are treated or scientific work is conducted. Conversely, others induce the audience to check their mobile phones or take a nap because they are so difficult to concentrate on.
What exactly makes great medical research presentations great? Empirical or even experimental data on this question are scarce [ 1 ], [ 2 ], [ 3 ], [ 4 ]. However, more than 80 authors of expert opinion articles have described what they believe a medical presenter should or should not do. The aim of this review was to extract all recommendations from these articles and determine whether the experts agree on what makes a medical research presentation either effective or poor.
Parts of this study were obtained from a previous dissertation by Sondermann, 2014 [ 5 ].
Presentation-related terms were searched within the titles of articles listed in PubMed, restricting the search to English-language articles published from January 1975 to July 2015. The search terms were:
(scientific[ti] AND presentation*[ti]) OR (conference[ti] AND presentation*[ti]) OR (oral[ti] AND presentation*[ti]) OR (research[ti] AND presentation*[ti]) OR (scientific[ti] AND meeting*[ti]) OR (public[ti] AND speaking[ti]) OR (public[ti] AND speech[ti]) OR (Power[ti] AND Point[ti]) OR PowerPoint[ti] OR (scientific[ti] AND talk*[ti]) OR lecturing[ti] OR lectures[ti] OR (scientific[ti] AND conference*[ti]) OR (medical[ti] AND presentation*[ti]) OR (paper[ti] AND presentation*[ti]) AND "1975/01/01"[PDAT]:"2015/07/31"[PDAT] AND English[lang]
The bibliographies of eligible articles were reviewed for further references.
We included expert opinion articles and editorials that provided advice on how to give a medical research presentation at scientific conferences. We excluded articles exclusively referring to lectures to students, continued medical education, or health care management.
Recommendations were extracted from each article, including both direct (e.g., “You should…”) and indirect recommendations (e.g., “Remember the audience’s time (…) should not be abused by presentation of uninteresting preliminary material” [ 6 ]). Mere suggestions were not extracted; these were typically signaled by words such as “consider.” We also excluded recommendations on abstract writing, use of outdated technology (e.g., diapositives), radiologic images (for being too specific), and technical aspects (e.g., choice of software).
Differently worded advice from two authors was regarded as the same recommendation if equal in content (e.g., “initially, rehearse alone” [ 7 ] and “initially, practice the talk alone” [ 8 ]). Similar recommendations were grouped into more general but still concrete advice. For example, “limit the number of lines on a slide to six” [ 9 ] and “no more than seven lines per slide” [ 10 ] were grouped into “limit the number of lines per slide.” Finally, we determined the frequency of recommendations, counting those given in two articles by the same first author only once.
The PubMed search delivered 4,140 hits, 91 of which met the inclusion criteria [ 6 ], [ 7 ], [ 8 ], [ 9 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ], [ 17 ], [ 18 ], [ 19 ], [ 20 ], [ 21 ], [ 22 ], [ 23 ], [ 24 ], [ 25 ], [ 26 ], [ 27 ], [ 28 ], [ 29 ], [ 30 ], [ 31 ], [ 32 ], [ 33 ], [ 34 ], [ 35 ], [ 36 ], [ 37 ], [ 38 ], [ 39 ], [ 40 ], [ 41 ], [ 42 ], [ 43 ], [ 44 ], [ 45 ], [ 46 ], [ 47 ], [ 48 ], [ 49 ], [ 50 ], [ 51 ], [ 52 ], [ 53 ], [ 54 ], [ 55 ], [ 56 ], [ 57 ], [ 58 ], [ 59 ], [ 60 ], [ 61 ], [ 62 ], [ 63 ], [ 64 ], [ 65 ], [ 66 ], [ 67 ], [ 68 ], [ 69 ], [ 70 ], [ 71 ], [ 72 ], [ 73 ], [ 74 ], [ 75 ], [ 76 ], [ 77 ], [ 78 ], [ 79 ], [ 80 ], [ 81 ], [ 82 ], [ 83 ], [ 84 ], [ 85 ], [ 86 ], [ 87 ], [ 88 ], [ 89 ], [ 90 ], [ 91 ], [ 92 ], [ 93 ], [ 94 ], [ 95 ], [ 96 ]. Of the 91 articles, 63 were from the medical field and 28 from related fields such as nursing. We found 3 to 103 different recommendations in each article, totaling 3,135 recommendations. Identification of identical recommendations and grouping similar ones resulted in 679 different recommendations. Of these, 349 were given in only one article each; for example, “remain in the hall from the start of the session until your talk” [ 94 ].
The most frequent advice, given in 62.9% of articles, was to keep slides simple. In particular, authors stated that one should not overload slides or include too much detail, but use clear, concise, simply designed visuals instead. Simplicity of visuals was also the subject of 5 of the 29 most frequent recommendations (see Table 1 (Tab. 1) ), including limiting the number of lines per slide (42.9%) and number of words per line (28.6%), using simple tables and graphs (34.1%), using animations carefully (27.5%), and putting phrases, not sentences, on slides (24.2%).

The second most frequent advice, to know one’s audience (52.7%), referred to who the audience is (e.g., profession, size, age, education), what they already know of the topic, or why they are there (i.e., what their expectations, attitudes, and interests are). Authors advised adjusting the presentation accordingly instead of using canned talks.
Making eye contact was the third most frequent advice (46.2%). This was specified by some authors as making eye contact with many or all persons, making eye contact with persons in all sections of the audience, or making continuous eye contact.
Rehearsal of the presentation was recommended in 44.0% of the articles. In addition, one-third of the articles advised rehearsal in front of other persons. Taken together, 56.0% of the articles gave at least one of these two recommendations. Timing the presentation beforehand – recommended by 38.5% – can ensure that the presenter will stick to the allotted time, an advice given by 40.7%. Further advice calling for thorough preparation was to know one’s topic “like the back of one’s hand” (31.9%), to develop an objective for the talk (28.6%), to and prepare for questions (20.9%). All equipment should be tested beforehand (27.5%).
When delivering the presentation, one should not read the talk from either slides or a manuscript (44.0%). For this purpose (and for simplicity) slides should contain words or phrases instead of complete sentences (24.2%).
The presenter should vary the presentation of his or her voice instead of speaking monotonously (29.7%), not speak too fast (24.2%), face the audience (23.1%), and show some enthusiasm, excitement, or energy (20.9%). To enhance understanding, one should keep the presentation clear and simple (26.4%), be logical (23.1%), and end with a summary (26.4%). The number of slides should be limited (27.5%); most articles specified one slide per minute (n=7, 7.7%).
The slides should be readable (42.9%), referring to both text and visuals. This was probably also the reason for recommending large font sizes (this advice was not included in the 29 most frequent recommendations, however; n=18, 19.8%). Authors generally disagreed regarding the exact size to be used, which ranged from 18 to 32 points; a font size of 24 points was recommended most frequently (n=8, 8.8%).
Authors agreed that the slide design should be consistent throughout the presentation (20.9%) and that contrasting colors should be used (20.9%). Most authors recommended using a dark background (26.4%), while only few recommended using a light background (n=3, 3.3%), arguing that this makes slides easier to read [ 15 ], [ 46 ]; one paper [ 89 ] recommended light background for charts and graphs, but not for text slides (without giving reasons).
None of the included articles gave advice that was the complete opposite of these 29 most frequent recommendations (except for the light versus dark background). However, limiting advice was occasionally given, such as not to practice too much in order to save some enthusiasm [ 62 ] or not to exceed >10% of the original time [ 19 ]. Authors also disagreed on a few topics that did not make it to the 29 most frequent recommendations, including whether clipart or cartoons should be included, whether using a pointer is recommended, and whether information should be added sequentially on a slide.
4. Conclusions
This review extracted recommendations from 91 expert opinion articles on how to give a medical research presentation. We found a high degree of concordance among authors, with 29 recommendations given in more than one-fifth of articles each and very little explicit discordance.
Our findings are limited by the fact that we restricted the literature search to one database and to article titles (without the latter, our search would have yielded 195,766 hits). Nevertheless, we included 91 articles on the presentation of medical research and thus considerably more than two previous reviews, which included 9 expert opinion articles on podium presentations each [ 97 ], [ 98 ].
In addition, the distinction between what authors meant to be recommendations versus mere suggestions was a matter of interpretation; the same is true for decisions on whether recommendations were similar enough to be grouped.
The fact that many authors recommend a behavior does not necessarily mean it will indeed be effective. This can be tested in experimental studies that systematically vary a presenter’s behavior. As in clinical studies, the outcome of interest would need to be defined, which is rarely done in expert opinion articles. We propose as “presenter-relevant outcomes” a) to induce learning effects (i.e., comprehension and retention [ 99 ]), b) to change attitudes, c) to interest and entertain, and d) to improve the presenter’s reputation (e.g., by appearing competent).
To our knowledge, experimental studies have only been done for presentations other than medical research presentations. Surprisingly, the recommendation given most often in this study, “keep your slides simple”, has not been supported with regard to the amount of text on a slide (an aspect also related to further recommendations, like “limit the number of lines per slide”, “limit the number of words per line”, and “put phrases, not sentences, on slides”). A number of studies in students did not find significant differences in retention of information after presentations with concise slides as compared to presentations with more detailed slides [ 100 ], [ 101 ], [ 102 ], as would have been expected by cognitive load theory. This theory states that information will not be encoded adequately if the capacity of our working memory is overloaded [ 103 ], [ 104 ], for example when trying to understand detailed slides and at the same time listen to the presenter. These surprising findings underline the necessity of experimental research on presentation techniques. However, simple slides have been found to be more effective with regard to a different aspect: that is, whether they include pictures not related to the content of the talk. Here, recall was better in students who attended a presentation using slides with irrelevant pictures [ 105 ].
The third most frequent advice, to make eye contact, was found to be effective in one study: Not only did students consider a speaker who made eye contact to be more credible and his talk to be more comprehensible, but they actually learned more as indicated by a subsequent multiple-choice test [ 102 ]. In this study, the “eye contact” condition also differed from the control condition in that the presentation was more lively (recommendation no. 13: “vary your voice“) and in that the presenter did not read from written text only but also made colloquial interjections (recommendation no. 5: “do not read the talk from slides or a manuscript”).
It is quite possible that empirical studies will contradict the advice found in this opinion-based study. For example, there is reason to assume that dark backgrounds (recommended by 24 experts as compared to 3 experts recommending light background) may have disadvantages. For example, they may require dimming the lights so that the audience can read the slides, which in turn may lead to reduced levels of attention due to increased tiredness.
In addition, findings from previous studies may not be generalizable to medical conference presentations where the audience may differ in important aspects from students (which have been the subjects of many of the experiments [ 106 ]) – for example with regard to their reasons for attendance and their prior knowledge of the topic. Future experimental studies should therefore investigate whether the recommendations found in this study are indeed effective, looking at different audiences and contexts, and focusing also on rarely explored aspects related to the preparation of the presentation, like adjustment of the talk to the specific audience (recommendation no. 2) and rehearsal (recommendation no. 4).
Probably one of the main reasons that a particular piece of advice was given in the expert opinion papers is that the authors believed that many presenters did not yet follow it. The 29 most frequent recommendations can thus be interpreted as the 29 most common mistakes made by conference presenters. Most of them appear to be common sense and are generally well known [ 99 ]; therefore, why are flaws so common, even in senior presenters [ 98 ]? Researchers may be unwilling to invest time in thorough preparation [ 107 ], or perhaps they have competing interests such as drawing the audience’s attention away from themselves or using slides as a memory aid [ 104 ]. However, if presenters want their talk to be inspiring and practice-changing, they should adhere to the agreed advice found in this review.
Future experimental studies should investigate the effectiveness of the recommendations found in this opinion-based review.
Funding sources
The authors have no funding sources to declare.
Authors' contributions
CB conceived of the study, participated in its design, conduction, and analysis, and drafted the manuscript. HS participated in the study design, conduction, and analysis and helped draft the manuscript. MA participated in the study design. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Medical Presentations: How to Present Effectively on Urgent Topics

In the face of the pandemic that consumed 2020, we saw an uptick in medical presentations. And rightfully so. The world was in a state of panic over the unknown of a new virus, people were craving information, and organizations like the World Health Organization (WHO) were scrambling to provide data and resources to help address questions and concerns. Whether it was news stories, or medical research, the world needed to understand what we were up against with COVID-19. Naturally, presentations helped to deliver that information. But this isn’t the first time a virus or disease has rattled communities, and it’s certainly not the first time professionals have used medical presentations to educate the masses. Medical presentations are a helpful tool for medical professionals, research clinics, and organizations to help inform and educate their communities on a wide variety of urgent topics. This can include patient treatment, clinical trial research and results, training for medical staff, general education, medical research, or important data regarding diseases.
While medical presentations tend to be fundamentally different from normal presentations in that they include critical and sensitive information, there are still design best practices just like any other deck. That said, what works for a sales pitch might not resonate well with a medical presentation.
Keep these five things in mind when you want to present effectively on urgent medical presentation topics.
Consider your audience
You may be presenting to a group of doctors within your organization to get the team up to speed on new practices, sharing treatment plans with a patient, or educating the community on new health threats. How you structure your medical presentation is not a one-size-fits-all situation. How you talk to internal staff, versus how you would deliver information to a scared patient is not the same. When you’re crafting your message, consider your audience, and tailor the narrative to their overarching concerns and needs.
Keep things straightforward
Unless you’re presenting to third year residents, your audience probably won’t be able to digest complicated medical terminology. It’s important to avoid medical jargon, complex definitions, or overcomplicated explanations that will confuse your audience. Instead, break things down in layman's terms and relate the information back to your audience and how it will affect them. Keeping things straightforward, and clear, will help your audience digest and process the information quicker. The end goal is that your audience leaves with clarity, feeling more educated on the topic and its urgency.
Use icons to reflect the urgency of the situation
The use of visual aids, such as compelling images or meaningful icons, can help paint the picture of urgency in any presentation. Things like clocks, alarms, lightning bolts, or exclamation points can depict emergencies and symbolize something significant in your presentation. The use of impactful visuals will help engage your audience and let them know what they absolutely need to pay attention to. It helps you control the narrative, and highlight any pertinent information or key takeaways.
Beautiful.ai’s free library of hundreds of thousands of images and icons can help take your presentation to the next level. Our custom icons were thoughtfully created by one of our in-house designers, and are a great way to compliment your data and add urgency to your slide .
Hit them with the facts
In most medical presentations, factual data carries the slides. Whether it’s a survey, research results, or statistics about a particular disease, numerical data will help people understand the urgency or severity of the topic. For example, it was common for nearly every COVID-19 presentation or article to include statistics of the percentage of the population infected, which regions were seeing the greatest spikes in cases, death tolls by county, and data relevant to high-risk individuals. While the numbers may not always be fun— especially as they pertain to a pandemic— they paint a clear picture of what the audience needs to understand. Seeing scary statistics can put into perspective just how real the situation is.
Using the proper charts, graphs , or infographics allows you to dictate exactly what information the audience is consuming. Data visualization with infographics can also help the audience understand and retain otherwise complicated data. However, even with the best charts, you can still overwhelm the audience with information. Opt to include only the most relevant info and useful data.
Allow time to process
Regardless of what you’re presenting— big or small— you should leave time at the end for questions. Medical presentations can be paralyzing, and your audience will likely be seeking more answers. Give your audience a minute or two following the presentation to process what they learned, and then give them a chance to ask questions. You may need to elaborate on specific slides, or revisit a piece of data, to help provide clarification. When it comes to urgent topics, you want your audience to leave feeling more knowledgeable and at ease than they were prior to tuning in.

Jordan Turner
Jordan is a Bay Area writer, social media manager, and content strategist.
Recommended Articles
The 7 essential presentation tips for non-designers, grab your audience’s attention right away, up-level your presentation in minutes with visual aids, 7 simple tips for choosing visual presentation ideas for students to engage the class and impress teachers.
3 types of medical presentations (and how to give them)
Here are some tips for presenting the top three types of medical presentations: lectures, research presentations, and case reports.
Derek Murray
Building presentations

With your long to-do list as a medical professional, giving presentations is probably not a high priority. Yet, medical presentations are inevitable. Are you ready to give them when your job requires it? If so, where do you even start?
We want to make it a little easier for you to present data-heavy medical topics in an easy-to-understand way.
So, let’s dive right in with the top three types of medical presentations.
Key Takeaways:
- Structure your medical presentation into a story to make it memorable.
- Medical presentations can be lectures, research, or case presentations.
- Customize the presentation based on the type and goal.
1. Lectures
Medical lectures educate an audience about a medical topic. They’re one of the most challenging presentations. According to the Learning Pyramid , lectures are the most passive learning techniques, which is also why they have the lowest retention rates.

There are several settings for educational lectures, including:
- Conferences
- University or school lectures
Medical lectures help students or an audience comprehend complex medical information and then turn what they learned into actionable strategies.
For example, you may teach students with little medical knowledge about a new medical concept. But they must understand the topic and be able to recall it for examinations.
Tips for giving medical lectures
How can you turn one of the most challenging presentations into an engaging, memorable lecture? Here are a few tips to ace your educational medical lectures:
- Be interactive : Use Q&As, activities, and open discussions.
- Hand out resources: Give physical booklets students can review after the presentation.
- Use multimedia: Add audio-visual elements like images, video, and audio clips.
- Use simple language: Your audience is learning, so they need simple language and plenty of definitions to understand the topic.
- Make it entertaining: Keep your audience’s attention with a more engaging and entertaining presentation.
UnitedHealth Group incorporated imagery and movement to show rather than tell about mental health in 2022 to boost their engagement on the topic.

2. Research presentations
The most information-heavy medical presentation is the research presentation. Research presentations share findings with experienced medical professionals, usually in conference settings. Some of the audience includes:
- Investigators
- Ph.D. students
- Medical professionals and experienced doctors
Research presentations can also be part of healthcare marketing . You may have to introduce a new process, pharmaceutical, or device to encourage other healthcare professionals to adopt it in their practices.
Tips for giving research presentations
Use these tips to improve your research presentations :
- Speak on a higher level: You’re talking to a knowledgeable audience, so they expect a higher level of research.
- Back all facts with data: Use statistics and research to back all claims.
- Use power poses: Build authority with a confident presentation.
- Grab the audience’s attention: Start your presentation by giving your audience a reason to care, like a problem you want to solve.
- Build up the conclusion: Structure the research in a natural, progressive order that builds up to your conclusion.
- Look at the future: Conclude with how the research findings will impact the future of medicine.
- Visualize data : Simplify findings and data with visuals and charts.
Cardinal Health transformed the complex research for Smart Compression into understandable slides using a mix of graphics and storytelling in their medical presentation.
3. Case reports
Medical professionals must give oral case reports when transferring information between providers or a team. These presentations are very brief and often don’t require visuals.
Sometimes a case is especially unique and offers educational value to others. In that case, presenters should transform their quick oral case reports into a longer presentation that incorporates data and visuals.
Tips for giving case reports
Case reports use a similar structure to oral patient presentations, except with more details about each point. You’ll still want to pack as much information in a short presentation as possible.
- Begin the presentation with a patient overview: Start by introducing the patient, including all relevant demographic details in summarized graphics and lists.
- Present the history of the patient: Describe the patient’s history, why they sought care, and the symptoms they presented in charts and visuals.
- Explore medical information: Dive into the medical details, like treatment and history, using a storytelling structure to connect the information.
- Offer a plan: Outline a treatment plan alongside proof.
Summarize details in charts: You’ll pack a large amount of information in a concise presentation, so use plenty of charts and diagrams to summarize data and simplify outcomes.
Tips for preparing engaging medical presentations
Your medical presentations have highly complex topics rich with data. These topics can easily feel overwhelming or even boring if they don’t have the right structure and appearance.
Here are three medical presentation tips we’ve learned to help you prepare and present high-quality medical presentations that engage AND inform.
Know your audience’s knowledge level
Before building and presenting a medical topic, you must know your audience’s knowledge level. A lecture to a class of first-year college students will sound far different from a presentation to doctors with 10+ years of industry experience.
Build a presentation around your audience’s knowledge, so it’s understandable yet challenging. By taking this extra step, you’ll know what points need more explanation and what topics you can dig deeper into based on your audience’s experience.
Build a structured story
A complex topic becomes easy to understand and follow if you use a storytelling structure . You might ask, “How can a lecture on a new treatment be a story?”
Any time you communicate, it’s a story: You have the challenge to solve, potential solutions to try, and a final winner (like when presenting medical research). You can structure that story in a progressive order or by announcing one primary outcome and providing a list of proofs (like with patient case studies).
Focus on a goal
The goal of medical presentations can be educating, training, or persuading the audience, depending on the type of medical presentation. Knowing your goal guides which data is most relevant to bring your desired outcome.
Communicate at the speed of healthcare with Prezent
Whether you’re preparing a lecture, research presentation, or case report, creating presentation slides is probably far down your priority list. The fast-paced healthcare industry has enough duties vying for attention. So how are you supposed to squeeze in hours to build an engaging presentation?
Prezent has your back. No need to sweat the details as we have already developed leading presentation templates perfect for data-driven presentations. Personalize to your audience’s knowledge and presentation preferences with AI-powered technology. Save time and energy with access to 35,000+ custom-built slide templates designed with key business and pharma storylines in mind.
You’ll have an engaging and clear presentation deck in minutes rather than hours. Take back your time and communicate efficiently with Prezent so you can focus on turning your ideas and insights into action.
Our proof is in our results. Schedule a demo to see the platform in action.
More blog articles

How AI is revolutionizing presentations

The Power of AI in Art and Photography: Blending Creativity and Technology

Product launch planning: The roadmap for creating a successful product launch
Get the latest from Prezent community
Join thousands of subscribers who receive our best practices on communication, storytelling, presentation design, and more. New tips weekly. (No spam, we promise!)
- Google Slides Presentation Design
- Pitch Deck Design
- Powerpoint Redesign
- Other Design Services

- Business Slides
- Guide & How to's
Make an impact with an engaging medical presentation
If you want to explain medical concepts or demonstrate a new medical invention, you’d better use medical presentations in PowerPoint. It allows you to make your slides modern & visually appealing with a few creative design moves. Suppose you need to illustrate a healthcare document or make a presentation on a medical topic. In that case, PowerPoint is good for organizing all points to mention, supporting your speech with images, and attracting people with great animation.
You can find plenty of medical presentation examples on the web to inspire or borrow some elements, e.g., icons, colors, themes, etc. If you lack time and skills, you can always address professional services and order medical or business presentation slides . It helps to devote more time to speech and full sleep.
Today, let us help you find out when to use, how to start, and what to add to create modern-looking healthcare PowerPoint visuals.

When to Use Medical PPT Presentation?
Initially, presentations are used to inform, educate or persuade different external and internal audiences. Medicine includes hard and simple explanations, so you can create a healthcare presentation for both children and scientists.
Using the power of words and correct animation, you can deliver the most complex concepts and explain to pupils how blood cells move. So, medical slide presentations are used for:
- Medical conferences;
- Medical cases;
- Medical training;
- Medical networking;
- Medical investment pitch;
- Medical services presentation;
- Medical TED talk;
- Medical university/college/school lecture;
- Medical invention demonstration.
We bet you can make up more situations where medical presentations fit, and we’ve collected the most common causes. Anytime you talk about healthcare problems or news, you need a medical presentation.
How to Start a Presentation on Healthcare?
Medicine topics refer to the section of hard ones, so PowerPoint presentations must be used wisely and correctly to make speech easier to understand. If you have to explain complex concepts, the presentation can be your life-saver if you approach it in a meaningful way.
Step 1: Rely on visuals
The first step is to look for visuals that can accompany your text. PowerPoint was created for animation, but many people incorrectly use slides for paragraphs of scientific information. Meanwhile, we grasp visual information 60,000 times faster than written one.
So, whenever you present technical information, your audience would want relevant visuals to support their understanding. Do not name types of bone fractures or blood cells, show them!
Step 2: Crop and enlarge your images
The next step is the extension of the first one. We recommend using one picture per slide and enlarging it if it contains tiny elements. For example, you want to show a cataract, so increase the image in size for all people to see clearly. Do not be afraid to sacrifice text for the big high-quality picture.
Step 3: Use charts to visualize numbers
Please, forget about bullet points and endless lists on slides. Pity your audience.
- Decide how many numbers or statistics you have to add as separate slides.
- Do not mix pictures with charts or graphs.
- Make them simple but clear.
- Use contrasting backgrounds and comment on every figure.
See, bullet points are only good in articles to make some space and differentiation in a long text.
Step 4: Make your graphics look more professional
Google for medical presentation video tutorials or address custom presentation services to improve PowerPoint presentation . If you need to present in front of professionals, they will most likely have expectations. Thus, use high-resolution images, position every element accordingly, match sizes of arrows/lines within one slide, and just remove all alien elements that clog the animation.

8 Simple Tips to Improve Your Healthcare PowerPoint Presentation
Even though the following tips are simple and easy to implement, they will have a significant impact on your medical slides.
Think ‘Non-Linear’
If you have to explain some definitions, do not present them in a boring linear way. It can easily disengage the audience from the slide. Instead, create an animated explanation with arrows: make the main word big in the middle of the slide and ‘draw’ around it. Why use only words if you work with PowerPoint?
Use simple animated visuals to explain concepts
For example, you have to explain how molecules move in the electric field. A sheet of hard-to-understand text does not attract the audience at all. To engage people better, draw how charged molecules move forward and back. Besides, add an oral explanation for people to visualize better. Thus, the information sticks to the audience’s brains and keeps them involved till the presentation ends.

This slide does not just give a list of 3D printing examples but shows its real usage, which helps the audience visualize the information.
Label your images right
Images are an integral part of any medical presentation, but some presenters misuse them and create eye hops. It means the number of places the eyes have to land on a slide to gather information. When you create a presentation, THINK ABOUT THE AUDIENCE. Try to imagine how their eyes walk through the slide and make this path as convenient as possible.
For example, when you label throat parts, do not create a 1-5 list next to the picture. It may get people tired to walk from the list back to the image and again to the list. It is better to avoid numbers and label parts with names immediately.

Here is a great example of a visually attractive and informative slide. The author has exactly thought about the people because he helped them perceive the information step by step.
Use tables for comparison
Bullet points are good, but slide space is limited, so you’d better use it wisely. Even if you apply custom animation using bullet points, you still present in a linear way. Accordingly, we advise you to use the table to compare two items with a column that defines the characteristics you oppose. It helps the audience of different levels to follow your thoughts. If people do not understand, they distract faster. So, do not let them do it.
Pay attention to information clarity
Make sure the images you place on the slide match with headlines or other marks. Sometimes, people are afraid of many slides and try to put images and text into one. And they disregard the fact that the audience in the back seats sees nothing.

For example, this slide is good and informative, but the text might not be visible for the last lines.
Use charts to present numbers
For example, you want to list etiological factors for a specific disease. Instead of simply saying percentages, show them! People perceive and remember visual information better, so use charts to show the share of each factor. PowerPoint is created for animations, so always look for ways to avoid many words.
Lead with appropriate visuals
We highly do not recommend using photos of wounds, skin/organ diseases, or other body health problems. It may avert some people because these pictures aren’t indeed attractive. Instead, use drawn pictures, e.g., do not show SSI classification on real skin but use cross-section (like the one used in medicine books).

Avoid Using Photos as Slide Backgrounds
Strangely, many medical presenters still use photos for background for some unknown to us purposes. On the contrary, we suppose it is extremely hard for the audience to differentiate the main image or words from the background clog. Background photos do not bring you much value, but people perceive things better on a pure basis. So, please, stop using this habit. The simpler, the better!
Eye-catching animation has never spoiled anyone’s medical presentation. By adding suitable colors and pictures for a neat look, you demonstrate your expertise and support your speech. You will no more get lost if someone interrupts you. Complex topics are better explained with attractive visuals because all people perceive information better if accompanied by images. Therefore, you should use this preference to fit the audience of any size, age, and gender. Master medical presentations in PowerPoint and enjoy people’s attention!
#ezw_tco-2 .ez-toc-widget-container ul.ez-toc-list li.active::before { background-color: #ededed; } Table of contents
- Presenting techniques
- 50 tips on how to improve PowerPoint presentations in 2022-2023 [Updated]
- Present financial information visually in PowerPoint to drive results
- Keynote VS PowerPoint
- Types of presentations
The importance of visual storytelling in presentations (+ effective tips to consider)
- Design Tips
Why presentation of data is important?

8 rules of effective presentation

The Ultimate Patient Case Presentation Template for Med Students
- April 6, 2024
- Reviewed by: Amy Rontal, MD

Knowing how to deliver a patient presentation is one of the most important skills to learn on your journey to becoming a physician. After all, when you’re on a medical team, you’ll need to convey all the critical information about a patient in an organized manner without any gaps in knowledge transfer.
One big caveat: opinions about the correct way to present a patient are highly personal and everyone is slightly different. Additionally, there’s a lot of variation in presentations across specialties, and even for ICU vs floor patients.
My goal with this blog is to give you the most complete version of a patient presentation, so you can tailor your presentations to the preferences of your attending and team. So, think of what follows as a model for presenting any general patient.
Here’s a breakdown of what goes into the typical patient presentation.
Looking for some help studying your shelf/Step 2 studying with clinical rotations? Try our combined Step 2 & Shelf Exams Qbank with 5,500 practice questions— free for 7 days!
7 Ingredients for a Patient Case Presentation Template
1. the one-liner.
The one-liner is a succinct sentence that primes your listeners to the patient.
A typical format is: “[Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y].
2. The Chief Complaint
This is a very brief statement of the patient’s complaint in their own words. A common pitfall is when medical students say that the patient had a chief complaint of some medical condition (like cholecystitis) and the attending asks if the patient really used that word!
An example might be, “Patient has chief complaint of difficulty breathing while walking.”
3. History of Present Illness (HPI)
The goal of the HPI is to illustrate the story of the patient’s complaint. I remember when I first began medical school, I had a lot of trouble determining what was relevant and ended up giving a lot of extra details. Don’t worry if you have the same issue. With time, you’ll learn which details are important.
The OPQRST Framework
In the beginning of your clinical experience, a helpful framework to use is OPQRST:
Describe when the issue started, and if it occurs during certain environmental or personal exposures.
P rovocative
Report if there are any factors that make the pain better or worse. These can be broad, like noting their shortness of breath worsened when lying flat, or their symptoms resolved during rest.
Relay how the patient describes their pain or associated symptoms. For example, does the patient have a burning versus a pressure sensation? Are they feeling weakness, stiffness, or pain?
R egion/Location
Indicate where the pain is located and if it radiates anywhere.
Talk about how bad the pain is for the patient. Typically, a 0-10 pain scale is useful to provide some objective measure.
Discuss how long the pain lasts and how often it occurs.
A Case Study
While the OPQRST framework is great when starting out, it can be limiting. Let’s take an example where the patient is not experiencing pain and comes in with altered mental status along with diffuse jaundice of the skin and a history of chronic liver disease. You will find that certain sections of OPQRST do not apply. In this event, the HPI is still a story, but with a different framework. Try to go in chronological order. Include relevant details like if there have been any changes in medications, diet, or bowel movements.
Pertinent Positive and Negative Symptoms
Regardless of the framework you use, the name of the game is pertinent positive and negative symptoms the patient is experiencing. I’d like to highlight the word “pertinent.” It’s less likely the patient’s chronic osteoarthritis and its management is related to their new onset shortness of breath, but it’s still important for knowing the patient’s complete medical picture. A better place to mention these details would be in the “Past Medical History” section, and reserve the HPI portion for more pertinent history. As you become exposed to more illness scripts, experience will teach you which parts of the history are most helpful to state. Also, as you spend more time on the wards, you will pick up on which questions are relevant and important to ask during the patient interview. By painting a clear picture with pertinent positives and negatives during your presentation, the history will guide what may be higher or lower on the differential diagnosis. Some other important components to add are the patient’s additional past medical/surgical history, family history, social history, medications, allergies, and immunizations.
The HEADSSS Method
Particularly, the social history is an important time to describe the patient as a complete person and understand how their life story may affect their present condition. One way of organizing the social history is the HEADSSS method: – H ome living situation and relationships – E ducation and employment – A ctivities and hobbies – D rug use (alcohol, tobacco, cocaine, etc.) Note frequency of use, and if applicable, be sure to add which types of alcohol consumption (like beer versus hard liquor) and forms of drug use. – S exual history (partners, STI history, pregnancy plans) – S uicidality and depression – S piritual and religious history Again, there’s a lot of variation in presenting social history, so just follow the lead of your team. For example, it’s not always necessary/relevant to obtain a sexual history, so use your judgment of the situation.
4. Review of Symptoms
Oftentimes, most elements of this section are embedded within the HPI. If there are any additional symptoms not mentioned in the HPI, it’s appropriate to state them here.
5. Objective
Vital signs.
Some attendings love to hear all five vital signs: temperature, blood pressure (mean arterial pressure if applicable), heart rate, respiratory rate, and oxygen saturation. Others are happy with “afebrile and vital signs stable.” Just find out their preference and stick to that.
Physical Exam
This is one of the most important parts of the patient presentation for any specialty. It paints a picture of how the patient looks and can guide acute management like in the case of a rigid abdomen. As discussed in the HPI section, typically you should report pertinent positives and negatives. When you’re starting out, your attending and team may prefer for you to report all findings as part of your learning. For example, pulmonary exam findings can be reported as: “Regular chest appearance. No abnormalities on palpation. Lungs resonant to percussion. Clear to auscultation bilaterally without crackles, rhonchi, or wheezing.” Typically, you want to report the physical exams in a head to toe format: General Appearance, Mental Status, Neurologic, Eyes/Ears/Nose/Mouth/Neck, Cardiovascular, Pulmonary, Breast, Abdominal, Genitourinary, Musculoskeletal, and Skin. Depending on the situation, additional exams can be incorporated as applicable.
Now comes reporting pertinent positive and negative labs. Several labs are often drawn upon admission. It’s easy to fall into the trap of reading off all the labs and losing everyone’s attention. Here are some pieces of advice:
You normally can’t go wrong sticking to abnormal lab values.
One qualification is that for a patient with concern for acute coronary syndrome, reporting a normal troponin is essential. Also, stating the normalization of previously abnormal lab values like liver enzymes is important.
Demonstrate trends in lab values.
A lab value is just a single point in time and does not paint the full picture. For example, a hemoglobin of 10g/dL in a patient at 15g/dL the previous day is a lot more concerning than a patient who has been stable at 10g/dL for a week.
Try to avoid editorializing in this section.
Save your analysis of the labs for the assessment section. Again, this can be a point of personal preference. In my experience, the team typically wants the raw objective data in this section. This is also a good place to state the ins and outs of your patient (if applicable). In some patients, these metrics are strictly recorded and are typically reported as total fluid in and out over the past day followed by the net fluid balance. For example, “1L in, 2L out, net -1L over the past 24 hours.”
6. Diagnostics/Imaging
Next, you’ll want to review any important diagnostic tests and imaging. For example, describe how the EKG and echo look in a patient presenting with chest pain or the abdominal CT scan in a patient with right lower quadrant abdominal pain. Try to provide your own interpretation to develop your skills and then include the final impression. Also, report if a diagnostic test is still pending.
7. Assessment/Plan
This is the fun part where you get to use your critical thinking (aka doctor) skills! For the scope of this blog, we’ll review a problem-based plan. It’s helpful to begin with a summary statement that incorporates the one-liner, presenting issue(s)/diagnosis(es), and patient stability. Then, go through all the problems relevant to the admission. You can impress your audience by casting a wide differential diagnosis and going through the elements of your patient presentation that support one diagnosis over another. Following your assessment, try to suggest a management plan. In a patient with congestive heart failure exacerbation, initiating a diuresis regimen and measuring strict ins/outs are good starting points. You may even suggest a follow-up on their latest ejection fraction with an echo and check if they’re on guideline-directed medical therapy. Again, with more time on the clinical wards you’ll start to pick up on what management plan to suggest. One pointer is to talk about all relevant problems, not just the presenting issue. For example, a patient with diabetes may need to be put on a sliding scale insulin regimen or another patient may require physical/occupational therapy. Just try to stay organized and be comprehensive.
A Note About Patient Presentation Skills
When you’re doing your first patient presentations, it’s common to feel nervous. There may be a lot of “uhs” and “ums.”
Here’s the good news: you don’t have to be perfect! You just need to make a good faith attempt and keep on going with the presentation.
With time, your confidence will build. Practice your fluency in the mirror when you have a chance. No one was born knowing medicine and everyone has gone through the same stages of learning you are!
Practice your presentation a couple times before you present to the team if you have time. Pull a resident aside if they have the bandwidth to make sure you have all the information you need.
One big piece of advice: NEVER LIE. If you don’t know a specific detail, it’s okay to say, “I’m not sure, but I can look that up.” Someone on your team can usually retrieve the information while you continue on with your presentation.
Example Patient Case Presentation Template
Here’s a blank patient case presentation template that may come in handy. You can adapt it to best fit your needs. One-Liner: Chief Complaint: History of Present Illness: Past Medical History: Past Surgical History: Family History: Social History: Medications: Allergies: Immunizations: ROS: Objective: Vital Signs : Temp ___ BP ___ /___ HR ___ RR ___ O2 sat ___ Physical Exam:
General Appearance:
Mental Status:
Neurological:
Eyes, Ears, Nose, Mouth, and Neck:
Cardiovascular:
Genitourinary:
Musculoskeletal:
Most Recent Labs:
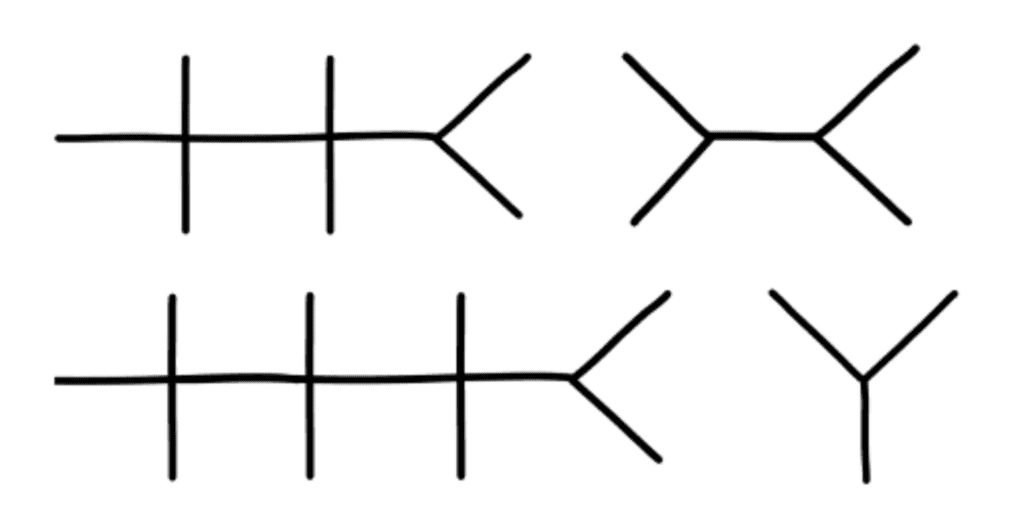
Previous Labs:
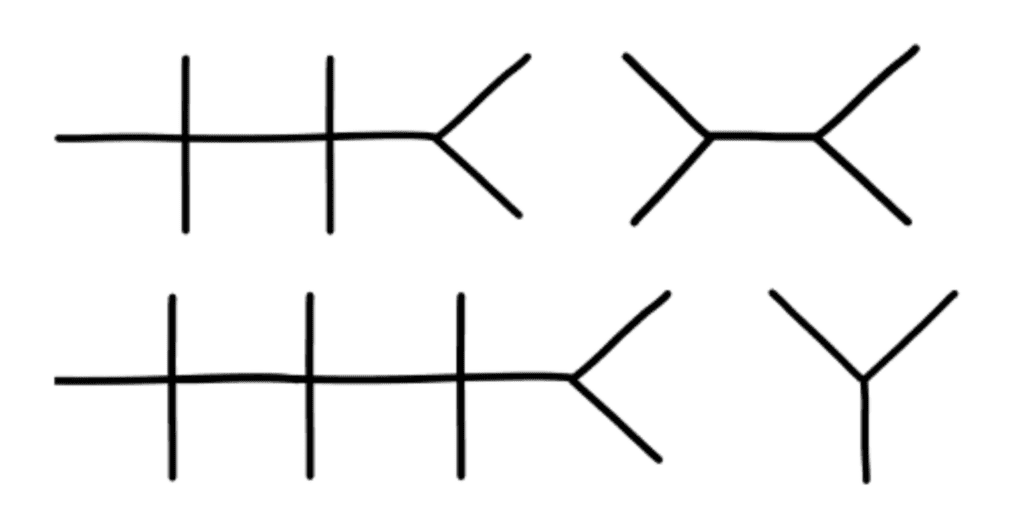
Diagnostics/Imaging:
Impression/Interpretation:
Assessment/Plan:
One-line summary:
#Problem 1:
Assessment:
#Problem 2:
Final Thoughts on Patient Presentations
I hope this post demystified the patient presentation for you. Be sure to stay organized in your delivery and be flexible with the specifications your team may provide. Something I’d like to highlight is that you may need to tailor the presentation to the specialty you’re on. For example, on OB/GYN, it’s important to include a pregnancy history. Nonetheless, the aforementioned template should set you up for success from a broad overview perspective. Stay tuned for my next post on how to give an ICU patient presentation. And if you’d like me to address any other topics in a blog, write to me at [email protected] ! Looking for more (free!) content to help you through clinical rotations? Check out these other posts from Blueprint tutors on the Med School blog:
- How I Balanced My Clinical Rotations with Shelf Exam Studying
- How (and Why) to Use a Qbank to Prepare for USMLE Step 2
- How to Study For Shelf Exams: A Tutor’s Guide
About the Author
Hailing from Phoenix, AZ, Neelesh is an enthusiastic, cheerful, and patient tutor. He is a fourth year medical student at the Keck School of Medicine of the University of Southern California and serves as president for the Class of 2024. He is applying to surgery programs for residency. He also graduated as valedictorian of his high school and the USC Viterbi School of Engineering, obtaining a B.S. in Biomedical Engineering in 2020. He discovered his penchant for teaching when he began tutoring his friends for the SAT and ACT in the summer of 2015 out of his living room. Outside of the academic sphere, Neelesh enjoys surfing at San Onofre Beach and hiking in the Santa Monica Mountains. Twitter: @NeeleshBagrodia LinkedIn: http://www.linkedin.com/in/neelesh-bagrodia

Related Posts
How to Study For Shelf Exams: A Tutor’s Guide
- May 6, 2024

The Ultimate ICU Patient Presentation Template for Med Students
- May 3, 2024

Quiz: Which “Scrubs” Character Are You in Your Clinical Rotations?
- March 26, 2024
- Recommended

A medical student’s first patient presentation
In medical school, you’re not taught how to give stellar patient presentations. Yes, you’re shown the traditional order of things: “Give an effective one-liner first, then tell the HPI [history of present illness] but only give pertinent info, etc.” Just exactly how to deliver the punch that impresses your attending is an art. And it’s an art that takes some time to perfect.
My very first time presenting a patient was terrifying, and it was during my neurology rotation. My attending was the head of the neurology and rehabilitation department, and I was the only first-year med student. On the team were two third-years, one fellow, and three residents.
David was a 21-year-old Asian male who came to the ER for upper extremity weakness. He and his mom spoke Cantonese to each other and me, so our interactions were assisted by one of the mobile translator stations. It had a tablet attached to a pole about 4 or so feet off the ground, and once you selected your language, an interpreter was online within a minute.
As is usual with new patients, students are the first to meet them and to gather the HPI. Then, the residents see the same patients, and with the students together formulate the differential diagnosis and management plan for each patient. The resident I worked with, Catherine, was wonderful, and an MD/PhD. Though, she notoriously had high expectations of students.
“Alright, tell me your presentation.”
“David is a 21-year-old Asian male who came to the ER this morning for a three-day history of upper extremity weakness in both arms.”
“Good. Keep going.”
“This is new to him, and he was not in an accident or any incidence of trauma recently or in the past.”
“No. What did you learn? OLDCARTS. Onset. Location. Duration. Character. Aggravating or Alleviating factors. Radiation. Timing. Severity. You already said onset, location, and duration. Did he feel any pain prior to or during his weakness? Does the weakness come and go? Anything he does make it better or worse? You have to go in order; if not I won’t follow you.”
“OK …”
I was ready to give it another go-around, but by that time the team phone rang and it was the attending on speakerphone.
“Good morning everyone. Ready for rounds?”
“Yes, Dr. Lezinsky,” said one of the residents.
“Great, meet me outside room 13-A.”
Wonderful. That’s the room my patient was in.
As I walked in the middle of the pack of alternating short and long white coats to my patient’s room, I felt my heart beat at an alarming rate. My watch even vibrated continuously, with the screen showing my heart rate above 100. I casually silenced my watch and also my head so that I could stop being so nervous.
At the door, we were greeted by my patient’s nurse and saw Dr. Lezinsky for the first time. He was a legend at the hospital and was also the neurology residency program director. I’ve heard stories of him being one of the best attendings you’ll ever have the pleasure of listening and learning from, but that he was also hard on students.
Without many words, he said, “Which medical student has the first patient?”
“That would be me.”
“What year?”
“First-year, sir.”
“Let’s hear the story.”
I have a bad habit of overly relying on handwritten or printed notes if I have them on hand. I remembered most of the beginning of the presentation, but slowly started to read off of my paper so that I wouldn’t say anything out of order or incorrectly.
About halfway through, I quickly glanced at my resident. Catherine gave me the look of, “What are you literally doing? Didn’t we rehearse?” In stark contrast, Dr. Lezinsky was devoid of emotion and instead nodded his head every so often. But was that an affirmative nod? Or a nod that meant, “Not right, but we’ll talk about it once you’re done presenting.”
In what seemed like an eternity with my palms now clammy, I concluded the presentation with the one-liner, my differential as to my thoughts on what could be causing David’s symptoms, and my proposed management plan.
“Is that all, T.J.?”
“I believe so, sir.”
“OK, Catherine, anything else to add?”
“Only that he is up to date with all of his vaccinations, and that he and his family only speak Cantonese.”
“T.J., can you get the … oh great! You have the tablet. I’ll let you introduce the team to the family, and we’ll have the interpreter join us to help.”
The team met David and his parents, and it was smooth sailing from there. Myasthenia gravis is what we thought he had because of his weakness worsening as the day progressed along with slurred speech in the evenings. Immunosuppressive treatment was soon started and David’s condition improved.
As we entered the elevator to the next patient floor, it was Dr. Lezinsky at the front and me right behind him. As the door closed, Dr. Lezinsky turned his body towards me.
“Was this your first time presenting?”
“Yes, it was.”
“That was really good. Over time, you’ll find yourself not referring to your notes, but relying more on your understanding of the patient’s history and possible disease etiology.”
“Thank you so much, Dr. Lezinsky. That really means a lot.”
Looking back to my first presentation, I’ve improved since then. After you do something so many times over, you start creating your own personal style. Yet, I know that there is always room to improve and the way you present a patient varies tremendously depending on the environment and the status of the patient. It all boils down to this: If you can give an effective and memorable presentation, you’re a better advocate for your patient.
Ton La, Jr. is a medical student and can be reached on LinkedIn .
Image credit: Shutterstock.com

Private equity in gastroenterology: Is it the future?

Even the most seasoned patients are no match for the Medical Insurance Industrial Complex

Tagged as: Hospital-Based Medicine , Neurology
More by Ton La, Jr., MD, JD

Pain and laughter for a veteran patient

Unlock the secrets to aging gracefully: specialized care and support for elderly patients

Unveiling the global pandemic threat: insights into risk factors and urgent measures for prevention
Related posts.

A medical student was discriminated against by a patient

Simultaneously being a medical student and patient

A patient becomes a medical student

A medical student as a patient. She thanks her support systems.

What inspires this medical student

3 medical student tips to improve patient communication
More in education.

From toe pain to financial strain: the hidden costs of medical care

Why speaking up in medical school could save lives

How a group of British medical students fought for social prescribing

Physicians’ social media criticism of trainees sparks controversy

Inside Out 2: How new emotions mirror medical student struggles

Making medicine my home
Most popular.

The truth behind opioid use disorder

A night of stars: Finding solace in the vastness of the sea

How corporate health care is failing physicians and patients alike

ER doctor’s adrenaline-fueled night: from life-saving procedures to unpredictable chaos
Past 6 months.

Struggles of navigating prestigious medical systems

Quiet firing in medicine: my journey from burnout to freedom

The sham peer review: a hidden contributor to the doctor shortage

Creating a subspecialty track for experienced hospitalists

Palliative care is plagued by misunderstanding
Recent posts.
![Inside the hidden world of sham peer reviews in medicine [PODCAST] how to give a medical presentation](https://www.kevinmd.com/wp-content/uploads/Inside-the-hidden-world-of-sham-peer-reviews-in-medicine-190x100.jpg)
Inside the hidden world of sham peer reviews in medicine [PODCAST]

Prevent youth suicide: essential steps for parents to secure their home

The heartbreaking decision that taught me the power of boundaries
![How psychotherapy can rescue burned-out physicians [PODCAST] how to give a medical presentation](https://www.kevinmd.com/wp-content/uploads/How-psychotherapy-can-rescue-burned-out-physicians-190x100.jpg)
How psychotherapy can rescue burned-out physicians [PODCAST]
Subscribe to kevinmd and never miss a story.
Get free updates delivered free to your inbox.
Find jobs at Careers by KevinMD.com
Search thousands of physician, PA, NP, and CRNA jobs now.
CME Spotlights
A medical student’s first patient presentation 3 comments
Comments are moderated before they are published. Please read the comment policy .

6 Powerful Ways to Start a Presentation to Doctors
The beginning of your talk will set the tone for your allotted time.
Whatever you do during the first 30-60 seconds should succeed in captivating the audience securely enough for them to turn all of their attention to you for the duration of your presentation. Loosen them up, fascinate them, or make them curious from the very beginning.
Consider using one of the six presentation openers listed below if you would like to try something new.
1. Start with a personal story
Open up to your audience by illustrating how the subject at hand is personally important to you. When you start off with a personal tale of medicine, illness, cure, or perhaps gain and loss, you are inviting everyone present to identify with you. Suddenly you all become a part of the presentation. Rather than having to agree or disagree with the cold facts that you produce, they will actually be able to feel what you are saying once you make yourself seem more personable.
A colleague of mine was giving a similar presentation to another group of doctors just last month. He told me that the number one point the doctors were concerned about was xxxx.
2. Start with a story of a patient
Make your presentation entirely relevant by taking it directly to the case of a patient your medical device had treated. Deliver your story in a clear and intriguing way that lets doctors know that it is to be trusted and is not anecdotal. Before you present, make sure you establish the specific facts of the story so that you have a mental guideline to follow throughout your fluid talk. With your patient story you will start off by creating relevance and accountability for yourself and your message.
A doctor I met in the past told me of a patient who refused xxxxx equipment on the grounds that it was too uncomfortable.
3. Start with a statistic
Give doctors a reason to listen to the rest of your presentation. Rather than asking them to blindly trust you before you get to the proof of your facts, start off with that proof. Deliver a relevant statistic that illuminates the importance of your entire presentation. The data you offer will provide a black and white, irrefutable example of why the topic of your discussion matters to your listeners. Using a statistic also illustrates that you are knowledgeable in the area, giving just one more reason why what you are discussing is worth hearing.
Did you know that the xxxx industry has been growing at a rate of xx% per year?
4. Start with a video
Movies of your medical device or how your technology works are guaranteed to draw attention as long as they are good and well structured. Videos are extremely useful when your medical device is too small to present to a group of doctors, is used inside the patient’s body, or is not mobile and is too large to bring into the room. Another type of video you can use is a video testimonial of a colleague they know and respect.
5. Start with a silence
What can be more powerful than a silence when you are expecting a speech? That period of waiting can be intense as the listeners wait for what is coming next. When you are ready to begin your business presentation , try surprising listeners by providing them with a single sentence, and then a moment of complete silence. Maintain complete composure during the pause so that the doctors do not fear that you have forgotten what you were saying, or perhaps that you are angry or waiting for anything in particular. If you wish, say a few more words only to be followed by yet another silent period. In less than a minute you will have taken complete ownership of the room as all attention has turned to you, waiting for what you have to say next.
6. Start with humor
Laughter is a fun way to draw people’s focus. If you are confident that you will make your listeners laugh, using humor is a strong way of opening a presentation to doctors. The first step however is knowing your audience. You must know what the doctors in front of you will find funny or amusing before you bust out your best joke-telling skills. Then make sure your joke is relevant to your topic as well. A joke is meant to loosen the audience and make them feel comfortable and open to what you are about to say. However, if you botch the joke, you will be in for a rough recovery over the next few minutes.
Related Posts

Presentation Checklist Before you Take the Podium

Medical communications lessons learned from the London Underground map

9 mistakes preparing a presentation for doctors
More From Forbes
15 presentation tips for captivating your audience and commanding the room.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Person speaking in front of audience
Public speaking can be a daunting task, especially when addressing a large audience. Whether you're giving a presentation in the boardroom or delivering a keynote speech at a conference, holding your audience's attention and maintaining command of the room is paramount. The ability to captivate your audience and leave a lasting impression not only enhances your message's impact but also builds your reputation as a confident and effective speaker.
Here, Forbes Coaches Council members share invaluable tips and strategies to help you conquer your fear of public speaking and ensure that your next presentation or speech is a resounding success.
1. Be Confident
Be grounded and confident to be yourself and then tell great stories. Use your voice and the stage to bring the stories alive. Your audience will connect to the emotion of the story but make sure that it is relevant for your audience and related to the topic. - Cath Daley , Cath Daley Ltd
2. Find A Way To Actively Engage The Audience
Be prepared with ways to get your audience engaged and keep their focus. Whether that's relating to your audience, telling a joke or asking questions, actively driving engagement will make for a more effective presentation or speech. - Luke Feldmeier , Online Leadership Training - Career and Leadership Accelerator for Engineers
3. Create An Emotional Connection
Creating an emotional connection with the audience and involving them in your session fosters active participation, and ensures your audience stays engaged throughout. This also serves to enhance your presence and to create memories that stay with them long after your presentation ends. - Kristin Andree , Andree Group
4. Put Your Unique Take Front And Center
Do you have something unexpected to say about your topic? Something that goes against the mainstream opinion in your industry or is maybe even slightly provocative? If so, putting your unique take front and center in the title and the beginning of your talk and explaining or resolving it later keeps your audience engaged and interested. - Micha Goebig , Go Big Coaching & Communications, LLC
5. Remember That The Audience Doesn't Know Your Planned Speech
No one wants to see you fail as a speaker. Remember that the focus shouldn't be on whether or not you can recall verbatim every word of your planned speech. The focus should be on how to connect to your audience with a few key points using a combination of storytelling and facts. - Sheri Nasim , Center for Executive Excellence
6. Adapt Your Language To The Audience
Talk about something they are interested in or include elements that will keep them interested. Start by asking why your topic matters to each and every one of them. Use language adapted to the audience. Keep the key messages to two or three maximum. Show them what you think and why you care about the topic. - Isabelle Claus Teixeira , Business and Human Development Consulting Pte Ltd
7. Try To Incorporate An Element Of Surprise
Engagement is the key to keeping the audience's attention. Invite participation, tell stories, walk around, have visuals, include humor, raise your voice and ask questions. Think of a comedian who points at someone in the audience: "Hey, you with the red shirt?" Everyone pays attention. What element of surprise can you present? - Susan Jordan, MBA, MSODL, PCC , Sphereshift Coaching and Consulting
8. Know Your Audience
Doing research ahead of time to ensure you're providing the subject matter in a personalized manner will keep their attention. The topic will dictate the necessary vibe. Based on that, providing opportunities for the group to engage, such as shouting out a word, raising a hand, etc., will also help maintain their interest. - Lindsay Miller , Reverie Organizational Development Specialists
9. Use The Problem-Agitation-Solution Approach
Don't just give a presentation — share a story. It must be a story-audience fit though. Use the P.A.S. — problem-agitation-solution — approach. Start with introducing a problem, follow by agitating the problem via telling a relevant anecdote and conclude by offering a solution by giving an audience a clear, direct way to avoid the pain and learn the lesson. - Alla Adam , Alla Adam Coaching
10. Tell The Audience What They Need To Hear
Instead of trying to figure out what to say, figure out what the audience wants and needs to hear. This shift in perspective allows you to tailor your speech in a way that keeps audiences actively engaged because it's good content that they want to hear. - Robin Pou , The Confident Leader
11. Go All In
To command your audience's attention you have to get into the spirit of what you're teaching and go all in without second-guessing yourself. People want to be led, but they'll be unwilling to follow someone who isn't confident in what they are communicating. - Arash Vossoughi , Voss Coaching Co.
12. Use A Compelling Opening
Start your speech/presentation with a compelling opening that grabs the audience's attention. This could be a surprising fact, a relevant story or a thought-provoking question. This initial engagement can help you establish a strong connection with the audience and set the stage for a captivating presentation. - Moza-Bella Tram , Moza-Bella LLC
Forbes Coaches Council is an invitation-only community for leading business and career coaches. Do I qualify?
13. Be Authentic
Connect deeply with your essence and purpose. Radiate authenticity. When you're centered in genuine passion and truth others feel it, creating an unspoken bond. It's not about performing; it's about being present and real and offering value from the heart. That's magnetic. - Anna Yusim, MD , Yusim Psychiatry, Consulting & Executive Coaching
14. Let Your Audience Talk
There is nothing worse than stealing everyone's craving for autonomy and speaking the whole time. The person who does the talking does the learning. So, give some autonomy to the audience. Let them talk. Even if it's thinking time and talking to themselves, or to their neighbor or table group. This gains trust and they will lean into what you have to say even more. - Alex Draper , DX Learning Solutions
15. Leverage Non-Verbal Cues
My top tip is to engage your audience through storytelling. A compelling narrative captures attention, evokes emotion and makes complex ideas more relatable. Additionally, use body language and eye contact effectively. These non-verbal cues can significantly enhance your connection with the audience. - Peter Boolkah , The Transition Guy

- Editorial Standards
- Reprints & Permissions
- ACS Foundation
- Diversity, Equity, and Inclusion
- ACS Archives
- Careers at ACS
- Federal Legislation
- State Legislation
- Regulatory Issues
- Get Involved
- SurgeonsPAC
- About ACS Quality Programs
- Accreditation & Verification Programs
- Data & Registries
- Standards & Staging
- Membership & Community
- Practice Management
- Professional Growth
- News & Publications
- Information for Patients and Family
- Preparing for Your Surgery
- Recovering from Your Surgery
- Jobs for Surgeons
- Become a Member
- Media Center
Our top priority is providing value to members. Your Member Services team is here to ensure you maximize your ACS member benefits, participate in College activities, and engage with your ACS colleagues. It's all here.
- Membership Benefits
- Find a Surgeon
- Find a Hospital or Facility
- Quality Programs
- Education Programs
- Member Benefits
- August 13, 2024 Issue
- Surgeons Describe Why They...
Surgeons Describe Why They Love Their Discipline
August 13, 2024
Residents and medical students who are considering careers in surgery have many incredible career options. See why surgeons from three different disciplines love their areas of practice. This video features:
- Nikolaus Sneshkoff, MD, FACS, otolaryngologist
- Gaby Iskander, MD, MS, acute care surgeon
- Vineet Choudhry, MD, FACS, general surgeon
See how the ACS is the true House of Surgery and how it supports all specialties.
In This Issue

Submit Nominations for the RAS-ACS Outstanding Mentor of the Year Award
Resident Members and Associate Fellows can nominate an inspiring mentor Monday, August 19.

Submit Abstracts for 2025 ACS Surgical Simulation Summit before August 21 Deadline
Original research representing all surgical specialties, and all disciplines that utilize simulation, is encouraged—apply today.

International Surgeons Are Invited to Apply for Community Surgeons Travel Awards
The travel awards provide $4,000 each to support surgeons in attending Clinical Congress. Applications are due September 13.

Don’t Miss Immersive Courses at Clinical Congress 2024
Check out the didactic and skills courses being offered at this year's Clinical Congress.

Access Free Guide for Managing Breast Cancer in Low- and Middle-Income Countries
The downloadable guide covers epidemiology and risk factors, management of benign disease, and more.

Download Free 2025 Trauma Data Dictionary
An updated version of the NTDS Data Dictionary has been released for free download, applicable to patients in 2025.

Energized Florida Chapter Meeting Creates Fellowship among Surgeons
Read Dr. Tyler Hughes's highlights of the May meeting in Florida.

Updated Guidelines Are Release for Management of Intra-Abdominal Infections
This latest update provided clear recommendations for antimicrobial management of this condition based on patient risk assessment, potential for infection caused by multidrug resistant organisms, and more.

Antiplatelets Can Continue Prior to Ventral Hernia Repair
This study used data to compare rates of bleeding complications in patients undergoing ventral hernia repair who were taking either oral anticoagulants or antiplatelet agents.

Opioids Are Prescribed to Only Small Proportion of Pediatric Surgery Patients
In this study, opioid prescriptions were provided to patients who had been hospitalized for care of burns, traumatic injuries, and pectus excavatum repairs.

Abdominoperineal Resection and Low Anterior Resection in Very-Low Rectal Cancer Are Both Acceptable Approaches
Authors of this study queried a national rectal cancer database to determine long-term disease-free survival in patients with low rectal cancers.
- Presentations
- Most Recent
- Infographics
- Data Visualizations
- Forms and Surveys
- Video & Animation
- Case Studies
- Design for Business
- Digital Marketing
- Design Inspiration
- Visual Thinking
- Product Updates
- Visme Webinars
- Artificial Intelligence
How to Create a Successful Project Presentation

Written by: Unenabasi Ekeruke

You’ve spent time working on a project that could be a potential game-changer for your company or client. Now you’re buzzing to present it to your team, investors and other key stakeholders.
Creating and delivering project presentations can be nerve-racking and you probably have one question running through your mind.
How do you get the decision-makers to understand your project or secure their buy-in?
Considering that some companies have had about 12% of failed projects in the past year, you want to create presentations that are not only convincing but memorable.
With the right project presentation deck, you can win and keep your audience’s attention long enough to explain project details and why it’s sure to succeed.
Not sure how to create successful project presentations? We’ve got you covered.
This article will show you how to set project goals and create winning presentations that take your project to the next level.
Here’s a short selection of 8 easy-to-edit project presentation templates you can edit, share and download with Visme. View more templates below:

Let's get to it.
1 Set Goals for Your Project
Before you dive into the main details of your project presentation, you want to answer these questions:
- What is your project set out to achieve?
- Why is it important for you and your team to achieve your set goals?
- How do you plan to communicate your goals to your audience?
If you have to make long guesses before answering these questions, you’ve got a lot of work to do.
Here’s what you should know. Beautiful or well-articulated project presentations aren’t a substitute for project planning. Without clear goals, your project is already set up to fail. And your investors might think, “why bother listening?”
Many project managers tend to rush through the goal-setting phase, but we don't recommend this. That’s because you could be setting yourself up for failure.
Once you clearly define your project goals, you can get stakeholders to buy into them.
Now the question is, how do you set goals for your project and achieve them? One way to do that is by using the SMART goal setting method.
Setting SMART Project Goals
SMART is an acronym that stands for S pecific, M easurable, A chievable, R elevant and T ime-Bound.
SMART goals are a staple for planning and executing successful projects. It takes a deeper look into the finer details your audience care about, such as:
- Project plan and schedule,
- Project timelines,
- Milestones,
- Potential roadblocks and more
For example, let's say your project aims to improve customer experience on web and mobile devices. Notice this example describes the end goal. But it doesn’t specify how you’ll work to enhance customer experience.
Here’s how using SMART goals provides direction for your planned project.
When setting your goals, be clear and specific about what you want to achieve in the end.
A specific goal could be: “We want to build a responsive website and mobile app for our company to improve customer experience. This project will require inputs from our product design, software and marketing department”.
Measurable
During your presentation, you'd have to answer questions like:
- What metrics will you use to determine if you meet the goal?
- How will you know you’re on the right track?
Having metrics in place will help you evaluate your project. Plus, you’d be able to monitor progress and optimize your project to achieve better results.
It doesn’t matter if you’re planning a short-term or long-term project. Ensure you set metrics and milestones that count towards your goal.
From our earlier example, a measurable goal could be to have:
- Over 100,000 mobile app downloads on Google Playstore and Apple App Store.
- A 20% bounce rate on your website and a 15% conversion rate on mobile and web.
Attainable
One of the most critical questions you want to ask during goal-setting is, “Can we achieve our set goal?” Do we have the resources to accomplish the goal within the available time frame?
If the answer is no, then you’d have to consider what it would take to achieve those goals. This may require adjusting your goals or the resources needed to achieve your goal.
Although it’s okay to be ambitious, you should also be realistic. For example, getting 200,000 app downloads in one week could be overly ambitious if you’ve just launched your app. However, if you set out to achieve that goal in three months, that could make your project practicable.
Transform technical, complex information into easy-to-understand reports
- Create detailed diagrams of workflows , systems and processes to see how they interset
- Easily create and share resources for your team , from login credentials to security best practices
- Get more visual with your communication to ensure intricate information is resonating and sinking in
Sign up. It’s free.

Your project goals need to align with your broader business goals. Are your goals relevant to the growth and success of the company? Are they worth allocating resources for?
For instance, if your company is B2B and doesn’t plan to expand to the B2C market, launching an e-commerce website would be an irrelevant goal.
Time-Bound
Regardless of your project type and size, you should set time frames. Setting target dates for deliverables creates a sense of urgency and motivates you to hit your goals.
From our example above, a time-bound goal could be “We aim to achieve 100,000 mobile app downloads and a 15% conversion rate by the end of the fiscal year. Our company will launch the mobile app by Q3 with a robust marketing campaign that will run through the end of next fiscal year.”
Setting SMART goals doesn’t have to be a challenging task. Use the template below to set project goals that position your business for success.
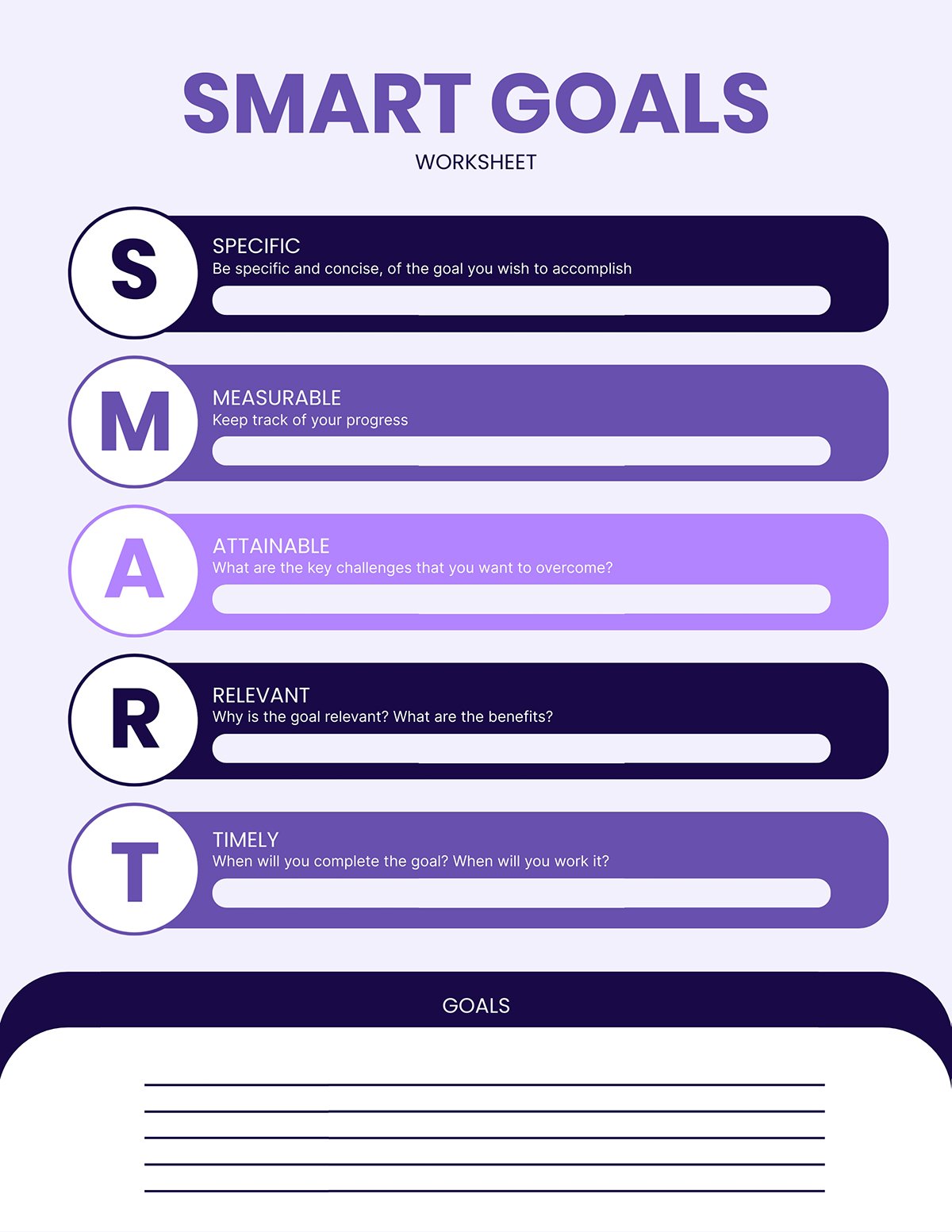
Communicate Project Goals to Your Team Members
After you've set your goals, your team will play a key role in helping you achieve them. So you ensure they understand these things:
- Why the project goals are in place
- What it's supposed to deliver for your business and customers
- How their role, team and department contributes to the success of the project
Unless you’re clear on this, the project can derail and move in all sorts of unwanted directions.
Rather than slam the goals you’ve set on your team, make it a collaborative effort. Spend time talking to your team and stakeholders about the project goals.
Don't limit your communication to people within your department. You can reach out to people in other departments like sales, operations, finance, etc., to see how well your goals align with theirs.
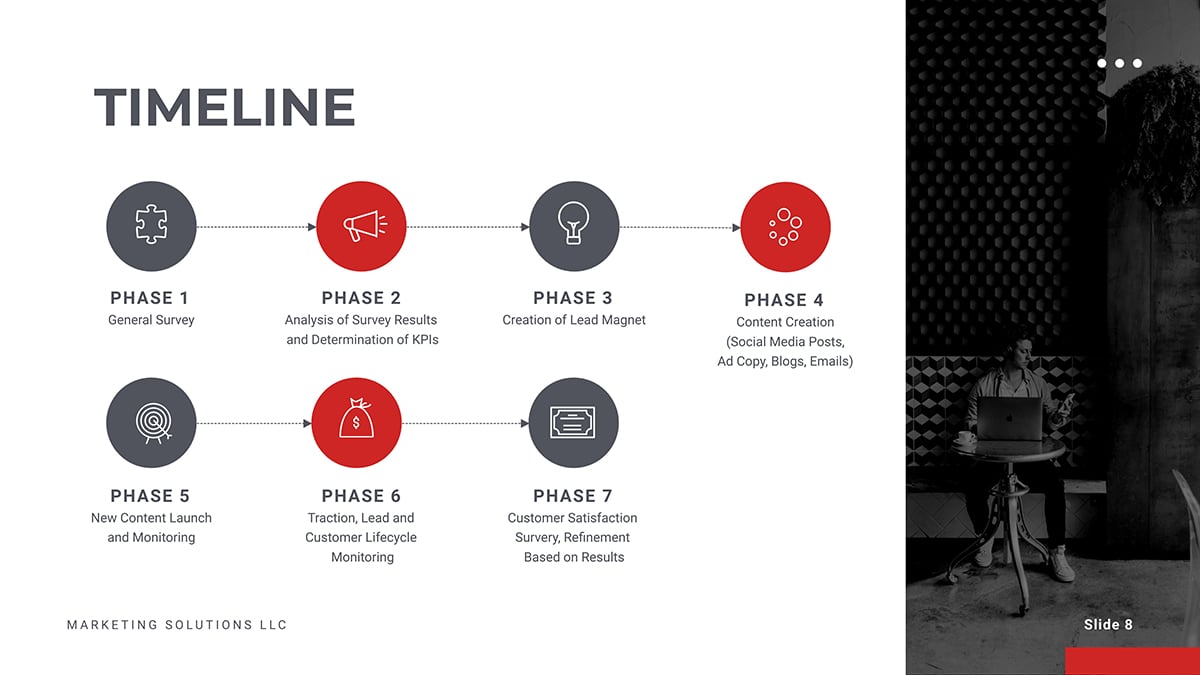
To give your team a better understanding, you can communicate your project goals in a variety of ways, including:
- Visuals (videos, images, charts, infographics, etc.)
- Verbal presentation
- Documentations
By doing that, you’re sure to get their valuable feedback, buy-in and commitment to the project. Plus, getting your team on board with your project plan will up your chances of successful execution.
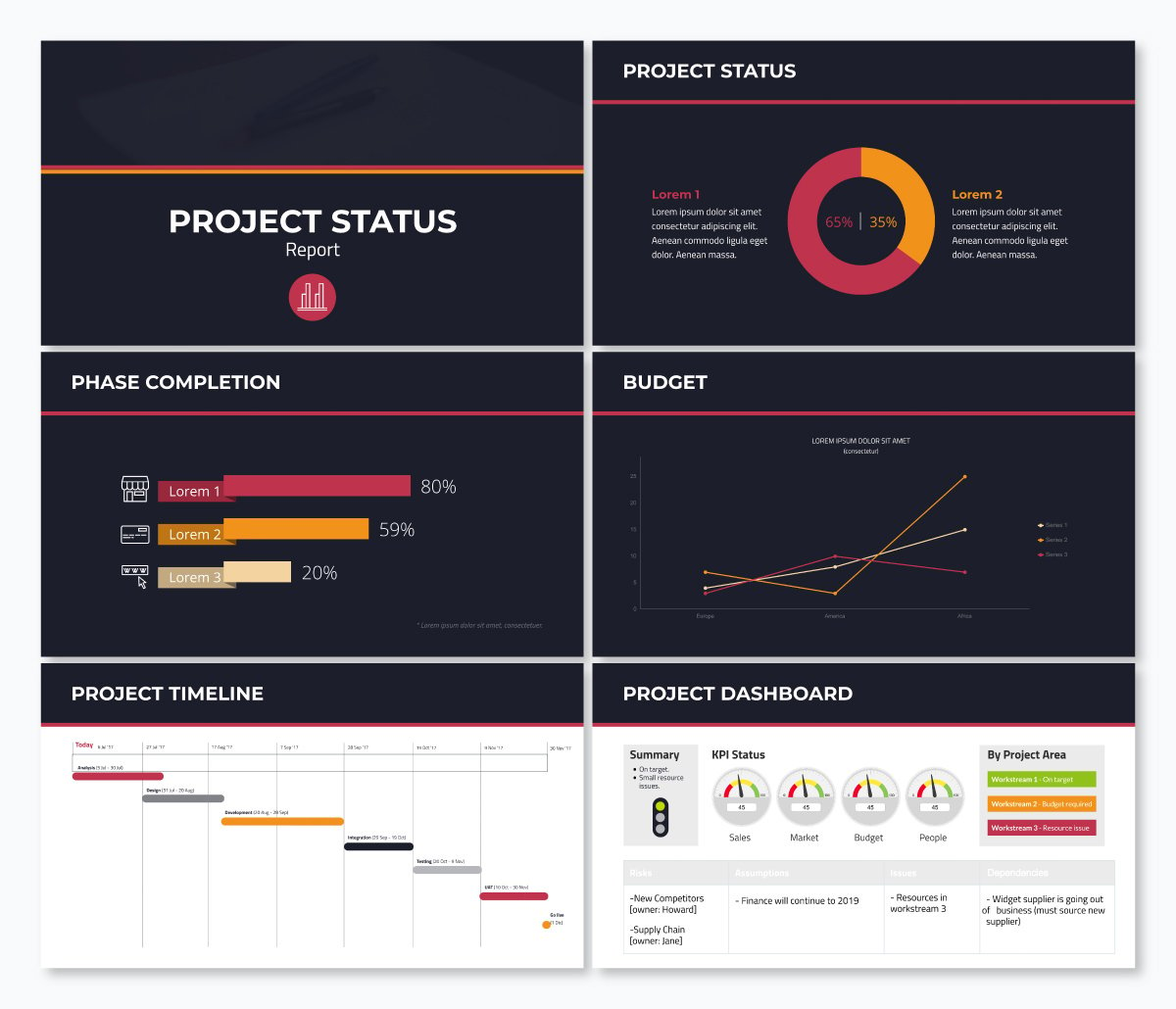
2 Lay Out Your Project Plan
Once you’ve set your goals, the next big step is to outline how you'll achieve them. An excellent place to start is by organizing your project into an actionable plan and steps for execution.
You might wonder why this step is important for creating a successful project presentation.
Whether you’re planning a small or big project, writing a detailed plan, structure and layout puts everything into perspective. It eliminates vagueness and helps your audience grasp the project roadmap without missing the points.
Your project plan should contain the technical and non-technical project details. Therefore, you want to give yourself an edge by using a project presentation template that clearly explains all the activities and steps.
Not only that, your presentation structure should be simple and easy to follow.
Depending on the project type, your plan could include key details such as:
- The goals and objectives you've outlined earlier
- Your project scope, methodology and framework
- Project milestones, deliverable and acceptance criteria
- Project schedule and timelines
- Resources and budget estimates, etc.
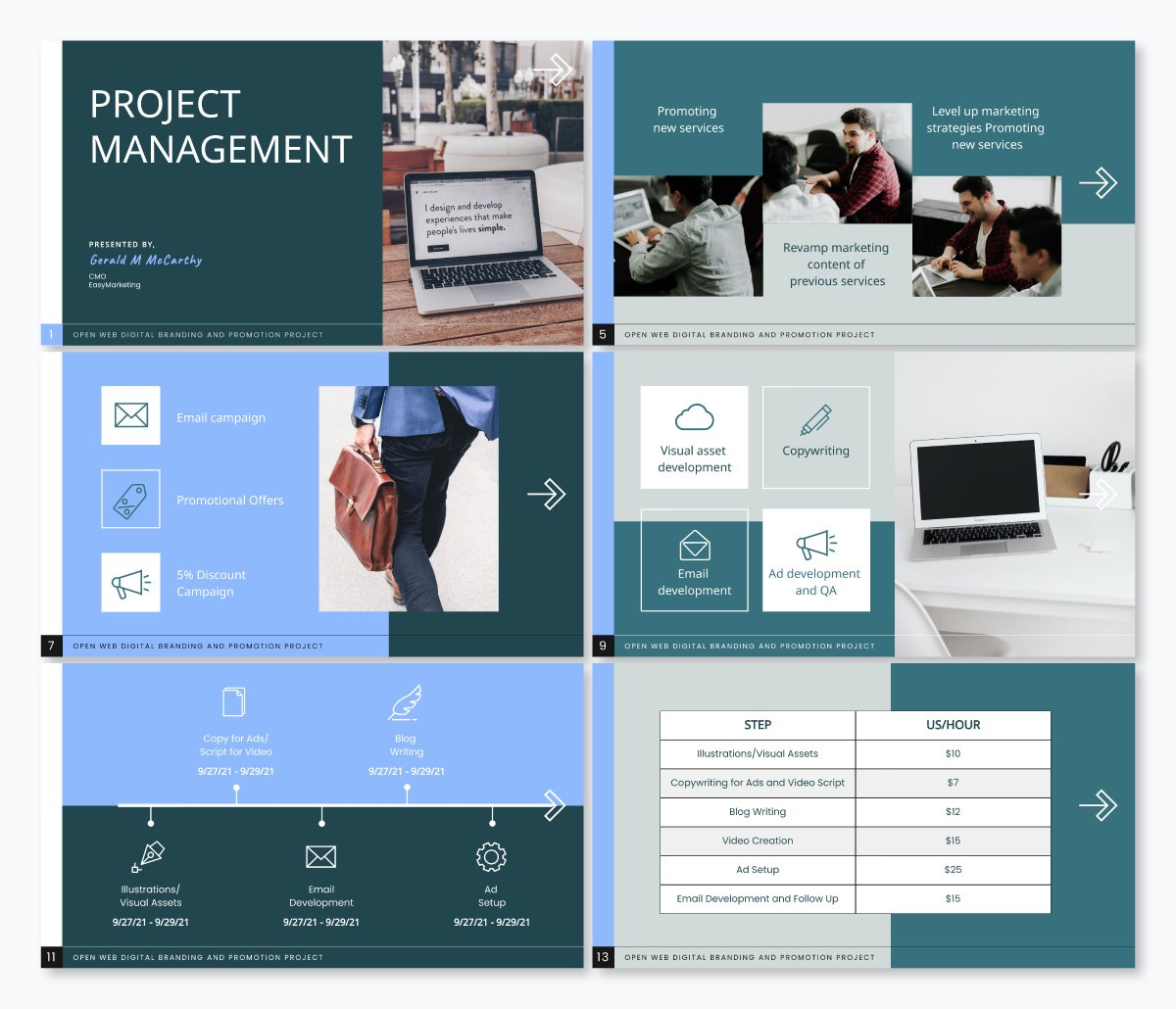
There's no hard and fast rule for laying out your project plan. However, if you want to create a memorable plan that will keep your audience engaged, you could break it down into three parts, including:
Introduction
- Conclusion and key takeaways
Your introduction should provide a brief overview of what you’re going to talk about and why it’s relevant to your audience. You could start by writing down the project name and the executive summary.
Think of your executive summary as an abridged version of the project plan.
If your audience read only your executive summary, would they have all the information they need about your project? If the answer is yes, your executive summary has served its purpose.
The length of your executive summary will depend on what you intend to cover in your project plan. However, we recommend keeping your executive summary one or two pages long.
You can include key information such as:
- Objectives of the project
- Key points of the project plan
- Results, conclusions and project recommendations
Keep in mind that not everyone will have the time to dive into the details of your project plan.
Having a snapshot of your project brings clarity to key stakeholders and collaborators. It also enables people who aren't actively involved in the project to understand it at a glance.
Ready to create your own presentation in minutes?
- Add your own text, images and more
- Customize colors, fonts and everything else
- Choose from hundreds of slide designs and templates
- Add interactive buttons and animations
The body of your project plan is where you have the full project details and everything relevant to its success.
Here you can break your project into deliverables, tasks, milestones and schedules (start and end dates).
Ensure you precisely define the resources you need to complete the project, including finances, team, time, technology, physical resources and more.
This is the part where you sum up your project plan with key takeaways. Your conclusion should include what you expect from your audience, including key action points and next steps.
Writing your intro, body and conclusion may sound like a lot of information. But instead of writing multiple pages of text, incorporating visuals can make your project presentations more effective.
By using images, videos, infographics and charts , you can capture all the vital information and help your audience understand your message better.
Visme presentation templates are effective for visualizing different sections of your project plan. They are professionally designed and easy for anyone to craft high-quality project plans that keep their team on track.
Use the project plan templates below to kickstart your project planning process.

3 Outline the Problem and Solution
You've just spent time crafting your project action plan. Now it’s time to communicate your project plan and goals with your audience.
Project presentations are a lot like sales pitches. Whether you’re presenting your project plan to clients or creating a pitch deck for investors, your job is to keep your audience hooked right from the start till the end.
One of the most potent ways of grabbing your audience's attention is by highlighting their pain points.
It’s not enough to have beautiful slides that showcase your amazing product features and project activities.
Make sure you set up your project presentation to:
- Outline your audience pain points
- Emphasize how your project, product or service works to address their pain points
- Explain how they’ll benefit from using your product or investing in your project
In a nutshell, your audience should have a clear insight into how your project makes their life better. When they’re clear on this, they’ll most likely listen to the solutions you bring to the table and take the desired action.
Don’t make sweeping assumptions about your audience.
If you’re looking to get them on board, dedicate a slide to discuss their problems and solutions. Make them understand how your project benefits them.
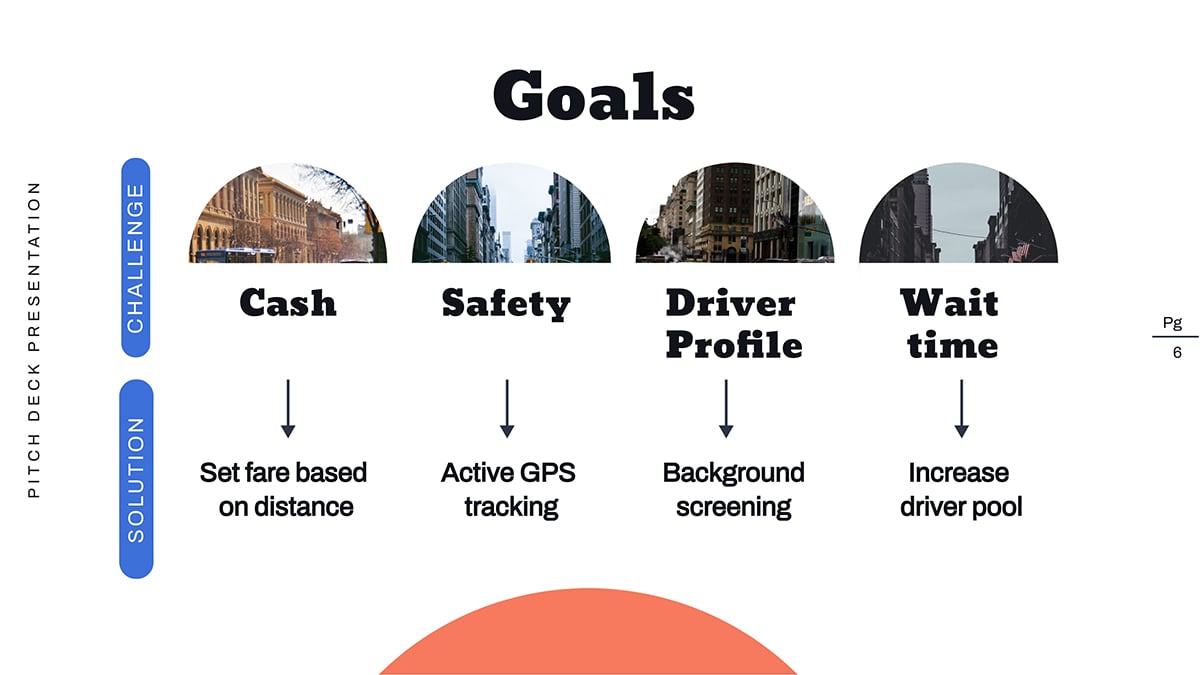
Not sure what your audience's pain points are? Go ahead and do these things:
- Run a persona survey or interview existing customers. This will help you build a data-driven user persona that you can use for all types of business and marketing decisions.
- Talk to your customer support and success team. They have close relationships with your customers, so they know their challenges and what they want. If they don’t know these things, do them a favor and create a customer success program .
- Interact with your community, ask for feedback and involvement. The more you engage with your consumers, the more you understand their challenges, work toward solving and get them invested in your brand.
- Keeping an eye on relevant social media trends, Twitter hashtags, Facebook trends
- Join relevant online forums like Quora, Reddit, Stack Exchange, etc.
RELATED: How to Write an Effective Presentation Outline
4 Keep Your Presentation Slides Short
When creating project presentations, prioritize quality over quantity. Be sure to keep your slides short and simple. When you do this, your audience will be glad you value their time.
Remember, this isn’t the time to slam your audience with lengthy and irrelevant jargon. Instead, keep your slides on topics and hit the main points without the boring and unnecessary details.
Here’s why you need to keep your presentation brief:
- Concise presentation slides are not only powerful, but they are also memorable.
- Studies have shown that during project or business presentations, attention levels drop sharply after 30 minutes . By creating lengthy presentations, you risk losing your audience's attention halfway.
- Nobody wants to sit and watch you flip tons of slides for hours. With shorter slides, you can capture your audience's attention and get them to focus on the message.
- Most people might have limited time or have short attention spans. So they’d want to quickly digest information and move on to the next best thing.
How do you keep your project presentations short?
- If your slide doesn’t add value to your presentation, it shouldn’t earn a spot on your deck.
- Supercharge your slide deck with captivating visuals that capture more information
- Adopt proven methods for preparing your slide
For example, the 10/20/30 rule by Guy Kawasaki is one of the most popular methods used by experts. The rule recommends using ten slides for 20 minutes presentations (about two minutes per slide). It also specifies using a font size of at least 30 for text.
This will enable your audience to digest the messages on your screen while you’re talking.
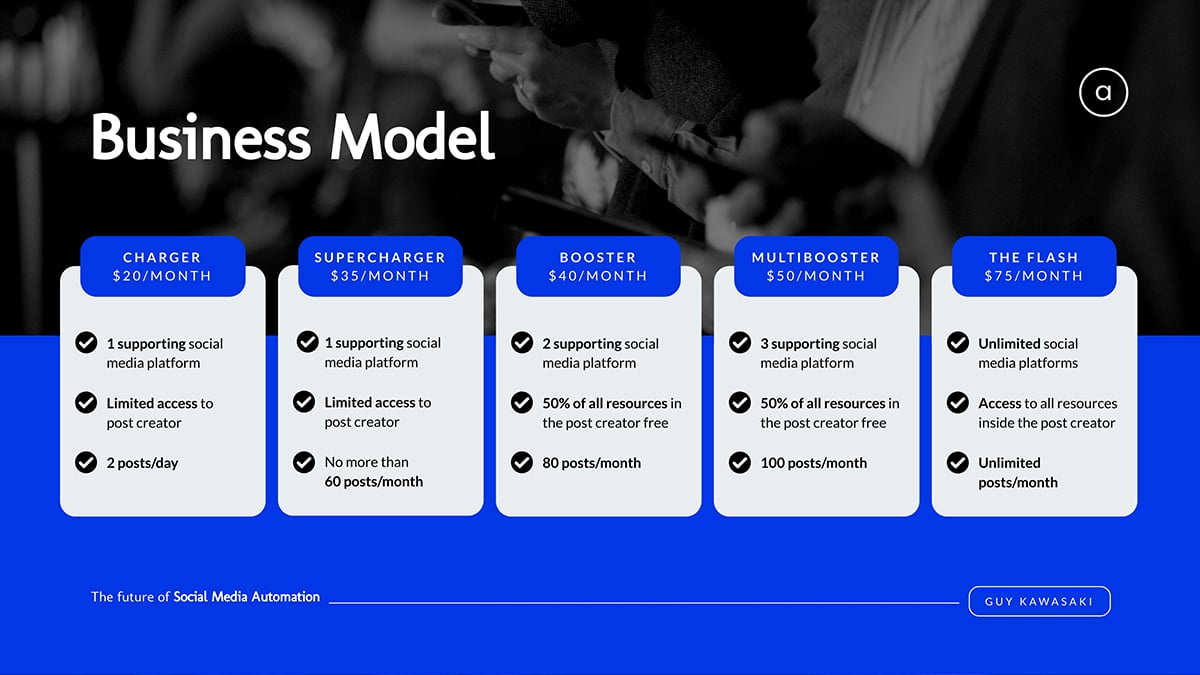
Keep in mind that this isn’t an iron-clad rule for presentation. There are other rules such as Pecha Kucha method , Takahashi method, Lessig method, etc. You can adapt any of these rules to suit your project presentation needs.
5 Use Less Text and More Visuals
Another great way to keep your slides brief yet interesting is using less text and more visuals.
Remember, your slide should aid your verbal presentation and not replace it. So you want to avoid crowding too much information on one slide.
Cluttering your presentation with too much text could:
- Overwhelm your audiences and bore them
- Shift your audience's attention to the text, making your presentation less effective.
Instead, use one slide to present each idea. Marketing guru Seth Godin recommends no more than six words per slide .
People retain more information when it’s presented in bite-size chunks and visuals. This applies to B2B, B2C audiences, project managers and corporate executives.
About 59% of business executives say they’d rather watch a video about a topic than read about it. Hence the need to supercharge your project presentation with compelling visuals that capture and bring your audience’s attention right where you want it.
Steve Jobs’ MacWorld Keynote presentation in 2007 is an excellent example of how to enhance your presentation with compelling visuals.

During the presentation, Steve Jobs used live and interactive visuals to show how the iPhone 1 works.
Read on to learn more tips on creating engaging presentations that will wow your audience.
With Visme's presentation maker , you can make stunning project presentations with a rich blend of text and compelling visuals. Hook your audience and inspire action with stellar project presentation templates like the one below.

6 Use Quality Visuals, Diagrams and Presentation Aids
Visuals are important for making successful project presentations. Beyond grabbing the audience’s attention and keeping them engaged, viewers recall 95% of a message when presented in visual form. But when shared via text, they retain only about 10%.
There are many types of visual aids you can use in your presentations, including:
- Graphs and charts
- Heat and choropleth maps
- Scatter plots
- Screenshots and more
Using images and videos will up your chances of getting audience engagements and positive responses to your call-to-action (CTA).
Gantt charts , whiteboard drawings and mind maps are ideal for visualizing early-stage project designs. You can use charts, diagrams, maps and trees to present the project architecture for technology-related projects.
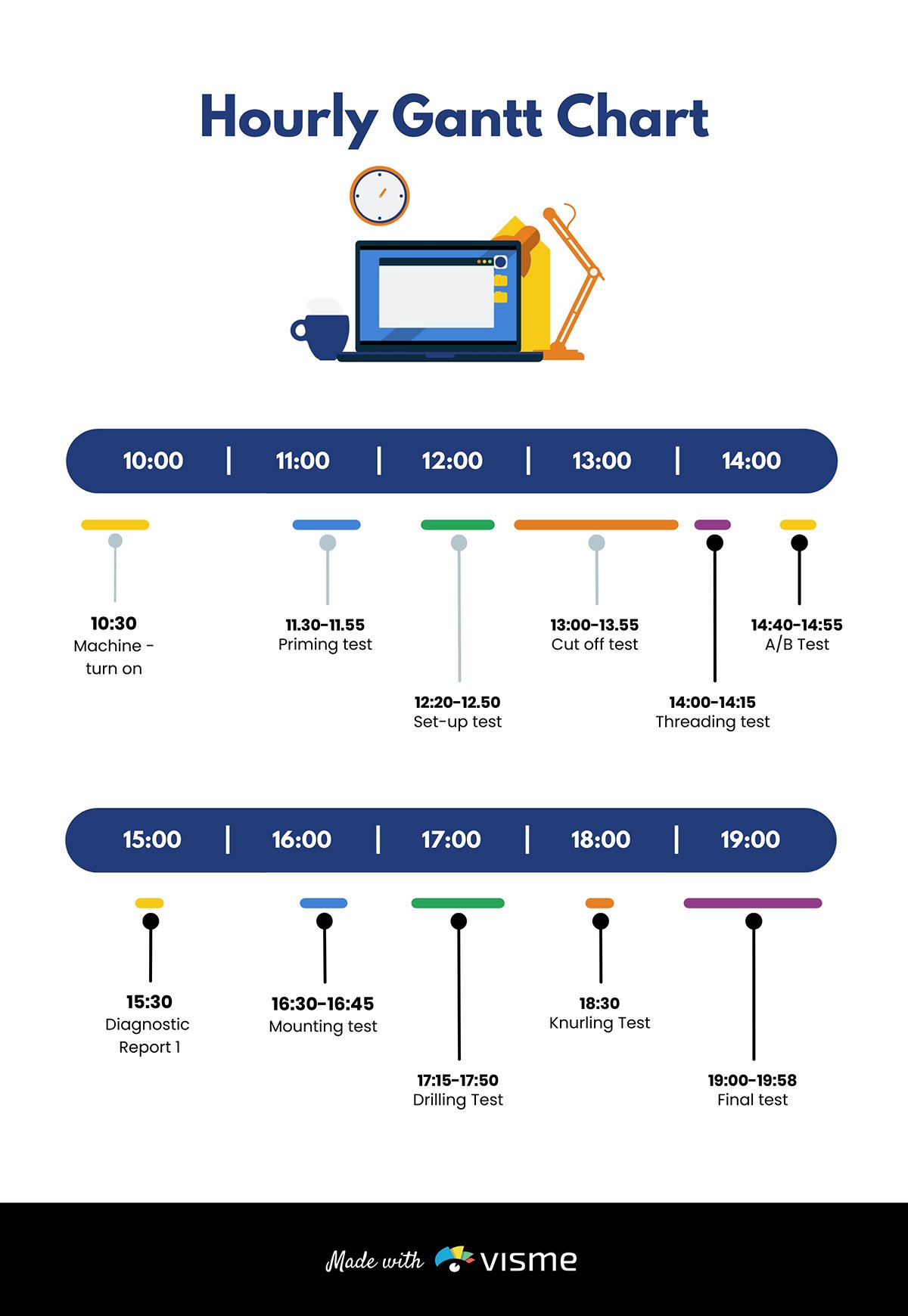
If you’re working on product development projects, consider adding sketches, flowcharts , models and prototypes to your slide.
Pie charts are excellent for showing percentages. Vertical bar charts indicate changes over time, while horizontal bar charts help you compare quantities.
Infographics are perfect for visualizing data and explaining complex information like market trends.
Here’s the interesting part. Visme has the tools you need for every job. The software allows you to add different visuals, infographics, charts and graphs to your deck and customize them to suit your needs.
You can change design, text and background colors, add or remove legends, animate charts, etc.
You can also use maps to represent geographic information. Or, use progress bars, thermometers, radials and widgets to visualize stats and figures as shown in the template below.

When adding visuals to your slide, don’t go overboard. Stick to a minimum of two images per slide. In addition, make sure your visuals are relevant to your project presentation.
While designing your presentation slides , always stick to high-quality visuals. Blurry or low-resolution images or videos can be a major turn-off for viewers.
With high-quality visuals, your presentations will be crisp and clear, even on large screens.
The slide below is an excellent example of how to power your presentations with compelling visuals.
7 Pay Attention to Design
Want to create impressive presentations that pop? If the answer is yes, you need to pay attention to your design details. Your design can make or break your project presentation.
Whether you are an experienced designer or a novice, design tools like Visme give you an edge. You can create compelling presentation designs for your business in a few minutes.
The beautiful thing is that you don’t have to break the bank to make stunning project presentations. You'll find beautiful ready-made templates and millions of stunning royalty-free images for your slides.
Here are tips you should consider while designing your slides.
Use the Right Color Combination
If you want to make your presentations appealing, use color moderately.
We get it; everyone loves color. But using too many colors can make your presentations look chaotic and unpleasant.
Your color choice can influence how your audience grasps and responds to your presentation. A general rule of thumb is to pick colors that evoke positive emotions in your audience.
For example, warm colors like yellow, orange and red convey feelings of excitement and positivity. On the other hand, cool colors (blue, green and violet) reflect an aura of calmness.
When combining colors, aim for a balanced color scheme. For example, if your slide or image background is dark, your text and design elements should have bright colors. This contrast will make your project presentation legible and visually appealing.
You can learn about color psychology and how to use it in your next presentation design by watching the video below.

Use Clear and Consistent Typography
Optimizing your typography can make a difference in how people perceive your message. So you want to make sure your slide looks organized, professional and sends the right message.
Here’s how you can make this happen:
- Use fonts that embody the spirit of your brand
- Keep your text styles consistent throughout your presentation. We recommend you stick to a maximum of three fonts.
- Avoid fancy fonts and tiny text that strain the reader's eyes. Rather use fonts like Arial, Time News Roman, Calibri and other legible fonts suited for small and large screens.
- Use a font size of at least 30 for the body text and 36 for titles.
In addition, remember to present your text using the color scheme we mentioned earlier. This will keep your text visible over your background.
Take a look at this slide from one of our presentation templates. Notice how the design, fonts and color combination blends in to make the visuals pop.
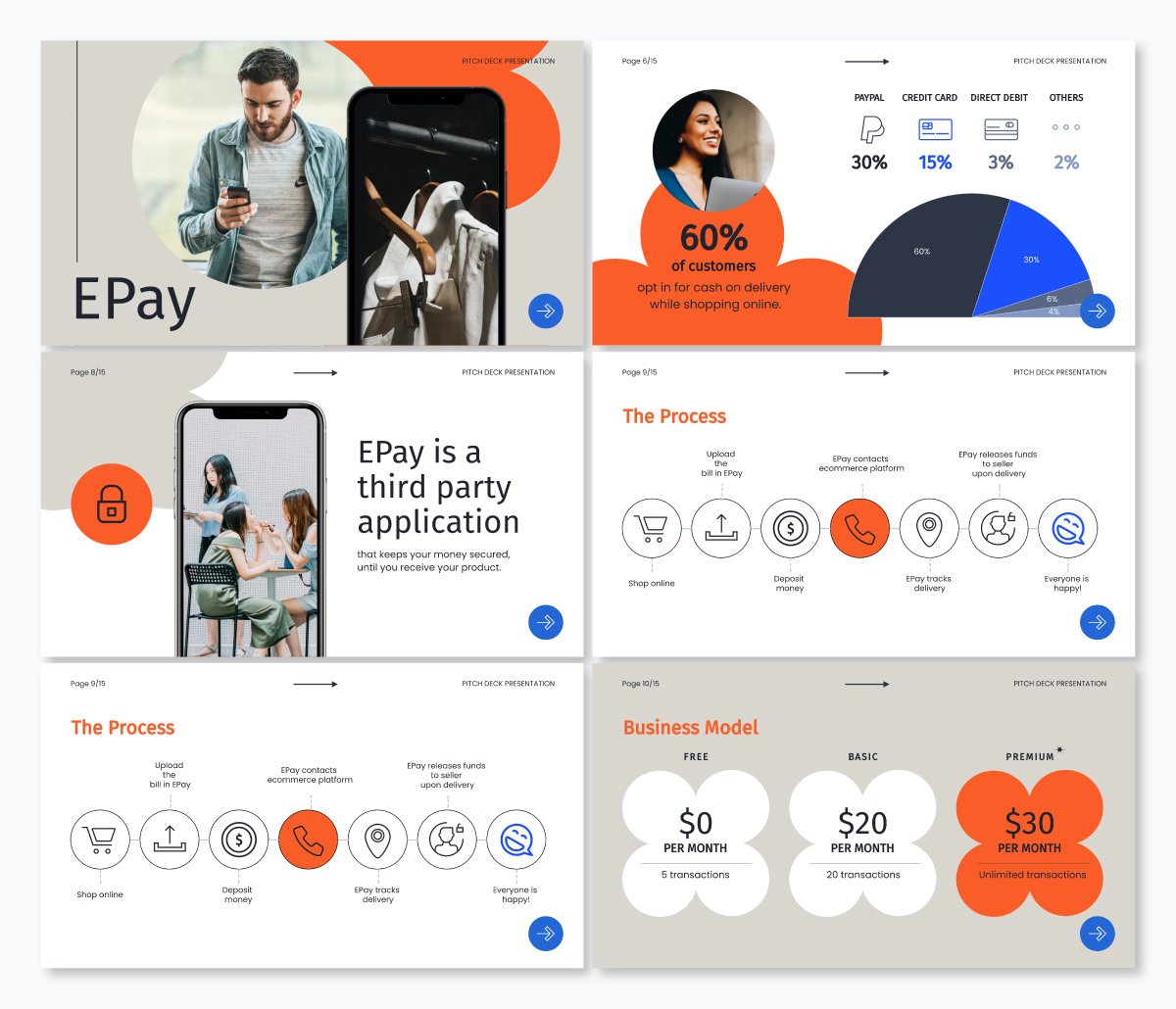
8 Start With a Presentation Template
Whether you’re a newbie or pro, creating project presentations that pack a punch can be time-consuming.
Let’s say you’ve got a deadline looming. You’d have to deal with writing your project outline, preparing your slide notes, designing your slides, sourcing and incorporating visuals and more.
Handling these things from scratch could slow you down or make your presentations untidy.
Using presentation templates could save you from all the stress. They help you make professional-looking project presentations fast and easy.
Since the slides are pre-designed, you’ll find a place to insert every possible piece of content you need. Be it a progress bar, chart, graph, table, video or image, the design is right there.
All you need to do is type your content, input data or insert the image. And boom, your presentation is ready to go.
In addition, using presentation templates offers brand consistency in terms of font, style, layout, colors and overall design. You can customize and share templates with your project team to keep your presentations uniform.
The title and main body slide, image and chart layout and fonts are set in the template. Therefore formatting your slide becomes a breeze—no more messy or cluttered project presentations.
Visme has a wide selection of templates designed to make your presentations shine. You’ll find millions of pixel-perfect graphics, icons, design elements and professionally designed templates for any purpose, industry and project type.
Regardless of your skill level, you can customize your templates like the one below. Just add your content and your project presentations will be ready in a few minutes.

9 Present Your Project Like a Pro
If you follow all the tips we shared above, you’ve probably got the perfect project presentation on paper. Great stuff, but your job isn’t done yet.
Your delivery is the final piece of the puzzle, and you’ve got to make it count.
Here’s the thing. Your presentation could flop if the delivery isn’t convincing. Hence the need to plan your delivery and drive your message across with passion and enthusiasm.
Here's how to deliver project presentations that leave an impact.
Practice Makes Perfect
Did you know that Steve Jobs used to spend two days prepping for presentations? Yes, you read that right.
Practice is one of the key steps to nailing your delivery.
You can practice by reading out loud in your quiet space. While you’re at it, make audio and video recordings and watch them repeatedly.
Ask your friends and colleagues to serve as a test audience and give feedback on your presentation.
This run-through will help ensure your presentation captures the main points within the allotted time. It will also help you maintain the correct body posture during your project presentation.
Make time to check if the equipment is working and get familiar with the settings and operations. This is especially important if you plan to use video or audio in your slides.
Start With a Strong Opening
Your audiences could have short attention spans, so make those first moments count. With solid openings, you can hook your audience and set the mood for a successful presentation.
Steve Jobs’ 2005 Stanford commencement speech at Stanford is an excellent example of having a solid opening. With over 4 million views on YouTube, it’s one of the most memorable and watched speeches in history.

Notice how he hooks the audience with powerful anecdotes about his life, beginning from dropping out of college. And then, he goes on to share the lessons he learned in his early days at Apple, losing his job in 1985 and reflections on death.
Here’s how to make an excellent opening speech that grabs the audience’s attention and convinces them you’re worth listening to:
- Ask a question
- Tell a compelling story
- Share mind-blowing facts and statistics
- Show captivating video and visuals that spark curiosity
- Open your presentation with humor
Be sure to tailor your opening hook to your audience. To make this effective, it’d help to know about your audiences, including their likes, dislikes, cultural and ethical dispositions, etc.
If you want to learn more about making captivating presentation openings and more, read our guide on starting a presentation .
While presenting your project, focus on your audience’s needs. By doing this, you’ll build an emotional connection and drive action.
However, don’t go overboard. Be genuine and focus on getting the points across to them. This way, you’ll gain their trust and build excitement about your project.
Keep in mind that everything may not go as planned. It’s best to have backup materials and be flexible enough to make necessary adjustments. Preparing for unexpected events will give you more control over them.
End Your Presentation on a High Note
After you've delivered a fantastic presentation, make sure you wrap it up in a memorable way. Doing this will leave a lasting impression and nudge your audiences to take action.
One way to end your project presentation is to use a powerful call to action.
You can also tell memorable stories, summarize the main points and highlight compelling figures about the project.
For example you can mention some really intriguing figures like:
- Expected growth rate, return on investment and profit margin
- Potential company valuation in the next five to ten years.
- Projected earnings and market position etc.
The goal is to hype your audiences and stimulate them to take action.
You can check out our other article to learn more about ending your presentation on a great note.
Get To Work: Create Powerful Project Presentations With Visme
Creating a successful project presentation starts with setting your goals and having a clear plan to achieve them. It also requires crafting compelling content, paying attention to design and excellent delivery.
If you’re going to close those deals, you need a solid pitch deck to explain your project details and why it will succeed. We recommend using an intuitive project presentation software like Visme .
Visme is the perfect design tool for creating stunning and engaging project presentations . With Visme, you’ll have access to a wide range of features and tools to help bring your project ideas to life.
The tool has hundreds of presentation templates, design elements, font styles, built-in stock images and videos, data visualization tools and more to make your project presentation a hit. You can download your design in different formats and share it across multiple social media channels.
Now you have all the tips and tools for nailing your next project presentations. Go ahead and make it memorable with Visme's project presentation software.
Create beautiful presentations faster with Visme.

Trusted by leading brands
Recommended content for you:

Create Stunning Content!
Design visual brand experiences for your business whether you are a seasoned designer or a total novice.
About the Author
Unenabasi is a content expert with many years of experience in digital marketing, business development, and strategy. He loves to help brands tell stories that drive engagement, growth, and competitive advantage. He’s adept at creating compelling content on lifestyle, marketing, business, e-commerce, and technology. When he’s not taking the content world by storm, Unenabasi enjoys playing or watching soccer.

- THE WEEK TV
- ENTERTAINMENT
- WEB STORIES
- JOBS AND CAREER
- Home Home -->
- News News -->
- India India -->
Kolkata doctor's rape-murder: As it happened at court today as protesters give probe team ultimatum
A team of the CBI and CFSL visited RG Kar Medical College and Hospital today

The Calcutta High Court, while hearing multiple petitions related to the alleged rape and murder case of a medical student at the RG Kar Medical College and Hospital, observed that the police’s role when the victim was found dead and eventually during the investigation was questionable.
The lawyer of the victim’s parents appealed that “if the State police is permitted to continue the investigation, in all probabilities, the investigation will be derailed”, a feeling shared by protesting students.
ALSO READ | Medical services affected, patients suffer as doctors continue protests
Prime facie noting that no significant process has been made by the local police which has “not arrested any other person, who may be allegedly involved in the commission of the offence”, the Calcutta High Court bench of Chief Justice T.S. Sivagnanam and Justice Hiranmay Bhattacharya gave CBI the charge of investigation and asked the central agency to file progress reports periodically before the court.
The court also recorded that the then principal of RG Kar Medical College and Hospital, Dr. Sandip Ghosh did not do his duty as the principal of the institution. The court noted, “This, in our view, was a clear dereliction of duty on the part of the Principal and the officers under his command and this has led to various repercussions and it has been admitted by the authorities that the situation became chaotic and Rapid Action Force had to be brought in.”
ALSO READ | BJP alleges bid to tamper evidence; CBI team arrives at KG Kar Hospital
A day after the court asked the CBI to take charge of the investigation of the case, the central agency began its probe on Wednesday. The accused in the case, a civic volunteer who was in custody of the local police, was handed over to the CBI after his medical examination at the IPGME&R and SSKM Hospital. The CBI then took him to the Central Government-run ESIC Hospital for another round of medical.
A team of the CBI and CFSL (Central Forensic Science Laboratory) then visited RG Kar Medical College and Hospital at around 3:45 pm. They carried on their investigation at the chest medicine department, where the victim’s dead body was found in the early hours of Friday last week.
Meanwhile, students and doctors are continuing with their protests in front of the main gate of the hospital. They are hopeful of an impartial investigation by the central agency but say they will not end their movement unless all culprits are arrested and convicted.
They are raising slogan, “Aamar didir bichar chai (We want justice for our sister).”
ALSO READ | NHRC takes suo motu case, issues notice to DGP, chief secretary
They gave an ultimatum on Wednesday to the investigating agency to arrest all the culprits within the next 48 hours. They also demanded that local police officials involved in the initial investigation must also be probed. Protesters also want adequate security and protection of doctors in every hospital and medical institutes.
The inner parts of the campus, however, wear an eerie calmness with confusion and fright palpable on the face of students. They fear that the RG Kar Medical College and Hospital authorities might be destroying evidence.
“We heard that authorities are renovating some rooms next to the seminar hall where the victim was found dead. Why do they need to do the renovation work right now,” asked Dr. Aniket Mahato of the anaesthesia department at RG Kar Medical College and Hospital.
The same issue was flagged by the head of the department, Dr. Arunabha Dutta Chowdhury of the chest medicine department. He said he didn’t give any permission for construction works. Dr. Dutta Chowdhury also expressed his solidarity with the students’ movement.
He said, “I support their protest. The person who died was like my daughter. I joined as the HOD only on August 1 and on August 8 she died. I feel so helpless that I couldn’t save her.” However, the students are also demanding his resignation.
A delegation of Indian Medical Association, including its all-India president Dr. RV Asokan also visited the protesting student. Expressing their solidarity towards the students’ cause, the IMA President said, “IMA is your second home. I will take your message across India. We want security of hospitals at par with airports.”
Doctors and medical students are also continuing their protests in other government-run medical colleges and hospitals across West Bengal. The Joint Platform for Doctors, West Bengal, had called for a strike in non-emergency departments in all government and private hospitals.
Meanwhile, multiple rallies, including by the BJP, Congress and by civil society members, were taken out in different parts of Kolkata. A rally by medical representatives also visited RG Kar Medical College and Hospital to show their support for the movement.
On Wednesday night, women from all sections of society are planning to gather under the banner of ‘Reclaim The Night’ in more than 80 locations across West Bengal and in other cities of India as well. The idea behind the gathering will be to assert their right to move freely and securely during night.
- West Bengal
Join our WhatsApp Channel to get the latest news, exclusives and videos on WhatsApp

IDF says it came 'minutes away' from catching Yahya Sinawar: 'The coffee was still hot'

No Olympic silver medal for Vinesh Phogat, CAS dismisses wrestler's plea against disqualification

'Double iSmart' review and release updates: Ram Pothineni gives glimpses of what the film is all about

Will US recession fears have an effect on Indian IT sector?

Explained: Why is ISRO's third developmental flight SSLV-D3 unique?
Editor's pick.

A lesson from Bangladesh: Intimidating students is a recipe for disaster

From food concierge services to in-kitchen dining, culinary experiences get interactive

Meet the youngest person to skydive solo with a prosthetic leg

Evolving luxury
*Articles appearing as INFOCUS/THE WEEK FOCUS are marketing initiatives

- < Previous Event
- Next Event >
Home > USC Upstate > University Centers > SARS > SCURS > 2024symposium > 2024PRESENTATIONS > 18
Full Breakout Session Schedule
Four Examples of Healthcare Chatbots
Presenter Information
William L. Eldridge Mr. , University of South Carolina - Spartanburg Follow Uma Gupta Mrs. , University of South Carolina - Spartanburg Follow
12-4-2024 4:00 PM
Document Type
Presentation
William Eldridge
Research Symposium Abstract
Healthcare is an important industry. Without healthcare, we would not be able to have any medical support. Today chatbots play a very important role in healthcare. They are responsible for many tasks from scheduling pensions appointments, to managing patient files, and even helping to train healthcare professionals. In this abstract, I will go over four of the most popular chatbots in healthcare. The first healthcare chatbot I will go over is Babylon Health. Babylon Health is an “AI-driven chatbot that was designed to check for symptoms and give a possible diagnosis to patients” (chatGPT). Since its introduction to healthcare Babylon Health has greatly reduced the workload on healthcare professionals, which frees up time for them to help other patients who are in more need of their assistance. The next chatbot is Ada Health. Ada Health What's the sign for the same purpose as Babylon Health in that it was “designed to check the symptoms of patients and give a diagnosis” (chatGPT). Also, like Babylon Health it works in the same way in that, “it will ask the patient serious questions and based on the responses they will provide a possible course of action to take” (chatGPT). It has also had the same impact on healthcare that Babylon Health has had. The third chatbot is Woebot. Unlike the previous two, Woebot was designed “to provide mental health services such as therapy” (chatGPT). It performs this task by “giving the patient an empathetic response” (chatGPT). Woebot has provided mental health assistance to many people around the US and has also reduced the workload on many therapists around the US. The final chatbot is Florence. Florence is designed to “act as a personal assistant for healthcare providers and users for medical management and health tracking” (chatGPT). Through Florence, healthcare has become more efficient and is better able to manage its time and resources which allows healthcare to provide better care to patients. There are many other chatbots used in health care these are just some examples. Overall chatbots have greatly improved healthcare by making it more efficient allowing healthcare to provide better care to patients.
This document is currently not available here.
Since April 01, 2024
Symposium Links
- Scope & Purpose
- Policies & Agreements
- Register to Attend
- Keynote & Brief Schedule
- Map & Directions
Submissions
Advanced Search
- Notify me via email or RSS
- Collections
- Disciplines
- Access, Use and Removal Policy
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
- Sports Betting
- Sports Entertainment
- New York Giants
- New York Jets
- Transactions
Recommended
Giants’ malik nabers has ‘no doubt’ he’ll be ready for week 1 after ankle scare.
Fear not, Giants fans, Malik Nabers has “no doubt” he’ll be ready in time to play in the season opener.
The rookie wide receiver admitted Tuesday that he initially believed the left ankle sprain he sustained Sunday was worse than it turned out to be.
Nabers said he was “feeling good” and “absolutely” relieved when X-rays and an MRI showed it’s “nothing too serious,” and he hopes to be back on the practice field well ahead of what would be his NFL debut in the Giants’ Week 1 game against the Vikings on Sept. 8.

“As a football player, you’re always thinking the worst of everything if you’re not able to play,” Nabers said after doing some stretching and light jogging at the team’s practice facility. “So to hear the good news come back that it was really nothing and just was gonna take a little rehab and time, that was good to hear.”
The Giants certainly feel the same way after drafting the potential impact player with the sixth pick of this year’s draft out of LSU.
“He’s good. We’ll keep him down today. He’ll go out there and do stretch, but he’s good, he’ll be good,” head coach Brian Daboll said before practice. “It’s not long-term or anything like that. … He’s OK. He’ll be OK. It’s nothing serious.”
The Giants have time to take precaution with the 21-year-old Nabers after he limped off the practice field Sunday.

That probably means holding him out of Saturday’s preseason game in Houston, but he could play in the finale against the Jets one week later.
“It’s a game rep, so every opportunity I get, of course I want to take advantage of it, but if that’s what my coaches decide on and what I decide on, that’s what it’s gonna be,” Nabers said. “We [have been] pretty cautious just to see how I feel and make sure I’m 100 percent and can play at a high speed and at full speed.
“I’m always trying to be 100 percent healthy when I’m out there on the field. But I always want to be available to play.”

Another member of Nabers’ draft class, rookie running back Tyrone Tracy Jr. appeared to suffer a serious ankle injury after fumbling a kickoff during Tuesday’s practice.
But after leaving for an area hospital for further testing, he was back at the practice facilities and attending meetings.
“I heard about it after practice. I just heard that he went down,” Nabers said before it was revealed Tracy seems to have escaped a major injury. “It’s bad for an incoming person, coming into a new team, going down to an injury.
“I’m not sure of the injury, I just know that he went down. My prayers are gonna be out to him and I hope he has a speedy recovery so we can get him back on the field. Because he’s a pretty good back and he makes our offense better.”
Nabers certainly is expected to do that at an even greater level as the expected No. 1 wide receiver with quarterback Daniel Jones returning from knee surgery.
That expectation already has elevated the confident Nabers to one of the most important and popular players on the team before playing a single down in the NFL.
“It really ain’t hit me. I take it as just football,” Nabers said. “Whether I’m this famous person or not, if I don’t do my job at the end of the day, I’m not gonna be this praised receiver like everybody’s saying.
“It has its pros and cons, I would say. When you got a lot of attention going on, you gotta know how to handle it, know what to say and what not to say, what to do and what not to do.”
And there is one thing he needs to do, first and foremost.

“I always want to get back on the field, but like I said, being healthy and 100 percent is what I’m focused on right now,” Nabers said. “I can’t play out there with an ankle sprain, ankle injury, because if I’m not healthy, I’m not available to the team to help win games. I gotta make sure that I’m as healthy as possible.”

Advertisement

IMAGES
COMMENTS
Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you've described the story in an accurate way. ... In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the ...
The opening statement of an oral presentations differs from a written H&P in that the oral presentation usually begins with some basic demographics and reads more like the first line of the HPI than a written H&P, which begins with a chief complaint. Do: Give basic demographics and a few items of past medical history that are relevant to the
The ability to deliver oral case presentations is a core skill for any physician. Effective oral case presentations help facilitate information transfer among physicians and are essential to delivering quality patient care. Oral case presentations are also a key component of how medical students and residents are assessed during their training.
After building up the background, address how you arrived at your research question. The most exciting part of your presentation should be explaining your conclusions and the path you took to get there. Finish up strong by discussing the implications of your findings and how they will have an impact in the field.
Here's how to create an effective and engaging medical presentation — without wasting hours on PowerPoint! Simple is better. Be wise with your color choice. Don't overcrowd slides with text. Give your audience time to process.
Delivery. It is important to dress appropriately, stand up straight, and project your voice towards the back of the room. Practise using a microphone, or any other presentation aids, in advance. If you don't have your own presenting style, think of the style of inspirational scientific speakers you have seen and imitate it.
An easy way to do this is by using the 5×5 rule. This means using no more than 5 bullet points per slide, with no more than 5 words per bullet point. It is also good to break up the text-heavy slides with ones including diagrams or graphs. This can also help to convey your results in a more visual and easy-to-understand way.
The ability to design and deliver an effective presentation is an important skill for all learners to develop. The Undergraduate Medical Education Section of the Group on Educational Affairs developed this toolkit as a resource for medical students and health professions trainees as you learn to create and give effective presentations in the classroom, in the clinical setting, and at academic ...
In medical presentations, lots of PowerPoints are still used, and it can be your friend, but it can often be your enemy. ... The other important point is the organization of your presentation. An audience will give us somewhere between 5 and 30 seconds before they make a judgment of us and our material, and if you don't hook them, out come the ...
0 shares Share0 Share +10 Tweet0 Pin0 Share0 About Medical PresentationsMedical presentations are fundamentally different from other presentation types. In fact, they are one of the toughest type of presentations to design.Medical slides have research facts, data charts, diagrams and illustrations that demand a totally different approach to design. You need a slide creation method […]
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it.
Background: This systematic review aimed to extract recommendations from expert opinion articles on how to give a medical research presentation on a scientific conference and to determine whether the experts agree on what makes an effective or poor presentation. Methods: Presentation-related terms were searched within article titles listed in PubMed, restricting the search to English-language ...
Medical presentations are a helpful tool for medical professionals, research clinics, and organizations to help inform and educate their communities on a wide variety of urgent topics. ... Give your audience a minute or two following the presentation to process what they learned, and then give them a chance to ask questions. You may need to ...
3 types of medical presentations (and how to give them) Here are some tips for presenting the top three types of medical presentations: lectures, research presentations, and case reports. With your long to-do list as a medical professional, giving presentations is probably not a high priority. Yet, medical presentations are inevitable.
Step 2: Crop and enlarge your images. The next step is the extension of the first one. We recommend using one picture per slide and enlarging it if it contains tiny elements. For example, you want to show a cataract, so increase the image in size for all people to see clearly.
7 Ingredients for a Patient Case Presentation Template. 1. The One-Liner. The one-liner is a succinct sentence that primes your listeners to the patient. A typical format is: " [Patient name] is a [age] year-old [gender] with past medical history of [X] presenting with [Y]. 2.
You've heard tips on how to give a great oral presentation, but it's hard to put tips into context without seeing examples. Here's an example of a pretty goo...
In medical school, you're not taught how to give stellar patient presentations. Yes, you're shown the traditional order of things: "Give an effective one-liner first, then tell the HPI [history of present illness] but only give pertinent info, etc." Just exactly how to deliver the punch that impresses your attending is an art.
Follow the 10-20-30 rule and your presentation will be brilliant. 10. Your medical presentation should only have 10 slides to ensure that there is not too much information, that the line of the speech is easy to follow, and that only the essentials are included. At the very maximum, you should only show 15 slides.
Medical presentations should be created from the audience's rather than the presenter's perspective. Medical presentations should follow a solution logic rather than a research logic. The ...
3. Start with a statistic. Give doctors a reason to listen to the rest of your presentation. Rather than asking them to blindly trust you before you get to the proof of your facts, start off with that proof. Deliver a relevant statistic that illuminates the importance of your entire presentation. The data you offer will provide a black and ...
Don't just give a presentation — share a story. It must be a story-audience fit though. Use the P.A.S. — problem-agitation-solution — approach. Start with introducing a problem, follow by ...
Residents and medical students who are considering careers in surgery have many incredible career options. See why surgeons from three different disciplines love their areas of practice. This video features: Nikolaus Sneshkoff, MD, FACS, otolaryngologist; Gaby Iskander, MD, MS, acute care surgeon; Vineet Choudhry, MD, FACS, general surgeon
During the presentation, Steve Jobs used live and interactive visuals to show how the iPhone 1 works. Read on to learn more tips on creating engaging presentations that will wow your audience. With Visme's presentation maker, you can make stunning project presentations with a rich blend of text and compelling visuals. Hook your audience and ...
Kolkata doctor rape and murder: The Calcutta High Court, while hearing multiple petitions related to the alleged rape and murder case of a medical student at the RG Kar Medical College and Hospital, observed that the police's role when the victim was found dead and eventually during the investigation was questionable.
Matthew Peters, a spokesman for Nashville's Metro Department of Health — which oversees the School Health Division — says the full extent of the law's impact remains to be seen.
William Eldridge Research Symposium Abstract Four Examples of Healthcare Chatbots Healthcare is an important industry. Without healthcare, we would not be able to have any medical support. Today chatbots play a very important role in healthcare. They are responsible for many tasks from scheduling pensions appointments, to managing patient files, and even helping to train healthcare professionals.
Fear not, Giants fans, Malik Nabers has "no doubt" he'll be ready in time to play in the season opener. The rookie wide receiver admitted Tuesday that he initially believed the left ankle ...