Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article

University students’ strategies of coping with stress during the coronavirus pandemic: Data from Poland
Contributed equally to this work with: Anna Babicka-Wirkus, Lukasz Wirkus, Krzysztof Stasiak, Paweł Kozłowski
Roles Conceptualization, Formal analysis, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute of Pedagogy, Pomeranian University in Słupsk, Słupsk, Poland
Roles Conceptualization, Data curation, Investigation, Project administration, Resources, Software, Writing – original draft, Writing – review & editing
Affiliation Institute of Pedagogy, Faculty of Social Science, University of Gdańsk, Gdańsk, Poland
Roles Investigation, Resources, Software, Supervision, Writing – review & editing
Affiliation Department of Material Criminal Law and Criminology, Faculty of Law and Administration, University of Gdańsk, Gdańsk, Poland
Roles Data curation, Software, Validation, Writing – review & editing
- Anna Babicka-Wirkus,
- Lukasz Wirkus,
- Krzysztof Stasiak,
- Paweł Kozłowski

- Published: July 26, 2021
- https://doi.org/10.1371/journal.pone.0255041
- Reader Comments
The COVID-19 pandemic has changed the functioning of universities worldwide. In Poland, the transfer to online teaching was announced without prior warning, which radically changed students’ daily functioning. This situation clearly showed the students’ helplessness and difficulties with coping with this new, stressful situation, highlighted in many previous studies. A sudden and far-reaching change in daily functioning caused anxiety, depression, and stress in this group. Thus, from a pedagogical and psychological point of view, it is pertinent to examine the students’ strategies of coping with stress caused by the COVID-19 pandemic. To this end, in 2020, a sample of Polish students was anonymously measured using the Mini-COPE questionnaire. Data was gathered from 577 students from 17 universities. The statistical analysis showed that during the coronavirus pandemic, Polish students most often used the coping strategies of: acceptance, planning, and seeking emotional support. Such factors as age, gender, and place of residence influenced the choice of specific strategies of coping with stress during the COVID-19 pandemic. The results also showed that the youngest students had the lowest coping skills. The results allow for concluding that the students’ maladaptive strategies of coping with stress, especially during the pandemic, may result in long-term consequences for their psychophysiological health and academic achievements. Thus, based on the current results and on the participatory model of intervention, a support program for students is proposed which would involve psychological, organizational, and instrumental support.
Citation: Babicka-Wirkus A, Wirkus L, Stasiak K, Kozłowski P (2021) University students’ strategies of coping with stress during the coronavirus pandemic: Data from Poland. PLoS ONE 16(7): e0255041. https://doi.org/10.1371/journal.pone.0255041
Editor: Shah Md Atiqul Haq, Shahjalal University of Science and Technology, BANGLADESH
Received: March 24, 2021; Accepted: July 9, 2021; Published: July 26, 2021
Copyright: © 2021 Babicka-Wirkus et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: The author(s) received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
University studies are a stressful period as they mean the transition to independent, adult life. Beginning studies can be stressful to many students, since it means the necessity to establish new relationships, develop new studying habits related to the chosen program, cope with overwork, learn time management, and often also change one’s place of residence [ 1 , 2 ]. In its later stages, university education is related to new, further stressors, such as concern over being able to find employment after graduation. Studies thus far show that many students struggle to cope with these stressors and that the incidence of stress among students is increasing [ 3 , 4 ]. Among other consequences, it has a negative impact on mental health [ 2 , 5 ]. In the US, around 10% of university students reported suffering from depression [ 2 ], and this proportion has increased to 15% since 2000 [ 6 – 9 ]. A significant causal factor behind this increase is the stress related to studying.
Stress is undoubtedly a part of students’ lives and it may impact their ways of coping with the demands of university life. Their daily responsibilities involve numerous challenges which lead to stress [ 10 ]. Results from various studies carried out thus far show a clear increase in mental health problems among students [ 11 ]. As some of them indicate, there is also an urgent need to assess the impact of the current pandemic on students’ mental health and wellbeing [ 12 ], which legitimizes carrying out such studies in various countries, including Poland.
In 2020, a new situation appeared which necessitates a different approach to stress and its causal factors–the SARS-CoV-2 virus. Data published by the Johns Hopkins University indicates that thus far, over 100 million people have become infected with COVID-19, and around 2.5 million have died [ 13 ]. The COVID-19 disease affects everyone, including students [ 14 , 15 ], since even those who have not been infected are subject to various restrictions which many countries have implemented to limit the spread of the disease. The reality of the pandemic has also negatively impacted the students’ quality of social life. Studying at a university is also a period of establishing new relationships and intense social life. This is facilitated by the fact that young people exhibit greater levels of extraversion and openness to experience than do older people [ 16 ]. Studies show that contacts with others positively influence quality of life [ 17 ]. Lack of regular contact with friends throughout all phases of the coronavirus pandemic, results in loneliness, which might not be fully mitigated by regular contacts via telephone or other means [ 18 ]. These conclusions are supported by evidence from studies carried out in Great Britain (with participants aged between 13 and 25 years), in which young people reported having lost support, daily routine, social ties, and experiencing anxiety, loneliness, and loss of motivation and aim. Higher incidence of depression and anxiety, both during as well as after periods of social isolation, was also confirmed [ 19 , 20 ]. This may lead to harmful social and psychological consequences [ 21 – 23 ].
In response to the pandemic, most countries have implemented severe restrictions in societal functioning which comprise many spheres of life: social, economic, cultural, and educational. They led to limited interpersonal contacts, changes in the mode of education (online teaching), and reduced economic activity. As a result, an economic recession has affected nearly all countries (including Poland) [ 24 ], which worsened the material conditions of many people (increased unemployment). This significantly impacts students, as it intensifies their concerns about being able to find or retain a job and thus support themselves during their studies and after graduation. Essen and Owusu showed that work and studies are the most frequent causes of stress for students [ 25 ]. Historical data shows that previous pandemics have negatively impacted young people’s material conditions, which had long-term consequences for their physical and mental health as well as academic achievement [ 26 ]. For many students, COVID-19 has additionally complicated their current plans and changed their mode of functioning.
More recently, Matthew H. E. M. Browning et al. identified a range of psychological consequences of the COVID-19 pandemic on students’ psychosocial functioning. All students in the sample indicated that the pandemic impacted them negatively, with 59% reporting a high level of psychological impact [ 27 ]. Other studies on the effects of the pandemic on student mental health also show greater stress, anxiety, depression symptoms, concerns for own and one’s family’s health, reduced social interactions, and increased concerns over academic achievements. Students try to cope with stress, seek support from others, and prefer either negative or positive coping strategies [ 11 , 28 ].
The COVID-19 situation, its rapid spread, insufficient preparation, and significant changes in everyday functioning, including university culture, may contribute to increased stress among students. When not managed properly, chronic stress leads to emotional and psychosomatic consequences which manifest through physical, cognitive, and emotional exhaustion as well as depersonalization and lowered professional–in case of students, academic–efficiency [ 29 ]. The consequences of stress lower efficiency, productivity, and engagement in life activities as well as the satisfaction with their results [ 30 , 31 ]. As Adler and Park point out, effective coping with stress might buffer the impact of stressful events on the physical and mental health, and individuals differ with regards to the coping strategies they use [ 32 ]. Therefore, the aims of the study were: identifying the students’ dominant strategies of coping with stress in the pandemic situation, assessing the influence of sociodemographic factors on the dominant coping strategies, and diagnosing differences in the students’ coping strategies depending on expected social support and its sources.
The stress and coping concept is the most popular study approach, also explaining the mechanisms mediating between personality and disease. Currently, the transactional model of stress by Lazarus and Folkman [ 33 ] is employed increasingly frequently. It posits mutual interactions between people and their environment. This model served as the theoretical basis of the current study. The perception of stress is a subjective and variable phenomenon. Particular attention is paid to the processes of coping with stress, which decide the positive and negative impact of stress on the individual. Using different strategies of coping with stress involves mobilizing cognitive and behavioral resources to meet the demands which are subjectively perceived as surpassing personal capabilities. The course of the coping process depends on personal resources and social support. It can also lead to various behaviors which have negative health effects (substance use) or are maladaptive [ 34 ]. Also, according to Lazarus and Folkman, coping with stress might be related to negative health behaviors [ 35 ]. Metzger et al. analyzed the frequency of negative health behaviors among students. They found that increased alcohol consumption and risky sexual behaviors are typical for people at risk for significant stress [ 36 ]. Styles of coping with stress are determined by gender, education, age, health, well-being, the nature of the stressful situation, personality factors, and others [ 20 ]. Efficient use of emotions allows for more effective problem solving, while venting anger and frustration and denial of reality are potentially destructive reactions to stress [ 37 ]. Expressing emotions might also lead to lower depression and hostility levels in stressful situations [ 38 ]. Some authors distinguish between emotion-focused and problem-focused coping styles, while others distinguish active and avoidant coping or identify maladaptive coping strategies (denial, substance use, venting of negative emotions) which allow for lowering subjectively experienced stress [ 39 – 41 ].
Research questions
The study concerned students’ strategies of coping with stress during the pandemic. The following research questions were put forward:
- What strategies of coping with stress are most often used by students during the coronavirus pandemic?
- What is the relationship between sociodemographic variables and the dominant coping strategies among students?
- How does anticipated support differentiate the coping strategies used by students?
Study population and procedure
In 2019, 1.230 million students studied at around 400 universities in Poland. Sixty-five percent were full-time students. Seventy-three percent studied at public (national) universities. The number of foreign students is relatively low in Poland, being only 61 thousand in 2019. Moreover, a decisive majority—around 60%—of students in Poland are women [ 42 , 43 ]. This proportion reaches 65% for MA studies. Meanwhile, in the EU in general, women comprise around 54% of students [ 44 ].
In early spring of 2020, soon after online teaching was instituted, the questionnaire was distributed to students of four randomly chosen Polish universities. Those students who filled out the online questionnaire were also asked to share it with their acquaintances from other universities. Using snowball sampling method was determined by difficulties in reaching students directly, as well as by their reluctance, especially in the first phase of the pandemic in Poland, to take part in studies and fill out online questionnaires. Having students to invite their acquaintances to also take part in the study allowed for gathering a relatively large sample in a short time. There were no missing data, since the online platform did not allow for submitting incomplete questionnaires.
Participation in the study was voluntary. Informed written consent was obtained from every participant. Before participants started to fill out the online study questionnaire, they had to read the information about the project and its aims and checked the option ’I agree to take part in the study’. The data were analyzed anonymously. The research project and its procedure were approved by the Commission of Bioethics and Human Rights.
Using the snowball sampling method, data from 17 Polish institutions was obtained: universities, technical universities, medical universities, and higher vocational schools. This allowed for measuring coping strategies during the pandemic among students from various universities in various regions of Poland. However, it has to be noted that snowball sampling does not allow for generalizing the results to the entire student population in Poland. Nevertheless, based on the obtained data, certain trends in coping strategies among social sciences students can be shown.
The study took place in April-May 2020. Five hundred and seventy-seven complete questionnaires were collected. Table 1 shows the demographic characteristics of the sample divided by universities.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0255041.t001
The data was divided into six groups based on the number of students from each given university who took part in the study. The largest group were the students from the University of Gdańsk (UG). Next, the sample comprised students from: Adam Mickiewicz University in Poznań (UAM) - 22.2%, University of Warsaw (UW) - 17.2%, Jan Kochanowski University of Kielce (UJK- 13.7%, and Pomeranian University in Słupsk (5.9%). Due to a low number of students from other universities, an additional group (different universities—DU) was created, which comprised 6.0% of the total sample.
Polish universities vary with respect to their size and educational profile. There are relatively few large universities with over 20 thousand people (roughly 20 out of 400). Most universities are of medium or small size. The largest university in Poland is the University of Warsaw. It also has one of the broadest selections of programs. A characteristic aspect of Polish universities is that they offer specific educational profiles, for example, universities focusing on medical education. Another example is the Pomeranian University, which specializes in teaching education. Table 2 shows basic characteristics of universities which were widely represented in the research sample [ 45 – 50 ].
https://doi.org/10.1371/journal.pone.0255041.t002
In the current study, women represented 89.6% of the sample. Participants between 21 and 24 years of age and those living in large cities represented the largest group (59.5% and 36.7%, respectively) Over 80% of the participants were full-time students, which reflected the general population distribution of students in Poland [ 51 ]. Undergraduate students also represented a larger group.
The multidimensional COPE inventory by Carver et al [ 52 , 53 ] is one of the most popular measures of strategies of coping with stress. It can be used to measure dispositional (typical) and situational coping. The Mini-COPE inventory in a Polish adaptation by Juczyński and Ogińska-Bulik [ 54 ] was used in the current study. The internal consistency of the Polish version of the Mini-COPE was estimated based on a sample of 200 people aged between 25 and 60. The split-half reliability was 0.86 (Guttman’s coefficient = 0.87). The repeatability was satisfactory for the majority of the scales. The Polish version of the Mini-COPE comprises 28 items, which form 14 coping strategies. It is used to measure typical reactions in situations of intense stress. The main question is: What do you usually do when you are stressed by a problem? The coping strategies are described in statements such as “I work or do other things in order not to think about the problem.” Each statement is graded on a four-point Likert scale: 1 = very seldom, 2 = fairly seldom, 3 = fairly often, 4 = very often. Each of the 14 coping strategies is measured by two items.
The Mini-COPE inventory was supplemented with two other semi-open questions. The first concerned the type of support the students expected during the pandemic. The available answers were: psychological, emotional, financial, organizational support, no support needed, and other (to be filled out by the students if necessary). The second supplemental question concerned the sources from which the students expected support during the pandemic. In this case, the students could select the closest appropriate answer from among: family, friends, the university, the government, and other (to be filled out by the students if necessary). Fig 1 shows the distribution of the students’ answers to the supplementary questions about support.
https://doi.org/10.1371/journal.pone.0255041.g001
Regarding the source of support, 5.0% of the students chose “other.” This category comprised the following answers: significant other (0.9%), nobody (1.2%), psychologist/therapist (0.5%), myself (1.4%), all of the above (0.3%), and other combinations indicating two sources, for example, family and the government (0.7%).
Statistical analyses were carried out using the IBM SPSS Statistics 25.0 software. The program was used to calculate basic descriptive statistics together with the Kolmogorov-Smirnov test of normality. Additionally, the Cronbach’s α coefficient was used to calculate the reliability of the Mini-COPE scales. To compare coping strategies between two groups, Mann-Whitney’s U test was used. To compare a higher number of groups, a one-way analysis of variance (ANOVA) was used, and if variance was not equal between the groups, Welch’s correction was additionally applied. Tukey’s HSD test (if variance was homogenous) or Dunnett’s T3 test (if variance was heterogenous) was used for post hoc analyses. To estimate intergroup differences in coping strategies, Pearson’s r correlation analysis was carried out. The significance level was set at α = 0.05. In order to distinguish the groups of participants in terms of coping strategies, a two-step cluster analysis was carried out.
Students’ dominant strategies of coping with stress during the pandemic
Based on the descriptive statistics and the results of the Kolmogorov-Smirnov test of normality, it was concluded that neither of the analyzed variables assumed a distribution close to the Gaussian curve. Skewness values were within the <-2;2> range, which means that it was not significant [ 55 ]. Additionally, the Cronbach’s α coefficient was used to calculate the reliability of the Mini-COPE scales. The analysis showed satisfactory reliability for most of the scales. Relatively low reliability was obtained for the scales of acceptance, humor, self-distraction, and venting of emotions. Detailed results are shown in Table 3 .
https://doi.org/10.1371/journal.pone.0255041.t003
The dominant coping strategies among Polish students were: acceptance, planning, and seeking emotional support. The least frequent strategies were: substance use, denial, behavioral disengagement, and religious coping.
Pearson’s correlation analysis was used to examine the relationships between individual coping strategies in the current sample ( Table 4 ). Active coping was positively correlated with the following coping strategies: planning (strong correlation), positive reframing, religious coping, emotional support seeking, instrumental support seeking, self-distraction, venting of emotions, and self-blame (weak correlations). The higher the frequency of active coping, the higher the frequencies of the above strategies as well. Active coping was moderately and negatively correlated with behavioral disengagement, which means that the higher the frequency of active coping, the lower the frequency of behavioral disengagement.
https://doi.org/10.1371/journal.pone.0255041.t004
Another coping strategy—planning—was positively and weakly-to-moderately correlated with positive reframing, acceptance, religious coping, emotional support seeking, instrumental support seeking, self-distraction, and self-blame. A weak, negative correlation occurred between planning and denial, and a moderate one between behavioral activation—the higher the frequency of planning, the lower the frequency of denial and behavioral disengagement.
Positive reframing was positively and weakly-to-moderately correlated with acceptance, humor, religious coping, emotional support seeking, instrumental support seeking, and self-distraction. This coping strategy was also weakly and negatively correlated with behavioral disengagement and self-blame.
Acceptance was weakly and positively correlated with humor and negatively with denial, behavioral disengagement, and self-blame. In turn, humor was weakly and positively correlated with emotional support seeking, self-distraction, and substance use. A weak and positive correlation also occurred between religious coping and emotional support seeking, instrumental support seeking, and venting of emotions. Religious coping was also weakly and negatively correlated with substance use.
Another strategy—emotional support seeking—was strongly and positively correlated with instrumental support seeking. A weak and positive correlation occurred between the following coping strategies: self-distraction and venting of emotions. Emotional support seeking was weakly and negatively correlated with behavioral disengagement.
On the other hand, seeking instrumental support was weakly-to-moderately and positively correlated with self-distraction, venting of emotions, and self-blame.
Self-distraction was weakly-to-moderately and positively correlated with denial, venting of emotions, substance use, behavioral disengagement, and self-blame.
Denial, venting of emotions, substance use, behavioral disengagement, and self-blame were positively correlated with each other on a weak-to-moderate level (the relationship between behavioral disengagement and self-blame).
The remaining correlations between the coping strategies were not statistically significant.
Students’ strategies of coping with stress–cluster analysis
To distinguish groups of participants based on their coping strategies, a two-step cluster analysis was carried out. It allowed for distinguishing two clusters ( Fig 2 ) for which the silhouette value was 0.2, indicating a satisfactory quality of clustering. From among the coping strategies included in the model, the most important ones were: seeking instrumental support, seeking emotional support, and planning. These strategies differentiated the two clusters to the highest degree. The least important strategies were substance use, denial, and self-blame.
https://doi.org/10.1371/journal.pone.0255041.g002
Table 5 shows the comparison of the clusters with regard to the analyzed strategies. The analysis showed no statistically significant differences for denial, substance use, and self-blame. Differences for other coping strategies were statistically significant, with Cluster 1 participants scoring higher on active coping, planning, positive reframing, humor, religious coping, seeking emotional and instrumental support, self-distraction, and venting of emotions, and lower on behavioral disengagement compared to Cluster 2 participants.
https://doi.org/10.1371/journal.pone.0255041.t005
Sociodemographic factors and strategies of coping with stress
To estimate the gender differences in coping strategies, Mann-Whitney’s U test was used. The analysis showed statistically significant gender differences for humor, emotional support seeking, instrumental support seeking, self-distraction, denial, and venting of emotions. Men in the current sample reported using humor significantly more often than women, but they reported using religious coping, emotional support seeking, instrumental support seeking, self-distraction, and denial less frequently. The results of the analysis are shown in Table 6 .
https://doi.org/10.1371/journal.pone.0255041.t006
Gender differences could result from differences in gender role socialization [ 56 , 57 ]. Women are socialized to be more emotional and seek support in interpersonal relationships. On the other hand, men are socialized to cope with their problems on their own or use humor.
Using a one-way analysis of variance (ANOVA), coping strategy use was compared between age groups ( Table 7 ). The analysis showed statistically significant differences for six strategies: active coping, planning, positive reframing, venting of emotions, behavioral disengagement, and self-blame. To estimate the character of the intergroup differences, an additional post hoc analysis using Tukey’s HSD test was carried out when the variance was equal between the groups, and Dunnett’s T3 test, when the variance was unequal. This type of post hoc analysis was used due to the disproportions in the size of the compared groups. In the case of unequal variances, the Welch correction was also applied.
https://doi.org/10.1371/journal.pone.0255041.t007
18-20-year-olds reported statistically significantly less frequent active coping than did 25-30-year-olds ( p = 0.032) and those 31 and over ( p = 0.032). The youngest participants also reported less frequent planning than did 25-30-year-olds ( p = 0.039) and those 31 and over ( p = 0.045), while 21-24-year-olds reported significantly less frequent planning than 25-30-year-olds ( p = 0.015) and those 31 and over ( p = 0.030). The coping strategy of positive reframing was more frequent in the oldest group compared to the younger groups (p ≤ 0.013). Those 31 and over also reported significantly less frequent venting of emotions compared to 18-20-year-olds ( p = 0.007) and 21-24-year-olds ( p = 0.002). Behavioral disengagement differed significantly between the youngest and the oldest group ( p = 0.014), with the higher frequency of this strategy being reported in the 18-20-year-olds group. Those 31 and over reported less frequent self-blame than did 18-20-year-olds ( p = 0.036) and 25-30-year-olds ( p = 0.019).
The current data show that the oldest students used active coping strategies more often during the pandemic than did the younger students. The aim of these strategies is to solve the problem causing difficult internal tension rather than to avoid the situation altogether. This effect may be related to the older students having greater life experience, including academic experience, at 31 years of age.
In the next step, differences in coping strategy use depending on the place of residence were examined ( Table 8 ). To this end, a one-factor ANOVA was carried out. It showed significant intergroup differences for the following coping strategies: active coping, planning, humor, religious coping, denial, and substance use. Participants living in cities with over 100 thousand residents reported using planning significantly more often than those living in villages ( p < 0.001) or towns up to 20 thousand residents ( p = 0.006).
https://doi.org/10.1371/journal.pone.0255041.t008
Participants living in towns up to 20 thousand residents reported using humor significantly less frequently than those living in cities with over 100 thousand residents ( p = 0.021). Participants living in villages reported using religious coping significantly more often than those living in cities with over 100 thousand residents ( p = 0.004). This is related to a more traditional upbringing and culture in Polish rural regions, where religious rituals play a significant role. Participants living in cities with over 100 thousand residents reported using denial significantly less frequently than those living in villages ( p = 0.002) and in towns with between 20 and 100 thousand residents ( p = 0.034). Substance use was reported more frequently among participants living in biggest cities compared to participants living in villages ( p = 0.002). This is because various psychoactive substances are more easily available in large cities.
After the correction for multiple comparisons was applied, a post hoc analysis using Tukey’s HSD test did not reveal statistically significant intergroup differences in active coping.
To compare full-time and extramural students’ use of coping strategies, Mann-Whitney’s U test was used. It showed that extramural students reported using active coping and positive reframing more frequently, and humor, instrumental support seeking, self-distraction, venting of emotions, substance use, and self-blame less frequently compared to full-time students. The results of the analysis are presented in Table 9 .
https://doi.org/10.1371/journal.pone.0255041.t009
Using a one-factor ANOVA, coping strategies were compared between students in different program years. The analysis showed significant differences for four strategies: active coping ( Fig 3 ), planning ( Fig 4 ), positive reframing ( Fig 5 ), and behavioral disengagement ( Fig 6 ).
I U–I Undergraduate (n = 142), II U–II Undergraduate (n = 100), III U–III Undergraduate (n = 104), I G–I Graduate (n = 66), II G–II Graduate (n = 70), I-III M–I-III uniform Master’s studies (n = 64), IV-V M–IV-V uniform Master’s studies (n = 31).
https://doi.org/10.1371/journal.pone.0255041.g003
https://doi.org/10.1371/journal.pone.0255041.g004
* Welch’s correction was applied.
https://doi.org/10.1371/journal.pone.0255041.g005
https://doi.org/10.1371/journal.pone.0255041.g006
A detailed post hoc analysis showed that first year undergraduate students reported using active coping less frequently compared to second year graduate students ( p = 0.048), first-third year uniform Master’s students ( p = 0.009), and fourth-fifth year uniform Master’s students ( p < 0.001). Second year undergraduate students also reported using active coping less frequently than did fourth-fifth year uniform Master’s students ( p = 0.001), similar to third year undergraduate students ( p = 0.004). First year undergraduate students reported using planning less frequently compared to second year graduate students ( p = 0.006) and fourth-fifth year uniform Master’s students ( p < 0.001). Fourth-fifth year uniform Master’s students reported using planning more frequently than second year ( p = 0.018) and third year ( p = 0.007) undergraduate students. A significant difference in the frequency of using behavioral disengagement occurred between first year undergraduate students and fourth-fifth year uniform Master’s students ( p = 0.015). First year undergraduate students reported using behavioral disengagement more frequently than did fourth-fifth year uniform Master’s students. For positive reframing, after applying the correction for multiple comparisons, Dunnett’s T3 test did not show statistically significant intergroup differences. A statistical trend ( p = 0.053) was observed between third year undergraduate students and first year graduate students—first year graduate students reported a slightly higher frequency of using positive reframing than did third year undergraduate students.
Students’ strategies of coping with stress and the type and source of needed social support
A one-way ANOVA was used to estimate the differences in coping strategy use depending on the need for a given type of social support ( Table 10 ). The post hoc analysis showed that participants who indicated a need for psychological support reported using the coping strategy of positive reframing less frequently than those who did not indicate any need for support ( p = 0.027). Also, those who indicated a need for financial support reported using positive reframing less frequently than those who did not indicate any need for support ( p = 0.034). Those who did not indicate any need for support used the coping strategy of acceptance more frequently than those who indicated a need for psychological ( p = 0.013) and emotional ( p = 0.002) support. This is due to the fact that these individuals cope with the pandemic-related difficulties on their own. Those who indicated a need for financial support also used religious coping less frequently than those who indicated a need for emotional support ( p = 0.007). Participants who indicated a need for emotional support reported using the coping strategy of emotional support seeking more frequently than those who indicated a need for financial support ( p = 0.004) and those who did not indicate any need for support ( p = 0.034). Analogous differences were observed for instrumental support seeking. Participants who indicated a need for emotional support reported using this coping strategy more often than did those who indicated a need for financial support ( p < 0.001) and those who did not indicate any need for support ( p = 0.001). Those who did not indicate any need for support reported using self-distraction less frequently than those who indicated needing psychological ( p = 0.014) and emotional ( p = 0.003) support. Also, participants who did not indicate any need for support reported using the coping strategy of denial less frequently than did those who indicated a need for psychological ( p = 0.002) or emotional ( p = 0.002) support. Participants who did not indicate any need for support reported using venting of emotions less frequently than did those who indicated a need for psychological ( p < 0.001) and emotional ( p < 0.001) support, whereas participants who indicated a need for financial support reported using venting of emotions less frequently than did those who indicated a need for emotional support ( p = 0.003). Participants who indicated a need for psychological support reported more frequent substance use than did those who did not indicate any need for support ( p = 0.002). Participants also used behavioral disengagement more often than did those who indicated a need for financial ( p = 0.001) and organizational support ( p = 0.001), or did not indicate any need for support ( p < 0.001). In turn, those participants who indicated a need for emotional support reported using behavioral disengagement more frequently than those who did not indicate any need for support at all ( p = 0.006).
https://doi.org/10.1371/journal.pone.0255041.t010
Participants who indicated a need for psychological support and emotional support reported using self-blame more often than did those who indicated a need for financial ( p < 0.001, p = 0.003 respectively). Self-blame is a cognitive judgment related to a belief that not making mistakes is extremely important. However, self-blame causes withdrawal from interpersonal relationships and prevents learning from one’s mistakes. Thus, normal sadness and guilt becomes transformed into depressive disorders [ 58 ]. In this case, seeking psychological support seems warranted. People seek to relieve their suffering and solve their problems through utilizing psychological consultations or therapy. However, in contrast to seeking emotional support from significant others within close relationships, individuals seeking psychological support may discount their own agency, responsibility for their decisions, and independent solution-seeking to a greater extent. Additionally, when describing the pandemic situation, it is worth to consider another context of self-blame, namely, the phenomenon of guiltless guilt, that is, guilt without any specific influence on a given situation which is the source of self-blame. This creates a vicious circle which depends psychological suffering [ 59 ].
A one-factor ANOVA also revealed significant differences between the groups distinguished by the source of expected support. These differences were significant for three coping strategies: religious coping ( Fig 7 ), substance use ( Fig 8 ), and self-blame ( Fig 9 ). A detailed post hoc analysis revealed that those participants who expected support from the government used religious coping less frequently than those who expected support from their families ( p = 0.043) or their universities ( p = 0.026). Participants who expected support from their families reported using the coping strategy of substance abuse significantly less frequently than those who expected support from their friends ( p = 0.013). In turn, participants who expected support from their friends reported using self-blame significantly more often than did those who expected support from the government ( p = 0.027).
https://doi.org/10.1371/journal.pone.0255041.g007
https://doi.org/10.1371/journal.pone.0255041.g008
https://doi.org/10.1371/journal.pone.0255041.g009
The aim of the current study was to examine the strategies of coping with stress among Polish university students during the coronavirus pandemic, as well as to assess the type of support they expected. An analysis of the empirical results allows for drawing conclusions on this topic.
The transactional model of stress [ 33 ] allowed for identifying a specific relation formed between an individual and their surroundings. The participants in the currents study found themselves in a stressful transaction in which they experienced a real risk in the form of the pandemic situation. Coping is a specific adaptative reaction chosen during the secondary appraisal. It emerges when an individual appraises the situation in terms of harm or risk, that is, as a difficulty. Students differed with respect to their tendency to use specific coping strategies, which does not mean that a given individual’s coping strategies are the same in every situation. Emotion-oriented coping strategies seek to reduce tension and unpleasant emotions which arise in reaction to stressful situations. They are unavoidable particularly when the individual has no influence on the external events. Problem-focused coping involves cognitive and behavioral efforts to reduce stress by trying to solve the problem [ 33 ]. Thus, the main condition for appropriate functioning is to develop optimal strategies of coping with stress.
The results of the current study showed that during the stressful situation of the pandemic, which can cause feelings of uncertainty and crisis [ 60 ], Polish students mainly chose such coping strategies as acceptance, planning, and seeking emotional support. The current studies showed that students more often use coping strategies which, according to Lazarus and Folkman’s theory [ 33 ] are emotion-focused (acceptance, seeking emotional support). On the other hand, planning is a problem-focused coping strategy. These three main strategies seem constructive as they direct people towards a future temporal perspective and might facilitate a reorganization of the values–goals–life plans triad driving the dynamic character of the personality [ 61 ], especially in decisive periods of personal crises [ 62 ]. It is also related to reframing one’s own life situation. Substance use, denial, behavioral disengagement, and religious coping were used the least frequently by Polish students to cope with stress during the pandemic.
Among all groups of people in education, students exhibited higher levels of emotional problems and pressure related to the changes in the educational and social situation during the pandemic than did primary and high school students [ 63 , 64 ]. Thus, it was important to assess their need for support and the sources they expect this support from. The results showed that 78% of the students needed support, while 22% did not express such needs. The greatest proportion of students—25%—needed emotional support. This type of support was mainly sought from family (38%) and friends (26%). Participants who expected emotional support simultaneously chose strategies of support seeking and religious coping. Their search for personal resources which would facilitate coping was oriented at close interpersonal relationships. They most likely allowed for conversations which supported another coping strategy preferred by this group, namely, venting and self-blame. Students seeking emotional support–in contrast to those seeking psychological support–likely maintained closer and deeper interpersonal relationships. On the other hand, psychological support was expected by 16% of the participants. They scored the lowest on the strategy of positive reframing. However, they scored higher on substance use, denial, and venting, as well as self-blame. Such a pattern of coping strategies suggests that use of professional psychological help is warranted. These participants showed such difficulties in coping with the pandemic situation that they concluded they should seek professional help from a psychologist.
Those students who expected organizational (18%) and financial (17%) support reported using different coping strategies than did those who expected emotional and psychological support. Such coping strategies as religious coping, support seeking, venting, substance use, behavioral disengagement, and self-blame were lower in this group. Rather, these participants were oriented at gaining concrete material support and support related to organizing their life in the city where they studied, and sometimes also worked to support themselves financially.
Further analyses showed that those students who indicated a need for emotional and social support reported using the coping strategies of positive reframing and acceptance of the pandemic situation less frequently. Need for emotional, organizational, and psychological support was related to typical stressors (studying, pressure to achieve high grades, pass exams, and qualify for scholarships) [ 65 , 66 ], which remained at similar levels during online teaching. However, it was also related to additional limitations stemming from the digitalization of the teaching process [ 67 ]. Moreover, the need for support was also increased by isolation, limitations in social relationships with peers, and limited possibilities for establishing new relationships and realizing affiliative needs [ 68 , 69 ]. Importantly, these needs concern direct relationships rather than telephone or online contact, as these do not fully mitigate loneliness and do not provide the same amount of support [ 18 ]. Seeking real, direct support, the students expressed a perspective of building psychological resilience and improving their emotional state, which corresponds with the results of Bernabé and Botia [ 70 ]. Students mainly expressed a need for emotional, organizational, and psychological support from their families and friends in order to maintain a high level of functioning, which might be explained through the perspective of the resilience theory [ 71 , 72 ]. This is because resilience is strongly related to, among others, perceived emotional support and close, safe relationships with one’s family and friends [ 73 , 74 ], which create networks of emotional and social support [ 75 , 76 ]. The ability to use support serves as a buffer for stress and its negative consequences. It can also prevent the deepening of the problems by providing resources for coping when stress occurs. Studies confirm that people with access to support show less reactivity to stress factors and enjoy higher mental health [ 77 ].
Next, it was showed that the chosen strategies of coping with stress were related to sociodemographic variables such as gender, age, and place of residence, which was confirmed by Cantor [ 61 ]. A detailed analysis revealed gender differences in the use of some specific coping strategies, which is also supported by other studies [ 78 – 80 ]. Women used the strategies of emotional and instrumental support seeking statistically significantly more often than did men. On the other hand, men used humor as a coping strategy more often than did women.
Regarding age, it was shown that younger people who began studying (18-20-year-olds) reported using active coping and planning statistically significantly less frequently than older students (21-24-year-olds, 25-30-year-olds, and those 31 and above). In turn, the higher frequency of using positive reframing and the lowest frequency of using venting of emotions was reported by the oldest students (31 and above). These age-related differences are difficult to relate to previous studies due to methodological differences [ 81 – 83 ]. The strategy of active coping, characteristic for older students, was positively correlated with planning (strong relationship), positive reframing, religious coping, and emotional and instrumental support seeking, which was confirmed by the cluster analysis. Cluster 1 results (statistically significantly higher active coping, planning, positive reframing, humor, religious coping, emotional and instrumental support seeking, self-distraction, and venting, and lower behavioral disengagement) correspond to this profile of active coping.
The youngest students (18–20 years old) did not choose active (adaptive) coping strategies, in contrast to the older students. It is worth noting that, as the youngest persons in the academic community, they have less life and experience and less environmental resources due to the fact that they did not yet develop close and deep social and emotional relationships. This is related to identity development [ 84 , 85 ]. Additionally, the university is a new setting for such students, which makes it more difficult for them to perceive it as a source of instrumental and organizational support. Thus, the youngest students in particular should be the recipients of complex (psychological, instrumental, possibly also spiritual) support from the university intended to shape appropriate adaptive conditions.
Comparing the full-time and extramural students with respect to their coping strategies, it was found that extramural students scored higher on active coping and positive reframing, and lower on humor, instrumental support seeking, self-distraction, venting, substance use, and self-blame compared to full-time students. It is worth noting that extramural students are usually older than full-time students. Thus, they are at a different developmental period in their lives. They often live with their own families, including their children. They attend classes only during the weekends and are most often employed and financially independent Thus, they have different areas of life activities and exhibit different strategies of coping with stress.
Analyzing the variable of place of residence, it was found that students living in cities with over 100 thousand residents used the coping strategies of planning, humor, and substance use more frequently than did students from smaller towns and villages. These results can be interpreter with reference to Bronfebrenner’s [ 86 ] ecological theory. Larger cities have more (both on the mesosystem and the exosystem levels) infrastructural resources, opportunities related to social life, and institutional offers (even during the periods of pandemic-related restrictions). Thus, people living in large cities were subjected to less social isolation during the pandemic than were the people living in rural areas. However, they used religious coping and denial less frequently, which was used more often by students living in villages. Studies on Polish students carried out before the pandemic using the Mini-COPE did not show differences in coping strategies related to place of residence.
The results of the current study allowed for the identification of coping strategies among students. This is important for the process of designing support strategies at universities. Our study also identified the mechanisms of active (adaptive) and passive (maladaptive) coping and directions of support seeking.
Taking into account the current results, future empirical studies can focus on more detailed examinations of the relationships between specific coping strategies used by students. Additional studies on the influence of the later stages of the pandemic on students’ mental health are necessary, as the consequences of this difficult situation may last for a long time, beyond the most intense period of the pandemic.
Strengths and limitations
The strengths of the current study include an examination of students’ strategies of coping with stress during the pandemic as a global situation which, to some extent, warrants the introduction of monitoring and prevention of the “post-COVID syndrome” in the context of students’ coping with stress and rebuilding social and emotional relationships.
The current results might also serve as a point of reference and comparison for further studies on coping strategies among students in other countries. In turn, this could support the development of local strategies of supporting students in organizing their academic careers and personal lives. This is especially important considering the fact that the occurrence of subsequent pandemics is only a matter of time, as was cautioned by the Director General of the World Health Organization, Tedros Adhanom Ghebreyesus. The UN resolution naming December 27 as the International Day of Epidemic Preparedness acknowledges the disproportional harm they cause in people’s lives and highlights the need for increased awareness, exchange of scientific knowledge, and searching for the best solutions on both the local and national levels. This message finds direct expression in the topic of the current study.
A limitation of the current study is the high proportion of female students of social sciences and humanities in the current sample. In Poland, these programs are more often chosen by women (73%) than men (27%) [ 87 ]. This resulted in a high gender imbalance in the current sample.
Recommendations for universities
The results of the current study lead to formulating several recommendations for universities regarding the organization of teaching in ways that consider the students’ psychosocial functioning to a greater extent. These suggestions include: implementing assessments of students’ psychosocial functioning in order to determine the potential need for emotional, social, and psychological support, and establishing psychological consultation points for students requiring such support.
It also seems warranted to introduce interpersonal training and stress coping workshops for individual student groups. Regarding organizational support, the current results are an argument for providing material support and career counseling in part-time employment for students.
The current results serve as a basis for designing a model of support and-self support solutions for students during the pandemic. The participatory model of intervention development [ 88 ] may be particularly useful in this regard. The Participatory Intervention Model (PIM), rooted in participatory action research, provides aa mechanism for integrating theory, research and practice and for promoting involvement of stakeholders in intervention efforts [ 88 ]. Based on this model, it seems pertinent to revise the role of the year mentor ( opiekun roku ; in Polish universities, students at each year of their academic program are assigned an academic teacher who meets with the students, acquaints them with the university’s structure and the program, etc.) by including screening assessments of the students’ expected sources of support. Additionally, the role of the university counselor should be created. It is worth noting that the youngest students in particular should be incorporated in the design process for such solutions. This is because the presented study shows that the youngest full-time students showed passive and maladaptive coping strategies. Support solutions designed through the participatory model of intervention should be useful for students, should address their specific needs, and should consider the students’ cultural, organizational, and social contexts, including the context of the pandemic and its consequences. Efforts towards designing adequate interventions may prove insufficient if no attempts are made to understand the students’ beliefs, motivations, practices, language, and culture. Such practices can help universities offer more comprehensive support to students of specific populations. Thus, the particular attention should be draw to the notion of acceptability within PIM, which reflects the perception of the beneficiaries (mainly the university inn this context) as partners in identifying problems and developing the offer of psychological, organizational, and instrumental support solutions created through the process of researching the specificity of the pandemic situation and post-pandemic adaptation. Identifying problems, as well as the scope and range of partnership between the university and its personal and infrastructural resources in planning psychological, organizational, and infrastructural support for students requires an evidence base.
The necessity of carrying out research that would lead to effective practical solutions through PIM is also underscored by Nastasi (et. al.) [ 89 ]. The study presented in this article fits this proposal. The current study results showed also that 10% of the sample expecting support from the university. This situation indicates that the current support offer could be insufficient in the context of the pandemic. Thus far, support given to students has been limited mainly to material support–financial support and academic scholarships. Verifying its role as a source of support and an important social environment for its students is also a significant new challenge for universities in the pandemic and post-pandemic reality.
Conclusions
Studies in this direction should continue in order to examine how students cope with subsequent stages of studying both during the pandemic as well as after its end.
Despite the limitations indicated above, the current results contribute to understanding the social and emotional changes related to the coronavirus pandemic, especially in the area of higher education. Studies on stress and coping among students carried out thus far have not sufficiently considered a range of factors such as the study system (paid vs. free), sources of institutional support (scholarships, student loans, material support), unemployment, or job prospects after graduation. Additionally, similarities and differences in the experience of stress and coping strategies between students in various countries (ethnic and cultural differences) have not been researched to an appropriate degree.
The current study indicates, among others, that younger students who are in the beginning stages of their academic careers cope with stress less effectively. This is largely a consequence of the fact that they do not yet possess appropriate life experience, and thus do not have sufficient competences in coping with difficult situations. This suggests that university administrations should pay particular attention to this group. An obligatory course on coping skills should be recommended for the first year curriculum. This could improve students’ competences, wellbeing, and resilience.
Supporting information
https://doi.org/10.1371/journal.pone.0255041.s001
- View Article
- Google Scholar
- PubMed/NCBI
- 3. Gallagher RP. National Survey of Counseling Center Directors 2008 [Internet]. The International Association of Counseling Services, Inc., 2008 [cited 2021 Feb 23]. Available from: https://www.immagic.com/eLibrary/ARCHIVES/GENERAL/ACCA_US/A081007G.pdf
- 7. American College Health Association—National College Health Assessment: Reference Group Executive Summary Spring 2000 [cited 2021 Feb 10]. Available from: https://www.acha.org/documents/ncha/ACHA-NCHA_Reference_Group_ExecutiveSummary_Spring2000.pdf
- 9. American College Health Association–National College Health Assessment: Reference Group Executive Summary Spring 2014 [cited 2021 Feb 10]. Available from: https://www.acha.org/documents/ncha/ACHA-NCHA-II_ReferenceGroup_ExecutiveSummary_Spring2014.pdf
- 13. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). [Internet]. Public Health Update; 2021 Feb 7 [cited 2021 Feb 23]. Available from: https://coronavirus.jhu.edu/map.html
- 16. Costa PT Jr, McCrea RR. Stability and Change in Personality from Adolescence Through Adulthood. In: Halverson CF Jr, Kohnstamm GA, Martin RR, editors. The Developing Structure of Temperament and Personality from Infancy to Adulthood. Hillsdale, NJ: Erlbaum; 1995. pp. 139–155.
- 19. Thomas E. Coronavirus: Impact on Young People with Mental Health Needs [Internet]. London: YoungMinds; 2020. [cited 2021 Feb 21] Available from: https://youngminds.org.uk/media/3904/coronavirus-report-summer-2020-final.pdf
- 20. Wrześniewski K. Style a strategie radzenia sobie ze stresem. Problemy pomiaru [Styles and strategies of coping with stress. Issues in measurement]. In: Heszen-Niejodek I, Ratajczak Z. editors. Człowiek w sytuacji stresu. Problemy teoretyczne i metodologiczne [People in situations of stress. Theoretical and methodological issues]. Katowice: Wyd. Uniwersytetu Śląskiego; 1996. pp.44–64.
- 24. General assessment of the macroeconomic situation. [Internet]. 2021 Feb 7 [cited 2021 Feb 21]. Available from: https://www.oecd-ilibrary.org/sites/39a88ab1-en/1/3/1/index.html?itemId=/content/publication/39a88ab1-en&_csp_=fd64cf2a9a06f738f45c7aeb5a6f5024&itemIGO=oecd&itemContentType=issue
- 25. Owusu P, Essel G. Causes of students’ stress, its effects on their academic success, and stress management by students, Case study at Seinajoki University of Applied Sciences, Finland. Thesis. Seinaioki University of Apllied Sciences. 2017; 30–61. Available from: https://www.academia.edu/34566514/Causes_of_students_stress_its_effects_on_their_academic_success_and_stress_management_by_students
- 26. Cantillon B, Chzhen Y, Handa S, Nolan B. Children of austerity. Impact of the great recession on child poverty in rich countries. UNICEF, New York: Oxford University Press, 2017. Available from: https://www.unicef-irc.org/publications/pdf/Children_of_austerity.pdf
- 33. Lazarus RS, Folkman S. Stress, appraisal and coping. New York: Hemisphere; 1984.
- 37. Hobfoll SE. Stres, kultura i społeczność. Psychologia i filozofia stresu [Stress, culture, and society. The psychology and philosophy of stress]. Gdańsk: Gdańskie Wydawnictwo Psychologiczne; 2006.
- 38. Ogińska-Bulik N, Juczyński Z. Osobowość, stres a zdrowie [Personality, stress, and health]. Warsaw: Difin; 2008.
- 42. Statistic Poland. Higher education institutions and their finances in 2018. Warsaw- Gdańsk; 2019.
- 43. Tertiary education statistics. 2020 Sep [cited 2021 Feb 23]. Available from: https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Tertiary_education_statistics
- 44. Education and Training Monitor 2020. [cited 2021 Feb 23]. Available from: https://op.europa.eu/webpub/eac/education-and-training-monitor-2020/countries/poland.html
- 45. University of Gdańsk. 2021 May 10 [cited 2021 May12]. Available from: https://ug.edu.pl/o_uczelni/ug_w_liczbach
- 46. Adam Mickiewicz University in Poznań. 2021 May 10 [cited 2021 May12]. Available from: http://100lat.aum.edu.pl/uam/
- 47. University of Warsaw. 2021 May 10 [cited 2021 May 12]. Available from: https://www.uw.edu.pl/uniwersytet/materialy-o-uw-do-pobrania/publikacje/
- 48. Jan Kochanowski University of Kielce. 2021 May 10 [cited 2021 May 12]. Available from: https://www.ujk.edu.pl/Uczelnia_w_liczbach.html
- 49. Pomeranian University in Słupsk. 2021 May 10 [cited 2021 May12]. Available from: https://rekrutacja.apsl.edu.pl/Rekrutacja/O-uczelni
- 50. Poland in numbers. 2021 May 10 [cited 2021 May12]. Available from: https://www.polskawliczbach.pl/najwieksze_miasta_w_polsce_pod_wzgledem_liczby_ludnosci
- 51. Statistical Office in Gdańsk, Centre for Education and Human Capital Statistic. Higher education and its finances in 2019. Warsaw-Gdańsk; 2020.
- 54. Juczyński Z, Ogińska-Bulik N. Narzędzia pomiaru stresu i radzenia sobie ze stresem [Measures of stress and coping]. Warsaw; 2009. pp.45–55.
- 55. George D, Mallery P. IBM SPSS statistics 23 step by step: A simple guide and reference. Routledge; 2016.
- 57. Neetu AJ, Stoebenau K, Ritter S, Edmeades J, Balvin N. Gender Socialization during Adolescence in Low- and Middle-Income Countries: Conceptualization, influences and outcomes, UNICEF; 2017.
- 58. Horwitz A, Wakefield J. The Loss of Sadness. How Psychiatry Transformed Normal Sorrow Into Depressive Disorder. Oxford; 2007.
- 66. Cohen S, Underwood LG, Gottlieb BH. Social Support Measurement and Intervention. Oxford, UK: Oxford University Press; 2000.
- 71. Masten AS. Resilience in individual development: Successful adaptation despite risk and adversity. In: Wang MC, Gordon EW, editors. Educational resilience in innercity America: Challenges and prospects. Hillsdale, NJ: Erlbaum; 1994. pp. 3–25.
- 76. Kozłowski P. Wartości, cele i plany życiowe młodzieży nieprzystosowanej społecznie [Values, goals and life plans of socially maladjusted youth]. Kraków: Impuls; 2016.
- 84. Marcia JE. Identity in adolescence, In: Adelson J, editor. Handbook of adolescent psychology. New York: Wiley;1980.
- 85. Erikson EH, Identity; youth and crisis. New York: W. W. Norton Company; 1968.
- 86. Bronfenbrenner U. Ecological systems theory. In: Vasta R, editor. Six theories of child development: Revised formulations and current issues. London, Bristol, Pennsylvania: Jessica Kingsley Publishers; 1992; 187–249. https://doi.org/10.1111/j.1467-8624.1992.tb01638.x pmid:1611945
- 87. Statistics Poland, Szkolnictwo wyższe w roku akademickim 2018/2019 (wyniki wstępne) [Higher education in the 2018/2019 academic year (preliminary results). [citied 2021 Feb 23] Available from: https://stat.gov.pl/obszary-tematyczne/edukacja/edukacja/szkolnictwo-wyzsze-w-roku-akademickim-20182019-wyniki-wstepne ,8,6.html
Writing about COVID-19 in a college admission essay
by: Venkates Swaminathan | Updated: September 14, 2020
Print article

For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic’s impact. The different sections have differing goals. You must understand how to use each section for its appropriate use.
The CommonApp COVID-19 question
First, the CommonApp this year has an additional question specifically about COVID-19 :
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces. Please use this space to describe how these events have impacted you.
This question seeks to understand the adversity that students may have had to face due to the pandemic, the move to online education, or the shelter-in-place rules. You don’t have to answer this question if the impact on you wasn’t particularly severe. Some examples of things students should discuss include:
- The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic.
- The candidate had to deal with personal or family issues, such as abusive living situations or other safety concerns
- The student suffered from a lack of internet access and other online learning challenges.
- Students who dealt with problems registering for or taking standardized tests and AP exams.
Jeff Schiffman of the Tulane University admissions office has a blog about this section. He recommends students ask themselves several questions as they go about answering this section:
- Are my experiences different from others’?
- Are there noticeable changes on my transcript?
- Am I aware of my privilege?
- Am I specific? Am I explaining rather than complaining?
- Is this information being included elsewhere on my application?
If you do answer this section, be brief and to-the-point.
Counselor recommendations and school profiles
Second, counselors will, in their counselor forms and school profiles on the CommonApp, address how the school handled the pandemic and how it might have affected students, specifically as it relates to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
Students don’t have to mention these matters in their application unless something unusual happened.
Writing about COVID-19 in your main essay
Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. That you had to stay home and study online isn’t sufficient, as millions of other students faced the same situation. But sometimes, it can be appropriate and helpful to write about something related to the pandemic in your essay. For example:
- One student developed a website for a local comic book store. The store might not have survived without the ability for people to order comic books online. The student had a long-standing relationship with the store, and it was an institution that created a community for students who otherwise felt left out.
- One student started a YouTube channel to help other students with academic subjects he was very familiar with and began tutoring others.
- Some students used their extra time that was the result of the stay-at-home orders to take online courses pursuing topics they are genuinely interested in or developing new interests, like a foreign language or music.
Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely important about the student. For many students whose lives have been shaped by this pandemic, it can be a critical part of their college application.
Want more? Read 6 ways to improve a college essay , What the &%$! should I write about in my college essay , and Just how important is a college admissions essay? .

Homes Nearby
Homes for rent and sale near schools

How our schools are (and aren't) addressing race

The truth about homework in America

What should I write my college essay about?
What the #%@!& should I write about in my college essay?
Yes! Sign me up for updates relevant to my child's grade.
Please enter a valid email address
Thank you for signing up!
Server Issue: Please try again later. Sorry for the inconvenience
- Future Students
- Current Students
- Faculty/Staff

News and Media
- News & Media Home
- Research Stories
- School’s In
- In the Media
You are here
Student stress during the pandemic.

High school students are experiencing rising stress levels and lower engagement with learning since the start of the COVID-19 pandemic, according to a new study by NBC News and Challenge Success, a nonprofit affiliated with Stanford Graduate School of Education (GSE).
Kids feel that “they are more stressed than they were before the pandemic, they have more work, they are less engaged in school, and their relationships with teachers and [other] kids are strained,” says Denise Pope, a senior lecturer at Stanford GSE and co-founder of Challenge Success.
On this episode of School’s In , Pope talks with show co-host and GSE Dean Dan Schwartz about the study – one of the largest national research projects to shed light on the pandemic’s impact on student connection, engagement and mental health. She also shares what parents and educators might take from its findings in the days and years ahead.
In addition to grades, workload and time management, the study found that one of the top sources of stress for students was lack of sleep. This surprised Pope, who thought remote learning would give students more flexibility and time to sleep. But 43 percent of the students reported sleeping less, and about 5 percent said they were getting less than four hours a night.
Other sources of stress included college and the future, finances and a lack of time to play and relax. Females and students of color in particular experienced high levels of stress and pressure.
Some good news: “People are now much more aware of these problems,” says Pope. “I think more teachers recognize the importance of checking in on mental health and how it’s connected to academics, and how it’s part of their job.”
You can listen to School's In on SiriusXM , Apple Podcasts , Google Podcasts , Spotify , Stitcher and Soundcloud .
⟵ Go to all School's In
Get the Educator
Subscribe to our monthly newsletter.
Stanford Graduate School of Education
482 Galvez Mall Stanford, CA 94305-3096 Tel: (650) 723-2109
- Contact Admissions
- GSE Leadership
- Site Feedback
- Web Accessibility
- Career Resources
- Faculty Open Positions
- Explore Courses
- Academic Calendar
- Office of the Registrar
- Cubberley Library
- StanfordWho
- StanfordYou
Improving lives through learning

- Stanford Home
- Maps & Directions
- Search Stanford
- Emergency Info
- Terms of Use
- Non-Discrimination
- Accessibility
© Stanford University , Stanford , California 94305 .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves
Mirko manchia.
a Section of Psychiatry, Department of Medical Sciences and Public Health, University of Cagliari, Cagliari, Italy
b Unit of Clinical Psychiatry, University Hospital Agency of Cagliari, Cagliari, Italy
c Department of Pharmacology, Dalhousie University, Halifax, NS, Abbreviation:
Anouk W. Gathier
d Department of Psychiatry (GGZ inGeest), Amsterdam UMC (location VUmc), Vrije University, Amsterdam Public Health and Amsterdam Neuroscience research institutes, Amsterdam, Netherlands
Hale Yapici-Eser
e Department of Psychiatry, Koç University School of Medicine, Istanbul, Turkey
f Research Center for Translational Medicine, Koç University, Istanbul, Turkey
Mathias V. Schmidt
g Research Group Neurobiology of Stress Resilience, Max Planck Institute of Psychiatry, Munich, Germany
Dominique de Quervain
h Division of Cognitive Neuroscience, Department of Psychology, Department of Medicine, University of Basel, Switzerland
Therese van Amelsvoort
i Department of Psychiatry and Neuropsychology, Maastricht University, Maastricht, Netherlands
Jonathan I. Bisson
j Division of Psychological Medicine and Clinical Neurosciences, Cardiff University School of Medicine, Cardiff, United Kingdom
John F. Cryan
k Dept Anatomy & Neuroscience, University College Cork, Cork, Ireland & APC Microbiome Ireland, University College Cork, Cork, Ireland
Oliver D. Howes
l King's College London, London, SE5 8AF Imperial College London, London, W12 0NN Lundbeck A/v, Valby, Denmark
Luisa Pinto
m Life and Health Sciences Research Institute (ICVS), School of Health Sciences, University of Minho, Braga, Portugal
n Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal
Nic J. van der Wee
o Department of Psychiatry, Leiden University Medical Center, LUMC Neuroscience and Leiden Institute for Brain and Cognition, Leiden, Netherlands
Katharina Domschke
p Department of Psychiatry and Psychotherapy, Medical Center – University of Freiburg, Faculty of Medicine, University of Freiburg, Freiburg, Germany
q Center for Basics in NeuroModulation, Faculty of Medicine, University of Freiburg, Freiburg, Germany
Igor Branchi
r Center for Behavioral Sciences and Mental Health, Istituto Superiore di Sanità, Rome, Italy
Christiaan H. Vinkers
s Department of Psychiatry (GGZ inGeest), Amsterdam UMC (location VUmc), Vrije University, Amsterdam Public Health and Amsterdam Neuroscience research institutes, Amsterdam, Netherlands
t Department of Anatomy and Neurosciences, Amsterdam UMC (location VUmc), Vrije University, Amsterdam, Netherlands
The global public health crisis caused by COVID-19 has lasted longer than many of us would have hoped and expected. With its high uncertainty and limited control, the COVID-19 pandemic has undoubtedly asked a lot from all of us. One important central question is: how resilient have we proved in face of the unprecedented and prolonged coronavirus pandemic? There is a vast and rapidly growing literature that has examined the impact of the pandemic on mental health both on the shorter (2020) and longer (2021) term. This not only concerns pandemic-related effects on resilience in the general population, but also how the pandemic has challenged stress resilience and mental health outcomes across more specific vulnerable population groups: patients with a psychiatric disorder, COVID-19 diagnosed patients, health care workers, children and adolescents, pregnant women, and elderly people. It is challenging to keep up to date with, and interpret, this rapidly increasing scientific literature. In this review, we provide a critical overview on how the COVID-19 pandemic has impacted mental health and how human stress resilience has been shaped by the pandemic on the shorter and longer term. The vast literature is dominated by a wealth of data which are, however, not always of the highest quality and heavily depend on online and self-report surveys. Nevertheless, it appears that we have proven surprisingly resilient over time, with fast recovery from COVID-19 measures. Still, vulnerable groups such as adolescents and health care personnel that have been severely impacted by the COVID-19 pandemic do exist. Large interindividual differences exist, and for future pandemics there is a clear need to comprehensively and integratively assess resilience from the start to provide personalized help and interventions tailored to the specific needs for vulnerable groups.
Key messages
- • The early stages of the COVID-19 pandemic were often associated with increased levels of distress and depressive and anxiety symptoms in the general population.
- • A substantial group of individuals has been either largely unaffected or is even doing better during the pandemic.
- • Longitudinal follow up showed remarkable signs of resilience.
- • Health care workers appear to be at an increased risk of stress-related psychological symptoms.
- • The mental health of children, adolescents, and students has been particularly affected by the pandemic.
- • Elderly people are more vulnerable to the physical effects of COVID-19, but also report lower psychopathology during the pandemic.
- • Individuals with an existing psychiatric disorder are experiencing detrimental impact on their mental health from the COVID-19 pandemic, but do not seem to have further increased symptom severity compared with their pre-pandemic levels.
- • A high risk exists for psychiatric sequelae following a COVID-19 infection.
- • Many methodological shortcomings occur in the current literature which is often cross-sectional and relies on self-report, and it is moreover hard to directly compare results across many of the studies.
- • There is an urgent need for a personalized approach when it comes to identifying individuals at risk or resilient for the stressful effects of the COVID-19 pandemic.
- • The effects of stress and the resilience capacity are dependent on (neuro)biological, psychological, and environmental factors and also are heavily dependent on an individual's unique context.
1. Introduction
In 2020 many of us had hoped that the COVID-19 pandemic would be over in 2021, and that normal life would have resumed. The situation is clearly different: the pandemic is still ongoing with novel and more contagious variants leading to increased infection rates across the globe, with consequently more stringent restrictions in social interactions and more lockdowns. By the spring of 2021, over 156 million confirmed cases and more than 3.2 million deaths of COVID-19 have been reported ( https://covid19.who.int/ ), with health care systems worldwide being overburdened at certain times. As in 2020, summer was expected to be associated to a reduced impact of the pandemic. However, new variants of the virus emerged, such as the Delta variant and there is still concern for what will occur during fall and winter. The pandemic and the accompanying measures have led to changes in people's daily routines, limited social interactions, as well as formed tensions among families in lockdown together, and fear of getting ill and/or spreading the virus. At the same time, the prospect of mass vaccination efforts has given rise to hope. Undoubtedly, the pandemic has asked a lot from all of us given the high uncertainty and limited control over the situation. For mental health professionals, the key questions are: what are the effects of the COVID-19 pandemic on mental health, and what have we learnt from this unprecedented and prolonged pandemic regarding resilience at the individual and societal level? During the first wave of the pandemic, our Thematic Working Group on Resilience from the European College for Neuropsychopharmacology (ECNP) wrote an overview of stress resilience during the early stages of the pandemic ( Vinkers et al., 2020 ). Now, almost a year later, there has been a second wave and, in many countries, a third wave. Numerous studies have attempted to identify how the stressful pandemic has impacted mental health in the shorter and longer term across a wide range of populations. In fact, by April 2021, a staggering 120,000 publications on COVID-19 had appeared, with over 5,000 dealing with the impact of the pandemic on mental health and how stress resilience is shaped during the prolonged COVID-19 pandemic. Given that the pandemic is continuing, and there is the risk of future outbreaks, it is timely to consider its impact on mental health and factors that are linked to resilience against mental illness to guide the ongoing response to it. In view of this, we aim to provide a critical overview of how the pandemic has affected mental health in general, and how human stress resilience has shaped its impact on the shorter and longer term. Moreover, we aim to summarize whether there are specific effects of the COVID-19 pandemic on stress resilience across groups that may be more vulnerable (such as health care workers and adolescents), and what we can learn for possible future pandemics. In this selective review, we did not apply a systematic approach but rather used a targeted Medline search strategy related to COVID-19 topics complemented with a thorough search of references in key publications. A general premise should be made in the interpretation of the results of this review as several caveats impact on the interpretation of the evidence here summarized. First, most of the studies were conducted in the first wave of the pandemic, often with limited duration of follow-up, and are based on cross-sectional assessments and online surveys. Secondly, and possibly more importantly, the impact of the pandemic (as measured in terms of infections and death rates) as well as lockdown measures varied significantly from country to country. However, although these methodological limitations could reduce the robustness of the findings as well as their comparability among different countries, we believe this data synthesis might guide the reader in interpreting the impact of the pandemic on mental health and the modulating role of resilience.
2. The general population
The pandemic has affected almost every individual directly or indirectly, either due to (or fear of) COVID-19 infection, or because of the effects of far-reaching measures and their economic and social impact. Consequently, the impact of the pandemic on mental health outcomes has been frequently examined in the general population. In a study conducted in April 2020, using a probability sample ( N = 1468) and the Kessler-6 psychological distress scale (0–24 with 13 as a cutoff for serious distress), 13.6% of US adults reported symptoms of serious psychological distress, relative to 3.9% in 2018 ( McGinty et al., 2020 ). In another study among 9565 individuals from 78 countries, during the height of the lockdown (April – June 2020), the pandemic was experienced as at least moderately stressful for most people, and 11% reported the highest levels of stress. Symptoms of depression were also high, including 25% of the sample indicating that the things they did were not reinforcing, 33% reporting high levels of boredom, and nearly 50% indicating they wasted a lot of time ( Gloster et al., 2020 ). In a similar study which also used the Kessler-6 psychological distress scale ( N = 2555), distress levels did not increase, with equal numbers of US adults experienced serious psychological distress in February 2019 (prior to the pandemic) as in May 2020 ( Breslau et al., 2021 ). In the UK Household Longitudinal Study (UKHLS, N = 17,452), mental health was assessed with the 12-item General Health Questionnaire (GHQ-12) before and during the pandemic ( Pierce et al., 2020 ). In this study, the population prevalence of clinically significant levels of mental distress rose from 19% in 2018–19 to 27% in April 2020 (1 month into the UK lockdown). In a later report on the UKHLS, most individuals had either consistently good (39% of the participants) or consistently very good (38%) mental health across the first 6 months of the pandemic ( Pierce et al., 2021 ). A recovering group (12%) showed worsened mental health during the initial shock of the pandemic and then returned to pre-pandemic levels of mental health. The two remaining groups were characterized by poor mental health throughout the observation period, either with initial but sustained worsening in mental health (4%) or a steady and sustained decline in mental health over time (7%). Concerning major affective disorders, a nationally representative survey study of US adults (March – April 2020, N = 1,441) showed that the prevalence of depressive symptoms was more than three-fold higher during the COVID-19 pandemic when compared to the pre-pandemic prevalence (2017 – 2018) ( Ettman et al., 2020 ). Indeed, a recent quantitative data synthesis, conducted by the Global Burden of Disease (GBD) Resource center, has shown that the pandemic has impacted substantially on the risk of major depressive disorder and anxiety disorders, estimating an additional 53.2 million cases of major depressive disorder and an additional 76.2 million cases of anxiety disorders globally due to the COVID-19 pandemic ( COVID-19 Mental Disorders Collaborators, 2021 ; Santomauro et al., 2021). Further support for the link between the COVID-19 pandemic and the onset of affective disturbances comes from the large cohort study of Lob et al. (March – April 2020, N = 51,417), showing that severe depressive symptoms were developed by 11% of their sample equaling 5656 participants, while moderate symptoms were experienced by 29% of the subjects during the COVID-19 pandemic ( Iob et al., 2020a ). In Italy ( N = 130), quarantine resulted in increased internalizing symptoms, particularly in those individuals with pre-existing psychopathology or experiencing negative economic consequences ( Castellini et al., 2021 ). In another study conducted in the US (March – June 2020, N = 7138), both increases and decreases in distress during the pandemic, assessed with the Patient Health Questionnaire-4 (PHQ-4), could be explained by perceived infection risk and risk of death, perceived financial risks, lifestyle changes resulting from the virus, perceived discrimination, and changes in substance use and employment status (explained variation: 70% for the increase in distress between March and April 2020, and 46% for the decline in April and June 2020) ( Robinson and Daly, 2020 ). Among Chinese students ( N = 68,685), levels of stress decreased after remission of the first outbreak (end of March – beginning of April), even though anxiety symptoms (22 to 26%) and depressive symptoms (11 to 15%) still increased, particularly in those with limited physical exercise and perceived social support ( Li et al., 2021b ). This indicates that the pandemic may have longer-lasting negative effects on mental health outcomes that might take time to fully emerge. Finally, a survey performed in 1,310 Spanish adults during the first lock-down period (March 2020) showed that regression models containing a series of variables (i.e. being female, having a younger age, having negative self-perceptions about aging, more time being exposed to news about COVID- 19, having more contact with relatives different to those that participants co-reside with) explained 48% and 33% of the variance of distress and loneliness respectively ( Losada-Baltar et al., 2021 ). Although the methodological quality of studies was quite heterogeneous, with sometimes limited sample size, no longitudinal measures, and only sparse information about mental health status, adaptive responses after the first wave of the pandemic were frequently reported.
In contrast to studies showing increases in mental health problems in the general population, there is also convincing evidence that most individuals are sufficiently able to cope with the pandemic and its associated measures and even that increased resilience building in the general population may have occurred. In the Netherlands, for example, a longitudinal study among adults ( N = 3,983) showed no apparent increase was found in anxiety and depression symptoms between March 2019 and March 2020 when the pandemic broke out ( van der Velden et al., 2020 ). Moreover, in a Chinese general population study ( N = 1738), which was conducted during the initial outbreak (end of January – beginning of February 2020) and the epidemic's peak four weeks later, there were no significant longitudinal changes in stress, anxiety and depression levels ( Wang et al., 2020a ). In Switzerland, a survey study ( N = 10,472) documented increased stress in 50% of participants, but 24% showed no change and 26% even felt less stressed during the lockdown in April 2020 compared to the pre-pandemic period ( https://osf.io/jqw6a/ ). More encouraging news stems from the UCL COVID-19 Social Study showing that, between March and August 2020, in over 36,500 adults, the highest levels of depression and anxiety occurred in the early stages of lockdown but declined fairly rapidly as individuals adapted to the changing circumstances, even though the sample is not representative of the national population ( Fancourt et al., 2021 ). In Spain ( N = 3480), after the confinement was lifted, depressive symptoms rapidly decreased after an initial increase during the confinement, but no clear effects on anxiety were found ( Gonzalez-Sanguino et al., 2020 ). In Germany, worrying and depressive symptoms among the general population ( N = 2376) decreased on average between March and June 2020 ( Bendau et al., 2020b ). Another US sample ( N = 7319) found increased psychological distress (PHQ-4) between March and April 2020 as the COVID-19 crisis emerged and lockdown restrictions began, which subsequently declined to mid-March (baseline) levels by June 2020 ( Daly and Robinson, 2020 ). In 1166 UK adults, a low-stable profile characterized by little-to-no psychological distress was the most common trajectory for both anxiety-depression and COVID-19-related PTSD ( Shevlin et al., 2021 ). Assessment of loneliness in 1545 American adults in January, March, and April 2020 showed no significant changes in loneliness but rather increased perceived support from others ( Luchetti et al., 2020 ).
Conclusion: In the general population, the early stages of the COVID-19 pandemic were often associated with increased levels of distress and depressive and anxiety symptoms. However, the effects of the pandemic on mental health in the general population have been quite heterogeneous from the beginning, and a substantial group has been either largely unaffected or is even doing better during the pandemic period. More importantly, longitudinal follow up has shown signs of resilience in the general population, with surprising ability to bounce back and adapt. For an overview of findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in the general population, see Table 1 .
The impact of COVID-19 on stress resilience and mental health in the general population.
| US Adults aged 18 years or older | April 7–13 2020 | Cross-sectional, = 1468 | Psychological distress and loneliness among US adults in April 2020 (Johns Hopkins COVID-19 Civic Life and Public Health Survey) compared to the 2018 National Health Interview Survey (NHIS) | Unknown | 3.9% of US adults reported psychological distress in 2018 compared to 13.6% in April 2020. In April 2020, 13.8% of US adults reported that they always or often felt lonely. | |
| Adults aged 18 years or older from 78 different countries | April 7 - June 7 2020, | Cross-sectional, = 9565 | The impact of COVID-19 pandemic associated lockdowns on mental health outcomes (stress (PSS), depression (MSBS) positive/negative affect (PANAS), wellbeing (MHC-SF)) | Being at least 18 years of age and being able to read one of the 18 languages (English, Greek, German, French, Spanish, Turkish, Dutch, Latvian, Italian, Portuguese, Finnish, Slovenian, Polish, Romanian, Hong Kong, Hungarian, Montenegrin, & Persian) | The highest level of mental health difficulties were found in approximately 10% of the population. The pandemic was experienced moderately and highly stressful for 55.9% and 11% respectively. Symptoms of depression were high, with 25% reporting lack of reinforcement, 33% indicating boredom and nearly 50% indicating having wasted a lot of time. | |
| US adults aged 20 years or older | Two waves: T1 (February 2019; prior to pandemic) and T2 (May 2020; during pandemic) | Longitudinal, = 2555 | The impact of the COVID-19 pandemic by comparing psychological distress (Kessler-6) experienced during the pandemic with the highest level of distress respondents had experienced during a 12-month period prior to the pandemic | Unknown | In 12.8%, an increase in psychological distress was found during COVID-19 (T2) relative to the highest level of distress before COVID-19 (T1) (95% CI 9.9%–15.7%).The experience of severe distress before at T1 was a strong predictor for the experience of severe stress at T2.. | |
| UK people aged 16 years or older | April 23–30 2020; secondary analysis of the UK Household Longitudinal Study (UKHLS)) | Longitudinal cohort, = 17,452 (8.8% aged 16–24 years, 11.2% 25–34 years, 16.0% 35–44 years, 20.1% 45–54 years, 28.9% 55–69 years, 15.1% ≥ 70 years, 58.2% female, 80.4% white British, 4.5% non-white British, 1.6% mixed, 7.3% Asian, 2.2% black, 0.5% other ethnicity, 3.4% ethnicity missing) | Changes in adult mental health in the UK population before (using data from UKHLS) and during the lockdown. | Participation in either of the two most recent UKHLS data collections (Waves 8 or 9), being 16 years or older | The prevalence of clinically significant levels of mental distress was 27.3% (95% CI 26.3–28.2) in April 2020, compared to 18.9% (95% CI 17.8–20.0) in 2018–19. This increase in mental distress was higher than expected, given previous annual trends and particularly found in young people and in women. | |
| UK people aged 16 years or older | Late April – early October 2020), secondary analysis of the UK Household Longitudinal Study (UKHLS) | Longitudinal cohort, = 19,763 (58.1% female) | Mental health trajectories during the COVID-19 pandemic and predictors of deterioration | Participation in either of the two most recent UKHLS data collections (Waves 8 or 9), being 16 years or older | Across the first 6 months of the COVID-19 pandemic up to October 2020, the mental health of most UK adults remained resilient (76.8%) or returned to pre-pandemic levels. (12.0%). For 4.1%there was an initial worsening in mental health that was sustained with highly elevated scores and 7.0% had little initial acute deterioration in their mental health, but reported a steady and sustained decline in mental health over time. | |
| US adults aged 18 or older | March 31, - April 13, 2020 (‘during COVID-19 sample’) and 2017–2018 (‘pre-COVID-19 sample’) | Cross-sectional, = 1441 during COVID-19 (38.0% aged 18–39, 32.4% aged 40–59, 29.7% aged ≥ 60, 51.9% female) and = 5065 pre-COVID-19 (37.8% aged 18–39, 34.2% aged 40–59, 28.0% aged ≥ 60, 51.4% female) | Prevalence of depression symptoms (PHQ-9) and factors associated with depression of US adults during vs before the COVID-19 pandemic | Being 18 years or older, speaking English, having completed an AmeriSpeak survey in the past 6 months | Prevalence of depressive symptoms was more than 3-fold higher during COVID-19 (8.5% before COVID-19 and 27.8% during COVID-19). Being exposed to more stressors and low income was associated with greater odds of depressive symptoms. | |
| Iob, E. et al., 2020 | UK adults aged 18 or older | March 21- April 2, 2020 | Cohort (part of longitudinal study of adults residing in the UK (the COVID-19 Social Study), = 51,417 (mean age 48.8 years (±16.8), 51.1% female, 12.0% of Black, Asian, and minority racial/ethnic communities) | Severity of depressive symptoms (PHQ-9) over time among individuals at high risk in the UK during the COVID-19 pandemic | Having completed at least 1 interview of the COVID-19 Social Study | UK adults with low socioeconomic position (SEP) and with psychosocial and health-related risk factors were at heightened risk of experiencing moderate and severe depressive symptoms during the COVID-19 pandemic. |
| Italian adults aged 18–60 years | Two waves: T0 (December 1 2019, - January 15 2020,; pre-lockdown) and T1 (April 22 - May 3 2020,; 1,5 month after the declaration of lockdown) | (Longitudinal and cross-sectional, = 671 ( = 130longitudinal, = 541 cross-sectional; 71.4% female, mean age women 33.1 years (±14.1), mean age men 35.0 years (±14.0), | The impact of the lockdown during the pandemic on mental health (BSI) by using a longitudinal (2 waves; T0 and T1) and a cross-sectional observation (T1). | Age between 18 and 60 years, having an Italian nationality, being a resident in Tuscany | Phobic anxiety (T0: 0.26 ± 0.43; T1: 0.48 ± 0.63; <0.001). and depressive symptoms (T0: 0.57 ± 0.48; T1: 0.73 ± 0.65; = 0.003) increased during the lockdown as compared to a few weeks before the COVID-19 outbreak, whereas interpersonal sensitivity (T0: 0.58 ± 0.61; T1: 0.35 ± 0.61; <0.001) and paranoid ideation (T0: 0.49 ± 0.49; T1: 0.32 ± 0.49; <0.001) decreased. | |
| US adults aged 18 years or older | Six waves covering a period from March 10 -June 9 2020, | = 7138 (34,125 observations, mean age 49.0 years (±16.5), 51.2% female) | Distress (PHQ-4) during the COVID-19 crisis and explanatory psychosocial and behavioural factors, | Being a participant in the Understanding America Study (UAS) and being 18 years or older | Personal health concerns, perceived financial risks and lifestyle changes increased and this accounted for a substantial amount of respectively 21% and 14–15% of the initial rise in distress. Reduction in personal health concerns, financial concerns, and changes in lifestyle all mediated the decrease in psychological distress. | |
| Li, Y. et al., 2021 | Chinese college students | Two waves; T1 (early phase of COVID-19 February 3–10 2020) and T2 (‘under control’ phase of COVID-19 March 24-April 3 2020,) | Longitudinal, = 68,685 (T1 63.2% female, T2 62.6% female) | Trajectory changes of acute stress (IES-6), anxiety (GAD-7), and depressive symptoms (PHQ-9) | Being a student in one of the target universities (22 universities in Guangdong Province) | Rates of acute stress decreased over time (34.6% at T1 vs 16.4% at T2), while rates of probable depression (21.6% vs 26.3%) and anxiety (11.4% vs 14.7%) significantly increased. |
| Spanish adults aged 18 years or older | March 21–24 2020, after the mandatory lockdown which started on March 16 2020, | Cross-sectional, = 1310 (mean age 42.36 years (±16.20), 71.1% female) | Loneliness and distress in people exposed to COVID-19 lock-down measures and explanatory personal and relational variables | Being older than 18 year, living in Spain and experiencing the required (mandatory) situation of lock-down at home | Being female, having a younger age, having negative self-perceptions about aging, more time being exposed to news about COVID- 19, having more contact with relatives (different to those that participants co-reside with) explained 48% and 33% of the variance of distress and loneliness respectively. | |
| Dutch adults aged 18 years or older | Four waves; T1 (November 2018, data from the longitudinal LISS panel), T2 (March 2019, data from the longitudinal VICTIMS study), T3 (November 2019, data from the longitudinal LISS panel), T4 (March 2020, longitudinal data from the VICTIMS study) | Longitudinal, = 3983 (T1: 50.7% female, 26.7% aged 18–45, 23.6% aged 35–49, 25.9% aged 50–64, 23.8% aged ≥ 65; T2: not reported; T3: 50.7% female, 24.9% aged 18–45, 22.9% aged 35–49, 26.1% aged 50–64, 26.1% aged ≥ 65; T4: not reported) | Prevalence of high Anxiety and Depression Symptom (ADS) levels and lack of Emotional Support (ES) before the COVID-19 outbreak during the period in which the COVID-19 pandemic developed very rapidly in the Netherlands | Being older than 18 years | No significant differences in high ADS levels were found between November 2018 (16.7%) and March 2019 (16.8%) and between November 2019 (16.9%) and March 2020 (17.0%). For lack of ES, no significant differences were found between March 2019 (20.4%) and March 2020 (19.7%), although the total scores of lack of ES were significantly lower in March 2020 ( = 10.2, SD = 3.41) than in March 2019 ( = 10.4, SD = 3.55), t(3982) = 3.50, <0.001). | |
| Wang, C. et al., 2020 | Chinese general population (from 194 cities in China) | Two waves/surveys; T1 (January 31 - February 2, 2020), T2 (February 28 - March 1, 2020) | Longitudinal, = 1738 with = 333 participated in both waves (T1: 60.3% female, 53.1% aged 21.4–30.8 years; T2: 75.0% female, 46.5% aged 21.4–30.8 years) | Temporal psychological impact (IES-R) and adverse mental health status (DASS-21) during the initial outbreak and peak of COVID-19 | Unknown | There were no significant longitudinal changes in mean DASS-stress (T1: = 7.76, SD =7.74, T2: = 7.86, SD), anxiety subscale (T1: = 6.16, SD =6.57, T2: = 6.16, SD =6.94) and depression scores subscale (T1: = 6.25, SD = 7.16, T2: = 6.38, SD =7.39) during the initial outbreak and the peak of the COVID-19 epidemic. The mean IES-R score of the second-survey respondents ( = 30.76, SD = 16.34) was significantly lower than the first-survey respondents ( = 32.98, SD = 15.42). . |
| The Swiss Corona Stress Study, first wave (between April 6 and 8, 2020)(prep-print: ) | Swiss general population, aged 14 years and older | April 6 - 8, 2020, starting 3 weeks after the beginning of confinement | Cross-sectional, = 10,472 (mean age 40.3 years (± 13.6, 71% female) | The adaptation of the Swiss population to the COVID-19 outbreak and risk- and resilience factors | Living in Switzerland, being 14 years or older, having completed the survey by April 8 2020, | While 24.4% of the participants reported no change in stress levels, 49.6% of the participants reported an increase in stress levels during confinement as compared to the time before the COVID-19 pandemic. |
| UK adults, aged 18 years and older | March 23 (start of the first lockdown in the UK) - August 9, 2020 | Prospective longitudinal observational, = 36,520 (7.5% aged 18–29, 29.2% aged 30–45, 33.0% aged 46–59, 30.4% aged ≥ 60, 76% female) | Trajectories of anxiety and depression over the 20 weeks after lockdown was announced in England, | Having at least three repeated measures between March 23 and August 9, 2020 | Anxiety and depression levels both declined across the first 20 weeks following the introduction of lockdown in England ( = –1.93, SE=0.26, < 0.0001 for anxiety; = –2.52, SE = 0.28, < 0.0001 for depressive symptoms). | |
| Spanish adults | Three waves; T1 (March 21 – 29 2020), T2 (April 13 – 27 2020, during the hardest moments of the confinement with the greatest impact at the socioeconomic level) and T3 (May 21 – June 4 2020,, during initiation of de-escalation on the restrictive measures) | Longitudinal observational cohort, = 3480 (T1: 35% aged 18–29 years, 59% aged 30–59 years, 6% aged ≥ 60 years, 75% female; T2: 29% aged 18–29 years, 64% aged 30–59 years, 7% aged ≥ 60 years, 81% female; T3: 27% aged 18–29 years, 65% aged 30–59 years, 8% aged ≥ 60 years, 81% female) | Effects of the pandemic and alarm situation on the mental health of the general population. | Being over 18 years of age, living in Spain, acceptance to participate in the successive evaluations of the study | Depressive symptoms increased significantly throughout the confinement (Z(T0-T1) = 7.06, p < 0.001, decreasing at the last assessment but not dropping to previous levels, with significant differences between the first and third evaluations (Z(T0-T2) = 4.02, p < 0.001). | |
| Bendau, A. et al., 2020 | German general population | Four waves; T1 (March 27 – April 6 2020,, during lockdown), T2 (April 24 – May 4 2020,, stepwise reduction of restrictive measures), T3 (May 15 – 35 2020) and T4 (June 6 – 15 2020, first cities introduce obligation of wearing face masks in public) | Longitudinal observational cohort, = 2376 ( = 503 completed all four waves, mean age at T1 38.76 years (± 12.01, 76.7% female) | Symptoms of (un‐) specific anxiety and depression along different stages of the pandemic | Having an minimum age of 18 years, living in Germany, being able to complete the questionnaires in German, having participated in at least two waves of data collection | Specific COVID‐19‐related anxiety and the average daily amount of preoccupation with the pandemic decreased continuously over the four waves. |
| US adults, nationally representative data from eight waves of the Understanding America Study (UAS) | Eight waves; T1 (March 10–18 2020), T2 (April 1 – 14 2020), T3 (April 14 – 28 2020), T4 (April 29 – May 12 2020,), T5 (Mat 13 – 26 2020), T6 (May 27 – June 9 2020,), T7 (June 10 – 23 2020), T8 (June 24 – July 20 2020,) | Longitudinal observational cohort, = 7319 (22.8% aged 18–34 years, 29.6% aged 35–49 years, 26.9% aged 50–64 years, 20.7% ≥ 65 years, 51.3% female) | Psychological distress following the emergence of the COVID-19 crisis in the United States | Unknown | On average psychological distress increased significantly by 0.27 standard deviations (95% CI [0.23,0.31], p < .001) from March 10–18 to April 1–14, 2020 as the COVID-19 crisis emerged and lockdown restrictions began in the US. | |
| UK adults | Three waves; T1 (March 21 −28 2020, during first week of first UK lockdown), T2 (April 22 – May 1 2020,,) and T3 (July 9 – 23 2020) | Longitudinal, = 2025 at T1, = 1406 at T2 and = 1166 at T3 | Clinically relevant levels of anxiety-depression (PHQ-ADS) and COVID-19 related PTSD (ITQ) over the first 4 months of the pandemic | Unknown | 20.7% of the participants met the criteria for anxiety-depression at W1 with no significant change at W2 (18.6%) or W3 (20.0%). 16.8% of the participants met criteria for COVID-19 related PTSD at W1 and this percentage decreased to 15.8% at W2 and 14.4% at W3. The ITQ mean scores were similar at W1 ( = 4.58) and W2 ( = 4.51), but decreased at W3 ( = 4.07), with the mean at W3 being significantly lower than the mean at W1. | |
| US adults | Three waves; T1 (January 31 – February 10 2020,, before the COVID-19 outbreak), T2 (March 18 – 29 2020, during the “15 Days to Slow the Spread” campaign) and T3 (April 23 – 29 2020, (during the “stay-at-home” policies of most states) | Longitudinal observational cohort, = 1545 (mean age: 53.68 years (± 15.63, 45% female) | Change in loneliness in response to the social restriction measures taken to control the coronavirus spread | Unknown | Despite some detrimental impact on vulnerable individuals, in the present sample, there was no large increase in loneliness across the three assessments ( = 0.04, > 0.05) but remarkable resilience in response to COVID-19. |
3. Health care personnel
Health care personnel have been particularly affected by the COVID-19 pandemic and exposed to more stressful circumstances than many other professional groups. This is due to several factors, including the increased infection risk, fear of infecting other people and being isolated from their families, working overtime, demanding work conditions with lengthy shifts, directly witnessing the suffering and death of patients, and witnessing the crowded and challenging situations in hospitals. Hence, it is not surprising that many studies on stress resilience and mental health outcomes during the COVID-19 pandemic have specifically focused on health care personnel. A meta-analysis of COVID-19-related stress and psychiatric symptoms in nurses already identified 93 studies published between January to September 2020 ( Al Maqbali et al., 2021 ). In this meta-analysis, over one third of over 90,000 nurses reported stress, sleep disturbances and increased mood and anxiety symptoms. This seems considerably higher than findings from studies in nurses working during smaller-scale pandemics like SARS or when compared to the general population at the same time period ( Chen et al., 2005 ). A similar picture arises from other studies. A survey of dental academics across 28 countries (March – May 2020, N = 1862) indicated considerable psychological impact of the COVID-19 pandemic with significantly increased worries and altered individual behavior ( Ammar et al., 2020 ). Moreover, in a Spanish cohort of health care workers (April 2020, N = 1422) over half of the participants reported symptoms of post-traumatic stress disorder (PTSD) and anxiety disorders, and nearly 50% reported symptoms of depression, with women and younger people showing an even higher risk ( Luceno-Moreno et al., 2020 ). A study of medical staff in China (February – March 2020, N = 899) indicated a significantly increased prevalence of psychiatric symptoms such as depression, anxiety and insomnia compared to the general population ( Liang et al., 2020 ). A longitudinal study among Japanese adults (March 2020 and May 2020, N = 1015) showed that indices of fatigue, anxiety and depression increased among health care compared to non-health care workers during the COVID-19 outbreak ( Sasaki et al., 2020 ). In Portugal, a cross-sectional study (May 2020) showed that physicians working at the frontline of COVID-19 ( N = 420) presented worse mental health outcomes (anxiety, depression, stress and obsessive-compulsive symptoms) than other physicians. Moreover, this study found that being female and working at the frontline are risk factors for increased stress, while having a garden at home was a protective factor for anxiety and stress symptoms ( Ferreira et al., 2021 ). In Turkey, when 939 health care workers were assessed cross-sectionally in April-May 2020, more than 60% of the participants reported anxiety and depression symptoms ( Sahin et al., 2020 ). These studies stress the need for successful intervention or prevention strategies for health care personnel. To avoid long-term effects of stress, strategies to counteract the negative impact of the COVID-19 pandemic on mental health, particularly in highly affected populations, may be helpful. For instance, in a group of Italian general practitioners ( N = 102), Di Monte and colleagues found that the implementation of task-orientated project management seemed protective against symptoms of burnout during the pandemic ( Di Monte et al., 2020 ). In another study, specific pandemic-related stress factors were identified in health care personnel, including workload burden and fear of infection ( Mosheva et al., 2020 ). Heath and colleagues reviewed several strategies to increase resilience among health care workers during and after the COVID-19 pandemic, also guided by the experiences of previous pandemics ( Heath et al., 2020 ). They identified several interventions and approaches, ranging from individual strategies without professional help (e.g. increased self-care or mindfulness practice) to strategies implemented at the group or organizational level (e.g. competency / resilience training, availability of psychological first aid or implementation of effective leadership and organizational justice). Importantly, some of these intervention strategies, including computer-assisted resilience training, have already been developed and successfully tested ( Aiello et al., 2011 ; Maunder et al., 2010 ; Weerkamp-Bartholomeus et al., 2020 ).
Conclusion: Overall, health care workers appear to be at an increased risk of stress-related psychological symptoms during a pandemic, compared to the general population. However, longitudinal studies are still largely lacking, and it remains to be seen whether the increase in symptoms is transient and can be considered a normal response to an abnormal temporally limited situation. For more solid conclusions, large-scale prospective longitudinal studies on the specific risk of health care personnel during and after a pandemic are needed. Such studies are already being planned ( Roberts et al., 2020 ). This is particularly relevant as the COVID-19 pandemic has been present over a prolonged period and already spans several waves of infection. Importantly, specific prevention and intervention strategies at the individual as well as at the organizational level may be crucial, with studies already showing beneficial effects of these strategies. See Table 2 for an overview of findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in health care personnel.
The impact of COVID-19 on stress resilience and mental health in health care personnel.
| Taiwanese female nurses | Mid-May 2003,(at the peak of the SARS outbreak) | Cross-sectional and case control, = 128 (high risk group = 65, mean age 27.2 years (± 3.6), conscripted group = 21, mean age 26.1 years (± 2.9), control group = 42, mean age 25.7 years (± 2.2)) | Symptoms of distress when working during the SARS crisis | Working as a nurse in the Kaohsiung Municipal Hsiao-Kang hospital during mid May 2003 | 11% of the nurses surveyed had stress reaction syndrome. Symptoms included anxiety, depression, hostility, and somatization. The highest rate of stress reaction syndrome was observed in the group that originally worked in a high-risk unit, and the conscripted group experienced the most severe distress on average.. | |
| Adult dentists worldwide (28 countries) | March - May 2020 | Cross-sectional, = 1862 (27.8% aged 25–35 years, 32.9% aged >35–45 years, 20.2% aged >45–55 years, 13.7% aged >55–65 years, 5.4% >65 years, 53.4% female) | Psychological impact of COVID-19 on dental academics globally and on changes in their behaviours | Being a dental academic, training and/or educating dental student in a university or institution at the time of the study | COVID-19 had a considerable psychological impact on dental academics. There was a direct, dose-dependent association between change in behaviours (more frequent handwashing, avoiding crowded places) and worries but no association between these changes and training on public health emergencies. | |
| Spanish adult healthcare workers | April 1 – 30 2020, during lockdown | Cross-sectional, = 1422 (mean age 43.9 years (±10.8), 86.4% female) | Symptoms of posttraumatic stress, anxiety, depression, levels of burnout and resilience in Spanish health workers during the COVID-19 pandemic | Being a Spanish healthcare worker and being in contact with patients of COVID-19 | 56.6% of health workers presented symptoms of posttraumatic stress disorder, 58.6% anxiety disorder, 46% depressive disorder and 41.1% felt emotionally drained. | |
| Chinese adult medical workers | February 14 - March 29 2020, | Cross-sectional, = 899 frontline medical workers (1.9% aged ≤ 20 years, 67.5% aged 21–40, 30.4% aged 41–60, 0.2% aged >60, 81.3% female) and = 1104 respondents in the general population (19.5% aged ≤ 20 years, 66.1% aged 21–40, 13.8% aged 41–60, 0.6% aged >60, 69.5% female) | Psychological symptoms in frontline medical workers during the COVID-19 epidemic in compared to the general population | Being a frontline medical worker during the COVID-19 pandemic | Overall, 30.43%, 20.29%, and 14.49% of frontline medical workers in Hubei Province and 23.13%, 13.14%, and 10.64% of frontline medical workers in other regions reported symptoms of depression, anxiety, and insomnia, respectively. In addition, 23.33%, 16.67%, and 6.67% of the general population in Hubei Province and 18.25%, 9.22%, and 7.17% of the general population in other regions reported symptoms of depression, anxiety, and insomnia, respectively.. | |
| Sasaki, N. et al., 2020 | Japanese adults (healthcare and non-healthcare workers) | Two waves; T1 (March 19 – 22 2020) and T2 (May 22 – 26 2020). OnApril 16, a state of national emergency was declared, which continued until 25 May | Longitudinal, = 1015 with = 111 healthcare (21.6% aged 20–29 years, 31.5% aged 30–39 years, 22.5% aged 40–49 years, 21.6% aged 50–59 years, 2.7% >60 years, 64.9% female) and = 904 non-healthcare workers (17.8% aged 20–29 years, 27.2% aged 30–39 years, 26.3% aged 40–49 years, 26.8% aged 50–59 years, 1.9% >60 years, 47.8% female) | Longitudinal change in the mental health of healthcare and non-healthcare workers during two months of the COVID-19 outbreak in Japan | Being a Japanese full-time employee that had previously participated in a large digital marketing research survey | Psychological distress (and subscales of fatigue, anxiety, and depression) as well as fear and worry of COVID-19 increased statistically significantly more among healthcare than non-healthcare workers. |
| Portuguese physicians | May 4 - 25 2020 | Cross-sectional, = 420 ( = 200 in frontline group (mean age 47.0 years, 53.5% female) and = 220 in the control group (mean age 60.0 years, 43.6% female) | Alterations in mental health status (depression, anxiety, stress measured with the DAS-21 and OCD symptoms, measured with OCI-R) of Portuguese physicians working at the COVID-19 frontline compared to those not working at the frontline | Being an active physician in Portugal | 7.5% of physicians in the frontline group had severe depressive symptoms, compared to 4.5% of physicians in the control group. Regarding anxiety, 9.0% of physicians in the frontline group presented severe symptoms of anxiety compared to 5.9% of physicians in the control group. 11.5% of participants in the frontline group presented severe stress symptoms, compared to 4.4% in the control group. Being female and working at the frontline were found as potential risk factors for stress. | |
| Turkish healthcare workers | April 23 – May 23 2020, | Cross-sectional, = 939 (11.5% aged 18–25 years, 36.1% aged 26–30 years, 29.4% aged 31–40 years, 23.0% aged >40 years, 66.0% female) | Prevalence of depression, anxiety, distress, and insomnia and related factors in healthcare workers during the COVID-19 pandemic in Turkey | Being a healthcare worker in Turkey between 23rd of April and 23rd of May 2020 | 729 (77.6%) participants exhibited depression, 565 (60.2%) anxiety, 473 (50.4%) insomnia, and 717 (76.4%) distress symptoms. Depression, anxiety, insomnia, and distress symptoms were significantly greater among females, individuals with a history of psychiatric illness, and individuals receiving psychiatric support during the COVID-19 pandemic. | |
| Italian general practitioners (GPs) | March 10 – May 18 2020, | Cross-sectional, = 102 (mean age 55.1 years (±11.4), 62.7% female) | Dimensions of burnout and various psychological features among Italian general practitioners during the COVID-19 emergency | Being an active general practitioner in Italy between March 10th and May 18th 2020 | The COVID-19 emergency had a significant impact on GPs’ work Implementing task-oriented problem management, rather than emotional strategies, appears to protect against burnout in these circumstances. | |
| Israeli physicians | March 19 – 22 2020 | Cross-sectional, = 1106 (mean age 46.1 years (±13.2), 49.0% female) | The association between pandemic‐related stress factors (PRSF) and anxiety and the potential effect of resilience on anxiety | Being a physician in Israel in March 2020 | Physicians reported high levels of anxiety with a mean score of 59.20 ± 7.95. An inverse association between resilience and anxiety was found. Four salient PRSF (mental exhaustion, anxiety about being infected, anxiety infecting family members, and sleep difficulties) positively associated with anxiety scores | |
| Canadian adult hospital workers | September 2008-January 2009 | Cross-sectional, = 158 (86% female) | Feasibility and effectiveness of an interactive, computer-assisted training course (short, medium and high version) designed to build resilience to the stresses of working during a pandemic | Being employee/professional staff member of the Mount Sinai Hospital in Toronto, Canada | Computer-assisted resilience training in healthcare workers appears to be of significant benefit and merits further study under pandemic conditions. Comparing three “doses” of the course suggested that the medium course was optimal. | |
| Canadian adults | Unknown | Cross-sectional, = 1020 | Development, implementation, and results of resilience training in the Mount Sinai Hospital setting prior to the emergence of the H1N1 pandemic | Being a staff member of the Mount Sinai Hospital | The proportion of participants who felt better able to cope after the session (76%) was significantly higher than the proportion who felt prepared to deal confidently with the pandemic before the session (35%). Ten key themes emerged from a qualitative analysis of written comments, including family-work balance, antiviral prophylaxis, and mistrust or fear towards health care workers | |
| Dutch patients with stress-related complaints | Precise period unknown, but during lockdown | Non randomized, single-arm intervention, = 37 (mean age 47.6 years (±18.7), 73% female) | Efficacy of remotely delivered ‘Wiring Affect with ReAttach’ (W.A.R.A.) in the reduction of negative affect and to compare the results with results of a previous study that investigated the efficacy of face-to-face W.A.R.A. in a cohort of 46 patients | Absence of suicidality risk and alcohol or drug abuse at the time of the online consultation | … |
4. Children, adolescents, and college students
It is plausible that the impact of the COVID-19 pandemic on mental health might vary as a function of age and levels of educational attainment. In this section, we present findings focusing first on the effects of the pandemic on mental health in children and their parents, and subsequently we discuss findings in studies performed in adolescents and college students.
4.1. Children and their parents
Due to measures to decrease the spread of the COVID-19 virus, schools have been closed and the opportunity to interact with peers, play outdoors and exercise decreased ( de Lannoy et al., 2020 ; Moore et al., 2020 ), whereas sleep and screen time have increased ( Orgiles et al., 2020 ). Parental stress significantly increased after the school closures ( Hiraoka and Tomoda, 2020 ). Parents experienced financial and health problems and needed to comply with home schooling in addition to their own responsibilities, which affected parental routines. Parents’ financial concerns increased verbal aggression, increased loneliness was associated with child neglect, whereas worries increased physical abuse of the children. In general, wellbeing of the parents significantly affected children's mental health ( Carroll et al., 2020 ). A national survey from the US in June 2020 ( N = 1011) reported worsening of mental health for 26.9% of the parents and 14.3% of the children, whereas the reported effect on physical health was smaller. Lost regular health care and delay in health care visits added to the worsening of children's mental health ( Patrick et al., 2020 ). In Italy (April – May 2020, N = 463) ( Cusinato et al., 2020 ) and in Spain (April 2020, N = 1049) ( Romero et al., 2020 ), parental stress was associated with more conduct problems of their children. In Hong Kong (March 2020, N = 29,202 families), children with special education needs, chronic illnesses, mothers with mental illness, and children coming from single-parent and low income families were reported as more vulnerable to the increased stress levels as a result of the pandemic ( Tso et al., 2020 ). In Brazil (April - May 2020, N = 289), parents reported anxiety in 19.4% of their children. In particular, children living with a person other than their parents reported higher anxiety levels, especially when a guardian had a lower age and lower educational level ( Garcia de Avila et al., 2020 ). Having a house without an outdoor exit to a garden or terrace significantly predicted psychiatric symptomatology ( Francisco et al., 2020 ). Overall, there are concerns that the risk of child maltreatment might be heightened during the COVID-19 pandemic due to a range of stressors such as increased loneliness, reduced physical activity, economic stress, social distancing, homeschooling, marital conflicts and violence, and intensified child–parent relationships ( Katz et al., 2020 ). In a recent study of 169 preschoolers, increased depressive and externalizing symptoms were observed compared to pre-COVID levels. A structured, predicable home environment adherent to family routines appears to mitigate these adverse effects ( Glynn et al., 2021 ).
4.2. Adolescents
In adolescents, determinants of resilience are less related to the parental situation and stressors associated with parental stress. A large-scale cross-sectional study from China (during the COVID-19 outbreak, N = 3613) revealed that among 3254 adolescents, anxiety and depressive symptoms were common during the COVID-19 pandemic ( Duan et al., 2020 ), as assessed by the Chinese version of the Spence Child Anxiety Scale (SCAS). In another cross-sectional study conducted in China (February – March 2020, N = 1784), following almost 30 days of confinement, depressive and anxiety symptoms were reported in around 23% of adolescents, with an association with less optimism about the pandemic and with being more worried about being infected with COVID-19 ( Xie et al., 2020 ). A Swiss survey study (November 2020, during the second pandemic wave, N = 11,612) found that the youngest age group (14–24 years old, including students) were at higher risk for moderate-severe depressive symptoms (PHQ-9 ≥ 15) compared to individuals over 24 years old, and that this age-dependent effect became more prominent over the course of the pandemic ( https://osf.io/6cseh/ ). A cross-sectional study from China (March -April 2020, N = 7890) reported a prevalence of 21.7% for anxiety and 24.6% for depression symptoms (HADS subscale score >7) ( Li et al., 2021a ). Another study from China (March 2020, N = 8079) revealed that the prevalence of mild to severe depressive symptoms was 43.7% (assessed by the PHQ-9) and anxiety symptoms were 37.4% (assessed by the GAD-7) ( Zhou et al., 2020a ). Being in senior high school ( Zhou et al., 2020a ), female gender ( Zhou et al., 2020a ) ( Chen et al., 2020 ), lack of physical exercise ( Chen et al., 2020 ), and less social support increased the risk for depressive and anxiety symptomatology ( Qi et al., 2020 ). Furthermore, adverse childhood experiences, being exposed to COVID-19 and the presence of fear of exposure to COVID-19 were predictive of elevated levels of PTSD and anxiety in a Chinese cross-sectional cohort (February 2020, N = 6196) ( Guo et al., 2020 ). Moreover, a longitudinal study among Australian adolescents ( N = 248) showed that adolescents experienced significant increases in depressive and anxiety symptoms and a decrease in life satisfaction during the epidemic compared to 12 months leading up to the COVID-19 outbreak. COVID-19 related worries, online learning difficulties, and increased conflict with parents negatively affected the mental health outcomes, whereas adherence to lockdown measures and feeling socially connected during lockdown were protective factors ( Magson et al., 2020 ). In Indonesia, decreased parental support was associated with total mental health difficulties, whereas anxiety due to the COVID-19 pandemic was associated with higher pro-social problems (April –May 2020, N = 113) ( Wiguna et al., 2020 ).
The previous findings seem to imply that the effects of the COVID-19 pandemic were unanimously negative regarding stress, coping and mental outcomes. However, the literature is more nuanced. A longitudinal study from the US ( N = 322) reported significantly lower internalizing, externalizing, and attention problems in adolescents during the lockdown (April 2020) compared to January 2020 (prior to the spread of COVID-19 in the US), which was associated with better family functioning in youth that reported elevated mental health problems before the pandemic ( Penner et al., 2020 ). Even though a decrease in physical activity and an increase in sleep and screen time were reported for adolescents in a Chinese cross-sectional study (May 2020, N = 10,082) ( Yang et al., 2020a ), an Italian study (April 2020, N = 306) showed that the great majority of the adolescents did not notice or only noticed very little changes in psychological well-being in the early phase of the pandemic ( Pigaiani et al., 2020 ). In Belgium and Italy (April - May 2020, N = 825), 5% of the participants reported having increased mental health care needs during the pandemic and 44% reported stability in needs for mental health care, with another 52% of the assessed youth reported no need for mental health care either before or after the pandemic ( Marchini et al., 2020 ). A study from Japan focusing on monthly suicide rates of people younger than 20 years old (January – May 2020, N = 138), found that suicide rates from March 2020 to May 2020 slightly decreased during the school closure time and were not significantly different from the previous two years ( Isumi et al., 2020 ). In Canada (March 2020, N = 683), almost half of a study sample of adolescents reported that the pandemic also exerted positive effects, with more time to spend with family and more time for exercise and hobbies. In addition, suicidal thoughts were reported to be lower than 6%. The type of motivation for social distancing was found to be associated with psychiatric symptomatology: social distancing due to fear of personally getting sick or to avoid judgement was related to higher anxiety, whereas social distancing due to the preference of staying home was associated with less anxiety and depressive symptoms ( Oosterhoff et al., 2020 ).
4.3. College students
Among university students in Spain (March 2020, N = 2530), moderate to extremely severe levels of anxiety, depression, and stress were reported by 21%, 34%, and 28% of the participants, respectively ( Odriozola-Gonzalez et al., 2020 ). In a Chinese cross-sectional study (February – March 2020, N = 407), the incidence of concerns about somatic symptoms, assessed by a somatic self-rating scale among college students, was 35%, mainly related to concerns regarding COVID-19 ( Liu et al., 2020a ). In Bangladesh (May 2020, N = 476), over 80% of students exhibited any form of (mild to severe) depressive and anxiety symptoms, also related to worrying about academic activities ( Islam et al., 2020 ). In France (April – May 2020, N = 69,054), the prevalence of suicidal thoughts, severe depression, and high levels of anxiety were 11%, 16%, and 28%, respectively ( Wathelet et al., 2020 ). In separate studies, female gender, social isolation, low quality of social relations were found as risk factors for lower mental health ( Wathelet et al., 2020 ). In a US study (April 2020, N = 195), 71% of college students reported increased stress and anxiety, worry about their own and loved ones’ health, sleep disruptions, difficulty with concentration, and concerns about academic performance as pandemic-related stressors ( Son et al., 2020 ). For Chinese college students, 25% of the students reported mild to moderate anxiety when cross-sectionally assessed during the pandemic ( N = 7143), with living in urban areas, income stability, social support, and living with parents as protective factors against anxiety ( Cao et al., 2020 ). Worry about the economic influences of the pandemic, the academic delays and the influence of the pandemic on daily life also contributed to students’ anxiety ( Cao et al., 2020 ). In a Dutch study which ecologically followed students before and during the lockdown (March 2020, N = 78), mood homeostasis decreased significantly during lockdown, a finding that was in turn associated with lower mood and decreased engagement in activities that improved mood. Also, participants with previous mental illness showed a significantly higher decrease in mood homeostasis ( Taquet et al., 2020 ). In Italy (March – April 2020, N = 934), students’ concerns about the COVID-19 pandemic increased PTSD symptoms, whereas positive thoughts about managing the epidemic showed the opposite effect ( Nania et al., 2020 ). Another longitudinal study conducted in the US ( N = 675) showed that a group of college students reported a slight improvement in internalizing symptoms, but worsening of externalizing symptoms and attention when assessed before (beginning of Spring semester 2020) and during the pandemic (end of Spring semester 2020) ( Copeland et al., 2021 ). Around 70% of a sample of 950 US students (March 2020) reported that using a coping strategy such as staying connected, trying to relax, keeping busy, having a day-to-day routine, hobbies, doing school work and exercising, were protective factors during the pandemic ( Waselewski et al., 2020 ). A cohort from the Zurich Project on the Social Development from Childhood to Adulthood ( N = 768) was assessed before the pandemic at the age of 20 and during the pandemic at the age of 22, and it was found that even though internalizing symptoms decreased, stress levels and anger increased during the pandemic. Moreover, only 30.5% reported feeling notably worse, whereas others were either feeling the same or better ( Shanahan et al., 2020 ).
Conclusion: In general, the pandemic has had negative effects on the mental health of children, adolescents, and students. Nevertheless, the effects vary widely within and across groups, and there are many methodological shortcomings in the current literature which is often cross-sectional and relies on self-report. Moreover, it is difficult to directly compare results across many of the studies. In children and younger adolescents, parental stress and decreased physical activity seem to be important risk factors for worse mental health, but for adolescents and students, COVID-19-and academic related worries, familial conflicts, loneliness, and not engaging in health behaviors seem to be important risk factors. Although children, adolescent, and students seem particularly vulnerable for the negative effects of the pandemic in general, there are also some studies finding signs of resilience, such as the use of effective coping strategies. Findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in children, adolescents and college students are presented in Table 3 .
The impact of COVID-19 on stress resilience and mental health in parents, children, adolescents, and college students.
| Canadian children 5–17 years old | Precise period unknown, but during the initial period of the COVID-19 crisis | Cross-sectional, = 1472 (mean age of age group 5–11 years = 8.12 (±2.04), mean age of age group 12–17 years = 14.85 (±1.68), 52.6% female) | The impact of COVID-19 restrictions on movement and play behaviours in children and youth (parent-reported) | Being a volunteer participant of the Manu/Matchbox consumer online database | There was a significant decline in all physical activities in both children and youth. The highest decline was observed in outdoor physical activity and sport. Leisure screen time and social media use was higher than before. | |
| Italian and Spanish children 3 to 18 years old | Italy: March 25 – April 9 2020,, Spain: March 31 – April 15 2020,, data collection in both countries started 15 days after lockdown | Cross-sectional, = 1143 (mean age 9.08 years (± 4.22), 47.5% female) | Emotional impact of the quarantine on children and adolescents from Italy and Spain (parent-reported) | Unknown | Children had more difficulty concentrating (76.6%), felt more bored than usual (52%), were more irritable (39%), were more restless (38.8%), were more nervous (38%), felt lonelier (31.3%), were more uneasy (30.4%), and more worried. | |
| Japanese parents of 0–18 year old children | April 29–30 2020, many children had remained at home from school from March 2 to at least until the end of April 2020 | Cross-sectional, = 353 (mean age 37.6 (±6.11), 78% female) | Qualitative structure of parenting stress | Unknown | Personal distress scores (Parenting Stress Index- Short Form) before school closures and after school closures were 2.39 (SD = 0.80) and 2.49 (SD = 0.72), respectively. Parents’ current personal distress levels were significantly higher ( = 4.89, < 0.01, = 0.12) than before the school closures had occurred. | |
| Canadian families of young children | April 20 -May 15 2020, | Cross-sectional, = 235 mothers and = 126 father from 254 families (children's mean age = 6 years (±2.0), mothers’ mean age = 37 years (±4.8), fathers’ mean age = 39 years (±5.5)) | Health behaviours, level of stress, financial and food security among Canadian families with young children. | Being a family with at least one child between 18 months and 5 years of age at the time of registration for the study, living within the Guelph-Wellington area in Ontario, being comfortable with English to respond to survey questionnaires | More than half the sample (mothers, 70%; fathers, 60%; children, 51%) stated their eating and meal routines has changed since COVID-19. Screen time increased among 74% of mothers, 61% of fathers, and 87% of children and physical activity decreased among 59% of mothers, 52% of fathers, and 52% of children | |
| US parents and their children (aged < 18 years) | June 2020 | Cross-sectional, N = 1011 | Physical and emotional well-being of parents and children through early June 2020, using March 2020 as the reference point for the period before or at the beginning of the pandemic | Being a participating parent in the Ipsos KnowledgePanel and having at least 1 child aged <18 years old in the household | Compared to March 2020, 26.9% of parents reported worsening of mental health, 14.3% reported worsening in their children's behavioural health and 9.6% reported worsening of both their mental health and their children's behavioural health. Female and unmarried parents reported higher rates of worsening of their own mental health. | |
| Italian parents of children aged 5–17 years | April 25 – May 8 2020, | Cross-sectional, = 463 parents’ (mean age = 43.4 years (±5.88), 90.5% female, children's mean age = 9.72 (±3.29, 43.8% female) | Potential risk and protective factors for parents’ and children's well-being during a potentially traumatic event such as the COVID-19 quarantine | Having at least one child aged 5 to 17 years old living at home and having answered both child behavior questionnaires in their entirety | Confinement measures and changes in daily routine negatively affected parents’ psychological dimensions, thus exposing children to a significant risk for their well-being. | |
| Caregivers of Spanish children | April 2020 (precise period unknown, lockdown started on March 142,020 and on March 29, even more restrictive measures were imposed) | Cross-sectional, = 1049 caregivers (data of = 1123 children with a mean age of 7.26 years (±2.39), 50% female) | Effects of the Spanish confinement derived from the COVID-19 crisis on children and their families, accounting for child's age | Unknown | Preschool children showed a higher increase (38.2%) in conduct problems and hyperactivity as compared to their school-aged counterparts (20.3–24.4%). Child adjustment was influenced by a chain of effects, derived from parents’ perceived distress and emotional response to the COVID-19 crisis, via parenting distress and specific parenting practices. | |
| Parents with 2–12 year old children from Hong Kong | March 2020 (precise period unknown) | Cross-sectional, = 29,202 families ( = 12,163 parents with children aged 2–5 years and = 17,029 parents with children aged 6–12 years. Mean age children 6.50 years (±2.84), 48.6% female | Characteristics of children vulnerable to the negative impacts of the COVID-19 pandemic factors that can promote psychosocial wellbeing within families during the COVID-1 pandemic (parent-reported) | Being a parent of a child aged 2–12 years | Compared to the reference means, children demonstrated significantly more psychosocial problems measured by the SDQ total difficulties score (12.79 (5.13) for age 2–5 and 11.59 (5.57) for age 6–12), fewer prosocial behaviours measured by the SDQ prosocial behavior score (6.19 (1.97) for age 2–5 and 6.49 (2.00) for age 6–12), and poorer functioning measured by PedsQL total score (79.83 (13.38) for age 2–5 and 79.67 (13.41) for age 6–12). Compared to the reference group, their parents exhibited higher levels of parenting stress measured by the PSS scale (48.88 (10.10) for age 2–5 and 49.72 (10.72) for age 6–12). | |
| Brazilian children aged 6–12 years and their guardians (mean age = 38.97 years (±6.54)) | April 25 – May 25 2020, | Cross-sectional, = 289 (157 girls and 132 boys, mean age 8.84 years (±2.05), 54.3% female | Prevalence of anxiety (Children's Anxiety Questionnaire; CAQ) among Brazilian children and its associated factors during social distancing during COVID-19 (parent-reported) | Unknown | The prevalence of anxiety among the children during the COVID-19 pandemic in this group was 19.4% ( = 56), according to the CAQ, and 21.8% ( = 63), according to the NRS. These results are higher than the prevalence reported for children under normal conditions (6.5%). | |
| Italian, Spanish and Portuguese children and adolescents aged 3–18 years old | 15 days between March and April 2020 (precise period unknown) | Cross-sectional, = 1480 children (mean age 9.15 years (±4.27), 47.2& female) | Immediate psychological and behavioural symptoms (anxiety, mood, sleep, behavioural, feeding, and cognitive alterations) associated with COVID-19 quarantine in children and adolescents, its explanatory factors and differences across countries (parent-reported) | Unknown | An increase in children's psychological and behavioural symptoms, increased screen-time, reduced physical activity, and more sleep hours/night was observed, with Portuguese and Spanish children presenting more psychological and behavioural symptoms compared with Italian children. Having an outdoor exit in the house was associated with lower levels of psychological and behavioural symptomatology. | |
| US Mother-child pairs of preschool children in Southern California | May 5 2020, (On March 19 2020,, a state-wide stay at home order was issued which was in place until May 8 2020,) | Cross-sectional, = 169 children (mean age 4.1 years (±0.93, 46.7% female) | Mental health symptoms in American preschool children during the COVID-19 pandemic (parent-reported)) | Having completed the survey by June 9, 2020 | 39.9% of the children scored above the recommended cut-off (≥3) for referral for further evaluation for clinical depression. The proportion of children scoring above the cut-off was elevated compared to those reported in a pre-COVID German population–based sample (5.7%; Fuhrmann et al., 2014) and more similar to a pre-COVID high risk US sample enriched for depression (43.7%); Luby et al., 2012). | |
| Chinese children and adolescents | During the COVID-19 outbreak (precise period unknown) | Cross-sectional, = 3613 (9.9% aged 7–12 years, 90.1% aged 13–18 years, 49.9% female) | Psychological effects on children and adolescents associated with the early phase of COVID-19 pandemic | Being in high school (grade one to grade three; aged 7–18 years) in mainland China | Findings indicate that the COVID-19 outbreak has had a significant psychosocial impact on children and adolescents. 22.28% was suffering from depressive symptoms and levels of anxiety in children and adolescents during the epidemic were much higher than before the pandemic. | |
| Chinese children | February 28 – March 5 2020,, participants had been restricted to home for a mean (SD) of 33.7 (2.1) days when completing the survey | Cross-sectional, = 1784 (43.3% female) | Depressive and anxiety symptoms among adolescents in Hubei province, China | Being in primary school (grade 2 through 6) in Hubei province | 22.6% and 18.9% of adolescents reported having depressive symptoms and anxiety symptoms, respectively. | |
| Li, W. et al., 2021 | Chinese high school students | March 30 - April 7 2020, (quarantine was imposed in Wuhan from January 23, 2020, to April 8, 2020) | Cross-sectional, = 7890 (37.6% aged 12–14 years, 35.1% aged 15–16 years, 27.2% aged 17–18 years, 52.1% female) | Prevalence of depression and anxiety and their associations with lifestyle changes among adolescents in Wuhan | Being a current resident in Wuhan, aged 12–18 years old, not having a diagnosis of COVID-19 | During the COVID-19 quarantine period, more than 20% of adolescents had anxiety and depression. The prevalence was 21.7% (n = 1708) for anxiety and 24.6% (n = 1941) for depression. |
| The Swiss Corona Stress Study: second pandemic wave, November 2020 (pre-print: ) | General Swiss population aged ≥14 years | November 11–19 2020 (during the second pandemic wave) | Cross-sectional, = 11,612 (mean age 39.3 years (±13.4), 73.8% female) | Stress levels and depressive symptoms (PHQ-9) in comparison to the first survey during lockdown in April 2020 | Living in Switzerland, being ≥14 years | While the proportion of people reporting maximum stress levels was around 11% during the April lockdown, it rose to 20% in the second pandemic wave in November. The proportion of respondents with moderately severe or severe depressive symptoms was 3% before the pandemic, 9% during the April lockdown, and 12% during May, it increased to 18% in November. |
| Zhou, S. J. et al., 2020 | Chinese adolescents | March 8 - 15 2020 | Cross-sectional, = 8079 (median age 16 years, 53.5% female) | Prevalence rate and socio-demographic correlates of depressive and anxiety symptoms | Having an age of 12–18 years | The prevalence of depressive symptoms, anxiety symptoms, and a combination of depressive and anxiety symptoms was 43.7%, 37.4%, and 31.3%, respectively, among Chinese high school students during the COVID-19 outbreak. |
| Chinese children and adolescents | April 16 - 23 2020 | Cross-sectional, = 1109 ( = 343 aged 6–8 years, = 310 ages 9–12 years, = 353 13–15 years, 45.5% female) | Prevalence of depression and anxiety among Chinese children and adolescents | Unknown | 112 (11.78%) adolescents with depression, 196 (18.92%) adolescents with anxiety, and 68 (6.56%) adolescents with both depression and anxiety were identified. | |
| Chinese adolescents | March 8 - 15 2020 | Cross-sectional, = 7202 (median age 16.0 years (interquartile range [IQR] = 2.0, range 14.0–18.0), 53.6% female) | The association between the levels of social support and mental health) among Chinese adolescents | Being a junior high school or senior high school student, being a WeChat or QQ user, having submitted only one survey using the same IP address | COVID-19 exposure was associated with a higher prevalence of depression symptoms (OR = 1.38, 95% CI: 1.14–1.66) and anxiety symptoms (OR = 1.26, 95% CI: 1.04–1.52). Only 24.6% of adolescents reported high levels of social support. | |
| Chinese adolescents | February 8 −27 2020 | Cross-sectional, = 6196 (age range 11–18 years, 52.10% female) | Levels of anxiety and post-traumatic stress symptoms and whether pre-pandemic maltreatment experiences exacerbate this impact on mental health in adolescents | Being a student at one of the selected high school and middle schools in Zhenping County of Henan Province | Exposure to COVID-19 predicted higher levels of PTSS and anxiety with effect sizes ranging from 0.06 to 0.15 (standardized betas). The largest variance in PTSS and anxiety problems was explained by adverse childhood events (ACEs), with more pre-pandemic maltreatment experiences predicting more PTSS and more anxiety. | |
| Australian adolescents | Two waves; T1 (12 months leading up to the COVID-19 outbreak) and T2 (two months following the implementation of government restrictions and online learning). | Longitudinal, = 248 (mean age 14.4 years (± 0.5), 51% female, 81.8% Caucasian) | The impact of the COVID-19 pandemic on adolescents’ mental health | Being part of the larger longitudinal Risks to Adolescent Wellbeing Project (the RAW Project) | Significant increases in adolescents’ symptoms of depression, (t(1, 247) = 6.26, p < 0.001, d = 0.15), and anxiety, (t(1, 244) = 5.26, p < 0.001, d = 0.40), and a significant decrease in life satisfaction, (t(1, 244) = −5.26, p < 0.001, d = 0.61) from T1 (before the pandemic) to T2 (2 months into the pandemic) was observed. | |
| Indonesian adolescents | April 15 - May 10 2020, | Cross-sectional, = 113 mean age 14.07 years (±2.18), 46.9% female) | Behavioural and emotional problems during the pandemic | Being a family with at least one child of 11–17 years old, informed consent by parents and child | 10.6% of the participating adolescents were at risk for emotional problems, 15.0% for conduct behavior, 38.1% for peer-relationship problems, 8% for hyperactivity behavior, and 28.3% for pro-social behavior problems. | |
| US adolescents | Baseline measure (January 2020, prior to the spread of COVID-19 in the United States) and follow-up measures (mid-April 2020, 1 Month After School In-Person Closure) | Longitudinal, = 322 (mean age 11.99 years (± 1.16), 55.0% female, 72.7% Hispanic/Latin, 9.3% = Black or African American, 5.9% Multiple Races, 5.0% Asian, 1.6% White, 1.2% American Indian, and 4.3% ‘other’ | Longitudinal change in mental health before and during the pandemic | Being a public school student (grade 5–8) | For adolescents who had elevated levels of internalizing, attention, externalizing, or total problems before the pandemic, a significant reduction in mental health problems from baseline to follow-up measures was observed, controlling for age and gender. | |
| Yang, S. et al., 2020 | Chinese adolescents | Early May 2020 (precise period unknown) | Cross-sectional, = 10,082 (mean age 17.5 years (±1.2), 71.7% female) | The impact of the pandemic on obesity, weight, BMI and activity patterns among youth | Unknown | During the COVID-19 lockdown, the prevalence of overweight/obesity and obesity significantly increased in all participating adolescents and significant changes were observed in patterns of all forms of physical activity, with more adolescents having increased their sedentary, sleeping, and screen time. |
| Italian adolescents | April 1 – 10 2020 | Cross-sectional, = 306 (mean age 18.1 years (±0.9), 27.1% female) | Lifestyle behaviours, coping strategies and well-being among Italian adolescents | Being 18 years or older, being a student at one of the three participating high schools located in Verona, Milan and Rome | Although most students (50.7%))did not report or reported only a little change in subjective well-being, 49.4% and 39.9% reported a change in subjective well-being and symptoms of anxiety respectively. Factors predicting a change in subjective wellbeing included adaptive coping strategies (physical activity, engaging in different activities than before), family issues (finding hard to stay at home, having quarrels), school-related behaviours (fearing a negative educational outcome) and female gender. | |
| Italian, Belgian adolescents | April 7 - May 4 2020, (just after the enactment of lockdown measures in Italy (March 9) and Belgium (March 18)) | Cross-sectional, = 825 (median age 20 years (IQR 20–24 years), 74.7% female, 53.7% living in Belgium, 46.3% living in Italy) | The relationship between resilience and loneliness and the emergence of new or increased mental health care needs (MHCNs) during lockdown measures | Speaking French or Italian, being a resident in Belgium or Italy | More loneliness, and lower resilience was observed in youth who needed help prior/during lockdown. | |
| Japanese adolescents | January 2018 - May 2020 | Cross-sectional, = 138 | Suicide rates per month between January 2018 and May 2020 from public data on suicide statistics compiled by the Ministry of Health, Labor and Welfare | Being younger than 20 years old | During the school closure due to the COVID-19 crisis (March to May 2020), no significant change of suicide rates was found (incidence rate ratio (IRR) =1.15, 95% confidence interval (CI): 0.81 to 1.64), compared with the same months in 2018 and 2019. | |
| Oosterhoff, B. et al., 2020 | US adolescents | March 29–30 2020 (two weeks after COVID-19 was declared a national emergency in the US) | Cross-sectional, = 683 (mean age 16.35 years (±1.13), 75.3% female, 77.0% white/Caucasian, 15.5% Hispanic/Latino, 5.6% African-American/Black, 11.2% Asian American/Pacific Islander, 3.2% American Indian/Alaskan Native, 2.9% other | Connections between social distancing motivation, anxiety and depressive symptoms and social health (belongingness and burdensomeness) | Being 13 – 18 years old | Almost all respondents (98.1%) reported engaging in at least a little social distancing. No evidence of an association between degree of social distancing engagement and any indicator of mental or social health was found. |
| Spanish university members | March 28 – April 4 2020, (during the first days of confinement | Cross-sectional, = 3707 (mean age 27.9 years (±12.4), 66,1% female, 76.8% students) | The emotional impact of COVID-19 in the university community, using the Depression Anxiety Stress Scale (DASS-21) and the Impact of Event Scale (IES) | Being a university member living in Spain | 50.43% of the participating university members reported moderate to severe emotional impact of the COVID-19 outbreak 21.34%, 34.19% and 28.14% of the respondents reported moderate to extremely severe scores of anxiety, depression and stress, respectively. | |
| Liu, S., et al., 2020 | Chinese primary and university students | February - March 2020 (precise period unknown) | Cross-sectional, = 407 ( = 209 primary school, = 198 college, 60.4% female) | The impact of the COVID −19 pandemic on primary and university students | Being a university or primary school student in Sichuan Province | Somatic symptoms were observed in 34.85% of the college students and in 2.39% of the primary school students. Somatic symptoms were associated with concerns about COVID-19. |
| Bangladeshi university students | May 6 – 12 2020 (all education institutions were closed initially from March 18 to March 31, 2020 and later extended to the mid of June 2020 in phases) | Cross-sectional, = 476 (24.2% aged 17–20 years, 67% aged 21–24 years, 8.8% aged >24 years, 32,8% female)) | The prevalence of depression and anxiety of university students in Bangladesh | Being a university student | During the ongoing COVID-19 pandemic, a large percentage of Bangladeshi university students have been suffering from depression and anxiety symptoms with 82.4% of the students reported to have mild to severe depressive symptoms and 87.7% reported to have mild to severe anxiety symptoms. | |
| French university students | April 17 2020, - unknown | Cross-sectional, = 69,054 (median age 20 years (IQR 18–22 years), 72,8% female) | The prevalence of self-reported suicidal thoughts and symptoms of distress, stress, depression, and anxiety in university students during the COVID-19 pandemic. | Being a university student | Prevalence rates were 11.4%, for suicidal thoughts, 22.4%, for severe distress, 24.7%, for high levels of perceived stress, 16.1% for severe depression, and 27.5% for high levels of anxiety. Factors associated with all mental health issues were having a low level of physical activity, not living with family, having a weak sense of integration, having a low quality of social relations, and receiving low-quality information. | |
| US undergraduate students | One month after the stay-at-home order in April 2020 (precise period unknown) | Cross-sectional, = 195 (mean age = 20.7 years (± 1.7), 56,9% female) | The impact of the pandemic on the mental health of college students (general stress, depressive and suicidal thoughts) | Being a undergraduate student | 71% of the students reported that their stress and anxiety had increased due to the COVID-19 pandemic, 91% indicated that the pandemic increased the level of fear and worry about their own health and the health of their loved ones, 86% reported disruptions to their sleep patterns caused by the COVID-19 pandemic, 44% mentioned having experiencing some depressive thoughts during the COVID-19 pandemic, and 8% stated that the pandemic has led to some suicidal thoughts. | |
| Chinese college students | During the COVID-19 outbreak (precise period unknown) | Cross-sectional, = 7143 (69.65% female) | The impact of the pandemic on the mental health of college students | Being a college student | 24.9% of college students experienced COVID-19 related anxiety. Living in urban areas (OR= 0.810, 95% CI = 0.709 - 0.925), stability of students’ family income (OR= 0.726, 95% CI = 0.645 - 0.817), and living with parents (OR= 0.752, 95% CI = 0.596 - 0.950) were protective factor against anxiety. | |
| Dutch students | March 16 – 29 2020 (ecological momentary assessment 4 times every day) | Longitudinal, = 78 (mean age 20.4 years (± 3.7), 76% female) | Mood homeostasis | Being a student | Mood homeostasis was significantly higher before than during lockdown with mood homeostasis decreasing significantly more among people with vs without a history of mental illness. | |
| Italian students | March –April 2020 (precise period unknown but during the peak of COVID-19 in Italy) | Cross-sectional, = 934 (mean age 23.6 years (± 4.9), 79,6% female) | Risk and protective factors associated with PTSD during the peak of COVID-19 in Italy | Being a university student | Students’ COVID-19 related concerns increased by 30% the likelihood of having PTSD. However, when the interaction of health engagement with risk and protective factors was taken into account, the association between concerns and PTSD decreased by roughly 20%. | |
| US college students) | Two waves; T0 (beginning of the Spring semester 2020), T1 (end of the Spring semester 2020) and daily surveys across the school year | Longitudinal, = 675 (91.4% aged 18 years, 7.6% aged 19 years, 0.6% aged 20 years, 0.3% aged 21 years, 74,1% female) | The impact of the pandemic on the mental health of college students | Being a full-time, first-year UVM undergraduate student, being aged 18 to 25 years old, having an iPhone 5 or newer (for app compatibility) | Students reported how disruptive COVID had been to them personally. The mean level of disruptiveness (total score ranging from 0 to 10) was 7.8 (SD=2.1),with 87.3% reporting a score of 6 or greater. After the onset of the COVID-19 pandemic, externalizing problems and attention problems increased after the onset of COVID, while internalizing symptoms did not increase. | |
| US youth | March 20 2020, | Cross-sectional, = 950 (mean age 18.9 years (±2.8), 52.1% female), 67.7% White, 14.5% Black, 5.4% Asian, 12.4% other race) | The needs, emotions, and coping behaviours of US youth during COVID-19 | Being part of the MyVoice cohort | 32.6% of the respondents felt resources they needed, or could need, were readily available, while 35.2% of participants felt resources were difficult to access or unavailable. Respondents described both emotional responses (27.4%) and coping strategies (69.8%) to handle the impact of COVID-19. | |
| Swiss young adults | Two waves; T0 (before COVID when participants were 20 years old, precise period unknown) and T1 (April 11 – 18 2020, during week 4 of the Swiss national lockdown) | Longitudinal, = 768 (48.1% female) | The influence of previous distress and stressors in emotional distress (PSS) during the COVID-19 pandemic and to investigate how COVID-19-related stressors and coping strategies are associated with emotional distress when pre-pandemic distress was accounted for | Being a participant of the ‘age 20 assessment’ (wave 8) of the Zurich Project on the Social Development from Childhood to Adulthood (z-proso) | Perceived stress ( = 2.91, SD=0.92) and anger ( = 2.59, SD=0.95) during the pandemic was higher compared to perceived stress ( = 2.79, SD=0.95) and anger ( = 2.37, SD=0.75) in the pre-pandemic period (wave 8 z-proso), although no increase in internalizing symptoms was observed. The largest risk factor for emotional distress during COVID-19 was previous emotional distress. | |

5. Elderly people
Elderly people have been more directly affected by the pandemic than younger age groups as the physical impact of COVID-19 is substantially higher in this population. In addition, even though elderly people have higher levels of comorbidities that need to be taken care of, the availability of physician appointments and medical care has also been negatively impacted by the lockdown periods ( Spalletta et al., 2020 ). In general, elderly people have lower access to technology and social media, which can make it more difficult to compensate for lockdown-related changes and have adequate access to food, news, and social interaction ( Martins Van Jaarsveld, 2020 ). They are more isolated from their families and social connections, leading to an increased risk of developing psychiatric symptoms and therefore impairing their cognitive performance and daily functioning ( Yang et al., 2020b ). Elderly people also have been subject to change in health behaviors. A Cross-sectional study on the psychological, social and health-related challenges in Spanish older adults during the first COVID-19 wave (March 2020, N = 528) showed that while a quarter of the elderly people could increase their intellectual activity during the first lockdown, more than 60% of them reported decreased physical activity ( Rodriguez-Gonzalez et al., 2020 ). In Greece, 80% of the elderly reported moderate to severe anxiety and depression levels three weeks after a national lockdown (March 2020, N = 103) ( Parlapani et al., 2020 ), and these effects were also apparent in elderly with dementia in Argentina after the first 8 weeks of quarantine ( N = 119) ( Cohen et al., 2020 ). A German study (March – May 2020, N = 15,308) showed that while generalized anxiety significantly decreased with age, COVID-19 related fear significantly increased in elderly participants ( Schweda et al., 2021 ), even though this was not found in other studies.
In contrast, despite all the challenges that the elderly population faces, lower rates of psychiatric symptoms in this population compared to younger age groups were reported. During the COVID-19 pandemic in Germany, older individuals showed higher life satisfaction and quality of life and lower levels of trait anxiety compared to younger age groups (March – April 2020, N = 494) ( Bidzan-Bluma et al., 2020 ). A cross-sectional study in the US (March – April 2020, N = 833) showed that subjects of 60–70 years of age reported higher stress levels compared to older people (>71 years) ( Emerson, 2020 ). Another US survey study with elderly (March 2020, N = 825) revealed that less than 15% of the participants reported pandemic-related stress from confinement/restrictions, isolation, loneliness and concern for others and the unknown future. In particular, stress from concern for others and the unknown future was associated with poorer psychological well-being ( Whitehead and Torossian, 2021 ). In Spain (March - April 2020, N = 1639) ( Garcia-Fernandez et al., 2020 ) and the UK (April - May 2020, N = 15,530) ( Li and Wang, 2020 ), elderly people reported less psychopathology compared to younger people. Also, when compared to younger age groups, lower COVID-19 Peritraumatic Distress Index (CPDI) scores (Brazil, March 2020, N = 638) ( Zhang et al., 2021 ), lower rates of suicidal ideation (Greece, April - May 2020, N = 5116) ( Papadopoulou et al., 2021 ), and lower rates of depression, anxiety and stress (Northern Spain, March - April 2020, N = 1933), were reported in the elderly ( Ozamiz-Etxebarria et al., 2020 ). These findings might indicate that at least a sub-population of the elderly is remarkable resilient, potentially due to their complex experiences during their previous lives. The discrepancy of the findings in elderly people might heavily depend on the geographical location, timing of the measurements, and the nature of the assessed sample.
5.1. Elderly with cognitive symptoms and dementia
Elderly with cognitive symptoms may be more prone to the mental effects of the pandemic. In Italy (April – May 2020, N = 126), daily physical activity and adherence to a healthy diet were found to be decreased in this population. However, less than 20% of the participants reported depression and anxiety, which was related to living alone, having less social interaction and reduction in leisure activities ( Di Santo et al., 2020 ). Based on a review on patients with a dementia diagnosis (summarizing 20 studies from March 2020 and June 2020), anxiety, apathy, and agitation were the most reported neuropsychiatric symptoms during the COVID-19 pandemic, probably due to decreased social interaction ( Simonetti et al., 2020 ).
Conclusion: Recent evidence points out that even though elderly people are more vulnerable to the physical effects of COVID-19, they also report lower psychopathology during the pandemic period compared to younger age groups. In the elderly population, patients with cognitive decline may be more vulnerable to the mental health effects of the pandemic. However, there is quite some heterogeneity within groups, and a significant proportion of the elderly people may still be at risk for worse mental health outcomes. Table 4 presents findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in elderly people.
The impact of COVID-19 on stress resilience and mental health in elderly people.
| Italian patients with mild and major neurocognitive disorders (NCD) | January - April 2020 (precise period unknown) | Cross-sectional, = 251 canceled scheduled appointments | Number of canceled appointments for patients with NCD due to COVID-19 compared to these numbers in January – April 2019 | Having recorded the number of appointments that were canceled at the Santa Lucia Foundation IRCCS due to the government-enforced reduction of non-urgent healthcare services in Italy during the lockdown | 251 scheduled appointments were canceled (follow-up appointments = 211; first-time appointments = 40). There was a significant difference in the proportion of canceled follow-up and first-time appointments in March and April 2020 compared to the same periods in 2019. | |
| Spanish adults | March 2020, during the lockdown of the COVID-19 first wave (precise period unknown) | Cross-sectional, = 528 (mean age 69.25 years (±6.75), 64.6% female) | Psychological and social implications and health-related behaviours involved in the lockdown due to the COVID-19 pandemic | Being 60 years or older, living in Galicia (North-West region of Spain, Europe) during the lockdown declared in March 2020 by the Spanish government due to the COVID-19 pandemic | 76.5% of sample belonged to active aging organizations before lockdown, but only 33.7% continued to be active during lockdown; 65.7% performed less physical activity than before the lockdown; 25.6% of the sample reported an increase in intellectual activity; 66.3% feel that their physical health will not worsen; 67.6% believe that this situation will not have a positive effect. | |
| Greek adults | The survey was online for a period of three days, three weeks after a national lockdown had been imposed in Greece (March 23 2020,) | Cross-sectional, = 103 (mean age 69.85 years (±5.26), 61.2% female) | Psychological response of older adults during the acute phase of the pandemic in Greece | Being older than 60 years, having online access to the survey via social media | 81.6% reported moderate to severe depressive symptoms; 84.5% reported moderate to severe anxiety symptoms; 37.9% reported disrupted sleep. Females disproportionately reported significantly higher levels of COVID-19–related fear, depression, sleep disturbances, and an intolerance of uncertainty. | |
| Cohen, G. et al., 2020 | Argentinian family members of patients of the Aging and Memory Center of FLENI with Alzheimer´s dementia (AD) and related disorders | After the first 8 weeks of quarantine (starting medio March 2020, precise period unknown) | Cross-sectional, = 119 caregivers of persons with AD or related dementia living at home (mean age of patients 81.16 years (±7.03), 64.7% female) | To study the extent mandatory quarantine due to COVID-19 affected behavioural symptoms in subjects with dementia after the first 8 weeks of quarantine | Being a family member of patients of the Aging and Memory Center of FLENI in Argentina, with AD and related disorders | Family members reported 60.5% new onset or exacerbation of pre-existing behavioural symptoms; 33% anxiety, 12.8% depression, and 14.7% sleep disorders were reported; 40% reported increasing gait difficulties; 20% increased use of antipsychotics, 15% benzodiazepines, 6% hypnotics, and 10% antidepressants. 76% discontinued physical therapy, 91% occupational therapy, and 77% cognitive rehabilitation. |
| German general population | March 1 - May 4 2020, (period in which people lived under the curtailment of their individual freedoms and partly unprecedented governmental restrictions) | Cross-sectional, = 15,308 (13.9% aged 18–24 years, 24.8% aged 25–34 years, 23.0% aged 35–44 years, 19.0% aged 45–54 years, 14.2% aged 55–64 years, 4.4% aged 65–74 years, 0.8% aged >75 years, 70.7% female) | Psychological reactions in response to real or perceived COVID-19 infection threats | Being involved in social media groups, living under the curtailment of individual freedom between March 10 - May 4 2020, | COVID-19 related fear correlated with generalized anxiety (ρ = 0.377, < 0.001, 95%-CI = [0.363: 0.391]). COVID-19 related fear increased with age; generalized anxiety decreased with age. | |
| German and Polish adults | March 27 - end of April 2020 (during the period of COVID-19 restrictions) | Cross-sectional, = 494 (mean age 42.97 years (±9.77), 72% female, 80.6% German, 19.4% Polish) | Predictors of quality of life, well-being, sleep, and life satisfaction, including factors such as risk behavior, trait anxiety, feeling of threat, sleep quality, and optimism, during the pandemic in older people from Germany and Poland | Being 18 years or older, having access to the internet in order to fill out the study survey | Older people rated quality of life, life satisfaction, and well-being higher than young people and scored less than young people on anxiety (mean difference= −9.19, SE = 1.90, < 0.01) and greater than young people on risk tolerance (mean difference = 1.38, SE = 0.33, < 0.01 difference=0.91, SE = 0.31, < 0.05). | |
| US adults aged 60 years and older | March 30 - April 12 2020, | Cross-sectional, = 833 (age range 60–80 years, 62.8% aged 60–70 years, 80.5% female, 96.0% White, 1.9% Black or African American, 0.2% American Indian or Alaska Native, 1.6% Asian, 2.1% other) | The impact of sheltering in place and social distancing among adults aged 60 and older | Being 60 years or older, living in the US and practicing social distancing between March 30 and April 12, 2020 | 36% reported being stressed and 42.5% reported being lonely. Loneliness increased with time of social distancing. | |
| US adults aged 60 and older | March 22–23 2020 (period in which stay-at-home orders were beginning to be issued) | Cross-sectional, = 825 (63.8% aged 60–69 years, 30.7% aged 70–79 years, 5.5% aged ≥80 year, 79,3% female) | Older adults’ reports of what was stressful about the pandemic, and what was joyful and comforting amidst the stress | Being 60 years or older, having access to the online survey | 13.2% reported restrictions and resulting confinement as a source of stress and 31.6% mentioned family or friends as the most frequently reported source of joy or comfort. Stress over concern for others, the unknown future, and contracting the virus was significantly associated with poorer psychological well-being; whereas faith, exercise/self-care, and nature were associated with more positive psychological well-being. | |
| Spanish adults | March 29 - April 5 2020,, covering the peak of the COVID-19 infection in Spain | Cross-sectional, = 1639 ( = 150 ≥ 60 years old, 58.7% female, = 1489 <60 years old, 69.2% female) | COVID-19 outbreak-related emotional symptoms, gender differences, and the relationship between the emotional state and environmental features in the elderly | Not being a healthcare worker, not having a current or past mental illness | The ≥60 age group showed lower depression scores and lower acute distress scores than the <60 age group. There were no gender differences in any of the clinical measures. | |
| UK adults aged from 18 to over 65 years old | April 24 – 30 2020 | Cross-sectional, = 15,530 | The prevalence and predictors of general psychiatric disorders and loneliness after the first diagnosis of COVID-19 | Having participated in the first wave of Understanding Society COVID-19 Study | This study showed high prevalence rates of general psychiatric disorders (29.2%) and loneliness (35.86%) during the COVID-19 pandemic. People with current or past COVID-19-related symptoms or various disadvantaged socioeconomic backgrounds were at significantly higher risks of general psychiatric disorders and loneliness. | |
| Brazilian adults | March 25 –28 2020 (one month after the first COVID-19 case in Brazil | Cross-sectional, = 638 (18.5% aged 18–25 years, 32.3% aged 26–35 years, 24.4% aged 36–45 years, 13.5% aged 46–55 years, 8.8% aged 56–65 years, 2.5% aged >65 years, 57.7% female) | Mental distress and its associated predictors among adults one month into the COVID-19 crisis in Brazil | Unknown | 52% of the sampled adults experienced mild or moderate distress, and 18.8% suffered severe distress. Adults who were female, younger, more educated, and exercised less reported higher levels of distress. | |
| Greek adults | April 7 - May 3 2020, | Cross-sectional, = 5116 (28.15% aged 35–44 years, 23.60% aged 45–54 years, 73.64% female) | Prevalence of suicidal ideation in the community as well as the risk and protective factors of suicidal ideation during restriction measures in Greece | Unknown | 5.20% reported suicidal thoughts, 14.17% were potential clinical cases of anxiety, and 26.51% of depression. Participants presented significantly higher suicidal ideation rates during the last two weeks of the lockdown compared to its previous two weeks. | |
| Spanish adults | March 11- 18 2020 (55.8% of participants) and April 2–12 2020. (44.2% of participants) | Cross-sectional, = 1933 (mean age 33.80 years (± 16.65), 79.5% female) | Psychological state of the general population during the COBID-19 lockdown | Unknown | More than a quarter of the participants reported symptoms of depression (27.5%), anxiety (26.9%) and stress (26.5%) and as the time spent in lockdown has progressed, psychological symptoms have risen. | |
| Italian adults with mild cognitive impairment (MCI) or subjective cognitive decline (SCD) | April 21 - May 7 2020, | Cross-sectional, = 126 ( = 70 MCI and = 56 SCD patients, mean age 74.29 years (6.51±), 81.0% female) | The effects of COVID-19 and quarantine measures on lifestyles and mental health of elderly at increased risk of dementia | Being 60 years or older, having undergone the last study visit in the preceding 18 months, not having a significant functional impairment in the last study visit, having a diagnosis of MCI according to the International Working Group criteria, and having a cognitive impairment, operationalized as a MMSE score ≥ 20 and ≤ 26 (or ≤ 28 for participants with 16 or more years of education) or as a score under the normative cut-off in at least one domain-specific cognitive test from an extensive neuropsychological battery | Over 1/3 of the sample reduced their physical activity and nearly 70% reported an increase in idle time. Adherence to the Mediterranean diet decreased in almost 1/3 of respondents and over 35% reported weight gain. Social activities were abolished and 1/6 of participants also decreased productive and mental-stimulating activities. 19.8% were depressed, 9.5% anxious, and 9.5% apathetic. | |
6. Pregnant women
During the first days of the pandemic, it was not clear whether a COVID-19 infection would affect pregnant women and whether the virus would be transmitted to the fetus. Many pregnant women therefore avoided visiting hospitals, and obstetricians in India reported that a great majority of their pregnant patients experienced anxiety about their hospital visits during the first wave of the COVID-19 pandemic (April - May 5, 2020, N = 118) ( Nanjundaswamy et al., 2020 ). These worries in pregnant women were related to COVID-19-related concerns about being present in public places, perceived infection risk, visiting hospitals, health of the fetus, delivery concerns, a family member being infected, or transmission of COVID-19 to the baby during delivery ( Akgor et al., 2021 ; Taubman-Ben-Ari et al., 2020 ; Zhang et al., 2020 ). A nationwide cross-sectional study from Mexico (May – June 2020, N = 503) found that 33.2% of pregnant women reported being stressed based on the Perceived Stress Scale, with perceived stress being significantly correlated with later gestational age ( Medina-Jimenez et al., 2020 ). In China (February – March 2020, N = 560), over half of pregnant women reported feeling horrified, apprehensive, or helpless during the pandemic ( Zhang and Ma, 2020 ). A Turkish study reported that half of the 172 enrolled pregnant women in the third trimester reported feeling vulnerable to the effects of the pandemic (April 2020) ( Yassa et al., 2020a ). In a Pakistani (August 2020, N = 552) and Chinese study (February 2020, N = 1947), more than 80% of the pregnant women reported that they themselves and their fetuses were more vulnerable to the effects of the pandemic compared to the general population ( Liu et al., 2020b ; Shahid et al., 2020 ), but moderate to severe anxiety was reported in only 3% ( Liu et al., 2020b ). A systematic review, that included 15 studies examining depression and anxiety symptoms in pregnant or delivered women during the COVID-19 pandemic, reported a pooled overall prevalence of 30% for depression and of 34% for anxiety ( Sun et al., 2020 ). In addition, the prevalence of depression and anxiety symptoms was around two times higher compared to non-pregnant women ( Sun et al., 2020 ). Another systematic review and meta-analysis that included 19 studies about the mental health status of pregnant women during the COVID-19 pandemic reported a prevalence between 5 and 38% for depression and anxiety symptoms (overall prevalence of 25%) and a pooled overall prevalence of anxiety of 42% ( Fan et al., 2020 ). A rare longitudinal study in Argentina confirmed significant increases in depressive, anxiety and negative affect in 102 pregnant women at 2, 14, and 47 days after the start of the lockdown compared to 102 non-pregnant women ( Lopez-Morales et al., 2021 ). During the pandemic, 1754 pregnant women in Canada reported significantly higher levels of depressive, anxiety, dissociative and post-traumatic stress symptoms compared to a pre-COVID-19 cohort of pregnant women ( Berthelot et al., 2020 ). However, again, conflicting results are reported. A Turkish study (April 2020) found lower state anxiety in 203 pregnant women compared to 101 non-pregnant women ( Yassa et al., 2020b ). In China (February - March 2020, N = 859;), pregnancy was associated with a lower risk for depression, anxiety, insomnia, and PTSD ( Zhou et al., 2020b ). Another Israelian study (March – May 2020, N = 369) also reported lower rates of depression in pregnant women hospitalized during the pandemic, compared to pregnant women that were hospitalized before the pandemic ( Sade et al., 2020 ). Pre-existing psychiatric disorders appear to increase the experience of depressive, anxiety and dissociative symptoms in pregnant women during the pandemic ( Berthelot et al., 2020 ; Liu et al., 2021 ; Ravaldi et al., 2020 ), and previous anxiety disorders increases health-related and society-related anxiety levels ( Berthelot et al., 2020 ; Ravaldi et al., 2020 ).
There are several factors that may impact on the level of stress resilience specifically in pregnant women. Maternal social support in China and Ethiopia significantly decreased anxiety levels in pregnant women ( Yue et al., 2020 ), and also increased health-related quality of life ( Dule et al., 2021 ). Social support in Canada was also negatively correlated with depression and insomnia, whereas negative cognitive appraisal positively correlated with these symptoms ( Khoury et al., 2021 ). Risk of COVID-19 infection ( Bo et al., 2020 ), social isolation ( Durankus and Aksu, 2020 ), financial and relationship difficulties ( Bo et al., 2020 ; Khoury et al., 2021 ; Lebel et al., 2020 ; Matsushima and Horiguchi, 2020 ; Mortazavi et al., 2021 ), marital life satisfaction ( Effati-Daryani et al., 2020 ), intimate partner violence ( Almeida et al., 2020 ), sleep difficulties ( Lin et al., 2021 ), were reported factors that relate to psychopathology in pregnant women during the COVID-19 pandemic. In addition, having a relative with COVID-19 infection, a history of abortion, and an age below 30 increased pregnant women's worries ( Mortazavi et al., 2021 ). In the US (April – May 2020, N = 787), compared to white women, black women reported significantly higher rates of depression, more pregnancy-related worries, more worries about the financial burden of the pandemic and having a job that is negatively affected by the pandemic ( Gur et al., 2020 ). Finally, a report from Iran (March – April 2020, N = 580) showed that fear of COVID-19 was associated with suicidal ideation, quality of life and depression in 290 pregnant women ( Ahorsu et al., 2020 ).
Conclusion: Although several cross-sectional studies, mostly surveys, report that pregnant women experienced higher levels of stress, depression and anxiety during the pandemic period compared to non-pregnant women, several other studies found comparable or even better mental health outcomes. It remains quite challenging to assess the prevalence of anxiety and depression in pregnant women during the COVID-19 pandemic compared to the pre-pandemic period. Regarding risk factors, lack of social support and fear about pandemic-related issues reduced the stress resilience of pregnant women. An important aspect for future studies will be to assess the impact of the pandemic-related stress exposure during pregnancy on the children of these mothers. For an overview of findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in pregnant women, see Table 5 .
The impact of COVID-19 on stress resilience and mental health in pregnant women.
| Indian obstetricians | April 5 - May 5 2020, | Cross-sectional, = 118 (89.83% female) | COVID-19 related concerns expressed to obstetricians by pregnant and postpartum women | Unknown | 40,86% of the participants reported anxieties related to social media. The most common anxieties and distress reported were related to worrying social media messages, fear about contracting the infection, social isolation, family members not following infection control and missing out on childbirth-related rituals. | |
| Israeli Jewish and Arab pregnant women | March 18–28 2020 | Cross-sectional, = 336 ( = 225 Jewish women, mean age 31.00 years (±5.18) and = 111 Arab women, mean age 28.43 years (±3.89) | COVID-19 related distress and anxiety | Being pregnant and being able to complete questionnaires in Hebrew | Participating pregnant women reported high COVID-19- related anxiety, with leaving the home (taking public transportation or being in public places) being the greatest cause for concern. Specifically, the use of public transportation (87.5%) was reported as the cause of the highest anxiety, followed by the potential infection of other family members (71.7%), being in public places (70%), concern for the fetus (70%), going for pregnancy check-ups (68.7%), being infected themselves (59.2%), and the delivery (55.4%). Arab women were more distressed and anxious compared to Jewish women. | |
| Chinese pregnant women | February 13–16 2020 | Cross-sectional, = 1901 (mean age 28.9 years (±4.7) | Presence of prenatal depression (PND) and post-traumatic stress disorder (PTSD) during the COVID-19 pandemic | Being in the second or third trimester of pregnancy | During the early stage of the COVID‐19 outbreak, high anxiety levels, a high prevalence of probable PND (34%) and a high prevalence of suspected PTSD (40%) was observed among pregnant women. | |
| Pregnant women without psychiatric history attending an university clinic in Ankara, Turkey | May 2020 (precise period unknown) | Cross-sectional, = 297 (mean age 27.64 years (±5.27)) | The psychological impact and perceptions during the COVID-19 pandemic in pregnant women | Not having a psychiatric history | The majority of pregnant women in this study reported COVID-19 related concerns about their pregnancy and delivery (i.e. concerns about infecting their baby during delivery, not being able to reach their doctors and pregnancy complications because of canceled/postponed check-ups). | |
| Mexican pregnant women | May 5 - June 12 2020, | Cross-sectional, = 503 (mean age 28.1 years (±6.25)) | The impact of the COVID−19 pandemic on the levels of stress (Perceived Stress Scale; PSS) and depression (Edinburgh's Postnatal Depression Scale; EPDS) of pregnant women in Mexico | Attending prenatal care from public and private hospitals | 33.2% of the participants was highly stressed (having a score of 27 or higher on the PSS) and a significant increase in PSS scores was observed in the third trimester of pregnancy. 17.5% of the participating pregnant women were considered as being depressed (having a score of 14 or higher on de EPDS). | |
| Chinese pregnant women residing in Liaoning Province | February - March 2020 (precise period unknown) | Cross-sectional, = 560 (mean age 25.8 years (±2.7)) | The attitude towards COVID-19, psychological and stress impact among pregnant women amid the COVID-19 pandemic's immediate wake | Having a Chinese nationality, being 18 years or older | During the early stages of the COVID-19 pandemic, Chinese pregnant women reported moderate-to-severe stressful and psychological impact of the pandemic. | |
| Yassa, M. et al., 2020 | Turkish pregnant woman at a single tertiary “Coronavirus Pandemic Hospital” referral center | April 2020 (precise period unknown) | Cross-sectional, = 172 (mean age 27.5 years (±5.3)) | The attitude, concerns, and knowledge of non-infected pregnant women towards the COVID-19 outbreak | Not being infected with COVID-19, not having a psychiatric history, having a confirmed pregnancy over the 30th gestational week | Women had a positive attitude and compliance towards the COVID-19 outbreak and the healthcare staff. However, the majority of the women also felt vulnerable and approximately one third of the pregnant women reported concerns about getting infected during or following the delivery or their new-born baby getting infected. |
| Pakistani pregnant women at an out-patient clinic in Pakistan | August 6 −20, 2020 | Cross-sectional, = 552 (mean age 32.0 years (±7.3)) | Levels of depression, anxiety and impact of the COVID-19 outbreak | Not having a psychiatric history or other comorbidities | 61% of pregnant women neither felt depressed nor anxious and were likely to be well. 39% of pregnant women stated that the COVID‐19 pandemic had caused them depression and anxiety, while 33% were found to have possible depression, with EPDS scores of 10 or greater. Pregnancy was a determinant factor for negative perceptions of the COVID‐19 pandemic (e.g. being exposed, more vulnerable, and fearing vertical transmission or harm to the pregnant woman). | |
| Liu, X. et al., 2020 | Chinese pregnant women registered for prenatal care in Wuhan and Chongqing | February 3–9 2020 | Cross-sectional, = 1947 ( = 932 women form Wuhan, 90.45% aged <35 years, = 1015 women from Chongqing, 87.78% aged <35 years) | The mental status (Self-Rating Anxiety Scale; SAS) of pregnant women and their obstetric decisions during the COVID-19 outbreak | Being registered for prenatal care in hospitals in Wuhan and Chiongqing | More women in Wuhan felt anxious (24.5% versus 10.4% of non-Wuhan women). Factors that influenced anxiety included household income, subjective symptom and attitudes. Overall, obstetric decisions also revealed city-based difference. |
| Argentinian women | Three waves; T0 (March 22 - 25 2020), T1 (April 3–9 2020), T2 (May 6–10 2020) 2, 14, and 47 days after the start of the lockdown respectively | Prospective longitudinal case-control (3 waves), = 204 (mean age 32.56 years (±4.71)) | Psychopathological consequences of the COVID-19 pandemic in pregnant women, compared to non-pregnant women | Being older than 18 years, living in Argentina, not having serious physical/psychological diseases and absence of risk factors for COVID-19, for pregnant mothers: only having a single pregnancy (in any week of gestation) | In a time range of 50 days of quarantine, pregnant women showed a higher increase in depression, anxiety and negative affect and a higher decrease in positive affect compared to non-pregnant women. | |
| Two cohorts of Canadian women (one pre and one post-COVID-19) | April 2–13 2020 (COVID-19 cohort) | Cross-sectional, = 1754 (mean age 29.27 years (±4.23)) | The extent to which the COVID-19 pandemic may aggravate the prenatal distress and psychiatric symptomatology of pregnant women | Being 18 years or older, having sufficient reading skills to complete self-report instruments | Pregnant women during the COVID-19 pandemic reported higher levels of depressive, anxiety, dissociative and PTSD symptoms, negative affectivity and less positive affectivity compared to a pre-COVID-19 cohort of pregnant women. | |
| Yassa, M. et al., 2020 | Turkish pregnant and non-pregnant woman at a single tertiary “Coronavirus Pandemic Hospital” referral center | April 2020 (precise period unknown) | Cross-sectional, = 404 (mean age 27.4 years (±5.3)) | State/trait anxiety and obsessive-compulsive symptoms during the COVID-19 pandemic of pregnant women compared to non-pregnant women | Not having a COVID-19 and psychiatric history | Pregnant women showed increased OCD symptoms and less severe anxiety levels compared with non-pregnant women. |
| Zhou, Y. et al., 2020 | Chinese pregnant and non-pregnant women in several Maternal and Child Health Hospitals in Beijing during the epidemic of COVID-19 | February 28 - March 12 2020, | Cross-sectional, = 859 ( = 544 pregnant women, mean age 31.1 years (±3.9) and = 315 non-pregnant women, mean age 35.4 years (±5.7)) | The prevalence of depression, anxiety, physical discomfort, insomnia and post-traumatic stress disorder (PTSD) during the COVID-19 pandemic | Having a childbearing age | During the COVID/19 pandemic, pregnant women had lower scores of symptoms of depression, anxiety, and PTSD (all p < 0.05) compared to non-pregnant women. |
| Israeli women hospitalized in the high-risk pregnancy units of a University Medical Center in Israel | March 19 - May 26 2020, | Cross-sectional, = 369 ( = 84 women hospitalized during COVID-19 (2.4% aged <20 years, 79.8% aged 20–35 years, 17.9% aged >35 years), and = 270 women hospitalized before COVID-19 (4.3% aged <20 years, 82.4% aged 20–35 years, 13.3% aged >35 years)) | The incidence of depression among women hospitalized in the high-risk units during the COVID-19 strict isolation period | Having a high-risk pregnancy | Results showed that women hospitalized in the high-risk pregnancy units during the COVID-19 pandemic had comparable risk for depression compared to the comparison group of high-risk pregnant women not hospitalized during the pandemic. | |
| Italian pregnant women | March 18–31 2020 | Cross-sectional, = 737 (median age 34.4 years (range 18.4–47.4)) | The association of concern, anxiety and PTSD symptoms with age, gestational weeks, parity, days of COVID-19 lockdown, assisted reproductive technology use, psychopathological history, and previous perinatal losses during the first period of lock-down | Being currently pregnant and being older than 18 years | Pregnant women were very concerned about COVID-19 and showed a high prevalence of anxiety and posttraumatic stress disorder symptom. Women with self-reported history of anxiety and/or depression were significantly more concerned about COVID-19 and were at a higher risk of developing symptoms of anxiety and posttraumatic stress disorder. | |
| Liu, C. H. et al., 2021 | US perinatal women | May 21 - August 17 2020, | Cross-sectional, = 1123 (mean age 33.10 years (± 3.77)) | COVID-19-related health, worries and grief, and depression, generalized anxiety and PTSD symptoms | Being older than 18 years, starting from the second trimester of pregnancy or having given birth in the past six months | Pre-existing mental health diagnoses as well as COVID-19-related health worries and grief experiences may increase the likelihood of mental health symptoms in perinatal women. |
| Yue, C. et al., | Chinese pregnant women | February 16–21 2020 | Cross-sectional, = 308 (mean age 31.02 years (±3.9)) | The relationship between social support, risk perception and anxiety among third-trimester pregnant women during the COVID-19 pandemic | Having a current pregnancy (third trimester) | The third trimester pregnant women had a high level of social support, a medium level of risk perception to COVID-19 and were susceptible to anxiety. Risk perception played a mediating role between social support and anxiety. |
| Dule, A. et al., | Ethiopian pregnant mothers | August 1 −15, 2020 | Cross-sectional, = 384 (mean age 31.3 years (± 7.7)) | The quality of life among pregnant mothers during COVID-19 and its association with social support and fear of the pandemic | Not having a high-risk pregnancy | Perceived social support was positively linked to quality of life and COVID-19-related fear impaired quality of life. |
| Canadian pregnant women | June 3 - July 31 2020, | Cross-sectional, = 303 (mean age 32.13 years (±4.22)) | The prevalence of mental health difficulties in pregnant individuals during the COVID-19 pandemic | Living in Ontario, Canada, being able to read and write in English, being 18 years or older, ≤ 36 weeks gestation | During the COVID-19 pandemic, pregnant women experienced significantly elevated symptoms of depression and anxiety and comparable rates of insomnia compared to a pre-COVID-19 sample of pregnant women. | |
| Chinese women | February 22 - March 10 2020, | Cross-sectional, = 1309 (mean age 29.99 years (±4.53)) | The prevalence of depression (9-item Patient Health Questionnaire - PHQ-9) during the COVID-19 pandemic and its associated factors in women in the perinatal stages | Being a woman in the third semester of pregnancy, or post-partum period (from the beginning of pregnancy to one week after childbirth), being 18 years or older, not having a pre-existing psychiatric disorder | A high prevalence of depression in women across the perinatal stages was observed. Worries about infection and interrupted routine medical check-ups were associated with an increased risk of depression. | |
| Turkish pregnant women | Not reported | Cross-sectional, = 260 (mean age 29.56 years (±3.83))) | The effects of the COVID-19 pandemic on depression and anxiety in pregnant women, using the Edinburgh Postnatal Depression Scale (EPDS) | Not having a history of a psychiatric disorder | 35.4% of the participating pregnant women scored higher than 13 on the EPDS and were thus being considered as being at risk of developing depression. COVID-19 pandemic effects regarding psychology and social isolation, anxiety symptoms and depressive symptoms contributed to increased depression in pregnant women. | |
| Canadian pregnant women | April 5–20 2020 | Cross-sectional, = 1987 (mean age 32.4 years (±4.2)) | The prevalence of anxiety and depression symptoms in pregnant women during the COVID-19 pandemic and potential resilience factors associated with lower symptoms | Having a confirmed pregnancy (<35 weeks gestation) | Elevated symptoms of anxiety and depression were found among pregnant individuals during the COVID-19 pandemic; potential protective factors included increased social support and physical exercise. | |
| Japanese women | May 31 - June 6 2020, | Cross-sectional, = 1777 (5.35% aged <25 years, 29.21% aged 25–30 years, 37.20% aged 30–34 years, 28.25% aged ≥35 years) | Depressive symptoms in pregnant women during the COVID-19 pandemic, using the Japanese version of the Edinburgh Postnatal Depression Scale (EPDS) | Being pregnant or recently gave birth (postpartum) | 17% of pregnant women suffered from depressive symptoms. Depression scores were positively correlated with cancelation of planned informal support, higher perceived risk for infection, difficulties in household finances, lack of social support; being younger, being less wealthy, being unemployed, and not having a partner. | |
| Iranian pregnant women | May 5 - August 5 2020, | Cross-sectional, = 484 (mean age 28.3 years (±5.8)) | Well-being (WHO-5 Well-Being Index) of pregnant women and the effect of concerns and fears (Cambridge Worry Scale) on maternal well-being during the COVID-19 pandemic | Having a single healthy fetus and no significant psychological disorder | The percentage of women experiencing a low well-being state was relatively high. Predictors of experiencing low well-being were worry about own health, health of others and the fetus, having at least one infected person with COVID-19 among relatives. | |
| Iranian pregnant women | March - April 2020 (precise period unknown) | Cross-sectional, = 205 (mean age 39.3 years (±5.5)) | Depression, stress, and anxiety levels, and their predictive factors in pregnant women during the COVID-19 pandemic | Having a file in the health centers of Tabriz, having a mobile phone and a healthy pregnancy, not having a history of mental illness, medical problems during pregnancy, and high-risk pregnancies | Higher depression, stress and anxiety levels were correlated with education level, spouse's support and job, marital life satisfaction, number of pregnancies, household income sufficiency. | |
| Chinese pregnant women | February 17 - March 16 2020, | Cross-sectional, = 751 (mean age 30.51 years (±4.28)) | Mental manifestations of the COVID-19 pandemic and the impact of sleep conditions on mental health status | Not having a severe physical or mental disorder | A notable proportion of pregnant women exhibited mild anxiety and depression symptoms during the epidemic of COVID-19 mediated by sleep conditions. | |
| US pregnant women | April 17 - May 1 2020, | Cross-sectional, = 787 (mean age 32.45 years (±4.83), 27.4% Black, 72.6% White-Non Latina/Hispanic) | Race-related differences in COVID-19-related burden on mental health and resilience factors | Being pregnant | Significant racial disparities were observed regarding the impact of the COVID-19 pandemic and the experience of healthcare on the well-being of pregnant women. Self-reliance and emotion regulation was higher in Black women, although not related to a reduced risk for depression. | |
| Iranian pregnant women | March 7 - April 21 2020, | Cross-sectional, = 580 ( = 290 pregnant women, mean age 29.54 years (± 5.84) and = 290 husbands, mean age 33.62 years (±6.36)) | The interdependencies between fear of COVID-19, mental health, and preventive COVID-19 behaviours | Being pregnant, being 18 years or older, being enrolled in the Integrated Health System (IHS), having a husband who agrees to participate | Significant dyadic relationships were observed between husbands and their pregnant wives' fear of COVID-19, mental health, and preventive behaviours. |
7. Patients with a psychiatric disorder
7.1. adults with a psychiatric disorder.
Whilst facing the COVID-19 pandemic has important negative consequences in terms of mental health and increases the vulnerability for psychological problems, severe mental illness in turn has been shown to represent a vulnerability factor for COVID-19 infection. Several studies have shown that patients affected by severe mental illness have an increased risk to become infected compared to the general population (odds ratios ranging from 5.7 to 7.6) ( Lee et al., 2020 ; Li et al., 2020 ; Wang et al., 2020b ), which is linked to poorer environmental conditions, such as socioeconomic deprivation. Furthermore, they might have more difficulties with being compliant to the rules and obligations established to fight the pandemic and tend to be generally exempt by wearing personal protective equipment such as masks ( Ayuso-Mateos et al., 2020 ). Indeed, in their analysis of anonymized electronic health records of 62,354 US patients affected by COVID-19 (January – August 2020), Taquet et al. clearly showed that the presence of a pre-existing psychiatric illness was significantly associated with a higher risk of a COVID-19 diagnosis (RR=1.65, 95% CI: 1.59–1.71, p < 0.0001), independent of known physical health or economic and housing risk factors ( Taquet et al., 2021 ). This finding was confirmed by a recent analysis of de-identified population-level electronic health records data ( N = 61,783,950) from US hospitals, which showed that individuals with a recent diagnosis of a mental disorder had a significantly increased risk for COVID-19 infection, with an effect strongest for depression (OR=7.6) and schizophrenia (OR=7.34) ( Wang et al., 2020b ). Of interest, this increased risk was further exacerbated among African Americans and women. It is plausible that these patterns of associations might be also related to the effect that COVID-19 has exerted on the levels of clinical care in psychiatry which showed a substantial decrease since the start of the pandemic ( Carpiniello et al., 2020 ; Yao et al., 2020 ).
In this context, stress resilience appears among one of the many plausible moderators of the identified increased risk of infection in patients affected by severe mental illness ( Ameis et al., 2020 ; Jacob et al., 2020 ). This is of relevance given that building resilience in the general population and at-risk patient populations will be a key instrument to decrease the impact of the COVID-19 related socioeconomic shock ( Jacob et al., 2020 ). Indeed, there is evidence that specific factors such as having a higher academic level, being autonomous, having self-efficacy, and the presence of optimism have been shown to be significant predictors of resilience in the general population during the COVID-19 pandemic ( Robles-Bello et al., 2020 ), protecting individuals from the development of mental disorders. This points to the importance of building resilience in at risk population such as those affected by severe mental disorders. Indeed, the work from Burrai et al. has shown that Italian psychiatric patients in residential community (April – May 2020, N = 82) scored lower than healthy individuals in levels of stress although, as expected, they showed higher levels of anxiety, perceived risk of getting infected with COVID-19 and worry about the emergency situation ( Burrai et al., 2020 ). This finding is probably justified by the perceived and experienced support that residential patients receive from mental health workers and peers.
At the same time, there is evidence that COVID-19 has exerted a role as a precipitating factor for an exacerbation of existing psychiatric disorders, particularly in those disorders where stress is a key trigger, such as PTSD, mood disorders, and schizophrenia ( Ettman et al., 2020 ; Horn et al., 2020 ; Jolly et al., 2020 ; Ma et al., 2020 ; Pinkham et al., 2020 ; Rutherford et al., 2021 ). For instance, in China (January – April 2020), 30 patients with schizophrenia who were socially isolated after having close contact with a COVID-19 case showed a higher severity of symptoms, including higher levels of perceived stress and anxiety and lower quality of sleep, as well as a higher inflammatory load compared to 30 patients with schizophrenia not subjected to quarantine measures ( Ma et al., 2020 ). Of interest, there is anecdotal evidence of two cases in the US where symptoms of PTSD might have been exacerbated by public masking ( Jolly et al., 2020 ). However, Pinkham et al. showed in 148 US individuals with severe mental illness (92 with schizophrenia spectrum illnesses and 56 with affective disorders) that affective symptoms and sleep were stable after five months from the start of the pandemic ( Pinkham et al., 2020 ). Convincing evidence stems from three longitudinal Dutch case-control cohorts (NESDA: N = 2329 cases and N = 652 controls; NESDO: N = 378 cases and N = 132 controls; NOCDA: N = 419 cases), showing that patients with depressive, anxiety, or obsessive-compulsive disorders are not experiencing a large detrimental impact on their mental health during the COVID-19 pandemic compared to before, even though symptom severity remained substantially high – and many more times higher than healthy controls, indicating the burden and severity of psychiatric disorders compared to general population symptom levels ( Pan et al., 2021 ). With regard to suicidality, a series of studies have shown that the suicide risk increased significantly during the pandemic ( Iob et al., 2020b ; John et al., 2020 ; Nomura et al., 2021 ; Sáiz et al., 2020 ; Singh, 2020 ; Tanaka and Okamoto, 2021 ). While the grim forecast from predictive models showed increased rates of suicide during the pandemic ( John et al., 2020 ), data emerging from epidemiological observations in countries as the Netherlands and Japan found that monthly suicide rates declined during the first months of the pandemic, even though levels in Japan increased by 16% during the second wave ( Tanaka and Okamoto, 2021 ). Other studies showed increased rates of various suicidal behavior components in the general population including passive suicidal ideation ( Sáiz et al., 2020 ) and self-harm ( Iob et al., 2020b ).
7.2. Children and adolescents with a psychiatric disorder
Children and adolescents with an eating disorder diagnosis represent a vulnerable group. Reactivation of eating disorder symptoms occurred in 42% of 365 young patients followed up in an eating disorder clinic in Spain during the first 8 weeks of COVID-19, particularly in adolescents (March – May 2020, N = 365). In half of the cases, the clinical worsening was associated with eating restriction and excessive exercising due to reactivation of weight phobia. Social isolation and increase in family conflicts were reported as relevant factors ( Graell et al., 2020 ). Obsessive compulsive disorder symptoms were also reported to increase in the first months of the pandemic in most children and adolescents diagnosed with OCD, in addition to increased anxiety and depressive symptoms (Denmark, April-May 2020, N = 67) ( Nissen et al., 2020 ). In a Turkish study, 61 participants aged 6–18 years who had been diagnosed with OCD were assessed in April 2020. 54% reported worsening of their symptoms and 36% reported more than a 30% increase in CY-BOCS scores. On the other hand, 11.4% of the patients reported decreased symptoms. More than half of the patients who were in remission also reported increased symptoms that reached a clinically significant threshold. Among the factors that predicted worsening of OCD symptoms during the pandemic were daily preoccupation with COVID-19, searching on social media about COVID-19, duration of OCD diagnosis and a diagnosis of COVID-19 in someone familiar ( Tanir et al., 2020 ).
Children with neurodevelopmental disorders such as attention deficit hyperactivity disorder (ADHD) and autism have shown to be at risk during the COVID-19 outbreak. A survey completed by 241 Chinese parents of children aged 6–15 years old who were diagnosed with ADHD, showed that ADHD symptoms significantly worsened during the lockdown ( Zhang et al., 2020a ). In a survey study in Italy (April 2020, N = 527), parents reported that respectively 36% and 42% of children diagnosed with an autism spectrum disorder (ASD) experienced more intense and more frequent behavioral problems compared to the period before the pandemic ( Colizzi et al., 2020 ). Further, Turkish children diagnosed with ASD reported more sleep problems during the home confinement period which mediated autism symptom severity (May 2020, N = 46)) ( Turkoglu et al., 2020 ). In another Turkish study that included 87 ASD patients (aged 3 to 29 years old), it was found that parents’ anxiety levels were significantly correlated with the child's total score on the ABC (Aberrant Behavior Checklist). Half of the parents reported that their children became more aggressive, around one third of the parents reported sleep and appetite changes in their children and a quarter of the parents reported that their child's tics increased, or new tics emerged ( Mutluer et al., 2020 ).
Conclusion: Overall, people with existing psychiatric disorders are experiencing a detrimental impact on their mental health from the COVID-19 pandemic, for example in OCD and PTSD, which requires close monitoring in clinical practice. The COVID-19 pandemic, however, does not seem to have further increased symptom severity in adult patients with depressive and anxiety disorders compared to their pre-pandemic levels ( Pinkham et al., 2020 );( Pan et al., 2021 ). Longitudinal observations with adequate time of follow-up suggest an increased risk for suicidality associated with the pandemic, even though there are conflicting reports. Regarding children and adolescents diagnosed with a psychiatric disorder, studies have generally reported a worsening of symptoms in young patients with eating disorders, obsessive compulsive disorders, and neurodevelopmental disorders such as ADHD and ASD. Severe mental illness in turn has been shown to represent an important vulnerability factor for COVID-19 infection. Basing on the increased vulnerability to COVID-19 in psychiatric patients, several European countries have prioritized them for vaccination. Many other countries are currently evaluating this option ( De Picker et al., 2021 ). See Table 6 . for an overview of findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in patients with a psychiatric disorder.
The impact of COVID-19 on stress resilience and mental health in patients with a psychiatric disorder.
| Lee, S. W. et al., | South Korean adult patients with non-affective or affective disorders with psychotic features | Jan 1 - May 15 2020, | Cross-sectional, = 164,540 individuals without a mental illness (mean age 46.2 years (±18.3) and = 51,878 with a mental illness (mean age 61.6 years (±19.2) | The associations between mental illness and the likelihood of a positive COVID-19 test result and the clinical outcomes of COVID-19 | Being older than 20 years, presence of a SARS-CoV-2 test during the study period | 1391 (3.0%) people without a mental illness and 1383 (2.9%) of those with a mental illness tested positive for COVID-19. People with a previous diagnosis of a mental illness had the same risk for testing positive for COVID-19 as people with no history of mental illness in a nationwide cohort from South Korea. |
| Li, L. et al., | US adults, hospitalized COVID-19 positive patients | Two waves; T1: February 15 - April 25 2020,, and T2: May 27 2020, | Cohort, = 1685 | The association between having any prior psychiatric diagnosis and COVID-19 related mortality of hospitalized patients with COVID-19 | Being hospitalized for COVID-19 | Patients with a prior psychiatric diagnosis while hospitalized for COVID-19 had a higher mortality rate compared those without a psychiatric disorder (hazard ratio, 1.5; 95% CI, 1.1–1.9; = 0.003). |
| Wang, Q. et al., 2020 | US adult patients | Up to July 2020 | Case-control, = 61,783,950 | The impact of a recent (within past year) diagnosis of a mental disorder – including attention-deficit/hyperactivity disorder (ADHD), bipolar disorder, depression and schizophrenia – on the risk for COVID-19 infection and related mortality and hospitalization rates | Having an electronic health record | Patients with a recent (within past year) diagnosis of a mental disorder had a significantly higher risk for COVID-19 infection as compared to patients without mental disorders, and also present a worse out- come as evidenced by higher rates of hospitalization and death. |
| Taquet, M. et al., | US adult patients (anonymised data from electronic health records in 54 health-care organisations in the US) | January 20 - August 1 2020, | Cohort, = 69.8 million ( = 62,354 with COVID-19, mean age 49.3 years (±19.7), 55.4% female) | Bidirectional associations between COVID-19 and psychiatric disorders | Having an electronic health record | Survivors of COVID-19 appear to be at increased risk of psychiatric sequelae, and a psychiatric diagnosis might be an independent risk factor for COVID-19. |
| Italian Community Mental Health Centres (CMHC) and General Hospital Psychiatric Wards (GHPW) | April 1–11 2020 | Cross-sectional, = 71 (52.9%) of the 134 (MHDs) and = 107 (32.6%) of the 318 GHPWs | The impact of the current emergency on the activities of the Italian Mental Health Departments | Being included in the list of Mental Health Departments, updated annually by the Italian Society of Psychiatry | The pandemic has led to a drastic reduction in levels of care, which may produce a severe impact on the mental health of the population. | |
| Spanish adults in a sample affected by the COVID-19 pandemic | April 15–26 2020 | Cross-sectional, = 1345 (15.57% aged 18–28 years, 17.03% aged 29–39 years, 18.01% aged 40–49 years, 16.95% aged 50–59 years, 17.36% aged 60–69 years, 15.08% aged ≥70 years, 63.35% female) | The level of resilience of the general Spanish population exposed to a traumatic situation by the COVID-19 pandemic | Being 18 years or older, having a Spanish nationality, being a resident in Spain, having read the information sheet and accepted the informed consent, having completed the questionnaire. | The Spanish population exposed to confinement presented high levels of resilience, but no relevant post-traumatic growth took place. Having a higher academic level, being autonomous), along with self-efficacy) and to a lesser extent optimism predicted a resilient outcome. | |
| Italian adult patients in Residential Rehabilitation Communities and healthy controls | April - May 2020 (precise period unknown) | Cross-sectional, = 77 psychiatric patients (mean age 46.61 years (±12.81), 33.8% female) and = 100 healthy controls (mean age 46.40 (±11.52), 50% female) | The psychological and emotional impact of isolation on patients in these psychiatric communities, compared to healthy controls | Being 18 years or older and having a diagnosis of at least one psychotic disorder | Statistically significant differences were observed between psychiatric patients and controls on Anxiety, Stress, Worry, and Risk Perception variables. | |
| French adult patients infected by COVID-19 | March 17 - May 11, 2020 | Cross-sectional, = 180 (mean age 53.0 (±16.0)) | The prevalence of PTSD in patients with laboratory-confirmed COVID-19 | Having a laboratory-confirmed diagnosis of COVID-19, being 18 years or older and being willing to participate | Results showed that 6.5% of the patients presented with probable PTSD. Psychotropic medication, hospitalization, and distress during the acute phase of COVID-19 were significantly associated with the severity of the PTSD symptoms. | |
| US adult patients affected by PTSD | April 1 - May 8 2020, | Cross-sectional, = 76 ( = 46 with PTSD (mean age 62.5 years (±9.0)) and = 30 trauma-exposed comparison subjects; TE (mean age 67.4 (±9.4)) | PTSD symptoms, social isolation and loneliness among older adults with PTSD compared to TEs | Being 50 years or older, being currently diagnosed with PTSD, having a PTSD duration of at least 6 months, having a Post-traumatic Stress Disorder Checklist (PCL-5) score ≥33, having a score of ≥25 on the Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) | PTSD symptoms significantly declined among PTSD participants relative to TEs. Sources of resilience may exist based on experience with prior traumas as well as increasing age promoting more adaptive coping styles. | |
| Pinkham, A. et al., 2020 | US adult patients affected by severe mental illness | April 3, - June 4 2020, | Longitudinal, = 148 ( = 92 with schizophrenia spectrum illnesses and = 56 with affective disorders) | To compare the severity of pre-pandemic symptoms and affective experiences to current symptoms | Having a diagnosis of schizophrenia, schizoaffective disorder, bipolar disorder (I or II) with or without psychotic features or major depression with psychotic features | There were no significant changes in mood experiences or psychotic symptoms over time, and sleep duration was also unaffected. |
| Chinese adult schizophrenic patients medically isolated from 10 January 2020 to 30 April 2020, due to having close contact with COVID-19 patients at Wuhan Mental Health Center (aged between 20 and 70 years old) | January 10 - April 30 2020, | Cross-sectional, = 30 patients with schizophrenia were recruited from Wuhan Mental Health Center (isolation group) = 30 patients matched with the isolation group recruited from another branch of Wuhan Mental Health Center as controls | To explore the impact of social isolation due to COVID on common inflammatory indicators and psychological characteristics | Having been in close contact with COVID-19 patients, not having a COVID-19 infection after isolation and screening, having been medically isolation for ≥ 14 days, being diagnosed with schizophrenia in accordance with the Diagnostic and Statistical Manual of Mental Diagnostic criteria (DSM-VI), being hospitalizatized for ≥2 years before isolation, being between 20 and 70 years old | Social isolation led to worse anxiety and sleep quality. No effect on inflammatory parameters. | |
| Dutch adults with and without depressive, anxiety, or obsessive-compulsive disorders (three cohorts:1) the Netherlands Study of Depression and Anxiety (NESDA), 2) the Netherlands Study of Depression in Older Persons (NESDO), and 3) the Netherlands Obsessive Compulsive Disorder Association Study (NOCDA) | April 1 - May 13 2020, | Longitudinal, NESDA: = 2329 individuals with a depression or anxiety disorder, = 652 controls NESDO: = 378 individuals with a depressive disorder, = 132 controls NOCDA: = 419 individuals with a lifetime diagnosis of obsessive-compulsive disorder | The impact of the COVID-19 pandemic on mental health in people with pre-existing mental health disorders | NESDA: being aged 18=65 years; NESDO: being 60 years or older; NOCDA: being 18 years or older | Although people with depressive, anxiety, or obsessive-compulsive disorders scored higher on all four symptom scales than did individuals without these mental health disorders, both before and during the COVID-19 pandemic, they did not report a greater increase in symptoms during the pandemic | |
| Japanese general population | February - June 2020 (first wave of pandemic) and July - October 2020 (second wave of pandemic) | Cross-sectional, = 126 million (data derived from suicide statistics published by the Ministry of Health, Labour, and Welfare) | Suicide mortality during the pandemic in the Japanese population | Unknown | The suicide rate declined substantially during the first wave of the COVID-19 pandemic (February to June 2020), but increased rapidly during the second outbreak (July to October 2020). The COVID-19 pandemic affected almost every community and citizen concurrently. | |
| Japanese general population | December 2010-September 2020 (precise period unknown, montly mortality data was obtained from the National Police Agency) | Cross-sectional, N: Unknown | Suicide mortality during the pandemic in the Japanese population | Unknown | For women, excess deaths of 110.00–160.75 (percent excess 22.08–32.26) were observed in July 2020, 96.00–163.56 (19.34–32.95) in August 2020, and 95.00–161.00 (19.83–33.61) in September 2020. No excess deaths from suicide were observed before 2020. For men, no excess deaths were found during the same period. | |
| General Spanish population aged 18 and older | March 19 −26 2020 | Cross-sectional, = 21,207 (mean age 39.7 years (±14.0), 69.6% female) | The prevalence of passive suicidal ideation in a sample of the general Spanish population early in the COVID-19 pandemic and lockdown factors associated with suicidal thoughts | Being 18 years or older | Being of female sex, married or living as married, and working were protective factors against passive suicidal ideation while risk factors were very low income, having elderly dependents, and having a personal history of past/current mental disorder. | |
| Iob, E. et al., 2020 (144) | UK general population (COVID-19 Social Study) | March 21- April 20 2020, | Cross-sectional, = 44,775 (17.5% aged 18–29 years, 23.2% aged 30–44, 26.9% aged 45–49, 32.4% aged >60 years, 51.0% female) | Patterns of abuse, self-harm and thoughts of suicide/self-harm in the UK during the first month of the COVID-19 pandemic | Presence of data on abuse, self-harm and thoughts of suicide or self-harm on at least one occasion | The reported frequency of abuse, self-harm and thoughts of suicide/self-harm was higher among women, Black, Asian and minority ethnic (BAME) groups and people experiencing socioeconomic disadvantage, unemployment, disability, chronic physical illnesses, mental disorders and COVID-19 diagnosis. |
| Patients undergoing treatment in the outpatient clinic, day hospital, and the inpatient program of the Child and Adolescent Eating Disorders Unit (CAEDU) of the Hospital Infantil Universitario Niño Jesús in Madrid. | March 16 - May 10, 2020 | Cross-sectional, = 365 (1818 outpatient consultations; 73.10% remotely and 26.9% face‐to‐face) | The efficacy of a combined teletherapy program aimed at allowing continuity of care for children and adolescents with an eating disorder | Undergoing treatment in the Eating Disorders unit at the time of state-decreed confinement and during the 8-week lockdown period | Almost half of the children and adolescents studied experienced reactivation of eating disorder symptoms despite treatment, and severe patients (25%) presented self‐harm and suicide risk, | |
| Danish children and adolescents, newly diagnosed with OCD (clinical group) and Danish children and adolescents who were diagnosed years ago and completed their primary treatment (survey group) | April–May 2020 (precise period unknown) | Cross-sectional, = 65 (first sample, clinical group, mean age 14.9 (±2.66)); = 37 (second sample, survey group, mean age 14.14 years (±2.79)) | The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder (OCD) | Having been diagnosed with OCD | In both samples, but with an effect more pronounced in the survey group, participants experienced a worsening of their OCD, anxiety, and depressive symptoms | |
| Turkish children and adolescents who had been diagnosed with OCD | September 2019 to April 2020 (precise period unknown) | Cross-sectional, = 61 (mean age 13.62 years (±2.72), 44.3% female) | The effects of COVID-19 pandemic and related confinement on symptom profile, symptom severity and exacerbation of obsessive-compulsive disorder (OCD) | Being diagnosed with OCD and having a Children's Yale-Brown Obsessive Compulsive Scale (CY-BOCS) score from before the pandemic period | Young subjects with OCD developed additional symptoms and worsen already existing symptoms of OCD during COVID-19 pandemic. There was a significant relationship between the change in CY-BOCS scores with talking/searching in the social environment about COVID-19, daily preoccupation about COVID-19, duration of OCD diagnosis and diagnosis of COVID-19 in someone familiar. | |
| Zhang, J. et al., 2020 | Chinese children with ADHD diagnosis | Not specified | Cross-sectional, = 241 (mean age 9.43 years (±2.39), 19.5% female) | Mental health related conditions of children with ADHD during the COVID-19 outbreak | Being diagnosed with ADHD | During the COVID-19 outbreak, children's ADHD symptoms worsened significantly compared to normal state. Data were reported by parents, and medication status was not known. |
| Italian children with ASD | April 6–20 2020 | Cross-sectional, = 527 (mean age 13.0 years (± 8.1)) | The impact of the COVID-19 pandemic on Autism Spectrum Disorder (ASD) individuals | Being diagnosed with ASD by healthcare professionals affiliated with the Veneto Autism Spectrum Disorder Regional center at the Integrated University Hospital of Verona | The COVID-19 outbreak increased difficulties among autism spectrum disorder individuals. | |
| Turkish drug-naive children diagnosed with ASD | May 7–14 2020 (during the fifth week following commencement of home confinement) | Cross-sectional, = 46 (mean age 7.89 years ()range 4–17 years), 17.39% female) | The relationship between chronotype preference/sleep problems and symptom severity of children with Autism Spectrum Disorder (ASD) during the confinement and social isolation of the COVID-19 outbreak | Being diagnosed with ASD and having been regularly monitored and received conventional assessment forms during the 2 months before the commencement of home confinement | ASD exhibited significantly greater sleep problems and chronotype score (eveningness) during the home confinement period compared to non-home confinement. Children with ASD forced into home confinement due to the COVID-19 pandemic showed also increased ASD symptoms. | |
| Turkish individuals with ASD (aged 3–29 years old) | Not specified | Cross-sectional, = 87 (mean age 13.96 years (±6.1), 17% female) | Response of individuals with ASD to COVID-19 in terms of comprehension and adherence to implemented measure and changes in their behavioural problems | Having been diagnosed with ASD according to DSM-5 criteria by child psychiatrists with over 10 years of experience in ASD | ASD-related behaviours, sleep quality, and hypersensitivity changed significantly from before the pandemic to during the pandemic. COVID-19 inflicted important challenges to individuals with ASD and their caregivers. | |
8. COVID-19 patients
Previous SARS and MERS pandemics have shown that infection with the virus itself can be associated with increased symptoms as well as new diagnoses/symptoms of anxiety, depression, impaired memory, fatigue and insomnia in the acute as well as post-illness phase, and there is burgeoning evidence for substantial psychiatric symptoms related to COVID-infection ( Rogers et al., 2020 ; Taquet et al., 2021 ). An electronic health record network cohort study using data from 69 million individuals showed that in the three months following testing positive for COVID-19, 1 in 5 survivors was recorded as having a first time diagnosis of anxiety, depression or insomnia. This was about twice as likely as for other groups of patients in the same period ( Taquet et al., 2021 ). Furthermore, Horn et al. found that the prevalence of PTSD in patients with COVID-19 was around 6.5%, and a similar rate was also reported in COVID-19 patients discharged from hospitals in Wuhan ( Horn et al., 2020 ). In an Italian cross-sectional study (April - October 2020) that included 381 patients who had recovered from COVID-19 within 30 to 120 days, a PTSD prevalence of 30.2% was reported after acute COVID-19 infection ( Janiri et al., 2021 ). It is crucial to determine protective factors increasing resilience against mental health impairment following infection with COVID-19. This is illustrated by findings in a sample of 296 Chinese patients with mild symptoms of COVID-19, where higher resilience measured with the Connor-Davidson Resilience Scale was correlated with lower anxiety ( r = −0.391, p < 0.001) and depression ( r = −0.472, p < 0.001) scores. Patients with high resilience (upper 27%) were much less likely to display symptoms of anxiety (OR = 0.362, p < 0.001) or depression (OR = 0.301, p < 0.001) ( Zhang et al., 2020b ). Education about disease-related facts, emotional support and confidence of rehabilitation may enhance resilience in COVID-19 affected patients ( Zhang et al., 2020b ). Following up on these first data, longitudinal studies correcting for potential confounders such as pre-existing mental disorders, concomitant somatic disorders, severity of infection, degree of physiological compromise, immunological response, extent of medical interventions and socioeconomic situation, are warranted to further elucidate the role of resilience and its determining factors in promoting mental health in COVID-19 patients in order to develop targeted preventive interventions strengthening coping skills, self-efficacy, will power, daily routines and opportunities to share the emotional burden ( Richards and Scowcroft 2020 ).
Conclusion: In sum, given the high risk of psychiatric sequelae of COVID-19 infection, preventive measures promoting mental health as well as intensified screening for symptoms of mental disorders should be routinely implemented in the standard care of COVID-19 patients to increase resilience towards mental disorders particularly in this patient group. Table 7 presents findings from cross-sectional and longitudinal studies on the impact of COVID-19 on stress resilience and mental health in COVID-19 patients.
The impact of COVID-19 on stress resilience and mental health in COVID-19 patients.
| Italian patients who presented to the emergency department with COVID-19 and recovered from COVID-19 infection | April 21 - October 15 2020, | Cross-sectional, = 381 (mean age 55.26 years (± 14.86), 43.6% female) | PTSD prevalence after severe COVID-19 infection | Having to meet PTSD criteria, in addition to traumatic event exposure (criterion A), having at least 1 DSM-5 criterion B and C symptom and at least 2 criterion D and E symptoms | A PTSD prevalence of 30.2% was observed after acute COVID-19 infection. Associated characteristics were female sex, history of psychiatric disorders, and delirium or agitation during acute illness. In the PTSD group, more persistent medical symptoms, were often reported by patients after recovery from severe COVID-19. | |
| Zhang, J. et al., 2020 | Chinese adult patients with mild symptoms of COVID-19 | March 3 –5 2020 | Cross-sectional, = 296 (2.7% aged 18–20 years, 53.0% aged 21–40 years, 40.5% aged 41–60 years, 3.7% aged ≥ 61 years, 41.6% female) | Resilience, anxiety and depression among patients with mild symptoms of COVID-19 | Being diagnosed with COVID-19, having stayed in FangCang Hospital and received relevant treatment (e.g., oxygen therapy and antiviral therapy), being 18 years or older, not having a history of mental illness, a severe cognitive impairment and/or audiovisua impairment, poor physical condition, or having participated in other relevant studies | A small number of the patients in this study had above threshold anxiety and depression. The mean total resilience score of the participants was slightly below the normal level of ordinary Chinese adults. Resilience was inversely associated with and was a protective factor for both anxiety and depression. |
9. Interindividual differences in stress resilience: implications for the pandemic
From the previous sections it is apparent that the effects of the pandemic, either related to COVID-19 itself or the associated measures, are surprisingly heterogeneous across populations. Trajectories of mental distress varied markedly by resilience level during the early months of the COVID-19 pandemic ( Riehm et al., 2021 ). It is thus of paramount importance to understand which individuals are resilient or vulnerable to apply a personalized medicine approach ( Willis and Lord, 2015 ). This approach harnesses the individual's genetic, genomic, proteomic, clinical, socioeconomic and lifestyle information to identify the factors causing the differential resilience/vulnerability to the virus. Such information allows to define resilient/vulnerable subpopulations, to refine targeted therapeutic strategies and to develop an effective public health approach. A meta-analysis examining 68 studies comprising 288,830 participants from 19 countries on factors associated with psychological distress during the COVID-19 pandemic (December 2019 - July 2020), showed that being female, being younger than 35 years old, living in rural areas, lower socioeconomic status, higher COVID-19 infection risk, longer social media exposure and having pre-existing physical or mental conditions were associated with higher anxiety and depression odds ( Wang et al., 2020c ). Higher social/family support, physical activity and positive coping strategies were associated with lower odds of anxiety and depression and thus a reduced risk of psychological distress ( Wang et al., 2020c ).
With regard to mental health, psychological attitudes towards how to manage the risk of infection, as well as towards specific medical, socioeconomic, personality and lifestyle factors, have been suggested to be key for the individual's resilience to distress and psychiatric disorders during a pandemic ( Chen and Bonanno, 2020 ; WHO, 2020 ; Zager Kocjan et al., 2021 ). Individual trait resilience and well-being scores, measured respectively with the 10-item Connor-Davidson Resilience Scale and the Recovery from War Scale, have been found to predict effective coping with the COVID-19 threat ( Kimhi et al., 2020 ; Ran et al., 2020 ). In addition, strategies aimed at reducing psychological distress such as paying attention to a healthy lifestyle, social support, good quality of sleep, acceptance of negative emotions, and avoidance of suppression and substance abuse, have been suggested to increase psychological resilience and may be key in coping with the COVID-19 related distress ( Bozdag and Ergun, 2020 ; Petzold et al., 2020 ). By contrast, loneliness, or negative psychological reactions, including panic response, hysteria, hopelessness and desperation, have been associated with negative outcomes, including suicidal ideation ( Killgore et al., 2020a ; Lee, 2020 ; Serafini et al., 2020 ; Thakur and Jain, 2020 ). Although the impact of the pandemic is still under investigation and initial large scale data analysis show that suicide numbers have remained largely unchanged or declined in the early months of the pandemic compared with the expected levels based on the pre-pandemic period in high-income and upper-middle-income countries it is plausible that more accurate figures will be detected in the long-term even after the pandemic will decrease its burden globally. Mental distress can be exacerbated by being quarantined ( Xin et al., 2020 ). It is worth noting that young people have reported to experience greater psychological distress than adults ( McGinty et al., 2020 ; Pierce et al., 2020 ; Varma et al., 2020 ). Unfortunately, to the best of our knowledge, no data on potential genetic, epigenetic, or brain function markers of resilience to mental illness in the face of the pandemic have been published yet. However, it can be hypothesized that neurobiological factors usually involved in the stress response, emotion-regulation, and the ability to adapt to new life conditions, such as immune system activation, hypothalamic-pituitary-adrenal axis activity and neural plasticity processes, might be involved ( Branchi and Giuliani, 2020 ; Zorn et al., 2017 ).
The three-dimensional vulnerability-stress-coping model may help understanding risk and resilience for mental disorders in relation to stress during the COVID-19 pandemic. This gene x environment x coping (G x E x C) model has been proposed to include the three factors a) genetic vulnerability, b) risk-increasing external stressors and c) resilience-increasing coping mechanisms, such as self-efficacy buffering the impact of a high genetic vulnerability and/or adverse environment. Exemplary studies have demonstrated this complex, three-fold interaction regarding risk or resilience towards anxiety phenotypes ( Schiele et al., 2020 , 2016 ). Finally, epigenetic mechanisms at the interface between biology and biography and impacting on stress-response and emotion-regulating capacities might add another level to confer individual risk as well as resilience towards mental disorders under adverse and advantageous environmental conditions ( Vinkers et al., 2015 ). Therefore, an extended (Epi) G x E x C model might prove useful in informing future personalized preventive interventions increasing resilience towards mental disorders. At the same time, existing hypotheses as the stress inoculation or match/mismatch hypothesis for psychiatric disorders may help to understand why selected population groups show increased resilience levels, for instance due to previous life experiences that now enable them to deal appropriately with the current challenges ( Nederhof and Schmidt, 2012 ; Schmidt, 2011 ).
Conclusion: There is an urgent need for a personalized approach when it comes to identifying individuals at risk or resilient for the stressful effects of the COVID-19 pandemic. The effects of stress and the resilience capacity are dependent on (neuro)biological, psychological, and environmental factors and are heavily dependent on an individual's unique context. Intensified research into (epi)genetic, proteomic, immunological, clinical, neuropsychological, socioeconomic and lifestyle factors conveying mental disorder risk or resilience in the context of the present pandemic is urgently warranted to provide individually tailored and thus most efficient resilience-increasing preventive measures. Findings from cross-sectional and longitudinal studies on interindividual differences in stress resilience are presented in Table 8 .
Interindividual differences in stress resilience: implications for the pandemic.
| US adults | Ten waves; baseline: March 10–31 2020 and nine follow-up waves conducted between April 1 - August 4 2020, | Longitudinal, = 6008 (12.3% aged 18–29 years, 39.5% aged 30–49 years, 27.2% aged 50–64 years, 20.9% aged ≥65 years, 51.0% female, 64.1% White 11.6% Black, 15.5% Hispanic/Latino, 8.8% other) | The association between resilience and trajectories of mental distress during the COVID-19 pandemic | Being a participant of the Understanding America Study (UAS) | 16.6% of the participants reported low resilience, 66.2% reported normal resilience, and 17.2% reported high resilience. Trajectories of mental distress varied markedly by resilience level during the early months of the COVID-19 pandemic, with adults reporting low or normal levels of resilience experiencing approximately a twofold increase in the odds of mental distress, whereas adults reporting high resilience reported no change in mental distress. | |
| Slovene adults | March 2020 (precise period unknown) | Cross-sectional, = 2722 (mean age 36.40 years (±13.10), 74.90% female) | Resilience, personality traits and psychological functioning during the COVID-19 pandemic | Unknown | Resilience fully or partially mediated the relationship of all the Big Five personality traits (except extraversion) with psychological functioning. | |
| Jewish Israelis | Unknown | Cross-sectional, = 1346 (mean age 42.00 years (±16.35), 62.0% female) | To investigate the extent to which individual resilience, well-being and demographic characteristics may predict two indicators of Coronavirus pandemic: distress symptoms and perceived danger | Unknown | Significant negative correlations were found between individual/community resilience and sense of danger (−0.220 and −0.255 respectively; p < .001) and distress symptoms (- 0.398 and −0.544 respectively; p < .001). Individual resilience and well-being showed to be the first and foremost predictors of COVID-19 anxiety. | |
| Chinese citizens | February 23 - March 2 2020, | Cross-sectional, = 1770 (mean age 28.70 years (±10.64), 666.9% female | The relationship between psychological resilience and mental health (depression, anxiety, somatization symptoms) among the general population in China | Being a citizen of the different provinces of China affected by COVID-19 from February 23 2020, to March 2 2020,, not being diagnosed with emotional or mental disorders, not being a newly diagnosed or suspected COVID-10 patient, not having had, not being a medical (COVID-19) staff member, not having a family member affected by COVID-19 | The prevalence of depression, anxiety, somatization symptoms was found to be 47.1%, 31.9%, 45.9%, respectively. Psychological resilience was negatively correlated with depression (standardized β = −0.490, < 0.001), anxiety (standardized β = −0.443, < 0.001), and somatization symptom scores (standardized β = −0.358, < 0.001), while controlling for confounding factors.. | |
| German general population | March 27 – April 6 2020, | Cross-sectional, = 6509 (mean age 36.2 years (±11.65), 70.1% female) | The negative impact on mental health in the current COVID‐19 pandemic | Being of 18 years or older, being a resident in Germany, being able to complete the questionnaire in German | Over 50% expressed suffering from anxiety and psychological distress regarding the COVID-19 pandemic. | |
| Bozdag, F. & Ergun, N., 2020 | Turkish healthcare workers | April 6 – 10 2020 | Cross-sectional, = 214 (mean age 33.29 years (6.82±), 56.1% female) | Psychological resilience of healthcare workers | Unknown | Differences between psychological resilience of women and men were statistically significant. Having children and being a doctor negatively predicted psychological resilience. Occupation, worry about becoming infected by the virus and quality of sleep significantly predicted the psychological resilience of healthcare professionals. |
| Killgore, W. D. S. et al., 2020 | US adults aged 18–35 years old | April 9–10 2020 | Cross-sectional, = 1013 (age range 15–35 years, 55.97% female) | Loneliness in the US Population, related to COVID-19 | Unknown | Loneliness was elevated, with 43% of respondents scoring above published cut-offs, and was strongly associated with greater depression and suicidal ideation. |
| Chinese students (26 universities in 16 Chinese cities) | February 1–10 2020 | Cross-sectional, = 24,378 (mean age 19.9 years (±1.6), 67.7% female) | The associations between mandatory quarantine status and negative cognitions and mental health | Being a full-time students of one of the selected universities, and being able to read and write Chinese | Mandatory quarantined status was significantly and positively associated with perceived discrimination (Cohen's = 0.62), perceived high/very high risk of infection (OR = 1.61), emotional distress (Cohen's = 0.46), probable depression (OR = 2.54), and self-harm/suicidal ideation (OR = 4.98). | |
| Adults from 63 countries | April 9 - May 25 2020, | Cross-sectional, = 1653 (mean age 42.90 years (± 13.63), 67.7% female, 61.2% Caucasian of Caucasian mixed, 20.2% Asian or Asian Indian, 3.6% Hispanic or Latino, 1.7% African or African American, 2.0% self-described) | The impact of the COVID-19 pandemic on psychological distress | Unknown | Over 70% of the respondents had greater than moderate levels of stress, with 59% meeting the criteria for clinically significant anxiety and 39% reporting moderate depressive symptoms. |
10. Conclusions and future perspective
We believe resilience research is in a unique position to make a significant contribution to understand the psychological and psychiatric impact of this pandemic and inform future clinical and research directions. This is not limited to the current COVID-19 pandemic but also applies to other local or global challenges. From the current literature, a surprising level of resilience is apparent across populations, even though there are individuals and groups that are at increased risk for the stressful effects of the COVID-19 pandemic ( Fig. 1 ). Nevertheless, firm conclusions cannot be drawn as most of the current literature has major methodological limitations. Most studies on stress resilience and mental health outcomes during the pandemic are observational, cross-sectional, using convenience samples with often rather small sample sizes and rather limited assessment of contextual and personal characteristics that are essential to understand stress vulnerability and resilience. Interpretation of observational studies from non-representative samples is likely to suffer from bias, particularly regarding collider bias ( Griffith et al., 2020 ). There is a stark contrast between the very limited number of extensive longitudinal studies with pre-pandemic assessments and a broad array of outcomes, and the vast number of cross-sectional studies with one or two outcomes. Where newer cohorts lack baseline data from before the pandemic, large established cohorts move relatively slowly and mostly sample infrequently. This makes more fine-grained assessments of resilience and mental health more challenging. Finally, there is lack of observational data on how the general public and patients with psychiatric disorders actually deal with self‐care, nutrition, physical activity or restorative sleep during confinement ( Balanza-Martinez et al., 2020 ). Thus, public policies will need to be informed by data gathered in observational studies of lifestyle behaviors during the compulsory isolation ( Balanza-Martinez et al., 2020 ). This research gap has been partly filled by very recent data confirming that psychiatric patients, particularly those affected by depression and anxiety tended to have higher levels of psychopathological distress ( Sole et al., 2021 ), and that the presence of depressive symptoms was a predictor of poorer resilience ( Verdolini et al., 2021 ).

Resilience and mental health related to the COVID-19 pandemic.
Nevertheless, studies during the pandemic consistently show that children and young people are the most vulnerable group with increased psychological distress, probably because their needs for social interactions are stronger. Moreover, young women appear to be more vulnerable than young men, and parents with young children appear to be at particularly high risk for mental health problems. However, these are rather broad conclusions which cannot be used at the individual level. There is still an urgent need to identify individuals and populations with higher risk of psychological distress during the COVID-19 pandemic to offer targeted mental health care and to improve social support, physical activity, and coping strategies in these individuals. These approaches are needed to boost resilience factors protecting the individual against psychological distress. For example, social support from and connectedness with family, friends, and a special caring loved one were each independently associated with greater resilience ( Killgore et al., 2020b ; Nitschke et al., 2020 ) ( South et al., 2020 ) ( Prime et al., 2020 ). Moreover, there seems to be a role for media with regard to resilience and mental health during the pandemic. Nuanced and balanced news coverage around the COVID-19 pandemic is essential in order that nocebo effects as a result of negative and alarming news coverage occur ( Bendau et al., 2020a ). Next, employers are taken up on their promise to assist their employees by building up resilience strategies at the organizational level. It remains to be seen how stress resilience will be shaped because of longer-term effects of the pandemic, or when society will need to find a new balance after the lockdown and pandemic. This is particularly pressing considering possible economic sequelae that will emerge while at the same time individuals will be forced to change from a lockdown situation to a more proactive attitude when all societal processes will start to function again.
About the methodological quality of the resilience literature during the COVID-19 pandemic, several lessons can be learned for future research to provide a more detailed and fine-grained picture, with possibilities for targeted prevention and intervention. First, the use of longitudinal data and large samples is important to identify potentially causal relationships, and changes over time ( Kalisch et al., 2017 ). How we respond to stress is a surprisingly dynamic process. Stress initiates a cascade of behavioral, (neuro)biological, and physiological changes. To this end, we need prospective data of adequate duration and of sufficient temporal resolution to observe (dis)continuous changes in resilience. Second, concerning outcomes and context, biological, psychological, and environmental data should be combined and integrated to understand the impact of (pandemic-related) stress at different levels with understanding of the individual's unique context. Third, we would encourage interdisciplinary collaborations, for example between physicians treating COVID-19 patients, psychiatrists, sociologists, advanced data experts, and neurobiologists. Fourth, we need not only to identify how stress resilience is shaped during a (prolonged) pandemic, but also develop efficient mental health interventions at a governmental, institutional, and individual level to minimize its long-term consequences. In conclusion, it is apparent that we have shown a remarkable level of resilience during the prolonged COVID-19 pandemic, but that large interindividual differences exist. Above all, it provides an opportunity but also an imperative for scientists and clinicians to work together to help understanding and addressing the pandemic.
Contributions
CV wrote the first draft. All authors provided critical input and revisions.
Conflicts of Interest
There are no conflicts of interest
Acknowledgements
No acknowledgements.
- Ahorsu D.K., Imani V., Lin C.Y., Timpka T., Brostrom A., Updegraff J.A., Arestedt K., Griffiths M.D., Pakpour A.H. Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-partner interdependence modelling. Int. J. Ment Health Addict. 2020:1–15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aiello A., Khayeri M.Y., Raja S., Peladeau N., Romano D., Leszcz M., Maunder R.G., Rose M., Adam M.A., Pain C., Moore A., Savage D., Schulman R.B. Resilience training for hospital workers in anticipation of an influenza pandemic. J. Contin. Educ. Health Prof. 2011; 31 :15–20. [ PubMed ] [ Google Scholar ]
- Akgor U., Fadiloglu E., Soyak B., Unal C., Cagan M., Temiz B.E., Erzenoglu B.E., Ak S., Gultekin M., Ozyuncu O. Anxiety, depression and concerns of pregnant women during the COVID-19 pandemic. Arch. Gynecol. Obstet. 2021 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Al Maqbali M, Al Sinani M., Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: a systematic review and meta-analysis. J. Psychosom. Res. 2021; 141 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Almeida M., Shrestha A.D., Stojanac D., Miller L.J. The impact of the COVID-19 pandemic on women's mental health. Arch. Womens Ment. Health. 2020; 23 :741–748. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ameis S.H., Lai M.C., Mulsant B.H., Szatmari P. Coping, fostering resilience, and driving care innovation for autistic people and their families during the COVID-19 pandemic and beyond. Mol. Autism. 2020; 11 :61. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ammar N., Aly N.M., Folayan M.O., Khader Y., Virtanen J.I., Al-Batayneh O.B., Mohebbi S.Z., Attia S., Howaldt H.P., Boettger S., Maharani D.A., Rahardjo A., Khan I., Madi M., Rashwan M., Pavlic V., Cicmil S., Choi Y.H., Joury E., Castillo J.L., Noritake K., Shamala A., Galluccio G., Polimeni A., Phantumvanit P., Mancino D., Kim J.B., Abdelsalam M.M., Arheiam A., Dama M.A., Nyan M., Hussein I., Alkeshan M.M., Vukovic A.P., Iandolo A., Kemoli A.M., El Tantawi M. Behavior change due to COVID-19 among dental academics-The theory of planned behavior: stresses, worries, training, and pandemic severity. PLoS ONE. 2020; 15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ayuso-Mateos J.L., Soriano J.B., Ancochea J. Face mask exemptions, psychiatric patients, and COVID-19. Eur Psychiatry. 2020; 64 :e6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Balanza-Martinez V., Atienza-Carbonell B., Kapczinski F., De Boni R.B. Lifestyle behaviours during the COVID-19 - time to connect. Acta Psychiatr. Scand. 2020; 141 :399–400. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bendau A., Petzold M.B., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Grosse J., Strohle A., Plag J. Associations between COVID-19 related media consumption and symptoms of anxiety, depression and COVID-19 related fear in the general population in Germany. Eur. Arch. Psychiatry Clin. Neurosci. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bendau A., Plag J., Kunas S., Wyka S., Strohle A., Petzold M.B. Longitudinal changes in anxiety and psychological distress, and associated risk and protective factors during the first three months of the COVID-19 pandemic in Germany. Brain Behav. 2020:e01964. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Berthelot N., Lemieux R., Garon-Bissonnette J., Drouin-Maziade C., Martel E., Maziade M. Uptrend in distress and psychiatric symptomatology in pregnant women during the coronavirus disease 2019 pandemic. Acta Obstet. Gynecol. Scand. 2020; 99 :848–855. [ PubMed ] [ Google Scholar ]
- Bidzan-Bluma I., Bidzan M., Jurek P., Bidzan L., Knietzsch J., Stueck M., Bidzan M. A Polish and German population study of quality of life, well-being, and life satisfaction in older adults during the COVID-19 pandemic. Front Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bo H.X., Yang Y., Chen J., Zhang M., Zhang D.Y., Li Y., Li R., Cheung T., Ng C.H., Wu X.J., Xiang Y.T. Prevalence of depressive symptoms among Chinese pregnant and postpartum women during the COVID-19 pandemic. Psychosom Med Publish Ahead of Print. 2020 [ PubMed ] [ Google Scholar ]
- Bozdag F., Ergun N. Psychological resilience of healthcare professionals during COVID-19 pandemic. Psychol Rep. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Branchi I., Giuliani A. Shaping therapeutic trajectories in mental health: instructive vs. permissive causality. Eur. Neuropsychopharmacol. 2020 [ PubMed ] [ Google Scholar ]
- Breslau J., Finucane M.L., Locker A.R., Baird M.D., Roth E.A., Collins R.L. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev. Med. 2021; 143 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Burrai J., Roma P., Barchielli B., Biondi S., Cordellieri P., Fraschetti A., Pizzimenti A., Mazza C., Ferracuti S., Giannini A.M. Psychological and emotional impact of patients living in psychiatric treatment communities during COVID-19 lockdown in Italy. J. Clin. Med. 2020; 9 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020; 287 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Carpiniello B., Tusconi M., Zanalda E., Di Sciascio G., Di Giannantonio M. Psychiatry during the Covid-19 pandemic: a survey on mental health departments in Italy. BMC Psychiatry. 2020; 20 :593. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Carroll N., Sadowski A., Laila A., Hruska V., Nixon M., Ma D.W.L., Haines J. The impact of COVID-19 on health behavior, stress, financial and food security among middle to high income Canadian families with young children. Nutrients. 2020; 12 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Castellini G., Rossi E., Cassioli E., Sanfilippo G., Innocenti M., Gironi V., Silvestri C., Voller F., Ricca V. A longitudinal observation of general psychopathology before the COVID-19 outbreak and during lockdown in Italy. J. Psychosom. Res. 2021; 141 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen C.S., Wu H.Y., Yang P., Yen C.F. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr Serv. 2005; 56 :76–79. [ PubMed ] [ Google Scholar ]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav. Immun. 2020; 88 :36–38. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen, S., Bonanno, G.A., 2020. Psychological adjustment during the global outbreak of COVID-19: a resilience perspective. Psychological trauma: theory, research, practice and policy. [ PubMed ]
- Cohen G., Russo M.J., Campos J.A., Allegri R.F. COVID-19 epidemic in Argentina: worsening of behavioral symptoms in elderly subjects with dementia living in the community. Front Psychiatry. 2020; 11 :866. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Colizzi M., Sironi E., Antonini F., Ciceri M.L., Bovo C., Zoccante L. Psychosocial and behavioral impact of COVID-19 in autism spectrum disorder: an online parent survey. Brain Sci. 2020:10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Copeland W.E., McGinnis E., Bai Y., Adams Z., Nardone H., Devadanam V., Rettew J., Hudziak J.J. Impact of COVID-19 pandemic on college student mental health and wellness. J. Am. Acad. Child Adolesc. Psychiatry. 2021; 60 :134–141. e132. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cusinato M., Iannattone S., Spoto A., Poli M., Moretti C., Gatta M., Miscioscia M. Stress, resilience, and well-being in Italian children and their parents during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020; 17 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr Res. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- de Lannoy L., Rhodes R.E., Moore S.A., Faulkner G., Tremblay M.S. Regional differences in access to the outdoors and outdoor play of Canadian children and youth during the COVID-19 outbreak. Can. J. Public Health. 2020; 111 :988–994. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- De Picker L.J., Dias M.C., Benros M.E., Vai B., Branchi I., Benedetti F., Borsini A., Leza J.C., Karkkainen H., Mannikko M., Pariante C.M., Gungor E.S., Szczegielniak A., Tamouza R., van der Markt A., Fusar-Poli P., Beezhold J., Leboyer M. Severe mental illness and European COVID-19 vaccination strategies. The lancet. Psychiatry. 2021; 8 :356–359. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Di Monte C., Monaco S., Mariani R., Di Trani M. From resilience to burnout: psychological features of Italian general practitioners during COVID-19 emergency. Front Psychol. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Di Santo S.G., Franchini F., Filiputti B., Martone A., Sannino S. The effects of COVID-19 and quarantine measures on the lifestyles and mental health of people over 60 at increased risk of dementia. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020; 275 :112–118. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Dule A., Hajure M., Mohammedhussein M., Abdu Z. Health-related quality of life among Ethiopian pregnant women during COVID-19 pandemic. Brain Behav. 2021:e02045. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Durankus F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: a preliminary study. J. Matern. Fetal. Neonatal Med. 2020:1–7. [ PubMed ] [ Google Scholar ]
- Effati-Daryani F., Zarei S., Mohammadi A., Hemmati E., Ghasemi Yngyknd S., Mirghafourvand M. Depression, stress, anxiety and their predictors in Iranian pregnant women during the outbreak of COVID-19. BMC Psychol. 2020; 8 :99. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Emerson K.G. Coping with being cooped up: social distancing during COVID-19 among 60+ in the United States. Rev. Panam. Salud. Publica. 2020; 44 :e81. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in us adults before and during the COVID-19 pandemic. JAMA Network Open. 2020; 3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fan S., Guan J., Cao L., Wang M., Zhao H., Chen L., Yan L. Psychological effects caused by COVID-19 pandemic on pregnant women: a systematic review with meta-analysis. Asian J. Psychiatr. 2020; 56 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021; 8 :141–149. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ferreira S., Sousa M.M., Moreira P.S., Sousa N., Pico-Perez M., Morgado P. JMIR Public Health Surveill; 2021. A Wake-Up Call for Burnout in Portuguese Physicians During the COVID-19 outbreak: a National Survey Study. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Francisco R., Pedro M., Delvecchio E., Espada J.P., Morales A., Mazzeschi C., Orgiles M. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Front Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Garcia-Fernandez L., Romero-Ferreiro V., Lopez-Roldan P.D., Padilla S., Rodriguez-Jimenez R. Mental health in elderly spanish people in times of COVID-19 outbreak. Am. J. Geriatr. Psychiatry. 2020; 28 :1040–1045. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Garcia de Avila M.A., Hamamoto Filho P.T., Jacob F., Alcantara L.R.S., Berghammer M., Jenholt Nolbris M., Olaya-Contreras P., Nilsson S. Children's anxiety and factors related to the COVID-19 pandemic: an exploratory study using the children's anxiety questionnaire and the numerical rating scale. Int. J. Environ. Res. Public Health. 2020; 17 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gloster A.T., Lamnisos D., Lubenko J., Presti G., Squatrito V., Constantinou M., Nicolaou C., Papacostas S., Aydin G., Chong Y.Y., Chien W.T., Cheng H.Y., Ruiz F.J., Garcia-Martin M.B., Obando-Posada D.P., Segura-Vargas M.A., Vasiliou V.S., McHugh L., Hofer S., Baban A., Dias Neto D., Nunes da Silva, A., Monestes J.L., Alvarez-Galvez J., Paez-Blarrina M., Montesinos F., Valdivia-Salas S., Ori D., Kleszcz B., Lappalainen R., Ivanovic I., Gosar D., Dionne F., Merwin R.M., Kassianos A.P., Karekla M. Impact of COVID-19 pandemic on mental health: an international study. PLoS ONE. 2020; 15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Glynn L.M., Davis E.P., Luby J.L., Baram T.Z., Sandman C.A. A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiol. Stress. 2021; 14 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gonzalez-Sanguino C., Ausin B., Castellanos M.A., Saiz J., Munoz M. Mental health consequences of the COVID-19 outbreak in Spain. A longitudinal study of the alarm situation and return to the new normality. Prog Neuropsychopharmacol. Biol. Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Graell M., Moron-Nozaleda M.G., Camarneiro R., Villasenor A., Yanez S., Munoz R., Martinez-Nunez B., Miguelez-Fernandez C., Munoz M., Faya M. Children and adolescents with eating disorders during COVID-19 confinement: difficulties and future challenges. Eur. Eat Disord. Rev. 2020; 28 :864–870. [ PubMed ] [ Google Scholar ]
- Griffith G.J., Morris T.T., Tudball M.J., Herbert A., Mancano G., Pike L., Sharp G.C., Sterne J., Palmer T.M., Davey Smith G., Tilling K., Zuccolo L., Davies N.M., Hemani G. Collider bias undermines our understanding of COVID-19 disease risk and severity. Nat. Commun. 2020; 11 :5749. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Guo J., Fu M., Liu D., Zhang B., Wang X., van I.M.H. Is the psychological impact of exposure to COVID-19 stronger in adolescents with pre-pandemic maltreatment experiences? A survey of rural Chinese adolescents. Child Abuse Negl. 2020; 110 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gur R.E., White L.K., Waller R., Barzilay R., Moore T.M., Kornfield S., Njoroge W.F.M., Duncan A.F., Chaiyachati B.H., Parish-Morris J., Maayan L., Himes M.M., Laney N., Simonette K., Riis V., Elovitz M.A. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res. 2020; 293 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Heath C., Sommerfield A., von Ungern-Sternberg B.S. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020; 75 :1364–1371. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hiraoka D., Tomoda A. Relationship between parenting stress and school closures due to the COVID-19 pandemic. Psychiatry Clin. Neurosci. 2020; 74 :497–498. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Horn M., Wathelet M., Fovet T., Amad A., Vuotto F., Faure K., Astier T., Noel H., Duhem S., Vaiva G., D'Hondt F., Henry M. Is COVID-19 associated with posttraumatic stress disorder? J. Clin. Psychiatry. 2020; 82 [ PubMed ] [ Google Scholar ]
- Iob E., Frank P., Steptoe A., Fancourt D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Network open. 2020; 3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Iob E., Steptoe A., Fancourt D. Abuse, self-harm and suicidal ideation in the UK during the COVID-19 pandemic. Br. J. Psychiatry. 2020; 217 :543–546. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Islam M.A., Barna S.D., Raihan H., Khan M.N.A., Hossain M.T. Depression and anxiety among university students during the COVID-19 pandemic in Bangladesh: a web-based cross-sectional survey. PLoS ONE. 2020; 15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Isumi A., Doi S., Yamaoka Y., Takahashi K., Fujiwara T. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl. 2020; 110 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jacob C.M., Briana D.D., Di Renzo G.C., Modi N., Bustreo F., Conti G., Malamitsi-Puchner A., Hanson M. Building resilient societies after COVID-19: the case for investing in maternal, neonatal, and child health. Lancet Public Health. 2020; 5 :e624–e627. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Janiri D., Carfì A., Kotzalidis G.D., Bernabei R., Landi F., Sani G., COVID G.A., Group P.-A.C.S. Posttraumatic stress disorder in patients after severe COVID-19 infection. JAMA Psychiatry. 2021 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- John A., Pirkis J., Gunnell D., Appleby L., Morrissey J. Trends in suicide during the covid-19 pandemic. BMJ. 2020; 371 :m4352. [ PubMed ] [ Google Scholar ]
- Jolly, T.S., Pandian, G., Batchelder, E., Jain, A., 2020. Posttraumatic Stress Disorder Exacerbation as a Result of Public Masking in Times of COVID-19. The primary care companion for CNS disorders 22. [ PubMed ]
- Kalisch R., Baker D.G., Basten U., Boks M.P., Bonanno G.A., Brummelman E., Chmitorz A., Fernandez G., Fiebach C.J., Galatzer-Levy I., Geuze E., Groppa S., Helmreich I., Hendler T., Hermans E.J., Jovanovic T., Kubiak T., Lieb K., Lutz B., Muller M.B., Murray R.J., Nievergelt C.M., Reif A., Roelofs K., Rutten B.P.F., Sander D., Schick A., Tuscher O., Diest I.V., Harmelen A.V., Veer I.M., Vermetten E., Vinkers C.H., Wager T.D., Walter H., Wessa M., Wibral M., Kleim B. The resilience framework as a strategy to combat stress-related disorders. Nat. Human Behav. 2017; 1 :784–790. [ PubMed ] [ Google Scholar ]
- Katz C., Priolo Filho S.R., Korbin J., Berube A., Fouche A., Haffejee S., Kaawa-Mafigiri D., Maguire-Jack K., Munoz P., Spilsbury J., Tarabulsy G., Tiwari A., Thembekile Levine D., Truter E., Varela N. Child maltreatment in the time of the COVID-19 pandemic: a proposed global framework on research, policy and practice. Child Abuse Negl. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Khoury J.E., Bennett T., Jack S.M., Gonzalez A. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J. Affect. Disord. 2021; 282 :1161–1169. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020; 290 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Killgore W.D.S., Taylor E.C., Cloonan S.A., Dailey N.S. Psychological resilience during the COVID-19 lockdown. Psychiatry Res. 2020; 291 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kimhi S., Marciano H., Eshel Y., Adini B. Resilience and demographic characteristics predicting distress during the COVID-19 crisis. Soc. Sci. Med. 2020; 265 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J. Affect. Disord. 2020; 277 :5–13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee S.A. How much "Thinking" about COVID-19 is clinically dysfunctional? Brain Behav. Immun. 2020; 87 :97–98. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lee S.W., Yang J.M., Moon S.Y., Yoo I.K., Ha E.K., Kim S.Y., Park U.M., Choi S., Lee S.H., Ahn Y.M., Kim J.M., Koh H.Y., Yon D.K. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. The Lancet. Psychiatry. 2020; 7 :1025–1031. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li L., Li F., Fortunati F., Krystal J.H. Association of a prior psychiatric diagnosis with mortality among hospitalized patients with coronavirus disease 2019 (COVID-19) infection. JAMA network open. 2020; 3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020; 291 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li W., Zhang Y., Wang J., Ozaki A., Wang Q., Chen Y., Jiang Q. Association of home quarantine and mental health among teenagers in Wuhan, China, during the COVID-19 pandemic. JAMA Pediatr. 2021; 175 :313–316. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li Y., Zhao J., Ma Z., McReynolds L.S., Lin D., Chen Z., Wang T., Wang D., Zhang Y., Zhang J., Fan F., Liu X. Mental health among college students during the COVID-19 pandemic in China: a 2-wave longitudinal survey. J. Affect. Disord. 2021; 281 :597–604. [ PubMed ] [ Google Scholar ]
- Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int. J. Environ. Res. Public Health. 2020:17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lin W., Wu B., Chen B., Lai G., Huang S., Li S., Liu K., Zhong C., Huang W., Yuan S., Wang Y. Sleep conditions associate with anxiety and depression symptoms among pregnant women during the epidemic of COVID-19 in Shenzhen. J. Affect. Disord. 2021; 281 :567–573. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Res. 2021; 295 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu S., Liu Y., Liu Y. Somatic symptoms and concern regarding COVID-19 among Chinese college and primary school students: a cross-sectional survey. Psychiatry Res. 2020; 289 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu X., Chen M., Wang Y., Sun L., Zhang J., Shi Y., Wang J., Zhang H., Sun G., Baker P.N., Luo X., Qi H. Prenatal anxiety and obstetric decisions among pregnant women in Wuhan and Chongqing during the COVID-19 outbreak: a cross-sectional study. BJOG. 2020; 127 :1229–1240. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lopez-Morales H., Del Valle M.V., Canet-Juric L., Andres M.L., Galli J.I., Poo F., Urquijo S. Mental health of pregnant women during the COVID-19 pandemic: a longitudinal study. Psychiatry Res. 2021; 295 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Losada-Baltar A., Jimenez-Gonzalo L., Gallego-Alberto L., Pedroso-Chaparro M.D.S., Fernandes-Pires J., Marquez-Gonzalez M. "We are staying at home." association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021; 76 :e10–e16. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Luceno-Moreno L., Talavera-Velasco B., Garcia-Albuerne Y., Martin-Garcia J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health. 2020:17. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. Am. Psychol. 2020; 75 :897–908. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ma J., Hua T., Zeng K., Zhong B., Wang G., Liu X. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: a case-control study. Transl. Psychiatry. 2020; 10 :411. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Marchini S., Zaurino E., Bouziotis J., Brondino N., Delvenne V., Delhaye M. Study of resilience and loneliness in youth (18-25 years old) during the COVID-19 pandemic lockdown measures. J. Commun. Psychol. 2020 [ PubMed ] [ Google Scholar ]
- Martins Van Jaarsveld G. The effects of COVID-19 among the elderly population: a case for closing the digital divide. Front Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Matsushima M., Horiguchi H. The COVID-19 pandemic and mental well-being of pregnant women in japan: need for economic and social policy interventions. Disaster Med. Public Health Prep. 2020:1–6. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Maunder R.G., Lancee W.J., Mae R., Vincent L., Peladeau N., Beduz M.A., Hunter J.J., Leszcz M. Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv. Res. 2010; 10 :72. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- McGinty E.E., Presskreischer R., Han H., Barry C.L. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020; 324 :93–94. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Medina-Jimenez V., Bermudez-Rojas M.L., Murillo-Bargas H., Rivera-Camarillo A.C., Munoz-Acosta J., Ramirez-Abarca T.G., Esparza-Valencia D.M., Angeles-Torres A.C., Lara-Avila L., Hernandez-Munoz V.A., Madrigal-Tejeda F.J., Estudillo-Jimenez G.E., Jacobo-Enciso L.M., Torres-Torres J., Espino Y.S.S., Baltazar-Martinez M., Villanueva-Calleja J., Nava-Sanchez A.E., Mendoza-Carrera C.E., Aguilar-Torres C., Celis-Gonzalez C., Martinez-Portilla R.J. The impact of the COVID-19 pandemic on depression and stress levels in pregnant women: a national survey during the COVID-19 pandemic in Mexico. J. Maternal-Fetal Neonatal Med. 2020:1–3. [ PubMed ] [ Google Scholar ]
- Moore S.A., Faulkner G., Rhodes R.E., Brussoni M., Chulak-Bozzer T., Ferguson L.J., Mitra R., O'Reilly N., Spence J.C., Vanderloo L.M., Tremblay M.S. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int. J. Behav. Nutr. Phys. Act. 2020; 17 :85. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mortazavi F., Mehrabadi M., KiaeeTabar R. Pregnant women's well-being and worry during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth. 2021; 21 :59. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mosheva M., Hertz-Palmor N., Dorman Ilan S., Matalon N., Pessach I.M., Afek A., Ziv A., Kreiss Y., Gross R., Gothelf D. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress Anxiety. 2020; 37 :965–971. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mutluer T., Doenyas C., Aslan Genc H. Behavioral implications of the COVID-19 process for autism spectrum disorder, and individuals' comprehension of and reactions to the pandemic conditions. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nania T., Dellafiore F., Caruso R., Barello S. Risk and protective factors for psychological distress among Italian university students during the COVID-19 pandemic: the beneficial role of health engagement. Int. J. Soc. Psychiatry. 2020 [ PubMed ] [ Google Scholar ]
- Nanjundaswamy M.H., Shiva L., Desai G., Ganjekar S., Kishore T., Ram U., Satyanarayana V., Thippeswamy H., Chandra P.S. COVID-19-related anxiety and concerns expressed by pregnant and postpartum women-a survey among obstetricians. Arch. Womens Ment. Health. 2020; 23 :787–790. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nederhof E., Schmidt M.V. Mismatch or cumulative stress: toward an integrated hypothesis of programming effects. Physiol. Behav. 2012; 106 :691–700. [ PubMed ] [ Google Scholar ]
- Nissen J.B., Hojgaard D., Thomsen P.H. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020; 20 :511. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nitschke J.P., Forbes P.A.G., Ali N., Cutler J., Apps M.A.J., Lockwood P.L., Lamm C. Resilience during uncertainty? Greater social connectedness during COVID-19 lockdown is associated with reduced distress and fatigue. Br. J. Health Psychol. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nomura S., Kawashima T., Yoneoka D., Tanoue Y., Eguchi A., Gilmour S., Kawamura Y., Harada N., Hashizume M. Trends in suicide in Japan by gender during the COVID-19 pandemic, up to September 2020. Psychiatry Res. 2021; 295 [ PubMed ] [ Google Scholar ]
- Odriozola-Gonzalez P., Planchuelo-Gomez A., Irurtia M.J., de Luis-Garcia R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020; 290 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Oosterhoff B., Palmer C.A., Wilson J., Shook N. Adolescents' motivations to engage in social distancing during the COVID-19 pandemic: associations with mental and social health. J. Adolesc. Health. 2020; 67 :179–185. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Orgiles M., Morales A., Delvecchio E., Mazzeschi C., Espada J.P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front. Psychol. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ozamiz-Etxebarria N., Idoiaga Mondragon N., Dosil Santamaria M., Picaza Gorrotxategi M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in Northern Spain. Front. Psychol. 2020; 11 :1491. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pan K.Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jorg F., Luteijn R.A., Rhebergen D., Oppen P.V., Giltay E.J., Penninx B. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021; 8 :121–129. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Papadopoulou A., Efstathiou V., Yotsidi V., Pomini V., Michopoulos I., Markopoulou E., Papadopoulou M., Tsigkaropoulou E., Kalemi G., Tournikioti K., Douzenis A., Gournellis R. Suicidal ideation during COVID-19 lockdown in Greece: prevalence in the community, risk and protective factors. Psychiatry Res. 2021; 297 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Parlapani E., Holeva V., Nikopoulou V.A., Sereslis K., Athanasiadou M., Godosidis A., Stephanou T., Diakogiannis I. Intolerance of Uncertainty and Loneliness in Older Adults During the COVID-19 Pandemic. Front Psychiatry. 2020; 11 :842. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., Letterie M., Davis M.M. Well-being of parents and children during the COVID-19 pandemic: a national survey. Pediatrics. 2020; 146 [ PubMed ] [ Google Scholar ]
- Penner F., Ortiz J.H., Sharp C. Change in youth mental health during the COVID-19 pandemic in a majority hispanic/Latinx US sample. J. Am. Acad. Child Adolesc. Psychiatry. 2020 [ PubMed ] [ Google Scholar ]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., Rogoll J., Grosse J., Strohle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020; 10 :e01745. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet. Psychiatry. 2020; 7 :883–892. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S., John A., Kontopantelis E., Webb R.T., Wessely S., Abel K.M. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pigaiani Y., Zoccante L., Zocca A., Arzenton A., Menegolli M., Fadel S., Ruggeri M., Colizzi M. Adolescent lifestyle behaviors, coping strategies and subjective wellbeing during the COVID-19 pandemic: an online student survey. Healthcare. 2020; 8 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pinkham A.E., Ackerman R.A., Depp C.A., Harvey P.D., Moore R.C. A longitudinal investigation of the effects of the COVID-19 pandemic on the mental health of individuals with pre-existing severe mental illnesses. Psychiatry Res. 2020; 294 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. Am. Psychol. 2020; 75 :631–643. [ PubMed ] [ Google Scholar ]
- Qi M., Zhou S.J., Guo Z.C., Zhang L.G., Min H.J., Li X.M., Chen J.X. The effect of social support on mental health in chinese adolescents during the outbreak of COVID-19. J. Adolesc. Health. 2020; 67 :514–518. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ran L., Wang W., Ai M., Kong Y., Chen J., Kuang L. Psychological resilience, depression, anxiety, and somatization symptoms in response to COVID-19: a study of the general population in China at the peak of its epidemic. Soc. Sci. Med. 2020; 262 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ravaldi C., Ricca V., Wilson A., Homer C., Vannacci A. Previous psychopathology predicted severe COVID-19 concern, anxiety, and PTSD symptoms in pregnant women during "lockdown" in Italy. Arch. Womens Ment. Health. 2020; 23 :783–786. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Richards T., Scowcroft H. Patient and public involvement in covid-19 policy making. BMJ. 2020; 370 :m2575. [ PubMed ] [ Google Scholar ]
- Riehm K.E., Brenneke S.G., Adams L.B., Gilan D., Lieb K., Kunzler A.M., Smail E.J., Holingue C., Stuart E.A., Kalb L.G., Thrul J. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J. Affect. Disord. 2021; 282 :381–385. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Roberts T., Daniels J., Hulme W., Horner D., Lyttle M.D., Samuel K., Graham B., Hirst R., Reynard C., Barrett M., Carlton E. COVID-19 emergency response assessment study: a prospective longitudinal survey of frontline doctors in the UK and Ireland: study protocol. BMJ Open. 2020; 10 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Robinson E., Daly M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: longitudinal evidence from the Understanding America Study. Br. J. Health Psychol. 2020 [ PubMed ] [ Google Scholar ]
- Robles-Bello M.A., Sanchez-Teruel D., Valencia Naranjo N. Variables protecting mental health in the Spanish population affected by the COVID-19 pandemic. Curr. Psychol. 2020:1–12. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rodriguez-Gonzalez R., Facal D., Martinez-Santos A.E., Gandoy-Crego M. Psychological, social and health-related challenges in spanish older adults during the lockdown of the COVID-19 first wave. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020; 7 :611–627. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Romero E., Lopez-Romero L., Dominguez-Alvarez B., Villar P., Gomez-Fraguela J.A. Testing the effects of COVID-19 confinement in Spanish children: the role of parents' distress, emotional problems and specific parenting. Int. J. Environ. Res. Public Health. 2020; 17 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rutherford B.R., Choi C.J., Chrisanthopolous M., Salzman C., Zhu C., Montes-Garcia C., Liu Y., Brown P.J., Yehuda R., Flory J., Neria Y., Roose S.P. The COVID-19 pandemic as a traumatic stressor: mental health responses of older adults with chronic PTSD. Am. J. Geriatr. Psychiatry. 2021; 29 :105–114. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sade S., Sheiner E., Wainstock T., Hermon N., Yaniv Salem S., Kosef T., Lanxner Battat T., Oron S., Pariente G. Risk for depressive symptoms among hospitalized women in high-risk pregnancy units during the COVID-19 pandemic. J. Clin. Med. 2020; 9 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sahin M.K., Aker S., Sahin G., Karabekiroglu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J. Commun. Health. 2020; 45 :1168–1177. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sáiz P.A., de la Fuente-Tomas L., García-Alvarez L., Bobes-Bascarán M.T., Moya-Lacasa C., García-Portilla M.P., Bobes J. Prevalence of passive suicidal ideation in the early stage of the coronavirus disease 2019 (COVID-19) pandemic and lockdown in a large Spanish sample. J. Clin. Psychiatry. 2020:81. [ PubMed ] [ Google Scholar ]
- Sasaki N., Kuroda R., Tsuno K., Kawakami N. The deterioration of mental health among healthcare workers during the COVID-19 outbreak: a population-based cohort study of workers in Japan. Scand J. Work Environ. Health. 2020; 46 :639–644. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schiele M.A., Herzog K., Kollert L., Schartner C., Leehr E.J., Bohnlein J., Repple J., Rosenkranz K., Lonsdorf T.B., Dannlowski U., Zwanzger P., Reif A., Pauli P., Deckert J., Domschke K. Extending the vulnerability-stress model of mental disorders: three-dimensional NPSR1 x environment x coping interaction study in anxiety. Br. J. Psychiatry. 2020; 217 :645–650. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schiele M.A., Ziegler C., Holitschke K., Schartner C., Schmidt B., Weber H., Reif A., Romanos M., Pauli P., Zwanzger P., Deckert J., Domschke K. Influence of 5-HTT variation, childhood trauma and self-efficacy on anxiety traits: a gene-environment-coping interaction study. J. Neural Transm. (Vienna) 2016; 123 :895–904. [ PubMed ] [ Google Scholar ]
- Schmidt M.V. Animal models for depression and the mismatch hypothesis of disease. Psychoneuroendocrinology. 2011; 36 :330–338. [ PubMed ] [ Google Scholar ]
- Schweda A., Weismuller B., Bauerle A., Dorrie N., Musche V., Fink M., Kohler H., Teufel M., Skoda E.M. Phenotyping mental health: age, community size, and depression differently modulate COVID-19-related fear and generalized anxiety. Compr. Psychiatry. 2021; 104 [ PubMed ] [ Google Scholar ]
- Serafini G., Parmigiani B., Amerio A., Aguglia A., Sher L., Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shahid A., Javed A., Rehman S., Tariq R., Ikram M., Suhail M. Evaluation of psychological impact, depression, and anxiety among pregnant women during the COVID-19 pandemic in Lahore, Pakistan. Int. J. Gynaecol. Obstet. 2020; 151 :462–465. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shanahan L., Steinhoff A., Bechtiger L., Murray A.L., Nivette A., Hepp U., Ribeaud D., Eisner M. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol. Med. 2020:1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shevlin M., Butter S., McBride O., Murphy J., Gibson-Miller J., Hartman T.K., Levita L., Mason L., Martinez A.P., McKay R., Stocks T.V.A., Bennett K., Hyland P., Bentall R.P. Refuting the myth of a 'tsunami' of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol. Med. 2021:1–9. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simonetti A., Pais C., Jones M., Cipriani M.C., Janiri D., Monti L., Landi F., Bernabei R., Liperoti R., Sani G. Neuropsychiatric symptoms in elderly with dementia during COVID-19 pandemic: definition, treatment, and future directions. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Singh, G.P., 2020. Lockdown and 3 Waves of Suicide in India During the COVID-19 Pandemic. The primary care companion for CNS disorders 22. [ PubMed ]
- Sole B., Verdolini N., Amoretti S., Montejo L., Rosa A.R., Hogg B., Garcia-Rizo C., Mezquida G., Bernardo M., Martinez-Aran A., Vieta E., Torrent C. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J. Affect. Disord. 2021; 281 :13–23. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Son C., Hegde S., Smith A., Wang X., Sasangohar F. Effects of COVID-19 on college students' mental health in the united states: interview survey study. J. Med. Internet Res. 2020; 22 :e21279. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- South J., Stansfield J., Amlot R., Weston D. Sustaining and strengthening community resilience throughout the COVID-19 pandemic and beyond. Perspect. Public Health. 2020; 140 :305–308. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spalletta G., Porcari D.E., Banaj N., Ciullo V., Palmer K. Effects of COVID-19 infection control measures on appointment cancelation in an italian outpatient memory clinic. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sun F., Zhu J., Tao H., Ma Y., Jin W. A systematic review involving 11,187 participants evaluating the impact of COVID-19 on anxiety and depression in pregnant women. J. Psychosom. Obstet. Gynaecol. 2020:1–9. [ PubMed ] [ Google Scholar ]
- Tanaka T., Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 2021; 5 :229–238. [ PubMed ] [ Google Scholar ]
- Tanir Y., Karayagmurlu A., Kaya I., Kaynar T.B., Turkmen G., Dambasan B.N., Meral Y., Coskun M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020; 293 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021; 8 :130–140. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taquet M., Quoidbach J., Fried E.I., Goodwin G.M. Mood homeostasis before and during the coronavirus disease 2019 (COVID-19) lockdown among students in the Netherlands. JAMA Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Taubman-Ben-Ari O., Chasson M., Abu Sharkia S., Weiss E. Distress and anxiety associated with COVID-19 among Jewish and Arab pregnant women in Israel. J. Reprod. Infant Psychol. 2020; 38 :340–348. [ PubMed ] [ Google Scholar ]
- Thakur V., Jain A. COVID 2019-suicides: a global psychological pandemic. Brain Behav. Immun. 2020; 88 :952–953. [ PMC free article ] [ PubMed ] [ Google Scholar ] Retracted
- Tso W.W.Y., Wong R.S., Tung K.T.S., Rao N., Fu K.W., Yam J.C.S., Chua G.T., Chen E.Y.H., Lee T.M.C., Chan S.K.W., Wong W.H.S., Xiong X., Chui C.S., Li X., Wong K., Leung C., Tsang S.K.M., Chan G.C.F., Tam P.K.H., Chan K.L., Kwan M.Y.W., Ho M.H.K., Chow C.B., Wong I.C.K., Lp P. Vulnerability and resilience in children during the COVID-19 pandemic. Eur. Child Adolesc. Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Turkoglu S., Ucar H.N., Cetin F.H., Guler H.A., Tezcan M.E. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol. Int. 2020; 37 :1207–1213. [ PubMed ] [ Google Scholar ]
- van der Velden P.G., Contino C., Das M., van Loon P., Bosmans M.W.G. Anxiety and depression symptoms, and lack of emotional support among the general population before and during the COVID-19 pandemic. A prospective national study on prevalence and risk factors. J. Affect. Disord. 2020; 277 :540–548. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Varma P., Junge M., Meaklim H., Jackson M.L. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: a global cross-sectional survey. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Verdolini N., Amoretti S., Montejo L., Garcia-Rizo C., Hogg B., Mezquida G., Rabelo-da-Ponte F.D., Vallespir C., Radua J., Martinez-Aran A., Pacchiarotti I., Rosa A.R., Bernardo M., Vieta E., Torrent C., Sole B. Resilience and mental health during the COVID-19 pandemic. J. Affect. Disord. 2021; 283 :156–164. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vinkers C.H., Kalafateli A.L., Rutten B.P., Kas M.J., Kaminsky Z., Turner J.D., Boks M.P. Traumatic stress and human DNA methylation: a critical review. Epigenomics. 2015; 7 :593–608. [ PubMed ] [ Google Scholar ]
- Vinkers C.H., van Amelsvoort T., Bisson J.I., Branchi I., Cryan J.F., Domschke K., Howes O.D., Manchia M., Pinto L., de Quervain D., Schmidt M.V., van der Wee N.J.A. Stress resilience during the coronavirus pandemic. Eur. Neuropsychopharmacol. 2020; 35 :12–16. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020; 87 :40–48. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Y., Kala M.P., Jafar T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS ONE. 2020; 15 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Waselewski E.A., Waselewski M.E., Chang T. Needs and Coping Behaviors of Youth in the US During COVID-19. J. Adolesc. Health. 2020; 67 :649–652. [ PubMed ] [ Google Scholar ]
- Wathelet M., Duhem S., Vaiva G., Baubet T., Habran E., Veerapa E., Debien C., Molenda S., Horn M., Grandgenevre P., Notredame C.E., D'Hondt F. Factors associated with mental health disorders among university students in france confined during the COVID-19 pandemic. JAMA Netw. Open. 2020; 3 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weerkamp-Bartholomeus P., Marazziti D., van Amelsvoort T. Remote W.A.R.A. Compared with face-to-face W.A.R.A.: a pilot study. Front. Psychol. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Whitehead B.R., Torossian E. Older adults' experience of the COVID-19 pandemic: a mixed-methods analysis of stresses and joys. Gerontologist. 2021; 61 :36–47. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- WHO Mental health and psychosocial considerations during the COVID-19 outbreak. World Health Organ. 2020 [ Google Scholar ]
- Wiguna T., Anindyajati G., Kaligis F., Ismail R.I., Minayati K., Hanafi E., Murtani B.J., Wigantara N.A., Putra A.A., Pradana K. Brief research report on adolescent mental well-being and school closures during the COVID-19 pandemic in Indonesia. Front. Psychiatry. 2020; 11 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Willis J.C., Lord G.M. Immune biomarkers: the promises and pitfalls of personalized medicine. Nat. Rev. Immunol. 2015; 15 :323–329. [ PubMed ] [ Google Scholar ]
- Xie X., Xue Q., Zhou Y., Zhu K., Liu Q., Zhang J., Song R. Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 2020; 174 :898–900. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Xin M., Luo S., She R., Yu Y., Li L., Wang S., Ma L., Tao F., Zhang J., Zhao J., Li L., Hu D., Zhang G., Gu J., Lin D., Wang H., Cai Y., Wang Z., You H., Hu G., Lau J.T. Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. Am. Psychol. 2020; 75 :607–617. [ PubMed ] [ Google Scholar ]
- Yang S., Guo B., Ao L., Yang C., Zhang L., Zhou J., Jia P. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin. Obes. 2020; 10 :e12416. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yang Y., Li W., Zhang Q., Zhang L., Cheung T., Xiang Y.T. Mental health services for older adults in China during the COVID-19 outbreak. The Lancet. Psychiatry. 2020; 7 :e19. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. The Lancet. Psychiatry. 2020; 7 :e21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yassa M., Birol P., Yirmibes C., Usta C., Haydar A., Yassa A., Sandal K., Tekin A.B., Tug N. Near-term pregnant women's attitude toward, concern about and knowledge of the COVID-19 pandemic. J. Matern. Fetal Neonatal. Med. 2020; 33 :3827–3834. [ PubMed ] [ Google Scholar ]
- Yassa M., Yassa A., Yirmibes C., Birol P., Unlu U.G., Tekin A.B., Sandal K., Mutlu M.A., Cavusoglu G., Tug N. Anxiety levels and obsessive compulsion symptoms of pregnant women during the COVID-19 pandemic. Turk J. Obstet. Gynecol. 2020; 17 :155–160. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Yue C., Liu C., Wang J., Zhang M., Wu H., Li C., Yang X. Association between social support and anxiety among pregnant women in the third trimester during the coronavirus disease 2019 (COVID-19) epidemic in Qingdao, China: the mediating effect of risk perception. Int. J. Soc. Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zager Kocjan G., Kavcic T., Avsec A. Resilience matters: explaining the association between personality and psychological functioning during the COVID-19 pandemic. Int. J. Clin. Health Psychol. 2021; 21 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang C.J., He Z., Chan N.K., Huang J., Wang H., Yin Z., Akinwunmi B., Ming W.K. Psychobehavioral responses, post-traumatic stress and depression in pregnancy during the early phase of COVID-19 outbreak. Psychiatric Res. Clin. Pract. 2020 W.H. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang J., Shuai L., Yu H., Wang Z., Qiu M., Lu L., Cao X., Xia W., Wang Y., Chen R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatr. 2020; 51 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang J., Yang Z., Wang X., Li J., Dong L., Wang F., Li Y., Wei R., Zhang J. The relationship between resilience, anxiety and depression among patients with mild symptoms of COVID-19 in China: a cross-sectional study. J. Clin. Nurs. 2020; 29 :4020–4029. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang S.X., Wang Y., Jahanshahi A.A., Li J., Schmitt V.G.H. Early evidence and predictors of mental distress of adults one month in the COVID-19 epidemic in Brazil. J. Psychosom Res. 2021; 142 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang Y., Ma Z.F. Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int. J. Soc. Psychiatry. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., Liu M., Chen X., Chen J.X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020; 29 :749–758. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou Y., Shi H., Liu Z., Peng S., Wang R., Qi L., Li Z., Yang J., Ren Y., Song X., Zeng L., Qian W., Zhang X. The prevalence of psychiatric symptoms of pregnant and non-pregnant women during the COVID-19 epidemic. Transl. Psychiatry. 2020; 10 :319. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zorn J.V., Schur R.R., Boks M.P., Kahn R.S., Joels M., Vinkers C.H. Cortisol stress reactivity across psychiatric disorders: a systematic review and meta-analysis. Psychoneuroendocrinology. 2017; 77 :25–36. [ PubMed ] [ Google Scholar ]

The Many Faces of Stress During the COVID-19 Pandemic
Emerging themes from population-based studies on stress during the pandemic..
Posted November 25, 2020 | Reviewed by Devon Frye
- What Is Stress?
- Take our Burnout Test
- Find a therapist to overcome stress
Prior to the global pandemic, America had already been dealing with a host of pervasive stressors such as health care access, mass shootings , climate change , rising suicide rates, and an opioid epidemic. Fast forward to the present day, as our country continues to struggle with our new reality amidst the global pandemic, select groups of our country are facing greater stress and poorer outcomes. It’s important to consider the many factors that create stress and related mental health issues so we can find new solutions in an increasingly complex time.
There are two recent studies that help shed light on the trends creating increased challenges for many people:
Two months ago, the CDC published a study by Czeisler et al. that identified potential epidemiological trends in mental health amongst adults in the U.S. throughout a several-month period of the COVID-19 pandemic. This month, the American Psychological Association (APA), through its Stress in America initiative conducted by the Harris Poll on behalf of the APA, published their findings based on surveys of people across the United States focusing on how stress has been impacting their lives.
There are inherent limitations to both studies, including measurement bias due to self-reporting of symptoms without a clinician-based assessment and sampling bias. This limits the degree of generalizations we can make to the larger U.S. population.
However, we can identify themes based on these two studies and then examine how these have expressed themselves through individual patient narratives. These include:
Uncertainty of the Future
One of the greatest human fears is that of uncertainty, or loss of our sense of control. The pandemic has introduced a significant amount of stress due to uncertainty for Gen Z adults (ages 18-23) who are unable to attend college on campus or are encountering limited open jobs and career opportunities upon graduating. Gen Z adults report that the future of our nation is a significant source of stress with the majority also citing the U.S. presidential election as a stressful source of uncertainty.
Moral Injury as a Result of Human Injustice
Moral injury is defined as an inner mental conflict that results when one’s actions or obligations are in direct opposition to a person's values and beliefs. Largely due to the pandemic and sociopolitical climate, 2020 has brought increased awareness of systemic racism in our nation. Nearly 2 in 3 adults—regardless of race—report police violence towards minorities as a significant source of stress, up from 1 in 3 adults who responded with the same answer in 2016. Furthermore, minorities, in particular Black Americans, are most likely to report discrimination as a stressor.
Disruption of Customs and Traditions
Traditions offer us a way to celebrate, reflect, grieve, and commemorate milestones in our lives. Young individuals in particular are sacrificing their graduations, college experiences, and social celebrations, making them feel lost and without a sense of belonging. For some young adults, the pandemic has disrupted wedding celebrations which represent a major milestone being postponed or reduced in scope. Across all walks of life, funeral services for loved ones have been greatly limited in attendance, often being performed virtually. These impacts on religious ceremonies and holidays have created a great deal of grief and separation where there was once celebration and togetherness.
Caretaking Overload and Burnout
For many, the mandated sheltering-at-home orders have magnified the duties and responsibility of caregivers. If the caregiver has previously relied on a combination of school and professional care, the COVID-19 pandemic has introduced a larger source of stress of balancing work and family. This has led to fatigue, stress, and—in some cases— depression .
Grief and Loss
The pandemic has brought loss into the forefront. For many Americans, the pandemic has resulted in a loss of jobs leading to financial instability. The drastic reduction in social interactions has led to increasing loneliness . And the loss of loved ones—in some cases without having a chance to sit at a bedside or say goodbye—has led to an overwhelming sense of dread, pessimism , and a lack of closure. For all of us, the pandemic has changed the way that we live our lives and we have had to grapple with and grieve the loss of our “normal” lives.
Trauma Due to COVID-19 Exposure
Studies of frontline health care workers during the COVID-19 pandemic have shown that rates of trauma-related symptoms, depression, and anxiety have increased during the pandemic. These have been related to experienced helplessness related to treating severely ill patients in a stressed and overwhelmed health system that has not yet identified effective and consistent treatments. In addition, the experience of continually exposing themselves (and family) to a virus that can lead to a life-threatening illness creates elevated stress levels in front-line workers.

With all of these factors in play, it can feel overwhelming to support ourselves and others through this challenging time. It’s important to remember that we are resilient as humans and that there are solutions we can turn to.
Czeisler MÉ , Lane RI, Petrosky E, et al. Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–1057.
https://www.apa.org/news/press/releases/stress/2020/report-october

Marc Lener, MD, is a psychiatrist in private practice in New York City and Founder and Chief Executive Officer of Singula Institute, a 501(c)(3) organization, whose vision is to transform mental health diagnostics and treatment for individuals at risk for anxiety and depression.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

Sticking up for yourself is no easy task. But there are concrete skills you can use to hone your assertiveness and advocate for yourself.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- JME Commentaries
- BMJ Journals
You are here
- Volume 47, Issue 6
- Levels of stress in medical students due to COVID-19
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-3700-2782 Lorcan O'Byrne 1 ,
- http://orcid.org/0000-0002-5338-906X Blánaid Gavin 2 ,
- http://orcid.org/0000-0003-1315-1695 Dimitrios Adamis 3 , 4 ,
- You Xin Lim 1 ,
- http://orcid.org/0000-0001-9428-6908 Fiona McNicholas 2 , 5
- 1 School of Medicine , University College Dublin , Dublin , Ireland
- 2 Department of Child and Adolescent Psychiatry, SMMS , University College Dublin , Dublin , Ireland
- 3 Department of Psychiatry , National University of Ireland Galway , Galway , Ireland
- 4 Department of Psychiatry , University of Limerick , Limerick , Ireland
- 5 Department of Child and Adolescent Psychiatry , Our Lady's Children's Hospital , Crumlin , Dublin , Ireland
- Correspondence to Lorcan O'Byrne, University College Dublin, Dublin 4, Ireland; lorcan.obyrne{at}ucdconnect.ie
For medical schools, the COVID-19 pandemic necessitated examination and curricular restructuring as well as significant changes to clinical attachments. With the available evidence suggesting that medical students’ mental health status is already poorer than that of the general population, with academic stress being a chief predictor, such changes are likely to have a significant effect on these students. This online, cross-sectional study aimed to determine the impact of COVID-19 on perceived stress levels of medical students, investigate possible contributing and alleviating factors, and produce recommendations for medical schools to implement during future healthcare emergencies. The majority (54.5%) of respondents reported levels of stress ranging from moderate to extreme. Higher levels of stress were significantly associated with female gender (p=0.039) and international status (p=0.031). A significant association was also noted between reported stress and the transition to online learning (p<0.0001) and online assessment formatting (p<0.0001), concerns for personal health (p<0.0001) and for the health of family members (p<0.0001). Students who reported higher stress levels were less confident in their government’s management of the crisis (p=0.041). Additionally, students who reported lower stress agreed highly that their medical school had an appropriate response to the crisis (p<0.0001), had provided sufficient information regarding the crisis (p=0.015), that they trust their school in handling the continuing of their education (p=0.020) and that their school had appropriate plans in place to support the continuing of education (p=0.017)
Data availability statement
Data are available upon request.
This article is made freely available for use in accordance with BMJ’s website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
https://doi.org/10.1136/medethics-2020-107155
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Contributors Conception or design of the work—LO’B, FMcN and BG. Acquisition of data for the work—LO’B, FMcN, BG and YXL. Analysis of data for the work—LO’B, YXL and DA. Interpretation of data for the work—LO’B and DA. Drafting the work or revising it critically for important intellectual content—LO’B, FMcN, BG, YXL and DA. Final approval of the version to be published—LO’B, FMcN, BG, YXL and DA. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved—LO’B, FMcN, BG, YXL and DA.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Other content recommended for you.
- Value of a UK medical degree for international students (VISION): a cross-sectional study Chun Hei Li et al., BMJ Open, 2023
- Mental burden and perception of the study situation among undergraduate students during the COVID-19 pandemic: a cross-sectional study and comparison of dental and medical students Jennifer Guse et al., BMJ Open, 2021
- Burden and factors associated with perceived stress amidst COVID-19: a population web-based study in Pakistan Maryam Pyar Ali Lakhdir et al., BMJ Open, 2022
- Nutrition education in medical school: the case of international medical students in China William Kwame Amakye et al., BMJ Nutrition, Prevention & Health, 2020
- Impact of COVID-19 pandemic on the mental health of healthcare workers during the first wave in Portugal: a cross-sectional and correlational study Ivone Duarte et al., BMJ Open, 2022
- Impact of the COVID-19 pandemic on the experience and mental health of university students studying in Canada and the UK: a cross-sectional study Jennifer A Appleby et al., BMJ Open, 2022
- Social and psychological impact of the COVID-19 pandemic on UK medical and nursing students: protocol for a national medical and nursing student survey George E Richardson et al., BMJ Open, 2022
- Potential barriers to veterinary student access to counselling and other support systems: perceptions of staff and students at a UK veterinary school K. J. Pickles et al., Veterinary Record, 2011
- Quality of life and associated factors among university students during the COVID-19 pandemic: a cross-sectional study Mohammad Farris Iman Leong Bin Abdullah et al., BMJ Open, 2021
- Role of COVID-19 pandemic in the academic life and well-being of private sector university students: an exploratory qualitative study Naureen Akber Ali et al., BMJ Open, 2022
- Open access
- Published: 28 March 2024
Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support
- Helen M West ORCID: orcid.org/0000-0001-8712-5890 1 ,
- Luke Flain ORCID: orcid.org/0000-0001-7296-6304 2 ,
- Rowan M Davies 3 , 4 ,
- Benjamin Shelley 3 , 5 &
- Oscar T Edginton ORCID: orcid.org/0000-0001-5298-9402 3 , 6
BMC Psychology volume 12 , Article number: 179 ( 2024 ) Cite this article
1018 Accesses
2 Citations
Metrics details
A Publisher Correction to this article was published on 26 June 2024
This article has been updated
Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the ‘coping reservoir’ model of wellbeing.
In synchronous interactive pre-recorded webinars, 78 fourth-year medical students in the UK responded to reflective prompts. Participants wrote open-text comments on a Padlet site. Responses were analysed using reflexive thematic analysis.
Analysis identified five themes. COVID-19 exacerbated academic pressures, while reducing the strategies available to cope with stress. Relational connections with family and friends were affected by the pandemic, leading to isolation and reliance on housemates for informal support. Relationships with patients were adversely affected by masks and telephone consultations, however attending placement was protective for some students’ wellbeing. Experiences of formal support were generally positive, but some students experienced attitudinal and practical barriers.
Conclusions
This study used a novel methodology to elicit medical students’ reflections on their mental wellbeing during COVID-19. Our findings reinforce and extend the ‘coping reservoir’ model, increasing our understanding of factors that contribute to resilience or burnout. Many stressors that medical students typically face were exacerbated during COVID-19, and their access to coping strategies and support were restricted. The changes to relationships with family, friends, patients, and staff resulted in reduced support and isolation. Recognising the importance of relational connections upon medical students’ mental wellbeing can inform future support.
Peer Review reports
Medical students are known to experience high levels of stress, anxiety, depression and burnout due to the nature, intensity and length of their course [ 1 ]. Medical students are apprehensive about seeking support for their mental wellbeing due to perceived stigma and concerns about facing fitness to practise proceedings [ 2 ], increasing their vulnerability to poor mental health.
Research has identified that the stressors medical students experience include a demanding workload, maintaining work–life balance, relationships, personal life events, pressure to succeed, finances, administrative issues, career uncertainty, pressure around assessments, ethical concerns, and exposure to patient death [ 3 , 4 ]. In March 2020, the COVID-19 pandemic introduced additional stressors into medical students’ lives. These included sudden alterations to clinical placements, the delivery of online teaching, uncertainty around exams and progression, ambiguity regarding adequate Personal Protective Equipment (PPE), fear of infection, and increased exposure to death and dying [ 5 , 6 ]. Systematic reviews have reported elevated levels of anxiety, depression and stress among medical students during COVID-19 [ 7 ] and that the prevalence of depression and anxiety during COVID-19 was higher among medical students than in the general population or healthcare workers [ 8 ].
While training, medical students are expected to develop awareness of personal mental wellbeing and learn healthy coping strategies for dealing with stress [ 9 ]. Developing adaptive methods of self-care and stress reduction is beneficial both while studying medicine, and in a doctor’s future career. Protecting and promoting psychological wellbeing has the potential to improve medical students’ academic attainment, as well as their physical and mental wellbeing [ 10 ], and it is therefore important for medical educators to consider how mental wellbeing is fostered. Feeling emotionally supported while at medical school reduces the risk of psychological distress and burnout, and is related to whether students contemplate dropping out of medical training [ 11 ]. In their systematic narrative review of support systems for medical students during COVID-19, Ardekani et al. [ 12 ] propose a framework incorporating four levels: policies that promote a supportive culture and environment, active support for students at higher risk of mental health problems, screening for support needs, and provision for students wishing to access support. This emphasis on preventative strategies aligns with discussions of trauma-informed approaches to medical education, which aim to support student learning and prevent harm to mental wellbeing [ 13 ]. Dunn et al. [ 14 ] proposed a ‘coping reservoir’ model to conceptualise the factors that deplete and restore medical students’ mental wellbeing (Fig. 1 ). This reservoir is drained and filled repeatedly, as a student faces demands for their time, energy, and cognitive and emotional resources. This dynamic process leads to positive or negative outcomes such as resilience or burnout.
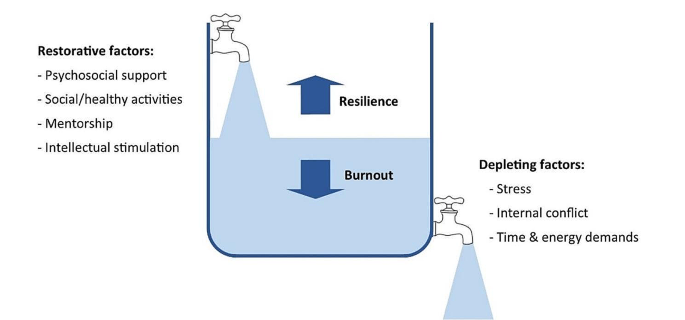
Coping reservoir model– adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
At present we have limited evidence to indicate why medical students’ mental wellbeing was so profoundly affected by COVID-19 and whether students developed coping strategies that enhanced their resilience, as suggested by Kelly et al. [ 15 ]. This study therefore sought to conceptualise the challenges medical students experienced during COVID-19, the coping strategies they developed in response to these stressors, and the supportive measures they valued. The ‘coping reservoir’ model [ 14 ] was chosen as the conceptual framework for this study because it includes both restorative and depleting influences. Understanding the factors that mediate medical students’ mental wellbeing will enable the development of interventions and support that are effective during crises such as the pandemic and more generally.
Methodology
This research study is based on a critical realist paradigm, recognising that our experience of reality is socially located [ 16 ]. Participant responses were understood to represent a shared understanding of that reality, acknowledging the social constructivist position that subjective meanings are formed through social norms and interactions with others, including while participating in this study. It also draws on hermeneutic phenomenology in aiming to interpret everyday experienced meanings for medical students during COVID-19 [ 17 ]. The use of an e-learning environment demonstrates an application of connectivism [ 18 ], a learning theory in which students participate in technological enabled networks. We recognise that meaning is co-constructed by the webinar content, prompts, ‘coping reservoir’ framework and through the process of analysis.
The multidisciplinary research team included a psychologist working in medical education, two medical students, and two Foundation level doctors. The team’s direct experience of the phenomenon studied was an important resource throughout the research process, and the researchers regularly reflected on how their subjective experiences and beliefs informed their interpretation of the data. Reflexive thematic analysis was chosen because it provides access to a socially contextualised reality, encompasses both deductive and inductive orientations so that analysis could be informed by the ‘coping reservoir’ while also generating unanticipated insights, and enables actionable outcomes to be produced [ 19 ].
Ethical approval
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365).
Participants
Fourth-year medical students at the University of Liverpool were invited to participate in the study during an online webinar in their Palliative Medicine placement. During six webinars between November 2020 and June 2021, 78 out of 113 eligible students participated, giving a response rate of 69%. This was a convenience sample of medical students who had a timetabled session on mental wellbeing. At the time, these medical students were attending clinical placements, however COVID-19 measures in the United Kingdom meant that academic teaching and support was conducted online, travel was limited, and contact with family and friends was restricted.
Students were informed about the study prior to the synchronous interactive pre-recorded webinar and had an opportunity to ask questions. Those who consented to participate accessed a Padlet ( www.padlet.com ) site during the webinar that provided teaching on mental wellbeing, self-care and resilience in the context of palliative medicine. Padlet is a collaborative online platform that hosts customisable virtual bulletin boards. During this recording, participants were asked to write anonymous open-text responses to reflective prompts developed from reviewing the literature (Appendix 1 ), and post these on Padlet. The Padlet board contained an Introduction to the webinar, sections for each prompt, links to references, and signposting to relevant support services. Data files were downloaded to Excel and stored securely, in line with the University of Liverpool Research Data Management Policy.
The research team used the six steps of reflexive thematic analysis to analyse the dataset. This process is described in Table 1 , and the four criteria for trustworthiness in qualitative research proposed by Lincoln and Guba [ 20 ] are outlined in Table 2 . We have used the purposeful approach to reporting thematic analysis recommended by Nowell et al. [ 21 ] and SRQR reporting standards [ 22 ] (Appendix 2 ).
Five themes were identified from the analysis:
COVID-19 exacerbated academic pressures.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress.
COVID-19 changed relationships with family and friends, which affected mental wellbeing.
COVID-19 changed interactions with patients, with positive and negative effects.
Formal support was valued but seeking it was perceived as more difficult during COVID-19.
COVID-19 exacerbated academic pressures
‘Every day feels the same, it’s hard to find motivation to do anything.’
Many participants reported feeling under chronic academic pressure due to studying medicine. Specific stressors reported were exams, revision, deadlines, workload, specific course requirements, timetables, online learning, placement, and communication from University. Some participants also reported negative effects on their mental wellbeing from feelings of comparison and competition, feeling unproductive, and overthinking.
Massive amounts of work load that feels unachievable.
COVID-19 exacerbated these academic stresses, with online learning and monotony identified as particularly draining. However, other students found online learning beneficial, due to reduced travelling.
I miss being able to see people face to face and zoom is becoming exhausting. My mental wellbeing hasn’t been great recently and I think the effects of the pandemic are slowly beginning to affect me.
I also prefer zoom as it is less tiring than travelling to campus/placement.
Clinical placements provided routine and social interaction. However, with few social interactions outside placement, this became monotonous. A reduction in other commitments helped some students to focus on their academic requirements.
‘Most social activity only taking place on placement has made every day feel the same’.
Some students placed high value on continuing to be productive and achieve academically despite the disruption of a pandemic, potentially to the detriment of their mental wellbeing. Time that felt unproductive was frustrating and draining.
‘Having a productive day i.e. going for a run and a good amount of work completed in the day’.
‘Unproductive days of revision or on placement’.
COVID-19 affected students’ lifestyles and reduced their ability to cope with stress
‘Everyone’s mental well-being decreased as things they used for mental health were no longer available’.
Students often found it difficult to sustain motivation for academic work without the respite of their usual restorative activities challenging.
‘Not being able to balance work and social life to the same extent makes you resent work and placement more’.
The competing demands medical students encounter for their time and energy were repeatedly reported by participants.
‘Sometimes having to go to placement + travel + study + look after myself is really tough to juggle!’
However, removing some of the boundaries around academic contact and structure of extracurricular activities heightened the impact of stressors. Many participants focused on organising and managing their time to cope with this. Students were aware that setting time aside for relaxation, enjoyment, creativity, and entertainment would be beneficial for their wellbeing.
‘Taking time off on the weekends to watch movies’.
However, they found it difficult to prioritise these without feeling guilty or believing they needed to ‘earn’ them, and academic commitments were prioritised over mental wellbeing.
‘Try to stop feeling guilty for doing something that isn’t medicine’. ‘Would like to say I’d do more to increase my mental wellbeing but finals are approaching and that will probably have to take priority for the next few months’.
Medical students were generally aware that multiple factors such as physical activity, time with loved ones, spiritual care, nourishment and hobbies had a positive impact on their mental wellbeing. During COVID-19, many of the coping strategies that students had previously found helpful were unavailable.
‘Initially it improved my mental well-being as I found time to care for myself, but with time I think everyone’s mental well-being decreased as things they used for mental health were no longer available e.g. gym, counselling, seeing friends’.
Participants adapted to use coping strategies that remained available during the pandemic. These included walks and time spent outdoors, exercise, journaling, reflection, nutrition, and sleep.
‘Running’. ‘Yoga’. ‘Fresh air and walks’.
A few students also reported that they tried to avoid unhelpful coping strategies, such as social media and alcohol.
‘Not reading the news, not using social media’.
‘Avoiding alcohol as it leads to poor sleep and time wasted’.
Many participants commented on increased loneliness, anxiety, low mood, frustration, and somatic symptoms.
‘Everyone is worn out and demotivated’. ‘Feel that as I am feeling low I don’t want to bring others down’. ‘Feel a lot more anxious than is normal and also easily annoyed and irritable.’
However, not all students reported that COVID-19 had a negative effect on wellbeing. A small minority responded that their wellbeing had improved in some way.
‘I think covid-19 has actually helped me become more self reliant in terms of well-being’.
COVID-19 changed relationships with family and friends, which affected mental wellbeing
‘Family are a huge support for me and I miss seeing them and the lack of human contact.’
Feeling emotionally supported by family and friends was important for medical students to maintain good mental wellbeing. However, COVID-19 predominantly had a negative impact on these relationships. Restrictions, such as being unable to socialise or travel during lockdowns, led to isolation and poor mental wellbeing.
‘Not being able to see friends or travel back home to see friends/family there’.
Participants frequently reported that spending too much time with people, feeling socially isolated, being unable to see people, or having negative social experiences had an adverse effect on their mental wellbeing. Relationships with housemates were a key source of support for some students. However, the increased intensity in housemate relationships caused tension in some cases, which had a particularly negative effect.
‘Much more difficult to have relationships with peers and began feeling very isolated’. ‘Talk about some of the experiences I’ve had on placement with my housemates’. ‘Added strain on my housemates to be the only ones to support me’.
Knowing that their peers were experiencing similar stressors helped to normalise common difficulties. The awareness that personal contacts were also struggling sometimes curtailed seeking informal support to avoid being a burden.
‘Actually discussing difficulties with friends has been most helpful, as it can sometimes feel like you’re the only one struggling, when actually most people are finding this year really difficult’. ‘Family and friends, but also don’t want to burden them as I know I can feel overwhelmed if people are always coming to me for negative conversations’.
COVID-19 changed interactions with patients, with positive and negative effects
‘With patients there has been limited contact and I miss speaking to patients.’
Some students reported positive effects on relationships with patients, and feeling a sense of purpose in talking to patients when their families were not allowed to visit. Medical students felt a moral responsibility to protect patients and other vulnerable people from infection, which contributed to a reduction in socialising even when not constrained by lockdown.
‘Talking to patients who can’t get visitors has actually made me feel more useful’. ‘Anxiety over giving COVID-19 to patients or elderly relatives’.
Students occasionally reported that wearing PPE made interactions with patients more challenging. Students’ contact with patients changed on some placements due to COVID-19, for example replacing in-person appointments with telephone consultations, and they found this challenging and disappointing.
‘Masks are an impediment to meaningful connections with new people’. ‘GP block when I saw no patients due to it all being on the telephone’.
Formal support was valued but seeking it was perceived as more difficult during COVID-19
‘Feel a burden on academic and clinical staff/in the way/annoying so tend to just keep to myself.’
Many participants emphasised the primary importance of support from family and friends, and their responses indicated that most had not sought formal support. While staff remained available and created opportunities for students to seek support, factors such as online learning and increased clinical workloads meant that some students found it harder to build supportive relationships with academic and placement staff and felt disconnected from them, which was detrimental for wellbeing and engagement.
‘Staff have been really helpful on placement but it was clear that in some cases, staff were overwhelmed with the workload created by COVID’. ‘Even though academic staff are available having to arrange meetings over zoom rather than face to face to discuss any problem is off putting’.
A few students described difficulty knowing what support was available, and identifying when they needed it.
‘It’s difficult to access support when you’re not sure what is available. Also you may feel your problems aren’t as serious as other people’s so hold off on seeking support’.
Formal support provided within the University included meetings with Academic Advisors, the School of Medicine wellbeing team, and University counselling service and mental health advisory team. It was also available from NHS services, such as GPs and psychological therapies. Those who had accessed formal support mostly described positive experiences with services. However, barriers to seeking formal support, such as perceived stigma, practicalities, waiting times for certain services, and concern that it may impact their future career were reported by some participants.
‘It is good that some services offer appointments that are after 5pm- this makes it more accessible to healthcare students’. ‘Had good experience with GPs about mental health personally’. ‘Admitting you need help or asking for help would make you look weak’. ‘Reassurance should be provided to medical students that accessing the wellbeing team is not detrimental to their degree. If anything it should be marketed as a professional and responsible thing to do’.
Some students preferred the convenience of remote access, others found phone or video impersonal and preferred in-person contact.
Students expressed that it was helpful when wellbeing support was integrated with academic systems, for example Academic Advisors or placement supervisors.
‘My CCT [primary-care led small group teaching] makes sure to ask how we are getting on and how our placements are going, so I think small groups of people with more contact with someone are more useful then large groups over zoom’. ‘Someone to speak to on palliative care placement, individual time with supervisor to check how we are doing (wellbeing, mental health) - would be a nice quick checkup’.
Participants typically felt able to share openly in an anonymous forum. Reading peers’ comments helped them to see that other students were having similar experiences and challenged unhealthy comparisons.
‘I definitely shared more than I would have done on a zoom call’. ‘I loved this session as it makes you feel like you’re not alone’. ‘Reassuring to know that there are others going through similar things as you’.
Our findings demonstrate that the COVID-19 pandemic exacerbated the stressors medical students experience, and removed some rewarding elements of learning, while reducing access to pre-existing coping strategies. The results support many aspects of the ‘coping reservoir’ framework [ 14 ]. Findings corroborate the restorative effects of psychosocial support and social/healthy activities such as sleep and physical activity, and the depletion of wellbeing due to time and energy demands, stress, and disruptions relating to the pandemic such as online teaching and limited social interaction. Feeling a sense of purpose, from continuing studying or interactions with patients for example, was restorative for wellbeing. Mentorship and intellectual stimulation were present in the responses, but received less attention than psychosocial support and social/healthy activities. Internal conflict is primarily characterised by Dunn et al. [ 14 ] as ambivalence about pursuing a career in medicine, which was not expressed by participants during the study. However, participants identified that their wellbeing was reduced by feeling unproductive and lacking purpose, feeling guilty about taking time for self-care, competing priorities, and comparison with peers, all of which could be described as forms of internal conflict. Different restorative and draining factors appeared to not be equally weighted by the participants responding to the prompts: some appear to be valued more highly, or rely on other needs being met. Possible explanations are that students may be less likely to find intellectual stimulation and mentorship beneficial if they are experiencing reduced social support or having difficulty sleeping, and internal conflict about pursuing a career in medicine might be overshadowed by more immediate concerns, for example about the pandemic. This prioritisation resembles the relationship between physiological and psychological needs being met and academic success [ 23 ], based on Maslow’s hierarchy of needs [ 24 ]. A revised ‘coping reservoir’ model is shown in Fig. 2 .
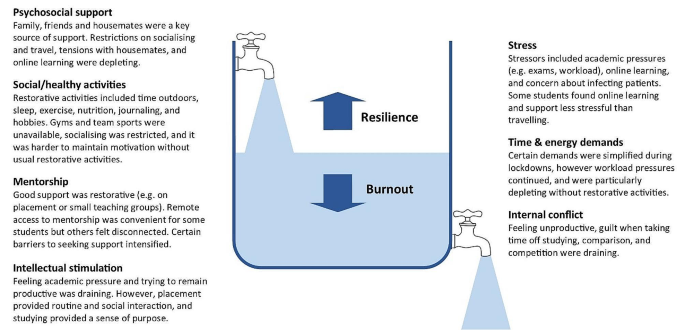
Coping reservoir model - the effects of COVID-19 on restorative and depleting factors for medical students, adapted from Dunn et al. [ 14 ], with permission from the authors and Springer Nature
Relational connections with family, friends, patients, and staff were protective factors for mental wellbeing. Feeling emotionally supported by family and friends is considered especially important for medical students to maintain good mental wellbeing [ 11 ]. These relationships usually mitigate the challenges of medical education [ 25 ], however they were fundamentally affected by the pandemic. Restrictions affecting support from family and friends, and changes to contact with patients on placement, had a negative effect on many participants’ mental wellbeing. Wellbeing support changed during the pandemic, with in-person support temporarily replaced by online consultations due to Government guidelines. Barriers to seeking formal support, such as perceived stigma, practicalities, and concern that it may impact their future career were reported by participants, reflecting previous research [ 26 ]. Despite initiatives to increase and publicise formal support, some students perceived that this was less available and accessible during COVID-19, due to online learning and awareness of the increased workload of clinicians, as described by Rich et al. [ 27 ]. These findings provide further support for the job demand-resources theory [ 28 , 29 ] where key relationships and support provide a protective buffer against the negative effects of challenging work.
In line with previous research, many participants reported feeling under chronic academic pressure while studying medicine [ 3 ]. Our findings indicate that medical students often continued to focus on achievement, productivity and competitiveness, despite the additional pressures of the pandemic. Remaining productive in their studies might have protected some students’ mental wellbeing by providing structure and purpose, however students’ responses primarily reflected the adverse effect this mindset had upon their wellbeing. Some students felt guilty taking time away from studying to relax, which contributes to burnout [ 30 ] , and explicitly prioritised academic achievement over their mental wellbeing.
Students were aware of the factors that have a positive impact on their mental wellbeing, such as physical activity, time with loved ones, spiritual care, nourishment and hobbies [ 31 ]. However, COVID-19 restrictions affected many replenishing factors, such as socialising, team sports, and gyms, and intensified draining factors, such as academic stressors. Students found ways to adapt to the removal of most coping strategies, for example doing home workouts instead of going to the gym, showing how they developed coping strategies that enhanced their resilience [ 15 ]. However, they found it more difficult to mitigate the effect of restrictions on relational connections with peers, patients and staff, and this appears to have had a particularly negative impact on mental wellbeing. While clinical placements provided helpful routine, social interaction and a sense of purpose, some students reported that having few social interactions outside placement became monotonous.
Our findings show that medical students often felt disconnected from peers and academic staff, and reported loneliness, isolation and decreased wellbeing during COVID-19. This corresponds with evidence that many medical students felt isolated [ 32 ], and students in general were at higher risk of loneliness than the general population during COVID-19 lockdowns [ 33 ]. Just as ‘belongingness’ mediates subjective wellbeing among University students [ 34 ], feeling connected and supported acts as a protective buffer for medical students’ psychological wellbeing [ 25 ].
Translation into practice
Based on the themes identified in this study, specific interventions can be recommended to support medical students’ mental wellbeing, summarised in Table 3 . This study provides evidence to support the development of interventions that increase relational connections between medical students, as a method of promoting mental wellbeing and preventing burnout. Our findings highlight the importance of interpersonal relationships and informal support mechanisms, and indicate that medical student wellbeing could be improved by strengthening these. Possible ways to do this include encouraging collaboration over competition, providing sufficient time off to visit family, having a peer mentor network, events that encourage students to meet each other, and wellbeing sessions that combine socialising with learning relaxation and mindfulness techniques. Students could be supported in their interactions with patients and peers by embedding reflective practice such as placement debrief sessions, Schwartz rounds [ 35 ] or Balint groups [ 36 ], and simulated communication workshops for difficult situations.
Experiencing guilt [ 30 ] and competition [ 4 ] while studying medicine are consistently recognised as contributing to distress and burnout, so interventions targeting these could improve mental wellbeing. Based on the responses from students, curriculum-based measures to protect mental wellbeing include manageable workloads, supportive learning environments, cultivating students’ sense of purpose, and encouraging taking breaks from studying without guilt. Normalising sharing of difficulties and regularly including content within the curriculum on self-care and stress reduction would improve mental wellbeing.
In aiming to reduce psychological distress among medical students, it is important that promotion of individual self-care is accompanied by reducing institutional stressors [ 11 , 29 ]. While the exploration of individual factors is important, such as promoting healthy lifestyle habits, reflection, time management, and mindset changes, this should not detract from addressing factors within the culture, learning and work environment that diminish mental wellbeing [ 37 ]. Heath et al. [ 38 ] propose a pro-active, multi-faceted approach, incorporating preventative strategies, organisational justice, individual strategies and organisational strategies to support resilience in healthcare workers. Similarly, trauma-informed medical education practices [ 13 ] involve individual and institutional strategies to promote student wellbeing.
Students favoured formal support that was responsive, individualised, and accessible. For example, integrating conversations about wellbeing into routine academic systems, and accommodating in-person and remote access to support. There has been increased awareness of the wellbeing needs of medical students in recent years, especially since the start of the pandemic, which has led to improvements in many of these areas, as reported in reviews by Ardekani et al. [ 12 ] and Klein and McCarthy [ 39 ]. Continuing to address stigma around mental health difficulties and embedding discussions around wellbeing in the curriculum are crucial for medical students to be able to seek appropriate support.
Strengths & limitations
By using qualitative open-text responses, rather than enforcing preconceived categories, this study captured students’ lived experience and priorities [ 4 , 31 ]. This increased the salience and depth of responses and generated categories of responses beyond the existing evidence, which is particularly important given the unprecedented experiences of COVID-19. Several strategies were used to establish rigour and trustworthiness, based on the four criteria proposed by Lincoln and Guba [ 20 ] (Table 2 ). These included the active involvement of medical students and recent medical graduates in data analysis and the development of themes, increasing the credibility of the research findings.
Potential limitations of the study are that participants may have been primed to think about certain aspects of wellbeing due to data being collected during a webinar delivered by medical educators including the lead author at the start of their palliative medicine placement, and the choice of prompts. Data was collected during the COVID-19 pandemic, and therefore represents fourth year medical students’ views in specific and unusual circumstances. Information on this context is provided to enable the reader to evaluate whether the findings have transferability to their setting. Responses were visible to others in the group, so participants may have influenced each other to give socially acceptable responses. This process of forming subjective meanings through social interactions is recognised as part of the construction of a shared understanding of reality, and we therefore view it as an inherent feature of this methodology rather than a hindrance. Feedback on the webinar indicated that students benefitted from this process of collective meaning-making. Similarly, researcher subjectivity is viewed as a contextual resource for knowledge generation in reflexive thematic analysis, rather than a limitation to be managed [ 19 ]. The study design meant that different demographic groups could not be compared.
Padlet provided a novel and acceptable method of data collection, offering researchers and educators the potential benefits of an anonymous forum in which students can see their peers’ responses. The use of an interactive webinar demonstrated a potential application of connectivist pedagogical principles [ 18 ]. Researchers are increasingly using content from online forums for qualitative research [ 40 ], and Padlet has been extensively used as an educational tool. However, to the authors’ knowledge, Padlet has not previously been used as a data collection platform for qualitative research. Allowing anonymity carried the risk of students posting comments that were inappropriate or unprofessional. However, with appropriate guidance it appeared to engender honesty and reflection, provided a safe and collaborative learning environment, and student feedback was overwhelmingly positive. It would be useful to evaluate the effects of this reflective webinar on medical students’ mental wellbeing, given that it acted as an intervention in addition to a teaching session and research study.
Students were prompted to plan what they would do following the webinar to improve their mental wellbeing. A longitudinal study to determine how students enacted these plans would allow a more detailed investigation of students’ self-care behaviour.
While we hope that the stressors of COVID-19 will not be repeated, this study provides valuable insight into medical students’ mental wellbeing, which can inform support beyond this exceptional time. The lasting impact of the pandemic upon medical education and mental wellbeing remains to be seen. Nevertheless, our findings reinforce and extend the coping reservoir model proposed by Dunn et al. [ 14 ], adding to our understanding of the factors that contribute to resilience or burnout. In particular, it provides evidence for the development of interventions that increase experiences of relational connectedness and belonging, which are likely to act as a buffer against emotional distress among medical students.
Data availability
The datasets generated and analysed during the study are available from the corresponding author on reasonable request.
Change history
26 june 2024.
A Correction to this paper has been published: https://doi.org/10.1186/s40359-024-01813-7
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. JAMA. 2016;316(21):2214.
Article PubMed PubMed Central Google Scholar
Awad F, Awad M, Mattick K, Dieppe P. Mental health in medical students: time to act. Clin Teach. 2019;16(4):312–6.
Article PubMed Google Scholar
Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: causes, consequences, and proposed solutions. Mayo Clin Proc. 2005;80(12):1613–22.
Hill MR, Goicochea S, Merlo LJ. In their own words: stressors facing medical students in the millennial generation. Med Educ Online. 2018;23(1):1530558.
Papapanou M, Routsi E, Tsamakis K, Fotis L, Marinos G, Lidoriki I, et al. Medical education challenges and innovations during COVID-19 pandemic. Postgrad Med J. 2021;0:1–7.
Google Scholar
De Andres Crespo M, Claireaux H, Handa AI. Medical students and COVID-19: lessons learnt from the 2020 pandemic. Postgrad Med J. 2021;97(1146):209–10.
Paz DC, Bains MS, Zueger ML, Bandi VR, Kuo VY, Cook K et al. COVID-19 and mental health: a systematic review of international medical student surveys. Front Psychol. 2022;(November):1–13.
Jia Q, Qu Y, Sun H, Huo H, Yin H, You D. Mental health among medical students during COVID-19: a systematic review and meta-analysis. Front Psychol. 2022;13:846789.
General Medical Council. Outcomes for Graduates. London; 2020 https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates [accessed 13 Feb 2024].
Shiralkar MT, Harris TB, Eddins-Folensbee FF, Coverdale JH. A systematic review of stress-management programs for medical students. Acad Psychiatry. 2013;37(3):158–64.
McLuckie A, Matheson KM, Landers AL, Landine J, Novick J, Barrett T, et al. The relationship between psychological distress and perception of emotional support in medical students and residents and implications for educational institutions. Acad Psychiatry. 2018;42(1):41–7.
Ardekani A, Hosseini SA, Tabari P, Rahimian Z, Feili A, Amini M. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med Educ. 2021;21:352.
Brown T, Berman S, McDaniel K, Radford C, Mehta P, Potter J, et al. Trauma-informed medical education (TIME): advancing curricular content and educational context. Acad Med. 2021;96(5):661–7.
Dunn LB, Iglewicz A, Moutier C. Promoting resilience and preventing burnout. Acad Psychiatry. 2008;32(1):44–53.
Kelly EL, Casola AR, Smith K, Kelly S, Syl M, Cruz D, De. A qualitative analysis of third-year medical students ’ reflection essays regarding the impact of COVID-19 on their education. BMC Med Educ. 2021;21(481).
Pilgrim D. Some implications of critical realism for mental health research. Soc Theory Heal. 2014;12:1–21.
Article Google Scholar
Henriksson C, Friesen N. Introduction. In: Friesen N, Henriksson C, Saevi T, editors. Hermeneutic phenomenology in education. Sense; 2012. pp. 1–17.
Goldie JGS, Connectivism. A knowledge learning theory for the digital age? Med Teach. 2016;38(10):1064–9.
Braun V, Clarke V. Thematic analysis: a practical guide. SAGE Publications Ltd; 2021.
Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills, California: SAGE; 1985.
Book Google Scholar
Nowell LS, Norris JM, White DE, Moules NJ. Thematic analysis: striving to meet the trustworthiness criteria. 2017;16:1–13.
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for Reporting Qualitative Research: Acad Med. 2014;89(9):1245–51.
PubMed Google Scholar
Freitas FA, Leonard LJ. Maslow’s hierarchy of needs and student academic success. Teach Learn Nurs. 2011;6(1):9–13.
Maslow AH. Motivation and personality. 3rd ed. New York: Longman; 1954.
MacArthur KR, Sikorski J. A qualitative analysis of the coping reservoir model of pre-clinical medical student well-being: human connection as making it worth it. BMC Med Educ. 2020;20(1):1–11.
Simpson V, Halpin L, Chalmers K, Joynes V. Exploring well-being: medical students and staff. Clin Teach. 2019;16(4):356–61.
Rich A, Viney R, Silkens M, Griffin A, Medisauskaite A. UK medical students’ mental health during the COVID-19 pandemic: a qualitative interview study. BMJ Open. 2023;13:e070528.
Bakker AAB, Demerouti E. Job demands-resources theory: taking stock and looking forward. J Occup Health Psychol. 2017;22(3):273–85.
Riley R, Kokab F, Buszewicz M, Gopfert A, Van Hove M, Taylor AK et al. Protective factors and sources of support in the workplace as experienced by UK foundation and junior doctors: a qualitative study. BMJ Open. 2021;11(6).
Greenmyer JR, Montgomery M, Hosford C, Burd M, Miller V, Storandt MH, et al. Guilt and burnout in medical students. Teach Learn Med. 2021;34(1):69–77.
Ayala EE, Omorodion AM, Nmecha D, Winseman JS, Mason HRC. What do medical students do for self-care? A student-centered approach to well-being. Teach Learn Med. 2017;29(3):237–46.
Wurth S, Sader J, Cerutti B, Broers B, Bajwa MN, Carballo S, et al. Medical students’ perceptions and coping strategies during the first wave of the COVID-19 pandemic: studies, clinical implication, and professional identity. BMC Med Educ. 2021;21(1):620.
Bu F, Steptoe A, Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31–4.
Arslan G, Loneliness C, Belongingness. Subjective vitality, and psychological adjustment during coronavirus pandemic: development of the college belongingness questionnaire. J Posit Sch Psychol. 2021;5(1):17–31.
Maben J, Taylor C, Dawson J, Leamy M, McCarthy I, Reynolds E et al. A realist informed mixed-methods evaluation of Schwartz center rounds in England. Heal Serv Deliv Res. 2018;6(37).
Monk A, Hind D, Crimlisk H. Balint groups in undergraduate medical education: a systematic review. Psychoanal Psychother. 2018;8734:1–26.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132–49.
Heath C, Sommerfield A, Von Ungern-Sternberg BS. Resilience strategies to manage psychological distress among healthcare workers during the COVID-19 pandemic: a narrative review. Anaesthesia. 2020;75(10):1364–71.
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(92).
Smedley RM, Coulson NS. A practical guide to analysing online support forums. Qual Res Psychol. 2021;18(1):76–103.
Download references
Acknowledgements
We would like to thank Dr P Byrne for providing guidance, Mrs A Threlfall and Professor VCT Goddard-Fuller for commenting on drafts, and the medical students who participated in the webinars.
This study was unfunded.
Author information
Authors and affiliations.
Department of Psychology, University of Liverpool, Eleanor Rathbone Building, Bedford Street South, Liverpool, L69 7ZA, UK
Helen M West
Liverpool University Hospitals NHS Foundation Trust, Liverpool, UK
School of Medicine, University of Liverpool, Liverpool, UK
Rowan M Davies, Benjamin Shelley & Oscar T Edginton
Salford Royal NHS Foundation Trust, Manchester, UK
Rowan M Davies
Calderdale and Huddersfield NHS Foundation Trust, West Yorkshire, UK
Benjamin Shelley
Leeds Teaching Hospitals NHS Foundation Trust, Leeds, UK
Oscar T Edginton
You can also search for this author in PubMed Google Scholar
Contributions
HMW conceptualised the study and collected the data. HMW, LF, RMD, BS and OTE conducted data analysis. HMW, LF, RMD and OTE wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Correspondence to Helen M West .
Ethics declarations
Ethical approval and consent to participate.
Approval was granted by the University of Liverpool Institute of Population Health Research Ethics Committee (Reference: 8365). Students were fully informed about the study prior to the workshop and had an opportunity to ask questions. Participants provided informed consent, completing an electronic consent form before responding to prompts. The study was conducted in accordance with relevant guidelines and regulations, including the University of Liverpool Research Ethics and Research Data Management Policies, and the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
West, H.M., Flain, L., Davies, R.M. et al. Medical student wellbeing during COVID-19: a qualitative study of challenges, coping strategies, and sources of support. BMC Psychol 12 , 179 (2024). https://doi.org/10.1186/s40359-024-01618-8
Download citation
Received : 12 December 2023
Accepted : 22 February 2024
Published : 28 March 2024
DOI : https://doi.org/10.1186/s40359-024-01618-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Mental wellbeing
- Medical student
- Student doctor
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]

IMAGES
COMMENTS
As highlighted in previous research on college students' academic stress, preparing exams, courses, and papers should exhibit a negative effect on individual health. During the COVID-19 outbreak, Chinese college students' learning was not suspended, but they attend the various courses offered online follow the regular schedule.
Mental well-being and test anxiety among students preparing for the university admission exam during the pandemic. Eleyza Yatkin, 1 Neriman Aral, 2 Lugen Ceren Gunes, 3 , * , † and Selim Tosun ... Evaluation of anxiety disorder and post-trauma stress disorder related to the covid-19 pandemic in parents of children with primary ...
It is no surprise that undergraduate students are under great distress—or the discomforting, emotional psychological response to a particular stressor (Ridner, 2004)—during the novel coronavirus (COVID-19) pandemic.The pandemic has had far-reaching academic consequences, an early one for undergraduates being the need to rapidly modify their learning contexts away from in-person supports.
Abbott (2021) investigated stress caused by the COVID-19 pandemic and its related consequences and found that there is an increase in prevalence of stress, anxiety, and depression in the U.S. population from 11% to 42% due to this pandemic. The surge in stress among people is also during the rise of new COVID-19 covariant cases.
As highlighted in previous research on college students' academic stress, preparing exams, courses, and papers should exhibit a negative effect on individual health. During the COVID-19 outbreak, Chinese college students' learning was not suspended, but they attend the various courses offered online follow the regular schedule.
Hence, coping strategy plays a significant mediating role between exam anxiety and academic stress (Estimate = 0.133, P = 0.009). Therefore, it can be concluded that from the mediation of the coping strategy the impact of exam anxiety on academic stress is decreased. Hence, H5 is accepted at a 1% significance level. 5.
In this study, around one third of students from Faculties of Medical Sciences reported stress with remote E-exams during the Covid-19 pandemic. The main factors related to students' stress include exam duration, navigation mode and technical problems. Other factors include concern that teaching methods have not properly covered the material ...
Purpose The Covid-19 pandemic has brought unprecedented stress to students and educational institutions across the world. We aimed to estimate the effect of the pandemic on the mental health of college students. Methods We used data on 419 first-year students (ages 18-20) at a large public university in North Carolina both before (October 2019-February 2020) and after (June/July 2020) the ...
Furthermore, the major factors related to study habits and exams that are significantly associated with the level of academic stress were difficulty in remembering all that is studied (66.7%, P=0.006), worrying about the exams (54.1%, P=0.011), exam papers are tough and do not value well (23.8%, P=0.001), and the exams are too difficult ...
The COVID-19 pandemic has changed the functioning of universities worldwide. In Poland, the transfer to online teaching was announced without prior warning, which radically changed students' daily functioning. This situation clearly showed the students' helplessness and difficulties with coping with this new, stressful situation, highlighted in many previous studies. A sudden and far ...
As a research focused on student stress patterns during COVID-19, the study aims to address the following research questions (RQs): (a) the most prolific authors and affiliates in publications; (b) trends in keywords and novelty in future research on student stress during COVID-19; (c) potential for post-COVID-19 school curriculum development. 2.
And there are ways to lessen your stress. HOW TO COPE. PRACTICE SELF-CARE. Basic self-care will keep your immune system strong and your emotional reserves full. Get enough sleep. Exercise regularly. Eat well. Try mindfulness apps. Find activities that engage different parts of yourself.
The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic. The student suffered from a lack of internet access and other online learning challenges. Students who dealt with problems registering for or taking standardized tests and AP exams. Jeff Schiffman of the Tulane University admissions ...
March 22, 2021. SHARE: PRINT. High school students are experiencing rising stress levels and lower engagement with learning since the start of the COVID-19 pandemic, according to a new study by NBC News and Challenge Success, a nonprofit affiliated with Stanford Graduate School of Education (GSE). Kids feel that "they are more stressed than ...
Stress reappraisal and mindset interventions have high potential to assist in stress management during the COVID‐19 pandemic based on their demonstrated efficacy in laboratory and selected applied contexts (Crum et al., 2013, 2017; Keech et al., 2019). Research demonstrating that such interventions are highly translatable and have consistent ...
The prevalence of depression, anxiety, physical discomfort, insomnia and post-traumatic stress disorder (PTSD) during the COVID-19 pandemic: Having a childbearing age: During the COVID/19 pandemic, pregnant women had lower scores of symptoms of depression, anxiety, and PTSD (all p < 0.05) compared to non-pregnant women. Sade et al., 2020
The first step to lower your stress is to keep a daily schedule. Make or maintain healthy habits and routines. This can help boost your mood and energy levels. Make sleep a priority. Get up at about the same time every day. Go to bed at about the same time every day. Make sure that you are getting enough restful sleep.
Play with puzzles, a board game, do a treasure hunt, tackle a project, reorganize something, or start a new book that is unrelated to coronavirus coverage. Connect with others. "I can't stress ...
Stress management is an effective way to lead a healthy and a stress-free life! Continue Reading to discover strategies to manage stress during exams below. 10 Pointers to Write Exam Stress Management Strategies During COVID-19 Essay in English . Managing exam stress is often a difficult job for school students.
Trauma Due to COVID-19 Exposure. Studies of frontline health care workers during the COVID-19 pandemic have shown that rates of trauma-related symptoms, depression, and anxiety have increased ...
While social and traditional media discussed work-related stress and burnout during the COVID-19 pandemic, there was little empirical research to examine the phenomena except for a few high-level surveys (Brynjolfsson et al., 2020; Center for National Health Statistics, 2020; CVS Health, 2020; Petterson et al., 2020).Although the quickly forced shift to working from home was brought on by ...
For medical schools, the COVID-19 pandemic necessitated examination and curricular restructuring as well as significant changes to clinical attachments. With the available evidence suggesting that medical students' mental health status is already poorer than that of the general population, with academic stress being a chief predictor, such changes are likely to have a significant effect on ...
Background Medical students face challenges to their mental wellbeing and have a high prevalence of mental health problems. During training, they are expected to develop strategies for dealing with stress. This study investigated factors medical students perceived as draining and replenishing during COVID-19, using the 'coping reservoir' model of wellbeing. Methods In synchronous ...